User login
Less Invasive, Overlooked Option in Cardiac Surgery May Offer Benefit
Compared with traditional replacement valves, sutureless valves placed through minimally invasive cardiac surgery have less data supporting their use but offer unique features that might make them the preferred option for certain patients, reported specialists.
The sutureless device known as Perceval (Corcym) and a rapidly deployed device called Intuity (Edwards Lifesciences) are used as an alternative to surgical aortic valve replacement (SAVR) and transcatheter aortic valve replacement (TAVR). But despite being commercially available since 2016, the devices are still not being used much.
The devices are not discussed in substantial detail in either the joint guidelines from the American College of Cardiology and American Heart Association issued in 2020 or guidelines from the European Society of Cardiology issued in 2022.
Cristiano Spadaccio, MD, PhD, a cardiothoracic surgeon associated with Lancashire Cardiac Centre in Blackpool, England, and his colleagues reviewed the small number of studies evaluating the alternate approach to “make the cardiology world aware” of alternatives “that can relieve the surgical burden by minimizing the implantation time and length of the operation,” he said.
The comprehensive review is published in the Journal of the American College of Cardiology.
A Neglected Alternative
The sutureless Perceval device is held in place by a stent frame that self-expands. The Intuity device also relies primarily on its framework to anchor the valve in place but does involve three sutures. Both devices are still referred to as sutureless in the new review of them.
Only a small number of centers perform minimally invasive cardiac surgeries, and the main advantage of the devices — rapid deployment — has been eroded with the advent of automated knotting which has significantly reduced the time to implant and sutured valve.
The underuse of these devices is largely caused by the limited amount of comparative and prospective data, said Dr. Spadaccio. “The entire literature on sutureless aortic valve replacement with the exception of one randomized controlled trial is observational.”
That trial, PERSIST-AVR, found that the sutureless valves were just as good as conventional ones when it comes to major adverse cardiovascular events including all-cause death, myocardial infarction, stroke, or valve reintervention at 1 year.
In a subanalysis limited to patients who had isolated aortic valve replacement, the sutureless procedure was associated with lower adverse events (5.2% vs 10.8%) at the cost of a higher rate of pacemaker implantation (11% vs 1.6%).
There are also multiple retrospective studies and registries that have generated observational data comparing sutureless aortic valve replacement with SAVR and TAVR in various patient populations, said Dr. Spadaccio, and the review was based on more than a dozen studies published since 2015. Long-term follow-up data for sutureless aortic valve replacements, which now exceeds 10 years, suggest rates of structural valve deterioration and reintervention have been acceptably low.
The minimally invasive procedures have other advantages too. For example, relative to the greater trauma associated with open heart surgery, minimally invasive surgeries typically involve faster recovery, an advantage likely to appeal to many patients who are candidates for either.
Quicker Recovery
Collectively, these data suggest that sutureless aortic valve replacement might be a reasonable or even a more appropriate alternative to either SAVR or TAVR when considering specific patient characteristics and goals, according to the review, which included an algorithm identifying specifically where sutureless aortic valve replacement fits with SAVR and TAVR.
“The algorithm is based on different clinical scenarios and reflects current guidelines for SAVR,” said Dr. Spadaccio. For example, current guidelines identify SAVR as preferred in patients younger than 65 years and in older patients with a low Society of Thoracic Surgeons (STS) score, but there are many instances in which sutureless aortic valve replacement might be more attractive, such as in those also undergoing mitral valve repair, coronary artery bypass grafting, or another surgical procedure.
Dr. Spadaccio said that the STS score should not be considered in isolation when evaluating a patient for SAVR or TAVR. Other features such as mobility, frailty score, and comorbid liver or renal disease should also be considered when discussing the three options with patients. As a result, the algorithm emphasizes a detailed evaluation of patient characteristics in selecting one procedure over another.
“The treatment should be really tailored on the individual patient basis,” said Dr. Spadaccio.
Dr. Spadaccio acknowledged that there is a need for more comparative trials, particularly in regard to sutureless aortic valve replacement as an alternative to TAVR. “I really think that a 1:1 RCT on sutureless aortic valve replacement vs TAVR could give better answers to all of these interrogatives.”
But despite the limitations outlined in this review, Dr. Spadaccio and colleagues challenged the perception that current data are not sufficient to allow clinicians to consider sutureless aortic valve replacement in the mix of options.
A Viable Option
This comprehensive summary of what is known about sutureless aortic valve replacement compared with the other options addresses an important knowledge gap, said S. Chris Malaisrie, MD, a cardiac surgeon at Northwestern University Feinberg School of Medicine, Chicago, Illinois.
He said he agrees this option has unique qualities. “Minimally invasive surgery has been largely ignored by guideline writers, but patients certainly demand options that are less invasive than standard open heart surgery. Sutureless and rapid deployment valves facilitate minimally invasive surgery and offer an advantageous option for younger patients.”
Dr. Malaisrie said the review is generating discussion about a potentially valuable option within the cardiology community. And that is exactly what Dr. Spadaccio was hoping for. “This paper was meant to educate as much as possible on these details to assist and inform decision-making,” he said.
A version of this article first appeared on Medscape.com.
Compared with traditional replacement valves, sutureless valves placed through minimally invasive cardiac surgery have less data supporting their use but offer unique features that might make them the preferred option for certain patients, reported specialists.
The sutureless device known as Perceval (Corcym) and a rapidly deployed device called Intuity (Edwards Lifesciences) are used as an alternative to surgical aortic valve replacement (SAVR) and transcatheter aortic valve replacement (TAVR). But despite being commercially available since 2016, the devices are still not being used much.
The devices are not discussed in substantial detail in either the joint guidelines from the American College of Cardiology and American Heart Association issued in 2020 or guidelines from the European Society of Cardiology issued in 2022.
Cristiano Spadaccio, MD, PhD, a cardiothoracic surgeon associated with Lancashire Cardiac Centre in Blackpool, England, and his colleagues reviewed the small number of studies evaluating the alternate approach to “make the cardiology world aware” of alternatives “that can relieve the surgical burden by minimizing the implantation time and length of the operation,” he said.
The comprehensive review is published in the Journal of the American College of Cardiology.
A Neglected Alternative
The sutureless Perceval device is held in place by a stent frame that self-expands. The Intuity device also relies primarily on its framework to anchor the valve in place but does involve three sutures. Both devices are still referred to as sutureless in the new review of them.
Only a small number of centers perform minimally invasive cardiac surgeries, and the main advantage of the devices — rapid deployment — has been eroded with the advent of automated knotting which has significantly reduced the time to implant and sutured valve.
The underuse of these devices is largely caused by the limited amount of comparative and prospective data, said Dr. Spadaccio. “The entire literature on sutureless aortic valve replacement with the exception of one randomized controlled trial is observational.”
That trial, PERSIST-AVR, found that the sutureless valves were just as good as conventional ones when it comes to major adverse cardiovascular events including all-cause death, myocardial infarction, stroke, or valve reintervention at 1 year.
In a subanalysis limited to patients who had isolated aortic valve replacement, the sutureless procedure was associated with lower adverse events (5.2% vs 10.8%) at the cost of a higher rate of pacemaker implantation (11% vs 1.6%).
There are also multiple retrospective studies and registries that have generated observational data comparing sutureless aortic valve replacement with SAVR and TAVR in various patient populations, said Dr. Spadaccio, and the review was based on more than a dozen studies published since 2015. Long-term follow-up data for sutureless aortic valve replacements, which now exceeds 10 years, suggest rates of structural valve deterioration and reintervention have been acceptably low.
The minimally invasive procedures have other advantages too. For example, relative to the greater trauma associated with open heart surgery, minimally invasive surgeries typically involve faster recovery, an advantage likely to appeal to many patients who are candidates for either.
Quicker Recovery
Collectively, these data suggest that sutureless aortic valve replacement might be a reasonable or even a more appropriate alternative to either SAVR or TAVR when considering specific patient characteristics and goals, according to the review, which included an algorithm identifying specifically where sutureless aortic valve replacement fits with SAVR and TAVR.
“The algorithm is based on different clinical scenarios and reflects current guidelines for SAVR,” said Dr. Spadaccio. For example, current guidelines identify SAVR as preferred in patients younger than 65 years and in older patients with a low Society of Thoracic Surgeons (STS) score, but there are many instances in which sutureless aortic valve replacement might be more attractive, such as in those also undergoing mitral valve repair, coronary artery bypass grafting, or another surgical procedure.
Dr. Spadaccio said that the STS score should not be considered in isolation when evaluating a patient for SAVR or TAVR. Other features such as mobility, frailty score, and comorbid liver or renal disease should also be considered when discussing the three options with patients. As a result, the algorithm emphasizes a detailed evaluation of patient characteristics in selecting one procedure over another.
“The treatment should be really tailored on the individual patient basis,” said Dr. Spadaccio.
Dr. Spadaccio acknowledged that there is a need for more comparative trials, particularly in regard to sutureless aortic valve replacement as an alternative to TAVR. “I really think that a 1:1 RCT on sutureless aortic valve replacement vs TAVR could give better answers to all of these interrogatives.”
But despite the limitations outlined in this review, Dr. Spadaccio and colleagues challenged the perception that current data are not sufficient to allow clinicians to consider sutureless aortic valve replacement in the mix of options.
A Viable Option
This comprehensive summary of what is known about sutureless aortic valve replacement compared with the other options addresses an important knowledge gap, said S. Chris Malaisrie, MD, a cardiac surgeon at Northwestern University Feinberg School of Medicine, Chicago, Illinois.
He said he agrees this option has unique qualities. “Minimally invasive surgery has been largely ignored by guideline writers, but patients certainly demand options that are less invasive than standard open heart surgery. Sutureless and rapid deployment valves facilitate minimally invasive surgery and offer an advantageous option for younger patients.”
Dr. Malaisrie said the review is generating discussion about a potentially valuable option within the cardiology community. And that is exactly what Dr. Spadaccio was hoping for. “This paper was meant to educate as much as possible on these details to assist and inform decision-making,” he said.
A version of this article first appeared on Medscape.com.
Compared with traditional replacement valves, sutureless valves placed through minimally invasive cardiac surgery have less data supporting their use but offer unique features that might make them the preferred option for certain patients, reported specialists.
The sutureless device known as Perceval (Corcym) and a rapidly deployed device called Intuity (Edwards Lifesciences) are used as an alternative to surgical aortic valve replacement (SAVR) and transcatheter aortic valve replacement (TAVR). But despite being commercially available since 2016, the devices are still not being used much.
The devices are not discussed in substantial detail in either the joint guidelines from the American College of Cardiology and American Heart Association issued in 2020 or guidelines from the European Society of Cardiology issued in 2022.
Cristiano Spadaccio, MD, PhD, a cardiothoracic surgeon associated with Lancashire Cardiac Centre in Blackpool, England, and his colleagues reviewed the small number of studies evaluating the alternate approach to “make the cardiology world aware” of alternatives “that can relieve the surgical burden by minimizing the implantation time and length of the operation,” he said.
The comprehensive review is published in the Journal of the American College of Cardiology.
A Neglected Alternative
The sutureless Perceval device is held in place by a stent frame that self-expands. The Intuity device also relies primarily on its framework to anchor the valve in place but does involve three sutures. Both devices are still referred to as sutureless in the new review of them.
Only a small number of centers perform minimally invasive cardiac surgeries, and the main advantage of the devices — rapid deployment — has been eroded with the advent of automated knotting which has significantly reduced the time to implant and sutured valve.
The underuse of these devices is largely caused by the limited amount of comparative and prospective data, said Dr. Spadaccio. “The entire literature on sutureless aortic valve replacement with the exception of one randomized controlled trial is observational.”
That trial, PERSIST-AVR, found that the sutureless valves were just as good as conventional ones when it comes to major adverse cardiovascular events including all-cause death, myocardial infarction, stroke, or valve reintervention at 1 year.
In a subanalysis limited to patients who had isolated aortic valve replacement, the sutureless procedure was associated with lower adverse events (5.2% vs 10.8%) at the cost of a higher rate of pacemaker implantation (11% vs 1.6%).
There are also multiple retrospective studies and registries that have generated observational data comparing sutureless aortic valve replacement with SAVR and TAVR in various patient populations, said Dr. Spadaccio, and the review was based on more than a dozen studies published since 2015. Long-term follow-up data for sutureless aortic valve replacements, which now exceeds 10 years, suggest rates of structural valve deterioration and reintervention have been acceptably low.
The minimally invasive procedures have other advantages too. For example, relative to the greater trauma associated with open heart surgery, minimally invasive surgeries typically involve faster recovery, an advantage likely to appeal to many patients who are candidates for either.
Quicker Recovery
Collectively, these data suggest that sutureless aortic valve replacement might be a reasonable or even a more appropriate alternative to either SAVR or TAVR when considering specific patient characteristics and goals, according to the review, which included an algorithm identifying specifically where sutureless aortic valve replacement fits with SAVR and TAVR.
“The algorithm is based on different clinical scenarios and reflects current guidelines for SAVR,” said Dr. Spadaccio. For example, current guidelines identify SAVR as preferred in patients younger than 65 years and in older patients with a low Society of Thoracic Surgeons (STS) score, but there are many instances in which sutureless aortic valve replacement might be more attractive, such as in those also undergoing mitral valve repair, coronary artery bypass grafting, or another surgical procedure.
Dr. Spadaccio said that the STS score should not be considered in isolation when evaluating a patient for SAVR or TAVR. Other features such as mobility, frailty score, and comorbid liver or renal disease should also be considered when discussing the three options with patients. As a result, the algorithm emphasizes a detailed evaluation of patient characteristics in selecting one procedure over another.
“The treatment should be really tailored on the individual patient basis,” said Dr. Spadaccio.
Dr. Spadaccio acknowledged that there is a need for more comparative trials, particularly in regard to sutureless aortic valve replacement as an alternative to TAVR. “I really think that a 1:1 RCT on sutureless aortic valve replacement vs TAVR could give better answers to all of these interrogatives.”
But despite the limitations outlined in this review, Dr. Spadaccio and colleagues challenged the perception that current data are not sufficient to allow clinicians to consider sutureless aortic valve replacement in the mix of options.
A Viable Option
This comprehensive summary of what is known about sutureless aortic valve replacement compared with the other options addresses an important knowledge gap, said S. Chris Malaisrie, MD, a cardiac surgeon at Northwestern University Feinberg School of Medicine, Chicago, Illinois.
He said he agrees this option has unique qualities. “Minimally invasive surgery has been largely ignored by guideline writers, but patients certainly demand options that are less invasive than standard open heart surgery. Sutureless and rapid deployment valves facilitate minimally invasive surgery and offer an advantageous option for younger patients.”
Dr. Malaisrie said the review is generating discussion about a potentially valuable option within the cardiology community. And that is exactly what Dr. Spadaccio was hoping for. “This paper was meant to educate as much as possible on these details to assist and inform decision-making,” he said.
A version of this article first appeared on Medscape.com.
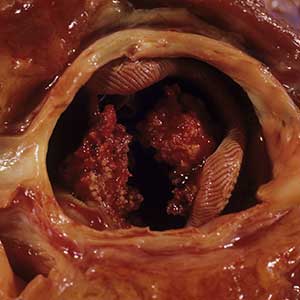
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
A step forward in diabetic foot disease management
As we navigate the ever-evolving landscape of diabetic foot disease management, The goal is to create a common language of risk that is easily related from clinician to clinician to patient.
Whatever language we use, though, the problem we face is vast:
- Diabetic foot ulcers affect approximately 18.6 million people worldwide and 1.6 million in the United States each year.
- They are associated with high rates of premature death, with a 5-year mortality rate of 30%. This rate is greater than 70% for those with above-foot amputations, worse than all but the most aggressive cancers.
- The direct costs of treating diabetic foot ulcers in the United States is estimated at $9 billion-$13 billion annually.
- Over 550 million people worldwide have diabetes, with 18.6 million developing foot ulcers annually. Up to 34% of those with diabetes will develop a foot ulcer.
- About 20% of those with a diabetic foot ulcer will undergo amputation, a major cause of which is infection, which affects 50% of foot ulcers.
- Up to 20% of those with a foot ulcer require hospitalization, with 15%-20% undergoing amputation. Inequities exist in diabetes-related foot complications:
- –Rates of major amputation are higher in non-Hispanic Black, Hispanic, and Native American populations, compared with non-Hispanic White populations.
- –Non-Hispanic Black and Hispanic populations present with more advanced ulcers and peripheral artery disease, and are more likely to undergo amputation without revascularization attempt.
The IWGDF, a multidisciplinary team of international experts, has recently updated its guidelines. This team, comprising endocrinologists, internal medicine physicians, physiatrists, podiatrists, and vascular surgeons from across the globe, has worked tirelessly to provide us with a comprehensive guide to managing diabetes-related foot ulcers.
The updated guidelines address five critical clinical questions, each with up to 13 important outcomes. The systematic review that underpins these guidelines identified 149 eligible studies, assessing 28 different systems. This exhaustive research has led to the development of seven key recommendations that address the clinical questions and consider the existence of different clinical settings.
One of the significant updates in the 2023 guidelines is the recommendation of SINBAD – site, ischemia, neuropathy, bacterial infection, area, and depth – as the priority wound classification system for people with diabetes and a foot ulcer. This system is particularly useful for interprofessional communication, describing each composite variable, and conducting clinical audits using the full score. However, the guidelines also recommend the use of other, more specific assessment systems for infection and peripheral artery disease from the Infectious Diseases Society of America/IWGDF when resources and an appropriate level of expertise exist.
The introduction of the Wound, Ischemia and Foot Infection (WIfI) classification system in the guidelines is also a noteworthy development. This system is crucial in assessing perfusion and the likely benefit of revascularization in a person with diabetes and a foot ulcer. By assessing the level of wound ischemia and infection, we can make informed decisions about the need for vascular intervention, which can significantly affect the patient’s outcome. This can be done simply by classifying each of the three categories of wound, ischemia, or foot infection as none, mild, moderate, or severe. By simplifying the very dynamic comorbidities of tissue loss, ischemia, and infection into a usable and predictive scale, it helps us to communicate risk across disciplines. This has been found to be highly predictive of healing, amputation, and mortality.
We use WIfI every day across our system. An example might include a patient we recently treated:
A 76-year-old woman presented with a wound to her left foot. Her past medical history revealed type 2 diabetes, peripheral neuropathy, and documented peripheral artery disease with prior bilateral femoral-popliteal bypass conducted at an external facility. In addition to gangrenous changes to her fourth toe, she displayed erythema and lymphangitic streaking up her dorsal foot. While she was afebrile, her white cell count was 13,000/mcL. Radiographic examinations did not show signs of osteomyelitis. Noninvasive vascular evaluations revealed an ankle brachial index of 0.4 and a toe pressure of 10 mm Hg. An aortogram with a lower-extremity runoff arteriogram confirmed the obstruction of her left femoral-popliteal bypass.
Taking these results into account, her WIfI score was determined as: wound 2 (moderate), ischemia 3 (severe), foot infection 2 (moderate, no sepsis), translating to a clinical stage 4. This denotes a high risk for major amputation.
Following a team discussion, she was taken to the operating room for an initial debridement of her infection which consisted of a partial fourth ray resection to the level of the mid-metatarsal. Following control of the infection, she received a vascular assessment which ultimately constituted a femoral to distal anterior tibial bypass. Following both of these, she was discharged on a negative-pressure wound therapy device, receiving a split-thickness skin graft 4 weeks later.
