User login
FDA updates warning about Impella RP System
The Food and Drug Administration has reported that the higher postapproval mortality rates seen with Abiomed’s Impella RP System seem concentrated in a certain subgroup of patients only, according to a letter to health care providers.
The letter updates one from February regarding the observation of higher postapproval mortality rates with the temporary right heart pump.
This subgroup, which did not qualify for premarket clinical studies, was more likely to have been in cardiogenic shock for longer than 48 hours, experienced a cardiac arrest, or suffered a preimplant hypoxic or ischemic neurologic event prior to receiving the device, the FDA suggested in this new letter to health care providers. The 30-day survival rate in this subgroup within a postapproval study (PAS) was 10.7% (3 out of 28), while that among patients who would have qualified for the premarket clinical studies was 64.3% (9 of 14), according to the most recent interim results of that study. The rate among patients who would have qualified for premarket studies is similar to that seen among those premarket studies (73.4%); the overall 30-day survival rate in this PAS was 28.6%.
The FDA said that, based on these analyses, it still believes the benefits outweigh the risks when the Impella RP System is “used for the currently approved indication in appropriately selected patients.”
The FDA advises that health care providers review the device’s revised labeling, which now includes a checklist to help understand which patients could benefit the most. It also advises providers to promptly report any adverse events through MedWatch, which can help the FDA identify and understand the risks associated with the Impella RP System.
More information can be found in the FDA’s letter to health care providers, which is available on the FDA website.
The Food and Drug Administration has reported that the higher postapproval mortality rates seen with Abiomed’s Impella RP System seem concentrated in a certain subgroup of patients only, according to a letter to health care providers.
The letter updates one from February regarding the observation of higher postapproval mortality rates with the temporary right heart pump.
This subgroup, which did not qualify for premarket clinical studies, was more likely to have been in cardiogenic shock for longer than 48 hours, experienced a cardiac arrest, or suffered a preimplant hypoxic or ischemic neurologic event prior to receiving the device, the FDA suggested in this new letter to health care providers. The 30-day survival rate in this subgroup within a postapproval study (PAS) was 10.7% (3 out of 28), while that among patients who would have qualified for the premarket clinical studies was 64.3% (9 of 14), according to the most recent interim results of that study. The rate among patients who would have qualified for premarket studies is similar to that seen among those premarket studies (73.4%); the overall 30-day survival rate in this PAS was 28.6%.
The FDA said that, based on these analyses, it still believes the benefits outweigh the risks when the Impella RP System is “used for the currently approved indication in appropriately selected patients.”
The FDA advises that health care providers review the device’s revised labeling, which now includes a checklist to help understand which patients could benefit the most. It also advises providers to promptly report any adverse events through MedWatch, which can help the FDA identify and understand the risks associated with the Impella RP System.
More information can be found in the FDA’s letter to health care providers, which is available on the FDA website.
The Food and Drug Administration has reported that the higher postapproval mortality rates seen with Abiomed’s Impella RP System seem concentrated in a certain subgroup of patients only, according to a letter to health care providers.
The letter updates one from February regarding the observation of higher postapproval mortality rates with the temporary right heart pump.
This subgroup, which did not qualify for premarket clinical studies, was more likely to have been in cardiogenic shock for longer than 48 hours, experienced a cardiac arrest, or suffered a preimplant hypoxic or ischemic neurologic event prior to receiving the device, the FDA suggested in this new letter to health care providers. The 30-day survival rate in this subgroup within a postapproval study (PAS) was 10.7% (3 out of 28), while that among patients who would have qualified for the premarket clinical studies was 64.3% (9 of 14), according to the most recent interim results of that study. The rate among patients who would have qualified for premarket studies is similar to that seen among those premarket studies (73.4%); the overall 30-day survival rate in this PAS was 28.6%.
The FDA said that, based on these analyses, it still believes the benefits outweigh the risks when the Impella RP System is “used for the currently approved indication in appropriately selected patients.”
The FDA advises that health care providers review the device’s revised labeling, which now includes a checklist to help understand which patients could benefit the most. It also advises providers to promptly report any adverse events through MedWatch, which can help the FDA identify and understand the risks associated with the Impella RP System.
More information can be found in the FDA’s letter to health care providers, which is available on the FDA website.
SCAI releases first definition of cardiogenic shock
LAS VEGAS – The Society for Cardiovascular Angiography & Interventions released on May 19 the first-ever classification scheme for cardiogenic shock, dividing the condition into five severity levels.

The expert consensus panel that devised the new definition and classification model hopes it will spearhead a reset of research into the management of cardiogenic shock so that clinicians can assess interventions and introduce them into practice in a more precise, reproducible, and systematic way, Srihari S. Naidu, MD, said while presenting the proposal at the society’s annual scientific sessions.
The writing panel’s hope is that the new definition will “drive earlier recognition of shock and at a more precise stage to guide appropriate and timely escalation of care” and to “better define prospectively the value of mechanical circulatory support, extracorporeal membrane oxygenation, and other therapies,” said Dr. Naidu, chair of the writing group, as well as professor of medicine at New York Medical College and director of the cardiac catheterization laboratory at Westchester Medical Center, both in Valhalla, N.Y.
At the core of the classification scheme are the definitions for five strata of disease, which start at stage A, the “at-risk” patients before shock onset, and progress through stage B, “beginning”; stage C, “classic”; stage D, “deteriorating”; and stage E, “extremis,” which defines a patient with circulatory collapse (Catheter Cardiovasc Interv. 2019 May 19; doi: 10.1002/ccd.28329). Another key element of the classification model is the cardiac arrest “modifier,” designated by a subscripted letter A, which identifies patients who have had a cardiac arrest, regardless of duration. So a patient could be a stage BA, which identifies a patient with clinical evidence of relative hypotension or tachycardia without hypoperfusion and with a history of cardiac arrest.
The statement also itemizes several biomarkers and hemodynamic measurements that need regular, serial monitoring, such as blood lactate and right arterial pressure. Although the document leaves specific, defining values for some of these measures vaguely defined – the intent is that future research will fill in these gaps – the overall message is that clinicians caring for cardiogenic shock patients “need to be aggressive and look for these things,” Dr. Naidu said in a video interview.
“Until we agree on a definition of cardiogenic shock, we can’t go anywhere,” commented Larry S. Dean, MD, professor of medicine at and director of the Regional Heart Center of the University of Washington in Seattle. “There are a lot of conflicting data out there, and until we have a shared definition, we can’t advance our practice. We need to start looking at shock patients in a more precise way.”
“Without a clear definition of cardiogenic shock we will never improve patient outcomes. Every shock trial must define shock. If investigators just say ‘patients were in shock,’ I don’t know what that means,” noted Navin K. Kapur, MD, director of the Interventional Research Laboratories at Tufts Medical Center in Boston and a member of the writing panel.
Dr. Naidu and others on the panel highlighted the need to now validate the classification scheme’s ability to consistently categorize patients and predict their disease trajectories. They have begun the validation process with a 10,000-patient database of “all-comers” with cardiogenic shock maintained by the Mayo Clinic. Full results from this analysis will be out soon, but Dr. Naidu revealed in passing that it successfully provided validation of the proposed scheme.
The new definition received endorsements from the American College of Cardiology, the American Heart Association, the Society of Critical Care Medicine, and the Society of Thoracic Surgeons.
Dr. Naidu had no disclosures.
LAS VEGAS – The Society for Cardiovascular Angiography & Interventions released on May 19 the first-ever classification scheme for cardiogenic shock, dividing the condition into five severity levels.

The expert consensus panel that devised the new definition and classification model hopes it will spearhead a reset of research into the management of cardiogenic shock so that clinicians can assess interventions and introduce them into practice in a more precise, reproducible, and systematic way, Srihari S. Naidu, MD, said while presenting the proposal at the society’s annual scientific sessions.
The writing panel’s hope is that the new definition will “drive earlier recognition of shock and at a more precise stage to guide appropriate and timely escalation of care” and to “better define prospectively the value of mechanical circulatory support, extracorporeal membrane oxygenation, and other therapies,” said Dr. Naidu, chair of the writing group, as well as professor of medicine at New York Medical College and director of the cardiac catheterization laboratory at Westchester Medical Center, both in Valhalla, N.Y.
At the core of the classification scheme are the definitions for five strata of disease, which start at stage A, the “at-risk” patients before shock onset, and progress through stage B, “beginning”; stage C, “classic”; stage D, “deteriorating”; and stage E, “extremis,” which defines a patient with circulatory collapse (Catheter Cardiovasc Interv. 2019 May 19; doi: 10.1002/ccd.28329). Another key element of the classification model is the cardiac arrest “modifier,” designated by a subscripted letter A, which identifies patients who have had a cardiac arrest, regardless of duration. So a patient could be a stage BA, which identifies a patient with clinical evidence of relative hypotension or tachycardia without hypoperfusion and with a history of cardiac arrest.
The statement also itemizes several biomarkers and hemodynamic measurements that need regular, serial monitoring, such as blood lactate and right arterial pressure. Although the document leaves specific, defining values for some of these measures vaguely defined – the intent is that future research will fill in these gaps – the overall message is that clinicians caring for cardiogenic shock patients “need to be aggressive and look for these things,” Dr. Naidu said in a video interview.
“Until we agree on a definition of cardiogenic shock, we can’t go anywhere,” commented Larry S. Dean, MD, professor of medicine at and director of the Regional Heart Center of the University of Washington in Seattle. “There are a lot of conflicting data out there, and until we have a shared definition, we can’t advance our practice. We need to start looking at shock patients in a more precise way.”
“Without a clear definition of cardiogenic shock we will never improve patient outcomes. Every shock trial must define shock. If investigators just say ‘patients were in shock,’ I don’t know what that means,” noted Navin K. Kapur, MD, director of the Interventional Research Laboratories at Tufts Medical Center in Boston and a member of the writing panel.
Dr. Naidu and others on the panel highlighted the need to now validate the classification scheme’s ability to consistently categorize patients and predict their disease trajectories. They have begun the validation process with a 10,000-patient database of “all-comers” with cardiogenic shock maintained by the Mayo Clinic. Full results from this analysis will be out soon, but Dr. Naidu revealed in passing that it successfully provided validation of the proposed scheme.
The new definition received endorsements from the American College of Cardiology, the American Heart Association, the Society of Critical Care Medicine, and the Society of Thoracic Surgeons.
Dr. Naidu had no disclosures.
LAS VEGAS – The Society for Cardiovascular Angiography & Interventions released on May 19 the first-ever classification scheme for cardiogenic shock, dividing the condition into five severity levels.

The expert consensus panel that devised the new definition and classification model hopes it will spearhead a reset of research into the management of cardiogenic shock so that clinicians can assess interventions and introduce them into practice in a more precise, reproducible, and systematic way, Srihari S. Naidu, MD, said while presenting the proposal at the society’s annual scientific sessions.
The writing panel’s hope is that the new definition will “drive earlier recognition of shock and at a more precise stage to guide appropriate and timely escalation of care” and to “better define prospectively the value of mechanical circulatory support, extracorporeal membrane oxygenation, and other therapies,” said Dr. Naidu, chair of the writing group, as well as professor of medicine at New York Medical College and director of the cardiac catheterization laboratory at Westchester Medical Center, both in Valhalla, N.Y.
At the core of the classification scheme are the definitions for five strata of disease, which start at stage A, the “at-risk” patients before shock onset, and progress through stage B, “beginning”; stage C, “classic”; stage D, “deteriorating”; and stage E, “extremis,” which defines a patient with circulatory collapse (Catheter Cardiovasc Interv. 2019 May 19; doi: 10.1002/ccd.28329). Another key element of the classification model is the cardiac arrest “modifier,” designated by a subscripted letter A, which identifies patients who have had a cardiac arrest, regardless of duration. So a patient could be a stage BA, which identifies a patient with clinical evidence of relative hypotension or tachycardia without hypoperfusion and with a history of cardiac arrest.
The statement also itemizes several biomarkers and hemodynamic measurements that need regular, serial monitoring, such as blood lactate and right arterial pressure. Although the document leaves specific, defining values for some of these measures vaguely defined – the intent is that future research will fill in these gaps – the overall message is that clinicians caring for cardiogenic shock patients “need to be aggressive and look for these things,” Dr. Naidu said in a video interview.
