User login
Clinical Care Conundrums Provide Learning Potential for Hospitalists
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
At A Glance
Series: Hospital Medicine: Current Concepts
Title: Clinical Care Conundrums: Challenging Diagnoses in Hospital Medicine
Edited by: James C. Pile, Thomas E. Baudendistel, Brian Harte
Series Editors: Scott Flanders, Sanjay Saint
Pages: 208
Clinical Care Conundrums is written in 22 chapters, each discussing a clinical case presentation in a format similar to the series by the same name, published frequently in the Journal of Hospital Medicine.
An expert clinician’s approach to the “clinical conundrums” is disclosed using the presentation of an actual patient case in a prototypical “morning report” style. As in a patient care situation, sequential pieces of information are provided to the expert clinician, who is unfamiliar with the case. The focus of each case is the thought processes of both the clinical team caring for the patient and the commentator.
Excerpt
“Clinicians rely heavily on diagnostic test information, yet diagnostic tests are also susceptible to error. About 18% of critical laboratory results are judged nonrepresentative of the patient’s clinical condition after a chart review. …CT scans have 1.7% misinterpretation rate. Pathologic discrepancies occur in 11%-19% of cancer biopsy specimens. These data should remind clinicians to question…”
Each case provides great learning potential, not only in the unusual presentation of common diseases or more typical presentations of unusual diseases, but also in discussions of the possibilities in differential diagnoses. The range of information is wide. Readers are taken through discussions of conditions infrequently encountered but potentially fatal in the event of missed or delayed diagnosis, such as strongyloides hyperinfection, a condition that we are reminded is not always accompanied by eosinophilia. Some discussions of the more common conditions include:
- Evaluation of confusion;
- Etiologies of cirrhosis;
- Malignancies associated with hypercalcemia; and
- Work-up for new-onset seizures.
My interest remained high throughout the book, because I never knew what to expect. For example, a patient presenting with acute chest pain caused by esophageal perforation resulting in delayed diagnosis might follow the index case presentation of Whipple’s disease. We are also reminded that, despite the insistence of Gregory House, MD, (Dr. House is the titular character from the television series “House”) that “it’s never lupus,” it sometimes is actually lupus. A couple of interesting lupus cases are presented in a realistically perplexing manner, followed by beneficial discussion.
Analysis
The real value in this book lies in continued reminders of how and why clinicians make diagnostic errors. In fact, an early chapter in the book deals explicitly with improving diagnostic safety.
Robert Wachter, MD, MHM, reminds us in the introductory chapter that diagnostic errors comprise nearly one in five preventable adverse events. Until recently, diagnostic errors have been given relatively little attention, most likely because they are difficult to measure and harder to fix.
As hospital-based providers, the more awareness we have about the “anatomy and physiology” of both good and faulty decision making, the more likely we are to make better decisions. This book can be a crucial resource for any hospital-based care provider.
Dr. Lindsey is medical director of hospital-based physician services at Hospital Corporation of America (HCA).
Multi-Site Hospitalist Leaders: HM15 Session Summary
Session: Multi-site Hospitalist Leaders: Unique Challenges/What You Should Know
HM15 Presenter/Moderator: Scott Rissmiller, MD
Summation: This standing-room-only session was the result of a popular HMX e-community, which has become an active discussion board. As hospitals and health systems continue to consolidate across the country, there has been a rapid growth of multi-hospital systems. The role of the “Chief Hospitalist,” whose job is to lead multiple hospitalist groups within these systems, is evolving. These “Chief Hospitalists” are growing in number and they, as well as their followers, face unique challenges.
These points regarding organization structure were discussed, and as you look at your own organizational structure, these questions deserve your attention:
- Purpose of your structure?
- Is your structure centralized or decentralized?
- How does your organizational structure support decision-making?
- How does the structure ensure proper communication?
- How are resources shared across geography?
- What is your administrative support structure?
- How is administrative time allocated for physician leaders?
- How do you ensure engagement from all providers?
- How does your organization structure create alignment with the healthcare system?
The following compensation issues were discussed, and can be used as a discussion outline for most groups:
- How does your compensation (comp) plan align with the goals and values of the system?
- How does your comp plan account for regional variances?
- How does the comp plan encourage teamwork and sharing of resources?
- How does comp plan account for differences in acuity, hospital size, night frequency, etc.?
- Are goals and incentives group based, site based, or individual based?
- How does the comp plan fairly reward “non-RVU” work? (teaching, committee service, etc.)
- Should all site leaders receive the same comp regardless of group size?
- Does the comp plan incorporate “minimum work standards”/social compact?
Key Points/HM Takeaways:
- Panel discussion was valuable and reassured attendees that there are multiple ways to make groups successful. One common variable of successful groups is open lines of communication at all levels.
- Physician on-boarding is critical and should be utilized to set clear expectations.
- HM Goals/expectations must be aligned with those of the hospital and health system.