The guidelines also emphasize the need for specific training, skills, and experience to ensure the accuracy of the recommended systems for characterizing foot ulcers. The person applying these systems should be appropriately trained and, according to their national or regional standards, should have the knowledge, expertise, and skills necessary to manage people with a diabetes-related foot ulcer.
As we continue to navigate the complexities of diabetes-related foot disease, these guidelines serve as a valuable compass, guiding our decisions and actions. They remind us of the importance of continuous learning, collaboration, and the application of evidence-based practice in our work.
I encourage you to delve into these guidelines. Let’s use them to improve our practice, enhance our communication, and, ultimately, provide better care for our patients.
Dr. Armstrong is professor of surgery, director of limb preservation, University of Southern California, Los Angeles. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
As we navigate the ever-evolving landscape of diabetic foot disease management, The goal is to create a common language of risk that is easily related from clinician to clinician to patient.
Whatever language we use, though, the problem we face is vast:
- Diabetic foot ulcers affect approximately 18.6 million people worldwide and 1.6 million in the United States each year.
- They are associated with high rates of premature death, with a 5-year mortality rate of 30%. This rate is greater than 70% for those with above-foot amputations, worse than all but the most aggressive cancers.
- The direct costs of treating diabetic foot ulcers in the United States is estimated at $9 billion-$13 billion annually.
- Over 550 million people worldwide have diabetes, with 18.6 million developing foot ulcers annually. Up to 34% of those with diabetes will develop a foot ulcer.
- About 20% of those with a diabetic foot ulcer will undergo amputation, a major cause of which is infection, which affects 50% of foot ulcers.
- Up to 20% of those with a foot ulcer require hospitalization, with 15%-20% undergoing amputation. Inequities exist in diabetes-related foot complications:
- –Rates of major amputation are higher in non-Hispanic Black, Hispanic, and Native American populations, compared with non-Hispanic White populations.
- –Non-Hispanic Black and Hispanic populations present with more advanced ulcers and peripheral artery disease, and are more likely to undergo amputation without revascularization attempt.
The IWGDF, a multidisciplinary team of international experts, has recently updated its guidelines. This team, comprising endocrinologists, internal medicine physicians, physiatrists, podiatrists, and vascular surgeons from across the globe, has worked tirelessly to provide us with a comprehensive guide to managing diabetes-related foot ulcers.
The updated guidelines address five critical clinical questions, each with up to 13 important outcomes. The systematic review that underpins these guidelines identified 149 eligible studies, assessing 28 different systems. This exhaustive research has led to the development of seven key recommendations that address the clinical questions and consider the existence of different clinical settings.
One of the significant updates in the 2023 guidelines is the recommendation of SINBAD – site, ischemia, neuropathy, bacterial infection, area, and depth – as the priority wound classification system for people with diabetes and a foot ulcer. This system is particularly useful for interprofessional communication, describing each composite variable, and conducting clinical audits using the full score. However, the guidelines also recommend the use of other, more specific assessment systems for infection and peripheral artery disease from the Infectious Diseases Society of America/IWGDF when resources and an appropriate level of expertise exist.
The introduction of the Wound, Ischemia and Foot Infection (WIfI) classification system in the guidelines is also a noteworthy development. This system is crucial in assessing perfusion and the likely benefit of revascularization in a person with diabetes and a foot ulcer. By assessing the level of wound ischemia and infection, we can make informed decisions about the need for vascular intervention, which can significantly affect the patient’s outcome. This can be done simply by classifying each of the three categories of wound, ischemia, or foot infection as none, mild, moderate, or severe. By simplifying the very dynamic comorbidities of tissue loss, ischemia, and infection into a usable and predictive scale, it helps us to communicate risk across disciplines. This has been found to be highly predictive of healing, amputation, and mortality.
We use WIfI every day across our system. An example might include a patient we recently treated:
A 76-year-old woman presented with a wound to her left foot. Her past medical history revealed type 2 diabetes, peripheral neuropathy, and documented peripheral artery disease with prior bilateral femoral-popliteal bypass conducted at an external facility. In addition to gangrenous changes to her fourth toe, she displayed erythema and lymphangitic streaking up her dorsal foot. While she was afebrile, her white cell count was 13,000/mcL. Radiographic examinations did not show signs of osteomyelitis. Noninvasive vascular evaluations revealed an ankle brachial index of 0.4 and a toe pressure of 10 mm Hg. An aortogram with a lower-extremity runoff arteriogram confirmed the obstruction of her left femoral-popliteal bypass.
Taking these results into account, her WIfI score was determined as: wound 2 (moderate), ischemia 3 (severe), foot infection 2 (moderate, no sepsis), translating to a clinical stage 4. This denotes a high risk for major amputation.
Following a team discussion, she was taken to the operating room for an initial debridement of her infection which consisted of a partial fourth ray resection to the level of the mid-metatarsal. Following control of the infection, she received a vascular assessment which ultimately constituted a femoral to distal anterior tibial bypass. Following both of these, she was discharged on a negative-pressure wound therapy device, receiving a split-thickness skin graft 4 weeks later.
The guidelines also emphasize the need for specific training, skills, and experience to ensure the accuracy of the recommended systems for characterizing foot ulcers. The person applying these systems should be appropriately trained and, according to their national or regional standards, should have the knowledge, expertise, and skills necessary to manage people with a diabetes-related foot ulcer.
As we continue to navigate the complexities of diabetes-related foot disease, these guidelines serve as a valuable compass, guiding our decisions and actions. They remind us of the importance of continuous learning, collaboration, and the application of evidence-based practice in our work.
I encourage you to delve into these guidelines. Let’s use them to improve our practice, enhance our communication, and, ultimately, provide better care for our patients.
Dr. Armstrong is professor of surgery, director of limb preservation, University of Southern California, Los Angeles. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
As we navigate the ever-evolving landscape of diabetic foot disease management, The goal is to create a common language of risk that is easily related from clinician to clinician to patient.
Whatever language we use, though, the problem we face is vast:
- Diabetic foot ulcers affect approximately 18.6 million people worldwide and 1.6 million in the United States each year.
- They are associated with high rates of premature death, with a 5-year mortality rate of 30%. This rate is greater than 70% for those with above-foot amputations, worse than all but the most aggressive cancers.
- The direct costs of treating diabetic foot ulcers in the United States is estimated at $9 billion-$13 billion annually.
- Over 550 million people worldwide have diabetes, with 18.6 million developing foot ulcers annually. Up to 34% of those with diabetes will develop a foot ulcer.
- About 20% of those with a diabetic foot ulcer will undergo amputation, a major cause of which is infection, which affects 50% of foot ulcers.
- Up to 20% of those with a foot ulcer require hospitalization, with 15%-20% undergoing amputation. Inequities exist in diabetes-related foot complications:
- –Rates of major amputation are higher in non-Hispanic Black, Hispanic, and Native American populations, compared with non-Hispanic White populations.
- –Non-Hispanic Black and Hispanic populations present with more advanced ulcers and peripheral artery disease, and are more likely to undergo amputation without revascularization attempt.
The IWGDF, a multidisciplinary team of international experts, has recently updated its guidelines. This team, comprising endocrinologists, internal medicine physicians, physiatrists, podiatrists, and vascular surgeons from across the globe, has worked tirelessly to provide us with a comprehensive guide to managing diabetes-related foot ulcers.
The updated guidelines address five critical clinical questions, each with up to 13 important outcomes. The systematic review that underpins these guidelines identified 149 eligible studies, assessing 28 different systems. This exhaustive research has led to the development of seven key recommendations that address the clinical questions and consider the existence of different clinical settings.
One of the significant updates in the 2023 guidelines is the recommendation of SINBAD – site, ischemia, neuropathy, bacterial infection, area, and depth – as the priority wound classification system for people with diabetes and a foot ulcer. This system is particularly useful for interprofessional communication, describing each composite variable, and conducting clinical audits using the full score. However, the guidelines also recommend the use of other, more specific assessment systems for infection and peripheral artery disease from the Infectious Diseases Society of America/IWGDF when resources and an appropriate level of expertise exist.
The introduction of the Wound, Ischemia and Foot Infection (WIfI) classification system in the guidelines is also a noteworthy development. This system is crucial in assessing perfusion and the likely benefit of revascularization in a person with diabetes and a foot ulcer. By assessing the level of wound ischemia and infection, we can make informed decisions about the need for vascular intervention, which can significantly affect the patient’s outcome. This can be done simply by classifying each of the three categories of wound, ischemia, or foot infection as none, mild, moderate, or severe. By simplifying the very dynamic comorbidities of tissue loss, ischemia, and infection into a usable and predictive scale, it helps us to communicate risk across disciplines. This has been found to be highly predictive of healing, amputation, and mortality.
We use WIfI every day across our system. An example might include a patient we recently treated:
A 76-year-old woman presented with a wound to her left foot. Her past medical history revealed type 2 diabetes, peripheral neuropathy, and documented peripheral artery disease with prior bilateral femoral-popliteal bypass conducted at an external facility. In addition to gangrenous changes to her fourth toe, she displayed erythema and lymphangitic streaking up her dorsal foot. While she was afebrile, her white cell count was 13,000/mcL. Radiographic examinations did not show signs of osteomyelitis. Noninvasive vascular evaluations revealed an ankle brachial index of 0.4 and a toe pressure of 10 mm Hg. An aortogram with a lower-extremity runoff arteriogram confirmed the obstruction of her left femoral-popliteal bypass.
Taking these results into account, her WIfI score was determined as: wound 2 (moderate), ischemia 3 (severe), foot infection 2 (moderate, no sepsis), translating to a clinical stage 4. This denotes a high risk for major amputation.
Following a team discussion, she was taken to the operating room for an initial debridement of her infection which consisted of a partial fourth ray resection to the level of the mid-metatarsal. Following control of the infection, she received a vascular assessment which ultimately constituted a femoral to distal anterior tibial bypass. Following both of these, she was discharged on a negative-pressure wound therapy device, receiving a split-thickness skin graft 4 weeks later.
The guidelines also emphasize the need for specific training, skills, and experience to ensure the accuracy of the recommended systems for characterizing foot ulcers. The person applying these systems should be appropriately trained and, according to their national or regional standards, should have the knowledge, expertise, and skills necessary to manage people with a diabetes-related foot ulcer.
As we continue to navigate the complexities of diabetes-related foot disease, these guidelines serve as a valuable compass, guiding our decisions and actions. They remind us of the importance of continuous learning, collaboration, and the application of evidence-based practice in our work.
I encourage you to delve into these guidelines. Let’s use them to improve our practice, enhance our communication, and, ultimately, provide better care for our patients.
Dr. Armstrong is professor of surgery, director of limb preservation, University of Southern California, Los Angeles. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
U.S. News ranks top cardiology, heart surgery hospitals
In the magazine’s 2023-2024 list, Cedars-Sinai Medical Center, Los Angeles, takes over the No. 2 spot from Mayo Clinic, Rochester, Minn., which dropped to No. 3. Cedars-Sinai held the No. 3 on the 2022-2023 rankings.
Mount Sinai Hospital in New York City holds the No. 4 spot in 2023-2024, up from No. 6; NYU Langone Hospitals, New York, continue to hold the No. 5 spot.
New York–Presbyterian Hospital–Columbia and Cornell in New York City is No. 6, down from No. 4 i.
Northwestern Medicine-Northwestern Memorial Hospital in Chicago takes over the No. 7 spot (up from No. 8), while Massachusetts General Hospital in Boston holds the No. 8 (down from No. 7).
Stanford (Calif.) Health Care–Stanford Hospital holds the No. 9 spot, the same as 2, and Lenox Hill Hospital at Northwell Health in New York is No. 10 on the list.
U.S. News evaluated 779 hospitals and ranked the top 50 that care for patients with challenging heart and vascular cases, including heart transplants; implantation of cardiac devices, such as pacemakers and defibrillators; major chest procedures and patients with cardiovascular disease and other complex conditions, such as endocarditis; and heart failure and circulatory issues.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Best hospitals overall honor roll
In 2023-2024, as in prior years, U.S. News also recognized Honor Roll hospitals that have excelled across multiple areas of care. However, in 2023-2024, for the first time, there is no ordinal ranking of hospitals making honor roll.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate their website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the Honor Roll hospitals have attained the highest standard of care in the nation,” the letter reads.
With the new format, honor roll hospitals are listed in alphabetical order. In 2023-2024, there are 22.
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania–Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York
- New York–Presbyterian Hospital–Columbia and Cornell
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla (Calif.) and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health, Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
According to U.S. News, to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles on the U.S. News website feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
In the magazine’s 2023-2024 list, Cedars-Sinai Medical Center, Los Angeles, takes over the No. 2 spot from Mayo Clinic, Rochester, Minn., which dropped to No. 3. Cedars-Sinai held the No. 3 on the 2022-2023 rankings.
Mount Sinai Hospital in New York City holds the No. 4 spot in 2023-2024, up from No. 6; NYU Langone Hospitals, New York, continue to hold the No. 5 spot.
New York–Presbyterian Hospital–Columbia and Cornell in New York City is No. 6, down from No. 4 i.
Northwestern Medicine-Northwestern Memorial Hospital in Chicago takes over the No. 7 spot (up from No. 8), while Massachusetts General Hospital in Boston holds the No. 8 (down from No. 7).
Stanford (Calif.) Health Care–Stanford Hospital holds the No. 9 spot, the same as 2, and Lenox Hill Hospital at Northwell Health in New York is No. 10 on the list.
U.S. News evaluated 779 hospitals and ranked the top 50 that care for patients with challenging heart and vascular cases, including heart transplants; implantation of cardiac devices, such as pacemakers and defibrillators; major chest procedures and patients with cardiovascular disease and other complex conditions, such as endocarditis; and heart failure and circulatory issues.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Best hospitals overall honor roll
In 2023-2024, as in prior years, U.S. News also recognized Honor Roll hospitals that have excelled across multiple areas of care. However, in 2023-2024, for the first time, there is no ordinal ranking of hospitals making honor roll.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate their website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the Honor Roll hospitals have attained the highest standard of care in the nation,” the letter reads.
With the new format, honor roll hospitals are listed in alphabetical order. In 2023-2024, there are 22.
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania–Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York
- New York–Presbyterian Hospital–Columbia and Cornell
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla (Calif.) and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health, Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
According to U.S. News, to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles on the U.S. News website feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
In the magazine’s 2023-2024 list, Cedars-Sinai Medical Center, Los Angeles, takes over the No. 2 spot from Mayo Clinic, Rochester, Minn., which dropped to No. 3. Cedars-Sinai held the No. 3 on the 2022-2023 rankings.
Mount Sinai Hospital in New York City holds the No. 4 spot in 2023-2024, up from No. 6; NYU Langone Hospitals, New York, continue to hold the No. 5 spot.
New York–Presbyterian Hospital–Columbia and Cornell in New York City is No. 6, down from No. 4 i.
Northwestern Medicine-Northwestern Memorial Hospital in Chicago takes over the No. 7 spot (up from No. 8), while Massachusetts General Hospital in Boston holds the No. 8 (down from No. 7).
Stanford (Calif.) Health Care–Stanford Hospital holds the No. 9 spot, the same as 2, and Lenox Hill Hospital at Northwell Health in New York is No. 10 on the list.
U.S. News evaluated 779 hospitals and ranked the top 50 that care for patients with challenging heart and vascular cases, including heart transplants; implantation of cardiac devices, such as pacemakers and defibrillators; major chest procedures and patients with cardiovascular disease and other complex conditions, such as endocarditis; and heart failure and circulatory issues.
“Consumers want useful resources to help them assess which hospital can best meet their specific care needs,” Ben Harder, chief of health analysis and managing editor at U.S. News, said in a statement.
“The 2023-2024 Best Hospitals rankings offer patients and the physicians with whom they consult a data-driven source for comparing performance in outcomes, patient satisfaction, and other metrics that matter to them,” Mr. Harder said.
Best hospitals overall honor roll
In 2023-2024, as in prior years, U.S. News also recognized Honor Roll hospitals that have excelled across multiple areas of care. However, in 2023-2024, for the first time, there is no ordinal ranking of hospitals making honor roll.
In a letter to hospital leaders, U.S. News explained that the major change in format came after months of deliberation, feedback from health care organizations and professionals, and an analysis of how consumers navigate their website.
Ordinal ranking of hospitals that make the honor roll “obscures the fact that all of the Honor Roll hospitals have attained the highest standard of care in the nation,” the letter reads.
With the new format, honor roll hospitals are listed in alphabetical order. In 2023-2024, there are 22.
- Barnes-Jewish Hospital, St. Louis
- Brigham and Women’s Hospital, Boston
- Cedars-Sinai Medical Center, Los Angeles
- Cleveland Clinic
- Hospitals of the University of Pennsylvania–Penn Medicine, Philadelphia
- Houston Methodist Hospital
- Johns Hopkins Hospital, Baltimore
- Massachusetts General Hospital, Boston
- Mayo Clinic, Rochester, Minn.
- Mount Sinai Hospital, New York
- New York–Presbyterian Hospital–Columbia and Cornell
- North Shore University Hospital at Northwell Health, Manhasset, N.Y.
- Northwestern Memorial Hospital, Chicago
- NYU Langone Hospitals, New York
- Rush University Medical Center, Chicago
- Stanford (Calif.) Health Care–Stanford Hospital
- UC San Diego Health–La Jolla (Calif.) and Hillcrest Hospitals
- UCLA Medical Center, Los Angeles
- UCSF Health–UCSF Medical Center, San Francisco
- University of Michigan Health, Ann Arbor
- UT Southwestern Medical Center, Dallas
- Vanderbilt University Medical Center, Nashville, Tenn.
According to U.S. News, to keep pace with consumers’ needs and the ever-evolving landscape of health care, “several refinements” are reflected in the latest best hospitals rankings.
These include the introduction of outpatient outcomes in key specialty rankings and surgical ratings, the expanded inclusion of other outpatient data, an increased weight on objective quality measures, and a reduced weight on expert opinion.
In addition, hospital profiles on the U.S. News website feature refined health equity measures, including a new measure of racial disparities in outcomes.
The full report for best hospitals, best specialty hospitals, and methodology is available online.
A version of this article first appeared on Medscape.com.