“Until we agree on a definition of cardiogenic shock, we can’t go anywhere,” commented Larry S. Dean, MD, professor of medicine at and director of the Regional Heart Center of the University of Washington in Seattle. “There are a lot of conflicting data out there, and until we have a shared definition, we can’t advance our practice. We need to start looking at shock patients in a more precise way.”
“Without a clear definition of cardiogenic shock we will never improve patient outcomes. Every shock trial must define shock. If investigators just say ‘patients were in shock,’ I don’t know what that means,” noted Navin K. Kapur, MD, director of the Interventional Research Laboratories at Tufts Medical Center in Boston and a member of the writing panel.
Dr. Naidu and others on the panel highlighted the need to now validate the classification scheme’s ability to consistently categorize patients and predict their disease trajectories. They have begun the validation process with a 10,000-patient database of “all-comers” with cardiogenic shock maintained by the Mayo Clinic. Full results from this analysis will be out soon, but Dr. Naidu revealed in passing that it successfully provided validation of the proposed scheme.
The new definition received endorsements from the American College of Cardiology, the American Heart Association, the Society of Critical Care Medicine, and the Society of Thoracic Surgeons.
Dr. Naidu had no disclosures.
REPORTING FROM SCAI 2019
CABANA: Heart failure patients got biggest bang from AFib ablation
SAN FRANCISCO – Catheter ablation of atrial fibrillation (AFib) in the roughly one-third of patients with heart failure enrolled in the CABANA multicenter, randomized trial produced striking, statistically significant improvements both in the study’s primary, combined endpoint and in all-cause mortality in intention-to-treat analyses.
These findings, from prespecified secondary analyses, contrasted with the study’s overall result, which showed no benefit in the primary endpoint analysis in the total study population of 2,204 patients with AFib (JAMA. 2019 Apr 2;321[13]:1261-74). They are also at odds with the primary endpoint result in the two-thirds of enrolled patients without heart failure, which showed no significant between-group differences in these two outcome measures among the patients assigned to the catheter ablation arm and the study’s control, which was medical management arm.
Among the 778 AFib patients enrolled in CABANA with any form of heart failure (35% of the total study enrollment), the incidence of the study’s primary endpoint – the combined rate of death, disabling stroke, serious bleeding, or cardiac arrest during a median follow-up of slightly more than 4 years – was 36% lower among the catheter-ablated heart failure patients than in the heart failure patients assigned to medical treatment, according to an intention-to-treat analysis, which was a statistically significant difference. The incidence of all-cause mortality during follow-up was 43% lower in the ablated heart failure patients, compared with the controls, Douglas L. Packer, MD, said at the annual scientific sessions of the Heart Rhythm Society.
In contrast, among enrolled patients without heart failure, the intention-to-treat primary endpoint was 6% higher in the ablated patients, and all-cause mortality was a relative 27% higher, although neither difference was statistically significant.
It’s a “little surprising” that the results showed this much benefit in the patients with heart failure, said Dr. Packer, professor of medicine at the Mayo Clinic in Rochester, Minn., and lead investigator of the CABANA (Catheter Ablation vs Anti-Arrhythmic Drug Therapy for Atrial Fibrillation) trial. “I think these data confirm the results of the CASTLE-AF trial, but without some of the glitches some people have cited” about that study, such as concerns about a high level of patient selection in CASTLE-AF and its relatively modest number of enrolled patients, he said in an interview.
The CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) study, run entirely in patients with heart failure with reduced ejection fraction and AFib, showed a statistically significant improvement in patient survival and heart failure hospitalization after catheter ablation compared with medical management (N Engl J Med. 2018 Feb 1;378[5]:417-27). Prior to the CASTLE-AF report, results from several other small studies (J Interv Card Electrophysiol. 2018 Oct;53[1]:19-29), as well as those from the AATAC trial (Circulation. 2016 Apr 26;133[17]:1637-44), also showed consistent evidence for benefit from catheter ablation in patients with heart failure and AFib, noted CABANA coinvestigator Jonathan P. Piccini, MD, during a separate talk at the meeting.
“The improvement of cardiovascular outcomes with ablation in patients with heart failure and AFib is consistent across multiple trials, at least with respect to heart failure with reduced ejection fraction” concluded Dr. Piccini, a cardiac electrophysiologist at Duke University in Durham, N.C.
As a result of the new heart failure analysis, “I think the guidelines will change,” predicted Dr. Packer, with catheter ablation receiving a firmer endorsement for patients with heart failure the next time U.S. guidelines for heart failure and AFib management are updated. The findings say “there is substantial benefit of catheter ablation in heart failure patients, but I don’t think our findings lessen the utility of ablation in patients without heart failure,” he stressed. Even patients without heart failure showed reduction in AFib burden and improvement in quality of life that were similar to what was seen in the heart failure patients.
The new report from CABANA of benefit from AFib catheter ablation in patients with heart failure “absolutely advances the evidence,” commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago. “A number of us were quite circumspect about this based on the CASTLE-AF data, but the new CABANA analyses have addressed our anxiety that the CASTLE-AF results were just by chance.” The new CABANA analyses “may not confirm CASTLE-AF, but it enriches the conversation and makes it possible that we are seeing benefit in some patients with heart failure who get ablated.”
Dr. Yancy, who chaired the most recent update to the U.S. heart failure management guideline (J Am Coll Cardiol. 2017 Aug 8;70[6]:776-803) stopped short of saying that the cumulative evidence now supports a guideline change, but he acknowledged in an interview that the evidence could legitimately influence practice. Catheter ablation should now be “strongly considered” in patients with heart failure and AFib, he said, although he also had three qualifications for opting for this approach: Patients must already be on guideline-directed medical therapy for their heart failure, the catheter ablation needs to be performed by an experienced and skilled operator, and follow-up surveillance must focus on both the patient’s AFib and heart failure. “It’s absolutely appropriate to consider catheter ablation” for heart failure patients, but the evidence is not yet there for guideline change, Dr. Yancy concluded.
It remains uncertain why catheter ablation of AFib should be more effective in patients with heart failure than in those without. Dr. Packer speculated that one reason may be the heart rate reduction that AFib ablation produces may especially benefit heart failure patients. An additional helpful effect of ablation in heart failure patients may be reducing heart rate variability. Another notable finding of the new analysis was that 79% of patients with heart failure in CABANA had heart failure with preserved ejection fraction, with a left ventricular ejection fraction of at least 50%. “Getting rid of AFib in patients with heart failure with preserved ejection fraction will be more important than we have thought,” Dr. Packer said.
Other new CABANA analyses presented for the first time in separate talks at the meeting also showed that, while catheter ablation had no meaningful difference in effect on outcomes based on the sex of patients, both age and minority ethnic and racial status appeared to make a substantial difference. For CABANA’s primary endpoint, catheter ablation was especially effective for improving outcomes in patients 64 years old or younger, and the analysis showed a signal of possibly worse outcomes in patients who were at least 75 years old. The “substantially” better outcomes in minority-group patients represented the largest between-group difference among subgroups seen in CABANA and is a “big deal,” said Dr. Packer, who predicted that future catheter ablation use will likely rise in patients with heart failure, in younger patients, and in minority patients.
Dr. Piccini noted that, “it’s possible that CABANA identified some patient subgroups that do really well after ablation, but the problem is that, in the United States, we now often don’t treat” minority patients or those with reduced left ventricular ejection fractions with ablation, according to recent registry findings.
CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and/or received research funding from these four companies, as well as numerous drug and device companies, and has a financial interest in a licensed AFib mapping technology. Dr. Piccini has ties Boston Scientific, Medtronic, and numerous other drug and device companies, and disclosed an unspecified relationship with GlaxoSmithKline. Dr. Yancy disclosed an unspecified relationship with Abbott Laboratories.
SOURCE: Packer DL. Heart Rhythm 2019, Abstract S-AB14-06.
SAN FRANCISCO – Catheter ablation of atrial fibrillation (AFib) in the roughly one-third of patients with heart failure enrolled in the CABANA multicenter, randomized trial produced striking, statistically significant improvements both in the study’s primary, combined endpoint and in all-cause mortality in intention-to-treat analyses.
These findings, from prespecified secondary analyses, contrasted with the study’s overall result, which showed no benefit in the primary endpoint analysis in the total study population of 2,204 patients with AFib (JAMA. 2019 Apr 2;321[13]:1261-74). They are also at odds with the primary endpoint result in the two-thirds of enrolled patients without heart failure, which showed no significant between-group differences in these two outcome measures among the patients assigned to the catheter ablation arm and the study’s control, which was medical management arm.
Among the 778 AFib patients enrolled in CABANA with any form of heart failure (35% of the total study enrollment), the incidence of the study’s primary endpoint – the combined rate of death, disabling stroke, serious bleeding, or cardiac arrest during a median follow-up of slightly more than 4 years – was 36% lower among the catheter-ablated heart failure patients than in the heart failure patients assigned to medical treatment, according to an intention-to-treat analysis, which was a statistically significant difference. The incidence of all-cause mortality during follow-up was 43% lower in the ablated heart failure patients, compared with the controls, Douglas L. Packer, MD, said at the annual scientific sessions of the Heart Rhythm Society.
In contrast, among enrolled patients without heart failure, the intention-to-treat primary endpoint was 6% higher in the ablated patients, and all-cause mortality was a relative 27% higher, although neither difference was statistically significant.
It’s a “little surprising” that the results showed this much benefit in the patients with heart failure, said Dr. Packer, professor of medicine at the Mayo Clinic in Rochester, Minn., and lead investigator of the CABANA (Catheter Ablation vs Anti-Arrhythmic Drug Therapy for Atrial Fibrillation) trial. “I think these data confirm the results of the CASTLE-AF trial, but without some of the glitches some people have cited” about that study, such as concerns about a high level of patient selection in CASTLE-AF and its relatively modest number of enrolled patients, he said in an interview.
The CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) study, run entirely in patients with heart failure with reduced ejection fraction and AFib, showed a statistically significant improvement in patient survival and heart failure hospitalization after catheter ablation compared with medical management (N Engl J Med. 2018 Feb 1;378[5]:417-27). Prior to the CASTLE-AF report, results from several other small studies (J Interv Card Electrophysiol. 2018 Oct;53[1]:19-29), as well as those from the AATAC trial (Circulation. 2016 Apr 26;133[17]:1637-44), also showed consistent evidence for benefit from catheter ablation in patients with heart failure and AFib, noted CABANA coinvestigator Jonathan P. Piccini, MD, during a separate talk at the meeting.
“The improvement of cardiovascular outcomes with ablation in patients with heart failure and AFib is consistent across multiple trials, at least with respect to heart failure with reduced ejection fraction” concluded Dr. Piccini, a cardiac electrophysiologist at Duke University in Durham, N.C.
As a result of the new heart failure analysis, “I think the guidelines will change,” predicted Dr. Packer, with catheter ablation receiving a firmer endorsement for patients with heart failure the next time U.S. guidelines for heart failure and AFib management are updated. The findings say “there is substantial benefit of catheter ablation in heart failure patients, but I don’t think our findings lessen the utility of ablation in patients without heart failure,” he stressed. Even patients without heart failure showed reduction in AFib burden and improvement in quality of life that were similar to what was seen in the heart failure patients.
The new report from CABANA of benefit from AFib catheter ablation in patients with heart failure “absolutely advances the evidence,” commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago. “A number of us were quite circumspect about this based on the CASTLE-AF data, but the new CABANA analyses have addressed our anxiety that the CASTLE-AF results were just by chance.” The new CABANA analyses “may not confirm CASTLE-AF, but it enriches the conversation and makes it possible that we are seeing benefit in some patients with heart failure who get ablated.”
Dr. Yancy, who chaired the most recent update to the U.S. heart failure management guideline (J Am Coll Cardiol. 2017 Aug 8;70[6]:776-803) stopped short of saying that the cumulative evidence now supports a guideline change, but he acknowledged in an interview that the evidence could legitimately influence practice. Catheter ablation should now be “strongly considered” in patients with heart failure and AFib, he said, although he also had three qualifications for opting for this approach: Patients must already be on guideline-directed medical therapy for their heart failure, the catheter ablation needs to be performed by an experienced and skilled operator, and follow-up surveillance must focus on both the patient’s AFib and heart failure. “It’s absolutely appropriate to consider catheter ablation” for heart failure patients, but the evidence is not yet there for guideline change, Dr. Yancy concluded.
