User login
Role grows for heart failure patient-reported outcomes
DALLAS – The Food and Drug Administration is keenly seeking patient-reported outcomes as endpoints in cardiovascular drug or device trials, particularly for heart failure patients, but the bar remains high for getting such an outcome into labeling, said agency officials who regulate cardiovascular disease therapies.
The FDA issued guidance nearly 8 years ago on how to integrate patient-reported outcome (PRO) measures into medical product development, but so far no heart failure drug nor device has met the agency’s standards for documented success in improving a PRO, despite the clear need for these patients to receive patient-centered care, clinicians said.
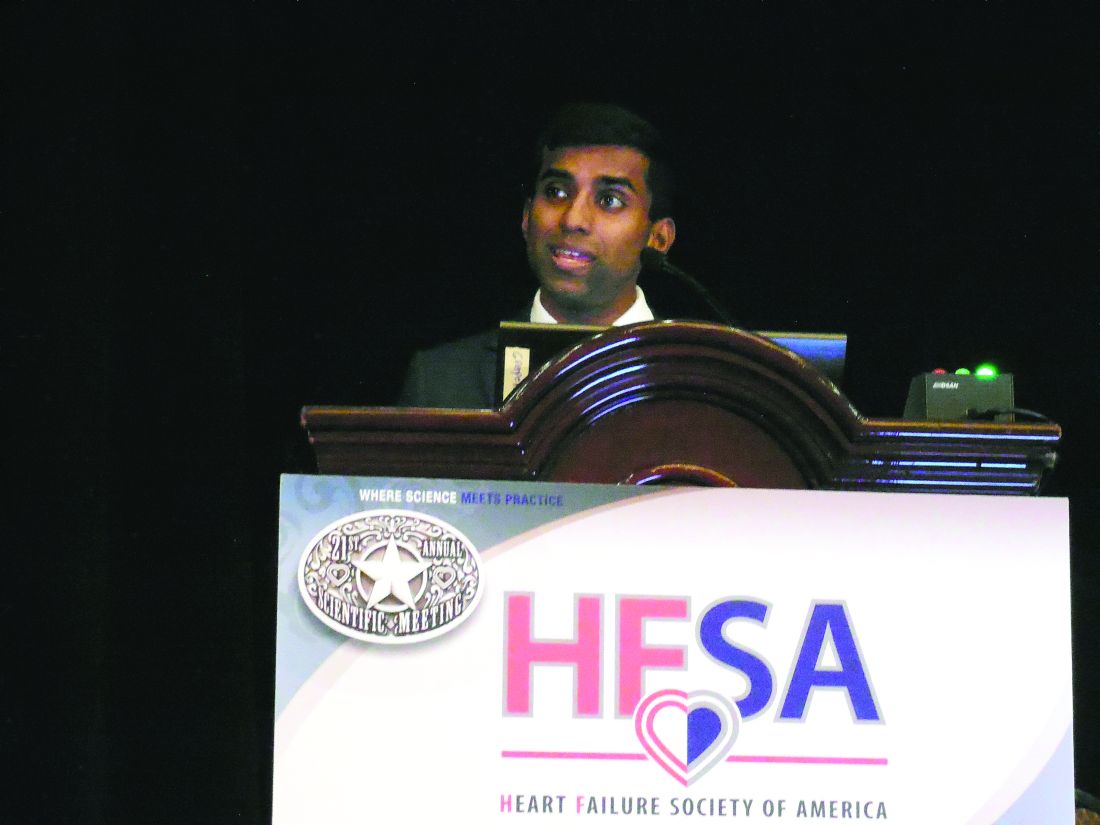
“We don’t yet have a patient-reported outcome in a label for heart failure,” Paul A. Heidenreich, MD, said during a session on PROs at the annual scientific meeting of the Heart Failure Society of America. He voiced hope that a PRO might end up on the label of a heart failure drug or device sometime in 2018. “Almost half of FDA submissions now include a PRO” as part of the data package, added Dr. Heidenreich, a cardiologist and professor of medicine at Stanford (Calif.) University.
For years, PROs for heart failure weren’t often used in trials, and they remain largely absent from routine practice – an absence Dr. Heidenreich lamented. “Just focusing on mortality in heart failure is really not patient centered,” he said.
Heart failure physicians “are very good at disease-centered care” that focuses on survival and reducing hospitalizations, but “survival is often not as important to patients,” noted Mary Norine Walsh, MD, medical director of the heart failure and cardiac transplantation program at St. Vincent Medical Group in Indianapolis. She suggested “tailoring treatment to improve patient symptoms, physical function, and quality of life” without necessarily reducing hospital readmissions or increasing survival rates. “Self-reported measures have more meaning for patients,” she said, and called for using PROs to better target interventions to the patients who can most benefit from them.
Two FDA representatives who spoke during the session agreed on the importance of PROs and attested to the agency’s interest in greater reliance on them.
“PROs are a critical complement to the other measures made in device trials,” said Bram Zuckerman, MD, director of the FDA’s division of cardiovascular devices. “We need PRO information because it reflects important aspects of patients’ health-related quality of life.”
The most commonly used PRO measures in device trials today are the Kansas City Cardiomyopathy Questionnaire (J Am Coll Cardiol. 2000 Apr;35[5]:1245-55) and the Minnesota Living With Heart Failure questionnaire, he noted.
“Neither is perfect, but there is a track record in heart failure device development that these two PROs can be helpful.” The FDA’s cardiovascular device division “wants to use PRO information,” Dr. Zuckerman said.
“All-cause mortality is the most unbiased endpoint, but there is interest in PROs,” agreed Ebony Dashiell-Aje, PhD, from the FDA’s office of new drugs in the Center for Drug Evaluation and Research. She highlighted the encouragement that the FDA gave to drug and device developers to include PROs in trials, both in its 2009 guidance document as well as in a “roadmap” from the agency on how to measure PROs in clinical trials. “Unfortunately, in heart failure we struggle to find tools that can adequately measure the patient’s perspective and be sensitive enough to detect a treatment benefit,” she said.
Norman Stockbridge, MD, director of the division of cardiovascular and renal products in the agency’s Office of Drug Evaluation, cited even bigger barriers to FDA approval of PROs as labeled effects from drugs or devices.
Getting a PRO endpoint supported by clinical-trial results that qualify it for an FDA label faces two big challenges. One challenge, he said, is “how much of an effect we need to see in a complex scoring algorithm to know that patients actually received some benefit in a disease that often varies from day to day and from week to week.” The second challenge is that, “in a disease with a high background rate of bad outcomes, you need some evidence that the benefit [from the treatment] is worth any risk,” which is something that can be hard to prove in heart failure when many patients don’t live more than 2 years with the disease, Dr. Stockbridge said in an interview.
“You need to be able to make the argument that the [PRO] benefit is likely perceptible to patients, but that is only half the problem. The other half is whether the developer can rule out that survival is not less than it would have been with no treatment. If patients take this, will they feel better but have a greater risk of being hurt?”
So far, no drug or device developer has succeeded in proving this to the FDA, despite the agency’s 2009 guidance on how it could be done.
That guidance “is one of the two worst and most destructive guidance documents we ever published,” Dr. Stockbridge declared.
Dr. Walsh, Dr. Heidenreich, Dr. Zuckerman, Dr. Dashiell-Aje, and Dr. Stockbridge had no relevant disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – The Food and Drug Administration is keenly seeking patient-reported outcomes as endpoints in cardiovascular drug or device trials, particularly for heart failure patients, but the bar remains high for getting such an outcome into labeling, said agency officials who regulate cardiovascular disease therapies.
The FDA issued guidance nearly 8 years ago on how to integrate patient-reported outcome (PRO) measures into medical product development, but so far no heart failure drug nor device has met the agency’s standards for documented success in improving a PRO, despite the clear need for these patients to receive patient-centered care, clinicians said.
“We don’t yet have a patient-reported outcome in a label for heart failure,” Paul A. Heidenreich, MD, said during a session on PROs at the annual scientific meeting of the Heart Failure Society of America. He voiced hope that a PRO might end up on the label of a heart failure drug or device sometime in 2018. “Almost half of FDA submissions now include a PRO” as part of the data package, added Dr. Heidenreich, a cardiologist and professor of medicine at Stanford (Calif.) University.
For years, PROs for heart failure weren’t often used in trials, and they remain largely absent from routine practice – an absence Dr. Heidenreich lamented. “Just focusing on mortality in heart failure is really not patient centered,” he said.
Heart failure physicians “are very good at disease-centered care” that focuses on survival and reducing hospitalizations, but “survival is often not as important to patients,” noted Mary Norine Walsh, MD, medical director of the heart failure and cardiac transplantation program at St. Vincent Medical Group in Indianapolis. She suggested “tailoring treatment to improve patient symptoms, physical function, and quality of life” without necessarily reducing hospital readmissions or increasing survival rates. “Self-reported measures have more meaning for patients,” she said, and called for using PROs to better target interventions to the patients who can most benefit from them.
Two FDA representatives who spoke during the session agreed on the importance of PROs and attested to the agency’s interest in greater reliance on them.
“PROs are a critical complement to the other measures made in device trials,” said Bram Zuckerman, MD, director of the FDA’s division of cardiovascular devices. “We need PRO information because it reflects important aspects of patients’ health-related quality of life.”
The most commonly used PRO measures in device trials today are the Kansas City Cardiomyopathy Questionnaire (J Am Coll Cardiol. 2000 Apr;35[5]:1245-55) and the Minnesota Living With Heart Failure questionnaire, he noted.
“Neither is perfect, but there is a track record in heart failure device development that these two PROs can be helpful.” The FDA’s cardiovascular device division “wants to use PRO information,” Dr. Zuckerman said.
“All-cause mortality is the most unbiased endpoint, but there is interest in PROs,” agreed Ebony Dashiell-Aje, PhD, from the FDA’s office of new drugs in the Center for Drug Evaluation and Research. She highlighted the encouragement that the FDA gave to drug and device developers to include PROs in trials, both in its 2009 guidance document as well as in a “roadmap” from the agency on how to measure PROs in clinical trials. “Unfortunately, in heart failure we struggle to find tools that can adequately measure the patient’s perspective and be sensitive enough to detect a treatment benefit,” she said.
Norman Stockbridge, MD, director of the division of cardiovascular and renal products in the agency’s Office of Drug Evaluation, cited even bigger barriers to FDA approval of PROs as labeled effects from drugs or devices.
Getting a PRO endpoint supported by clinical-trial results that qualify it for an FDA label faces two big challenges. One challenge, he said, is “how much of an effect we need to see in a complex scoring algorithm to know that patients actually received some benefit in a disease that often varies from day to day and from week to week.” The second challenge is that, “in a disease with a high background rate of bad outcomes, you need some evidence that the benefit [from the treatment] is worth any risk,” which is something that can be hard to prove in heart failure when many patients don’t live more than 2 years with the disease, Dr. Stockbridge said in an interview.
“You need to be able to make the argument that the [PRO] benefit is likely perceptible to patients, but that is only half the problem. The other half is whether the developer can rule out that survival is not less than it would have been with no treatment. If patients take this, will they feel better but have a greater risk of being hurt?”
So far, no drug or device developer has succeeded in proving this to the FDA, despite the agency’s 2009 guidance on how it could be done.
That guidance “is one of the two worst and most destructive guidance documents we ever published,” Dr. Stockbridge declared.
Dr. Walsh, Dr. Heidenreich, Dr. Zuckerman, Dr. Dashiell-Aje, and Dr. Stockbridge had no relevant disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – The Food and Drug Administration is keenly seeking patient-reported outcomes as endpoints in cardiovascular drug or device trials, particularly for heart failure patients, but the bar remains high for getting such an outcome into labeling, said agency officials who regulate cardiovascular disease therapies.
The FDA issued guidance nearly 8 years ago on how to integrate patient-reported outcome (PRO) measures into medical product development, but so far no heart failure drug nor device has met the agency’s standards for documented success in improving a PRO, despite the clear need for these patients to receive patient-centered care, clinicians said.
“We don’t yet have a patient-reported outcome in a label for heart failure,” Paul A. Heidenreich, MD, said during a session on PROs at the annual scientific meeting of the Heart Failure Society of America. He voiced hope that a PRO might end up on the label of a heart failure drug or device sometime in 2018. “Almost half of FDA submissions now include a PRO” as part of the data package, added Dr. Heidenreich, a cardiologist and professor of medicine at Stanford (Calif.) University.
For years, PROs for heart failure weren’t often used in trials, and they remain largely absent from routine practice – an absence Dr. Heidenreich lamented. “Just focusing on mortality in heart failure is really not patient centered,” he said.
Heart failure physicians “are very good at disease-centered care” that focuses on survival and reducing hospitalizations, but “survival is often not as important to patients,” noted Mary Norine Walsh, MD, medical director of the heart failure and cardiac transplantation program at St. Vincent Medical Group in Indianapolis. She suggested “tailoring treatment to improve patient symptoms, physical function, and quality of life” without necessarily reducing hospital readmissions or increasing survival rates. “Self-reported measures have more meaning for patients,” she said, and called for using PROs to better target interventions to the patients who can most benefit from them.
Two FDA representatives who spoke during the session agreed on the importance of PROs and attested to the agency’s interest in greater reliance on them.
“PROs are a critical complement to the other measures made in device trials,” said Bram Zuckerman, MD, director of the FDA’s division of cardiovascular devices. “We need PRO information because it reflects important aspects of patients’ health-related quality of life.”
The most commonly used PRO measures in device trials today are the Kansas City Cardiomyopathy Questionnaire (J Am Coll Cardiol. 2000 Apr;35[5]:1245-55) and the Minnesota Living With Heart Failure questionnaire, he noted.
“Neither is perfect, but there is a track record in heart failure device development that these two PROs can be helpful.” The FDA’s cardiovascular device division “wants to use PRO information,” Dr. Zuckerman said.
“All-cause mortality is the most unbiased endpoint, but there is interest in PROs,” agreed Ebony Dashiell-Aje, PhD, from the FDA’s office of new drugs in the Center for Drug Evaluation and Research. She highlighted the encouragement that the FDA gave to drug and device developers to include PROs in trials, both in its 2009 guidance document as well as in a “roadmap” from the agency on how to measure PROs in clinical trials. “Unfortunately, in heart failure we struggle to find tools that can adequately measure the patient’s perspective and be sensitive enough to detect a treatment benefit,” she said.
Norman Stockbridge, MD, director of the division of cardiovascular and renal products in the agency’s Office of Drug Evaluation, cited even bigger barriers to FDA approval of PROs as labeled effects from drugs or devices.
Getting a PRO endpoint supported by clinical-trial results that qualify it for an FDA label faces two big challenges. One challenge, he said, is “how much of an effect we need to see in a complex scoring algorithm to know that patients actually received some benefit in a disease that often varies from day to day and from week to week.” The second challenge is that, “in a disease with a high background rate of bad outcomes, you need some evidence that the benefit [from the treatment] is worth any risk,” which is something that can be hard to prove in heart failure when many patients don’t live more than 2 years with the disease, Dr. Stockbridge said in an interview.
“You need to be able to make the argument that the [PRO] benefit is likely perceptible to patients, but that is only half the problem. The other half is whether the developer can rule out that survival is not less than it would have been with no treatment. If patients take this, will they feel better but have a greater risk of being hurt?”
So far, no drug or device developer has succeeded in proving this to the FDA, despite the agency’s 2009 guidance on how it could be done.
That guidance “is one of the two worst and most destructive guidance documents we ever published,” Dr. Stockbridge declared.
Dr. Walsh, Dr. Heidenreich, Dr. Zuckerman, Dr. Dashiell-Aje, and Dr. Stockbridge had no relevant disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM THE HFSA ANNUAL SCIENTIFIC MEETING
Fentanyl in the cath lab questioned
BARCELONA – The current routine use of intravenous fentanyl in the cardiac catheterization lab for patient comfort during coronary angiography has been called into question by the results of a double-blind randomized trial presented at the annual congress of the European Society of Cardiology.
The trial, known as PACIFY, showed that IV fentanyl delayed absorption of the oral P2Y12 inhibitor ticagrelor (Brilinta) by up to 4 hours. That’s a disturbing finding that could account for the relatively high risk of stent thrombosis in the first hours after percutaneous coronary intervention, according to lead investigator John W. McEvoy, MD, a cardiologist at Johns Hopkins University in Baltimore.
“These data challenge the routine and nonselective use of fentanyl for cardiac catheterization and PCI, particularly when rapid platelet inhibition is desirable,” he said, adding, “This would represent a significant change in U.S. cath lab practice.”
PACIFY (Platelet Aggregation After Ticagrelor Inhibition and Fentanyl) was a single-center trial in which 212 patients undergoing PCI were randomized in double-blind fashion to fentanyl or no fentanyl on top of a local anesthetic and IV midazolam (Versed). In addition, the 70 subjects undergoing PCI with stent placement received a 180-mg loading dose of ticagrelor intraprocedurally.
The primary endpoint was ticagrelor plasma concentration during the first 24 hours after the drug’s administration. Secondary endpoints were patients’ self-reported maximum pain during the procedure and platelet inhibition at 2 hours.
The plasma concentration time area under the curve over the course of 24 hours was superior in the no-fentanyl group by a margin of 3,441 ng/mL–1 per hour to 2,016 ng/mL–1 per hour. Moreover, 37% of fentanyl recipients displayed high platelet reactivity at 2 hours as measured by light transmission platelet aggregometry, compared with none of the no-fentanyl controls.
Pain was similarly well controlled in both treatment arms, casting doubt on the widespread belief among U.S. interventionalists that routine administration of fentanyl in the cath lab is necessary for patient comfort. Patients in the control arm could receive bailout fentanyl upon request; only two did so.
Dr. McEvoy reported having no financial conflicts regarding this study, which was conducted free of commercial support.
BARCELONA – The current routine use of intravenous fentanyl in the cardiac catheterization lab for patient comfort during coronary angiography has been called into question by the results of a double-blind randomized trial presented at the annual congress of the European Society of Cardiology.
