User login
Drug granted priority review, breakthrough designation for ECD
The US Food and Drug Administration (FDA) has granted priority review and breakthrough therapy designation to vemurafenib (Zelboraf®) as a treatment for Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug is already FDA-approved to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation as detected by an FDA-approved test.
The FDA is expected to make a decision on the approval of vemurafenib in ECD by December 7, 2017.
The supplemental new drug application for vemurafenib in this indication is supported by data from the phase 2 VE-BASKET study.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
Final results for the 22 people with ECD showed a best overall response rate of 54.5%. The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events were joint pain, rash, hair loss, change in heart rhythm, fatigue, skin tags, diarrhea, and thickening of the skin. The most common grade 3 or higher adverse events were new skin cancers, high blood pressure, rash, and joint pain.
Initial results from this study were published in NEJM in August 2015.
About priority review
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted priority review and breakthrough therapy designation to vemurafenib (Zelboraf®) as a treatment for Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug is already FDA-approved to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation as detected by an FDA-approved test.
The FDA is expected to make a decision on the approval of vemurafenib in ECD by December 7, 2017.
The supplemental new drug application for vemurafenib in this indication is supported by data from the phase 2 VE-BASKET study.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
Final results for the 22 people with ECD showed a best overall response rate of 54.5%. The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events were joint pain, rash, hair loss, change in heart rhythm, fatigue, skin tags, diarrhea, and thickening of the skin. The most common grade 3 or higher adverse events were new skin cancers, high blood pressure, rash, and joint pain.
Initial results from this study were published in NEJM in August 2015.
About priority review
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
The US Food and Drug Administration (FDA) has granted priority review and breakthrough therapy designation to vemurafenib (Zelboraf®) as a treatment for Erdheim-Chester disease (ECD) with BRAF V600 mutation.
Vemurafenib is a kinase inhibitor designed to inhibit some mutated forms of BRAF.
The drug is already FDA-approved to treat patients with unresectable or metastatic melanoma with BRAF V600E mutation as detected by an FDA-approved test.
The FDA is expected to make a decision on the approval of vemurafenib in ECD by December 7, 2017.
The supplemental new drug application for vemurafenib in this indication is supported by data from the phase 2 VE-BASKET study.
VE-BASKET was designed to investigate the use of vemurafenib in patients with BRAF V600 mutation-positive diseases, including ECD.
Final results for the 22 people with ECD showed a best overall response rate of 54.5%. The median duration of response, progression-free survival, and overall survival were not reached at a median follow-up of 26.6 months.
The most common adverse events were joint pain, rash, hair loss, change in heart rhythm, fatigue, skin tags, diarrhea, and thickening of the skin. The most common grade 3 or higher adverse events were new skin cancers, high blood pressure, rash, and joint pain.
Initial results from this study were published in NEJM in August 2015.
About priority review
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
About breakthrough designation
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need. ![]()
Long-term maintenance deemed feasible in PV
MADRID—Long-term maintenance with ropeginterferon alfa-2b is feasible, effective, and well-tolerated in patients with polycythemia vera (PV), according to researchers.
In the ongoing phase 1/2 PEGINVERA study, patients have received ropeginterferon alfa-2b for a median of 4 years.
After the first 2 years, patients switched from bi-weekly dosing to receiving ropeginterferon alfa-2b once every 4 weeks.
None of the patients discontinued treatment after the switch, and many were able to maintain their best response.
Most adverse events (AEs) were mild, although there were several severe treatment-related AEs.
These results were presented in a poster (abstract P707) at the 22nd Congress of the European Hematology Association (EHA). The research was funded by AOP Orphan Pharmaceuticals AG.
The trial enrolled 51 patients, but the researchers reported results in the 29 patients who had completed 2 years of treatment and switched from bi-weekly dosing to receiving treatment once every 4 weeks.
All 29 patients remained on the 4-week schedule with a median observation period of roughly 2 years. The median monthly dose was 308 μg before the switch and 165 μg after.
At study entry, the patients’ median age was 58 (range, 40-80), and 76% were male. Their median spleen length was 12.8 cm (range, 8.0-22.0), and 34% of patients had prior treatment with hydroxyurea.
Patients’ median hematocrit was 45.40% (range, 36.9-53.8), their median platelet count was 431 G/L (range, 225-1016), their median leukocyte count was 11.1 G/L (range, 4.7-30.9), and their median JAKV617F allelic burden was 78% (range, 2-91.5).
Results
More than 80% of patients achieved a hematologic response, with more than 50% achieving a complete hematologic response. The same percentage of patients maintained their best hematologic response before and 6 months after switching to the 4-week schedule—51.7%.
More than 80% of patients achieved a molecular response, with nearly 20% achieving a complete molecular response. The percentage of patients maintaining their best molecular response was 62.1% before switching to the 4-week schedule and 58.6% 6 months after the switch.
The researchers said changes in hematocrit, platelet count, leukocyte count, and spleen size after the switch were “minimal and without clinical relevance.”
The median hematocrit changed from 42.3% to 42.6%, the median platelet count changed from 201.0 x 109/L to 211.9 x 109/L, the median leukocyte count changed from 5.0 x 109/L to 5.6 x 109/L, and the median spleen size changed from 12.8 cm to 12.4 cm.
The need for phlebotomy did not change, with 24.1% of patients requiring phlebotomy both before and 6 months after the switch.
The researchers also noted that ropeginterferon alfa-2b decreased mutant JAK2 allele burden in all of the patients over time, with the strongest effect observed in the second year of treatment.
After 2 years, most patients had a burden below 10%, and this was not affected by the change in dosing.
There were no cases of progression to myelofibrosis or leukemic transformation.
Seventy-one percent of AEs were mild, and 40.4% were considered likely related to ropeginterferon alfa-2b. The most frequent treatment-related AEs were arthralgia (29.4%) and fatigue (21.6%).
There were 34 severe AEs, 11 of which were related to ropeginterferon alfa-2b. ![]()
MADRID—Long-term maintenance with ropeginterferon alfa-2b is feasible, effective, and well-tolerated in patients with polycythemia vera (PV), according to researchers.
In the ongoing phase 1/2 PEGINVERA study, patients have received ropeginterferon alfa-2b for a median of 4 years.
After the first 2 years, patients switched from bi-weekly dosing to receiving ropeginterferon alfa-2b once every 4 weeks.
None of the patients discontinued treatment after the switch, and many were able to maintain their best response.
Most adverse events (AEs) were mild, although there were several severe treatment-related AEs.
These results were presented in a poster (abstract P707) at the 22nd Congress of the European Hematology Association (EHA). The research was funded by AOP Orphan Pharmaceuticals AG.
The trial enrolled 51 patients, but the researchers reported results in the 29 patients who had completed 2 years of treatment and switched from bi-weekly dosing to receiving treatment once every 4 weeks.
All 29 patients remained on the 4-week schedule with a median observation period of roughly 2 years. The median monthly dose was 308 μg before the switch and 165 μg after.
At study entry, the patients’ median age was 58 (range, 40-80), and 76% were male. Their median spleen length was 12.8 cm (range, 8.0-22.0), and 34% of patients had prior treatment with hydroxyurea.
Patients’ median hematocrit was 45.40% (range, 36.9-53.8), their median platelet count was 431 G/L (range, 225-1016), their median leukocyte count was 11.1 G/L (range, 4.7-30.9), and their median JAKV617F allelic burden was 78% (range, 2-91.5).
Results
More than 80% of patients achieved a hematologic response, with more than 50% achieving a complete hematologic response. The same percentage of patients maintained their best hematologic response before and 6 months after switching to the 4-week schedule—51.7%.
More than 80% of patients achieved a molecular response, with nearly 20% achieving a complete molecular response. The percentage of patients maintaining their best molecular response was 62.1% before switching to the 4-week schedule and 58.6% 6 months after the switch.
The researchers said changes in hematocrit, platelet count, leukocyte count, and spleen size after the switch were “minimal and without clinical relevance.”
The median hematocrit changed from 42.3% to 42.6%, the median platelet count changed from 201.0 x 109/L to 211.9 x 109/L, the median leukocyte count changed from 5.0 x 109/L to 5.6 x 109/L, and the median spleen size changed from 12.8 cm to 12.4 cm.
The need for phlebotomy did not change, with 24.1% of patients requiring phlebotomy both before and 6 months after the switch.
The researchers also noted that ropeginterferon alfa-2b decreased mutant JAK2 allele burden in all of the patients over time, with the strongest effect observed in the second year of treatment.
After 2 years, most patients had a burden below 10%, and this was not affected by the change in dosing.
There were no cases of progression to myelofibrosis or leukemic transformation.
Seventy-one percent of AEs were mild, and 40.4% were considered likely related to ropeginterferon alfa-2b. The most frequent treatment-related AEs were arthralgia (29.4%) and fatigue (21.6%).
There were 34 severe AEs, 11 of which were related to ropeginterferon alfa-2b. ![]()
MADRID—Long-term maintenance with ropeginterferon alfa-2b is feasible, effective, and well-tolerated in patients with polycythemia vera (PV), according to researchers.
In the ongoing phase 1/2 PEGINVERA study, patients have received ropeginterferon alfa-2b for a median of 4 years.
After the first 2 years, patients switched from bi-weekly dosing to receiving ropeginterferon alfa-2b once every 4 weeks.
None of the patients discontinued treatment after the switch, and many were able to maintain their best response.
Most adverse events (AEs) were mild, although there were several severe treatment-related AEs.
These results were presented in a poster (abstract P707) at the 22nd Congress of the European Hematology Association (EHA). The research was funded by AOP Orphan Pharmaceuticals AG.
The trial enrolled 51 patients, but the researchers reported results in the 29 patients who had completed 2 years of treatment and switched from bi-weekly dosing to receiving treatment once every 4 weeks.
All 29 patients remained on the 4-week schedule with a median observation period of roughly 2 years. The median monthly dose was 308 μg before the switch and 165 μg after.