It remains uncertain why catheter ablation of AFib should be more effective in patients with heart failure than in those without. Dr. Packer speculated that one reason may be the heart rate reduction that AFib ablation produces may especially benefit heart failure patients. An additional helpful effect of ablation in heart failure patients may be reducing heart rate variability. Another notable finding of the new analysis was that 79% of patients with heart failure in CABANA had heart failure with preserved ejection fraction, with a left ventricular ejection fraction of at least 50%. “Getting rid of AFib in patients with heart failure with preserved ejection fraction will be more important than we have thought,” Dr. Packer said.
Other new CABANA analyses presented for the first time in separate talks at the meeting also showed that, while catheter ablation had no meaningful difference in effect on outcomes based on the sex of patients, both age and minority ethnic and racial status appeared to make a substantial difference. For CABANA’s primary endpoint, catheter ablation was especially effective for improving outcomes in patients 64 years old or younger, and the analysis showed a signal of possibly worse outcomes in patients who were at least 75 years old. The “substantially” better outcomes in minority-group patients represented the largest between-group difference among subgroups seen in CABANA and is a “big deal,” said Dr. Packer, who predicted that future catheter ablation use will likely rise in patients with heart failure, in younger patients, and in minority patients.
Dr. Piccini noted that, “it’s possible that CABANA identified some patient subgroups that do really well after ablation, but the problem is that, in the United States, we now often don’t treat” minority patients or those with reduced left ventricular ejection fractions with ablation, according to recent registry findings.
CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and/or received research funding from these four companies, as well as numerous drug and device companies, and has a financial interest in a licensed AFib mapping technology. Dr. Piccini has ties Boston Scientific, Medtronic, and numerous other drug and device companies, and disclosed an unspecified relationship with GlaxoSmithKline. Dr. Yancy disclosed an unspecified relationship with Abbott Laboratories.
SOURCE: Packer DL. Heart Rhythm 2019, Abstract S-AB14-06.
SAN FRANCISCO – Catheter ablation of atrial fibrillation (AFib) in the roughly one-third of patients with heart failure enrolled in the CABANA multicenter, randomized trial produced striking, statistically significant improvements both in the study’s primary, combined endpoint and in all-cause mortality in intention-to-treat analyses.
These findings, from prespecified secondary analyses, contrasted with the study’s overall result, which showed no benefit in the primary endpoint analysis in the total study population of 2,204 patients with AFib (JAMA. 2019 Apr 2;321[13]:1261-74). They are also at odds with the primary endpoint result in the two-thirds of enrolled patients without heart failure, which showed no significant between-group differences in these two outcome measures among the patients assigned to the catheter ablation arm and the study’s control, which was medical management arm.
Among the 778 AFib patients enrolled in CABANA with any form of heart failure (35% of the total study enrollment), the incidence of the study’s primary endpoint – the combined rate of death, disabling stroke, serious bleeding, or cardiac arrest during a median follow-up of slightly more than 4 years – was 36% lower among the catheter-ablated heart failure patients than in the heart failure patients assigned to medical treatment, according to an intention-to-treat analysis, which was a statistically significant difference. The incidence of all-cause mortality during follow-up was 43% lower in the ablated heart failure patients, compared with the controls, Douglas L. Packer, MD, said at the annual scientific sessions of the Heart Rhythm Society.
In contrast, among enrolled patients without heart failure, the intention-to-treat primary endpoint was 6% higher in the ablated patients, and all-cause mortality was a relative 27% higher, although neither difference was statistically significant.
It’s a “little surprising” that the results showed this much benefit in the patients with heart failure, said Dr. Packer, professor of medicine at the Mayo Clinic in Rochester, Minn., and lead investigator of the CABANA (Catheter Ablation vs Anti-Arrhythmic Drug Therapy for Atrial Fibrillation) trial. “I think these data confirm the results of the CASTLE-AF trial, but without some of the glitches some people have cited” about that study, such as concerns about a high level of patient selection in CASTLE-AF and its relatively modest number of enrolled patients, he said in an interview.
The CASTLE-AF (Catheter Ablation vs. Standard Conventional Treatment in Patients With LV Dysfunction and AF) study, run entirely in patients with heart failure with reduced ejection fraction and AFib, showed a statistically significant improvement in patient survival and heart failure hospitalization after catheter ablation compared with medical management (N Engl J Med. 2018 Feb 1;378[5]:417-27). Prior to the CASTLE-AF report, results from several other small studies (J Interv Card Electrophysiol. 2018 Oct;53[1]:19-29), as well as those from the AATAC trial (Circulation. 2016 Apr 26;133[17]:1637-44), also showed consistent evidence for benefit from catheter ablation in patients with heart failure and AFib, noted CABANA coinvestigator Jonathan P. Piccini, MD, during a separate talk at the meeting.
“The improvement of cardiovascular outcomes with ablation in patients with heart failure and AFib is consistent across multiple trials, at least with respect to heart failure with reduced ejection fraction” concluded Dr. Piccini, a cardiac electrophysiologist at Duke University in Durham, N.C.
As a result of the new heart failure analysis, “I think the guidelines will change,” predicted Dr. Packer, with catheter ablation receiving a firmer endorsement for patients with heart failure the next time U.S. guidelines for heart failure and AFib management are updated. The findings say “there is substantial benefit of catheter ablation in heart failure patients, but I don’t think our findings lessen the utility of ablation in patients without heart failure,” he stressed. Even patients without heart failure showed reduction in AFib burden and improvement in quality of life that were similar to what was seen in the heart failure patients.
The new report from CABANA of benefit from AFib catheter ablation in patients with heart failure “absolutely advances the evidence,” commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago. “A number of us were quite circumspect about this based on the CASTLE-AF data, but the new CABANA analyses have addressed our anxiety that the CASTLE-AF results were just by chance.” The new CABANA analyses “may not confirm CASTLE-AF, but it enriches the conversation and makes it possible that we are seeing benefit in some patients with heart failure who get ablated.”
Dr. Yancy, who chaired the most recent update to the U.S. heart failure management guideline (J Am Coll Cardiol. 2017 Aug 8;70[6]:776-803) stopped short of saying that the cumulative evidence now supports a guideline change, but he acknowledged in an interview that the evidence could legitimately influence practice. Catheter ablation should now be “strongly considered” in patients with heart failure and AFib, he said, although he also had three qualifications for opting for this approach: Patients must already be on guideline-directed medical therapy for their heart failure, the catheter ablation needs to be performed by an experienced and skilled operator, and follow-up surveillance must focus on both the patient’s AFib and heart failure. “It’s absolutely appropriate to consider catheter ablation” for heart failure patients, but the evidence is not yet there for guideline change, Dr. Yancy concluded.
It remains uncertain why catheter ablation of AFib should be more effective in patients with heart failure than in those without. Dr. Packer speculated that one reason may be the heart rate reduction that AFib ablation produces may especially benefit heart failure patients. An additional helpful effect of ablation in heart failure patients may be reducing heart rate variability. Another notable finding of the new analysis was that 79% of patients with heart failure in CABANA had heart failure with preserved ejection fraction, with a left ventricular ejection fraction of at least 50%. “Getting rid of AFib in patients with heart failure with preserved ejection fraction will be more important than we have thought,” Dr. Packer said.
Other new CABANA analyses presented for the first time in separate talks at the meeting also showed that, while catheter ablation had no meaningful difference in effect on outcomes based on the sex of patients, both age and minority ethnic and racial status appeared to make a substantial difference. For CABANA’s primary endpoint, catheter ablation was especially effective for improving outcomes in patients 64 years old or younger, and the analysis showed a signal of possibly worse outcomes in patients who were at least 75 years old. The “substantially” better outcomes in minority-group patients represented the largest between-group difference among subgroups seen in CABANA and is a “big deal,” said Dr. Packer, who predicted that future catheter ablation use will likely rise in patients with heart failure, in younger patients, and in minority patients.
Dr. Piccini noted that, “it’s possible that CABANA identified some patient subgroups that do really well after ablation, but the problem is that, in the United States, we now often don’t treat” minority patients or those with reduced left ventricular ejection fractions with ablation, according to recent registry findings.
CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and/or received research funding from these four companies, as well as numerous drug and device companies, and has a financial interest in a licensed AFib mapping technology. Dr. Piccini has ties Boston Scientific, Medtronic, and numerous other drug and device companies, and disclosed an unspecified relationship with GlaxoSmithKline. Dr. Yancy disclosed an unspecified relationship with Abbott Laboratories.
SOURCE: Packer DL. Heart Rhythm 2019, Abstract S-AB14-06.
REPORTING FROM HEART RHYTHM 2019
Key clinical point: Catheter ablation for atrial fibrillation is especially effective in patients with heart failure.
Major finding: Heart failure patients treated with catheter ablation had a 36% relative cut in the primary endpoint, compared with control patients.
Study details: CABANA, a multicenter, randomized trial with 2,204 patients, including 778 patients with heart failure.
Disclosures: CABANA received partial funding from Biosense Webster, Boston Scientific, Medtronic, and St. Jude. Dr. Packer has been a consultant to and/or received research funding from these four companies, as well as numerous drug and device companies, and has a financial interest in a licensed AFib mapping technology. Source: Packer DL. Heart Rhythm 2019, Abstract S-AB14-06.
BMI in male teens predicts cardiomyopathy risk
and their risk increased as body mass index increased, according to the results of a nationwide, prospective, registry-based cohort study from Sweden.
The association was strongest for dilated cardiomyopathy, wrote Josefina Robertson, MD, and associates at the University of Gothenburg (Sweden). Over a median of 27 years of follow-up, the risk for dilated cardiomyopathy in adulthood was approximately 38% greater when adolescent body mass index was 22.5-25.0 kg/m2, using a lean but not underweight BMI (18.5-20.0 kg/m2) as the reference group. The increase in risk for dilated cardiomyopathy continued to rise with adolescent BMI and exceeded 700% at a BMI over 35.
The rate of hospitalizations for heart failure caused by cardiomyopathy more than doubled in Sweden from 1987 to 2006, the researchers noted. Adolescent obesity is strongly linked to early heart failure, but few studies have assessed whether adiposity as measured by BMI is associated with cardiomyopathy, and none have confirmed diagnostic validity or looked at subtypes of cardiomyopathy.
“The already marked importance of weight control in youth is further strengthened by [our] findings,” the researchers wrote, “as well as greater evidence for obesity as a potential important cause of adverse cardiac remodeling independent of clinically evident ischemic heart disease.”
The study included 1,668,893 male adolescents who had enlisted for military service in Sweden between 1969 and 2005, when compulsory enlistment ended. It excluded women and the small proportion of men lacking weight or height data. A total of 4,477 cases of cardiomyopathy were diagnosed during follow-up, 59% were dilated cardiomyopathy, 15% were hypertrophic cardiomyopathy, and 11% were alcohol or drug-related cardiomyopathy.
The link between even slightly elevated BMI and dilated cardiomyopathy did not depend on age, year, location, or baseline comorbidities. For each unit increase in BMI, the adjusted risk of dilated cardiomyopathy rose by approximately 15%, the risk of hypertrophic cardiomyopathy rose by 9%, and the risk for drug- or alcohol-related cardiomyopathy rose by 10%. Estimated risks were generally similar after controlling for blood pressure, cardiorespiratory fitness, muscle strength, parents’ level of education, and alcohol or substance use disorders.
Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life, and Welfare. The researchers reported having no conflicts of interest.
SOURCE: Robertson J et al. Circulation. 2019 May 20.
and their risk increased as body mass index increased, according to the results of a nationwide, prospective, registry-based cohort study from Sweden.
The association was strongest for dilated cardiomyopathy, wrote Josefina Robertson, MD, and associates at the University of Gothenburg (Sweden). Over a median of 27 years of follow-up, the risk for dilated cardiomyopathy in adulthood was approximately 38% greater when adolescent body mass index was 22.5-25.0 kg/m2, using a lean but not underweight BMI (18.5-20.0 kg/m2) as the reference group. The increase in risk for dilated cardiomyopathy continued to rise with adolescent BMI and exceeded 700% at a BMI over 35.