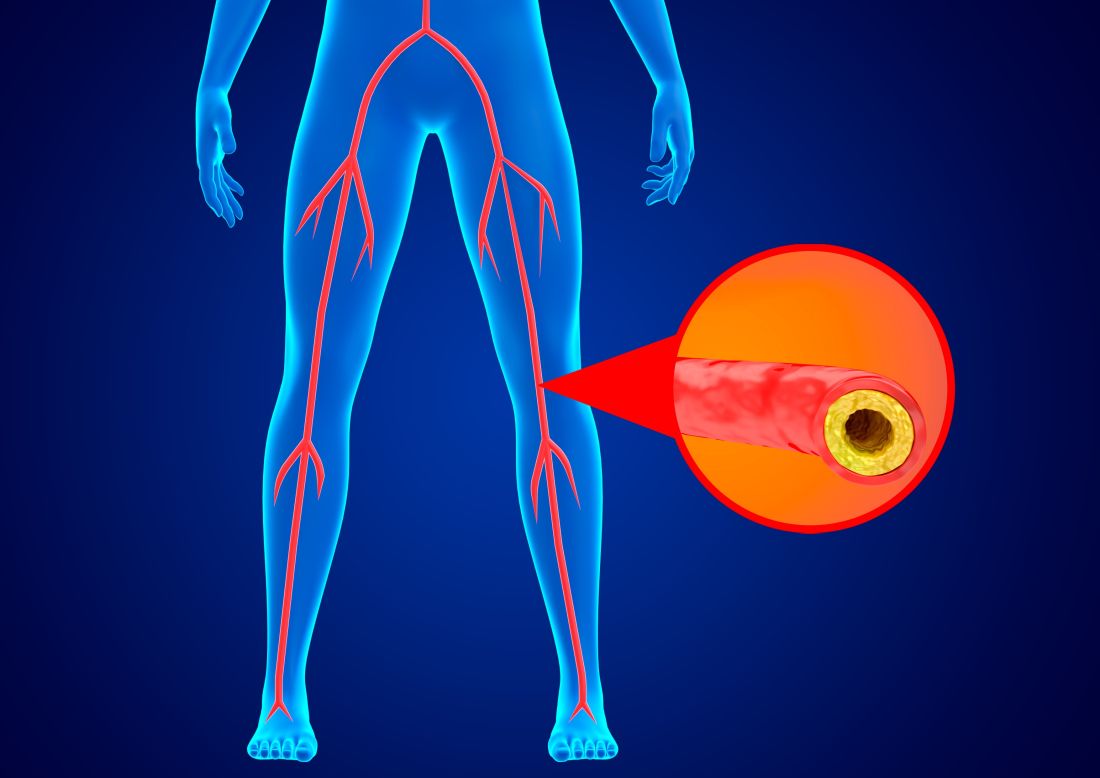
PAD procedure overuse: A field in peril or ‘a few bad apples’?
On May 24, the news outlet ProPublica published a scathing investigation of Jeffery Dormu, DO, said to have performed hundreds of “medically unnecessary and invasive vascular procedures” in his Laurel, Md. office, putting patients’ limbs and lives at risk.
On July 15, The New York Times published a broader-based investigation of several vascular specialists said to have performed “risky” procedures on patients with peripheral artery disease (PAD) who subsequently had to have amputations, or died. The focus was mainly on Michigan-based interventional cardiologist Jihad Mustapha, MD.
This follows a 2019 analysis of Medicare claims data that identified outlier physicians with a high early intervention rate for patients newly diagnosed with claudication. According to the American Heart Association statistics, PAD affects approximately 8.5 million U.S. adults age 40 and older (some claim that’s an underestimate); most cases don’t require invasive treatment.
Responding to the Times’ revelations, Joseph L. Mills, MD, president of the Society for Vascular Surgery, wrote on the society’s website: “The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology are providing high-quality, evidence-based care with safety and the best patient outcomes in mind.
“This is a complex issue that requires the examination not only of the events detailed in this story ... but of the underlying health care economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.”
‘A few bad apples’
“I think it’s a case of a few bad apples,” Sunil V. Rao, MD, director of interventional cardiology at NYU Langone Health, New York, said in an interview. “In general, I think physicians who take care of patients with vascular issues are trying to do the right thing. I think all of us who take care of patients with vascular disease see patients who are very, very complex, and there are going to be some procedures that have complications.
“Without knowing the clinical details, it’s hard to know whether the procedures described in the articles were overuse or unnecessary, or exactly what led to the amputations,” he said. “All we know is that these physicians are outliers in terms of the number of procedures they were billing for.
“But although correlation is not causation, it certainly is cause for concern because you would expect that the use of procedures for specific indications would fall within a certain range,” he added.
Lifestyle changes first
PAD is often asymptomatic or mild, making it difficult to diagnose. Revascularization procedures usually are reserved for the 5%-8% of patients at risk for chronic limb-threatening ischemia (CLTI) or those in whom the cornerstones of PAD treatment – lifestyle changes and, if needed, medication – fail.
Revascularization options include balloon angioplasty or stent placement; atherectomy to remove plaques from the artery; or bypass surgery if a long portion of a leg artery is completely blocked. All carry a risk of long-term adverse outcomes, but the rates are highest for atherectomy.
Lifestyle changes include regular exercise, following a healthy diet, quitting smoking, and controlling diabetes and high blood pressure. When PAD continues or progresses despite these modifications, medications such as antiplatelet agents, antihypertensives, and/or lipid-lowering drugs may be prescribed.
‘Medically unnecessary’
According to the latest American Heart Association/American College of Cardiology guideline on managing patients with lower-extremity PAD, patients should be selected for revascularization based on symptom severity.
Factors to consider include a significant disability as assessed by the patient, and adequacy of response to medical and structured exercise therapy.
There’s the rub regarding the clinicians investigated in the Times and ProPublica. Many patients, apparently, were not encouraged to make lifestyle changes, nor did they receive medication. Instead, they were advised from the get-go to undergo invasive procedures, and often multiple times. Underuse of prevention and lifestyle counseling n the management of PAD has long been a concern.
Furthermore, in at least some cases, patients without any symptoms were encouraged to be screened for blockages that were then treated invasively, according to the Times.
Dr. Dormu, as highlighted in ProPublica, positioned his practice as “life and limb saving.” Yet, in investigative findings that led to a suspension of Dr. Dormu’s license to practice medicine in Maryland, peer reviewers expressed concern regarding his repeated use of invasive and medically unnecessary procedures, exposing patients to “potential risks such as bleeding, infection, blood vessel injuries which could acutely or chronically worsen the patient’s circulation, and limb loss.”
The peer reviewers concurred that Dr. Dormu failed to use conservative management techniques to address the patients’ vascular complaints before resorting to invasive procedures.
Dr. Mustapha is described in the Times as a “high-volume” atherectomy provider. From 2017 to 2021, about half of Medicare’s atherectomy payments – $1.4 billion – went to 200 high-volume providers, with Dr. Mustapha near the top of the list.
Some of Dr. Mustapha’s patients underwent multiple procedures said to help prevent leg amputation, but their legs were amputated anyway, possibly because of the multiple atherectomies, according to the Times.
Judith Lin, MD, MBA, who treated some of Dr. Mustapha’s former patients, was among those who complained about his practice to Michigan’s licensing board. Some of the patients she treated needed amputations; others needed to have leftover wires extracted from their legs.
In 2020, the board investigated Dr. Lin’s complaint and referred it to Michigan’s attorney general, who brought a disciplinary action against Dr. Mustapha. An expert hired by the state to review eight patient cases concluded that Dr. Mustapha’s practice “was characterized by overtreatment and poor documentation.” In some cases, the expert wrote, “unnecessary procedures hastened amputations.”
The statement issued by Dr. Mills, the president of SVS, noted that the society’s practice guideline proposes a threshold of at least 2 years of likely durability for an intervention performed for claudication.
“The growing frequency of multiple, repeated procedures [is] emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous,” he wrote.
Financial incentives to blame?
In 2008, Medicare created incentives for physicians to perform vascular procedures in offices rather than hospitals, in an effort to reduce medical costs, according to both investigative articles. But the effort backfired.
Before the changes, an office provider inserting a stent could make about $1,700 from Medicare; deploying a balloon could bring in roughly $3,800. By 2011, the payments rose to about $6,400 and $4,800, respectively.
Office-based atherectomies soared when, in 2011, the Centers for Medicare & Medicaid Services started reimbursing $13,500 per procedure, as opposed to roughly $11,450 in a hospital. Atherectomies increased by 60% from 2011 to 2014, and Medicare’s overall costs for peripheral vascular treatments climbed by nearly half a billion dollars.
“The government is really to blame for setting these tremendously high reimbursement values without looking into whether these procedures are helping people or are just worthless procedures or, in fact, are hurting people,” Dipankar Mukherjee, MD, a vascular surgeon and chief of vascular surgery at Inova Fairfax (Va.) Hospital, said in ProPublica.
The result, noted Dr. Rao, is that “there can be perverse or nefarious incentives for doing these procedures. People are incentivized by reimbursement to do something that really falls in the area of clinical judgment and guidelines.”
Major incentives also come from device manufacturers, who often reward physicians who do the most vascular procedures with payments for consulting and other services, according to the Times. In addition, these companies lend money to help physicians or their clinics to finance the purchase of equipment used to perform the procedures.
“Vascular medicine now is the frontier of the Wild West,” Marty Makary, MD, MPH, a professor of surgery and health care quality researcher at Johns Hopkins University, Baltimore, told ProPublica. “People are flying blind walking into the clinics of these doctors with egregious practice patterns, and we know that their pattern is indefensible.”
Recognizing that the situation posed a threat to patients and also damaged the credibility of his specialty, Kim J. Hodgson, MD, a former SVS president, told attendees at the 2021 annual meeting of the SVS, “Somebody has to address what should never have been allowed to get to this level of threat to us and our patients in the first place. We can play whack-a-mole every time the bad actors surface until the cows come home, but that leaves a trail of harmed patients and wasted resources.”
Dr. Hodgson described atherectomy as “a procedure that many believe provides no demonstrable value whatsoever to the patient” and challenged those who disagree to prove it.
Multidisciplinary teams needed
Other experts believe there are times that revascularization procedures, including atherectomy, are appropriate. However, the majority of patients with PAD do not require a procedure, Soo Hyun (Esther) Kim, MD, MPH, director of the Center for Women’s Cardiovascular Health at Atrium Health Sanger Heart and Vascular Institute in Charlotte, N.C., said in an interview. In fact, “many patients do not even know they have leg artery blockages.”
Invasive procedures may well be appropriate for patients with severe PAD, especially those with CLTI, and disparities may be keeping those who truly need such interventions – or for whom they may be at least considered – from accessing them. If PAD is not diagnosed and treated in a timely way, Dr. Kim said, those individuals “do indeed lose their limbs.”
Multidisciplinary teams can help, Dr. Kim said. “Specialists from multiple different training backgrounds [can] take good care of patients with PAD,” she said. This is important when access to a particular type of specialist is limited, and because patients with PAD often have complex medical problems that can benefit from a team approach.
Transcatheter aortic valve replacement heart teams and complex coronary disease heart teams are two examples, Dr. Kim noted. “When a high-stakes procedure is being considered, the patient’s case is reviewed by multiple stakeholders to ensure appropriateness of the procedure and collaboratively evaluate risk.”
Dr. Rao also emphasized a team approach. “PAD does not belong to a single specialty,” he said. The revelations from the Times, ProPublica, and other sources “point to the fact that we all – cardiologists, vascular surgeons, interventional radiologists – should start thinking about how best to police ourselves and also account for the variation in clinical judgment.”
Use of a multidisciplinary team is a “guideline-recommended approach” for coronary artery revascularization, he said, “I think the same should apply for PAD.”
PAD is a sign of systemic atherosclerosis, Dr. Kim noted. “The treatment of PAD includes addressing leg pain and wounds with procedures, but the interventions that will keep people alive are the medications we use to prevent heart attack and stroke. Patients with PAD need to understand that treatment is much more than opening up a blockage in the leg.”
Dr. Rao and Dr. Kim disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
On May 24, the news outlet ProPublica published a scathing investigation of Jeffery Dormu, DO, said to have performed hundreds of “medically unnecessary and invasive vascular procedures” in his Laurel, Md. office, putting patients’ limbs and lives at risk.
On July 15, The New York Times published a broader-based investigation of several vascular specialists said to have performed “risky” procedures on patients with peripheral artery disease (PAD) who subsequently had to have amputations, or died. The focus was mainly on Michigan-based interventional cardiologist Jihad Mustapha, MD.
This follows a 2019 analysis of Medicare claims data that identified outlier physicians with a high early intervention rate for patients newly diagnosed with claudication. According to the American Heart Association statistics, PAD affects approximately 8.5 million U.S. adults age 40 and older (some claim that’s an underestimate); most cases don’t require invasive treatment.
Responding to the Times’ revelations, Joseph L. Mills, MD, president of the Society for Vascular Surgery, wrote on the society’s website: “The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology are providing high-quality, evidence-based care with safety and the best patient outcomes in mind.
“This is a complex issue that requires the examination not only of the events detailed in this story ... but of the underlying health care economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.”
‘A few bad apples’
“I think it’s a case of a few bad apples,” Sunil V. Rao, MD, director of interventional cardiology at NYU Langone Health, New York, said in an interview. “In general, I think physicians who take care of patients with vascular issues are trying to do the right thing. I think all of us who take care of patients with vascular disease see patients who are very, very complex, and there are going to be some procedures that have complications.
“Without knowing the clinical details, it’s hard to know whether the procedures described in the articles were overuse or unnecessary, or exactly what led to the amputations,” he said. “All we know is that these physicians are outliers in terms of the number of procedures they were billing for.
“But although correlation is not causation, it certainly is cause for concern because you would expect that the use of procedures for specific indications would fall within a certain range,” he added.
Lifestyle changes first
PAD is often asymptomatic or mild, making it difficult to diagnose. Revascularization procedures usually are reserved for the 5%-8% of patients at risk for chronic limb-threatening ischemia (CLTI) or those in whom the cornerstones of PAD treatment – lifestyle changes and, if needed, medication – fail.
Revascularization options include balloon angioplasty or stent placement; atherectomy to remove plaques from the artery; or bypass surgery if a long portion of a leg artery is completely blocked. All carry a risk of long-term adverse outcomes, but the rates are highest for atherectomy.
Lifestyle changes include regular exercise, following a healthy diet, quitting smoking, and controlling diabetes and high blood pressure. When PAD continues or progresses despite these modifications, medications such as antiplatelet agents, antihypertensives, and/or lipid-lowering drugs may be prescribed.
‘Medically unnecessary’
According to the latest American Heart Association/American College of Cardiology guideline on managing patients with lower-extremity PAD, patients should be selected for revascularization based on symptom severity.
Factors to consider include a significant disability as assessed by the patient, and adequacy of response to medical and structured exercise therapy.
There’s the rub regarding the clinicians investigated in the Times and ProPublica. Many patients, apparently, were not encouraged to make lifestyle changes, nor did they receive medication. Instead, they were advised from the get-go to undergo invasive procedures, and often multiple times. Underuse of prevention and lifestyle counseling n the management of PAD has long been a concern.
Furthermore, in at least some cases, patients without any symptoms were encouraged to be screened for blockages that were then treated invasively, according to the Times.
Dr. Dormu, as highlighted in ProPublica, positioned his practice as “life and limb saving.” Yet, in investigative findings that led to a suspension of Dr. Dormu’s license to practice medicine in Maryland, peer reviewers expressed concern regarding his repeated use of invasive and medically unnecessary procedures, exposing patients to “potential risks such as bleeding, infection, blood vessel injuries which could acutely or chronically worsen the patient’s circulation, and limb loss.”
The peer reviewers concurred that Dr. Dormu failed to use conservative management techniques to address the patients’ vascular complaints before resorting to invasive procedures.
Dr. Mustapha is described in the Times as a “high-volume” atherectomy provider. From 2017 to 2021, about half of Medicare’s atherectomy payments – $1.4 billion – went to 200 high-volume providers, with Dr. Mustapha near the top of the list.
Some of Dr. Mustapha’s patients underwent multiple procedures said to help prevent leg amputation, but their legs were amputated anyway, possibly because of the multiple atherectomies, according to the Times.
Judith Lin, MD, MBA, who treated some of Dr. Mustapha’s former patients, was among those who complained about his practice to Michigan’s licensing board. Some of the patients she treated needed amputations; others needed to have leftover wires extracted from their legs.
In 2020, the board investigated Dr. Lin’s complaint and referred it to Michigan’s attorney general, who brought a disciplinary action against Dr. Mustapha. An expert hired by the state to review eight patient cases concluded that Dr. Mustapha’s practice “was characterized by overtreatment and poor documentation.” In some cases, the expert wrote, “unnecessary procedures hastened amputations.”
The statement issued by Dr. Mills, the president of SVS, noted that the society’s practice guideline proposes a threshold of at least 2 years of likely durability for an intervention performed for claudication.
“The growing frequency of multiple, repeated procedures [is] emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous,” he wrote.
Financial incentives to blame?
In 2008, Medicare created incentives for physicians to perform vascular procedures in offices rather than hospitals, in an effort to reduce medical costs, according to both investigative articles. But the effort backfired.
Before the changes, an office provider inserting a stent could make about $1,700 from Medicare; deploying a balloon could bring in roughly $3,800. By 2011, the payments rose to about $6,400 and $4,800, respectively.
Office-based atherectomies soared when, in 2011, the Centers for Medicare & Medicaid Services started reimbursing $13,500 per procedure, as opposed to roughly $11,450 in a hospital. Atherectomies increased by 60% from 2011 to 2014, and Medicare’s overall costs for peripheral vascular treatments climbed by nearly half a billion dollars.
“The government is really to blame for setting these tremendously high reimbursement values without looking into whether these procedures are helping people or are just worthless procedures or, in fact, are hurting people,” Dipankar Mukherjee, MD, a vascular surgeon and chief of vascular surgery at Inova Fairfax (Va.) Hospital, said in ProPublica.
The result, noted Dr. Rao, is that “there can be perverse or nefarious incentives for doing these procedures. People are incentivized by reimbursement to do something that really falls in the area of clinical judgment and guidelines.”
Major incentives also come from device manufacturers, who often reward physicians who do the most vascular procedures with payments for consulting and other services, according to the Times. In addition, these companies lend money to help physicians or their clinics to finance the purchase of equipment used to perform the procedures.
“Vascular medicine now is the frontier of the Wild West,” Marty Makary, MD, MPH, a professor of surgery and health care quality researcher at Johns Hopkins University, Baltimore, told ProPublica. “People are flying blind walking into the clinics of these doctors with egregious practice patterns, and we know that their pattern is indefensible.”
Recognizing that the situation posed a threat to patients and also damaged the credibility of his specialty, Kim J. Hodgson, MD, a former SVS president, told attendees at the 2021 annual meeting of the SVS, “Somebody has to address what should never have been allowed to get to this level of threat to us and our patients in the first place. We can play whack-a-mole every time the bad actors surface until the cows come home, but that leaves a trail of harmed patients and wasted resources.”
Dr. Hodgson described atherectomy as “a procedure that many believe provides no demonstrable value whatsoever to the patient” and challenged those who disagree to prove it.
Multidisciplinary teams needed
Other experts believe there are times that revascularization procedures, including atherectomy, are appropriate. However, the majority of patients with PAD do not require a procedure, Soo Hyun (Esther) Kim, MD, MPH, director of the Center for Women’s Cardiovascular Health at Atrium Health Sanger Heart and Vascular Institute in Charlotte, N.C., said in an interview. In fact, “many patients do not even know they have leg artery blockages.”
Invasive procedures may well be appropriate for patients with severe PAD, especially those with CLTI, and disparities may be keeping those who truly need such interventions – or for whom they may be at least considered – from accessing them. If PAD is not diagnosed and treated in a timely way, Dr. Kim said, those individuals “do indeed lose their limbs.”
Multidisciplinary teams can help, Dr. Kim said. “Specialists from multiple different training backgrounds [can] take good care of patients with PAD,” she said. This is important when access to a particular type of specialist is limited, and because patients with PAD often have complex medical problems that can benefit from a team approach.
Transcatheter aortic valve replacement heart teams and complex coronary disease heart teams are two examples, Dr. Kim noted. “When a high-stakes procedure is being considered, the patient’s case is reviewed by multiple stakeholders to ensure appropriateness of the procedure and collaboratively evaluate risk.”
