User login
Quality Data Dashboards Provide Performance Feedback to Physicians
A best-of-research plenary presentation at HM15 in National Harbor, Md., described a project to link physicians’ schedules to the electronic health record (EHR) in order to provide real-time, individualized performance feedback on key quality improvement and value metrics.
The abstract’s lead author, Victoria Valencia, MPH, a research data and project manager at the University of California San Francisco (UCSF), explains that quality improvement priorities have driven feedback of quality metrics at the department level.
“Where I came in was to try to get the same quality metrics down to the level of the team,” she says. “We take data from our EPIC EHR, clean it up by removing outliers, merge it with our online scheduling program, and provide a robust visual presentation of individualized, real-time performance feedback to the clinical team.”
–Dr. Valencia
One example is counting the total number of phlebotomy “sticks” per day, per patient. Reporting this data helped to reduce the number of “sticks per day” by 20%, to 1.6 from 2.0. A similar approach is used for care transitions and the percentage of discharges with high-quality, after-visit summaries.
“The feedback is timely and actionable and allows the teams to address areas needing improvement,” Valencia says.
How have the doctors responded to this feedback?
“Our division is used to receiving quality feedback as part of an ongoing process that includes working meetings where the metrics are reviewed,” she says, adding that there hasn’t been pushback from the teams over these reports.
A best-of-research plenary presentation at HM15 in National Harbor, Md., described a project to link physicians’ schedules to the electronic health record (EHR) in order to provide real-time, individualized performance feedback on key quality improvement and value metrics.
The abstract’s lead author, Victoria Valencia, MPH, a research data and project manager at the University of California San Francisco (UCSF), explains that quality improvement priorities have driven feedback of quality metrics at the department level.
“Where I came in was to try to get the same quality metrics down to the level of the team,” she says. “We take data from our EPIC EHR, clean it up by removing outliers, merge it with our online scheduling program, and provide a robust visual presentation of individualized, real-time performance feedback to the clinical team.”
–Dr. Valencia
One example is counting the total number of phlebotomy “sticks” per day, per patient. Reporting this data helped to reduce the number of “sticks per day” by 20%, to 1.6 from 2.0. A similar approach is used for care transitions and the percentage of discharges with high-quality, after-visit summaries.
“The feedback is timely and actionable and allows the teams to address areas needing improvement,” Valencia says.
How have the doctors responded to this feedback?
“Our division is used to receiving quality feedback as part of an ongoing process that includes working meetings where the metrics are reviewed,” she says, adding that there hasn’t been pushback from the teams over these reports.
A best-of-research plenary presentation at HM15 in National Harbor, Md., described a project to link physicians’ schedules to the electronic health record (EHR) in order to provide real-time, individualized performance feedback on key quality improvement and value metrics.
The abstract’s lead author, Victoria Valencia, MPH, a research data and project manager at the University of California San Francisco (UCSF), explains that quality improvement priorities have driven feedback of quality metrics at the department level.
“Where I came in was to try to get the same quality metrics down to the level of the team,” she says. “We take data from our EPIC EHR, clean it up by removing outliers, merge it with our online scheduling program, and provide a robust visual presentation of individualized, real-time performance feedback to the clinical team.”
–Dr. Valencia
One example is counting the total number of phlebotomy “sticks” per day, per patient. Reporting this data helped to reduce the number of “sticks per day” by 20%, to 1.6 from 2.0. A similar approach is used for care transitions and the percentage of discharges with high-quality, after-visit summaries.
“The feedback is timely and actionable and allows the teams to address areas needing improvement,” Valencia says.
How have the doctors responded to this feedback?
“Our division is used to receiving quality feedback as part of an ongoing process that includes working meetings where the metrics are reviewed,” she says, adding that there hasn’t been pushback from the teams over these reports.