The rate of hospitalizations for heart failure caused by cardiomyopathy more than doubled in Sweden from 1987 to 2006, the researchers noted. Adolescent obesity is strongly linked to early heart failure, but few studies have assessed whether adiposity as measured by BMI is associated with cardiomyopathy, and none have confirmed diagnostic validity or looked at subtypes of cardiomyopathy.
“The already marked importance of weight control in youth is further strengthened by [our] findings,” the researchers wrote, “as well as greater evidence for obesity as a potential important cause of adverse cardiac remodeling independent of clinically evident ischemic heart disease.”
The study included 1,668,893 male adolescents who had enlisted for military service in Sweden between 1969 and 2005, when compulsory enlistment ended. It excluded women and the small proportion of men lacking weight or height data. A total of 4,477 cases of cardiomyopathy were diagnosed during follow-up, 59% were dilated cardiomyopathy, 15% were hypertrophic cardiomyopathy, and 11% were alcohol or drug-related cardiomyopathy.
The link between even slightly elevated BMI and dilated cardiomyopathy did not depend on age, year, location, or baseline comorbidities. For each unit increase in BMI, the adjusted risk of dilated cardiomyopathy rose by approximately 15%, the risk of hypertrophic cardiomyopathy rose by 9%, and the risk for drug- or alcohol-related cardiomyopathy rose by 10%. Estimated risks were generally similar after controlling for blood pressure, cardiorespiratory fitness, muscle strength, parents’ level of education, and alcohol or substance use disorders.
Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life, and Welfare. The researchers reported having no conflicts of interest.
SOURCE: Robertson J et al. Circulation. 2019 May 20.
and their risk increased as body mass index increased, according to the results of a nationwide, prospective, registry-based cohort study from Sweden.
The association was strongest for dilated cardiomyopathy, wrote Josefina Robertson, MD, and associates at the University of Gothenburg (Sweden). Over a median of 27 years of follow-up, the risk for dilated cardiomyopathy in adulthood was approximately 38% greater when adolescent body mass index was 22.5-25.0 kg/m2, using a lean but not underweight BMI (18.5-20.0 kg/m2) as the reference group. The increase in risk for dilated cardiomyopathy continued to rise with adolescent BMI and exceeded 700% at a BMI over 35.
The rate of hospitalizations for heart failure caused by cardiomyopathy more than doubled in Sweden from 1987 to 2006, the researchers noted. Adolescent obesity is strongly linked to early heart failure, but few studies have assessed whether adiposity as measured by BMI is associated with cardiomyopathy, and none have confirmed diagnostic validity or looked at subtypes of cardiomyopathy.
“The already marked importance of weight control in youth is further strengthened by [our] findings,” the researchers wrote, “as well as greater evidence for obesity as a potential important cause of adverse cardiac remodeling independent of clinically evident ischemic heart disease.”
The study included 1,668,893 male adolescents who had enlisted for military service in Sweden between 1969 and 2005, when compulsory enlistment ended. It excluded women and the small proportion of men lacking weight or height data. A total of 4,477 cases of cardiomyopathy were diagnosed during follow-up, 59% were dilated cardiomyopathy, 15% were hypertrophic cardiomyopathy, and 11% were alcohol or drug-related cardiomyopathy.
The link between even slightly elevated BMI and dilated cardiomyopathy did not depend on age, year, location, or baseline comorbidities. For each unit increase in BMI, the adjusted risk of dilated cardiomyopathy rose by approximately 15%, the risk of hypertrophic cardiomyopathy rose by 9%, and the risk for drug- or alcohol-related cardiomyopathy rose by 10%. Estimated risks were generally similar after controlling for blood pressure, cardiorespiratory fitness, muscle strength, parents’ level of education, and alcohol or substance use disorders.
Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life, and Welfare. The researchers reported having no conflicts of interest.
SOURCE: Robertson J et al. Circulation. 2019 May 20.
FROM CIRCULATION
Key clinical point: Overweight in male teens predicts subsequent cardiomyopathy. The association increases with BMI and is strongest for dilated cardiomyopathy.
Major finding: Over a median of 27 years of follow-up, the hazard ratio for dilated cardiomyopathy in adulthood was 1.38 when adolescent body mass index was 22.5-25.0 kg/m2, using a BMI of 18.5-20.0 as the reference group. At a BMI over 35, the hazard ratio reached 8.11.
Study details: A nationwide, prospective registry cohort study of 1.67 million adolescent males in Sweden.
Disclosures: Funders included the Swedish government; Swedish Research Council; Swedish Heart and Lung Foundation; and Swedish Council for Health, Working Life and Welfare. The researchers reported having no conflicts of interest.
New risk score predicts cardiac-device infection
SAN FRANCISCO – Researchers have devised a five-item scoring formula to quantify the risk for infection in patients undergoing placement, revision, or removal of a cardiac-rhythm device based on data from nearly 20,000 patients enrolled in a recent infection-prophylaxis trial.
The risk score can help identify patients who might benefit from intensified antibiotic prophylaxis, and it can also help during shared decision making with patients to better understand the risk a patient faces from infection, compared with their predicted device benefit, David H. Birnie, MD, said at the annual scientific sessions of the Heart Rhythm Society.
The new risk score produced a concordance statistic, the area under the receiver-operator characteristic curve, of 0.704. It showed that, although it could use further validation, the score as it currently stands has substantial predictive value, said Dr. Birnie, professor of medicine at the University of Ottawa and deputy chief of cardiology at the University of Ottawa Heart Institute. “It’s certainly better than anything we have now,” he said in a video interview.
Dr. Birnie and his associates used data they collected on baseline characteristics and infection outcomes of the 19,603 patients enrolled in PADIT (Prevention of Arrhythmia Device Infection Trial) who underwent a rhythm-device procedure at 1 of 28 participating Canadian centers. The primary aim of PADIT was to assess the safety and efficacy of an intensified antibiotic-prophylaxis regimen, compared with a standard regimen of a cefazolin infusion just before the procedure. The study’s primary endpoint was the incidence of hospitalization for device infection during 1-year follow-up, and while the intensified prophylactic regimen linked with a 23% relative reduction in the hospitalization rate, compared with standard treatment, the difference was not statistically significant (J Am Coll Cardiol. 2018 Dec 18;72[24]:3098-109).
The researchers analyzed the baseline patient data and the blindly adjudicated infection outcomes and identified five factors that were independently associated with an increased infection rate. They organized the five factors and produced a formula they call the PADIT score (see chart). Those five factors are: prior procedures (the greater the number the greater the risk), age (which unexpectedly had an inverse relationship with infection incidence), depressed renal function, immuno-compromised status, and type of procedure. A patient can potentially score 0-15 points.
Among the PADIT patients a score of 0 correlated with about a 0.3% rate of hospitalization for a device-related infection during 1 year of follow-up, a score of 5 with about a 1.1% rate, a score of 6 with about a 1.8% rate, and a score of seven or more with a 3.4% infection rate over the following year. About 5% of patients had a score of 7 or more, and roughly another 5% had a score of 5 or 6, Dr. Birnie said. At his center, clinicians have begun routinely calculating scores for patients scheduled for an arrhythmia-device procedure, and they are considering routinely administering added antibiotic prophylaxis to patients with a preprocedural score of 6 or higher. They may also use the score to determine whether to use the antibacterial envelope recently reported to prevent cardiac-device infections (N Engl J Med. 2019 May 16;380[20]:1895-905).
“It’s very easy for patients to get to a PADIT score of 7 or higher,” Dr. Birnie noted. As an example, he cited a common patient, an 85-year-old with renal dysfunction who is under consideration for a second replacement of an implantable cardioverter defibrillator. The patient would score 1 point for renal insufficiency, 2 points for the type of device, and 4 points for having a prior history of two devices, and the consequent 3.4% risk for infection might counterbalance the potential benefit this elderly patient could expect from the new device. The score will be very important for targeting treatment, shared decision making, and selection of patients for future intervention trials, he concluded.
“I think this risk score will change practice by giving clinicians a better idea of a patient’s risk for infection,” commented Fred M. Kusumoto, MD, professor of medicine at the Mayo Medical School, Rochester, Minn., and director of heart rhythm services at the Mayo Clinic in Jacksonville, Fla. The PADIT score will help identify patients for whom leaving a device in place is a better option than taking it out because of their infection risk. The risk score could also help improve the cost effectiveness of preventive treatments, such as antibiotic-eluting envelopes, by targeting treatment to higher-risk patients, Dr. Kusumoto said during a press briefing.
SOURCE: Birnie DH. Heart Rhythm 2019, Absract S-LCT02-01.
I like this new infection risk score. It addresses a very clinically relevant issue. It’s important for the electrophysiology community to better understand how to best manage infections related to cardiac rhythm devices and ideally prevent them from happening.
I’m not a big fan of risk scores in general because they can sometimes detract from independent thinking about how to manage a patient. However, it is also helpful to have this type of risk-assessment information when discussing management options with a patient.
The PADIT risk score may also help identify which patients could potentially benefit the most from an antibiotic-eluting envelope when receiving an implanted cardiac-rhythm device. Recently reported results from WRAP-IT showed that routinely using envelopes cut the incidence of major infections by a relative 40%, but in absolute terms, the number needed to treat with the envelop to prevent one major infection was about 200 patients, a big number given the high cost of the envelope (N Engl J Med. 2019 May 16;380[20]:1895-905). It is therefore very interesting to think about using the PADIT risk score to better target an effective but expensive preventive measure like an antibiotic-eluting envelop to patients at the highest risk for infection.
Ulrika Birgersdotter-Green, MD , professor of medicine and director of pacemaker and ICD services at the University of California, San Diego, made these comments as a designated discussant for the report. She has been a consultant to and received honoraria from Abbott, Boston Scientific, and Medtronic.
I like this new infection risk score. It addresses a very clinically relevant issue. It’s important for the electrophysiology community to better understand how to best manage infections related to cardiac rhythm devices and ideally prevent them from happening.
I’m not a big fan of risk scores in general because they can sometimes detract from independent thinking about how to manage a patient. However, it is also helpful to have this type of risk-assessment information when discussing management options with a patient.
The PADIT risk score may also help identify which patients could potentially benefit the most from an antibiotic-eluting envelope when receiving an implanted cardiac-rhythm device. Recently reported results from WRAP-IT showed that routinely using envelopes cut the incidence of major infections by a relative 40%, but in absolute terms, the number needed to treat with the envelop to prevent one major infection was about 200 patients, a big number given the high cost of the envelope (N Engl J Med. 2019 May 16;380[20]:1895-905). It is therefore very interesting to think about using the PADIT risk score to better target an effective but expensive preventive measure like an antibiotic-eluting envelop to patients at the highest risk for infection.
Ulrika Birgersdotter-Green, MD , professor of medicine and director of pacemaker and ICD services at the University of California, San Diego, made these comments as a designated discussant for the report. She has been a consultant to and received honoraria from Abbott, Boston Scientific, and Medtronic.
I like this new infection risk score. It addresses a very clinically relevant issue. It’s important for the electrophysiology community to better understand how to best manage infections related to cardiac rhythm devices and ideally prevent them from happening.
I’m not a big fan of risk scores in general because they can sometimes detract from independent thinking about how to manage a patient. However, it is also helpful to have this type of risk-assessment information when discussing management options with a patient.
The PADIT risk score may also help identify which patients could potentially benefit the most from an antibiotic-eluting envelope when receiving an implanted cardiac-rhythm device. Recently reported results from WRAP-IT showed that routinely using envelopes cut the incidence of major infections by a relative 40%, but in absolute terms, the number needed to treat with the envelop to prevent one major infection was about 200 patients, a big number given the high cost of the envelope (N Engl J Med. 2019 May 16;380[20]:1895-905). It is therefore very interesting to think about using the PADIT risk score to better target an effective but expensive preventive measure like an antibiotic-eluting envelop to patients at the highest risk for infection.
Ulrika Birgersdotter-Green, MD , professor of medicine and director of pacemaker and ICD services at the University of California, San Diego, made these comments as a designated discussant for the report. She has been a consultant to and received honoraria from Abbott, Boston Scientific, and Medtronic.
