User login
Ultrasound More Common at the Bedside
A recent “Current Concepts” article in the New England Journal of Medicine (2011;364:749) by a pair of Yale University physicians asserts that the day is close at hand when ultrasound interpretations by clinicians at the patient’s bedside will become as routine in hospital care as the trusty stethoscope. Ultrasound, a noninvasive form of imaging related to oceanographic sonar, has moved beyond its traditional home in radiology to myriad other medical specialties and practice areas. The technology has become smaller, less expensive, and higher in resolution in recent years, the authors note, adding that it has been used on Mount Everest and the international space station, as well as in battlefield situations.
“It’s becoming more accessible, and more training is available to physicians who aren’t radiologists,” says Diane Sliwka, MD, a hospitalist at the University of California at San Francisco (UCSF).
Dr. Sliwka says the NEJM article represents a milestone in the dissemination of bedside ultrasound. She conducts monthly faculty development training in procedural ultrasound at UCSF, workshops at HM and internal-medicine conferences, and training sessions for other hospitals.
The most common uses for bedside, “point of care” ultrasound include guiding procedures, such as thoracentesis and paracentesis, with improved safety over doing such insertions “blind.” Emerging procedural uses include lumbar puncture and arthrocentesis. Diagnostically, bedside ultrasound can provide quick screening and assessment, for example, of fluid buildup around the heart; previously, it could take hours to get the results from a formal heart study.
As with the stethoscope, Dr. Sliwka says, training in its correct use and scope of appropriate bedside practice is essential: “My advice is to learn from the experts at your facility, including the radiologists, critical care, or emergency physicians.” Ultrasound courses are increasing at hospitalist conferences, but space often is limited, and further supervised practice back home is needed.
The next step for hospitalists could be the definition of appropriate scope of practice, training, and competencies for its use. “Creating a niche in this area can be a nice change of pace from our traditional work as hospitalists,” Dr. Sliwka says. —LB
Technology
Video Chat Takes Off for Physicians
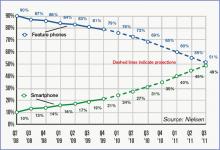
A recent study of digital adoption trends found that 7% of U.S. physicians now use video consultations to communicate with patients.
Manhattan Research’s 2011 “Taking the Pulse” survey of 2,000 physicians’ use of technology found that video chat is emerging as a way to consult with patients about nonurgent issues and follow-up questions or with geographically dispersed patients. Psychiatrists and oncologists are more likely to use the new technology. Doctors’ concerns regarding reimbursement, liability, and HIPAA privacy rules remain barriers to adoption.
For more information, visit ManhattanResearch.com/News-and-Events/Press-Releases/physician-patient-online-video-conferencing.—LB
Legal
Positive Outcomes from Full Disclosure of Medical Errors
The University of Michigan Health System’s (UMHS) risk-management model of full disclosure with offer of compensation for medical errors sparked hospitalist Allen Kachalia, MD, JD, of Brigham & Women’s Hospital in Boston to retrospectively study the outcomes of malpractice-claims-related performance before and after UMHS implemented the system in 2001.
Among the results Dr. Kachalia reported in his research abstract plenary at HM10, and subsequently published in Annals of Internal Medicine (2010;153(4):213-221), the mean monthly rate of new claims per 100,000 patient contacts decreased 36% after the full-disclosure model was adopted, while the rate of claims resulting in lawsuits declined by 65%. Claims also were resolved more quickly with the full-disclosure model.
Disclosure of medical error, Dr. Kachalia says, means “if someone is injured by medical care caused by medical error, the physician tells the patient they made the error, how it happened, and, often, what they’ll do to fix it.” An apology is somewhat different, he adds, and there’s no generic script for an apology. “What patients want is sincerity,” he says.
How can hospitalists work with full disclosure? “The general advice most institutions give is that when you want to disclose a medical error, first get your risk-management and patient-safety officers involved. They can help during every step of the process of investigating the event and disclosing,” Dr. Kachalia explains. “Assure patients that you are going to look into their concerns. Then make sure that a thorough investigation is done.”—LB
Practice Management
AMA-MGMA Toolkit Sorts Transitional-Care Software Options
HM practices with physicians in outpatient settings—be they discharge clinics or transitional-care centers—don’t always know how to determine the most useful practice-management software for their needs. So for those not helped by informatics staff, consider the new “Practice Management System Software Directory” from AMA and the Medical Group Management Association (MGMA).
The online repository, which launched in May, is a companion to the “Selecting a Practice Management System” toolkit the joint venture unveiled last fall. While the system is geared toward ambulatory-care settings, Robert Tennant, a senior policy advisor with MGMA, says any HM group with practitioners working on transitional care would find it useful.
Overall, the directory’s goal is to guide providers on how to navigate the increasingly complex world of practice-management options as new guidelines for “meaningful use” are defined, as well as new rules governing electronic claims processing. A new claims standard, known as HIPAA version 5010, is going live Jan. 1, 2012, so Tennant believes the directory is timely.
“It’s very difficult, whether in a practice or a hospital, to know the best software to pick,” he says. “There are plenty of vendors out there telling you they’re the best. There’s no easy way to comparison-shop.”
Now physicians can use the toolkit to measure basic functions. The directory, which will be updated on a rolling basis, will catalogue price range (excluding implementation costs), the number of installed customers, the target market for the product, what year the software was first offered, and whether the vendor also offers an electronic health record (EHR) system. That last point is of particular note to hospitalists as a link between practice management and medical records can help make a practice more efficient, Tennant says.
“What we’ve seen,” he adds, “is those that have that seamless integration between practice-management systems and EHR have higher productivity and higher levels of satisfaction.” —RQ
By The Numbers
$131,564
The average amount of money HM groups received in support per full-time equivalent (FTE) in fiscal year 2010, according to new SHM-MGMA survey data. The data point—the so-called “subsidy”—was first revealed at HM11 in Dallas.
After several years of leveling off at roughly $100,000, some hospitalists say they were surprised to see the figure rise so quickly. The report also shows that 19% of hospitalist practices receive no support, a finding that prompted new SHM President Joseph Li, MD, SFHM, to ask: “Are we looking at two business models or two care models?”—RQ
A recent “Current Concepts” article in the New England Journal of Medicine (2011;364:749) by a pair of Yale University physicians asserts that the day is close at hand when ultrasound interpretations by clinicians at the patient’s bedside will become as routine in hospital care as the trusty stethoscope. Ultrasound, a noninvasive form of imaging related to oceanographic sonar, has moved beyond its traditional home in radiology to myriad other medical specialties and practice areas. The technology has become smaller, less expensive, and higher in resolution in recent years, the authors note, adding that it has been used on Mount Everest and the international space station, as well as in battlefield situations.
“It’s becoming more accessible, and more training is available to physicians who aren’t radiologists,” says Diane Sliwka, MD, a hospitalist at the University of California at San Francisco (UCSF).
Dr. Sliwka says the NEJM article represents a milestone in the dissemination of bedside ultrasound. She conducts monthly faculty development training in procedural ultrasound at UCSF, workshops at HM and internal-medicine conferences, and training sessions for other hospitals.
The most common uses for bedside, “point of care” ultrasound include guiding procedures, such as thoracentesis and paracentesis, with improved safety over doing such insertions “blind.” Emerging procedural uses include lumbar puncture and arthrocentesis. Diagnostically, bedside ultrasound can provide quick screening and assessment, for example, of fluid buildup around the heart; previously, it could take hours to get the results from a formal heart study.
As with the stethoscope, Dr. Sliwka says, training in its correct use and scope of appropriate bedside practice is essential: “My advice is to learn from the experts at your facility, including the radiologists, critical care, or emergency physicians.” Ultrasound courses are increasing at hospitalist conferences, but space often is limited, and further supervised practice back home is needed.
The next step for hospitalists could be the definition of appropriate scope of practice, training, and competencies for its use. “Creating a niche in this area can be a nice change of pace from our traditional work as hospitalists,” Dr. Sliwka says. —LB
Technology
Video Chat Takes Off for Physicians
A recent study of digital adoption trends found that 7% of U.S. physicians now use video consultations to communicate with patients.
Manhattan Research’s 2011 “Taking the Pulse” survey of 2,000 physicians’ use of technology found that video chat is emerging as a way to consult with patients about nonurgent issues and follow-up questions or with geographically dispersed patients. Psychiatrists and oncologists are more likely to use the new technology. Doctors’ concerns regarding reimbursement, liability, and HIPAA privacy rules remain barriers to adoption.
For more information, visit ManhattanResearch.com/News-and-Events/Press-Releases/physician-patient-online-video-conferencing.—LB
Legal
Positive Outcomes from Full Disclosure of Medical Errors
The University of Michigan Health System’s (UMHS) risk-management model of full disclosure with offer of compensation for medical errors sparked hospitalist Allen Kachalia, MD, JD, of Brigham & Women’s Hospital in Boston to retrospectively study the outcomes of malpractice-claims-related performance before and after UMHS implemented the system in 2001.
Among the results Dr. Kachalia reported in his research abstract plenary at HM10, and subsequently published in Annals of Internal Medicine (2010;153(4):213-221), the mean monthly rate of new claims per 100,000 patient contacts decreased 36% after the full-disclosure model was adopted, while the rate of claims resulting in lawsuits declined by 65%. Claims also were resolved more quickly with the full-disclosure model.
Disclosure of medical error, Dr. Kachalia says, means “if someone is injured by medical care caused by medical error, the physician tells the patient they made the error, how it happened, and, often, what they’ll do to fix it.” An apology is somewhat different, he adds, and there’s no generic script for an apology. “What patients want is sincerity,” he says.
How can hospitalists work with full disclosure? “The general advice most institutions give is that when you want to disclose a medical error, first get your risk-management and patient-safety officers involved. They can help during every step of the process of investigating the event and disclosing,” Dr. Kachalia explains. “Assure patients that you are going to look into their concerns. Then make sure that a thorough investigation is done.”—LB
Practice Management
AMA-MGMA Toolkit Sorts Transitional-Care Software Options
HM practices with physicians in outpatient settings—be they discharge clinics or transitional-care centers—don’t always know how to determine the most useful practice-management software for their needs. So for those not helped by informatics staff, consider the new “Practice Management System Software Directory” from AMA and the Medical Group Management Association (MGMA).
The online repository, which launched in May, is a companion to the “Selecting a Practice Management System” toolkit the joint venture unveiled last fall. While the system is geared toward ambulatory-care settings, Robert Tennant, a senior policy advisor with MGMA, says any HM group with practitioners working on transitional care would find it useful.
Overall, the directory’s goal is to guide providers on how to navigate the increasingly complex world of practice-management options as new guidelines for “meaningful use” are defined, as well as new rules governing electronic claims processing. A new claims standard, known as HIPAA version 5010, is going live Jan. 1, 2012, so Tennant believes the directory is timely.
“It’s very difficult, whether in a practice or a hospital, to know the best software to pick,” he says. “There are plenty of vendors out there telling you they’re the best. There’s no easy way to comparison-shop.”
Now physicians can use the toolkit to measure basic functions. The directory, which will be updated on a rolling basis, will catalogue price range (excluding implementation costs), the number of installed customers, the target market for the product, what year the software was first offered, and whether the vendor also offers an electronic health record (EHR) system. That last point is of particular note to hospitalists as a link between practice management and medical records can help make a practice more efficient, Tennant says.
“What we’ve seen,” he adds, “is those that have that seamless integration between practice-management systems and EHR have higher productivity and higher levels of satisfaction.” —RQ
By The Numbers
$131,564
The average amount of money HM groups received in support per full-time equivalent (FTE) in fiscal year 2010, according to new SHM-MGMA survey data. The data point—the so-called “subsidy”—was first revealed at HM11 in Dallas.
After several years of leveling off at roughly $100,000, some hospitalists say they were surprised to see the figure rise so quickly. The report also shows that 19% of hospitalist practices receive no support, a finding that prompted new SHM President Joseph Li, MD, SFHM, to ask: “Are we looking at two business models or two care models?”—RQ
A recent “Current Concepts” article in the New England Journal of Medicine (2011;364:749) by a pair of Yale University physicians asserts that the day is close at hand when ultrasound interpretations by clinicians at the patient’s bedside will become as routine in hospital care as the trusty stethoscope. Ultrasound, a noninvasive form of imaging related to oceanographic sonar, has moved beyond its traditional home in radiology to myriad other medical specialties and practice areas. The technology has become smaller, less expensive, and higher in resolution in recent years, the authors note, adding that it has been used on Mount Everest and the international space station, as well as in battlefield situations.
“It’s becoming more accessible, and more training is available to physicians who aren’t radiologists,” says Diane Sliwka, MD, a hospitalist at the University of California at San Francisco (UCSF).
Dr. Sliwka says the NEJM article represents a milestone in the dissemination of bedside ultrasound. She conducts monthly faculty development training in procedural ultrasound at UCSF, workshops at HM and internal-medicine conferences, and training sessions for other hospitals.
The most common uses for bedside, “point of care” ultrasound include guiding procedures, such as thoracentesis and paracentesis, with improved safety over doing such insertions “blind.” Emerging procedural uses include lumbar puncture and arthrocentesis. Diagnostically, bedside ultrasound can provide quick screening and assessment, for example, of fluid buildup around the heart; previously, it could take hours to get the results from a formal heart study.
As with the stethoscope, Dr. Sliwka says, training in its correct use and scope of appropriate bedside practice is essential: “My advice is to learn from the experts at your facility, including the radiologists, critical care, or emergency physicians.” Ultrasound courses are increasing at hospitalist conferences, but space often is limited, and further supervised practice back home is needed.
The next step for hospitalists could be the definition of appropriate scope of practice, training, and competencies for its use. “Creating a niche in this area can be a nice change of pace from our traditional work as hospitalists,” Dr. Sliwka says. —LB
Technology
Video Chat Takes Off for Physicians
A recent study of digital adoption trends found that 7% of U.S. physicians now use video consultations to communicate with patients.
Manhattan Research’s 2011 “Taking the Pulse” survey of 2,000 physicians’ use of technology found that video chat is emerging as a way to consult with patients about nonurgent issues and follow-up questions or with geographically dispersed patients. Psychiatrists and oncologists are more likely to use the new technology. Doctors’ concerns regarding reimbursement, liability, and HIPAA privacy rules remain barriers to adoption.