The trial, known as PACIFY, showed that IV fentanyl delayed absorption of the oral P2Y12 inhibitor ticagrelor (Brilinta) by up to 4 hours. That’s a disturbing finding that could account for the relatively high risk of stent thrombosis in the first hours after percutaneous coronary intervention, according to lead investigator John W. McEvoy, MD, a cardiologist at Johns Hopkins University in Baltimore.
“These data challenge the routine and nonselective use of fentanyl for cardiac catheterization and PCI, particularly when rapid platelet inhibition is desirable,” he said, adding, “This would represent a significant change in U.S. cath lab practice.”
PACIFY (Platelet Aggregation After Ticagrelor Inhibition and Fentanyl) was a single-center trial in which 212 patients undergoing PCI were randomized in double-blind fashion to fentanyl or no fentanyl on top of a local anesthetic and IV midazolam (Versed). In addition, the 70 subjects undergoing PCI with stent placement received a 180-mg loading dose of ticagrelor intraprocedurally.
The primary endpoint was ticagrelor plasma concentration during the first 24 hours after the drug’s administration. Secondary endpoints were patients’ self-reported maximum pain during the procedure and platelet inhibition at 2 hours.
The plasma concentration time area under the curve over the course of 24 hours was superior in the no-fentanyl group by a margin of 3,441 ng/mL–1 per hour to 2,016 ng/mL–1 per hour. Moreover, 37% of fentanyl recipients displayed high platelet reactivity at 2 hours as measured by light transmission platelet aggregometry, compared with none of the no-fentanyl controls.
Pain was similarly well controlled in both treatment arms, casting doubt on the widespread belief among U.S. interventionalists that routine administration of fentanyl in the cath lab is necessary for patient comfort. Patients in the control arm could receive bailout fentanyl upon request; only two did so.
Dr. McEvoy reported having no financial conflicts regarding this study, which was conducted free of commercial support.
BARCELONA – The current routine use of intravenous fentanyl in the cardiac catheterization lab for patient comfort during coronary angiography has been called into question by the results of a double-blind randomized trial presented at the annual congress of the European Society of Cardiology.
The trial, known as PACIFY, showed that IV fentanyl delayed absorption of the oral P2Y12 inhibitor ticagrelor (Brilinta) by up to 4 hours. That’s a disturbing finding that could account for the relatively high risk of stent thrombosis in the first hours after percutaneous coronary intervention, according to lead investigator John W. McEvoy, MD, a cardiologist at Johns Hopkins University in Baltimore.
“These data challenge the routine and nonselective use of fentanyl for cardiac catheterization and PCI, particularly when rapid platelet inhibition is desirable,” he said, adding, “This would represent a significant change in U.S. cath lab practice.”
PACIFY (Platelet Aggregation After Ticagrelor Inhibition and Fentanyl) was a single-center trial in which 212 patients undergoing PCI were randomized in double-blind fashion to fentanyl or no fentanyl on top of a local anesthetic and IV midazolam (Versed). In addition, the 70 subjects undergoing PCI with stent placement received a 180-mg loading dose of ticagrelor intraprocedurally.
The primary endpoint was ticagrelor plasma concentration during the first 24 hours after the drug’s administration. Secondary endpoints were patients’ self-reported maximum pain during the procedure and platelet inhibition at 2 hours.
The plasma concentration time area under the curve over the course of 24 hours was superior in the no-fentanyl group by a margin of 3,441 ng/mL–1 per hour to 2,016 ng/mL–1 per hour. Moreover, 37% of fentanyl recipients displayed high platelet reactivity at 2 hours as measured by light transmission platelet aggregometry, compared with none of the no-fentanyl controls.
Pain was similarly well controlled in both treatment arms, casting doubt on the widespread belief among U.S. interventionalists that routine administration of fentanyl in the cath lab is necessary for patient comfort. Patients in the control arm could receive bailout fentanyl upon request; only two did so.
Dr. McEvoy reported having no financial conflicts regarding this study, which was conducted free of commercial support.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: High platelet reactivity at 2 hours was present in 37% of patients who underwent coronary angiography with IV fentanyl and in none randomized to going without the opiate.
Data source: PACIFY, a single-center, double-blind, randomized trial included 212 patients undergoing coronary angiography.
Disclosures: The presenter reported having no financial conflicts regarding this study, which was conducted free of commercial support.
CardioMEMS shows real-world success as use expands
DALLAS – Management of outpatients with advanced heart failure using an implanted pulmonary artery pressure monitor continues to show real-world efficacy and safety at least as impressive as in the pivotal trial for the device.
Data from the first waves of patients to receive the CardioMEMS implanted pulmonary artery pressure (PAP) monitor since it got Food and Drug Administration marketing approval in May 2014 also showed steady uptake of this fluid volume management strategy for patients with advanced heart failure, despite Medicare reimbursement issues in some U.S. regions, J. Thomas Heywood, MD, said at the at the annual scientific meeting of the Heart Failure Society of America. He estimated that more than 6,000 U.S. heart failure patients have now had a CardioMEMS PAP monitor implanted.
“The clinicians using CardioMEMS now have a lot more experience” than they had during the trial, he said in an interview. “They have more experience using the device, they know what treatments to use to lower PAP more effectively, and they are now convinced that patients will benefit from reducing diastolic PAP.”
Dr. Heywood estimated that tens of thousands more U.S. heart failure patients with New York Heart Association class III disease and a recent history of at least one heart failure hospitalization are eligible to receive an implanted PAP monitor, dwarfing the more than 6,000 patients who received a device so far.
The postapproval study
The newest efficacy data come from the first 300 patients enrolled in the CardioMEMS HF System Post Approval Study, a registry of patients receiving an implanted PAP monitor funded by the device’s manufacturer and scheduled to include a total of 1,200 patients. Dr. Heywood said full enrollment was on track for completion by the end of October 2017.
The first 300 patients enrolled in the postapproval study were older than the CHAMPION cohort; they averaged about 69 years of age, compared with about 62 years in CHAMPION, were more often women (38% vs. 28% in CHAMPION), and were more likely to have heart failure with preserved ejection fraction (41% vs. about 22%).
A similar pattern existed for the 6-month cumulative tally of PAP area under the curve, which showed an average rise of 42 mm Hg/day in the CHAMPION control patients, an average drop of 160 mm Hg/day in the CHAMPION patients managed using their CardioMEMS data, and a drop of 281 mm Hg/day in the 300 postapproval study patients.
“We’re now using the implanted sensor in a broader population of patients, and one wonders whether the effect will be diluted. What we see is at least as good as in the CHAMPION trial. This is just an early snapshot, but it is exciting that we see no erosion of the benefit. It’s a great indication that the correct patients are receiving it,” Dr. Raval said while presenting a poster at the meeting.
Further scrutiny of the same 300 patients showed another feature of the impact of PAP monitoring on patient outcomes: The first 90 days with the PAP monitor in place led to a greater number of tweaks in patient treatment and a steady fall in PAP. During days 91-180, PAP tended to level off, the number of medication adjustments dropped, and heart failure hospitalizations fell even more than in the first 90 days, Joanna M. Joly, MD, reported in a separate poster at the meeting.
The data showed “effective reduction” of PAP during the second half of the study despite fewer medication adjustments. How was that possible? Patients who transmit data on their PAPs undergo “modeling of their behavior” based on the feedback they receive from the device, Dr. Joly suggested. Regular measurement of their PAP and seeing how the number relates to their clinical status helps patients “understand the impact of their nonadherence to diet and their medications.” Another factor could be the growing familiarity clinicians develop over time with PAP fluctuations that individual patients display repeatedly that are usually self-correcting. Also, patients may undergo “hemodynamic remodeling” that results in improved self-correction of minor shifts in fluid volume and vascular tone, she said.
This pattern of a reduced need for interventions after the first 90 days with a PAP implant suggests that many patients managed this way may be able to transition to care largely delivered by local providers, or even play a greater role in their own self-care once their PAP and clinical state stabilizes, Dr. Joly said.
The findings imply that by the end of the first 90 days, “patients accept the device and manage themselves better. It becomes basically a behavioral device” that helps patients better optimize their diet and behavior, Dr. Raval observed.
Safety holds steady
Continued real-world use of PAP monitoring has also resulted in new safety insights. During the first 3 years when the CardioMEMS device was on the U.S. market, May 2014–May 2017, the FDA’s adverse event reporting system for devices, the Manufacturer and User Facility Device Experience (MAUDE) received reports on 177 unique adverse events in 155 patients implanted with a PAP monitor, Muthiah Vaduganathan, MD, reported at the meeting. During the same 3-year period, he estimated that at least 5,500 U.S. patients had received a CardioMEMS device, based on data Dr. Vaduganathan obtained from the manufacturer, Abbott. This works out to an adverse event rate of about 2.8%, virtually identical to the rate reported from CHAMPION, noted Dr. Vaduganathan, a cardiologist also at Brigham and Women’s.
Analysis of both the 22 deaths as well as the episodes of pulmonary artery injury or hemoptysis showed that the preponderance occurred relatively early after introduction for U.S. use, suggesting that “a learning curve may exist for the most serious complications,” he said. “Improved safety and device durability may result from careful patient selection, increased operator training, and refined technologies.”
Dr. Vaduganathan cautioned that the MAUDE database is limited by its bias toward serious adverse events, selective reporting, and lack of adjudication for the reported events. Concurrently with his report at the meeting, a written version appeared online (JAMA Cardiol. 2017 Sep 18. doi:10.1001/jamacardio.2017.3791).
“The adverse event rate was reassuringly low, well below the accepted threshold for device safety. It bodes favorably for the device,” he said in an interview.
“But with a passive surveillance system like MAUDE, adverse events are likely underreported; we see in MAUDE the most severe adverse events. There is certainly a larger spectrum of more minor events that we are not seeing, but I think these numbers accurately reflect serious events.” A full registry of every U.S. patient who receives the device, similar to what’s in place for U.S. patients who undergo transcatheter aortic valve replacement, would provide a more complete picture of the risks, Dr. Vaduganathan suggested.
He also voiced some surprise about the frequency of pulmonary artery injury, which was not as apparent in the 550 total patients enrolled in CHAMPION. Clinicians who place the PAP monitor are required to first take a training program, but the manufacturer has no mandated minimum number of placements an operator must assist on before launching a new CardioMEMS practice, Dr. Vaduganathan said. Many of the pulmonary artery injuries reported to MAUDE resulted from wire perforations that resulted from loss of wire control, he noted.
Clarifying the optimal CardioMEMS recipients
PAP monitoring for patients with advanced heart failure “is a major advance for certain patients who have historically been very challenging to manage,” especially patients with heart failure with preserved ejection fraction, which has few other treatment options. But “it’s often difficult to know when to pull the trigger” and proceed with placing a PAP monitor in an eligible patient, he said. “Greater experience will help us better understand that,” Dr. Vaduganathan predicted.
Dr. Heywood said that, in addition to the standard criteria of NYHA class III symptoms and a recent history of a heart failure hospitalization, the other clinical feature he looks for in a patient who is a possible CardioMEMS recipient is a persistently elevated systolic PAP as measured using echocardiography.
“These are patients with evidence of an ongoing hemodynamic problem despite treatment, and I need more data to do a better job of getting their PAP down.” Although the PAP that patients self-measure once they have the device in place is their diastolic PAP, measuring systolic PAP by echo is usually a good surrogate for finding patients who also have a persistently elevated diastolic PAP, he explained.
Another important selection criterion is to look for the patients who are dying from heart failure rather than with heart failure, Dr. Heywood added.
“If heart failure is the major thing wrong, then we can improve their quality of life” by guiding fluid management with regular PAP measurement, especially patients with preserved left ventricular ejection fraction who have few other treatment options right now, he said.
The CardioMEMS HF System Post Approval Study is sponsored by Abbott, which markets CardioMEMS. Dr Heywood has been a consultant to and/or has received research funding from Abbott as well as Impedimed, Medtronic, Novartis, and Otsuka. Dr. Raval has been a consultant to Abbott. Dr. Joly and Dr. Vaduganathan had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – Management of outpatients with advanced heart failure using an implanted pulmonary artery pressure monitor continues to show real-world efficacy and safety at least as impressive as in the pivotal trial for the device.
Data from the first waves of patients to receive the CardioMEMS implanted pulmonary artery pressure (PAP) monitor since it got Food and Drug Administration marketing approval in May 2014 also showed steady uptake of this fluid volume management strategy for patients with advanced heart failure, despite Medicare reimbursement issues in some U.S. regions, J. Thomas Heywood, MD, said at the at the annual scientific meeting of the Heart Failure Society of America. He estimated that more than 6,000 U.S. heart failure patients have now had a CardioMEMS PAP monitor implanted.
“The clinicians using CardioMEMS now have a lot more experience” than they had during the trial, he said in an interview. “They have more experience using the device, they know what treatments to use to lower PAP more effectively, and they are now convinced that patients will benefit from reducing diastolic PAP.”
Dr. Heywood estimated that tens of thousands more U.S. heart failure patients with New York Heart Association class III disease and a recent history of at least one heart failure hospitalization are eligible to receive an implanted PAP monitor, dwarfing the more than 6,000 patients who received a device so far.
The postapproval study
The newest efficacy data come from the first 300 patients enrolled in the CardioMEMS HF System Post Approval Study, a registry of patients receiving an implanted PAP monitor funded by the device’s manufacturer and scheduled to include a total of 1,200 patients. Dr. Heywood said full enrollment was on track for completion by the end of October 2017.
The first 300 patients enrolled in the postapproval study were older than the CHAMPION cohort; they averaged about 69 years of age, compared with about 62 years in CHAMPION, were more often women (38% vs. 28% in CHAMPION), and were more likely to have heart failure with preserved ejection fraction (41% vs. about 22%).
A similar pattern existed for the 6-month cumulative tally of PAP area under the curve, which showed an average rise of 42 mm Hg/day in the CHAMPION control patients, an average drop of 160 mm Hg/day in the CHAMPION patients managed using their CardioMEMS data, and a drop of 281 mm Hg/day in the 300 postapproval study patients.
“We’re now using the implanted sensor in a broader population of patients, and one wonders whether the effect will be diluted. What we see is at least as good as in the CHAMPION trial. This is just an early snapshot, but it is exciting that we see no erosion of the benefit. It’s a great indication that the correct patients are receiving it,” Dr. Raval said while presenting a poster at the meeting.
Further scrutiny of the same 300 patients showed another feature of the impact of PAP monitoring on patient outcomes: The first 90 days with the PAP monitor in place led to a greater number of tweaks in patient treatment and a steady fall in PAP. During days 91-180, PAP tended to level off, the number of medication adjustments dropped, and heart failure hospitalizations fell even more than in the first 90 days, Joanna M. Joly, MD, reported in a separate poster at the meeting.
The data showed “effective reduction” of PAP during the second half of the study despite fewer medication adjustments. How was that possible? Patients who transmit data on their PAPs undergo “modeling of their behavior” based on the feedback they receive from the device, Dr. Joly suggested. Regular measurement of their PAP and seeing how the number relates to their clinical status helps patients “understand the impact of their nonadherence to diet and their medications.” Another factor could be the growing familiarity clinicians develop over time with PAP fluctuations that individual patients display repeatedly that are usually self-correcting. Also, patients may undergo “hemodynamic remodeling” that results in improved self-correction of minor shifts in fluid volume and vascular tone, she said.
This pattern of a reduced need for interventions after the first 90 days with a PAP implant suggests that many patients managed this way may be able to transition to care largely delivered by local providers, or even play a greater role in their own self-care once their PAP and clinical state stabilizes, Dr. Joly said.
The findings imply that by the end of the first 90 days, “patients accept the device and manage themselves better. It becomes basically a behavioral device” that helps patients better optimize their diet and behavior, Dr. Raval observed.
Safety holds steady
Continued real-world use of PAP monitoring has also resulted in new safety insights. During the first 3 years when the CardioMEMS device was on the U.S. market, May 2014–May 2017, the FDA’s adverse event reporting system for devices, the Manufacturer and User Facility Device Experience (MAUDE) received reports on 177 unique adverse events in 155 patients implanted with a PAP monitor, Muthiah Vaduganathan, MD, reported at the meeting. During the same 3-year period, he estimated that at least 5,500 U.S. patients had received a CardioMEMS device, based on data Dr. Vaduganathan obtained from the manufacturer, Abbott. This works out to an adverse event rate of about 2.8%, virtually identical to the rate reported from CHAMPION, noted Dr. Vaduganathan, a cardiologist also at Brigham and Women’s.
Analysis of both the 22 deaths as well as the episodes of pulmonary artery injury or hemoptysis showed that the preponderance occurred relatively early after introduction for U.S. use, suggesting that “a learning curve may exist for the most serious complications,” he said. “Improved safety and device durability may result from careful patient selection, increased operator training, and refined technologies.”
Dr. Vaduganathan cautioned that the MAUDE database is limited by its bias toward serious adverse events, selective reporting, and lack of adjudication for the reported events. Concurrently with his report at the meeting, a written version appeared online (JAMA Cardiol. 2017 Sep 18. doi:10.1001/jamacardio.2017.3791).
“The adverse event rate was reassuringly low, well below the accepted threshold for device safety. It bodes favorably for the device,” he said in an interview.
“But with a passive surveillance system like MAUDE, adverse events are likely underreported; we see in MAUDE the most severe adverse events. There is certainly a larger spectrum of more minor events that we are not seeing, but I think these numbers accurately reflect serious events.” A full registry of every U.S. patient who receives the device, similar to what’s in place for U.S. patients who undergo transcatheter aortic valve replacement, would provide a more complete picture of the risks, Dr. Vaduganathan suggested.
He also voiced some surprise about the frequency of pulmonary artery injury, which was not as apparent in the 550 total patients enrolled in CHAMPION. Clinicians who place the PAP monitor are required to first take a training program, but the manufacturer has no mandated minimum number of placements an operator must assist on before launching a new CardioMEMS practice, Dr. Vaduganathan said. Many of the pulmonary artery injuries reported to MAUDE resulted from wire perforations that resulted from loss of wire control, he noted.
