Summary of guideline-based recommendations
Treatment guidelines published in the National Guidelines Clearinghouse address depression, CAD screening, and specific cardiac therapies, including ACE inhibitors, angiotensin-receptor blockers, oral anticoagulants, platelet inhibitors, beta blockers, and lifestyle modification.
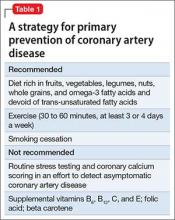
Primary prevention. Recommendations for treatment to prevent CAD are listed in Table 1.
Secondary prevention. Recommendations for treatment after a diagnosis of CAD are listed in Table 2.
Special considerations for psychiatric providers
You should be comfortable with patients’ use of antihypertensive therapies and familiar with the potential these agents have to interact with psychotropics; in addition, you can take a more active role in prescribing, and monitoring patients’ responses to, these medications. Provide appropriate monitoring of ACE inhibitors, statins, and beta blockers; also, provide appropriate monitoring of psychotropics in patients who take recommended cardioprotective medications.
In situations that prompt referral (such as recent MI, new symptoms of heart failure, any history of syncope or new identification of T2DM), ideally you should collaborate with the patient’s primary care provider to help enhance adherence to recommended treatment strategies. You also should employ motivational interviewing techniques and offer strategies by which patients can engage in meaningful lifestyle modification.
There are official recommendations for depression screening strategies26 and psychosocial risk screening for patients in whom CAD has been identified.27 Official screening strategies for CAD in patients with psychiatric illness have not, however, been spelled out.
Primary CAD prevention with medication is not routinely recommended for the general population, but the increased risk of CAD associated with psychiatric diagnoses (particularly schizophrenia, as well as the medications used to treat it) might warrant consideration of aggressive primary prevention strategies.28 For example, some experts recommend starting metformin to reduce the risk of T2DM in patients who have been started on olanzapine or clozapine, regardless of the baseline fasting blood glucose level.29
You should be fully informed and aware of patients’ underlying medical conditions and the medications that are recommended to treat their conditions. Ideally, an integrated care strategy or, at the least, clear communication between you and the patient’s primary care providers should be in place to avoid foreseeable problems.
Stimulants. Systematic reviews suggest an association between prescription stimulants and at least the 2 cardiovascular risk factors of elevated heart rate and blood pressure. Stimulants are not recommended, therefore, for routine use in patients who have known hypertension or CAD.30
Second-generation antipsychotics are associated with significant weight gain and development of metabolic syndrome.
Selective serotonin reuptake inhibitors are associated with an increased risk of gastrointestinal bleeding risk related to platelet inhibition and gastric effects. Risk increases with additional platelet inhibitors, such as aspirin or clopidogrel.31
Lithium is excreted solely by the kidney. Guidelines recommend ACE inhibitors and angiotensin receptor-blockers for patients with CAD or T2DM, and many patients with symptomatic congestive heart failure are prescribed a diuretic; all of these classes of medications impair excretion of lithium. In a nested case-control study, 3% of observed cases of lithium toxicity were attributable to a newly initiated ACE inhibitor or angiotensin receptor-blocker.32 It is essential that you, and your patients taking lithium, be aware of the need to monitor the drug level frequently and be vigilant for symptoms of mild toxicity.
Beta blockers. No prospectively collected data support a association between beta blockers and depression.33 Patients with CAD should be given a trial of a beta blocker to achieve optimal medical management; because they are at increased risk of depression in the first place, all patients with CAD should undergo monitoring for depressive symptoms.
Clopidogrel is activated through the cytochrome P450 2C19 isoenzyme; medications such as fluoxetine and fluvoxamine that inhibit the function of CYP2C19 can impair the effectiveness of clopidogrel.31
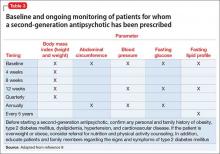
Other considerations. Patients taking a second-generation antipsychotic should have baseline and periodic (monthly for the first quarter, then quarterly) assessments of BMI and, after monitoring at 3 months after baseline, annual monitoring of blood pressure, the fasting glucose level, and abdominal waist circumference. Lipid levels should be monitored every 5 years9 (Table 3).
Baseline and periodic monitoring of hepatic enzymes is recommended for patients taking a statin. You, and the patient, should be alert to the possible development of muscle weakness or pain; establish a low threshold for screening for an elevated creatine kinase level, which signals rhabdomyolysis.
Case concluded
Ms. S’s psychiatrist measures her blood pressure and finds that it is 147/92 mm Hg. He uses the Pooled Cohort Equations to determine that her lifetime risk of cardiovascular event is 50% (compared with a 8% lifetime risk among a cohort in whom risk factors are optimized) and that her 10-year risk is 41% (compared with a 2.2% risk among optimized controls).