User login
New ACC guidance on heart failure with preserved ejection fraction
The American College of Cardiology has released an Expert Consensus Decision Pathway (ECDP) on the management of heart failure with preserved ejection fraction (HFpEF).
The 44-page document highlights the “critical need” to accurately diagnose HFpEF to permit timely implementation of evidence- and guideline-based therapies to improve patient outcomes.
Although the incidence of overall HF in the United States appears to be stable or declining, the incidence of HFpEF continues to rise in tandem with increasing age and burdens of obesity, sedentary lifestyle, and cardiometabolic disorders.
HFpEF now accounts for more than one half of HF cases but remains “underrecognized” in everyday clinical practice, said the writing group, led by Michelle Kittleson, MD, PhD, professor of medicine, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles.
HFpEF is a complex condition, often with multiple overlapping comorbidities, including hypertension, diabetes, obesity, and sleep apnea; optimal management requires a multidisciplinary approach, the writing group said.
The ECDP on HFpEF lays out a structure for diagnosis, clinical decision-making, management of comorbidities, implementation of the latest guideline-directed medical therapy (pharmacologic and nonpharmacologic), and equitable delivery of care.
The document was published online in the Journal of the American College of Cardiology.
It aligns with and builds on recommendations from the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure.
“HFpEF is one of the most pressing diagnostic and therapeutic challenges in clinical medicine today given its increasing prevalence, under diagnosis, poor prognosis, limited therapeutic options, and substantial burden on the health care system worldwide,” wrote the authors of a companion scientific statement on HFpEF.
Despite these challenges, the success of recent sodium-glucose cotransporter 2 inhibitor trials has shown that HFpEF is treatable, Barry Borlaug, MD, department of cardiovascular medicine, Mayo Clinic, Rochester, Minn., and coauthors pointed out.
They noted that “ongoing large-scale studies of HFpEF pathobiology, an increasing number of translational studies spanning the gap between the bedside and the bench, and numerous clinical trials of novel therapeutics in HFpEF offer a glimpse of hope toward a future of reduced prevalence, morbidity, and mortality associated with HFpEF, which would be a major advance for population health.”
A version of this article originally appeared on Medscape.com.
The American College of Cardiology has released an Expert Consensus Decision Pathway (ECDP) on the management of heart failure with preserved ejection fraction (HFpEF).
The 44-page document highlights the “critical need” to accurately diagnose HFpEF to permit timely implementation of evidence- and guideline-based therapies to improve patient outcomes.
Although the incidence of overall HF in the United States appears to be stable or declining, the incidence of HFpEF continues to rise in tandem with increasing age and burdens of obesity, sedentary lifestyle, and cardiometabolic disorders.
HFpEF now accounts for more than one half of HF cases but remains “underrecognized” in everyday clinical practice, said the writing group, led by Michelle Kittleson, MD, PhD, professor of medicine, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles.
HFpEF is a complex condition, often with multiple overlapping comorbidities, including hypertension, diabetes, obesity, and sleep apnea; optimal management requires a multidisciplinary approach, the writing group said.
The ECDP on HFpEF lays out a structure for diagnosis, clinical decision-making, management of comorbidities, implementation of the latest guideline-directed medical therapy (pharmacologic and nonpharmacologic), and equitable delivery of care.
The document was published online in the Journal of the American College of Cardiology.
It aligns with and builds on recommendations from the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure.
“HFpEF is one of the most pressing diagnostic and therapeutic challenges in clinical medicine today given its increasing prevalence, under diagnosis, poor prognosis, limited therapeutic options, and substantial burden on the health care system worldwide,” wrote the authors of a companion scientific statement on HFpEF.
Despite these challenges, the success of recent sodium-glucose cotransporter 2 inhibitor trials has shown that HFpEF is treatable, Barry Borlaug, MD, department of cardiovascular medicine, Mayo Clinic, Rochester, Minn., and coauthors pointed out.
They noted that “ongoing large-scale studies of HFpEF pathobiology, an increasing number of translational studies spanning the gap between the bedside and the bench, and numerous clinical trials of novel therapeutics in HFpEF offer a glimpse of hope toward a future of reduced prevalence, morbidity, and mortality associated with HFpEF, which would be a major advance for population health.”
A version of this article originally appeared on Medscape.com.
The American College of Cardiology has released an Expert Consensus Decision Pathway (ECDP) on the management of heart failure with preserved ejection fraction (HFpEF).
The 44-page document highlights the “critical need” to accurately diagnose HFpEF to permit timely implementation of evidence- and guideline-based therapies to improve patient outcomes.
Although the incidence of overall HF in the United States appears to be stable or declining, the incidence of HFpEF continues to rise in tandem with increasing age and burdens of obesity, sedentary lifestyle, and cardiometabolic disorders.
HFpEF now accounts for more than one half of HF cases but remains “underrecognized” in everyday clinical practice, said the writing group, led by Michelle Kittleson, MD, PhD, professor of medicine, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles.
HFpEF is a complex condition, often with multiple overlapping comorbidities, including hypertension, diabetes, obesity, and sleep apnea; optimal management requires a multidisciplinary approach, the writing group said.
The ECDP on HFpEF lays out a structure for diagnosis, clinical decision-making, management of comorbidities, implementation of the latest guideline-directed medical therapy (pharmacologic and nonpharmacologic), and equitable delivery of care.
The document was published online in the Journal of the American College of Cardiology.
It aligns with and builds on recommendations from the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure.
“HFpEF is one of the most pressing diagnostic and therapeutic challenges in clinical medicine today given its increasing prevalence, under diagnosis, poor prognosis, limited therapeutic options, and substantial burden on the health care system worldwide,” wrote the authors of a companion scientific statement on HFpEF.
Despite these challenges, the success of recent sodium-glucose cotransporter 2 inhibitor trials has shown that HFpEF is treatable, Barry Borlaug, MD, department of cardiovascular medicine, Mayo Clinic, Rochester, Minn., and coauthors pointed out.
They noted that “ongoing large-scale studies of HFpEF pathobiology, an increasing number of translational studies spanning the gap between the bedside and the bench, and numerous clinical trials of novel therapeutics in HFpEF offer a glimpse of hope toward a future of reduced prevalence, morbidity, and mortality associated with HFpEF, which would be a major advance for population health.”
A version of this article originally appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
‘Substantial’ variation in responses to BP meds
A new study has shown a substantial variation in the blood pressure response to various antihypertensive medications between individuals, raising the possibility of future personalized therapy.
“We found that using the optimal antihypertensive drug for a particular patient resulted in an average of a 4.4 mm Hg greater reduction of blood pressure compared with a random choice of the other drugs. That is quite a substantial difference, and could be equivalent to adding in another drug,” lead author Johan Sundström, MD, Uppsala (Sweden) University Hospital, told this news organization.
“These preliminary findings suggest that some people may be better treated with one antihypertensive drug rather than another. This is opening up the field of hypertension for personalized medicine,” he added.
The study was published online in the Journal of the American Medical Association.
The authors noted that despite global access to multiple classes of highly effective blood pressure-lowering drugs, only one in four women and one in five men with hypertension reach treatment targets. While most hypertension guidelines advocate combination pharmacotherapy, many patients in routine care continue to be treated with monotherapy, with adverse effects and nonadherence being important clinical problems.
“One drug often does not give enough blood pressure reduction, but patients are often reluctant to up-titrate to two drugs,” Dr. Sundström said. “While we know that the four recommended classes of antihypertensives lower blood pressure equally well on average, we don’t know if their efficacy is the same in individual patients.
“We wondered whether there could be different optimal drugs for different people, and if we could identify the optimal drug for each person then maybe more patients could get to target levels with just one drug,” he said.
The researchers conducted a randomized, double-blind, repeated crossover trial at an outpatient research clinic in Sweden, studying 280 men and women with grade 1 hypertension at low risk for cardiovascular events.
Each participant was scheduled for 2 months’ treatment in random order with each of four different classes of antihypertensive drugs: an ACE inhibitor, lisinopril; an angiotensin II blocker, candesartan; a thiazide diuretic, hydrochlorothiazide; a calcium channel blocker, amlodipine.
There were then repeated treatment periods for two drug classes to try to account for any effect of a particular event that might have affected the blood pressure at one point in time. Ambulatory daytime systolic blood pressure was measured at the end of each treatment period.
Results showed that variation in systolic blood pressure was large between treatments on average, between participants on average, within participants taking the same treatment, and between treatments in the same participant.
Overall, personalized treatment using the optimal single-drug therapy led to a 4.4–mm Hg lower systolic blood pressure in the trial population than a random choice of any of the other drug classes.
Taking into consideration that lisinopril was found to be on average the most efficacious of the drugs at the selected doses, personalized treatment compared with lisinopril still led to a 3.1–mm Hg improvement in systolic blood pressure.
The researchers noted that the mean additional blood pressure reduction achievable by using the optimal agent was of a magnitude twice that achieved by doubling the dose of a first drug, and more than half that of adding a second drug on average.
While there were only small differences between certain drugs (e.g., candesartan vs. lisinopril; amlodipine vs. hydrochlorothiazide), for all other comparisons tested, the choice was important, with particularly large gains to be made by personalizing the choice between candesartan vs. amlodipine and between lisinopril vs. amlodipine.
In addition, some people showed very large differences in response to different drugs, whereas others did not have much difference at all.
How to identify the optimal drug?
“The million-dollar question is how we identify the best drug for each individual patient,” Dr. Sundström said. “This study has opened Pandora’s box. We now need to figure out how to go forward and how we tailor treatment in each patient.”
In the study, the researchers suggest that personalizing therapy could be achieved either by identifying the phenotypic characteristics that are associated with enhanced response to one treatment vs. another or by directly measuring the individual’s responses to a series of treatments to ascertain which is most effective.
Addressing the first scenario, Dr. Sundström explained: “We can analyze the characteristics of patients who did best on each drug. There are many variables we can look at here such as age, diet, baseline blood pressure, exercise levels, smoking status, race, body weight, salt intake, and findings from genetic tests. We are going to try to look into these to see if we can find any predictors of response to various different drugs.”
For the second strategy, he suggested that patients starting pharmacologic therapy could try a few different treatments. “For example, we could give patients two different drugs and ask them to alternate treatment periods with each of them and measure their blood pressure with a home monitoring kit and record adverse effects.”
Nonadherence “is such a big problem with antihypertensives,” he added. “This approach may allow patients to be more empowered when choosing the right treatment, which should help adherence in the longer term.”
‘Proof-of-principle’
Commenting on the study in an accompanying editorial, Robert M. Carey, MD, University of Virginia Health System, Charlottesville, wrote: “At this stage, the findings are more theoretical than immediately practical for the implementation of personalized antihypertensive drug therapy, but the study does provide proof-of-principle and the authors suggest a few scenarios in which a personalized approach could be used in the future.”
He said the practical ramifications of personally targeted therapy remain unclear, given that determination of an individual’s response to a series of short test treatments before selecting long-term therapy may be considered too cumbersome, and currently few phenotypic markers are currently available that would be likely to accurately predict the individual response to a particular therapy.
Dr. Carey concluded that the results of this study “encourage the further pursuit of larger randomized trials using similar repeated crossover designs to validate this concept and eventually in trials with longer follow-up data to determine whether there is improvement in long-term clinical outcomes compared with current strategies.”
He added that the results support the possibility that personalized medical treatment of hypertension “may ultimately supplement or even supplant the current method of antihypertensive drug decision-making in the future.”
This study was supported by the Swedish Research Council; Kjell and Märta Beijer Foundation; and Anders Wiklöf. Dr. Sundström reported owning stock in Symptoms Europe AB and Anagram Kommunikation AB. Coauthor Emil Hagström, MD, PhD, reported receiving grants from Pfizer and Amgen and personal fees from Amgen, Novo Nordisk, Bayer, AstraZeneca, Amarin, and Novartis. Coauthor Ollie Östlund, PhD, reported fees from Uppsala University paid to his institution, Uppsala Clinical Research Center, for its participation in the PHYSIC trial during the conduct of the study. Dr. Carey reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study has shown a substantial variation in the blood pressure response to various antihypertensive medications between individuals, raising the possibility of future personalized therapy.
“We found that using the optimal antihypertensive drug for a particular patient resulted in an average of a 4.4 mm Hg greater reduction of blood pressure compared with a random choice of the other drugs. That is quite a substantial difference, and could be equivalent to adding in another drug,” lead author Johan Sundström, MD, Uppsala (Sweden) University Hospital, told this news organization.
“These preliminary findings suggest that some people may be better treated with one antihypertensive drug rather than another. This is opening up the field of hypertension for personalized medicine,” he added.
The study was published online in the Journal of the American Medical Association.
The authors noted that despite global access to multiple classes of highly effective blood pressure-lowering drugs, only one in four women and one in five men with hypertension reach treatment targets. While most hypertension guidelines advocate combination pharmacotherapy, many patients in routine care continue to be treated with monotherapy, with adverse effects and nonadherence being important clinical problems.
“One drug often does not give enough blood pressure reduction, but patients are often reluctant to up-titrate to two drugs,” Dr. Sundström said. “While we know that the four recommended classes of antihypertensives lower blood pressure equally well on average, we don’t know if their efficacy is the same in individual patients.
“We wondered whether there could be different optimal drugs for different people, and if we could identify the optimal drug for each person then maybe more patients could get to target levels with just one drug,” he said.
The researchers conducted a randomized, double-blind, repeated crossover trial at an outpatient research clinic in Sweden, studying 280 men and women with grade 1 hypertension at low risk for cardiovascular events.
Each participant was scheduled for 2 months’ treatment in random order with each of four different classes of antihypertensive drugs: an ACE inhibitor, lisinopril; an angiotensin II blocker, candesartan; a thiazide diuretic, hydrochlorothiazide; a calcium channel blocker, amlodipine.
There were then repeated treatment periods for two drug classes to try to account for any effect of a particular event that might have affected the blood pressure at one point in time. Ambulatory daytime systolic blood pressure was measured at the end of each treatment period.
Results showed that variation in systolic blood pressure was large between treatments on average, between participants on average, within participants taking the same treatment, and between treatments in the same participant.
Overall, personalized treatment using the optimal single-drug therapy led to a 4.4–mm Hg lower systolic blood pressure in the trial population than a random choice of any of the other drug classes.
Taking into consideration that lisinopril was found to be on average the most efficacious of the drugs at the selected doses, personalized treatment compared with lisinopril still led to a 3.1–mm Hg improvement in systolic blood pressure.
The researchers noted that the mean additional blood pressure reduction achievable by using the optimal agent was of a magnitude twice that achieved by doubling the dose of a first drug, and more than half that of adding a second drug on average.
While there were only small differences between certain drugs (e.g., candesartan vs. lisinopril; amlodipine vs. hydrochlorothiazide), for all other comparisons tested, the choice was important, with particularly large gains to be made by personalizing the choice between candesartan vs. amlodipine and between lisinopril vs. amlodipine.
In addition, some people showed very large differences in response to different drugs, whereas others did not have much difference at all.
How to identify the optimal drug?
“The million-dollar question is how we identify the best drug for each individual patient,” Dr. Sundström said. “This study has opened Pandora’s box. We now need to figure out how to go forward and how we tailor treatment in each patient.”
In the study, the researchers suggest that personalizing therapy could be achieved either by identifying the phenotypic characteristics that are associated with enhanced response to one treatment vs. another or by directly measuring the individual’s responses to a series of treatments to ascertain which is most effective.