SAN FRANCISCO – Researchers have devised a five-item scoring formula to quantify the risk for infection in patients undergoing placement, revision, or removal of a cardiac-rhythm device based on data from nearly 20,000 patients enrolled in a recent infection-prophylaxis trial.
The risk score can help identify patients who might benefit from intensified antibiotic prophylaxis, and it can also help during shared decision making with patients to better understand the risk a patient faces from infection, compared with their predicted device benefit, David H. Birnie, MD, said at the annual scientific sessions of the Heart Rhythm Society.
The new risk score produced a concordance statistic, the area under the receiver-operator characteristic curve, of 0.704. It showed that, although it could use further validation, the score as it currently stands has substantial predictive value, said Dr. Birnie, professor of medicine at the University of Ottawa and deputy chief of cardiology at the University of Ottawa Heart Institute. “It’s certainly better than anything we have now,” he said in a video interview.
Dr. Birnie and his associates used data they collected on baseline characteristics and infection outcomes of the 19,603 patients enrolled in PADIT (Prevention of Arrhythmia Device Infection Trial) who underwent a rhythm-device procedure at 1 of 28 participating Canadian centers. The primary aim of PADIT was to assess the safety and efficacy of an intensified antibiotic-prophylaxis regimen, compared with a standard regimen of a cefazolin infusion just before the procedure. The study’s primary endpoint was the incidence of hospitalization for device infection during 1-year follow-up, and while the intensified prophylactic regimen linked with a 23% relative reduction in the hospitalization rate, compared with standard treatment, the difference was not statistically significant (J Am Coll Cardiol. 2018 Dec 18;72[24]:3098-109).
The researchers analyzed the baseline patient data and the blindly adjudicated infection outcomes and identified five factors that were independently associated with an increased infection rate. They organized the five factors and produced a formula they call the PADIT score (see chart). Those five factors are: prior procedures (the greater the number the greater the risk), age (which unexpectedly had an inverse relationship with infection incidence), depressed renal function, immuno-compromised status, and type of procedure. A patient can potentially score 0-15 points.
Among the PADIT patients a score of 0 correlated with about a 0.3% rate of hospitalization for a device-related infection during 1 year of follow-up, a score of 5 with about a 1.1% rate, a score of 6 with about a 1.8% rate, and a score of seven or more with a 3.4% infection rate over the following year. About 5% of patients had a score of 7 or more, and roughly another 5% had a score of 5 or 6, Dr. Birnie said. At his center, clinicians have begun routinely calculating scores for patients scheduled for an arrhythmia-device procedure, and they are considering routinely administering added antibiotic prophylaxis to patients with a preprocedural score of 6 or higher. They may also use the score to determine whether to use the antibacterial envelope recently reported to prevent cardiac-device infections (N Engl J Med. 2019 May 16;380[20]:1895-905).
“It’s very easy for patients to get to a PADIT score of 7 or higher,” Dr. Birnie noted. As an example, he cited a common patient, an 85-year-old with renal dysfunction who is under consideration for a second replacement of an implantable cardioverter defibrillator. The patient would score 1 point for renal insufficiency, 2 points for the type of device, and 4 points for having a prior history of two devices, and the consequent 3.4% risk for infection might counterbalance the potential benefit this elderly patient could expect from the new device. The score will be very important for targeting treatment, shared decision making, and selection of patients for future intervention trials, he concluded.
“I think this risk score will change practice by giving clinicians a better idea of a patient’s risk for infection,” commented Fred M. Kusumoto, MD, professor of medicine at the Mayo Medical School, Rochester, Minn., and director of heart rhythm services at the Mayo Clinic in Jacksonville, Fla. The PADIT score will help identify patients for whom leaving a device in place is a better option than taking it out because of their infection risk. The risk score could also help improve the cost effectiveness of preventive treatments, such as antibiotic-eluting envelopes, by targeting treatment to higher-risk patients, Dr. Kusumoto said during a press briefing.
SOURCE: Birnie DH. Heart Rhythm 2019, Absract S-LCT02-01.
SAN FRANCISCO – Researchers have devised a five-item scoring formula to quantify the risk for infection in patients undergoing placement, revision, or removal of a cardiac-rhythm device based on data from nearly 20,000 patients enrolled in a recent infection-prophylaxis trial.
The risk score can help identify patients who might benefit from intensified antibiotic prophylaxis, and it can also help during shared decision making with patients to better understand the risk a patient faces from infection, compared with their predicted device benefit, David H. Birnie, MD, said at the annual scientific sessions of the Heart Rhythm Society.
The new risk score produced a concordance statistic, the area under the receiver-operator characteristic curve, of 0.704. It showed that, although it could use further validation, the score as it currently stands has substantial predictive value, said Dr. Birnie, professor of medicine at the University of Ottawa and deputy chief of cardiology at the University of Ottawa Heart Institute. “It’s certainly better than anything we have now,” he said in a video interview.
Dr. Birnie and his associates used data they collected on baseline characteristics and infection outcomes of the 19,603 patients enrolled in PADIT (Prevention of Arrhythmia Device Infection Trial) who underwent a rhythm-device procedure at 1 of 28 participating Canadian centers. The primary aim of PADIT was to assess the safety and efficacy of an intensified antibiotic-prophylaxis regimen, compared with a standard regimen of a cefazolin infusion just before the procedure. The study’s primary endpoint was the incidence of hospitalization for device infection during 1-year follow-up, and while the intensified prophylactic regimen linked with a 23% relative reduction in the hospitalization rate, compared with standard treatment, the difference was not statistically significant (J Am Coll Cardiol. 2018 Dec 18;72[24]:3098-109).
The researchers analyzed the baseline patient data and the blindly adjudicated infection outcomes and identified five factors that were independently associated with an increased infection rate. They organized the five factors and produced a formula they call the PADIT score (see chart). Those five factors are: prior procedures (the greater the number the greater the risk), age (which unexpectedly had an inverse relationship with infection incidence), depressed renal function, immuno-compromised status, and type of procedure. A patient can potentially score 0-15 points.
Among the PADIT patients a score of 0 correlated with about a 0.3% rate of hospitalization for a device-related infection during 1 year of follow-up, a score of 5 with about a 1.1% rate, a score of 6 with about a 1.8% rate, and a score of seven or more with a 3.4% infection rate over the following year. About 5% of patients had a score of 7 or more, and roughly another 5% had a score of 5 or 6, Dr. Birnie said. At his center, clinicians have begun routinely calculating scores for patients scheduled for an arrhythmia-device procedure, and they are considering routinely administering added antibiotic prophylaxis to patients with a preprocedural score of 6 or higher. They may also use the score to determine whether to use the antibacterial envelope recently reported to prevent cardiac-device infections (N Engl J Med. 2019 May 16;380[20]:1895-905).
“It’s very easy for patients to get to a PADIT score of 7 or higher,” Dr. Birnie noted. As an example, he cited a common patient, an 85-year-old with renal dysfunction who is under consideration for a second replacement of an implantable cardioverter defibrillator. The patient would score 1 point for renal insufficiency, 2 points for the type of device, and 4 points for having a prior history of two devices, and the consequent 3.4% risk for infection might counterbalance the potential benefit this elderly patient could expect from the new device. The score will be very important for targeting treatment, shared decision making, and selection of patients for future intervention trials, he concluded.
“I think this risk score will change practice by giving clinicians a better idea of a patient’s risk for infection,” commented Fred M. Kusumoto, MD, professor of medicine at the Mayo Medical School, Rochester, Minn., and director of heart rhythm services at the Mayo Clinic in Jacksonville, Fla. The PADIT score will help identify patients for whom leaving a device in place is a better option than taking it out because of their infection risk. The risk score could also help improve the cost effectiveness of preventive treatments, such as antibiotic-eluting envelopes, by targeting treatment to higher-risk patients, Dr. Kusumoto said during a press briefing.
SOURCE: Birnie DH. Heart Rhythm 2019, Absract S-LCT02-01.
REPORTING FROM HEART RHYTHM 2019
Key clinical point: Researchers have devised a five-item scoring formula to predict a patient’s risk for infection from an cardiac rhythm–device procedure.
Major finding: The risk score had an optimism-corrected concordance statistic of 0.704.
Study details: Investigators developed the risk score using data from PADIT, a multicenter, randomized trial with 19,603 patients.
Disclosures: PADIT received no commercial funding. Dr. Birnie had no relevant disclosures.
Source: Birnie DH. Heart Rhythm 2019, Absract S-LCT02-01.
Severe OSA increases cardiovascular risk after surgery
Unrecognized severe obstructive sleep apnea is a risk factor for cardiovascular complications after major noncardiac surgery, according to a study published in JAMA.
The researchers state that perioperative mismanagement of obstructive sleep apnea can lead to serious medical consequences. “General anesthetics, sedatives, and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilatory response to hypoxemia and hypercapnia. Each of these events exacerbates [obstructive sleep apnea] and may predispose patients to postoperative cardiovascular complications,” said researchers who conducted the The Postoperative vascular complications in unrecognised Obstructive Sleep apnoea (POSA) study (NCT01494181).
They undertook a prospective observational cohort study involving 1,218 patients undergoing major noncardiac surgery, who were already considered at high risk of postoperative cardiovascular events – having, for example, a history of coronary artery disease, stroke, diabetes, or renal impairment. However, none had a prior diagnosis of obstructive sleep apnea.
Preoperative sleep monitoring revealed that two-thirds of the cohort had unrecognized and untreated obstructive sleep apnea, including 11.2% with severe obstructive sleep apnea.
At 30 days after surgery, patients with obstructive sleep apnea had a 49% higher risk of the primary outcome of myocardial injury, cardiac death, heart failure, thromboembolism, atrial fibrillation, or stroke, compared with those without obstructive sleep apnea.
However, this association was largely due to a significant 2.23-fold higher risk among patients with severe obstructive sleep apnea, while those with only moderate or mild sleep apnea did not show a significant increased risk of cardiovascular complications.
Patients in this study with severe obstructive sleep apnea had a 13-fold higher risk of cardiac death, 80% higher risk of myocardial injury, more than sixfold higher risk of heart failure, and nearly fourfold higher risk of atrial fibrillation.
Researchers also saw an association between obstructive sleep apnea and increased risk of infective outcomes, unplanned tracheal intubation, postoperative lung ventilation, and readmission to the ICU.
The majority of patients received nocturnal oximetry monitoring during their first 3 nights after surgery. This revealed that patients without obstructive sleep apnea had significant increases in oxygen desaturation index during their first night after surgery, while those with sleep apnea did not return to their baseline oxygen desaturation index until the third night after surgery.
“Despite a substantial decrease in ODI [oxygen desaturation index] with oxygen therapy in patients with OSA during the first 3 postoperative nights, supplemental oxygen did not modify the association between OSA and postoperative cardiovascular event,” wrote Matthew T.V. Chan, MD, of Chinese University of Hong Kong, Prince of Wales Hospital, and coauthors.
Given that the events were associated with longer durations of severe oxyhemoglobin desaturation, more aggressive interventions such as positive airway pressure or oral appliances may be required, they noted.
“However, high-level evidence demonstrating the effect of these measures on perioperative outcomes is lacking [and] further clinical trials are now required to test if additional monitoring or alternative interventions would reduce the risk,” they wrote.
The study was supported by the Health and Medical Research Fund (Hong Kong), National Healthcare Group–Khoo Teck Puat Hospital, University Health Network Foundation, University of Malaya, Malaysian Society of Anaesthesiologists, Auckland Medical Research Foundation, and ResMed. One author declared grants from private industry and a patent pending on an obstructive sleep apnea risk questionnaire used in the study.
SOURCE: Chan M et al. JAMA 2019;321[18]:1788-98. doi: 10.1001/jama.2019.4783.
This study is large, prospective, and rigorous and adds important new information to the puzzle of the impact of sleep apnea on postoperative risk, Dennis Auckley, MD, and Stavros Memtsoudis, MD, wrote in an editorial accompanying this study. The study focused on predetermined clinically significant and measurable events, used standardized and objective sleep apnea testing, and attempted to control for many of the confounders that might have influenced outcomes.
The results suggest that obstructive sleep apnea should be recognized as a major perioperative risk factor, and it should receive the same attention and optimization efforts as comorbidities such as diabetes.
