User login
How does lecanemab work in Alzheimer’s?
Lecanemab (Lequembi, Esai), an amyloid-beta–directed antibody therapy, is approved by the Food and Drug Administration for the treatment of Alzheimer’s disease (AD). But exactly how the drug clears amyloid-beta wasn’t clear.
The investigators tested the effectiveness of various forms of amyloid-beta in activating the plasma contact system and found that amyloid-beta protofibrils, known to be the most toxic form of amyloid-beta, promoted the activation of this molecular cascade and that lecanemab inhibited pathway activation.
“In our study, we looked at lecanemab and found it can block the activation of the contact system, which could be one of the reasons that it works so well for AD,” study coinvestigator Erin Norris, PhD, research associate professor, Rockefeller University, New York, said in an interview.
The study was published online in the Proceedings of the National Academy of Science.
Unknown mechanism
“Many years ago, we started looking at the involvement of vascular dysfunction in AD,” Dr. Norris said. “We wanted to see whether or not irregular blood clotting or problems with blood flow was problematic in Alzheimer’s patients.”
The researchers found that fibrin, a major component involved in blood clotting, can extravasate into the brain.
“The blood-brain barrier can break down in Alzheimer’s, so things from the blood can move into the brain and deposit there,” she added. Fibrin then interacts with amyloid-beta, the major pathogenic protein in AD.
Dr. Norris explained that fibrin clots can form in two different ways. One is through the normal process that occurs when there’s an injury and bleeding. The second is through intrinsic clotting, which takes place through the contact system.
“We started looking into this system and found that the plasma of Alzheimer’s patients showed irregular levels of these enzymes and proteins that are part of the intrinsic clotting system compared to those of normal controls,” said Dr. Norris.
“This paper was an extension of years studying this pathway and these mechanisms. It was also inspired by the approval of lecanemab and its release for use in Alzheimer’s patients,” she added.
In previous research, the same researchers found that amyloid-beta has different forms. “It’s normally soluble, and it’s a very tiny molecule,” Dr. Norris said. “But over time, and in different situations, it can start to aggregate, becoming bigger and bigger.”
Implications beyond Alzheimer’s
Postmortem tissue analysis has found fibrillar plaques that are “clumped together.” These are insoluble and hard to get rid of, she said. “Protofibrils are the step before amyloid-beta forms fibrils and are considered to be the most toxic form, although the mechanism behind why it’s so toxic is not understood.”
Previous research has already shown that amyloid-beta can activate the contact system. The contact system has two “arms,” the first of which is involved with clotting, and the second with inflammation, Dr. Norris said. In fact, it’s the plasma contact system that links vascular and inflammatory pathways.
The plasma contact system leads to the clotting of fibrin, Dr. Norris continued. It activates factor XII, which leads to blood clotting by binding to coagulation factor XI.
The contact system also causes inflammation – the second “arm.” Bradykinin, a potent inflammatory molecule, is released by binding to high-molecular-weight kininogen (HK). In addition to inflammation, bradykinin can cause edema and blood-brain barrier permeability.
Although it’s been known that amyloid-beta can activate the contact system, the particular form of amyloid-beta implicated in this cascade has not been identified. And so, the researchers incubated amyloid-beta42 with human plasma, testing various types of amyloid-beta – monomers, oligomers, protofibrils, and fibrils – to see which would activate the contact system.
Amyloid-beta protofibrils promoted the activation of the contact system, as evidenced by several reactions, including activation of factor XII, while other forms of amyloid-beta did not. HK also “bound tightly” to amyloid-beta protofibrils, with “weaker” binding to other amyloid-beta species, the authors reported, confirming that amyloid-beta protofibrils bind to HK and factor XII.
Bradykinin levels were increased by amyloid-beta protofibrils, which also induced faster clotting, compared with other forms of amyloid-beta.
The researchers introduced lecanemab into the picture and found it “dramatically inhibited” contact system activation induced by amyloid-beta protofibrils. For example, it blocked the binding of factor XII to amyloid-beta. By contrast, human IgG (which the researchers used as a control) had no effect.
Additionally, lecanemab also prevented accelerated intrinsic coagulation in normal human plasma mediated by amyloid-beta protofibril.
Senior author Sidney Strickland, PhD, the Zachary and Elizabeth M. Fisher professor in Alzheimer’s and neurodegenerative disease, Rockefeller University, said in an interview: “One of the strong motivators for conducting this study was the fact that this drug, which is effective in AD, targets this specific form of amyloid-beta; but no one knows why it›s more toxic. We thought we could see if we could tie it to what we›re working on, and we found it ties in beautifully.”
The findings have implications that go beyond AD, Dr. Strickland said. “The contact system is implicated in lots of different pathologies, including sickle cell anemia, sepsis, inflammatory bowel disease, and so on.” Blocking the contact system might be a helpful approach in these conditions too.
Innovative, plausible, but still preliminary
In a comment, Heather M. Snyder, PhD, vice president of medical and scientific relations at the Alzheimer’s Association, called the investigation “innovative,” with ideas that are “certainly plausible.” However, “at this time, the work is preliminary and not conclusive.”
The hypothesized mechanisms for why amyloid (lecanemab’s target) is toxic to the brain “does incorporate important AD-related brain changes that have been observed in other studies, including inflammatory/immune changes and vascular-related changes,” said Dr. Snyder, who was not involved with the current study.
However, “additional studies that look both in model systems and in humans are needed to further illuminate these relationships,” Dr. Snyder said.
The study was supported by grants from the National Institutes of Health as well as the Robertson Therapeutic Development Fund, Samuel Newhouse Foundation, John A. Herrmann, and the May and Samuel Rudin Family Foundation. Dr. Norris, Dr. Strickland, and Dr. Snyder declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lecanemab (Lequembi, Esai), an amyloid-beta–directed antibody therapy, is approved by the Food and Drug Administration for the treatment of Alzheimer’s disease (AD). But exactly how the drug clears amyloid-beta wasn’t clear.
The investigators tested the effectiveness of various forms of amyloid-beta in activating the plasma contact system and found that amyloid-beta protofibrils, known to be the most toxic form of amyloid-beta, promoted the activation of this molecular cascade and that lecanemab inhibited pathway activation.
“In our study, we looked at lecanemab and found it can block the activation of the contact system, which could be one of the reasons that it works so well for AD,” study coinvestigator Erin Norris, PhD, research associate professor, Rockefeller University, New York, said in an interview.
The study was published online in the Proceedings of the National Academy of Science.
Unknown mechanism
“Many years ago, we started looking at the involvement of vascular dysfunction in AD,” Dr. Norris said. “We wanted to see whether or not irregular blood clotting or problems with blood flow was problematic in Alzheimer’s patients.”
The researchers found that fibrin, a major component involved in blood clotting, can extravasate into the brain.
“The blood-brain barrier can break down in Alzheimer’s, so things from the blood can move into the brain and deposit there,” she added. Fibrin then interacts with amyloid-beta, the major pathogenic protein in AD.
Dr. Norris explained that fibrin clots can form in two different ways. One is through the normal process that occurs when there’s an injury and bleeding. The second is through intrinsic clotting, which takes place through the contact system.
“We started looking into this system and found that the plasma of Alzheimer’s patients showed irregular levels of these enzymes and proteins that are part of the intrinsic clotting system compared to those of normal controls,” said Dr. Norris.
“This paper was an extension of years studying this pathway and these mechanisms. It was also inspired by the approval of lecanemab and its release for use in Alzheimer’s patients,” she added.
In previous research, the same researchers found that amyloid-beta has different forms. “It’s normally soluble, and it’s a very tiny molecule,” Dr. Norris said. “But over time, and in different situations, it can start to aggregate, becoming bigger and bigger.”
Implications beyond Alzheimer’s
Postmortem tissue analysis has found fibrillar plaques that are “clumped together.” These are insoluble and hard to get rid of, she said. “Protofibrils are the step before amyloid-beta forms fibrils and are considered to be the most toxic form, although the mechanism behind why it’s so toxic is not understood.”
Previous research has already shown that amyloid-beta can activate the contact system. The contact system has two “arms,” the first of which is involved with clotting, and the second with inflammation, Dr. Norris said. In fact, it’s the plasma contact system that links vascular and inflammatory pathways.
The plasma contact system leads to the clotting of fibrin, Dr. Norris continued. It activates factor XII, which leads to blood clotting by binding to coagulation factor XI.
The contact system also causes inflammation – the second “arm.” Bradykinin, a potent inflammatory molecule, is released by binding to high-molecular-weight kininogen (HK). In addition to inflammation, bradykinin can cause edema and blood-brain barrier permeability.
Although it’s been known that amyloid-beta can activate the contact system, the particular form of amyloid-beta implicated in this cascade has not been identified. And so, the researchers incubated amyloid-beta42 with human plasma, testing various types of amyloid-beta – monomers, oligomers, protofibrils, and fibrils – to see which would activate the contact system.
Amyloid-beta protofibrils promoted the activation of the contact system, as evidenced by several reactions, including activation of factor XII, while other forms of amyloid-beta did not. HK also “bound tightly” to amyloid-beta protofibrils, with “weaker” binding to other amyloid-beta species, the authors reported, confirming that amyloid-beta protofibrils bind to HK and factor XII.
Bradykinin levels were increased by amyloid-beta protofibrils, which also induced faster clotting, compared with other forms of amyloid-beta.
The researchers introduced lecanemab into the picture and found it “dramatically inhibited” contact system activation induced by amyloid-beta protofibrils. For example, it blocked the binding of factor XII to amyloid-beta. By contrast, human IgG (which the researchers used as a control) had no effect.
Additionally, lecanemab also prevented accelerated intrinsic coagulation in normal human plasma mediated by amyloid-beta protofibril.
Senior author Sidney Strickland, PhD, the Zachary and Elizabeth M. Fisher professor in Alzheimer’s and neurodegenerative disease, Rockefeller University, said in an interview: “One of the strong motivators for conducting this study was the fact that this drug, which is effective in AD, targets this specific form of amyloid-beta; but no one knows why it›s more toxic. We thought we could see if we could tie it to what we›re working on, and we found it ties in beautifully.”
The findings have implications that go beyond AD, Dr. Strickland said. “The contact system is implicated in lots of different pathologies, including sickle cell anemia, sepsis, inflammatory bowel disease, and so on.” Blocking the contact system might be a helpful approach in these conditions too.
Innovative, plausible, but still preliminary
In a comment, Heather M. Snyder, PhD, vice president of medical and scientific relations at the Alzheimer’s Association, called the investigation “innovative,” with ideas that are “certainly plausible.” However, “at this time, the work is preliminary and not conclusive.”
The hypothesized mechanisms for why amyloid (lecanemab’s target) is toxic to the brain “does incorporate important AD-related brain changes that have been observed in other studies, including inflammatory/immune changes and vascular-related changes,” said Dr. Snyder, who was not involved with the current study.
However, “additional studies that look both in model systems and in humans are needed to further illuminate these relationships,” Dr. Snyder said.
The study was supported by grants from the National Institutes of Health as well as the Robertson Therapeutic Development Fund, Samuel Newhouse Foundation, John A. Herrmann, and the May and Samuel Rudin Family Foundation. Dr. Norris, Dr. Strickland, and Dr. Snyder declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Lecanemab (Lequembi, Esai), an amyloid-beta–directed antibody therapy, is approved by the Food and Drug Administration for the treatment of Alzheimer’s disease (AD). But exactly how the drug clears amyloid-beta wasn’t clear.
The investigators tested the effectiveness of various forms of amyloid-beta in activating the plasma contact system and found that amyloid-beta protofibrils, known to be the most toxic form of amyloid-beta, promoted the activation of this molecular cascade and that lecanemab inhibited pathway activation.
“In our study, we looked at lecanemab and found it can block the activation of the contact system, which could be one of the reasons that it works so well for AD,” study coinvestigator Erin Norris, PhD, research associate professor, Rockefeller University, New York, said in an interview.
The study was published online in the Proceedings of the National Academy of Science.
Unknown mechanism
“Many years ago, we started looking at the involvement of vascular dysfunction in AD,” Dr. Norris said. “We wanted to see whether or not irregular blood clotting or problems with blood flow was problematic in Alzheimer’s patients.”
The researchers found that fibrin, a major component involved in blood clotting, can extravasate into the brain.
“The blood-brain barrier can break down in Alzheimer’s, so things from the blood can move into the brain and deposit there,” she added. Fibrin then interacts with amyloid-beta, the major pathogenic protein in AD.
Dr. Norris explained that fibrin clots can form in two different ways. One is through the normal process that occurs when there’s an injury and bleeding. The second is through intrinsic clotting, which takes place through the contact system.
“We started looking into this system and found that the plasma of Alzheimer’s patients showed irregular levels of these enzymes and proteins that are part of the intrinsic clotting system compared to those of normal controls,” said Dr. Norris.
“This paper was an extension of years studying this pathway and these mechanisms. It was also inspired by the approval of lecanemab and its release for use in Alzheimer’s patients,” she added.
In previous research, the same researchers found that amyloid-beta has different forms. “It’s normally soluble, and it’s a very tiny molecule,” Dr. Norris said. “But over time, and in different situations, it can start to aggregate, becoming bigger and bigger.”
Implications beyond Alzheimer’s
Postmortem tissue analysis has found fibrillar plaques that are “clumped together.” These are insoluble and hard to get rid of, she said. “Protofibrils are the step before amyloid-beta forms fibrils and are considered to be the most toxic form, although the mechanism behind why it’s so toxic is not understood.”
Previous research has already shown that amyloid-beta can activate the contact system. The contact system has two “arms,” the first of which is involved with clotting, and the second with inflammation, Dr. Norris said. In fact, it’s the plasma contact system that links vascular and inflammatory pathways.
The plasma contact system leads to the clotting of fibrin, Dr. Norris continued. It activates factor XII, which leads to blood clotting by binding to coagulation factor XI.
The contact system also causes inflammation – the second “arm.” Bradykinin, a potent inflammatory molecule, is released by binding to high-molecular-weight kininogen (HK). In addition to inflammation, bradykinin can cause edema and blood-brain barrier permeability.
Although it’s been known that amyloid-beta can activate the contact system, the particular form of amyloid-beta implicated in this cascade has not been identified. And so, the researchers incubated amyloid-beta42 with human plasma, testing various types of amyloid-beta – monomers, oligomers, protofibrils, and fibrils – to see which would activate the contact system.
Amyloid-beta protofibrils promoted the activation of the contact system, as evidenced by several reactions, including activation of factor XII, while other forms of amyloid-beta did not. HK also “bound tightly” to amyloid-beta protofibrils, with “weaker” binding to other amyloid-beta species, the authors reported, confirming that amyloid-beta protofibrils bind to HK and factor XII.
Bradykinin levels were increased by amyloid-beta protofibrils, which also induced faster clotting, compared with other forms of amyloid-beta.
The researchers introduced lecanemab into the picture and found it “dramatically inhibited” contact system activation induced by amyloid-beta protofibrils. For example, it blocked the binding of factor XII to amyloid-beta. By contrast, human IgG (which the researchers used as a control) had no effect.
Additionally, lecanemab also prevented accelerated intrinsic coagulation in normal human plasma mediated by amyloid-beta protofibril.
Senior author Sidney Strickland, PhD, the Zachary and Elizabeth M. Fisher professor in Alzheimer’s and neurodegenerative disease, Rockefeller University, said in an interview: “One of the strong motivators for conducting this study was the fact that this drug, which is effective in AD, targets this specific form of amyloid-beta; but no one knows why it›s more toxic. We thought we could see if we could tie it to what we›re working on, and we found it ties in beautifully.”
The findings have implications that go beyond AD, Dr. Strickland said. “The contact system is implicated in lots of different pathologies, including sickle cell anemia, sepsis, inflammatory bowel disease, and so on.” Blocking the contact system might be a helpful approach in these conditions too.
Innovative, plausible, but still preliminary
In a comment, Heather M. Snyder, PhD, vice president of medical and scientific relations at the Alzheimer’s Association, called the investigation “innovative,” with ideas that are “certainly plausible.” However, “at this time, the work is preliminary and not conclusive.”
The hypothesized mechanisms for why amyloid (lecanemab’s target) is toxic to the brain “does incorporate important AD-related brain changes that have been observed in other studies, including inflammatory/immune changes and vascular-related changes,” said Dr. Snyder, who was not involved with the current study.
However, “additional studies that look both in model systems and in humans are needed to further illuminate these relationships,” Dr. Snyder said.
The study was supported by grants from the National Institutes of Health as well as the Robertson Therapeutic Development Fund, Samuel Newhouse Foundation, John A. Herrmann, and the May and Samuel Rudin Family Foundation. Dr. Norris, Dr. Strickland, and Dr. Snyder declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCE
Sedentary lifestyle tied to increased dementia risk
The study of nearly 50,000 adults in the UK Biobank shows that dementia risk increased 8% with 10 hours of sedentary time and 63% with 12 hours. That’s particularly concerning because Americans spend an average of 9.5 hours a day sitting.
Sleep wasn’t factored into the sedentary time and how someone accumulated the 10 hours – either in one continuous block or broken up throughout the day – was irrelevant.
“Our analysis cannot determine whether there is a causal link, so prescriptive conclusions are not really possible; however. I think it is very reasonable to conclude that sitting less and moving more may help reduce risk of dementia,” lead investigator David Raichlen, PhD, professor of biological sciences and anthropology, University of Southern California, Los Angeles, said in an interview.
The findings were published online in JAMA.
A surprising find?
The study is a retrospective analysis of prospectively collected data from the UK Biobank of 49,841 adults aged 60 years or older who wore an accelerometer on their wrists 24 hours a day for a week. Participants had no history of dementia when they wore the movement monitoring device.
Investigators used machine-based learning to determine sedentary time based on readings from the accelerometers. Sleep was not included as sedentary behavior.
Over a mean follow-up of 6.72 years, 414 participants were diagnosed with dementia.
Investigators found that dementia risk rises by 8% at 10 hours a day (adjusted hazard ratio, 1.08; P < .001) and 63% at 12 hours a day (aHR, 1.63; P < .001), compared with 9.27 hours a day. Those who logged 15 hours of sedentary behavior a day had more than triple the dementia risk (aHR, 3.21; P < .001).
Although previous studies had found that breaking up sedentary periods with short bursts of activity help offset some negative health effects of sitting, that wasn’t the case here. Dementia risk was elevated whether participants were sedentary for 10 uninterrupted hours or multiple sedentary periods that totaled 10 hours over the whole day.
“This was surprising,” Dr. Raichlen said. “We expected to find that patterns of sedentary behavior would play a role in risk of dementia, but once you take into account the daily volume of time spent sedentary, how you get there doesn’t seem to matter as much.”
The study did not examine how participants spent sedentary time, but an earlier study by Dr. Raichlen found that watching TV was associated with a greater risk of dementia in older adults, compared with working on a computer.
More research welcome
Dr. Raichlen noted that the number of dementia cases in the study is low and that the view of sedentary behavior is based on 1 week of accelerometer readings. A longitudinal study is needed to determine if the findings last over a longer time period.
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach for the Alzheimer’s Association, says that earlier studies reported an association between sedentary time and dementia, so these results aren’t “particularly surprising.”
“However, reports that did not find an association have also been published, so additional research on possible associations is welcome,” she said.