Dr. Rao also emphasized a team approach. “PAD does not belong to a single specialty,” he said. The revelations from the Times, ProPublica, and other sources “point to the fact that we all – cardiologists, vascular surgeons, interventional radiologists – should start thinking about how best to police ourselves and also account for the variation in clinical judgment.”
Use of a multidisciplinary team is a “guideline-recommended approach” for coronary artery revascularization, he said, “I think the same should apply for PAD.”
PAD is a sign of systemic atherosclerosis, Dr. Kim noted. “The treatment of PAD includes addressing leg pain and wounds with procedures, but the interventions that will keep people alive are the medications we use to prevent heart attack and stroke. Patients with PAD need to understand that treatment is much more than opening up a blockage in the leg.”
Dr. Rao and Dr. Kim disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
On May 24, the news outlet ProPublica published a scathing investigation of Jeffery Dormu, DO, said to have performed hundreds of “medically unnecessary and invasive vascular procedures” in his Laurel, Md. office, putting patients’ limbs and lives at risk.
On July 15, The New York Times published a broader-based investigation of several vascular specialists said to have performed “risky” procedures on patients with peripheral artery disease (PAD) who subsequently had to have amputations, or died. The focus was mainly on Michigan-based interventional cardiologist Jihad Mustapha, MD.
This follows a 2019 analysis of Medicare claims data that identified outlier physicians with a high early intervention rate for patients newly diagnosed with claudication. According to the American Heart Association statistics, PAD affects approximately 8.5 million U.S. adults age 40 and older (some claim that’s an underestimate); most cases don’t require invasive treatment.
Responding to the Times’ revelations, Joseph L. Mills, MD, president of the Society for Vascular Surgery, wrote on the society’s website: “The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients, including those trained in vascular medicine, interventional cardiology, and interventional radiology are providing high-quality, evidence-based care with safety and the best patient outcomes in mind.
“This is a complex issue that requires the examination not only of the events detailed in this story ... but of the underlying health care economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.”
‘A few bad apples’
“I think it’s a case of a few bad apples,” Sunil V. Rao, MD, director of interventional cardiology at NYU Langone Health, New York, said in an interview. “In general, I think physicians who take care of patients with vascular issues are trying to do the right thing. I think all of us who take care of patients with vascular disease see patients who are very, very complex, and there are going to be some procedures that have complications.
“Without knowing the clinical details, it’s hard to know whether the procedures described in the articles were overuse or unnecessary, or exactly what led to the amputations,” he said. “All we know is that these physicians are outliers in terms of the number of procedures they were billing for.
“But although correlation is not causation, it certainly is cause for concern because you would expect that the use of procedures for specific indications would fall within a certain range,” he added.
Lifestyle changes first
PAD is often asymptomatic or mild, making it difficult to diagnose. Revascularization procedures usually are reserved for the 5%-8% of patients at risk for chronic limb-threatening ischemia (CLTI) or those in whom the cornerstones of PAD treatment – lifestyle changes and, if needed, medication – fail.
Revascularization options include balloon angioplasty or stent placement; atherectomy to remove plaques from the artery; or bypass surgery if a long portion of a leg artery is completely blocked. All carry a risk of long-term adverse outcomes, but the rates are highest for atherectomy.
Lifestyle changes include regular exercise, following a healthy diet, quitting smoking, and controlling diabetes and high blood pressure. When PAD continues or progresses despite these modifications, medications such as antiplatelet agents, antihypertensives, and/or lipid-lowering drugs may be prescribed.
‘Medically unnecessary’
According to the latest American Heart Association/American College of Cardiology guideline on managing patients with lower-extremity PAD, patients should be selected for revascularization based on symptom severity.
Factors to consider include a significant disability as assessed by the patient, and adequacy of response to medical and structured exercise therapy.
There’s the rub regarding the clinicians investigated in the Times and ProPublica. Many patients, apparently, were not encouraged to make lifestyle changes, nor did they receive medication. Instead, they were advised from the get-go to undergo invasive procedures, and often multiple times. Underuse of prevention and lifestyle counseling n the management of PAD has long been a concern.
Furthermore, in at least some cases, patients without any symptoms were encouraged to be screened for blockages that were then treated invasively, according to the Times.
Dr. Dormu, as highlighted in ProPublica, positioned his practice as “life and limb saving.” Yet, in investigative findings that led to a suspension of Dr. Dormu’s license to practice medicine in Maryland, peer reviewers expressed concern regarding his repeated use of invasive and medically unnecessary procedures, exposing patients to “potential risks such as bleeding, infection, blood vessel injuries which could acutely or chronically worsen the patient’s circulation, and limb loss.”
The peer reviewers concurred that Dr. Dormu failed to use conservative management techniques to address the patients’ vascular complaints before resorting to invasive procedures.
Dr. Mustapha is described in the Times as a “high-volume” atherectomy provider. From 2017 to 2021, about half of Medicare’s atherectomy payments – $1.4 billion – went to 200 high-volume providers, with Dr. Mustapha near the top of the list.
Some of Dr. Mustapha’s patients underwent multiple procedures said to help prevent leg amputation, but their legs were amputated anyway, possibly because of the multiple atherectomies, according to the Times.
Judith Lin, MD, MBA, who treated some of Dr. Mustapha’s former patients, was among those who complained about his practice to Michigan’s licensing board. Some of the patients she treated needed amputations; others needed to have leftover wires extracted from their legs.
In 2020, the board investigated Dr. Lin’s complaint and referred it to Michigan’s attorney general, who brought a disciplinary action against Dr. Mustapha. An expert hired by the state to review eight patient cases concluded that Dr. Mustapha’s practice “was characterized by overtreatment and poor documentation.” In some cases, the expert wrote, “unnecessary procedures hastened amputations.”
The statement issued by Dr. Mills, the president of SVS, noted that the society’s practice guideline proposes a threshold of at least 2 years of likely durability for an intervention performed for claudication.
“The growing frequency of multiple, repeated procedures [is] emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous,” he wrote.
Financial incentives to blame?
In 2008, Medicare created incentives for physicians to perform vascular procedures in offices rather than hospitals, in an effort to reduce medical costs, according to both investigative articles. But the effort backfired.
Before the changes, an office provider inserting a stent could make about $1,700 from Medicare; deploying a balloon could bring in roughly $3,800. By 2011, the payments rose to about $6,400 and $4,800, respectively.
Office-based atherectomies soared when, in 2011, the Centers for Medicare & Medicaid Services started reimbursing $13,500 per procedure, as opposed to roughly $11,450 in a hospital. Atherectomies increased by 60% from 2011 to 2014, and Medicare’s overall costs for peripheral vascular treatments climbed by nearly half a billion dollars.
“The government is really to blame for setting these tremendously high reimbursement values without looking into whether these procedures are helping people or are just worthless procedures or, in fact, are hurting people,” Dipankar Mukherjee, MD, a vascular surgeon and chief of vascular surgery at Inova Fairfax (Va.) Hospital, said in ProPublica.
The result, noted Dr. Rao, is that “there can be perverse or nefarious incentives for doing these procedures. People are incentivized by reimbursement to do something that really falls in the area of clinical judgment and guidelines.”
Major incentives also come from device manufacturers, who often reward physicians who do the most vascular procedures with payments for consulting and other services, according to the Times. In addition, these companies lend money to help physicians or their clinics to finance the purchase of equipment used to perform the procedures.
“Vascular medicine now is the frontier of the Wild West,” Marty Makary, MD, MPH, a professor of surgery and health care quality researcher at Johns Hopkins University, Baltimore, told ProPublica. “People are flying blind walking into the clinics of these doctors with egregious practice patterns, and we know that their pattern is indefensible.”
Recognizing that the situation posed a threat to patients and also damaged the credibility of his specialty, Kim J. Hodgson, MD, a former SVS president, told attendees at the 2021 annual meeting of the SVS, “Somebody has to address what should never have been allowed to get to this level of threat to us and our patients in the first place. We can play whack-a-mole every time the bad actors surface until the cows come home, but that leaves a trail of harmed patients and wasted resources.”
Dr. Hodgson described atherectomy as “a procedure that many believe provides no demonstrable value whatsoever to the patient” and challenged those who disagree to prove it.
Multidisciplinary teams needed
Other experts believe there are times that revascularization procedures, including atherectomy, are appropriate. However, the majority of patients with PAD do not require a procedure, Soo Hyun (Esther) Kim, MD, MPH, director of the Center for Women’s Cardiovascular Health at Atrium Health Sanger Heart and Vascular Institute in Charlotte, N.C., said in an interview. In fact, “many patients do not even know they have leg artery blockages.”
Invasive procedures may well be appropriate for patients with severe PAD, especially those with CLTI, and disparities may be keeping those who truly need such interventions – or for whom they may be at least considered – from accessing them. If PAD is not diagnosed and treated in a timely way, Dr. Kim said, those individuals “do indeed lose their limbs.”
Multidisciplinary teams can help, Dr. Kim said. “Specialists from multiple different training backgrounds [can] take good care of patients with PAD,” she said. This is important when access to a particular type of specialist is limited, and because patients with PAD often have complex medical problems that can benefit from a team approach.
Transcatheter aortic valve replacement heart teams and complex coronary disease heart teams are two examples, Dr. Kim noted. “When a high-stakes procedure is being considered, the patient’s case is reviewed by multiple stakeholders to ensure appropriateness of the procedure and collaboratively evaluate risk.”
Dr. Rao also emphasized a team approach. “PAD does not belong to a single specialty,” he said. The revelations from the Times, ProPublica, and other sources “point to the fact that we all – cardiologists, vascular surgeons, interventional radiologists – should start thinking about how best to police ourselves and also account for the variation in clinical judgment.”
Use of a multidisciplinary team is a “guideline-recommended approach” for coronary artery revascularization, he said, “I think the same should apply for PAD.”
PAD is a sign of systemic atherosclerosis, Dr. Kim noted. “The treatment of PAD includes addressing leg pain and wounds with procedures, but the interventions that will keep people alive are the medications we use to prevent heart attack and stroke. Patients with PAD need to understand that treatment is much more than opening up a blockage in the leg.”
Dr. Rao and Dr. Kim disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Differences in 30-Day Readmission Rates in Older Adults With Dementia
Study 1 Overview (Park et al)
Objective: To compare rates of adverse events and 30-day readmission among patients with dementia who undergo percutaneous coronary intervention (PCI) with those without dementia.
Design: This cohort study used a national database of hospital readmissions developed by the Agency for Healthcare Research and Quality.
Setting and participants: Data from State Inpatient Databases were used to derive this national readmissions database representing 80% of hospitals from 28 states that contribute data. The study included all individuals aged 18 years and older who were identified to have had a PCI procedure in the years 2017 and 2018. International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify PCI procedures, including drug-eluting stent placement, bare-metal stent placement, and balloon angioplasty, performed in patients who presented with myocardial infarction and unstable angina and those with stable ischemic heart disease. Patients were stratified into those with or without dementia, also defined using ICD-10 codes. A total of 755,406 index hospitalizations were included; 2.3% of the patients had dementia.
Main outcome measures: The primary study outcome was 30-day all-cause readmission, with the cause classified as cardiovascular or noncardiovascular. Secondary outcome measures examined were delirium, in-hospital mortality, cardiac arrest, blood transfusion, acute kidney injury, fall in hospital, length of hospital stay, and other adverse outcomes. Location at discharge was also examined. Other covariates included in the analysis were age, sex, comorbidities, hospital characteristics, primary payer, and median income. For analysis, a propensity score matching algorithm was applied to match patients with and without dementia. Kaplan-Meier curves were used to examine 30-day readmission rates, and a Cox proportional hazards model was used to calculate hazard ratios (HR) for those with and without dementia. For secondary outcomes, logistic regression models were used to calculate odds ratios (OR) of outcomes between those with and without dementia.
Main results: The average age of those with dementia was 78.8 years vs 64.9 years in those without dementia. Women made up 42.8% of those with dementia and 31.3% of those without dementia. Those with dementia also had higher rates of comorbidities, such as heart failure, renal failure, and depression. After propensity score matching, 17,309 and 17,187 patients with and without dementia, respectively, were included. Covariates were balanced between the 2 groups after matching. For the primary outcome, patients with dementia were more likely to be readmitted at 30 days (HR, 1.11; 95% CI, 1.05-1.18; P < .01) when compared to those without dementia. For other adverse outcomes, delirium was significantly more likely to occur for those with dementia (OR, 4.37; 95% CI, 3.69-5.16; P < .01). Patients with dementia were also more likely to die in hospital (OR, 1.15; 95% CI, 1.01-1.30; P = .03), have cardiac arrest (OR, 1.19; 95% CI, 1.01-1.39; P = .04), receive a blood transfusion (OR, 1.17; 95% CI, 1.00-1.36; P = .05), experience acute kidney injury (OR, 1.30; 95% CI, 1.21-1.39; P < .01), and fall in hospital (OR, 2.51; 95% CI, 2.06-3.07; P < .01). Hospital length of stay was higher for those with dementia, with a mean difference of 1.43 days. For discharge location, patients with dementia were more likely to be sent to a skilled nursing facility (30.1% vs 12.2%) and less likely to be discharged home.
Conclusion: Patients with dementia are more likely to experience adverse events, including delirium, mortality, kidney injury, and falls after PCI, and are more likely to be readmitted to the hospital in 30 days compared to those without dementia.
Study 2 Overview (Gilmore-Bykovskyi et al)
Objective: To examine the association between race and 30-day readmissions in Black and non-Hispanic White Medicare beneficiaries with dementia.
Design: This was a retrospective cohort study that used 100% Medicare fee-for service claims data from all hospitalizations between January 1, 2014, and November 30, 2014, for all enrollees with a dementia diagnosis. The claims data were linked to the patient, hospital stay, and hospital factors. Patients with dementia were identified using a validated algorithm that requires an inpatient, skilled nursing facility, home health, or Part B institutional or noninstitutional claim with a qualifying diagnostic code during a 3-year period. Persons enrolled in a health maintenance organization plan were excluded.
Main outcome measures: The primary outcome examined in this study was 30-day all-cause readmission. Self-reported race and ethnic identity was a baseline covariate. Persons who self-reported Black or non-Hispanic White race were included in the study; other categories of race and ethnicity were excluded because of prior evidence suggesting low accuracy of these categories in Medicare claims data. Other covariates included neighborhood disadvantage, measured using the Area Deprivation Index (ADI), and rurality; hospital-level and hospital stay–level characteristics such as for-profit status and number of annual discharges; and individual demographic characteristics and comorbidities. The ADI is constructed using variables of poverty, education, housing, and employment and is represented as a percentile ranking of level of disadvantage. Unadjusted and adjusted analyses of 30-day hospital readmission were conducted. Models using various levels of adjustment were constructed to examine the contributions of the identified covariates to the estimated association between 30-day readmission and race.
Main results: A total of 1,523,142 index hospital stays among 945,481 beneficiaries were included; 215,815 episodes were among Black beneficiaries and 1,307,327 episodes were among non-Hispanic White beneficiaries. Mean age was 81.5 years, and approximately 61% of beneficiaries were female. Black beneficiaries were younger but had higher rates of dual Medicare/Medicaid eligibility and disability; they were also more likely to reside in disadvantaged neighborhoods. Black beneficiaries had a 30-day readmission rate of 24.1% compared with 18.5% in non-Hispanic White beneficiaries (unadjusted OR, 1.37; 95% CI, 1.35-1.39). The differences in outcomes persisted after adjusting for geographic factors, social factors, hospital characteristics, hospital stay factors, demographics, and comorbidities, suggesting that unmeasured underlying racial disparities not included in this model accounted for the differences. The effects of certain variables, such as neighborhood, differed by race; for example, the protective effect of living in a less disadvantaged neighborhood was observed among White beneficiaries but not Black beneficiaries.
Conclusion: Racial and geographic disparities in 30-day readmission rates were observed among Medicare beneficiaries with dementia. Protective effects associated with neighborhood advantage may confer different levels of benefit for people of different race.
Commentary
Adults living with dementia are at higher risk of adverse outcomes across settings. In the first study, by Park et al, among adults who underwent a cardiac procedure (PCI), those with dementia were more likely to experience adverse events compared to those without dementia. These outcomes include increased rates of 30-day readmissions, delirium, cardiac arrest, and falls. These findings are consistent with other studies that found a similar association among patients who underwent other cardiac procedures, such as transcatheter aortic valve replacement.1 Because dementia is a strong predisposing factor for delirium, it is not surprising that delirium is observed across patients who underwent different procedures or hospitalization episodes.2 Because of the potential hazards for inpatients with dementia, hospitals have developed risk-reduction programs, such as those that promote recognition of dementia, and management strategies that reduce the risk of delirium.3 Delirium prevention may also impact other adverse outcomes, such as falls, discharge to institutional care, and readmissions.
Racial disparities in care outcomes have been documented across settings, including hospital4 and hospice care settings.5 In study 2, by Gilmore-Bykovskyi et al, the findings of higher rates of hospital readmission among Black patients when compared to non-Hispanic White patients were not surprising. The central finding of this study is that even when accounting for various levels of factors, including hospital-level, hospital stay–level, individual (demographics, comorbidities), and neighborhood characteristics (disadvantage), the observed disparity diminished but persisted, suggesting that while these various levels of factors contributed to the observed disparity, other unmeasured factors also contributed. Another key finding is that the effect of the various factors examined in this study may affect different subgroups in different ways, suggesting underlying factors, and thus potential solutions to reduce disparities in care outcomes, could differ among subgroups.
Applications for Clinical Practice and System Implementation
These 2 studies add to the literature on factors that can affect 30-day hospital readmission rates in patients with dementia. These data could allow for more robust discussions of what to anticipate when adults with dementia undergo specific procedures, and also further build the case that improvements in care, such as delirium prevention programs, could offer benefits. The observation about racial and ethnic disparities in care outcomes among patients with dementia highlights the continued need to better understand the drivers of these disparities so that hospital systems and policy makers can consider and test possible solutions. Future studies should further disentangle the relationships among the various levels of factors and observed disparities in outcomes, especially for this vulnerable population of adults living with dementia.
Practice Points
- Clinicians should be aware of the additional risks for poor outcomes that dementia confers.
- Awareness of this increased risk will inform discussions of risks and benefits for older adults considered for procedures.
–William W. Hung, MD, MPH
1. Park DY, Sana MK, Shoura S, et al. Readmission and in-hospital outcomes after transcatheter aortic valve replacement in patients with dementia. Cardiovasc Revasc Med. 2023;46:70-77. doi:10.1016/j.carrev.2022.08.016
2. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. doi:10.1034/j.1600-0579.2003.00201.x
3. Weldingh NM, Mellingsæter MR, Hegna BW, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22(1):266. doi:10.1186/s12877-022-02949-0
4. Hermosura AH, Noonan CJ, Fyfe-Johnson AL, et al. Hospital disparities between native Hawaiian and other pacific islanders and non-Hispanic whites with Alzheimer’s disease and related dementias. J Aging Health. 2020;32(10):1579-1590. doi:10.1177/0898264320945177
5. Zhang Y, Shao H, Zhang M, Li J. Healthcare utilization and mortality after hospice live discharge among Medicare patients with and without Alzheimer’s disease and related dementias. J Gen Intern Med. 2023 Jan 17. doi:10.1007/s11606-023-08031-8
Study 1 Overview (Park et al)
Objective: To compare rates of adverse events and 30-day readmission among patients with dementia who undergo percutaneous coronary intervention (PCI) with those without dementia.