Clarifying the optimal CardioMEMS recipients
PAP monitoring for patients with advanced heart failure “is a major advance for certain patients who have historically been very challenging to manage,” especially patients with heart failure with preserved ejection fraction, which has few other treatment options. But “it’s often difficult to know when to pull the trigger” and proceed with placing a PAP monitor in an eligible patient, he said. “Greater experience will help us better understand that,” Dr. Vaduganathan predicted.
Dr. Heywood said that, in addition to the standard criteria of NYHA class III symptoms and a recent history of a heart failure hospitalization, the other clinical feature he looks for in a patient who is a possible CardioMEMS recipient is a persistently elevated systolic PAP as measured using echocardiography.
“These are patients with evidence of an ongoing hemodynamic problem despite treatment, and I need more data to do a better job of getting their PAP down.” Although the PAP that patients self-measure once they have the device in place is their diastolic PAP, measuring systolic PAP by echo is usually a good surrogate for finding patients who also have a persistently elevated diastolic PAP, he explained.
Another important selection criterion is to look for the patients who are dying from heart failure rather than with heart failure, Dr. Heywood added.
“If heart failure is the major thing wrong, then we can improve their quality of life” by guiding fluid management with regular PAP measurement, especially patients with preserved left ventricular ejection fraction who have few other treatment options right now, he said.
The CardioMEMS HF System Post Approval Study is sponsored by Abbott, which markets CardioMEMS. Dr Heywood has been a consultant to and/or has received research funding from Abbott as well as Impedimed, Medtronic, Novartis, and Otsuka. Dr. Raval has been a consultant to Abbott. Dr. Joly and Dr. Vaduganathan had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – Management of outpatients with advanced heart failure using an implanted pulmonary artery pressure monitor continues to show real-world efficacy and safety at least as impressive as in the pivotal trial for the device.
Data from the first waves of patients to receive the CardioMEMS implanted pulmonary artery pressure (PAP) monitor since it got Food and Drug Administration marketing approval in May 2014 also showed steady uptake of this fluid volume management strategy for patients with advanced heart failure, despite Medicare reimbursement issues in some U.S. regions, J. Thomas Heywood, MD, said at the at the annual scientific meeting of the Heart Failure Society of America. He estimated that more than 6,000 U.S. heart failure patients have now had a CardioMEMS PAP monitor implanted.
“The clinicians using CardioMEMS now have a lot more experience” than they had during the trial, he said in an interview. “They have more experience using the device, they know what treatments to use to lower PAP more effectively, and they are now convinced that patients will benefit from reducing diastolic PAP.”
Dr. Heywood estimated that tens of thousands more U.S. heart failure patients with New York Heart Association class III disease and a recent history of at least one heart failure hospitalization are eligible to receive an implanted PAP monitor, dwarfing the more than 6,000 patients who received a device so far.
The postapproval study
The newest efficacy data come from the first 300 patients enrolled in the CardioMEMS HF System Post Approval Study, a registry of patients receiving an implanted PAP monitor funded by the device’s manufacturer and scheduled to include a total of 1,200 patients. Dr. Heywood said full enrollment was on track for completion by the end of October 2017.
The first 300 patients enrolled in the postapproval study were older than the CHAMPION cohort; they averaged about 69 years of age, compared with about 62 years in CHAMPION, were more often women (38% vs. 28% in CHAMPION), and were more likely to have heart failure with preserved ejection fraction (41% vs. about 22%).
A similar pattern existed for the 6-month cumulative tally of PAP area under the curve, which showed an average rise of 42 mm Hg/day in the CHAMPION control patients, an average drop of 160 mm Hg/day in the CHAMPION patients managed using their CardioMEMS data, and a drop of 281 mm Hg/day in the 300 postapproval study patients.
“We’re now using the implanted sensor in a broader population of patients, and one wonders whether the effect will be diluted. What we see is at least as good as in the CHAMPION trial. This is just an early snapshot, but it is exciting that we see no erosion of the benefit. It’s a great indication that the correct patients are receiving it,” Dr. Raval said while presenting a poster at the meeting.
Further scrutiny of the same 300 patients showed another feature of the impact of PAP monitoring on patient outcomes: The first 90 days with the PAP monitor in place led to a greater number of tweaks in patient treatment and a steady fall in PAP. During days 91-180, PAP tended to level off, the number of medication adjustments dropped, and heart failure hospitalizations fell even more than in the first 90 days, Joanna M. Joly, MD, reported in a separate poster at the meeting.
The data showed “effective reduction” of PAP during the second half of the study despite fewer medication adjustments. How was that possible? Patients who transmit data on their PAPs undergo “modeling of their behavior” based on the feedback they receive from the device, Dr. Joly suggested. Regular measurement of their PAP and seeing how the number relates to their clinical status helps patients “understand the impact of their nonadherence to diet and their medications.” Another factor could be the growing familiarity clinicians develop over time with PAP fluctuations that individual patients display repeatedly that are usually self-correcting. Also, patients may undergo “hemodynamic remodeling” that results in improved self-correction of minor shifts in fluid volume and vascular tone, she said.
This pattern of a reduced need for interventions after the first 90 days with a PAP implant suggests that many patients managed this way may be able to transition to care largely delivered by local providers, or even play a greater role in their own self-care once their PAP and clinical state stabilizes, Dr. Joly said.
The findings imply that by the end of the first 90 days, “patients accept the device and manage themselves better. It becomes basically a behavioral device” that helps patients better optimize their diet and behavior, Dr. Raval observed.
Safety holds steady
Continued real-world use of PAP monitoring has also resulted in new safety insights. During the first 3 years when the CardioMEMS device was on the U.S. market, May 2014–May 2017, the FDA’s adverse event reporting system for devices, the Manufacturer and User Facility Device Experience (MAUDE) received reports on 177 unique adverse events in 155 patients implanted with a PAP monitor, Muthiah Vaduganathan, MD, reported at the meeting. During the same 3-year period, he estimated that at least 5,500 U.S. patients had received a CardioMEMS device, based on data Dr. Vaduganathan obtained from the manufacturer, Abbott. This works out to an adverse event rate of about 2.8%, virtually identical to the rate reported from CHAMPION, noted Dr. Vaduganathan, a cardiologist also at Brigham and Women’s.
Analysis of both the 22 deaths as well as the episodes of pulmonary artery injury or hemoptysis showed that the preponderance occurred relatively early after introduction for U.S. use, suggesting that “a learning curve may exist for the most serious complications,” he said. “Improved safety and device durability may result from careful patient selection, increased operator training, and refined technologies.”
Dr. Vaduganathan cautioned that the MAUDE database is limited by its bias toward serious adverse events, selective reporting, and lack of adjudication for the reported events. Concurrently with his report at the meeting, a written version appeared online (JAMA Cardiol. 2017 Sep 18. doi:10.1001/jamacardio.2017.3791).
“The adverse event rate was reassuringly low, well below the accepted threshold for device safety. It bodes favorably for the device,” he said in an interview.
“But with a passive surveillance system like MAUDE, adverse events are likely underreported; we see in MAUDE the most severe adverse events. There is certainly a larger spectrum of more minor events that we are not seeing, but I think these numbers accurately reflect serious events.” A full registry of every U.S. patient who receives the device, similar to what’s in place for U.S. patients who undergo transcatheter aortic valve replacement, would provide a more complete picture of the risks, Dr. Vaduganathan suggested.
He also voiced some surprise about the frequency of pulmonary artery injury, which was not as apparent in the 550 total patients enrolled in CHAMPION. Clinicians who place the PAP monitor are required to first take a training program, but the manufacturer has no mandated minimum number of placements an operator must assist on before launching a new CardioMEMS practice, Dr. Vaduganathan said. Many of the pulmonary artery injuries reported to MAUDE resulted from wire perforations that resulted from loss of wire control, he noted.
Clarifying the optimal CardioMEMS recipients
PAP monitoring for patients with advanced heart failure “is a major advance for certain patients who have historically been very challenging to manage,” especially patients with heart failure with preserved ejection fraction, which has few other treatment options. But “it’s often difficult to know when to pull the trigger” and proceed with placing a PAP monitor in an eligible patient, he said. “Greater experience will help us better understand that,” Dr. Vaduganathan predicted.
Dr. Heywood said that, in addition to the standard criteria of NYHA class III symptoms and a recent history of a heart failure hospitalization, the other clinical feature he looks for in a patient who is a possible CardioMEMS recipient is a persistently elevated systolic PAP as measured using echocardiography.
“These are patients with evidence of an ongoing hemodynamic problem despite treatment, and I need more data to do a better job of getting their PAP down.” Although the PAP that patients self-measure once they have the device in place is their diastolic PAP, measuring systolic PAP by echo is usually a good surrogate for finding patients who also have a persistently elevated diastolic PAP, he explained.
Another important selection criterion is to look for the patients who are dying from heart failure rather than with heart failure, Dr. Heywood added.
“If heart failure is the major thing wrong, then we can improve their quality of life” by guiding fluid management with regular PAP measurement, especially patients with preserved left ventricular ejection fraction who have few other treatment options right now, he said.
The CardioMEMS HF System Post Approval Study is sponsored by Abbott, which markets CardioMEMS. Dr Heywood has been a consultant to and/or has received research funding from Abbott as well as Impedimed, Medtronic, Novartis, and Otsuka. Dr. Raval has been a consultant to Abbott. Dr. Joly and Dr. Vaduganathan had no disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
MI, stroke risk from HFrEF surpasses HFpEF
DALLAS – Patients newly diagnosed with heart failure with reduced ejection fraction had about an 8% incidence of MIs during the subsequent 9 months, and a 5% incidence of ischemic strokes in a retrospective review of more than 1,600 community-dwelling U.S. patients.
The MI and ischemic stroke incidence rates in heart failure patients with reduced ejection fraction (HFrEF) were both significantly higher than in more than 4,000 patients with heart failure with preserved ejection fraction (HFpEF), Gregg C. Fonarow, MD, said while presenting a poster at the annual scientific meeting of the Heart Failure Society of America.
The findings suggest that greater attention is needed to reduce the risks for MI and stroke in HFrEF patients, suggested Dr. Fonarow, professor and cochief of cardiology at the University of California, Los Angeles, and his associates in their poster.
The study used claims data collected during July 2009-September 2016 from more than 10 million people enrolled in the United Health Group, who received care at more than 650 hospitals and about 6,600 clinics. The study included all patients diagnosed with heart failure during a hospital or emergency room visit and who had no history of a heart failure diagnosis or episode during the preceding 18 months, a left ventricular ejection fraction measurement made close to the time of the index encounter, and no stroke or MI apparent at the time of the index event. The study included 1,622 patients with HFrEF, defined as a left ventricular ejection fraction of less than 40%, 4,288 with HFpEF, defined as an ejection fraction of 50% or more, and 1,095 with heart failure with a borderline ejection fraction of 40%-49%.
The HFrEF patients had an average ejection fraction of 28%, they averaged 72 years old, 36% were women, and 8% had a prior stroke. The HFpEF patients averaged 74 years old, their average ejection fraction was 61%, 55% were women, and 11% had a prior stroke. Follow-up data on all patients were available for an average of nearly 9 months following their index heart failure event, with some patients followed as long as 1 year.
During follow-up, the incidence of ischemic stroke was 5.4% in the HFrEF patients and 3.9% in those with HFpEF, a difference that worked out to a statistically significant 40% higher ischemic stroke rate in HFrEF patients after adjustment for baseline differences between the two patient groups, Dr. Fonarow reported. The patients with a borderline ejection fraction had a 3.7% stroke incidence that fell short of a significant difference, compared with the HFrEF patient.The rate of new MIs during follow-up was 7.5% in the HFrEF patients and 3.2% in the HFpEF patients, a statistically significant 2.5-fold relatively higher MI rate with HFrEF, a statistically significant difference after adjustments. The MI incidence in patients with a borderline ejection fraction was 5.9%
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – Patients newly diagnosed with heart failure with reduced ejection fraction had about an 8% incidence of MIs during the subsequent 9 months, and a 5% incidence of ischemic strokes in a retrospective review of more than 1,600 community-dwelling U.S. patients.
The MI and ischemic stroke incidence rates in heart failure patients with reduced ejection fraction (HFrEF) were both significantly higher than in more than 4,000 patients with heart failure with preserved ejection fraction (HFpEF), Gregg C. Fonarow, MD, said while presenting a poster at the annual scientific meeting of the Heart Failure Society of America.
The findings suggest that greater attention is needed to reduce the risks for MI and stroke in HFrEF patients, suggested Dr. Fonarow, professor and cochief of cardiology at the University of California, Los Angeles, and his associates in their poster.
The study used claims data collected during July 2009-September 2016 from more than 10 million people enrolled in the United Health Group, who received care at more than 650 hospitals and about 6,600 clinics. The study included all patients diagnosed with heart failure during a hospital or emergency room visit and who had no history of a heart failure diagnosis or episode during the preceding 18 months, a left ventricular ejection fraction measurement made close to the time of the index encounter, and no stroke or MI apparent at the time of the index event. The study included 1,622 patients with HFrEF, defined as a left ventricular ejection fraction of less than 40%, 4,288 with HFpEF, defined as an ejection fraction of 50% or more, and 1,095 with heart failure with a borderline ejection fraction of 40%-49%.
The HFrEF patients had an average ejection fraction of 28%, they averaged 72 years old, 36% were women, and 8% had a prior stroke. The HFpEF patients averaged 74 years old, their average ejection fraction was 61%, 55% were women, and 11% had a prior stroke. Follow-up data on all patients were available for an average of nearly 9 months following their index heart failure event, with some patients followed as long as 1 year.
During follow-up, the incidence of ischemic stroke was 5.4% in the HFrEF patients and 3.9% in those with HFpEF, a difference that worked out to a statistically significant 40% higher ischemic stroke rate in HFrEF patients after adjustment for baseline differences between the two patient groups, Dr. Fonarow reported. The patients with a borderline ejection fraction had a 3.7% stroke incidence that fell short of a significant difference, compared with the HFrEF patient.The rate of new MIs during follow-up was 7.5% in the HFrEF patients and 3.2% in the HFpEF patients, a statistically significant 2.5-fold relatively higher MI rate with HFrEF, a statistically significant difference after adjustments. The MI incidence in patients with a borderline ejection fraction was 5.9%
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – Patients newly diagnosed with heart failure with reduced ejection fraction had about an 8% incidence of MIs during the subsequent 9 months, and a 5% incidence of ischemic strokes in a retrospective review of more than 1,600 community-dwelling U.S. patients.
The MI and ischemic stroke incidence rates in heart failure patients with reduced ejection fraction (HFrEF) were both significantly higher than in more than 4,000 patients with heart failure with preserved ejection fraction (HFpEF), Gregg C. Fonarow, MD, said while presenting a poster at the annual scientific meeting of the Heart Failure Society of America.
The findings suggest that greater attention is needed to reduce the risks for MI and stroke in HFrEF patients, suggested Dr. Fonarow, professor and cochief of cardiology at the University of California, Los Angeles, and his associates in their poster.
The study used claims data collected during July 2009-September 2016 from more than 10 million people enrolled in the United Health Group, who received care at more than 650 hospitals and about 6,600 clinics. The study included all patients diagnosed with heart failure during a hospital or emergency room visit and who had no history of a heart failure diagnosis or episode during the preceding 18 months, a left ventricular ejection fraction measurement made close to the time of the index encounter, and no stroke or MI apparent at the time of the index event. The study included 1,622 patients with HFrEF, defined as a left ventricular ejection fraction of less than 40%, 4,288 with HFpEF, defined as an ejection fraction of 50% or more, and 1,095 with heart failure with a borderline ejection fraction of 40%-49%.
The HFrEF patients had an average ejection fraction of 28%, they averaged 72 years old, 36% were women, and 8% had a prior stroke. The HFpEF patients averaged 74 years old, their average ejection fraction was 61%, 55% were women, and 11% had a prior stroke. Follow-up data on all patients were available for an average of nearly 9 months following their index heart failure event, with some patients followed as long as 1 year.
During follow-up, the incidence of ischemic stroke was 5.4% in the HFrEF patients and 3.9% in those with HFpEF, a difference that worked out to a statistically significant 40% higher ischemic stroke rate in HFrEF patients after adjustment for baseline differences between the two patient groups, Dr. Fonarow reported. The patients with a borderline ejection fraction had a 3.7% stroke incidence that fell short of a significant difference, compared with the HFrEF patient.The rate of new MIs during follow-up was 7.5% in the HFrEF patients and 3.2% in the HFpEF patients, a statistically significant 2.5-fold relatively higher MI rate with HFrEF, a statistically significant difference after adjustments. The MI incidence in patients with a borderline ejection fraction was 5.9%
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: HFrEF patients had a 40% higher incidence of stroke and a 2.5-fold higher incidence of MI, compared with HFpEF patients.
Data source: Retrospective review of 7,005 U.S. patients newly diagnosed with heart failure.
Disclosures: The study was funded by Janssen. Dr. Fonarow had no relevant disclosures.
Higher stroke risk found for TAVR versus SAVR
SAN DIEGO – There was an 86% greater risk of ischemic stroke after transcatheter aortic valve replacement, compared with surgical aortic valve replacement, and a more than sixfold increased risk of hemorrhagic stroke, in a review of more than 44,000 patients in the Nationwide Readmissions Database who were followed out to a year after having one procedure or the other.
“Our data suggest an elevated risk of both ischemic and hemorrhagic stroke after TAVR [transcatheter aortic valve replacement]. I see a lot of people that have strokes after” TAVR, so “I wasn’t all that surprised that there is an increased risk, but could I have guessed it would have been so high? No.” Perhaps “we are offering it to people we shouldn’t be offering it to,” said lead investigator Laura Stein, MD, a vascular neurology fellow at Mount Sinai Hospital, New York.
The 2013 Nationwide Readmissions Database used in the study captured more than 14 million readmissions in the United States across all payers and the uninsured. “We used this database because its captures all comers” and reflects “more real-world practice,” Dr. Stein said.