- When multiple hospitals are part of a larger system, it is desirable for goals to be aligned across the health system.
- Two-way open communication is necessary for success.
- Try to take a walk in your colleague’s/stakeholder’s shoes:
- How does my hospital administrative partner see this issue?
- How does my regional director/system lead see this issue?
- How does my bedside hospitalist physician/provider see this issue?
- How would my patients view this issue?
- Issues facing different types of groups, academic vs. community and for profit vs. not for profit, are somewhat variable.
- The leadership Dyad consisting of a physician and practice management professional in partnership is an effective and well-proven management model.
Many thanks to Drs. T.J. Richardson and Dan Duzan for their input and assistance with this session summary. Dr. Richardson is a Regional Medical Director and Dr. Duzan is a Facility Medical Director, both work for TeamHealth.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
Session: Multi-site Hospitalist Leaders: Unique Challenges/What You Should Know
HM15 Presenter/Moderator: Scott Rissmiller, MD
Summation: This standing-room-only session was the result of a popular HMX e-community, which has become an active discussion board. As hospitals and health systems continue to consolidate across the country, there has been a rapid growth of multi-hospital systems. The role of the “Chief Hospitalist,” whose job is to lead multiple hospitalist groups within these systems, is evolving. These “Chief Hospitalists” are growing in number and they, as well as their followers, face unique challenges.
These points regarding organization structure were discussed, and as you look at your own organizational structure, these questions deserve your attention:
- Purpose of your structure?
- Is your structure centralized or decentralized?
- How does your organizational structure support decision-making?
- How does the structure ensure proper communication?
- How are resources shared across geography?
- What is your administrative support structure?
- How is administrative time allocated for physician leaders?
- How do you ensure engagement from all providers?
- How does your organization structure create alignment with the healthcare system?
The following compensation issues were discussed, and can be used as a discussion outline for most groups:
- How does your compensation (comp) plan align with the goals and values of the system?
- How does your comp plan account for regional variances?
- How does the comp plan encourage teamwork and sharing of resources?
- How does comp plan account for differences in acuity, hospital size, night frequency, etc.?
- Are goals and incentives group based, site based, or individual based?
- How does the comp plan fairly reward “non-RVU” work? (teaching, committee service, etc.)
- Should all site leaders receive the same comp regardless of group size?
- Does the comp plan incorporate “minimum work standards”/social compact?
Key Points/HM Takeaways:
- Panel discussion was valuable and reassured attendees that there are multiple ways to make groups successful. One common variable of successful groups is open lines of communication at all levels.
- Physician on-boarding is critical and should be utilized to set clear expectations.
- HM Goals/expectations must be aligned with those of the hospital and health system.
- When multiple hospitals are part of a larger system, it is desirable for goals to be aligned across the health system.
- Two-way open communication is necessary for success.
- Try to take a walk in your colleague’s/stakeholder’s shoes:
- How does my hospital administrative partner see this issue?
- How does my regional director/system lead see this issue?
- How does my bedside hospitalist physician/provider see this issue?
- How would my patients view this issue?
- Issues facing different types of groups, academic vs. community and for profit vs. not for profit, are somewhat variable.
- The leadership Dyad consisting of a physician and practice management professional in partnership is an effective and well-proven management model.
Many thanks to Drs. T.J. Richardson and Dan Duzan for their input and assistance with this session summary. Dr. Richardson is a Regional Medical Director and Dr. Duzan is a Facility Medical Director, both work for TeamHealth.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
Session: Multi-site Hospitalist Leaders: Unique Challenges/What You Should Know
HM15 Presenter/Moderator: Scott Rissmiller, MD
Summation: This standing-room-only session was the result of a popular HMX e-community, which has become an active discussion board. As hospitals and health systems continue to consolidate across the country, there has been a rapid growth of multi-hospital systems. The role of the “Chief Hospitalist,” whose job is to lead multiple hospitalist groups within these systems, is evolving. These “Chief Hospitalists” are growing in number and they, as well as their followers, face unique challenges.
These points regarding organization structure were discussed, and as you look at your own organizational structure, these questions deserve your attention:
- Purpose of your structure?
- Is your structure centralized or decentralized?
- How does your organizational structure support decision-making?
- How does the structure ensure proper communication?
- How are resources shared across geography?
- What is your administrative support structure?
- How is administrative time allocated for physician leaders?
- How do you ensure engagement from all providers?
- How does your organization structure create alignment with the healthcare system?
The following compensation issues were discussed, and can be used as a discussion outline for most groups:
- How does your compensation (comp) plan align with the goals and values of the system?
- How does your comp plan account for regional variances?
- How does the comp plan encourage teamwork and sharing of resources?
- How does comp plan account for differences in acuity, hospital size, night frequency, etc.?
- Are goals and incentives group based, site based, or individual based?
- How does the comp plan fairly reward “non-RVU” work? (teaching, committee service, etc.)