Why Physicians Override Best Practice Alerts
Research published earlier this year in the Journal of Hospital Medicine finds that rationales offered by physicians for overriding interruptive, computerized best practice alerts (BPAs) regarding whether or not to give blood transfusions vary widely, including specialty service protocolized behaviors, anticipation of surgical or procedural interventions, and imminent hospital transfers.
The electronic health record at Stanford University Medical Center in Palo Alto, Calif., has an automated alert function to check reported hemoglobin level and trigger a pop-up reminder when a doctor orders a transfusion for a patient with a hemoglobin level of 9 or above—outside of the recognized guidelines—prompting the doctor to either abort the transfusion or provide a reason for the override, explains co-author Lisa Shieh, MD, PhD, FHM, medical director of quality in the department of medicine at Stanford.
“Our study was trying to understand why providers still transfuse, even when we provide just-in-time education on transfusion recommendations,” she says. “We can’t say that all of these orders are inappropriate. But, for many reasons, blood has harms and is costly.
“We want to convey an overall understanding about why this issue is important.”
Although a substantial number of transfusions continue outside of the recommended guidelines, Stanford has reduced its numbers significantly.
“I’m a big believer in clinical decision support … if it’s designed well and doesn’t add to alert fatigue,” Dr. Shieh says. “I think this BPA was effective in education and making people stop and think why they were ordering transfusions. Our next step will be to look at the outlier practices and maybe have a conversation with them, doctor to doctor.”
Stanford is looking at sepsis treatment as a next target.
Research published earlier this year in the Journal of Hospital Medicine finds that rationales offered by physicians for overriding interruptive, computerized best practice alerts (BPAs) regarding whether or not to give blood transfusions vary widely, including specialty service protocolized behaviors, anticipation of surgical or procedural interventions, and imminent hospital transfers.
The electronic health record at Stanford University Medical Center in Palo Alto, Calif., has an automated alert function to check reported hemoglobin level and trigger a pop-up reminder when a doctor orders a transfusion for a patient with a hemoglobin level of 9 or above—outside of the recognized guidelines—prompting the doctor to either abort the transfusion or provide a reason for the override, explains co-author Lisa Shieh, MD, PhD, FHM, medical director of quality in the department of medicine at Stanford.
“Our study was trying to understand why providers still transfuse, even when we provide just-in-time education on transfusion recommendations,” she says. “We can’t say that all of these orders are inappropriate. But, for many reasons, blood has harms and is costly.
“We want to convey an overall understanding about why this issue is important.”
Although a substantial number of transfusions continue outside of the recommended guidelines, Stanford has reduced its numbers significantly.
“I’m a big believer in clinical decision support … if it’s designed well and doesn’t add to alert fatigue,” Dr. Shieh says. “I think this BPA was effective in education and making people stop and think why they were ordering transfusions. Our next step will be to look at the outlier practices and maybe have a conversation with them, doctor to doctor.”
Stanford is looking at sepsis treatment as a next target.
Research published earlier this year in the Journal of Hospital Medicine finds that rationales offered by physicians for overriding interruptive, computerized best practice alerts (BPAs) regarding whether or not to give blood transfusions vary widely, including specialty service protocolized behaviors, anticipation of surgical or procedural interventions, and imminent hospital transfers.
The electronic health record at Stanford University Medical Center in Palo Alto, Calif., has an automated alert function to check reported hemoglobin level and trigger a pop-up reminder when a doctor orders a transfusion for a patient with a hemoglobin level of 9 or above—outside of the recognized guidelines—prompting the doctor to either abort the transfusion or provide a reason for the override, explains co-author Lisa Shieh, MD, PhD, FHM, medical director of quality in the department of medicine at Stanford.
“Our study was trying to understand why providers still transfuse, even when we provide just-in-time education on transfusion recommendations,” she says. “We can’t say that all of these orders are inappropriate. But, for many reasons, blood has harms and is costly.
“We want to convey an overall understanding about why this issue is important.”
Although a substantial number of transfusions continue outside of the recommended guidelines, Stanford has reduced its numbers significantly.