It’s also important to note that this observational study doesn’t establish a causal relationship between inactivity and cognitive function, which Dr. Sexton said means the influence of other dementia risk factors that are also exacerbated by sedentary behavior can’t be ruled out.
“Although results remained significant after adjusting for several of these factors, further research is required to better understand the various elements that may influence the observed relationship,” noted Dr. Sexton, who was not part of the study. “Reverse causality – that changes in the brain related to dementia are causing the sedentary behavior – cannot be ruled out.”
The study was funded by the National Institutes of Health, the state of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Dr. Raichlen and Dr. Sexton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study of nearly 50,000 adults in the UK Biobank shows that dementia risk increased 8% with 10 hours of sedentary time and 63% with 12 hours. That’s particularly concerning because Americans spend an average of 9.5 hours a day sitting.
Sleep wasn’t factored into the sedentary time and how someone accumulated the 10 hours – either in one continuous block or broken up throughout the day – was irrelevant.
“Our analysis cannot determine whether there is a causal link, so prescriptive conclusions are not really possible; however. I think it is very reasonable to conclude that sitting less and moving more may help reduce risk of dementia,” lead investigator David Raichlen, PhD, professor of biological sciences and anthropology, University of Southern California, Los Angeles, said in an interview.
The findings were published online in JAMA.
A surprising find?
The study is a retrospective analysis of prospectively collected data from the UK Biobank of 49,841 adults aged 60 years or older who wore an accelerometer on their wrists 24 hours a day for a week. Participants had no history of dementia when they wore the movement monitoring device.
Investigators used machine-based learning to determine sedentary time based on readings from the accelerometers. Sleep was not included as sedentary behavior.
Over a mean follow-up of 6.72 years, 414 participants were diagnosed with dementia.
Investigators found that dementia risk rises by 8% at 10 hours a day (adjusted hazard ratio, 1.08; P < .001) and 63% at 12 hours a day (aHR, 1.63; P < .001), compared with 9.27 hours a day. Those who logged 15 hours of sedentary behavior a day had more than triple the dementia risk (aHR, 3.21; P < .001).
Although previous studies had found that breaking up sedentary periods with short bursts of activity help offset some negative health effects of sitting, that wasn’t the case here. Dementia risk was elevated whether participants were sedentary for 10 uninterrupted hours or multiple sedentary periods that totaled 10 hours over the whole day.
“This was surprising,” Dr. Raichlen said. “We expected to find that patterns of sedentary behavior would play a role in risk of dementia, but once you take into account the daily volume of time spent sedentary, how you get there doesn’t seem to matter as much.”
The study did not examine how participants spent sedentary time, but an earlier study by Dr. Raichlen found that watching TV was associated with a greater risk of dementia in older adults, compared with working on a computer.
More research welcome
Dr. Raichlen noted that the number of dementia cases in the study is low and that the view of sedentary behavior is based on 1 week of accelerometer readings. A longitudinal study is needed to determine if the findings last over a longer time period.
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach for the Alzheimer’s Association, says that earlier studies reported an association between sedentary time and dementia, so these results aren’t “particularly surprising.”
“However, reports that did not find an association have also been published, so additional research on possible associations is welcome,” she said.
It’s also important to note that this observational study doesn’t establish a causal relationship between inactivity and cognitive function, which Dr. Sexton said means the influence of other dementia risk factors that are also exacerbated by sedentary behavior can’t be ruled out.
“Although results remained significant after adjusting for several of these factors, further research is required to better understand the various elements that may influence the observed relationship,” noted Dr. Sexton, who was not part of the study. “Reverse causality – that changes in the brain related to dementia are causing the sedentary behavior – cannot be ruled out.”
The study was funded by the National Institutes of Health, the state of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Dr. Raichlen and Dr. Sexton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The study of nearly 50,000 adults in the UK Biobank shows that dementia risk increased 8% with 10 hours of sedentary time and 63% with 12 hours. That’s particularly concerning because Americans spend an average of 9.5 hours a day sitting.
Sleep wasn’t factored into the sedentary time and how someone accumulated the 10 hours – either in one continuous block or broken up throughout the day – was irrelevant.
“Our analysis cannot determine whether there is a causal link, so prescriptive conclusions are not really possible; however. I think it is very reasonable to conclude that sitting less and moving more may help reduce risk of dementia,” lead investigator David Raichlen, PhD, professor of biological sciences and anthropology, University of Southern California, Los Angeles, said in an interview.
The findings were published online in JAMA.
A surprising find?
The study is a retrospective analysis of prospectively collected data from the UK Biobank of 49,841 adults aged 60 years or older who wore an accelerometer on their wrists 24 hours a day for a week. Participants had no history of dementia when they wore the movement monitoring device.
Investigators used machine-based learning to determine sedentary time based on readings from the accelerometers. Sleep was not included as sedentary behavior.
Over a mean follow-up of 6.72 years, 414 participants were diagnosed with dementia.
Investigators found that dementia risk rises by 8% at 10 hours a day (adjusted hazard ratio, 1.08; P < .001) and 63% at 12 hours a day (aHR, 1.63; P < .001), compared with 9.27 hours a day. Those who logged 15 hours of sedentary behavior a day had more than triple the dementia risk (aHR, 3.21; P < .001).
Although previous studies had found that breaking up sedentary periods with short bursts of activity help offset some negative health effects of sitting, that wasn’t the case here. Dementia risk was elevated whether participants were sedentary for 10 uninterrupted hours or multiple sedentary periods that totaled 10 hours over the whole day.
“This was surprising,” Dr. Raichlen said. “We expected to find that patterns of sedentary behavior would play a role in risk of dementia, but once you take into account the daily volume of time spent sedentary, how you get there doesn’t seem to matter as much.”
The study did not examine how participants spent sedentary time, but an earlier study by Dr. Raichlen found that watching TV was associated with a greater risk of dementia in older adults, compared with working on a computer.
More research welcome
Dr. Raichlen noted that the number of dementia cases in the study is low and that the view of sedentary behavior is based on 1 week of accelerometer readings. A longitudinal study is needed to determine if the findings last over a longer time period.
In a comment, Claire Sexton, DPhil, senior director of scientific programs and outreach for the Alzheimer’s Association, says that earlier studies reported an association between sedentary time and dementia, so these results aren’t “particularly surprising.”
“However, reports that did not find an association have also been published, so additional research on possible associations is welcome,” she said.
It’s also important to note that this observational study doesn’t establish a causal relationship between inactivity and cognitive function, which Dr. Sexton said means the influence of other dementia risk factors that are also exacerbated by sedentary behavior can’t be ruled out.
“Although results remained significant after adjusting for several of these factors, further research is required to better understand the various elements that may influence the observed relationship,” noted Dr. Sexton, who was not part of the study. “Reverse causality – that changes in the brain related to dementia are causing the sedentary behavior – cannot be ruled out.”
The study was funded by the National Institutes of Health, the state of Arizona, the Arizona Department of Health Services, and the McKnight Brain Research Foundation. Dr. Raichlen and Dr. Sexton report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
Abdominal fat linked to lower brain volume in midlife
In a large study of healthy middle-aged adults, greater visceral and subcutaneous abdominal fat on abdominal MRI predicted brain atrophy on imaging, especially in women.
“The study shows that excess fat is bad for the brain and worse in women, including in Alzheimer’s disease risk regions,” lead author Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, Mo., said in an interview.
The study was published online in the journal Aging and Disease
Modifiable risk factor
Multiple studies have suggested a connection between body fat accumulation and increased dementia risk. But few have examined the relationship between types of fat (visceral and subcutaneous) and brain volume.
For the new study, 10,000 healthy adults aged 20-80 years (mean age, 52.9 years; 53% men) underwent a short whole-body MRI protocol. Regression analyses of abdominal fat types and normalized brain volumes were evaluated, controlling for age and sex.
The research team found that higher amounts of both visceral and subcutaneous abdominal fat predicted lower total gray and white matter volume, as well as lower volume in the hippocampus, frontal cortex, and temporal, parietal, and occipital lobes.
“The findings are quite dramatic,” Dr. Raji told this news organization. “Overall, we found that both subcutaneous and visceral fat has similar levels of negative relationships with brain volumes.”
Women had a higher burden of brain atrophy with increased visceral fat than men. However, it’s difficult to place the sex differences in context because of the lack of prior work specifically investigating visceral fat, brain volume loss, and sex differences, the researchers caution.
They also note that while statistically significant relationships were observed between visceral fat levels and gray matter volume changes, their effect sizes were generally small.
“Thus, the statistical significance of this work is influenced by the large sample size and less so by large effect size in any given set of regions,” the investigators write.
Other limitations include the cross-sectional nature of the study, which precludes conclusions about causality. The analysis also did not account for other lifestyle factors such as physical activity, diet, and genetic variables.
The researchers call for further investigation “to better elucidate underlying mechanisms and discover possible interventions targeting abdominal fat reduction as a strategy to maintain brain health.”
‘Helpful addition to the literature’
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, noted that “previous studies have linked obesity with cognitive decline and increased risk of dementia. Rather than using BMI as a proxy for body fat, the current study examined visceral and subcutaneous fat directly using imaging techniques.”
Dr. Sexton, who was not associated with this study, said the finding that increased body fat was associated with reduced brain volumes suggests “a possible mechanism to explain the previously reported associations between obesity and cognition.”
“Though some degree of atrophy and brain shrinkage is common with old age, awareness of this association is important because reduced brain volume may be associated with problems with thinking, memory, and performing everyday tasks, and because rates of obesity continue to rise in the United States, along with obesity-related conditions including heart disease, stroke, type 2 diabetes and certain types of cancer,” she added.
“While a helpful addition to the literature, the study does have important limitations. As an observational study, it cannot establish whether higher levels of body fat directly causes reduced brain volumes,” Dr. Sexton cautioned.
In addition, the study did not take into account important related factors like physical activity and diet, which may influence any relationship between body fat and brain volumes, she noted. “Overall, it is not just one factor that is important to consider when considering risk for cognitive decline and dementia, but multiple factors.
“Obesity and the location of body fat must be considered in combination with one’s total lived experience and habits, including physical activity, education, head injury, sleep, mental health, and the health of your heart/cardiovascular system and other key bodily systems,” Dr. Sexton said.
The Alzheimer’s Association is leading a 2-year clinical trial known as U.S. POINTER to see whether combining physical activity, healthy nutrition, social and intellectual challenges, and improved self-management of medical conditions can protect cognitive function in older adults who are at increased risk for cognitive decline.
This work was supported in part by Providence St. Joseph Health in Seattle; Saint John’s Health Center Foundation; Pacific Neuroscience Institute and Foundation; Will and Cary Singleton; and the McLoughlin family. Dr. Raji is a consultant for Brainreader, Apollo Health, Voxelwise, Neurevolution, Pacific Neuroscience Institute Foundation, and Icometrix. Dr. Sexton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large study of healthy middle-aged adults, greater visceral and subcutaneous abdominal fat on abdominal MRI predicted brain atrophy on imaging, especially in women.
“The study shows that excess fat is bad for the brain and worse in women, including in Alzheimer’s disease risk regions,” lead author Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, Mo., said in an interview.
The study was published online in the journal Aging and Disease
Modifiable risk factor
Multiple studies have suggested a connection between body fat accumulation and increased dementia risk. But few have examined the relationship between types of fat (visceral and subcutaneous) and brain volume.
For the new study, 10,000 healthy adults aged 20-80 years (mean age, 52.9 years; 53% men) underwent a short whole-body MRI protocol. Regression analyses of abdominal fat types and normalized brain volumes were evaluated, controlling for age and sex.
The research team found that higher amounts of both visceral and subcutaneous abdominal fat predicted lower total gray and white matter volume, as well as lower volume in the hippocampus, frontal cortex, and temporal, parietal, and occipital lobes.
“The findings are quite dramatic,” Dr. Raji told this news organization. “Overall, we found that both subcutaneous and visceral fat has similar levels of negative relationships with brain volumes.”
Women had a higher burden of brain atrophy with increased visceral fat than men. However, it’s difficult to place the sex differences in context because of the lack of prior work specifically investigating visceral fat, brain volume loss, and sex differences, the researchers caution.
They also note that while statistically significant relationships were observed between visceral fat levels and gray matter volume changes, their effect sizes were generally small.
“Thus, the statistical significance of this work is influenced by the large sample size and less so by large effect size in any given set of regions,” the investigators write.
Other limitations include the cross-sectional nature of the study, which precludes conclusions about causality. The analysis also did not account for other lifestyle factors such as physical activity, diet, and genetic variables.
The researchers call for further investigation “to better elucidate underlying mechanisms and discover possible interventions targeting abdominal fat reduction as a strategy to maintain brain health.”
‘Helpful addition to the literature’
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, noted that “previous studies have linked obesity with cognitive decline and increased risk of dementia. Rather than using BMI as a proxy for body fat, the current study examined visceral and subcutaneous fat directly using imaging techniques.”
Dr. Sexton, who was not associated with this study, said the finding that increased body fat was associated with reduced brain volumes suggests “a possible mechanism to explain the previously reported associations between obesity and cognition.”
“Though some degree of atrophy and brain shrinkage is common with old age, awareness of this association is important because reduced brain volume may be associated with problems with thinking, memory, and performing everyday tasks, and because rates of obesity continue to rise in the United States, along with obesity-related conditions including heart disease, stroke, type 2 diabetes and certain types of cancer,” she added.
“While a helpful addition to the literature, the study does have important limitations. As an observational study, it cannot establish whether higher levels of body fat directly causes reduced brain volumes,” Dr. Sexton cautioned.
In addition, the study did not take into account important related factors like physical activity and diet, which may influence any relationship between body fat and brain volumes, she noted. “Overall, it is not just one factor that is important to consider when considering risk for cognitive decline and dementia, but multiple factors.
“Obesity and the location of body fat must be considered in combination with one’s total lived experience and habits, including physical activity, education, head injury, sleep, mental health, and the health of your heart/cardiovascular system and other key bodily systems,” Dr. Sexton said.
The Alzheimer’s Association is leading a 2-year clinical trial known as U.S. POINTER to see whether combining physical activity, healthy nutrition, social and intellectual challenges, and improved self-management of medical conditions can protect cognitive function in older adults who are at increased risk for cognitive decline.
This work was supported in part by Providence St. Joseph Health in Seattle; Saint John’s Health Center Foundation; Pacific Neuroscience Institute and Foundation; Will and Cary Singleton; and the McLoughlin family. Dr. Raji is a consultant for Brainreader, Apollo Health, Voxelwise, Neurevolution, Pacific Neuroscience Institute Foundation, and Icometrix. Dr. Sexton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a large study of healthy middle-aged adults, greater visceral and subcutaneous abdominal fat on abdominal MRI predicted brain atrophy on imaging, especially in women.
“The study shows that excess fat is bad for the brain and worse in women, including in Alzheimer’s disease risk regions,” lead author Cyrus Raji, MD, PhD, with the Mallinckrodt Institute of Radiology, Washington University, St. Louis, Mo., said in an interview.
The study was published online in the journal Aging and Disease
Modifiable risk factor
Multiple studies have suggested a connection between body fat accumulation and increased dementia risk. But few have examined the relationship between types of fat (visceral and subcutaneous) and brain volume.
For the new study, 10,000 healthy adults aged 20-80 years (mean age, 52.9 years; 53% men) underwent a short whole-body MRI protocol. Regression analyses of abdominal fat types and normalized brain volumes were evaluated, controlling for age and sex.
The research team found that higher amounts of both visceral and subcutaneous abdominal fat predicted lower total gray and white matter volume, as well as lower volume in the hippocampus, frontal cortex, and temporal, parietal, and occipital lobes.
“The findings are quite dramatic,” Dr. Raji told this news organization. “Overall, we found that both subcutaneous and visceral fat has similar levels of negative relationships with brain volumes.”
Women had a higher burden of brain atrophy with increased visceral fat than men. However, it’s difficult to place the sex differences in context because of the lack of prior work specifically investigating visceral fat, brain volume loss, and sex differences, the researchers caution.
They also note that while statistically significant relationships were observed between visceral fat levels and gray matter volume changes, their effect sizes were generally small.
“Thus, the statistical significance of this work is influenced by the large sample size and less so by large effect size in any given set of regions,” the investigators write.
Other limitations include the cross-sectional nature of the study, which precludes conclusions about causality. The analysis also did not account for other lifestyle factors such as physical activity, diet, and genetic variables.
The researchers call for further investigation “to better elucidate underlying mechanisms and discover possible interventions targeting abdominal fat reduction as a strategy to maintain brain health.”
‘Helpful addition to the literature’
In a comment, Claire Sexton, DPhil, Alzheimer’s Association senior director of scientific programs and outreach, noted that “previous studies have linked obesity with cognitive decline and increased risk of dementia. Rather than using BMI as a proxy for body fat, the current study examined visceral and subcutaneous fat directly using imaging techniques.”
Dr. Sexton, who was not associated with this study, said the finding that increased body fat was associated with reduced brain volumes suggests “a possible mechanism to explain the previously reported associations between obesity and cognition.”
“Though some degree of atrophy and brain shrinkage is common with old age, awareness of this association is important because reduced brain volume may be associated with problems with thinking, memory, and performing everyday tasks, and because rates of obesity continue to rise in the United States, along with obesity-related conditions including heart disease, stroke, type 2 diabetes and certain types of cancer,” she added.
“While a helpful addition to the literature, the study does have important limitations. As an observational study, it cannot establish whether higher levels of body fat directly causes reduced brain volumes,” Dr. Sexton cautioned.
In addition, the study did not take into account important related factors like physical activity and diet, which may influence any relationship between body fat and brain volumes, she noted. “Overall, it is not just one factor that is important to consider when considering risk for cognitive decline and dementia, but multiple factors.
“Obesity and the location of body fat must be considered in combination with one’s total lived experience and habits, including physical activity, education, head injury, sleep, mental health, and the health of your heart/cardiovascular system and other key bodily systems,” Dr. Sexton said.
The Alzheimer’s Association is leading a 2-year clinical trial known as U.S. POINTER to see whether combining physical activity, healthy nutrition, social and intellectual challenges, and improved self-management of medical conditions can protect cognitive function in older adults who are at increased risk for cognitive decline.
This work was supported in part by Providence St. Joseph Health in Seattle; Saint John’s Health Center Foundation; Pacific Neuroscience Institute and Foundation; Will and Cary Singleton; and the McLoughlin family. Dr. Raji is a consultant for Brainreader, Apollo Health, Voxelwise, Neurevolution, Pacific Neuroscience Institute Foundation, and Icometrix. Dr. Sexton reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AGING AND DISEASES
The magic of music
I’m really going to miss Jimmy Buffett.
I’ve liked his music as far back as I can remember, and was lucky enough to see him in person in the mid-90s.
I’ve written about music before, but its affect on us never fails to amaze me. Songs can be background noise conducive to getting things done. They can also be in the foreground, serving as a mental vacation (or accompanying a real one). They can transport you to another place, briefly clearing your head from the daily goings-on around you. Even if it’s just during the drive home, it’s a welcome escape to a virtual beach and tropical drink.