- Should all site leaders receive the same comp regardless of group size?
- Does the comp plan incorporate “minimum work standards”/social compact?
Key Points/HM Takeaways:
- Panel discussion was valuable and reassured attendees that there are multiple ways to make groups successful. One common variable of successful groups is open lines of communication at all levels.
- Physician on-boarding is critical and should be utilized to set clear expectations.
- HM Goals/expectations must be aligned with those of the hospital and health system.
- When multiple hospitals are part of a larger system, it is desirable for goals to be aligned across the health system.
- Two-way open communication is necessary for success.
- Try to take a walk in your colleague’s/stakeholder’s shoes:
- How does my hospital administrative partner see this issue?
- How does my regional director/system lead see this issue?
- How does my bedside hospitalist physician/provider see this issue?
- How would my patients view this issue?
- Issues facing different types of groups, academic vs. community and for profit vs. not for profit, are somewhat variable.
- The leadership Dyad consisting of a physician and practice management professional in partnership is an effective and well-proven management model.
Many thanks to Drs. T.J. Richardson and Dan Duzan for their input and assistance with this session summary. Dr. Richardson is a Regional Medical Director and Dr. Duzan is a Facility Medical Director, both work for TeamHealth.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
Palliative Care and Last-Minute Heroics
4/8/15
HM15 Presenter: Tammie Quest, MD
Summation: Heroics- a set of medical actions that attempt to prolong life with a low likelihood of success.
Palliative care- an approach of care provided to patients and families suffering from serious and/or life limiting illness; focus on physical, spiritual, psychological and social aspects of distress.
Hospice care- intense palliative care provided when the patient has terminal illness with a prognosis of 6 months or less if the disease runs its usual course.
We underutilize Palliative and Hospice care in the US. Here in the US fewer than 50% of all persons receive hospice care at EOL, of those who receive hospice care more than half receive care for less than 20 days, and 1 in 5 patients die in an ICU. Palliative Care can/should co-exist with life prolonging care following the diagnosis of serious illness.
Common therapies/interventions to be contemplated and discussed with patient at end of life: cpr, mechanical ventilation, central venous/arterial access, renal replacement therapy, surgical procedures, valve therapies, ventricular assist devices, continuous infusions, IV fluids, supplemental oxygen, artificial nutrition, antimicrobials, blood products, cancer directed therapy, antithrombotics, anticoagulation.
Practical Elements of Palliative Care: pain and symptom management, advance care planning, communication/goals of care, truth-telling, social support, spiritual support, psychological support, risk/burden assessment of treatments.
Key Points/HM Takeaways:
1-Palliative Care Bedside Talking Points-
- Cardiac arrest is the moment of death, very few people survive an attempt at reversing death
- If you are one of the few who survive to discharge, you may do well but few will survive to discharge
- Antibiotics DO improve survival, antibiotics DO NOT improve comfort
- No evidence to show that dying from pneumonia, or other infection, is painful
- Allowing natural death includes permitting the body to shut itself down through natural mechanisms, including infection
- Dialysis may extend life, but there will be progressive functional decline
2-Goals of Care define what therapies are indicated. Balance prolongation of life with illness experience.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
4/8/15
HM15 Presenter: Tammie Quest, MD
Summation: Heroics- a set of medical actions that attempt to prolong life with a low likelihood of success.
Palliative care- an approach of care provided to patients and families suffering from serious and/or life limiting illness; focus on physical, spiritual, psychological and social aspects of distress.
Hospice care- intense palliative care provided when the patient has terminal illness with a prognosis of 6 months or less if the disease runs its usual course.
We underutilize Palliative and Hospice care in the US. Here in the US fewer than 50% of all persons receive hospice care at EOL, of those who receive hospice care more than half receive care for less than 20 days, and 1 in 5 patients die in an ICU. Palliative Care can/should co-exist with life prolonging care following the diagnosis of serious illness.
Common therapies/interventions to be contemplated and discussed with patient at end of life: cpr, mechanical ventilation, central venous/arterial access, renal replacement therapy, surgical procedures, valve therapies, ventricular assist devices, continuous infusions, IV fluids, supplemental oxygen, artificial nutrition, antimicrobials, blood products, cancer directed therapy, antithrombotics, anticoagulation.
Practical Elements of Palliative Care: pain and symptom management, advance care planning, communication/goals of care, truth-telling, social support, spiritual support, psychological support, risk/burden assessment of treatments.
Key Points/HM Takeaways:
1-Palliative Care Bedside Talking Points-
- Cardiac arrest is the moment of death, very few people survive an attempt at reversing death
- If you are one of the few who survive to discharge, you may do well but few will survive to discharge
- Antibiotics DO improve survival, antibiotics DO NOT improve comfort
- No evidence to show that dying from pneumonia, or other infection, is painful
- Allowing natural death includes permitting the body to shut itself down through natural mechanisms, including infection
- Dialysis may extend life, but there will be progressive functional decline
2-Goals of Care define what therapies are indicated. Balance prolongation of life with illness experience.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
4/8/15
HM15 Presenter: Tammie Quest, MD
Summation: Heroics- a set of medical actions that attempt to prolong life with a low likelihood of success.