Addressing the first scenario, Dr. Sundström explained: “We can analyze the characteristics of patients who did best on each drug. There are many variables we can look at here such as age, diet, baseline blood pressure, exercise levels, smoking status, race, body weight, salt intake, and findings from genetic tests. We are going to try to look into these to see if we can find any predictors of response to various different drugs.”
For the second strategy, he suggested that patients starting pharmacologic therapy could try a few different treatments. “For example, we could give patients two different drugs and ask them to alternate treatment periods with each of them and measure their blood pressure with a home monitoring kit and record adverse effects.”
Nonadherence “is such a big problem with antihypertensives,” he added. “This approach may allow patients to be more empowered when choosing the right treatment, which should help adherence in the longer term.”
‘Proof-of-principle’
Commenting on the study in an accompanying editorial, Robert M. Carey, MD, University of Virginia Health System, Charlottesville, wrote: “At this stage, the findings are more theoretical than immediately practical for the implementation of personalized antihypertensive drug therapy, but the study does provide proof-of-principle and the authors suggest a few scenarios in which a personalized approach could be used in the future.”
He said the practical ramifications of personally targeted therapy remain unclear, given that determination of an individual’s response to a series of short test treatments before selecting long-term therapy may be considered too cumbersome, and currently few phenotypic markers are currently available that would be likely to accurately predict the individual response to a particular therapy.
Dr. Carey concluded that the results of this study “encourage the further pursuit of larger randomized trials using similar repeated crossover designs to validate this concept and eventually in trials with longer follow-up data to determine whether there is improvement in long-term clinical outcomes compared with current strategies.”
He added that the results support the possibility that personalized medical treatment of hypertension “may ultimately supplement or even supplant the current method of antihypertensive drug decision-making in the future.”
This study was supported by the Swedish Research Council; Kjell and Märta Beijer Foundation; and Anders Wiklöf. Dr. Sundström reported owning stock in Symptoms Europe AB and Anagram Kommunikation AB. Coauthor Emil Hagström, MD, PhD, reported receiving grants from Pfizer and Amgen and personal fees from Amgen, Novo Nordisk, Bayer, AstraZeneca, Amarin, and Novartis. Coauthor Ollie Östlund, PhD, reported fees from Uppsala University paid to his institution, Uppsala Clinical Research Center, for its participation in the PHYSIC trial during the conduct of the study. Dr. Carey reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study has shown a substantial variation in the blood pressure response to various antihypertensive medications between individuals, raising the possibility of future personalized therapy.
“We found that using the optimal antihypertensive drug for a particular patient resulted in an average of a 4.4 mm Hg greater reduction of blood pressure compared with a random choice of the other drugs. That is quite a substantial difference, and could be equivalent to adding in another drug,” lead author Johan Sundström, MD, Uppsala (Sweden) University Hospital, told this news organization.
“These preliminary findings suggest that some people may be better treated with one antihypertensive drug rather than another. This is opening up the field of hypertension for personalized medicine,” he added.
The study was published online in the Journal of the American Medical Association.
The authors noted that despite global access to multiple classes of highly effective blood pressure-lowering drugs, only one in four women and one in five men with hypertension reach treatment targets. While most hypertension guidelines advocate combination pharmacotherapy, many patients in routine care continue to be treated with monotherapy, with adverse effects and nonadherence being important clinical problems.
“One drug often does not give enough blood pressure reduction, but patients are often reluctant to up-titrate to two drugs,” Dr. Sundström said. “While we know that the four recommended classes of antihypertensives lower blood pressure equally well on average, we don’t know if their efficacy is the same in individual patients.
“We wondered whether there could be different optimal drugs for different people, and if we could identify the optimal drug for each person then maybe more patients could get to target levels with just one drug,” he said.
The researchers conducted a randomized, double-blind, repeated crossover trial at an outpatient research clinic in Sweden, studying 280 men and women with grade 1 hypertension at low risk for cardiovascular events.
Each participant was scheduled for 2 months’ treatment in random order with each of four different classes of antihypertensive drugs: an ACE inhibitor, lisinopril; an angiotensin II blocker, candesartan; a thiazide diuretic, hydrochlorothiazide; a calcium channel blocker, amlodipine.
There were then repeated treatment periods for two drug classes to try to account for any effect of a particular event that might have affected the blood pressure at one point in time. Ambulatory daytime systolic blood pressure was measured at the end of each treatment period.
Results showed that variation in systolic blood pressure was large between treatments on average, between participants on average, within participants taking the same treatment, and between treatments in the same participant.
Overall, personalized treatment using the optimal single-drug therapy led to a 4.4–mm Hg lower systolic blood pressure in the trial population than a random choice of any of the other drug classes.
Taking into consideration that lisinopril was found to be on average the most efficacious of the drugs at the selected doses, personalized treatment compared with lisinopril still led to a 3.1–mm Hg improvement in systolic blood pressure.
The researchers noted that the mean additional blood pressure reduction achievable by using the optimal agent was of a magnitude twice that achieved by doubling the dose of a first drug, and more than half that of adding a second drug on average.
While there were only small differences between certain drugs (e.g., candesartan vs. lisinopril; amlodipine vs. hydrochlorothiazide), for all other comparisons tested, the choice was important, with particularly large gains to be made by personalizing the choice between candesartan vs. amlodipine and between lisinopril vs. amlodipine.
In addition, some people showed very large differences in response to different drugs, whereas others did not have much difference at all.
How to identify the optimal drug?
“The million-dollar question is how we identify the best drug for each individual patient,” Dr. Sundström said. “This study has opened Pandora’s box. We now need to figure out how to go forward and how we tailor treatment in each patient.”
In the study, the researchers suggest that personalizing therapy could be achieved either by identifying the phenotypic characteristics that are associated with enhanced response to one treatment vs. another or by directly measuring the individual’s responses to a series of treatments to ascertain which is most effective.
Addressing the first scenario, Dr. Sundström explained: “We can analyze the characteristics of patients who did best on each drug. There are many variables we can look at here such as age, diet, baseline blood pressure, exercise levels, smoking status, race, body weight, salt intake, and findings from genetic tests. We are going to try to look into these to see if we can find any predictors of response to various different drugs.”
For the second strategy, he suggested that patients starting pharmacologic therapy could try a few different treatments. “For example, we could give patients two different drugs and ask them to alternate treatment periods with each of them and measure their blood pressure with a home monitoring kit and record adverse effects.”
Nonadherence “is such a big problem with antihypertensives,” he added. “This approach may allow patients to be more empowered when choosing the right treatment, which should help adherence in the longer term.”
‘Proof-of-principle’
Commenting on the study in an accompanying editorial, Robert M. Carey, MD, University of Virginia Health System, Charlottesville, wrote: “At this stage, the findings are more theoretical than immediately practical for the implementation of personalized antihypertensive drug therapy, but the study does provide proof-of-principle and the authors suggest a few scenarios in which a personalized approach could be used in the future.”
He said the practical ramifications of personally targeted therapy remain unclear, given that determination of an individual’s response to a series of short test treatments before selecting long-term therapy may be considered too cumbersome, and currently few phenotypic markers are currently available that would be likely to accurately predict the individual response to a particular therapy.
Dr. Carey concluded that the results of this study “encourage the further pursuit of larger randomized trials using similar repeated crossover designs to validate this concept and eventually in trials with longer follow-up data to determine whether there is improvement in long-term clinical outcomes compared with current strategies.”
He added that the results support the possibility that personalized medical treatment of hypertension “may ultimately supplement or even supplant the current method of antihypertensive drug decision-making in the future.”
This study was supported by the Swedish Research Council; Kjell and Märta Beijer Foundation; and Anders Wiklöf. Dr. Sundström reported owning stock in Symptoms Europe AB and Anagram Kommunikation AB. Coauthor Emil Hagström, MD, PhD, reported receiving grants from Pfizer and Amgen and personal fees from Amgen, Novo Nordisk, Bayer, AstraZeneca, Amarin, and Novartis. Coauthor Ollie Östlund, PhD, reported fees from Uppsala University paid to his institution, Uppsala Clinical Research Center, for its participation in the PHYSIC trial during the conduct of the study. Dr. Carey reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AHA statement targets nuance in CVD risk assessment of women
In a new scientific statement, the American Heart Association highlighted the importance of incorporating nonbiological risk factors and social determinants of health in cardiovascular disease (CVD) risk assessment for women, particularly women from different racial and ethnic backgrounds.
CVD risk assessment in women is multifaceted and goes well beyond traditional risk factors to include sex-specific biological risk factors, as well as social, behavioral, and environmental factors, the writing group noted.
They said a greater focus on addressing all CVD risk factors among women from underrepresented races and ethnicities is warranted to avert future CVD.
The scientific statement was published online in Circulation.
Look beyond traditional risk factors
“Risk assessment is the first step in preventing heart disease, yet there are many limitations to traditional risk factors and their ability to comprehensively estimate a woman’s risk for cardiovascular disease,” Jennifer H. Mieres, MD, vice chair of the writing group and professor of cardiology at Hofstra University, Hempstead, N.Y., said in a news release.
“The delivery of equitable cardiovascular health care for women depends on improving the knowledge and awareness of all members of the healthcare team about the full spectrum of cardiovascular risk factors for women, including female-specific and female-predominant risk factors,” Dr. Mieres added.
Female-specific factors that should be included in CVD risk assessment include pregnancy-related conditions such as preeclampsia, preterm delivery, and gestational diabetes, the writing group said.
Other factors include menstrual cycle history; types of birth control and/or hormone replacement therapy used; polycystic ovarian syndrome (PCOS), which affects 10% of women of reproductive age and is associated with increased CVD risk; and autoimmune disorders, depression, and PTSD, all of which are more common in women and are also associated with higher risk for CVD.
The statement also highlights the key role that social determinants of health (SDOH) play in the development of CVD in women, particularly women from diverse racial and ethnic backgrounds. SDOH include education level, economic stability, neighborhood safety, working conditions, environmental hazards, and access to quality health care.
“It is critical that risk assessment be expanded to include [SDOH] as risk factors if we are to improve health outcomes in all women,” Laxmi Mehta, MD, chair of the writing group and director of preventative cardiology and women’s cardiovascular health at Ohio State University Wexner Medical Center, Columbus, said in the news release.
“It is also important for the health care team to consider [SDOH] when working with women on shared decisions about cardiovascular disease prevention and treatment,” Dr. Mehta noted.
No one-size-fits-all approach
The statement highlighted significant differences in CVD risk among women of different racial and ethnic backgrounds and provides detailed CV risk factor profiles for non-Hispanic Black, Hispanic/Latinx, Asian and American Indian/Alaska Native women.
It noted that language barriers, discrimination, acculturation, and health care access disproportionately affect women of underrepresented racial and ethnic groups. These factors result in a higher prevalence of CVD and significant challenges in CVD diagnosis and treatment.
“When customizing CVD prevention and treatment strategies to improve cardiovascular health for women, a one-size-fits-all approach is unlikely to be successful,” Dr. Mieres said.
“We must be cognizant of the complex interplay of sex, race and ethnicity, as well as social determinants of health, and how they impact the risk of cardiovascular disease and adverse outcomes in order to avert future CVD morbidity and mortality,” Dr. Mieres added.
Looking ahead, the writing group said future CVD prevention guidelines could be strengthened by including culturally-specific lifestyle recommendations.
They also said community-based approaches, faith-based community partnerships, and peer support to encourage a healthy lifestyle could play a key role in preventing CVD among all women.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA’s Cardiovascular Disease and Stroke in Women and Underrepresented Populations Committee of the Council on Clinical Cardiology, the Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Lifestyle and Cardiometabolic Health, the Council on Peripheral Vascular Disease, and the Stroke Council.
A version of this article first appeared on Medscape.com.
In a new scientific statement, the American Heart Association highlighted the importance of incorporating nonbiological risk factors and social determinants of health in cardiovascular disease (CVD) risk assessment for women, particularly women from different racial and ethnic backgrounds.
CVD risk assessment in women is multifaceted and goes well beyond traditional risk factors to include sex-specific biological risk factors, as well as social, behavioral, and environmental factors, the writing group noted.
They said a greater focus on addressing all CVD risk factors among women from underrepresented races and ethnicities is warranted to avert future CVD.
The scientific statement was published online in Circulation.
Look beyond traditional risk factors
“Risk assessment is the first step in preventing heart disease, yet there are many limitations to traditional risk factors and their ability to comprehensively estimate a woman’s risk for cardiovascular disease,” Jennifer H. Mieres, MD, vice chair of the writing group and professor of cardiology at Hofstra University, Hempstead, N.Y., said in a news release.
“The delivery of equitable cardiovascular health care for women depends on improving the knowledge and awareness of all members of the healthcare team about the full spectrum of cardiovascular risk factors for women, including female-specific and female-predominant risk factors,” Dr. Mieres added.
Female-specific factors that should be included in CVD risk assessment include pregnancy-related conditions such as preeclampsia, preterm delivery, and gestational diabetes, the writing group said.
Other factors include menstrual cycle history; types of birth control and/or hormone replacement therapy used; polycystic ovarian syndrome (PCOS), which affects 10% of women of reproductive age and is associated with increased CVD risk; and autoimmune disorders, depression, and PTSD, all of which are more common in women and are also associated with higher risk for CVD.
The statement also highlights the key role that social determinants of health (SDOH) play in the development of CVD in women, particularly women from diverse racial and ethnic backgrounds. SDOH include education level, economic stability, neighborhood safety, working conditions, environmental hazards, and access to quality health care.
“It is critical that risk assessment be expanded to include [SDOH] as risk factors if we are to improve health outcomes in all women,” Laxmi Mehta, MD, chair of the writing group and director of preventative cardiology and women’s cardiovascular health at Ohio State University Wexner Medical Center, Columbus, said in the news release.
“It is also important for the health care team to consider [SDOH] when working with women on shared decisions about cardiovascular disease prevention and treatment,” Dr. Mehta noted.
No one-size-fits-all approach
The statement highlighted significant differences in CVD risk among women of different racial and ethnic backgrounds and provides detailed CV risk factor profiles for non-Hispanic Black, Hispanic/Latinx, Asian and American Indian/Alaska Native women.
It noted that language barriers, discrimination, acculturation, and health care access disproportionately affect women of underrepresented racial and ethnic groups. These factors result in a higher prevalence of CVD and significant challenges in CVD diagnosis and treatment.
“When customizing CVD prevention and treatment strategies to improve cardiovascular health for women, a one-size-fits-all approach is unlikely to be successful,” Dr. Mieres said.
“We must be cognizant of the complex interplay of sex, race and ethnicity, as well as social determinants of health, and how they impact the risk of cardiovascular disease and adverse outcomes in order to avert future CVD morbidity and mortality,” Dr. Mieres added.
Looking ahead, the writing group said future CVD prevention guidelines could be strengthened by including culturally-specific lifestyle recommendations.
They also said community-based approaches, faith-based community partnerships, and peer support to encourage a healthy lifestyle could play a key role in preventing CVD among all women.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA’s Cardiovascular Disease and Stroke in Women and Underrepresented Populations Committee of the Council on Clinical Cardiology, the Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Lifestyle and Cardiometabolic Health, the Council on Peripheral Vascular Disease, and the Stroke Council.
A version of this article first appeared on Medscape.com.
In a new scientific statement, the American Heart Association highlighted the importance of incorporating nonbiological risk factors and social determinants of health in cardiovascular disease (CVD) risk assessment for women, particularly women from different racial and ethnic backgrounds.
CVD risk assessment in women is multifaceted and goes well beyond traditional risk factors to include sex-specific biological risk factors, as well as social, behavioral, and environmental factors, the writing group noted.