For more information, visit ManhattanResearch.com/News-and-Events/Press-Releases/physician-patient-online-video-conferencing.—LB
Legal
Positive Outcomes from Full Disclosure of Medical Errors
The University of Michigan Health System’s (UMHS) risk-management model of full disclosure with offer of compensation for medical errors sparked hospitalist Allen Kachalia, MD, JD, of Brigham & Women’s Hospital in Boston to retrospectively study the outcomes of malpractice-claims-related performance before and after UMHS implemented the system in 2001.
Among the results Dr. Kachalia reported in his research abstract plenary at HM10, and subsequently published in Annals of Internal Medicine (2010;153(4):213-221), the mean monthly rate of new claims per 100,000 patient contacts decreased 36% after the full-disclosure model was adopted, while the rate of claims resulting in lawsuits declined by 65%. Claims also were resolved more quickly with the full-disclosure model.
Disclosure of medical error, Dr. Kachalia says, means “if someone is injured by medical care caused by medical error, the physician tells the patient they made the error, how it happened, and, often, what they’ll do to fix it.” An apology is somewhat different, he adds, and there’s no generic script for an apology. “What patients want is sincerity,” he says.
How can hospitalists work with full disclosure? “The general advice most institutions give is that when you want to disclose a medical error, first get your risk-management and patient-safety officers involved. They can help during every step of the process of investigating the event and disclosing,” Dr. Kachalia explains. “Assure patients that you are going to look into their concerns. Then make sure that a thorough investigation is done.”—LB
Practice Management
AMA-MGMA Toolkit Sorts Transitional-Care Software Options
HM practices with physicians in outpatient settings—be they discharge clinics or transitional-care centers—don’t always know how to determine the most useful practice-management software for their needs. So for those not helped by informatics staff, consider the new “Practice Management System Software Directory” from AMA and the Medical Group Management Association (MGMA).
The online repository, which launched in May, is a companion to the “Selecting a Practice Management System” toolkit the joint venture unveiled last fall. While the system is geared toward ambulatory-care settings, Robert Tennant, a senior policy advisor with MGMA, says any HM group with practitioners working on transitional care would find it useful.
Overall, the directory’s goal is to guide providers on how to navigate the increasingly complex world of practice-management options as new guidelines for “meaningful use” are defined, as well as new rules governing electronic claims processing. A new claims standard, known as HIPAA version 5010, is going live Jan. 1, 2012, so Tennant believes the directory is timely.
“It’s very difficult, whether in a practice or a hospital, to know the best software to pick,” he says. “There are plenty of vendors out there telling you they’re the best. There’s no easy way to comparison-shop.”
Now physicians can use the toolkit to measure basic functions. The directory, which will be updated on a rolling basis, will catalogue price range (excluding implementation costs), the number of installed customers, the target market for the product, what year the software was first offered, and whether the vendor also offers an electronic health record (EHR) system. That last point is of particular note to hospitalists as a link between practice management and medical records can help make a practice more efficient, Tennant says.
“What we’ve seen,” he adds, “is those that have that seamless integration between practice-management systems and EHR have higher productivity and higher levels of satisfaction.” —RQ
By The Numbers
$131,564
The average amount of money HM groups received in support per full-time equivalent (FTE) in fiscal year 2010, according to new SHM-MGMA survey data. The data point—the so-called “subsidy”—was first revealed at HM11 in Dallas.
After several years of leveling off at roughly $100,000, some hospitalists say they were surprised to see the figure rise so quickly. The report also shows that 19% of hospitalist practices receive no support, a finding that prompted new SHM President Joseph Li, MD, SFHM, to ask: “Are we looking at two business models or two care models?”—RQ
What Is Your Value?
For those of you who attended Bob Wachter’s talk at HM11 in Dallas, you learned that Bob drives a particular model of a popular SUV made by a well-known Japanese manufacturer. When he was in the market for a vehicle, he decided he wanted to buy an SUV. He acknowledged there were certainly less expensive SUVs on the market, along with more expensive alternatives.
So why did he choose to purchase that particular model? Was it the color, the seat warmers, or the keyless entry system? The answer is simple: He decided to purchase the popular SUV because he thought it was the best value for his dollar.
I have this vision of Bob, head cocked to one side, with his index finger resting against his chin and a text bubble above his head reading, “What is the quality of this vehicle and what is the price tag?”
These are decisions all of us make in our everyday lives. I make the same value judgment when I pull into the gasoline station to purchase gas (regular or premium?) or when I go to the grocery store (brand-name or generic orange juice?). But we know that higher cost doesn’t always mean higher quality. Think American-made automobiles versus Japanese-made vehicles in the 1970s and ’80s.
Along those same lines, let’s think about the U.S. healthcare system in 2011. America is trying to move its healthcare toward a value-based system. How do we receive the best healthcare for the—many times taxpayer—dollar? I am a taxpayer and I am all for higher-quality healthcare for my dollars.
At HM11, I heard from many supporters of healthcare reform, but I also heard many people vilify the government’s efforts at reforming our healthcare system. Just about everyone agreed that the future is uncertain. The current healthcare system certainly values hospitalists. It is hard to argue with the facts. In less than 15 years, our healthcare system has created jobs for more than 30,000 hospitalists, the majority of whom require nonclinical revenue from hospitals to meet expenses. The latest SHM-MGMA data show that the average hospitalist full-time equivalent (FTE) receives more than $131,500 of nonclinical revenue (primarily from hospitals) annually.
Payors of healthcare are no different than Bob when it comes to purchasing a car, or me when it comes to purchasing orange juice. Payors will pay for hospitalists as long as they perceive value in their investment.
But what is the basis of this notion that hospitalists are high-value healthcare providers, and is it justified? At HM11, I heard about the continued rise in hospitalist salaries. Higher costs mean we will have to increase quality if we hope to achieve the same value (value=quality/cost).
Don’t Worry, Share Your Data
I have listened to many presentations about healthcare value, quality, and cost. My perception is that it makes the most sense if it is personal. I live in Massachusetts, and my state government has been aggressive at helping everyone understand the quality and the cost of care being delivered at our hospitals. For example, our state government generates a massive annual report that describes the quality and cost of healthcare being delivered at individual hospitals; a PDF of the report is available at www.mass.gov. (For full disclosure, I work at Beth Israel Deaconess Medical Center [BIDMC] in Boston and I serve on a Massachusetts Department of Public Health Stroke Advisory Committee.)
The annual report shows there is not as much of a direct relationship between quality and cost as one would like to see. But I applaud Massachusetts for producing this report. Recognizing and understanding a problem is the first step in creating a solution to the problem. One cannot create a value-based system without understanding the existing quality and cost.
This is one of the reasons why, several years ago, the BIDMC leadership posted my hospital’s quality data online for public consumption (www.bidmc.org/QualityandSafety.aspx). The BIDMC website even features a short video of hospitalist Ken Sands, MD, who also happens to be the vice president of quality at BIDMC, telling you about the hospital quality data. Before the hospital posted this data online, most of our hospital staff and providers, let alone our patients and their families, were unaware of the data. BIDMC is not the only hospital who does this. I understand Cedars-Sinai Medical Center in Los Angeles and Dartmouth-Hitchcock Medical Center in New Hampshire have long shared their quality data publicly.
But the truth is, if you look hard enough, you can find these data for just about all acute-care hospitals in the country. Start with Medicare’s Hospital Compare website (www.hospitalcompare.hhs.gov). However, BIDMC and others have simply made it easier to find the data by putting it directly on their websites.
Policy of Transparency
An interesting thing happened over the past decade at BIDMC. In 1997, there were no hospitalists who cared for BIDMC patients. Today, hospitalists manage nearly 100% of the patients hospitalized on our large medical service.
When you look at the data being reported by BIDMC and the state of Massachusetts about nonsurgical conditions, doesn’t that reflect the care being provided by the hospitalists who work at BIDMC? I imagine that is what will run through my CEO and CFO’s minds when we discuss the hospitalist budget this summer. They will ask themselves, “What is the value of our hospitalists? What is the quality of their care? How much do they cost us?”
Some of you might be in a similar position. Do your hospitalists now provide the bulk of the care at your hospital? Are your hospital’s data being publicly reported? I think the answer is a resounding “yes” for many of you.
Allow me to ask this question: What are you doing to collect data to understand the quality and cost of your hospitalist program? Wouldn’t you rather know this information before your hospital or state government tells you?
As the director of my hospitalist group, I spearhead our group efforts to better understand the quality of care we provide. This proactive, introspective approach is essential, especially if hospitalist groups around the country hope to continue being perceived as “high value” providers.
I am interested in hearing from you about your efforts to understand the care being provided by your hospitalists. Feel free to email me at JosephLi@HospitalMedicine.org. TH
Dr. Li is president of SHM.
For those of you who attended Bob Wachter’s talk at HM11 in Dallas, you learned that Bob drives a particular model of a popular SUV made by a well-known Japanese manufacturer. When he was in the market for a vehicle, he decided he wanted to buy an SUV. He acknowledged there were certainly less expensive SUVs on the market, along with more expensive alternatives.
So why did he choose to purchase that particular model? Was it the color, the seat warmers, or the keyless entry system? The answer is simple: He decided to purchase the popular SUV because he thought it was the best value for his dollar.
I have this vision of Bob, head cocked to one side, with his index finger resting against his chin and a text bubble above his head reading, “What is the quality of this vehicle and what is the price tag?”
These are decisions all of us make in our everyday lives. I make the same value judgment when I pull into the gasoline station to purchase gas (regular or premium?) or when I go to the grocery store (brand-name or generic orange juice?). But we know that higher cost doesn’t always mean higher quality. Think American-made automobiles versus Japanese-made vehicles in the 1970s and ’80s.
Along those same lines, let’s think about the U.S. healthcare system in 2011. America is trying to move its healthcare toward a value-based system. How do we receive the best healthcare for the—many times taxpayer—dollar? I am a taxpayer and I am all for higher-quality healthcare for my dollars.
At HM11, I heard from many supporters of healthcare reform, but I also heard many people vilify the government’s efforts at reforming our healthcare system. Just about everyone agreed that the future is uncertain. The current healthcare system certainly values hospitalists. It is hard to argue with the facts. In less than 15 years, our healthcare system has created jobs for more than 30,000 hospitalists, the majority of whom require nonclinical revenue from hospitals to meet expenses. The latest SHM-MGMA data show that the average hospitalist full-time equivalent (FTE) receives more than $131,500 of nonclinical revenue (primarily from hospitals) annually.
Payors of healthcare are no different than Bob when it comes to purchasing a car, or me when it comes to purchasing orange juice. Payors will pay for hospitalists as long as they perceive value in their investment.
But what is the basis of this notion that hospitalists are high-value healthcare providers, and is it justified? At HM11, I heard about the continued rise in hospitalist salaries. Higher costs mean we will have to increase quality if we hope to achieve the same value (value=quality/cost).
Don’t Worry, Share Your Data
I have listened to many presentations about healthcare value, quality, and cost. My perception is that it makes the most sense if it is personal. I live in Massachusetts, and my state government has been aggressive at helping everyone understand the quality and the cost of care being delivered at our hospitals. For example, our state government generates a massive annual report that describes the quality and cost of healthcare being delivered at individual hospitals; a PDF of the report is available at www.mass.gov. (For full disclosure, I work at Beth Israel Deaconess Medical Center [BIDMC] in Boston and I serve on a Massachusetts Department of Public Health Stroke Advisory Committee.)
The annual report shows there is not as much of a direct relationship between quality and cost as one would like to see. But I applaud Massachusetts for producing this report. Recognizing and understanding a problem is the first step in creating a solution to the problem. One cannot create a value-based system without understanding the existing quality and cost.
This is one of the reasons why, several years ago, the BIDMC leadership posted my hospital’s quality data online for public consumption (www.bidmc.org/QualityandSafety.aspx). The BIDMC website even features a short video of hospitalist Ken Sands, MD, who also happens to be the vice president of quality at BIDMC, telling you about the hospital quality data. Before the hospital posted this data online, most of our hospital staff and providers, let alone our patients and their families, were unaware of the data. BIDMC is not the only hospital who does this. I understand Cedars-Sinai Medical Center in Los Angeles and Dartmouth-Hitchcock Medical Center in New Hampshire have long shared their quality data publicly.
But the truth is, if you look hard enough, you can find these data for just about all acute-care hospitals in the country. Start with Medicare’s Hospital Compare website (www.hospitalcompare.hhs.gov). However, BIDMC and others have simply made it easier to find the data by putting it directly on their websites.
Policy of Transparency
An interesting thing happened over the past decade at BIDMC. In 1997, there were no hospitalists who cared for BIDMC patients. Today, hospitalists manage nearly 100% of the patients hospitalized on our large medical service.
When you look at the data being reported by BIDMC and the state of Massachusetts about nonsurgical conditions, doesn’t that reflect the care being provided by the hospitalists who work at BIDMC? I imagine that is what will run through my CEO and CFO’s minds when we discuss the hospitalist budget this summer. They will ask themselves, “What is the value of our hospitalists? What is the quality of their care? How much do they cost us?”
Some of you might be in a similar position. Do your hospitalists now provide the bulk of the care at your hospital? Are your hospital’s data being publicly reported? I think the answer is a resounding “yes” for many of you.
Allow me to ask this question: What are you doing to collect data to understand the quality and cost of your hospitalist program? Wouldn’t you rather know this information before your hospital or state government tells you?
As the director of my hospitalist group, I spearhead our group efforts to better understand the quality of care we provide. This proactive, introspective approach is essential, especially if hospitalist groups around the country hope to continue being perceived as “high value” providers.
I am interested in hearing from you about your efforts to understand the care being provided by your hospitalists. Feel free to email me at JosephLi@HospitalMedicine.org. TH
Dr. Li is president of SHM.
For those of you who attended Bob Wachter’s talk at HM11 in Dallas, you learned that Bob drives a particular model of a popular SUV made by a well-known Japanese manufacturer. When he was in the market for a vehicle, he decided he wanted to buy an SUV. He acknowledged there were certainly less expensive SUVs on the market, along with more expensive alternatives.