Palliative care- an approach of care provided to patients and families suffering from serious and/or life limiting illness; focus on physical, spiritual, psychological and social aspects of distress.
Hospice care- intense palliative care provided when the patient has terminal illness with a prognosis of 6 months or less if the disease runs its usual course.
We underutilize Palliative and Hospice care in the US. Here in the US fewer than 50% of all persons receive hospice care at EOL, of those who receive hospice care more than half receive care for less than 20 days, and 1 in 5 patients die in an ICU. Palliative Care can/should co-exist with life prolonging care following the diagnosis of serious illness.
Common therapies/interventions to be contemplated and discussed with patient at end of life: cpr, mechanical ventilation, central venous/arterial access, renal replacement therapy, surgical procedures, valve therapies, ventricular assist devices, continuous infusions, IV fluids, supplemental oxygen, artificial nutrition, antimicrobials, blood products, cancer directed therapy, antithrombotics, anticoagulation.
Practical Elements of Palliative Care: pain and symptom management, advance care planning, communication/goals of care, truth-telling, social support, spiritual support, psychological support, risk/burden assessment of treatments.
Key Points/HM Takeaways:
1-Palliative Care Bedside Talking Points-
- Cardiac arrest is the moment of death, very few people survive an attempt at reversing death
- If you are one of the few who survive to discharge, you may do well but few will survive to discharge
- Antibiotics DO improve survival, antibiotics DO NOT improve comfort
- No evidence to show that dying from pneumonia, or other infection, is painful
- Allowing natural death includes permitting the body to shut itself down through natural mechanisms, including infection
- Dialysis may extend life, but there will be progressive functional decline
2-Goals of Care define what therapies are indicated. Balance prolongation of life with illness experience.
Julianna Lindsey is a hospitalist and physician leader based in the Dallas-Fort Worth Metroplex. Her focus is patient safety/quality and physician leadership. She is a member of TeamHospitalist.
Implementing Physician Value-Based Purchasing in Your Practice: HM15 Session Analysis
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
HM15 Session: Putting Your Nickel Down: The What, Why, and How of Implementing Physician Value-Based Purchasing in Your Practice
Presenters: Stephen Besch, Simone Karp RPh, Patrick Torcson MD MMM SFHM, Gregory Seymann MD SFHM
Medicare is transforming itself from a “passive payer” to an “active purchaser” of high quality, efficient healthcare. As such- active participation by physicians, physician groups, and hospitals is required for payment eligibility.
At the physician/group level, hospitalists should be reporting PQRS measures. Incentive payments for PQRS ended in 2014, Medicare is now making “negative payment adjustments.” Penalties are equal to a percentage of all Medicare Part B FFS (Fee-for-Service) charges and there is a 2-year delay between reporting or performance failure and penalization.
Physician Value-Based Purchasing (P-VBP) affects all Eligible Providers (EPs) in 2015. P4P (Pay for Performance) assesses both quality and cost. Aim is for budget neutrality via “quality tiering” which rewards “high quality/low cost” practices with penalties from “low quality/high cost” practices. As of now (2015) ACPs and therapists can be penalized under P-VBP.
Key Points/HM Takeaways:
- Hospitalists should be reporting PQRS measures- penalty phase has begun
- Key PQRS Changes for 2015:
- 6 measures applicable to inpatient billing removed
- no useful inpatient measures added
- penalty avoidance requires 9 measures at 50% or higher rates, covering at least 3 of the 6 NQS (National Quality Strategy) domains- including 1 cross-cutting measure
- all 2015 PQRS data will be posted to Physician Compare website in 2016
- 3 Examples of hospitalist applicable “cross-cutting measures” are
- 47-advance care plan
- 130-documentation of current medications
- 317-preventative care: bp screening
- PQRS data must be reported with respect to MAV clusters (Measure Applicability Validation)- reporting only measure that have no MAV cluster is a safe strategy so long as one of the measures is “cross-cutting”
- Maximum P-VBP penalties automatically apply if group does not report enough PQRS data
- visit CMS website for more information
Hot Topics in Practice Management; HM15 Session Analysis
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Presenters: Roy Sittig MD SFHM, Jeffrey Frank MD MBA, Jodi Braun
Summation: Speakers covered timely topics regarding the Accountable Care Act, namely Medicaid Expansion and Bundled Payment arrangements; and reviewed the seminal paper on “Key Principals and Characteristics of an Effective Hospitalist Medicine Group” and lessons learned in implementing those 10 Key Principles.