There were 6,015 TAVR and 38,624 SAVR cases in 2013, and the team found consistently elevated cumulative risks of ischemic and hemorrhagic stroke after TAVR, compared with SAVR, according to a presentation at the annual meeting of the American Neurological Association.
Compared with SAVR, the hazard ratio for ischemic stroke with TAVR was 1.86 (95% confidence interval, 1.12-3.08; P = .016) and, for hemorrhagic stroke, 6.17 (95% CI, 1.97-19.33; P = .0018). Dr. Stein declined to release absolute numbers of strokes in the two groups, pending publication.
“A lot of attention is being paid to this topic because there has been a push, a lot of it by the device makers, to prove that [TAVR] outcomes are just as good as with traditional surgery, and that we should be offering [TAVR] to more people with higher risk factor profiles who might not have been offered repair otherwise. Our job is to help patients make the most informed decisions. Having another source of data like [ours]” adds to the conversation about risks and benefits, she said.
The investigators adjusted for a large number of potential confounders to make sure the comparison was as fair as possible given the limits of database reviews. Among other variables, they controlled for baseline cardiovascular risk factors, carotid artery disease, heart failure, obesity, smoking, surgical complications, mortality, and illness severity scores, as well as hospital size, teaching hospital status, and urban versus rural location.
“What we can’t know is what medications these patients were on that might have increased their bleeding or ischemia risk. Also, we were relying on coding done by other people,” Dr. Stein said.
The next step is to look at the impact of stenting and other concomitant procedures. “We were surprised by the number of people that had multiple procedures at the same time.” The ultimate goal is to develop a risk score to help patients and doctors decide between the two procedures, she said.
Meanwhile, the team found no difference in stroke risk between coronary artery bypass grafting and percutaneous coronary interventions in the 2013 database.
Three was no industry funding for the work, and Dr. Stein did not have any relevant disclosures.
SAN DIEGO – There was an 86% greater risk of ischemic stroke after transcatheter aortic valve replacement, compared with surgical aortic valve replacement, and a more than sixfold increased risk of hemorrhagic stroke, in a review of more than 44,000 patients in the Nationwide Readmissions Database who were followed out to a year after having one procedure or the other.
“Our data suggest an elevated risk of both ischemic and hemorrhagic stroke after TAVR [transcatheter aortic valve replacement]. I see a lot of people that have strokes after” TAVR, so “I wasn’t all that surprised that there is an increased risk, but could I have guessed it would have been so high? No.” Perhaps “we are offering it to people we shouldn’t be offering it to,” said lead investigator Laura Stein, MD, a vascular neurology fellow at Mount Sinai Hospital, New York.
The 2013 Nationwide Readmissions Database used in the study captured more than 14 million readmissions in the United States across all payers and the uninsured. “We used this database because its captures all comers” and reflects “more real-world practice,” Dr. Stein said.
There were 6,015 TAVR and 38,624 SAVR cases in 2013, and the team found consistently elevated cumulative risks of ischemic and hemorrhagic stroke after TAVR, compared with SAVR, according to a presentation at the annual meeting of the American Neurological Association.
Compared with SAVR, the hazard ratio for ischemic stroke with TAVR was 1.86 (95% confidence interval, 1.12-3.08; P = .016) and, for hemorrhagic stroke, 6.17 (95% CI, 1.97-19.33; P = .0018). Dr. Stein declined to release absolute numbers of strokes in the two groups, pending publication.
“A lot of attention is being paid to this topic because there has been a push, a lot of it by the device makers, to prove that [TAVR] outcomes are just as good as with traditional surgery, and that we should be offering [TAVR] to more people with higher risk factor profiles who might not have been offered repair otherwise. Our job is to help patients make the most informed decisions. Having another source of data like [ours]” adds to the conversation about risks and benefits, she said.
The investigators adjusted for a large number of potential confounders to make sure the comparison was as fair as possible given the limits of database reviews. Among other variables, they controlled for baseline cardiovascular risk factors, carotid artery disease, heart failure, obesity, smoking, surgical complications, mortality, and illness severity scores, as well as hospital size, teaching hospital status, and urban versus rural location.
“What we can’t know is what medications these patients were on that might have increased their bleeding or ischemia risk. Also, we were relying on coding done by other people,” Dr. Stein said.
The next step is to look at the impact of stenting and other concomitant procedures. “We were surprised by the number of people that had multiple procedures at the same time.” The ultimate goal is to develop a risk score to help patients and doctors decide between the two procedures, she said.
Meanwhile, the team found no difference in stroke risk between coronary artery bypass grafting and percutaneous coronary interventions in the 2013 database.
Three was no industry funding for the work, and Dr. Stein did not have any relevant disclosures.
SAN DIEGO – There was an 86% greater risk of ischemic stroke after transcatheter aortic valve replacement, compared with surgical aortic valve replacement, and a more than sixfold increased risk of hemorrhagic stroke, in a review of more than 44,000 patients in the Nationwide Readmissions Database who were followed out to a year after having one procedure or the other.
“Our data suggest an elevated risk of both ischemic and hemorrhagic stroke after TAVR [transcatheter aortic valve replacement]. I see a lot of people that have strokes after” TAVR, so “I wasn’t all that surprised that there is an increased risk, but could I have guessed it would have been so high? No.” Perhaps “we are offering it to people we shouldn’t be offering it to,” said lead investigator Laura Stein, MD, a vascular neurology fellow at Mount Sinai Hospital, New York.
The 2013 Nationwide Readmissions Database used in the study captured more than 14 million readmissions in the United States across all payers and the uninsured. “We used this database because its captures all comers” and reflects “more real-world practice,” Dr. Stein said.
There were 6,015 TAVR and 38,624 SAVR cases in 2013, and the team found consistently elevated cumulative risks of ischemic and hemorrhagic stroke after TAVR, compared with SAVR, according to a presentation at the annual meeting of the American Neurological Association.
Compared with SAVR, the hazard ratio for ischemic stroke with TAVR was 1.86 (95% confidence interval, 1.12-3.08; P = .016) and, for hemorrhagic stroke, 6.17 (95% CI, 1.97-19.33; P = .0018). Dr. Stein declined to release absolute numbers of strokes in the two groups, pending publication.
“A lot of attention is being paid to this topic because there has been a push, a lot of it by the device makers, to prove that [TAVR] outcomes are just as good as with traditional surgery, and that we should be offering [TAVR] to more people with higher risk factor profiles who might not have been offered repair otherwise. Our job is to help patients make the most informed decisions. Having another source of data like [ours]” adds to the conversation about risks and benefits, she said.
The investigators adjusted for a large number of potential confounders to make sure the comparison was as fair as possible given the limits of database reviews. Among other variables, they controlled for baseline cardiovascular risk factors, carotid artery disease, heart failure, obesity, smoking, surgical complications, mortality, and illness severity scores, as well as hospital size, teaching hospital status, and urban versus rural location.
“What we can’t know is what medications these patients were on that might have increased their bleeding or ischemia risk. Also, we were relying on coding done by other people,” Dr. Stein said.
The next step is to look at the impact of stenting and other concomitant procedures. “We were surprised by the number of people that had multiple procedures at the same time.” The ultimate goal is to develop a risk score to help patients and doctors decide between the two procedures, she said.
Meanwhile, the team found no difference in stroke risk between coronary artery bypass grafting and percutaneous coronary interventions in the 2013 database.
Three was no industry funding for the work, and Dr. Stein did not have any relevant disclosures.
AT ANA 2017
Key clinical point:
Major finding: There was an 86% greater risk of ischemic stroke after transcatheter aortic valve replacement, compared with surgical aortic valve replacement, and a more than sixfold increased risk of hemorrhagic stroke.
Data source: Database review of more than 44,000 patients
Disclosures: Three was no industry funding for the work, and the lead investigator did not have any relevant disclosures.
VIDEO: Intermittent furosemide during acute HFpEF favors kidneys
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
In the Diuretic Optimization Strategies Evaluation (DOSE) trial, we enrolled heart failure patients with a mix of reduced ejection fraction and preserved ejection fraction. The DOSE results showed no relationship between ejection fraction and the response to furosemide treatment by intermittent bolus or by continuous infusion in patients hospitalized with acute decompensated heart failure. The results also showed that continuous infusion was no better than intermittent bolus treatment, and following our report in 2011 (N Engl J Med. 2011 Mar 3;364[9]:797-805), many centers that had previously relied on continuous furosemide switched to use of bolus doses primarily because continuous infusion is much less convenient.
But it is important to keep in mind that trial results focus on averages and populations of patients. Anecdotally, we see some acute heart failure patients who seem to respond better to continuous infusion, and so some clinicians switch patients who do not respond well to bolus treatment to continuous infusion. In DOSE, we only tested the efficacy of the initial strategy; we have no evidence on whether or not changing the dosing strategy helps patients who do not respond adequately to an initial strategy of intermittent bolus doses.
G. Michael Felker, MD , professor of medicine at Duke University, Durham, N.C., made these comments in an interview. He has been a consultant to Amgen, Bristol-Myers Squibb, GlaxoSmithKline, Medtronic, MyoKardia, Novartis, Stealth, and Trevena.
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS – Patients with heart failure with preserved ejection fraction who were hospitalized for acute decompensation had a significantly smaller rise in serum creatinine when treated with intermittent, bolus doses of furosemide, compared with patients who received a continuous furosemide infusion in a single-center, randomized trial with 90 patients.
Intermittent furosemide also resulted in many fewer episodes of worsening renal function. In the trial, 12% of patients who received bolus furosemide doses developed worsening renal function during hospitalization compared with 36% of patients treated with a continuous furosemide infusion, Kavita Sharma, MD, said at the annual scientific meeting of the Heart Failure Society of America.
While acknowledging that this finding is preliminary because it was made in a relatively small, single-center study, “I’d be cautious about continuous infusion” in acute decompensated patients with heart failure with preserved ejection fraction (HFpEF); “bolus is preferred,” Dr. Sharma said in a video interview.
Results from the prior Diuretic Optimization Strategies Evaluation (DOSE) trial, published in 2011, had shown no significant difference in renal function in hospitalized heart failure patients randomized to receive either bolus or continuous furosemide, but that study largely enrolled patients with heart failure with reduced ejection fraction (HFrEF) (N Engl J Med. 2011 Mar 3;364[9]:797-805).
“When patients with HFpEF are hospitalized with acute heart failure there is a high rate of kidney injury, that often results in slowing diuresis leading to longer hospital stays. With adjustment for changes in blood pressure and volume of diuresis we saw a fourfold increase in worsening renal failure [with continuous infusion], so you should think twice before using continuous dosing,” said Dr. Sharma, a heart failure cardiologist at Johns Hopkins Medicine in Baltimore.
She presented results from Diuretics and Dopamine in Heart Failure With Preserved Ejection Fraction (ROPA-DOP), which randomized 90 hospitalized heart failure patients with a left ventricular ejection fraction of at least 50% and an estimated glomerular filtration rate of more than 15 mL/min/1.73 m2. The enrolled patients averaged 66 years old, 61% were women, their average body mass index was 41 kg/m2, and their average estimated glomerular filtration rate was 58 mL/min/1.73 m2.
The study’s primary endpoint was percent change in creatinine during hospitalization, which rose by an average 5% in the patients who received intermittent bolus furosemide and by an average 16% in patient who received a continuous infusion, a statistically significant difference. In a regression analysis that controlled for between-group differences in patient’s age, sex, race, body mass index, smoking status, changes in systolic blood pressure, heart rate, fluid balance after 72 hours, and other variables, patients treated with continuous furosemide infusion averaged an 11% greater increase in serum creatinine, Dr. Sharma reported. After similar adjustments, the secondary endpoint rate of worsening renal function was more than four times more likely to occur in the patients on continuous infusion compared with those who received intermittent bolus treatment, she said.
A second aspect of the ROPA-DOP trial randomized the same patients to received either low dose (3 mcg/kg per min) dopamine or placebo during hospitalization. The results showed that low-dose dopamine had no significant impact on either change in creatinine levels or on the incidence of worsening renal function compared with placebo, though dopamine treatment did link with a nonsignificant trend toward somewhat greater diuresis. These results were consistent with prior findings in the Renal Optimization Strategies Evaluation (ROSE) trial (JAMA. 2013 Nov 18;310[23]:2533-43), which used a mixed population of patients with HFpEF or HFrEF but predominantly patients with HFrEF, Dr. Sharma noted.
“It was a neutral finding [for dopamine in ROPA-DOP], and while there was no harm from dopamine there was clearly no benefit,” she said. It is possible that HFpEF patients with right ventricular dysfunction secondary to pulmonary hypertension might benefit from low-dose dopamine, but this needs further study, Dr. Sharma said.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Serum creatinine rose by an average 5% with intermittent bolus furosemide and by 16% with continuous infusion.
Data source: ROPA-DOP, a single-center randomized trial with 90 patients.
Disclosures: Dr. Sharma had no disclosures.
Phrenic nerve stimulator shows heart failure benefits
DALLAS– Heart failure patients with central sleep apnea who received treatment with a transvenous phrenic nerve–stimulating device showed dramatic improvement in their global self-assessment, compared with control patients, in a subgroup analysis of 80 patients enrolled in the device’s pivotal trial.
Among 35 patients with heart failure enrolled in the remedē System pivotal trial and treated for 6 months with phrenic nerve stimulation, 57% reported that they had “markedly” or “moderately” improved, compared with a 9% rate for this self-rating among 44 control heart failure patients in the trial, a statistically significant difference, Lee R. Goldberg, MD, said at the annual scientific meeting of the Heart Failure Society of America.
Further analysis focused on echocardiographic examinations after 12 months in 23 of the heart failure patients who entered the study with a left ventricular ejection fraction of 45% or less and received 12 months of phrenic nerve stimulation. The average LVEF rose in these patients from 30% at baseline to 35%, a statistically significant difference, and left ventricular end systolic volume fell by an average of almost 11 mL from baseline, a difference just short of statistical significance, findings Dr. Goldberg called “a little exciting.”
“It is very encouraging to see some evidence for ventricular remodeling,” commented Lynne W. Stevenson, MD, professor of medicine and a heart failure specialist at Vanderbilt University in Nashville, Tenn.
The FDA approved the use of this device for the treatment of moderate to severe central sleep apnea on Oct. 6. “I think we would use it” in heart failure patients with intolerable symptoms from central sleep apnea, Dr. Goldberg said in an interview during the meeting.
“There is a tight connection between sleep-disordered breathing, sleep apnea, heart failure, and cardiovascular disease, and we have been pretty aggressive in trying to treat the sleep apnea. Even if phrenic nerve stimulation just improves patients’ quality of life and is neutral for other outcomes,” it would be reasonable to offer it to patients, he said. “But many of us think there is a bigger connection that results in a therapeutic benefit [to heart failure patients] by treating their central sleep apnea.”
The pivotal trial enrolled a total of 151 patients with central sleep apnea at 31 centers in Germany, Poland, and the United States who were selected based on having an apnea-hypopnea index of at least 20 events per hour. All participants received a transvenous phrenic nerve–stimulator implant, and then randomization assigned 73 patients to have the device turned on for the first 6 months while 78 device recipients had their devices left off to serve as controls. The study’s primary efficacy endpoint was the percentage of patients having at least a 50% cut in their apnea-hypopnea index, which happened in 51% of evaluable patients in the active treatment arm and in 11% of the evaluable controls. The primary results were published last year (Lancet. 2016 Sep 3;388[10048]974-82).
“We hope this treatment will have the collateral effect of improving cardiovascular disease outcomes, but we don’t know that yet. The initial target will be patients with apnea-hypopnea episodes that affect their quality of life,” Dr. Goldberg said.
The apparent safety of this approach for treating central sleep apnea may relate to its mechanism of action, he suggested. The mortality-boosting effect of adaptive servo-ventilation may correlate with the positive pressure it creates in a patient’s chest that perhaps causes myocardial stress or hemodynamic problems. In contrast, phrenic nerve stimulation produces diaphragm motion that mimics normal breathing and creates negative chest pressure. “A lot of hypothesis generation needs to happen to better understand the underlying physiology,” Dr. Goldberg conceded.
At the end of the 6-month period that compared active treatment with control, the heart failure subgroup also showed statistically significant benefits from treatment for several sleep metrics, including apnea-hypopnea index, the central apnea index, and oxygen desaturation, and also for daytime sleepiness measured on the Epworth Sleepiness Scale. After 12 months on active treatment, patients also showed a significant improvement over baseline in their score on the Minnesota Living With Heart Failure Questionnaire, Dr. Goldberg reported.
The trial was sponsored by Respicardia, the company developing the remedē System. Dr. Goldberg has been a consultant to and has received research funding from Respicardia. Dr. Stevenson had no relevant disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS– Heart failure patients with central sleep apnea who received treatment with a transvenous phrenic nerve–stimulating device showed dramatic improvement in their global self-assessment, compared with control patients, in a subgroup analysis of 80 patients enrolled in the device’s pivotal trial.
Among 35 patients with heart failure enrolled in the remedē System pivotal trial and treated for 6 months with phrenic nerve stimulation, 57% reported that they had “markedly” or “moderately” improved, compared with a 9% rate for this self-rating among 44 control heart failure patients in the trial, a statistically significant difference, Lee R. Goldberg, MD, said at the annual scientific meeting of the Heart Failure Society of America.
Further analysis focused on echocardiographic examinations after 12 months in 23 of the heart failure patients who entered the study with a left ventricular ejection fraction of 45% or less and received 12 months of phrenic nerve stimulation. The average LVEF rose in these patients from 30% at baseline to 35%, a statistically significant difference, and left ventricular end systolic volume fell by an average of almost 11 mL from baseline, a difference just short of statistical significance, findings Dr. Goldberg called “a little exciting.”
“It is very encouraging to see some evidence for ventricular remodeling,” commented Lynne W. Stevenson, MD, professor of medicine and a heart failure specialist at Vanderbilt University in Nashville, Tenn.