At study entry, the patients’ median age was 58 (range, 40-80), and 76% were male. Their median spleen length was 12.8 cm (range, 8.0-22.0), and 34% of patients had prior treatment with hydroxyurea.
Patients’ median hematocrit was 45.40% (range, 36.9-53.8), their median platelet count was 431 G/L (range, 225-1016), their median leukocyte count was 11.1 G/L (range, 4.7-30.9), and their median JAKV617F allelic burden was 78% (range, 2-91.5).
Results
More than 80% of patients achieved a hematologic response, with more than 50% achieving a complete hematologic response. The same percentage of patients maintained their best hematologic response before and 6 months after switching to the 4-week schedule—51.7%.
More than 80% of patients achieved a molecular response, with nearly 20% achieving a complete molecular response. The percentage of patients maintaining their best molecular response was 62.1% before switching to the 4-week schedule and 58.6% 6 months after the switch.
The researchers said changes in hematocrit, platelet count, leukocyte count, and spleen size after the switch were “minimal and without clinical relevance.”
The median hematocrit changed from 42.3% to 42.6%, the median platelet count changed from 201.0 x 109/L to 211.9 x 109/L, the median leukocyte count changed from 5.0 x 109/L to 5.6 x 109/L, and the median spleen size changed from 12.8 cm to 12.4 cm.
The need for phlebotomy did not change, with 24.1% of patients requiring phlebotomy both before and 6 months after the switch.
The researchers also noted that ropeginterferon alfa-2b decreased mutant JAK2 allele burden in all of the patients over time, with the strongest effect observed in the second year of treatment.
After 2 years, most patients had a burden below 10%, and this was not affected by the change in dosing.
There were no cases of progression to myelofibrosis or leukemic transformation.
Seventy-one percent of AEs were mild, and 40.4% were considered likely related to ropeginterferon alfa-2b. The most frequent treatment-related AEs were arthralgia (29.4%) and fatigue (21.6%).
There were 34 severe AEs, 11 of which were related to ropeginterferon alfa-2b. ![]()
FDA clears use of reagents to detect hematopoietic neoplasia
The US Food and Drug Administration (FDA) has allowed marketing of the ClearLLab Reagent Panel, a combination of conjugated antibody cocktails designed to aid the detection of hematopoietic neoplasia.
This includes chronic and acute leukemias, non-Hodgkin lymphoma, myeloma, myelodysplastic syndromes, and myeloproliferative neoplasms.
The ClearLLab reagents are intended for in vitro diagnostic use to identify various cell populations by immunophenotyping on an FC 500 flow cytometer.
The reagents are directed against B, T, and myeloid lineage antigens and intended to identify relevant leukocyte surface molecules.
ClearLLab provides 2 T-cell tubes, 2 B-cell tubes, and a myeloid tube, each consisting of pre-mixed 4- to 5-color cocktails. Together, this totals 18 markers as directly conjugated antibodies.
The reagents can be used with peripheral whole blood, bone marrow, and lymph node specimens.
The results obtained via testing with the ClearLLab reagents should be interpreted along with additional clinical and laboratory findings, according to Beckman Coulter, Inc., the company that will be marketing the reagents.
The FDA reviewed data for the ClearLLab reagents through the de novo premarket review pathway, a regulatory pathway for novel, low-to-moderate-risk devices that are not substantially equivalent to an already legally marketed device.
The FDA’s clearance of the ClearLLab reagents was supported by a study designed to demonstrate the reagents’ performance, which was conducted on 279 samples at 4 independent clinical sites.
Results with the ClearLLab reagents were compared to results with alternative detection methods used at the sites.
The ClearLLab results aligned with the study sites’ final diagnosis 93.4% of the time and correctly detected abnormalities 84.2% of the time.
Along with its clearance of the ClearLLab reagents, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the reagents’ accuracy, reliability, and clinical relevance.
These special controls, when met along with general controls, provide reasonable assurance of safety and effectiveness for the ClearLLab reagents and similar tools.
The special controls also describe the least burdensome regulatory pathway for future developers of similar diagnostic tests. ![]()
The US Food and Drug Administration (FDA) has allowed marketing of the ClearLLab Reagent Panel, a combination of conjugated antibody cocktails designed to aid the detection of hematopoietic neoplasia.
This includes chronic and acute leukemias, non-Hodgkin lymphoma, myeloma, myelodysplastic syndromes, and myeloproliferative neoplasms.
The ClearLLab reagents are intended for in vitro diagnostic use to identify various cell populations by immunophenotyping on an FC 500 flow cytometer.
The reagents are directed against B, T, and myeloid lineage antigens and intended to identify relevant leukocyte surface molecules.
ClearLLab provides 2 T-cell tubes, 2 B-cell tubes, and a myeloid tube, each consisting of pre-mixed 4- to 5-color cocktails. Together, this totals 18 markers as directly conjugated antibodies.
The reagents can be used with peripheral whole blood, bone marrow, and lymph node specimens.
The results obtained via testing with the ClearLLab reagents should be interpreted along with additional clinical and laboratory findings, according to Beckman Coulter, Inc., the company that will be marketing the reagents.
The FDA reviewed data for the ClearLLab reagents through the de novo premarket review pathway, a regulatory pathway for novel, low-to-moderate-risk devices that are not substantially equivalent to an already legally marketed device.
The FDA’s clearance of the ClearLLab reagents was supported by a study designed to demonstrate the reagents’ performance, which was conducted on 279 samples at 4 independent clinical sites.
Results with the ClearLLab reagents were compared to results with alternative detection methods used at the sites.
The ClearLLab results aligned with the study sites’ final diagnosis 93.4% of the time and correctly detected abnormalities 84.2% of the time.
Along with its clearance of the ClearLLab reagents, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the reagents’ accuracy, reliability, and clinical relevance.
These special controls, when met along with general controls, provide reasonable assurance of safety and effectiveness for the ClearLLab reagents and similar tools.
The special controls also describe the least burdensome regulatory pathway for future developers of similar diagnostic tests. ![]()
The US Food and Drug Administration (FDA) has allowed marketing of the ClearLLab Reagent Panel, a combination of conjugated antibody cocktails designed to aid the detection of hematopoietic neoplasia.
This includes chronic and acute leukemias, non-Hodgkin lymphoma, myeloma, myelodysplastic syndromes, and myeloproliferative neoplasms.
The ClearLLab reagents are intended for in vitro diagnostic use to identify various cell populations by immunophenotyping on an FC 500 flow cytometer.
The reagents are directed against B, T, and myeloid lineage antigens and intended to identify relevant leukocyte surface molecules.
ClearLLab provides 2 T-cell tubes, 2 B-cell tubes, and a myeloid tube, each consisting of pre-mixed 4- to 5-color cocktails. Together, this totals 18 markers as directly conjugated antibodies.
The reagents can be used with peripheral whole blood, bone marrow, and lymph node specimens.
The results obtained via testing with the ClearLLab reagents should be interpreted along with additional clinical and laboratory findings, according to Beckman Coulter, Inc., the company that will be marketing the reagents.
The FDA reviewed data for the ClearLLab reagents through the de novo premarket review pathway, a regulatory pathway for novel, low-to-moderate-risk devices that are not substantially equivalent to an already legally marketed device.
The FDA’s clearance of the ClearLLab reagents was supported by a study designed to demonstrate the reagents’ performance, which was conducted on 279 samples at 4 independent clinical sites.
Results with the ClearLLab reagents were compared to results with alternative detection methods used at the sites.
The ClearLLab results aligned with the study sites’ final diagnosis 93.4% of the time and correctly detected abnormalities 84.2% of the time.
Along with its clearance of the ClearLLab reagents, the FDA is establishing criteria, called special controls, which clarify the agency’s expectations in assuring the reagents’ accuracy, reliability, and clinical relevance.
These special controls, when met along with general controls, provide reasonable assurance of safety and effectiveness for the ClearLLab reagents and similar tools.
The special controls also describe the least burdensome regulatory pathway for future developers of similar diagnostic tests. ![]()
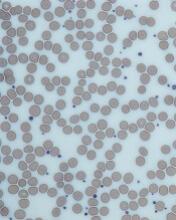
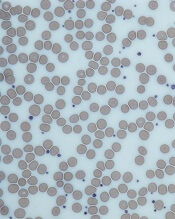
Patients with thrombocytosis should be tested for cancers, team says
Researchers have found evidence to suggest that thrombocytosis is a strong predictor of cancer, particularly lung and colorectal cancer.
The team therefore believes patients with thrombocytosis should be evaluated for an underlying malignancy, as such investigation could speed up cancer diagnosis and save lives.
“We know that early diagnosis is absolutely key in whether people survive cancer,” said Sarah Bailey, PhD, of the University of Exeter Medical School in the UK.
“Our research suggests that substantial numbers of people could have their cancer diagnosed up to 3 months earlier if thrombocytosis prompted investigation for cancer. This time could make a vital difference in achieving earlier diagnosis.”
Dr Bailey and her colleagues described their research in the British Journal of General Practice.
The team conducted a prospective cohort study using Clinical Practice Research Datalink data spanning the period from 2000 to 2013.
They compared the 1-year cancer incidence in 40,000 patients (age 40 and older) with thrombocytosis (platelet count >400 × 109/L) and 10,000 matched controls with normal platelet counts.
Patients with thrombocytosis had a higher incidence of cancer than individuals with normal platelet counts.
The cancer incidence was 6.2% (1355/21,826) in women with thrombocytosis and 2.2% (119/5370) in women with normal platelet counts.
The cancer incidence was 11.6% (1098/9435) in men with thrombocytosis and 4.1% (106/2599) in men with normal platelet counts.
If patients in the thrombocytosis group had a second raised platelet count recorded within 6 months of their index date, the risk of cancer increased to 18.1% for men and 10.1% for women.
Lung and colorectal cancer were more common among patients with thrombocytosis than among individuals with normal platelet counts.