Songs can bring back memories of certain events or people that we link them to. My dad loved anything by Neil Diamond, and nothing brings back thoughts of Dad more than when my iTunes randomly picks “I Am ... I Said.” Or John Williams’ Star Wars theme, taking me back to the summer of 1977 when I sat, spellbound, by this incredible movie whose magic is still going strong two generations later.
It’s amazing how our brain tries to make music out of nothing. Even in silence we have ear worms, the songs stuck in our head for hours to days (recently I’ve had “I Sing the Body Electric” from the 1980 movie Fame playing in there).
My office is over an MRI scanner, so I can always hear the chiller pumps softly running in the background. Sometimes my brain will turn their rhythmic chirping into a song, altering the pace of the song to fit them. The soft clicking of the ceiling fan, in my home office, does the same thing (for some reason my brain usually tries to fit “Yellow Submarine” to that one, no idea why).
Music is a part of that mysterious essence that makes us human. It touches all of us in some way, which varies between people, songs, and artists.
Jimmy Buffet’s music has a vacation vibe. Songs of the Caribbean & Keys, beaches, bars, boats, and tropical drinks. The 4:12 running time of his most well-known song, “Margaritaville,” gives a brief respite from my day when it comes on.
He passes into the beyond, to the sadness of his family, friends, and fans. But, unlike people, music can be immortal, and so he lives on through his creations. Like, Bach, Lennon, Bowie, Joplin, Sousa, and too many others to count, his work – and the enjoyment we get from it – are a gift left behind for the future.
Tight lines, Jimmy.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m really going to miss Jimmy Buffett.
I’ve liked his music as far back as I can remember, and was lucky enough to see him in person in the mid-90s.
I’ve written about music before, but its affect on us never fails to amaze me. Songs can be background noise conducive to getting things done. They can also be in the foreground, serving as a mental vacation (or accompanying a real one). They can transport you to another place, briefly clearing your head from the daily goings-on around you. Even if it’s just during the drive home, it’s a welcome escape to a virtual beach and tropical drink.
Songs can bring back memories of certain events or people that we link them to. My dad loved anything by Neil Diamond, and nothing brings back thoughts of Dad more than when my iTunes randomly picks “I Am ... I Said.” Or John Williams’ Star Wars theme, taking me back to the summer of 1977 when I sat, spellbound, by this incredible movie whose magic is still going strong two generations later.
It’s amazing how our brain tries to make music out of nothing. Even in silence we have ear worms, the songs stuck in our head for hours to days (recently I’ve had “I Sing the Body Electric” from the 1980 movie Fame playing in there).
My office is over an MRI scanner, so I can always hear the chiller pumps softly running in the background. Sometimes my brain will turn their rhythmic chirping into a song, altering the pace of the song to fit them. The soft clicking of the ceiling fan, in my home office, does the same thing (for some reason my brain usually tries to fit “Yellow Submarine” to that one, no idea why).
Music is a part of that mysterious essence that makes us human. It touches all of us in some way, which varies between people, songs, and artists.
Jimmy Buffet’s music has a vacation vibe. Songs of the Caribbean & Keys, beaches, bars, boats, and tropical drinks. The 4:12 running time of his most well-known song, “Margaritaville,” gives a brief respite from my day when it comes on.
He passes into the beyond, to the sadness of his family, friends, and fans. But, unlike people, music can be immortal, and so he lives on through his creations. Like, Bach, Lennon, Bowie, Joplin, Sousa, and too many others to count, his work – and the enjoyment we get from it – are a gift left behind for the future.
Tight lines, Jimmy.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I’m really going to miss Jimmy Buffett.
I’ve liked his music as far back as I can remember, and was lucky enough to see him in person in the mid-90s.
I’ve written about music before, but its affect on us never fails to amaze me. Songs can be background noise conducive to getting things done. They can also be in the foreground, serving as a mental vacation (or accompanying a real one). They can transport you to another place, briefly clearing your head from the daily goings-on around you. Even if it’s just during the drive home, it’s a welcome escape to a virtual beach and tropical drink.
Songs can bring back memories of certain events or people that we link them to. My dad loved anything by Neil Diamond, and nothing brings back thoughts of Dad more than when my iTunes randomly picks “I Am ... I Said.” Or John Williams’ Star Wars theme, taking me back to the summer of 1977 when I sat, spellbound, by this incredible movie whose magic is still going strong two generations later.
It’s amazing how our brain tries to make music out of nothing. Even in silence we have ear worms, the songs stuck in our head for hours to days (recently I’ve had “I Sing the Body Electric” from the 1980 movie Fame playing in there).
My office is over an MRI scanner, so I can always hear the chiller pumps softly running in the background. Sometimes my brain will turn their rhythmic chirping into a song, altering the pace of the song to fit them. The soft clicking of the ceiling fan, in my home office, does the same thing (for some reason my brain usually tries to fit “Yellow Submarine” to that one, no idea why).
Music is a part of that mysterious essence that makes us human. It touches all of us in some way, which varies between people, songs, and artists.
Jimmy Buffet’s music has a vacation vibe. Songs of the Caribbean & Keys, beaches, bars, boats, and tropical drinks. The 4:12 running time of his most well-known song, “Margaritaville,” gives a brief respite from my day when it comes on.
He passes into the beyond, to the sadness of his family, friends, and fans. But, unlike people, music can be immortal, and so he lives on through his creations. Like, Bach, Lennon, Bowie, Joplin, Sousa, and too many others to count, his work – and the enjoyment we get from it – are a gift left behind for the future.
Tight lines, Jimmy.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Abnormal sexual behaviors in frontotemporal dementia
Mr. S, age 77, is admitted to a long-term care facility due to progressive cognitive impairment and sexually inappropriate behavior. He has a history of sexual assault of medical staff. His medical history includes significant frontotemporal dementia (FTD) with behavioral disturbances, abnormal sexual behaviors, subclinical hypothyroidism, schizoid personality disorder, Parkinson disease, posttraumatic stress disorder, and hyperammonemia.
Upon admission, Mr. S’s vital signs are within normal limits except for an elevated thyroid-stimulating hormone (4.54 mIU/L; reference range 0.40 to 4.50 mIU/L). Prior cognitive testing results and updated ammonia levels are unavailable. Mr. S’s current medications include acetaminophen 650 mg every 4 hours as needed for pain, calcium carbonate/vitamin D twice daily for bone health, carbidopa/levodopa 25/100 mg twice daily for Parkinson disease, melatonin 3 mg/d at bedtime for insomnia, quetiapine 25 mg twice daily for psychosis with disturbance of behavior and 12.5 mg every 4 hours as needed for agitation, and trazodone 50 mg/d at bedtime for insomnia. Before Mr. S was admitted, previous therapy with selective serotonin reuptake inhibitors (SSRIs) had been tapered and discontinued. Mr. S had also started antipsychotic therapy at another facility due to worsening behaviors.
In patients with dementia, the brain is experiencing neurodegeneration. Progressively, neurons may stop functioning, lose connections with other neurons, and ultimately face cell death. The specific dementia diagnosis and its clinical features depend on the type of neurons and region of the brain affected.1,2
FTD occurs in response to damage to the frontal and temporal lobes. The frontal lobe correlates to executive functioning, while the temporal lobe plays a role in speech and comprehension. Damage to these areas may result in loss of movement, trouble speaking, difficulty solving complex problems, and problems with social behavior. Specifically, damage to the orbital frontal cortex may cause disinhibition and abnormal behaviors, including emotional lability, vulgarity, and indifference to social nuances.1 Within an FTD diagnosis, there are 3 disorders: behavioral-variant FTD (bvFTD), semantic dementia, and progressive nonfluent aphasia.1 Specifically, bvFTD can result in abnormal sexual behaviors such as making sexually inappropriate statements, masturbating in public, undressing in public, inappropriately or aggressively touching others, or confusing another individual as an intimate partner. In addition to cognitive impairment, these neurobehavioral symptoms can significantly impact an individual’s quality of life while increasing caregiver burden.2
Occurring at a similar frequency to Alzheimer’s disease in patients age <65, FTD is one of the more common causes of early-onset dementia. The mean age of onset is 58 and onset after age 75 is particularly unusual. Memory may not be affected early in the course of the disease, but social changes are likely. As FTD progresses, symptoms will resemble those of Alzheimer’s disease and patients will require assistance with activities of daily living. In later stages of FTD, patients will exhibit language and behavior symptoms. Due to its unique progression, FTD can be commonly misdiagnosed as other mental illnesses or neurocognitive disorders.1
Approaches to treatment: What to consider
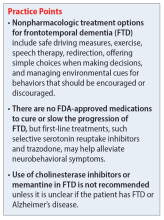
Both nonpharmacologic and pharmacologic interventions are appropriate for addressing FTD. Because nonpharmacologic options improve patient safety and overall physical health, they should be used whenever practical. These interventions include safe driving measures, exercise, speech therapy, redirection, offering simple choices when making decisions, and managing environmental cues for behaviors that should be encouraged or discouraged.3
There are no FDA-approved medications to cure or slow the progression of FTD. Therefore, treatment is focused on alleviating neurobehavioral symptoms. The symptoms depend on the type of FTD the patient has; they include cognitive impairment, anxiety, insomnia or sleep disturbances, compulsive behaviors, speech and language problems, and agitation. While many medications have been commonly used for symptomatic relief, evidence for the efficacy of these treatments in FTD is limited.2
Continue to: A review of the literature...
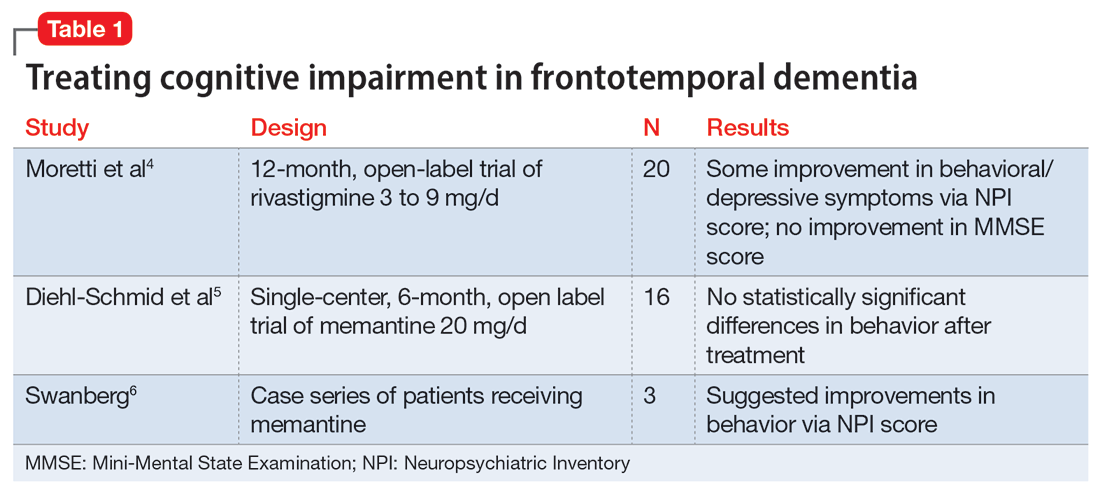
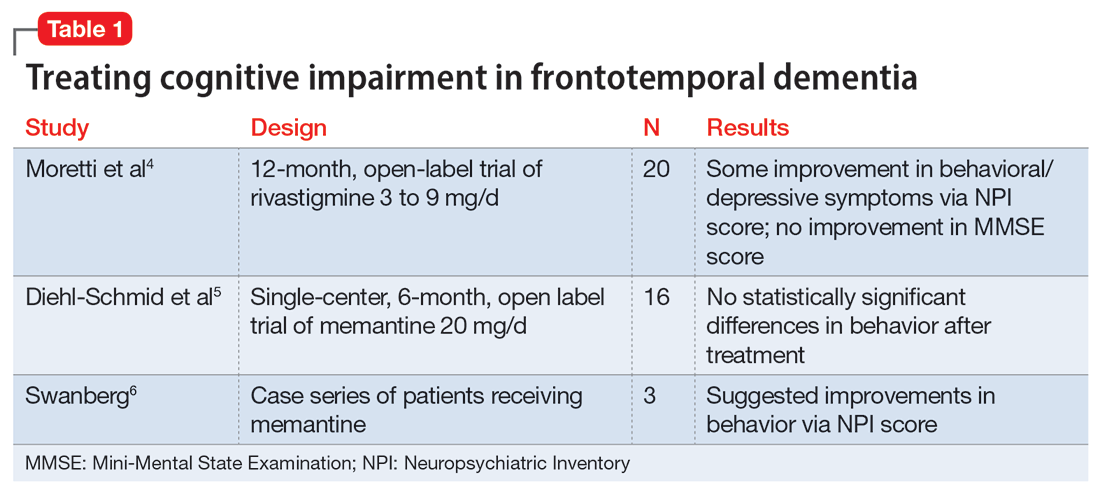
A review of the literature on potential treatments for cognitive impairment and behavioral symptoms of FTD identified 2 trials and 1 case series (Table 14-6) in addition to a 2014 review article7 of current pharmacologic treatments. These trials evaluated cognitive improvement with rivastigmine, memantine, galantamine, and donepezil. None of the trials found a significant benefit from any of these medications for cognitive improvement in FTD. Data were conflicting on whether these medications improved or worsened behavioral symptoms. For example, the case series of 3 patients by Swanberg6 suggested improvement in behavior with memantine, while an open-label study analyzed in a 2014 review article7 found that donepezil may have worsened behaviors. Use of cholinesterase inhibitors or memantine in FTD is not recommended unless it is not certain if the patient has FTD or Alzheimer’s disease.7
Addressing sexual behaviors. Creating a treatment regimen for FTD behavioral symptoms—specifically for abnormal sexual behaviors—can be challenging. Before starting pharmacotherapy directed at behavioral symptoms secondary to FTD, other causes of symptoms such as delirium, pain, or discomfort should be excluded. Nonpharmacologic approaches should be aimed at the type of sexual behavior and likely underlying environmental cause. For example, patients may inappropriately disrobe themselves. To address this behavior, hospital staff or caregivers should first eliminate environmental causes by ensuring the room is at a comfortable temperature, dressing the patient in light, breathable clothing, or checking if the patient needs to use the bathroom. If no environmental causes are found, a one-piece jumpsuit with closures on the back of the garment could be utilized to increase the difficulty of undressing.
Other nonpharmacologic methods include providing private areas for patients who are behaving inappropriately or removing potentially stimulating television or media from the environment. Another option is to increase the use of positive, pleasant stimuli. One approach that has shown benefit is music therapy, utilizing popular music genres from the patient’s youth.3
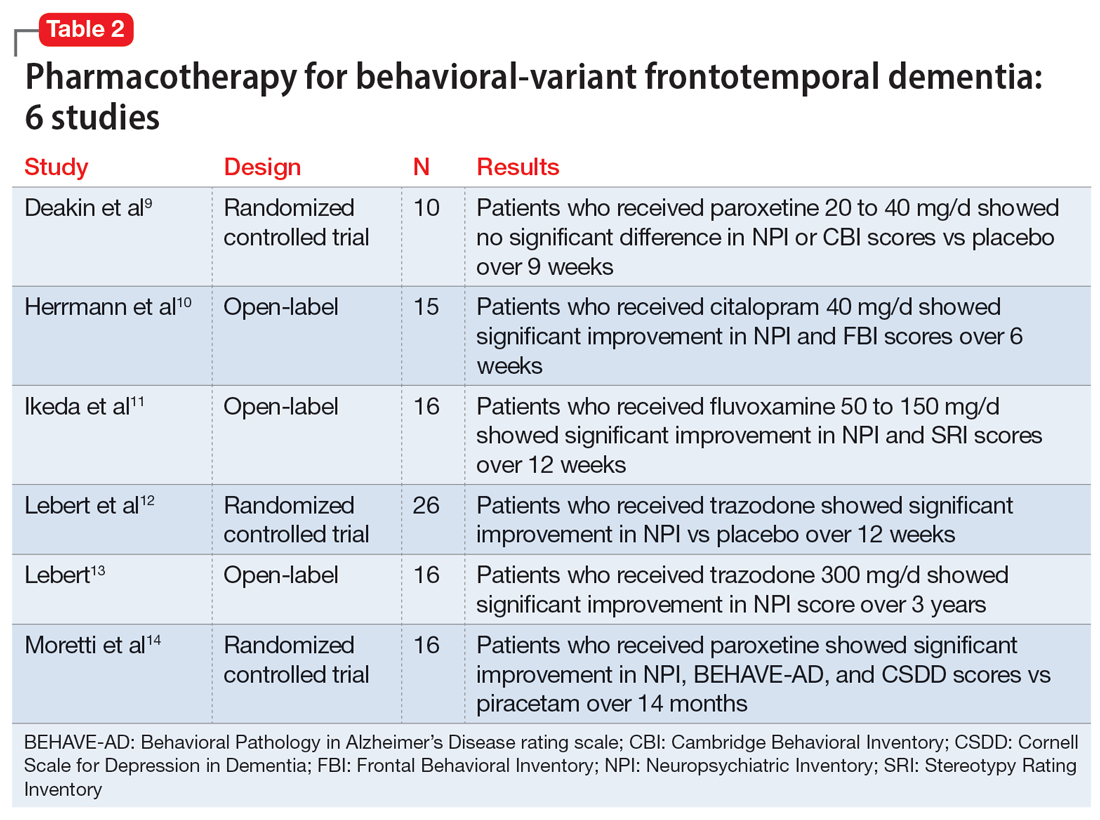
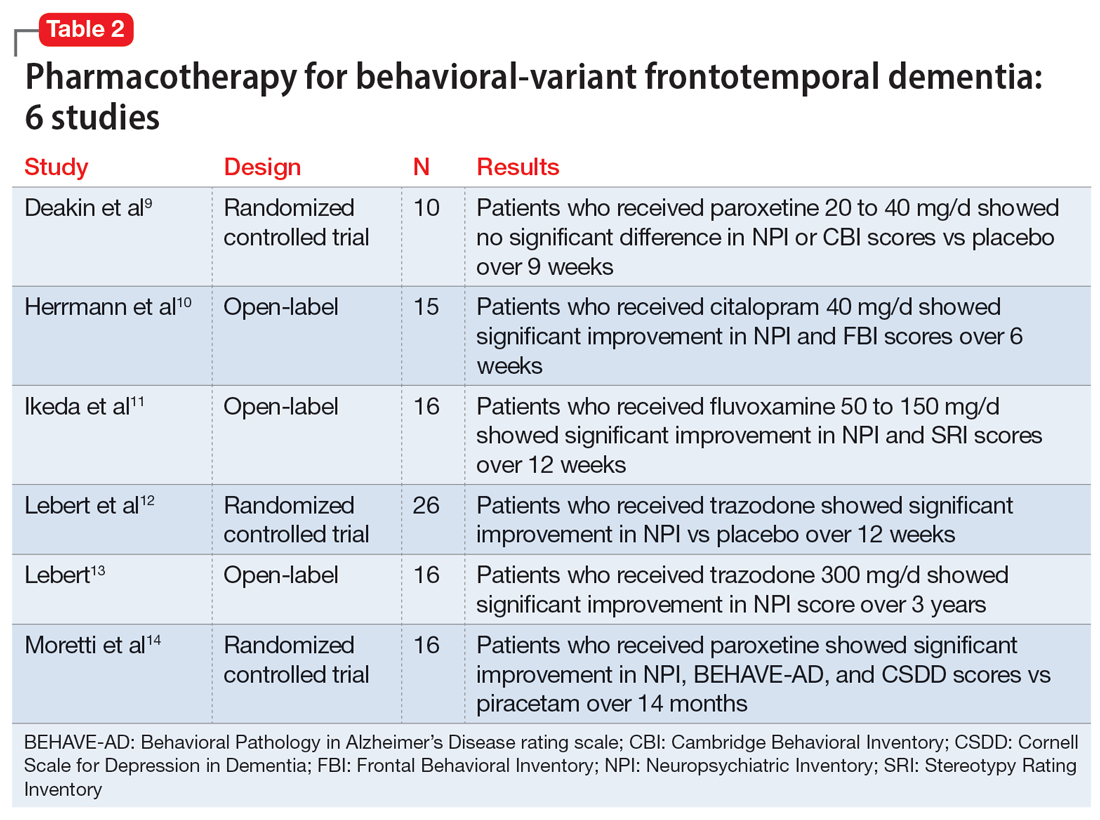
Evidence for pharmacotherapy is limited and largely from case reports and case series. A 2020 meta-analysis by Trieu et al8 reviewed 23 studies to expand on current clinical guidance for patients with bvFTD. These studies showed improvements in behavioral symptoms and reductions in caregiver fatigue with citalopram, trazodone, paroxetine, and fluvoxamine. Six of the trials included in this meta-analysis that evaluated these 4 medications are summarized in Table 2.9-14
Due to the lower risk of adverse effects and favorable safety profiles, SSRIs and trazodone are considered first-line treatment options. Benefit from these medications is theorized to be a result of their serotonergic effects, because serotonin abnormalities and dysfunction have been linked to FTD symptoms. For example, in a patient experiencing hypersexuality, the common adverse effect of low libido associated with SSRIs can be particularly beneficial.8
Continue to: Other medication classes studied in patients...
