Clinical Review

Endometriosis: Expert answers to 7 crucial questions on diagnosis
The notorious delay in diagnosis associated with this condition stems in part from its ability to mimic other diseases. The expert answers...
Jessica C. Francis, MD, and Jennifer E. Dietrich, MD, MSc
Dr. Francis is Assistant Professor and Associate Director, Residency Program, Department of Obstetrics and Gynecology, Medical College of Wisconsin, Milwaukee.
Dr. Dietrich is Chief, Pediatric and Adolescent Gynecology, Texas Children’s Hospital, Houston, and Division and Fellowship Director, Pediatric and Adolescent Gynecology, and Associate Professor, Departments of Obstetrics and Gynecology and Pediatrics, Baylor College of Medicine, Houston, Texas.
The authors report no financial relationships relevant to this article.
Developed in partnership with the North American Society for Pediatric and Adolescent Gynecology (NASPAG).

These adolescent health experts present 4 cases of acutely painful or nontender pelvic masses in patients aged 12 to 18, offering pearls for examination, diagnosis, and appropriate treatment
In this Article
Pelvic masses frequently are the reason for the medical evaluation of young women and girls. Regardless of what prompted the work-up that led to the mass’ discovery, the patient inevitably will be sent to a gynecologist for further evaluation, and such a practitioner should be involved whenever there is suspicion for a mass involving the reproductive tract.
While it does not happen often, it is possible that a mass diagnosed as ovarian, based on imaging, is then determined to be of another organ system at the time of surgery. Most frequently, this occurs with ruptured appendicitis, as the presence of an appendiceal abscess can mimic a complex ovarian mass or tubo-ovarian abscess (TOA).1
The full differential diagnosis of non-gynecologic pelvic masses is extensive and includes mesenteric duplication cysts, presacral masses, pelvic kidney, peritoneal inclusion cysts, and urachal cysts (TABLE). It can be difficult to distinguish pathology as gynecologic or nongynecologic even if a thorough work-up is performed.
Differential diagnosis for a pelvic mass
|
In this review, we offer several cases involving varying presentations of pelvic masses related to the reproductive tract.
Case 1: Severe pelvic pain in an 18-year-old
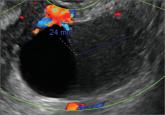
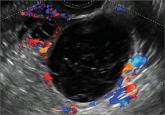
An 18-year-old adolescent presents to your office reporting worsening pelvic pain over the past 3 days. The pain is severe in the left lower quadrant. She reports a foul discharge and thinks she has a fever but hasn’t checked her temperature. She says she has been sexually active in the past few months with 2 different male partners. She has not been using condoms consistently and hasn’t been tested for sexually transmitted infections. Physical examination reveals a mucopurulent discharge at the cervix and copious white blood cells noted on wet mount. Bimanual examination reveals cervical motion tenderness and tenderness over the left adnexa. Ultrasound reveals a mass in the left adnexa with debris and internal echoes.
Diagnosis: Tubo-ovarian abscess.
Treatment: Admission to the hospital for intravenous antibiotic therapy.
It is important to note that TOAs can be seen in patients who have not been sexually active, as well as in cases related not to an ascending infection but rather to a history of pelvic surgery or complex structural anomaly.2 The majority of the time a TOA is a result of pelvic inflammatory disease (PID). Often, patients with uncomplicated PID can be treated on an outpatient basis if they meet strict criteria, but patients with a TOA need to be treated as an inpatient due to the severity of this infection.
Clinical pearl. If a patient has an IUD in place, close clinical follow up is critical to determine response to therapy. The Centers for Disease Control and Prevention’s sexually transmitted infection treatment guidelines state that removal of the IUD is not mandatory, but if the patient is not responding to treatment removal ultimately may be necessary. The IUD should be removed if there is no improvement in the patient’s symptoms with antibiotic therapy, there is no decrease in size of the TOA with antibiotic therapy, or if there is no positive test of cure after treatment for the TOA is completed.
If a patient has progressive abdominal pain and other findings consistent with infectious etiology, consider that a ruptured appendix could have a very similar appearance to a TOA. Computed tomography can be a useful tool to aid in firm diagnosis in cases in which gastroenterologic entities must be ruled out, but ultimately the gold standard of diagnosis for both of these procedures is diagnostic laparoscopy. Diagnostic surgery can be performed if the patient does not respond to medical therapy. In an effort to avoid surgical intervention, interventional radiology may be an option to drain the TOA. If this is performed, it is useful to repeat the ultrasound to confirm resolution prior to removal of the drain.
Case 2: Acute-onset severe pelvic pain in a young adolescent
A 12-year-old girl presents to the emergency department with acute-onset right lower quadrant pain. She states that about 2 hours ago she was playing in the yard and suddenly doubled over with pain. She also has had nausea and vomiting since that time.
She is in obvious distress and is resting in the fetal position. Examination reveals normal vital signs and tenderness to palpation over the right lower pelvic quadrant. There is no palpable abdominal mass. Genital examination reveals Tanner stage 4 external genitalia with normal introitus and patent, intact, annular hymen.

The notorious delay in diagnosis associated with this condition stems in part from its ability to mimic other diseases. The expert answers...
In this commentary, Dr. Javier F. Magrina describes screening techniques that differentiate benign from malignant adnexal masses, and discusses...
Whether you scan the patient yourself or refer her to an ultrasonography lab, you need to be able to identify both physiologic and pathologic...
A 25-year-old patient presents with pelvic pain and dyspareunia. A 19-year-old patient with a history of ovarian cystectomy for dermoid cyst...
Myriad sonographic features characterize cystic adnexal pathology. Here, three cases of benign, resolving cysts, including when to follow-up.