“I’m a big believer in clinical decision support … if it’s designed well and doesn’t add to alert fatigue,” Dr. Shieh says. “I think this BPA was effective in education and making people stop and think why they were ordering transfusions. Our next step will be to look at the outlier practices and maybe have a conversation with them, doctor to doctor.”
Stanford is looking at sepsis treatment as a next target.
Hospitals with Hotel-Like Amenities Don’t Improve Satisfaction Scores
Hospital design may not contribute to patients’ satisfaction with the care given by their hospital professionals, according to new research from Johns Hopkins Hospital in Baltimore, published in the Journal of Hospital Medicine. Newly built hospitals often emphasize patient-centered features like reduced noise, natural light, visitor-friendly facilities, well-designed rooms, and hotel-like amenities, note the authors, led by Zishan Siddiqui, MD, attending physician and assistant professor of medicine at Johns Hopkins.
When Hopkins moved a number of its hospital units to the sleek new Sheikh Zayed Tower in 2012, researchers used a pre-post design experiment to compare patient satisfaction in the newer, more pleasing surroundings via Press Ganey and HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey scores. Patients responded positively to the new environment, with significant improvement in facility-related satisfaction, but were able to distinguish that satisfaction from their ratings of their doctors and nurses, which were not impacted by the new environment.
“It is more likely that provider-level interventions will have a greater impact on provider level and overall satisfaction,” the authors conclude. “Hospital administrators should not use outdated facilities as an excuse for suboptimal provider satisfaction scores.”
Hospital design may not contribute to patients’ satisfaction with the care given by their hospital professionals, according to new research from Johns Hopkins Hospital in Baltimore, published in the Journal of Hospital Medicine. Newly built hospitals often emphasize patient-centered features like reduced noise, natural light, visitor-friendly facilities, well-designed rooms, and hotel-like amenities, note the authors, led by Zishan Siddiqui, MD, attending physician and assistant professor of medicine at Johns Hopkins.
When Hopkins moved a number of its hospital units to the sleek new Sheikh Zayed Tower in 2012, researchers used a pre-post design experiment to compare patient satisfaction in the newer, more pleasing surroundings via Press Ganey and HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey scores. Patients responded positively to the new environment, with significant improvement in facility-related satisfaction, but were able to distinguish that satisfaction from their ratings of their doctors and nurses, which were not impacted by the new environment.
“It is more likely that provider-level interventions will have a greater impact on provider level and overall satisfaction,” the authors conclude. “Hospital administrators should not use outdated facilities as an excuse for suboptimal provider satisfaction scores.”
Hospital design may not contribute to patients’ satisfaction with the care given by their hospital professionals, according to new research from Johns Hopkins Hospital in Baltimore, published in the Journal of Hospital Medicine. Newly built hospitals often emphasize patient-centered features like reduced noise, natural light, visitor-friendly facilities, well-designed rooms, and hotel-like amenities, note the authors, led by Zishan Siddiqui, MD, attending physician and assistant professor of medicine at Johns Hopkins.
When Hopkins moved a number of its hospital units to the sleek new Sheikh Zayed Tower in 2012, researchers used a pre-post design experiment to compare patient satisfaction in the newer, more pleasing surroundings via Press Ganey and HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) survey scores. Patients responded positively to the new environment, with significant improvement in facility-related satisfaction, but were able to distinguish that satisfaction from their ratings of their doctors and nurses, which were not impacted by the new environment.
“It is more likely that provider-level interventions will have a greater impact on provider level and overall satisfaction,” the authors conclude. “Hospital administrators should not use outdated facilities as an excuse for suboptimal provider satisfaction scores.”
Implementing Physician Value-Based Purchasing in Your Practice: HM15 Session Analysis
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
Hot Topics in Practice Management; HM15 Session Analysis
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
LISTEN NOW: Bob Wachter, MD, MHM discusses the many facets of healthcare IT
Listen to more of our interview with Bob Wachter, MD, MHM, on the gains, losses, and consequences resulting from healthcare IT.