They said a greater focus on addressing all CVD risk factors among women from underrepresented races and ethnicities is warranted to avert future CVD.
The scientific statement was published online in Circulation.
Look beyond traditional risk factors
“Risk assessment is the first step in preventing heart disease, yet there are many limitations to traditional risk factors and their ability to comprehensively estimate a woman’s risk for cardiovascular disease,” Jennifer H. Mieres, MD, vice chair of the writing group and professor of cardiology at Hofstra University, Hempstead, N.Y., said in a news release.
“The delivery of equitable cardiovascular health care for women depends on improving the knowledge and awareness of all members of the healthcare team about the full spectrum of cardiovascular risk factors for women, including female-specific and female-predominant risk factors,” Dr. Mieres added.
Female-specific factors that should be included in CVD risk assessment include pregnancy-related conditions such as preeclampsia, preterm delivery, and gestational diabetes, the writing group said.
Other factors include menstrual cycle history; types of birth control and/or hormone replacement therapy used; polycystic ovarian syndrome (PCOS), which affects 10% of women of reproductive age and is associated with increased CVD risk; and autoimmune disorders, depression, and PTSD, all of which are more common in women and are also associated with higher risk for CVD.
The statement also highlights the key role that social determinants of health (SDOH) play in the development of CVD in women, particularly women from diverse racial and ethnic backgrounds. SDOH include education level, economic stability, neighborhood safety, working conditions, environmental hazards, and access to quality health care.
“It is critical that risk assessment be expanded to include [SDOH] as risk factors if we are to improve health outcomes in all women,” Laxmi Mehta, MD, chair of the writing group and director of preventative cardiology and women’s cardiovascular health at Ohio State University Wexner Medical Center, Columbus, said in the news release.
“It is also important for the health care team to consider [SDOH] when working with women on shared decisions about cardiovascular disease prevention and treatment,” Dr. Mehta noted.
No one-size-fits-all approach
The statement highlighted significant differences in CVD risk among women of different racial and ethnic backgrounds and provides detailed CV risk factor profiles for non-Hispanic Black, Hispanic/Latinx, Asian and American Indian/Alaska Native women.
It noted that language barriers, discrimination, acculturation, and health care access disproportionately affect women of underrepresented racial and ethnic groups. These factors result in a higher prevalence of CVD and significant challenges in CVD diagnosis and treatment.
“When customizing CVD prevention and treatment strategies to improve cardiovascular health for women, a one-size-fits-all approach is unlikely to be successful,” Dr. Mieres said.
“We must be cognizant of the complex interplay of sex, race and ethnicity, as well as social determinants of health, and how they impact the risk of cardiovascular disease and adverse outcomes in order to avert future CVD morbidity and mortality,” Dr. Mieres added.
Looking ahead, the writing group said future CVD prevention guidelines could be strengthened by including culturally-specific lifestyle recommendations.
They also said community-based approaches, faith-based community partnerships, and peer support to encourage a healthy lifestyle could play a key role in preventing CVD among all women.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA’s Cardiovascular Disease and Stroke in Women and Underrepresented Populations Committee of the Council on Clinical Cardiology, the Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, the Council on Lifelong Congenital Heart Disease and Heart Health in the Young, the Council on Lifestyle and Cardiometabolic Health, the Council on Peripheral Vascular Disease, and the Stroke Council.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
NSAID use in diabetes may worsen risk for first HF hospitalization
suggests a prospective, controlled study.
Certain subgroups may account for much of the excess risk, the results suggest, including the very elderly, patients with uncontrolled diabetes, those prescribed an NSAID for the first time, and patients already taking both a renin-angiotensin system inhibitor (RASi) and a diuretic.
Such patients with a firm indication for NSAIDs potentially could “be the ones benefiting most from closer follow-up, reduced dosage, or other mitigation strategies,” Anders Holt, MD, said in an interview.
Dr. Holt, of Copenhagen University Hospital and Herlev-Gentofte Hospital in Hellerup, Denmark, is lead author on the analysis of Danish registry data published in the Journal of the American College of Cardiology. He presented essentially the same results in preliminary form at the 2022 annual congress of the European Society of Cardiology.
HF hospitalizations linked to NSAIDs, the published report notes, are often attributed to symptoms from temporary fluid overload, often without worsening cardiac function, that stem from the drugs’ renal effects.
“One could speculate,” Dr. Holt said, that such HF events might be less severe and even associated with better outcomes, compared with other forms of heart failure.
But the current analysis provides a hint to the contrary, he observed. The 5-year mortality was similar for patients with HF linked to NSAIDs and those with other forms of HF, “which could suggest that NSAID-associated heart failure is more than transient fluid overload.”
The drugs may promote HF through direct effects on the heart by any of several proposed mechanisms, including “induction of arrhythmias and heart fibrosis, vasoconstriction, subclinical inflammation, and blood pressure elevation,” Dr. Holt said.
The current study doesn’t determine whether NSAID-associated HF stems from transient fluid overload or direct cardiac effects, but it’s “most likely both.”
In other limitations, the analysis is unable to “reliably explore” whether promotion of HF is an NSAID class effect, a “clinically relevant” point given the drugs’ varying effects on cardiovascular risk, states an accompanying editorial. Nor was it able to determine whether the drugs exert a dose-response effect on HF risk, noted Hassan Khan, MD, PhD, Norton Healthcare, Louisville, Ky., and Setor K. Kunutsor, MD, PhD, University of Leicester (England).
Still, “given the well-established relationship between the use of NSAIDs and increased HF, these findings are not unexpected because type 2 diabetes is also a major risk factor for HF.”
But it may be “premature to issue guideline recommendations based on a single observational study,” the editorialists wrote. “Further robust clinical trial evidence is needed to replicate these results and investigate the relationship of the type and dose of NSAIDs with HF risk. However, it should be realized that short-term or long-term use of NSAIDs may be detrimental to cardiovascular health.”
The analysis covered 23,308 patients from throughout Denmark with a type 2 diabetes diagnosis and no HF history who experienced a first HF hospitalization; their age averaged 76 years and 39% were women.
They served as their own controls; their NSAID exposures at two 28-day periods preceding the HF event, the one immediately before and the other preceding it by 56 days, were compared as the index and control periods, respectively.
Exposure to NSAIDs was defined as obtaining a prescription for celecoxib, diclofenac, ibuprofen, or naproxen, “as these are NSAIDs used primarily in Denmark,” the report states.
The odds ratios for HF hospitalization associated with NSAID exposure within 28 days preceding the event were 1.43 (95% confidence interval, 1.27-1.63) overall, 1.41 (95% CI, 1.16-1.71) for an NSAID given on top of both RASi and diuretics, 1.68 (95% CI, 1.00-2.88) for patients with elevated hemoglobin A1c, 1.78 (95% CI, 1.39-2.28) for those 80 or older, and 2.71 (95% CI, 1.78-4.23) for those with prior NSAID use.
That NSAID use and diabetes are each associated with increased risk for HF is well established, Dr. Holt observed. Yet the drugs had been prescribed to 16% of patients in the study.
“One of the more surprising findings, to me, was the quite substantial use of prescribed NSAIDs in a population of patients with diabetes, a patient group with a well-established cardiovascular risk,” he said.
“This patient group is only growing, so emphasis on the possible associations between even short-term NSAID use and incident heart failure is probably timely and perhaps needed.”
Dr. Holt and the study were supported by grants from Ib Mogens Kristiansens Almene Fond, Helsefonden, Snedkermester Sophus Jacobsen og hustru Astrid Jacobsen Fond, Marie og M.B. Richters Fond, and the Dagmar Marshalls Fond. Dr. Khan and Dr. Kunutsor reported no relevant relationships.
A version of this article first appeared on Medscape.com.
suggests a prospective, controlled study.
Certain subgroups may account for much of the excess risk, the results suggest, including the very elderly, patients with uncontrolled diabetes, those prescribed an NSAID for the first time, and patients already taking both a renin-angiotensin system inhibitor (RASi) and a diuretic.
Such patients with a firm indication for NSAIDs potentially could “be the ones benefiting most from closer follow-up, reduced dosage, or other mitigation strategies,” Anders Holt, MD, said in an interview.
Dr. Holt, of Copenhagen University Hospital and Herlev-Gentofte Hospital in Hellerup, Denmark, is lead author on the analysis of Danish registry data published in the Journal of the American College of Cardiology. He presented essentially the same results in preliminary form at the 2022 annual congress of the European Society of Cardiology.
HF hospitalizations linked to NSAIDs, the published report notes, are often attributed to symptoms from temporary fluid overload, often without worsening cardiac function, that stem from the drugs’ renal effects.
“One could speculate,” Dr. Holt said, that such HF events might be less severe and even associated with better outcomes, compared with other forms of heart failure.
But the current analysis provides a hint to the contrary, he observed. The 5-year mortality was similar for patients with HF linked to NSAIDs and those with other forms of HF, “which could suggest that NSAID-associated heart failure is more than transient fluid overload.”
The drugs may promote HF through direct effects on the heart by any of several proposed mechanisms, including “induction of arrhythmias and heart fibrosis, vasoconstriction, subclinical inflammation, and blood pressure elevation,” Dr. Holt said.
The current study doesn’t determine whether NSAID-associated HF stems from transient fluid overload or direct cardiac effects, but it’s “most likely both.”
In other limitations, the analysis is unable to “reliably explore” whether promotion of HF is an NSAID class effect, a “clinically relevant” point given the drugs’ varying effects on cardiovascular risk, states an accompanying editorial. Nor was it able to determine whether the drugs exert a dose-response effect on HF risk, noted Hassan Khan, MD, PhD, Norton Healthcare, Louisville, Ky., and Setor K. Kunutsor, MD, PhD, University of Leicester (England).
Still, “given the well-established relationship between the use of NSAIDs and increased HF, these findings are not unexpected because type 2 diabetes is also a major risk factor for HF.”
But it may be “premature to issue guideline recommendations based on a single observational study,” the editorialists wrote. “Further robust clinical trial evidence is needed to replicate these results and investigate the relationship of the type and dose of NSAIDs with HF risk. However, it should be realized that short-term or long-term use of NSAIDs may be detrimental to cardiovascular health.”
The analysis covered 23,308 patients from throughout Denmark with a type 2 diabetes diagnosis and no HF history who experienced a first HF hospitalization; their age averaged 76 years and 39% were women.
They served as their own controls; their NSAID exposures at two 28-day periods preceding the HF event, the one immediately before and the other preceding it by 56 days, were compared as the index and control periods, respectively.
Exposure to NSAIDs was defined as obtaining a prescription for celecoxib, diclofenac, ibuprofen, or naproxen, “as these are NSAIDs used primarily in Denmark,” the report states.
The odds ratios for HF hospitalization associated with NSAID exposure within 28 days preceding the event were 1.43 (95% confidence interval, 1.27-1.63) overall, 1.41 (95% CI, 1.16-1.71) for an NSAID given on top of both RASi and diuretics, 1.68 (95% CI, 1.00-2.88) for patients with elevated hemoglobin A1c, 1.78 (95% CI, 1.39-2.28) for those 80 or older, and 2.71 (95% CI, 1.78-4.23) for those with prior NSAID use.
That NSAID use and diabetes are each associated with increased risk for HF is well established, Dr. Holt observed. Yet the drugs had been prescribed to 16% of patients in the study.
“One of the more surprising findings, to me, was the quite substantial use of prescribed NSAIDs in a population of patients with diabetes, a patient group with a well-established cardiovascular risk,” he said.
“This patient group is only growing, so emphasis on the possible associations between even short-term NSAID use and incident heart failure is probably timely and perhaps needed.”
Dr. Holt and the study were supported by grants from Ib Mogens Kristiansens Almene Fond, Helsefonden, Snedkermester Sophus Jacobsen og hustru Astrid Jacobsen Fond, Marie og M.B. Richters Fond, and the Dagmar Marshalls Fond. Dr. Khan and Dr. Kunutsor reported no relevant relationships.
A version of this article first appeared on Medscape.com.
suggests a prospective, controlled study.
Certain subgroups may account for much of the excess risk, the results suggest, including the very elderly, patients with uncontrolled diabetes, those prescribed an NSAID for the first time, and patients already taking both a renin-angiotensin system inhibitor (RASi) and a diuretic.
Such patients with a firm indication for NSAIDs potentially could “be the ones benefiting most from closer follow-up, reduced dosage, or other mitigation strategies,” Anders Holt, MD, said in an interview.
Dr. Holt, of Copenhagen University Hospital and Herlev-Gentofte Hospital in Hellerup, Denmark, is lead author on the analysis of Danish registry data published in the Journal of the American College of Cardiology. He presented essentially the same results in preliminary form at the 2022 annual congress of the European Society of Cardiology.
HF hospitalizations linked to NSAIDs, the published report notes, are often attributed to symptoms from temporary fluid overload, often without worsening cardiac function, that stem from the drugs’ renal effects.
“One could speculate,” Dr. Holt said, that such HF events might be less severe and even associated with better outcomes, compared with other forms of heart failure.
But the current analysis provides a hint to the contrary, he observed. The 5-year mortality was similar for patients with HF linked to NSAIDs and those with other forms of HF, “which could suggest that NSAID-associated heart failure is more than transient fluid overload.”
The drugs may promote HF through direct effects on the heart by any of several proposed mechanisms, including “induction of arrhythmias and heart fibrosis, vasoconstriction, subclinical inflammation, and blood pressure elevation,” Dr. Holt said.
The current study doesn’t determine whether NSAID-associated HF stems from transient fluid overload or direct cardiac effects, but it’s “most likely both.”
In other limitations, the analysis is unable to “reliably explore” whether promotion of HF is an NSAID class effect, a “clinically relevant” point given the drugs’ varying effects on cardiovascular risk, states an accompanying editorial. Nor was it able to determine whether the drugs exert a dose-response effect on HF risk, noted Hassan Khan, MD, PhD, Norton Healthcare, Louisville, Ky., and Setor K. Kunutsor, MD, PhD, University of Leicester (England).
Still, “given the well-established relationship between the use of NSAIDs and increased HF, these findings are not unexpected because type 2 diabetes is also a major risk factor for HF.”
But it may be “premature to issue guideline recommendations based on a single observational study,” the editorialists wrote. “Further robust clinical trial evidence is needed to replicate these results and investigate the relationship of the type and dose of NSAIDs with HF risk. However, it should be realized that short-term or long-term use of NSAIDs may be detrimental to cardiovascular health.”
The analysis covered 23,308 patients from throughout Denmark with a type 2 diabetes diagnosis and no HF history who experienced a first HF hospitalization; their age averaged 76 years and 39% were women.
They served as their own controls; their NSAID exposures at two 28-day periods preceding the HF event, the one immediately before and the other preceding it by 56 days, were compared as the index and control periods, respectively.
Exposure to NSAIDs was defined as obtaining a prescription for celecoxib, diclofenac, ibuprofen, or naproxen, “as these are NSAIDs used primarily in Denmark,” the report states.
The odds ratios for HF hospitalization associated with NSAID exposure within 28 days preceding the event were 1.43 (95% confidence interval, 1.27-1.63) overall, 1.41 (95% CI, 1.16-1.71) for an NSAID given on top of both RASi and diuretics, 1.68 (95% CI, 1.00-2.88) for patients with elevated hemoglobin A1c, 1.78 (95% CI, 1.39-2.28) for those 80 or older, and 2.71 (95% CI, 1.78-4.23) for those with prior NSAID use.