And about one-third of patients with thrombocytosis and lung/colorectal cancer had no other symptoms that would indicate they had cancer.
In addition, the researchers found that “substantial proportions” of lung/colorectal cancer diagnoses could be expedited if thrombocytosis were routinely investigated.
The team calculated that if 5% of patients with cancer have thrombocytosis before a cancer diagnosis, one-third of them have the potential to have their diagnosis expedited by at least 3 months if their doctor investigates the possibility of cancer based on the presence of thrombocytosis. This equates to 5500 earlier diagnoses annually.
“The UK lags well behind other developed countries on early cancer diagnosis,” said study author Willie Hamilton, MD, of the University of Exeter Medical School.
“In 2014, 163,000 people died of cancer in this country. Our findings on thrombocytosis show a strong association with cancer, particularly in men—far stronger than that of a breast lump for breast cancer in women. It is now crucial that we roll out cancer investigation of thrombocytosis. It could save hundreds of lives each year.” ![]()
Researchers have found evidence to suggest that thrombocytosis is a strong predictor of cancer, particularly lung and colorectal cancer.
The team therefore believes patients with thrombocytosis should be evaluated for an underlying malignancy, as such investigation could speed up cancer diagnosis and save lives.
“We know that early diagnosis is absolutely key in whether people survive cancer,” said Sarah Bailey, PhD, of the University of Exeter Medical School in the UK.
“Our research suggests that substantial numbers of people could have their cancer diagnosed up to 3 months earlier if thrombocytosis prompted investigation for cancer. This time could make a vital difference in achieving earlier diagnosis.”
Dr Bailey and her colleagues described their research in the British Journal of General Practice.
The team conducted a prospective cohort study using Clinical Practice Research Datalink data spanning the period from 2000 to 2013.
They compared the 1-year cancer incidence in 40,000 patients (age 40 and older) with thrombocytosis (platelet count >400 × 109/L) and 10,000 matched controls with normal platelet counts.
Patients with thrombocytosis had a higher incidence of cancer than individuals with normal platelet counts.
The cancer incidence was 6.2% (1355/21,826) in women with thrombocytosis and 2.2% (119/5370) in women with normal platelet counts.
The cancer incidence was 11.6% (1098/9435) in men with thrombocytosis and 4.1% (106/2599) in men with normal platelet counts.
If patients in the thrombocytosis group had a second raised platelet count recorded within 6 months of their index date, the risk of cancer increased to 18.1% for men and 10.1% for women.
Lung and colorectal cancer were more common among patients with thrombocytosis than among individuals with normal platelet counts.
And about one-third of patients with thrombocytosis and lung/colorectal cancer had no other symptoms that would indicate they had cancer.
In addition, the researchers found that “substantial proportions” of lung/colorectal cancer diagnoses could be expedited if thrombocytosis were routinely investigated.
The team calculated that if 5% of patients with cancer have thrombocytosis before a cancer diagnosis, one-third of them have the potential to have their diagnosis expedited by at least 3 months if their doctor investigates the possibility of cancer based on the presence of thrombocytosis. This equates to 5500 earlier diagnoses annually.
“The UK lags well behind other developed countries on early cancer diagnosis,” said study author Willie Hamilton, MD, of the University of Exeter Medical School.
“In 2014, 163,000 people died of cancer in this country. Our findings on thrombocytosis show a strong association with cancer, particularly in men—far stronger than that of a breast lump for breast cancer in women. It is now crucial that we roll out cancer investigation of thrombocytosis. It could save hundreds of lives each year.” ![]()
Researchers have found evidence to suggest that thrombocytosis is a strong predictor of cancer, particularly lung and colorectal cancer.
The team therefore believes patients with thrombocytosis should be evaluated for an underlying malignancy, as such investigation could speed up cancer diagnosis and save lives.
“We know that early diagnosis is absolutely key in whether people survive cancer,” said Sarah Bailey, PhD, of the University of Exeter Medical School in the UK.
“Our research suggests that substantial numbers of people could have their cancer diagnosed up to 3 months earlier if thrombocytosis prompted investigation for cancer. This time could make a vital difference in achieving earlier diagnosis.”
Dr Bailey and her colleagues described their research in the British Journal of General Practice.
The team conducted a prospective cohort study using Clinical Practice Research Datalink data spanning the period from 2000 to 2013.
They compared the 1-year cancer incidence in 40,000 patients (age 40 and older) with thrombocytosis (platelet count >400 × 109/L) and 10,000 matched controls with normal platelet counts.
Patients with thrombocytosis had a higher incidence of cancer than individuals with normal platelet counts.
The cancer incidence was 6.2% (1355/21,826) in women with thrombocytosis and 2.2% (119/5370) in women with normal platelet counts.
The cancer incidence was 11.6% (1098/9435) in men with thrombocytosis and 4.1% (106/2599) in men with normal platelet counts.
If patients in the thrombocytosis group had a second raised platelet count recorded within 6 months of their index date, the risk of cancer increased to 18.1% for men and 10.1% for women.
Lung and colorectal cancer were more common among patients with thrombocytosis than among individuals with normal platelet counts.
And about one-third of patients with thrombocytosis and lung/colorectal cancer had no other symptoms that would indicate they had cancer.
In addition, the researchers found that “substantial proportions” of lung/colorectal cancer diagnoses could be expedited if thrombocytosis were routinely investigated.
The team calculated that if 5% of patients with cancer have thrombocytosis before a cancer diagnosis, one-third of them have the potential to have their diagnosis expedited by at least 3 months if their doctor investigates the possibility of cancer based on the presence of thrombocytosis. This equates to 5500 earlier diagnoses annually.
“The UK lags well behind other developed countries on early cancer diagnosis,” said study author Willie Hamilton, MD, of the University of Exeter Medical School.
“In 2014, 163,000 people died of cancer in this country. Our findings on thrombocytosis show a strong association with cancer, particularly in men—far stronger than that of a breast lump for breast cancer in women. It is now crucial that we roll out cancer investigation of thrombocytosis. It could save hundreds of lives each year.” ![]()
Role of TET2 in hematologic malignancies
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
New research appears to explain how TET2 mutations increase the risk of hematologic malignancies.
In studying mouse models and patient samples, researchers found evidence to suggest that loss of TET2 opens the door for mutations that drive lymphoid and myeloid malignancies.
The researchers said loss of TET2 leads to hypermutagenicity in hematopoietic stem and progenitor cells (HSPCs), and although TET2-deficient HSPCs are likely not malignant, the higher mutation rates in these cells may result in additional driver mutations in TET2 target genes over time.
“If you lose TET2, it’s not a malignant state per se,” said Mingjiang Xu, MD, PhD, of the University of Miami Miller School of Medicine in Florida.
“But it’s creating a situation for other mutations to happen, leading to all types of blood cancer.”
Dr Xu and his colleagues reported these findings in Nature Communications.
The researchers found that Tet2-knockout mice developed spontaneous, lethal hematologic malignancies. Most (92%) developed myeloid malignancies, but 3.5% developed T-cell malignancies, and 4.5% developed B-cell malignancies.
In sequencing tumor and non-tumor cells from the Tet2-knockout mice, the researchers observed that loss of Tet2 leads to hypermutagenicity in HSPCs.
The team identified 190 genes with recurrent single-nucleotide variants. This included genes that are recurrently altered in human hematologic malignancies—Apc, Nf1, Flt3, Cbl, Notch1, and Mll2.
The researchers also analyzed samples from patients with acute myeloid leukemia, myeloproliferative neoplasms, and myelodysplastic syndromes.
The team found that patients with TET2 mutations had “significantly more mutational events than patients with wild-type TET2.” And TET2 mutations were associated with subclonal events in APC, NF1, ASXL1, CBL, and ZRSR2, among other genes.
These findings suggest that targeting TET2 could potentially prevent the development of hematologic malignancies.
The researchers noted that TET2 mutations occur in healthy elderly individuals with clonal hematopoiesis, and these individuals would be ideal candidates for a preventive therapy targeting TET2.
“We are developing a method to target TET2,” Dr Xu said. “If we target that population [with TET2 mutations] for early therapy, we could potentially prevent those downstream mutations from happening.” ![]()
Assay intended to aid PV diagnosis cleared for use in US
The US Food and Drug Administration has granted 510(k) clearance for QIAGEN’s ipsogen® JAK2 RGQ PCR Kit (ipsogen JAK2 assay), and the company has launched the assay in the US.
The ipsogen JAK2 assay is designed to detect the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The assay is intended for use in conjunction with other clinicopathological factors to aid the diagnosis of polycythemia vera (PV).
The test does not detect less common mutations associated with PV, including mutations in exon 12, and is not intended for stand-alone diagnosis of PV.
The ipsogen JAK2 assay is a real-time polymerase chain reaction test performed on the QIAGEN Rotor-Gene Q MDx instrument.
Researchers evaluated the utility of the ipsogen JAK2 assay for PV diagnosis in a prospective trial enrolling more than 200 subjects.
Data from this trial have not been published. However, according to QIAGEN, the assay provided 94.6% sensitivity and 98.1% specificity, together with a 100% positive percentage agreement and a 99.4% negative percentage agreement to bi-directional sequencing.
QIAGEN said these results suggest the ipsogen JAK2 assay enables detection of PV in the majority of subjects with the disease and helps rule out PV in the majority of individuals without it.
“We are pleased to be able to offer our ipsogen JAK2 assay, which is already available in Europe and other markets, for use in the United States and make it easier for hematologists and oncologists to follow recommended diagnostic testing algorithms and international guidelines for suspected PV patients,” said Thierry Bernard, senior vice president and head of QIAGEN’s Molecular Diagnostics Business Area. ![]()
The US Food and Drug Administration has granted 510(k) clearance for QIAGEN’s ipsogen® JAK2 RGQ PCR Kit (ipsogen JAK2 assay), and the company has launched the assay in the US.