So why did he choose to purchase that particular model? Was it the color, the seat warmers, or the keyless entry system? The answer is simple: He decided to purchase the popular SUV because he thought it was the best value for his dollar.
I have this vision of Bob, head cocked to one side, with his index finger resting against his chin and a text bubble above his head reading, “What is the quality of this vehicle and what is the price tag?”
These are decisions all of us make in our everyday lives. I make the same value judgment when I pull into the gasoline station to purchase gas (regular or premium?) or when I go to the grocery store (brand-name or generic orange juice?). But we know that higher cost doesn’t always mean higher quality. Think American-made automobiles versus Japanese-made vehicles in the 1970s and ’80s.
Along those same lines, let’s think about the U.S. healthcare system in 2011. America is trying to move its healthcare toward a value-based system. How do we receive the best healthcare for the—many times taxpayer—dollar? I am a taxpayer and I am all for higher-quality healthcare for my dollars.
At HM11, I heard from many supporters of healthcare reform, but I also heard many people vilify the government’s efforts at reforming our healthcare system. Just about everyone agreed that the future is uncertain. The current healthcare system certainly values hospitalists. It is hard to argue with the facts. In less than 15 years, our healthcare system has created jobs for more than 30,000 hospitalists, the majority of whom require nonclinical revenue from hospitals to meet expenses. The latest SHM-MGMA data show that the average hospitalist full-time equivalent (FTE) receives more than $131,500 of nonclinical revenue (primarily from hospitals) annually.
Payors of healthcare are no different than Bob when it comes to purchasing a car, or me when it comes to purchasing orange juice. Payors will pay for hospitalists as long as they perceive value in their investment.
But what is the basis of this notion that hospitalists are high-value healthcare providers, and is it justified? At HM11, I heard about the continued rise in hospitalist salaries. Higher costs mean we will have to increase quality if we hope to achieve the same value (value=quality/cost).
Don’t Worry, Share Your Data
I have listened to many presentations about healthcare value, quality, and cost. My perception is that it makes the most sense if it is personal. I live in Massachusetts, and my state government has been aggressive at helping everyone understand the quality and the cost of care being delivered at our hospitals. For example, our state government generates a massive annual report that describes the quality and cost of healthcare being delivered at individual hospitals; a PDF of the report is available at www.mass.gov. (For full disclosure, I work at Beth Israel Deaconess Medical Center [BIDMC] in Boston and I serve on a Massachusetts Department of Public Health Stroke Advisory Committee.)
The annual report shows there is not as much of a direct relationship between quality and cost as one would like to see. But I applaud Massachusetts for producing this report. Recognizing and understanding a problem is the first step in creating a solution to the problem. One cannot create a value-based system without understanding the existing quality and cost.
This is one of the reasons why, several years ago, the BIDMC leadership posted my hospital’s quality data online for public consumption (www.bidmc.org/QualityandSafety.aspx). The BIDMC website even features a short video of hospitalist Ken Sands, MD, who also happens to be the vice president of quality at BIDMC, telling you about the hospital quality data. Before the hospital posted this data online, most of our hospital staff and providers, let alone our patients and their families, were unaware of the data. BIDMC is not the only hospital who does this. I understand Cedars-Sinai Medical Center in Los Angeles and Dartmouth-Hitchcock Medical Center in New Hampshire have long shared their quality data publicly.
But the truth is, if you look hard enough, you can find these data for just about all acute-care hospitals in the country. Start with Medicare’s Hospital Compare website (www.hospitalcompare.hhs.gov). However, BIDMC and others have simply made it easier to find the data by putting it directly on their websites.
Policy of Transparency
An interesting thing happened over the past decade at BIDMC. In 1997, there were no hospitalists who cared for BIDMC patients. Today, hospitalists manage nearly 100% of the patients hospitalized on our large medical service.
When you look at the data being reported by BIDMC and the state of Massachusetts about nonsurgical conditions, doesn’t that reflect the care being provided by the hospitalists who work at BIDMC? I imagine that is what will run through my CEO and CFO’s minds when we discuss the hospitalist budget this summer. They will ask themselves, “What is the value of our hospitalists? What is the quality of their care? How much do they cost us?”
Some of you might be in a similar position. Do your hospitalists now provide the bulk of the care at your hospital? Are your hospital’s data being publicly reported? I think the answer is a resounding “yes” for many of you.
Allow me to ask this question: What are you doing to collect data to understand the quality and cost of your hospitalist program? Wouldn’t you rather know this information before your hospital or state government tells you?
As the director of my hospitalist group, I spearhead our group efforts to better understand the quality of care we provide. This proactive, introspective approach is essential, especially if hospitalist groups around the country hope to continue being perceived as “high value” providers.
I am interested in hearing from you about your efforts to understand the care being provided by your hospitalists. Feel free to email me at JosephLi@HospitalMedicine.org. TH
Dr. Li is president of SHM.
Virtual Mentorship
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
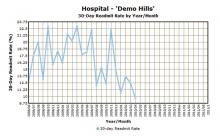
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
With more than 250 hospitals adopting them in the last three years, SHM’s mentored implementation programs make a compelling case for the need to address care transitions, improve the management of diabetes, and prevent VTEs in hospitalized patients. And early results from the sites show that the mentored implementation model, with its combination of a best-practices toolkit and individualized support from national experts, can make a real difference.
“Quality improvement (QI) is the niche of hospital medicine; our mentored implementation programs have achieved both the goals of improving care in a clinical area nationwide as well as creating quality improvement leaders within our ranks,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, associate professor of medicine and hospital medicine section chief at the University of New Mexico Health Sciences Center’s Department of Internal Medicine.
That’s the reasoning behind SHM’s new eQUIPS program. In essence, eQUIPS (Electronic Quality Improvement Programs) is SHM’s proven mentored implementation program, but without the mentor. Participants can access the same educational tools and resources, the same data center for tracking performance, and participate in the same online collaborative available to mentored implementation sites.

“SHM’s eQUIPS program takes the collective knowledge from the programs and offers it as a self-guided program that includes robust data collection and display programs,” Dr. Rogers says. “It will allow hospital quality-improvement teams more time to focus on driving change through the effective use of data, rather than spending their time trying to get the data.”
eQUIPS empowers hospitalists to move forward on valuable QI programs at their own pace, at any time. Hospitalists begin with the confidence that an entire community of likeminded physicians is supporting them, sharing their information, challenges, and successes.
Now, hospitalists can bring best practices to their hospitals and show their directors and executive leadership that they are on the cutting edge of addressing some of the most pervasive challenges in today’s hospitals.
Although they share a similar approach, each of eQUIPS’ three programs tackles the individual challenges of care transitions, VTE, and glycemic control separately. Hospitals can subscribe to any combination of the three topics.
Because eQUIPS is meant for year-after-year use and designed so that its utility grows along with its user base, access to eQUIPS is based on a yearly subscription model. The first year of access to eQUIPS is $2,500, which includes a one-time technology start-up fee. Each following year’s subscription is $1,500.
Hospitalists can apply for eQUIPS at www.hospitalmedicine.org/equips.
Educational Resources Get eQUIPS Users Started
Regardless of how far a hospital has advanced its programs, the educational materials that come with the subscription take hospitalists through the best in evidence-based medicine to address care transitions, VTE, and glycemic control, essentially forming a toolkit of relevant journal articles, presentations, step-by-step implementation guides, clinical tools, program files submitted by participants, and on-demand educational webinars facilitated by content experts.
Analysis and Reporting
Most experts agree that tracking and reporting results are the linchpins of QI programs. eQUIPS makes it easier with secure online tools for recording, benchmarking, process management, and tracking milestones.
Plus, eQUIPS enables hospitalists to compare their programs to others across the country. By uploading performance data to the secure eQUIPS data center for performance tracking, hospitals can analyze and compare outcomes from their programs to other eQUIPS sites and national norms (see Figure 1).
And hospitalists can assure their hospitals’ legal staffs that SHM has taken steps to ensure HIPAA compliance through third-party reviews. eQUIPS subscribers log into the site through a secured-password authentication similar to those of other online public health and financial institutions. In addition, SHM’s QI programs have earned the Patient Safety Organization (PSO) designation from the Agency for Healthcare Research and Quality (AHRQ), which makes it easier for hospitals to share performance data with SHM.
Real-Time Collaboration
Every hospital faces unique challenges, but they also have much in common when it comes to implementing new programs. As eQUIPS subscribers join, they can share their QI experiences and ask others for feedback in finding solutions.
The eQUIPS community website feature serves as a central, on-demand repository for sharing documents and educational materials, while the online workspace enables hospitalists to collaborate in real time by posting documents and editing them with other participating eQUIPS sites.
eQUIPS also brings collaboration right to users’ inboxes. Access to QI listservs has been a productive way for hospitalists to connect and benefit from the collective experience of the group; it’s a key component of the eQUIPS programs.
For Rogers, eQUIPS and its collaborative tools are a logistical extension of SHM’s successful QI track record. TH
Brendon Shank is assistant vice president of communications for SHM.
Med Students’ Simple Idea Has Serious Potential
The difficulties in routinely recalling each and every action to take with a patient has encouraged hospitalists to abide by checklists that remind them of just what to do. So why shouldn’t patients have the same systematic prodding? That’s exactly what two first-year students at the University of Michigan Medical School in Ann Arbor—Andrew Lin and Aaron Farberg—thought two years ago, prompting them to invent Dear Doctor.
With the help of senior physicians, including former SHM president Scott Flanders, MD, SFHM, FACP, Lin and Farberg conducted a three-month study that provided bedside notepads to patients. The patients were encouraged to jot down questions for their doctors whenever a question occurred to them, not just when the physician was in the room. The students produced 1,000 notepads, even shrink-wrapping them with companion pens.
The simple yet seemingly effective approach worked so well that “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication” earned the budding physicians the 2010 Innovation Poster award in the Research, Innovations, and Clinical Vignettes competition at HM10.
“This isn’t groundbreaking work here,” Lin says. “It’s a notepad, scraps of paper. Look around your desk and you’ve got sticky notes around. That’s what this is.”
Lin and Farberg both say they were surprised no one had crafted a similar communication tool as a potential quality-improvement (QI) measure. To wit, they are now working on publishing their research in the Journal of Hospital Medicine to further draw attention to the concept. They envision a day when the notes patients write down could be included in electronic medical records.
The ultimate goal is to give hospitalists and other physicians another way to communicate with their patients. “We want to institutionalize [Dear Doctor] to the point it’s a recognized necessity for the hospital system,” Lin says.—RQ
Toolkit Addresses Small-Business Security Concerns
The Healthcare Information and Management Systems Society (HIMSS) has had a privacy and security toolkit for physicians for a decade, but after its last annual security survey with the Medical Group Management Association (MGMA), it became clear that small- to medium-sized organizations were behind in implementation.
And so was born the HIMSS Privacy and Security Toolkit for Small Provider Organizations. The joint initiative is one that HM groups in rural or small settings should take advantage of, says Lisa Gallagher, HIMSS’ senior director of privacy and security.
Hospitalists “need to understand the reporting environment,” Gallagher says. “They are the subject of a lot of the policies and technology. We need them to be knowledgeable about it. They’re the ones who have access.”
HM’s role at the juncture of different departments and physicians, particularly at smaller hospitals that rely on hospitalists as traffic cops, makes it all the more important for hospitalists to understand the nuances of both privacy and security.
The interactive toolkit allows users to submit their own suggestions for improved processes and features introductions to the Centers for Medicare & Medicaid Services’ (CMS) “meaningful use” standard. Gallagher is hopeful that an engaged physician response to the toolkit will only bolster its efficacy in the coming months. “This is going to continue to evolve,” she says.—RQ
QUALITY RESEARCH
Care Transitions, Readmissions Concern Other Countries
International studies suggest that the recent torrent of attention toward improving care transitions and preventing hospital readmissions is not just an American trend. For example, a literature survey of physician “handovers” (aka handoffs) in international hospitals published in the British Medical Journal for Quality and Safety identified 32 papers on the subject.1 The authors conclude that the existing literature rarely examines pre- and post-handover phases or evaluates the quality of handover practices, and thus “does not fully identify where communication failures typically occur.” More systematic analysis of all stages of handoffs by physicians is warranted, the authors suggest.
In the same journal, a literature search of English-language publications from 1990 to 2010 found a dozen studies—eight from the U.S.—documenting failure to perform adequate follow-up for patients’ test results.2 The lack of follow-up ranged from 20% to 62% for hospitalized patients, and from 1% to 75% for patients treated in the ED. Two areas where problems were particularly evident were critical test results and results for patients moving across healthcare settings. “The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions,” the authors conclude. They recommend further study of the effectiveness of such interventions as online endorsement of results, and integration of information technology into clinical work practices.
The World Alliance for Patient Safety, which was convened in 2004 by the World Health Organization, recently pointed to poor test result follow-up as one of the major processes contributing to unsafe patient care internationally.1 The organization has identified nine “patient-safety solutions,” one of which is ensuring medication accuracy at transitions of care.
For more information on the alliance and WHO’s interest in patient safety, visit http://www.who.int/topics/patient_safety/en/. —LB
References
- Raduma-Tomás MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospi- tals: a literature review. BMJ Qual Saf. 2011;20:128-133.
- Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194-199.
The difficulties in routinely recalling each and every action to take with a patient has encouraged hospitalists to abide by checklists that remind them of just what to do. So why shouldn’t patients have the same systematic prodding? That’s exactly what two first-year students at the University of Michigan Medical School in Ann Arbor—Andrew Lin and Aaron Farberg—thought two years ago, prompting them to invent Dear Doctor.
With the help of senior physicians, including former SHM president Scott Flanders, MD, SFHM, FACP, Lin and Farberg conducted a three-month study that provided bedside notepads to patients. The patients were encouraged to jot down questions for their doctors whenever a question occurred to them, not just when the physician was in the room. The students produced 1,000 notepads, even shrink-wrapping them with companion pens.
The simple yet seemingly effective approach worked so well that “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication” earned the budding physicians the 2010 Innovation Poster award in the Research, Innovations, and Clinical Vignettes competition at HM10.
“This isn’t groundbreaking work here,” Lin says. “It’s a notepad, scraps of paper. Look around your desk and you’ve got sticky notes around. That’s what this is.”