Listen to more of our interview with Bob Wachter, MD, MHM, on the gains, losses, and consequences resulting from healthcare IT.
Listen to more of our interview with Bob Wachter, MD, MHM, on the gains, losses, and consequences resulting from healthcare IT.
Lean Six Sigma Improves Pediatric Discharge Times
Research published online in the Journal of Hospital Medicine shows how quality improvement incorporating Lean Six Sigma, rigorous, problem-focused process improvement methodologies, improved pediatric hospital discharge times. Michael J. Beck, MD, FAAP, SSGB, chief of the division of pediatric hospital medicine at Penn State Hershey Children’s Hospital in Pa., and Kirk Gosik of the department of public health sciences at Penn State Hershey College of Medicine assessed the impact of these methods on times from placement of discharge orders to discharge from the hospital, along with secondary outcomes of length of stay and readmissions rates.
“In our hospital, we did not have enough beds for what we were being asked to accomplish,” Dr. Beck says. “The process and structure of going through rounds and discharging patients wasn’t working. Based on a lot of calls from the ER, we decided to try a one-month pilot of restructuring the daily rounds to improve throughput.”
Reengineering included reallocating staff and creating a standardized work flow and discharge checklist. The rounding team was split into two smaller teams, with patients planned for discharge that day seen first and the necessary discharge paperwork entered into the electronic health record during the rounding.
The new process resulted in significantly faster times for order entry and for actual patient discharge, with a larger proportion of patients discharged before noon and before 2 p.m. The project has continued, using a PDSA (plan/do/study/act) process to advance and consolidate its gains. It appears to be sustainable, Dr. Beck says, and 13 months of data were to be presented as an abstract at HM15 in National Harbor, Md.
Larry Beresford is a freelance writer in Alameda, Calif.
Research published online in the Journal of Hospital Medicine shows how quality improvement incorporating Lean Six Sigma, rigorous, problem-focused process improvement methodologies, improved pediatric hospital discharge times. Michael J. Beck, MD, FAAP, SSGB, chief of the division of pediatric hospital medicine at Penn State Hershey Children’s Hospital in Pa., and Kirk Gosik of the department of public health sciences at Penn State Hershey College of Medicine assessed the impact of these methods on times from placement of discharge orders to discharge from the hospital, along with secondary outcomes of length of stay and readmissions rates.
“In our hospital, we did not have enough beds for what we were being asked to accomplish,” Dr. Beck says. “The process and structure of going through rounds and discharging patients wasn’t working. Based on a lot of calls from the ER, we decided to try a one-month pilot of restructuring the daily rounds to improve throughput.”
Reengineering included reallocating staff and creating a standardized work flow and discharge checklist. The rounding team was split into two smaller teams, with patients planned for discharge that day seen first and the necessary discharge paperwork entered into the electronic health record during the rounding.
The new process resulted in significantly faster times for order entry and for actual patient discharge, with a larger proportion of patients discharged before noon and before 2 p.m. The project has continued, using a PDSA (plan/do/study/act) process to advance and consolidate its gains. It appears to be sustainable, Dr. Beck says, and 13 months of data were to be presented as an abstract at HM15 in National Harbor, Md.
Larry Beresford is a freelance writer in Alameda, Calif.
Research published online in the Journal of Hospital Medicine shows how quality improvement incorporating Lean Six Sigma, rigorous, problem-focused process improvement methodologies, improved pediatric hospital discharge times. Michael J. Beck, MD, FAAP, SSGB, chief of the division of pediatric hospital medicine at Penn State Hershey Children’s Hospital in Pa., and Kirk Gosik of the department of public health sciences at Penn State Hershey College of Medicine assessed the impact of these methods on times from placement of discharge orders to discharge from the hospital, along with secondary outcomes of length of stay and readmissions rates.