The ipsogen JAK2 assay is designed to detect the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The assay is intended for use in conjunction with other clinicopathological factors to aid the diagnosis of polycythemia vera (PV).
The test does not detect less common mutations associated with PV, including mutations in exon 12, and is not intended for stand-alone diagnosis of PV.
The ipsogen JAK2 assay is a real-time polymerase chain reaction test performed on the QIAGEN Rotor-Gene Q MDx instrument.
Researchers evaluated the utility of the ipsogen JAK2 assay for PV diagnosis in a prospective trial enrolling more than 200 subjects.
Data from this trial have not been published. However, according to QIAGEN, the assay provided 94.6% sensitivity and 98.1% specificity, together with a 100% positive percentage agreement and a 99.4% negative percentage agreement to bi-directional sequencing.
QIAGEN said these results suggest the ipsogen JAK2 assay enables detection of PV in the majority of subjects with the disease and helps rule out PV in the majority of individuals without it.
“We are pleased to be able to offer our ipsogen JAK2 assay, which is already available in Europe and other markets, for use in the United States and make it easier for hematologists and oncologists to follow recommended diagnostic testing algorithms and international guidelines for suspected PV patients,” said Thierry Bernard, senior vice president and head of QIAGEN’s Molecular Diagnostics Business Area. ![]()
The US Food and Drug Administration has granted 510(k) clearance for QIAGEN’s ipsogen® JAK2 RGQ PCR Kit (ipsogen JAK2 assay), and the company has launched the assay in the US.
The ipsogen JAK2 assay is designed to detect the JAK2 V617F/G1849T allele in genomic DNA extracted from EDTA whole blood.
The assay is intended for use in conjunction with other clinicopathological factors to aid the diagnosis of polycythemia vera (PV).
The test does not detect less common mutations associated with PV, including mutations in exon 12, and is not intended for stand-alone diagnosis of PV.
The ipsogen JAK2 assay is a real-time polymerase chain reaction test performed on the QIAGEN Rotor-Gene Q MDx instrument.
Researchers evaluated the utility of the ipsogen JAK2 assay for PV diagnosis in a prospective trial enrolling more than 200 subjects.
Data from this trial have not been published. However, according to QIAGEN, the assay provided 94.6% sensitivity and 98.1% specificity, together with a 100% positive percentage agreement and a 99.4% negative percentage agreement to bi-directional sequencing.
QIAGEN said these results suggest the ipsogen JAK2 assay enables detection of PV in the majority of subjects with the disease and helps rule out PV in the majority of individuals without it.
“We are pleased to be able to offer our ipsogen JAK2 assay, which is already available in Europe and other markets, for use in the United States and make it easier for hematologists and oncologists to follow recommended diagnostic testing algorithms and international guidelines for suspected PV patients,” said Thierry Bernard, senior vice president and head of QIAGEN’s Molecular Diagnostics Business Area. ![]()
Company again withdraws application for pacritinib
CTI BioPharma has withdrawn its application for marketing authorization of pacritinib (Enpaxiq) in the European Union, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The company was seeking approval for pacritinib, a JAK2/FLT3 inhibitor, to treat splenomegaly or symptoms of myelofibrosis (MF) in adults with primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
When the application was withdrawn, the CHMP was of the provisional opinion that pacritinib could not have been approved for this indication.
Last year, CTI BioPharma withdrew its application for approval of pacritinib in the US.
Issues preventing approval
The CHMP said it had a number of concerns related to the PERSIST-1 trial, which was used to support the application for approval in the European Union. In this trial, researchers compared pacritinib to best available therapy, excluding JAK inhibitors, in patients with MF.
The CHMP said the reduction in spleen size, which was the main efficacy outcome in the study, appeared to be lower with pacritinib than with another medicine of its class, with no improvement in symptom scores.
In addition, the incidence of thrombocytopenia was higher in patients treated with pacritinib.
And more deaths occurred in patients taking pacritinib than in those receiving best available therapy, including deaths due to bleeding and adverse effects on the heart.
The CHMP also said it needs more information about the starting materials used in the manufacture of pacritinib and how the drug acts on target proteins.
Given these concerns, the CHMP was of the opinion that pacritinib’s benefits had not been shown to outweigh its risks.
CTI BioPharma said it could address the CHMP’s concerns by providing data from a second study of pacritinib, PERSIST-2.
However, there was not enough time in the current application procedure to provide the data, so the company decided to withdraw the application.
CTI BioPharma said it intends to integrate data from PERSIST-2 into its current dossier before approaching the European Medicines Agency to discuss a new application.
The company also said the withdrawal of its application will not affect patients currently enrolled in clinical trials of pacritinib or compassionate use programs for the drug.
Previous withdrawal, clinical hold
CTI BioPharma withdrew its application for approval of pacritinib in the US after the US Food and Drug Administration (FDA) placed a full clinical hold on trials of the drug.
The FDA placed the hold on pacritinib trials in February 2016 after results from PERSIST-1 and PERSIST-2 showed excess mortality in patients who received pacritinib.
The FDA lifted the hold in January 2017 after CTI BioPharma agreed to conduct dose-exploration studies for pacritinib, submit final study reports and data sets for PERSIST-1 and PERSIST-2, and make modifications to protocols and study-related documents. ![]()
CTI BioPharma has withdrawn its application for marketing authorization of pacritinib (Enpaxiq) in the European Union, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The company was seeking approval for pacritinib, a JAK2/FLT3 inhibitor, to treat splenomegaly or symptoms of myelofibrosis (MF) in adults with primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
When the application was withdrawn, the CHMP was of the provisional opinion that pacritinib could not have been approved for this indication.
Last year, CTI BioPharma withdrew its application for approval of pacritinib in the US.
Issues preventing approval
The CHMP said it had a number of concerns related to the PERSIST-1 trial, which was used to support the application for approval in the European Union. In this trial, researchers compared pacritinib to best available therapy, excluding JAK inhibitors, in patients with MF.
The CHMP said the reduction in spleen size, which was the main efficacy outcome in the study, appeared to be lower with pacritinib than with another medicine of its class, with no improvement in symptom scores.
In addition, the incidence of thrombocytopenia was higher in patients treated with pacritinib.
And more deaths occurred in patients taking pacritinib than in those receiving best available therapy, including deaths due to bleeding and adverse effects on the heart.
The CHMP also said it needs more information about the starting materials used in the manufacture of pacritinib and how the drug acts on target proteins.
Given these concerns, the CHMP was of the opinion that pacritinib’s benefits had not been shown to outweigh its risks.
CTI BioPharma said it could address the CHMP’s concerns by providing data from a second study of pacritinib, PERSIST-2.
However, there was not enough time in the current application procedure to provide the data, so the company decided to withdraw the application.
CTI BioPharma said it intends to integrate data from PERSIST-2 into its current dossier before approaching the European Medicines Agency to discuss a new application.
The company also said the withdrawal of its application will not affect patients currently enrolled in clinical trials of pacritinib or compassionate use programs for the drug.
Previous withdrawal, clinical hold
CTI BioPharma withdrew its application for approval of pacritinib in the US after the US Food and Drug Administration (FDA) placed a full clinical hold on trials of the drug.
The FDA placed the hold on pacritinib trials in February 2016 after results from PERSIST-1 and PERSIST-2 showed excess mortality in patients who received pacritinib.
The FDA lifted the hold in January 2017 after CTI BioPharma agreed to conduct dose-exploration studies for pacritinib, submit final study reports and data sets for PERSIST-1 and PERSIST-2, and make modifications to protocols and study-related documents. ![]()
CTI BioPharma has withdrawn its application for marketing authorization of pacritinib (Enpaxiq) in the European Union, according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The company was seeking approval for pacritinib, a JAK2/FLT3 inhibitor, to treat splenomegaly or symptoms of myelofibrosis (MF) in adults with primary MF, post-polycythemia vera MF, or post-essential thrombocythemia MF.
When the application was withdrawn, the CHMP was of the provisional opinion that pacritinib could not have been approved for this indication.
Last year, CTI BioPharma withdrew its application for approval of pacritinib in the US.
Issues preventing approval
The CHMP said it had a number of concerns related to the PERSIST-1 trial, which was used to support the application for approval in the European Union. In this trial, researchers compared pacritinib to best available therapy, excluding JAK inhibitors, in patients with MF.
The CHMP said the reduction in spleen size, which was the main efficacy outcome in the study, appeared to be lower with pacritinib than with another medicine of its class, with no improvement in symptom scores.
In addition, the incidence of thrombocytopenia was higher in patients treated with pacritinib.
And more deaths occurred in patients taking pacritinib than in those receiving best available therapy, including deaths due to bleeding and adverse effects on the heart.
The CHMP also said it needs more information about the starting materials used in the manufacture of pacritinib and how the drug acts on target proteins.
Given these concerns, the CHMP was of the opinion that pacritinib’s benefits had not been shown to outweigh its risks.
CTI BioPharma said it could address the CHMP’s concerns by providing data from a second study of pacritinib, PERSIST-2.
However, there was not enough time in the current application procedure to provide the data, so the company decided to withdraw the application.
CTI BioPharma said it intends to integrate data from PERSIST-2 into its current dossier before approaching the European Medicines Agency to discuss a new application.
The company also said the withdrawal of its application will not affect patients currently enrolled in clinical trials of pacritinib or compassionate use programs for the drug.
Previous withdrawal, clinical hold
CTI BioPharma withdrew its application for approval of pacritinib in the US after the US Food and Drug Administration (FDA) placed a full clinical hold on trials of the drug.
The FDA placed the hold on pacritinib trials in February 2016 after results from PERSIST-1 and PERSIST-2 showed excess mortality in patients who received pacritinib.
The FDA lifted the hold in January 2017 after CTI BioPharma agreed to conduct dose-exploration studies for pacritinib, submit final study reports and data sets for PERSIST-1 and PERSIST-2, and make modifications to protocols and study-related documents.