Lin and Farberg both say they were surprised no one had crafted a similar communication tool as a potential quality-improvement (QI) measure. To wit, they are now working on publishing their research in the Journal of Hospital Medicine to further draw attention to the concept. They envision a day when the notes patients write down could be included in electronic medical records.
The ultimate goal is to give hospitalists and other physicians another way to communicate with their patients. “We want to institutionalize [Dear Doctor] to the point it’s a recognized necessity for the hospital system,” Lin says.—RQ
Toolkit Addresses Small-Business Security Concerns
The Healthcare Information and Management Systems Society (HIMSS) has had a privacy and security toolkit for physicians for a decade, but after its last annual security survey with the Medical Group Management Association (MGMA), it became clear that small- to medium-sized organizations were behind in implementation.
And so was born the HIMSS Privacy and Security Toolkit for Small Provider Organizations. The joint initiative is one that HM groups in rural or small settings should take advantage of, says Lisa Gallagher, HIMSS’ senior director of privacy and security.
Hospitalists “need to understand the reporting environment,” Gallagher says. “They are the subject of a lot of the policies and technology. We need them to be knowledgeable about it. They’re the ones who have access.”
HM’s role at the juncture of different departments and physicians, particularly at smaller hospitals that rely on hospitalists as traffic cops, makes it all the more important for hospitalists to understand the nuances of both privacy and security.
The interactive toolkit allows users to submit their own suggestions for improved processes and features introductions to the Centers for Medicare & Medicaid Services’ (CMS) “meaningful use” standard. Gallagher is hopeful that an engaged physician response to the toolkit will only bolster its efficacy in the coming months. “This is going to continue to evolve,” she says.—RQ
QUALITY RESEARCH
Care Transitions, Readmissions Concern Other Countries
International studies suggest that the recent torrent of attention toward improving care transitions and preventing hospital readmissions is not just an American trend. For example, a literature survey of physician “handovers” (aka handoffs) in international hospitals published in the British Medical Journal for Quality and Safety identified 32 papers on the subject.1 The authors conclude that the existing literature rarely examines pre- and post-handover phases or evaluates the quality of handover practices, and thus “does not fully identify where communication failures typically occur.” More systematic analysis of all stages of handoffs by physicians is warranted, the authors suggest.
In the same journal, a literature search of English-language publications from 1990 to 2010 found a dozen studies—eight from the U.S.—documenting failure to perform adequate follow-up for patients’ test results.2 The lack of follow-up ranged from 20% to 62% for hospitalized patients, and from 1% to 75% for patients treated in the ED. Two areas where problems were particularly evident were critical test results and results for patients moving across healthcare settings. “The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions,” the authors conclude. They recommend further study of the effectiveness of such interventions as online endorsement of results, and integration of information technology into clinical work practices.
The World Alliance for Patient Safety, which was convened in 2004 by the World Health Organization, recently pointed to poor test result follow-up as one of the major processes contributing to unsafe patient care internationally.1 The organization has identified nine “patient-safety solutions,” one of which is ensuring medication accuracy at transitions of care.
For more information on the alliance and WHO’s interest in patient safety, visit http://www.who.int/topics/patient_safety/en/. —LB
References
- Raduma-Tomás MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospi- tals: a literature review. BMJ Qual Saf. 2011;20:128-133.
- Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194-199.
The difficulties in routinely recalling each and every action to take with a patient has encouraged hospitalists to abide by checklists that remind them of just what to do. So why shouldn’t patients have the same systematic prodding? That’s exactly what two first-year students at the University of Michigan Medical School in Ann Arbor—Andrew Lin and Aaron Farberg—thought two years ago, prompting them to invent Dear Doctor.
With the help of senior physicians, including former SHM president Scott Flanders, MD, SFHM, FACP, Lin and Farberg conducted a three-month study that provided bedside notepads to patients. The patients were encouraged to jot down questions for their doctors whenever a question occurred to them, not just when the physician was in the room. The students produced 1,000 notepads, even shrink-wrapping them with companion pens.
The simple yet seemingly effective approach worked so well that “Dear Doctor: A Tool to Facilitate Patient-Centered Care and Enhance Communication” earned the budding physicians the 2010 Innovation Poster award in the Research, Innovations, and Clinical Vignettes competition at HM10.
“This isn’t groundbreaking work here,” Lin says. “It’s a notepad, scraps of paper. Look around your desk and you’ve got sticky notes around. That’s what this is.”
Lin and Farberg both say they were surprised no one had crafted a similar communication tool as a potential quality-improvement (QI) measure. To wit, they are now working on publishing their research in the Journal of Hospital Medicine to further draw attention to the concept. They envision a day when the notes patients write down could be included in electronic medical records.
The ultimate goal is to give hospitalists and other physicians another way to communicate with their patients. “We want to institutionalize [Dear Doctor] to the point it’s a recognized necessity for the hospital system,” Lin says.—RQ
Toolkit Addresses Small-Business Security Concerns
The Healthcare Information and Management Systems Society (HIMSS) has had a privacy and security toolkit for physicians for a decade, but after its last annual security survey with the Medical Group Management Association (MGMA), it became clear that small- to medium-sized organizations were behind in implementation.
And so was born the HIMSS Privacy and Security Toolkit for Small Provider Organizations. The joint initiative is one that HM groups in rural or small settings should take advantage of, says Lisa Gallagher, HIMSS’ senior director of privacy and security.
Hospitalists “need to understand the reporting environment,” Gallagher says. “They are the subject of a lot of the policies and technology. We need them to be knowledgeable about it. They’re the ones who have access.”
HM’s role at the juncture of different departments and physicians, particularly at smaller hospitals that rely on hospitalists as traffic cops, makes it all the more important for hospitalists to understand the nuances of both privacy and security.
The interactive toolkit allows users to submit their own suggestions for improved processes and features introductions to the Centers for Medicare & Medicaid Services’ (CMS) “meaningful use” standard. Gallagher is hopeful that an engaged physician response to the toolkit will only bolster its efficacy in the coming months. “This is going to continue to evolve,” she says.—RQ
QUALITY RESEARCH
Care Transitions, Readmissions Concern Other Countries
International studies suggest that the recent torrent of attention toward improving care transitions and preventing hospital readmissions is not just an American trend. For example, a literature survey of physician “handovers” (aka handoffs) in international hospitals published in the British Medical Journal for Quality and Safety identified 32 papers on the subject.1 The authors conclude that the existing literature rarely examines pre- and post-handover phases or evaluates the quality of handover practices, and thus “does not fully identify where communication failures typically occur.” More systematic analysis of all stages of handoffs by physicians is warranted, the authors suggest.
In the same journal, a literature search of English-language publications from 1990 to 2010 found a dozen studies—eight from the U.S.—documenting failure to perform adequate follow-up for patients’ test results.2 The lack of follow-up ranged from 20% to 62% for hospitalized patients, and from 1% to 75% for patients treated in the ED. Two areas where problems were particularly evident were critical test results and results for patients moving across healthcare settings. “The existing evidence suggests that the problem of missed test results is considerable and reported negative impacts on patients warrant the exploration of solutions,” the authors conclude. They recommend further study of the effectiveness of such interventions as online endorsement of results, and integration of information technology into clinical work practices.
The World Alliance for Patient Safety, which was convened in 2004 by the World Health Organization, recently pointed to poor test result follow-up as one of the major processes contributing to unsafe patient care internationally.1 The organization has identified nine “patient-safety solutions,” one of which is ensuring medication accuracy at transitions of care.
For more information on the alliance and WHO’s interest in patient safety, visit http://www.who.int/topics/patient_safety/en/. —LB
References
- Raduma-Tomás MA, Flin R, Yule S, Williams D. Doctors’ handovers in hospi- tals: a literature review. BMJ Qual Saf. 2011;20:128-133.
- Callen J, Georgiou A, Li J, Westbrook JI. The safety implications of missed test results for hospitalised patients: a systematic review. BMJ Qual Saf. 2011;20:194-199.
The Future of Better Patient Care
GRAPEVINE, Texas—Hospitalist Michael Monge, MD, of Cogent Healthcare in San Bernardino, Calif., watched an instructor squeeze the lubricating gel on the transponder and press it gently, but firmly, into the crook of a woman’s arm. Veins practically popped off an ultrasound monitor, serving as a literal road map for vascular access.
And he thought: Wouldn’t it be great if I had this technology all the time, just like I remember from my residency?
“A lot of my ER attendings were able to do a study at the bedside in a manner of minutes, not 30 or 45 minutes,” says Dr. Monge, who practices at Saint Bernardine Medical Center. “If they saw something abnormal, sure enough, they got the full study. But they were able to get that glimpse. Ultimately, it’s just better patient care.”
Dr. Monge’s ultrasound lesson was a first for the SHM annual meeting. In past years, training on ultrasounds was wrapped into the “Medical Procedures for the Hospitalist” pre-course. But at HM11, thanks to the growing prevalence and portability of the technology, the training was expanded into its own half-day pre-course, appropriately dubbed “Portable Ultrasound for the Hospitalist.”
“The ultrasound will be the stethoscope of the 21st century,” says Mark Ault, director of the Division of General Internal Medicine and assistant chairman for clinical affairs of the Department of Medicine at Cedars-Sinai Medical Center in Los Angeles. “And the goal will be to have an ultrasound in the hands of every internist.”
Only time will tell whether portable ultrasound becomes as commonplace as Dr. Ault envisions, but what is clear is that the evolution of the technology makes it widely applicable to hospitalists, says Bradley Rosen, MD, MBA, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Medical Center.
Pricing is one such example. In years past, ultrasound machines were bulky and costly, with price tags in the hundreds of thousands of dollars. Now, portable units, depending on the number of transducers and functionality, can come as low as $20,000, though more-advanced machines quickly jump into the $40,000 to $60,000 range.
Still, Dr. Rosen views the practical uses of the technology as almost endless, and could include vascular access, placing central and PICC lines, and insertion and removal of catheters. Most hospitalists, however, continue to have limited experience with portable ultrasound, meaning those interested in learning more likely have to seek out physicians in other departments to provide the training and mentorship required. Dr. Rosen suggests working with ED physicians, OB-GYNs, and radiologists, although he notes you should be careful to be clear that the HM community is not looking to supplant anyone, or take billing opportunities away.
Hospitalists “don’t know how to use it, and people don’t know where to go to learn how to use it,” he says. “This is a starting point that will allow people … to take these ideas back and, hopefully, generate enough of a critical mass that it becomes a louder and louder chorus asking for this technology.”
GRAPEVINE, Texas—Hospitalist Michael Monge, MD, of Cogent Healthcare in San Bernardino, Calif., watched an instructor squeeze the lubricating gel on the transponder and press it gently, but firmly, into the crook of a woman’s arm. Veins practically popped off an ultrasound monitor, serving as a literal road map for vascular access.
And he thought: Wouldn’t it be great if I had this technology all the time, just like I remember from my residency?
“A lot of my ER attendings were able to do a study at the bedside in a manner of minutes, not 30 or 45 minutes,” says Dr. Monge, who practices at Saint Bernardine Medical Center. “If they saw something abnormal, sure enough, they got the full study. But they were able to get that glimpse. Ultimately, it’s just better patient care.”
Dr. Monge’s ultrasound lesson was a first for the SHM annual meeting. In past years, training on ultrasounds was wrapped into the “Medical Procedures for the Hospitalist” pre-course. But at HM11, thanks to the growing prevalence and portability of the technology, the training was expanded into its own half-day pre-course, appropriately dubbed “Portable Ultrasound for the Hospitalist.”
“The ultrasound will be the stethoscope of the 21st century,” says Mark Ault, director of the Division of General Internal Medicine and assistant chairman for clinical affairs of the Department of Medicine at Cedars-Sinai Medical Center in Los Angeles. “And the goal will be to have an ultrasound in the hands of every internist.”
Only time will tell whether portable ultrasound becomes as commonplace as Dr. Ault envisions, but what is clear is that the evolution of the technology makes it widely applicable to hospitalists, says Bradley Rosen, MD, MBA, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Medical Center.
Pricing is one such example. In years past, ultrasound machines were bulky and costly, with price tags in the hundreds of thousands of dollars. Now, portable units, depending on the number of transducers and functionality, can come as low as $20,000, though more-advanced machines quickly jump into the $40,000 to $60,000 range.
Still, Dr. Rosen views the practical uses of the technology as almost endless, and could include vascular access, placing central and PICC lines, and insertion and removal of catheters. Most hospitalists, however, continue to have limited experience with portable ultrasound, meaning those interested in learning more likely have to seek out physicians in other departments to provide the training and mentorship required. Dr. Rosen suggests working with ED physicians, OB-GYNs, and radiologists, although he notes you should be careful to be clear that the HM community is not looking to supplant anyone, or take billing opportunities away.
Hospitalists “don’t know how to use it, and people don’t know where to go to learn how to use it,” he says. “This is a starting point that will allow people … to take these ideas back and, hopefully, generate enough of a critical mass that it becomes a louder and louder chorus asking for this technology.”
GRAPEVINE, Texas—Hospitalist Michael Monge, MD, of Cogent Healthcare in San Bernardino, Calif., watched an instructor squeeze the lubricating gel on the transponder and press it gently, but firmly, into the crook of a woman’s arm. Veins practically popped off an ultrasound monitor, serving as a literal road map for vascular access.
And he thought: Wouldn’t it be great if I had this technology all the time, just like I remember from my residency?
“A lot of my ER attendings were able to do a study at the bedside in a manner of minutes, not 30 or 45 minutes,” says Dr. Monge, who practices at Saint Bernardine Medical Center. “If they saw something abnormal, sure enough, they got the full study. But they were able to get that glimpse. Ultimately, it’s just better patient care.”
Dr. Monge’s ultrasound lesson was a first for the SHM annual meeting. In past years, training on ultrasounds was wrapped into the “Medical Procedures for the Hospitalist” pre-course. But at HM11, thanks to the growing prevalence and portability of the technology, the training was expanded into its own half-day pre-course, appropriately dubbed “Portable Ultrasound for the Hospitalist.”
“The ultrasound will be the stethoscope of the 21st century,” says Mark Ault, director of the Division of General Internal Medicine and assistant chairman for clinical affairs of the Department of Medicine at Cedars-Sinai Medical Center in Los Angeles. “And the goal will be to have an ultrasound in the hands of every internist.”