Dr. Auckley is from the division of pulmonary, critical care and sleep medicine at MetroHealth Medical Center, Case Western Reserve University, Cleveland, and Dr. Memtsoudis is clinical professor of anesthesiology at Cornell University, New York. These comments are adapted from an editorial (JAMA 2019;231[18]:1775-6). Both declared board and executive positions with the Society of Anesthesia and Sleep Medicine. Dr. Auckley declared research funding from Medtronic, and Dr. Memtsoudis declared personal fees from Teikoku and Sandoz.
This study is large, prospective, and rigorous and adds important new information to the puzzle of the impact of sleep apnea on postoperative risk, Dennis Auckley, MD, and Stavros Memtsoudis, MD, wrote in an editorial accompanying this study. The study focused on predetermined clinically significant and measurable events, used standardized and objective sleep apnea testing, and attempted to control for many of the confounders that might have influenced outcomes.
The results suggest that obstructive sleep apnea should be recognized as a major perioperative risk factor, and it should receive the same attention and optimization efforts as comorbidities such as diabetes.
Dr. Auckley is from the division of pulmonary, critical care and sleep medicine at MetroHealth Medical Center, Case Western Reserve University, Cleveland, and Dr. Memtsoudis is clinical professor of anesthesiology at Cornell University, New York. These comments are adapted from an editorial (JAMA 2019;231[18]:1775-6). Both declared board and executive positions with the Society of Anesthesia and Sleep Medicine. Dr. Auckley declared research funding from Medtronic, and Dr. Memtsoudis declared personal fees from Teikoku and Sandoz.
This study is large, prospective, and rigorous and adds important new information to the puzzle of the impact of sleep apnea on postoperative risk, Dennis Auckley, MD, and Stavros Memtsoudis, MD, wrote in an editorial accompanying this study. The study focused on predetermined clinically significant and measurable events, used standardized and objective sleep apnea testing, and attempted to control for many of the confounders that might have influenced outcomes.
The results suggest that obstructive sleep apnea should be recognized as a major perioperative risk factor, and it should receive the same attention and optimization efforts as comorbidities such as diabetes.
Dr. Auckley is from the division of pulmonary, critical care and sleep medicine at MetroHealth Medical Center, Case Western Reserve University, Cleveland, and Dr. Memtsoudis is clinical professor of anesthesiology at Cornell University, New York. These comments are adapted from an editorial (JAMA 2019;231[18]:1775-6). Both declared board and executive positions with the Society of Anesthesia and Sleep Medicine. Dr. Auckley declared research funding from Medtronic, and Dr. Memtsoudis declared personal fees from Teikoku and Sandoz.
Unrecognized severe obstructive sleep apnea is a risk factor for cardiovascular complications after major noncardiac surgery, according to a study published in JAMA.
The researchers state that perioperative mismanagement of obstructive sleep apnea can lead to serious medical consequences. “General anesthetics, sedatives, and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilatory response to hypoxemia and hypercapnia. Each of these events exacerbates [obstructive sleep apnea] and may predispose patients to postoperative cardiovascular complications,” said researchers who conducted the The Postoperative vascular complications in unrecognised Obstructive Sleep apnoea (POSA) study (NCT01494181).
They undertook a prospective observational cohort study involving 1,218 patients undergoing major noncardiac surgery, who were already considered at high risk of postoperative cardiovascular events – having, for example, a history of coronary artery disease, stroke, diabetes, or renal impairment. However, none had a prior diagnosis of obstructive sleep apnea.
Preoperative sleep monitoring revealed that two-thirds of the cohort had unrecognized and untreated obstructive sleep apnea, including 11.2% with severe obstructive sleep apnea.
At 30 days after surgery, patients with obstructive sleep apnea had a 49% higher risk of the primary outcome of myocardial injury, cardiac death, heart failure, thromboembolism, atrial fibrillation, or stroke, compared with those without obstructive sleep apnea.
However, this association was largely due to a significant 2.23-fold higher risk among patients with severe obstructive sleep apnea, while those with only moderate or mild sleep apnea did not show a significant increased risk of cardiovascular complications.
Patients in this study with severe obstructive sleep apnea had a 13-fold higher risk of cardiac death, 80% higher risk of myocardial injury, more than sixfold higher risk of heart failure, and nearly fourfold higher risk of atrial fibrillation.
Researchers also saw an association between obstructive sleep apnea and increased risk of infective outcomes, unplanned tracheal intubation, postoperative lung ventilation, and readmission to the ICU.
The majority of patients received nocturnal oximetry monitoring during their first 3 nights after surgery. This revealed that patients without obstructive sleep apnea had significant increases in oxygen desaturation index during their first night after surgery, while those with sleep apnea did not return to their baseline oxygen desaturation index until the third night after surgery.
“Despite a substantial decrease in ODI [oxygen desaturation index] with oxygen therapy in patients with OSA during the first 3 postoperative nights, supplemental oxygen did not modify the association between OSA and postoperative cardiovascular event,” wrote Matthew T.V. Chan, MD, of Chinese University of Hong Kong, Prince of Wales Hospital, and coauthors.
Given that the events were associated with longer durations of severe oxyhemoglobin desaturation, more aggressive interventions such as positive airway pressure or oral appliances may be required, they noted.
“However, high-level evidence demonstrating the effect of these measures on perioperative outcomes is lacking [and] further clinical trials are now required to test if additional monitoring or alternative interventions would reduce the risk,” they wrote.
The study was supported by the Health and Medical Research Fund (Hong Kong), National Healthcare Group–Khoo Teck Puat Hospital, University Health Network Foundation, University of Malaya, Malaysian Society of Anaesthesiologists, Auckland Medical Research Foundation, and ResMed. One author declared grants from private industry and a patent pending on an obstructive sleep apnea risk questionnaire used in the study.
SOURCE: Chan M et al. JAMA 2019;321[18]:1788-98. doi: 10.1001/jama.2019.4783.
Unrecognized severe obstructive sleep apnea is a risk factor for cardiovascular complications after major noncardiac surgery, according to a study published in JAMA.
The researchers state that perioperative mismanagement of obstructive sleep apnea can lead to serious medical consequences. “General anesthetics, sedatives, and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilatory response to hypoxemia and hypercapnia. Each of these events exacerbates [obstructive sleep apnea] and may predispose patients to postoperative cardiovascular complications,” said researchers who conducted the The Postoperative vascular complications in unrecognised Obstructive Sleep apnoea (POSA) study (NCT01494181).
They undertook a prospective observational cohort study involving 1,218 patients undergoing major noncardiac surgery, who were already considered at high risk of postoperative cardiovascular events – having, for example, a history of coronary artery disease, stroke, diabetes, or renal impairment. However, none had a prior diagnosis of obstructive sleep apnea.
Preoperative sleep monitoring revealed that two-thirds of the cohort had unrecognized and untreated obstructive sleep apnea, including 11.2% with severe obstructive sleep apnea.
At 30 days after surgery, patients with obstructive sleep apnea had a 49% higher risk of the primary outcome of myocardial injury, cardiac death, heart failure, thromboembolism, atrial fibrillation, or stroke, compared with those without obstructive sleep apnea.
However, this association was largely due to a significant 2.23-fold higher risk among patients with severe obstructive sleep apnea, while those with only moderate or mild sleep apnea did not show a significant increased risk of cardiovascular complications.
Patients in this study with severe obstructive sleep apnea had a 13-fold higher risk of cardiac death, 80% higher risk of myocardial injury, more than sixfold higher risk of heart failure, and nearly fourfold higher risk of atrial fibrillation.
Researchers also saw an association between obstructive sleep apnea and increased risk of infective outcomes, unplanned tracheal intubation, postoperative lung ventilation, and readmission to the ICU.
The majority of patients received nocturnal oximetry monitoring during their first 3 nights after surgery. This revealed that patients without obstructive sleep apnea had significant increases in oxygen desaturation index during their first night after surgery, while those with sleep apnea did not return to their baseline oxygen desaturation index until the third night after surgery.
“Despite a substantial decrease in ODI [oxygen desaturation index] with oxygen therapy in patients with OSA during the first 3 postoperative nights, supplemental oxygen did not modify the association between OSA and postoperative cardiovascular event,” wrote Matthew T.V. Chan, MD, of Chinese University of Hong Kong, Prince of Wales Hospital, and coauthors.
Given that the events were associated with longer durations of severe oxyhemoglobin desaturation, more aggressive interventions such as positive airway pressure or oral appliances may be required, they noted.
“However, high-level evidence demonstrating the effect of these measures on perioperative outcomes is lacking [and] further clinical trials are now required to test if additional monitoring or alternative interventions would reduce the risk,” they wrote.
The study was supported by the Health and Medical Research Fund (Hong Kong), National Healthcare Group–Khoo Teck Puat Hospital, University Health Network Foundation, University of Malaya, Malaysian Society of Anaesthesiologists, Auckland Medical Research Foundation, and ResMed. One author declared grants from private industry and a patent pending on an obstructive sleep apnea risk questionnaire used in the study.
SOURCE: Chan M et al. JAMA 2019;321[18]:1788-98. doi: 10.1001/jama.2019.4783.
FROM JAMA
Arsenic exposure increases risk of left ventricular hypertrophy
Young Native Americans had increased left ventricular thickness and left ventricular hypertrophy after being exposed to arsenic, and had a greater risk if they showed signs of prehypertension or hypertension, according to recent research.
“The stronger association in subjects with elevated blood pressure suggests that individuals with preclinical heart disease might be more prone to the toxic effects of arsenic on the heart,” Gernot Pichler, MD, PhD, a cardiologist at Hospital Hietzing/Heart Center Clinic Floridsdorf in Vienna, stated in a press release.
Dr. Pichler and colleagues evaluated 1,337 individuals (mean age, 31 years; 61% female) in the Strong Heart Family Study, an extension of the Strong Heart Study that was designed to study cardiovascular disease in Native Americans. The researchers noted that, while the studies were not originally intended to evaluate arsenic exposure in these populations, “the importance of studying arsenic was recognized overtime as increasing evidence supported the role of arsenic in cardiovascular disease and the relatively high arsenic exposure in tribal communities, compared to other general populations in the United States.”
Arsenic exposure was determined through the sum of inorganic and methylated arsenic concentrations in urine, and researchers used transthoracic ECG at baseline and follow-up to compare left ventricular geometry and function. The mean follow-up was 5.6 years and baseline median sum of inorganic and methylated arsenic concentrations in urine was 4.24 (interquartile range, 2.82-6.90) mcg/g creatinine.
Prevalence of left ventricular hypertrophy was 4.6% overall, and the odds ratio of left ventricular hypertrophy per 100% increase in arsenic in the urine was 1.47 (95% confidence interval, 1.05-2.08) overall and 1.58 for individuals with prehypertension or hypertension (95% CI, 1.04-2.41).
“People drinking water from private wells, which are not regulated, need to be aware that arsenic may increase the risk for cardiovascular disease,” said Dr. Pichler. “Testing those wells is a critical first step to take action and prevent exposure.”
Prospective and cross-sectional analyses both showed changes in left ventricular geometry – such as in the left atrial systolic diameter, interventricular septum, and left ventricular posterior wall thickness and mass index – were associated with exposure to arsenic. In addition, left ventricular function factors such as isovolumic relaxation time and stroke volume were also affected by arsenic exposure. However, the researchers noted that their study was limited by a single method of arsenic exposure and having no long-term follow-up for participants.
“The study raises the question of whether the changes in heart structure are reversible if exposure is reduced. Some changes have occurred in water sources in the study communities, and it will be important to check the potential health impact of reducing arsenic exposure,” said Dr. Pichler.
This study was funded by the National Institute of Health Sciences and grants from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
SOURCE: Pichler G et al. Circ Cardiovasc Imaging. 2019 May 1. doi: 10.1161/CIRCIMAGING.119.009018.
The results from Pichler et al. show the effects of recent arsenic exposure on left ventricular (LV) hypertrophy, but other questions remain as to the long-term effects of arsenic and its interactions with other environmental metals, Rajiv Chowdhury, MBBS, PhD, and Kim van Daalen, BSc, MPhil, wrote in a related editorial.