FDA lifts full clinical hold on pacritinib

The US Food and Drug Administration (FDA) has lifted the full clinical hold placed on all clinical trials conducted under the investigational new drug application for pacritinib, an oral kinase inhibitor being developed as a treatment for myelofibrosis (MF).
The FDA placed the hold on pacritinib trials in February 2016 after results from 2 phase 3 trials, PERSIST-1 and PERSIST-2, showed excess mortality in patients who received pacritinib.
Both trials suggested pacritinib can be more effective than the best available therapy for MF.
However, interim overall survival results from PERSIST-2 indicated that pacritinib had a detrimental effect on survival, which was consistent with the results from PERSIST-1.
Due to the full clinical hold, CTI BioPharma withdrew the new drug application for pacritinib while reviewing data from PERSIST-2.
When the FDA enacted the hold, the agency recommended that CTI BioPharma conduct dose-exploration studies for pacritinib, submit final study reports and data sets for PERSIST-1 and PERSIST-2, make certain modifications to protocols and study-related documents, and request a meeting with the FDA prior to submitting a response to the full clinical hold.
CTI BioPharma followed the FDA’s recommendations and submitted a response to the hold that included final clinical study reports for PERSIST-1 and PERSIST-2 and a protocol for a dose-exploration trial.
The trial, PAC203, should enroll up to approximately 105 patients with primary MF who have failed prior ruxolitinib therapy. The goal is to evaluate the safety and the dose-response relationship for efficacy (spleen volume reduction at 24 weeks) of pacritinib at 3 doses: 100 mg once daily, 100 mg twice daily (BID), and 200 mg BID. The 200 mg BID dose regimen was used in PERSIST-2.
CTI BioPharma said it expects to start the trial in the second quarter of 2017.
“We are pleased to resolve the full clinical hold through working diligently with the FDA to provide a comprehensive response to their requests,” said Richard Love, interim president and chief executive officer of CTI BioPharma.
“We look forward to discussing with the FDA the future development of pacritinib. We believe pacritinib can ultimately address the unmet need of patients with myelofibrosis who are ineligible to receive or are not benefitting from the approved JAK1/JAK2 inhibitor, ruxolitinib, as these patients have limited treatment options.” ![]()

The US Food and Drug Administration (FDA) has lifted the full clinical hold placed on all clinical trials conducted under the investigational new drug application for pacritinib, an oral kinase inhibitor being developed as a treatment for myelofibrosis (MF).
The FDA placed the hold on pacritinib trials in February 2016 after results from 2 phase 3 trials, PERSIST-1 and PERSIST-2, showed excess mortality in patients who received pacritinib.
Both trials suggested pacritinib can be more effective than the best available therapy for MF.
However, interim overall survival results from PERSIST-2 indicated that pacritinib had a detrimental effect on survival, which was consistent with the results from PERSIST-1.
Due to the full clinical hold, CTI BioPharma withdrew the new drug application for pacritinib while reviewing data from PERSIST-2.
When the FDA enacted the hold, the agency recommended that CTI BioPharma conduct dose-exploration studies for pacritinib, submit final study reports and data sets for PERSIST-1 and PERSIST-2, make certain modifications to protocols and study-related documents, and request a meeting with the FDA prior to submitting a response to the full clinical hold.
CTI BioPharma followed the FDA’s recommendations and submitted a response to the hold that included final clinical study reports for PERSIST-1 and PERSIST-2 and a protocol for a dose-exploration trial.
The trial, PAC203, should enroll up to approximately 105 patients with primary MF who have failed prior ruxolitinib therapy. The goal is to evaluate the safety and the dose-response relationship for efficacy (spleen volume reduction at 24 weeks) of pacritinib at 3 doses: 100 mg once daily, 100 mg twice daily (BID), and 200 mg BID. The 200 mg BID dose regimen was used in PERSIST-2.
CTI BioPharma said it expects to start the trial in the second quarter of 2017.
“We are pleased to resolve the full clinical hold through working diligently with the FDA to provide a comprehensive response to their requests,” said Richard Love, interim president and chief executive officer of CTI BioPharma.
“We look forward to discussing with the FDA the future development of pacritinib. We believe pacritinib can ultimately address the unmet need of patients with myelofibrosis who are ineligible to receive or are not benefitting from the approved JAK1/JAK2 inhibitor, ruxolitinib, as these patients have limited treatment options.” ![]()

The US Food and Drug Administration (FDA) has lifted the full clinical hold placed on all clinical trials conducted under the investigational new drug application for pacritinib, an oral kinase inhibitor being developed as a treatment for myelofibrosis (MF).
The FDA placed the hold on pacritinib trials in February 2016 after results from 2 phase 3 trials, PERSIST-1 and PERSIST-2, showed excess mortality in patients who received pacritinib.
Both trials suggested pacritinib can be more effective than the best available therapy for MF.
However, interim overall survival results from PERSIST-2 indicated that pacritinib had a detrimental effect on survival, which was consistent with the results from PERSIST-1.
Due to the full clinical hold, CTI BioPharma withdrew the new drug application for pacritinib while reviewing data from PERSIST-2.
When the FDA enacted the hold, the agency recommended that CTI BioPharma conduct dose-exploration studies for pacritinib, submit final study reports and data sets for PERSIST-1 and PERSIST-2, make certain modifications to protocols and study-related documents, and request a meeting with the FDA prior to submitting a response to the full clinical hold.
CTI BioPharma followed the FDA’s recommendations and submitted a response to the hold that included final clinical study reports for PERSIST-1 and PERSIST-2 and a protocol for a dose-exploration trial.
The trial, PAC203, should enroll up to approximately 105 patients with primary MF who have failed prior ruxolitinib therapy. The goal is to evaluate the safety and the dose-response relationship for efficacy (spleen volume reduction at 24 weeks) of pacritinib at 3 doses: 100 mg once daily, 100 mg twice daily (BID), and 200 mg BID. The 200 mg BID dose regimen was used in PERSIST-2.
CTI BioPharma said it expects to start the trial in the second quarter of 2017.
“We are pleased to resolve the full clinical hold through working diligently with the FDA to provide a comprehensive response to their requests,” said Richard Love, interim president and chief executive officer of CTI BioPharma.
“We look forward to discussing with the FDA the future development of pacritinib. We believe pacritinib can ultimately address the unmet need of patients with myelofibrosis who are ineligible to receive or are not benefitting from the approved JAK1/JAK2 inhibitor, ruxolitinib, as these patients have limited treatment options.” ![]()
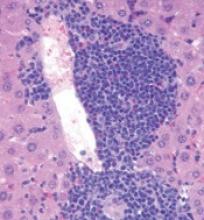
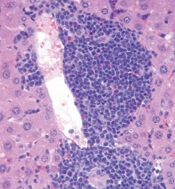
Trial supports early treatment of lower-risk ET

Photo courtesy of CDC
SAN DIEGO—Results from the ARETA trial suggest patients with essential thrombocythemia (ET) can benefit from early treatment even if they are not considered high-risk.
In this phase 3 trial, non-high-risk patients were less likely to experience ET-related cardiovascular events or disease progression if they received extended-release anagrelide rather than placebo.
Patients who received extended-release anagrelide were also less likely to become high-risk over time.
And extended-release anagrelide had a safety profile consistent with conventional anagrelide formulations, according to investigator Heinz Gisslinger, MD, of the Medical University of Vienna in Austria.
Dr Gisslinger reported final results of the ARETA trial at the 2016 ASH Annual Meeting (abstract 476).
The trial was sponsored by AOP Orphan Pharmaceuticals AG, the company developing the extended-release formulation of anagrelide, known as anagrelide retard (AR).
Dr Gisslinger noted that the goals of developing AR are to achieve lower peak plasma concentration of anagrelide, reduce the frequency and intensity of peak concentration related to adverse events (AEs), allow for an easier dosing scheme (once daily vs 2 to 3 times daily), and improve patient compliance.
He also pointed out that results of the phase 3 TEAM-ET trial suggest AR is non-inferior to the standard formulation of anagrelide (Thromboreductin, also a product of AOP Orphan Pharmaceuticals).
So with the ARETA trial, Dr Gisslinger and his colleagues set out to determine if AR would be beneficial as an early intervention in patients with non-high-risk ET.
Patients
The trial enrolled 146 patients who had platelet counts below 1000 G/L and met at least 1 of the following criteria:
- Age 40 to 60 years
- ET duration of more than 3 years
- Any risk factor for thrombotic complications (JAK2 mutation, protein C and/or S deficiency, antithrombin III deficiency, factor V Leiden or prothrombin mutation, or cardiovascular risk factors).
Seventy-seven patients were randomized to AR, and 69 were randomized to placebo. In both treatment arms, 100% of patients were Caucasian, and about 74% were female.
The mean age was 40.9 (range, 20-60) in the AR arm and 45.2 (range, 19-59) in the placebo arm. The median disease duration was 75.0 days (range, 1-2502) and 78.0 days (range, 1-2195), respectively. The mean platelet count was 748.6 G/L and 745.3 G/L, respectively.
A majority of patients in both arms had JAK2 mutations (62.7% in the AR arm and 63.8% in the placebo arm). Fewer had CALR mutations (22.7% and 13.6%, respectively) and MPL mutations (16.7% and 12.5%).
Treatment
Patients were stratified by JAK2 status and randomized to receive AR at 2 to 8 mg/day or placebo.
The dosing of AR started at 1 tablet (2 mg) per day during week 1 and was titrated up according to platelet response to 2 tablets in week 2. Dosing was further increased or decreased according to platelet response in weeks 3 and 4.
The maximum dose was 4 tablets (8 mg) per day. After week 4, the maximum dose to achieve optimal platelet counts (<450 G/L) was maintained, and patients continued with weekly visits through week 6.
After that, patients had visits every 3 months in both the main phase of this study and the extension phase. The main phase lasted 1 year, and the extension phase lasted up to 3 years.