Other medication classes studied in patients with FTD include antipsychotics, stimulants, anticonvulsants, benzodiazepines, and hormonal therapies. In addition to a black box warning for increased mortality in older patients with dementia-related psychosis, antipsychotics are associated with other serious adverse effects and should be used with caution.7
FTD is a debilitating disease that has a major impact on quality of life, particularly when behavioral symptoms accompany cognitive decline. Though some therapies may possibly improve behavioral symptoms, their routine use remains controversial due to a lack of clear evidence of benefit. In caring for patients with FTD and behavioral symptoms, a multimodal, team-based approach is vital.1
CASE CONTINUED
The treatment team starts Mr. S on several of the modalities discussed in this article over the span of 2 years, with limited efficacy. Nonpharmacologic methods do not provide much benefit because Mr. S is extremely difficult to redirect. Given Mr. S’s past trials of SSRIs prior to admission, sertraline was retrialed and titrated over 2 years. The highest dose utilized during his admission was 200 mg/d. The team starts estrogen therapy but tapers and discontinues it due to ineffectiveness. Mr. S’s use of carbidopa/levodopa is thought to be contributing to his behavioral abnormalities, so the team tapers it to discontinuation; however, Mr. S’s sexually inappropriate behaviors and agitation continue. The team initiates a plan to reduce the dose of quetiapine and switch to gabapentin, but Mr. S fails gradual dose reduction due to his worsening behaviors. He starts gabapentin. The team gradually increases the dose of gabapentin to decrease libido and agitation, respectively. The increase in sertraline dose and use of nonpharmacologic modalities causes Mr. S’s use of as-needed antipsychotics to decrease.
Related Resources
- Ellison JM. What are the stages of frontotemporal dementia? BrightFocus Foundation. July 5, 2021. Accessed July 7, 2023. https://www.brightfocus.org/alzheimers/article/what-are-stages-frontotemporal-dementia
- Dementia and sexually inappropriate behavior. ReaDementia. January 31, 2022. Accessed July 7, 2023. https://readementia.com/dementia-and-sexually-inappropriate-behavior/
Drug Brand Names
Carbidopa/levodopa • Sinemet
Citalopram • Celexa
Donepezil • Aricept
Fluvoxamine • Luvox
Gabapentin • Neurontin
Galantamine • Razadyne
Memantine • Namenda
Paroxetine • Paxil
Quetiapine • Seroquel
Rivastigmine • Exelon
Sertraline • Zoloft
Trazodone • Desyrel
1. Grossman M. Frontotemporal dementia: a review. J Int Neuropsychol Soc. 2002;8(4):566-583. doi:10.1017/s1355617702814357
2. The Johns Hopkins University. Frontotemporal dementia. Johns Hopkins Medicine. Accessed September 12, 2021. https://www.hopkinsmedicine.org/health/conditions-and-diseases/dementia/frontotemporal-dementia
3. Shinagawa S, Nakajima S, Plitman E, et al. Non-pharmacological management for patients with frontotemporal dementia: a systematic review. J Alzheimers Dis. 2015;45(1):283-293. doi:10.3233/JAD-142109
4. Moretti R, Torre P, Antonello RM, et al. Rivastigmine in frontotemporal dementia: an open-label study. Drugs Aging. 2004;21(14):931-937. doi:10.2165/00002512-200421140-00003
5. Diehl-Schmid J, Förstl H, Perneczky R, et al. A 6-month, open-label study for memantine in patients with frontotemporal dementia. In J Geriatr Psychiatry. 2008;23(7):754-759. doi:10.1002/gps.1973
6. Swanberg MM. Memantine for behavioral disturbances in frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2007;21(2):164-166. doi:10.1097/WAD.0b013e318047df5d
7. Tsai RM, Boxer AL. Treatment of frontotemporal dementia. Curr Treat Options Neurol. 2014;16(11):319. doi:10.1007/s11940-014-0319-0
8. Trieu C, Gossink F, Stek ML, et al. Effectiveness of pharmacological interventions for symptoms of behavioral variant frontotemporal dementia: a systematic review. Cogn Behav Neurol. 2020;33(1):1-15. doi:10.1097/WNN.0000000000000217
9. Deakin JB, Rahman S, Nestor PJ, et al. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology (Berl). 2004;172(4):400-408. doi:10.1007/s00213-003-1686-5
10. Herrmann N, Black SE, Chow T, et al. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry. 2012;20(9):789-797. doi:10.1097/JGP.0b013e31823033f3
11. Ikeda M, Shigenobu K, Fukuhara R, et al. Efficacy of fluvoxamine as a treatment for behavioral symptoms in frontotemporal lobar degeneration patients. Dement Geriatr Cogn Disord. 2004;17(3):117-121. doi:10.1159/000076343
12. Lebert F, Stekke W, Hasenbroekx C, et al. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17(4):355-359. doi:10.1159/000077171
13. Lebert F. Behavioral benefits of trazodone are sustained for the long term in frontotemporal dementia. Therapy. 2006;3(1):93-96. doi:10.1586/14750708.3.1.93
14. Moretti R, Torre P, Antonello RM, et al. Frontotemporal dementia: paroxetine as a possible treatment of behavior symptoms. A randomized, controlled, open 14-month study. Eur Neurol. 2003;49(1):13-19. doi:10.1159/000067021
Mr. S, age 77, is admitted to a long-term care facility due to progressive cognitive impairment and sexually inappropriate behavior. He has a history of sexual assault of medical staff. His medical history includes significant frontotemporal dementia (FTD) with behavioral disturbances, abnormal sexual behaviors, subclinical hypothyroidism, schizoid personality disorder, Parkinson disease, posttraumatic stress disorder, and hyperammonemia.
Upon admission, Mr. S’s vital signs are within normal limits except for an elevated thyroid-stimulating hormone (4.54 mIU/L; reference range 0.40 to 4.50 mIU/L). Prior cognitive testing results and updated ammonia levels are unavailable. Mr. S’s current medications include acetaminophen 650 mg every 4 hours as needed for pain, calcium carbonate/vitamin D twice daily for bone health, carbidopa/levodopa 25/100 mg twice daily for Parkinson disease, melatonin 3 mg/d at bedtime for insomnia, quetiapine 25 mg twice daily for psychosis with disturbance of behavior and 12.5 mg every 4 hours as needed for agitation, and trazodone 50 mg/d at bedtime for insomnia. Before Mr. S was admitted, previous therapy with selective serotonin reuptake inhibitors (SSRIs) had been tapered and discontinued. Mr. S had also started antipsychotic therapy at another facility due to worsening behaviors.
In patients with dementia, the brain is experiencing neurodegeneration. Progressively, neurons may stop functioning, lose connections with other neurons, and ultimately face cell death. The specific dementia diagnosis and its clinical features depend on the type of neurons and region of the brain affected.1,2
FTD occurs in response to damage to the frontal and temporal lobes. The frontal lobe correlates to executive functioning, while the temporal lobe plays a role in speech and comprehension. Damage to these areas may result in loss of movement, trouble speaking, difficulty solving complex problems, and problems with social behavior. Specifically, damage to the orbital frontal cortex may cause disinhibition and abnormal behaviors, including emotional lability, vulgarity, and indifference to social nuances.1 Within an FTD diagnosis, there are 3 disorders: behavioral-variant FTD (bvFTD), semantic dementia, and progressive nonfluent aphasia.1 Specifically, bvFTD can result in abnormal sexual behaviors such as making sexually inappropriate statements, masturbating in public, undressing in public, inappropriately or aggressively touching others, or confusing another individual as an intimate partner. In addition to cognitive impairment, these neurobehavioral symptoms can significantly impact an individual’s quality of life while increasing caregiver burden.2
Occurring at a similar frequency to Alzheimer’s disease in patients age <65, FTD is one of the more common causes of early-onset dementia. The mean age of onset is 58 and onset after age 75 is particularly unusual. Memory may not be affected early in the course of the disease, but social changes are likely. As FTD progresses, symptoms will resemble those of Alzheimer’s disease and patients will require assistance with activities of daily living. In later stages of FTD, patients will exhibit language and behavior symptoms. Due to its unique progression, FTD can be commonly misdiagnosed as other mental illnesses or neurocognitive disorders.1
Approaches to treatment: What to consider
Both nonpharmacologic and pharmacologic interventions are appropriate for addressing FTD. Because nonpharmacologic options improve patient safety and overall physical health, they should be used whenever practical. These interventions include safe driving measures, exercise, speech therapy, redirection, offering simple choices when making decisions, and managing environmental cues for behaviors that should be encouraged or discouraged.3
There are no FDA-approved medications to cure or slow the progression of FTD. Therefore, treatment is focused on alleviating neurobehavioral symptoms. The symptoms depend on the type of FTD the patient has; they include cognitive impairment, anxiety, insomnia or sleep disturbances, compulsive behaviors, speech and language problems, and agitation. While many medications have been commonly used for symptomatic relief, evidence for the efficacy of these treatments in FTD is limited.2
Continue to: A review of the literature...
A review of the literature on potential treatments for cognitive impairment and behavioral symptoms of FTD identified 2 trials and 1 case series (Table 14-6) in addition to a 2014 review article7 of current pharmacologic treatments. These trials evaluated cognitive improvement with rivastigmine, memantine, galantamine, and donepezil. None of the trials found a significant benefit from any of these medications for cognitive improvement in FTD. Data were conflicting on whether these medications improved or worsened behavioral symptoms. For example, the case series of 3 patients by Swanberg6 suggested improvement in behavior with memantine, while an open-label study analyzed in a 2014 review article7 found that donepezil may have worsened behaviors. Use of cholinesterase inhibitors or memantine in FTD is not recommended unless it is not certain if the patient has FTD or Alzheimer’s disease.7
Addressing sexual behaviors. Creating a treatment regimen for FTD behavioral symptoms—specifically for abnormal sexual behaviors—can be challenging. Before starting pharmacotherapy directed at behavioral symptoms secondary to FTD, other causes of symptoms such as delirium, pain, or discomfort should be excluded. Nonpharmacologic approaches should be aimed at the type of sexual behavior and likely underlying environmental cause. For example, patients may inappropriately disrobe themselves. To address this behavior, hospital staff or caregivers should first eliminate environmental causes by ensuring the room is at a comfortable temperature, dressing the patient in light, breathable clothing, or checking if the patient needs to use the bathroom. If no environmental causes are found, a one-piece jumpsuit with closures on the back of the garment could be utilized to increase the difficulty of undressing.
Other nonpharmacologic methods include providing private areas for patients who are behaving inappropriately or removing potentially stimulating television or media from the environment. Another option is to increase the use of positive, pleasant stimuli. One approach that has shown benefit is music therapy, utilizing popular music genres from the patient’s youth.3
Evidence for pharmacotherapy is limited and largely from case reports and case series. A 2020 meta-analysis by Trieu et al8 reviewed 23 studies to expand on current clinical guidance for patients with bvFTD. These studies showed improvements in behavioral symptoms and reductions in caregiver fatigue with citalopram, trazodone, paroxetine, and fluvoxamine. Six of the trials included in this meta-analysis that evaluated these 4 medications are summarized in Table 2.9-14
Due to the lower risk of adverse effects and favorable safety profiles, SSRIs and trazodone are considered first-line treatment options. Benefit from these medications is theorized to be a result of their serotonergic effects, because serotonin abnormalities and dysfunction have been linked to FTD symptoms. For example, in a patient experiencing hypersexuality, the common adverse effect of low libido associated with SSRIs can be particularly beneficial.8
Continue to: Other medication classes studied in patients...
Other medication classes studied in patients with FTD include antipsychotics, stimulants, anticonvulsants, benzodiazepines, and hormonal therapies. In addition to a black box warning for increased mortality in older patients with dementia-related psychosis, antipsychotics are associated with other serious adverse effects and should be used with caution.7
FTD is a debilitating disease that has a major impact on quality of life, particularly when behavioral symptoms accompany cognitive decline. Though some therapies may possibly improve behavioral symptoms, their routine use remains controversial due to a lack of clear evidence of benefit. In caring for patients with FTD and behavioral symptoms, a multimodal, team-based approach is vital.1
CASE CONTINUED
The treatment team starts Mr. S on several of the modalities discussed in this article over the span of 2 years, with limited efficacy. Nonpharmacologic methods do not provide much benefit because Mr. S is extremely difficult to redirect. Given Mr. S’s past trials of SSRIs prior to admission, sertraline was retrialed and titrated over 2 years. The highest dose utilized during his admission was 200 mg/d. The team starts estrogen therapy but tapers and discontinues it due to ineffectiveness. Mr. S’s use of carbidopa/levodopa is thought to be contributing to his behavioral abnormalities, so the team tapers it to discontinuation; however, Mr. S’s sexually inappropriate behaviors and agitation continue. The team initiates a plan to reduce the dose of quetiapine and switch to gabapentin, but Mr. S fails gradual dose reduction due to his worsening behaviors. He starts gabapentin. The team gradually increases the dose of gabapentin to decrease libido and agitation, respectively. The increase in sertraline dose and use of nonpharmacologic modalities causes Mr. S’s use of as-needed antipsychotics to decrease.
Related Resources
- Ellison JM. What are the stages of frontotemporal dementia? BrightFocus Foundation. July 5, 2021. Accessed July 7, 2023. https://www.brightfocus.org/alzheimers/article/what-are-stages-frontotemporal-dementia
- Dementia and sexually inappropriate behavior. ReaDementia. January 31, 2022. Accessed July 7, 2023. https://readementia.com/dementia-and-sexually-inappropriate-behavior/
Drug Brand Names
Carbidopa/levodopa • Sinemet
Citalopram • Celexa
Donepezil • Aricept
Fluvoxamine • Luvox
Gabapentin • Neurontin
Galantamine • Razadyne
Memantine • Namenda
Paroxetine • Paxil
Quetiapine • Seroquel
Rivastigmine • Exelon
Sertraline • Zoloft
Trazodone • Desyrel
Mr. S, age 77, is admitted to a long-term care facility due to progressive cognitive impairment and sexually inappropriate behavior. He has a history of sexual assault of medical staff. His medical history includes significant frontotemporal dementia (FTD) with behavioral disturbances, abnormal sexual behaviors, subclinical hypothyroidism, schizoid personality disorder, Parkinson disease, posttraumatic stress disorder, and hyperammonemia.
Upon admission, Mr. S’s vital signs are within normal limits except for an elevated thyroid-stimulating hormone (4.54 mIU/L; reference range 0.40 to 4.50 mIU/L). Prior cognitive testing results and updated ammonia levels are unavailable. Mr. S’s current medications include acetaminophen 650 mg every 4 hours as needed for pain, calcium carbonate/vitamin D twice daily for bone health, carbidopa/levodopa 25/100 mg twice daily for Parkinson disease, melatonin 3 mg/d at bedtime for insomnia, quetiapine 25 mg twice daily for psychosis with disturbance of behavior and 12.5 mg every 4 hours as needed for agitation, and trazodone 50 mg/d at bedtime for insomnia. Before Mr. S was admitted, previous therapy with selective serotonin reuptake inhibitors (SSRIs) had been tapered and discontinued. Mr. S had also started antipsychotic therapy at another facility due to worsening behaviors.
In patients with dementia, the brain is experiencing neurodegeneration. Progressively, neurons may stop functioning, lose connections with other neurons, and ultimately face cell death. The specific dementia diagnosis and its clinical features depend on the type of neurons and region of the brain affected.1,2
FTD occurs in response to damage to the frontal and temporal lobes. The frontal lobe correlates to executive functioning, while the temporal lobe plays a role in speech and comprehension. Damage to these areas may result in loss of movement, trouble speaking, difficulty solving complex problems, and problems with social behavior. Specifically, damage to the orbital frontal cortex may cause disinhibition and abnormal behaviors, including emotional lability, vulgarity, and indifference to social nuances.1 Within an FTD diagnosis, there are 3 disorders: behavioral-variant FTD (bvFTD), semantic dementia, and progressive nonfluent aphasia.1 Specifically, bvFTD can result in abnormal sexual behaviors such as making sexually inappropriate statements, masturbating in public, undressing in public, inappropriately or aggressively touching others, or confusing another individual as an intimate partner. In addition to cognitive impairment, these neurobehavioral symptoms can significantly impact an individual’s quality of life while increasing caregiver burden.2
Occurring at a similar frequency to Alzheimer’s disease in patients age <65, FTD is one of the more common causes of early-onset dementia. The mean age of onset is 58 and onset after age 75 is particularly unusual. Memory may not be affected early in the course of the disease, but social changes are likely. As FTD progresses, symptoms will resemble those of Alzheimer’s disease and patients will require assistance with activities of daily living. In later stages of FTD, patients will exhibit language and behavior symptoms. Due to its unique progression, FTD can be commonly misdiagnosed as other mental illnesses or neurocognitive disorders.1
Approaches to treatment: What to consider
Both nonpharmacologic and pharmacologic interventions are appropriate for addressing FTD. Because nonpharmacologic options improve patient safety and overall physical health, they should be used whenever practical. These interventions include safe driving measures, exercise, speech therapy, redirection, offering simple choices when making decisions, and managing environmental cues for behaviors that should be encouraged or discouraged.3
There are no FDA-approved medications to cure or slow the progression of FTD. Therefore, treatment is focused on alleviating neurobehavioral symptoms. The symptoms depend on the type of FTD the patient has; they include cognitive impairment, anxiety, insomnia or sleep disturbances, compulsive behaviors, speech and language problems, and agitation. While many medications have been commonly used for symptomatic relief, evidence for the efficacy of these treatments in FTD is limited.2
Continue to: A review of the literature...