That NSAID use and diabetes are each associated with increased risk for HF is well established, Dr. Holt observed. Yet the drugs had been prescribed to 16% of patients in the study.
“One of the more surprising findings, to me, was the quite substantial use of prescribed NSAIDs in a population of patients with diabetes, a patient group with a well-established cardiovascular risk,” he said.
“This patient group is only growing, so emphasis on the possible associations between even short-term NSAID use and incident heart failure is probably timely and perhaps needed.”
Dr. Holt and the study were supported by grants from Ib Mogens Kristiansens Almene Fond, Helsefonden, Snedkermester Sophus Jacobsen og hustru Astrid Jacobsen Fond, Marie og M.B. Richters Fond, and the Dagmar Marshalls Fond. Dr. Khan and Dr. Kunutsor reported no relevant relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Spherical heart may predict cardiomyopathy, AFib
A round heart, or left ventricle sphericity, predicted cardiomyopathy and atrial fibrillation (AFib) in a deep learning analysis of MRI images from close to 39,000 participants in the UK Biobank, a new study shows.
An increase of 1 standard deviation in the sphericity index (short axis length/long axis length) was associated with a 47% increased incidence of cardiomyopathy and a 20% increased incidence of AFib, independent of clinical factors and traditional MRI measures.
Furthermore, a genetic analysis suggested a shared architecture between sphericity and nonischemic cardiomyopathy, pointing to NICM as a possible causal factor for left ventricle sphericity among individuals with normal LV size and function.
“Physicians have known the heart gets rounder after heart attacks and as we get older,” David Ouyang, MD, a cardiologist in the Smidt Heart Institute at Cedars-Sinai Medical Center, Los Angeles, and a researcher in the division of artificial intelligence in medicine, said in an interview. “We wanted to see if this sphericity is prognostic of future disease even in healthy individuals.”
Although it is too early to recommend heart shape assessment in healthy asymptomatic people, he said, “physicians should be extra careful and think about treatments when they notice a patient’s heart is particularly round.”
The study was published online March 29 in the journal Med.
Sphericity index key
The investigators hypothesized that there is variation in LV sphericity within the spectrum of normal LV chamber size and systolic function, and that such variation might be a marker of cardiac risk with genetic influences.
To test this hypothesis, they used automated deep-learning segmentation of cardiac MRI data to estimate and analyze the sphericity index in a cohort of 38,897 individuals participating in the UK Biobank.
After adjustment for age at MRI and sex, an increased sphericity index was associated with an increased risk for cardiomyopathy (hazard ratio, 1.57), AFib (HR, 1.35), and heart failure (HR, 1.37).
No significant association was seen with cardiac arrest.
The team then stratified the cohort into quintiles and compared the top 20%, middle 60%, and bottom 20%. The relationship between the sphericity index and risk extended across the distribution; individuals with higher than median sphericity had increased disease incidence, and those with lower than median sphericity had decreased incidence.
Overall, a single standard deviation in the sphericity index was associated with increased risk of cardiomyopathy (HR, 1.47) and of AFib (HR, 1.20), independent of clinical factors and usual MRI measurements.
In a minimally adjusted model, the sphericity index was a predictor of incident cardiomyopathy, AFib, and heart failure.
Adjustment for clinical factors partially attenuated the heart failure association; additional adjustment for MRI measurements fully attenuated that association and partially attenuated the association with AFib.
However, in all adjusted models, the association with cardiomyopathy showed little attenuation.
Furthermore, the team identified four loci associated with sphericity at genomewide significance – PLN, ANGPT1, PDZRN3, and HLA DR/DQ – and Mendelian randomization supported NICM as a cause of LV sphericity.
Looking ahead
“While conventional imaging metrics have significant diagnostic and prognostic value, some of these measurements have been adopted out of convenience or tradition,” the authors noted. “By representing a specific multidimensional remodeling phenotype, sphericity has emerged as a distinct morphologic trait with features not adequately captured by conventional measurements.
“We expect that the search space of potential imaging measurements is vast, and we have only begun to scratch at the surface of disease associations.”
Indeed, Dr. Ouyang said his group is “trying to evaluate the sphericity in echocardiograms or heart ultrasounds, which are more common and cheaper than MRI.”
“The main caveat is translating the information directly to patient care,” Richard C. Becker, MD, director and physician-in-chief of the University of Cincinnati Heart, Lung, and Vascular Institute, said in an interview. “Near-term yield could include using the spherical calculation in routine MRI of the heart, and based on the findings, following patients more closely if there is an abnormal shape. Or performing an MRI and targeted gene testing if there is a family history of cardiomyopathy or [of] an abnormal shape of the heart.”
“Validation of the findings and large-scale evaluation of the genes identified, and how they interact with patient and environmental factors, will be very important,” he added.
Nevertheless, “the study was well done and may serve as a foundation for future research,” Dr. Becker said. “The investigators used several powerful tools, including MRI, genomics, and [artificial intelligence] to draw their conclusions. This is precisely the way that ‘big data’ should be used – in a complementary fashion.”
The study authors and Dr. Becker reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A round heart, or left ventricle sphericity, predicted cardiomyopathy and atrial fibrillation (AFib) in a deep learning analysis of MRI images from close to 39,000 participants in the UK Biobank, a new study shows.
An increase of 1 standard deviation in the sphericity index (short axis length/long axis length) was associated with a 47% increased incidence of cardiomyopathy and a 20% increased incidence of AFib, independent of clinical factors and traditional MRI measures.
Furthermore, a genetic analysis suggested a shared architecture between sphericity and nonischemic cardiomyopathy, pointing to NICM as a possible causal factor for left ventricle sphericity among individuals with normal LV size and function.
“Physicians have known the heart gets rounder after heart attacks and as we get older,” David Ouyang, MD, a cardiologist in the Smidt Heart Institute at Cedars-Sinai Medical Center, Los Angeles, and a researcher in the division of artificial intelligence in medicine, said in an interview. “We wanted to see if this sphericity is prognostic of future disease even in healthy individuals.”
Although it is too early to recommend heart shape assessment in healthy asymptomatic people, he said, “physicians should be extra careful and think about treatments when they notice a patient’s heart is particularly round.”
The study was published online March 29 in the journal Med.
Sphericity index key
The investigators hypothesized that there is variation in LV sphericity within the spectrum of normal LV chamber size and systolic function, and that such variation might be a marker of cardiac risk with genetic influences.
To test this hypothesis, they used automated deep-learning segmentation of cardiac MRI data to estimate and analyze the sphericity index in a cohort of 38,897 individuals participating in the UK Biobank.
After adjustment for age at MRI and sex, an increased sphericity index was associated with an increased risk for cardiomyopathy (hazard ratio, 1.57), AFib (HR, 1.35), and heart failure (HR, 1.37).
No significant association was seen with cardiac arrest.
The team then stratified the cohort into quintiles and compared the top 20%, middle 60%, and bottom 20%. The relationship between the sphericity index and risk extended across the distribution; individuals with higher than median sphericity had increased disease incidence, and those with lower than median sphericity had decreased incidence.
Overall, a single standard deviation in the sphericity index was associated with increased risk of cardiomyopathy (HR, 1.47) and of AFib (HR, 1.20), independent of clinical factors and usual MRI measurements.
In a minimally adjusted model, the sphericity index was a predictor of incident cardiomyopathy, AFib, and heart failure.
Adjustment for clinical factors partially attenuated the heart failure association; additional adjustment for MRI measurements fully attenuated that association and partially attenuated the association with AFib.
However, in all adjusted models, the association with cardiomyopathy showed little attenuation.
Furthermore, the team identified four loci associated with sphericity at genomewide significance – PLN, ANGPT1, PDZRN3, and HLA DR/DQ – and Mendelian randomization supported NICM as a cause of LV sphericity.
Looking ahead
“While conventional imaging metrics have significant diagnostic and prognostic value, some of these measurements have been adopted out of convenience or tradition,” the authors noted. “By representing a specific multidimensional remodeling phenotype, sphericity has emerged as a distinct morphologic trait with features not adequately captured by conventional measurements.
“We expect that the search space of potential imaging measurements is vast, and we have only begun to scratch at the surface of disease associations.”
Indeed, Dr. Ouyang said his group is “trying to evaluate the sphericity in echocardiograms or heart ultrasounds, which are more common and cheaper than MRI.”
“The main caveat is translating the information directly to patient care,” Richard C. Becker, MD, director and physician-in-chief of the University of Cincinnati Heart, Lung, and Vascular Institute, said in an interview. “Near-term yield could include using the spherical calculation in routine MRI of the heart, and based on the findings, following patients more closely if there is an abnormal shape. Or performing an MRI and targeted gene testing if there is a family history of cardiomyopathy or [of] an abnormal shape of the heart.”
“Validation of the findings and large-scale evaluation of the genes identified, and how they interact with patient and environmental factors, will be very important,” he added.
Nevertheless, “the study was well done and may serve as a foundation for future research,” Dr. Becker said. “The investigators used several powerful tools, including MRI, genomics, and [artificial intelligence] to draw their conclusions. This is precisely the way that ‘big data’ should be used – in a complementary fashion.”
The study authors and Dr. Becker reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A round heart, or left ventricle sphericity, predicted cardiomyopathy and atrial fibrillation (AFib) in a deep learning analysis of MRI images from close to 39,000 participants in the UK Biobank, a new study shows.
An increase of 1 standard deviation in the sphericity index (short axis length/long axis length) was associated with a 47% increased incidence of cardiomyopathy and a 20% increased incidence of AFib, independent of clinical factors and traditional MRI measures.
Furthermore, a genetic analysis suggested a shared architecture between sphericity and nonischemic cardiomyopathy, pointing to NICM as a possible causal factor for left ventricle sphericity among individuals with normal LV size and function.
“Physicians have known the heart gets rounder after heart attacks and as we get older,” David Ouyang, MD, a cardiologist in the Smidt Heart Institute at Cedars-Sinai Medical Center, Los Angeles, and a researcher in the division of artificial intelligence in medicine, said in an interview. “We wanted to see if this sphericity is prognostic of future disease even in healthy individuals.”
Although it is too early to recommend heart shape assessment in healthy asymptomatic people, he said, “physicians should be extra careful and think about treatments when they notice a patient’s heart is particularly round.”
The study was published online March 29 in the journal Med.
Sphericity index key
The investigators hypothesized that there is variation in LV sphericity within the spectrum of normal LV chamber size and systolic function, and that such variation might be a marker of cardiac risk with genetic influences.
To test this hypothesis, they used automated deep-learning segmentation of cardiac MRI data to estimate and analyze the sphericity index in a cohort of 38,897 individuals participating in the UK Biobank.
After adjustment for age at MRI and sex, an increased sphericity index was associated with an increased risk for cardiomyopathy (hazard ratio, 1.57), AFib (HR, 1.35), and heart failure (HR, 1.37).
No significant association was seen with cardiac arrest.
The team then stratified the cohort into quintiles and compared the top 20%, middle 60%, and bottom 20%. The relationship between the sphericity index and risk extended across the distribution; individuals with higher than median sphericity had increased disease incidence, and those with lower than median sphericity had decreased incidence.
Overall, a single standard deviation in the sphericity index was associated with increased risk of cardiomyopathy (HR, 1.47) and of AFib (HR, 1.20), independent of clinical factors and usual MRI measurements.
In a minimally adjusted model, the sphericity index was a predictor of incident cardiomyopathy, AFib, and heart failure.
Adjustment for clinical factors partially attenuated the heart failure association; additional adjustment for MRI measurements fully attenuated that association and partially attenuated the association with AFib.
However, in all adjusted models, the association with cardiomyopathy showed little attenuation.
Furthermore, the team identified four loci associated with sphericity at genomewide significance – PLN, ANGPT1, PDZRN3, and HLA DR/DQ – and Mendelian randomization supported NICM as a cause of LV sphericity.
Looking ahead
“While conventional imaging metrics have significant diagnostic and prognostic value, some of these measurements have been adopted out of convenience or tradition,” the authors noted. “By representing a specific multidimensional remodeling phenotype, sphericity has emerged as a distinct morphologic trait with features not adequately captured by conventional measurements.
“We expect that the search space of potential imaging measurements is vast, and we have only begun to scratch at the surface of disease associations.”
Indeed, Dr. Ouyang said his group is “trying to evaluate the sphericity in echocardiograms or heart ultrasounds, which are more common and cheaper than MRI.”
“The main caveat is translating the information directly to patient care,” Richard C. Becker, MD, director and physician-in-chief of the University of Cincinnati Heart, Lung, and Vascular Institute, said in an interview. “Near-term yield could include using the spherical calculation in routine MRI of the heart, and based on the findings, following patients more closely if there is an abnormal shape. Or performing an MRI and targeted gene testing if there is a family history of cardiomyopathy or [of] an abnormal shape of the heart.”
“Validation of the findings and large-scale evaluation of the genes identified, and how they interact with patient and environmental factors, will be very important,” he added.
Nevertheless, “the study was well done and may serve as a foundation for future research,” Dr. Becker said. “The investigators used several powerful tools, including MRI, genomics, and [artificial intelligence] to draw their conclusions. This is precisely the way that ‘big data’ should be used – in a complementary fashion.”
The study authors and Dr. Becker reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MED
AHA, ACC push supervised exercise training for HFpEF
A statement released by the American Heart Association and the American College of Cardiology advocates use of supervised exercise training in patients with heart failure with preserved ejection fraction (HFpEF), as well as coverage for these services by third-party payers.
The authors hope to boost the stature of supervised exercise training (SET) in HFpEF among practitioners and show Medicare and insurers that it deserves reimbursement. Currently, they noted, clinicians tend to recognize exercise as therapy more in HF with reduced ejection fraction (HFrEF). And Medicare covers exercise training within broader cardiac rehabilitation programs for patients with HFrEF but not HFpEF.
Yet exercise has been broadly effective in HFpEF clinical trials, as outlined in the document. And there are good mechanistic reasons to believe that patients with the disorder can gain as much or more from SET than those with HFrEF.
“The signals for improvement from exercise training, in symptoms and objective measures of exercise capacity, are considerably larger for HFpEF than for HFrEF,” Dalane W. Kitzman, MD, Wake Forest University, Winston-Salem, N.C., said in an interview.
So, it’s a bit of a paradox that clinicians don’t prescribe it as often in HFpEF, probably because of the lack of reimbursement but also from less “awareness” and understanding of the disease itself, he proposed.
Dr. Kitzman is senior author on the statement sponsored by the AHA and the ACC. It was published in the societies’ flagship journals Circulation and the Journal of the American College of Cardiology. The statement was also endorsed by the Heart Failure Society of America, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the American Association of Heart Failure Nurses.
Carefully chosen words
The statement makes its case in HFpEF specifically for SET rather than cardiac rehabilitation, the latter typically a comprehensive program that goes beyond exercise, Dr. Kitzman noted. And SET is closer to the exercise interventions used in the supportive HFpEF trials.
“Also, Medicare in recent years has approved something called ‘supervised exercise training’ for other disorders, such as peripheral artery disease.” So, the document specifies SET “to be fully aligned with the evidence base,” he said, as well as “align it with a type of treatment that Medicare has a precedent for approving for other disorders.”
Data and physiologic basis
Core features of the AHA/ACC statement is its review of HFpEF exercise physiology, survey of randomized trials supporting SET in the disease, and characterization of exercise as an especially suitable pleiotropic therapy.