Sixty patients (77.9%) in the AR arm and 52 (75.4%) in the placebo arm completed the main phase of the study.
Fifty-seven patients in the AR arm entered the extension phase, and 44 (57.1%) completed it. Thirty-four patients in the placebo arm entered the extension phase, and 21 (30.4%) completed it.
Efficacy
The primary endpoint was time to ET-related cardiovascular events (as confirmed by a blinded expert panel) or disease progression/worsening (platelet increase >1000 G/L).
The 1-year event-free rate (patients who did not meet criteria for the primary endpoint) was 87% in the AR arm and 69% in the placebo arm (hazard ratio=0.356, P=0.0008).
According to the expert panel, there were 12 ET-related events in 11 patients in the AR arm, as well as 17 such events in 14 patients in the placebo arm. This included major and minor arterial, venous, and bleeding events.
In total, there were 13 patients who had ET-related events or met platelet criteria in the AR arm (13 events) and 26 patients who had ET-related events or met platelet criteria in the placebo arm (30 events).
Nine patients in the AR arm (11.7%) and 18 in the placebo arm (26.1%) changed to high-risk status at some point during the trial (odds ratio=2.67, P=0.033).
Safety
The overall incidence of AEs was 88.3% in the AR arm and 69.6% in the placebo arm. The incidence of treatment-related AEs was 76.6% and 27.5%, respectively.
The incidence of treatment-related serious AEs was 1.3% and 0%, respectively. And the incidence of treatment-related AEs leading to withdrawal was 9.1% and 7.2%, respectively.
Treatment-related AEs occurring in more than 10% of patients in either arm (the AR and placebo arms, respectively) included headache (41.6% and 15.9%), dizziness (35.1% and 14.5%), palpitations (28.6% and 1.4%), and tachycardia (10.4% and 1.4%).
In closing, Dr Gisslinger noted that the primary endpoint of this study was met, and AR allowed for platelet count normalization and delayed progression to high-risk status.
Furthermore, the safety profile of AR is consistent with conventional anagrelide formulations, but AR allows for a more convenient dosing schedule.
Dr Gisslinger concluded, “[T]hese data from the ARETA study support an early treatment concept for all ET patients where platelet count or symptom reduction is a goal and those patients who can be attributed as intermediate-risk patients.” ![]()

Photo courtesy of CDC
SAN DIEGO—Results from the ARETA trial suggest patients with essential thrombocythemia (ET) can benefit from early treatment even if they are not considered high-risk.
In this phase 3 trial, non-high-risk patients were less likely to experience ET-related cardiovascular events or disease progression if they received extended-release anagrelide rather than placebo.
Patients who received extended-release anagrelide were also less likely to become high-risk over time.
And extended-release anagrelide had a safety profile consistent with conventional anagrelide formulations, according to investigator Heinz Gisslinger, MD, of the Medical University of Vienna in Austria.
Dr Gisslinger reported final results of the ARETA trial at the 2016 ASH Annual Meeting (abstract 476).
The trial was sponsored by AOP Orphan Pharmaceuticals AG, the company developing the extended-release formulation of anagrelide, known as anagrelide retard (AR).
Dr Gisslinger noted that the goals of developing AR are to achieve lower peak plasma concentration of anagrelide, reduce the frequency and intensity of peak concentration related to adverse events (AEs), allow for an easier dosing scheme (once daily vs 2 to 3 times daily), and improve patient compliance.
He also pointed out that results of the phase 3 TEAM-ET trial suggest AR is non-inferior to the standard formulation of anagrelide (Thromboreductin, also a product of AOP Orphan Pharmaceuticals).
So with the ARETA trial, Dr Gisslinger and his colleagues set out to determine if AR would be beneficial as an early intervention in patients with non-high-risk ET.
Patients
The trial enrolled 146 patients who had platelet counts below 1000 G/L and met at least 1 of the following criteria:
- Age 40 to 60 years
- ET duration of more than 3 years
- Any risk factor for thrombotic complications (JAK2 mutation, protein C and/or S deficiency, antithrombin III deficiency, factor V Leiden or prothrombin mutation, or cardiovascular risk factors).
Seventy-seven patients were randomized to AR, and 69 were randomized to placebo. In both treatment arms, 100% of patients were Caucasian, and about 74% were female.
The mean age was 40.9 (range, 20-60) in the AR arm and 45.2 (range, 19-59) in the placebo arm. The median disease duration was 75.0 days (range, 1-2502) and 78.0 days (range, 1-2195), respectively. The mean platelet count was 748.6 G/L and 745.3 G/L, respectively.
A majority of patients in both arms had JAK2 mutations (62.7% in the AR arm and 63.8% in the placebo arm). Fewer had CALR mutations (22.7% and 13.6%, respectively) and MPL mutations (16.7% and 12.5%).
Treatment
Patients were stratified by JAK2 status and randomized to receive AR at 2 to 8 mg/day or placebo.
The dosing of AR started at 1 tablet (2 mg) per day during week 1 and was titrated up according to platelet response to 2 tablets in week 2. Dosing was further increased or decreased according to platelet response in weeks 3 and 4.
The maximum dose was 4 tablets (8 mg) per day. After week 4, the maximum dose to achieve optimal platelet counts (<450 G/L) was maintained, and patients continued with weekly visits through week 6.
After that, patients had visits every 3 months in both the main phase of this study and the extension phase. The main phase lasted 1 year, and the extension phase lasted up to 3 years.
Sixty patients (77.9%) in the AR arm and 52 (75.4%) in the placebo arm completed the main phase of the study.
Fifty-seven patients in the AR arm entered the extension phase, and 44 (57.1%) completed it. Thirty-four patients in the placebo arm entered the extension phase, and 21 (30.4%) completed it.
Efficacy
The primary endpoint was time to ET-related cardiovascular events (as confirmed by a blinded expert panel) or disease progression/worsening (platelet increase >1000 G/L).
The 1-year event-free rate (patients who did not meet criteria for the primary endpoint) was 87% in the AR arm and 69% in the placebo arm (hazard ratio=0.356, P=0.0008).
According to the expert panel, there were 12 ET-related events in 11 patients in the AR arm, as well as 17 such events in 14 patients in the placebo arm. This included major and minor arterial, venous, and bleeding events.
In total, there were 13 patients who had ET-related events or met platelet criteria in the AR arm (13 events) and 26 patients who had ET-related events or met platelet criteria in the placebo arm (30 events).
Nine patients in the AR arm (11.7%) and 18 in the placebo arm (26.1%) changed to high-risk status at some point during the trial (odds ratio=2.67, P=0.033).
Safety
The overall incidence of AEs was 88.3% in the AR arm and 69.6% in the placebo arm. The incidence of treatment-related AEs was 76.6% and 27.5%, respectively.
The incidence of treatment-related serious AEs was 1.3% and 0%, respectively. And the incidence of treatment-related AEs leading to withdrawal was 9.1% and 7.2%, respectively.
Treatment-related AEs occurring in more than 10% of patients in either arm (the AR and placebo arms, respectively) included headache (41.6% and 15.9%), dizziness (35.1% and 14.5%), palpitations (28.6% and 1.4%), and tachycardia (10.4% and 1.4%).
In closing, Dr Gisslinger noted that the primary endpoint of this study was met, and AR allowed for platelet count normalization and delayed progression to high-risk status.
Furthermore, the safety profile of AR is consistent with conventional anagrelide formulations, but AR allows for a more convenient dosing schedule.
Dr Gisslinger concluded, “[T]hese data from the ARETA study support an early treatment concept for all ET patients where platelet count or symptom reduction is a goal and those patients who can be attributed as intermediate-risk patients.” ![]()

Photo courtesy of CDC
SAN DIEGO—Results from the ARETA trial suggest patients with essential thrombocythemia (ET) can benefit from early treatment even if they are not considered high-risk.
In this phase 3 trial, non-high-risk patients were less likely to experience ET-related cardiovascular events or disease progression if they received extended-release anagrelide rather than placebo.
Patients who received extended-release anagrelide were also less likely to become high-risk over time.
And extended-release anagrelide had a safety profile consistent with conventional anagrelide formulations, according to investigator Heinz Gisslinger, MD, of the Medical University of Vienna in Austria.
Dr Gisslinger reported final results of the ARETA trial at the 2016 ASH Annual Meeting (abstract 476).
The trial was sponsored by AOP Orphan Pharmaceuticals AG, the company developing the extended-release formulation of anagrelide, known as anagrelide retard (AR).
Dr Gisslinger noted that the goals of developing AR are to achieve lower peak plasma concentration of anagrelide, reduce the frequency and intensity of peak concentration related to adverse events (AEs), allow for an easier dosing scheme (once daily vs 2 to 3 times daily), and improve patient compliance.
He also pointed out that results of the phase 3 TEAM-ET trial suggest AR is non-inferior to the standard formulation of anagrelide (Thromboreductin, also a product of AOP Orphan Pharmaceuticals).
So with the ARETA trial, Dr Gisslinger and his colleagues set out to determine if AR would be beneficial as an early intervention in patients with non-high-risk ET.
Patients
The trial enrolled 146 patients who had platelet counts below 1000 G/L and met at least 1 of the following criteria:
- Age 40 to 60 years
- ET duration of more than 3 years
- Any risk factor for thrombotic complications (JAK2 mutation, protein C and/or S deficiency, antithrombin III deficiency, factor V Leiden or prothrombin mutation, or cardiovascular risk factors).
Seventy-seven patients were randomized to AR, and 69 were randomized to placebo. In both treatment arms, 100% of patients were Caucasian, and about 74% were female.
The mean age was 40.9 (range, 20-60) in the AR arm and 45.2 (range, 19-59) in the placebo arm. The median disease duration was 75.0 days (range, 1-2502) and 78.0 days (range, 1-2195), respectively. The mean platelet count was 748.6 G/L and 745.3 G/L, respectively.