The FDA approved the use of this device for the treatment of moderate to severe central sleep apnea on Oct. 6. “I think we would use it” in heart failure patients with intolerable symptoms from central sleep apnea, Dr. Goldberg said in an interview during the meeting.
“There is a tight connection between sleep-disordered breathing, sleep apnea, heart failure, and cardiovascular disease, and we have been pretty aggressive in trying to treat the sleep apnea. Even if phrenic nerve stimulation just improves patients’ quality of life and is neutral for other outcomes,” it would be reasonable to offer it to patients, he said. “But many of us think there is a bigger connection that results in a therapeutic benefit [to heart failure patients] by treating their central sleep apnea.”
The pivotal trial enrolled a total of 151 patients with central sleep apnea at 31 centers in Germany, Poland, and the United States who were selected based on having an apnea-hypopnea index of at least 20 events per hour. All participants received a transvenous phrenic nerve–stimulator implant, and then randomization assigned 73 patients to have the device turned on for the first 6 months while 78 device recipients had their devices left off to serve as controls. The study’s primary efficacy endpoint was the percentage of patients having at least a 50% cut in their apnea-hypopnea index, which happened in 51% of evaluable patients in the active treatment arm and in 11% of the evaluable controls. The primary results were published last year (Lancet. 2016 Sep 3;388[10048]974-82).
“We hope this treatment will have the collateral effect of improving cardiovascular disease outcomes, but we don’t know that yet. The initial target will be patients with apnea-hypopnea episodes that affect their quality of life,” Dr. Goldberg said.
The apparent safety of this approach for treating central sleep apnea may relate to its mechanism of action, he suggested. The mortality-boosting effect of adaptive servo-ventilation may correlate with the positive pressure it creates in a patient’s chest that perhaps causes myocardial stress or hemodynamic problems. In contrast, phrenic nerve stimulation produces diaphragm motion that mimics normal breathing and creates negative chest pressure. “A lot of hypothesis generation needs to happen to better understand the underlying physiology,” Dr. Goldberg conceded.
At the end of the 6-month period that compared active treatment with control, the heart failure subgroup also showed statistically significant benefits from treatment for several sleep metrics, including apnea-hypopnea index, the central apnea index, and oxygen desaturation, and also for daytime sleepiness measured on the Epworth Sleepiness Scale. After 12 months on active treatment, patients also showed a significant improvement over baseline in their score on the Minnesota Living With Heart Failure Questionnaire, Dr. Goldberg reported.
The trial was sponsored by Respicardia, the company developing the remedē System. Dr. Goldberg has been a consultant to and has received research funding from Respicardia. Dr. Stevenson had no relevant disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
DALLAS– Heart failure patients with central sleep apnea who received treatment with a transvenous phrenic nerve–stimulating device showed dramatic improvement in their global self-assessment, compared with control patients, in a subgroup analysis of 80 patients enrolled in the device’s pivotal trial.
Among 35 patients with heart failure enrolled in the remedē System pivotal trial and treated for 6 months with phrenic nerve stimulation, 57% reported that they had “markedly” or “moderately” improved, compared with a 9% rate for this self-rating among 44 control heart failure patients in the trial, a statistically significant difference, Lee R. Goldberg, MD, said at the annual scientific meeting of the Heart Failure Society of America.
Further analysis focused on echocardiographic examinations after 12 months in 23 of the heart failure patients who entered the study with a left ventricular ejection fraction of 45% or less and received 12 months of phrenic nerve stimulation. The average LVEF rose in these patients from 30% at baseline to 35%, a statistically significant difference, and left ventricular end systolic volume fell by an average of almost 11 mL from baseline, a difference just short of statistical significance, findings Dr. Goldberg called “a little exciting.”
“It is very encouraging to see some evidence for ventricular remodeling,” commented Lynne W. Stevenson, MD, professor of medicine and a heart failure specialist at Vanderbilt University in Nashville, Tenn.
The FDA approved the use of this device for the treatment of moderate to severe central sleep apnea on Oct. 6. “I think we would use it” in heart failure patients with intolerable symptoms from central sleep apnea, Dr. Goldberg said in an interview during the meeting.
“There is a tight connection between sleep-disordered breathing, sleep apnea, heart failure, and cardiovascular disease, and we have been pretty aggressive in trying to treat the sleep apnea. Even if phrenic nerve stimulation just improves patients’ quality of life and is neutral for other outcomes,” it would be reasonable to offer it to patients, he said. “But many of us think there is a bigger connection that results in a therapeutic benefit [to heart failure patients] by treating their central sleep apnea.”
The pivotal trial enrolled a total of 151 patients with central sleep apnea at 31 centers in Germany, Poland, and the United States who were selected based on having an apnea-hypopnea index of at least 20 events per hour. All participants received a transvenous phrenic nerve–stimulator implant, and then randomization assigned 73 patients to have the device turned on for the first 6 months while 78 device recipients had their devices left off to serve as controls. The study’s primary efficacy endpoint was the percentage of patients having at least a 50% cut in their apnea-hypopnea index, which happened in 51% of evaluable patients in the active treatment arm and in 11% of the evaluable controls. The primary results were published last year (Lancet. 2016 Sep 3;388[10048]974-82).
“We hope this treatment will have the collateral effect of improving cardiovascular disease outcomes, but we don’t know that yet. The initial target will be patients with apnea-hypopnea episodes that affect their quality of life,” Dr. Goldberg said.
The apparent safety of this approach for treating central sleep apnea may relate to its mechanism of action, he suggested. The mortality-boosting effect of adaptive servo-ventilation may correlate with the positive pressure it creates in a patient’s chest that perhaps causes myocardial stress or hemodynamic problems. In contrast, phrenic nerve stimulation produces diaphragm motion that mimics normal breathing and creates negative chest pressure. “A lot of hypothesis generation needs to happen to better understand the underlying physiology,” Dr. Goldberg conceded.
At the end of the 6-month period that compared active treatment with control, the heart failure subgroup also showed statistically significant benefits from treatment for several sleep metrics, including apnea-hypopnea index, the central apnea index, and oxygen desaturation, and also for daytime sleepiness measured on the Epworth Sleepiness Scale. After 12 months on active treatment, patients also showed a significant improvement over baseline in their score on the Minnesota Living With Heart Failure Questionnaire, Dr. Goldberg reported.
The trial was sponsored by Respicardia, the company developing the remedē System. Dr. Goldberg has been a consultant to and has received research funding from Respicardia. Dr. Stevenson had no relevant disclosures.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: Patient-reported global assessment improved markedly or moderately in 57% of treated patients and in 9% of controls.
Data source: Subgroup analysis of the remedē System pivotal trial.
Disclosures: The trial was sponsored by Respicardia, the company developing the remedē System. Dr. Goldberg has been a consultant to and has received research funding from Respicardia. Dr. Stevenson had no relevant disclosures.
Cardio-oncology booms but awareness lags
Cardio-oncology is expanding, fed by a steadily increasing population of cancer survivors at elevated risk for a range of cardiovascular diseases and complications because of the anticancer treatments they received. Cardio-oncology’s quick growth has also been driven by the rapidly expanding universe of cancer treatments with direct or indirect adverse effects on a diverse range of cardiovascular functions.
During the past year, the field’s rapid evolution has featured the first formal diagnostic and care standards in two iterations: A position paper on the cardiovascular toxicities of cancer treatment from the European Society of Cardiology (ESC), released in August 2016 (Eur Heart J. 2016 Sept 21;37[36]:2766-801); and a guideline for preventing and monitoring cardiac dysfunction in adult cancer survivors, issued last December by the American Society of Clinical Oncology (ASCO) and endorsed by the American Heart Association (J Clin Oncol. 2017 March 10;35[8]:893-913), but notably not endorsed by the American College of Cardiology, despite having an ACC representative on the guideline panel. In 2015, the ACC started a Cardio-Oncology Section, one of 20 special-interest sections it maintains, and by mid-2017 the section had some 500 members.
“I’ve had recent conversations with cardiologists who said ‘I’m not sure what cardio-oncology is,’ ” said Tomas G. Neilan, MD, director of the cardio-oncology program at Massachusetts General Hospital in Boston.
More than just heart failure
A few decades ago, in the primordial days of cardio-oncology, the concept of cardiovascular damage during cancer therapy focused entirely on myocardial damage caused by anthracyclines and chest radiation, a concern that eventually expanded to include trastuzumab (Herceptin) and other agents that target the human epidermal growth factor receptor 2 (HER2). These treatments cause significantly reduced left ventricular ejection fractions and heart failure in a significant minority of treated patients. Patients who receive combined treatment with an anthracycline and trastuzumab are at the highest risk for developing heart failure with reduced ejection fraction, but even among patients treated with this combination, fewer than 5% develop outright heart failure.
While this parochial view of cardio-oncology has recently shifted, it remains true that myocardial damage from a relatively large cumulative anthracycline dose, or from radiation, causes some of the most extreme cases of cardiovascular adverse effects and remains an ongoing problem as these treatments stay front line for selected cancer patients.
But some of the recent burgeoning of cardio-oncology has followed the recognition that many other drugs and drug classes can cause a spectrum of adverse cardiovascular effects.
“There has been a significant focus on heart failure and cardiomyopathy due to anthracyclines and HER2-targeted therapies. I think the field will continue to evolve over the next 5 years to focus on other cardiovascular complications, including arrhythmias and vascular disease,” observed Michael Fradley, MD, director of cardio-oncology at Moffitt Cancer Center in Tampa. “In addition, there will be an increased focus on targeted drugs and immunotherapies,” agents that Dr. Fradley said “have many unique cardiovascular complications. We need additional guidelines regarding the management of a variety of cardiotoxicities as well as long-term monitoring strategies.”
In a review article Dr. Moslehi published toward the end of 2016, he fleshed out the wider scope of adverse cardiovascular effects from cancer therapies, noting that the vascular endothelial growth factor (VEGF) signaling pathway inhibitors, drugs such as bevacizumab (Avastin) and aflibercept (Zaltrap), have been documented to cause hypertension, arterial thromboembolic events, and cardiomyopathy; and that tyrosine kinase inhibitors have been shown to cause vascular events, QT interval prolongation, and cerebral and peripheral vascular events (N Engl J Med. 2016 Oct 13;375[15]:1457-67).
In his own recent review, Dr. Fradley highlighted adverse cardiovascular effects from additional anticancer drug classes, including proteasome inhibitors, which can trigger hypertension and cardiomyopathy; immunomodulators, implicated in causing both venous and arterial thromboembolism; and the immune checkpoint inhibitors, linked with myocarditis, arrhythmias, hypotension, and myocardial ischemia (Eur Heart J. 2016 Sept 21;37[36]:2740-2). A similarly broad spectrum of adverse cardiovascular effects linked with a wide range of anticancer treatments also appeared in the ESC 2016 position paper on cancer treatments.
But while the range of cancer treatments that can have some impact on the cardiovascular system is strikingly large, experts uniformly caution that far from every patient treated for cancer needs an immediate cardiology consult and work-up, especially when the cancers appear in young adults.
“We’re not quite at the point where every cancer patient needs to be seen by a cardiologist or cardio-oncologist,” Dr. Fradley noted in an interview.
“If a patient develops hypertension while on treatment I refer them to a PCP or cardiologist. I don’t treat hypertension myself. But if a patient is ‘normal’ they don’t need a cardiology assessment up front. It’s impossible to refer all patients, especially younger patients, with current resources. There are too many patients who receive cardiotoxic therapies to refer everyone. I involve the cardiologist once there is evidence of damage,”she explained.
Cardio-oncology centers or community practice?
The rise of cardio-oncology, especially over the last decade or so, has given rise to a new academic niche, the cardio-oncology clinic. Starting from almost no programs a few years ago, by 2016 one tally put the total number of U.S. self-designated cardio-oncology centers at about 40 (Heart Fail Clin. 2017 April;13[2]:347-55), and that number undoubtedly grew even more during the year since. While these programs promote and advance the nascent subspecialty of cardio-oncology, and provide a foundation for development of formalized training programs, many experts see a clear hierarchy of risk that distinguishes the patients who should ideally be managed at these focused, multidisciplinary programs from the lower-risk patients who probably do fine under the care of just their oncologist or their oncologist in collaboration with a community cardiologist or primary care physician.
“The cardio-oncology community recognizes that it is nice to have programs at academic centers but it’s more important to deliver this care in the community,” said Dr. Lenihan. “Many cancer patients have no prior history of cardiovascular disease. These low-risk patients don’t necessarily need a cardio-oncologist. They may need to have their blood pressure managed more effectively or receive other preventive care, but that can certainly be done locally. There are low-risk patients who don’t need to go to a major center.” Dr. Lenihan and other cardio-oncologists see the majority of cancer patients as low risk when it comes to cardiovascular complications.
But it’s different when patients receive an anthracycline or an anthracycline plus trastuzumab. “This high-risk population is best seen at a cardio-oncology center.” Dr. Lenihan also included in this high-risk subgroup patients treated with mediastinal radiation, an option often used during the 1980s-2000s.
“Any time a patient receives treatment with the potential to cause a cardiovascular effect, which is pretty much any drug that now comes out, you need an accurate baseline assessment. But that doesn’t mean you need do anything different; you still treat the patient’s cancer. A thorough baseline assessment is a necessity, but it does not need to be done at a cardio-oncology center,” Dr. Lenihan said in an interview.
“For the vast majority of patients, care can be at community hospitals, similar to the delivery of the vast majority of oncology care. Some patients need referral to tertiary cardiology centers for advanced heart failure or to undergo advanced procedures, but that is a very small percentage of patients,” said Ana Barac, MD, director of the cardio-oncology program at the MedStar Heart Institute in Washington, and chair of the ACC’s Cardio-Oncology Section.
“Patients receiving more novel or unusual therapies, and those participating in trials” are appropriate for centers, while community care by a cardiologist and oncologist should suffice for more routine patients, said Dr. Fradley.
“Cardio-oncology centers are good for patients with type I damage from anthracycline treatment, especially patients who already had underlying heart disease,” said Michael S. Ewer, MD, a cardiologist and professor of medicine at MD Anderson Cancer Center in Houston. Specialist centers are also for patients with cardiovascular risk factors: older age, diabetes, preexisting coronary artery disease, and patients who receive cardiotoxic type I therapy (J Clin Oncol. 2005 May;23[13]:2900-2). Also, patients with a significant, immediate cardiac reaction to treatment, and those with an unexpected cardiac reaction, Dr. Ewer said.
A somewhat more expansive view of the typical cardio-oncology patient came from Dr. Neilan, based on the patients he sees at his program in Boston. Dr. Neilan estimated that roughly 60%-70% of his patients first present while they undergo active cancer treatment, with another 20% coming to the program as cancer survivors, and a small percentage of patients showing up for cardiology assessments and treatments without a cancer history. Among those with a cancer history, he guessed that perhaps 10%-20% were treated with an anthracycline, at least 10% received trastuzumab, and about 10% received radiation treatment. “I also see a lot of patients with complications from treatment” with tyrosine kinase inhibitors, VEGF inhibitors, and immunotherapies. “I don’t see a lot of patients for cardiovascular disease assessment before they start cancer therapy,” Dr. Neilan added.
Cardio-oncology heads toward a new cardiology subspecialty
These views of how cardio-oncology is practiced in the real world raise a question about the role of the growing roster of U.S. cardio-oncology programs. If most cancer patients can have their cardiology needs taken care of in the community, how do all the academic programs fit in? The answer seems to be that they model successful oncology and cardiology collaborations, provide a training ground for physicians from both specialties to learn how to collaborate, and serve as the home for research that broadens the field’s evidence base and moves knowledge forward.
“Education and partnerships with oncology teams is the key,” said Dr. Barac. “Our traditional subspecialty training focused on ‘treating cancer’ and ‘treating cardiovascular disease.’ Learning about and seeing effective partnerships during training” is the best model to foster cardiology and oncology partnerships among early-career physicians, she suggested.
“What is the spectrum of knowledge required to be proficient in cardio-oncology, and how do we enhance training at the resident or fellowship level? How do we get [all cardiology] trainees exposed to this knowledge?” wondered Dr. Lenihan, who viewed cardio-oncology programs as a way to meet these needs. “Cardio-oncology is not an established subspecialty. A goal is to establish training requirements and expand training opportunities. And the whole field needs to contribute to clinical research. We need cardio-oncologists to share their experience and improve our level of research.”
ASCO’s cardiac dysfunction practice guideline, first released last December and formally published in March, is likely helping to further entrench cardio-oncology as a new subspecialty. The guideline was “a remarkable step forward,” said Dr. Barac. In addition to establishing a U.S. standard of care for preventing and monitoring cardiac dysfunction in cancer patients, “I use it as a guide for creation of referral pathways with my oncology colleagues, as well as in education of cardiovascular and oncology trainees,” she said in an interview.
Though produced primarily through ASCO’s leadership, the target audience for the guideline seems to be as much cardiologists as it is oncologists. Dissemination of the guideline to cardiologists snagged when it failed to appear in the cardiology literature. That wasn’t the original plan, said guideline participants.
“Before we started, it was agreed that both ASCO and the ACC would publish it. We had a [letter] signed by the president of the ACC saying the ACC would publish it,” recalled Dr. Lenihan, a guideline coauthor. “After all the details were settled, the ACC bailed. They said that they had changed their organizational structure and that they wouldn’t publish the guideline even though they had agreed to.” Not having the guideline appear simultaneously in the cardiology literature “hinders getting the message to the cardiology community,” he said, a sentiment echoed by other cardio-oncologists.
“I served as the ACC representative on the guideline, and the lack of ACC endorsement was the unfortunate consequence of approval and publication timing that coincided with restructuring of the ACC committees,” said Dr. Barac. “It absolutely does not reflect a lack of interest from the ACC.” As an example of the College’s commitment example, she cited an ACC 1.5-day educational course on cardiovascular care of oncology patients held for the first time in February 2017 and scheduled for a second edition next February.