Increasingly, “HFpEF is now accepted as a systemic disorder that affects and impacts all organs,” Dr. Kitzman observed. “With a systemic multiorgan disorder, it would make sense that a broad treatment like exercise might be just the right thing. We think that’s the reason that its benefits are really quite large in magnitude.”
The document notes that exercise seems “potentially well suited for the treatment of both the cardiac and, in particular, the extracardiac abnormalities that contribute to exercise intolerance in HFpEF.”
Its effects in the disorder are “anti-inflammatory, rheological, lipid lowering, antihypertensive, positive inotropic, positive lusitropic, negative chronotropic, vasodilation, diuretic, weight-reducing, hypoglycemic, hypnotic, and antidepressive,” the statement notes. It achieves them via multiple pathways involving the heart, lungs, vasculature and, notably, the skeletal muscles.
“It’s been widely overlooked that at least 50% of low exercise capacity and symptoms in HFpEF are due to skeletal muscle dysfunction,” said Dr. Kitzman, an authority on exercise physiology in heart failure.
“But we’ve spent about 95% of our attention trying to modify and understand the cardiac component.” Skeletal muscles, he said, “are not an innocent bystander. They’re part of the problem. And that’s why we should really spend more time focusing on them.”
Dr. Kitzman disclosed receiving consulting fees from Bayer, Medtronic, Corvia Medical, Boehringer Ingelheim, Keyto, Rivus, NovoNordisk, AstraZeneca, and Pfizer; holding stock in Gilead; and receiving grants to his institution from Bayer, Novo Nordisk, AstraZeneca, Rivus, and Pfizer.
A version of this article first appeared on Medscape.com.
A statement released by the American Heart Association and the American College of Cardiology advocates use of supervised exercise training in patients with heart failure with preserved ejection fraction (HFpEF), as well as coverage for these services by third-party payers.
The authors hope to boost the stature of supervised exercise training (SET) in HFpEF among practitioners and show Medicare and insurers that it deserves reimbursement. Currently, they noted, clinicians tend to recognize exercise as therapy more in HF with reduced ejection fraction (HFrEF). And Medicare covers exercise training within broader cardiac rehabilitation programs for patients with HFrEF but not HFpEF.
Yet exercise has been broadly effective in HFpEF clinical trials, as outlined in the document. And there are good mechanistic reasons to believe that patients with the disorder can gain as much or more from SET than those with HFrEF.
“The signals for improvement from exercise training, in symptoms and objective measures of exercise capacity, are considerably larger for HFpEF than for HFrEF,” Dalane W. Kitzman, MD, Wake Forest University, Winston-Salem, N.C., said in an interview.
So, it’s a bit of a paradox that clinicians don’t prescribe it as often in HFpEF, probably because of the lack of reimbursement but also from less “awareness” and understanding of the disease itself, he proposed.
Dr. Kitzman is senior author on the statement sponsored by the AHA and the ACC. It was published in the societies’ flagship journals Circulation and the Journal of the American College of Cardiology. The statement was also endorsed by the Heart Failure Society of America, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the American Association of Heart Failure Nurses.
Carefully chosen words
The statement makes its case in HFpEF specifically for SET rather than cardiac rehabilitation, the latter typically a comprehensive program that goes beyond exercise, Dr. Kitzman noted. And SET is closer to the exercise interventions used in the supportive HFpEF trials.
“Also, Medicare in recent years has approved something called ‘supervised exercise training’ for other disorders, such as peripheral artery disease.” So, the document specifies SET “to be fully aligned with the evidence base,” he said, as well as “align it with a type of treatment that Medicare has a precedent for approving for other disorders.”
Data and physiologic basis
Core features of the AHA/ACC statement is its review of HFpEF exercise physiology, survey of randomized trials supporting SET in the disease, and characterization of exercise as an especially suitable pleiotropic therapy.
Increasingly, “HFpEF is now accepted as a systemic disorder that affects and impacts all organs,” Dr. Kitzman observed. “With a systemic multiorgan disorder, it would make sense that a broad treatment like exercise might be just the right thing. We think that’s the reason that its benefits are really quite large in magnitude.”
The document notes that exercise seems “potentially well suited for the treatment of both the cardiac and, in particular, the extracardiac abnormalities that contribute to exercise intolerance in HFpEF.”
Its effects in the disorder are “anti-inflammatory, rheological, lipid lowering, antihypertensive, positive inotropic, positive lusitropic, negative chronotropic, vasodilation, diuretic, weight-reducing, hypoglycemic, hypnotic, and antidepressive,” the statement notes. It achieves them via multiple pathways involving the heart, lungs, vasculature and, notably, the skeletal muscles.
“It’s been widely overlooked that at least 50% of low exercise capacity and symptoms in HFpEF are due to skeletal muscle dysfunction,” said Dr. Kitzman, an authority on exercise physiology in heart failure.
“But we’ve spent about 95% of our attention trying to modify and understand the cardiac component.” Skeletal muscles, he said, “are not an innocent bystander. They’re part of the problem. And that’s why we should really spend more time focusing on them.”
Dr. Kitzman disclosed receiving consulting fees from Bayer, Medtronic, Corvia Medical, Boehringer Ingelheim, Keyto, Rivus, NovoNordisk, AstraZeneca, and Pfizer; holding stock in Gilead; and receiving grants to his institution from Bayer, Novo Nordisk, AstraZeneca, Rivus, and Pfizer.
A version of this article first appeared on Medscape.com.
A statement released by the American Heart Association and the American College of Cardiology advocates use of supervised exercise training in patients with heart failure with preserved ejection fraction (HFpEF), as well as coverage for these services by third-party payers.
The authors hope to boost the stature of supervised exercise training (SET) in HFpEF among practitioners and show Medicare and insurers that it deserves reimbursement. Currently, they noted, clinicians tend to recognize exercise as therapy more in HF with reduced ejection fraction (HFrEF). And Medicare covers exercise training within broader cardiac rehabilitation programs for patients with HFrEF but not HFpEF.
Yet exercise has been broadly effective in HFpEF clinical trials, as outlined in the document. And there are good mechanistic reasons to believe that patients with the disorder can gain as much or more from SET than those with HFrEF.
“The signals for improvement from exercise training, in symptoms and objective measures of exercise capacity, are considerably larger for HFpEF than for HFrEF,” Dalane W. Kitzman, MD, Wake Forest University, Winston-Salem, N.C., said in an interview.
So, it’s a bit of a paradox that clinicians don’t prescribe it as often in HFpEF, probably because of the lack of reimbursement but also from less “awareness” and understanding of the disease itself, he proposed.
Dr. Kitzman is senior author on the statement sponsored by the AHA and the ACC. It was published in the societies’ flagship journals Circulation and the Journal of the American College of Cardiology. The statement was also endorsed by the Heart Failure Society of America, the American Association of Cardiovascular and Pulmonary Rehabilitation, and the American Association of Heart Failure Nurses.
Carefully chosen words
The statement makes its case in HFpEF specifically for SET rather than cardiac rehabilitation, the latter typically a comprehensive program that goes beyond exercise, Dr. Kitzman noted. And SET is closer to the exercise interventions used in the supportive HFpEF trials.
“Also, Medicare in recent years has approved something called ‘supervised exercise training’ for other disorders, such as peripheral artery disease.” So, the document specifies SET “to be fully aligned with the evidence base,” he said, as well as “align it with a type of treatment that Medicare has a precedent for approving for other disorders.”
Data and physiologic basis
Core features of the AHA/ACC statement is its review of HFpEF exercise physiology, survey of randomized trials supporting SET in the disease, and characterization of exercise as an especially suitable pleiotropic therapy.
Increasingly, “HFpEF is now accepted as a systemic disorder that affects and impacts all organs,” Dr. Kitzman observed. “With a systemic multiorgan disorder, it would make sense that a broad treatment like exercise might be just the right thing. We think that’s the reason that its benefits are really quite large in magnitude.”
The document notes that exercise seems “potentially well suited for the treatment of both the cardiac and, in particular, the extracardiac abnormalities that contribute to exercise intolerance in HFpEF.”
Its effects in the disorder are “anti-inflammatory, rheological, lipid lowering, antihypertensive, positive inotropic, positive lusitropic, negative chronotropic, vasodilation, diuretic, weight-reducing, hypoglycemic, hypnotic, and antidepressive,” the statement notes. It achieves them via multiple pathways involving the heart, lungs, vasculature and, notably, the skeletal muscles.
“It’s been widely overlooked that at least 50% of low exercise capacity and symptoms in HFpEF are due to skeletal muscle dysfunction,” said Dr. Kitzman, an authority on exercise physiology in heart failure.
“But we’ve spent about 95% of our attention trying to modify and understand the cardiac component.” Skeletal muscles, he said, “are not an innocent bystander. They’re part of the problem. And that’s why we should really spend more time focusing on them.”
Dr. Kitzman disclosed receiving consulting fees from Bayer, Medtronic, Corvia Medical, Boehringer Ingelheim, Keyto, Rivus, NovoNordisk, AstraZeneca, and Pfizer; holding stock in Gilead; and receiving grants to his institution from Bayer, Novo Nordisk, AstraZeneca, Rivus, and Pfizer.
A version of this article first appeared on Medscape.com.
COAPT 5-year results ‘remarkable,’ but patient selection issues remain
It remained an open question in 2018, on the unveiling of the COAPT trial’s 2-year primary results, whether the striking reductions in mortality and heart-failure (HF) hospitalization observed for transcatheter edge-to-edge repair (TEER) with the MitraClip (Abbott) would be durable with longer follow-up.
The trial had enrolled an especially sick population of symptomatic patients with mitral regurgitation (MR) secondary to HF.
As it turns out, the therapy’s benefits at 2 years were indeed durable, at least out to 5 years, investigators reported March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The results were simultaneously published in the New England Journal of Medicine.
Patients who received the MitraClip on top of intensive medical therapy, compared with a group assigned to medical management alone, benefited significantly at 5 years with risk reductions of 51% for HF hospitalization, 28% for death from any cause, and 47% for the composite of the two events.
Still, mortality at 5 years among the 614 randomized patients was steep at 57.3% in the MitraClip group and 67.2% for those assigned to meds only, underscoring the need for early identification of patients appropriate for the device therapy, Gregg W. Stone, MD, said during his presentation.
Dr. Stone, of the Icahn School of Medicine at Mount Sinai, New York, is a COAPT co-principal investigator and lead author of the 5-year outcomes publication.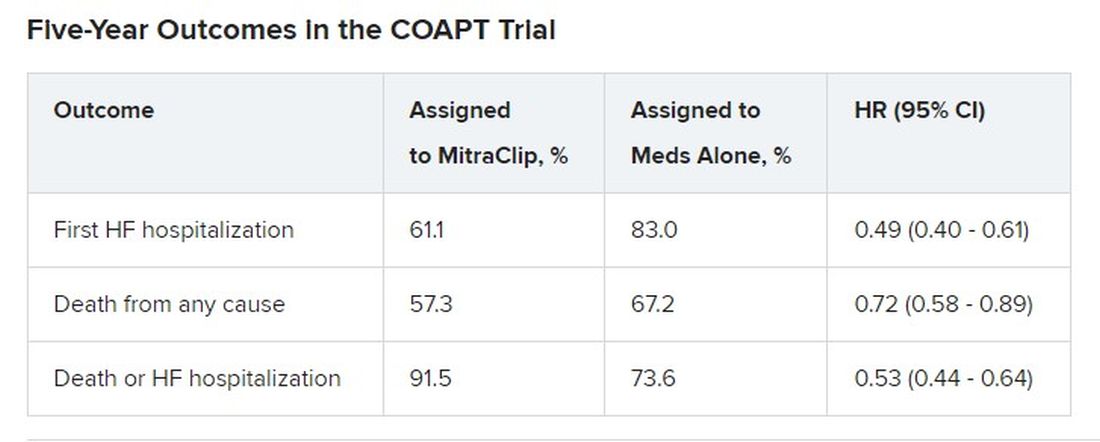
Outcomes were consistent across all prespecified patient subgroups, including by age, sex, MR, left ventricular (LV) function and volume, cardiomyopathy etiology, and degree of surgical risk, the researchers reported.
Symptom status, as measured by New York Heart Association (NYHA) functional class, improved throughout the 5-year follow-up for patients assigned to the MitraClip group, compared with the control group, and the intervention group was significantly more likely to be in NYHA class 1 or 2, the authors noted.
The relative benefits in terms of clinical outcomes of MitraClip therapy narrowed after 2-3 years, Dr. Stone said, primarily because at 2 years, patients who had been assigned to meds only were eligible to undergo TEER. Indeed, he noted, 45% of the 138 patients in the control group who were eligible for TEER at 2 years “crossed over” to receive a MitraClip. Those patients benefited despite their delay in undergoing the procedure, he observed.
However, nearly half of the control patients died before becoming eligible for crossover at 2 years. “We have to identify the appropriate patients for treatment and treat them early because the mortality is very high in this population,” Dr. Stone said.
“We need to do more because the MitraClip doesn’t do anything directly to the underlying left ventricular dysfunction, which is the cause of the patient’s disease,” he said. “We need advanced therapies to address the underlying left ventricular dysfunction” in this high-risk population.
Exclusions based on LV dimension
The COAPT trial included 614 patients with HF and symptomatic MR despite guideline-directed medical therapy. They were required to have moderate to severe (3+) or severe (4+) MR confirmed by an echocardiographic core laboratory and a left ventricular ejection fraction (LVEF) of 20%-50%.
Among the exclusion criteria were an LV end-systolic diameter greater than 70 mm, severe pulmonary hypertension, and moderate to severe symptomatic right ventricular failure.
The systolic LV dimension exclusion helped address the persistent question of whether “severe mitral regurgitation is a marker of a bad left ventricle or ... contributes to the pathophysiology” of MR and its poor outcomes, Dr. Stone said.
The 51% reduction in risk for time-to-first HF hospitalization among patients assigned to TEER “accrued very early,” Dr. Stone pointed out. “You can see the curves start to separate almost immediately after you reduce left atrial pressure and volume overload with the MitraClip.”
The curves stopped diverging after about 3 years because of crossover from the control group, he said. Still, “we had shown a substantial absolute 17% reduction in mortality at 2 years” with MitraClip. “That has continued out to 5 years, with a statistically significant 28% relative reduction,” he continued, and the absolute risk reduction reaching 10%.
Patients in the control group who crossed over “basically assumed the death and heart failure hospitalization rate of the MitraClip group,” Dr. Stone said. That wasn’t surprising “because most of the patients enrolled in the trial originally had chronic heart failure.” It’s “confirmation of the principal results of the trial.”
Comparison With MITRA-FR
“We know that MITRA-FR was a negative trial,” observed Wayne B. Batchelor, MD, an invited discussant following Dr. Stone’s presentation, referring to an earlier similar trial that showed no advantage for MitraClip. Compared with MITRA-FR, COAPT “has created an entirely different story.”
The marked reductions in mortality and risk for adverse events and low number-needed-to-treat with MitraClip are “really remarkable,” said Dr. Batchelor, who is with the Inova Heart and Vascular Institute, Falls Church, Va.
But the high absolute mortality for patients in the COAPT control group “speaks volumes to me and tells us that we’ve got to identify our patients well early,” he agreed, and to “implement transcatheter edge-to-edge therapy in properly selected patients on guideline-directed medical therapy in order to avoid that.”
The trial findings “suggest that we’re reducing HF hospitalization,” he said, “so this is an extremely potent therapy, potentially.
“The dramatic difference between the treated arm and the medical therapy arm in this trial makes me feel that this therapy is here to stay,” Dr. Batchelor concluded. “We just have to figure out how to deploy it properly in the right patients.”