It has been established that chronic, low to moderate inorganic arsenic exposure may be linked to cardiovascular disease (CVD) and risk factors such as hypertension and diabetes, but it is unclear how different exposure pathways contribute as well as what pathophysiological mechanisms contribute to CVD, and whether arsenic directly or indirectly contributes to cardiac functioning or a worse cardiometabolic profile, respectively, they wrote.
While the results contribute to the understanding of arsenic exposure through drinking water and its relationship to LV function and geometry, urinary arsenic reflects recent exposure and cannot measure arsenic exposure over a period of time. The study also does not account for an individual’s CVD risk or LV functioning/geometry with daily exposure to co-occurring environmental metals, particularly heavy metals, together with arsenic. Factors such as genetics, age, gender, and nutrition also impact an individual’s reaction to arsenic, and studies should be able to differentiate inorganic arsenic obtained from food and other sources.
While “this elegant analysis ... helps to clarify the observational associations of [arsenic] with LV geometry and function, it stimulates further complimentary work,” they wrote. “Such studies would be essential since CVD remains the single leading cause of adult premature death worldwide, and millions of individuals globally are exposed to arsenic and other metal contaminants.”
Dr. Chowdhury and Dr. Daalen are from the cardiovascular epidemiology unit in the department of public health and primary care at the University of Cambridge (England).
The results from Pichler et al. show the effects of recent arsenic exposure on left ventricular (LV) hypertrophy, but other questions remain as to the long-term effects of arsenic and its interactions with other environmental metals, Rajiv Chowdhury, MBBS, PhD, and Kim van Daalen, BSc, MPhil, wrote in a related editorial.
It has been established that chronic, low to moderate inorganic arsenic exposure may be linked to cardiovascular disease (CVD) and risk factors such as hypertension and diabetes, but it is unclear how different exposure pathways contribute as well as what pathophysiological mechanisms contribute to CVD, and whether arsenic directly or indirectly contributes to cardiac functioning or a worse cardiometabolic profile, respectively, they wrote.
While the results contribute to the understanding of arsenic exposure through drinking water and its relationship to LV function and geometry, urinary arsenic reflects recent exposure and cannot measure arsenic exposure over a period of time. The study also does not account for an individual’s CVD risk or LV functioning/geometry with daily exposure to co-occurring environmental metals, particularly heavy metals, together with arsenic. Factors such as genetics, age, gender, and nutrition also impact an individual’s reaction to arsenic, and studies should be able to differentiate inorganic arsenic obtained from food and other sources.
While “this elegant analysis ... helps to clarify the observational associations of [arsenic] with LV geometry and function, it stimulates further complimentary work,” they wrote. “Such studies would be essential since CVD remains the single leading cause of adult premature death worldwide, and millions of individuals globally are exposed to arsenic and other metal contaminants.”
Dr. Chowdhury and Dr. Daalen are from the cardiovascular epidemiology unit in the department of public health and primary care at the University of Cambridge (England).
The results from Pichler et al. show the effects of recent arsenic exposure on left ventricular (LV) hypertrophy, but other questions remain as to the long-term effects of arsenic and its interactions with other environmental metals, Rajiv Chowdhury, MBBS, PhD, and Kim van Daalen, BSc, MPhil, wrote in a related editorial.
It has been established that chronic, low to moderate inorganic arsenic exposure may be linked to cardiovascular disease (CVD) and risk factors such as hypertension and diabetes, but it is unclear how different exposure pathways contribute as well as what pathophysiological mechanisms contribute to CVD, and whether arsenic directly or indirectly contributes to cardiac functioning or a worse cardiometabolic profile, respectively, they wrote.
While the results contribute to the understanding of arsenic exposure through drinking water and its relationship to LV function and geometry, urinary arsenic reflects recent exposure and cannot measure arsenic exposure over a period of time. The study also does not account for an individual’s CVD risk or LV functioning/geometry with daily exposure to co-occurring environmental metals, particularly heavy metals, together with arsenic. Factors such as genetics, age, gender, and nutrition also impact an individual’s reaction to arsenic, and studies should be able to differentiate inorganic arsenic obtained from food and other sources.
While “this elegant analysis ... helps to clarify the observational associations of [arsenic] with LV geometry and function, it stimulates further complimentary work,” they wrote. “Such studies would be essential since CVD remains the single leading cause of adult premature death worldwide, and millions of individuals globally are exposed to arsenic and other metal contaminants.”
Dr. Chowdhury and Dr. Daalen are from the cardiovascular epidemiology unit in the department of public health and primary care at the University of Cambridge (England).
Young Native Americans had increased left ventricular thickness and left ventricular hypertrophy after being exposed to arsenic, and had a greater risk if they showed signs of prehypertension or hypertension, according to recent research.
“The stronger association in subjects with elevated blood pressure suggests that individuals with preclinical heart disease might be more prone to the toxic effects of arsenic on the heart,” Gernot Pichler, MD, PhD, a cardiologist at Hospital Hietzing/Heart Center Clinic Floridsdorf in Vienna, stated in a press release.
Dr. Pichler and colleagues evaluated 1,337 individuals (mean age, 31 years; 61% female) in the Strong Heart Family Study, an extension of the Strong Heart Study that was designed to study cardiovascular disease in Native Americans. The researchers noted that, while the studies were not originally intended to evaluate arsenic exposure in these populations, “the importance of studying arsenic was recognized overtime as increasing evidence supported the role of arsenic in cardiovascular disease and the relatively high arsenic exposure in tribal communities, compared to other general populations in the United States.”
Arsenic exposure was determined through the sum of inorganic and methylated arsenic concentrations in urine, and researchers used transthoracic ECG at baseline and follow-up to compare left ventricular geometry and function. The mean follow-up was 5.6 years and baseline median sum of inorganic and methylated arsenic concentrations in urine was 4.24 (interquartile range, 2.82-6.90) mcg/g creatinine.
Prevalence of left ventricular hypertrophy was 4.6% overall, and the odds ratio of left ventricular hypertrophy per 100% increase in arsenic in the urine was 1.47 (95% confidence interval, 1.05-2.08) overall and 1.58 for individuals with prehypertension or hypertension (95% CI, 1.04-2.41).
“People drinking water from private wells, which are not regulated, need to be aware that arsenic may increase the risk for cardiovascular disease,” said Dr. Pichler. “Testing those wells is a critical first step to take action and prevent exposure.”
Prospective and cross-sectional analyses both showed changes in left ventricular geometry – such as in the left atrial systolic diameter, interventricular septum, and left ventricular posterior wall thickness and mass index – were associated with exposure to arsenic. In addition, left ventricular function factors such as isovolumic relaxation time and stroke volume were also affected by arsenic exposure. However, the researchers noted that their study was limited by a single method of arsenic exposure and having no long-term follow-up for participants.
“The study raises the question of whether the changes in heart structure are reversible if exposure is reduced. Some changes have occurred in water sources in the study communities, and it will be important to check the potential health impact of reducing arsenic exposure,” said Dr. Pichler.
This study was funded by the National Institute of Health Sciences and grants from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
SOURCE: Pichler G et al. Circ Cardiovasc Imaging. 2019 May 1. doi: 10.1161/CIRCIMAGING.119.009018.
Young Native Americans had increased left ventricular thickness and left ventricular hypertrophy after being exposed to arsenic, and had a greater risk if they showed signs of prehypertension or hypertension, according to recent research.
“The stronger association in subjects with elevated blood pressure suggests that individuals with preclinical heart disease might be more prone to the toxic effects of arsenic on the heart,” Gernot Pichler, MD, PhD, a cardiologist at Hospital Hietzing/Heart Center Clinic Floridsdorf in Vienna, stated in a press release.
Dr. Pichler and colleagues evaluated 1,337 individuals (mean age, 31 years; 61% female) in the Strong Heart Family Study, an extension of the Strong Heart Study that was designed to study cardiovascular disease in Native Americans. The researchers noted that, while the studies were not originally intended to evaluate arsenic exposure in these populations, “the importance of studying arsenic was recognized overtime as increasing evidence supported the role of arsenic in cardiovascular disease and the relatively high arsenic exposure in tribal communities, compared to other general populations in the United States.”
Arsenic exposure was determined through the sum of inorganic and methylated arsenic concentrations in urine, and researchers used transthoracic ECG at baseline and follow-up to compare left ventricular geometry and function. The mean follow-up was 5.6 years and baseline median sum of inorganic and methylated arsenic concentrations in urine was 4.24 (interquartile range, 2.82-6.90) mcg/g creatinine.
Prevalence of left ventricular hypertrophy was 4.6% overall, and the odds ratio of left ventricular hypertrophy per 100% increase in arsenic in the urine was 1.47 (95% confidence interval, 1.05-2.08) overall and 1.58 for individuals with prehypertension or hypertension (95% CI, 1.04-2.41).
“People drinking water from private wells, which are not regulated, need to be aware that arsenic may increase the risk for cardiovascular disease,” said Dr. Pichler. “Testing those wells is a critical first step to take action and prevent exposure.”
Prospective and cross-sectional analyses both showed changes in left ventricular geometry – such as in the left atrial systolic diameter, interventricular septum, and left ventricular posterior wall thickness and mass index – were associated with exposure to arsenic. In addition, left ventricular function factors such as isovolumic relaxation time and stroke volume were also affected by arsenic exposure. However, the researchers noted that their study was limited by a single method of arsenic exposure and having no long-term follow-up for participants.
“The study raises the question of whether the changes in heart structure are reversible if exposure is reduced. Some changes have occurred in water sources in the study communities, and it will be important to check the potential health impact of reducing arsenic exposure,” said Dr. Pichler.
This study was funded by the National Institute of Health Sciences and grants from the National Heart, Lung, and Blood Institute. The authors reported no relevant conflicts of interest.
SOURCE: Pichler G et al. Circ Cardiovasc Imaging. 2019 May 1. doi: 10.1161/CIRCIMAGING.119.009018.
FROM CIRCULATION: CARDIOVASCULAR IMAGING
Higher plasma cell-free DNA tracks with worse PAH survival
NEW ORLEANS – Cell-free (cf) DNA looked like an informative biomarker for both the severity of pulmonary artery hypertension and the survival prognosis for patients with this disease, based on results from two preliminary studies involving a total of 173 people.
“Plasma levels of cell-free DNA are elevated in patients with pulmonary artery hypertension, compared with healthy controls, and may predict disease severity and mortality,” Samuel B. Brusca, MD, said at the at the annual meeting of the American College of Cardiology.
A growing biomedical literature has documented a role for cfDNA in tracking the course of cancer, septic shock, and transplanted organs (Transplantation. 2019 Feb;103[2]:273-83) (Cell-Free DNA: Applications in Different Diseases, in “Cell-free DNA as Diagnostic Markers.” [New York: Humana Press, 2018, pp. 3-12]). Based on this background Dr. Brusca and his associates decided to examine whether plasma levels of cfDNA linked with pulmonary artery hypertension (PAH) severity and survival.
Their first study included seven patients with mild PAH (defined as patients with a tricuspid annular plane systolic excursion [TAPSE] of more than 18 mm and a maximum oxygen uptake [VO2] of at least 75% of predicted), eight with severe PAH (a TAPSE of 18 mm or less and a VO2 of less than 75%), and seven healthy adult controls. Measurement of plasma cfDNA showed an average level of 19.4 ng/mL among the healthy controls (prior reports had indicated that 10-20 ng/mL were normal levels), 22.0 ng/mL among patients with mild PAH, and 36.2 ng/mL in those with severe PAH. The level among the severe PAH patients was significantly higher than the level in controls by two different statistical tests, said Dr. Brusca, a critical care medicine physician at the National Institutes of Health Clinical Center in Bethesda, Md.
The second analysis by Dr. Brusca and his associates included 151 PAH patients followed by physicians at the Clinical Center for an average of 40 months. Their analysis tracked survival of these patients relative to their baseline levels of cfDNA and divided into tertiles. Patients in the lowest tertile had a starting cfDNA level of up to 39 ng/mL, those in the middle tertile had levels of 39.1-64.0 ng/mL, and those in the top tertile had levels of at least 64.1 ng/mL. A Kaplan-Meier analysis showed statistically significant differences in survival rates between each of the tertiles. Patients in the lowest tertile had a 5-year actuarial survival rate of about 65%, those in the middle tertile had a survival rate of about 48%, and those in the tertile with the highest level of cfDNA had a survival rate of about 28%.
