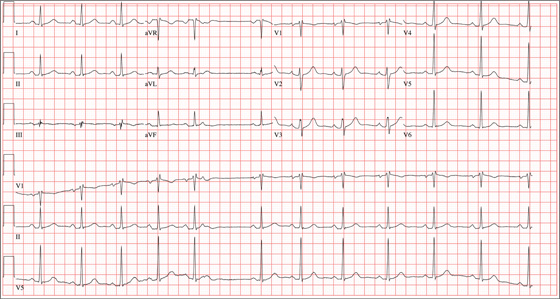
A 24-year-old graduate student presents to the student clinic with a history of palpitations. He first noticed them while snowboarding two months ago, but says they’re now occurring daily and much more frequently. He is concerned about the risk for “another” episode of tachycardia, which, through careful questioning, you learn he has experienced twice before. He recalls that each of the episodes—which occurred while he was “pulling all-nighters” for final exams during his undergrad years—began abruptly and lasted for approximately an hour. He had no chest pain, symptoms of near-syncope, or syncope, but recalls feeling very “jittery,” which he attributed to drinking a full pot of coffee while studying. The patient has no prior cardiac or pulmonary history and considers himself to be in excellent health. He has run two half-marathons in the preceding six months and is an avid snowboarder. He also competes in local road cycling competitions with reasonable success. Medical history is remarkable only for fractures of the right ankle and the left clavicle. He takes no medications and has no drug allergies. Family history is significant for stroke (paternal grandfather), diabetes (maternal grandmother), and hypertension (father). He consumes alcohol socially, primarily on weekends, and does not binge drink. He smokes marijuana during snowboard season but denies use at other times of the year. A 12-point review of systems is positive only for athlete’s foot and psoriasis on both upper extremities. The physical exam reveals a healthy, athletic-appearing male in no distress. Vital signs include a blood pressure of 126/68 mm Hg; pulse, 78 beats/min; respiratory rate, 14 breaths/min; and O2 saturation, 99% on room air. He is afebrile. His height is 70” and weight, 158 lb. Auscultation of the heart reveals no murmurs, rubs, or gallops, but you do detect several pauses. As you listen, he emphatically states, “There’s one … there’s another.” Following the physical exam, the patient asks you to order an ECG. The resultant tracing reveals the following: a ventricular rate of 70 beats/min; PR interval, 178 ms; QRS duration, 90 ms; QT/QTc interval, 402/434 ms; P axis, 23°, R axis, 38°; and T axis, 31°. What is your interpretation of this ECG?