Design: This cohort study used a national database of hospital readmissions developed by the Agency for Healthcare Research and Quality.
Setting and participants: Data from State Inpatient Databases were used to derive this national readmissions database representing 80% of hospitals from 28 states that contribute data. The study included all individuals aged 18 years and older who were identified to have had a PCI procedure in the years 2017 and 2018. International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify PCI procedures, including drug-eluting stent placement, bare-metal stent placement, and balloon angioplasty, performed in patients who presented with myocardial infarction and unstable angina and those with stable ischemic heart disease. Patients were stratified into those with or without dementia, also defined using ICD-10 codes. A total of 755,406 index hospitalizations were included; 2.3% of the patients had dementia.
Main outcome measures: The primary study outcome was 30-day all-cause readmission, with the cause classified as cardiovascular or noncardiovascular. Secondary outcome measures examined were delirium, in-hospital mortality, cardiac arrest, blood transfusion, acute kidney injury, fall in hospital, length of hospital stay, and other adverse outcomes. Location at discharge was also examined. Other covariates included in the analysis were age, sex, comorbidities, hospital characteristics, primary payer, and median income. For analysis, a propensity score matching algorithm was applied to match patients with and without dementia. Kaplan-Meier curves were used to examine 30-day readmission rates, and a Cox proportional hazards model was used to calculate hazard ratios (HR) for those with and without dementia. For secondary outcomes, logistic regression models were used to calculate odds ratios (OR) of outcomes between those with and without dementia.
Main results: The average age of those with dementia was 78.8 years vs 64.9 years in those without dementia. Women made up 42.8% of those with dementia and 31.3% of those without dementia. Those with dementia also had higher rates of comorbidities, such as heart failure, renal failure, and depression. After propensity score matching, 17,309 and 17,187 patients with and without dementia, respectively, were included. Covariates were balanced between the 2 groups after matching. For the primary outcome, patients with dementia were more likely to be readmitted at 30 days (HR, 1.11; 95% CI, 1.05-1.18; P < .01) when compared to those without dementia. For other adverse outcomes, delirium was significantly more likely to occur for those with dementia (OR, 4.37; 95% CI, 3.69-5.16; P < .01). Patients with dementia were also more likely to die in hospital (OR, 1.15; 95% CI, 1.01-1.30; P = .03), have cardiac arrest (OR, 1.19; 95% CI, 1.01-1.39; P = .04), receive a blood transfusion (OR, 1.17; 95% CI, 1.00-1.36; P = .05), experience acute kidney injury (OR, 1.30; 95% CI, 1.21-1.39; P < .01), and fall in hospital (OR, 2.51; 95% CI, 2.06-3.07; P < .01). Hospital length of stay was higher for those with dementia, with a mean difference of 1.43 days. For discharge location, patients with dementia were more likely to be sent to a skilled nursing facility (30.1% vs 12.2%) and less likely to be discharged home.
Conclusion: Patients with dementia are more likely to experience adverse events, including delirium, mortality, kidney injury, and falls after PCI, and are more likely to be readmitted to the hospital in 30 days compared to those without dementia.
Study 2 Overview (Gilmore-Bykovskyi et al)
Objective: To examine the association between race and 30-day readmissions in Black and non-Hispanic White Medicare beneficiaries with dementia.
Design: This was a retrospective cohort study that used 100% Medicare fee-for service claims data from all hospitalizations between January 1, 2014, and November 30, 2014, for all enrollees with a dementia diagnosis. The claims data were linked to the patient, hospital stay, and hospital factors. Patients with dementia were identified using a validated algorithm that requires an inpatient, skilled nursing facility, home health, or Part B institutional or noninstitutional claim with a qualifying diagnostic code during a 3-year period. Persons enrolled in a health maintenance organization plan were excluded.
Main outcome measures: The primary outcome examined in this study was 30-day all-cause readmission. Self-reported race and ethnic identity was a baseline covariate. Persons who self-reported Black or non-Hispanic White race were included in the study; other categories of race and ethnicity were excluded because of prior evidence suggesting low accuracy of these categories in Medicare claims data. Other covariates included neighborhood disadvantage, measured using the Area Deprivation Index (ADI), and rurality; hospital-level and hospital stay–level characteristics such as for-profit status and number of annual discharges; and individual demographic characteristics and comorbidities. The ADI is constructed using variables of poverty, education, housing, and employment and is represented as a percentile ranking of level of disadvantage. Unadjusted and adjusted analyses of 30-day hospital readmission were conducted. Models using various levels of adjustment were constructed to examine the contributions of the identified covariates to the estimated association between 30-day readmission and race.
Main results: A total of 1,523,142 index hospital stays among 945,481 beneficiaries were included; 215,815 episodes were among Black beneficiaries and 1,307,327 episodes were among non-Hispanic White beneficiaries. Mean age was 81.5 years, and approximately 61% of beneficiaries were female. Black beneficiaries were younger but had higher rates of dual Medicare/Medicaid eligibility and disability; they were also more likely to reside in disadvantaged neighborhoods. Black beneficiaries had a 30-day readmission rate of 24.1% compared with 18.5% in non-Hispanic White beneficiaries (unadjusted OR, 1.37; 95% CI, 1.35-1.39). The differences in outcomes persisted after adjusting for geographic factors, social factors, hospital characteristics, hospital stay factors, demographics, and comorbidities, suggesting that unmeasured underlying racial disparities not included in this model accounted for the differences. The effects of certain variables, such as neighborhood, differed by race; for example, the protective effect of living in a less disadvantaged neighborhood was observed among White beneficiaries but not Black beneficiaries.
Conclusion: Racial and geographic disparities in 30-day readmission rates were observed among Medicare beneficiaries with dementia. Protective effects associated with neighborhood advantage may confer different levels of benefit for people of different race.
Commentary
Adults living with dementia are at higher risk of adverse outcomes across settings. In the first study, by Park et al, among adults who underwent a cardiac procedure (PCI), those with dementia were more likely to experience adverse events compared to those without dementia. These outcomes include increased rates of 30-day readmissions, delirium, cardiac arrest, and falls. These findings are consistent with other studies that found a similar association among patients who underwent other cardiac procedures, such as transcatheter aortic valve replacement.1 Because dementia is a strong predisposing factor for delirium, it is not surprising that delirium is observed across patients who underwent different procedures or hospitalization episodes.2 Because of the potential hazards for inpatients with dementia, hospitals have developed risk-reduction programs, such as those that promote recognition of dementia, and management strategies that reduce the risk of delirium.3 Delirium prevention may also impact other adverse outcomes, such as falls, discharge to institutional care, and readmissions.
Racial disparities in care outcomes have been documented across settings, including hospital4 and hospice care settings.5 In study 2, by Gilmore-Bykovskyi et al, the findings of higher rates of hospital readmission among Black patients when compared to non-Hispanic White patients were not surprising. The central finding of this study is that even when accounting for various levels of factors, including hospital-level, hospital stay–level, individual (demographics, comorbidities), and neighborhood characteristics (disadvantage), the observed disparity diminished but persisted, suggesting that while these various levels of factors contributed to the observed disparity, other unmeasured factors also contributed. Another key finding is that the effect of the various factors examined in this study may affect different subgroups in different ways, suggesting underlying factors, and thus potential solutions to reduce disparities in care outcomes, could differ among subgroups.
Applications for Clinical Practice and System Implementation
These 2 studies add to the literature on factors that can affect 30-day hospital readmission rates in patients with dementia. These data could allow for more robust discussions of what to anticipate when adults with dementia undergo specific procedures, and also further build the case that improvements in care, such as delirium prevention programs, could offer benefits. The observation about racial and ethnic disparities in care outcomes among patients with dementia highlights the continued need to better understand the drivers of these disparities so that hospital systems and policy makers can consider and test possible solutions. Future studies should further disentangle the relationships among the various levels of factors and observed disparities in outcomes, especially for this vulnerable population of adults living with dementia.
Practice Points
- Clinicians should be aware of the additional risks for poor outcomes that dementia confers.
- Awareness of this increased risk will inform discussions of risks and benefits for older adults considered for procedures.
–William W. Hung, MD, MPH
Study 1 Overview (Park et al)
Objective: To compare rates of adverse events and 30-day readmission among patients with dementia who undergo percutaneous coronary intervention (PCI) with those without dementia.
Design: This cohort study used a national database of hospital readmissions developed by the Agency for Healthcare Research and Quality.
Setting and participants: Data from State Inpatient Databases were used to derive this national readmissions database representing 80% of hospitals from 28 states that contribute data. The study included all individuals aged 18 years and older who were identified to have had a PCI procedure in the years 2017 and 2018. International Classification of Diseases, Tenth Revision (ICD-10) codes were used to identify PCI procedures, including drug-eluting stent placement, bare-metal stent placement, and balloon angioplasty, performed in patients who presented with myocardial infarction and unstable angina and those with stable ischemic heart disease. Patients were stratified into those with or without dementia, also defined using ICD-10 codes. A total of 755,406 index hospitalizations were included; 2.3% of the patients had dementia.
Main outcome measures: The primary study outcome was 30-day all-cause readmission, with the cause classified as cardiovascular or noncardiovascular. Secondary outcome measures examined were delirium, in-hospital mortality, cardiac arrest, blood transfusion, acute kidney injury, fall in hospital, length of hospital stay, and other adverse outcomes. Location at discharge was also examined. Other covariates included in the analysis were age, sex, comorbidities, hospital characteristics, primary payer, and median income. For analysis, a propensity score matching algorithm was applied to match patients with and without dementia. Kaplan-Meier curves were used to examine 30-day readmission rates, and a Cox proportional hazards model was used to calculate hazard ratios (HR) for those with and without dementia. For secondary outcomes, logistic regression models were used to calculate odds ratios (OR) of outcomes between those with and without dementia.
Main results: The average age of those with dementia was 78.8 years vs 64.9 years in those without dementia. Women made up 42.8% of those with dementia and 31.3% of those without dementia. Those with dementia also had higher rates of comorbidities, such as heart failure, renal failure, and depression. After propensity score matching, 17,309 and 17,187 patients with and without dementia, respectively, were included. Covariates were balanced between the 2 groups after matching. For the primary outcome, patients with dementia were more likely to be readmitted at 30 days (HR, 1.11; 95% CI, 1.05-1.18; P < .01) when compared to those without dementia. For other adverse outcomes, delirium was significantly more likely to occur for those with dementia (OR, 4.37; 95% CI, 3.69-5.16; P < .01). Patients with dementia were also more likely to die in hospital (OR, 1.15; 95% CI, 1.01-1.30; P = .03), have cardiac arrest (OR, 1.19; 95% CI, 1.01-1.39; P = .04), receive a blood transfusion (OR, 1.17; 95% CI, 1.00-1.36; P = .05), experience acute kidney injury (OR, 1.30; 95% CI, 1.21-1.39; P < .01), and fall in hospital (OR, 2.51; 95% CI, 2.06-3.07; P < .01). Hospital length of stay was higher for those with dementia, with a mean difference of 1.43 days. For discharge location, patients with dementia were more likely to be sent to a skilled nursing facility (30.1% vs 12.2%) and less likely to be discharged home.
Conclusion: Patients with dementia are more likely to experience adverse events, including delirium, mortality, kidney injury, and falls after PCI, and are more likely to be readmitted to the hospital in 30 days compared to those without dementia.
Study 2 Overview (Gilmore-Bykovskyi et al)
Objective: To examine the association between race and 30-day readmissions in Black and non-Hispanic White Medicare beneficiaries with dementia.
Design: This was a retrospective cohort study that used 100% Medicare fee-for service claims data from all hospitalizations between January 1, 2014, and November 30, 2014, for all enrollees with a dementia diagnosis. The claims data were linked to the patient, hospital stay, and hospital factors. Patients with dementia were identified using a validated algorithm that requires an inpatient, skilled nursing facility, home health, or Part B institutional or noninstitutional claim with a qualifying diagnostic code during a 3-year period. Persons enrolled in a health maintenance organization plan were excluded.
Main outcome measures: The primary outcome examined in this study was 30-day all-cause readmission. Self-reported race and ethnic identity was a baseline covariate. Persons who self-reported Black or non-Hispanic White race were included in the study; other categories of race and ethnicity were excluded because of prior evidence suggesting low accuracy of these categories in Medicare claims data. Other covariates included neighborhood disadvantage, measured using the Area Deprivation Index (ADI), and rurality; hospital-level and hospital stay–level characteristics such as for-profit status and number of annual discharges; and individual demographic characteristics and comorbidities. The ADI is constructed using variables of poverty, education, housing, and employment and is represented as a percentile ranking of level of disadvantage. Unadjusted and adjusted analyses of 30-day hospital readmission were conducted. Models using various levels of adjustment were constructed to examine the contributions of the identified covariates to the estimated association between 30-day readmission and race.
Main results: A total of 1,523,142 index hospital stays among 945,481 beneficiaries were included; 215,815 episodes were among Black beneficiaries and 1,307,327 episodes were among non-Hispanic White beneficiaries. Mean age was 81.5 years, and approximately 61% of beneficiaries were female. Black beneficiaries were younger but had higher rates of dual Medicare/Medicaid eligibility and disability; they were also more likely to reside in disadvantaged neighborhoods. Black beneficiaries had a 30-day readmission rate of 24.1% compared with 18.5% in non-Hispanic White beneficiaries (unadjusted OR, 1.37; 95% CI, 1.35-1.39). The differences in outcomes persisted after adjusting for geographic factors, social factors, hospital characteristics, hospital stay factors, demographics, and comorbidities, suggesting that unmeasured underlying racial disparities not included in this model accounted for the differences. The effects of certain variables, such as neighborhood, differed by race; for example, the protective effect of living in a less disadvantaged neighborhood was observed among White beneficiaries but not Black beneficiaries.
Conclusion: Racial and geographic disparities in 30-day readmission rates were observed among Medicare beneficiaries with dementia. Protective effects associated with neighborhood advantage may confer different levels of benefit for people of different race.
Commentary
Adults living with dementia are at higher risk of adverse outcomes across settings. In the first study, by Park et al, among adults who underwent a cardiac procedure (PCI), those with dementia were more likely to experience adverse events compared to those without dementia. These outcomes include increased rates of 30-day readmissions, delirium, cardiac arrest, and falls. These findings are consistent with other studies that found a similar association among patients who underwent other cardiac procedures, such as transcatheter aortic valve replacement.1 Because dementia is a strong predisposing factor for delirium, it is not surprising that delirium is observed across patients who underwent different procedures or hospitalization episodes.2 Because of the potential hazards for inpatients with dementia, hospitals have developed risk-reduction programs, such as those that promote recognition of dementia, and management strategies that reduce the risk of delirium.3 Delirium prevention may also impact other adverse outcomes, such as falls, discharge to institutional care, and readmissions.
Racial disparities in care outcomes have been documented across settings, including hospital4 and hospice care settings.5 In study 2, by Gilmore-Bykovskyi et al, the findings of higher rates of hospital readmission among Black patients when compared to non-Hispanic White patients were not surprising. The central finding of this study is that even when accounting for various levels of factors, including hospital-level, hospital stay–level, individual (demographics, comorbidities), and neighborhood characteristics (disadvantage), the observed disparity diminished but persisted, suggesting that while these various levels of factors contributed to the observed disparity, other unmeasured factors also contributed. Another key finding is that the effect of the various factors examined in this study may affect different subgroups in different ways, suggesting underlying factors, and thus potential solutions to reduce disparities in care outcomes, could differ among subgroups.
Applications for Clinical Practice and System Implementation
These 2 studies add to the literature on factors that can affect 30-day hospital readmission rates in patients with dementia. These data could allow for more robust discussions of what to anticipate when adults with dementia undergo specific procedures, and also further build the case that improvements in care, such as delirium prevention programs, could offer benefits. The observation about racial and ethnic disparities in care outcomes among patients with dementia highlights the continued need to better understand the drivers of these disparities so that hospital systems and policy makers can consider and test possible solutions. Future studies should further disentangle the relationships among the various levels of factors and observed disparities in outcomes, especially for this vulnerable population of adults living with dementia.
Practice Points
- Clinicians should be aware of the additional risks for poor outcomes that dementia confers.
- Awareness of this increased risk will inform discussions of risks and benefits for older adults considered for procedures.
–William W. Hung, MD, MPH
1. Park DY, Sana MK, Shoura S, et al. Readmission and in-hospital outcomes after transcatheter aortic valve replacement in patients with dementia. Cardiovasc Revasc Med. 2023;46:70-77. doi:10.1016/j.carrev.2022.08.016
2. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. doi:10.1034/j.1600-0579.2003.00201.x
3. Weldingh NM, Mellingsæter MR, Hegna BW, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22(1):266. doi:10.1186/s12877-022-02949-0
4. Hermosura AH, Noonan CJ, Fyfe-Johnson AL, et al. Hospital disparities between native Hawaiian and other pacific islanders and non-Hispanic whites with Alzheimer’s disease and related dementias. J Aging Health. 2020;32(10):1579-1590. doi:10.1177/0898264320945177
5. Zhang Y, Shao H, Zhang M, Li J. Healthcare utilization and mortality after hospice live discharge among Medicare patients with and without Alzheimer’s disease and related dementias. J Gen Intern Med. 2023 Jan 17. doi:10.1007/s11606-023-08031-8
1. Park DY, Sana MK, Shoura S, et al. Readmission and in-hospital outcomes after transcatheter aortic valve replacement in patients with dementia. Cardiovasc Revasc Med. 2023;46:70-77. doi:10.1016/j.carrev.2022.08.016
2. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc. 2003;51(5):591-598. doi:10.1034/j.1600-0579.2003.00201.x
3. Weldingh NM, Mellingsæter MR, Hegna BW, et al. Impact of a dementia-friendly program on detection and management of patients with cognitive impairment and delirium in acute-care hospital units: a controlled clinical trial design. BMC Geriatr. 2022;22(1):266. doi:10.1186/s12877-022-02949-0
4. Hermosura AH, Noonan CJ, Fyfe-Johnson AL, et al. Hospital disparities between native Hawaiian and other pacific islanders and non-Hispanic whites with Alzheimer’s disease and related dementias. J Aging Health. 2020;32(10):1579-1590. doi:10.1177/0898264320945177
5. Zhang Y, Shao H, Zhang M, Li J. Healthcare utilization and mortality after hospice live discharge among Medicare patients with and without Alzheimer’s disease and related dementias. J Gen Intern Med. 2023 Jan 17. doi:10.1007/s11606-023-08031-8
Endovascular approach best for below-knee limb-threatening ischemia?
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
in a new randomized trial.
In the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL-2) trial, patients who received vein bypass as the first approach were more likely to require a major amputation or to die during follow-up than patients who were randomly assigned to the endovascular approach as first strategy.
“Our findings suggest that a best endovascular treatment first revascularization strategy is associated with a better amputation-free survival. This is mainly because the best endovascular treatment first revascularization strategy resulted in fewer deaths. Limb-related outcomes were similar between groups,” the authors stated.
“The BASIL-2 trial has produced a statistically robust and clinically meaningful result that is likely to have an influence on the management of chronic limb-threatening ischemia worldwide,” added the study’s chief investigator, Andrew Bradbury, MD, professor of vascular surgery at the University of Birmingham (England).
However, the results of the BASIL-2 trial conflict with those from two previous studies – BASIL-1 and BEST-CLI, which both suggested that a surgical approach for chronic limb-threatening ischemia may be most appropriate.