The COAPT trial presents “a practice-changing paradigm,” said Suzanne J. Baron, MD, of Lahey Hospital & Medical Center, Burlington, Mass., another invited discussant.
The crossover data “really jumped out,” she added. “Waiting to treat patients with TEER may be harmful, so if we’re going to consider treating earlier, how do we identify the right patient?” Dr. Baron asked, especially given the negative MITRA-FR results.
MITRA-FR didn’t follow patients beyond 2 years, Dr. Stone noted. Still, “we do think that the main difference was that COAPT enrolled a patient population with more severe MR and slightly less LV dysfunction, at least in terms of the LV not being as dilated, so they didn’t have end-stage LV disease. Whereas in MITRA-FR, more of the patients had only moderate mitral regurgitation.” And big dilated left ventricles “are less likely to benefit.”
There were also differences between the studies in technique and background medical therapies, he added.
The Food and Drug Administration has approved – and payers are paying – for the treatment of patients who meet the COAPT criteria, “in whom we can be very confident they have a benefit,” Dr. Stone said.
“The real question is: Where are the edges where we should consider this? LVEF slightly less than 20% or slightly greater than 50%? Or primary atrial functional mitral regurgitation? There are registry data to suggest that they would benefit,” he said, but “we need more data.”
COAPT was supported by Abbott. Dr. Stone disclosed receiving speaker honoraria from Abbott and consulting fees or equity from Neovasc, Ancora, Valfix, and Cardiac Success; and that Mount Sinai receives research funding from Abbott. Disclosures for the other authors are available at nejm.org. Dr. Batchelor has disclosed receiving consultant fees or honoraria from Abbott, Boston Scientific, Idorsia, and V-Wave Medical, and having other ties with Medtronic. Dr. Baron has disclosed receiving consultant fees or honoraria from Abiomed, Biotronik, Boston Scientific, Edwards Lifesciences, Medtronic, Shockwave, and Zoll Medical, and conducting research or receiving research grants from Abiomed and Boston Scientific.
A version of this article originally appeared on Medscape.com.
It remained an open question in 2018, on the unveiling of the COAPT trial’s 2-year primary results, whether the striking reductions in mortality and heart-failure (HF) hospitalization observed for transcatheter edge-to-edge repair (TEER) with the MitraClip (Abbott) would be durable with longer follow-up.
The trial had enrolled an especially sick population of symptomatic patients with mitral regurgitation (MR) secondary to HF.
As it turns out, the therapy’s benefits at 2 years were indeed durable, at least out to 5 years, investigators reported March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The results were simultaneously published in the New England Journal of Medicine.
Patients who received the MitraClip on top of intensive medical therapy, compared with a group assigned to medical management alone, benefited significantly at 5 years with risk reductions of 51% for HF hospitalization, 28% for death from any cause, and 47% for the composite of the two events.
Still, mortality at 5 years among the 614 randomized patients was steep at 57.3% in the MitraClip group and 67.2% for those assigned to meds only, underscoring the need for early identification of patients appropriate for the device therapy, Gregg W. Stone, MD, said during his presentation.
Dr. Stone, of the Icahn School of Medicine at Mount Sinai, New York, is a COAPT co-principal investigator and lead author of the 5-year outcomes publication.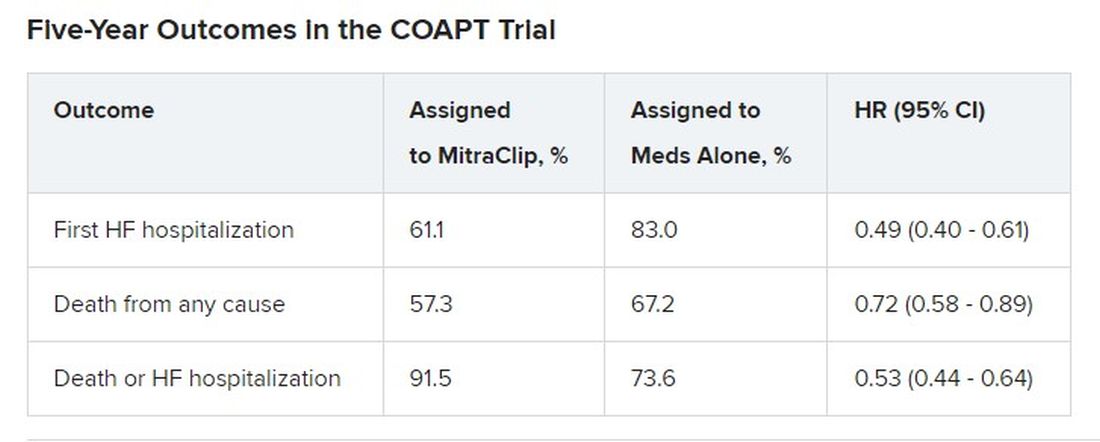
Outcomes were consistent across all prespecified patient subgroups, including by age, sex, MR, left ventricular (LV) function and volume, cardiomyopathy etiology, and degree of surgical risk, the researchers reported.
Symptom status, as measured by New York Heart Association (NYHA) functional class, improved throughout the 5-year follow-up for patients assigned to the MitraClip group, compared with the control group, and the intervention group was significantly more likely to be in NYHA class 1 or 2, the authors noted.
The relative benefits in terms of clinical outcomes of MitraClip therapy narrowed after 2-3 years, Dr. Stone said, primarily because at 2 years, patients who had been assigned to meds only were eligible to undergo TEER. Indeed, he noted, 45% of the 138 patients in the control group who were eligible for TEER at 2 years “crossed over” to receive a MitraClip. Those patients benefited despite their delay in undergoing the procedure, he observed.
However, nearly half of the control patients died before becoming eligible for crossover at 2 years. “We have to identify the appropriate patients for treatment and treat them early because the mortality is very high in this population,” Dr. Stone said.
“We need to do more because the MitraClip doesn’t do anything directly to the underlying left ventricular dysfunction, which is the cause of the patient’s disease,” he said. “We need advanced therapies to address the underlying left ventricular dysfunction” in this high-risk population.
Exclusions based on LV dimension
The COAPT trial included 614 patients with HF and symptomatic MR despite guideline-directed medical therapy. They were required to have moderate to severe (3+) or severe (4+) MR confirmed by an echocardiographic core laboratory and a left ventricular ejection fraction (LVEF) of 20%-50%.
Among the exclusion criteria were an LV end-systolic diameter greater than 70 mm, severe pulmonary hypertension, and moderate to severe symptomatic right ventricular failure.
The systolic LV dimension exclusion helped address the persistent question of whether “severe mitral regurgitation is a marker of a bad left ventricle or ... contributes to the pathophysiology” of MR and its poor outcomes, Dr. Stone said.
The 51% reduction in risk for time-to-first HF hospitalization among patients assigned to TEER “accrued very early,” Dr. Stone pointed out. “You can see the curves start to separate almost immediately after you reduce left atrial pressure and volume overload with the MitraClip.”
The curves stopped diverging after about 3 years because of crossover from the control group, he said. Still, “we had shown a substantial absolute 17% reduction in mortality at 2 years” with MitraClip. “That has continued out to 5 years, with a statistically significant 28% relative reduction,” he continued, and the absolute risk reduction reaching 10%.
Patients in the control group who crossed over “basically assumed the death and heart failure hospitalization rate of the MitraClip group,” Dr. Stone said. That wasn’t surprising “because most of the patients enrolled in the trial originally had chronic heart failure.” It’s “confirmation of the principal results of the trial.”
Comparison With MITRA-FR
“We know that MITRA-FR was a negative trial,” observed Wayne B. Batchelor, MD, an invited discussant following Dr. Stone’s presentation, referring to an earlier similar trial that showed no advantage for MitraClip. Compared with MITRA-FR, COAPT “has created an entirely different story.”
The marked reductions in mortality and risk for adverse events and low number-needed-to-treat with MitraClip are “really remarkable,” said Dr. Batchelor, who is with the Inova Heart and Vascular Institute, Falls Church, Va.
But the high absolute mortality for patients in the COAPT control group “speaks volumes to me and tells us that we’ve got to identify our patients well early,” he agreed, and to “implement transcatheter edge-to-edge therapy in properly selected patients on guideline-directed medical therapy in order to avoid that.”
The trial findings “suggest that we’re reducing HF hospitalization,” he said, “so this is an extremely potent therapy, potentially.
“The dramatic difference between the treated arm and the medical therapy arm in this trial makes me feel that this therapy is here to stay,” Dr. Batchelor concluded. “We just have to figure out how to deploy it properly in the right patients.”
The COAPT trial presents “a practice-changing paradigm,” said Suzanne J. Baron, MD, of Lahey Hospital & Medical Center, Burlington, Mass., another invited discussant.
The crossover data “really jumped out,” she added. “Waiting to treat patients with TEER may be harmful, so if we’re going to consider treating earlier, how do we identify the right patient?” Dr. Baron asked, especially given the negative MITRA-FR results.
MITRA-FR didn’t follow patients beyond 2 years, Dr. Stone noted. Still, “we do think that the main difference was that COAPT enrolled a patient population with more severe MR and slightly less LV dysfunction, at least in terms of the LV not being as dilated, so they didn’t have end-stage LV disease. Whereas in MITRA-FR, more of the patients had only moderate mitral regurgitation.” And big dilated left ventricles “are less likely to benefit.”
There were also differences between the studies in technique and background medical therapies, he added.
The Food and Drug Administration has approved – and payers are paying – for the treatment of patients who meet the COAPT criteria, “in whom we can be very confident they have a benefit,” Dr. Stone said.
“The real question is: Where are the edges where we should consider this? LVEF slightly less than 20% or slightly greater than 50%? Or primary atrial functional mitral regurgitation? There are registry data to suggest that they would benefit,” he said, but “we need more data.”
COAPT was supported by Abbott. Dr. Stone disclosed receiving speaker honoraria from Abbott and consulting fees or equity from Neovasc, Ancora, Valfix, and Cardiac Success; and that Mount Sinai receives research funding from Abbott. Disclosures for the other authors are available at nejm.org. Dr. Batchelor has disclosed receiving consultant fees or honoraria from Abbott, Boston Scientific, Idorsia, and V-Wave Medical, and having other ties with Medtronic. Dr. Baron has disclosed receiving consultant fees or honoraria from Abiomed, Biotronik, Boston Scientific, Edwards Lifesciences, Medtronic, Shockwave, and Zoll Medical, and conducting research or receiving research grants from Abiomed and Boston Scientific.
A version of this article originally appeared on Medscape.com.
It remained an open question in 2018, on the unveiling of the COAPT trial’s 2-year primary results, whether the striking reductions in mortality and heart-failure (HF) hospitalization observed for transcatheter edge-to-edge repair (TEER) with the MitraClip (Abbott) would be durable with longer follow-up.
The trial had enrolled an especially sick population of symptomatic patients with mitral regurgitation (MR) secondary to HF.
As it turns out, the therapy’s benefits at 2 years were indeed durable, at least out to 5 years, investigators reported March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. The results were simultaneously published in the New England Journal of Medicine.
Patients who received the MitraClip on top of intensive medical therapy, compared with a group assigned to medical management alone, benefited significantly at 5 years with risk reductions of 51% for HF hospitalization, 28% for death from any cause, and 47% for the composite of the two events.
Still, mortality at 5 years among the 614 randomized patients was steep at 57.3% in the MitraClip group and 67.2% for those assigned to meds only, underscoring the need for early identification of patients appropriate for the device therapy, Gregg W. Stone, MD, said during his presentation.
Dr. Stone, of the Icahn School of Medicine at Mount Sinai, New York, is a COAPT co-principal investigator and lead author of the 5-year outcomes publication.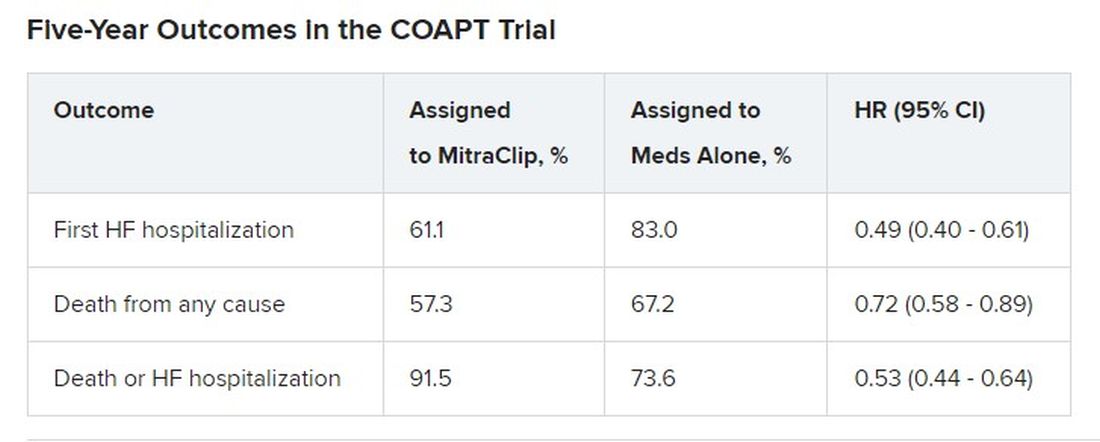
Outcomes were consistent across all prespecified patient subgroups, including by age, sex, MR, left ventricular (LV) function and volume, cardiomyopathy etiology, and degree of surgical risk, the researchers reported.
Symptom status, as measured by New York Heart Association (NYHA) functional class, improved throughout the 5-year follow-up for patients assigned to the MitraClip group, compared with the control group, and the intervention group was significantly more likely to be in NYHA class 1 or 2, the authors noted.
The relative benefits in terms of clinical outcomes of MitraClip therapy narrowed after 2-3 years, Dr. Stone said, primarily because at 2 years, patients who had been assigned to meds only were eligible to undergo TEER. Indeed, he noted, 45% of the 138 patients in the control group who were eligible for TEER at 2 years “crossed over” to receive a MitraClip. Those patients benefited despite their delay in undergoing the procedure, he observed.
However, nearly half of the control patients died before becoming eligible for crossover at 2 years. “We have to identify the appropriate patients for treatment and treat them early because the mortality is very high in this population,” Dr. Stone said.
“We need to do more because the MitraClip doesn’t do anything directly to the underlying left ventricular dysfunction, which is the cause of the patient’s disease,” he said. “We need advanced therapies to address the underlying left ventricular dysfunction” in this high-risk population.
Exclusions based on LV dimension
The COAPT trial included 614 patients with HF and symptomatic MR despite guideline-directed medical therapy. They were required to have moderate to severe (3+) or severe (4+) MR confirmed by an echocardiographic core laboratory and a left ventricular ejection fraction (LVEF) of 20%-50%.
Among the exclusion criteria were an LV end-systolic diameter greater than 70 mm, severe pulmonary hypertension, and moderate to severe symptomatic right ventricular failure.
The systolic LV dimension exclusion helped address the persistent question of whether “severe mitral regurgitation is a marker of a bad left ventricle or ... contributes to the pathophysiology” of MR and its poor outcomes, Dr. Stone said.
The 51% reduction in risk for time-to-first HF hospitalization among patients assigned to TEER “accrued very early,” Dr. Stone pointed out. “You can see the curves start to separate almost immediately after you reduce left atrial pressure and volume overload with the MitraClip.”
The curves stopped diverging after about 3 years because of crossover from the control group, he said. Still, “we had shown a substantial absolute 17% reduction in mortality at 2 years” with MitraClip. “That has continued out to 5 years, with a statistically significant 28% relative reduction,” he continued, and the absolute risk reduction reaching 10%.