A review of the literature on potential treatments for cognitive impairment and behavioral symptoms of FTD identified 2 trials and 1 case series (Table 14-6) in addition to a 2014 review article7 of current pharmacologic treatments. These trials evaluated cognitive improvement with rivastigmine, memantine, galantamine, and donepezil. None of the trials found a significant benefit from any of these medications for cognitive improvement in FTD. Data were conflicting on whether these medications improved or worsened behavioral symptoms. For example, the case series of 3 patients by Swanberg6 suggested improvement in behavior with memantine, while an open-label study analyzed in a 2014 review article7 found that donepezil may have worsened behaviors. Use of cholinesterase inhibitors or memantine in FTD is not recommended unless it is not certain if the patient has FTD or Alzheimer’s disease.7
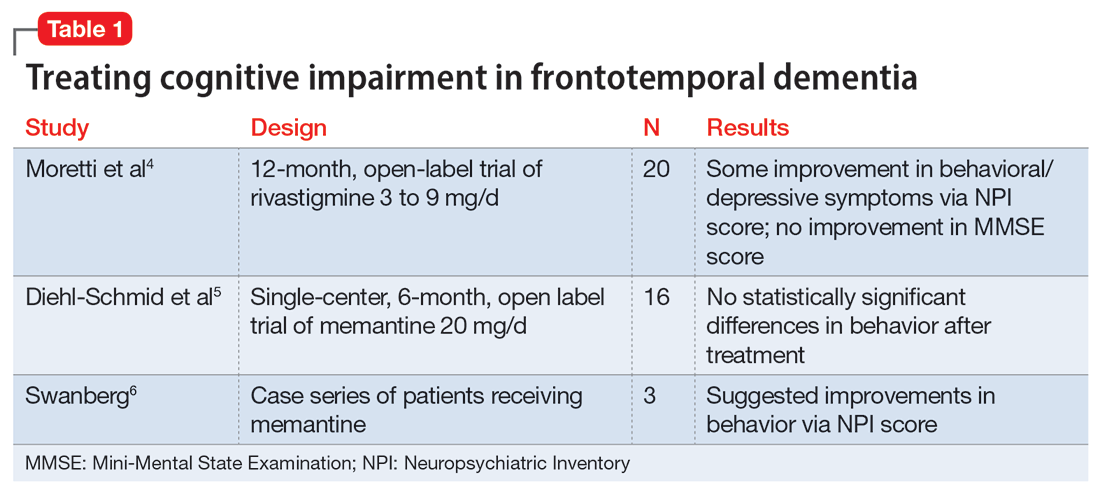
Addressing sexual behaviors. Creating a treatment regimen for FTD behavioral symptoms—specifically for abnormal sexual behaviors—can be challenging. Before starting pharmacotherapy directed at behavioral symptoms secondary to FTD, other causes of symptoms such as delirium, pain, or discomfort should be excluded. Nonpharmacologic approaches should be aimed at the type of sexual behavior and likely underlying environmental cause. For example, patients may inappropriately disrobe themselves. To address this behavior, hospital staff or caregivers should first eliminate environmental causes by ensuring the room is at a comfortable temperature, dressing the patient in light, breathable clothing, or checking if the patient needs to use the bathroom. If no environmental causes are found, a one-piece jumpsuit with closures on the back of the garment could be utilized to increase the difficulty of undressing.
Other nonpharmacologic methods include providing private areas for patients who are behaving inappropriately or removing potentially stimulating television or media from the environment. Another option is to increase the use of positive, pleasant stimuli. One approach that has shown benefit is music therapy, utilizing popular music genres from the patient’s youth.3
Evidence for pharmacotherapy is limited and largely from case reports and case series. A 2020 meta-analysis by Trieu et al8 reviewed 23 studies to expand on current clinical guidance for patients with bvFTD. These studies showed improvements in behavioral symptoms and reductions in caregiver fatigue with citalopram, trazodone, paroxetine, and fluvoxamine. Six of the trials included in this meta-analysis that evaluated these 4 medications are summarized in Table 2.9-14
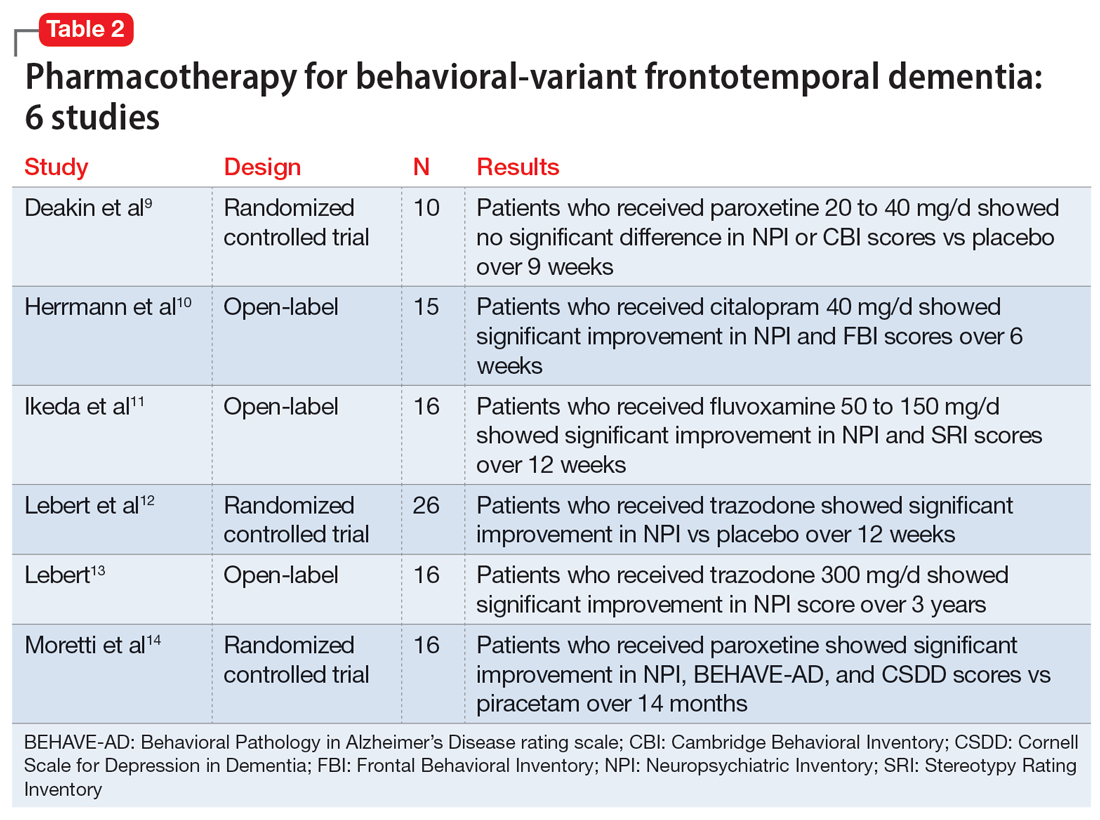
Due to the lower risk of adverse effects and favorable safety profiles, SSRIs and trazodone are considered first-line treatment options. Benefit from these medications is theorized to be a result of their serotonergic effects, because serotonin abnormalities and dysfunction have been linked to FTD symptoms. For example, in a patient experiencing hypersexuality, the common adverse effect of low libido associated with SSRIs can be particularly beneficial.8
Continue to: Other medication classes studied in patients...
Other medication classes studied in patients with FTD include antipsychotics, stimulants, anticonvulsants, benzodiazepines, and hormonal therapies. In addition to a black box warning for increased mortality in older patients with dementia-related psychosis, antipsychotics are associated with other serious adverse effects and should be used with caution.7
FTD is a debilitating disease that has a major impact on quality of life, particularly when behavioral symptoms accompany cognitive decline. Though some therapies may possibly improve behavioral symptoms, their routine use remains controversial due to a lack of clear evidence of benefit. In caring for patients with FTD and behavioral symptoms, a multimodal, team-based approach is vital.1
CASE CONTINUED
The treatment team starts Mr. S on several of the modalities discussed in this article over the span of 2 years, with limited efficacy. Nonpharmacologic methods do not provide much benefit because Mr. S is extremely difficult to redirect. Given Mr. S’s past trials of SSRIs prior to admission, sertraline was retrialed and titrated over 2 years. The highest dose utilized during his admission was 200 mg/d. The team starts estrogen therapy but tapers and discontinues it due to ineffectiveness. Mr. S’s use of carbidopa/levodopa is thought to be contributing to his behavioral abnormalities, so the team tapers it to discontinuation; however, Mr. S’s sexually inappropriate behaviors and agitation continue. The team initiates a plan to reduce the dose of quetiapine and switch to gabapentin, but Mr. S fails gradual dose reduction due to his worsening behaviors. He starts gabapentin. The team gradually increases the dose of gabapentin to decrease libido and agitation, respectively. The increase in sertraline dose and use of nonpharmacologic modalities causes Mr. S’s use of as-needed antipsychotics to decrease.
Related Resources
- Ellison JM. What are the stages of frontotemporal dementia? BrightFocus Foundation. July 5, 2021. Accessed July 7, 2023. https://www.brightfocus.org/alzheimers/article/what-are-stages-frontotemporal-dementia
- Dementia and sexually inappropriate behavior. ReaDementia. January 31, 2022. Accessed July 7, 2023. https://readementia.com/dementia-and-sexually-inappropriate-behavior/
Drug Brand Names
Carbidopa/levodopa • Sinemet
Citalopram • Celexa
Donepezil • Aricept
Fluvoxamine • Luvox
Gabapentin • Neurontin
Galantamine • Razadyne
Memantine • Namenda
Paroxetine • Paxil
Quetiapine • Seroquel
Rivastigmine • Exelon
Sertraline • Zoloft
Trazodone • Desyrel
1. Grossman M. Frontotemporal dementia: a review. J Int Neuropsychol Soc. 2002;8(4):566-583. doi:10.1017/s1355617702814357
2. The Johns Hopkins University. Frontotemporal dementia. Johns Hopkins Medicine. Accessed September 12, 2021. https://www.hopkinsmedicine.org/health/conditions-and-diseases/dementia/frontotemporal-dementia
3. Shinagawa S, Nakajima S, Plitman E, et al. Non-pharmacological management for patients with frontotemporal dementia: a systematic review. J Alzheimers Dis. 2015;45(1):283-293. doi:10.3233/JAD-142109
4. Moretti R, Torre P, Antonello RM, et al. Rivastigmine in frontotemporal dementia: an open-label study. Drugs Aging. 2004;21(14):931-937. doi:10.2165/00002512-200421140-00003
5. Diehl-Schmid J, Förstl H, Perneczky R, et al. A 6-month, open-label study for memantine in patients with frontotemporal dementia. In J Geriatr Psychiatry. 2008;23(7):754-759. doi:10.1002/gps.1973
6. Swanberg MM. Memantine for behavioral disturbances in frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2007;21(2):164-166. doi:10.1097/WAD.0b013e318047df5d
7. Tsai RM, Boxer AL. Treatment of frontotemporal dementia. Curr Treat Options Neurol. 2014;16(11):319. doi:10.1007/s11940-014-0319-0
8. Trieu C, Gossink F, Stek ML, et al. Effectiveness of pharmacological interventions for symptoms of behavioral variant frontotemporal dementia: a systematic review. Cogn Behav Neurol. 2020;33(1):1-15. doi:10.1097/WNN.0000000000000217
9. Deakin JB, Rahman S, Nestor PJ, et al. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology (Berl). 2004;172(4):400-408. doi:10.1007/s00213-003-1686-5
10. Herrmann N, Black SE, Chow T, et al. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry. 2012;20(9):789-797. doi:10.1097/JGP.0b013e31823033f3
11. Ikeda M, Shigenobu K, Fukuhara R, et al. Efficacy of fluvoxamine as a treatment for behavioral symptoms in frontotemporal lobar degeneration patients. Dement Geriatr Cogn Disord. 2004;17(3):117-121. doi:10.1159/000076343
12. Lebert F, Stekke W, Hasenbroekx C, et al. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17(4):355-359. doi:10.1159/000077171
13. Lebert F. Behavioral benefits of trazodone are sustained for the long term in frontotemporal dementia. Therapy. 2006;3(1):93-96. doi:10.1586/14750708.3.1.93
14. Moretti R, Torre P, Antonello RM, et al. Frontotemporal dementia: paroxetine as a possible treatment of behavior symptoms. A randomized, controlled, open 14-month study. Eur Neurol. 2003;49(1):13-19. doi:10.1159/000067021
1. Grossman M. Frontotemporal dementia: a review. J Int Neuropsychol Soc. 2002;8(4):566-583. doi:10.1017/s1355617702814357
2. The Johns Hopkins University. Frontotemporal dementia. Johns Hopkins Medicine. Accessed September 12, 2021. https://www.hopkinsmedicine.org/health/conditions-and-diseases/dementia/frontotemporal-dementia
3. Shinagawa S, Nakajima S, Plitman E, et al. Non-pharmacological management for patients with frontotemporal dementia: a systematic review. J Alzheimers Dis. 2015;45(1):283-293. doi:10.3233/JAD-142109
4. Moretti R, Torre P, Antonello RM, et al. Rivastigmine in frontotemporal dementia: an open-label study. Drugs Aging. 2004;21(14):931-937. doi:10.2165/00002512-200421140-00003
5. Diehl-Schmid J, Förstl H, Perneczky R, et al. A 6-month, open-label study for memantine in patients with frontotemporal dementia. In J Geriatr Psychiatry. 2008;23(7):754-759. doi:10.1002/gps.1973
6. Swanberg MM. Memantine for behavioral disturbances in frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2007;21(2):164-166. doi:10.1097/WAD.0b013e318047df5d
7. Tsai RM, Boxer AL. Treatment of frontotemporal dementia. Curr Treat Options Neurol. 2014;16(11):319. doi:10.1007/s11940-014-0319-0
8. Trieu C, Gossink F, Stek ML, et al. Effectiveness of pharmacological interventions for symptoms of behavioral variant frontotemporal dementia: a systematic review. Cogn Behav Neurol. 2020;33(1):1-15. doi:10.1097/WNN.0000000000000217
9. Deakin JB, Rahman S, Nestor PJ, et al. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology (Berl). 2004;172(4):400-408. doi:10.1007/s00213-003-1686-5
10. Herrmann N, Black SE, Chow T, et al. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry. 2012;20(9):789-797. doi:10.1097/JGP.0b013e31823033f3
11. Ikeda M, Shigenobu K, Fukuhara R, et al. Efficacy of fluvoxamine as a treatment for behavioral symptoms in frontotemporal lobar degeneration patients. Dement Geriatr Cogn Disord. 2004;17(3):117-121. doi:10.1159/000076343
12. Lebert F, Stekke W, Hasenbroekx C, et al. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17(4):355-359. doi:10.1159/000077171
13. Lebert F. Behavioral benefits of trazodone are sustained for the long term in frontotemporal dementia. Therapy. 2006;3(1):93-96. doi:10.1586/14750708.3.1.93
14. Moretti R, Torre P, Antonello RM, et al. Frontotemporal dementia: paroxetine as a possible treatment of behavior symptoms. A randomized, controlled, open 14-month study. Eur Neurol. 2003;49(1):13-19. doi:10.1159/000067021
Dementia diagnosis a good time to reduce polypharmacy
Physicians may be missing opportunities to reduce harmful polypharmacy in elderly patients with newly diagnosed dementia, investigators for a large study of Medicare beneficiaries reported.
They found that those with an incident dementia diagnosis were somewhat more likely to initiate central nervous system–active medications and slightly more likely to discontinue cardiometabolic and anticholinergic medications, compared with controls.
According to the authors, time of diagnosis can be a potential inflexion point for deprescribing long-term medications with high safety risks, limited likelihood of benefit, or possible association with impaired cognition.
“Understanding the chronology of medication changes following a first dementia diagnosis may identify targets for deprescribing interventions to reduce preventable medication-related harms, said Timothy S. Anderson, MD, MAS, of the division of general medicine at Beth Israel Deaconess Medical Center, Boston, and colleagues in JAMA Internal Medicine.
“Our results provide a baseline to inform efforts to rethink the clinical approach to medication use at the time of a new dementia diagnosis.”
Hundreds of thousands of Americans are diagnosed annually with Alzheimer’s and related dementias, the authors pointed out, and the majority have multiple other chronic conditions. Worsening cognitive impairment may alter the risk-benefit balance of medications taken for these conditions.
Matched cohort study
The sample consisted of adults 67 years or older enrolled in traditional Medicare and Medicare Part D. Patients with an initial incident dementia diagnosis between January 2012 and December 2018 were matched with controls (as of last doctor’s office visit) based on demographics, geographic location, and baseline medication count. Data were analyzed from 2021 to June 2023.
The study included 266,675 adults with incident dementia and 266,675 controls. In both groups, 65.1% were 80 years or older (mean age, 82.2) and 67.8% were female. At baseline, patients with incident dementia were more likely than controls to use CNS-active medications (54.32% vs. 48.39%) and anticholinergic medications (17.79% vs. 15.96%) and less likely to use most cardiometabolic medications (for example, antidiabetics, 31.19% vs. 36.45%).
Immediately following the index diagnosis, the dementia cohort had greater increases in the mean number of medications used: 0.41 vs. –0.06 (95% confidence interval, 0.27-0.66) and in the proportion using CNS-active medications (absolute change, 3.44% vs. 0.79%; 95% CI, 0.85%-4.45%). The rise was because of an increased use of antipsychotics, antidepressants, and antiepileptics.
The affected cohort showed a modestly greater decline in anticholinergic medications: quarterly change in use: −0.53% vs. −0.21% (95% CI, −0.55% to −0.08%); and in most cardiometabolic medications: for example, quarterly change in antihypertensive use: –0.84% vs. –0.40% (95% CI, –0.64% to –0.25%). Still, a year post diagnosis, 75.2% of dementia patients were using five or more medications, for a 2.8% increase.
The drug classes with the steepest rate of discontinuation – such as lipid-lowering and antihypertensive medications – had low risks for adverse drug events, while higher-risk classes – such as insulins and antiplatelet and anticoagulant agents – had smaller or no reductions in use.
While the findings point to opportunities to reduce polypharmacy by deprescribing long-term medications of dubious benefit, interventions to reduce polypharmacy and inappropriate medications have been modestly successful for patients without dementia, the authors said. But the recent OPTIMIZE trial, an educational effort aimed at primary care clinicians and patients with cognitive impairment, reduced neither polypharmacy nor potentially inappropriate medications.
Luke D. Kim, MD, a geriatrician at the Cleveland Clinic in Ohio, agreed that seniors with dementia can benefit from reassessment of their pharmacologic therapies. “Older adults in general are more prone to have side effects from medications as their renal and hepatic clearance and metabolism are different and lower than those of younger individuals. But they tend to take multiple medications owing to more comorbidities,” said Dr. Kim, who was not involved in the study. “While all older adults need to be more careful about medication management, those with dementia need an even more careful approach as they have diminished cognitive reserve and risk more potential harm from medications.”