Medicaid Expansion: EDs serving the 29 Medicaid expansion states are reporting higher volumes, likely due to 11.4million new lives now insured under the ACA. While the ACA does provide for higher Medicaid payment rates thus far, only 34% of providers accept Medicaid, a 21% drop since the ACA went into effect.
Bundled Payment Arrangements:
- Bundled Payment Care Initiative (BPCI) lexicon:
- Model 2-Episode Anchor (anchor admission) AND 90days post d/c; Medicare pays 98% of usual cost
- Model 3-90days post d/c AFTER anchor admission; Medicare pays 97% of usual cost
- Convener-entity that brings providers together and enters into CMS agreement to bear risk for bundles
- Awardee (entity having agreement with Medicare to assume risk and receive payment via BPCI) and Convener own the Bundle
- Episode initiator (EI) triggers “bundle period”
- Bundles based on DRG
10-Key Principles of an Effective Hospitalist Medicine Group:
- Effective Leadership
- Engaged Hospitalists
- Adequate Resources
- Planning and Management Infrastructure
- Alignment with Hospital/Health System
- Care Coordination Across Settings
- Leadership in Key Clinical Issues in the Hospital/Health System
- Thoughtful Approach to Scope of Activity
- Patient/Family-Centered, Team-Based Care; Effective Communication
- Recruiting/Retaining Qualified Clinicians
Key Points/HM Takeaways:
Medicaid Expansion- many of the 11.4M newly insured lives under the ACA have moved into Medicaid. Only about 1/3 of providers now accept Medicaid- 1 in 5 covered persons now have Medicaid, nearly 20% increase since 2013.
Bundled Payments- Majority of savings opportunity lies in Post-Acute Care. Awardee and Convener make profit is total cost is less than 98% of Target Price. In gainsharing agreements individuals can be reimbursed up to 150% usual Medicare rate. Pay occurs in usual Medicare fashion but is reconciled 60-90 days after end of bundle. For more information: http://innovation.cms.gov/initiatives/bundled-payments/
Effective HM Groups- Three important areas for focus when beginning to address group performance are: engaged hospitalists, planning and management infrastructure, care coordination across settings. These three topics have broad reaching implications into the hospitalist practice and patient care. [Cawley P, et al. Journal of Hospital Medicine 2014; 9(2):123-128]
HM15 Session Analysis: End-of-Life Discussions
Presenter: Julia Ragland, MD, FHM
Summation: Discussion of Prognosis in Advance Illness is a key component of informed decision-making and should be undertaken during a “Sentinel Hospitalization” and at times of other “triggers”. End-of-Life discussions are critical for providing the best care for patients with advanced diseases.
A Sentinel Hospitalization is a hospitalization in the patient’s disease course that heralds a need to reassess prognosis, patient understanding, treatment options and intensities, and goals of care.
Other triggers for discussing prognosis: new diagnosis of serious illness, major medical decision with uncertain outcome, frequent hospitalizations for advanced disease, patient/family query prognosis, patient/family request treatment inconsistent with good clinical judgment (futile care), patient actively dying, “No” answer to “Surprise Question” (“would you be surprised if this patient died in the next year?”)
How can we prognosticate? Data from studies, Clinical intuition and experience, Prognostic indices, Key indicators of worsening prognosis (declining functional status, weight loss/malnutrition, co-morbidities, frequent hospitalizations)
Resources for Prognostication: ePrognosis, Seattle Heart Failure Model, MELD, Charlson Comorbidity Index, MJHSpalliativeinstitute.org/e-learning, Palliative Care Fast Facts mobile app
Ask-Tell-Ask method for communicating prognosis
- ASK: if they want to talk about prognosis and what they already know
- TELL: give information in small amounts, build on what they already know, use simple straight-forward language
- ASK: repeat understanding of what has been said, if they would like to hear more
Key Points/HM Takeaways:
- Estimating and discussing prognosis are core competencies for hospitalists and should be utilized during a “sentinel hospitalization”
- Prognostic awareness in advanced illness is key for:
- Informed decision making (CPR, procedures, chemo, et al)
- Determining realistic goals of care
- Providing patient centered care
- Most patients and families want prognostic information, but not always- must ask to know. Give the patient the option not to discuss prognosis.
- Ask-Tell-Ask approach for discussing prognosis is effective
Presenter: Julia Ragland, MD, FHM
Summation: Discussion of Prognosis in Advance Illness is a key component of informed decision-making and should be undertaken during a “Sentinel Hospitalization” and at times of other “triggers”. End-of-Life discussions are critical for providing the best care for patients with advanced diseases.
A Sentinel Hospitalization is a hospitalization in the patient’s disease course that heralds a need to reassess prognosis, patient understanding, treatment options and intensities, and goals of care.
Other triggers for discussing prognosis: new diagnosis of serious illness, major medical decision with uncertain outcome, frequent hospitalizations for advanced disease, patient/family query prognosis, patient/family request treatment inconsistent with good clinical judgment (futile care), patient actively dying, “No” answer to “Surprise Question” (“would you be surprised if this patient died in the next year?”)