Publication of the guideline in a cardiology journal “would indeed help dissemination among U.S. cardiologists,” agreed Pamela S. Douglas, MD, professor of medicine at Duke University in Durham, N.C., and another of the several cardiologists who served on the ASCO guideline’s panel.
Further advancing awareness of patients with cardio-oncology issues, what Dr. Moslehi has called “an emerging epidemic,” seems the most fundamental of the goals currently advanced by many active in this field.
One step to grow the subspecialty that he and his associates at Vanderbilt have taken is to start this year a formally recognized fellowship program in cardio-oncology; an initial class of three cardiologists started in the program this summer. The Vanderbilt group also plans to launch a website before the end of 2017 that will include an oncology-drug database that compiles all available information on each agent’s cardiovascular effects. The planned website will aggregate links to all existing cardio-oncology programs.
“We will absolutely see the field grow,” said Dr. Swain. “It has only sprung up in the past 10 or so years. It is now getting recognition, people are being trained in cardio-oncology, and it will grow as a subspecialty. It’s very exciting, and it’s better for patients.”
“A cardiologist with no cancer patients or survivors in their practice is unheard of; many cardiologists just don’t realize that,” Dr. Lenihan said. At least 10%-15% of the U.S. population in their 60s or older has a cancer history, he noted. The common mindset among cardiologists has been that cancer patients and survivors are not among their patients.
“It’s unlikely that a busy cardiology practice has no cancer survivors or active cancer patients,” Dr. Douglas suggested. When this happens, a likely explanations is that the cardiologist simply failed to elicit a completely comprehensive history from the practice’s patient roster. And even a cardiology practice today that includes no cancer patients or survivors will likely see some turning up soon, she predicted, because so many are receiving cardiovascular-toxic therapies and then surviving longer than ever before.
“What oncologists and cardiologists want to do is to optimize oncologic outcomes but with an acceptable adverse event profile. The cardio-oncologist helps push that envelope. The goal is not to eliminate cardiac events at the expense of oncologic outcomes, but to shift the balance to fewer and less severe cardiac events without unduly compromising oncologic outcomes,” explained Dr. Ewer. Cardio-oncology grapples with one of the core challenges of medicine, how to balance the potential risks from treatment against its potential benefits, he observed.
Dr. Neilan has been a consultant to Ariad and Takeda. Dr. Lenihan has been a consultant to Janssen and Roche and has received research funding from Takeda. Dr. Moslehi has been a consultant to Acceleron, Ariad, Bristol-Myers Squibb, Incyte, Pfizer, Takeda/Millennium, Verastem and Vertex. Dr. Ewer, Dr. Fradley, and Dr. Barac had no relevant disclosures. Dr. Swain has been a consultant to Genentech and Roche. Dr. Douglas has been a consultant to CardioDx, Interleukin Genetics, and Omicia, and has an ownership interest in CardioDx.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
Cardio-oncology is expanding, fed by a steadily increasing population of cancer survivors at elevated risk for a range of cardiovascular diseases and complications because of the anticancer treatments they received. Cardio-oncology’s quick growth has also been driven by the rapidly expanding universe of cancer treatments with direct or indirect adverse effects on a diverse range of cardiovascular functions.
During the past year, the field’s rapid evolution has featured the first formal diagnostic and care standards in two iterations: A position paper on the cardiovascular toxicities of cancer treatment from the European Society of Cardiology (ESC), released in August 2016 (Eur Heart J. 2016 Sept 21;37[36]:2766-801); and a guideline for preventing and monitoring cardiac dysfunction in adult cancer survivors, issued last December by the American Society of Clinical Oncology (ASCO) and endorsed by the American Heart Association (J Clin Oncol. 2017 March 10;35[8]:893-913), but notably not endorsed by the American College of Cardiology, despite having an ACC representative on the guideline panel. In 2015, the ACC started a Cardio-Oncology Section, one of 20 special-interest sections it maintains, and by mid-2017 the section had some 500 members.
“I’ve had recent conversations with cardiologists who said ‘I’m not sure what cardio-oncology is,’ ” said Tomas G. Neilan, MD, director of the cardio-oncology program at Massachusetts General Hospital in Boston.
More than just heart failure
A few decades ago, in the primordial days of cardio-oncology, the concept of cardiovascular damage during cancer therapy focused entirely on myocardial damage caused by anthracyclines and chest radiation, a concern that eventually expanded to include trastuzumab (Herceptin) and other agents that target the human epidermal growth factor receptor 2 (HER2). These treatments cause significantly reduced left ventricular ejection fractions and heart failure in a significant minority of treated patients. Patients who receive combined treatment with an anthracycline and trastuzumab are at the highest risk for developing heart failure with reduced ejection fraction, but even among patients treated with this combination, fewer than 5% develop outright heart failure.
While this parochial view of cardio-oncology has recently shifted, it remains true that myocardial damage from a relatively large cumulative anthracycline dose, or from radiation, causes some of the most extreme cases of cardiovascular adverse effects and remains an ongoing problem as these treatments stay front line for selected cancer patients.
But some of the recent burgeoning of cardio-oncology has followed the recognition that many other drugs and drug classes can cause a spectrum of adverse cardiovascular effects.
“There has been a significant focus on heart failure and cardiomyopathy due to anthracyclines and HER2-targeted therapies. I think the field will continue to evolve over the next 5 years to focus on other cardiovascular complications, including arrhythmias and vascular disease,” observed Michael Fradley, MD, director of cardio-oncology at Moffitt Cancer Center in Tampa. “In addition, there will be an increased focus on targeted drugs and immunotherapies,” agents that Dr. Fradley said “have many unique cardiovascular complications. We need additional guidelines regarding the management of a variety of cardiotoxicities as well as long-term monitoring strategies.”
In a review article Dr. Moslehi published toward the end of 2016, he fleshed out the wider scope of adverse cardiovascular effects from cancer therapies, noting that the vascular endothelial growth factor (VEGF) signaling pathway inhibitors, drugs such as bevacizumab (Avastin) and aflibercept (Zaltrap), have been documented to cause hypertension, arterial thromboembolic events, and cardiomyopathy; and that tyrosine kinase inhibitors have been shown to cause vascular events, QT interval prolongation, and cerebral and peripheral vascular events (N Engl J Med. 2016 Oct 13;375[15]:1457-67).
In his own recent review, Dr. Fradley highlighted adverse cardiovascular effects from additional anticancer drug classes, including proteasome inhibitors, which can trigger hypertension and cardiomyopathy; immunomodulators, implicated in causing both venous and arterial thromboembolism; and the immune checkpoint inhibitors, linked with myocarditis, arrhythmias, hypotension, and myocardial ischemia (Eur Heart J. 2016 Sept 21;37[36]:2740-2). A similarly broad spectrum of adverse cardiovascular effects linked with a wide range of anticancer treatments also appeared in the ESC 2016 position paper on cancer treatments.
But while the range of cancer treatments that can have some impact on the cardiovascular system is strikingly large, experts uniformly caution that far from every patient treated for cancer needs an immediate cardiology consult and work-up, especially when the cancers appear in young adults.
“We’re not quite at the point where every cancer patient needs to be seen by a cardiologist or cardio-oncologist,” Dr. Fradley noted in an interview.
“If a patient develops hypertension while on treatment I refer them to a PCP or cardiologist. I don’t treat hypertension myself. But if a patient is ‘normal’ they don’t need a cardiology assessment up front. It’s impossible to refer all patients, especially younger patients, with current resources. There are too many patients who receive cardiotoxic therapies to refer everyone. I involve the cardiologist once there is evidence of damage,”she explained.
Cardio-oncology centers or community practice?
The rise of cardio-oncology, especially over the last decade or so, has given rise to a new academic niche, the cardio-oncology clinic. Starting from almost no programs a few years ago, by 2016 one tally put the total number of U.S. self-designated cardio-oncology centers at about 40 (Heart Fail Clin. 2017 April;13[2]:347-55), and that number undoubtedly grew even more during the year since. While these programs promote and advance the nascent subspecialty of cardio-oncology, and provide a foundation for development of formalized training programs, many experts see a clear hierarchy of risk that distinguishes the patients who should ideally be managed at these focused, multidisciplinary programs from the lower-risk patients who probably do fine under the care of just their oncologist or their oncologist in collaboration with a community cardiologist or primary care physician.
“The cardio-oncology community recognizes that it is nice to have programs at academic centers but it’s more important to deliver this care in the community,” said Dr. Lenihan. “Many cancer patients have no prior history of cardiovascular disease. These low-risk patients don’t necessarily need a cardio-oncologist. They may need to have their blood pressure managed more effectively or receive other preventive care, but that can certainly be done locally. There are low-risk patients who don’t need to go to a major center.” Dr. Lenihan and other cardio-oncologists see the majority of cancer patients as low risk when it comes to cardiovascular complications.
But it’s different when patients receive an anthracycline or an anthracycline plus trastuzumab. “This high-risk population is best seen at a cardio-oncology center.” Dr. Lenihan also included in this high-risk subgroup patients treated with mediastinal radiation, an option often used during the 1980s-2000s.
“Any time a patient receives treatment with the potential to cause a cardiovascular effect, which is pretty much any drug that now comes out, you need an accurate baseline assessment. But that doesn’t mean you need do anything different; you still treat the patient’s cancer. A thorough baseline assessment is a necessity, but it does not need to be done at a cardio-oncology center,” Dr. Lenihan said in an interview.
“For the vast majority of patients, care can be at community hospitals, similar to the delivery of the vast majority of oncology care. Some patients need referral to tertiary cardiology centers for advanced heart failure or to undergo advanced procedures, but that is a very small percentage of patients,” said Ana Barac, MD, director of the cardio-oncology program at the MedStar Heart Institute in Washington, and chair of the ACC’s Cardio-Oncology Section.
“Patients receiving more novel or unusual therapies, and those participating in trials” are appropriate for centers, while community care by a cardiologist and oncologist should suffice for more routine patients, said Dr. Fradley.
“Cardio-oncology centers are good for patients with type I damage from anthracycline treatment, especially patients who already had underlying heart disease,” said Michael S. Ewer, MD, a cardiologist and professor of medicine at MD Anderson Cancer Center in Houston. Specialist centers are also for patients with cardiovascular risk factors: older age, diabetes, preexisting coronary artery disease, and patients who receive cardiotoxic type I therapy (J Clin Oncol. 2005 May;23[13]:2900-2). Also, patients with a significant, immediate cardiac reaction to treatment, and those with an unexpected cardiac reaction, Dr. Ewer said.
A somewhat more expansive view of the typical cardio-oncology patient came from Dr. Neilan, based on the patients he sees at his program in Boston. Dr. Neilan estimated that roughly 60%-70% of his patients first present while they undergo active cancer treatment, with another 20% coming to the program as cancer survivors, and a small percentage of patients showing up for cardiology assessments and treatments without a cancer history. Among those with a cancer history, he guessed that perhaps 10%-20% were treated with an anthracycline, at least 10% received trastuzumab, and about 10% received radiation treatment. “I also see a lot of patients with complications from treatment” with tyrosine kinase inhibitors, VEGF inhibitors, and immunotherapies. “I don’t see a lot of patients for cardiovascular disease assessment before they start cancer therapy,” Dr. Neilan added.
Cardio-oncology heads toward a new cardiology subspecialty
These views of how cardio-oncology is practiced in the real world raise a question about the role of the growing roster of U.S. cardio-oncology programs. If most cancer patients can have their cardiology needs taken care of in the community, how do all the academic programs fit in? The answer seems to be that they model successful oncology and cardiology collaborations, provide a training ground for physicians from both specialties to learn how to collaborate, and serve as the home for research that broadens the field’s evidence base and moves knowledge forward.
“Education and partnerships with oncology teams is the key,” said Dr. Barac. “Our traditional subspecialty training focused on ‘treating cancer’ and ‘treating cardiovascular disease.’ Learning about and seeing effective partnerships during training” is the best model to foster cardiology and oncology partnerships among early-career physicians, she suggested.
“What is the spectrum of knowledge required to be proficient in cardio-oncology, and how do we enhance training at the resident or fellowship level? How do we get [all cardiology] trainees exposed to this knowledge?” wondered Dr. Lenihan, who viewed cardio-oncology programs as a way to meet these needs. “Cardio-oncology is not an established subspecialty. A goal is to establish training requirements and expand training opportunities. And the whole field needs to contribute to clinical research. We need cardio-oncologists to share their experience and improve our level of research.”
ASCO’s cardiac dysfunction practice guideline, first released last December and formally published in March, is likely helping to further entrench cardio-oncology as a new subspecialty. The guideline was “a remarkable step forward,” said Dr. Barac. In addition to establishing a U.S. standard of care for preventing and monitoring cardiac dysfunction in cancer patients, “I use it as a guide for creation of referral pathways with my oncology colleagues, as well as in education of cardiovascular and oncology trainees,” she said in an interview.
Though produced primarily through ASCO’s leadership, the target audience for the guideline seems to be as much cardiologists as it is oncologists. Dissemination of the guideline to cardiologists snagged when it failed to appear in the cardiology literature. That wasn’t the original plan, said guideline participants.
“Before we started, it was agreed that both ASCO and the ACC would publish it. We had a [letter] signed by the president of the ACC saying the ACC would publish it,” recalled Dr. Lenihan, a guideline coauthor. “After all the details were settled, the ACC bailed. They said that they had changed their organizational structure and that they wouldn’t publish the guideline even though they had agreed to.” Not having the guideline appear simultaneously in the cardiology literature “hinders getting the message to the cardiology community,” he said, a sentiment echoed by other cardio-oncologists.
“I served as the ACC representative on the guideline, and the lack of ACC endorsement was the unfortunate consequence of approval and publication timing that coincided with restructuring of the ACC committees,” said Dr. Barac. “It absolutely does not reflect a lack of interest from the ACC.” As an example of the College’s commitment example, she cited an ACC 1.5-day educational course on cardiovascular care of oncology patients held for the first time in February 2017 and scheduled for a second edition next February.
Publication of the guideline in a cardiology journal “would indeed help dissemination among U.S. cardiologists,” agreed Pamela S. Douglas, MD, professor of medicine at Duke University in Durham, N.C., and another of the several cardiologists who served on the ASCO guideline’s panel.
Further advancing awareness of patients with cardio-oncology issues, what Dr. Moslehi has called “an emerging epidemic,” seems the most fundamental of the goals currently advanced by many active in this field.
One step to grow the subspecialty that he and his associates at Vanderbilt have taken is to start this year a formally recognized fellowship program in cardio-oncology; an initial class of three cardiologists started in the program this summer. The Vanderbilt group also plans to launch a website before the end of 2017 that will include an oncology-drug database that compiles all available information on each agent’s cardiovascular effects. The planned website will aggregate links to all existing cardio-oncology programs.
“We will absolutely see the field grow,” said Dr. Swain. “It has only sprung up in the past 10 or so years. It is now getting recognition, people are being trained in cardio-oncology, and it will grow as a subspecialty. It’s very exciting, and it’s better for patients.”
“A cardiologist with no cancer patients or survivors in their practice is unheard of; many cardiologists just don’t realize that,” Dr. Lenihan said. At least 10%-15% of the U.S. population in their 60s or older has a cancer history, he noted. The common mindset among cardiologists has been that cancer patients and survivors are not among their patients.
“It’s unlikely that a busy cardiology practice has no cancer survivors or active cancer patients,” Dr. Douglas suggested. When this happens, a likely explanations is that the cardiologist simply failed to elicit a completely comprehensive history from the practice’s patient roster. And even a cardiology practice today that includes no cancer patients or survivors will likely see some turning up soon, she predicted, because so many are receiving cardiovascular-toxic therapies and then surviving longer than ever before.
“What oncologists and cardiologists want to do is to optimize oncologic outcomes but with an acceptable adverse event profile. The cardio-oncologist helps push that envelope. The goal is not to eliminate cardiac events at the expense of oncologic outcomes, but to shift the balance to fewer and less severe cardiac events without unduly compromising oncologic outcomes,” explained Dr. Ewer. Cardio-oncology grapples with one of the core challenges of medicine, how to balance the potential risks from treatment against its potential benefits, he observed.
Dr. Neilan has been a consultant to Ariad and Takeda. Dr. Lenihan has been a consultant to Janssen and Roche and has received research funding from Takeda. Dr. Moslehi has been a consultant to Acceleron, Ariad, Bristol-Myers Squibb, Incyte, Pfizer, Takeda/Millennium, Verastem and Vertex. Dr. Ewer, Dr. Fradley, and Dr. Barac had no relevant disclosures. Dr. Swain has been a consultant to Genentech and Roche. Dr. Douglas has been a consultant to CardioDx, Interleukin Genetics, and Omicia, and has an ownership interest in CardioDx.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
Cardio-oncology is expanding, fed by a steadily increasing population of cancer survivors at elevated risk for a range of cardiovascular diseases and complications because of the anticancer treatments they received. Cardio-oncology’s quick growth has also been driven by the rapidly expanding universe of cancer treatments with direct or indirect adverse effects on a diverse range of cardiovascular functions.
During the past year, the field’s rapid evolution has featured the first formal diagnostic and care standards in two iterations: A position paper on the cardiovascular toxicities of cancer treatment from the European Society of Cardiology (ESC), released in August 2016 (Eur Heart J. 2016 Sept 21;37[36]:2766-801); and a guideline for preventing and monitoring cardiac dysfunction in adult cancer survivors, issued last December by the American Society of Clinical Oncology (ASCO) and endorsed by the American Heart Association (J Clin Oncol. 2017 March 10;35[8]:893-913), but notably not endorsed by the American College of Cardiology, despite having an ACC representative on the guideline panel. In 2015, the ACC started a Cardio-Oncology Section, one of 20 special-interest sections it maintains, and by mid-2017 the section had some 500 members.
“I’ve had recent conversations with cardiologists who said ‘I’m not sure what cardio-oncology is,’ ” said Tomas G. Neilan, MD, director of the cardio-oncology program at Massachusetts General Hospital in Boston.