The authors noted that since decision-making models aligned with patient priorities for older adults without dementia led to reductions in overall medication use, that may be a path forward in populations with dementia.
The study was supported by grants from the National Institute on Aging, National Institutes of Health. The authors had no competing interests to disclose. Dr. Kim disclosed no competing interests relevant to his comments.
Physicians may be missing opportunities to reduce harmful polypharmacy in elderly patients with newly diagnosed dementia, investigators for a large study of Medicare beneficiaries reported.
They found that those with an incident dementia diagnosis were somewhat more likely to initiate central nervous system–active medications and slightly more likely to discontinue cardiometabolic and anticholinergic medications, compared with controls.
According to the authors, time of diagnosis can be a potential inflexion point for deprescribing long-term medications with high safety risks, limited likelihood of benefit, or possible association with impaired cognition.
“Understanding the chronology of medication changes following a first dementia diagnosis may identify targets for deprescribing interventions to reduce preventable medication-related harms, said Timothy S. Anderson, MD, MAS, of the division of general medicine at Beth Israel Deaconess Medical Center, Boston, and colleagues in JAMA Internal Medicine.
“Our results provide a baseline to inform efforts to rethink the clinical approach to medication use at the time of a new dementia diagnosis.”
Hundreds of thousands of Americans are diagnosed annually with Alzheimer’s and related dementias, the authors pointed out, and the majority have multiple other chronic conditions. Worsening cognitive impairment may alter the risk-benefit balance of medications taken for these conditions.
Matched cohort study
The sample consisted of adults 67 years or older enrolled in traditional Medicare and Medicare Part D. Patients with an initial incident dementia diagnosis between January 2012 and December 2018 were matched with controls (as of last doctor’s office visit) based on demographics, geographic location, and baseline medication count. Data were analyzed from 2021 to June 2023.
The study included 266,675 adults with incident dementia and 266,675 controls. In both groups, 65.1% were 80 years or older (mean age, 82.2) and 67.8% were female. At baseline, patients with incident dementia were more likely than controls to use CNS-active medications (54.32% vs. 48.39%) and anticholinergic medications (17.79% vs. 15.96%) and less likely to use most cardiometabolic medications (for example, antidiabetics, 31.19% vs. 36.45%).
Immediately following the index diagnosis, the dementia cohort had greater increases in the mean number of medications used: 0.41 vs. –0.06 (95% confidence interval, 0.27-0.66) and in the proportion using CNS-active medications (absolute change, 3.44% vs. 0.79%; 95% CI, 0.85%-4.45%). The rise was because of an increased use of antipsychotics, antidepressants, and antiepileptics.
The affected cohort showed a modestly greater decline in anticholinergic medications: quarterly change in use: −0.53% vs. −0.21% (95% CI, −0.55% to −0.08%); and in most cardiometabolic medications: for example, quarterly change in antihypertensive use: –0.84% vs. –0.40% (95% CI, –0.64% to –0.25%). Still, a year post diagnosis, 75.2% of dementia patients were using five or more medications, for a 2.8% increase.
The drug classes with the steepest rate of discontinuation – such as lipid-lowering and antihypertensive medications – had low risks for adverse drug events, while higher-risk classes – such as insulins and antiplatelet and anticoagulant agents – had smaller or no reductions in use.
While the findings point to opportunities to reduce polypharmacy by deprescribing long-term medications of dubious benefit, interventions to reduce polypharmacy and inappropriate medications have been modestly successful for patients without dementia, the authors said. But the recent OPTIMIZE trial, an educational effort aimed at primary care clinicians and patients with cognitive impairment, reduced neither polypharmacy nor potentially inappropriate medications.
Luke D. Kim, MD, a geriatrician at the Cleveland Clinic in Ohio, agreed that seniors with dementia can benefit from reassessment of their pharmacologic therapies. “Older adults in general are more prone to have side effects from medications as their renal and hepatic clearance and metabolism are different and lower than those of younger individuals. But they tend to take multiple medications owing to more comorbidities,” said Dr. Kim, who was not involved in the study. “While all older adults need to be more careful about medication management, those with dementia need an even more careful approach as they have diminished cognitive reserve and risk more potential harm from medications.”
The authors noted that since decision-making models aligned with patient priorities for older adults without dementia led to reductions in overall medication use, that may be a path forward in populations with dementia.
The study was supported by grants from the National Institute on Aging, National Institutes of Health. The authors had no competing interests to disclose. Dr. Kim disclosed no competing interests relevant to his comments.
Physicians may be missing opportunities to reduce harmful polypharmacy in elderly patients with newly diagnosed dementia, investigators for a large study of Medicare beneficiaries reported.
They found that those with an incident dementia diagnosis were somewhat more likely to initiate central nervous system–active medications and slightly more likely to discontinue cardiometabolic and anticholinergic medications, compared with controls.
According to the authors, time of diagnosis can be a potential inflexion point for deprescribing long-term medications with high safety risks, limited likelihood of benefit, or possible association with impaired cognition.
“Understanding the chronology of medication changes following a first dementia diagnosis may identify targets for deprescribing interventions to reduce preventable medication-related harms, said Timothy S. Anderson, MD, MAS, of the division of general medicine at Beth Israel Deaconess Medical Center, Boston, and colleagues in JAMA Internal Medicine.
“Our results provide a baseline to inform efforts to rethink the clinical approach to medication use at the time of a new dementia diagnosis.”
Hundreds of thousands of Americans are diagnosed annually with Alzheimer’s and related dementias, the authors pointed out, and the majority have multiple other chronic conditions. Worsening cognitive impairment may alter the risk-benefit balance of medications taken for these conditions.
Matched cohort study
The sample consisted of adults 67 years or older enrolled in traditional Medicare and Medicare Part D. Patients with an initial incident dementia diagnosis between January 2012 and December 2018 were matched with controls (as of last doctor’s office visit) based on demographics, geographic location, and baseline medication count. Data were analyzed from 2021 to June 2023.
The study included 266,675 adults with incident dementia and 266,675 controls. In both groups, 65.1% were 80 years or older (mean age, 82.2) and 67.8% were female. At baseline, patients with incident dementia were more likely than controls to use CNS-active medications (54.32% vs. 48.39%) and anticholinergic medications (17.79% vs. 15.96%) and less likely to use most cardiometabolic medications (for example, antidiabetics, 31.19% vs. 36.45%).
Immediately following the index diagnosis, the dementia cohort had greater increases in the mean number of medications used: 0.41 vs. –0.06 (95% confidence interval, 0.27-0.66) and in the proportion using CNS-active medications (absolute change, 3.44% vs. 0.79%; 95% CI, 0.85%-4.45%). The rise was because of an increased use of antipsychotics, antidepressants, and antiepileptics.
The affected cohort showed a modestly greater decline in anticholinergic medications: quarterly change in use: −0.53% vs. −0.21% (95% CI, −0.55% to −0.08%); and in most cardiometabolic medications: for example, quarterly change in antihypertensive use: –0.84% vs. –0.40% (95% CI, –0.64% to –0.25%). Still, a year post diagnosis, 75.2% of dementia patients were using five or more medications, for a 2.8% increase.
The drug classes with the steepest rate of discontinuation – such as lipid-lowering and antihypertensive medications – had low risks for adverse drug events, while higher-risk classes – such as insulins and antiplatelet and anticoagulant agents – had smaller or no reductions in use.
While the findings point to opportunities to reduce polypharmacy by deprescribing long-term medications of dubious benefit, interventions to reduce polypharmacy and inappropriate medications have been modestly successful for patients without dementia, the authors said. But the recent OPTIMIZE trial, an educational effort aimed at primary care clinicians and patients with cognitive impairment, reduced neither polypharmacy nor potentially inappropriate medications.
Luke D. Kim, MD, a geriatrician at the Cleveland Clinic in Ohio, agreed that seniors with dementia can benefit from reassessment of their pharmacologic therapies. “Older adults in general are more prone to have side effects from medications as their renal and hepatic clearance and metabolism are different and lower than those of younger individuals. But they tend to take multiple medications owing to more comorbidities,” said Dr. Kim, who was not involved in the study. “While all older adults need to be more careful about medication management, those with dementia need an even more careful approach as they have diminished cognitive reserve and risk more potential harm from medications.”
The authors noted that since decision-making models aligned with patient priorities for older adults without dementia led to reductions in overall medication use, that may be a path forward in populations with dementia.
The study was supported by grants from the National Institute on Aging, National Institutes of Health. The authors had no competing interests to disclose. Dr. Kim disclosed no competing interests relevant to his comments.
FROM JAMA INTERNAL MEDICINE
Most with early AD not eligible for new antiamyloid drugs
Only a small fraction of older adults in the early stages of Alzheimer’s disease (AD) meet eligibility criteria to receive treatment with newly approved antiamyloid drugs, largely because of the presence of medical conditions or neuroimaging findings, new research shows.
Applying the clinical trial criteria, only about 8%-17% of amyloid-positive individuals with early AD would be eligible for lecanemab (Leqembi), and even fewer, 5%-9%, would be eligible for aducanumab (Aduhelm), the researchers found.
This study highlights the “limited suitability” of most adults with mild cognitive impairment (MCI) or mild dementia with elevated brain amyloid for treatment with these anti–beta amyloid monoclonal antibodies, write Maria Vassilaki, MD, PhD, and colleagues with Mayo Clinic, Rochester, Minn.
The study was published online in Neurology
The authors of an accompanying editorial write that this study “provides an important estimate of treatment eligibility for amyloid-lowering monoclonal antibodies for early AD to help health systems make realistic plans for providing these treatments.”
More real-world data needed
Dr. Vassilaki and colleagues applied eligibility criteria for lecanemab and aducanumab to 237 older adults with MCI or mild dementia and increased brain amyloid burden from the Mayo Clinic Study of Aging (MCSA). Their mean age was 80.9 years, 55% were men, and most were White.
After applying lecanemab’s inclusion criteria, less than half of the study population was eligible to receive treatment (112 of 237, or 47%).
A total of 21 people were excluded because of a body mass index less than 17 or greater than or equal to 35; 48 due to a Clinical Dementia Rating (CDR) global score other than 0.5 or 1.0; 46 because they did not meet WMS-R Logical Memory II scores for age; 8 because of a Mini Mental State Examination (MMSE) score outside the bounds of 22-30; and two because of a CDR memory score less than 0.5.
Applying lecanemab’s exclusion criteria further narrowed the number of eligible participants from 112 to 19 (8% of 237).
Notable exclusions included cardiopulmonary contraindications, central nervous system–related exclusions such as brain cancer, Parkinson’s disease, epilepsy or brain injury, imaging findings, and history of cancer.
The results were similar for aducanumab, with 104 of the 237 participants (44%) meeting the trial’s inclusion criteria. Applying aducanumab’s exclusion criteria further reduced the number of eligible participants to 12 (5% of 237).
A sensitivity analysis including participants with MCI, without CDR global, MMSE, or WMS-R Logical Memory II score restrictions, resulted in a somewhat higher percentage of eligible participants (17.4% for lecanemab and 8.9% for aducanumab).
Shared decision-making
“Clinicians and health systems should be aware that by applying the clinical trial criteria, a smaller percentage might be eligible for these treatments than originally anticipated,” Dr. Vassilaki told this news organization. To help clinicians, there are published recommendations for the appropriate use of these treatments, she noted.
Given that clinical trial participants are typically healthier than the general population, Dr. Vassilaki said that research is needed to examine the safety and efficacy of antiamyloid therapies in larger, more diverse populations as well as in less healthy populations, before these therapies may be more widely available to people with AD.
“We can take advantage of the postmarketing surveillance of side effects, and also enrollment of patients receiving these treatments to registries could provide us with data useful for any necessary adjustment to drug use,” Dr. Vassilaki told this news organization.
‘Sharp focus’
This study “brings the issue of eligibility for amyloid-lowering antibody treatment into sharp focus,” Matthew Howe, MD, PhD, with Butler Hospital Memory & Aging Program, Providence, R.I., and colleagues note in their editorial.
“The results underscore the importance of careful patient selection to help identify patients most likely to benefit from treatment and exclude those at risk for serious outcomes,” they write.
They also write that appropriate use recommendations for lecanemab and aducanumab “will be revisited as more real-world data emerge, especially about safety.”
For now, clinicians “must exercise clinical judgment in selecting patients for treatment with shared decision-making with patients and families,” they add.
The study was supported by the National Institutes of Health, the National Institute on Aging, the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, the Mayo Foundation for Medical Education and Research, the Liston Award, the GHR Foundation and the Schuler Foundation. Dr. Vassilaki has consulted for F. Hoffmann-La Roche and has equity ownership in Abbott Laboratories, Johnson & Johnson, Medtronic, Merck, and Amgen. Dr. Howe has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Only a small fraction of older adults in the early stages of Alzheimer’s disease (AD) meet eligibility criteria to receive treatment with newly approved antiamyloid drugs, largely because of the presence of medical conditions or neuroimaging findings, new research shows.
Applying the clinical trial criteria, only about 8%-17% of amyloid-positive individuals with early AD would be eligible for lecanemab (Leqembi), and even fewer, 5%-9%, would be eligible for aducanumab (Aduhelm), the researchers found.
This study highlights the “limited suitability” of most adults with mild cognitive impairment (MCI) or mild dementia with elevated brain amyloid for treatment with these anti–beta amyloid monoclonal antibodies, write Maria Vassilaki, MD, PhD, and colleagues with Mayo Clinic, Rochester, Minn.
The study was published online in Neurology
The authors of an accompanying editorial write that this study “provides an important estimate of treatment eligibility for amyloid-lowering monoclonal antibodies for early AD to help health systems make realistic plans for providing these treatments.”
More real-world data needed
Dr. Vassilaki and colleagues applied eligibility criteria for lecanemab and aducanumab to 237 older adults with MCI or mild dementia and increased brain amyloid burden from the Mayo Clinic Study of Aging (MCSA). Their mean age was 80.9 years, 55% were men, and most were White.
After applying lecanemab’s inclusion criteria, less than half of the study population was eligible to receive treatment (112 of 237, or 47%).
A total of 21 people were excluded because of a body mass index less than 17 or greater than or equal to 35; 48 due to a Clinical Dementia Rating (CDR) global score other than 0.5 or 1.0; 46 because they did not meet WMS-R Logical Memory II scores for age; 8 because of a Mini Mental State Examination (MMSE) score outside the bounds of 22-30; and two because of a CDR memory score less than 0.5.
Applying lecanemab’s exclusion criteria further narrowed the number of eligible participants from 112 to 19 (8% of 237).
Notable exclusions included cardiopulmonary contraindications, central nervous system–related exclusions such as brain cancer, Parkinson’s disease, epilepsy or brain injury, imaging findings, and history of cancer.
The results were similar for aducanumab, with 104 of the 237 participants (44%) meeting the trial’s inclusion criteria. Applying aducanumab’s exclusion criteria further reduced the number of eligible participants to 12 (5% of 237).
A sensitivity analysis including participants with MCI, without CDR global, MMSE, or WMS-R Logical Memory II score restrictions, resulted in a somewhat higher percentage of eligible participants (17.4% for lecanemab and 8.9% for aducanumab).
Shared decision-making
“Clinicians and health systems should be aware that by applying the clinical trial criteria, a smaller percentage might be eligible for these treatments than originally anticipated,” Dr. Vassilaki told this news organization. To help clinicians, there are published recommendations for the appropriate use of these treatments, she noted.
Given that clinical trial participants are typically healthier than the general population, Dr. Vassilaki said that research is needed to examine the safety and efficacy of antiamyloid therapies in larger, more diverse populations as well as in less healthy populations, before these therapies may be more widely available to people with AD.
“We can take advantage of the postmarketing surveillance of side effects, and also enrollment of patients receiving these treatments to registries could provide us with data useful for any necessary adjustment to drug use,” Dr. Vassilaki told this news organization.
‘Sharp focus’
This study “brings the issue of eligibility for amyloid-lowering antibody treatment into sharp focus,” Matthew Howe, MD, PhD, with Butler Hospital Memory & Aging Program, Providence, R.I., and colleagues note in their editorial.
“The results underscore the importance of careful patient selection to help identify patients most likely to benefit from treatment and exclude those at risk for serious outcomes,” they write.
They also write that appropriate use recommendations for lecanemab and aducanumab “will be revisited as more real-world data emerge, especially about safety.”
For now, clinicians “must exercise clinical judgment in selecting patients for treatment with shared decision-making with patients and families,” they add.
The study was supported by the National Institutes of Health, the National Institute on Aging, the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, the Mayo Foundation for Medical Education and Research, the Liston Award, the GHR Foundation and the Schuler Foundation. Dr. Vassilaki has consulted for F. Hoffmann-La Roche and has equity ownership in Abbott Laboratories, Johnson & Johnson, Medtronic, Merck, and Amgen. Dr. Howe has no conflicts of interest.
A version of this article first appeared on Medscape.com.
Only a small fraction of older adults in the early stages of Alzheimer’s disease (AD) meet eligibility criteria to receive treatment with newly approved antiamyloid drugs, largely because of the presence of medical conditions or neuroimaging findings, new research shows.
Applying the clinical trial criteria, only about 8%-17% of amyloid-positive individuals with early AD would be eligible for lecanemab (Leqembi), and even fewer, 5%-9%, would be eligible for aducanumab (Aduhelm), the researchers found.
This study highlights the “limited suitability” of most adults with mild cognitive impairment (MCI) or mild dementia with elevated brain amyloid for treatment with these anti–beta amyloid monoclonal antibodies, write Maria Vassilaki, MD, PhD, and colleagues with Mayo Clinic, Rochester, Minn.
The study was published online in Neurology
The authors of an accompanying editorial write that this study “provides an important estimate of treatment eligibility for amyloid-lowering monoclonal antibodies for early AD to help health systems make realistic plans for providing these treatments.”
More real-world data needed
Dr. Vassilaki and colleagues applied eligibility criteria for lecanemab and aducanumab to 237 older adults with MCI or mild dementia and increased brain amyloid burden from the Mayo Clinic Study of Aging (MCSA). Their mean age was 80.9 years, 55% were men, and most were White.
After applying lecanemab’s inclusion criteria, less than half of the study population was eligible to receive treatment (112 of 237, or 47%).
A total of 21 people were excluded because of a body mass index less than 17 or greater than or equal to 35; 48 due to a Clinical Dementia Rating (CDR) global score other than 0.5 or 1.0; 46 because they did not meet WMS-R Logical Memory II scores for age; 8 because of a Mini Mental State Examination (MMSE) score outside the bounds of 22-30; and two because of a CDR memory score less than 0.5.
Applying lecanemab’s exclusion criteria further narrowed the number of eligible participants from 112 to 19 (8% of 237).
Notable exclusions included cardiopulmonary contraindications, central nervous system–related exclusions such as brain cancer, Parkinson’s disease, epilepsy or brain injury, imaging findings, and history of cancer.
The results were similar for aducanumab, with 104 of the 237 participants (44%) meeting the trial’s inclusion criteria. Applying aducanumab’s exclusion criteria further reduced the number of eligible participants to 12 (5% of 237).
A sensitivity analysis including participants with MCI, without CDR global, MMSE, or WMS-R Logical Memory II score restrictions, resulted in a somewhat higher percentage of eligible participants (17.4% for lecanemab and 8.9% for aducanumab).