Patients in the control group who crossed over “basically assumed the death and heart failure hospitalization rate of the MitraClip group,” Dr. Stone said. That wasn’t surprising “because most of the patients enrolled in the trial originally had chronic heart failure.” It’s “confirmation of the principal results of the trial.”
Comparison With MITRA-FR
“We know that MITRA-FR was a negative trial,” observed Wayne B. Batchelor, MD, an invited discussant following Dr. Stone’s presentation, referring to an earlier similar trial that showed no advantage for MitraClip. Compared with MITRA-FR, COAPT “has created an entirely different story.”
The marked reductions in mortality and risk for adverse events and low number-needed-to-treat with MitraClip are “really remarkable,” said Dr. Batchelor, who is with the Inova Heart and Vascular Institute, Falls Church, Va.
But the high absolute mortality for patients in the COAPT control group “speaks volumes to me and tells us that we’ve got to identify our patients well early,” he agreed, and to “implement transcatheter edge-to-edge therapy in properly selected patients on guideline-directed medical therapy in order to avoid that.”
The trial findings “suggest that we’re reducing HF hospitalization,” he said, “so this is an extremely potent therapy, potentially.
“The dramatic difference between the treated arm and the medical therapy arm in this trial makes me feel that this therapy is here to stay,” Dr. Batchelor concluded. “We just have to figure out how to deploy it properly in the right patients.”
The COAPT trial presents “a practice-changing paradigm,” said Suzanne J. Baron, MD, of Lahey Hospital & Medical Center, Burlington, Mass., another invited discussant.
The crossover data “really jumped out,” she added. “Waiting to treat patients with TEER may be harmful, so if we’re going to consider treating earlier, how do we identify the right patient?” Dr. Baron asked, especially given the negative MITRA-FR results.
MITRA-FR didn’t follow patients beyond 2 years, Dr. Stone noted. Still, “we do think that the main difference was that COAPT enrolled a patient population with more severe MR and slightly less LV dysfunction, at least in terms of the LV not being as dilated, so they didn’t have end-stage LV disease. Whereas in MITRA-FR, more of the patients had only moderate mitral regurgitation.” And big dilated left ventricles “are less likely to benefit.”
There were also differences between the studies in technique and background medical therapies, he added.
The Food and Drug Administration has approved – and payers are paying – for the treatment of patients who meet the COAPT criteria, “in whom we can be very confident they have a benefit,” Dr. Stone said.
“The real question is: Where are the edges where we should consider this? LVEF slightly less than 20% or slightly greater than 50%? Or primary atrial functional mitral regurgitation? There are registry data to suggest that they would benefit,” he said, but “we need more data.”
COAPT was supported by Abbott. Dr. Stone disclosed receiving speaker honoraria from Abbott and consulting fees or equity from Neovasc, Ancora, Valfix, and Cardiac Success; and that Mount Sinai receives research funding from Abbott. Disclosures for the other authors are available at nejm.org. Dr. Batchelor has disclosed receiving consultant fees or honoraria from Abbott, Boston Scientific, Idorsia, and V-Wave Medical, and having other ties with Medtronic. Dr. Baron has disclosed receiving consultant fees or honoraria from Abiomed, Biotronik, Boston Scientific, Edwards Lifesciences, Medtronic, Shockwave, and Zoll Medical, and conducting research or receiving research grants from Abiomed and Boston Scientific.
A version of this article originally appeared on Medscape.com.
FROM ACC 2023
Does new heart transplant method challenge definition of death?
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
Dapagliflozin’s HFpEF benefit tied to lower filling pressure
NEW ORLEANS – Treatment of patients with heart failure with preserved ejection fraction (HFpEF) with the SGLT2 inhibitor dapagliflozin (Farxiga) for 24 weeks produced significant and beneficial reductions in left-heart filling pressures in a mechanistic, randomized clinical study.
The findings “provide new insight into the mechanisms underlying the favorable clinical effects of dapagliflozin in patients with HFpEF,” Barry A. Borlaug, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. “Elevations in left heart filling pressures at rest and during exercise are fundamental pathophysiologic features of HFpEF,” he noted.
Results from prior studies documented the benefit of dapagliflozin for improving clinical outcomes in patients with HFpEF in the DELIVER trial, and for the related sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance) in the EMPEROR-Preserved trial. The new findings presented by Dr. Borlaug provide evidence from a placebo-controlled, prospective study for one way by which these SGLT2 inhibitors exert this benefit in patients with HFpEF.
The results of his single-center study showed that, in patients with HFpEF who also exhibited “severe” elevations in pulmonary capillary wedge pressure (PCWP) during exercise, 24 weeks of treatment with dapagliflozin led to a significant reduction in PCWP during exercise. The treatment produced an average 6.1–mm Hg drop from baseline compared with control patients who received placebo. A similar pattern occurred when these patients were at rest, when dapagliflozin treatment linked with a significant average reduction in PCWP from baseline of 3.5 mm Hg compared with controls.
Improving a ‘specific and fundamental’ feature of HFpEF
“This fantastic study looked at one of the fundamental aspects of HFpEF,” said John R. Teerlink, MD, designated discussant for the study. “You’ve shown that dapagliflozin targets a specific and fundamental” manifestation of HFpEF by lowering PCWP, said Dr. Teerlink, director of Heart Failure at the San Francisco Veterans Affairs Medical Center.
However, Dr. Teerlink added, the study did not directly address the related question of what physiologic action of dapagliflozin produces this notable drop in PCWP.
“We’re just starting to look at that,” replied Dr. Borlaug, a cardiologist and professor at the Mayo Clinic in Rochester, Minn.
He reported finding an intriguing correlate in the current study linked to the cut in PCWP with dapagliflozin treatment. The SGLT2 inhibitor at a standard daily 10-mg dose produced an average 3.5-kg drop in body weight in the dapagliflozin-treated patients that significantly linked with the changes in PCWP both at rest and during exercise. Dapagliflozin-treated patients also showed a significant reduction from their baseline plasma volume compared with placebo-treated patients, but this “poorly correlated” with the dapagliflozin-linked cuts in PCWP, Dr. Borlaug said.
“I don’t think this means weight loss is the cause of the hemodynamic benefit, but maybe it’s an indicator. When patients [with HFpEF] lose weight, they are in a metabolic state that leads to good changes in hemodynamics,” he suggested. “My guess is that there is probably a combination of many different little things [caused by dapagliflozin treatment of patients with HFpEF] that together result in the 20%-25% relative improvement we see in filling pressure.”
An ‘obese, cardiometabolic’ HFpEF phenotype
The study enrolled patients with HFpEF and a left ventricular ejection fraction of at least 50%, a New York Heart Association functional class of 2 or 3, and a PCWP during exercise of at least 25 mm Hg. Of the 37 evaluable patients, about two-thirds of the patients were women, more than two-thirds were in functional class 3, about 70% were obese, and their average ejection fraction was about 62%. The study excluded patients with HFpEF who also had type 1 diabetes, cardiomyopathy, pericardial disease, or other causes of dyspnea or heart failure.
Dr. Teerlink asked about the generalizability of the findings, as the study cohort seemed to differ in certain respects from the patients enrolled in the DELIVER trial, and because of the many apparently distinct patient phenotypes that exist within the scope of HFpEF.
An “obese, cardiometabolic phenotype” predominated the study cohort, Dr. Borlaug said. “The patients we enrolled look like the HFpEF patients seen in U.S. clinics.” However, he added that “in reality, many [HFpEF phenotypes] coexist in one patient. It’s not that simple,” that every patient with HFpEF can be categorized into a single HFpEF phenotype.
The researchers monitored PCWP invasively with high-fidelity micromanometer catheters.
The study was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Borlaug has received research funding from AstraZeneca, as well as from Corvia, GlaxoSmithKline, Medtronic, Mesoblast, Novo Nordisk, and Tenax. Dr. Teerlink has had financial relationships with AstraZeneca, as well as with Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Cytokinetics, Medtronic, Merck, Novartis, Servier, and Windtree Therapeutics.
NEW ORLEANS – Treatment of patients with heart failure with preserved ejection fraction (HFpEF) with the SGLT2 inhibitor dapagliflozin (Farxiga) for 24 weeks produced significant and beneficial reductions in left-heart filling pressures in a mechanistic, randomized clinical study.
The findings “provide new insight into the mechanisms underlying the favorable clinical effects of dapagliflozin in patients with HFpEF,” Barry A. Borlaug, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. “Elevations in left heart filling pressures at rest and during exercise are fundamental pathophysiologic features of HFpEF,” he noted.
Results from prior studies documented the benefit of dapagliflozin for improving clinical outcomes in patients with HFpEF in the DELIVER trial, and for the related sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance) in the EMPEROR-Preserved trial. The new findings presented by Dr. Borlaug provide evidence from a placebo-controlled, prospective study for one way by which these SGLT2 inhibitors exert this benefit in patients with HFpEF.
The results of his single-center study showed that, in patients with HFpEF who also exhibited “severe” elevations in pulmonary capillary wedge pressure (PCWP) during exercise, 24 weeks of treatment with dapagliflozin led to a significant reduction in PCWP during exercise. The treatment produced an average 6.1–mm Hg drop from baseline compared with control patients who received placebo. A similar pattern occurred when these patients were at rest, when dapagliflozin treatment linked with a significant average reduction in PCWP from baseline of 3.5 mm Hg compared with controls.
Improving a ‘specific and fundamental’ feature of HFpEF
“This fantastic study looked at one of the fundamental aspects of HFpEF,” said John R. Teerlink, MD, designated discussant for the study. “You’ve shown that dapagliflozin targets a specific and fundamental” manifestation of HFpEF by lowering PCWP, said Dr. Teerlink, director of Heart Failure at the San Francisco Veterans Affairs Medical Center.
However, Dr. Teerlink added, the study did not directly address the related question of what physiologic action of dapagliflozin produces this notable drop in PCWP.
“We’re just starting to look at that,” replied Dr. Borlaug, a cardiologist and professor at the Mayo Clinic in Rochester, Minn.
He reported finding an intriguing correlate in the current study linked to the cut in PCWP with dapagliflozin treatment. The SGLT2 inhibitor at a standard daily 10-mg dose produced an average 3.5-kg drop in body weight in the dapagliflozin-treated patients that significantly linked with the changes in PCWP both at rest and during exercise. Dapagliflozin-treated patients also showed a significant reduction from their baseline plasma volume compared with placebo-treated patients, but this “poorly correlated” with the dapagliflozin-linked cuts in PCWP, Dr. Borlaug said.
“I don’t think this means weight loss is the cause of the hemodynamic benefit, but maybe it’s an indicator. When patients [with HFpEF] lose weight, they are in a metabolic state that leads to good changes in hemodynamics,” he suggested. “My guess is that there is probably a combination of many different little things [caused by dapagliflozin treatment of patients with HFpEF] that together result in the 20%-25% relative improvement we see in filling pressure.”
An ‘obese, cardiometabolic’ HFpEF phenotype
The study enrolled patients with HFpEF and a left ventricular ejection fraction of at least 50%, a New York Heart Association functional class of 2 or 3, and a PCWP during exercise of at least 25 mm Hg. Of the 37 evaluable patients, about two-thirds of the patients were women, more than two-thirds were in functional class 3, about 70% were obese, and their average ejection fraction was about 62%. The study excluded patients with HFpEF who also had type 1 diabetes, cardiomyopathy, pericardial disease, or other causes of dyspnea or heart failure.
Dr. Teerlink asked about the generalizability of the findings, as the study cohort seemed to differ in certain respects from the patients enrolled in the DELIVER trial, and because of the many apparently distinct patient phenotypes that exist within the scope of HFpEF.
An “obese, cardiometabolic phenotype” predominated the study cohort, Dr. Borlaug said. “The patients we enrolled look like the HFpEF patients seen in U.S. clinics.” However, he added that “in reality, many [HFpEF phenotypes] coexist in one patient. It’s not that simple,” that every patient with HFpEF can be categorized into a single HFpEF phenotype.
The researchers monitored PCWP invasively with high-fidelity micromanometer catheters.
The study was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Borlaug has received research funding from AstraZeneca, as well as from Corvia, GlaxoSmithKline, Medtronic, Mesoblast, Novo Nordisk, and Tenax. Dr. Teerlink has had financial relationships with AstraZeneca, as well as with Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Cytokinetics, Medtronic, Merck, Novartis, Servier, and Windtree Therapeutics.
NEW ORLEANS – Treatment of patients with heart failure with preserved ejection fraction (HFpEF) with the SGLT2 inhibitor dapagliflozin (Farxiga) for 24 weeks produced significant and beneficial reductions in left-heart filling pressures in a mechanistic, randomized clinical study.
The findings “provide new insight into the mechanisms underlying the favorable clinical effects of dapagliflozin in patients with HFpEF,” Barry A. Borlaug, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. “Elevations in left heart filling pressures at rest and during exercise are fundamental pathophysiologic features of HFpEF,” he noted.
Results from prior studies documented the benefit of dapagliflozin for improving clinical outcomes in patients with HFpEF in the DELIVER trial, and for the related sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance) in the EMPEROR-Preserved trial. The new findings presented by Dr. Borlaug provide evidence from a placebo-controlled, prospective study for one way by which these SGLT2 inhibitors exert this benefit in patients with HFpEF.
The results of his single-center study showed that, in patients with HFpEF who also exhibited “severe” elevations in pulmonary capillary wedge pressure (PCWP) during exercise, 24 weeks of treatment with dapagliflozin led to a significant reduction in PCWP during exercise. The treatment produced an average 6.1–mm Hg drop from baseline compared with control patients who received placebo. A similar pattern occurred when these patients were at rest, when dapagliflozin treatment linked with a significant average reduction in PCWP from baseline of 3.5 mm Hg compared with controls.
Improving a ‘specific and fundamental’ feature of HFpEF
“This fantastic study looked at one of the fundamental aspects of HFpEF,” said John R. Teerlink, MD, designated discussant for the study. “You’ve shown that dapagliflozin targets a specific and fundamental” manifestation of HFpEF by lowering PCWP, said Dr. Teerlink, director of Heart Failure at the San Francisco Veterans Affairs Medical Center.
However, Dr. Teerlink added, the study did not directly address the related question of what physiologic action of dapagliflozin produces this notable drop in PCWP.
“We’re just starting to look at that,” replied Dr. Borlaug, a cardiologist and professor at the Mayo Clinic in Rochester, Minn.
He reported finding an intriguing correlate in the current study linked to the cut in PCWP with dapagliflozin treatment. The SGLT2 inhibitor at a standard daily 10-mg dose produced an average 3.5-kg drop in body weight in the dapagliflozin-treated patients that significantly linked with the changes in PCWP both at rest and during exercise. Dapagliflozin-treated patients also showed a significant reduction from their baseline plasma volume compared with placebo-treated patients, but this “poorly correlated” with the dapagliflozin-linked cuts in PCWP, Dr. Borlaug said.
“I don’t think this means weight loss is the cause of the hemodynamic benefit, but maybe it’s an indicator. When patients [with HFpEF] lose weight, they are in a metabolic state that leads to good changes in hemodynamics,” he suggested. “My guess is that there is probably a combination of many different little things [caused by dapagliflozin treatment of patients with HFpEF] that together result in the 20%-25% relative improvement we see in filling pressure.”