“In our hospital, we did not have enough beds for what we were being asked to accomplish,” Dr. Beck says. “The process and structure of going through rounds and discharging patients wasn’t working. Based on a lot of calls from the ER, we decided to try a one-month pilot of restructuring the daily rounds to improve throughput.”
Reengineering included reallocating staff and creating a standardized work flow and discharge checklist. The rounding team was split into two smaller teams, with patients planned for discharge that day seen first and the necessary discharge paperwork entered into the electronic health record during the rounding.
The new process resulted in significantly faster times for order entry and for actual patient discharge, with a larger proportion of patients discharged before noon and before 2 p.m. The project has continued, using a PDSA (plan/do/study/act) process to advance and consolidate its gains. It appears to be sustainable, Dr. Beck says, and 13 months of data were to be presented as an abstract at HM15 in National Harbor, Md.
Larry Beresford is a freelance writer in Alameda, Calif.
Good Hospital Discharge Summaries Identified
A Yale University research team has described what constitutes a good hospital discharge, based on its analysis of 1,500 discharge summaries from patients with exacerbations of heart failure at 46 hospitals enrolled in TeleMonitoring to Improve Heart Failure Outcomes (TELE-HF), a large multicenter study of patients hospitalized with heart failure.
“We consider a good discharge to be a three-legged stool composed of timeliness, transmission to the right person, and having the right components, as defined by The Joint Commission and the Transitions of Care Consensus Conference,” says co-author Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University.
“This study tells us for the first time that it is actually worth spending the time and effort to improve discharge communication, and patients do seem to benefit.”—Leora Horwitz, MD, MHS
Historically, discharge summaries were used primarily for billing, but the medical community has not made full use of them as tools for transition or considered what was really needed by the physician who will see the patient next, Dr. Horwitz says. In a previous study at Yale, as many as a third of discharge summaries were never received by a follow-up physician, and only 15% included the patient’s discharge weight—an essential detail for managing their cardiac care.
A second study using the TELE-HF data found that when the quality of the discharge summary was improved, readmissions rates were lower.
“This study tells us for the first time that it is actually worth spending the time and effort to improve discharge communication, and patients do seem to benefit,” Dr. Horwitz says.
Individual physicians should feel empowered by the result to work on system change in their hospitals, she says.
Larry Beresford is a freelance writer in Alameda, Calif.
A Yale University research team has described what constitutes a good hospital discharge, based on its analysis of 1,500 discharge summaries from patients with exacerbations of heart failure at 46 hospitals enrolled in TeleMonitoring to Improve Heart Failure Outcomes (TELE-HF), a large multicenter study of patients hospitalized with heart failure.
“We consider a good discharge to be a three-legged stool composed of timeliness, transmission to the right person, and having the right components, as defined by The Joint Commission and the Transitions of Care Consensus Conference,” says co-author Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University.
“This study tells us for the first time that it is actually worth spending the time and effort to improve discharge communication, and patients do seem to benefit.”—Leora Horwitz, MD, MHS
Historically, discharge summaries were used primarily for billing, but the medical community has not made full use of them as tools for transition or considered what was really needed by the physician who will see the patient next, Dr. Horwitz says. In a previous study at Yale, as many as a third of discharge summaries were never received by a follow-up physician, and only 15% included the patient’s discharge weight—an essential detail for managing their cardiac care.
A second study using the TELE-HF data found that when the quality of the discharge summary was improved, readmissions rates were lower.
“This study tells us for the first time that it is actually worth spending the time and effort to improve discharge communication, and patients do seem to benefit,” Dr. Horwitz says.
Individual physicians should feel empowered by the result to work on system change in their hospitals, she says.
Larry Beresford is a freelance writer in Alameda, Calif.
A Yale University research team has described what constitutes a good hospital discharge, based on its analysis of 1,500 discharge summaries from patients with exacerbations of heart failure at 46 hospitals enrolled in TeleMonitoring to Improve Heart Failure Outcomes (TELE-HF), a large multicenter study of patients hospitalized with heart failure.