How can we prognosticate? Data from studies, Clinical intuition and experience, Prognostic indices, Key indicators of worsening prognosis (declining functional status, weight loss/malnutrition, co-morbidities, frequent hospitalizations)
Resources for Prognostication: ePrognosis, Seattle Heart Failure Model, MELD, Charlson Comorbidity Index, MJHSpalliativeinstitute.org/e-learning, Palliative Care Fast Facts mobile app
Ask-Tell-Ask method for communicating prognosis
- ASK: if they want to talk about prognosis and what they already know
- TELL: give information in small amounts, build on what they already know, use simple straight-forward language
- ASK: repeat understanding of what has been said, if they would like to hear more
Key Points/HM Takeaways:
- Estimating and discussing prognosis are core competencies for hospitalists and should be utilized during a “sentinel hospitalization”
- Prognostic awareness in advanced illness is key for:
- Informed decision making (CPR, procedures, chemo, et al)
- Determining realistic goals of care
- Providing patient centered care
- Most patients and families want prognostic information, but not always- must ask to know. Give the patient the option not to discuss prognosis.
- Ask-Tell-Ask approach for discussing prognosis is effective
Presenter: Julia Ragland, MD, FHM
Summation: Discussion of Prognosis in Advance Illness is a key component of informed decision-making and should be undertaken during a “Sentinel Hospitalization” and at times of other “triggers”. End-of-Life discussions are critical for providing the best care for patients with advanced diseases.
A Sentinel Hospitalization is a hospitalization in the patient’s disease course that heralds a need to reassess prognosis, patient understanding, treatment options and intensities, and goals of care.
Other triggers for discussing prognosis: new diagnosis of serious illness, major medical decision with uncertain outcome, frequent hospitalizations for advanced disease, patient/family query prognosis, patient/family request treatment inconsistent with good clinical judgment (futile care), patient actively dying, “No” answer to “Surprise Question” (“would you be surprised if this patient died in the next year?”)
How can we prognosticate? Data from studies, Clinical intuition and experience, Prognostic indices, Key indicators of worsening prognosis (declining functional status, weight loss/malnutrition, co-morbidities, frequent hospitalizations)
Resources for Prognostication: ePrognosis, Seattle Heart Failure Model, MELD, Charlson Comorbidity Index, MJHSpalliativeinstitute.org/e-learning, Palliative Care Fast Facts mobile app
Ask-Tell-Ask method for communicating prognosis
- ASK: if they want to talk about prognosis and what they already know
- TELL: give information in small amounts, build on what they already know, use simple straight-forward language
- ASK: repeat understanding of what has been said, if they would like to hear more
Key Points/HM Takeaways:
- Estimating and discussing prognosis are core competencies for hospitalists and should be utilized during a “sentinel hospitalization”
- Prognostic awareness in advanced illness is key for:
- Informed decision making (CPR, procedures, chemo, et al)
- Determining realistic goals of care
- Providing patient centered care
- Most patients and families want prognostic information, but not always- must ask to know. Give the patient the option not to discuss prognosis.
- Ask-Tell-Ask approach for discussing prognosis is effective
Assessing, Managing Delirium in Hospitalized Patients
Summary: Delirium is a common problem in hospitalized patients, and all too often delirium is iatrogenic. Delirium is associated with poor outcomes such as prolonged hospitalization and functional decline, and it increases the risk of nursing home admission. The most common tool to assess the presence of delirium is the Confusion Assessment Method (CAM). Dr. Cumbler educated the audience on a more refined tool, the 3D CAM [PDF], and provided the algorithm for diagnosis and evaluation of hospital-onset delirium.
Where delirium is concerned (as with most conditions), “an ounce of prevention is worth a pound of cure.” Namely, avoid prescribing problem medications such as anticholinergics, sedative/hypnotics (except benzodiazepines for treatment of alcohol withdrawal), and antihistamines; and minimize narcotics, but don’t undertreat pain as uncontrolled pain is a more potent delirium trigger than narcotics.
Avoid sleep deprivation. Do we really require vital signs and phlebotomy between midnight and 6 a.m.? Make sure patients have their glasses and hearing aids, and keep them up and moving during daylight hours. Sleep and sensory deprivation are effective forms of human torture and are known to be rather disorienting.
Finally, antipsychotics are associated with increased mortality in dementia. Patients with agitated delirium may benefit from a low dose of haloperidol. When prescribing haloperidol, remember IV administration requires EKG monitoring (FDA black box warning), and a reasonable starting dose is 0.5 mg, NOT 5 mg.