More than just heart failure
A few decades ago, in the primordial days of cardio-oncology, the concept of cardiovascular damage during cancer therapy focused entirely on myocardial damage caused by anthracyclines and chest radiation, a concern that eventually expanded to include trastuzumab (Herceptin) and other agents that target the human epidermal growth factor receptor 2 (HER2). These treatments cause significantly reduced left ventricular ejection fractions and heart failure in a significant minority of treated patients. Patients who receive combined treatment with an anthracycline and trastuzumab are at the highest risk for developing heart failure with reduced ejection fraction, but even among patients treated with this combination, fewer than 5% develop outright heart failure.
While this parochial view of cardio-oncology has recently shifted, it remains true that myocardial damage from a relatively large cumulative anthracycline dose, or from radiation, causes some of the most extreme cases of cardiovascular adverse effects and remains an ongoing problem as these treatments stay front line for selected cancer patients.
But some of the recent burgeoning of cardio-oncology has followed the recognition that many other drugs and drug classes can cause a spectrum of adverse cardiovascular effects.
“There has been a significant focus on heart failure and cardiomyopathy due to anthracyclines and HER2-targeted therapies. I think the field will continue to evolve over the next 5 years to focus on other cardiovascular complications, including arrhythmias and vascular disease,” observed Michael Fradley, MD, director of cardio-oncology at Moffitt Cancer Center in Tampa. “In addition, there will be an increased focus on targeted drugs and immunotherapies,” agents that Dr. Fradley said “have many unique cardiovascular complications. We need additional guidelines regarding the management of a variety of cardiotoxicities as well as long-term monitoring strategies.”
In a review article Dr. Moslehi published toward the end of 2016, he fleshed out the wider scope of adverse cardiovascular effects from cancer therapies, noting that the vascular endothelial growth factor (VEGF) signaling pathway inhibitors, drugs such as bevacizumab (Avastin) and aflibercept (Zaltrap), have been documented to cause hypertension, arterial thromboembolic events, and cardiomyopathy; and that tyrosine kinase inhibitors have been shown to cause vascular events, QT interval prolongation, and cerebral and peripheral vascular events (N Engl J Med. 2016 Oct 13;375[15]:1457-67).
In his own recent review, Dr. Fradley highlighted adverse cardiovascular effects from additional anticancer drug classes, including proteasome inhibitors, which can trigger hypertension and cardiomyopathy; immunomodulators, implicated in causing both venous and arterial thromboembolism; and the immune checkpoint inhibitors, linked with myocarditis, arrhythmias, hypotension, and myocardial ischemia (Eur Heart J. 2016 Sept 21;37[36]:2740-2). A similarly broad spectrum of adverse cardiovascular effects linked with a wide range of anticancer treatments also appeared in the ESC 2016 position paper on cancer treatments.
But while the range of cancer treatments that can have some impact on the cardiovascular system is strikingly large, experts uniformly caution that far from every patient treated for cancer needs an immediate cardiology consult and work-up, especially when the cancers appear in young adults.
“We’re not quite at the point where every cancer patient needs to be seen by a cardiologist or cardio-oncologist,” Dr. Fradley noted in an interview.
“If a patient develops hypertension while on treatment I refer them to a PCP or cardiologist. I don’t treat hypertension myself. But if a patient is ‘normal’ they don’t need a cardiology assessment up front. It’s impossible to refer all patients, especially younger patients, with current resources. There are too many patients who receive cardiotoxic therapies to refer everyone. I involve the cardiologist once there is evidence of damage,”she explained.
Cardio-oncology centers or community practice?
The rise of cardio-oncology, especially over the last decade or so, has given rise to a new academic niche, the cardio-oncology clinic. Starting from almost no programs a few years ago, by 2016 one tally put the total number of U.S. self-designated cardio-oncology centers at about 40 (Heart Fail Clin. 2017 April;13[2]:347-55), and that number undoubtedly grew even more during the year since. While these programs promote and advance the nascent subspecialty of cardio-oncology, and provide a foundation for development of formalized training programs, many experts see a clear hierarchy of risk that distinguishes the patients who should ideally be managed at these focused, multidisciplinary programs from the lower-risk patients who probably do fine under the care of just their oncologist or their oncologist in collaboration with a community cardiologist or primary care physician.
“The cardio-oncology community recognizes that it is nice to have programs at academic centers but it’s more important to deliver this care in the community,” said Dr. Lenihan. “Many cancer patients have no prior history of cardiovascular disease. These low-risk patients don’t necessarily need a cardio-oncologist. They may need to have their blood pressure managed more effectively or receive other preventive care, but that can certainly be done locally. There are low-risk patients who don’t need to go to a major center.” Dr. Lenihan and other cardio-oncologists see the majority of cancer patients as low risk when it comes to cardiovascular complications.
But it’s different when patients receive an anthracycline or an anthracycline plus trastuzumab. “This high-risk population is best seen at a cardio-oncology center.” Dr. Lenihan also included in this high-risk subgroup patients treated with mediastinal radiation, an option often used during the 1980s-2000s.
“Any time a patient receives treatment with the potential to cause a cardiovascular effect, which is pretty much any drug that now comes out, you need an accurate baseline assessment. But that doesn’t mean you need do anything different; you still treat the patient’s cancer. A thorough baseline assessment is a necessity, but it does not need to be done at a cardio-oncology center,” Dr. Lenihan said in an interview.
“For the vast majority of patients, care can be at community hospitals, similar to the delivery of the vast majority of oncology care. Some patients need referral to tertiary cardiology centers for advanced heart failure or to undergo advanced procedures, but that is a very small percentage of patients,” said Ana Barac, MD, director of the cardio-oncology program at the MedStar Heart Institute in Washington, and chair of the ACC’s Cardio-Oncology Section.
“Patients receiving more novel or unusual therapies, and those participating in trials” are appropriate for centers, while community care by a cardiologist and oncologist should suffice for more routine patients, said Dr. Fradley.
“Cardio-oncology centers are good for patients with type I damage from anthracycline treatment, especially patients who already had underlying heart disease,” said Michael S. Ewer, MD, a cardiologist and professor of medicine at MD Anderson Cancer Center in Houston. Specialist centers are also for patients with cardiovascular risk factors: older age, diabetes, preexisting coronary artery disease, and patients who receive cardiotoxic type I therapy (J Clin Oncol. 2005 May;23[13]:2900-2). Also, patients with a significant, immediate cardiac reaction to treatment, and those with an unexpected cardiac reaction, Dr. Ewer said.
A somewhat more expansive view of the typical cardio-oncology patient came from Dr. Neilan, based on the patients he sees at his program in Boston. Dr. Neilan estimated that roughly 60%-70% of his patients first present while they undergo active cancer treatment, with another 20% coming to the program as cancer survivors, and a small percentage of patients showing up for cardiology assessments and treatments without a cancer history. Among those with a cancer history, he guessed that perhaps 10%-20% were treated with an anthracycline, at least 10% received trastuzumab, and about 10% received radiation treatment. “I also see a lot of patients with complications from treatment” with tyrosine kinase inhibitors, VEGF inhibitors, and immunotherapies. “I don’t see a lot of patients for cardiovascular disease assessment before they start cancer therapy,” Dr. Neilan added.
Cardio-oncology heads toward a new cardiology subspecialty
These views of how cardio-oncology is practiced in the real world raise a question about the role of the growing roster of U.S. cardio-oncology programs. If most cancer patients can have their cardiology needs taken care of in the community, how do all the academic programs fit in? The answer seems to be that they model successful oncology and cardiology collaborations, provide a training ground for physicians from both specialties to learn how to collaborate, and serve as the home for research that broadens the field’s evidence base and moves knowledge forward.
“Education and partnerships with oncology teams is the key,” said Dr. Barac. “Our traditional subspecialty training focused on ‘treating cancer’ and ‘treating cardiovascular disease.’ Learning about and seeing effective partnerships during training” is the best model to foster cardiology and oncology partnerships among early-career physicians, she suggested.
“What is the spectrum of knowledge required to be proficient in cardio-oncology, and how do we enhance training at the resident or fellowship level? How do we get [all cardiology] trainees exposed to this knowledge?” wondered Dr. Lenihan, who viewed cardio-oncology programs as a way to meet these needs. “Cardio-oncology is not an established subspecialty. A goal is to establish training requirements and expand training opportunities. And the whole field needs to contribute to clinical research. We need cardio-oncologists to share their experience and improve our level of research.”
ASCO’s cardiac dysfunction practice guideline, first released last December and formally published in March, is likely helping to further entrench cardio-oncology as a new subspecialty. The guideline was “a remarkable step forward,” said Dr. Barac. In addition to establishing a U.S. standard of care for preventing and monitoring cardiac dysfunction in cancer patients, “I use it as a guide for creation of referral pathways with my oncology colleagues, as well as in education of cardiovascular and oncology trainees,” she said in an interview.
Though produced primarily through ASCO’s leadership, the target audience for the guideline seems to be as much cardiologists as it is oncologists. Dissemination of the guideline to cardiologists snagged when it failed to appear in the cardiology literature. That wasn’t the original plan, said guideline participants.
“Before we started, it was agreed that both ASCO and the ACC would publish it. We had a [letter] signed by the president of the ACC saying the ACC would publish it,” recalled Dr. Lenihan, a guideline coauthor. “After all the details were settled, the ACC bailed. They said that they had changed their organizational structure and that they wouldn’t publish the guideline even though they had agreed to.” Not having the guideline appear simultaneously in the cardiology literature “hinders getting the message to the cardiology community,” he said, a sentiment echoed by other cardio-oncologists.
“I served as the ACC representative on the guideline, and the lack of ACC endorsement was the unfortunate consequence of approval and publication timing that coincided with restructuring of the ACC committees,” said Dr. Barac. “It absolutely does not reflect a lack of interest from the ACC.” As an example of the College’s commitment example, she cited an ACC 1.5-day educational course on cardiovascular care of oncology patients held for the first time in February 2017 and scheduled for a second edition next February.
Publication of the guideline in a cardiology journal “would indeed help dissemination among U.S. cardiologists,” agreed Pamela S. Douglas, MD, professor of medicine at Duke University in Durham, N.C., and another of the several cardiologists who served on the ASCO guideline’s panel.
Further advancing awareness of patients with cardio-oncology issues, what Dr. Moslehi has called “an emerging epidemic,” seems the most fundamental of the goals currently advanced by many active in this field.
One step to grow the subspecialty that he and his associates at Vanderbilt have taken is to start this year a formally recognized fellowship program in cardio-oncology; an initial class of three cardiologists started in the program this summer. The Vanderbilt group also plans to launch a website before the end of 2017 that will include an oncology-drug database that compiles all available information on each agent’s cardiovascular effects. The planned website will aggregate links to all existing cardio-oncology programs.
“We will absolutely see the field grow,” said Dr. Swain. “It has only sprung up in the past 10 or so years. It is now getting recognition, people are being trained in cardio-oncology, and it will grow as a subspecialty. It’s very exciting, and it’s better for patients.”
“A cardiologist with no cancer patients or survivors in their practice is unheard of; many cardiologists just don’t realize that,” Dr. Lenihan said. At least 10%-15% of the U.S. population in their 60s or older has a cancer history, he noted. The common mindset among cardiologists has been that cancer patients and survivors are not among their patients.
“It’s unlikely that a busy cardiology practice has no cancer survivors or active cancer patients,” Dr. Douglas suggested. When this happens, a likely explanations is that the cardiologist simply failed to elicit a completely comprehensive history from the practice’s patient roster. And even a cardiology practice today that includes no cancer patients or survivors will likely see some turning up soon, she predicted, because so many are receiving cardiovascular-toxic therapies and then surviving longer than ever before.
“What oncologists and cardiologists want to do is to optimize oncologic outcomes but with an acceptable adverse event profile. The cardio-oncologist helps push that envelope. The goal is not to eliminate cardiac events at the expense of oncologic outcomes, but to shift the balance to fewer and less severe cardiac events without unduly compromising oncologic outcomes,” explained Dr. Ewer. Cardio-oncology grapples with one of the core challenges of medicine, how to balance the potential risks from treatment against its potential benefits, he observed.
Dr. Neilan has been a consultant to Ariad and Takeda. Dr. Lenihan has been a consultant to Janssen and Roche and has received research funding from Takeda. Dr. Moslehi has been a consultant to Acceleron, Ariad, Bristol-Myers Squibb, Incyte, Pfizer, Takeda/Millennium, Verastem and Vertex. Dr. Ewer, Dr. Fradley, and Dr. Barac had no relevant disclosures. Dr. Swain has been a consultant to Genentech and Roche. Dr. Douglas has been a consultant to CardioDx, Interleukin Genetics, and Omicia, and has an ownership interest in CardioDx.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
Hyperlipidemia diagnosis protects against breast cancer
BARCELONA – Women diagnosed with hyperlipidemia had a strikingly reduced risk of subsequently developing breast cancer in a big-data, case-control study, Paul R. Carter, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, those baseline hyperlipidemic women who later got breast cancer had a 40% lower risk of all-cause mortality than did matched nonhyperlipidemic controls diagnosed with the malignancy during follow-up, according to Dr. Carter, a cardiology fellow at Cambridge (England) University.
The inference isn’t that hyperlipidemia somehow protects against the most common type of cancer in women. Indeed, preclinical evidence indicates high cholesterol drives several key steps in carcinogenesis. Rather, the strong implication is that the explanation for the observed preventive effect lies in the pleotropic effects of the statin therapy routinely prescribed in accordance with guidelines once women received the diagnosis of hyperlipidemia, he continued.
“The results of this study provide the strongest justification to date for a clinical trial evaluating the protective effect of statins in patients with breast cancer, and this is what we intend to do,” according to Dr. Carter.
He presented a retrospective longitudinal study of the Algorithm for Comorbidities, Associations, Length of Stay and Mortality database, comprising more than 1.2 million patients admitted for various reasons to selected hospitals in northern England during 2000-2014. This big-data study entailed recruitment of 16,043 women aged 40 years and older who were diagnosed with hyperlipidemia during their hospital stay along with an equal number of age-matched women with normal lipid levels. None of the participants had a breast cancer diagnosis at baseline.
The all-cause mortality rate in baseline hyperlipidemic women who later developed breast cancer was 27.4%, significantly lower than the 37.4% rate in normolipidemic women with breast cancer. This translated into an adjusted 40% relative risk reduction.
All-cause mortality occurred during follow-up in 13.7% of breast cancer–free women with baseline hyperlipidemia, compared with 23.6% of nonhyperlipidemic controls without breast cancer.
In an analysis adjusted for age, ethnicity, and the top-10 causes of death in the U.K., women with baseline hyperlipidemia were 40% less likely to die during follow-up than were women without high cholesterol.
Dr. Carter reported having no financial conflicts of interest regarding his study, which was conducted free of commercial support.
BARCELONA – Women diagnosed with hyperlipidemia had a strikingly reduced risk of subsequently developing breast cancer in a big-data, case-control study, Paul R. Carter, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, those baseline hyperlipidemic women who later got breast cancer had a 40% lower risk of all-cause mortality than did matched nonhyperlipidemic controls diagnosed with the malignancy during follow-up, according to Dr. Carter, a cardiology fellow at Cambridge (England) University.
The inference isn’t that hyperlipidemia somehow protects against the most common type of cancer in women. Indeed, preclinical evidence indicates high cholesterol drives several key steps in carcinogenesis. Rather, the strong implication is that the explanation for the observed preventive effect lies in the pleotropic effects of the statin therapy routinely prescribed in accordance with guidelines once women received the diagnosis of hyperlipidemia, he continued.
“The results of this study provide the strongest justification to date for a clinical trial evaluating the protective effect of statins in patients with breast cancer, and this is what we intend to do,” according to Dr. Carter.
He presented a retrospective longitudinal study of the Algorithm for Comorbidities, Associations, Length of Stay and Mortality database, comprising more than 1.2 million patients admitted for various reasons to selected hospitals in northern England during 2000-2014. This big-data study entailed recruitment of 16,043 women aged 40 years and older who were diagnosed with hyperlipidemia during their hospital stay along with an equal number of age-matched women with normal lipid levels. None of the participants had a breast cancer diagnosis at baseline.
The all-cause mortality rate in baseline hyperlipidemic women who later developed breast cancer was 27.4%, significantly lower than the 37.4% rate in normolipidemic women with breast cancer. This translated into an adjusted 40% relative risk reduction.
All-cause mortality occurred during follow-up in 13.7% of breast cancer–free women with baseline hyperlipidemia, compared with 23.6% of nonhyperlipidemic controls without breast cancer.
In an analysis adjusted for age, ethnicity, and the top-10 causes of death in the U.K., women with baseline hyperlipidemia were 40% less likely to die during follow-up than were women without high cholesterol.
Dr. Carter reported having no financial conflicts of interest regarding his study, which was conducted free of commercial support.
BARCELONA – Women diagnosed with hyperlipidemia had a strikingly reduced risk of subsequently developing breast cancer in a big-data, case-control study, Paul R. Carter, MD, reported at the annual congress of the European Society of Cardiology.
Moreover, those baseline hyperlipidemic women who later got breast cancer had a 40% lower risk of all-cause mortality than did matched nonhyperlipidemic controls diagnosed with the malignancy during follow-up, according to Dr. Carter, a cardiology fellow at Cambridge (England) University.
The inference isn’t that hyperlipidemia somehow protects against the most common type of cancer in women. Indeed, preclinical evidence indicates high cholesterol drives several key steps in carcinogenesis. Rather, the strong implication is that the explanation for the observed preventive effect lies in the pleotropic effects of the statin therapy routinely prescribed in accordance with guidelines once women received the diagnosis of hyperlipidemia, he continued.
“The results of this study provide the strongest justification to date for a clinical trial evaluating the protective effect of statins in patients with breast cancer, and this is what we intend to do,” according to Dr. Carter.
He presented a retrospective longitudinal study of the Algorithm for Comorbidities, Associations, Length of Stay and Mortality database, comprising more than 1.2 million patients admitted for various reasons to selected hospitals in northern England during 2000-2014. This big-data study entailed recruitment of 16,043 women aged 40 years and older who were diagnosed with hyperlipidemia during their hospital stay along with an equal number of age-matched women with normal lipid levels. None of the participants had a breast cancer diagnosis at baseline.