A majority of patients in both arms had JAK2 mutations (62.7% in the AR arm and 63.8% in the placebo arm). Fewer had CALR mutations (22.7% and 13.6%, respectively) and MPL mutations (16.7% and 12.5%).
Treatment
Patients were stratified by JAK2 status and randomized to receive AR at 2 to 8 mg/day or placebo.
The dosing of AR started at 1 tablet (2 mg) per day during week 1 and was titrated up according to platelet response to 2 tablets in week 2. Dosing was further increased or decreased according to platelet response in weeks 3 and 4.
The maximum dose was 4 tablets (8 mg) per day. After week 4, the maximum dose to achieve optimal platelet counts (<450 G/L) was maintained, and patients continued with weekly visits through week 6.
After that, patients had visits every 3 months in both the main phase of this study and the extension phase. The main phase lasted 1 year, and the extension phase lasted up to 3 years.
Sixty patients (77.9%) in the AR arm and 52 (75.4%) in the placebo arm completed the main phase of the study.
Fifty-seven patients in the AR arm entered the extension phase, and 44 (57.1%) completed it. Thirty-four patients in the placebo arm entered the extension phase, and 21 (30.4%) completed it.
Efficacy
The primary endpoint was time to ET-related cardiovascular events (as confirmed by a blinded expert panel) or disease progression/worsening (platelet increase >1000 G/L).
The 1-year event-free rate (patients who did not meet criteria for the primary endpoint) was 87% in the AR arm and 69% in the placebo arm (hazard ratio=0.356, P=0.0008).
According to the expert panel, there were 12 ET-related events in 11 patients in the AR arm, as well as 17 such events in 14 patients in the placebo arm. This included major and minor arterial, venous, and bleeding events.
In total, there were 13 patients who had ET-related events or met platelet criteria in the AR arm (13 events) and 26 patients who had ET-related events or met platelet criteria in the placebo arm (30 events).
Nine patients in the AR arm (11.7%) and 18 in the placebo arm (26.1%) changed to high-risk status at some point during the trial (odds ratio=2.67, P=0.033).
Safety
The overall incidence of AEs was 88.3% in the AR arm and 69.6% in the placebo arm. The incidence of treatment-related AEs was 76.6% and 27.5%, respectively.
The incidence of treatment-related serious AEs was 1.3% and 0%, respectively. And the incidence of treatment-related AEs leading to withdrawal was 9.1% and 7.2%, respectively.
Treatment-related AEs occurring in more than 10% of patients in either arm (the AR and placebo arms, respectively) included headache (41.6% and 15.9%), dizziness (35.1% and 14.5%), palpitations (28.6% and 1.4%), and tachycardia (10.4% and 1.4%).
In closing, Dr Gisslinger noted that the primary endpoint of this study was met, and AR allowed for platelet count normalization and delayed progression to high-risk status.
Furthermore, the safety profile of AR is consistent with conventional anagrelide formulations, but AR allows for a more convenient dosing schedule.
Dr Gisslinger concluded, “[T]hese data from the ARETA study support an early treatment concept for all ET patients where platelet count or symptom reduction is a goal and those patients who can be attributed as intermediate-risk patients.” ![]()
Novel interferon appears safer than HU in PV

Photo by Zak Hubbard
SAN DIEGO—Results of the PROUD-PV trial suggest ropeginterferon alfa-2b is safer than hydroxyurea (HU) for patients with polycythemia vera (PV).
In this phase 3 trial, ropeginterferon alfa-2b demonstrated non-inferiority to HU with regard to complete hematologic response (CHR).
Ropeginterferon alfa-2b also had a significantly better overall safety profile.
Unlike the patients who received HU, none of the patients on ropeginterferon alfa-2b developed secondary malignancies.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, presented these results at the 2016 ASH Annual Meeting (abstract 475). The PROUD-PV study was sponsored by AOP Orphan Pharmaceuticals AG.
Dr Gisslinger noted that interferons have been successful in treating PV since the 1980s, although toxicities contribute to discontinuation rates of approximately 25%. Still, interferons are the only known drugs with the potential for disease modification by specific targeting of the malignant clone.
Ropeginterferon alfa-2b is a long-acting, mono-pegylated proline interferon with improved pharmacokinetic properties that allow for administration once every 2 weeks.
The goal of PROUD-PV was to determine how this drug stacks up against HU in both treatment-naive and HU-pretreated patients with PV.
“Our results from the first and largest, prospective, controlled trial of an interferon in polycythemia vera confirm previously reported efficacy,” Dr Gisslinger said.
“The observed safety and tolerability profile of ropeginterferon appears to be superior compared to previously reported data of interferon treatment. The unique disease-modification capability of interferon and its potential to improve progression-free survival hold promise for long-term benefit for patients.”
Patients and treatment
PROUD-PV enrolled 254 patients, and they were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127). In both arms, 100% of patients were Caucasian, slightly more than half were female, and the median age was 60 (overall range, 21-85).
The median disease duration was 1.9 months in the ropeginterferon alfa-2b arm and 3.6 months in the HU arm. Thirty-seven percent (n=47) of patients in each arm had previously received HU.
The mean hematocrit was about 50% in both arms, the median spleen length was about 13 cm, about 90% of patients had a normal/slightly enlarged spleen, and the mean JAK2V617F burden was slightly more than 40%.
The median plateau dose was 450 µg in the ropeginterferon alfa-2b arm and 1250 mg in the HU arm.
A quarter (25.2%) of patients had dose reductions due to adverse events (AEs) in the ropeginterferon alfa-2b arm, as did 51.2% of patients in the HU arm. The 12-month discontinuation rate was 16.5% in the ropeginterferon alfa-2b arm and 12.6% in the HU arm.
Response
The study’s primary objective was to demonstrate non-inferiority of ropeginterferon alfa-2b compared to HU. For this, the researchers used the 12-month CHR rate. CHR was defined as normalization of red blood cell, white blood cell, and platelet counts (without phlebotomy).
At 12 months, in the intent-to-treat population, the CHR rate was 43.1% in the ropeginterferon alfa-2b arm and 45.6% in the HU arm (P=0.0028). In the per-protocol population, the CHR rate was 44.3% and 46.5%, respectively (P=0.0036).
The researchers therefore concluded that non-inferiority was demonstrated.
The study’s pre-specified primary endpoint was actually a composite of CHR and spleen length normality. However, this was confounded by the fact that the patients’ median spleen length was almost normal at baseline and the observed change was not clinically relevant.
In the intent-to-treat-population, CHR with spleen normality occurred in 21.3% of patients in the ropeginterferon alfa-2b arm and 27.6% of patients in the HU arm (P=0.2233).
Safety
The incidence of AEs was 81.9% in the ropeginterferon alfa-2b arm and 87.4% in the HU arm. The incidence of grade 3 AEs was 16.5% and 20.5%, respectively. And the incidence of treatment-related AEs was 59.6% and 75.6%, respectively (P<0.05).
There was a significantly higher incidence (P<0.01) of the following AEs in the HU arm than the ropeginterferon alfa-2b arm: anemia (24.4% vs 6.3%), leukopenia (21.3% vs 8.7%), thrombocytopenia (28.3% vs 15.0%), and nausea (11.8% vs 2.4%).
There was no significant difference in the incidence of fatigue—13.4% in the HU arm and 12.6% in the ropeginterferon alfa-2b arm.
Patients in the ropeginterferon alfa-2b arm had a significantly higher incidence of gamma-glutamyl transferase increase—14.2% vs 0.8% in the HU arm (P<0.01).
Patients in the ropeginterferon alfa-2b arm also had a higher—but non-significant—incidence of endocrine disorders (3.1% vs 0.8%), psychiatric disorders (1.6% vs 0%), cardiac/vascular disorders (3.1% vs 1.6%), and tissue disorders (1.6% vs 0%).
None of the patients in the ropeginterferon alfa-2b arm developed secondary related malignancies. In the HU arm, however, there were 2 cases of acute leukemia, 2 cases of basal cell carcinoma, and 1 case of malignant melanoma. (This includes data from the ongoing follow-up trial CONTINUATION-PV.)
Drug development
AOP Orphan Pharmaceuticals AG said that, in the coming months, it will submit data from PROUD-PV and the ongoing follow-up trial, CONTINUATION-PV, to obtain European marketing authorization for ropeginterferon alfa-2b.
PharmaEssentia plans to submit the same data to the US Food and Drug Administration.
PharmaEssentia discovered ropeginterferon alfa-2b and has licensed the rights for development and commercialization of the drug in myeloproliferative neoplasms to AOP Orphan Pharmaceuticals AG in Europe, the Commonwealth of Independent States, and Middle Eastern markets. ![]()
*Information presented at the meeting differs from the abstract.

Photo by Zak Hubbard
SAN DIEGO—Results of the PROUD-PV trial suggest ropeginterferon alfa-2b is safer than hydroxyurea (HU) for patients with polycythemia vera (PV).
In this phase 3 trial, ropeginterferon alfa-2b demonstrated non-inferiority to HU with regard to complete hematologic response (CHR).
Ropeginterferon alfa-2b also had a significantly better overall safety profile.
Unlike the patients who received HU, none of the patients on ropeginterferon alfa-2b developed secondary malignancies.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, presented these results at the 2016 ASH Annual Meeting (abstract 475). The PROUD-PV study was sponsored by AOP Orphan Pharmaceuticals AG.
Dr Gisslinger noted that interferons have been successful in treating PV since the 1980s, although toxicities contribute to discontinuation rates of approximately 25%. Still, interferons are the only known drugs with the potential for disease modification by specific targeting of the malignant clone.
Ropeginterferon alfa-2b is a long-acting, mono-pegylated proline interferon with improved pharmacokinetic properties that allow for administration once every 2 weeks.
The goal of PROUD-PV was to determine how this drug stacks up against HU in both treatment-naive and HU-pretreated patients with PV.
“Our results from the first and largest, prospective, controlled trial of an interferon in polycythemia vera confirm previously reported efficacy,” Dr Gisslinger said.