HM takeaways:
- Use CAM, 3D CAM to diagnose delirium;
- Avoid anticholinergic medications (promethazine, cyclobenzaprine, oxybutynin, amitriptyline, prednisolone, theophylline, dixogin, furosemide);
- Minimize, but do not avoid, narcotics in patients with both pain and delirium;
- Use low-dose antipsychotics, not benzodiazepines, for agitated delirium; and
- STOP antipsychotics ASAP, ideally prior to discharge; if not prior to discharge, then include discontinuation date on discharge medication list. TH
Summary: Delirium is a common problem in hospitalized patients, and all too often delirium is iatrogenic. Delirium is associated with poor outcomes such as prolonged hospitalization and functional decline, and it increases the risk of nursing home admission. The most common tool to assess the presence of delirium is the Confusion Assessment Method (CAM). Dr. Cumbler educated the audience on a more refined tool, the 3D CAM [PDF], and provided the algorithm for diagnosis and evaluation of hospital-onset delirium.
Where delirium is concerned (as with most conditions), “an ounce of prevention is worth a pound of cure.” Namely, avoid prescribing problem medications such as anticholinergics, sedative/hypnotics (except benzodiazepines for treatment of alcohol withdrawal), and antihistamines; and minimize narcotics, but don’t undertreat pain as uncontrolled pain is a more potent delirium trigger than narcotics.
Avoid sleep deprivation. Do we really require vital signs and phlebotomy between midnight and 6 a.m.? Make sure patients have their glasses and hearing aids, and keep them up and moving during daylight hours. Sleep and sensory deprivation are effective forms of human torture and are known to be rather disorienting.
Finally, antipsychotics are associated with increased mortality in dementia. Patients with agitated delirium may benefit from a low dose of haloperidol. When prescribing haloperidol, remember IV administration requires EKG monitoring (FDA black box warning), and a reasonable starting dose is 0.5 mg, NOT 5 mg.
HM takeaways:
- Use CAM, 3D CAM to diagnose delirium;
- Avoid anticholinergic medications (promethazine, cyclobenzaprine, oxybutynin, amitriptyline, prednisolone, theophylline, dixogin, furosemide);
- Minimize, but do not avoid, narcotics in patients with both pain and delirium;
- Use low-dose antipsychotics, not benzodiazepines, for agitated delirium; and
- STOP antipsychotics ASAP, ideally prior to discharge; if not prior to discharge, then include discontinuation date on discharge medication list. TH
Summary: Delirium is a common problem in hospitalized patients, and all too often delirium is iatrogenic. Delirium is associated with poor outcomes such as prolonged hospitalization and functional decline, and it increases the risk of nursing home admission. The most common tool to assess the presence of delirium is the Confusion Assessment Method (CAM). Dr. Cumbler educated the audience on a more refined tool, the 3D CAM [PDF], and provided the algorithm for diagnosis and evaluation of hospital-onset delirium.
Where delirium is concerned (as with most conditions), “an ounce of prevention is worth a pound of cure.” Namely, avoid prescribing problem medications such as anticholinergics, sedative/hypnotics (except benzodiazepines for treatment of alcohol withdrawal), and antihistamines; and minimize narcotics, but don’t undertreat pain as uncontrolled pain is a more potent delirium trigger than narcotics.
Avoid sleep deprivation. Do we really require vital signs and phlebotomy between midnight and 6 a.m.? Make sure patients have their glasses and hearing aids, and keep them up and moving during daylight hours. Sleep and sensory deprivation are effective forms of human torture and are known to be rather disorienting.
Finally, antipsychotics are associated with increased mortality in dementia. Patients with agitated delirium may benefit from a low dose of haloperidol. When prescribing haloperidol, remember IV administration requires EKG monitoring (FDA black box warning), and a reasonable starting dose is 0.5 mg, NOT 5 mg.
HM takeaways:
- Use CAM, 3D CAM to diagnose delirium;
- Avoid anticholinergic medications (promethazine, cyclobenzaprine, oxybutynin, amitriptyline, prednisolone, theophylline, dixogin, furosemide);
- Minimize, but do not avoid, narcotics in patients with both pain and delirium;
- Use low-dose antipsychotics, not benzodiazepines, for agitated delirium; and
- STOP antipsychotics ASAP, ideally prior to discharge; if not prior to discharge, then include discontinuation date on discharge medication list. TH
Mobile Apps to Improve Quality, Value at Point-of-Care for Inpatients
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
Summary: The panel of high-tech doctors helped a standing-room-only crowd navigate numerous apps to be used at point-of-care [PDF, 458 kb]. Groups worked through case studies utilizing applicable mobile apps. Examples and most useful apps, including occasional user reviews, follow:
Provider-to-Provider Communication, HIPAA secure
- Doximity.
- HIPAA-chat.
- Pros: HIPAA-secure, real-time communication.
- Cons: Both parties must be on app to securely communicate.
Provider-to-Patient Communication, Language Translators
- Google Translate: multiple platforms, free, 90 languages.
- MediBabble: iOS only, free, seven languages, dedicated medical application.
Diagnostic Apps for Providers
- Calculate by QxM.