“We consider a good discharge to be a three-legged stool composed of timeliness, transmission to the right person, and having the right components, as defined by The Joint Commission and the Transitions of Care Consensus Conference,” says co-author Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University.
“This study tells us for the first time that it is actually worth spending the time and effort to improve discharge communication, and patients do seem to benefit.”—Leora Horwitz, MD, MHS
Historically, discharge summaries were used primarily for billing, but the medical community has not made full use of them as tools for transition or considered what was really needed by the physician who will see the patient next, Dr. Horwitz says. In a previous study at Yale, as many as a third of discharge summaries were never received by a follow-up physician, and only 15% included the patient’s discharge weight—an essential detail for managing their cardiac care.
A second study using the TELE-HF data found that when the quality of the discharge summary was improved, readmissions rates were lower.
“This study tells us for the first time that it is actually worth spending the time and effort to improve discharge communication, and patients do seem to benefit,” Dr. Horwitz says.
Individual physicians should feel empowered by the result to work on system change in their hospitals, she says.
Larry Beresford is a freelance writer in Alameda, Calif.
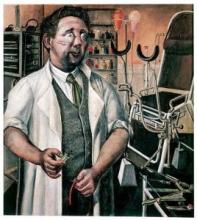
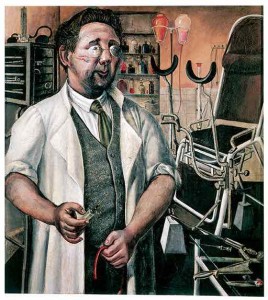
Art Helps Hospitalized Patients Manage Pain, Anxiety
A recent article in The North Jersey Record describes how art is being used to help manage hospitalized patients’ pain and anxiety.1 At Englewood (N.J.) Hospital and Medical Center, patients wheeled down a long corridor to the diagnostic testing department pass a dazzling array of 50 original art works—floral designs, landscapes, and abstracts—curated by the Art School at Old Church in Demarest.
Half of U.S. hospitals have some sort of art program, according to a 2009 report from the Society for the Arts in Healthcare. Although the research is still in its infancy, evidence suggests that programs incorporating art therapy can help reduce stress, anxiety, and pain in patients with cancer and other conditions, while increasing their satisfaction with their care.2,3,4
UK Arts in Healthcare at University of Kentucky HealthCare in Lexington brings the visual arts into health facilities and presents performing arts, music, and art therapies at Albert B. Chandler Hospital and other UK hospitals and clinics. Art in clinic waiting areas at UK improved patient satisfaction scores, which got the attention of hospital administrators, says Arts in Healthcare Program Director Jacqueline Hamilton.
Larry Beresford is a freelance writer in Alameda, Calif.
References
- Petrick J. Art is used to help healing process in hospitals. The North Jersey Record. January 25, 2015. Available at: http://www.northjersey.com/arts-and-entertainment/art/art-is-used-to-help-healing-process-in-hospitals-1.1251254. Accessed March 9, 2015.
- Puetz TW, Morley CA, Herring MP. Effects of creative arts therapies on psychological symptoms and quality of life in patients with cancer. JAMA Intern Med. 2013;173(11):960-969.
- Thyme KE, Sundin EC, Wiberg B, Öster I, Aström S, Lindh J. Individual brief art therapy can be helpful for women with breast cancer: a randomized controlled clinical study. Palliat Support Care. 2009;7(1):87-95.
- Wood MJM, Molassiotis A, Payne S. What research evidence is there for the use of art therapy in the management of symptoms in adults with cancer? A systematic review. Psychooncology. 2011;20(2):135-145.
