News
Trials say start sacubitril-valsartan in hospital in HF with ‘below normal’ LVEF
- Author:
- Steve Stiles
The risk-reduction benefit reached 41% among the overwhelming majority of patients with a left ventricular ejection fraction.
News
Hopeful insights, no overall HFpEF gains from splanchnic nerve ablation: REBALANCE-HF
- Author:
- Steve Stiles
The trial’s potential-responder cohort “seemed able to augment cardiac output in response to stress” and to “maintain or augment their orthostatic...
News
Spreading out daily meals and snacks may boost heart failure survival
- Author:
- Steve Stiles
A daily eating window of 11 or more hours, compared with less than 11 hours, corresponded to a greater than 40% drop in risk for CV mortality over...
News

Semaglutide win in HFpEF with obesity regardless of ejection fraction: STEP-HFpEF
- Author:
- Steve Stiles
It remains unknown, however, “whether the improvement in health status, functional status, and reduced inflammation” will translate to reduced...
News
The how and why of quad therapy in reduced-EF heart failure
- Author:
- Steve Stiles
“Yet, when we look at their actual implementation in clinical practice, we’ve seen this slow and variable uptake.”
News
Second pig-heart transplant patient at UM faring well
- Author:
- Steve Stiles
“We’re taking one day at a time. His immune system is still intact, despite the heavy immune suppression.”
News
Heart societies ready to split from ABIM over long-standing MOC disputes
- Author:
- Steve Stiles
“Cardiology is a distinct medical specialty, and physicians want and deserve a clinical competency and continuous certification program that is...
News
Anxiety, depression ease after AFib ablation: Clinical or placebo effect?
- Author:
- Steve Stiles
The finding, say researchers, may point to an overlooked potential benefit of ablation that can be discussed with patients considering whether to...
News

Should intravascular imaging be almost routine in PCI?
- Author:
- Steve Stiles
“The challenge, though, will be convincing the average interventional cardiologist worldwide that it was specifically the imaging and not the...
News
Recent leaps in heart failure therapy spur ESC guideline–focused update
- Author:
- Steve Stiles
The new document gives a boost to recommendations for HF with mildly reduced ejection fraction characterized by an LVEF > 40% to < 50%.
News

Parity for prompt and staged STEMI complete revascularization: MULTISTARS-AMI
- Author:
- Steve Stiles
It appears to be the first trial of its kind to show that operators and patients can safely choose either PCI approach and attain similar outcomes...
News

Advanced HF no obstacle to AFib ablation success: CASTLE-HTx
- Author:
- Steve Stiles
One of the study’s key messages “is that AF ablation is safe and effective in patients with end-stage heart failure” and “should be part of our...
News
FIRE a win for physiology-guided MI complete revascularization in older patients
- Author:
- Steve Stiles
"This is the first trial actually showing a benefit" from physiology-guided CR in older patients with acute MI that is similar to what the...
News
ECMO for shock in acute MI won’t help, may harm: ECLS-SHOCK
- Author:
- Steve Stiles
Risks for moderate or severe bleeding more than doubled and serious peripheral vascular complications almost tripled with addition of ECMO support...
News
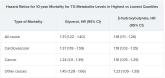
Triglyceride puzzle: Do TG metabolites better predict risk?
- Author:
- Steve Stiles
The results were “really, really surprising,” the study’s lead author said. They are “completely novel” and “may make people think differently”...