The BASIL-2 study was published online in The Lancet.
The authors explained that chronic limb-threatening ischemia, previously known as critical limb ischemia and severe ischemia of the leg, is the most severe form of peripheral arterial disease caused by atherosclerosis. Patients present with ischemic rest pain and tissue loss (ulceration, gangrene, or both) that usually affects the foot.
Mainly because of tobacco smoking and the growing prevalence of type 2 diabetes, chronic limb-threatening ischemia represents a growing burden on health care and social care services around the world.
Unless the blood supply to the affected limb is restored, patients with chronic limb-threatening ischemia are at high risk for amputation or death. Although it is universally agreed that – in addition to best medical therapy – virtually all patients with chronic limb-threatening ischemia should at least be considered for revascularization, there is continuing debate as to whether conducting vein bypass surgery, preferably using a vein taken from the patient’s own leg, or endovascular treatment (balloon angioplasty with or without stents) is preferable.
“BASIL-2 is the only randomized trial to specifically compare a vein bypass first with best endovascular treatment first revascularisation strategy in patients with chronic limb-threatening ischemia who required an infrapopliteal (with or without an additional more proximal infrainguinal) revascularization procedure to restore limb perfusion,” the authors noted.
For the trial, which was conducted at 41 vascular surgery units in the United Kingdom, Sweden, and Denmark, 345 patients with chronic limb-threatening ischemia who required an infrapopliteal revascularization procedure to restore limb perfusion were randomly assigned to receive either vein bypass or best endovascular treatment as their first revascularization procedure.
Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries. Most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Participants were followed up for a minimum of 2 years.
The primary outcome was amputation-free survival, defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population.
Results showed that major amputation or death occurred in 63% of patients in the vein bypass group and in 53% of those in the best endovascular treatment group (adjusted hazard ratio, 1.35; P = .037).
The results were driven by a higher death rate in the vein bypass group (53% vs. 45%; aHR, 1.37).
In both groups, the most common causes of morbidity and death, including death occurring within 30 days of first revascularization, were cardiovascular and respiratory events.
The authors noted that outcomes for the patients in the BASIL-2 trial were poor (median amputation-free survival was 3.8 years, and half the patients died within 5 years).
They pointed out that severe, multilevel atherosclerotic disease that causes chronic limb-threatening ischemia develops over many years, but at baseline in this study, around 20% of patients said they were still smoking, and around 70% of patients had diabetes, of whom around 50% required insulin. In addition, around 90% of the participants often had quite extensive tissue loss.
“These baseline data suggest that there might still be missed opportunities in public health and primary care to prevent chronic limb-threatening ischemia through medical therapy and lifestyle interventions and missed opportunities to refer patients to secondary care earlier once chronic limb-threatening ischemia begins to develop,” they suggested.
“Better prevention and timely referral are important: the BASIL-2 trial shows that, by the time patients present to vascular and endovascular surgeons and interventional radiologists with established chronic limb-threatening ischemia, their prognosis is often poor regardless of what form of revascularization they are offered,” they added.
Conflicting results
In an accompanying comment, Ankur Kalra, MD, Franciscan Health, Lafayette, Ind., and Ashish Kumar, MD, Cleveland Clinic Akron (Ohio) General, noted that atherosclerotic lower-extremity peripheral artery disease affects more than 230 million people worldwide, and prevalence is increasing. Chronic limb-threatening ischemia is a severe form of peripheral artery disease that affects 11% of patients with peripheral artery disease and is associated with significant cardiovascular morbidity and death.
Furthermore, amputation rates of 10%-40% during a 6-month follow-up of patients with chronic limb-threatening ischemia who were unable to undergo revascularization have been reported, highlighting the severity of atherosclerotic burden and the need for improved treatment strategies.
Dr. Kalra and Dr. Kumar pointed out that two previous randomized clinical trials compared surgical vein graft bypass with endovascular treatment for patients with chronic limb-threatening ischemia – the BASIL-1 trial, and the BEST-CLI trial.
In the BASIL-1 trial, vein bypass was associated with improved overall survival and amputation-free survival for patients who survived at least 2 years. The BEST-CLI trial also reported a lower risk of a composite of major adverse limb events or death among patients undergoing a surgery-first strategy, compared with endovascular therapy, mostly in patients with suitable single segment of great saphenous vein.
Dr. Kalra and Dr. Kumar said the findings of the BASIL-2 trial should be put in context with these previous studies, which report a positive or equivocal effect of surgery. The results of the BEST-CLI trial were driven by fewer major reinterventions and above-ankle amputations in the surgical group, whereas the results of the BASIL-2 trial were driven by fewer deaths in the best endovascular treatment group, “which potentially points towards a difference in the characteristics of the patients randomly assigned in the two trials.”
They concluded: “Considering the results of the BASIL-2 trial and the BEST-CLI trial, choice of intervention should be based on shared decision making between interventional cardiology, vascular surgery, and the patient, until more evidence is accrued.”
The BASIL-2 trial was funded by the U.K. National Institute of Health Research.
A version of this article first appeared on Medscape.com.
FROM THE LANCET
Meet the JCOM Author with Dr. Barkoudah: A Multidisciplinary Team–Based Clinical Care Pathway for Infective Endocarditis
Implementation of a Multidisciplinary Team–Based Clinical Care Pathway Is Associated With Increased Surgery Rates for Infective Endocarditis
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
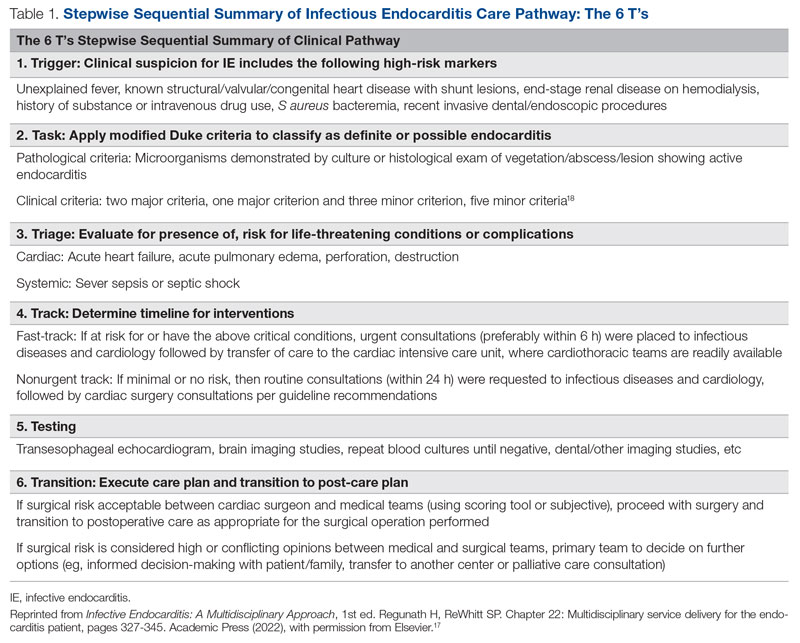
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
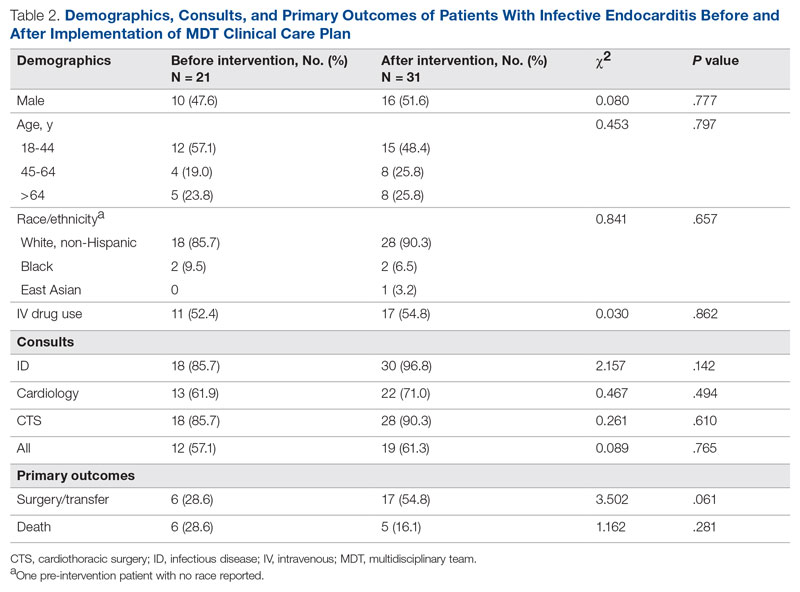
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
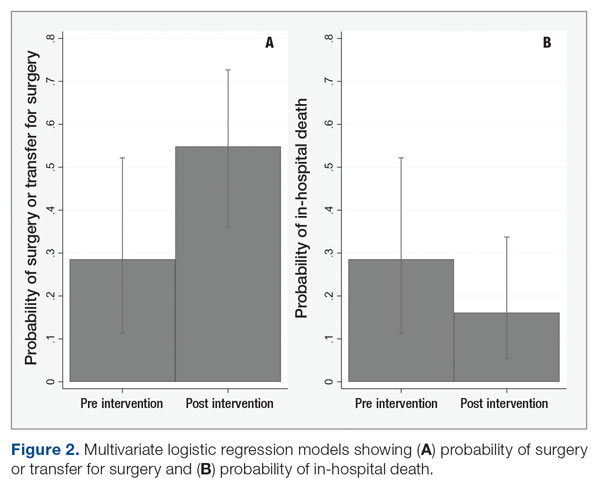
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; hwc2pd@health.missouri.edu
Disclosures: None reported.
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
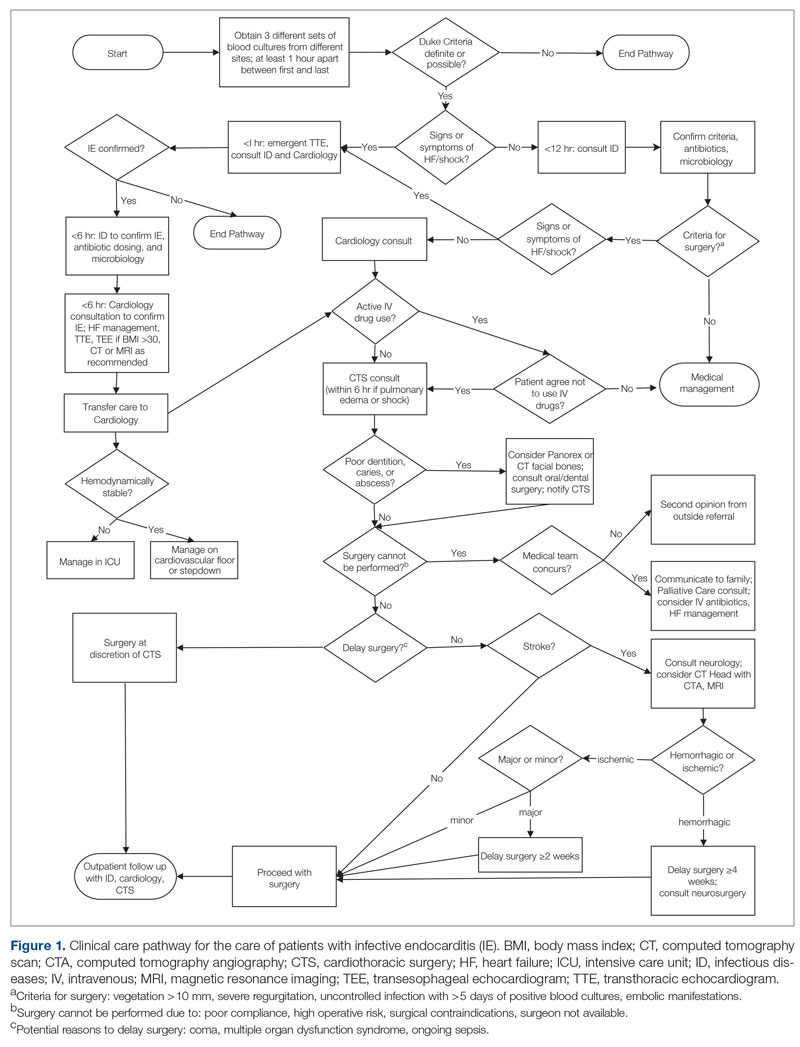
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
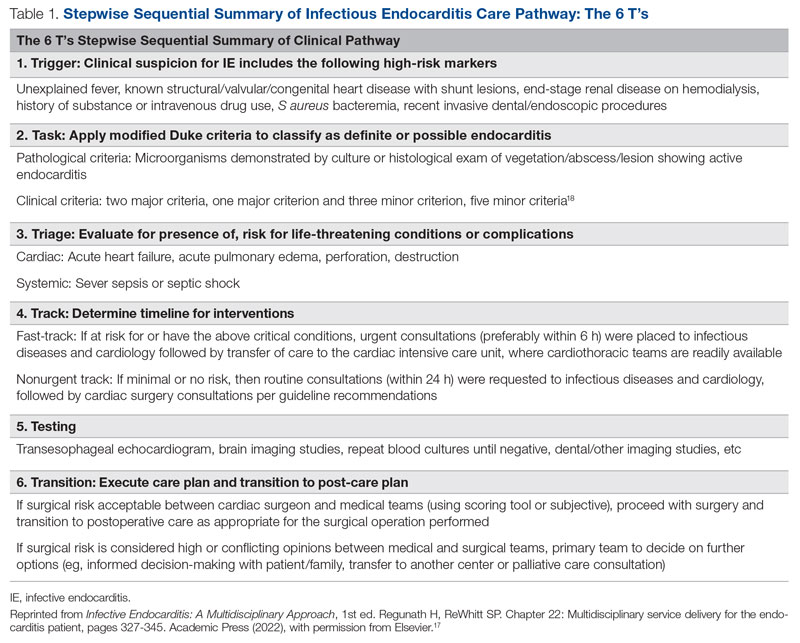
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
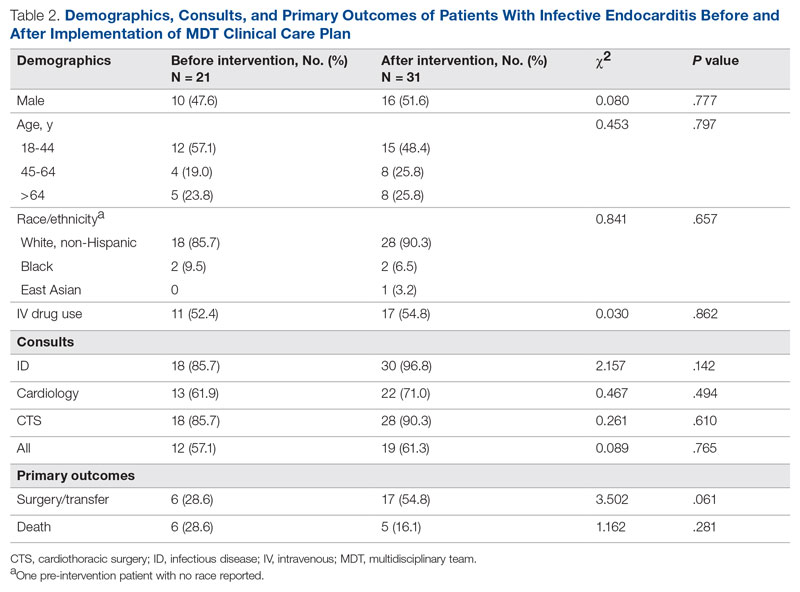
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
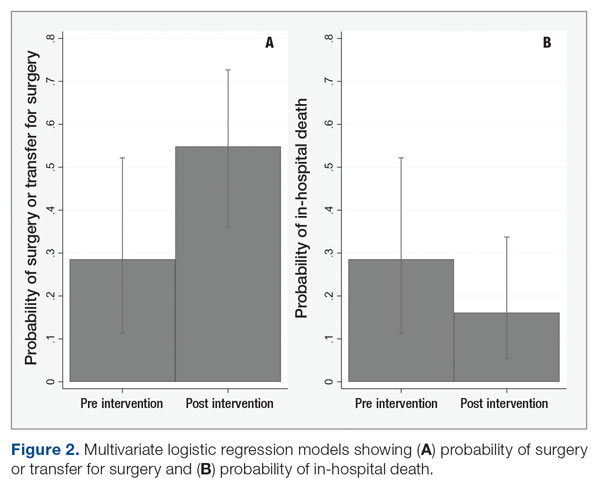
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; hwc2pd@health.missouri.edu
Disclosures: None reported.