Only time will tell whether portable ultrasound becomes as commonplace as Dr. Ault envisions, but what is clear is that the evolution of the technology makes it widely applicable to hospitalists, says Bradley Rosen, MD, MBA, medical director of the Inpatient Specialty Program (ISP) at Cedars-Sinai Medical Center.
Pricing is one such example. In years past, ultrasound machines were bulky and costly, with price tags in the hundreds of thousands of dollars. Now, portable units, depending on the number of transducers and functionality, can come as low as $20,000, though more-advanced machines quickly jump into the $40,000 to $60,000 range.
Still, Dr. Rosen views the practical uses of the technology as almost endless, and could include vascular access, placing central and PICC lines, and insertion and removal of catheters. Most hospitalists, however, continue to have limited experience with portable ultrasound, meaning those interested in learning more likely have to seek out physicians in other departments to provide the training and mentorship required. Dr. Rosen suggests working with ED physicians, OB-GYNs, and radiologists, although he notes you should be careful to be clear that the HM community is not looking to supplant anyone, or take billing opportunities away.
Hospitalists “don’t know how to use it, and people don’t know where to go to learn how to use it,” he says. “This is a starting point that will allow people … to take these ideas back and, hopefully, generate enough of a critical mass that it becomes a louder and louder chorus asking for this technology.”
HM=Improved Patient Care
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
GRAPEVINE, Texas—The most successful companies tend to have superior branding. Starbucks owns coffee. Disney owns family fun. And hospitalists own patient-safety and quality-improvement (QI) initiatives within their hospitals.
“We were pretty confident that if we embraced this, we would have a clear running field to ourselves,” says Robert Wachter, MD, MHM, professor, chief of the Division of Hospital Medicine, and chief of the Medical Service at the University of California at San Francisco Medical Center, former SHM president, and author of the Wachter’s World blog. “No other physician field would do the same thing, and by owning the patient-safety field, we would distinguish ourselves.”
Now comes the really hard part, though.
Three keynote speakers at HM11—Dr. Wachter, AMA President Cecil Wilson, MD, and Robert Kocher, MD, a healthcare policy advisor to President Obama—pointed to hospitalists as the physician cohort that can help shepherd the conceptual reform passed last year by Congress into daily practice in America’s hospitals. And all three also point to HM’s role at the vanguard of patient safety as a primary reason why.
Hurdles will arise, Dr. Wilson says. A solo practitioner most of his career, he says hospitalists can play a key role in the coming years as more patients receive insurance, but looming doctor shortages could stymie the cause. While many caution that the flood of newly insured patients will overburden primary-care physicians (PCPs), the expected shortage of physicians will plague HM as well.
“Hospitalists are primary-care physicians; the vast majority of them are general internists,” Dr. Wilson says. “… So when we say that the number of people who are going into primary care, particularly general internal medicine, is reducing, that reduces not only the pool of physicians in the community, but also the hospitalist pool. We’re in that boat together.”
Dr. Kocher, director of the McKinsey Center for U.S. Health System Reform in Washington, D.C., says hospitalists are in the best position to push for on-the-ground reform as they are the doctors who bridge all hospital departments, floors, and wards. He sees four broad areas where HM can take a particularly leading role:
- Increasing labor productivity. HM’s role as a link between specialties from cardiology to the pharmacy makes HM a natural conduit to push institutional values from a unique vantage point.
- Driving decision-making. Whether it’s recommending less costly drugs with similar outcomes, questioning whether expensive test batteries are truly necessary or being done for fear of missing something, or pausing to ask whether a “90-year-old hip replacement patient should receive orthopedic implants that will last far longer than their grandkids will be alive,” hospitalists can use their data to be a common-sense lynchpin of daily operations.
- Using technology to lower delivery costs. Many insurance companies are willing to enter into risk-based contracts with hospitals, but some hospital executives worry whether they will be able to perform well enough to justify the risk. “Hospitalists can help say, ‘We can do this. We can hit the thresholds.’ ”
- Shifting compensation models from “selling work RVUs to selling years of health.”
“The biggest thing [hospitalists] should begin doing,” Dr. Kocher adds, “is stop thinking about units of work, or RVUs, and start thinking about how much better patients can be by virtue of the care they’re delivering, how many readmissions are they avoiding, how many core measures/outcomes are they hitting, how much better is the patient experience, and how much smoother is the handoff.”
The push to improve quality and show better outcomes, of course, is intrinsically tied to payment reform. Bundled payments that reimburse a set fee for a case from pre-admission to a preset post-discharge deadline worry some hospitalists, who fear how the payments will be divvied up and who will be in charge of said payment decisions. Dr. Kocher says that even when the initial rules are set, the system is likely to evolve.
However, the hospitalist’s role as a driver of QI positions the field well, all three speakers noted. By quarterbacking patient handoffs and continuing to be seen by hospital executives as quality and safety leaders, HM groups can make the argument that they are worth the financial support they ask for in negotiations. Dr. Wachter adds that while quality research has become a staple of academics and residents, hospitalists should look to now tie value to the equation, effectively linking better patient outcomes to HM’s bottom line.
“There’s no question that physicians that can care for patients more efficiently, in a higher-quality way, in hospitals at lower costs, are going to do better no matter how the system evolves,” Dr. Kocher says. “I’m positive, as long as hospitalists are confident—and I think they should be—that they can deliver, more consistently, better care than those who aren’t hospitalists practicing in hospitals … and they’re going to do better economically.”
NEW DEPARTMENT: Innovations
No one becomes a doctor to make a fashion statement, but a new study (http://onlinelibrary.wiley.com/doi/10.1002/jhm.864/abstract) in the Journal of Hospital Medicine reports that the choice between long-sleeved white coats and freshly laundered scrubs might be a question of taste, not safety.
The report, “Newly Cleaned Physician Uniforms and Infrequently Washed White Coats Have Similar Rates of Bacterial Contamination After an 8-Hour Workday: A Randomized Controlled Trial,” found no statistically significant differences in bacterial or methicillin-resistant Staphylococcus aureus (MRSA) contamination of physicians’ white coats compared with scrubs or in contamination of the skin at the wrists of physicians wearing either garment.
In an email interview, Marisha Burden, MD, interim chief of hospital medicine at the Denver Health and Hospital Authority, says that the topic area came up during a review of research regarding MRSA and infection-control policies. Dr. Burden found references to the so-called “bare below the elbows” policy in the United Kingdom, a reference to 2007 rules from the British Department of Health banning long-sleeved coats in an attempt to stop nosocomial bacterial transmission.
“This policy was interesting to us secondary to the fact that there was no literature to support the measures being implemented,” Dr. Burden says. “ … Our data show that bacterial contamination of work clothes occurs within hours of putting them on, as well that at the end of an eight-hour workday, there is no difference in bacterial or MRSA contamination of either dress.”
Dr. Burden says the data do not support discarding white coats for uniforms that are changed on a daily basis, or for “requiring healthcare workers to avoid long-sleeved garments.” She also says that white coats have traditional lures as well as practical ones: Most of the physicians who declined to participate in the study did so because they refused to work without the pockets that came with their lab coats.
“I think we also have to consider the professional image that our physicians portray,” she adds. “Our patients expect their physicians to appear professional with clean, white coats.”—RQ
Technology
App Allows CT, MRI, PET Diagnoses Via iPhone, iPad
What can a hospitalist do the next time someone in the group has no immediate access to a work station but needs to make a medical diagnoses based on computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET)?
Grab the nearest iPhone.
The FDA recently approved an application from MIM Software Inc. of Cleveland to let doctors review medical images on the iPhone and iPad via a secure network transfer. The application, Mobile MIM, is the first with the FDA’s imprimatur. It allows hospitalists and other physicians to measure distance on the image and image intensity values and display measurement lines, annotations, and regions of interest, according to the FDA.
“Think of how cell phones were perceived a few decades ago; many dismissed ‘anytime access’ as not necessary,” MIM chief technology officer Mark Cain says in an email. “Yet now we know myriad of cases where the cell phone has proven immensely valuable. The same can be said of diagnostic medical image access. How many ways can this improve healthcare? More ways than I can predict.”—RQ
Quality Research
Research Confirms Benefits of ICU Safety Checklists
The value of checklists containing evidence-supported QI interventions to improve ICU outcomes, pioneered at Johns Hopkins in Baltimore, has been confirmed by several recent studies. The Keystone ICU Project, which sought to replicate the Hopkins experience in hospitals across Michigan, succeeded in nearly eliminating bloodstream infections and reducing mortality.1
Based on Medicare claims from 95 study hospitals and comparison data from 11 surrounding states, patients in hospitals using the checklist were significantly more likely to survive a hospital stay. The project was not, however, sufficiently powered to show a significant difference in length of stay.
A second Keystone Project study showed that five simple therapies aimed at lessening the time spent on ventilators, including elevating the head of the bed 30 degrees, giving anticoagulants, and lessening sedation, combined with education and a hospital culture supporting patient safety, reduced cases of ventilator-associated pneumonia by more than 70%.2
A comprehensive, video-conference-based intervention to support implementing six evidence-based quality practices in 15 community hospital ICUs in Canada improved the adoption of these practices. Expert-led forums and educational sessions promoted the sequential dissemination of treatment algorhythms, with a new practice targeted every four months.3—LB
References
- Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ. Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ. 2011;342:d219.
- Berenholtz SM, Pham JC, Thompson DA, Needhamm et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. Infect Control Hosp Epidemiol. 2011;(4):305-314.
- Scales DC, Dainty K, Hales B. A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA. 2011;305:363-372.
HM-Based Quality Research
Homeless Respite Helps Avoid Rehospitalizations
Some readmissions come about because things fall apart when patients are discharged with a follow-up plan that is not realistic to their circumstances. This is especially true for homeless patients, says Audrey Kuang, MD, a hospitalist at Santa Clara Valley Medical Center (SCVMC) in San Jose, Calif., and medical director of the Santa Clara County Medical Respite Program, a shelter for homeless patients following discharge from seven San Jose area hospitals.
Dr. Kuang described the collaborative program in a plenary presentation for the Research, Innovations, and Clinical Vignettes competition at HM10.
SCVMC is a county safety net hospital, and Dr. Kuang says the hospitalists “see a fair amount of homeless patients with recurrent exacerbations.” Patients given prescriptions for medications they can’t afford, special diets, or instructions for bed rest are then discharged to the street; inevitably, they are readmitted.
Dr. Kuang began tracking patients who had prolonged hospital stays because of homelessness or unsafe social situations. Her presentation to administrators led to participating hospitals contributing $25,000 each to launch the program with a multidisciplinary team, which included Dr. Kuang.
In its first year, 200 referrals were made to the respite program; 60% were accepted. The most common diagnoses were foot fractures, foot infections, and cancer. Quantified clinical outcomes are still being compiled, Dr. Kuang said, although the participating hospitals have reported decreased rehospitalizations and bed days—results documented in other studies of respite programs.1
“The main idea is post-acute medical care and support for homeless patients in need,” she explained. “Hospitalists may feel this is beyond our scope of practice, but it is our responsibility to know what’s going on out there.”—LB
Reference
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
By The Numbers
$44,000, $46,659, $120,000: EHR Implementation Costs Higher than Medicare Reimbursement
A new study in Health Affairs on the first-year costs of implementing electronic health records (EHR) in a 450-physician North Texas primary-care network doesn’t translate directly to HM, but figures showing that the installation cost is more for an average five-physician practice than Medicare is offering in incentive pay might serve as a warning sign for HM groups looking to build EHR into their practice:
- EHR incentive payments from Medicare over five years: $44,000;
- EHR implementation cost per doctor after first year: $46,659;
- EHR adoption costs per physician, estimated: $120,000.—RQ TH
No one becomes a doctor to make a fashion statement, but a new study (http://onlinelibrary.wiley.com/doi/10.1002/jhm.864/abstract) in the Journal of Hospital Medicine reports that the choice between long-sleeved white coats and freshly laundered scrubs might be a question of taste, not safety.
The report, “Newly Cleaned Physician Uniforms and Infrequently Washed White Coats Have Similar Rates of Bacterial Contamination After an 8-Hour Workday: A Randomized Controlled Trial,” found no statistically significant differences in bacterial or methicillin-resistant Staphylococcus aureus (MRSA) contamination of physicians’ white coats compared with scrubs or in contamination of the skin at the wrists of physicians wearing either garment.
In an email interview, Marisha Burden, MD, interim chief of hospital medicine at the Denver Health and Hospital Authority, says that the topic area came up during a review of research regarding MRSA and infection-control policies. Dr. Burden found references to the so-called “bare below the elbows” policy in the United Kingdom, a reference to 2007 rules from the British Department of Health banning long-sleeved coats in an attempt to stop nosocomial bacterial transmission.
“This policy was interesting to us secondary to the fact that there was no literature to support the measures being implemented,” Dr. Burden says. “ … Our data show that bacterial contamination of work clothes occurs within hours of putting them on, as well that at the end of an eight-hour workday, there is no difference in bacterial or MRSA contamination of either dress.”
Dr. Burden says the data do not support discarding white coats for uniforms that are changed on a daily basis, or for “requiring healthcare workers to avoid long-sleeved garments.” She also says that white coats have traditional lures as well as practical ones: Most of the physicians who declined to participate in the study did so because they refused to work without the pockets that came with their lab coats.
“I think we also have to consider the professional image that our physicians portray,” she adds. “Our patients expect their physicians to appear professional with clean, white coats.”—RQ
Technology
App Allows CT, MRI, PET Diagnoses Via iPhone, iPad
What can a hospitalist do the next time someone in the group has no immediate access to a work station but needs to make a medical diagnoses based on computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET)?
Grab the nearest iPhone.
The FDA recently approved an application from MIM Software Inc. of Cleveland to let doctors review medical images on the iPhone and iPad via a secure network transfer. The application, Mobile MIM, is the first with the FDA’s imprimatur. It allows hospitalists and other physicians to measure distance on the image and image intensity values and display measurement lines, annotations, and regions of interest, according to the FDA.
