Clinical Review

Endometriosis: Expert answers to 7 crucial questions on diagnosis
The notorious delay in diagnosis associated with this condition stems in part from its ability to mimic other diseases. The expert answers...
Jessica C. Francis, MD, and Jennifer E. Dietrich, MD, MSc
Dr. Francis is Assistant Professor and Associate Director, Residency Program, Department of Obstetrics and Gynecology, Medical College of Wisconsin, Milwaukee.
Dr. Dietrich is Chief, Pediatric and Adolescent Gynecology, Texas Children’s Hospital, Houston, and Division and Fellowship Director, Pediatric and Adolescent Gynecology, and Associate Professor, Departments of Obstetrics and Gynecology and Pediatrics, Baylor College of Medicine, Houston, Texas.
The authors report no financial relationships relevant to this article.
Developed in partnership with the North American Society for Pediatric and Adolescent Gynecology (NASPAG).

Sex cord−stromal tumors also are relatively common in the pediatric population.16 Of these, granulosa cell tumors are the most common and account for 2% to 5% of ovarian malignancies regardless of age at diagnosis. Juvenile-type granulosa ovarian cancers occur mainly in premenarchal girls and comprise roughly 5% of all granulosa cell tumors.17 The presenting problem usually is precocious puberty. Therefore, in any situation in which a prepubertal girl is developing too early and peripheral precocious puberty is suspected, sonography should be obtained to rule out a hormone-producing ovarian mass. Tumor markers most helpful in this situation include estradiol, testosterone, and inhibin B.17
When an adolescent is diagnosed with ovarian cancer, it is ideal to perform a fertility-sparing procedure whenever it is reasonable.18 While dermoid cysts can look concerning on sonography because of their heterogeneous appearance, the vast majority can be safely and effectively resected without oophorectomy in order to preserve fertility, as in most cases they are benign. Nonetheless, cystectomy does have a small, theoretic risk of cyst rupture, with the potential for pelvic peritonitis from dermoid content spillage.19 In the vast majority of cases in which a benign adnexal mass is identified, ovarian cystectomy is appropriate and oophorectomy is not indicated.20
Another very rare presentation of mature cystic teratoma can include acute neurologic decline in cases of paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis. Frequently, these teratomas will be small in size and discovered only incidentally during the work-up of a patient with altered mental status. Resection is indicated as soon as possible to stop the neurologic decline.21
Case 4: Cyclic pelvic pain and a pelvic mass in a 16-year-old
A 16-year-old adolescent presents to your office for evaluation of cyclic pelvic pain. She states that menarche occurred at age 12 years and menses have been irregular ever since, occurring every few months and associated with significant pain with the onset of bleeding.
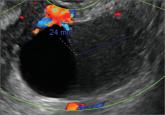
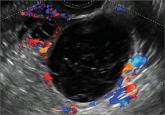
Physical examination reveals Tanner stage 4 breasts and Tanner stage 4 external genitalia. The introitus is normal with a visible intact, annular hymen. A mildly tender palpable mass at the level of the umbilicus is noted. The patient consents to having a Q-tip placed in the vagina, which reveals a bulge in the left vaginal wall that is nontender and fluctuant. Pelvic ultrasonography reveals uterine didelphys and an obstructed left hemivagina. A renal ultrasound reveals an absent left kidney.
Diagnosis: OHVIRA (obstructed hemivagina and ipsilateral renal anomaly) syndrome.
Treatment: Surgical resection of the vaginal septum.
Masses that appear complex on imaging can be deceiving, as they also can be related to obstructive reproductive tract anomalies. “Pelvic mass” is often the working diagnosis in cases of imperforate hymen, vaginal atresia, cervical agenesis, and uterine didelphys with obstructed hemivagina. This underscores the importance of taking an accurate menstrual history as well as performing a thorough physical examination. Usually this does not require an internal vaginal examination if the patient is unable to tolerate one, but a rectal examination can provide similar information in a patient presenting with a “pelvic mass” who will consent to this portion of the exam.
Clinical pearl. If a patient is not comfortable consenting to a rectal exam, a lubricated Q-tip can be used to palpate the vagina to minimize patient discomfort.
Before performing surgery…
Vaginal surgery can be corrective in the majority of these cases; however, magnetic resonance imaging is the gold standard for diagnosis and should be performed prior to surgical planning to further characterize the anomaly.22 Because Müllerian anomalies are associated with renal malformation such as absent kidney, pelvic kidney, collecting system duplication, or ectopic ureteral insertion around 40% of the time, imaging studies to assess for these structures is important prior to surgical intervention.23 If the patient is symptomatic and surgery cannot be performed immediately in a safe manner, she may require admission for pain control and placement of a Foley catheter (if the mass is obstructing urinary flow) until surgery can be performed safely.
A comprehensive review of Müllerian anomalies is beyond the scope of this article; it is important to note that these clinical scenarios are always unique and treatment should be individualized.
Conclusion
There are many sources of pelvic masses in children, adolescents, and young women; not all sources will be gynecologic. To avoid unnecessary surgical intervention, it is important to obtain as much information as possible from the patient’s history, physical examination, and laboratory and imaging studies.
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.

The notorious delay in diagnosis associated with this condition stems in part from its ability to mimic other diseases. The expert answers...
In this commentary, Dr. Javier F. Magrina describes screening techniques that differentiate benign from malignant adnexal masses, and discusses...
Whether you scan the patient yourself or refer her to an ultrasonography lab, you need to be able to identify both physiologic and pathologic...
A 25-year-old patient presents with pelvic pain and dyspareunia. A 19-year-old patient with a history of ovarian cystectomy for dermoid cyst...
Myriad sonographic features characterize cystic adnexal pathology. Here, three cases of benign, resolving cysts, including when to follow-up.