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
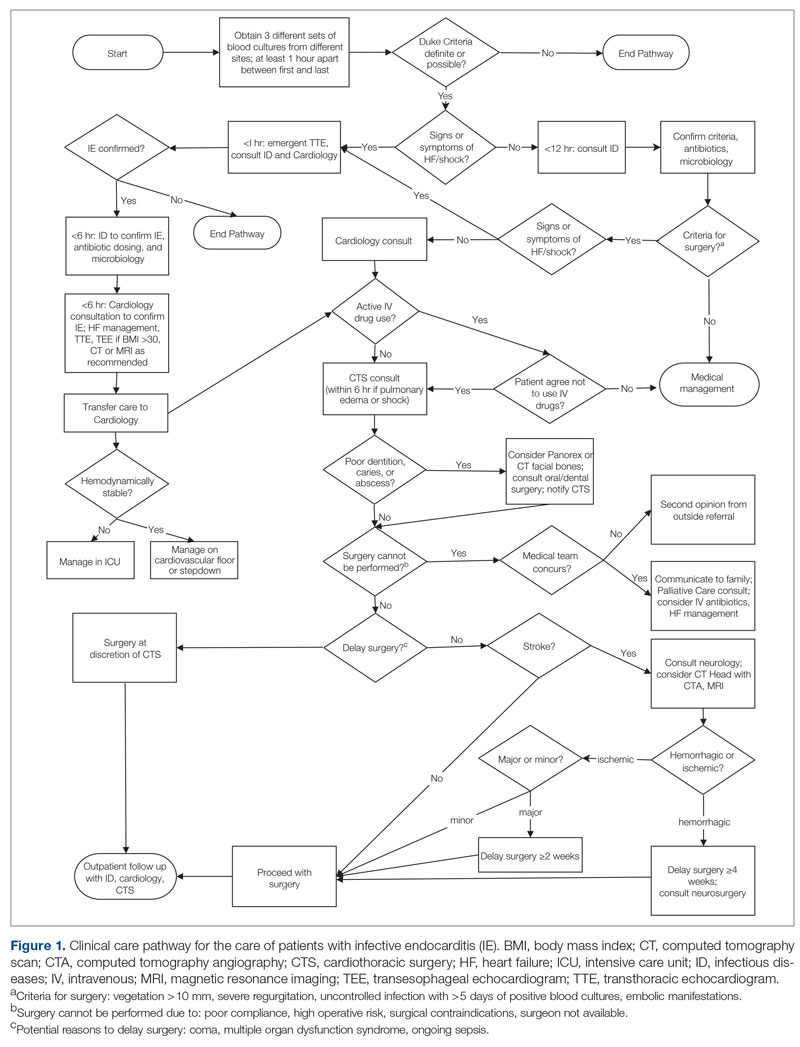
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
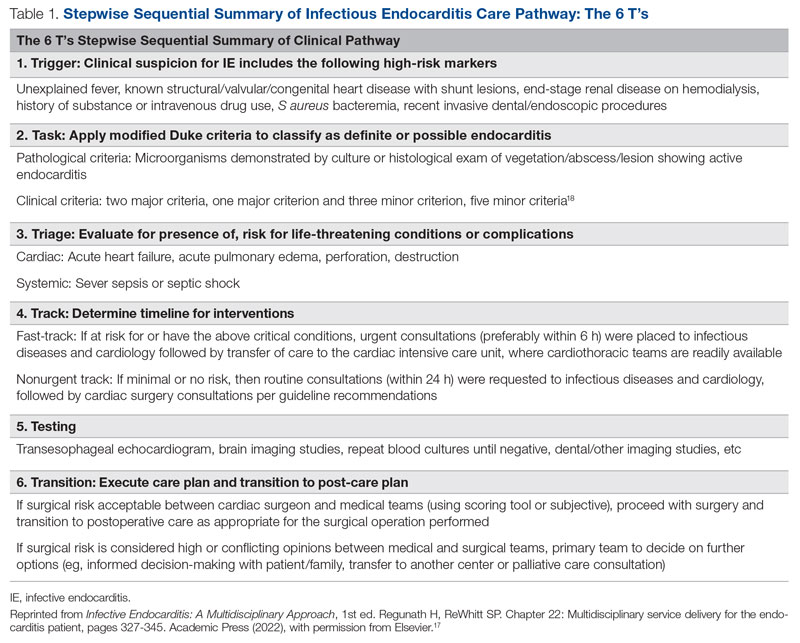
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
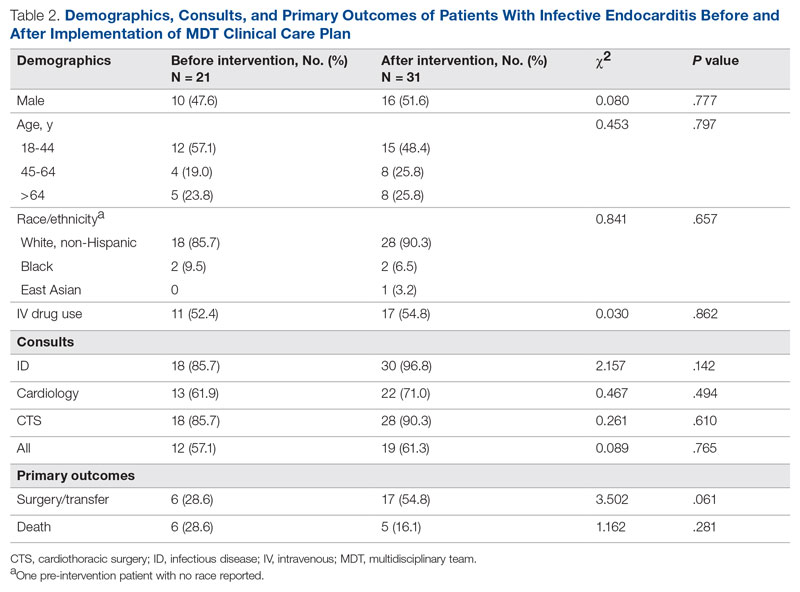
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
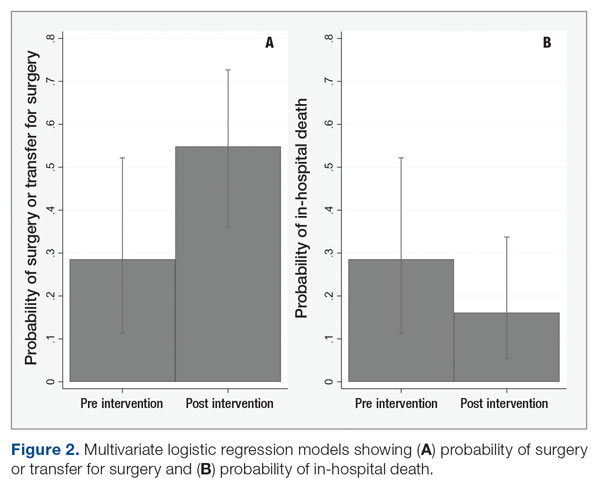
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; hwc2pd@health.missouri.edu
Disclosures: None reported.
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
The Shifting Landscape of Thrombolytic Therapy for Acute Ischemic Stroke
Study 1 Overview (Menon et al)
Objective: To determine whether a 0.25 mg/kg dose of intravenous tenecteplase is noninferior to intravenous alteplase 0.9 mg/kg for patients with acute ischemic stroke eligible for thrombolytic therapy.
Design: Multicenter, parallel-group, open-label randomized controlled trial.
Setting and participants: The trial was conducted at 22 primary and comprehensive stroke centers across Canada. A primary stroke center was defined as a hospital capable of offering intravenous thrombolysis to patients with acute ischemic stroke, while a comprehensive stroke center was able to offer thrombectomy services in addition. The involved centers also participated in Canadian quality improvement registries (either Quality Improvement and Clinical Research [QuiCR] or Optimizing Patient Treatment in Major Ischemic Stroke with EVT [OPTIMISE]) that track patient outcomes. Patients were eligible for inclusion if they were aged 18 years or older, had a diagnosis of acute ischemic stroke, presented within 4.5 hours of symptom onset, and were eligible for thrombolysis according to Canadian guidelines.
Patients were randomized in a 1:1 fashion to either intravenous tenecteplase (0.25 mg/kg single dose, maximum of 25 mg) or intravenous alteplase (0.9 mg/kg total dose to a maximum of 90 mg, delivered as a bolus followed by a continuous infusion). A total of 1600 patients were enrolled, with 816 randomly assigned to the tenecteplase arm and 784 to the alteplase arm; 1577 patients were included in the intention-to-treat (ITT) analysis (n = 806 tenecteplase; n = 771 alteplase). The median age of enrollees was 74 years, and 52.1% of the ITT population were men.
Main outcome measures: In the ITT population, the primary outcome measure was a modified Rankin score (mRS) of 0 or 1 at 90 to 120 days post treatment. Safety outcomes included symptomatic intracerebral hemorrhage, orolingual angioedema, extracranial bleeding that required blood transfusion (all within 24 hours of thrombolytic administration), and all-cause mortality at 90 days. The noninferiority threshold for intravenous tenecteplase was set as the lower 95% CI of the difference between the tenecteplase and alteplase groups in the proportion of patients who met the primary outcome exceeding –5%.
Main results: The primary outcome of mRS of either 0 or 1 at 90 to 120 days of treatment occurred in 296 (36.9%) of the 802 patients assigned to tenecteplase and 266 (34.8%) of the 765 patients assigned to alteplase (unadjusted risk difference, 2.1%; 95% CI, –2.6 to 6.9). The prespecified noninferiority threshold was met. There were no significant differences between the groups in rates of intracerebral hemorrhage at 24 hours or 90-day all-cause mortality.
Conclusion: Intravenous tenecteplase is a reasonable alternative to alteplase for patients eligible for thrombolytic therapy.
Study 2 Overview (Wang et al)
Objective: To determine whether tenecteplase (dose 0.25 mg/kg) is noninferior to alteplase in patients with acute ischemic stroke who are within 4.5 hours of symptom onset and eligible for thrombolytic therapy but either refused or were ineligible for endovascular thrombectomy.
Design: Multicenter, prospective, open-label, randomized, controlled noninferiority trial.
Setting and participants: This trial was conducted at 53 centers across China and included patients 18 years of age or older who were within 4.5 hours of symptom onset and were thrombolytic eligible, had a mRS ≤ 1 at enrollment, and had a National Institutes of Health Stroke Scale score between 5 and 25. Eligible participants were randomized 1:1 to either tenecteplase 0.25 mg/kg (maximum dose 25 mg) or alteplase 0.9 mg/kg (maximum dose 90 mg, administered as a bolus followed by infusion). During the enrollment period (June 12, 2021, to May 29, 2022), a total of 1430 participants were enrolled, and, of those, 716 were randomly assigned to tenecteplase and 714 to alteplase. Six patients assigned to tenecteplase and 7 assigned to alteplase did not receive drugs. At 90 days, 5 in the tenecteplase group and 11 in the alteplase group were lost to follow up.
Main outcome measures: The primary efficacy outcome was a mRS of 0 or 1 at 90 days. The primary safety outcome was intracranial hemorrhage within 36 hours. Safety outcomes included parenchymal hematoma 2, as defined by the European Cooperative Acute Stroke Study III; any intracranial or significant hemorrhage, as defined by the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries criteria; and death from all causes at 90 days. Noninferiority for tenecteplase would be declared if the lower 97.5% 1-sided CI for the relative risk (RR) for the primary outcome did not cross 0.937.
Main results: In the modified ITT population, the primary outcome occurred in 439 (62%) of the tenecteplase group and 405 (68%) of the alteplase group (RR, 1.07; 95% CI, 0.98-1.16). This met the prespecified margin for noninferiority. Intracranial hemorrhage within 36 hours was experienced by 15 (2%) patients in the tenecteplase group and 13 (2%) in the alteplase group (RR, 1.18; 95% CI, 0.56-2.50). Death at 90 days occurred in 46 (7%) patients in the tenecteplase group and 35 (5%) in the alteplase group (RR, 1.31; 95% CI, 0.86-2.01).
Conclusion: Tenecteplase was noninferior to alteplase in patients with acute ischemic stroke who met criteria for thrombolysis and either refused or were ineligible for endovascular thrombectomy.
Commentary
Alteplase has been FDA-approved for managing acute ischemic stroke since 1996 and has demonstrated positive effects on functional outcomes. Drawbacks of alteplase therapy, however, include bleeding risk as well as cumbersome administration of a bolus dose followed by a 60-minute infusion. In recent years, the question of whether or not tenecteplase could replace alteplase as the preferred thrombolytic for acute ischemic stroke has garnered much attention. Several features of tenecteplase make it an attractive option, including increased fibrin specificity, a longer half-life, and ease of administration as a single, rapid bolus dose. In phase 2 trials that compared tenecteplase 0.25 mg/kg with alteplase, findings suggested the potential for early neurological improvement as well as improved outcomes at 90 days. While the role of tenecteplase in acute myocardial infarction has been well established due to ease of use and a favorable adverse-effect profile,1 there is much less evidence from phase 3 randomized controlled clinical trials to secure the role of tenecteplase in acute ischemic stroke.2
Menon et al attempted to close this gap in the literature by conducting a randomized controlled clinical trial (AcT) comparing tenecteplase to alteplase in a Canadian patient population. The trial's patient population mirrors that of real-world data from global registries in terms of age, sex, and baseline stroke severity. In addition, the eligibility window of 4.5 hours from symptom onset as well as the inclusion and exclusion criteria for therapy are common to those utilized in other countries, making the findings generalizable. There were some limitations to the study, however, including the impact of COVID-19 on recruitment efforts as well as limitations of research infrastructure and staffing, which may have limited enrollment efforts at primary stroke centers. Nonetheless, the authors concluded that their results provide evidence that tenecteplase is comparable to alteplase, with similar functional and safety outcomes.
TRACE-2 focused on an Asian patient population and provided follow up to the dose-ranging TRACE-1 phase 2 trial. TRACE-1 showed that tenecteplase 0.25 mg/kg had a similar safety profile to alteplase 0.9 mg/kg in Chinese patients presenting with acute ischemic stroke. TRACE-2 sought to establish noninferiority of tenecteplase and excluded patients who were ineligible for or refused thrombectomy. Interestingly, the tenecteplase arm, as the authors point out, had numerically greater mortality as well as intracranial hemorrhage, but these differences were not statistically significant between the treatment groups at 90 days. The TRACE-2 results parallel those of AcT, and although there were differences in ethnicity between the 2 trials, the authors cite this as evidence that the results are consistent and provide evidence for the role of tenecteplase in the management of acute ischemic stroke. Limitations of this trial include potential bias from its open-label design, as well as exclusion of patients with more severe strokes eligible for thrombectomy, which may limit generalizability to patients with more disabling strokes who could have a higher risk of intracranial hemorrhage.
Application for Clinical Practice and System Implementation
Across the country, many organizations have adopted the off-label use of tenecteplase for managing fibrinolytic-eligible acute ischemic stroke patients. In most cases, the impetus for change is the ease of dosing and administration of tenecteplase compared to alteplase, while the inclusion and exclusion criteria and overall management remain the same. Timely administration of therapy in stroke is critical. This, along with other time constraints in stroke workflows, the weight-based calculation of alteplase doses, and alteplase’s administration method may lead to medication errors when using this agent to treat patients with acute stroke. The rapid, single-dose administration of tenecteplase removes many barriers that hospitals face when patients may need to be treated and then transferred to another site for further care. Without the worry to “drip and ship,” the completion of administration may allow for timely patient transfer and eliminate the need for monitoring of an infusion during transfer. For some organizations, there may be a potential for drug cost-savings as well as improved metrics, such as door-to-needle time, but the overall effects of switching from alteplase to tenecteplase remain to be seen. Currently, tenecteplase is included in stroke guidelines as a “reasonable choice,” though with a low level of evidence.3 However, these 2 studies support the role of tenecteplase in acute ischemic stroke treatment and may provide a foundation for further studies to establish the role of tenecteplase in the acute ischemic stroke population.
Practice Points
- Tenecteplase may be considered as an alternative to alteplase for acute ischemic stroke for patients who meet eligibility criteria for thrombolytics; this recommendation is included in the most recent stroke guidelines, although tenecteplase has not been demonstrated to be superior to alteplase.
- The ease of administration of tenecteplase as a single intravenous bolus dose represents a benefit compared to alteplase; it is an off-label use, however, and further studies are needed to establish the superiority of tenecteplase in terms of functional and safety outcomes.
– Carol Heunisch, PharmD, BCPS, BCCP
Pharmacy Department, NorthShore–Edward-Elmhurst Health, Evanston, IL
1. Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators; F Van De Werf, J Adgey, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716-722. doi:10.1016/s0140-6736(99)07403-6
2. Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischaemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50(8):2156-2162. doi:10.1161/STROKEAHA.119.025080
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi:10.1161/STR.0000000000000211
Study 1 Overview (Menon et al)
Objective: To determine whether a 0.25 mg/kg dose of intravenous tenecteplase is noninferior to intravenous alteplase 0.9 mg/kg for patients with acute ischemic stroke eligible for thrombolytic therapy.
Design: Multicenter, parallel-group, open-label randomized controlled trial.
Setting and participants: The trial was conducted at 22 primary and comprehensive stroke centers across Canada. A primary stroke center was defined as a hospital capable of offering intravenous thrombolysis to patients with acute ischemic stroke, while a comprehensive stroke center was able to offer thrombectomy services in addition. The involved centers also participated in Canadian quality improvement registries (either Quality Improvement and Clinical Research [QuiCR] or Optimizing Patient Treatment in Major Ischemic Stroke with EVT [OPTIMISE]) that track patient outcomes. Patients were eligible for inclusion if they were aged 18 years or older, had a diagnosis of acute ischemic stroke, presented within 4.5 hours of symptom onset, and were eligible for thrombolysis according to Canadian guidelines.
Patients were randomized in a 1:1 fashion to either intravenous tenecteplase (0.25 mg/kg single dose, maximum of 25 mg) or intravenous alteplase (0.9 mg/kg total dose to a maximum of 90 mg, delivered as a bolus followed by a continuous infusion). A total of 1600 patients were enrolled, with 816 randomly assigned to the tenecteplase arm and 784 to the alteplase arm; 1577 patients were included in the intention-to-treat (ITT) analysis (n = 806 tenecteplase; n = 771 alteplase). The median age of enrollees was 74 years, and 52.1% of the ITT population were men.
Main outcome measures: In the ITT population, the primary outcome measure was a modified Rankin score (mRS) of 0 or 1 at 90 to 120 days post treatment. Safety outcomes included symptomatic intracerebral hemorrhage, orolingual angioedema, extracranial bleeding that required blood transfusion (all within 24 hours of thrombolytic administration), and all-cause mortality at 90 days. The noninferiority threshold for intravenous tenecteplase was set as the lower 95% CI of the difference between the tenecteplase and alteplase groups in the proportion of patients who met the primary outcome exceeding –5%.
Main results: The primary outcome of mRS of either 0 or 1 at 90 to 120 days of treatment occurred in 296 (36.9%) of the 802 patients assigned to tenecteplase and 266 (34.8%) of the 765 patients assigned to alteplase (unadjusted risk difference, 2.1%; 95% CI, –2.6 to 6.9). The prespecified noninferiority threshold was met. There were no significant differences between the groups in rates of intracerebral hemorrhage at 24 hours or 90-day all-cause mortality.
Conclusion: Intravenous tenecteplase is a reasonable alternative to alteplase for patients eligible for thrombolytic therapy.
Study 2 Overview (Wang et al)
Objective: To determine whether tenecteplase (dose 0.25 mg/kg) is noninferior to alteplase in patients with acute ischemic stroke who are within 4.5 hours of symptom onset and eligible for thrombolytic therapy but either refused or were ineligible for endovascular thrombectomy.
Design: Multicenter, prospective, open-label, randomized, controlled noninferiority trial.
Setting and participants: This trial was conducted at 53 centers across China and included patients 18 years of age or older who were within 4.5 hours of symptom onset and were thrombolytic eligible, had a mRS ≤ 1 at enrollment, and had a National Institutes of Health Stroke Scale score between 5 and 25. Eligible participants were randomized 1:1 to either tenecteplase 0.25 mg/kg (maximum dose 25 mg) or alteplase 0.9 mg/kg (maximum dose 90 mg, administered as a bolus followed by infusion). During the enrollment period (June 12, 2021, to May 29, 2022), a total of 1430 participants were enrolled, and, of those, 716 were randomly assigned to tenecteplase and 714 to alteplase. Six patients assigned to tenecteplase and 7 assigned to alteplase did not receive drugs. At 90 days, 5 in the tenecteplase group and 11 in the alteplase group were lost to follow up.
Main outcome measures: The primary efficacy outcome was a mRS of 0 or 1 at 90 days. The primary safety outcome was intracranial hemorrhage within 36 hours. Safety outcomes included parenchymal hematoma 2, as defined by the European Cooperative Acute Stroke Study III; any intracranial or significant hemorrhage, as defined by the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries criteria; and death from all causes at 90 days. Noninferiority for tenecteplase would be declared if the lower 97.5% 1-sided CI for the relative risk (RR) for the primary outcome did not cross 0.937.
Main results: In the modified ITT population, the primary outcome occurred in 439 (62%) of the tenecteplase group and 405 (68%) of the alteplase group (RR, 1.07; 95% CI, 0.98-1.16). This met the prespecified margin for noninferiority. Intracranial hemorrhage within 36 hours was experienced by 15 (2%) patients in the tenecteplase group and 13 (2%) in the alteplase group (RR, 1.18; 95% CI, 0.56-2.50). Death at 90 days occurred in 46 (7%) patients in the tenecteplase group and 35 (5%) in the alteplase group (RR, 1.31; 95% CI, 0.86-2.01).
Conclusion: Tenecteplase was noninferior to alteplase in patients with acute ischemic stroke who met criteria for thrombolysis and either refused or were ineligible for endovascular thrombectomy.