Additional studies of cfDNA are needed in larger numbers of PAH patients, and cfDNA levels should be compared with levels of other, more established biomarkers, such as inflammatory cytokines, Dr. Brusca said in an interview.
Dr. Brusca had no disclosures. The study received no commercial funding.
SOURCE: Brusca SB et al. J Am Coll Cardiol. 2019 March 12;73(9 Suppl 1):1897.
I was very excited to hear Dr. Brusca’s report on using cell-free (cf) DNA to track the severity of pulmonary artery hypertension and survival of these patients. I’m now using cfDNA frequently to monitor heart transplant patients, and the information it provides has been very valuable. But cfDNA may be even better suited to assessing patients with pulmonary artery hypertension (PAH) because it’s a vascular disease, and increases in cfDNA appears to reflect damage to the vascular endothelium. It’s a brilliant application of this technology. Brain natriuretic peptide and troponin are markers of right heart damage, but cfDNA appears to be able to track the progression of the vascular component of PAH. It appears to be the first disease-specific biomarker we have for PAH. It’s time to start routinely measuring levels of cfDNA in trials so we can gather more data on the clinical correlates of changing levels of this biomarker.
I was very excited to hear Dr. Brusca’s report on using cell-free (cf) DNA to track the severity of pulmonary artery hypertension and survival of these patients. I’m now using cfDNA frequently to monitor heart transplant patients, and the information it provides has been very valuable. But cfDNA may be even better suited to assessing patients with pulmonary artery hypertension (PAH) because it’s a vascular disease, and increases in cfDNA appears to reflect damage to the vascular endothelium. It’s a brilliant application of this technology. Brain natriuretic peptide and troponin are markers of right heart damage, but cfDNA appears to be able to track the progression of the vascular component of PAH. It appears to be the first disease-specific biomarker we have for PAH. It’s time to start routinely measuring levels of cfDNA in trials so we can gather more data on the clinical correlates of changing levels of this biomarker.
I was very excited to hear Dr. Brusca’s report on using cell-free (cf) DNA to track the severity of pulmonary artery hypertension and survival of these patients. I’m now using cfDNA frequently to monitor heart transplant patients, and the information it provides has been very valuable. But cfDNA may be even better suited to assessing patients with pulmonary artery hypertension (PAH) because it’s a vascular disease, and increases in cfDNA appears to reflect damage to the vascular endothelium. It’s a brilliant application of this technology. Brain natriuretic peptide and troponin are markers of right heart damage, but cfDNA appears to be able to track the progression of the vascular component of PAH. It appears to be the first disease-specific biomarker we have for PAH. It’s time to start routinely measuring levels of cfDNA in trials so we can gather more data on the clinical correlates of changing levels of this biomarker.
NEW ORLEANS – Cell-free (cf) DNA looked like an informative biomarker for both the severity of pulmonary artery hypertension and the survival prognosis for patients with this disease, based on results from two preliminary studies involving a total of 173 people.
“Plasma levels of cell-free DNA are elevated in patients with pulmonary artery hypertension, compared with healthy controls, and may predict disease severity and mortality,” Samuel B. Brusca, MD, said at the at the annual meeting of the American College of Cardiology.
A growing biomedical literature has documented a role for cfDNA in tracking the course of cancer, septic shock, and transplanted organs (Transplantation. 2019 Feb;103[2]:273-83) (Cell-Free DNA: Applications in Different Diseases, in “Cell-free DNA as Diagnostic Markers.” [New York: Humana Press, 2018, pp. 3-12]). Based on this background Dr. Brusca and his associates decided to examine whether plasma levels of cfDNA linked with pulmonary artery hypertension (PAH) severity and survival.
Their first study included seven patients with mild PAH (defined as patients with a tricuspid annular plane systolic excursion [TAPSE] of more than 18 mm and a maximum oxygen uptake [VO2] of at least 75% of predicted), eight with severe PAH (a TAPSE of 18 mm or less and a VO2 of less than 75%), and seven healthy adult controls. Measurement of plasma cfDNA showed an average level of 19.4 ng/mL among the healthy controls (prior reports had indicated that 10-20 ng/mL were normal levels), 22.0 ng/mL among patients with mild PAH, and 36.2 ng/mL in those with severe PAH. The level among the severe PAH patients was significantly higher than the level in controls by two different statistical tests, said Dr. Brusca, a critical care medicine physician at the National Institutes of Health Clinical Center in Bethesda, Md.
The second analysis by Dr. Brusca and his associates included 151 PAH patients followed by physicians at the Clinical Center for an average of 40 months. Their analysis tracked survival of these patients relative to their baseline levels of cfDNA and divided into tertiles. Patients in the lowest tertile had a starting cfDNA level of up to 39 ng/mL, those in the middle tertile had levels of 39.1-64.0 ng/mL, and those in the top tertile had levels of at least 64.1 ng/mL. A Kaplan-Meier analysis showed statistically significant differences in survival rates between each of the tertiles. Patients in the lowest tertile had a 5-year actuarial survival rate of about 65%, those in the middle tertile had a survival rate of about 48%, and those in the tertile with the highest level of cfDNA had a survival rate of about 28%.
Additional studies of cfDNA are needed in larger numbers of PAH patients, and cfDNA levels should be compared with levels of other, more established biomarkers, such as inflammatory cytokines, Dr. Brusca said in an interview.
Dr. Brusca had no disclosures. The study received no commercial funding.
SOURCE: Brusca SB et al. J Am Coll Cardiol. 2019 March 12;73(9 Suppl 1):1897.
NEW ORLEANS – Cell-free (cf) DNA looked like an informative biomarker for both the severity of pulmonary artery hypertension and the survival prognosis for patients with this disease, based on results from two preliminary studies involving a total of 173 people.
“Plasma levels of cell-free DNA are elevated in patients with pulmonary artery hypertension, compared with healthy controls, and may predict disease severity and mortality,” Samuel B. Brusca, MD, said at the at the annual meeting of the American College of Cardiology.
A growing biomedical literature has documented a role for cfDNA in tracking the course of cancer, septic shock, and transplanted organs (Transplantation. 2019 Feb;103[2]:273-83) (Cell-Free DNA: Applications in Different Diseases, in “Cell-free DNA as Diagnostic Markers.” [New York: Humana Press, 2018, pp. 3-12]). Based on this background Dr. Brusca and his associates decided to examine whether plasma levels of cfDNA linked with pulmonary artery hypertension (PAH) severity and survival.
Their first study included seven patients with mild PAH (defined as patients with a tricuspid annular plane systolic excursion [TAPSE] of more than 18 mm and a maximum oxygen uptake [VO2] of at least 75% of predicted), eight with severe PAH (a TAPSE of 18 mm or less and a VO2 of less than 75%), and seven healthy adult controls. Measurement of plasma cfDNA showed an average level of 19.4 ng/mL among the healthy controls (prior reports had indicated that 10-20 ng/mL were normal levels), 22.0 ng/mL among patients with mild PAH, and 36.2 ng/mL in those with severe PAH. The level among the severe PAH patients was significantly higher than the level in controls by two different statistical tests, said Dr. Brusca, a critical care medicine physician at the National Institutes of Health Clinical Center in Bethesda, Md.
The second analysis by Dr. Brusca and his associates included 151 PAH patients followed by physicians at the Clinical Center for an average of 40 months. Their analysis tracked survival of these patients relative to their baseline levels of cfDNA and divided into tertiles. Patients in the lowest tertile had a starting cfDNA level of up to 39 ng/mL, those in the middle tertile had levels of 39.1-64.0 ng/mL, and those in the top tertile had levels of at least 64.1 ng/mL. A Kaplan-Meier analysis showed statistically significant differences in survival rates between each of the tertiles. Patients in the lowest tertile had a 5-year actuarial survival rate of about 65%, those in the middle tertile had a survival rate of about 48%, and those in the tertile with the highest level of cfDNA had a survival rate of about 28%.
Additional studies of cfDNA are needed in larger numbers of PAH patients, and cfDNA levels should be compared with levels of other, more established biomarkers, such as inflammatory cytokines, Dr. Brusca said in an interview.
Dr. Brusca had no disclosures. The study received no commercial funding.
SOURCE: Brusca SB et al. J Am Coll Cardiol. 2019 March 12;73(9 Suppl 1):1897.
REPORTING FROM ACC 2019
CardioMEMS cuts heart failure hospitalizations in post-approval study
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
REPORTING FROM ACC 2019
SGLT2 inhibitors prevent HF hospitalization regardless of baseline LVEF
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.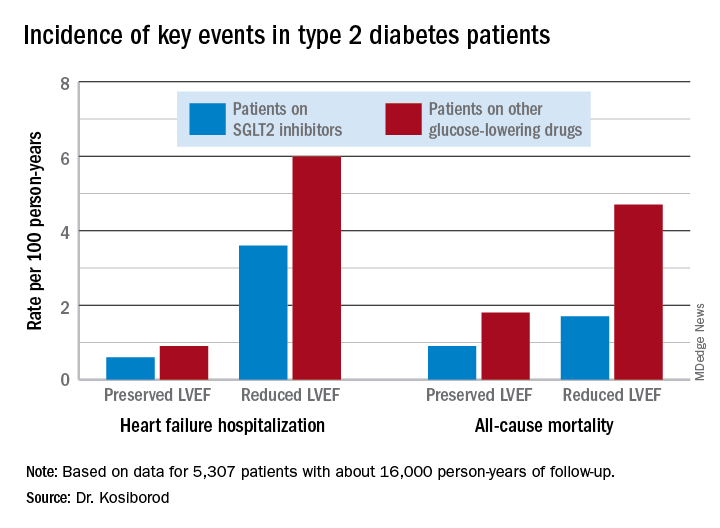
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.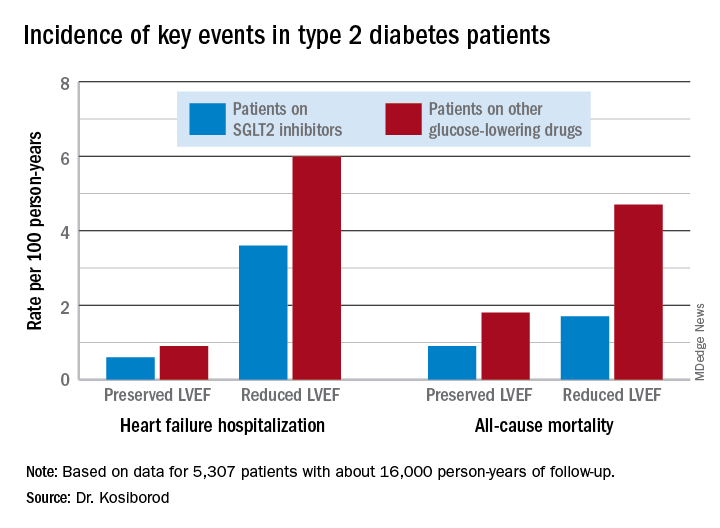
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.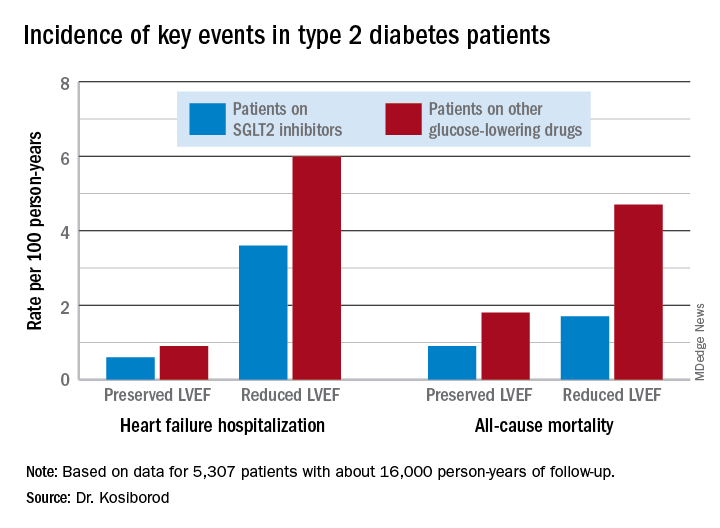
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
REPORTING FROM ACC 19