The all-cause mortality rate in baseline hyperlipidemic women who later developed breast cancer was 27.4%, significantly lower than the 37.4% rate in normolipidemic women with breast cancer. This translated into an adjusted 40% relative risk reduction.
All-cause mortality occurred during follow-up in 13.7% of breast cancer–free women with baseline hyperlipidemia, compared with 23.6% of nonhyperlipidemic controls without breast cancer.
In an analysis adjusted for age, ethnicity, and the top-10 causes of death in the U.K., women with baseline hyperlipidemia were 40% less likely to die during follow-up than were women without high cholesterol.
Dr. Carter reported having no financial conflicts of interest regarding his study, which was conducted free of commercial support.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: The risk of subsequent development of breast cancer was one-third lower in women diagnosed with hyperlipidemia than in controls with normal lipid levels.
Data source: A retrospective longitudinal case-control study of 16,043 U.K. women aged 40 years or older when diagnosed with hyperlipidemia and an equal number of age-matched women with normal lipids.
Disclosures: The presenter reported having no financial conflicts of interest regarding his study, which was conducted free of commercial support.
HOPE-3 wades into fray regarding optimal blood pressure targets
BARCELONA – How low to go in treating hypertension is a topic of considerable recent controversy. Now the HOPE-3 trial investigators have weighed in, reporting that optimal outcomes in their landmark randomized trial were seen with an achieved, on-treatment systolic blood pressure of 130-140 mm Hg and a diastolic blood pressure of 75-80 mm Hg, Eva M. Lonn, MD, reported at the annual congress of the European Society of Cardiology.
Those results stand in glaring contrast to the findings of the much-discussed SPRINT trial, in which hypertensive patients fared best with an on-treatment SBP driven below 120 mm Hg (N Engl J Med. 2015 Nov 26; 373:2103-16).
“Please note that lower blood pressures, both systolic and diastolic, weren’t associated with lower risk, whereas higher blood pressures considerably increased the risk for major vascular events,” she added.
HOPE-3 (the Third Heart Outcomes Prevention Evaluation) included 12,705 patients in 21 countries who did not have cardiovascular disease and were at intermediate risk, with an average age of 65 years at enrollment and a Framinhgam Risk Score of about 10%. They were randomized double-blind in a 2x2 factorial design to rosuvastatin at 10 mg per day or placebo and/or candesartan at 16 mg plus hydrochlorothiazide at 12.5 mg per day or placebo and prospectively followed for a median of 5.6 years.
The primary outcomes of HOPE-3 have been published (N Engl J Med. 2016 May 26;374[21]:2009-20 and 2021-31). This was a practice-changing trial that opened the door to broader use of statin therapy for primary prevention.
At the ESC congress in Barcelona, Dr. Lonn presented a secondary post-hoc analysis that focused on the impact of antihypertensive therapy in HOPE-3. The results shed new light on the optimal blood pressure levels for triggering initation of antihypertensive therapy, as well as defining the achieved blood pressures that resulted in the greatest reductions in major vascular events.
As this was essentially an all-comers trial of intermediate-risk patients, participants presented with a range of blood pressures at baseline. But more than 4,700 subjects had a baseline SBP of 140-159.9 mm Hg, and 833 had an SBP of 160 mm Hg or more.
The candesartan/hydrochlorothiazide regimen resulted in what Dr. Lonn termed a “moderate” net placebo-subtracted blood pressure reduction of 6/3 mm Hg. The higher the baseline blood pressure, the bigger the reduction.
In the one-third of subjects with a baseline SBP greater than 143.5 mm Hg, antihypertensive therapy resulted in a significant 27% reduction in the composite endpoint of cardiovascular death, MI, or stroke compared with placebo. Those with a baseline SBP of 150 mm Hg or more showed even greater benefit from antihypertensive therapy, with a composite event rate of 4.8% compared with 7.2% for placebo, representing a 34% relative risk reduction in which the event curves began separating at about 2 years.
In contrast, antihypertensive therapy brought no significant reduction in events in patients in the lower two tertiles of baseline SBP. And there was no association at all between baseline DBP and major cardiovascular events across the range of DBP values evaluated in HOPE-3.
But wait: Things get more interesting, according to the cardiac electrophysiologist.
“I find the association between mean in-trial blood pressure as recorded in many measurements and vascular outcomes to be the most interesting analysis. This may be a better look at the association between blood pressure and outcomes than a measurement obtained just once or twice at baseline,” she explained.
Of note, among the 6,356 subjects on candesartan/hydrochlorothiazide, those with a mean on-treatment SBP of 160 mm Hg or more had a 2.61% per year rate of the composite of cardiovascular death, MI, stroke, rescue from cardiac arrest, heart failure, or revascularization. This was more than three-fold higher than the 0.75% per year rate in patients with an on-treatment SBP of 120-139.9 mm Hg. The composite event rate was also significantly higher in those with a mean on-treatment SBP of 140-159.9 mm Hg, at 1.4% per year. The event rate in patients with an on-treatment SBP below 120 mm Hg was identical to that of patients with a value of 120-139.9 mm Hg.
Only among patients with an on-treatment DBP of 90 mm Hg or more was the composite event rate significantly greater than in those with a DBP of 70-79.9 mm Hg, who had the lowest event rate by a margin of 1.89% versus 0.75% per year.
An Australian cardiologist in the audience who has been involved in revamping hypertension treatment guidelines Down Under expressed frustration. He only recently succeeded in wrangling his fellow panelists into incorporating the SPRINT results into the draft guidelines; now HOPE-3 is sending a very different message. What gives? Could the disparate findings simply be due to play of chance? he asked.
Highly unlikely, Dr. Lonn replied.
“There were substantial differences between our trials,” she explained. “First of all, the SPRINT population was at substantially higher risk. They either had to have established cardiovascular disease – we eliminated those people – or significant renal disease – we eliminated those people, too – or age greater than 75, or a Framingham Risk Score above 15%.”
Also, the SPRINT protocol controversially called for unattended blood pressure measurement.
“This is a very pure way ot eliminating white coat hypertension, but it is different from other studies, so it is very difficult to compare SPRINT to older studies or to HOPE-3. Some other investigators have suggested that the difference between attended and unattended blood pressure is close to 10 mm Hg. So our SBP of 130 mm Hg, which had the best outcomes in HOPE-3, may be the same as about 120 mm Hg in SPRINT,” according to Dr. Lonn.
HOPE-3 was funded by the Canadian Institutes of Health Research and AstraZeneca. Dr. Lonn reported serving as a consultant to and receiving research grants from AstraZeneca, Amgen, Bayer, and Novartis.
BARCELONA – How low to go in treating hypertension is a topic of considerable recent controversy. Now the HOPE-3 trial investigators have weighed in, reporting that optimal outcomes in their landmark randomized trial were seen with an achieved, on-treatment systolic blood pressure of 130-140 mm Hg and a diastolic blood pressure of 75-80 mm Hg, Eva M. Lonn, MD, reported at the annual congress of the European Society of Cardiology.
Those results stand in glaring contrast to the findings of the much-discussed SPRINT trial, in which hypertensive patients fared best with an on-treatment SBP driven below 120 mm Hg (N Engl J Med. 2015 Nov 26; 373:2103-16).
“Please note that lower blood pressures, both systolic and diastolic, weren’t associated with lower risk, whereas higher blood pressures considerably increased the risk for major vascular events,” she added.
HOPE-3 (the Third Heart Outcomes Prevention Evaluation) included 12,705 patients in 21 countries who did not have cardiovascular disease and were at intermediate risk, with an average age of 65 years at enrollment and a Framinhgam Risk Score of about 10%. They were randomized double-blind in a 2x2 factorial design to rosuvastatin at 10 mg per day or placebo and/or candesartan at 16 mg plus hydrochlorothiazide at 12.5 mg per day or placebo and prospectively followed for a median of 5.6 years.
The primary outcomes of HOPE-3 have been published (N Engl J Med. 2016 May 26;374[21]:2009-20 and 2021-31). This was a practice-changing trial that opened the door to broader use of statin therapy for primary prevention.
At the ESC congress in Barcelona, Dr. Lonn presented a secondary post-hoc analysis that focused on the impact of antihypertensive therapy in HOPE-3. The results shed new light on the optimal blood pressure levels for triggering initation of antihypertensive therapy, as well as defining the achieved blood pressures that resulted in the greatest reductions in major vascular events.
As this was essentially an all-comers trial of intermediate-risk patients, participants presented with a range of blood pressures at baseline. But more than 4,700 subjects had a baseline SBP of 140-159.9 mm Hg, and 833 had an SBP of 160 mm Hg or more.
The candesartan/hydrochlorothiazide regimen resulted in what Dr. Lonn termed a “moderate” net placebo-subtracted blood pressure reduction of 6/3 mm Hg. The higher the baseline blood pressure, the bigger the reduction.
In the one-third of subjects with a baseline SBP greater than 143.5 mm Hg, antihypertensive therapy resulted in a significant 27% reduction in the composite endpoint of cardiovascular death, MI, or stroke compared with placebo. Those with a baseline SBP of 150 mm Hg or more showed even greater benefit from antihypertensive therapy, with a composite event rate of 4.8% compared with 7.2% for placebo, representing a 34% relative risk reduction in which the event curves began separating at about 2 years.
In contrast, antihypertensive therapy brought no significant reduction in events in patients in the lower two tertiles of baseline SBP. And there was no association at all between baseline DBP and major cardiovascular events across the range of DBP values evaluated in HOPE-3.
But wait: Things get more interesting, according to the cardiac electrophysiologist.
“I find the association between mean in-trial blood pressure as recorded in many measurements and vascular outcomes to be the most interesting analysis. This may be a better look at the association between blood pressure and outcomes than a measurement obtained just once or twice at baseline,” she explained.
Of note, among the 6,356 subjects on candesartan/hydrochlorothiazide, those with a mean on-treatment SBP of 160 mm Hg or more had a 2.61% per year rate of the composite of cardiovascular death, MI, stroke, rescue from cardiac arrest, heart failure, or revascularization. This was more than three-fold higher than the 0.75% per year rate in patients with an on-treatment SBP of 120-139.9 mm Hg. The composite event rate was also significantly higher in those with a mean on-treatment SBP of 140-159.9 mm Hg, at 1.4% per year. The event rate in patients with an on-treatment SBP below 120 mm Hg was identical to that of patients with a value of 120-139.9 mm Hg.
Only among patients with an on-treatment DBP of 90 mm Hg or more was the composite event rate significantly greater than in those with a DBP of 70-79.9 mm Hg, who had the lowest event rate by a margin of 1.89% versus 0.75% per year.
An Australian cardiologist in the audience who has been involved in revamping hypertension treatment guidelines Down Under expressed frustration. He only recently succeeded in wrangling his fellow panelists into incorporating the SPRINT results into the draft guidelines; now HOPE-3 is sending a very different message. What gives? Could the disparate findings simply be due to play of chance? he asked.
Highly unlikely, Dr. Lonn replied.
“There were substantial differences between our trials,” she explained. “First of all, the SPRINT population was at substantially higher risk. They either had to have established cardiovascular disease – we eliminated those people – or significant renal disease – we eliminated those people, too – or age greater than 75, or a Framingham Risk Score above 15%.”
Also, the SPRINT protocol controversially called for unattended blood pressure measurement.
“This is a very pure way ot eliminating white coat hypertension, but it is different from other studies, so it is very difficult to compare SPRINT to older studies or to HOPE-3. Some other investigators have suggested that the difference between attended and unattended blood pressure is close to 10 mm Hg. So our SBP of 130 mm Hg, which had the best outcomes in HOPE-3, may be the same as about 120 mm Hg in SPRINT,” according to Dr. Lonn.
HOPE-3 was funded by the Canadian Institutes of Health Research and AstraZeneca. Dr. Lonn reported serving as a consultant to and receiving research grants from AstraZeneca, Amgen, Bayer, and Novartis.
BARCELONA – How low to go in treating hypertension is a topic of considerable recent controversy. Now the HOPE-3 trial investigators have weighed in, reporting that optimal outcomes in their landmark randomized trial were seen with an achieved, on-treatment systolic blood pressure of 130-140 mm Hg and a diastolic blood pressure of 75-80 mm Hg, Eva M. Lonn, MD, reported at the annual congress of the European Society of Cardiology.
Those results stand in glaring contrast to the findings of the much-discussed SPRINT trial, in which hypertensive patients fared best with an on-treatment SBP driven below 120 mm Hg (N Engl J Med. 2015 Nov 26; 373:2103-16).
“Please note that lower blood pressures, both systolic and diastolic, weren’t associated with lower risk, whereas higher blood pressures considerably increased the risk for major vascular events,” she added.
HOPE-3 (the Third Heart Outcomes Prevention Evaluation) included 12,705 patients in 21 countries who did not have cardiovascular disease and were at intermediate risk, with an average age of 65 years at enrollment and a Framinhgam Risk Score of about 10%. They were randomized double-blind in a 2x2 factorial design to rosuvastatin at 10 mg per day or placebo and/or candesartan at 16 mg plus hydrochlorothiazide at 12.5 mg per day or placebo and prospectively followed for a median of 5.6 years.
The primary outcomes of HOPE-3 have been published (N Engl J Med. 2016 May 26;374[21]:2009-20 and 2021-31). This was a practice-changing trial that opened the door to broader use of statin therapy for primary prevention.
At the ESC congress in Barcelona, Dr. Lonn presented a secondary post-hoc analysis that focused on the impact of antihypertensive therapy in HOPE-3. The results shed new light on the optimal blood pressure levels for triggering initation of antihypertensive therapy, as well as defining the achieved blood pressures that resulted in the greatest reductions in major vascular events.
As this was essentially an all-comers trial of intermediate-risk patients, participants presented with a range of blood pressures at baseline. But more than 4,700 subjects had a baseline SBP of 140-159.9 mm Hg, and 833 had an SBP of 160 mm Hg or more.
The candesartan/hydrochlorothiazide regimen resulted in what Dr. Lonn termed a “moderate” net placebo-subtracted blood pressure reduction of 6/3 mm Hg. The higher the baseline blood pressure, the bigger the reduction.
In the one-third of subjects with a baseline SBP greater than 143.5 mm Hg, antihypertensive therapy resulted in a significant 27% reduction in the composite endpoint of cardiovascular death, MI, or stroke compared with placebo. Those with a baseline SBP of 150 mm Hg or more showed even greater benefit from antihypertensive therapy, with a composite event rate of 4.8% compared with 7.2% for placebo, representing a 34% relative risk reduction in which the event curves began separating at about 2 years.
In contrast, antihypertensive therapy brought no significant reduction in events in patients in the lower two tertiles of baseline SBP. And there was no association at all between baseline DBP and major cardiovascular events across the range of DBP values evaluated in HOPE-3.
But wait: Things get more interesting, according to the cardiac electrophysiologist.
“I find the association between mean in-trial blood pressure as recorded in many measurements and vascular outcomes to be the most interesting analysis. This may be a better look at the association between blood pressure and outcomes than a measurement obtained just once or twice at baseline,” she explained.
Of note, among the 6,356 subjects on candesartan/hydrochlorothiazide, those with a mean on-treatment SBP of 160 mm Hg or more had a 2.61% per year rate of the composite of cardiovascular death, MI, stroke, rescue from cardiac arrest, heart failure, or revascularization. This was more than three-fold higher than the 0.75% per year rate in patients with an on-treatment SBP of 120-139.9 mm Hg. The composite event rate was also significantly higher in those with a mean on-treatment SBP of 140-159.9 mm Hg, at 1.4% per year. The event rate in patients with an on-treatment SBP below 120 mm Hg was identical to that of patients with a value of 120-139.9 mm Hg.
Only among patients with an on-treatment DBP of 90 mm Hg or more was the composite event rate significantly greater than in those with a DBP of 70-79.9 mm Hg, who had the lowest event rate by a margin of 1.89% versus 0.75% per year.
An Australian cardiologist in the audience who has been involved in revamping hypertension treatment guidelines Down Under expressed frustration. He only recently succeeded in wrangling his fellow panelists into incorporating the SPRINT results into the draft guidelines; now HOPE-3 is sending a very different message. What gives? Could the disparate findings simply be due to play of chance? he asked.
Highly unlikely, Dr. Lonn replied.
“There were substantial differences between our trials,” she explained. “First of all, the SPRINT population was at substantially higher risk. They either had to have established cardiovascular disease – we eliminated those people – or significant renal disease – we eliminated those people, too – or age greater than 75, or a Framingham Risk Score above 15%.”
Also, the SPRINT protocol controversially called for unattended blood pressure measurement.
“This is a very pure way ot eliminating white coat hypertension, but it is different from other studies, so it is very difficult to compare SPRINT to older studies or to HOPE-3. Some other investigators have suggested that the difference between attended and unattended blood pressure is close to 10 mm Hg. So our SBP of 130 mm Hg, which had the best outcomes in HOPE-3, may be the same as about 120 mm Hg in SPRINT,” according to Dr. Lonn.
HOPE-3 was funded by the Canadian Institutes of Health Research and AstraZeneca. Dr. Lonn reported serving as a consultant to and receiving research grants from AstraZeneca, Amgen, Bayer, and Novartis.
AT THE ESC CONGRESS 2017
Key clinical point:
Major finding: The on-treatment systolic blood pressure target associated with the greatest reduction in vascular events in the HOPE-3 trial was 130-140 mm Hg.
Data source: The HOPE-3 trial was a randomized, double-blind, placebo-controlled study of 12,705 intermediate-cardiovascular-risk patients in 21 countries who were prospectively followed for a median 5.6 years.
Disclosures: HOPE-3 was funded by the Canadian Institutes of Health Research and AstraZeneca. The presenter reported serving as a consultant to and receiving research grants from AstraZeneca, Amgen, Bayer, and Novartis.