An ‘obese, cardiometabolic’ HFpEF phenotype
The study enrolled patients with HFpEF and a left ventricular ejection fraction of at least 50%, a New York Heart Association functional class of 2 or 3, and a PCWP during exercise of at least 25 mm Hg. Of the 37 evaluable patients, about two-thirds of the patients were women, more than two-thirds were in functional class 3, about 70% were obese, and their average ejection fraction was about 62%. The study excluded patients with HFpEF who also had type 1 diabetes, cardiomyopathy, pericardial disease, or other causes of dyspnea or heart failure.
Dr. Teerlink asked about the generalizability of the findings, as the study cohort seemed to differ in certain respects from the patients enrolled in the DELIVER trial, and because of the many apparently distinct patient phenotypes that exist within the scope of HFpEF.
An “obese, cardiometabolic phenotype” predominated the study cohort, Dr. Borlaug said. “The patients we enrolled look like the HFpEF patients seen in U.S. clinics.” However, he added that “in reality, many [HFpEF phenotypes] coexist in one patient. It’s not that simple,” that every patient with HFpEF can be categorized into a single HFpEF phenotype.
The researchers monitored PCWP invasively with high-fidelity micromanometer catheters.
The study was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Borlaug has received research funding from AstraZeneca, as well as from Corvia, GlaxoSmithKline, Medtronic, Mesoblast, Novo Nordisk, and Tenax. Dr. Teerlink has had financial relationships with AstraZeneca, as well as with Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Cytokinetics, Medtronic, Merck, Novartis, Servier, and Windtree Therapeutics.
AT ACC 2023
Mediterranean diet linked to 24% reduction in CVD risk in women
The Mediterranean diet appears to be associated with a lower incidence of cardiovascular disease (CVD) and mortality in women, new observational data suggest.
Those who had a higher adherence to a Mediterranean diet had a 24% lower risk for cardiovascular disease and 23% lower risk for death.
“A healthy diet is a huge factor in preventing heart disease. However, current guidelines on preventing heart disease lack sex-specific recommendations,” said senior author Sarah Zaman, MBBS, PhD, an associate professor of medicine and principal research fellow at the University of Sydney’s Westmead Applied Research Centre.
“Historically, research trials and studies have had predominantly male participants or lacked sex-specific analysis,” she said. “Our results will pave the way to bridge this gap and also highlight the need for more research to ensure health guidelines and policies include diverse perspectives.”
The study was published online in the journal Heart.
Analyzing cardiovascular outcomes
Dr. Zaman and colleagues conducted a systematic review and meta-analysis of 16 studies published between 2006 and 2021 that reported a Mediterranean diet score and included either all women or had stratified outcomes by sex. They excluded studies that referred to only certain components of the Mediterranean diet or combined it with other lifestyle-related factors.
The studies, which were mainly conducted in the United States and Europe, included 722,495 adult women without previous clinical or subclinical CVD, with a median follow-up of 12.5 years.
Higher Mediterranean diet adherence was defined as the highest category reporting the highest range of Mediterranean diet scores, and lower adherence was defined as the lowest category reporting lowest scores. Incident CVD included coronary heart disease, myocardial infarction, stroke, heart failure, cardiovascular death, major adverse cardiovascular events, major adverse cardiac cerebrovascular events, and patient-reported CVD.
Overall, higher adherence to a Mediterranean diet was associated with lower CVD incidence (hazard ratio, 0.76; 95% confidence interval, 0.72-0.81), total mortality (HR, 0.77; 95% CI, 0.74-0.80), and coronary heart disease (HR, 0.75; 95% CI, 0.65-0.87).
Stroke incidence was also lower among women who adhered to the Mediterranean diet, although it wasn’t considered statistically significant (HR, 0.87; 95% CI, 0.76-1.01).
Additional analyses found similar reductions in risk across women of different ethnicities. Higher Mediterranean diet adherence was associated with lower CVD incidence for both women of European descent (HR, 0.76; 95% CI, 0.59-0.98) and women of non-European descent – Asian, Native Hawaiian, and African American – (HR, 0.79; 95% CI, 0.72-0.87).
The results didn’t materially change in sensitivity analyses, the authors note. Excluding one study at a time, the pooled HRs for the highest versus the lowest Mediterranean diet adherence ranged from 0.76 (95% CI, 0.72-0.80) to 0.83 (95% CI, 0.70-0.98) for incident CVD and from 0.77 (95% CI, 0.75-0.80) to 0.77 (95% CI, 0.74-0.81) for total mortality among women.
At the same time, the authors pointed to several limitations, including the observational nature of all of the studies, the reliance on self-reported food frequency questionnaires, and heterogeneity in the adjustments for influential factors across the studies.
Additional considerations
Dr. Zaman and colleagues called for more sex-specific research in cardiology, including risk factors related to premature menopause, preeclampsia, gestational diabetes, and autoimmune diseases such as systemic lupus.
Future studies should also explore the underlying mechanisms that may explain the links between the Mediterranean diet, cardiovascular disease, and death, the authors write. For instance, the diet may reduce inflammation and cardiovascular risk factors through antioxidant and beneficial gut microbiome pathways. Other components of the diet – such as polyphenols, nitrates, omega-3 fatty acids, higher fiber intake, and reduced glycemic load – may also play a role.
“It was striking to see how strong the long-term cardioprotective properties of a Mediterranean-type dietary pattern were,” said Samia Mora, MD, MHS, a professor of medicine at Harvard Medical School and director of the Center for Lipid Metabolomics at Brigham and Women’s Hospital.
Dr. Mora, who wasn’t involved with this study, has researched potential mechanisms related to the Mediterranean diet, cardiovascular events, and diabetes in women. She and colleagues have found that women with high adherence to the diet are more likely to have lower inflammation, insulin resistance, body mass index, and blood pressure, as well as improved lipid and metabolic profiles.
“This could represent an opportunity to intervene earlier and more intensively on improving inflammation, insulin resistance, and cardiometabolic health through evidence-based dietary approaches such as the Mediterranean diet,” she said. “As health care providers, we should promote the healthy dietary attributes of the Mediterranean diet, especially as many of our patients in the U.S. are less familiar with the Mediterranean diet and how to incorporate its components into daily food intake.”
The study did not receive any funding. Dr. Zaman was supported by a Heart Foundation Future Leader Fellowship. The authors declared no conflicts of interest. Dr. Mora reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Mediterranean diet appears to be associated with a lower incidence of cardiovascular disease (CVD) and mortality in women, new observational data suggest.
Those who had a higher adherence to a Mediterranean diet had a 24% lower risk for cardiovascular disease and 23% lower risk for death.
“A healthy diet is a huge factor in preventing heart disease. However, current guidelines on preventing heart disease lack sex-specific recommendations,” said senior author Sarah Zaman, MBBS, PhD, an associate professor of medicine and principal research fellow at the University of Sydney’s Westmead Applied Research Centre.
“Historically, research trials and studies have had predominantly male participants or lacked sex-specific analysis,” she said. “Our results will pave the way to bridge this gap and also highlight the need for more research to ensure health guidelines and policies include diverse perspectives.”
The study was published online in the journal Heart.
Analyzing cardiovascular outcomes
Dr. Zaman and colleagues conducted a systematic review and meta-analysis of 16 studies published between 2006 and 2021 that reported a Mediterranean diet score and included either all women or had stratified outcomes by sex. They excluded studies that referred to only certain components of the Mediterranean diet or combined it with other lifestyle-related factors.
The studies, which were mainly conducted in the United States and Europe, included 722,495 adult women without previous clinical or subclinical CVD, with a median follow-up of 12.5 years.
Higher Mediterranean diet adherence was defined as the highest category reporting the highest range of Mediterranean diet scores, and lower adherence was defined as the lowest category reporting lowest scores. Incident CVD included coronary heart disease, myocardial infarction, stroke, heart failure, cardiovascular death, major adverse cardiovascular events, major adverse cardiac cerebrovascular events, and patient-reported CVD.
Overall, higher adherence to a Mediterranean diet was associated with lower CVD incidence (hazard ratio, 0.76; 95% confidence interval, 0.72-0.81), total mortality (HR, 0.77; 95% CI, 0.74-0.80), and coronary heart disease (HR, 0.75; 95% CI, 0.65-0.87).
Stroke incidence was also lower among women who adhered to the Mediterranean diet, although it wasn’t considered statistically significant (HR, 0.87; 95% CI, 0.76-1.01).
Additional analyses found similar reductions in risk across women of different ethnicities. Higher Mediterranean diet adherence was associated with lower CVD incidence for both women of European descent (HR, 0.76; 95% CI, 0.59-0.98) and women of non-European descent – Asian, Native Hawaiian, and African American – (HR, 0.79; 95% CI, 0.72-0.87).
The results didn’t materially change in sensitivity analyses, the authors note. Excluding one study at a time, the pooled HRs for the highest versus the lowest Mediterranean diet adherence ranged from 0.76 (95% CI, 0.72-0.80) to 0.83 (95% CI, 0.70-0.98) for incident CVD and from 0.77 (95% CI, 0.75-0.80) to 0.77 (95% CI, 0.74-0.81) for total mortality among women.
At the same time, the authors pointed to several limitations, including the observational nature of all of the studies, the reliance on self-reported food frequency questionnaires, and heterogeneity in the adjustments for influential factors across the studies.
Additional considerations
Dr. Zaman and colleagues called for more sex-specific research in cardiology, including risk factors related to premature menopause, preeclampsia, gestational diabetes, and autoimmune diseases such as systemic lupus.
Future studies should also explore the underlying mechanisms that may explain the links between the Mediterranean diet, cardiovascular disease, and death, the authors write. For instance, the diet may reduce inflammation and cardiovascular risk factors through antioxidant and beneficial gut microbiome pathways. Other components of the diet – such as polyphenols, nitrates, omega-3 fatty acids, higher fiber intake, and reduced glycemic load – may also play a role.
“It was striking to see how strong the long-term cardioprotective properties of a Mediterranean-type dietary pattern were,” said Samia Mora, MD, MHS, a professor of medicine at Harvard Medical School and director of the Center for Lipid Metabolomics at Brigham and Women’s Hospital.
Dr. Mora, who wasn’t involved with this study, has researched potential mechanisms related to the Mediterranean diet, cardiovascular events, and diabetes in women. She and colleagues have found that women with high adherence to the diet are more likely to have lower inflammation, insulin resistance, body mass index, and blood pressure, as well as improved lipid and metabolic profiles.
“This could represent an opportunity to intervene earlier and more intensively on improving inflammation, insulin resistance, and cardiometabolic health through evidence-based dietary approaches such as the Mediterranean diet,” she said. “As health care providers, we should promote the healthy dietary attributes of the Mediterranean diet, especially as many of our patients in the U.S. are less familiar with the Mediterranean diet and how to incorporate its components into daily food intake.”
The study did not receive any funding. Dr. Zaman was supported by a Heart Foundation Future Leader Fellowship. The authors declared no conflicts of interest. Dr. Mora reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The Mediterranean diet appears to be associated with a lower incidence of cardiovascular disease (CVD) and mortality in women, new observational data suggest.
Those who had a higher adherence to a Mediterranean diet had a 24% lower risk for cardiovascular disease and 23% lower risk for death.
“A healthy diet is a huge factor in preventing heart disease. However, current guidelines on preventing heart disease lack sex-specific recommendations,” said senior author Sarah Zaman, MBBS, PhD, an associate professor of medicine and principal research fellow at the University of Sydney’s Westmead Applied Research Centre.
“Historically, research trials and studies have had predominantly male participants or lacked sex-specific analysis,” she said. “Our results will pave the way to bridge this gap and also highlight the need for more research to ensure health guidelines and policies include diverse perspectives.”
The study was published online in the journal Heart.
Analyzing cardiovascular outcomes
Dr. Zaman and colleagues conducted a systematic review and meta-analysis of 16 studies published between 2006 and 2021 that reported a Mediterranean diet score and included either all women or had stratified outcomes by sex. They excluded studies that referred to only certain components of the Mediterranean diet or combined it with other lifestyle-related factors.
The studies, which were mainly conducted in the United States and Europe, included 722,495 adult women without previous clinical or subclinical CVD, with a median follow-up of 12.5 years.
Higher Mediterranean diet adherence was defined as the highest category reporting the highest range of Mediterranean diet scores, and lower adherence was defined as the lowest category reporting lowest scores. Incident CVD included coronary heart disease, myocardial infarction, stroke, heart failure, cardiovascular death, major adverse cardiovascular events, major adverse cardiac cerebrovascular events, and patient-reported CVD.
Overall, higher adherence to a Mediterranean diet was associated with lower CVD incidence (hazard ratio, 0.76; 95% confidence interval, 0.72-0.81), total mortality (HR, 0.77; 95% CI, 0.74-0.80), and coronary heart disease (HR, 0.75; 95% CI, 0.65-0.87).
Stroke incidence was also lower among women who adhered to the Mediterranean diet, although it wasn’t considered statistically significant (HR, 0.87; 95% CI, 0.76-1.01).
Additional analyses found similar reductions in risk across women of different ethnicities. Higher Mediterranean diet adherence was associated with lower CVD incidence for both women of European descent (HR, 0.76; 95% CI, 0.59-0.98) and women of non-European descent – Asian, Native Hawaiian, and African American – (HR, 0.79; 95% CI, 0.72-0.87).
The results didn’t materially change in sensitivity analyses, the authors note. Excluding one study at a time, the pooled HRs for the highest versus the lowest Mediterranean diet adherence ranged from 0.76 (95% CI, 0.72-0.80) to 0.83 (95% CI, 0.70-0.98) for incident CVD and from 0.77 (95% CI, 0.75-0.80) to 0.77 (95% CI, 0.74-0.81) for total mortality among women.
At the same time, the authors pointed to several limitations, including the observational nature of all of the studies, the reliance on self-reported food frequency questionnaires, and heterogeneity in the adjustments for influential factors across the studies.
Additional considerations
Dr. Zaman and colleagues called for more sex-specific research in cardiology, including risk factors related to premature menopause, preeclampsia, gestational diabetes, and autoimmune diseases such as systemic lupus.
Future studies should also explore the underlying mechanisms that may explain the links between the Mediterranean diet, cardiovascular disease, and death, the authors write. For instance, the diet may reduce inflammation and cardiovascular risk factors through antioxidant and beneficial gut microbiome pathways. Other components of the diet – such as polyphenols, nitrates, omega-3 fatty acids, higher fiber intake, and reduced glycemic load – may also play a role.
“It was striking to see how strong the long-term cardioprotective properties of a Mediterranean-type dietary pattern were,” said Samia Mora, MD, MHS, a professor of medicine at Harvard Medical School and director of the Center for Lipid Metabolomics at Brigham and Women’s Hospital.
Dr. Mora, who wasn’t involved with this study, has researched potential mechanisms related to the Mediterranean diet, cardiovascular events, and diabetes in women. She and colleagues have found that women with high adherence to the diet are more likely to have lower inflammation, insulin resistance, body mass index, and blood pressure, as well as improved lipid and metabolic profiles.
“This could represent an opportunity to intervene earlier and more intensively on improving inflammation, insulin resistance, and cardiometabolic health through evidence-based dietary approaches such as the Mediterranean diet,” she said. “As health care providers, we should promote the healthy dietary attributes of the Mediterranean diet, especially as many of our patients in the U.S. are less familiar with the Mediterranean diet and how to incorporate its components into daily food intake.”
The study did not receive any funding. Dr. Zaman was supported by a Heart Foundation Future Leader Fellowship. The authors declared no conflicts of interest. Dr. Mora reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.