“Think of how cell phones were perceived a few decades ago; many dismissed ‘anytime access’ as not necessary,” MIM chief technology officer Mark Cain says in an email. “Yet now we know myriad of cases where the cell phone has proven immensely valuable. The same can be said of diagnostic medical image access. How many ways can this improve healthcare? More ways than I can predict.”—RQ
Quality Research
Research Confirms Benefits of ICU Safety Checklists
The value of checklists containing evidence-supported QI interventions to improve ICU outcomes, pioneered at Johns Hopkins in Baltimore, has been confirmed by several recent studies. The Keystone ICU Project, which sought to replicate the Hopkins experience in hospitals across Michigan, succeeded in nearly eliminating bloodstream infections and reducing mortality.1
Based on Medicare claims from 95 study hospitals and comparison data from 11 surrounding states, patients in hospitals using the checklist were significantly more likely to survive a hospital stay. The project was not, however, sufficiently powered to show a significant difference in length of stay.
A second Keystone Project study showed that five simple therapies aimed at lessening the time spent on ventilators, including elevating the head of the bed 30 degrees, giving anticoagulants, and lessening sedation, combined with education and a hospital culture supporting patient safety, reduced cases of ventilator-associated pneumonia by more than 70%.2
A comprehensive, video-conference-based intervention to support implementing six evidence-based quality practices in 15 community hospital ICUs in Canada improved the adoption of these practices. Expert-led forums and educational sessions promoted the sequential dissemination of treatment algorhythms, with a new practice targeted every four months.3—LB
References
- Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ. Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ. 2011;342:d219.
- Berenholtz SM, Pham JC, Thompson DA, Needhamm et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. Infect Control Hosp Epidemiol. 2011;(4):305-314.
- Scales DC, Dainty K, Hales B. A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA. 2011;305:363-372.
HM-Based Quality Research
Homeless Respite Helps Avoid Rehospitalizations
Some readmissions come about because things fall apart when patients are discharged with a follow-up plan that is not realistic to their circumstances. This is especially true for homeless patients, says Audrey Kuang, MD, a hospitalist at Santa Clara Valley Medical Center (SCVMC) in San Jose, Calif., and medical director of the Santa Clara County Medical Respite Program, a shelter for homeless patients following discharge from seven San Jose area hospitals.
Dr. Kuang described the collaborative program in a plenary presentation for the Research, Innovations, and Clinical Vignettes competition at HM10.
SCVMC is a county safety net hospital, and Dr. Kuang says the hospitalists “see a fair amount of homeless patients with recurrent exacerbations.” Patients given prescriptions for medications they can’t afford, special diets, or instructions for bed rest are then discharged to the street; inevitably, they are readmitted.
Dr. Kuang began tracking patients who had prolonged hospital stays because of homelessness or unsafe social situations. Her presentation to administrators led to participating hospitals contributing $25,000 each to launch the program with a multidisciplinary team, which included Dr. Kuang.
In its first year, 200 referrals were made to the respite program; 60% were accepted. The most common diagnoses were foot fractures, foot infections, and cancer. Quantified clinical outcomes are still being compiled, Dr. Kuang said, although the participating hospitals have reported decreased rehospitalizations and bed days—results documented in other studies of respite programs.1
“The main idea is post-acute medical care and support for homeless patients in need,” she explained. “Hospitalists may feel this is beyond our scope of practice, but it is our responsibility to know what’s going on out there.”—LB
Reference
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
By The Numbers
$44,000, $46,659, $120,000: EHR Implementation Costs Higher than Medicare Reimbursement
A new study in Health Affairs on the first-year costs of implementing electronic health records (EHR) in a 450-physician North Texas primary-care network doesn’t translate directly to HM, but figures showing that the installation cost is more for an average five-physician practice than Medicare is offering in incentive pay might serve as a warning sign for HM groups looking to build EHR into their practice:
- EHR incentive payments from Medicare over five years: $44,000;
- EHR implementation cost per doctor after first year: $46,659;
- EHR adoption costs per physician, estimated: $120,000.—RQ TH
No one becomes a doctor to make a fashion statement, but a new study (http://onlinelibrary.wiley.com/doi/10.1002/jhm.864/abstract) in the Journal of Hospital Medicine reports that the choice between long-sleeved white coats and freshly laundered scrubs might be a question of taste, not safety.
The report, “Newly Cleaned Physician Uniforms and Infrequently Washed White Coats Have Similar Rates of Bacterial Contamination After an 8-Hour Workday: A Randomized Controlled Trial,” found no statistically significant differences in bacterial or methicillin-resistant Staphylococcus aureus (MRSA) contamination of physicians’ white coats compared with scrubs or in contamination of the skin at the wrists of physicians wearing either garment.
In an email interview, Marisha Burden, MD, interim chief of hospital medicine at the Denver Health and Hospital Authority, says that the topic area came up during a review of research regarding MRSA and infection-control policies. Dr. Burden found references to the so-called “bare below the elbows” policy in the United Kingdom, a reference to 2007 rules from the British Department of Health banning long-sleeved coats in an attempt to stop nosocomial bacterial transmission.
“This policy was interesting to us secondary to the fact that there was no literature to support the measures being implemented,” Dr. Burden says. “ … Our data show that bacterial contamination of work clothes occurs within hours of putting them on, as well that at the end of an eight-hour workday, there is no difference in bacterial or MRSA contamination of either dress.”
Dr. Burden says the data do not support discarding white coats for uniforms that are changed on a daily basis, or for “requiring healthcare workers to avoid long-sleeved garments.” She also says that white coats have traditional lures as well as practical ones: Most of the physicians who declined to participate in the study did so because they refused to work without the pockets that came with their lab coats.
“I think we also have to consider the professional image that our physicians portray,” she adds. “Our patients expect their physicians to appear professional with clean, white coats.”—RQ
Technology
App Allows CT, MRI, PET Diagnoses Via iPhone, iPad
What can a hospitalist do the next time someone in the group has no immediate access to a work station but needs to make a medical diagnoses based on computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET)?
Grab the nearest iPhone.
The FDA recently approved an application from MIM Software Inc. of Cleveland to let doctors review medical images on the iPhone and iPad via a secure network transfer. The application, Mobile MIM, is the first with the FDA’s imprimatur. It allows hospitalists and other physicians to measure distance on the image and image intensity values and display measurement lines, annotations, and regions of interest, according to the FDA.
“Think of how cell phones were perceived a few decades ago; many dismissed ‘anytime access’ as not necessary,” MIM chief technology officer Mark Cain says in an email. “Yet now we know myriad of cases where the cell phone has proven immensely valuable. The same can be said of diagnostic medical image access. How many ways can this improve healthcare? More ways than I can predict.”—RQ
Quality Research
Research Confirms Benefits of ICU Safety Checklists
The value of checklists containing evidence-supported QI interventions to improve ICU outcomes, pioneered at Johns Hopkins in Baltimore, has been confirmed by several recent studies. The Keystone ICU Project, which sought to replicate the Hopkins experience in hospitals across Michigan, succeeded in nearly eliminating bloodstream infections and reducing mortality.1
Based on Medicare claims from 95 study hospitals and comparison data from 11 surrounding states, patients in hospitals using the checklist were significantly more likely to survive a hospital stay. The project was not, however, sufficiently powered to show a significant difference in length of stay.
A second Keystone Project study showed that five simple therapies aimed at lessening the time spent on ventilators, including elevating the head of the bed 30 degrees, giving anticoagulants, and lessening sedation, combined with education and a hospital culture supporting patient safety, reduced cases of ventilator-associated pneumonia by more than 70%.2
A comprehensive, video-conference-based intervention to support implementing six evidence-based quality practices in 15 community hospital ICUs in Canada improved the adoption of these practices. Expert-led forums and educational sessions promoted the sequential dissemination of treatment algorhythms, with a new practice targeted every four months.3—LB
References
- Lipitz-Snyderman A, Steinwachs D, Needham DM, Colantuoni E, Morlock LL, Pronovost PJ. Impact of a statewide intensive care unit quality improvement initiative on hospital mortality and length of stay: retrospective comparative analysis. BMJ. 2011;342:d219.
- Berenholtz SM, Pham JC, Thompson DA, Needhamm et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. Infect Control Hosp Epidemiol. 2011;(4):305-314.
- Scales DC, Dainty K, Hales B. A multifaceted intervention for quality improvement in a network of intensive care units: a cluster randomized trial. JAMA. 2011;305:363-372.
HM-Based Quality Research
Homeless Respite Helps Avoid Rehospitalizations
Some readmissions come about because things fall apart when patients are discharged with a follow-up plan that is not realistic to their circumstances. This is especially true for homeless patients, says Audrey Kuang, MD, a hospitalist at Santa Clara Valley Medical Center (SCVMC) in San Jose, Calif., and medical director of the Santa Clara County Medical Respite Program, a shelter for homeless patients following discharge from seven San Jose area hospitals.
Dr. Kuang described the collaborative program in a plenary presentation for the Research, Innovations, and Clinical Vignettes competition at HM10.
SCVMC is a county safety net hospital, and Dr. Kuang says the hospitalists “see a fair amount of homeless patients with recurrent exacerbations.” Patients given prescriptions for medications they can’t afford, special diets, or instructions for bed rest are then discharged to the street; inevitably, they are readmitted.
Dr. Kuang began tracking patients who had prolonged hospital stays because of homelessness or unsafe social situations. Her presentation to administrators led to participating hospitals contributing $25,000 each to launch the program with a multidisciplinary team, which included Dr. Kuang.
In its first year, 200 referrals were made to the respite program; 60% were accepted. The most common diagnoses were foot fractures, foot infections, and cancer. Quantified clinical outcomes are still being compiled, Dr. Kuang said, although the participating hospitals have reported decreased rehospitalizations and bed days—results documented in other studies of respite programs.1
“The main idea is post-acute medical care and support for homeless patients in need,” she explained. “Hospitalists may feel this is beyond our scope of practice, but it is our responsibility to know what’s going on out there.”—LB
Reference
- Buchanan D, Doblin B, Sai T, Garcia P. The effects of respite care for homeless patients: a cohort study. Am J Public Health. 2006;96:1278-1281.
By The Numbers
$44,000, $46,659, $120,000: EHR Implementation Costs Higher than Medicare Reimbursement
A new study in Health Affairs on the first-year costs of implementing electronic health records (EHR) in a 450-physician North Texas primary-care network doesn’t translate directly to HM, but figures showing that the installation cost is more for an average five-physician practice than Medicare is offering in incentive pay might serve as a warning sign for HM groups looking to build EHR into their practice:
- EHR incentive payments from Medicare over five years: $44,000;
- EHR implementation cost per doctor after first year: $46,659;
- EHR adoption costs per physician, estimated: $120,000.—RQ TH
Tablet technology benefits HM efficiency, patient satisfaction
During my training in the 1990s, my white coat pockets were stuffed with books. The Internet, in its relative infancy, was not easily accessible in the hospital and contained a tiny fraction of its current knowledge. Back then, information was only at your fingertips when it was committed to memory or in your pocket.
Now, the Internet is at every workstation in the hospital, and all orders are entered electronically. Questions about any clinical situation are answered online in a matter of seconds. As a result, I spend much of my time not with my patients but in front of a computer—entering orders, reviewing labs, writing notes, and reading and sending email.
There is tremendous interest in increasing quality of care, patient satisfaction, and improving communication between doctors, patients, and caregivers.
However, our reliance on technology encourages physicians to spend time at computers that might be better spent with the patient. It seems like we could do a better job of integrating technology into a patient-centric hospital environment.
A few years ago, our hospital installed wireless access to our internal computer network and the Internet. To provide computers to the staff on the wards, the hospital now provides two or three COWs (computers on wheels) to each ward. Unfortunately, their physical design leaves a lot to be desired. They are large and bulky, and they can be hard to move around. The physician must stand with these machines between them and the patient, and even taking a few minutes to find one can feel like a burden during a busy day.
In stark contrast, many patients bring their own laptops into the hospital. They are able to research their condition online, and can be more connected at times than the doctor who is expected to know all the answers.
Because I only have been able to access our hospital network while at a COW, nurses’ station, or my desk, I keep a “to do” list on a piece of paper. My desire to keep a short list and promptly enter orders encourages me to get to a computer as often as possible. While entering my username and password dozens of time each day or waiting in line for a workstation, I can't help but think how nice it would be to spend more time on direct patient care and less time dealing with IT logistics.
Recently, I heard about the value of the iPad in a hospital setting from one of my colleagues. Last week, I set off for my first stint on the wards with an iPad, my stethoscope, a pen, and some business cards. My white coat pockets were empty.
I carried this new lightweight computer like a clipboard. Because of its onscreen keyboard and other characteristics (lightweight, small size, lightning-quick Web browsing), I found that I was naturally sitting alongside each patient as I listened to their concerns. When we determined that a switch of medication or diet was appropriate, I made the change quickly and easily without getting up from my seat—never leaving the patient’s side. Email was available to update the patient’s PCP, social worker, or other care team member.
I spent more time with each patient than I could remember. I did not feel the pressure to hurry out of the room to enter orders as soon as possible. Although I did spend time at a computer during the visit, my patients were able to watch me modify their orders and communicate with their outpatient care team.
Much of the mystery that often surrounds the physician/patient relationship was discarded as we sat side by side. I was able to reconcile medications on the computer with the patient watching and helping make sure that no errors were made. Errors might have been prevented since I no longer had to write down the medications on a piece of paper, carry it down the hall, and enter it on to a computer. It certainly saved me time, enabled the correct list to be entered, and could have provided the patient some confidence that it was done right.
My view of the hospital bed is no longer at the foot, standing up, with weighted pockets. It’s seated, in a chair, at the bedside. I hope to soon master the art of maximizing the benefit of my time with the patient with technology more as a collaborative tool and less as an obstacle.
Melissa L.P. Mattison, MD, SFHM, FACP,
associate director of hospital medicine,
Beth Israel Deaconess Medical Center, Boston
During my training in the 1990s, my white coat pockets were stuffed with books. The Internet, in its relative infancy, was not easily accessible in the hospital and contained a tiny fraction of its current knowledge. Back then, information was only at your fingertips when it was committed to memory or in your pocket.
Now, the Internet is at every workstation in the hospital, and all orders are entered electronically. Questions about any clinical situation are answered online in a matter of seconds. As a result, I spend much of my time not with my patients but in front of a computer—entering orders, reviewing labs, writing notes, and reading and sending email.