A recent article in The North Jersey Record describes how art is being used to help manage hospitalized patients’ pain and anxiety.1 At Englewood (N.J.) Hospital and Medical Center, patients wheeled down a long corridor to the diagnostic testing department pass a dazzling array of 50 original art works—floral designs, landscapes, and abstracts—curated by the Art School at Old Church in Demarest.
Half of U.S. hospitals have some sort of art program, according to a 2009 report from the Society for the Arts in Healthcare. Although the research is still in its infancy, evidence suggests that programs incorporating art therapy can help reduce stress, anxiety, and pain in patients with cancer and other conditions, while increasing their satisfaction with their care.2,3,4
UK Arts in Healthcare at University of Kentucky HealthCare in Lexington brings the visual arts into health facilities and presents performing arts, music, and art therapies at Albert B. Chandler Hospital and other UK hospitals and clinics. Art in clinic waiting areas at UK improved patient satisfaction scores, which got the attention of hospital administrators, says Arts in Healthcare Program Director Jacqueline Hamilton.
Larry Beresford is a freelance writer in Alameda, Calif.
References
- Petrick J. Art is used to help healing process in hospitals. The North Jersey Record. January 25, 2015. Available at: http://www.northjersey.com/arts-and-entertainment/art/art-is-used-to-help-healing-process-in-hospitals-1.1251254. Accessed March 9, 2015.
- Puetz TW, Morley CA, Herring MP. Effects of creative arts therapies on psychological symptoms and quality of life in patients with cancer. JAMA Intern Med. 2013;173(11):960-969.
- Thyme KE, Sundin EC, Wiberg B, Öster I, Aström S, Lindh J. Individual brief art therapy can be helpful for women with breast cancer: a randomized controlled clinical study. Palliat Support Care. 2009;7(1):87-95.
- Wood MJM, Molassiotis A, Payne S. What research evidence is there for the use of art therapy in the management of symptoms in adults with cancer? A systematic review. Psychooncology. 2011;20(2):135-145.
A recent article in The North Jersey Record describes how art is being used to help manage hospitalized patients’ pain and anxiety.1 At Englewood (N.J.) Hospital and Medical Center, patients wheeled down a long corridor to the diagnostic testing department pass a dazzling array of 50 original art works—floral designs, landscapes, and abstracts—curated by the Art School at Old Church in Demarest.
Half of U.S. hospitals have some sort of art program, according to a 2009 report from the Society for the Arts in Healthcare. Although the research is still in its infancy, evidence suggests that programs incorporating art therapy can help reduce stress, anxiety, and pain in patients with cancer and other conditions, while increasing their satisfaction with their care.2,3,4
UK Arts in Healthcare at University of Kentucky HealthCare in Lexington brings the visual arts into health facilities and presents performing arts, music, and art therapies at Albert B. Chandler Hospital and other UK hospitals and clinics. Art in clinic waiting areas at UK improved patient satisfaction scores, which got the attention of hospital administrators, says Arts in Healthcare Program Director Jacqueline Hamilton.
Larry Beresford is a freelance writer in Alameda, Calif.
References
- Petrick J. Art is used to help healing process in hospitals. The North Jersey Record. January 25, 2015. Available at: http://www.northjersey.com/arts-and-entertainment/art/art-is-used-to-help-healing-process-in-hospitals-1.1251254. Accessed March 9, 2015.
- Puetz TW, Morley CA, Herring MP. Effects of creative arts therapies on psychological symptoms and quality of life in patients with cancer. JAMA Intern Med. 2013;173(11):960-969.
- Thyme KE, Sundin EC, Wiberg B, Öster I, Aström S, Lindh J. Individual brief art therapy can be helpful for women with breast cancer: a randomized controlled clinical study. Palliat Support Care. 2009;7(1):87-95.
- Wood MJM, Molassiotis A, Payne S. What research evidence is there for the use of art therapy in the management of symptoms in adults with cancer? A systematic review. Psychooncology. 2011;20(2):135-145.
Mobile Apps to Improve Quality, Value at Point-of-Care for Inpatients
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH