User login
Survival higher with ICD in patients with LVEF of 30%-35%
Prophylactic implantable cardioverter-defibrillator use was associated with improved 3-year survival in Medicare beneficiaries with heart failure and a left ventricular ejection fraction of 30%-35% and in those with LVEF less than 30%, compared with no prophylactic ICD use in comparable patients in a retrospective cohort study.
All-cause mortality at 3 years in 408 patients with LVEF of 30% -35% who received a prophylactic ICD was 51.4%, compared with 55% in 408 matched controls without an ICD (hazard ratio, 0.83). The all-cause mortality rates at 3 years in 1,088 patients with LVEF of less than 30% was 45% in those with a prophylactic ICD vs. 57.6% in 1,088 matched controls without an ICD (HR, 0.72), Dr. Sana M. Al-Khatib of Duke University, Durham, N.C., and her colleagues reported in the June 4 issue of JAMA.
Study subjects were Medicare beneficiaries in the National Cardiovascular Data Registry ICD registry during 2006-2007, and similar patients in the Get With the Guidelines-Heart Failure database during 2005-2009 (JAMA 2014;311:2209-15).
Prior studies of prophylactic ICD use have included only a minority of patients with LVEF of 30%-35%; the current findings demonstrate a "clearly significant" benefit in this population and support guideline recommendations calling for prophylactic ICD use in eligible patients with an LVEF of 35% or less, the investigators concluded.
This study was funded by a National Heart, Lung, and Blood Institute grant. Dr. Al-Khatib reported having no disclosures. Detailed disclosures for several of the other study authors are available with the full text of the article at jama.com.
Prophylactic implantable cardioverter-defibrillator use was associated with improved 3-year survival in Medicare beneficiaries with heart failure and a left ventricular ejection fraction of 30%-35% and in those with LVEF less than 30%, compared with no prophylactic ICD use in comparable patients in a retrospective cohort study.
All-cause mortality at 3 years in 408 patients with LVEF of 30% -35% who received a prophylactic ICD was 51.4%, compared with 55% in 408 matched controls without an ICD (hazard ratio, 0.83). The all-cause mortality rates at 3 years in 1,088 patients with LVEF of less than 30% was 45% in those with a prophylactic ICD vs. 57.6% in 1,088 matched controls without an ICD (HR, 0.72), Dr. Sana M. Al-Khatib of Duke University, Durham, N.C., and her colleagues reported in the June 4 issue of JAMA.
Study subjects were Medicare beneficiaries in the National Cardiovascular Data Registry ICD registry during 2006-2007, and similar patients in the Get With the Guidelines-Heart Failure database during 2005-2009 (JAMA 2014;311:2209-15).
Prior studies of prophylactic ICD use have included only a minority of patients with LVEF of 30%-35%; the current findings demonstrate a "clearly significant" benefit in this population and support guideline recommendations calling for prophylactic ICD use in eligible patients with an LVEF of 35% or less, the investigators concluded.
This study was funded by a National Heart, Lung, and Blood Institute grant. Dr. Al-Khatib reported having no disclosures. Detailed disclosures for several of the other study authors are available with the full text of the article at jama.com.
Prophylactic implantable cardioverter-defibrillator use was associated with improved 3-year survival in Medicare beneficiaries with heart failure and a left ventricular ejection fraction of 30%-35% and in those with LVEF less than 30%, compared with no prophylactic ICD use in comparable patients in a retrospective cohort study.
All-cause mortality at 3 years in 408 patients with LVEF of 30% -35% who received a prophylactic ICD was 51.4%, compared with 55% in 408 matched controls without an ICD (hazard ratio, 0.83). The all-cause mortality rates at 3 years in 1,088 patients with LVEF of less than 30% was 45% in those with a prophylactic ICD vs. 57.6% in 1,088 matched controls without an ICD (HR, 0.72), Dr. Sana M. Al-Khatib of Duke University, Durham, N.C., and her colleagues reported in the June 4 issue of JAMA.
Study subjects were Medicare beneficiaries in the National Cardiovascular Data Registry ICD registry during 2006-2007, and similar patients in the Get With the Guidelines-Heart Failure database during 2005-2009 (JAMA 2014;311:2209-15).
Prior studies of prophylactic ICD use have included only a minority of patients with LVEF of 30%-35%; the current findings demonstrate a "clearly significant" benefit in this population and support guideline recommendations calling for prophylactic ICD use in eligible patients with an LVEF of 35% or less, the investigators concluded.
This study was funded by a National Heart, Lung, and Blood Institute grant. Dr. Al-Khatib reported having no disclosures. Detailed disclosures for several of the other study authors are available with the full text of the article at jama.com.
FROM JAMA
Key clinical point: Consider recommending an ICD for heart failure patients with an LVEF of 30%-35%, a population that is not well studied in clinical trials.
Major finding: All-cause mortality was 51.4% with and 55% without a prophylactic ICD (HR, 0.83).
Data source: A retrospective cohort study involving nearly 3,000 heart failure patients with an LVEF of 30%-35%.
Disclosures: This study was funded by a National Heart, Lung, and Blood Institute grant. Dr. Al-Khatib reported having no disclosures. Detailed disclosures for several of the other study authors are available with the full text of the article at jama.com.
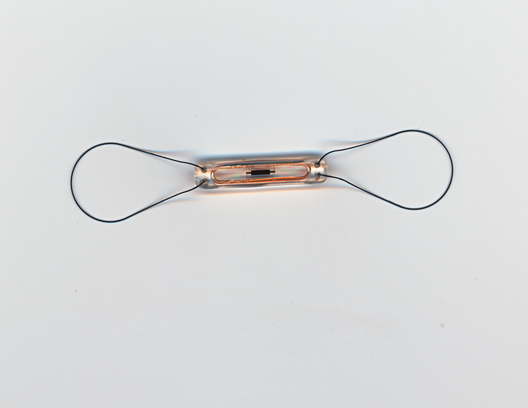
Implantable device approved for remotely monitoring PA in heart failure patients
An implantable device that provides measurements of pulmonary arterial pressure in patients with class III heart failure has been approved by the Food and Drug Administration, based on a study that showed the use of the device to remotely monitor patients reduced heart failure hospitalization rates.
The CardioMEMS HF System "is the first permanently implantable wireless system intended to provide PA pressure measurements, including systolic, diastolic, and mean PA pressures," according to the FDA statement announcing the approval on May 28. This information is remotely reviewed by the patient’s physician, who "can make decisions regarding the status of the patient and, if necessary, initiate changes in medical therapy, with the goal of reducing hospitalization due to heart failure," the statement said.
It is specifically approved for patients with New York Heart Association (NYHA) class III heart failure (HF) who have been hospitalized for heart failure in the previous year.
The three components of the system are the battery-free sensor/monitor that is permanently implanted in the pulmonary artery, a transvenous catheter that deploys the sensor in the distal PA, and an electronic system that receives and processes the signals from the sensor/monitor and transfers the PA pressure measurements to a secure database, the statement said. Patients can be monitored from their home or another remote location.
Approval was based on a study of 550 patients with NYHA class III HF and a recent hospitalization for HF, who had the device implanted. Physicians had access to daily PA measurements only for the patients randomized to the treatment group, and adjusted HF medications based on the values provided. At 6 months, the HF hospitalization rate was significantly lower among those in the treatment group. The FDA statement noted that at 6 months, almost 99% of the patients who had the device implanted or in whom implantation was attempted had no complications related to the device or system, and all of the devices that were implanted were operating normally.
However, concerns about the study held up approval of the device for several years, and at a meeting in December 2011, the majority of the FDA’s Circulatory System Devices Panel agreed that the risks of the device outweighed the benefits. The manufacturer, CardioMEMS, provided follow-up data and further analyses of the data that were provided at another meeting of the panel, in October 2013. At that meeting, the majority of the panel agreed that the benefits of the device outweighed its risks for monitoring patients who met the criteria specified in the indication that has been approved, patients with NYHA class III heart failure who have been hospitalized for HF in the previous year.
In the May 28 statement, the FDA said that the company is required to conduct a postmarketing study to evaluate the performance of the device when used outside of a clinical trial. One concern of the panelists who supported approval at the 2013 meeting was that the benefit in terms of HF hospitalizations was not evident in women in the study, which they said could have been due to the low number of women enrolled in the trial, and they recommended that the device be studied in more women.
An implantable device that provides measurements of pulmonary arterial pressure in patients with class III heart failure has been approved by the Food and Drug Administration, based on a study that showed the use of the device to remotely monitor patients reduced heart failure hospitalization rates.
The CardioMEMS HF System "is the first permanently implantable wireless system intended to provide PA pressure measurements, including systolic, diastolic, and mean PA pressures," according to the FDA statement announcing the approval on May 28. This information is remotely reviewed by the patient’s physician, who "can make decisions regarding the status of the patient and, if necessary, initiate changes in medical therapy, with the goal of reducing hospitalization due to heart failure," the statement said.
It is specifically approved for patients with New York Heart Association (NYHA) class III heart failure (HF) who have been hospitalized for heart failure in the previous year.
The three components of the system are the battery-free sensor/monitor that is permanently implanted in the pulmonary artery, a transvenous catheter that deploys the sensor in the distal PA, and an electronic system that receives and processes the signals from the sensor/monitor and transfers the PA pressure measurements to a secure database, the statement said. Patients can be monitored from their home or another remote location.
Approval was based on a study of 550 patients with NYHA class III HF and a recent hospitalization for HF, who had the device implanted. Physicians had access to daily PA measurements only for the patients randomized to the treatment group, and adjusted HF medications based on the values provided. At 6 months, the HF hospitalization rate was significantly lower among those in the treatment group. The FDA statement noted that at 6 months, almost 99% of the patients who had the device implanted or in whom implantation was attempted had no complications related to the device or system, and all of the devices that were implanted were operating normally.
However, concerns about the study held up approval of the device for several years, and at a meeting in December 2011, the majority of the FDA’s Circulatory System Devices Panel agreed that the risks of the device outweighed the benefits. The manufacturer, CardioMEMS, provided follow-up data and further analyses of the data that were provided at another meeting of the panel, in October 2013. At that meeting, the majority of the panel agreed that the benefits of the device outweighed its risks for monitoring patients who met the criteria specified in the indication that has been approved, patients with NYHA class III heart failure who have been hospitalized for HF in the previous year.
In the May 28 statement, the FDA said that the company is required to conduct a postmarketing study to evaluate the performance of the device when used outside of a clinical trial. One concern of the panelists who supported approval at the 2013 meeting was that the benefit in terms of HF hospitalizations was not evident in women in the study, which they said could have been due to the low number of women enrolled in the trial, and they recommended that the device be studied in more women.
An implantable device that provides measurements of pulmonary arterial pressure in patients with class III heart failure has been approved by the Food and Drug Administration, based on a study that showed the use of the device to remotely monitor patients reduced heart failure hospitalization rates.
The CardioMEMS HF System "is the first permanently implantable wireless system intended to provide PA pressure measurements, including systolic, diastolic, and mean PA pressures," according to the FDA statement announcing the approval on May 28. This information is remotely reviewed by the patient’s physician, who "can make decisions regarding the status of the patient and, if necessary, initiate changes in medical therapy, with the goal of reducing hospitalization due to heart failure," the statement said.
It is specifically approved for patients with New York Heart Association (NYHA) class III heart failure (HF) who have been hospitalized for heart failure in the previous year.
The three components of the system are the battery-free sensor/monitor that is permanently implanted in the pulmonary artery, a transvenous catheter that deploys the sensor in the distal PA, and an electronic system that receives and processes the signals from the sensor/monitor and transfers the PA pressure measurements to a secure database, the statement said. Patients can be monitored from their home or another remote location.
Approval was based on a study of 550 patients with NYHA class III HF and a recent hospitalization for HF, who had the device implanted. Physicians had access to daily PA measurements only for the patients randomized to the treatment group, and adjusted HF medications based on the values provided. At 6 months, the HF hospitalization rate was significantly lower among those in the treatment group. The FDA statement noted that at 6 months, almost 99% of the patients who had the device implanted or in whom implantation was attempted had no complications related to the device or system, and all of the devices that were implanted were operating normally.
However, concerns about the study held up approval of the device for several years, and at a meeting in December 2011, the majority of the FDA’s Circulatory System Devices Panel agreed that the risks of the device outweighed the benefits. The manufacturer, CardioMEMS, provided follow-up data and further analyses of the data that were provided at another meeting of the panel, in October 2013. At that meeting, the majority of the panel agreed that the benefits of the device outweighed its risks for monitoring patients who met the criteria specified in the indication that has been approved, patients with NYHA class III heart failure who have been hospitalized for HF in the previous year.
In the May 28 statement, the FDA said that the company is required to conduct a postmarketing study to evaluate the performance of the device when used outside of a clinical trial. One concern of the panelists who supported approval at the 2013 meeting was that the benefit in terms of HF hospitalizations was not evident in women in the study, which they said could have been due to the low number of women enrolled in the trial, and they recommended that the device be studied in more women.
Registry renal denervation skews from resistant hypertension
WASHINGTON – Renal denervation may have struck out as antihypertensive therapy in the sham-controlled SYMPLICITY HTN-3 trial reported in March at the American College of Cardiology’s annual meeting, but an independent report at the same meeting from a worldwide renal denervation registry showed that the vast majority of patients who’ve undergone with renal denervation recently were nothing like the patients enrolled in the failed trial.
In fact, patients who met enrollment criteria for the SYMPLICITY HTN-3 trial constituted a bare 8% of "real world" patients treated with renal denervation, based on results from the first 1,000 patients enrolled in the Global SYMPLICITY Registry, said Dr. Michael Böhm, professor and chairman of cardiology at Saarland University Hospital in Homburg/Saar, Germany.
Out of the 751 patients of the first 1,000 in the registry with data available on their office systolic blood pressure 6 months after treatment, 62 patients (8%) fulfilled the entry criteria of the SYMPLICITY HTN-3 (Renal Denervation in Patients With Uncontrolled Hypertension) trial by having an office systolic pressure of at least 160 mm Hg, a systolic pressure of at least 135 mm Hg by ambulatory blood pressure monitoring, and on treatment at maximally tolerated dosages with at least three different classes of antihypertensive medications (N. Engl. J. Med. 2014;370:1393-1401).
This low level of patients with clinically confirmed, resistant hypertension occurred against a backdrop in which a scant majority of registry patients even had severe hypertension, let alone a medically uncontrolled form. Among the 751 patients with 6-month follow-up blood pressure data, 433 (58%) received renal denervation with an office systolic blood pressure at baseline of at least 160 mm Hg, said Dr. Böhm.
"SYMPLICITY HTN-3 covered only a few percent of patients" who undergo renal denervation, he said. "The goal of the registry is to include a broad population, including patients without hypertension but other conditions associated with overactivity of the sympathetic nervous system" such as arrhythmia or heart failure.
Among the 433 patients with an office systolic blood pressure of at least 160 mm Hg – the minimum level of hypertension to warrant routine treatment by renal denervation according to several current policies – 244 (56%) were at this high pressure despite treatment with at least three classes of antihypertensive drugs. In this more clearly drug-resistant group, office systolic pressure fell by an average 20.2 mm Hg at 6 months after renal denervation. But only 62 patients on at least three types of drugs were also at maximally tolerated dosages of these drugs, another key element in defining drug resistance. Patients on maximally tolerated dosages represented only a quarter of all patients on multiple drugs in the Registry, and just 14% of the 433 patients with severe hypertension.
Among the 62 patients who matched the SYMPLICITY HTN-3 enrollment criteria, the average drop in office, systolic blood pressure at 6 months after treatment was 17.3 mm Hg, not too different from the average drop of 14.1 mm Hg seen in the renal denervation arm of SYMPLICITY HTN-3, Dr. Böhm noted.
The registry results showed that in patients with an office systolic pressure of less than 160 mm Hg, renal denervation was lousy at blood pressure reduction. Among the 222 patients who had pretreatment systolic pressures of 140-159 mm Hg and 6-month follow-up, office systolic blood pressure dropped by an average of 4.6 mm Hg. The procedure was even less effective in the 96 registry patients with an office systolic pressure of less than 140 mm Hg prior to treatment. In this subgroup systolic pressures averaged a 14.2-mm Hg increase 6 months after treatment.
"The only significant interaction between blood pressure lowering and no lowering was blood pressure at baseline," Dr. Böhm said. He gave no details on how many patients in the registry underwent renal denervation to treat hypertension and how many for other reasons.
The Global SYMPLICITY Register involves more than 200 centers in many European countries as well as in Canada, Australia, Korea, and elsewhere. A large number of registry centers are in Germany, and many centers there and elsewhere participated in the first two SYMPLICITY HTN trials. Participating centers entered the registry based on their experience with renal denervation and had to have performed at least 30 procedures prior to entry into the registry. The 6-month data also showed that renal denervation was "very safe," with "very low" rates of adverse events, Dr. Böhm said.
The Global SYMPLICITY Registry is sponsored by Medtronic, the company that markets Symplicity renal denervation devices. Dr, Böhm said that he has served on an advisory board to, been a speaker for, and received research support from Medtronic as well as from several other drug and device companies.
On Twitter @mitchelzoler
WASHINGTON – Renal denervation may have struck out as antihypertensive therapy in the sham-controlled SYMPLICITY HTN-3 trial reported in March at the American College of Cardiology’s annual meeting, but an independent report at the same meeting from a worldwide renal denervation registry showed that the vast majority of patients who’ve undergone with renal denervation recently were nothing like the patients enrolled in the failed trial.
In fact, patients who met enrollment criteria for the SYMPLICITY HTN-3 trial constituted a bare 8% of "real world" patients treated with renal denervation, based on results from the first 1,000 patients enrolled in the Global SYMPLICITY Registry, said Dr. Michael Böhm, professor and chairman of cardiology at Saarland University Hospital in Homburg/Saar, Germany.
Out of the 751 patients of the first 1,000 in the registry with data available on their office systolic blood pressure 6 months after treatment, 62 patients (8%) fulfilled the entry criteria of the SYMPLICITY HTN-3 (Renal Denervation in Patients With Uncontrolled Hypertension) trial by having an office systolic pressure of at least 160 mm Hg, a systolic pressure of at least 135 mm Hg by ambulatory blood pressure monitoring, and on treatment at maximally tolerated dosages with at least three different classes of antihypertensive medications (N. Engl. J. Med. 2014;370:1393-1401).
This low level of patients with clinically confirmed, resistant hypertension occurred against a backdrop in which a scant majority of registry patients even had severe hypertension, let alone a medically uncontrolled form. Among the 751 patients with 6-month follow-up blood pressure data, 433 (58%) received renal denervation with an office systolic blood pressure at baseline of at least 160 mm Hg, said Dr. Böhm.
"SYMPLICITY HTN-3 covered only a few percent of patients" who undergo renal denervation, he said. "The goal of the registry is to include a broad population, including patients without hypertension but other conditions associated with overactivity of the sympathetic nervous system" such as arrhythmia or heart failure.
Among the 433 patients with an office systolic blood pressure of at least 160 mm Hg – the minimum level of hypertension to warrant routine treatment by renal denervation according to several current policies – 244 (56%) were at this high pressure despite treatment with at least three classes of antihypertensive drugs. In this more clearly drug-resistant group, office systolic pressure fell by an average 20.2 mm Hg at 6 months after renal denervation. But only 62 patients on at least three types of drugs were also at maximally tolerated dosages of these drugs, another key element in defining drug resistance. Patients on maximally tolerated dosages represented only a quarter of all patients on multiple drugs in the Registry, and just 14% of the 433 patients with severe hypertension.
Among the 62 patients who matched the SYMPLICITY HTN-3 enrollment criteria, the average drop in office, systolic blood pressure at 6 months after treatment was 17.3 mm Hg, not too different from the average drop of 14.1 mm Hg seen in the renal denervation arm of SYMPLICITY HTN-3, Dr. Böhm noted.
The registry results showed that in patients with an office systolic pressure of less than 160 mm Hg, renal denervation was lousy at blood pressure reduction. Among the 222 patients who had pretreatment systolic pressures of 140-159 mm Hg and 6-month follow-up, office systolic blood pressure dropped by an average of 4.6 mm Hg. The procedure was even less effective in the 96 registry patients with an office systolic pressure of less than 140 mm Hg prior to treatment. In this subgroup systolic pressures averaged a 14.2-mm Hg increase 6 months after treatment.
"The only significant interaction between blood pressure lowering and no lowering was blood pressure at baseline," Dr. Böhm said. He gave no details on how many patients in the registry underwent renal denervation to treat hypertension and how many for other reasons.
The Global SYMPLICITY Register involves more than 200 centers in many European countries as well as in Canada, Australia, Korea, and elsewhere. A large number of registry centers are in Germany, and many centers there and elsewhere participated in the first two SYMPLICITY HTN trials. Participating centers entered the registry based on their experience with renal denervation and had to have performed at least 30 procedures prior to entry into the registry. The 6-month data also showed that renal denervation was "very safe," with "very low" rates of adverse events, Dr. Böhm said.
The Global SYMPLICITY Registry is sponsored by Medtronic, the company that markets Symplicity renal denervation devices. Dr, Böhm said that he has served on an advisory board to, been a speaker for, and received research support from Medtronic as well as from several other drug and device companies.
On Twitter @mitchelzoler
WASHINGTON – Renal denervation may have struck out as antihypertensive therapy in the sham-controlled SYMPLICITY HTN-3 trial reported in March at the American College of Cardiology’s annual meeting, but an independent report at the same meeting from a worldwide renal denervation registry showed that the vast majority of patients who’ve undergone with renal denervation recently were nothing like the patients enrolled in the failed trial.
In fact, patients who met enrollment criteria for the SYMPLICITY HTN-3 trial constituted a bare 8% of "real world" patients treated with renal denervation, based on results from the first 1,000 patients enrolled in the Global SYMPLICITY Registry, said Dr. Michael Böhm, professor and chairman of cardiology at Saarland University Hospital in Homburg/Saar, Germany.
Out of the 751 patients of the first 1,000 in the registry with data available on their office systolic blood pressure 6 months after treatment, 62 patients (8%) fulfilled the entry criteria of the SYMPLICITY HTN-3 (Renal Denervation in Patients With Uncontrolled Hypertension) trial by having an office systolic pressure of at least 160 mm Hg, a systolic pressure of at least 135 mm Hg by ambulatory blood pressure monitoring, and on treatment at maximally tolerated dosages with at least three different classes of antihypertensive medications (N. Engl. J. Med. 2014;370:1393-1401).
This low level of patients with clinically confirmed, resistant hypertension occurred against a backdrop in which a scant majority of registry patients even had severe hypertension, let alone a medically uncontrolled form. Among the 751 patients with 6-month follow-up blood pressure data, 433 (58%) received renal denervation with an office systolic blood pressure at baseline of at least 160 mm Hg, said Dr. Böhm.
"SYMPLICITY HTN-3 covered only a few percent of patients" who undergo renal denervation, he said. "The goal of the registry is to include a broad population, including patients without hypertension but other conditions associated with overactivity of the sympathetic nervous system" such as arrhythmia or heart failure.
Among the 433 patients with an office systolic blood pressure of at least 160 mm Hg – the minimum level of hypertension to warrant routine treatment by renal denervation according to several current policies – 244 (56%) were at this high pressure despite treatment with at least three classes of antihypertensive drugs. In this more clearly drug-resistant group, office systolic pressure fell by an average 20.2 mm Hg at 6 months after renal denervation. But only 62 patients on at least three types of drugs were also at maximally tolerated dosages of these drugs, another key element in defining drug resistance. Patients on maximally tolerated dosages represented only a quarter of all patients on multiple drugs in the Registry, and just 14% of the 433 patients with severe hypertension.
Among the 62 patients who matched the SYMPLICITY HTN-3 enrollment criteria, the average drop in office, systolic blood pressure at 6 months after treatment was 17.3 mm Hg, not too different from the average drop of 14.1 mm Hg seen in the renal denervation arm of SYMPLICITY HTN-3, Dr. Böhm noted.
The registry results showed that in patients with an office systolic pressure of less than 160 mm Hg, renal denervation was lousy at blood pressure reduction. Among the 222 patients who had pretreatment systolic pressures of 140-159 mm Hg and 6-month follow-up, office systolic blood pressure dropped by an average of 4.6 mm Hg. The procedure was even less effective in the 96 registry patients with an office systolic pressure of less than 140 mm Hg prior to treatment. In this subgroup systolic pressures averaged a 14.2-mm Hg increase 6 months after treatment.
"The only significant interaction between blood pressure lowering and no lowering was blood pressure at baseline," Dr. Böhm said. He gave no details on how many patients in the registry underwent renal denervation to treat hypertension and how many for other reasons.
The Global SYMPLICITY Register involves more than 200 centers in many European countries as well as in Canada, Australia, Korea, and elsewhere. A large number of registry centers are in Germany, and many centers there and elsewhere participated in the first two SYMPLICITY HTN trials. Participating centers entered the registry based on their experience with renal denervation and had to have performed at least 30 procedures prior to entry into the registry. The 6-month data also showed that renal denervation was "very safe," with "very low" rates of adverse events, Dr. Böhm said.
The Global SYMPLICITY Registry is sponsored by Medtronic, the company that markets Symplicity renal denervation devices. Dr, Böhm said that he has served on an advisory board to, been a speaker for, and received research support from Medtronic as well as from several other drug and device companies.
On Twitter @mitchelzoler
AT ACC 2014
Key clinical point: Real-world use of renal denervation has not targeted patients with drug-resistant hypertension.
Major finding: Only 8% of patient in the Global SYMPLICITY Registry for renal denervation matched the patients enrolled in the SYMPLICITY HTN-3 trial.
Data source: The Global SYMPLICITY Registry, which enrolled 1,000 patients who underwent renal denervation at more than 200 centers worldwide.
Disclosures: The registry is sponsored by Medtronic, the company that markets Symplicity renal denervation devices. Dr, Böhm said that he has served on an advisory board to, been a speaker for, and received research support from Medtronic as well as from several other drug and device companies.
In diabetes, women far more likely to develop CHD than men
Women with diabetes have a 44% greater chance of developing coronary heart disease than do men with diabetes, a large review and meta-analysis has shown.
In a retrospective review of data from more than 850,000 people that included over 28,000 confirmed coronary heart disease (CHD) events across the globe between 1966 and 2011, women with diabetes had nearly three times the likelihood (relative risk, 2.82) of developing CHD than did women without diabetes. Meanwhile, men with diabetes were only twice as likely (RR, 2.16) to have CHD than men without the disease. After adjustment for sex differences in other CHD factors such as tobacco use, women with diabetes had a 44% increased risk of developing heart disease, compared with men with the disease (RR, 1.44).
Sex differences in diabetes-related risk for CHD remained consistent across subgroups defined by age and region, and were unchanged when factoring nonfatal CHD events.
The study, conducted by researchers from Europe and Australia, appears online in Diabetologia 2014 [doi:10.1007/s00125-014-3260-6]. The findings corroborate a previous meta-analysis that also showed clinically meaningful sex differences lead to a greater CHD risk in women with diabetes than in men with diabetes (BMJ 2006;332:73-8 [doi:10.1136/bmj.38678.389583.7C]. Dr. Rachel Huxley of the University of Queensland School of Population Health in Australia, was an investigator in both studies.
Reasons for the disparity cannot be attributed to pharmacotherapy alone, according to the authors of the current study. Data reviewed in the study showed that women with diabetes were undertreated for cardiovascular disease risk factors prior to 1986, but that despite current increased awareness of the cardiovascular risks posed to women with diabetes, they are still less likely to achieve treatment targets.
“We hypothesize that the excess risk in women is due to a combination of both a greater deterioration in cardiovascular risk factor levels and a chronically elevated cardiovascular risk profile in the prediabetic state, driven by greater levels of adiposity in women, compared with men,” the authors wrote.
The authors cited previous research indicating that men develop diabetes at a lower body mass index (BMI), compared with women. As an example, in the UK General Practice Research Database, the BMI of those diagnosed with diabetes was on average 1.8 kg/m2 higher in women than in men. (Diabetologia 2012;55:1556-7).
“Greater awareness of early symptoms of CHD in women and sex-specific therapeutic risk factor management, irrespective of the presence of diabetes, is optimal for improving clinical outcomes in both women and men,” the authors concluded.
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
Women with diabetes have a 44% greater chance of developing coronary heart disease than do men with diabetes, a large review and meta-analysis has shown.
In a retrospective review of data from more than 850,000 people that included over 28,000 confirmed coronary heart disease (CHD) events across the globe between 1966 and 2011, women with diabetes had nearly three times the likelihood (relative risk, 2.82) of developing CHD than did women without diabetes. Meanwhile, men with diabetes were only twice as likely (RR, 2.16) to have CHD than men without the disease. After adjustment for sex differences in other CHD factors such as tobacco use, women with diabetes had a 44% increased risk of developing heart disease, compared with men with the disease (RR, 1.44).
Sex differences in diabetes-related risk for CHD remained consistent across subgroups defined by age and region, and were unchanged when factoring nonfatal CHD events.
The study, conducted by researchers from Europe and Australia, appears online in Diabetologia 2014 [doi:10.1007/s00125-014-3260-6]. The findings corroborate a previous meta-analysis that also showed clinically meaningful sex differences lead to a greater CHD risk in women with diabetes than in men with diabetes (BMJ 2006;332:73-8 [doi:10.1136/bmj.38678.389583.7C]. Dr. Rachel Huxley of the University of Queensland School of Population Health in Australia, was an investigator in both studies.
Reasons for the disparity cannot be attributed to pharmacotherapy alone, according to the authors of the current study. Data reviewed in the study showed that women with diabetes were undertreated for cardiovascular disease risk factors prior to 1986, but that despite current increased awareness of the cardiovascular risks posed to women with diabetes, they are still less likely to achieve treatment targets.
“We hypothesize that the excess risk in women is due to a combination of both a greater deterioration in cardiovascular risk factor levels and a chronically elevated cardiovascular risk profile in the prediabetic state, driven by greater levels of adiposity in women, compared with men,” the authors wrote.
The authors cited previous research indicating that men develop diabetes at a lower body mass index (BMI), compared with women. As an example, in the UK General Practice Research Database, the BMI of those diagnosed with diabetes was on average 1.8 kg/m2 higher in women than in men. (Diabetologia 2012;55:1556-7).
“Greater awareness of early symptoms of CHD in women and sex-specific therapeutic risk factor management, irrespective of the presence of diabetes, is optimal for improving clinical outcomes in both women and men,” the authors concluded.
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
Women with diabetes have a 44% greater chance of developing coronary heart disease than do men with diabetes, a large review and meta-analysis has shown.
In a retrospective review of data from more than 850,000 people that included over 28,000 confirmed coronary heart disease (CHD) events across the globe between 1966 and 2011, women with diabetes had nearly three times the likelihood (relative risk, 2.82) of developing CHD than did women without diabetes. Meanwhile, men with diabetes were only twice as likely (RR, 2.16) to have CHD than men without the disease. After adjustment for sex differences in other CHD factors such as tobacco use, women with diabetes had a 44% increased risk of developing heart disease, compared with men with the disease (RR, 1.44).
Sex differences in diabetes-related risk for CHD remained consistent across subgroups defined by age and region, and were unchanged when factoring nonfatal CHD events.
The study, conducted by researchers from Europe and Australia, appears online in Diabetologia 2014 [doi:10.1007/s00125-014-3260-6]. The findings corroborate a previous meta-analysis that also showed clinically meaningful sex differences lead to a greater CHD risk in women with diabetes than in men with diabetes (BMJ 2006;332:73-8 [doi:10.1136/bmj.38678.389583.7C]. Dr. Rachel Huxley of the University of Queensland School of Population Health in Australia, was an investigator in both studies.
Reasons for the disparity cannot be attributed to pharmacotherapy alone, according to the authors of the current study. Data reviewed in the study showed that women with diabetes were undertreated for cardiovascular disease risk factors prior to 1986, but that despite current increased awareness of the cardiovascular risks posed to women with diabetes, they are still less likely to achieve treatment targets.
“We hypothesize that the excess risk in women is due to a combination of both a greater deterioration in cardiovascular risk factor levels and a chronically elevated cardiovascular risk profile in the prediabetic state, driven by greater levels of adiposity in women, compared with men,” the authors wrote.
The authors cited previous research indicating that men develop diabetes at a lower body mass index (BMI), compared with women. As an example, in the UK General Practice Research Database, the BMI of those diagnosed with diabetes was on average 1.8 kg/m2 higher in women than in men. (Diabetologia 2012;55:1556-7).
“Greater awareness of early symptoms of CHD in women and sex-specific therapeutic risk factor management, irrespective of the presence of diabetes, is optimal for improving clinical outcomes in both women and men,” the authors concluded.
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
FROM DIABETOLOGIA
Key clinical point: Consider screening asymptomatic women for diabetes and offering risk
factor management.
Major finding: Women with diabetes are 44% more
likely to develop CHD than men with diabetes.
Data source: Systematic review and meta-analysis of
more than 850,000 people and over 28,000 CHD events recorded in 64 studies
worldwide between 1966 and 2011.
Disclosures: The authors of this study declared
they had no relevant disclosures.
Heart failure: Quality of life, diastolic function rose with intensity-interval exercise
WASHINGTON – A high-intensity cardiac rehabilitation program safely improved quality of life, diastolic function, depressive symptoms, and physical fitness in patients with systolic heart failure and reduced ejection fraction in a randomized controlled trial.
In the subgroup of study participants over age 65, however, the benefits were limited and the dropout rate high, Dr. Christina Chrysohoou said at the annual meeting of the American College of Cardiology. "I think patients over age 65 may benefit more from a less-intensive exercise time and rest periods."
Her study included 100 consecutive patients with a left ventricular ejection fraction (LVEF) below 30%; heart failure of ischemic etiology was present in 70%. One-third of subjects had an implantable cardioverter-defibrillator at study entry. All participants underwent pre-enrollment Holter monitoring with electrophysiologic follow-up as warranted. Participants were randomized to a high-intensity exercise program or to a control arm of standard dietary advice and a recommendation to walk for up to 2 miles daily, said Dr. Chrysohoou, a cardiologist at the University of Athens.
The exercise program consisted of a warm-up followed a 30-minute session of alternating 30-second bursts of ergometric exercise at 100% of a patient’s maximum workload followed by 30 seconds of recovery at 40%-60% of maximum workload. Maximum workload was determined from a baseline treadmill exercise test. The 12-week study was completed by 33 of 50 patients in the high-intensity exercise group and 39 of 50 controls.
Quality of life scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean score of 21 at baseline to 7 in the intensive-exercise group, and declined slightly from 19 to 21 in the control group.
At baseline, the mean score on the Zung Depression Scale was 37 out of a possible 80; at 12 weeks, scores improved to 30 in the high-intensity exercise group and increased to 41 in the controls.
Maximal oxygen consumption, or VO2max, improved from 16 to 21 mL/kg per minute in the interval-exercise group while remaining unchanged in controls. Similarly, peak power output increased from 84 to 105 W in the exercise program participants while remaining unchanged in controls. Six-minute walk time improved from 422 m to 476 m in the intensive exercisers, a 13% better result than that seen in controls.
Diastolic function on Doppler imaging significantly improved in the exercise group but not in the controls. The E/A wave ratio, which represents the relationship between early passive left ventricular filling and atrial contraction in late diastole, decreased by 24%. Also, the left ventricular outflow velocity integral increased by 4%.
There were no adverse events in either study arm.
LVEF did not significantly improve in either study arm, but that was not surprising, said Dr. Chrysohoou. "You may have an LVEF of 20% and be able to run a marathon, or an LVEF of 30%-35% and not even be able to walk around the house."
This was an unfunded study, and Dr. Chrysohoou reported having no financial conflicts.
WASHINGTON – A high-intensity cardiac rehabilitation program safely improved quality of life, diastolic function, depressive symptoms, and physical fitness in patients with systolic heart failure and reduced ejection fraction in a randomized controlled trial.
In the subgroup of study participants over age 65, however, the benefits were limited and the dropout rate high, Dr. Christina Chrysohoou said at the annual meeting of the American College of Cardiology. "I think patients over age 65 may benefit more from a less-intensive exercise time and rest periods."
Her study included 100 consecutive patients with a left ventricular ejection fraction (LVEF) below 30%; heart failure of ischemic etiology was present in 70%. One-third of subjects had an implantable cardioverter-defibrillator at study entry. All participants underwent pre-enrollment Holter monitoring with electrophysiologic follow-up as warranted. Participants were randomized to a high-intensity exercise program or to a control arm of standard dietary advice and a recommendation to walk for up to 2 miles daily, said Dr. Chrysohoou, a cardiologist at the University of Athens.
The exercise program consisted of a warm-up followed a 30-minute session of alternating 30-second bursts of ergometric exercise at 100% of a patient’s maximum workload followed by 30 seconds of recovery at 40%-60% of maximum workload. Maximum workload was determined from a baseline treadmill exercise test. The 12-week study was completed by 33 of 50 patients in the high-intensity exercise group and 39 of 50 controls.
Quality of life scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean score of 21 at baseline to 7 in the intensive-exercise group, and declined slightly from 19 to 21 in the control group.
At baseline, the mean score on the Zung Depression Scale was 37 out of a possible 80; at 12 weeks, scores improved to 30 in the high-intensity exercise group and increased to 41 in the controls.
Maximal oxygen consumption, or VO2max, improved from 16 to 21 mL/kg per minute in the interval-exercise group while remaining unchanged in controls. Similarly, peak power output increased from 84 to 105 W in the exercise program participants while remaining unchanged in controls. Six-minute walk time improved from 422 m to 476 m in the intensive exercisers, a 13% better result than that seen in controls.
Diastolic function on Doppler imaging significantly improved in the exercise group but not in the controls. The E/A wave ratio, which represents the relationship between early passive left ventricular filling and atrial contraction in late diastole, decreased by 24%. Also, the left ventricular outflow velocity integral increased by 4%.
There were no adverse events in either study arm.
LVEF did not significantly improve in either study arm, but that was not surprising, said Dr. Chrysohoou. "You may have an LVEF of 20% and be able to run a marathon, or an LVEF of 30%-35% and not even be able to walk around the house."
This was an unfunded study, and Dr. Chrysohoou reported having no financial conflicts.
WASHINGTON – A high-intensity cardiac rehabilitation program safely improved quality of life, diastolic function, depressive symptoms, and physical fitness in patients with systolic heart failure and reduced ejection fraction in a randomized controlled trial.
In the subgroup of study participants over age 65, however, the benefits were limited and the dropout rate high, Dr. Christina Chrysohoou said at the annual meeting of the American College of Cardiology. "I think patients over age 65 may benefit more from a less-intensive exercise time and rest periods."
Her study included 100 consecutive patients with a left ventricular ejection fraction (LVEF) below 30%; heart failure of ischemic etiology was present in 70%. One-third of subjects had an implantable cardioverter-defibrillator at study entry. All participants underwent pre-enrollment Holter monitoring with electrophysiologic follow-up as warranted. Participants were randomized to a high-intensity exercise program or to a control arm of standard dietary advice and a recommendation to walk for up to 2 miles daily, said Dr. Chrysohoou, a cardiologist at the University of Athens.
The exercise program consisted of a warm-up followed a 30-minute session of alternating 30-second bursts of ergometric exercise at 100% of a patient’s maximum workload followed by 30 seconds of recovery at 40%-60% of maximum workload. Maximum workload was determined from a baseline treadmill exercise test. The 12-week study was completed by 33 of 50 patients in the high-intensity exercise group and 39 of 50 controls.
Quality of life scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean score of 21 at baseline to 7 in the intensive-exercise group, and declined slightly from 19 to 21 in the control group.
At baseline, the mean score on the Zung Depression Scale was 37 out of a possible 80; at 12 weeks, scores improved to 30 in the high-intensity exercise group and increased to 41 in the controls.
Maximal oxygen consumption, or VO2max, improved from 16 to 21 mL/kg per minute in the interval-exercise group while remaining unchanged in controls. Similarly, peak power output increased from 84 to 105 W in the exercise program participants while remaining unchanged in controls. Six-minute walk time improved from 422 m to 476 m in the intensive exercisers, a 13% better result than that seen in controls.
Diastolic function on Doppler imaging significantly improved in the exercise group but not in the controls. The E/A wave ratio, which represents the relationship between early passive left ventricular filling and atrial contraction in late diastole, decreased by 24%. Also, the left ventricular outflow velocity integral increased by 4%.
There were no adverse events in either study arm.
LVEF did not significantly improve in either study arm, but that was not surprising, said Dr. Chrysohoou. "You may have an LVEF of 20% and be able to run a marathon, or an LVEF of 30%-35% and not even be able to walk around the house."
This was an unfunded study, and Dr. Chrysohoou reported having no financial conflicts.
AT ACC 14
Key clinical point: Cardiac rehabilitation benefits systolic heart failure patients, especially those under age 65.
Major finding: Quality of life scores on the Minnesota Living with Heart Failure Questionnaire improved from a mean of 21 to 7 over the course of a 12-week structured program of high-intensity interval exercise.
Data source: A 12-week, randomized, prospective study of 100 consecutive patients with heart failure and an LVEF below 30%.
Disclosures: This study was unfunded, and Dr. Chrysohoou reported having no financial conflicts.
FDA rejects serelaxin for acute heart failure
The Food and Drug Administration has decided that more evidence of serelaxin’s efficacy as a treatment for acute heart failure is needed before the drug can be approved in the United States, Novartis Pharmaceuticals announced May 16.
Serelaxin is a recombinant form of human relaxin-2 hormone that is administered in an intravenous infusion over 48 hours. For approval, the company submitted data from the phase III RELAX-AHF study, an international, randomized, placebo-controlled, double-blind study of about 1,100 patients with acute heart failure. At a meeting in March, the FDA’s Cardiovascular and Renal Drugs Advisory Committee agreed there was evidence that serelaxin had a positive effect on worsening heart failure in the study and that the data were promising, but unanimously voted against recommending approval, citing the need for more studies.
"In accordance with the FDA’s advice we will continue to expedite our clinical trial program to build the supporting body of evidence," Tim Wright, global head of development of the company, said in a statement issued by the company. He added that the company was encouraged by the FDA panel’s feedback.
The company is collecting more data on the drug in acute heart failure, which includes the RELAX-AHF-2 study, which will enroll more than 6,300 patients, according to the statement.
The FDA informs companies about nonapproval decisions in complete response letters, which include advice about what would be needed before the drug can be approved. The FDA does not announce these decisions, but companies often announce when these decisions are made.
The Food and Drug Administration has decided that more evidence of serelaxin’s efficacy as a treatment for acute heart failure is needed before the drug can be approved in the United States, Novartis Pharmaceuticals announced May 16.
Serelaxin is a recombinant form of human relaxin-2 hormone that is administered in an intravenous infusion over 48 hours. For approval, the company submitted data from the phase III RELAX-AHF study, an international, randomized, placebo-controlled, double-blind study of about 1,100 patients with acute heart failure. At a meeting in March, the FDA’s Cardiovascular and Renal Drugs Advisory Committee agreed there was evidence that serelaxin had a positive effect on worsening heart failure in the study and that the data were promising, but unanimously voted against recommending approval, citing the need for more studies.
"In accordance with the FDA’s advice we will continue to expedite our clinical trial program to build the supporting body of evidence," Tim Wright, global head of development of the company, said in a statement issued by the company. He added that the company was encouraged by the FDA panel’s feedback.
The company is collecting more data on the drug in acute heart failure, which includes the RELAX-AHF-2 study, which will enroll more than 6,300 patients, according to the statement.
The FDA informs companies about nonapproval decisions in complete response letters, which include advice about what would be needed before the drug can be approved. The FDA does not announce these decisions, but companies often announce when these decisions are made.
The Food and Drug Administration has decided that more evidence of serelaxin’s efficacy as a treatment for acute heart failure is needed before the drug can be approved in the United States, Novartis Pharmaceuticals announced May 16.
Serelaxin is a recombinant form of human relaxin-2 hormone that is administered in an intravenous infusion over 48 hours. For approval, the company submitted data from the phase III RELAX-AHF study, an international, randomized, placebo-controlled, double-blind study of about 1,100 patients with acute heart failure. At a meeting in March, the FDA’s Cardiovascular and Renal Drugs Advisory Committee agreed there was evidence that serelaxin had a positive effect on worsening heart failure in the study and that the data were promising, but unanimously voted against recommending approval, citing the need for more studies.
"In accordance with the FDA’s advice we will continue to expedite our clinical trial program to build the supporting body of evidence," Tim Wright, global head of development of the company, said in a statement issued by the company. He added that the company was encouraged by the FDA panel’s feedback.
The company is collecting more data on the drug in acute heart failure, which includes the RELAX-AHF-2 study, which will enroll more than 6,300 patients, according to the statement.
The FDA informs companies about nonapproval decisions in complete response letters, which include advice about what would be needed before the drug can be approved. The FDA does not announce these decisions, but companies often announce when these decisions are made.
20-study analysis finds no MACE increase with saxagliptin
Treatment with saxagliptin was not associated with an increased risk of major adverse cardiovascular events or heart failure in a pooled analysis of 20 studies of patients with type 2 diabetes.
The analysis also found no association with saxagliptin therapy and individual components of the major adverse cardiovascular events (MACE) endpoint, a composite of cardiovascular death, myocardial infarction, and stroke, according to a study being presented at the meeting. The results were released May 15 at the annual meeting of the American Association of Clinical Endocrinologists in Las Vegas.
Saxagliptin, a dipeptidyl peptidase–4 (DPP-44) inhibitor taken orally, was approved by the Food and Drug Administration in 2009 as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes.
The study evaluated adjudicated reports of MACE and investigator reports of heart failure associated with saxagliptin in 20 studies of saxagliptin as monotherapy or as add-on therapy in 9,156 patients with type 2 diabetes. Unlike the SAVOR-TIMI 53 study (Saxagliptin Assessment of Vascular Outcomes Recorded in Patient With Diabetes Mellitus–Thrombolysis in Myocardial Infarction 53) study, published in 2013, which found an increased risk of heart failure hospitalizations in patients with prior CV disease or multiple CV risk factors, the patients with type 2 diabetes enrolled in the 20 studies were at lower risk for CV events.
In the SAVOR-TIMI 53, which evaluated the drug’s cardiovascular safety in more than 16,000 patients with type 2 diabetes and established cardiovascular disease or risk factors for CHD, treatment with saxagliptin was not associated with an increased or reduced risk of ischemic risk for the composite of CV death, MI, or ischemic stroke, the primary endpoint, over a median of 2 years. But it was associated with a significantly greater risk of being hospitalized for heart failure (hazard ratio, 1.27) (N. Engl. J. Med. 2013;369:1317-26). In a January 2014 safety alert, the FDA said that the agency had requested the manufacturer of saxagliptin study “a possible association” between the use of the drug and heart failure, because of the increased risk of heart failure hospitalizations in that study.
In the 20-study analysis, based on 43 MACE reports in patients treated with saxagliptin and 31 MACE reports among controls, the MACE incidence rate (IR) – the number of events per 100 person-years – was 0.85/100 person-years for those on saxagliptin and 1.12/100 person-years for the controls. The IR ratio (the number of reports among saxagliptin-treated patients divided by the number of reports among the controls), was 0.74. The hazard ratio was 0.75, which suggests there is no increased risk of MACE associated with saxagliptin.
In a subset of 11 studies that evaluated saxagliptin as add-on therapy to metformin in 5,171 patients, the incidence rates were similar: 0.79/100 person-years for those on saxagliptin and 0.85/100 person-years for controls, with an IR ratio of 0.93.
In the 20 studies, the components of the MACE endpoint were also not statistically significantly different between those on saxagliptin and controls, and 21 patients on saxagliptin and 18 controls had heart failure, with an IR ratio of 0.55, he said.
Consistent with the SAVOR-TIMI 53 study, which analyzed MACE in patients with type 2 diabetes and cardiovascular disease or multiple cardiovascular risk factors, this 20-trial pooled analysis of patients from the general type 2 diabetes population found that saxagliptin was not associated with an increased risk of MACE or its components, or heart failure.
The pooled results “are somewhat reassuring in that the use of saxagliptin in patients with type 2 diabetes at lower risk for cardiovascular events is not associated with increased MACE risk,” and would have passed the FDA-recommended boundary for unacceptable risk for diabetes drugs (HR, 1.3), Dr. Sanjay Kaul said in an interview. However, he added, “it is disappointing that glycemic control did not translate into a macrovascular benefit, even though a lower risk population was evaluated.”
Moreover, the study “did not yield a sufficient number of heart failure events to reliably adjudicate the risk of heart failure in this patient population,” noted Dr. Kaul, professor of medicine, University of California, Los Angeles, who was not at the meeting. Dr. Kaul was a panelist at the FDA advisory panel meeting that reviewed the cardiovascular safety of rosiglitazone (Avandia) last year.
Three of the five authors are employed by Bristol-Myers Squibb; two are employed by AstraZeneca Dr. Kaul had no relevant disclosures related to saxagliptin; he has disclosures for diabetes agents manufactured by other companies.
Saxagliptin is marketed as Onglyza by AstraZeneca.
emechcatie@frontlinemedcom.com
Treatment with saxagliptin was not associated with an increased risk of major adverse cardiovascular events or heart failure in a pooled analysis of 20 studies of patients with type 2 diabetes.
The analysis also found no association with saxagliptin therapy and individual components of the major adverse cardiovascular events (MACE) endpoint, a composite of cardiovascular death, myocardial infarction, and stroke, according to a study being presented at the meeting. The results were released May 15 at the annual meeting of the American Association of Clinical Endocrinologists in Las Vegas.
Saxagliptin, a dipeptidyl peptidase–4 (DPP-44) inhibitor taken orally, was approved by the Food and Drug Administration in 2009 as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes.
The study evaluated adjudicated reports of MACE and investigator reports of heart failure associated with saxagliptin in 20 studies of saxagliptin as monotherapy or as add-on therapy in 9,156 patients with type 2 diabetes. Unlike the SAVOR-TIMI 53 study (Saxagliptin Assessment of Vascular Outcomes Recorded in Patient With Diabetes Mellitus–Thrombolysis in Myocardial Infarction 53) study, published in 2013, which found an increased risk of heart failure hospitalizations in patients with prior CV disease or multiple CV risk factors, the patients with type 2 diabetes enrolled in the 20 studies were at lower risk for CV events.
In the SAVOR-TIMI 53, which evaluated the drug’s cardiovascular safety in more than 16,000 patients with type 2 diabetes and established cardiovascular disease or risk factors for CHD, treatment with saxagliptin was not associated with an increased or reduced risk of ischemic risk for the composite of CV death, MI, or ischemic stroke, the primary endpoint, over a median of 2 years. But it was associated with a significantly greater risk of being hospitalized for heart failure (hazard ratio, 1.27) (N. Engl. J. Med. 2013;369:1317-26). In a January 2014 safety alert, the FDA said that the agency had requested the manufacturer of saxagliptin study “a possible association” between the use of the drug and heart failure, because of the increased risk of heart failure hospitalizations in that study.
In the 20-study analysis, based on 43 MACE reports in patients treated with saxagliptin and 31 MACE reports among controls, the MACE incidence rate (IR) – the number of events per 100 person-years – was 0.85/100 person-years for those on saxagliptin and 1.12/100 person-years for the controls. The IR ratio (the number of reports among saxagliptin-treated patients divided by the number of reports among the controls), was 0.74. The hazard ratio was 0.75, which suggests there is no increased risk of MACE associated with saxagliptin.
In a subset of 11 studies that evaluated saxagliptin as add-on therapy to metformin in 5,171 patients, the incidence rates were similar: 0.79/100 person-years for those on saxagliptin and 0.85/100 person-years for controls, with an IR ratio of 0.93.
In the 20 studies, the components of the MACE endpoint were also not statistically significantly different between those on saxagliptin and controls, and 21 patients on saxagliptin and 18 controls had heart failure, with an IR ratio of 0.55, he said.
Consistent with the SAVOR-TIMI 53 study, which analyzed MACE in patients with type 2 diabetes and cardiovascular disease or multiple cardiovascular risk factors, this 20-trial pooled analysis of patients from the general type 2 diabetes population found that saxagliptin was not associated with an increased risk of MACE or its components, or heart failure.
The pooled results “are somewhat reassuring in that the use of saxagliptin in patients with type 2 diabetes at lower risk for cardiovascular events is not associated with increased MACE risk,” and would have passed the FDA-recommended boundary for unacceptable risk for diabetes drugs (HR, 1.3), Dr. Sanjay Kaul said in an interview. However, he added, “it is disappointing that glycemic control did not translate into a macrovascular benefit, even though a lower risk population was evaluated.”
Moreover, the study “did not yield a sufficient number of heart failure events to reliably adjudicate the risk of heart failure in this patient population,” noted Dr. Kaul, professor of medicine, University of California, Los Angeles, who was not at the meeting. Dr. Kaul was a panelist at the FDA advisory panel meeting that reviewed the cardiovascular safety of rosiglitazone (Avandia) last year.
Three of the five authors are employed by Bristol-Myers Squibb; two are employed by AstraZeneca Dr. Kaul had no relevant disclosures related to saxagliptin; he has disclosures for diabetes agents manufactured by other companies.
Saxagliptin is marketed as Onglyza by AstraZeneca.
emechcatie@frontlinemedcom.com
Treatment with saxagliptin was not associated with an increased risk of major adverse cardiovascular events or heart failure in a pooled analysis of 20 studies of patients with type 2 diabetes.
The analysis also found no association with saxagliptin therapy and individual components of the major adverse cardiovascular events (MACE) endpoint, a composite of cardiovascular death, myocardial infarction, and stroke, according to a study being presented at the meeting. The results were released May 15 at the annual meeting of the American Association of Clinical Endocrinologists in Las Vegas.
Saxagliptin, a dipeptidyl peptidase–4 (DPP-44) inhibitor taken orally, was approved by the Food and Drug Administration in 2009 as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes.
The study evaluated adjudicated reports of MACE and investigator reports of heart failure associated with saxagliptin in 20 studies of saxagliptin as monotherapy or as add-on therapy in 9,156 patients with type 2 diabetes. Unlike the SAVOR-TIMI 53 study (Saxagliptin Assessment of Vascular Outcomes Recorded in Patient With Diabetes Mellitus–Thrombolysis in Myocardial Infarction 53) study, published in 2013, which found an increased risk of heart failure hospitalizations in patients with prior CV disease or multiple CV risk factors, the patients with type 2 diabetes enrolled in the 20 studies were at lower risk for CV events.
In the SAVOR-TIMI 53, which evaluated the drug’s cardiovascular safety in more than 16,000 patients with type 2 diabetes and established cardiovascular disease or risk factors for CHD, treatment with saxagliptin was not associated with an increased or reduced risk of ischemic risk for the composite of CV death, MI, or ischemic stroke, the primary endpoint, over a median of 2 years. But it was associated with a significantly greater risk of being hospitalized for heart failure (hazard ratio, 1.27) (N. Engl. J. Med. 2013;369:1317-26). In a January 2014 safety alert, the FDA said that the agency had requested the manufacturer of saxagliptin study “a possible association” between the use of the drug and heart failure, because of the increased risk of heart failure hospitalizations in that study.
In the 20-study analysis, based on 43 MACE reports in patients treated with saxagliptin and 31 MACE reports among controls, the MACE incidence rate (IR) – the number of events per 100 person-years – was 0.85/100 person-years for those on saxagliptin and 1.12/100 person-years for the controls. The IR ratio (the number of reports among saxagliptin-treated patients divided by the number of reports among the controls), was 0.74. The hazard ratio was 0.75, which suggests there is no increased risk of MACE associated with saxagliptin.
In a subset of 11 studies that evaluated saxagliptin as add-on therapy to metformin in 5,171 patients, the incidence rates were similar: 0.79/100 person-years for those on saxagliptin and 0.85/100 person-years for controls, with an IR ratio of 0.93.
In the 20 studies, the components of the MACE endpoint were also not statistically significantly different between those on saxagliptin and controls, and 21 patients on saxagliptin and 18 controls had heart failure, with an IR ratio of 0.55, he said.
Consistent with the SAVOR-TIMI 53 study, which analyzed MACE in patients with type 2 diabetes and cardiovascular disease or multiple cardiovascular risk factors, this 20-trial pooled analysis of patients from the general type 2 diabetes population found that saxagliptin was not associated with an increased risk of MACE or its components, or heart failure.
The pooled results “are somewhat reassuring in that the use of saxagliptin in patients with type 2 diabetes at lower risk for cardiovascular events is not associated with increased MACE risk,” and would have passed the FDA-recommended boundary for unacceptable risk for diabetes drugs (HR, 1.3), Dr. Sanjay Kaul said in an interview. However, he added, “it is disappointing that glycemic control did not translate into a macrovascular benefit, even though a lower risk population was evaluated.”
Moreover, the study “did not yield a sufficient number of heart failure events to reliably adjudicate the risk of heart failure in this patient population,” noted Dr. Kaul, professor of medicine, University of California, Los Angeles, who was not at the meeting. Dr. Kaul was a panelist at the FDA advisory panel meeting that reviewed the cardiovascular safety of rosiglitazone (Avandia) last year.
Three of the five authors are employed by Bristol-Myers Squibb; two are employed by AstraZeneca Dr. Kaul had no relevant disclosures related to saxagliptin; he has disclosures for diabetes agents manufactured by other companies.
Saxagliptin is marketed as Onglyza by AstraZeneca.
emechcatie@frontlinemedcom.com
FROM AACE 2014
Major finding: The incidence of MACE composite endpoint was similar among patients treated with saxagliptin (0.85/100 person-years) and controls (1.12/100 person-years) in 20 saxagliptin studies of patients with type 2 diabetes at a lower cardiovascular risk.
Data source: A pooled analysis of 20 randomized, controlled trials of saxagliptin as monotherapy or as add-on therapy in about 9,000 patients with type 2 diabetes compared the rates of the MACE endpoint and heart failure in patients on saxagliptin and controls.
Disclosures: Three of the five authors are employed by Bristol-Myers Squibb; two are employed by AstraZeneca.
OA-related walking disability on par with diabetes as CVD risk factor
PARIS – Greater walking disability is an independent predictor of all-cause death and major cardiovascular events in patients with symptomatic hip or knee osteoarthritis, according to a population-based study that confirms previous research.
For the composite cardiovascular disease (CVD) outcome of hospitalization for angina, acute myocardial infarction, coronary revascularization, congestive heart failure, stroke, or transient ischemic attack, the risk associated with a Health Assessment Questionnaire (HAQ) walking disability score of 2 was the same as that of diabetes and pre-existing CVD.
Total joint replacement reduced those risks by about 40%, Dr. Gillian A. Hawker said at the World Congress on Osteoarthritis (OA).
"I think the key piece here is that these data at least suggest that walking disability is a cardiovascular risk factor similar to diabetes," she said. "When we’re talking about risk assessment for cardiovascular outcomes, which everyone does pretty routinely in medicine, walking disability, which is really osteoarthritis, is one of the risk factors that they should be assessing ... If we can just start asking, hopefully it will get us thinking about, ‘Wow, this person has OA,’ and we need to start assessing it."
Session comoderator Ana M. Valdes, Ph.D., of the University of Nottingham (England) commented that the results are fascinating because this is not the first study to identify these associations. In 2011, British investigators reported that all-cause mortality, particularly due to CVD causes, was significantly related to baseline walking disability in patients with knee or hip OA (Br. Med. J. 2011;342:d1165).
"One of the things that happens often with OA is that it’s seen as just pain and if we can give them plenty of relief, they’ll be OK, but it’s actually life-threatening because if we do not address their disability, they are at risk of dying," Dr. Valdes said in an interview. "I think this should be put on the front pages of the weekly medical journals, so that people are aware of the dangers of not treating osteoarthritis properly."
Comorbidity is a barrier to OA care, and 90% of those aged 65 years and older with OA have at least one other chronic condition, such as diabetes and heart disease, observed Dr. Hawker, professor of medicine at the University of Toronto and physician-in-chief of medicine, Women’s College Hospital in Toronto.
Her group reported in a separate presentation at the meeting that walking disability also raises the risk for diabetes complications in those with both OA and diabetes.
For the current population-based study, the investigators linked provincial health administrative databases to baseline surveys from a population cohort of 2,156 patients with symptomatic moderate to severe OA who were recruited in 1996-1998 through a screening survey in Ontario.
Their mean age was 71 years (all were 55 years or older), 72% were female, 34% obese, 20% had diabetes, and 40% had prebaseline CVD. Their average HAQ walking disability score was 2 on a 3-point scale, and they had a mean WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) summary score of 41. Overall, 44% used a walking aid. (A walking disability score of 2 corresponds with walking outdoors on flat ground with much difficulty, whereas a score of 3 means the person is unable to do it.)
After a median follow-up period of 13.2 years, 57% of patients had died, and 38% experienced the composite CVD outcome with a median of 9.2 years follow-up.
In multivariable analysis, there was a very clear dose-response, where increased walking disability was associated with increasing risk of all-cause death, Dr. Hawker said. The adjusted hazard ratio per unit increase in HAQ walking score was 1.30 (P less than .001), after controlling for confounders including age, sex, preexisting CVD, diabetes, hypertension, body mass index, and smoking status.
A HAQ walking score of 2 was associated with an adjusted hazard ratio of 1.69, which was actually greater than that associated with preexisting cardiovascular disease or diabetes, she said.
For the composite CVD outcome, there was also a significant association with HAQ walking score (adjusted HR, 1.17; P = .001).
Sensitivity analyses performed in 402 patients (18%) receiving postbaseline total joint arthroplasty (TJA ) showed that controlling for TJA did not change the effect of baseline disability but was protective for both all-cause death (HR, 0.62; P less than .001) and CVD events (HR, 0.66; P less than .001), Dr. Hawker said at the meeting sponsored by the Osteoarthritis Research Society International.
Although the data were not dichotomized, she noted that there was "beautiful discrimination" when they looked at the outcomes based on whether or not patients used a walking aid.
"Obviously, it’s nice to see a dose-response, but simply knowing that someone’s using a walking aid and getting them to the point where they’ve got improved walking ability, could go a long way," she said.
Though the study was not designed to address potential mechanisms, Dr. Hawker said she’s long argued that physical activity and mobility are a key player of downstream effects on fitness, blood pressure, glucose control, and ability to participate in self-management activities and physician visits. The potential role for pain, mood, and stress also can not be excluded.
One audience member asked whether walking disability may be a "cheap and dirty version" of the stress test.
Dr. Hawker responded that walking disability is a proxy for a lot of things and is definitely OA-related, adding, "Yes, I think it is a very cheap and dirty stress test. It’s a lovely thing that if we focused more explicitly on it in randomized trials, for instance as a primary outcome, or in rehabilitation strategies, it would have global benefit."
The authors reported no competing interests.
PARIS – Greater walking disability is an independent predictor of all-cause death and major cardiovascular events in patients with symptomatic hip or knee osteoarthritis, according to a population-based study that confirms previous research.
For the composite cardiovascular disease (CVD) outcome of hospitalization for angina, acute myocardial infarction, coronary revascularization, congestive heart failure, stroke, or transient ischemic attack, the risk associated with a Health Assessment Questionnaire (HAQ) walking disability score of 2 was the same as that of diabetes and pre-existing CVD.
Total joint replacement reduced those risks by about 40%, Dr. Gillian A. Hawker said at the World Congress on Osteoarthritis (OA).
"I think the key piece here is that these data at least suggest that walking disability is a cardiovascular risk factor similar to diabetes," she said. "When we’re talking about risk assessment for cardiovascular outcomes, which everyone does pretty routinely in medicine, walking disability, which is really osteoarthritis, is one of the risk factors that they should be assessing ... If we can just start asking, hopefully it will get us thinking about, ‘Wow, this person has OA,’ and we need to start assessing it."
Session comoderator Ana M. Valdes, Ph.D., of the University of Nottingham (England) commented that the results are fascinating because this is not the first study to identify these associations. In 2011, British investigators reported that all-cause mortality, particularly due to CVD causes, was significantly related to baseline walking disability in patients with knee or hip OA (Br. Med. J. 2011;342:d1165).
"One of the things that happens often with OA is that it’s seen as just pain and if we can give them plenty of relief, they’ll be OK, but it’s actually life-threatening because if we do not address their disability, they are at risk of dying," Dr. Valdes said in an interview. "I think this should be put on the front pages of the weekly medical journals, so that people are aware of the dangers of not treating osteoarthritis properly."
Comorbidity is a barrier to OA care, and 90% of those aged 65 years and older with OA have at least one other chronic condition, such as diabetes and heart disease, observed Dr. Hawker, professor of medicine at the University of Toronto and physician-in-chief of medicine, Women’s College Hospital in Toronto.
Her group reported in a separate presentation at the meeting that walking disability also raises the risk for diabetes complications in those with both OA and diabetes.
For the current population-based study, the investigators linked provincial health administrative databases to baseline surveys from a population cohort of 2,156 patients with symptomatic moderate to severe OA who were recruited in 1996-1998 through a screening survey in Ontario.
Their mean age was 71 years (all were 55 years or older), 72% were female, 34% obese, 20% had diabetes, and 40% had prebaseline CVD. Their average HAQ walking disability score was 2 on a 3-point scale, and they had a mean WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) summary score of 41. Overall, 44% used a walking aid. (A walking disability score of 2 corresponds with walking outdoors on flat ground with much difficulty, whereas a score of 3 means the person is unable to do it.)
After a median follow-up period of 13.2 years, 57% of patients had died, and 38% experienced the composite CVD outcome with a median of 9.2 years follow-up.
In multivariable analysis, there was a very clear dose-response, where increased walking disability was associated with increasing risk of all-cause death, Dr. Hawker said. The adjusted hazard ratio per unit increase in HAQ walking score was 1.30 (P less than .001), after controlling for confounders including age, sex, preexisting CVD, diabetes, hypertension, body mass index, and smoking status.
A HAQ walking score of 2 was associated with an adjusted hazard ratio of 1.69, which was actually greater than that associated with preexisting cardiovascular disease or diabetes, she said.
For the composite CVD outcome, there was also a significant association with HAQ walking score (adjusted HR, 1.17; P = .001).
Sensitivity analyses performed in 402 patients (18%) receiving postbaseline total joint arthroplasty (TJA ) showed that controlling for TJA did not change the effect of baseline disability but was protective for both all-cause death (HR, 0.62; P less than .001) and CVD events (HR, 0.66; P less than .001), Dr. Hawker said at the meeting sponsored by the Osteoarthritis Research Society International.
Although the data were not dichotomized, she noted that there was "beautiful discrimination" when they looked at the outcomes based on whether or not patients used a walking aid.
"Obviously, it’s nice to see a dose-response, but simply knowing that someone’s using a walking aid and getting them to the point where they’ve got improved walking ability, could go a long way," she said.
Though the study was not designed to address potential mechanisms, Dr. Hawker said she’s long argued that physical activity and mobility are a key player of downstream effects on fitness, blood pressure, glucose control, and ability to participate in self-management activities and physician visits. The potential role for pain, mood, and stress also can not be excluded.
One audience member asked whether walking disability may be a "cheap and dirty version" of the stress test.
Dr. Hawker responded that walking disability is a proxy for a lot of things and is definitely OA-related, adding, "Yes, I think it is a very cheap and dirty stress test. It’s a lovely thing that if we focused more explicitly on it in randomized trials, for instance as a primary outcome, or in rehabilitation strategies, it would have global benefit."
The authors reported no competing interests.
PARIS – Greater walking disability is an independent predictor of all-cause death and major cardiovascular events in patients with symptomatic hip or knee osteoarthritis, according to a population-based study that confirms previous research.
For the composite cardiovascular disease (CVD) outcome of hospitalization for angina, acute myocardial infarction, coronary revascularization, congestive heart failure, stroke, or transient ischemic attack, the risk associated with a Health Assessment Questionnaire (HAQ) walking disability score of 2 was the same as that of diabetes and pre-existing CVD.
Total joint replacement reduced those risks by about 40%, Dr. Gillian A. Hawker said at the World Congress on Osteoarthritis (OA).
"I think the key piece here is that these data at least suggest that walking disability is a cardiovascular risk factor similar to diabetes," she said. "When we’re talking about risk assessment for cardiovascular outcomes, which everyone does pretty routinely in medicine, walking disability, which is really osteoarthritis, is one of the risk factors that they should be assessing ... If we can just start asking, hopefully it will get us thinking about, ‘Wow, this person has OA,’ and we need to start assessing it."
Session comoderator Ana M. Valdes, Ph.D., of the University of Nottingham (England) commented that the results are fascinating because this is not the first study to identify these associations. In 2011, British investigators reported that all-cause mortality, particularly due to CVD causes, was significantly related to baseline walking disability in patients with knee or hip OA (Br. Med. J. 2011;342:d1165).
"One of the things that happens often with OA is that it’s seen as just pain and if we can give them plenty of relief, they’ll be OK, but it’s actually life-threatening because if we do not address their disability, they are at risk of dying," Dr. Valdes said in an interview. "I think this should be put on the front pages of the weekly medical journals, so that people are aware of the dangers of not treating osteoarthritis properly."
Comorbidity is a barrier to OA care, and 90% of those aged 65 years and older with OA have at least one other chronic condition, such as diabetes and heart disease, observed Dr. Hawker, professor of medicine at the University of Toronto and physician-in-chief of medicine, Women’s College Hospital in Toronto.
Her group reported in a separate presentation at the meeting that walking disability also raises the risk for diabetes complications in those with both OA and diabetes.
For the current population-based study, the investigators linked provincial health administrative databases to baseline surveys from a population cohort of 2,156 patients with symptomatic moderate to severe OA who were recruited in 1996-1998 through a screening survey in Ontario.
Their mean age was 71 years (all were 55 years or older), 72% were female, 34% obese, 20% had diabetes, and 40% had prebaseline CVD. Their average HAQ walking disability score was 2 on a 3-point scale, and they had a mean WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index) summary score of 41. Overall, 44% used a walking aid. (A walking disability score of 2 corresponds with walking outdoors on flat ground with much difficulty, whereas a score of 3 means the person is unable to do it.)
After a median follow-up period of 13.2 years, 57% of patients had died, and 38% experienced the composite CVD outcome with a median of 9.2 years follow-up.
In multivariable analysis, there was a very clear dose-response, where increased walking disability was associated with increasing risk of all-cause death, Dr. Hawker said. The adjusted hazard ratio per unit increase in HAQ walking score was 1.30 (P less than .001), after controlling for confounders including age, sex, preexisting CVD, diabetes, hypertension, body mass index, and smoking status.
A HAQ walking score of 2 was associated with an adjusted hazard ratio of 1.69, which was actually greater than that associated with preexisting cardiovascular disease or diabetes, she said.
For the composite CVD outcome, there was also a significant association with HAQ walking score (adjusted HR, 1.17; P = .001).
Sensitivity analyses performed in 402 patients (18%) receiving postbaseline total joint arthroplasty (TJA ) showed that controlling for TJA did not change the effect of baseline disability but was protective for both all-cause death (HR, 0.62; P less than .001) and CVD events (HR, 0.66; P less than .001), Dr. Hawker said at the meeting sponsored by the Osteoarthritis Research Society International.
Although the data were not dichotomized, she noted that there was "beautiful discrimination" when they looked at the outcomes based on whether or not patients used a walking aid.
"Obviously, it’s nice to see a dose-response, but simply knowing that someone’s using a walking aid and getting them to the point where they’ve got improved walking ability, could go a long way," she said.
Though the study was not designed to address potential mechanisms, Dr. Hawker said she’s long argued that physical activity and mobility are a key player of downstream effects on fitness, blood pressure, glucose control, and ability to participate in self-management activities and physician visits. The potential role for pain, mood, and stress also can not be excluded.
One audience member asked whether walking disability may be a "cheap and dirty version" of the stress test.
Dr. Hawker responded that walking disability is a proxy for a lot of things and is definitely OA-related, adding, "Yes, I think it is a very cheap and dirty stress test. It’s a lovely thing that if we focused more explicitly on it in randomized trials, for instance as a primary outcome, or in rehabilitation strategies, it would have global benefit."
The authors reported no competing interests.
AT OARSI 2014
Key clinical point: A study confirming previous research suggests that a high level of walking disability in OA patients should be considered a strong risk factor for CVD.
Major finding: The adjusted hazard ratio per unit increase in HAQ walking score was 1.30 (P less than .001) for all-cause mortality and 1.17 (P = .001) for composite CVD events.
Data source: A population-based, cohort study in 2,156 hip and knee OA patients.
Disclosures: The authors reported no competing interests.
Vast majority of ED visits for acute heart failure become admissions
Nearly six of every seven patients presenting to U.S. emergency departments with acute heart failure are admitted. This means acute heart failure is "a major challenge" to emergency departments nationwide and consumes a sizeable portion of their resources.
"Strategies to reduce this clinical and economic burden are needed," said Dr. Alan B. Storrow of the department of emergency medicine, Vanderbilt University, Nashville, and his associates.
The investigators performed a retrospective cohort study to quantify the burden of acute heart failure on emergency medical care because "it is important ... to focus individual and health system strategies to address [these] challenges before they become overwhelming." To do so, they analyzed information from the Nationwide Emergency Department Sample, "the largest all-payer ED [emergency department] database in the United States," which contains 25-30 million records of ED visits for more than 950 hospitals.
For this study, the researchers assessed an average of 958,167 annual ED visits for acute heart failure over a 5-year period. They excluded patients with cardiogenic shock, unspecified shock, intubation, noninvasive ventilation, or acute myocardial infarction because such patients wouldn’t have been eligible for discharge from the ED, which was an important outcome for this analysis.
Overall, 83.7% of acute heart failure patients who presented to the ED were admitted for hospitalization. The median length of stay was 3.4 days. Median ED charges rose over time, from $1,075 to $1,558 per person (JACC Heart Failure 2014 April 30 [doi:10.1016/j.jchf.2014.01.006]).
Patients who presented to EDs at academic hospitals were 1.5 times more likely to be admitted than were those who presented to nonacademic hospitals.
Admission rates also varied with geographic location of the hospital. Patients who presented to EDs in the Northeast region of the country were the most likely to be admitted (90% admission rate), while those in the West were the least likely (79% admission rate).
Uninsured patients were admitted less often than insured patients, even though they were more likely to have significant comorbidities. However, uninsured patients who were admitted underwent more diagnostic and therapeutic procedures than did insured patients.
"These data strongly suggest the ED is increasingly being relied on to evaluate more complex patients, some of whom previously received care as outpatients, or were directly admitted from an outpatient setting. ... As a result, emergency physicians increasingly serve as the major decision makers for approximately one-half of all U.S. inpatient admissions," Dr. Storrow and his associates noted.
In addition, "Emergency physicians’ tolerance of ‘risk’ in relation to ED discharge decisions, especially for patients they do not have an ongoing relationship with, is likely lower than for other caregivers," they said.
Alternatives to admission must be considered, at least for a subset of patients who present to EDs with acute heart failure. For example, patients who are found not to have high-risk features could be managed for 24-48 hours in an observation unit or discharged home. "Exploring these alternative strategies is crucial because the prevalence of chronic heart failure, and ED presentations for acute heart failure, are expected to increase over the next decade," Dr. Storrow and his colleagues said.
They added that this study probably underestimated the burden of acute heart failure on EDs because some patients likely received primary diagnoses of pneumonia, chronic obstructive pulmonary disease, asthma, or pulmonary embolus, with acute heart failure listed only as a supporting diagnosis. Such patients wouldn’t have been included in the analysis.
This study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Storrow reported receiving grants from Abbott and Roche Diagnostics and is a consultant for Abbott, Astellas, and Novartis; his associates reported ties to numerous industry sources.
This study shows that the primary challenge is to identify which patients with acute heart failure who present to the emergency department can be rapidly and safely discharged or observed for a brief period, rather than admitted, said Dr. Peter S. Pang and Dr. Jeremiah D. Schuur.
A short observation period facilitates risk stratification, permits ongoing assessment of the patient’s response to initial therapy, and provides a chance to address immediate medical needs "as well as self-care, literacy, adherence, caregiver strain, and dietary education along with psychosocial and socioeconomic issues," they said.
"National efforts to decrease heart failure readmissions have received enormous support and focus. Why not an ED to home initiative or ED to observation unit to home strategy?"
Dr. Pang is in the department of emergency medicine and the Center for Cardiovascular Innovation at Northwestern University, Chicago. He reported ties to numerous pharmaceutical companies. Dr. Schuur is in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School, Boston. He reported ties to Blue Cross Blue Shield and United Healthcare. These remarks were taken from their accompanying editorial (JACC Heart Failure 2014 April 30 [doi:10.1016/j.jchf.2014.03.003).
This study shows that the primary challenge is to identify which patients with acute heart failure who present to the emergency department can be rapidly and safely discharged or observed for a brief period, rather than admitted, said Dr. Peter S. Pang and Dr. Jeremiah D. Schuur.
A short observation period facilitates risk stratification, permits ongoing assessment of the patient’s response to initial therapy, and provides a chance to address immediate medical needs "as well as self-care, literacy, adherence, caregiver strain, and dietary education along with psychosocial and socioeconomic issues," they said.
"National efforts to decrease heart failure readmissions have received enormous support and focus. Why not an ED to home initiative or ED to observation unit to home strategy?"
Dr. Pang is in the department of emergency medicine and the Center for Cardiovascular Innovation at Northwestern University, Chicago. He reported ties to numerous pharmaceutical companies. Dr. Schuur is in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School, Boston. He reported ties to Blue Cross Blue Shield and United Healthcare. These remarks were taken from their accompanying editorial (JACC Heart Failure 2014 April 30 [doi:10.1016/j.jchf.2014.03.003).
This study shows that the primary challenge is to identify which patients with acute heart failure who present to the emergency department can be rapidly and safely discharged or observed for a brief period, rather than admitted, said Dr. Peter S. Pang and Dr. Jeremiah D. Schuur.
A short observation period facilitates risk stratification, permits ongoing assessment of the patient’s response to initial therapy, and provides a chance to address immediate medical needs "as well as self-care, literacy, adherence, caregiver strain, and dietary education along with psychosocial and socioeconomic issues," they said.
"National efforts to decrease heart failure readmissions have received enormous support and focus. Why not an ED to home initiative or ED to observation unit to home strategy?"
Dr. Pang is in the department of emergency medicine and the Center for Cardiovascular Innovation at Northwestern University, Chicago. He reported ties to numerous pharmaceutical companies. Dr. Schuur is in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School, Boston. He reported ties to Blue Cross Blue Shield and United Healthcare. These remarks were taken from their accompanying editorial (JACC Heart Failure 2014 April 30 [doi:10.1016/j.jchf.2014.03.003).
Nearly six of every seven patients presenting to U.S. emergency departments with acute heart failure are admitted. This means acute heart failure is "a major challenge" to emergency departments nationwide and consumes a sizeable portion of their resources.
"Strategies to reduce this clinical and economic burden are needed," said Dr. Alan B. Storrow of the department of emergency medicine, Vanderbilt University, Nashville, and his associates.
The investigators performed a retrospective cohort study to quantify the burden of acute heart failure on emergency medical care because "it is important ... to focus individual and health system strategies to address [these] challenges before they become overwhelming." To do so, they analyzed information from the Nationwide Emergency Department Sample, "the largest all-payer ED [emergency department] database in the United States," which contains 25-30 million records of ED visits for more than 950 hospitals.
For this study, the researchers assessed an average of 958,167 annual ED visits for acute heart failure over a 5-year period. They excluded patients with cardiogenic shock, unspecified shock, intubation, noninvasive ventilation, or acute myocardial infarction because such patients wouldn’t have been eligible for discharge from the ED, which was an important outcome for this analysis.
Overall, 83.7% of acute heart failure patients who presented to the ED were admitted for hospitalization. The median length of stay was 3.4 days. Median ED charges rose over time, from $1,075 to $1,558 per person (JACC Heart Failure 2014 April 30 [doi:10.1016/j.jchf.2014.01.006]).
Patients who presented to EDs at academic hospitals were 1.5 times more likely to be admitted than were those who presented to nonacademic hospitals.
Admission rates also varied with geographic location of the hospital. Patients who presented to EDs in the Northeast region of the country were the most likely to be admitted (90% admission rate), while those in the West were the least likely (79% admission rate).
Uninsured patients were admitted less often than insured patients, even though they were more likely to have significant comorbidities. However, uninsured patients who were admitted underwent more diagnostic and therapeutic procedures than did insured patients.
"These data strongly suggest the ED is increasingly being relied on to evaluate more complex patients, some of whom previously received care as outpatients, or were directly admitted from an outpatient setting. ... As a result, emergency physicians increasingly serve as the major decision makers for approximately one-half of all U.S. inpatient admissions," Dr. Storrow and his associates noted.
In addition, "Emergency physicians’ tolerance of ‘risk’ in relation to ED discharge decisions, especially for patients they do not have an ongoing relationship with, is likely lower than for other caregivers," they said.
Alternatives to admission must be considered, at least for a subset of patients who present to EDs with acute heart failure. For example, patients who are found not to have high-risk features could be managed for 24-48 hours in an observation unit or discharged home. "Exploring these alternative strategies is crucial because the prevalence of chronic heart failure, and ED presentations for acute heart failure, are expected to increase over the next decade," Dr. Storrow and his colleagues said.
They added that this study probably underestimated the burden of acute heart failure on EDs because some patients likely received primary diagnoses of pneumonia, chronic obstructive pulmonary disease, asthma, or pulmonary embolus, with acute heart failure listed only as a supporting diagnosis. Such patients wouldn’t have been included in the analysis.
This study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Storrow reported receiving grants from Abbott and Roche Diagnostics and is a consultant for Abbott, Astellas, and Novartis; his associates reported ties to numerous industry sources.
Nearly six of every seven patients presenting to U.S. emergency departments with acute heart failure are admitted. This means acute heart failure is "a major challenge" to emergency departments nationwide and consumes a sizeable portion of their resources.
"Strategies to reduce this clinical and economic burden are needed," said Dr. Alan B. Storrow of the department of emergency medicine, Vanderbilt University, Nashville, and his associates.
The investigators performed a retrospective cohort study to quantify the burden of acute heart failure on emergency medical care because "it is important ... to focus individual and health system strategies to address [these] challenges before they become overwhelming." To do so, they analyzed information from the Nationwide Emergency Department Sample, "the largest all-payer ED [emergency department] database in the United States," which contains 25-30 million records of ED visits for more than 950 hospitals.
For this study, the researchers assessed an average of 958,167 annual ED visits for acute heart failure over a 5-year period. They excluded patients with cardiogenic shock, unspecified shock, intubation, noninvasive ventilation, or acute myocardial infarction because such patients wouldn’t have been eligible for discharge from the ED, which was an important outcome for this analysis.
Overall, 83.7% of acute heart failure patients who presented to the ED were admitted for hospitalization. The median length of stay was 3.4 days. Median ED charges rose over time, from $1,075 to $1,558 per person (JACC Heart Failure 2014 April 30 [doi:10.1016/j.jchf.2014.01.006]).
Patients who presented to EDs at academic hospitals were 1.5 times more likely to be admitted than were those who presented to nonacademic hospitals.
Admission rates also varied with geographic location of the hospital. Patients who presented to EDs in the Northeast region of the country were the most likely to be admitted (90% admission rate), while those in the West were the least likely (79% admission rate).
Uninsured patients were admitted less often than insured patients, even though they were more likely to have significant comorbidities. However, uninsured patients who were admitted underwent more diagnostic and therapeutic procedures than did insured patients.
"These data strongly suggest the ED is increasingly being relied on to evaluate more complex patients, some of whom previously received care as outpatients, or were directly admitted from an outpatient setting. ... As a result, emergency physicians increasingly serve as the major decision makers for approximately one-half of all U.S. inpatient admissions," Dr. Storrow and his associates noted.
In addition, "Emergency physicians’ tolerance of ‘risk’ in relation to ED discharge decisions, especially for patients they do not have an ongoing relationship with, is likely lower than for other caregivers," they said.
Alternatives to admission must be considered, at least for a subset of patients who present to EDs with acute heart failure. For example, patients who are found not to have high-risk features could be managed for 24-48 hours in an observation unit or discharged home. "Exploring these alternative strategies is crucial because the prevalence of chronic heart failure, and ED presentations for acute heart failure, are expected to increase over the next decade," Dr. Storrow and his colleagues said.
They added that this study probably underestimated the burden of acute heart failure on EDs because some patients likely received primary diagnoses of pneumonia, chronic obstructive pulmonary disease, asthma, or pulmonary embolus, with acute heart failure listed only as a supporting diagnosis. Such patients wouldn’t have been included in the analysis.
This study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Storrow reported receiving grants from Abbott and Roche Diagnostics and is a consultant for Abbott, Astellas, and Novartis; his associates reported ties to numerous industry sources.
FROM JACC: HEART FAILURE
Major finding: Overall, 83.7% of acute heart failure patients who presented to the ED were admitted for hospitalization.
Data source: A retrospective cohort study involving 958,167 annual ED visits for acute heart failure across the country.
Disclosures: This study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences. Dr. Storrow reported receiving grants from Abbott and Roche Diagnostics and is a consultant for Abbott, Astellas, and Novartis; his associates reported ties to numerous industry sources.
EXACT-HF: Allopurinol flops for heart failure
WASHINGTON – Allopurinol has no effect on heart failure, according to results from the multicenter, double-blind EXACT-HF study.
"In heart failure patients with reduced ejection fraction and hyperuricemia, xanthine oxidase inhibition with allopurinol safely lowers uric acid levels, but has no beneficial effect on clinical status, exercise capacity, quality of life, or left ventricular structure and function. Other adjunctive therapies for high-risk heart failure patients are clearly needed," Dr. Michael M. Givertz said in presenting the EXACT-HF results at the annual meeting of the American College of Cardiology.
Hopes were high going into EXACT-HF that xanthine oxidase inhibition would provide a much needed novel therapeutic approach to heart failure. A growing body of evidence suggests that oxidative stress plays a major role in ventricular remodeling and disease progression, and xanthine oxidase – a potential source of oxidative stress in heart failure – was a logical therapeutic target.
Moreover, in animal models of heart failure, as well as earlier short-term patient studies, allopurinol caused regression of left ventricular hypertrophy, improved endothelial function, and boosted myocardial efficiency while reducing myocardial oxygen demand, noted Dr. Givertz, medical director of heart transplant and circulatory assist at Brigham and Women’s Hospital, Boston.
EXACT-HF was a double-blind study in which 253 hyperuricemic heart failure patients with a median left ventricular ejection fraction (LVEF) of 24% and a median uric acid level of 11 mg/dL were placed on allopurinol or placebo and followed prospectively for 6 months. Allopurinol was started at 300 mg/day and, after 1 week, boosted to a target dose of 600 mg/day if tolerated.
The primary endpoint was a composite comprising death, hospitalization, or an emergency department or urgent care clinic visit for worsening heart failure; a medication change due to worsening heart failure; and patient global assessment. By this standard, roughly 45% of patients in both study arms were worse after 6 months, 16% were improved, and the rest were unchanged. Nor did the two groups differ significantly in terms of the various secondary and tertiary endpoints, including quality of life as assessed by the Kansas City Cardiomyopathy Score; the 6-minute walk test; levels of cystatin C, myeloperoxidase, and NT-proBNP (N-terminal of the prohormone brain natriuretic peptide); and left ventricular volume, mass, and ejection fraction.
Uric acid levels were reduced by about 45% in the allopurinol group. However, investigators never viewed hyperuricemia as a mediator of heart failure, but rather as a marker of more severe disease. And this was a population with fairly severe disease, as reflected in the 6% mortality rate at 6 months, along with a 30% rate of unscheduled outpatient visits and 38% rate of all-cause hospitalization, Dr. Givertz said.
Asked if he thought a longer treatment period might have shown therapeutic benefit, the cardiologist replied that there was one positive signal: The risk of heart failure hospitalization over the 6-month study was reduced by 33% in the allopurinol group, with the curves separating after 8-10 weeks, although the difference wasn’t statistically significant. But he was reluctant to make too much of this.
"It’s conceivable that if one treated for a year or longer with high doses of allopurinol, perhaps one might see a benefit. The argument against that is the consistency in the neutrality of the other endpoints at 6 months," according to Dr. Givertz.
Intriguingly, several recent studies suggest that colchicine – an even more venerable gout drug than allopurinol – may protect gout patients against cardiovascular events.
The EXACT-HF trial was sponsored by the National Heart, Lung, and Blood Institute and carried out by the NHLBI Heart Failure Clinical Research Network. Dr. Givertz reported serving as a consultant to Merck, Cardioxyl, and Janssen.
WASHINGTON – Allopurinol has no effect on heart failure, according to results from the multicenter, double-blind EXACT-HF study.
"In heart failure patients with reduced ejection fraction and hyperuricemia, xanthine oxidase inhibition with allopurinol safely lowers uric acid levels, but has no beneficial effect on clinical status, exercise capacity, quality of life, or left ventricular structure and function. Other adjunctive therapies for high-risk heart failure patients are clearly needed," Dr. Michael M. Givertz said in presenting the EXACT-HF results at the annual meeting of the American College of Cardiology.
Hopes were high going into EXACT-HF that xanthine oxidase inhibition would provide a much needed novel therapeutic approach to heart failure. A growing body of evidence suggests that oxidative stress plays a major role in ventricular remodeling and disease progression, and xanthine oxidase – a potential source of oxidative stress in heart failure – was a logical therapeutic target.
Moreover, in animal models of heart failure, as well as earlier short-term patient studies, allopurinol caused regression of left ventricular hypertrophy, improved endothelial function, and boosted myocardial efficiency while reducing myocardial oxygen demand, noted Dr. Givertz, medical director of heart transplant and circulatory assist at Brigham and Women’s Hospital, Boston.
EXACT-HF was a double-blind study in which 253 hyperuricemic heart failure patients with a median left ventricular ejection fraction (LVEF) of 24% and a median uric acid level of 11 mg/dL were placed on allopurinol or placebo and followed prospectively for 6 months. Allopurinol was started at 300 mg/day and, after 1 week, boosted to a target dose of 600 mg/day if tolerated.
The primary endpoint was a composite comprising death, hospitalization, or an emergency department or urgent care clinic visit for worsening heart failure; a medication change due to worsening heart failure; and patient global assessment. By this standard, roughly 45% of patients in both study arms were worse after 6 months, 16% were improved, and the rest were unchanged. Nor did the two groups differ significantly in terms of the various secondary and tertiary endpoints, including quality of life as assessed by the Kansas City Cardiomyopathy Score; the 6-minute walk test; levels of cystatin C, myeloperoxidase, and NT-proBNP (N-terminal of the prohormone brain natriuretic peptide); and left ventricular volume, mass, and ejection fraction.
Uric acid levels were reduced by about 45% in the allopurinol group. However, investigators never viewed hyperuricemia as a mediator of heart failure, but rather as a marker of more severe disease. And this was a population with fairly severe disease, as reflected in the 6% mortality rate at 6 months, along with a 30% rate of unscheduled outpatient visits and 38% rate of all-cause hospitalization, Dr. Givertz said.
Asked if he thought a longer treatment period might have shown therapeutic benefit, the cardiologist replied that there was one positive signal: The risk of heart failure hospitalization over the 6-month study was reduced by 33% in the allopurinol group, with the curves separating after 8-10 weeks, although the difference wasn’t statistically significant. But he was reluctant to make too much of this.
"It’s conceivable that if one treated for a year or longer with high doses of allopurinol, perhaps one might see a benefit. The argument against that is the consistency in the neutrality of the other endpoints at 6 months," according to Dr. Givertz.
Intriguingly, several recent studies suggest that colchicine – an even more venerable gout drug than allopurinol – may protect gout patients against cardiovascular events.
The EXACT-HF trial was sponsored by the National Heart, Lung, and Blood Institute and carried out by the NHLBI Heart Failure Clinical Research Network. Dr. Givertz reported serving as a consultant to Merck, Cardioxyl, and Janssen.
WASHINGTON – Allopurinol has no effect on heart failure, according to results from the multicenter, double-blind EXACT-HF study.
"In heart failure patients with reduced ejection fraction and hyperuricemia, xanthine oxidase inhibition with allopurinol safely lowers uric acid levels, but has no beneficial effect on clinical status, exercise capacity, quality of life, or left ventricular structure and function. Other adjunctive therapies for high-risk heart failure patients are clearly needed," Dr. Michael M. Givertz said in presenting the EXACT-HF results at the annual meeting of the American College of Cardiology.
Hopes were high going into EXACT-HF that xanthine oxidase inhibition would provide a much needed novel therapeutic approach to heart failure. A growing body of evidence suggests that oxidative stress plays a major role in ventricular remodeling and disease progression, and xanthine oxidase – a potential source of oxidative stress in heart failure – was a logical therapeutic target.
Moreover, in animal models of heart failure, as well as earlier short-term patient studies, allopurinol caused regression of left ventricular hypertrophy, improved endothelial function, and boosted myocardial efficiency while reducing myocardial oxygen demand, noted Dr. Givertz, medical director of heart transplant and circulatory assist at Brigham and Women’s Hospital, Boston.
EXACT-HF was a double-blind study in which 253 hyperuricemic heart failure patients with a median left ventricular ejection fraction (LVEF) of 24% and a median uric acid level of 11 mg/dL were placed on allopurinol or placebo and followed prospectively for 6 months. Allopurinol was started at 300 mg/day and, after 1 week, boosted to a target dose of 600 mg/day if tolerated.
The primary endpoint was a composite comprising death, hospitalization, or an emergency department or urgent care clinic visit for worsening heart failure; a medication change due to worsening heart failure; and patient global assessment. By this standard, roughly 45% of patients in both study arms were worse after 6 months, 16% were improved, and the rest were unchanged. Nor did the two groups differ significantly in terms of the various secondary and tertiary endpoints, including quality of life as assessed by the Kansas City Cardiomyopathy Score; the 6-minute walk test; levels of cystatin C, myeloperoxidase, and NT-proBNP (N-terminal of the prohormone brain natriuretic peptide); and left ventricular volume, mass, and ejection fraction.
Uric acid levels were reduced by about 45% in the allopurinol group. However, investigators never viewed hyperuricemia as a mediator of heart failure, but rather as a marker of more severe disease. And this was a population with fairly severe disease, as reflected in the 6% mortality rate at 6 months, along with a 30% rate of unscheduled outpatient visits and 38% rate of all-cause hospitalization, Dr. Givertz said.
Asked if he thought a longer treatment period might have shown therapeutic benefit, the cardiologist replied that there was one positive signal: The risk of heart failure hospitalization over the 6-month study was reduced by 33% in the allopurinol group, with the curves separating after 8-10 weeks, although the difference wasn’t statistically significant. But he was reluctant to make too much of this.
"It’s conceivable that if one treated for a year or longer with high doses of allopurinol, perhaps one might see a benefit. The argument against that is the consistency in the neutrality of the other endpoints at 6 months," according to Dr. Givertz.
Intriguingly, several recent studies suggest that colchicine – an even more venerable gout drug than allopurinol – may protect gout patients against cardiovascular events.
The EXACT-HF trial was sponsored by the National Heart, Lung, and Blood Institute and carried out by the NHLBI Heart Failure Clinical Research Network. Dr. Givertz reported serving as a consultant to Merck, Cardioxyl, and Janssen.
AT ACC 14
Major finding: Six months of therapy with allopurinol in patients with hyperuricemia and heart failure with reduced ejection fraction lowered their serum uric acid levels but had no effect on their heart failure.
Data source: EXACT-HF, a 6-month, double-blind, placebo-controlled trial conducted in 253 patients.
Disclosures: The EXACT-HF trial was sponsored by the National Heart, Lung, and Blood Institute and carried out by the NHLBI Heart Failure Clinical Research Network. Dr. Givertz reported serving as a consultant to Merck, Cardioxyl, and Janssen.