There is tremendous interest in increasing quality of care, patient satisfaction, and improving communication between doctors, patients, and caregivers.
However, our reliance on technology encourages physicians to spend time at computers that might be better spent with the patient. It seems like we could do a better job of integrating technology into a patient-centric hospital environment.
A few years ago, our hospital installed wireless access to our internal computer network and the Internet. To provide computers to the staff on the wards, the hospital now provides two or three COWs (computers on wheels) to each ward. Unfortunately, their physical design leaves a lot to be desired. They are large and bulky, and they can be hard to move around. The physician must stand with these machines between them and the patient, and even taking a few minutes to find one can feel like a burden during a busy day.
In stark contrast, many patients bring their own laptops into the hospital. They are able to research their condition online, and can be more connected at times than the doctor who is expected to know all the answers.
Because I only have been able to access our hospital network while at a COW, nurses’ station, or my desk, I keep a “to do” list on a piece of paper. My desire to keep a short list and promptly enter orders encourages me to get to a computer as often as possible. While entering my username and password dozens of time each day or waiting in line for a workstation, I can't help but think how nice it would be to spend more time on direct patient care and less time dealing with IT logistics.
Recently, I heard about the value of the iPad in a hospital setting from one of my colleagues. Last week, I set off for my first stint on the wards with an iPad, my stethoscope, a pen, and some business cards. My white coat pockets were empty.
I carried this new lightweight computer like a clipboard. Because of its onscreen keyboard and other characteristics (lightweight, small size, lightning-quick Web browsing), I found that I was naturally sitting alongside each patient as I listened to their concerns. When we determined that a switch of medication or diet was appropriate, I made the change quickly and easily without getting up from my seat—never leaving the patient’s side. Email was available to update the patient’s PCP, social worker, or other care team member.
I spent more time with each patient than I could remember. I did not feel the pressure to hurry out of the room to enter orders as soon as possible. Although I did spend time at a computer during the visit, my patients were able to watch me modify their orders and communicate with their outpatient care team.
Much of the mystery that often surrounds the physician/patient relationship was discarded as we sat side by side. I was able to reconcile medications on the computer with the patient watching and helping make sure that no errors were made. Errors might have been prevented since I no longer had to write down the medications on a piece of paper, carry it down the hall, and enter it on to a computer. It certainly saved me time, enabled the correct list to be entered, and could have provided the patient some confidence that it was done right.
My view of the hospital bed is no longer at the foot, standing up, with weighted pockets. It’s seated, in a chair, at the bedside. I hope to soon master the art of maximizing the benefit of my time with the patient with technology more as a collaborative tool and less as an obstacle.
Melissa L.P. Mattison, MD, SFHM, FACP,
associate director of hospital medicine,
Beth Israel Deaconess Medical Center, Boston
During my training in the 1990s, my white coat pockets were stuffed with books. The Internet, in its relative infancy, was not easily accessible in the hospital and contained a tiny fraction of its current knowledge. Back then, information was only at your fingertips when it was committed to memory or in your pocket.
Now, the Internet is at every workstation in the hospital, and all orders are entered electronically. Questions about any clinical situation are answered online in a matter of seconds. As a result, I spend much of my time not with my patients but in front of a computer—entering orders, reviewing labs, writing notes, and reading and sending email.
There is tremendous interest in increasing quality of care, patient satisfaction, and improving communication between doctors, patients, and caregivers.
However, our reliance on technology encourages physicians to spend time at computers that might be better spent with the patient. It seems like we could do a better job of integrating technology into a patient-centric hospital environment.
A few years ago, our hospital installed wireless access to our internal computer network and the Internet. To provide computers to the staff on the wards, the hospital now provides two or three COWs (computers on wheels) to each ward. Unfortunately, their physical design leaves a lot to be desired. They are large and bulky, and they can be hard to move around. The physician must stand with these machines between them and the patient, and even taking a few minutes to find one can feel like a burden during a busy day.
In stark contrast, many patients bring their own laptops into the hospital. They are able to research their condition online, and can be more connected at times than the doctor who is expected to know all the answers.
Because I only have been able to access our hospital network while at a COW, nurses’ station, or my desk, I keep a “to do” list on a piece of paper. My desire to keep a short list and promptly enter orders encourages me to get to a computer as often as possible. While entering my username and password dozens of time each day or waiting in line for a workstation, I can't help but think how nice it would be to spend more time on direct patient care and less time dealing with IT logistics.
Recently, I heard about the value of the iPad in a hospital setting from one of my colleagues. Last week, I set off for my first stint on the wards with an iPad, my stethoscope, a pen, and some business cards. My white coat pockets were empty.
I carried this new lightweight computer like a clipboard. Because of its onscreen keyboard and other characteristics (lightweight, small size, lightning-quick Web browsing), I found that I was naturally sitting alongside each patient as I listened to their concerns. When we determined that a switch of medication or diet was appropriate, I made the change quickly and easily without getting up from my seat—never leaving the patient’s side. Email was available to update the patient’s PCP, social worker, or other care team member.
I spent more time with each patient than I could remember. I did not feel the pressure to hurry out of the room to enter orders as soon as possible. Although I did spend time at a computer during the visit, my patients were able to watch me modify their orders and communicate with their outpatient care team.
Much of the mystery that often surrounds the physician/patient relationship was discarded as we sat side by side. I was able to reconcile medications on the computer with the patient watching and helping make sure that no errors were made. Errors might have been prevented since I no longer had to write down the medications on a piece of paper, carry it down the hall, and enter it on to a computer. It certainly saved me time, enabled the correct list to be entered, and could have provided the patient some confidence that it was done right.
My view of the hospital bed is no longer at the foot, standing up, with weighted pockets. It’s seated, in a chair, at the bedside. I hope to soon master the art of maximizing the benefit of my time with the patient with technology more as a collaborative tool and less as an obstacle.
Melissa L.P. Mattison, MD, SFHM, FACP,
associate director of hospital medicine,
Beth Israel Deaconess Medical Center, Boston
The Future is Near
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
Satish Misra, MD, a first-year internal-medicine resident at Johns Hopkins School of Medicine in Baltimore, used to carry a guidebook—many schools refer to it as their Red Book—around the hospital; it served as a tutorial on how to handle a litany of common medical problems. Now, Dr. Misra mostly scans his iPhone.
Henry Feldman, MD, a hospitalist at Beth Israel Deaconess Medical Center (BIDMC) in Boston who also serves as chief information architect for Harvard Medical Faculty Physicians, used to lug around a bulky copy of Netter’s Anatomy if he wanted to visually explain to a patient how their endoscopic retrograde cholangiopancreatography (ERCP) would work. Now, he pulls up the medical illustrations via an application on his iPad.
In an increasingly technological society in which there is an “app” for nearly everything, healthcare—and HM in particular—is no exception. The growing prevalence of touchscreen technology, mostly via smartphones and tablet computers, already has had an impact on how some hospitalists do their jobs. That upward trend should continue in the coming years, as both hardware and software technology become even more sophisticated and easy to use.
Of course, there are roadblocks. Patient privacy, wireless security, and the well-known reticence of healthcare as an industry to adopt information technology (IT) changes have—and will continue to—slowed the spread of the new technologies. However, with potential or practical usage already being forged in the arenas of patient interaction, billing and coding, and quality and patient safety initiatives, the integration of interactive devices into a physician’s daily workflow could become as commonplace in 10 years as the presence of hospitalists is today.
Still, the CEO of one software company points out that the presence of innovation alone does not translate to efficacy. The value of mobile and touchscreen technology to hospitalists—both from the hardware and the software perspectives—lies in how much a physician chooses to incorporate it into their daily practice.
“The number-one factor in these things being adopted is: Can you improve the quality of documentation … without negatively impacting a physician’s interaction with the patient?” says Todd Johnson, president of Salar Inc., a Baltimore-based firm that develops software applications for clinical documentation. Touchscreen technology “absolutely does help meet that goal, but it depends on the providers. It truly is different strokes for different folks.”
Steven Peskin, MD, MBA, FACP, executive vice president and CMO of Yardley, Pa.-based MediMedia USA, has long preached the value of digital technology for inpatient care, particularly for hospitalists. He categorizes the latest wave of technology into five silos:
- Smartphones: Powered by operating systems that turn them into pocket-size mini-computers, the smallest and most mobile of these technologies are ubiquitous in society and hospitals alike (see Table 1, right).
- Tablet PCs: Led by the iPad’s debut in April 2010, the product is a larger version of the smartphone; the oversized screen makes it practical to use as a virtual chalkboard to explain topics to patients.
- Peripherals: From blood pressure cuffs produced by iHealth Labs (www.ihealth99.com) and Withings (www.withings.com/en/bloodpressuremonitor) to Mobisante’s prototype plug-in ultrasound probe (www.technologyreview.com/biomedicine/), there is a burgeoning marketplace for devices that serve as accessories to a smartphone or tablet, effectively turning those devices into handheld versions of costly machines. Most are connected to a mobile device via simple plug-in cables.
- Applications: According to Dr. Feldman, “It’s not the mobile device that’s the gate to any of this. It’s the applications you interact with.” App stores already feature medical specialty sections, and the number of offerings is expected to grow exponentially in the coming years.
- Cloud computing: A cloud is a metaphorical moniker for the interactivity and interoperability of different devices, systems, and servers to provide immediate connectivity and access to remote data and processes (http://csrc.nist.gov/groups/SNS/cloud-computing/).

“There’s tremendous potential and power of medical computing systems out there, but the stumbling block is they’re bulky or not effective,” says Larry Nathanson, MD, director of emergency medical informatics for BIDMC’s Department of Emergency Medicine, who served as architect and programmer of the ED Dashboard, the information system that is used at BIDMC and a number of other hospitals. “By improving the user interface, the systems become easier to use and the systems become revolutionary.”
Impact: Cloudy, Optimistic
Experts agree that the exact role mobile and touchscreen technologies will play in hospitalist groups around the country remains murky because the field is still a novel one, mostly devoid of evidence-based conclusions. In one of the first planned research studies, the two-year-old University of Central Florida College of Medicine in Orlando has provided iPads to each student in order to research the use of technology in medical education.
Regardless, physicians and tablet manufacturers alike agree that the point-of-service efficiency offered by mobile devices inherently allows their users to be more efficient. Several hospitalists have taken to the Internet, touting how mobile devices have streamlined their efficiency. One popular (and anonymous) blogger, The Happy Hospitalist (http://thehappyhospitalist.blogspot.com/), noted in two recent posts how they were able to round on 16 patients in less than 4 1/2 hours using an iPhone or iPad. On one of those days, the blogger discharged 13 of those patients.
“I no longer have to walk back and forth between patient rooms and nursing stations,” according to The Happy Hospitalist. “I can just drink my coffee at the bedside. I don’t have to fight with other doctors and nurses to log into a paucity of computers that are often way too slow and way too unpredictable. I just sync my iPhone with the patient database app on my iPhone screen and I’m up and running with a real-time update of all my patient’s information.”
The mobile devices allow faster, possibly better, interactions with patients, Dr. Feldman says. For example, a patient tells their hospitalist they need a change to their pain medication. Having a handheld touchscreen device linked to other technologies allows the order to be placed instantly. It even can send the nursing station an alert to the change. The sloppiness of a handwritten note is taken out of play; plus, rounding never misses a beat. “I’m terrible at remembering what I wrote down six patients ago,” Dr. Feldman admits. “Ultimately, for saving money, if I can get things done sooner, theoretically, length of stay can be reduced. That hasn’t been studied, but it is common sense.”
Dr. Feldman, who describes himself as a “hardcore code jockey,” says hospitalists would do well to work closely with their IT staffs to help conceptualize and design in-house applications and interoperability that would make their jobs easier. In institutions with an informatics department, that conversation could be as simple as a one-on-one conversation between an HM group leader and the IT department head.
In other hospitals, a field trip can help. “We will take IT staff out on the wards,” Dr. Feldman explains. “Come observe the process you’re automating. When they come back, they’re very sobered.”
Dr. Misra, the Johns Hopkins intern, notes that mobile devices are perfect hosts for checklists. Their ease of use can even be viewed as a potential motivator to ensure that those checklists are completed, particularly for younger physicians who have either grown up with or started their careers with more exposure to technology than previous generations.
“The biggest strength of touchscreen technology is it’s interactive,” Dr. Misra says. “It’s fun to use, much more fun than checking off boxes on a piece of paper or on a computer screen.
“It’s portable, it’s lightweight, it’s where you are.”
Trouble Spots
The virtually limitless boundaries for touchscreen technology to replace functions in the hospitalist’s workflow is, of course, limited in one glaring respect: privacy. The security of devices, applications, or peripherals must be paramount to their effectiveness, Dr. Feldman says, adding patient information must “remain sacrosanct.”
At BIDMC, digital security is accomplished in part via a bifurcated wireless network that allows physicians access to a secure connection while simultaneously and transparently maintaining a free wireless network for patients and visitors. Not all hospitals can afford the infrastructure necessary for such a setup. And even for health systems that have separate wireless systems, the connectivity cuts both ways, says Mike Stinson, vice president of marketing for Motion in Computing, an Austin, Texas, firm that produces tablet computers for multiple industries, including healthcare.
“Are you willing to have every file on your personal system viewable and accessible by the IT guys so they can make sure you don’t have access to something you shouldn’t have access to?” Stinson asks. “It seems easy and appealing, but there are larger issues.”
Stinson says the privacy and safety concerns of the technology can be addressed. Even potential fears regarding the sterility of the equipment might be simply solved. To wit, a column in the Journal of Surgical Radiology in January found that the device worked well when put in an X-ray cassette sealed off with a hemostat.1
Dr. Nathanson, an ED physician who has worked closely with hospitalists at BIDMC in the past, says it’s clear to him that making the technology easy enough to use in a medical setting is no longer the hurdle. It’s the systemic timidity of physicians who are slow to endorse and incorporate cutting-edge technology into entrenched work patterns.
“In medicine, it tends to take a long time,” he says. “The adoption of technology in medicine can be very challenging. If nothing else, we’re very early in the process.” TH
Richard Quinn is a freelance writer based in New Jersey.
