User login
Up the Creek Without a Provider
ANSWER
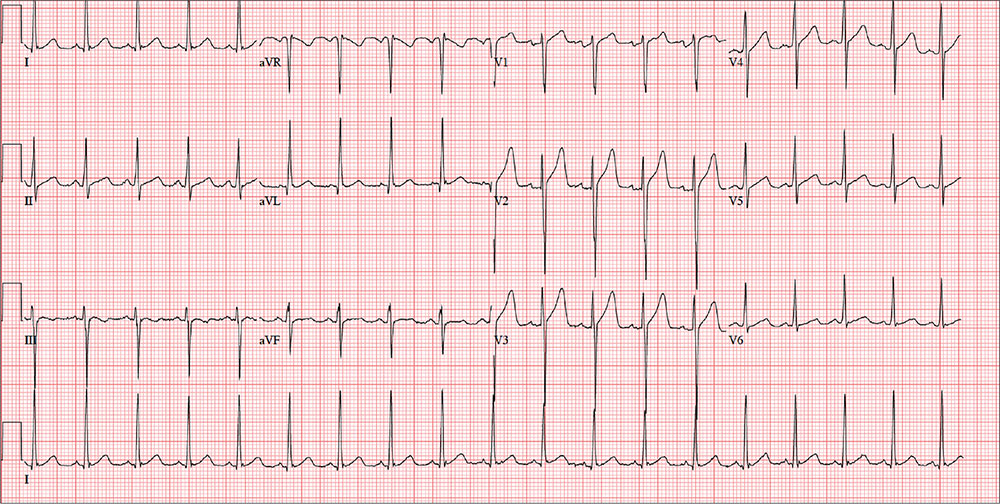
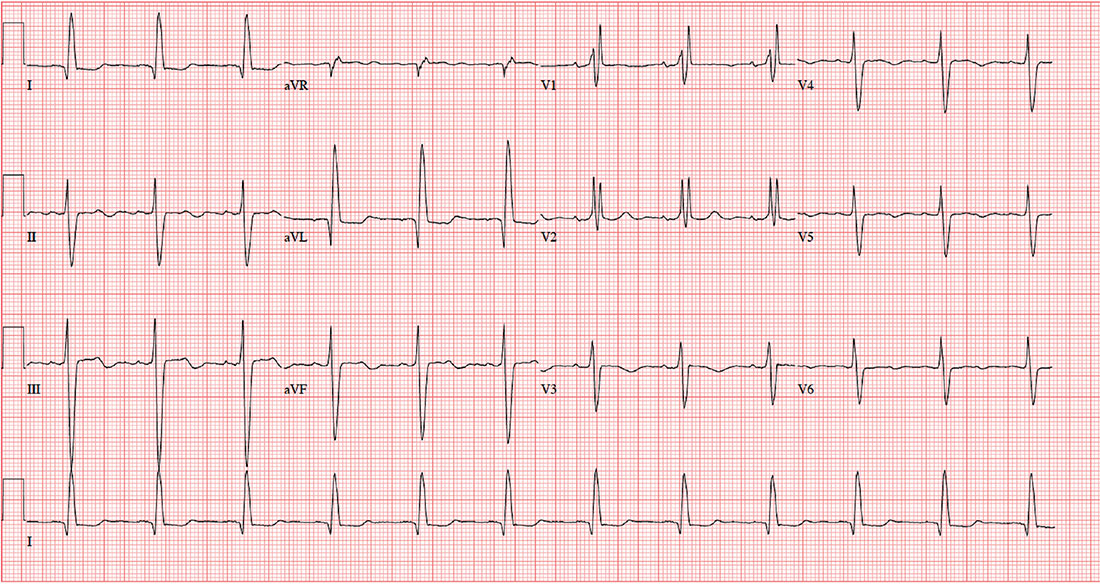
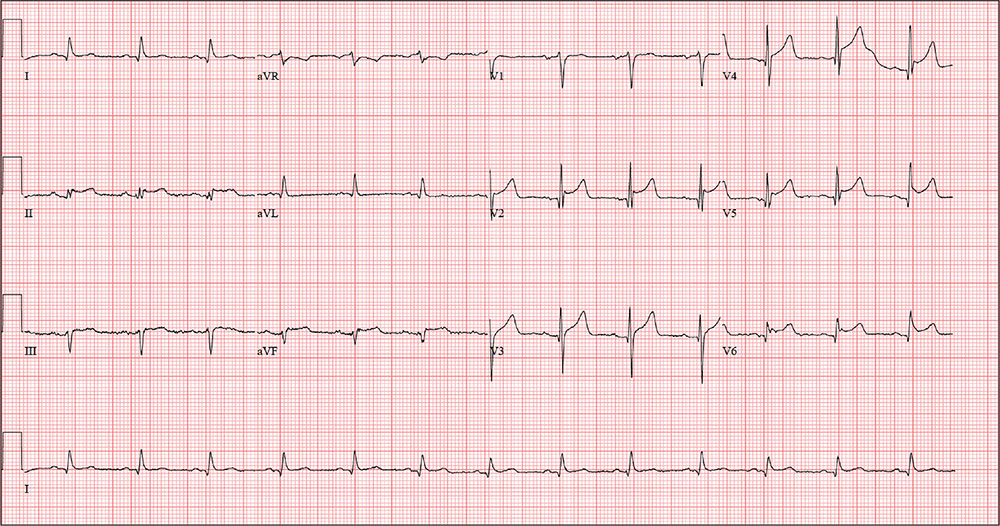
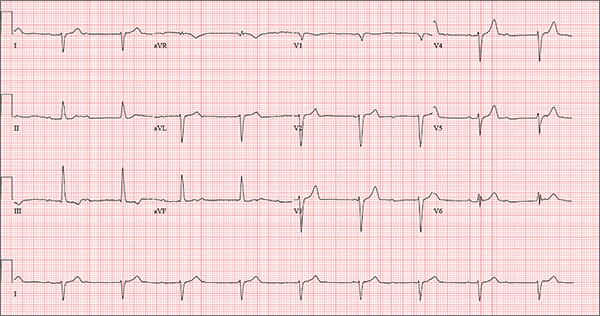
The ECG is remarkable for sinus tachycardia and left ventricular hypertrophy. Equal numbers of P and QRS complexes with a consistent PR interval indicate sinus tachycardia. High voltages in the limb leads (R in lead I and S in lead III ≥ 25 mm) or precordial leads (S in lead V1 and R in lead V5 or V6 ≥ 35 mm) constitute left ventricular hypertrophy.
ANSWER
The ECG is remarkable for sinus tachycardia and left ventricular hypertrophy. Equal numbers of P and QRS complexes with a consistent PR interval indicate sinus tachycardia. High voltages in the limb leads (R in lead I and S in lead III ≥ 25 mm) or precordial leads (S in lead V1 and R in lead V5 or V6 ≥ 35 mm) constitute left ventricular hypertrophy.
ANSWER
The ECG is remarkable for sinus tachycardia and left ventricular hypertrophy. Equal numbers of P and QRS complexes with a consistent PR interval indicate sinus tachycardia. High voltages in the limb leads (R in lead I and S in lead III ≥ 25 mm) or precordial leads (S in lead V1 and R in lead V5 or V6 ≥ 35 mm) constitute left ventricular hypertrophy.
A 40-year-old man presents to establish care with you as his primary care provider; he was recently forced to make this change because his prior network stopped accepting his insurance policy. He works as an electrical engineer and is a competitive rower. He began rowing at age 14; he was on his university’s team and now rows in a competitive, age-matched league.