Shared decision-making
“Clinicians and health systems should be aware that by applying the clinical trial criteria, a smaller percentage might be eligible for these treatments than originally anticipated,” Dr. Vassilaki told this news organization. To help clinicians, there are published recommendations for the appropriate use of these treatments, she noted.
Given that clinical trial participants are typically healthier than the general population, Dr. Vassilaki said that research is needed to examine the safety and efficacy of antiamyloid therapies in larger, more diverse populations as well as in less healthy populations, before these therapies may be more widely available to people with AD.
“We can take advantage of the postmarketing surveillance of side effects, and also enrollment of patients receiving these treatments to registries could provide us with data useful for any necessary adjustment to drug use,” Dr. Vassilaki told this news organization.
‘Sharp focus’
This study “brings the issue of eligibility for amyloid-lowering antibody treatment into sharp focus,” Matthew Howe, MD, PhD, with Butler Hospital Memory & Aging Program, Providence, R.I., and colleagues note in their editorial.
“The results underscore the importance of careful patient selection to help identify patients most likely to benefit from treatment and exclude those at risk for serious outcomes,” they write.
They also write that appropriate use recommendations for lecanemab and aducanumab “will be revisited as more real-world data emerge, especially about safety.”
For now, clinicians “must exercise clinical judgment in selecting patients for treatment with shared decision-making with patients and families,” they add.
The study was supported by the National Institutes of Health, the National Institute on Aging, the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, the Mayo Foundation for Medical Education and Research, the Liston Award, the GHR Foundation and the Schuler Foundation. Dr. Vassilaki has consulted for F. Hoffmann-La Roche and has equity ownership in Abbott Laboratories, Johnson & Johnson, Medtronic, Merck, and Amgen. Dr. Howe has no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Few meet eligibility for newer Alzheimer’s drugs
, a cross sectional study has found.
Reporting in the journal Neurology, researchers from the Mayo Clinic in Rochester, Minn., and the University of Chicago found that only a small percentage of patients in the Mayo Clinic Study of Aging (MCSA) with mild cognitive impairment (MCI) or mild dementia due to Alzheimer’s disease would meet the clinical trial eligibility requirements of either agent.
“Our study results show only a small percentage of people with early Alzheimer’s disease may be eligible to receive treatment, mostly due to chronic health conditions and brain scan abnormalities common in older adults,” said lead researcher Maria Vassilaki, MD, PhD, an epidemiologist at Mayo Clinic in Rochester, Minn.
Applying clinical trial exclusion criteria to a broader population
The study included 237 people aged 50-90, 222 who had MCI and 15 with mild dementia, and whose brain scans showed increased amounts of amyloid-beta plaques. Average age of the participants was 80.9 years and 97.5% were White (99.6% not Hispanic or Latino).
The researchers then looked at the eligibility criteria for the pivotal clinical trials for lecanemab, which the U.S. Food and Drug Administration approved in January this year, and aducanumab, which the FDA cleared in 2021. Both drugs received FDA accelerated approval.
For lecanemab, clinical trial inclusion required specific scores for the Clinical Dementia Rating (CDR) (other than 0.5 or 1.0), Wechsler Memory Scale (WMS-R) Logical Memory II (which varied with age group), or Mini-Mental State Examination (MMSE) (22 to 30). A body mass index between 17 and 35 kg/m2 was also an inclusion criteria. Only 112 people, or 47%, met the inclusion criteria. Exclusion criteria included a history of cardiovascular disease or cancer, Parkinson’s disease, or brain injury, or a positive brain scan. When the exclusion criteria were applied, only 19 people, or 8%, qualified for the lecanemab trial.
When the researchers modified the exclusion criteria to include all study participants with MCI but not applying results from additional cognitive tests, 17.4% of MCSA patients would have been eligible for the lecanemab trial.
Aducanumab clinical trial inclusion criteria were a CDR global score other than 0.5 and an MMSE below 24, with an age cutoff of 85 years. Only 104 of the MCSA population, or 44%, met the clinical trial criteria. When the researchers applied the exclusion criteria for cardiovascular disease, central nervous system-related exclusions (such as brain cancer or epilepsy), a history of cancer, or brain scan abnormalities, they found that only 12 people, or 5%, would have been eligible for an aducanumab trial.
“Clinical trials often have strict eligibility criteria and could exclude those with other conditions that could be common in older adults,” Dr. Vassilaki said in emailed comments. “Thus, we wanted to examine if we apply these criteria to a study that recruits participants from the community, how many of the individuals in the early symptomatic stages, mild cognitive impairment or mild dementia due to Alzheimer’s disease, would be eligible for the treatment.”
Dr. Vassilaki said these drugs need to be studied in larger, more diverse populations, as well as in less healthy populations, before they’re more widely available to people with Alzheimer’s disease. “In addition,” she said, “we can learn more from the postmarketing surveillance of side effects and also from registries of patients receiving these treatments.”
One limitation of the study Dr. Vassilaki pointed out is the overwhelmingly White population. Evaluating the clinical trial eligibility criteria in more diverse populations is crucial, she said.
Estimating the number of patients who would qualify for treatment
In an accompanying commentary, Matthew Howes, MD, of Butler Hospital and Brown University in Providence, R.I., and colleagues wrote that the study findings provide health systems planning to offer amyloid-lowering antibodies for Alzheimer’s disease an estimate of how many patients would be eligible for the treatments. “Providers must exercise clinical judgment in selecting patients for treatment with shared decision-making with patients and families,” the commentators wrote.
The study was supported by the National Institutes of Health, the National Institute on Aging, the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, the Mayo Foundation for Medical Education and Research, the Liston Award, the GHR Foundation, and the Schuler Foundation. Dr. Vassilaki disclosed relationships with F. Hoffmann-La Roche, Abbott Laboratories, Johnson & Johnson, Medtronic, Merck, and Amgen. Dr. Howe has no relevant disclosures.
, a cross sectional study has found.
Reporting in the journal Neurology, researchers from the Mayo Clinic in Rochester, Minn., and the University of Chicago found that only a small percentage of patients in the Mayo Clinic Study of Aging (MCSA) with mild cognitive impairment (MCI) or mild dementia due to Alzheimer’s disease would meet the clinical trial eligibility requirements of either agent.
“Our study results show only a small percentage of people with early Alzheimer’s disease may be eligible to receive treatment, mostly due to chronic health conditions and brain scan abnormalities common in older adults,” said lead researcher Maria Vassilaki, MD, PhD, an epidemiologist at Mayo Clinic in Rochester, Minn.
Applying clinical trial exclusion criteria to a broader population
The study included 237 people aged 50-90, 222 who had MCI and 15 with mild dementia, and whose brain scans showed increased amounts of amyloid-beta plaques. Average age of the participants was 80.9 years and 97.5% were White (99.6% not Hispanic or Latino).
The researchers then looked at the eligibility criteria for the pivotal clinical trials for lecanemab, which the U.S. Food and Drug Administration approved in January this year, and aducanumab, which the FDA cleared in 2021. Both drugs received FDA accelerated approval.
For lecanemab, clinical trial inclusion required specific scores for the Clinical Dementia Rating (CDR) (other than 0.5 or 1.0), Wechsler Memory Scale (WMS-R) Logical Memory II (which varied with age group), or Mini-Mental State Examination (MMSE) (22 to 30). A body mass index between 17 and 35 kg/m2 was also an inclusion criteria. Only 112 people, or 47%, met the inclusion criteria. Exclusion criteria included a history of cardiovascular disease or cancer, Parkinson’s disease, or brain injury, or a positive brain scan. When the exclusion criteria were applied, only 19 people, or 8%, qualified for the lecanemab trial.
When the researchers modified the exclusion criteria to include all study participants with MCI but not applying results from additional cognitive tests, 17.4% of MCSA patients would have been eligible for the lecanemab trial.
Aducanumab clinical trial inclusion criteria were a CDR global score other than 0.5 and an MMSE below 24, with an age cutoff of 85 years. Only 104 of the MCSA population, or 44%, met the clinical trial criteria. When the researchers applied the exclusion criteria for cardiovascular disease, central nervous system-related exclusions (such as brain cancer or epilepsy), a history of cancer, or brain scan abnormalities, they found that only 12 people, or 5%, would have been eligible for an aducanumab trial.
“Clinical trials often have strict eligibility criteria and could exclude those with other conditions that could be common in older adults,” Dr. Vassilaki said in emailed comments. “Thus, we wanted to examine if we apply these criteria to a study that recruits participants from the community, how many of the individuals in the early symptomatic stages, mild cognitive impairment or mild dementia due to Alzheimer’s disease, would be eligible for the treatment.”
Dr. Vassilaki said these drugs need to be studied in larger, more diverse populations, as well as in less healthy populations, before they’re more widely available to people with Alzheimer’s disease. “In addition,” she said, “we can learn more from the postmarketing surveillance of side effects and also from registries of patients receiving these treatments.”
One limitation of the study Dr. Vassilaki pointed out is the overwhelmingly White population. Evaluating the clinical trial eligibility criteria in more diverse populations is crucial, she said.
Estimating the number of patients who would qualify for treatment
In an accompanying commentary, Matthew Howes, MD, of Butler Hospital and Brown University in Providence, R.I., and colleagues wrote that the study findings provide health systems planning to offer amyloid-lowering antibodies for Alzheimer’s disease an estimate of how many patients would be eligible for the treatments. “Providers must exercise clinical judgment in selecting patients for treatment with shared decision-making with patients and families,” the commentators wrote.
The study was supported by the National Institutes of Health, the National Institute on Aging, the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, the Mayo Foundation for Medical Education and Research, the Liston Award, the GHR Foundation, and the Schuler Foundation. Dr. Vassilaki disclosed relationships with F. Hoffmann-La Roche, Abbott Laboratories, Johnson & Johnson, Medtronic, Merck, and Amgen. Dr. Howe has no relevant disclosures.
, a cross sectional study has found.
Reporting in the journal Neurology, researchers from the Mayo Clinic in Rochester, Minn., and the University of Chicago found that only a small percentage of patients in the Mayo Clinic Study of Aging (MCSA) with mild cognitive impairment (MCI) or mild dementia due to Alzheimer’s disease would meet the clinical trial eligibility requirements of either agent.
“Our study results show only a small percentage of people with early Alzheimer’s disease may be eligible to receive treatment, mostly due to chronic health conditions and brain scan abnormalities common in older adults,” said lead researcher Maria Vassilaki, MD, PhD, an epidemiologist at Mayo Clinic in Rochester, Minn.
Applying clinical trial exclusion criteria to a broader population
The study included 237 people aged 50-90, 222 who had MCI and 15 with mild dementia, and whose brain scans showed increased amounts of amyloid-beta plaques. Average age of the participants was 80.9 years and 97.5% were White (99.6% not Hispanic or Latino).
The researchers then looked at the eligibility criteria for the pivotal clinical trials for lecanemab, which the U.S. Food and Drug Administration approved in January this year, and aducanumab, which the FDA cleared in 2021. Both drugs received FDA accelerated approval.
For lecanemab, clinical trial inclusion required specific scores for the Clinical Dementia Rating (CDR) (other than 0.5 or 1.0), Wechsler Memory Scale (WMS-R) Logical Memory II (which varied with age group), or Mini-Mental State Examination (MMSE) (22 to 30). A body mass index between 17 and 35 kg/m2 was also an inclusion criteria. Only 112 people, or 47%, met the inclusion criteria. Exclusion criteria included a history of cardiovascular disease or cancer, Parkinson’s disease, or brain injury, or a positive brain scan. When the exclusion criteria were applied, only 19 people, or 8%, qualified for the lecanemab trial.
When the researchers modified the exclusion criteria to include all study participants with MCI but not applying results from additional cognitive tests, 17.4% of MCSA patients would have been eligible for the lecanemab trial.
Aducanumab clinical trial inclusion criteria were a CDR global score other than 0.5 and an MMSE below 24, with an age cutoff of 85 years. Only 104 of the MCSA population, or 44%, met the clinical trial criteria. When the researchers applied the exclusion criteria for cardiovascular disease, central nervous system-related exclusions (such as brain cancer or epilepsy), a history of cancer, or brain scan abnormalities, they found that only 12 people, or 5%, would have been eligible for an aducanumab trial.
“Clinical trials often have strict eligibility criteria and could exclude those with other conditions that could be common in older adults,” Dr. Vassilaki said in emailed comments. “Thus, we wanted to examine if we apply these criteria to a study that recruits participants from the community, how many of the individuals in the early symptomatic stages, mild cognitive impairment or mild dementia due to Alzheimer’s disease, would be eligible for the treatment.”
Dr. Vassilaki said these drugs need to be studied in larger, more diverse populations, as well as in less healthy populations, before they’re more widely available to people with Alzheimer’s disease. “In addition,” she said, “we can learn more from the postmarketing surveillance of side effects and also from registries of patients receiving these treatments.”
One limitation of the study Dr. Vassilaki pointed out is the overwhelmingly White population. Evaluating the clinical trial eligibility criteria in more diverse populations is crucial, she said.
Estimating the number of patients who would qualify for treatment
In an accompanying commentary, Matthew Howes, MD, of Butler Hospital and Brown University in Providence, R.I., and colleagues wrote that the study findings provide health systems planning to offer amyloid-lowering antibodies for Alzheimer’s disease an estimate of how many patients would be eligible for the treatments. “Providers must exercise clinical judgment in selecting patients for treatment with shared decision-making with patients and families,” the commentators wrote.
The study was supported by the National Institutes of Health, the National Institute on Aging, the Alexander Family Alzheimer’s Disease Research Professorship of the Mayo Clinic, the Mayo Foundation for Medical Education and Research, the Liston Award, the GHR Foundation, and the Schuler Foundation. Dr. Vassilaki disclosed relationships with F. Hoffmann-La Roche, Abbott Laboratories, Johnson & Johnson, Medtronic, Merck, and Amgen. Dr. Howe has no relevant disclosures.
FROM NEUROLOGY
Which factors distinguish superagers from the rest of us?
Even at an advanced age, superagers have the memory of someone 20 or 30 years their junior. But why is that? A new study shows that, in superagers, However, the study also emphasizes the importance of physical and mental fitness for a healthy aging process.
“One of the most important unanswered questions with regard to superagers is: ‘Are they resistant to age-related memory loss, or do they have coping mechanisms that allow them to better offset this memory loss?’ ” wrote Marta Garo-Pascual, a PhD candidate at the Autonomous University of Madrid, Spain, and colleagues in the Lancet Healthy Longevity. “Our results indicate that superagers are resistant to these processes.”
Six years’ monitoring
From a cohort of older adults who had participated in a study aiming to identify early indicators of Alzheimer’s disease, the research group chose 64 superagers and 55 normal senior citizens. The latter served as the control group. While the superagers performed just as well in a memory test as people 30 years their junior, the control group’s performance was in line with their age and level of education.
All study participants were over age 79 years. Both the group of superagers and the control group included more females than males. On average, they were monitored for 6 years. During this period, a checkup was scheduled annually with an MRI examination, clinical tests, blood tests, and documentation of lifestyle factors.
For Alessandro Cellerino, PhD, of the Leibniz Institute on Aging–Fritz Lipmann Institute in Jena, Germany, this is the most crucial aspect of the study. “Even before this study, we knew that superagers demonstrated less atrophy in certain areas of the brain, but this was always only ever based on a single measurement.”
Memory centers protected
The MRI examinations confirmed that in superagers, gray matter atrophy in the regions responsible for memory (such as the medial temporal lobe and cholinergic forebrain), as well in regions important for movement (such as the motor thalamus), was less pronounced. In addition, the volume of gray matter in these regions, especially in the medial temporal lobe, decreased much more slowly in the superagers than in the control subjects over the study period.
Ms. Garo-Pascual and associates used a machine-learning algorithm to differentiate between superagers and normal older adults. From the 89 demographic, lifestyle, and clinical factors entered into the algorithm, two were the most important for the classification: the ability to move and mental health.
Mobility and mental health
Clinical tests such as the Timed Up-and-Go Test and the Finger Tapping Test revealed that superagers can be distinguished from the normally aging control subjects with regard to their mobility and fine motor skills. Their physical condition was better, although they, by their own admission, did not move any more than the control subjects in day-to-day life. According to Dr. Cellerino, this finding confirms that physical activity is paramount for cognitive function. “These people were over 80 years old – the fact that there was not much difference between their levels of activity is not surprising. Much more relevant is the question of how you get there – i.e., how active you are at the ages of 40, 50 or even 60 years old.”
Remaining active is important
As a matter of fact, the superagers indicated that generally they had been more active than the control subjects during their middle years. “Attempting to stay physically fit is essential; even if it just means going for a walk or taking the stairs,” said Dr. Cellerino.
On average, the superagers also fared much better in tests on physical health than the control subjects. They suffered significantly less from depression or anxiety disorders. “Earlier studies suggest that depression and anxiety disorders may influence performance in memory tests across all ages and that they are risk factors for developing dementia,” said Dr. Cellerino.
To avoid mental health issues in later life, gerontologist Dr. Cellerino recommended remaining socially engaged and involved. “Depression and anxiety are commonly also a consequence of social isolation,” he said.
Potential genetic differences
Blood sample analyses demonstrated that the superagers exhibited lower concentrations of biomarkers for neurodegenerative diseases than the control group did. In contrast, there was no difference between the two groups in the prevalence of the apo e4 allele, one of the most important genetic risk factors for Alzheimer’s disease. Nevertheless, Ms. Garo-Pascual and associates assume that genetics also play a role. They found that, despite 89 variables employed, the algorithm used could only distinguish superagers from normal older adults 66% of the time. This suggests that additional factors must be in play, such as genetic differences.
Body and mind
Since this is an observational study, whether the determined factors have a direct effect on superaging cannot be ascertained, the authors wrote. However, the results are consistent with earlier findings.
“Regarding the management of old age, we actually haven’t learned anything more than what we already knew. But it does confirm that physical and mental function are closely entwined and that we must maintain both to age healthily,” Dr. Cellerino concluded.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
Even at an advanced age, superagers have the memory of someone 20 or 30 years their junior. But why is that? A new study shows that, in superagers, However, the study also emphasizes the importance of physical and mental fitness for a healthy aging process.
“One of the most important unanswered questions with regard to superagers is: ‘Are they resistant to age-related memory loss, or do they have coping mechanisms that allow them to better offset this memory loss?’ ” wrote Marta Garo-Pascual, a PhD candidate at the Autonomous University of Madrid, Spain, and colleagues in the Lancet Healthy Longevity. “Our results indicate that superagers are resistant to these processes.”
Six years’ monitoring
From a cohort of older adults who had participated in a study aiming to identify early indicators of Alzheimer’s disease, the research group chose 64 superagers and 55 normal senior citizens. The latter served as the control group. While the superagers performed just as well in a memory test as people 30 years their junior, the control group’s performance was in line with their age and level of education.
All study participants were over age 79 years. Both the group of superagers and the control group included more females than males. On average, they were monitored for 6 years. During this period, a checkup was scheduled annually with an MRI examination, clinical tests, blood tests, and documentation of lifestyle factors.
For Alessandro Cellerino, PhD, of the Leibniz Institute on Aging–Fritz Lipmann Institute in Jena, Germany, this is the most crucial aspect of the study. “Even before this study, we knew that superagers demonstrated less atrophy in certain areas of the brain, but this was always only ever based on a single measurement.”