Reference
- Wodajo, FM. The iPad in the hospital and operating room. Journal of Surgical Radiology website. Available at: www.surgisphere.com/SurgRad/issues/volume-2/1-january-2011—pages-1-112/152-column-the-ipad-in-the-hospital-and-operating-room.html. Accessed Jan. 3, 2011.
How You Can Save Your Hospital a Million Bucks
What is value-based purchasing (VBP) and why should I care? Well, for starters, your hospital’s CFO might not know that starting in 2013 (just two years from now), the Centers for Medicare & Medicaid Services (CMS) will be withholding at least 1% of all Medicare payments, but CMS is giving your hospital a chance to get some or all of that money back. For a busy hospital, the withholding will easily be $1 million; for many hospitals, that figure is more like $2 million to $3 million.
SHM thinks hospitalists are uniquely positioned to be champions for the C-suite, helping the hospital’s balance sheet, aiding in staff retention, and providing better care for our patients. And that’s where VBP comes in.
In March 2010, Congress passed the Patient Protection and Affordable Care Act (see “Health Reform Turns 1,” p. 16). This law includes a provision that establishes a VBP program for hospital payments beginning with discharges on Oct. 1, 2012. Payment will be based on hospital performance on quality measures determined by Health and Human Services (HHS). The VBP program will pay hospitals for their actual performance on quality measures, rather than for just reporting those measures, starting in 2013.
This is a null-set game, in which the funding for the best performers is clearly coming out of the hide of low-performing hospitals. Funding will be phased in from 2013 through 2017. Hospitals will have their payments for all Medicare DRGs reduced by 1% in 2013, 1.25% in 2014, 1.5% in 2015, 1.75% in 2016, and 2% in 2017 and beyond. Just ask your CFO what this means at your hospital and see his or her brow furrow.
The good news (i.e. carrot) is that a hospital that meets or exceeds the performance standards will be eligible to earn back all the Medicare money that was withheld and even earn a bonus of as much as 2%.
VBP Metrics
So just what performance will be measured in the new VBP program? While physicians might see quality in clinical terms, the VBP program defines performance more broadly; that means it includes the patient experience. In fact, about 70% of the quality measures will be based on clinical performance, and a full 30% will come from scores on post-discharge patient satisfaction questionnaires (e.g. HCAHPS). To understand the importance of the patient satisfaction part of the VBP equation, just note that Press Ganey, the largest private company helping hospitals understand what their customers are thinking, is jumping into the VBP arena with both feet. Your hospital’s CFO (and lead hospitalist) should contact Press Ganey and run your current performance numbers through their VBP calculator to see if you are on the hilltop or in a deep hole.
The clinical measures will be selected from those used in the current Medicare pay-for-reporting program and likely will include measures for myocardial infarction, heart failure, pneumonia, and surgical care. In addition, HHS is mandated to include measures of efficiency, looking at ways to assess the spending per Medicare beneficiary. This is the real value equation: value = outcomes ÷ cost.
HM to the Rescue
No one in the hospital community sits more at the nexus of clinical care on these measures, efficiency, and the patient experience than hospitalists. This is an opportunity and a risk for hospitalists; that is why SHM is actively planning strategies to help hospitalists assist their hospitals in assessing how their current performance would play out in the payment world post-2013. In addition, SHM will have tools to assist hospitalists in creating change to help their institutions be in the top half of the nation’s hospitals—those who will get their millions of withheld dollars back.
SHM’s board of directors recently passed the following position statement on value-based purchasing:
“SHM supports the Affordable Care Act (ACA) Section 3001 directing the Secretary of HHS to establish a value-based purchasing program under the hospital inpatient prospective payment system. We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment. We are pleased that under ACA the Secretary will establish performance standards that reward hospitals based on either attaining a certain performance standard or making improvements relative to a previous performance period. Hospitalists, who care for more hospitalized patients than any other physician group and lead system change and quality improvement efforts, will be critical to improving the performance of hospitals under this program.”
As mentioned above, the VBP program poses some risks to hospitalists. We cannot improve our hospital’s performance by ourselves, no matter how well motivated and trained we are. Hospitalists tend to attract a group of patients who traditionally have less satisfaction with their hospital experience (e.g. acutely ill patients admitted through the ED). But for more than a decade, hospitalists have been touting our goal to change the system for the better and to strive to be rewarded for value and performance, not simply for the doing.
In some ways, hospitals’ financial support of hospitalist groups has been predicated on the value we currently provide in efficiency (e.g. decreased length of stay, better use of resources) and effectiveness (e.g. improved measurable quality). The VBP program in ACA is just a first big step for the largest payor of hospital care—CMS—to change the ground rules.
Well-prepared hospitalists can provide leadership and help deliver their institutions to the top half of hospitals (those that will receive bonus payment) and, at the same time, begin to change the culture of their hospital to provide their patients with a better clinical outcome and a better patient experience.
Congress and President Obama are our allies here. A million dollars should get your hospital executives’ attention. Now is the time for hospitalists—with SHM’s help—to step up and show what we can do. TH
Dr. Wellikson is CEO of SHM.
What is value-based purchasing (VBP) and why should I care? Well, for starters, your hospital’s CFO might not know that starting in 2013 (just two years from now), the Centers for Medicare & Medicaid Services (CMS) will be withholding at least 1% of all Medicare payments, but CMS is giving your hospital a chance to get some or all of that money back. For a busy hospital, the withholding will easily be $1 million; for many hospitals, that figure is more like $2 million to $3 million.
SHM thinks hospitalists are uniquely positioned to be champions for the C-suite, helping the hospital’s balance sheet, aiding in staff retention, and providing better care for our patients. And that’s where VBP comes in.
In March 2010, Congress passed the Patient Protection and Affordable Care Act (see “Health Reform Turns 1,” p. 16). This law includes a provision that establishes a VBP program for hospital payments beginning with discharges on Oct. 1, 2012. Payment will be based on hospital performance on quality measures determined by Health and Human Services (HHS). The VBP program will pay hospitals for their actual performance on quality measures, rather than for just reporting those measures, starting in 2013.
This is a null-set game, in which the funding for the best performers is clearly coming out of the hide of low-performing hospitals. Funding will be phased in from 2013 through 2017. Hospitals will have their payments for all Medicare DRGs reduced by 1% in 2013, 1.25% in 2014, 1.5% in 2015, 1.75% in 2016, and 2% in 2017 and beyond. Just ask your CFO what this means at your hospital and see his or her brow furrow.
The good news (i.e. carrot) is that a hospital that meets or exceeds the performance standards will be eligible to earn back all the Medicare money that was withheld and even earn a bonus of as much as 2%.
VBP Metrics
So just what performance will be measured in the new VBP program? While physicians might see quality in clinical terms, the VBP program defines performance more broadly; that means it includes the patient experience. In fact, about 70% of the quality measures will be based on clinical performance, and a full 30% will come from scores on post-discharge patient satisfaction questionnaires (e.g. HCAHPS). To understand the importance of the patient satisfaction part of the VBP equation, just note that Press Ganey, the largest private company helping hospitals understand what their customers are thinking, is jumping into the VBP arena with both feet. Your hospital’s CFO (and lead hospitalist) should contact Press Ganey and run your current performance numbers through their VBP calculator to see if you are on the hilltop or in a deep hole.
The clinical measures will be selected from those used in the current Medicare pay-for-reporting program and likely will include measures for myocardial infarction, heart failure, pneumonia, and surgical care. In addition, HHS is mandated to include measures of efficiency, looking at ways to assess the spending per Medicare beneficiary. This is the real value equation: value = outcomes ÷ cost.
HM to the Rescue
No one in the hospital community sits more at the nexus of clinical care on these measures, efficiency, and the patient experience than hospitalists. This is an opportunity and a risk for hospitalists; that is why SHM is actively planning strategies to help hospitalists assist their hospitals in assessing how their current performance would play out in the payment world post-2013. In addition, SHM will have tools to assist hospitalists in creating change to help their institutions be in the top half of the nation’s hospitals—those who will get their millions of withheld dollars back.
SHM’s board of directors recently passed the following position statement on value-based purchasing:
“SHM supports the Affordable Care Act (ACA) Section 3001 directing the Secretary of HHS to establish a value-based purchasing program under the hospital inpatient prospective payment system. We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment. We are pleased that under ACA the Secretary will establish performance standards that reward hospitals based on either attaining a certain performance standard or making improvements relative to a previous performance period. Hospitalists, who care for more hospitalized patients than any other physician group and lead system change and quality improvement efforts, will be critical to improving the performance of hospitals under this program.”
As mentioned above, the VBP program poses some risks to hospitalists. We cannot improve our hospital’s performance by ourselves, no matter how well motivated and trained we are. Hospitalists tend to attract a group of patients who traditionally have less satisfaction with their hospital experience (e.g. acutely ill patients admitted through the ED). But for more than a decade, hospitalists have been touting our goal to change the system for the better and to strive to be rewarded for value and performance, not simply for the doing.
In some ways, hospitals’ financial support of hospitalist groups has been predicated on the value we currently provide in efficiency (e.g. decreased length of stay, better use of resources) and effectiveness (e.g. improved measurable quality). The VBP program in ACA is just a first big step for the largest payor of hospital care—CMS—to change the ground rules.
Well-prepared hospitalists can provide leadership and help deliver their institutions to the top half of hospitals (those that will receive bonus payment) and, at the same time, begin to change the culture of their hospital to provide their patients with a better clinical outcome and a better patient experience.
Congress and President Obama are our allies here. A million dollars should get your hospital executives’ attention. Now is the time for hospitalists—with SHM’s help—to step up and show what we can do. TH
Dr. Wellikson is CEO of SHM.
What is value-based purchasing (VBP) and why should I care? Well, for starters, your hospital’s CFO might not know that starting in 2013 (just two years from now), the Centers for Medicare & Medicaid Services (CMS) will be withholding at least 1% of all Medicare payments, but CMS is giving your hospital a chance to get some or all of that money back. For a busy hospital, the withholding will easily be $1 million; for many hospitals, that figure is more like $2 million to $3 million.
SHM thinks hospitalists are uniquely positioned to be champions for the C-suite, helping the hospital’s balance sheet, aiding in staff retention, and providing better care for our patients. And that’s where VBP comes in.
In March 2010, Congress passed the Patient Protection and Affordable Care Act (see “Health Reform Turns 1,” p. 16). This law includes a provision that establishes a VBP program for hospital payments beginning with discharges on Oct. 1, 2012. Payment will be based on hospital performance on quality measures determined by Health and Human Services (HHS). The VBP program will pay hospitals for their actual performance on quality measures, rather than for just reporting those measures, starting in 2013.
This is a null-set game, in which the funding for the best performers is clearly coming out of the hide of low-performing hospitals. Funding will be phased in from 2013 through 2017. Hospitals will have their payments for all Medicare DRGs reduced by 1% in 2013, 1.25% in 2014, 1.5% in 2015, 1.75% in 2016, and 2% in 2017 and beyond. Just ask your CFO what this means at your hospital and see his or her brow furrow.
The good news (i.e. carrot) is that a hospital that meets or exceeds the performance standards will be eligible to earn back all the Medicare money that was withheld and even earn a bonus of as much as 2%.
VBP Metrics
So just what performance will be measured in the new VBP program? While physicians might see quality in clinical terms, the VBP program defines performance more broadly; that means it includes the patient experience. In fact, about 70% of the quality measures will be based on clinical performance, and a full 30% will come from scores on post-discharge patient satisfaction questionnaires (e.g. HCAHPS). To understand the importance of the patient satisfaction part of the VBP equation, just note that Press Ganey, the largest private company helping hospitals understand what their customers are thinking, is jumping into the VBP arena with both feet. Your hospital’s CFO (and lead hospitalist) should contact Press Ganey and run your current performance numbers through their VBP calculator to see if you are on the hilltop or in a deep hole.
The clinical measures will be selected from those used in the current Medicare pay-for-reporting program and likely will include measures for myocardial infarction, heart failure, pneumonia, and surgical care. In addition, HHS is mandated to include measures of efficiency, looking at ways to assess the spending per Medicare beneficiary. This is the real value equation: value = outcomes ÷ cost.
HM to the Rescue
No one in the hospital community sits more at the nexus of clinical care on these measures, efficiency, and the patient experience than hospitalists. This is an opportunity and a risk for hospitalists; that is why SHM is actively planning strategies to help hospitalists assist their hospitals in assessing how their current performance would play out in the payment world post-2013. In addition, SHM will have tools to assist hospitalists in creating change to help their institutions be in the top half of the nation’s hospitals—those who will get their millions of withheld dollars back.
SHM’s board of directors recently passed the following position statement on value-based purchasing:
“SHM supports the Affordable Care Act (ACA) Section 3001 directing the Secretary of HHS to establish a value-based purchasing program under the hospital inpatient prospective payment system. We believe that the Medicare reimbursement system must be changed to promote value, and we strongly support policies that link quality measurement to performance-based payment. We are pleased that under ACA the Secretary will establish performance standards that reward hospitals based on either attaining a certain performance standard or making improvements relative to a previous performance period. Hospitalists, who care for more hospitalized patients than any other physician group and lead system change and quality improvement efforts, will be critical to improving the performance of hospitals under this program.”
As mentioned above, the VBP program poses some risks to hospitalists. We cannot improve our hospital’s performance by ourselves, no matter how well motivated and trained we are. Hospitalists tend to attract a group of patients who traditionally have less satisfaction with their hospital experience (e.g. acutely ill patients admitted through the ED). But for more than a decade, hospitalists have been touting our goal to change the system for the better and to strive to be rewarded for value and performance, not simply for the doing.
In some ways, hospitals’ financial support of hospitalist groups has been predicated on the value we currently provide in efficiency (e.g. decreased length of stay, better use of resources) and effectiveness (e.g. improved measurable quality). The VBP program in ACA is just a first big step for the largest payor of hospital care—CMS—to change the ground rules.
Well-prepared hospitalists can provide leadership and help deliver their institutions to the top half of hospitals (those that will receive bonus payment) and, at the same time, begin to change the culture of their hospital to provide their patients with a better clinical outcome and a better patient experience.
Congress and President Obama are our allies here. A million dollars should get your hospital executives’ attention. Now is the time for hospitalists—with SHM’s help—to step up and show what we can do. TH
Dr. Wellikson is CEO of SHM.