He has never had any health-related issues, apart from sprained ankles and a fractured right clavicle in childhood. He exercises daily at an exclusive men’s club. He has no history of hypertension, diabetes, hyperlipidemia, chest pain or discomfort, shortness of breath, or exertional dyspnea. He has no surgical history.
The patient is single and
He is not taking any medications and has no known drug allergies. The review of systems is remarkable only for recent rhinitis, which is resolving.
Vital signs include a blood pressure of 124/60 mm Hg; pulse, 110 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. His weight is 194 lb and his height, 75 in.
The physical exam reveals a mildly anxious male in no acute distress. When asked if he is nervous, he says yes, because he’s “used to having someone else examine him.” His HEENT exam is normal, as is his thyroid exam. He has no jugular venous distention. The lungs are clear bilaterally. His heart rate is 110 beats/min and regular with no murmurs, rubs, or gallops. The abdomen is soft and nontender, with no palpable organomegaly. Peripheral pulses are strong and equal bilaterally, and there is no peripheral edema. The neurologic exam is grossly intact.
Routine blood tests are performed, and an HIV titer, ECG, and chest x-ray are ordered. The ECG reveals a heart rate of 112 beats/min; PR interval, 132 ms; QRS duration, 76 ms; QT/QTc interval, 326/444 ms; P axis, 59°; R axis, –8°; T axis, 26°. What is your interpretation of this ECG?
Pilot Has a Flighty Heart
ANSWER
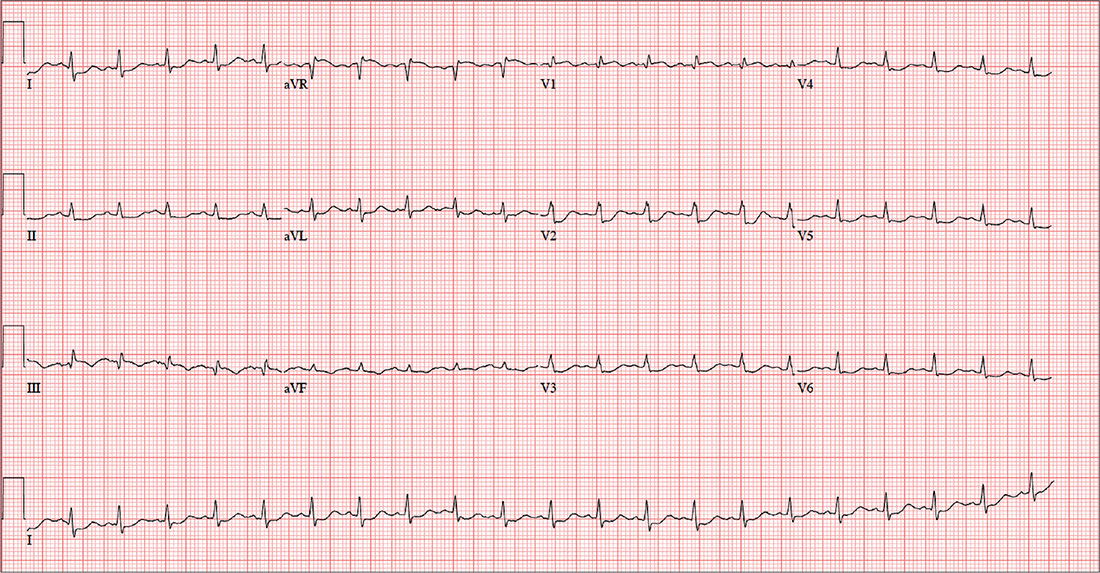
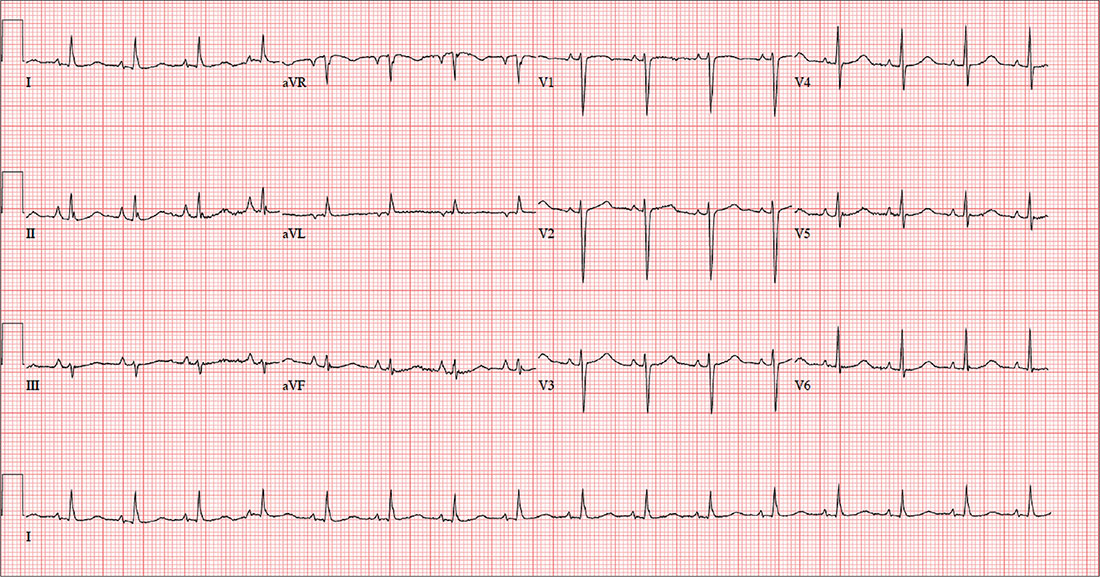
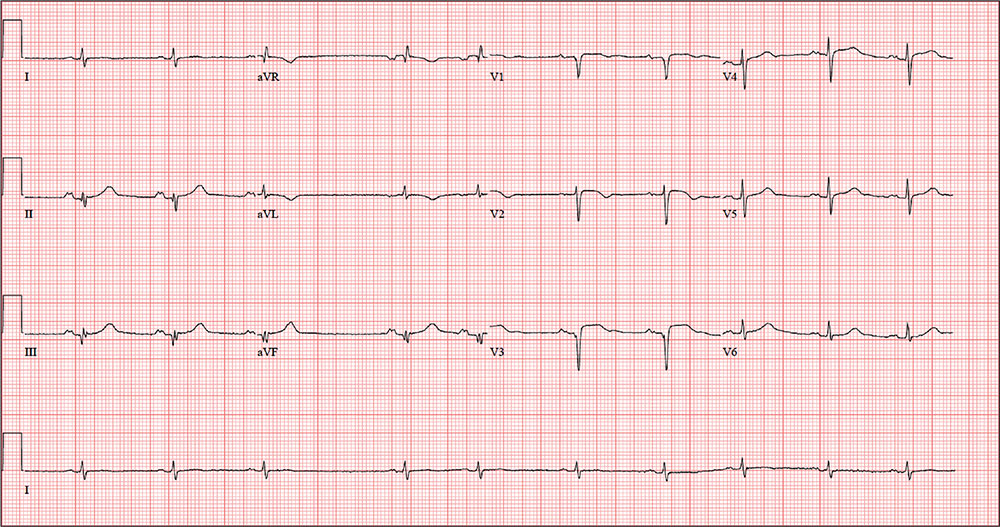
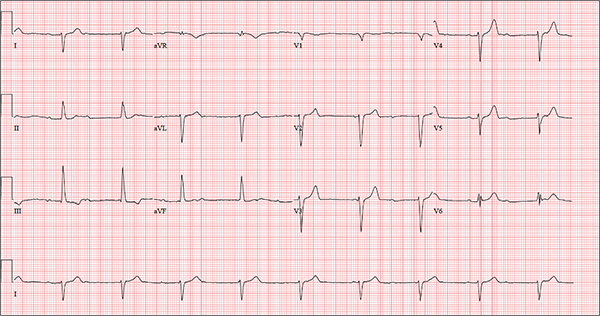
This ECG is consistent with sinus tachycardia, low-voltage QRS complexes, a posterior infarction, and ST- and T-wave abnormalities suggestive of inferior ischemia.