“The observed safety and tolerability profile of ropeginterferon appears to be superior compared to previously reported data of interferon treatment. The unique disease-modification capability of interferon and its potential to improve progression-free survival hold promise for long-term benefit for patients.”
Patients and treatment
PROUD-PV enrolled 254 patients, and they were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127). In both arms, 100% of patients were Caucasian, slightly more than half were female, and the median age was 60 (overall range, 21-85).
The median disease duration was 1.9 months in the ropeginterferon alfa-2b arm and 3.6 months in the HU arm. Thirty-seven percent (n=47) of patients in each arm had previously received HU.
The mean hematocrit was about 50% in both arms, the median spleen length was about 13 cm, about 90% of patients had a normal/slightly enlarged spleen, and the mean JAK2V617F burden was slightly more than 40%.
The median plateau dose was 450 µg in the ropeginterferon alfa-2b arm and 1250 mg in the HU arm.
A quarter (25.2%) of patients had dose reductions due to adverse events (AEs) in the ropeginterferon alfa-2b arm, as did 51.2% of patients in the HU arm. The 12-month discontinuation rate was 16.5% in the ropeginterferon alfa-2b arm and 12.6% in the HU arm.
Response
The study’s primary objective was to demonstrate non-inferiority of ropeginterferon alfa-2b compared to HU. For this, the researchers used the 12-month CHR rate. CHR was defined as normalization of red blood cell, white blood cell, and platelet counts (without phlebotomy).
At 12 months, in the intent-to-treat population, the CHR rate was 43.1% in the ropeginterferon alfa-2b arm and 45.6% in the HU arm (P=0.0028). In the per-protocol population, the CHR rate was 44.3% and 46.5%, respectively (P=0.0036).
The researchers therefore concluded that non-inferiority was demonstrated.
The study’s pre-specified primary endpoint was actually a composite of CHR and spleen length normality. However, this was confounded by the fact that the patients’ median spleen length was almost normal at baseline and the observed change was not clinically relevant.
In the intent-to-treat-population, CHR with spleen normality occurred in 21.3% of patients in the ropeginterferon alfa-2b arm and 27.6% of patients in the HU arm (P=0.2233).
Safety
The incidence of AEs was 81.9% in the ropeginterferon alfa-2b arm and 87.4% in the HU arm. The incidence of grade 3 AEs was 16.5% and 20.5%, respectively. And the incidence of treatment-related AEs was 59.6% and 75.6%, respectively (P<0.05).
There was a significantly higher incidence (P<0.01) of the following AEs in the HU arm than the ropeginterferon alfa-2b arm: anemia (24.4% vs 6.3%), leukopenia (21.3% vs 8.7%), thrombocytopenia (28.3% vs 15.0%), and nausea (11.8% vs 2.4%).
There was no significant difference in the incidence of fatigue—13.4% in the HU arm and 12.6% in the ropeginterferon alfa-2b arm.
Patients in the ropeginterferon alfa-2b arm had a significantly higher incidence of gamma-glutamyl transferase increase—14.2% vs 0.8% in the HU arm (P<0.01).
Patients in the ropeginterferon alfa-2b arm also had a higher—but non-significant—incidence of endocrine disorders (3.1% vs 0.8%), psychiatric disorders (1.6% vs 0%), cardiac/vascular disorders (3.1% vs 1.6%), and tissue disorders (1.6% vs 0%).
None of the patients in the ropeginterferon alfa-2b arm developed secondary related malignancies. In the HU arm, however, there were 2 cases of acute leukemia, 2 cases of basal cell carcinoma, and 1 case of malignant melanoma. (This includes data from the ongoing follow-up trial CONTINUATION-PV.)
Drug development
AOP Orphan Pharmaceuticals AG said that, in the coming months, it will submit data from PROUD-PV and the ongoing follow-up trial, CONTINUATION-PV, to obtain European marketing authorization for ropeginterferon alfa-2b.
PharmaEssentia plans to submit the same data to the US Food and Drug Administration.
PharmaEssentia discovered ropeginterferon alfa-2b and has licensed the rights for development and commercialization of the drug in myeloproliferative neoplasms to AOP Orphan Pharmaceuticals AG in Europe, the Commonwealth of Independent States, and Middle Eastern markets. ![]()
*Information presented at the meeting differs from the abstract.

Photo by Zak Hubbard
SAN DIEGO—Results of the PROUD-PV trial suggest ropeginterferon alfa-2b is safer than hydroxyurea (HU) for patients with polycythemia vera (PV).
In this phase 3 trial, ropeginterferon alfa-2b demonstrated non-inferiority to HU with regard to complete hematologic response (CHR).
Ropeginterferon alfa-2b also had a significantly better overall safety profile.
Unlike the patients who received HU, none of the patients on ropeginterferon alfa-2b developed secondary malignancies.
Heinz Gisslinger, MD, of the Medical University of Vienna in Austria, presented these results at the 2016 ASH Annual Meeting (abstract 475). The PROUD-PV study was sponsored by AOP Orphan Pharmaceuticals AG.
Dr Gisslinger noted that interferons have been successful in treating PV since the 1980s, although toxicities contribute to discontinuation rates of approximately 25%. Still, interferons are the only known drugs with the potential for disease modification by specific targeting of the malignant clone.
Ropeginterferon alfa-2b is a long-acting, mono-pegylated proline interferon with improved pharmacokinetic properties that allow for administration once every 2 weeks.
The goal of PROUD-PV was to determine how this drug stacks up against HU in both treatment-naive and HU-pretreated patients with PV.
“Our results from the first and largest, prospective, controlled trial of an interferon in polycythemia vera confirm previously reported efficacy,” Dr Gisslinger said.
“The observed safety and tolerability profile of ropeginterferon appears to be superior compared to previously reported data of interferon treatment. The unique disease-modification capability of interferon and its potential to improve progression-free survival hold promise for long-term benefit for patients.”
Patients and treatment
PROUD-PV enrolled 254 patients, and they were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127). In both arms, 100% of patients were Caucasian, slightly more than half were female, and the median age was 60 (overall range, 21-85).
The median disease duration was 1.9 months in the ropeginterferon alfa-2b arm and 3.6 months in the HU arm. Thirty-seven percent (n=47) of patients in each arm had previously received HU.
The mean hematocrit was about 50% in both arms, the median spleen length was about 13 cm, about 90% of patients had a normal/slightly enlarged spleen, and the mean JAK2V617F burden was slightly more than 40%.
The median plateau dose was 450 µg in the ropeginterferon alfa-2b arm and 1250 mg in the HU arm.
A quarter (25.2%) of patients had dose reductions due to adverse events (AEs) in the ropeginterferon alfa-2b arm, as did 51.2% of patients in the HU arm. The 12-month discontinuation rate was 16.5% in the ropeginterferon alfa-2b arm and 12.6% in the HU arm.
Response
The study’s primary objective was to demonstrate non-inferiority of ropeginterferon alfa-2b compared to HU. For this, the researchers used the 12-month CHR rate. CHR was defined as normalization of red blood cell, white blood cell, and platelet counts (without phlebotomy).
At 12 months, in the intent-to-treat population, the CHR rate was 43.1% in the ropeginterferon alfa-2b arm and 45.6% in the HU arm (P=0.0028). In the per-protocol population, the CHR rate was 44.3% and 46.5%, respectively (P=0.0036).
The researchers therefore concluded that non-inferiority was demonstrated.
The study’s pre-specified primary endpoint was actually a composite of CHR and spleen length normality. However, this was confounded by the fact that the patients’ median spleen length was almost normal at baseline and the observed change was not clinically relevant.
In the intent-to-treat-population, CHR with spleen normality occurred in 21.3% of patients in the ropeginterferon alfa-2b arm and 27.6% of patients in the HU arm (P=0.2233).
Safety
The incidence of AEs was 81.9% in the ropeginterferon alfa-2b arm and 87.4% in the HU arm. The incidence of grade 3 AEs was 16.5% and 20.5%, respectively. And the incidence of treatment-related AEs was 59.6% and 75.6%, respectively (P<0.05).
There was a significantly higher incidence (P<0.01) of the following AEs in the HU arm than the ropeginterferon alfa-2b arm: anemia (24.4% vs 6.3%), leukopenia (21.3% vs 8.7%), thrombocytopenia (28.3% vs 15.0%), and nausea (11.8% vs 2.4%).
There was no significant difference in the incidence of fatigue—13.4% in the HU arm and 12.6% in the ropeginterferon alfa-2b arm.
Patients in the ropeginterferon alfa-2b arm had a significantly higher incidence of gamma-glutamyl transferase increase—14.2% vs 0.8% in the HU arm (P<0.01).
Patients in the ropeginterferon alfa-2b arm also had a higher—but non-significant—incidence of endocrine disorders (3.1% vs 0.8%), psychiatric disorders (1.6% vs 0%), cardiac/vascular disorders (3.1% vs 1.6%), and tissue disorders (1.6% vs 0%).
None of the patients in the ropeginterferon alfa-2b arm developed secondary related malignancies. In the HU arm, however, there were 2 cases of acute leukemia, 2 cases of basal cell carcinoma, and 1 case of malignant melanoma. (This includes data from the ongoing follow-up trial CONTINUATION-PV.)
Drug development
AOP Orphan Pharmaceuticals AG said that, in the coming months, it will submit data from PROUD-PV and the ongoing follow-up trial, CONTINUATION-PV, to obtain European marketing authorization for ropeginterferon alfa-2b.
PharmaEssentia plans to submit the same data to the US Food and Drug Administration.
PharmaEssentia discovered ropeginterferon alfa-2b and has licensed the rights for development and commercialization of the drug in myeloproliferative neoplasms to AOP Orphan Pharmaceuticals AG in Europe, the Commonwealth of Independent States, and Middle Eastern markets. ![]()
*Information presented at the meeting differs from the abstract.