Memory centers protected
The MRI examinations confirmed that in superagers, gray matter atrophy in the regions responsible for memory (such as the medial temporal lobe and cholinergic forebrain), as well in regions important for movement (such as the motor thalamus), was less pronounced. In addition, the volume of gray matter in these regions, especially in the medial temporal lobe, decreased much more slowly in the superagers than in the control subjects over the study period.
Ms. Garo-Pascual and associates used a machine-learning algorithm to differentiate between superagers and normal older adults. From the 89 demographic, lifestyle, and clinical factors entered into the algorithm, two were the most important for the classification: the ability to move and mental health.
Mobility and mental health
Clinical tests such as the Timed Up-and-Go Test and the Finger Tapping Test revealed that superagers can be distinguished from the normally aging control subjects with regard to their mobility and fine motor skills. Their physical condition was better, although they, by their own admission, did not move any more than the control subjects in day-to-day life. According to Dr. Cellerino, this finding confirms that physical activity is paramount for cognitive function. “These people were over 80 years old – the fact that there was not much difference between their levels of activity is not surprising. Much more relevant is the question of how you get there – i.e., how active you are at the ages of 40, 50 or even 60 years old.”
Remaining active is important
As a matter of fact, the superagers indicated that generally they had been more active than the control subjects during their middle years. “Attempting to stay physically fit is essential; even if it just means going for a walk or taking the stairs,” said Dr. Cellerino.
On average, the superagers also fared much better in tests on physical health than the control subjects. They suffered significantly less from depression or anxiety disorders. “Earlier studies suggest that depression and anxiety disorders may influence performance in memory tests across all ages and that they are risk factors for developing dementia,” said Dr. Cellerino.
To avoid mental health issues in later life, gerontologist Dr. Cellerino recommended remaining socially engaged and involved. “Depression and anxiety are commonly also a consequence of social isolation,” he said.
Potential genetic differences
Blood sample analyses demonstrated that the superagers exhibited lower concentrations of biomarkers for neurodegenerative diseases than the control group did. In contrast, there was no difference between the two groups in the prevalence of the apo e4 allele, one of the most important genetic risk factors for Alzheimer’s disease. Nevertheless, Ms. Garo-Pascual and associates assume that genetics also play a role. They found that, despite 89 variables employed, the algorithm used could only distinguish superagers from normal older adults 66% of the time. This suggests that additional factors must be in play, such as genetic differences.
Body and mind
Since this is an observational study, whether the determined factors have a direct effect on superaging cannot be ascertained, the authors wrote. However, the results are consistent with earlier findings.
“Regarding the management of old age, we actually haven’t learned anything more than what we already knew. But it does confirm that physical and mental function are closely entwined and that we must maintain both to age healthily,” Dr. Cellerino concluded.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
Even at an advanced age, superagers have the memory of someone 20 or 30 years their junior. But why is that? A new study shows that, in superagers, However, the study also emphasizes the importance of physical and mental fitness for a healthy aging process.
“One of the most important unanswered questions with regard to superagers is: ‘Are they resistant to age-related memory loss, or do they have coping mechanisms that allow them to better offset this memory loss?’ ” wrote Marta Garo-Pascual, a PhD candidate at the Autonomous University of Madrid, Spain, and colleagues in the Lancet Healthy Longevity. “Our results indicate that superagers are resistant to these processes.”
Six years’ monitoring
From a cohort of older adults who had participated in a study aiming to identify early indicators of Alzheimer’s disease, the research group chose 64 superagers and 55 normal senior citizens. The latter served as the control group. While the superagers performed just as well in a memory test as people 30 years their junior, the control group’s performance was in line with their age and level of education.
All study participants were over age 79 years. Both the group of superagers and the control group included more females than males. On average, they were monitored for 6 years. During this period, a checkup was scheduled annually with an MRI examination, clinical tests, blood tests, and documentation of lifestyle factors.
For Alessandro Cellerino, PhD, of the Leibniz Institute on Aging–Fritz Lipmann Institute in Jena, Germany, this is the most crucial aspect of the study. “Even before this study, we knew that superagers demonstrated less atrophy in certain areas of the brain, but this was always only ever based on a single measurement.”
Memory centers protected
The MRI examinations confirmed that in superagers, gray matter atrophy in the regions responsible for memory (such as the medial temporal lobe and cholinergic forebrain), as well in regions important for movement (such as the motor thalamus), was less pronounced. In addition, the volume of gray matter in these regions, especially in the medial temporal lobe, decreased much more slowly in the superagers than in the control subjects over the study period.
Ms. Garo-Pascual and associates used a machine-learning algorithm to differentiate between superagers and normal older adults. From the 89 demographic, lifestyle, and clinical factors entered into the algorithm, two were the most important for the classification: the ability to move and mental health.
Mobility and mental health
Clinical tests such as the Timed Up-and-Go Test and the Finger Tapping Test revealed that superagers can be distinguished from the normally aging control subjects with regard to their mobility and fine motor skills. Their physical condition was better, although they, by their own admission, did not move any more than the control subjects in day-to-day life. According to Dr. Cellerino, this finding confirms that physical activity is paramount for cognitive function. “These people were over 80 years old – the fact that there was not much difference between their levels of activity is not surprising. Much more relevant is the question of how you get there – i.e., how active you are at the ages of 40, 50 or even 60 years old.”
Remaining active is important
As a matter of fact, the superagers indicated that generally they had been more active than the control subjects during their middle years. “Attempting to stay physically fit is essential; even if it just means going for a walk or taking the stairs,” said Dr. Cellerino.
On average, the superagers also fared much better in tests on physical health than the control subjects. They suffered significantly less from depression or anxiety disorders. “Earlier studies suggest that depression and anxiety disorders may influence performance in memory tests across all ages and that they are risk factors for developing dementia,” said Dr. Cellerino.
To avoid mental health issues in later life, gerontologist Dr. Cellerino recommended remaining socially engaged and involved. “Depression and anxiety are commonly also a consequence of social isolation,” he said.
Potential genetic differences
Blood sample analyses demonstrated that the superagers exhibited lower concentrations of biomarkers for neurodegenerative diseases than the control group did. In contrast, there was no difference between the two groups in the prevalence of the apo e4 allele, one of the most important genetic risk factors for Alzheimer’s disease. Nevertheless, Ms. Garo-Pascual and associates assume that genetics also play a role. They found that, despite 89 variables employed, the algorithm used could only distinguish superagers from normal older adults 66% of the time. This suggests that additional factors must be in play, such as genetic differences.
Body and mind
Since this is an observational study, whether the determined factors have a direct effect on superaging cannot be ascertained, the authors wrote. However, the results are consistent with earlier findings.
“Regarding the management of old age, we actually haven’t learned anything more than what we already knew. But it does confirm that physical and mental function are closely entwined and that we must maintain both to age healthily,” Dr. Cellerino concluded.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
FROM THE LANCET HEALTHY LONGEVITY
‘Emerging’ biomarker may predict mild cognitive impairment years before symptoms
, new research indicates.
“Our study shows that low NPTX2 levels are predictive of MCI symptom onset more than 7 years in advance, including among individuals who are in late middle age,” said study investigator Anja Soldan, PhD, associate professor of neurology, Johns Hopkins University School of Medicine, Baltimore.
NPTX2 is still considered an “emerging biomarker” because knowledge about this protein is limited, Dr. Soldan noted.
Prior studies have shown that levels of NPTX2 are lower in people with MCI and dementia than in those with normal cognition and that low levels of this protein in people with MCI are associated with an increased risk of developing dementia.
“Our study extends these prior findings by showing that low protein levels are also associated with the onset of MCI symptoms,” Dr. Soldan said.
The study was published online in Annals of Neurology.
New therapeutic target?
The researchers measured NPTX2, as well as amyloid beta 42/40, phosphorylated (p)-tau181, and total (t)-tau in CSF collected longitudinally from 269 cognitively normal adults from the BIOCARD study.
The average age at baseline was 57.7 years. Nearly all were White, 59% were women, most were college educated, and three-quarters had a close relative with Alzheimer’s disease.
During a mean follow-up average of 16 years, 77 participants progressed to MCI or dementia within or after 7 years of baseline measurements.
In Cox regression models, lower baseline NPTX2 levels were associated with an earlier time to MCI symptom onset (hazard ratio, 0.76; P = .023). This association was significant for progression within 7 years (P = .036) and after 7 years from baseline (P = .001), the investigators reported.
Adults who progressed to MCI had, on average, about 15% lower levels of NPTX2 at baseline, compared with adults who remained cognitively normal.
Baseline NPTX2 levels improved prediction of time to MCI symptom onset after accounting for baseline Alzheimer’s disease biomarker levels (P < .01), and NPTX2 did not interact with the CSF Alzheimer’s disease biomarkers or APOE-ε4 genetic status.
Higher baseline levels of p-tau181 and t-tau were associated with higher baseline NPTX2 levels (both P < .001) and with greater declines in NPTX2 over time, suggesting that NPTX2 may decline in response to tau pathology, the investigators suggested.
Dr. Soldan said NPTX2 may be “a novel target” for developing new therapeutics for Alzheimer’s disease and other dementing and neurodegenerative disorders, as it is not an Alzheimer’s disease–specific protein.
“Efforts are underway for developing a sensitive way to measure NPTX2 brain levels in blood, which could then help clinicians identify individuals at greatest risk for cognitive decline,” she explained.
“Other next steps are to examine how changes in NPTX2 over time relate to changes in brain structure and function and to identify factors that alter levels of NPTX2, including genetic factors and potentially modifiable lifestyle factors,” Dr. Soldan said.
“If having higher levels of NPTX2 in the brain provides some resilience against developing symptoms of Alzheimer’s disease, it would be great if we could somehow increase levels of the protein,” she noted.
Caveats, cautionary notes
Commenting on this research, Christopher Weber, PhD, Alzheimer’s Association director of global science initiatives, said, “Research has shown that when NPTX2 levels are low, it may lead to weaker connections between neurons and could potentially affect cognitive functions, including memory and learning.”
“This new study found an association between lower levels of NPTX2 in CSF and earlier time to MCI symptom onset, and when combined with other established Alzheimer’s biomarkers, they found that NPTX2 improved the prediction of Alzheimer’s symptom onset,” Dr. Weber said.
“This is in line with previous research that suggests NPTX2 levels are associated with an increased risk of progression from MCI to Alzheimer’s dementia,” Dr. Weber said.
However, he noted some limitations of the study. “Participants were primarily White [and] highly educated, and therefore findings may not be generalizable to a real-world population,” he cautioned.
Dr. Weber said it’s also important to note that NPTX2 is not considered an Alzheimer’s-specific biomarker but rather a marker of synaptic activity and neurodegeneration. “The exact role of NPTX2 in predicting dementia is unknown,” Dr. Weber said.
He said that more studies with larger, more diverse cohorts are needed to fully understand its significance as a biomarker or therapeutic target for neurodegenerative diseases, as well as to develop a blood test for NPTX2.
The study was supported by the National Institutes of Health. Dr. Soldan and Dr. Weber report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research indicates.
“Our study shows that low NPTX2 levels are predictive of MCI symptom onset more than 7 years in advance, including among individuals who are in late middle age,” said study investigator Anja Soldan, PhD, associate professor of neurology, Johns Hopkins University School of Medicine, Baltimore.
NPTX2 is still considered an “emerging biomarker” because knowledge about this protein is limited, Dr. Soldan noted.
Prior studies have shown that levels of NPTX2 are lower in people with MCI and dementia than in those with normal cognition and that low levels of this protein in people with MCI are associated with an increased risk of developing dementia.
“Our study extends these prior findings by showing that low protein levels are also associated with the onset of MCI symptoms,” Dr. Soldan said.
The study was published online in Annals of Neurology.
New therapeutic target?
The researchers measured NPTX2, as well as amyloid beta 42/40, phosphorylated (p)-tau181, and total (t)-tau in CSF collected longitudinally from 269 cognitively normal adults from the BIOCARD study.
The average age at baseline was 57.7 years. Nearly all were White, 59% were women, most were college educated, and three-quarters had a close relative with Alzheimer’s disease.
During a mean follow-up average of 16 years, 77 participants progressed to MCI or dementia within or after 7 years of baseline measurements.
In Cox regression models, lower baseline NPTX2 levels were associated with an earlier time to MCI symptom onset (hazard ratio, 0.76; P = .023). This association was significant for progression within 7 years (P = .036) and after 7 years from baseline (P = .001), the investigators reported.
Adults who progressed to MCI had, on average, about 15% lower levels of NPTX2 at baseline, compared with adults who remained cognitively normal.
Baseline NPTX2 levels improved prediction of time to MCI symptom onset after accounting for baseline Alzheimer’s disease biomarker levels (P < .01), and NPTX2 did not interact with the CSF Alzheimer’s disease biomarkers or APOE-ε4 genetic status.
Higher baseline levels of p-tau181 and t-tau were associated with higher baseline NPTX2 levels (both P < .001) and with greater declines in NPTX2 over time, suggesting that NPTX2 may decline in response to tau pathology, the investigators suggested.
Dr. Soldan said NPTX2 may be “a novel target” for developing new therapeutics for Alzheimer’s disease and other dementing and neurodegenerative disorders, as it is not an Alzheimer’s disease–specific protein.
“Efforts are underway for developing a sensitive way to measure NPTX2 brain levels in blood, which could then help clinicians identify individuals at greatest risk for cognitive decline,” she explained.
“Other next steps are to examine how changes in NPTX2 over time relate to changes in brain structure and function and to identify factors that alter levels of NPTX2, including genetic factors and potentially modifiable lifestyle factors,” Dr. Soldan said.
“If having higher levels of NPTX2 in the brain provides some resilience against developing symptoms of Alzheimer’s disease, it would be great if we could somehow increase levels of the protein,” she noted.
Caveats, cautionary notes
Commenting on this research, Christopher Weber, PhD, Alzheimer’s Association director of global science initiatives, said, “Research has shown that when NPTX2 levels are low, it may lead to weaker connections between neurons and could potentially affect cognitive functions, including memory and learning.”
“This new study found an association between lower levels of NPTX2 in CSF and earlier time to MCI symptom onset, and when combined with other established Alzheimer’s biomarkers, they found that NPTX2 improved the prediction of Alzheimer’s symptom onset,” Dr. Weber said.
“This is in line with previous research that suggests NPTX2 levels are associated with an increased risk of progression from MCI to Alzheimer’s dementia,” Dr. Weber said.
However, he noted some limitations of the study. “Participants were primarily White [and] highly educated, and therefore findings may not be generalizable to a real-world population,” he cautioned.
Dr. Weber said it’s also important to note that NPTX2 is not considered an Alzheimer’s-specific biomarker but rather a marker of synaptic activity and neurodegeneration. “The exact role of NPTX2 in predicting dementia is unknown,” Dr. Weber said.
He said that more studies with larger, more diverse cohorts are needed to fully understand its significance as a biomarker or therapeutic target for neurodegenerative diseases, as well as to develop a blood test for NPTX2.
The study was supported by the National Institutes of Health. Dr. Soldan and Dr. Weber report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research indicates.
“Our study shows that low NPTX2 levels are predictive of MCI symptom onset more than 7 years in advance, including among individuals who are in late middle age,” said study investigator Anja Soldan, PhD, associate professor of neurology, Johns Hopkins University School of Medicine, Baltimore.
NPTX2 is still considered an “emerging biomarker” because knowledge about this protein is limited, Dr. Soldan noted.
Prior studies have shown that levels of NPTX2 are lower in people with MCI and dementia than in those with normal cognition and that low levels of this protein in people with MCI are associated with an increased risk of developing dementia.
“Our study extends these prior findings by showing that low protein levels are also associated with the onset of MCI symptoms,” Dr. Soldan said.
The study was published online in Annals of Neurology.
New therapeutic target?
The researchers measured NPTX2, as well as amyloid beta 42/40, phosphorylated (p)-tau181, and total (t)-tau in CSF collected longitudinally from 269 cognitively normal adults from the BIOCARD study.
The average age at baseline was 57.7 years. Nearly all were White, 59% were women, most were college educated, and three-quarters had a close relative with Alzheimer’s disease.
During a mean follow-up average of 16 years, 77 participants progressed to MCI or dementia within or after 7 years of baseline measurements.
In Cox regression models, lower baseline NPTX2 levels were associated with an earlier time to MCI symptom onset (hazard ratio, 0.76; P = .023). This association was significant for progression within 7 years (P = .036) and after 7 years from baseline (P = .001), the investigators reported.
Adults who progressed to MCI had, on average, about 15% lower levels of NPTX2 at baseline, compared with adults who remained cognitively normal.
Baseline NPTX2 levels improved prediction of time to MCI symptom onset after accounting for baseline Alzheimer’s disease biomarker levels (P < .01), and NPTX2 did not interact with the CSF Alzheimer’s disease biomarkers or APOE-ε4 genetic status.
Higher baseline levels of p-tau181 and t-tau were associated with higher baseline NPTX2 levels (both P < .001) and with greater declines in NPTX2 over time, suggesting that NPTX2 may decline in response to tau pathology, the investigators suggested.
Dr. Soldan said NPTX2 may be “a novel target” for developing new therapeutics for Alzheimer’s disease and other dementing and neurodegenerative disorders, as it is not an Alzheimer’s disease–specific protein.
“Efforts are underway for developing a sensitive way to measure NPTX2 brain levels in blood, which could then help clinicians identify individuals at greatest risk for cognitive decline,” she explained.
“Other next steps are to examine how changes in NPTX2 over time relate to changes in brain structure and function and to identify factors that alter levels of NPTX2, including genetic factors and potentially modifiable lifestyle factors,” Dr. Soldan said.
“If having higher levels of NPTX2 in the brain provides some resilience against developing symptoms of Alzheimer’s disease, it would be great if we could somehow increase levels of the protein,” she noted.
Caveats, cautionary notes
Commenting on this research, Christopher Weber, PhD, Alzheimer’s Association director of global science initiatives, said, “Research has shown that when NPTX2 levels are low, it may lead to weaker connections between neurons and could potentially affect cognitive functions, including memory and learning.”
“This new study found an association between lower levels of NPTX2 in CSF and earlier time to MCI symptom onset, and when combined with other established Alzheimer’s biomarkers, they found that NPTX2 improved the prediction of Alzheimer’s symptom onset,” Dr. Weber said.
“This is in line with previous research that suggests NPTX2 levels are associated with an increased risk of progression from MCI to Alzheimer’s dementia,” Dr. Weber said.
However, he noted some limitations of the study. “Participants were primarily White [and] highly educated, and therefore findings may not be generalizable to a real-world population,” he cautioned.
Dr. Weber said it’s also important to note that NPTX2 is not considered an Alzheimer’s-specific biomarker but rather a marker of synaptic activity and neurodegeneration. “The exact role of NPTX2 in predicting dementia is unknown,” Dr. Weber said.
He said that more studies with larger, more diverse cohorts are needed to fully understand its significance as a biomarker or therapeutic target for neurodegenerative diseases, as well as to develop a blood test for NPTX2.
The study was supported by the National Institutes of Health. Dr. Soldan and Dr. Weber report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF NEUROLOGY