- PreOpEval14: iOS only.
- PreopRisk Assessment: Android only.
- ASCVD Risk Estimator.
- MDCalc.com in addition to usual formulas, great abg-analyzer (online version only).
- AnticoagEvaluator.
- epocrates: calculators.
Click here for a PDF of useful apps and resource links [PDF, 177 kb]
Resources for Evidence-Based Practice
- ACP Clinical Guidelines.
- ACP Smart Medicine.
- Read by QxMD.
- UpToDate.
- AHRQ ePPS: identifies clinical preventive services.
- epocrates.
Patient Engagement Apps
- Medication reminders: MediSafe, CareZone.
- Pharmaceutical costs: Walmart, Target Healthful, GoodRx.
- Proper inhaler usage: User Inhalers App.
- Smoking cessation: QuitSTART.
HM15 takeaways
- Apps are available to providers and patients to enhance quality, value, and compliance;
- Before “prescribing” any app to patients, vet the application yourself; and
- Use apps to supplement your clinical practice, but be wary of becoming over-reliant upon them, to the detriment of long-term memory. In order to utilize information in critical-thinking processes, it must be stored in long-term memory. TH
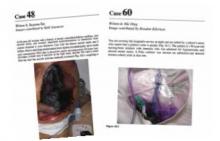
Clinical Images Capture Hospitalists’ Daily Rounds
EDITOR’S NOTE: Fourth in an occasional series of reviews of the Hospital Medicine: Current Concepts series by members of Team Hospitalist.
Summary
Hospital Images: A Clinical Atlas is a collection of 76 clinical cases discussing actual patient scenarios with accompanying clinical case questions, images, and evidence-based discussions. Cases are presented in the same manner a practicing hospitalist would encounter them during daily rounds—that is to say, randomly. Chosen cases vary widely, from aspiration pneumonitis to necrotizing fasciitis, and are also representative of a day in the life of most hospitalists. The clinical images are of excellent quality and accurately represent the conditions discussed. The case discussions are logical, clinically relevant, and evidence-based.
Analysis
In this reviewer’s opinion, Hospital Images: A Clinical Atlas is required reading for all practicing hospitalists. The full-color images are high resolution and presented as patients would be viewed from the bedside. The cases are diverse and absolutely pertinent to the practice of hospital medicine. I am confident even the most experienced reader will learn something that will quite probably improve his or her diagnostic capability.
Dr. Lindsey is a hospitalist and chief of staff at Victory Medical Center in McKinney, Texas. She has been a member of Team Hospitalist since 2013.
EDITOR’S NOTE: Fourth in an occasional series of reviews of the Hospital Medicine: Current Concepts series by members of Team Hospitalist.
Summary
Hospital Images: A Clinical Atlas is a collection of 76 clinical cases discussing actual patient scenarios with accompanying clinical case questions, images, and evidence-based discussions. Cases are presented in the same manner a practicing hospitalist would encounter them during daily rounds—that is to say, randomly. Chosen cases vary widely, from aspiration pneumonitis to necrotizing fasciitis, and are also representative of a day in the life of most hospitalists. The clinical images are of excellent quality and accurately represent the conditions discussed. The case discussions are logical, clinically relevant, and evidence-based.
Analysis
In this reviewer’s opinion, Hospital Images: A Clinical Atlas is required reading for all practicing hospitalists. The full-color images are high resolution and presented as patients would be viewed from the bedside. The cases are diverse and absolutely pertinent to the practice of hospital medicine. I am confident even the most experienced reader will learn something that will quite probably improve his or her diagnostic capability.
Dr. Lindsey is a hospitalist and chief of staff at Victory Medical Center in McKinney, Texas. She has been a member of Team Hospitalist since 2013.
EDITOR’S NOTE: Fourth in an occasional series of reviews of the Hospital Medicine: Current Concepts series by members of Team Hospitalist.
Summary
Hospital Images: A Clinical Atlas is a collection of 76 clinical cases discussing actual patient scenarios with accompanying clinical case questions, images, and evidence-based discussions. Cases are presented in the same manner a practicing hospitalist would encounter them during daily rounds—that is to say, randomly. Chosen cases vary widely, from aspiration pneumonitis to necrotizing fasciitis, and are also representative of a day in the life of most hospitalists. The clinical images are of excellent quality and accurately represent the conditions discussed. The case discussions are logical, clinically relevant, and evidence-based.
Analysis
In this reviewer’s opinion, Hospital Images: A Clinical Atlas is required reading for all practicing hospitalists. The full-color images are high resolution and presented as patients would be viewed from the bedside. The cases are diverse and absolutely pertinent to the practice of hospital medicine. I am confident even the most experienced reader will learn something that will quite probably improve his or her diagnostic capability.
Dr. Lindsey is a hospitalist and chief of staff at Victory Medical Center in McKinney, Texas. She has been a member of Team Hospitalist since 2013.