Sinus tachycardia is evidenced by the equal number of P and QRS complexes with a consistent PR interval. QRS complexes of lower amplitude than one would expect for the patient’s body habitus are deemed low voltage.
A posterior infarct is demonstrated by an R wave with no S wave in V1. Additionally, leads V2 and V3 show a pattern of a dominant R wave wit
Finally, inferior ischemia is identified by ST depressions in anterolateral leads I, aVL, V5, and V6, and T-wave inversions in inferior leads III and aVF.
ANSWER
This ECG is consistent with sinus tachycardia, low-voltage QRS complexes, a posterior infarction, and ST- and T-wave abnormalities suggestive of inferior ischemia.
Sinus tachycardia is evidenced by the equal number of P and QRS complexes with a consistent PR interval. QRS complexes of lower amplitude than one would expect for the patient’s body habitus are deemed low voltage.
A posterior infarct is demonstrated by an R wave with no S wave in V1. Additionally, leads V2 and V3 show a pattern of a dominant R wave wit
Finally, inferior ischemia is identified by ST depressions in anterolateral leads I, aVL, V5, and V6, and T-wave inversions in inferior leads III and aVF.
ANSWER
This ECG is consistent with sinus tachycardia, low-voltage QRS complexes, a posterior infarction, and ST- and T-wave abnormalities suggestive of inferior ischemia.
Sinus tachycardia is evidenced by the equal number of P and QRS complexes with a consistent PR interval. QRS complexes of lower amplitude than one would expect for the patient’s body habitus are deemed low voltage.
A posterior infarct is demonstrated by an R wave with no S wave in V1. Additionally, leads V2 and V3 show a pattern of a dominant R wave wit
Finally, inferior ischemia is identified by ST depressions in anterolateral leads I, aVL, V5, and V6, and T-wave inversions in inferior leads III and aVF.
For the past six hours, a 58-year-old man has been experiencing substernal chest discomfort. He is a commercial airline pilot for a regional carrier. Earlier today, he served as co-pilot on a roundtrip flight; about one hour before take-off, he started to feel a dull aching sensation in his chest that he attributed to his recently diagnosed gastroesophageal reflux disease (GERD). After landing, he purchased antacids in the airport terminal and took several, which provided only mild relief for the return trip. The pilot in command suggested he “get checked out” to make certain he didn’t have a bleeding ulcer.
Upon arrival at your facility, the patient appears uncomfortable but denies pain in his chest; there is no radiation to the neck, back, or arm. He denies palpitations, nausea, vomiting, diarrhea, and constipation. He says he feels more short of breath now than he did earlier, adding that “something just doesn’t feel right.”
The patient is a widower; his wife died of breast cancer at age 40. His daughter and son-in-law live in the same neighborhood so he can be close to his grandson. An avid triathlon participant, he has his own gym at home.
His medical history is remarkable for GERD, which was confirmed two months ago by upper endoscopy following several episodes of epigastric pain. He was prescribed a proton pump inhibitor, which he has forgotten to take for the past two days. His last flight physical, performed one year ago, was normal. Surgical history is remarkable for a tonsillectomy and a left inguinal hernia repair, both during childhood.
His current medication list includes lansoprazole and ibuprofen (as needed for musculoskeletal pain). He does not smoke, and he occasionally has a beer on the weekends when he isn’t working. The review of systems is noncontributory apart from his previously detailed symptoms.
Vital signs include a blood pressure of 130/86 mm Hg; pulse, 128 beats/min; respiratory rate, 12 breaths/min-1; and temperature, 97.9°F. His weight is 189 lb and his height, 73 in.
Physical exam reveals an uncomfortable, anxious-appearing male who is otherwise in excellent physical shape. Pertinent findings include a normal thyroid, no evidence of jugular venous distention, and clear lung fields bilaterally. The cardiac exam reveals a regular rate of 130 beats/min with no evidence of murmurs or rubs. The abdomen is flat and nontender, with no organomegaly. Peripheral pulses are equal bilaterally, and there is no peripheral edema. The neurologic exam is grossly intact.
A chest x-ray, ECG, and bloodwork are obtained. The ECG reveals a ventricular rate of 128 beats/min; PR interval, 136 ms; QRS duration, 72 ms; QT/QTc interval, 326/475 ms; P axis, 44°; R axis, 40°; and T axis, –47°. The ECG obtained during his flight physical one year ago showed normal sinus rhythm with nonspecific ST- and T-wave changes but was otherwise normal. With this history in mind, what is your interpretation of today’s ECG?
When Heart Problems Crop Up
ANSWER
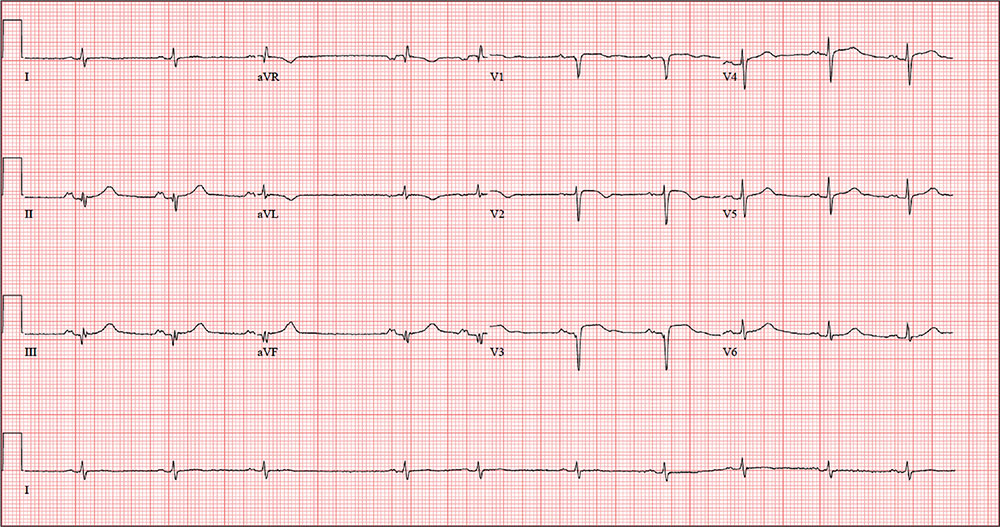
This ECG shows a sinus rhythm with premature atrial complexes, a normal axis, a right bundle branch block, and T-wave abnormalities consistent with lateral ischemia.
Sinus rhythm is evidenced by the P waves’ rate of ≥ 60 beats/min and ≤ 100 beats/min. The P waves that indicate premature atrial contractions have a different appearance than normal P waves, a result of the atrial activation from a site other than the sinus node. Because both the normal P wave and the premature atrial contraction conduct through the normal ventricular conduction system, the associated QRS complexes are identica
A right bundle branch block is identified by a QRS duration > 120 ms with a terminal broad S wave in lead I and an RSR’ complex in leads V1 and V2. The ST segment depressions in precordial leads V3 through V6 propagate the diagnosis of lateral ischemia.
The patient was not found to have atrial fibrillation, and his palpitations and evidence of lateral ischemia resolved when he resumed taking his ß-blocker.
ANSWER
This ECG shows a sinus rhythm with premature atrial complexes, a normal axis, a right bundle branch block, and T-wave abnormalities consistent with lateral ischemia.
Sinus rhythm is evidenced by the P waves’ rate of ≥ 60 beats/min and ≤ 100 beats/min. The P waves that indicate premature atrial contractions have a different appearance than normal P waves, a result of the atrial activation from a site other than the sinus node. Because both the normal P wave and the premature atrial contraction conduct through the normal ventricular conduction system, the associated QRS complexes are identica
A right bundle branch block is identified by a QRS duration > 120 ms with a terminal broad S wave in lead I and an RSR’ complex in leads V1 and V2. The ST segment depressions in precordial leads V3 through V6 propagate the diagnosis of lateral ischemia.
The patient was not found to have atrial fibrillation, and his palpitations and evidence of lateral ischemia resolved when he resumed taking his ß-blocker.
ANSWER
This ECG shows a sinus rhythm with premature atrial complexes, a normal axis, a right bundle branch block, and T-wave abnormalities consistent with lateral ischemia.
Sinus rhythm is evidenced by the P waves’ rate of ≥ 60 beats/min and ≤ 100 beats/min. The P waves that indicate premature atrial contractions have a different appearance than normal P waves, a result of the atrial activation from a site other than the sinus node. Because both the normal P wave and the premature atrial contraction conduct through the normal ventricular conduction system, the associated QRS complexes are identica
A right bundle branch block is identified by a QRS duration > 120 ms with a terminal broad S wave in lead I and an RSR’ complex in leads V1 and V2. The ST segment depressions in precordial leads V3 through V6 propagate the diagnosis of lateral ischemia.
The patient was not found to have atrial fibrillation, and his palpitations and evidence of lateral ischemia resolved when he resumed taking his ß-blocker.
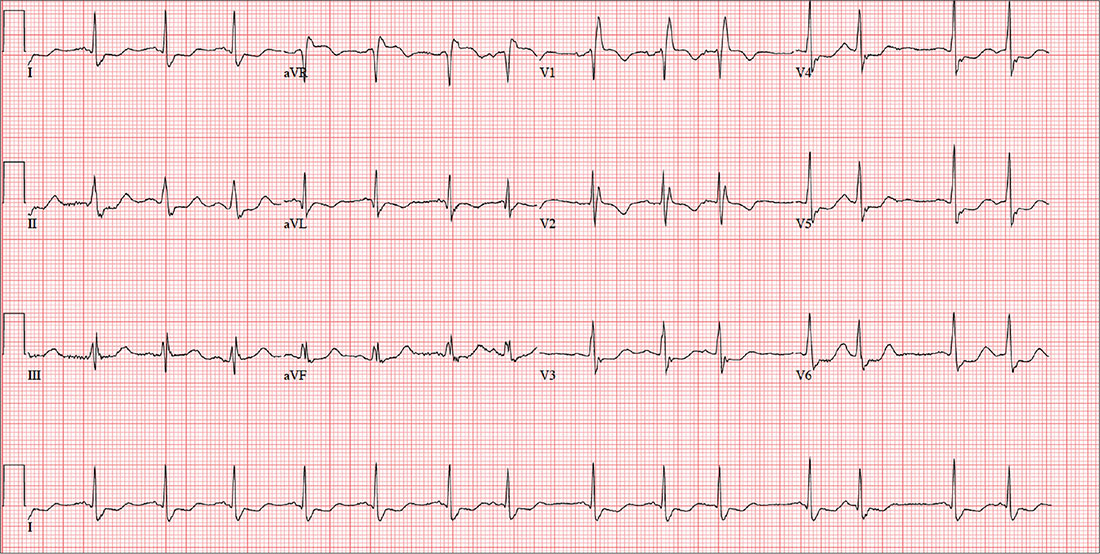
A 72-year-old farmer presents with heart palpitations he has had for the past three weeks. He fears he may be in atrial fibrillation and at risk for a stroke, stating that a few months ago his neighbor complained of palpitations (later attributed to atrial fibrillation) and had an embolic stroke due to a clot in the left atrium. The patient denies any history of cardiac arrhythmias, chest pain, syncope, or near-syncope. He does report occasional bouts of lightheadedness, which have increased in frequency. He is more concerned, though, by the strong, intensified heartbeats that he can feel in his throat.
Past medical and surgical histories are positive for type 2 diabetes, hypertension, and hyperlipidemia, as well as an appendectomy and cholecystectomy. He has also had several upper extremity fractures in the past, all of which have healed well.
The patient’s wife died recently from complications following a hip replacement surgery, but he and his two sons continue to work on the 460-acre family farm he has owned all his life. A chronic smoker, he has smoked one to two packs of cigarettes per day since he was 15. He does not drink alcohol but does consume one to two pots of coffee per day.
His medication list includes metformin, atorvastatin, and metoprolol. He hasn’t taken his metoprolol for two months, because he switched pharmacies and the pills he received were a different color so he didn’t believe they were the right drug (despite the label on the bottle). He has no known drug allergies, but sulfa drugs induce nausea.
The review of systems is remarkable for arthritic pain in his hands, shoulders, hips, knees, and ankles. The patient complains of gastric reflux and occasional diarrhea. He states his mood is still down from the loss of his wife, but he denies being depressed.
His weight is 232 lb and his height, 70 in. Vital signs include a blood pressure of 168/92 mm Hg; pulse, 84 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 99.2°F.
Physical exam reveals a weathered but otherwise healthy-looking male in no distress. He wears corrective lenses. The HEENT exam reveals surprisingly good dentition for a man his age. There are no carotid bruits. The lungs have expiratory crackles in both bases that change with coughing.
The cardiac exam reveals an irregular rate of 88 beats/min with a grade II/VI early systolic murmur at the left upper sternal border. There are no extra heart sounds or rubs. The abdomen is soft and nontender with old, well-healed cholecystectomy and appendectomy incision scars. The peripheral pulses are strong and equal bilaterally. Arthritic changes are evident in the hands and feet. The neurologic exam is grossly intact.
An ECG is performed; it reveals a ventricular rate of 87 beats/min; PR interval, 156 ms; QRS duration, 138 ms; QT/QTc interval, 440/529 ms; P axis, 58°; R axis, 26°; and T axis, 105°. What is your interpretation of this ECG?
Bury My Heart at Wounded Knee
ANSWER
The correct diagnosis includes normal sinus rhythm with a left-axis deviation, right bundle branch block, and left anterior fascicular block, consistent with bifascicular block.
Left-axis deviation is evidenced by an axis beyond –30°. A right bundle branch block is marked by a QRS duration > 120 ms, an RSR’ pattern in lead V1 and often V2 and V3, and wide S waves in lateral leads V5 and V6.
A left anterior fascicular block is identified by a left-axis deviation beyond –45°, a QR complex in lead I, and an RS complex in leads II and III.
The combination of a right bundle and left anterior fascicular block constitute bifascicular block. In this case, only the left fascicle conducts normally, putting this patient at risk for trifascicular block (ie, third-degree or complete heart block).
ANSWER
The correct diagnosis includes normal sinus rhythm with a left-axis deviation, right bundle branch block, and left anterior fascicular block, consistent with bifascicular block.
Left-axis deviation is evidenced by an axis beyond –30°. A right bundle branch block is marked by a QRS duration > 120 ms, an RSR’ pattern in lead V1 and often V2 and V3, and wide S waves in lateral leads V5 and V6.
A left anterior fascicular block is identified by a left-axis deviation beyond –45°, a QR complex in lead I, and an RS complex in leads II and III.
The combination of a right bundle and left anterior fascicular block constitute bifascicular block. In this case, only the left fascicle conducts normally, putting this patient at risk for trifascicular block (ie, third-degree or complete heart block).
ANSWER
The correct diagnosis includes normal sinus rhythm with a left-axis deviation, right bundle branch block, and left anterior fascicular block, consistent with bifascicular block.
Left-axis deviation is evidenced by an axis beyond –30°. A right bundle branch block is marked by a QRS duration > 120 ms, an RSR’ pattern in lead V1 and often V2 and V3, and wide S waves in lateral leads V5 and V6.
A left anterior fascicular block is identified by a left-axis deviation beyond –45°, a QR complex in lead I, and an RS complex in leads II and III.
The combination of a right bundle and left anterior fascicular block constitute bifascicular block. In this case, only the left fascicle conducts normally, putting this patient at risk for trifascicular block (ie, third-degree or complete heart block).
A 72-year-old man with chronic osteoarthritis is scheduled for left knee replacement and sent for preoperative assessment. He has been physically active his entire life, but in the past five years, both knees have developed osteoarthritis that prevents him from walking more than 20 feet without stopping. He is obese and has hyperlipidemia and type 2 diabetes. He has never had angina, shortness of breath, paroxysmal dyspnea, or hypertension.
The patient is retired after 27 years’ service in the Air Force followed by an 18-year career with a major airline. He is married, with three adult children who are all in good health. He quit smoking at age 35 but states half-seriously that he “gave up cigarettes for candy bars and ice cream.” He says he drank heavily during his early years of service but rarely has more than one or two beers per week now.
Medical and surgical histories are remarkable for multiple arthroscopic procedures involving the medial meniscus and anterior collateral ligament of both knees. He has also had xanthelasmas removed from both eyelids, surgical repair of a compound fracture of the left humerus, and shrapnel removed from the subcutaneous tissue on the left upper back.
His medication list includes atorvastatin and metformin. He is allergic to sulfa, which has induced anaphylaxis in the past.
The review of systems reveals he is hard of hearing; he has hearing aids but refuses to wear them. He wears trifocal glasses and a partial upper bridge. He denies any cardiac, pulmonary, neurologic, or gastrointestinal problems. He does report difficulty starting and stopping a stream of urine, as well as occasional accidents. He also admits to having erectile dysfunction but does not think it is a problem he needs to address.
Vital signs include a blood pressure of 124/74 mm Hg; pulse, 70 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. His weight is 264 lb and his height, 69 in. He is pleasant, cooperative, alert, and oriented.
Physical exam reveals normal heart sounds without murmurs, clicks, or rubs. The lungs are clear in all fields. The abdomen is large but soft, and the liver edge is palpable 3 cm below the costal margin. Peripheral pulses are 2+ bilaterally in all extremities. Surgical scars are present on the left humerus, left scapula, and both knees. Neurologically, the patient is intact, and there is no evidence of microvascular disease secondary to his diabetes.
An ECG is performed. It reveals a ventricular rate of 71 beats/min; PR interval, 152 ms; QRS duration, 142 ms; QT/QTc interval, 476/517 ms; P axis, 76°; R axis, –48°; and T axis, 161°. What is your interpretation of this ECG?
Chest Pain Numbs Holiday Cheer
ANSWER
The correct interpretation includes normal sinus rhythm and right atrial enlargement. The latter is suggested by tall P waves in leads II, III, and aVF (typically ≥ 2.5 mm), which may be caused by pressure or volume overload of the right atrium or by conditions causing pulmonary hypertension.
Given this patient’s presentation of right-side chest pain with a history of COPD, smoking, palpable left saphenous vein, and right atrial enlargement, a chest CT was performed. It confirmed the suspicion of a pulmonary embolus.
ANSWER
The correct interpretation includes normal sinus rhythm and right atrial enlargement. The latter is suggested by tall P waves in leads II, III, and aVF (typically ≥ 2.5 mm), which may be caused by pressure or volume overload of the right atrium or by conditions causing pulmonary hypertension.
Given this patient’s presentation of right-side chest pain with a history of COPD, smoking, palpable left saphenous vein, and right atrial enlargement, a chest CT was performed. It confirmed the suspicion of a pulmonary embolus.
ANSWER
The correct interpretation includes normal sinus rhythm and right atrial enlargement. The latter is suggested by tall P waves in leads II, III, and aVF (typically ≥ 2.5 mm), which may be caused by pressure or volume overload of the right atrium or by conditions causing pulmonary hypertension.
Given this patient’s presentation of right-side chest pain with a history of COPD, smoking, palpable left saphenous vein, and right atrial enlargement, a chest CT was performed. It confirmed the suspicion of a pulmonary embolus.
A 64-year-old woman presents with nondescript pain throughout her right chest. One week ago, she developed aching in both lower extremities, worse in the left leg than in the right. Two days ago, she noticed a tender area on her lower left leg that “feels like a hard rope.” She denies constitutional symptoms and changes in bowel or bladder habits.
Initial history-taking produces only the vague response that she’s “had my share of medical problems” through the years. A review of the electronic medical record reveals a history of chronic obstructive pulmonary disease (COPD), tobacco use, and recurrent community-acquired pneumonia—as well as a pattern of missed appointments. Her most recent visit was five years ago.
On further questioning, the patient informs you that she was shocked for a rapid heartbeat in the past year, following a weekend of binge-drinking on a cruise. She also reveals that she has increased her per-day cigarette habit from one to 2.5 packs to “deal with the stress of the holidays.” However, she reports no changes in her respiratory status or her “usual” productive morning cough. She denies shortness of breath, as well as any history of hypertension, diabetes, thyroid disorder, or cardiac-related chest pain.
The patient has been divorced for 11 years. Her job keeps her on the road between eight and 10 hours a day. She drinks alcohol on the weekend—anywhere from one six-pack to an entire case of beer. She began smoking at age 13 and hasn’t stopped since, refusing any offers of smoking cessation. She tried marijuana a few years ago but “didn’t like” how it made her feel. She denies using illicit or prescription drugs.
Family history reveals that the patient’s parents and both sets of grandparents were chronic smokers. Her paternal grandfather died of complications from emphysema, her maternal grandfather of asbestosis, and both grandmothers of strokes. Her parents are alive and reside in an assisted living facility. Her mother is being treated for colon cancer, and her father has had two myocardial infarctions. She had one brother who died in a motorcycle accident at age 15.
Her height is 69 in and her weight, 142 lb. Vital signs include a blood pressure of 152/94 mm Hg; pulse, 90 beats/min; respiratory rate, 16 breaths/min-1; and temperature, 97.2°F.
On physical exam, the patient appears older than her stated age but is in no distress. The HEENT exam is significant for corrective lenses, stained teeth, and leukoplakia on the oral mucosa. Neck veins are elevated, with a prominent A wave present. There is no thyromegaly or carotid bruits. The lungs reveal coarse rhonchi bilaterally in all lung fields, with no significant changes with coughing. The cardiac rate is regular with no evidence of a murmur or rub. Peripheral pulses are strong and equal bilaterally in both upper and lower extremities. The abdominal exam shows no evidence of organomegaly or masses, and the abdominal aorta is easily palpable. There is no edema in the lower extremities; however, a palpable cord is present along the entire length of the left greater saphenous vein. The neurologic exam is grossly intact without focal signs.
In addition to routine laboratory specimens, a chest x-ray and ECG are obtained. The ECG shows a ventricular rate of 96 beats/min; PR interval, 126 ms; QRS duration, 80 ms; QT/QTc interval, 384/485 ms; P axis, 79°; R axis, 18°; and T axis, 63°. What is your interpretation of this ECG?
A Stroke of Bad (Pot)luck
ANSWER
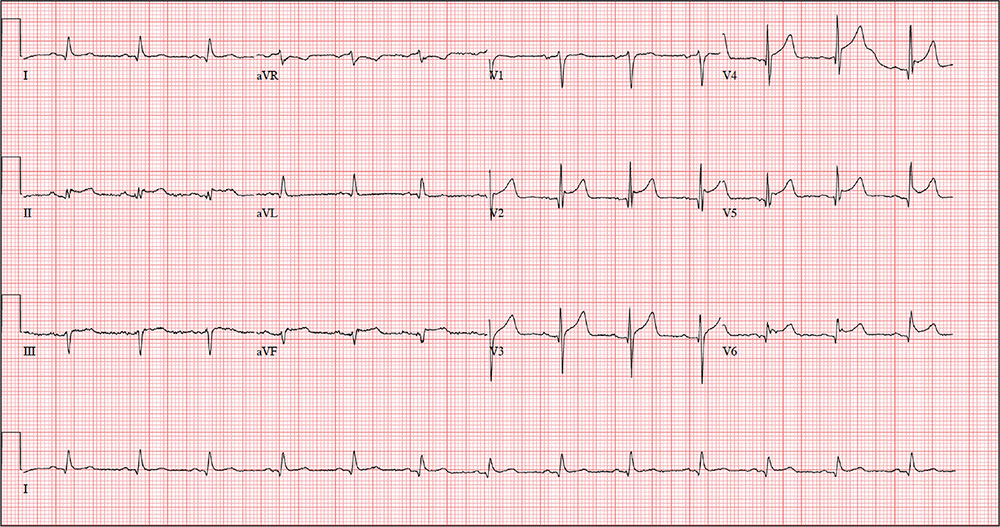
The correct interpretation includes normal sinus rhythm, acute ST elevation anterior myocardial infarction (STEMI), and inferolateral injury. Sinus rhythm is signified by a P wave for every QRS complex and a QRS complex for every P wave at a rate between 60 and 100 beats/min.
A STEMI is defined as new ST elevations at the J point in at least two contiguous leads—in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. The anterior location is evidenced by the significant Q waves in leads I, V2, V3, and V4. T-wave inversions in these leads are absent due to the STEMI.
Inferolateral injury is identified by the Q waves in leads I, aVL, V5, and V6. Pseudo Q waves are seen in leads II, III, and aVF.
Troponin levels were significant for an acute myocardial infarction (MI). Cardiac cauterization confirmed an occlusion of the proximal left anterior descending coronary artery, and significant stenosis of the first obtuse marginal branch of the circumflex coronary artery. The patient’s lack of chest pain represents a common presentation of an MI in women, particularly those with a history of diabetes.
ANSWER
The correct interpretation includes normal sinus rhythm, acute ST elevation anterior myocardial infarction (STEMI), and inferolateral injury. Sinus rhythm is signified by a P wave for every QRS complex and a QRS complex for every P wave at a rate between 60 and 100 beats/min.
A STEMI is defined as new ST elevations at the J point in at least two contiguous leads—in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. The anterior location is evidenced by the significant Q waves in leads I, V2, V3, and V4. T-wave inversions in these leads are absent due to the STEMI.
Inferolateral injury is identified by the Q waves in leads I, aVL, V5, and V6. Pseudo Q waves are seen in leads II, III, and aVF.
Troponin levels were significant for an acute myocardial infarction (MI). Cardiac cauterization confirmed an occlusion of the proximal left anterior descending coronary artery, and significant stenosis of the first obtuse marginal branch of the circumflex coronary artery. The patient’s lack of chest pain represents a common presentation of an MI in women, particularly those with a history of diabetes.
ANSWER
The correct interpretation includes normal sinus rhythm, acute ST elevation anterior myocardial infarction (STEMI), and inferolateral injury. Sinus rhythm is signified by a P wave for every QRS complex and a QRS complex for every P wave at a rate between 60 and 100 beats/min.
A STEMI is defined as new ST elevations at the J point in at least two contiguous leads—in women, 1.5 mm in leads V2 and V3 and 1 mm in all other leads; in men, 2 mm (those 40 and older) or 2.5 mm (those younger than 40) in leads V2 and V3 and 1 mm in all other leads. The anterior location is evidenced by the significant Q waves in leads I, V2, V3, and V4. T-wave inversions in these leads are absent due to the STEMI.
Inferolateral injury is identified by the Q waves in leads I, aVL, V5, and V6. Pseudo Q waves are seen in leads II, III, and aVF.
Troponin levels were significant for an acute myocardial infarction (MI). Cardiac cauterization confirmed an occlusion of the proximal left anterior descending coronary artery, and significant stenosis of the first obtuse marginal branch of the circumflex coronary artery. The patient’s lack of chest pain represents a common presentation of an MI in women, particularly those with a history of diabetes.
An active 74-year-old woman becomes nauseated and diaphoretic while cleaning up her church’s Sunday evening potluck. She shrugs it off, attributing it to something she ate, but while preparing to go home, she abruptly becomes short of breath and complains she can’t catch her breath. Two coworkers describe her appearance as pale with “complete loss of color” and insist on driving her to the local emergency department (ED).
When she arrives 10 minutes later, her shortness of breath is resolving. She denies chest pain, vomiting, and diarrhea. Despite receiving oxygen via nasal cannula, she still appears pale. An ECG and laboratory tests are ordered.
The patient’s medical history is remarkable for type 2 diabetes, hypothyroidism, obesity, and hypertension. Her surgical history is remarkable for a cholecystectomy and a hysterectomy 40 years ago, following the delivery of her third child.
The patient is a retired elementary school principal. She drinks alcohol socially and has never smoked. She lost her husband to colon cancer several years ago and now lives by herself in her home. She has three adult children who are all alive and well. Her mother died of heart failure, and her father was killed in an automobile accident.
Her current medication list includes metformin, levothyroxine, and hydrochlorothiazide. She states she has tried other medications for her diabetes and hypertension but prefers her current regimen. She is allergic to radiographic contrast media, with a documented near-anaphylactic reaction in the past.
Physical exam reveals a pleasant, cooperative, but apprehensive woman who appears her stated age. She wears corrective lenses and bilateral hearing aids. Her neck veins are not distended, and there is no evidence of thyromegaly. Respirations are rapid and shallow, with few crackles in both bases bilaterally but no rhonchi or rales. Her cardiac exam reveals a regular rate and rhythm with a soft, grade II, mid-systolic murmur at the left upper sternal border without radiation. There are no extra heart sounds or rubs. The abdomen is soft and nontender with well-healed surgical scars. The peripheral pulses are full and equal in both upper and lower extremities. The neurologic exam is grossly intact.
The review of systems shows that she has gained 14 pounds over the past four months, has been less physically active, and feels like she is “slowing down.” She also says her hearing and eyesight aren’t what they used to be, and she has chronic constipation. The remainder of her review of systems is unremarkable.
The patient’s weight is 218 lb and her height, 64 in. Vital signs include a blood pressure of 148/
110 mm Hg; pulse, 80 beats/min and regular; O2 saturation, 98% on 4 L O2 via nasal prongs; and respiratory rate, 20 breaths/min-1.
An ECG is obtained, and blood specimens for labwork—including a complete chemistry profile, complete blood count, thyroid function studies, and troponin levels—are collected. The ECG shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc intervals, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of this ECG?
Euphoric Man, Offbeat Rhythm
ANSWER
This ECG shows atrial fibrillation with aberrancy and a rapid ventricular response, left-axis deviation, and a left bundle branch block (LBBB).
While the physical exam can identify atrial fibrillation with a rapid ventricular response, an ECG is necessary to determine left-axis deviation and LBBB.
Left-axis deviation is evidenced by an R axis of –36°.
Aberrancy is identified by a QRS duration > 120 ms with poor R wave progression in precordial leads V1 to V3 and a wide positive R wave in V5 and V6.
Of note, the 10th beat on the rhythm strip is narrow and complex and is not aberrantly conducted.
ANSWER
This ECG shows atrial fibrillation with aberrancy and a rapid ventricular response, left-axis deviation, and a left bundle branch block (LBBB).
While the physical exam can identify atrial fibrillation with a rapid ventricular response, an ECG is necessary to determine left-axis deviation and LBBB.
Left-axis deviation is evidenced by an R axis of –36°.
Aberrancy is identified by a QRS duration > 120 ms with poor R wave progression in precordial leads V1 to V3 and a wide positive R wave in V5 and V6.
Of note, the 10th beat on the rhythm strip is narrow and complex and is not aberrantly conducted.
ANSWER
This ECG shows atrial fibrillation with aberrancy and a rapid ventricular response, left-axis deviation, and a left bundle branch block (LBBB).
While the physical exam can identify atrial fibrillation with a rapid ventricular response, an ECG is necessary to determine left-axis deviation and LBBB.
Left-axis deviation is evidenced by an R axis of –36°.
Aberrancy is identified by a QRS duration > 120 ms with poor R wave progression in precordial leads V1 to V3 and a wide positive R wave in V5 and V6.
Of note, the 10th beat on the rhythm strip is narrow and complex and is not aberrantly conducted.
A 70-year-old man recently diagnosed with prostate cancer is undergoing preoperative assessment for prostate surgery. His cardiac history is remarkable for longstanding hypertension, which has been well-managed with diuretics and a ß-blocker. Three years ago, he developed exertional angina. He underwent stress testing, was started on isosorbide dinitrate, and has had no further episodes.
He also has chronic obstructive pulmonary disease (COPD) due to chronic smoking, and sleep apnea for which he uses a continuous positive airway pressure (CPAP) device at night.
At age 24, he had an appendectomy for a ruptured appendix. The patient’s surgical history also includes bilateral total knee replacements (seven and eight years ago) and a laparoscopic cholecystectomy (converted to an open procedure due to adhesions) three years ago.
The patient is a retired mail carrier, a widower, and one of the most active members in his retirement community. Each night, he drinks one to two glasses of Scotch, and he has smoked one pack of cigarettes every day since he was 16. He has no interest in breaking either habit.
Family history reveals a father and mother who succumbed to myocardial infarction. His older brother died of complications following surgery, and his sister died of breast cancer.
The patient’s current medication list includes hydrochlorothiazide, metoprolol, and isosorbide dinitrate. He is allergic to sulfa, with a documented anaphylactic reaction in early adulthood. During the review of systems, he mentions that his heart has been “thumping” irregularly off and on for the past couple of months, corresponding with the expiration of his metoprolol prescription. He decided to wait for his preoperative assessment to have it refilled.
Vital signs include a blood pressure of 130/84 mm Hg; pulse, 110 beats/min and irregular; and temperature, 97.8°F.
On physical exam, his weight is 234 lb and his height, 69 in. He is a pleasant, euphoric male in no distress. He wears corrective lenses and hearing aids. Pertinent physical findings include crackles in both lower lung fields that clear with coughing; an irregularly irregular heart rhythm with an occasional early systolic murmur heard at the left upper sternal border; multiple old abdominal surgical scars; and surgical scars consistent with bilateral knee replacements. He is neurologically intact.
An ECG reveals a ventricular rate of 110 beats/min; QRS duration, 144 ms; QT/QTc interval, 298/403 ms; P axis, unmeasurable; R axis, –36°; T axis, 169°. What is your interpretation?
His Head Is In the Game–His Heart, Not So Much
ANSWER
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V2 to V6 and hyperacute ST-T wave changes. V1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.
ANSWER
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V2 to V6 and hyperacute ST-T wave changes. V1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.
ANSWER
The correct interpretation includes normal sinus rhythm with a new anterior myocardial infarction (MI) and inferolateral injury.
Criteria for an anterior MI include Q waves in leads V2 to V6 and hyperacute ST-T wave changes. V1 is usually spared.
Inferolateral injury is evidenced by the presence of Q waves and absence of R waves in leads III and aVF.
The patient’s cardiac catheterization revealed left anterior descending and circumflex artery disease.
While playing in a company racquetball tournament, a 47-year-old man suddenly collapses. He is unresponsive, without a pulse, and his coworkers immediately initiate CPR. A single shock from an on-site AED successfully resuscitates him from ventricular fibrillation. Paramedics arrive within 12 minutes, by which time the patient is conscious and responsive to commands.
During transportation to the emergency department, however, he develops ventricular tachycardia and loses consciousness; a single shock cardioverts him to normal sinus rhythm. An ECG is ordered and the cardiac catheterization team mobilized.
While waiting, you contact the patient’s wife by telephone. She tells you that her husband has been complaining of chest discomfort for the past week and woke up two nights ago with what he described as “indigestion.” She says she suggested he see a clinician, and he agreed to do so—but not until after the tournament.
His medical history is remarkable only for chronic gastroesophageal reflux disease (GERD), for which he takes chewable antacids on a daily basis. He has no prior cardiac or pulmonary history. There is no surgical history apart from a tonsillectomy in childhood.
The patient is the Chief Operating Officer at a local manufacturing facility. He is married and has three children. His parents and grandparents are alive and in good health, aside from some arthritis in the older generation.
The review of systems, obtained from his wife, is noncontributory. She says he is in excellent health—he jogs, rides mountain bikes, and enjoys racquetball. Her husband attributed his recent chest discomfort to GERD; when she asked if it could be cardiac related, he adamantly denied the possibility, as he was in “excellent health” with “good genes.”
Vital signs include a blood pressure of 118/56 mm Hg; pulse, 80 beats/min; respiratory rate, 18 breaths/min-1; and O2 saturation, 100% on 2 L oxygen. He is afebrile.
Physical exam reveals a thin, otherwise healthy male who appears anxious and apprehensive. He denies ongoing chest pain but states that his chest wall is sore beneath the defibrillator pads. A focal exam reveals normal lung sounds and a regular rate and rhythm with no murmurs, gallops, or rubs. The abdomen is soft and nontender. All peripheral pulses are strong and equal bilaterally, and there are no focal neurologic signs.
The ECG taken at admission shows a ventricular rate of 80 beats/min; PR interval, 162 ms; QRS duration, 106 ms; QT/QTc interval, 370/426 ms; P axis, 51°; R axis, –20°; and T axis, 70°. What is your interpretation of the ECG?
Man Shovels Path to Angina
ANSWERThe correct interpretation includes sinus rhythm with blocked premature atrial complexes, left-axis deviation, and serial changes of an evolving anterior MI.
The presence of a P wave without a QRS between the third and fourth QRS complex represents a blocked premature atrial complex. The fifth QRS complex also indicates a premature atrial complex; however, it is not blocked.
Left-axis deviation is evidenced by the R axis of –82°. The loss of an R wave in V1, the poor R-wave progression in V2 and V3, and the ST-T wave changes are all consistent with an evolving anterior MI.
ANSWERThe correct interpretation includes sinus rhythm with blocked premature atrial complexes, left-axis deviation, and serial changes of an evolving anterior MI.
The presence of a P wave without a QRS between the third and fourth QRS complex represents a blocked premature atrial complex. The fifth QRS complex also indicates a premature atrial complex; however, it is not blocked.
Left-axis deviation is evidenced by the R axis of –82°. The loss of an R wave in V1, the poor R-wave progression in V2 and V3, and the ST-T wave changes are all consistent with an evolving anterior MI.
ANSWERThe correct interpretation includes sinus rhythm with blocked premature atrial complexes, left-axis deviation, and serial changes of an evolving anterior MI.
The presence of a P wave without a QRS between the third and fourth QRS complex represents a blocked premature atrial complex. The fifth QRS complex also indicates a premature atrial complex; however, it is not blocked.
Left-axis deviation is evidenced by the R axis of –82°. The loss of an R wave in V1, the poor R-wave progression in V2 and V3, and the ST-T wave changes are all consistent with an evolving anterior MI.
While shoveling gravel several days ago, a 62-year-old man developed exertional angina. Though he stopped to rest, the pain persisted and radiated to his left arm. He called out for help, and his neighbor called 911. The patient was transported via ACLS ambulance to the hospital, where he ruled in for an anterior myocardial infarction (MI). Cardiac catheterization revealed left anterior descending coronary artery stenosis, which was treated with a drug-eluting stent.
One week after discharge, he presents for his first follow-up appointment. He is enrolled in a cardiac rehabilitation program but isn’t scheduled to start for another week. He has not experienced chest pain or discomfort following his MI, and he says he is diligently taking his ß-blocker and nitrates.
This retired Army (Airborne division) officer’s past surgical history is remarkable for multiple fractures in his lower extremities, sustained while skydiving. His past medical history is remarkable for malaria, yellow fever, and hepatitis. Prior to his MI, he had no history of cardiac disease or symptoms.
He is divorced and has no children. His parents are alive and well, with no known cardiac disease. His paternal grandfather died of a stroke associated with atrial fibrillation, but he does not know how his other grandparents died.
The patient was a smoker until five years ago. He consumes two or three glasses of Scotch per week, typically on the weekends. He denies recreational drug use and “doesn’t believe in” holistic or herbal medications.
Current medications include metoprolol, isosorbide dinitrate, and clopidogrel. He has no known drug allergies.
The review of systems is remarkable for fatigue, which he attributes to ß-blocker use. His right groin is sore following his interventional procedure, but the discomfort is resolving.
Vital signs include a blood pressure of 110/64 mm Hg; pulse, 60 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 97.6°F.
On physical exam, his weight is 224 lb and his height is 74 in. He is in good spirits and no distress. The HEENT exam is remarkable for corrective lenses. There is no evidence of thyromegaly or jugular venous distention. The lungs are clear; there are no murmurs, rubs, or gallops, and the abdomen is soft and nontender without organomegaly. The right groin has resolving ecchymosis and a small, palpable, organized hematoma. Peripheral pulses are strong bilaterally, and the neurologic exam is intact.
A follow-up ECG shows a ventricular rate of 61 beats/min; PR interval, 176 ms; QRS duration, 88 ms; QT/QTc interval, 402/404 ms; P axis, 71°; R axis, –82°; and T axis, 84°. What is your interpretation of the ECG?
An Exhausting Case of “Smoker’s Cough”
ANSWER
The correct interpretation includes sinus rhythm with complete heart block and a junctional rhythm, a rightward axis, and evidence of an anterior myocardial infarction (MI).
Sinus rhythm is evidenced by the regular rate and rhythm of the P waves.
Complete heart block is identified by the atrioventricular (AV) dissociation (QRS independent of the P wave), while the normal QRS duration—despite AV dissociation—confirms the existence of a junctional rhythm.
A positive R-wave axis slightly above the upper limit of normal, as seen with this patient, constitutes a rightward axis.
Finally, the posteriorly directed forces in the anterior precordial leads with poor R-wave progression denote an anterior MI.
ANSWER
The correct interpretation includes sinus rhythm with complete heart block and a junctional rhythm, a rightward axis, and evidence of an anterior myocardial infarction (MI).
Sinus rhythm is evidenced by the regular rate and rhythm of the P waves.
Complete heart block is identified by the atrioventricular (AV) dissociation (QRS independent of the P wave), while the normal QRS duration—despite AV dissociation—confirms the existence of a junctional rhythm.
A positive R-wave axis slightly above the upper limit of normal, as seen with this patient, constitutes a rightward axis.
Finally, the posteriorly directed forces in the anterior precordial leads with poor R-wave progression denote an anterior MI.
ANSWER
The correct interpretation includes sinus rhythm with complete heart block and a junctional rhythm, a rightward axis, and evidence of an anterior myocardial infarction (MI).
Sinus rhythm is evidenced by the regular rate and rhythm of the P waves.
Complete heart block is identified by the atrioventricular (AV) dissociation (QRS independent of the P wave), while the normal QRS duration—despite AV dissociation—confirms the existence of a junctional rhythm.
A positive R-wave axis slightly above the upper limit of normal, as seen with this patient, constitutes a rightward axis.
Finally, the posteriorly directed forces in the anterior precordial leads with poor R-wave progression denote an anterior MI.
One week ago, a 67-year-old African-American woman with a history of diabetes, hypertension, and smoking developed a nonproductive cough and chest discomfort. Over the past 24 hours, her symptoms have progressed, with increasing fatigue. She has delayed seeking care to spend time with visiting family, but this morning she calls for an appointment. At presentation, she describes her chest discomfort as a “vague, dull ache.” She denies sharp chest pain, radiation, syncope, near-syncope, and palpitations. She says her cough has resolved, aside from her usual early-morning “smoker’s cough.” However, she still experiences fatigue with exertion and must stop to rest after walking up one flight of stairs or about half a block on level ground. When asked about gardening, her favorite hobby, she tells you she stopped last week because she “didn’t have the energy” for it. Her medical history is remarkable for type 2 diabetes (for the past 10 years) and hypertension, for which she has been treated her entire adult life. She also has osteoarthritis. In the 20 years she has been in your patient panel, she has closely monitored her health and been vigilant about taking her medications. Her surgical history is remarkable for hysterectomy, cholecystectomy, and bilateral bunion resections. The patient retired two years ago after a 20-year career as a tax attorney. Her husband died of a myocardial infarction at age 56. She has two adult children, who also have hypertension. She has a 50–pack-year history of tobacco use and smokes up to one full pack of cigarettes per day. She denies alcohol and illicit drug use, aside from the occasional “nip” of brandy and infrequent marijuana use. Her medication list includes metformin, glyburide, hydrochlorothiazide, and lisinopril. She is allergic to sulfa. The review of systems is remarkable for hearing loss, diabetic neuropathy in both feet, and chronic loose stools. Vital signs include a blood pressure of 148/88 mm Hg—higher than measurements from her past three visits. Her pulse is 60 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.8°F. On physical exam, her weight is 201 lb and her height is 68 in; her weight has remained stable over the past two years. The HEENT exam findings include corrective lenses, bilateral hearing aids, and extensive dental work (including veneers). The neck is supple, without thyromegaly or jugular venous distention. The lungs are clear in all fields, apart from occasional crackles in both bases that clear with coughing. Her cardiac exam reveals a regular rate with no extra heart sounds or rubs, but a soft, early diastolic murmur at the left lower sternal border. The abdomen is soft and nontender with well-healed surgical scars and no palpable masses. Osteoarthritis is present in both hands, and her left hip has decreased range of motion, compared to her right. Peripheral pulses are strong bilaterally, and her neurologic exam is intact. You draw laboratory specimens and order a chest x-ray and ECG, which reveals a ventricular rate of 56 beats/min; PR interval, unmeasurable; QRS duration, 106 ms; QT/QTc interval, 400/386 ms; P axis, 36°; R axis, 120°; and T axis, 7°. What is your interpretation of this ECG?