Commentary
Alteplase has been FDA-approved for managing acute ischemic stroke since 1996 and has demonstrated positive effects on functional outcomes. Drawbacks of alteplase therapy, however, include bleeding risk as well as cumbersome administration of a bolus dose followed by a 60-minute infusion. In recent years, the question of whether or not tenecteplase could replace alteplase as the preferred thrombolytic for acute ischemic stroke has garnered much attention. Several features of tenecteplase make it an attractive option, including increased fibrin specificity, a longer half-life, and ease of administration as a single, rapid bolus dose. In phase 2 trials that compared tenecteplase 0.25 mg/kg with alteplase, findings suggested the potential for early neurological improvement as well as improved outcomes at 90 days. While the role of tenecteplase in acute myocardial infarction has been well established due to ease of use and a favorable adverse-effect profile,1 there is much less evidence from phase 3 randomized controlled clinical trials to secure the role of tenecteplase in acute ischemic stroke.2
Menon et al attempted to close this gap in the literature by conducting a randomized controlled clinical trial (AcT) comparing tenecteplase to alteplase in a Canadian patient population. The trial's patient population mirrors that of real-world data from global registries in terms of age, sex, and baseline stroke severity. In addition, the eligibility window of 4.5 hours from symptom onset as well as the inclusion and exclusion criteria for therapy are common to those utilized in other countries, making the findings generalizable. There were some limitations to the study, however, including the impact of COVID-19 on recruitment efforts as well as limitations of research infrastructure and staffing, which may have limited enrollment efforts at primary stroke centers. Nonetheless, the authors concluded that their results provide evidence that tenecteplase is comparable to alteplase, with similar functional and safety outcomes.
TRACE-2 focused on an Asian patient population and provided follow up to the dose-ranging TRACE-1 phase 2 trial. TRACE-1 showed that tenecteplase 0.25 mg/kg had a similar safety profile to alteplase 0.9 mg/kg in Chinese patients presenting with acute ischemic stroke. TRACE-2 sought to establish noninferiority of tenecteplase and excluded patients who were ineligible for or refused thrombectomy. Interestingly, the tenecteplase arm, as the authors point out, had numerically greater mortality as well as intracranial hemorrhage, but these differences were not statistically significant between the treatment groups at 90 days. The TRACE-2 results parallel those of AcT, and although there were differences in ethnicity between the 2 trials, the authors cite this as evidence that the results are consistent and provide evidence for the role of tenecteplase in the management of acute ischemic stroke. Limitations of this trial include potential bias from its open-label design, as well as exclusion of patients with more severe strokes eligible for thrombectomy, which may limit generalizability to patients with more disabling strokes who could have a higher risk of intracranial hemorrhage.
Application for Clinical Practice and System Implementation
Across the country, many organizations have adopted the off-label use of tenecteplase for managing fibrinolytic-eligible acute ischemic stroke patients. In most cases, the impetus for change is the ease of dosing and administration of tenecteplase compared to alteplase, while the inclusion and exclusion criteria and overall management remain the same. Timely administration of therapy in stroke is critical. This, along with other time constraints in stroke workflows, the weight-based calculation of alteplase doses, and alteplase’s administration method may lead to medication errors when using this agent to treat patients with acute stroke. The rapid, single-dose administration of tenecteplase removes many barriers that hospitals face when patients may need to be treated and then transferred to another site for further care. Without the worry to “drip and ship,” the completion of administration may allow for timely patient transfer and eliminate the need for monitoring of an infusion during transfer. For some organizations, there may be a potential for drug cost-savings as well as improved metrics, such as door-to-needle time, but the overall effects of switching from alteplase to tenecteplase remain to be seen. Currently, tenecteplase is included in stroke guidelines as a “reasonable choice,” though with a low level of evidence.3 However, these 2 studies support the role of tenecteplase in acute ischemic stroke treatment and may provide a foundation for further studies to establish the role of tenecteplase in the acute ischemic stroke population.
Practice Points
- Tenecteplase may be considered as an alternative to alteplase for acute ischemic stroke for patients who meet eligibility criteria for thrombolytics; this recommendation is included in the most recent stroke guidelines, although tenecteplase has not been demonstrated to be superior to alteplase.
- The ease of administration of tenecteplase as a single intravenous bolus dose represents a benefit compared to alteplase; it is an off-label use, however, and further studies are needed to establish the superiority of tenecteplase in terms of functional and safety outcomes.
– Carol Heunisch, PharmD, BCPS, BCCP
Pharmacy Department, NorthShore–Edward-Elmhurst Health, Evanston, IL
Study 1 Overview (Menon et al)
Objective: To determine whether a 0.25 mg/kg dose of intravenous tenecteplase is noninferior to intravenous alteplase 0.9 mg/kg for patients with acute ischemic stroke eligible for thrombolytic therapy.
Design: Multicenter, parallel-group, open-label randomized controlled trial.
Setting and participants: The trial was conducted at 22 primary and comprehensive stroke centers across Canada. A primary stroke center was defined as a hospital capable of offering intravenous thrombolysis to patients with acute ischemic stroke, while a comprehensive stroke center was able to offer thrombectomy services in addition. The involved centers also participated in Canadian quality improvement registries (either Quality Improvement and Clinical Research [QuiCR] or Optimizing Patient Treatment in Major Ischemic Stroke with EVT [OPTIMISE]) that track patient outcomes. Patients were eligible for inclusion if they were aged 18 years or older, had a diagnosis of acute ischemic stroke, presented within 4.5 hours of symptom onset, and were eligible for thrombolysis according to Canadian guidelines.
Patients were randomized in a 1:1 fashion to either intravenous tenecteplase (0.25 mg/kg single dose, maximum of 25 mg) or intravenous alteplase (0.9 mg/kg total dose to a maximum of 90 mg, delivered as a bolus followed by a continuous infusion). A total of 1600 patients were enrolled, with 816 randomly assigned to the tenecteplase arm and 784 to the alteplase arm; 1577 patients were included in the intention-to-treat (ITT) analysis (n = 806 tenecteplase; n = 771 alteplase). The median age of enrollees was 74 years, and 52.1% of the ITT population were men.
Main outcome measures: In the ITT population, the primary outcome measure was a modified Rankin score (mRS) of 0 or 1 at 90 to 120 days post treatment. Safety outcomes included symptomatic intracerebral hemorrhage, orolingual angioedema, extracranial bleeding that required blood transfusion (all within 24 hours of thrombolytic administration), and all-cause mortality at 90 days. The noninferiority threshold for intravenous tenecteplase was set as the lower 95% CI of the difference between the tenecteplase and alteplase groups in the proportion of patients who met the primary outcome exceeding –5%.
Main results: The primary outcome of mRS of either 0 or 1 at 90 to 120 days of treatment occurred in 296 (36.9%) of the 802 patients assigned to tenecteplase and 266 (34.8%) of the 765 patients assigned to alteplase (unadjusted risk difference, 2.1%; 95% CI, –2.6 to 6.9). The prespecified noninferiority threshold was met. There were no significant differences between the groups in rates of intracerebral hemorrhage at 24 hours or 90-day all-cause mortality.
Conclusion: Intravenous tenecteplase is a reasonable alternative to alteplase for patients eligible for thrombolytic therapy.
Study 2 Overview (Wang et al)
Objective: To determine whether tenecteplase (dose 0.25 mg/kg) is noninferior to alteplase in patients with acute ischemic stroke who are within 4.5 hours of symptom onset and eligible for thrombolytic therapy but either refused or were ineligible for endovascular thrombectomy.
Design: Multicenter, prospective, open-label, randomized, controlled noninferiority trial.
Setting and participants: This trial was conducted at 53 centers across China and included patients 18 years of age or older who were within 4.5 hours of symptom onset and were thrombolytic eligible, had a mRS ≤ 1 at enrollment, and had a National Institutes of Health Stroke Scale score between 5 and 25. Eligible participants were randomized 1:1 to either tenecteplase 0.25 mg/kg (maximum dose 25 mg) or alteplase 0.9 mg/kg (maximum dose 90 mg, administered as a bolus followed by infusion). During the enrollment period (June 12, 2021, to May 29, 2022), a total of 1430 participants were enrolled, and, of those, 716 were randomly assigned to tenecteplase and 714 to alteplase. Six patients assigned to tenecteplase and 7 assigned to alteplase did not receive drugs. At 90 days, 5 in the tenecteplase group and 11 in the alteplase group were lost to follow up.
Main outcome measures: The primary efficacy outcome was a mRS of 0 or 1 at 90 days. The primary safety outcome was intracranial hemorrhage within 36 hours. Safety outcomes included parenchymal hematoma 2, as defined by the European Cooperative Acute Stroke Study III; any intracranial or significant hemorrhage, as defined by the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries criteria; and death from all causes at 90 days. Noninferiority for tenecteplase would be declared if the lower 97.5% 1-sided CI for the relative risk (RR) for the primary outcome did not cross 0.937.
Main results: In the modified ITT population, the primary outcome occurred in 439 (62%) of the tenecteplase group and 405 (68%) of the alteplase group (RR, 1.07; 95% CI, 0.98-1.16). This met the prespecified margin for noninferiority. Intracranial hemorrhage within 36 hours was experienced by 15 (2%) patients in the tenecteplase group and 13 (2%) in the alteplase group (RR, 1.18; 95% CI, 0.56-2.50). Death at 90 days occurred in 46 (7%) patients in the tenecteplase group and 35 (5%) in the alteplase group (RR, 1.31; 95% CI, 0.86-2.01).
Conclusion: Tenecteplase was noninferior to alteplase in patients with acute ischemic stroke who met criteria for thrombolysis and either refused or were ineligible for endovascular thrombectomy.
Commentary
Alteplase has been FDA-approved for managing acute ischemic stroke since 1996 and has demonstrated positive effects on functional outcomes. Drawbacks of alteplase therapy, however, include bleeding risk as well as cumbersome administration of a bolus dose followed by a 60-minute infusion. In recent years, the question of whether or not tenecteplase could replace alteplase as the preferred thrombolytic for acute ischemic stroke has garnered much attention. Several features of tenecteplase make it an attractive option, including increased fibrin specificity, a longer half-life, and ease of administration as a single, rapid bolus dose. In phase 2 trials that compared tenecteplase 0.25 mg/kg with alteplase, findings suggested the potential for early neurological improvement as well as improved outcomes at 90 days. While the role of tenecteplase in acute myocardial infarction has been well established due to ease of use and a favorable adverse-effect profile,1 there is much less evidence from phase 3 randomized controlled clinical trials to secure the role of tenecteplase in acute ischemic stroke.2
Menon et al attempted to close this gap in the literature by conducting a randomized controlled clinical trial (AcT) comparing tenecteplase to alteplase in a Canadian patient population. The trial's patient population mirrors that of real-world data from global registries in terms of age, sex, and baseline stroke severity. In addition, the eligibility window of 4.5 hours from symptom onset as well as the inclusion and exclusion criteria for therapy are common to those utilized in other countries, making the findings generalizable. There were some limitations to the study, however, including the impact of COVID-19 on recruitment efforts as well as limitations of research infrastructure and staffing, which may have limited enrollment efforts at primary stroke centers. Nonetheless, the authors concluded that their results provide evidence that tenecteplase is comparable to alteplase, with similar functional and safety outcomes.
TRACE-2 focused on an Asian patient population and provided follow up to the dose-ranging TRACE-1 phase 2 trial. TRACE-1 showed that tenecteplase 0.25 mg/kg had a similar safety profile to alteplase 0.9 mg/kg in Chinese patients presenting with acute ischemic stroke. TRACE-2 sought to establish noninferiority of tenecteplase and excluded patients who were ineligible for or refused thrombectomy. Interestingly, the tenecteplase arm, as the authors point out, had numerically greater mortality as well as intracranial hemorrhage, but these differences were not statistically significant between the treatment groups at 90 days. The TRACE-2 results parallel those of AcT, and although there were differences in ethnicity between the 2 trials, the authors cite this as evidence that the results are consistent and provide evidence for the role of tenecteplase in the management of acute ischemic stroke. Limitations of this trial include potential bias from its open-label design, as well as exclusion of patients with more severe strokes eligible for thrombectomy, which may limit generalizability to patients with more disabling strokes who could have a higher risk of intracranial hemorrhage.
Application for Clinical Practice and System Implementation
Across the country, many organizations have adopted the off-label use of tenecteplase for managing fibrinolytic-eligible acute ischemic stroke patients. In most cases, the impetus for change is the ease of dosing and administration of tenecteplase compared to alteplase, while the inclusion and exclusion criteria and overall management remain the same. Timely administration of therapy in stroke is critical. This, along with other time constraints in stroke workflows, the weight-based calculation of alteplase doses, and alteplase’s administration method may lead to medication errors when using this agent to treat patients with acute stroke. The rapid, single-dose administration of tenecteplase removes many barriers that hospitals face when patients may need to be treated and then transferred to another site for further care. Without the worry to “drip and ship,” the completion of administration may allow for timely patient transfer and eliminate the need for monitoring of an infusion during transfer. For some organizations, there may be a potential for drug cost-savings as well as improved metrics, such as door-to-needle time, but the overall effects of switching from alteplase to tenecteplase remain to be seen. Currently, tenecteplase is included in stroke guidelines as a “reasonable choice,” though with a low level of evidence.3 However, these 2 studies support the role of tenecteplase in acute ischemic stroke treatment and may provide a foundation for further studies to establish the role of tenecteplase in the acute ischemic stroke population.
Practice Points
- Tenecteplase may be considered as an alternative to alteplase for acute ischemic stroke for patients who meet eligibility criteria for thrombolytics; this recommendation is included in the most recent stroke guidelines, although tenecteplase has not been demonstrated to be superior to alteplase.
- The ease of administration of tenecteplase as a single intravenous bolus dose represents a benefit compared to alteplase; it is an off-label use, however, and further studies are needed to establish the superiority of tenecteplase in terms of functional and safety outcomes.
– Carol Heunisch, PharmD, BCPS, BCCP
Pharmacy Department, NorthShore–Edward-Elmhurst Health, Evanston, IL
1. Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators; F Van De Werf, J Adgey, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716-722. doi:10.1016/s0140-6736(99)07403-6
2. Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischaemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50(8):2156-2162. doi:10.1161/STROKEAHA.119.025080
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi:10.1161/STR.0000000000000211
1. Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators; F Van De Werf, J Adgey, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716-722. doi:10.1016/s0140-6736(99)07403-6
2. Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischaemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50(8):2156-2162. doi:10.1161/STROKEAHA.119.025080
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi:10.1161/STR.0000000000000211
The Role of Revascularization and Viability Testing in Patients With Multivessel Coronary Artery Disease and Severely Reduced Ejection Fraction
Study 1 Overview (STICHES Investigators)
Objective: To assess the survival benefit of coronary-artery bypass grafting (CABG) added to guideline-directed medical therapy, compared to optimal medical therapy (OMT) alone, in patients with coronary artery disease, heart failure, and severe left ventricular dysfunction. Design: Multicenter, randomized, prospective study with extended follow-up (median duration of 9.8 years).
Setting and participants: A total of 1212 patients with left ventricular ejection fraction (LVEF) of 35% or less and coronary artery disease were randomized to medical therapy plus CABG or OMT alone at 127 clinical sites in 26 countries.
Main outcome measures: The primary endpoint was death from any cause. Main secondary endpoints were death from cardiovascular causes and a composite outcome of death from any cause or hospitalization for cardiovascular causes.
Main results: There were 359 primary outcome all-cause deaths (58.9%) in the CABG group and 398 (66.1%) in the medical therapy group (hazard ratio [HR], 0.84; 95% CI, 0.73-0.97; P = .02). Death from cardiovascular causes was reported in 247 patients (40.5%) in the CABG group and 297 patients (49.3%) in the medical therapy group (HR, 0.79; 95% CI, 0.66-0.93; P < .01). The composite outcome of death from any cause or hospitalization for cardiovascular causes occurred in 467 patients (76.6%) in the CABG group and 467 patients (87.0%) in the medical therapy group (HR, 0.72; 95% CI, 0.64-0.82; P < .01).
Conclusion: Over a median follow-up of 9.8 years in patients with ischemic cardiomyopathy with severely reduced ejection fraction, the rates of death from any cause, death from cardiovascular causes, and the composite of death from any cause or hospitalization for cardiovascular causes were significantly lower in patients undergoing CABG than in patients receiving medical therapy alone.
Study 2 Overview (REVIVED BCIS Trial Group)
Objective: To assess whether percutaneous coronary intervention (PCI) can improve survival and left ventricular function in patients with severe left ventricular systolic dysfunction as compared to OMT alone.
Design: Multicenter, randomized, prospective study.
Setting and participants: A total of 700 patients with LVEF <35% with severe coronary artery disease amendable to PCI and demonstrable myocardial viability were randomly assigned to either PCI plus optimal medical therapy (PCI group) or OMT alone (OMT group).
Main outcome measures: The primary outcome was death from any cause or hospitalization for heart failure. The main secondary outcomes were LVEF at 6 and 12 months and quality of life (QOL) scores.
Main results: Over a median follow-up of 41 months, the primary outcome was reported in 129 patients (37.2%) in the PCI group and in 134 patients (38.0%) in the OMT group (HR, 0.99; 95% CI, 0.78-1.27; P = .96). The LVEF was similar in the 2 groups at 6 months (mean difference, –1.6 percentage points; 95% CI, –3.7 to 0.5) and at 12 months (mean difference, 0.9 percentage points; 95% CI, –1.7 to 3.4). QOL scores at 6 and 12 months favored the PCI group, but the difference had diminished at 24 months.
Conclusion: In patients with severe ischemic cardiomyopathy, revascularization by PCI in addition to OMT did not result in a lower incidence of death from any cause or hospitalization from heart failure.
Commentary
Coronary artery disease is the most common cause of heart failure with reduced ejection fraction and an important cause of mortality.1 Patients with ischemic cardiomyopathy with reduced ejection fraction are often considered for revascularization in addition to OMT and device therapies. Although there have been multiple retrospective studies and registries suggesting that cardiac outcomes and LVEF improve with revascularization, the number of large-scale prospective studies that assessed this clinical question and randomized patients to revascularization plus OMT compared to OMT alone has been limited.
In the Surgical Treatment for Ischemic Heart Failure (STICH) study,2,3 eligible patients had coronary artery disease amendable to CABG and a LVEF of 35% or less. Patients (N = 1212) were randomly assigned to CABG plus OMT or OMT alone between July 2002 and May 2007. The original study, with a median follow-up of 5 years, did not show survival benefit, but the investigators reported that the primary outcome of death from any cause was significantly lower in the CABG group compared to OMT alone when follow-up of the same study population was extended to 9.8 years (58.9% vs 66.1%, P = .02). The findings from this study led to a class I guideline recommendation of CABG over medical therapy in patients with multivessel disease and low ejection fraction.4
Since the STICH trial was designed, there have been significant improvements in devices and techniques used for PCI, and the procedure is now widely performed in patients with multivessel disease.5 The advantages of PCI over CABG include shorter recovery times and lower risk of immediate complications. In this context, the recently reported Revascularization for Ischemic Ventricular Dysfunction (REVIVED) study assessed clinical outcomes in patients with severe coronary artery disease and reduced ejection fraction by randomizing patients to either PCI with OMT or OMT alone.6 At a median follow-up of 3.5 years, the investigators found no difference in the primary outcome of death from any cause or hospitalization for heart failure (37.2% vs 38.0%; 95% CI, 0.78-1.28; P = .96). Moreover, the degree of LVEF improvement, assessed by follow-up echocardiogram read by the core lab, showed no difference in the degree of LVEF improvement between groups at 6 and 12 months. Finally, although results of the QOL assessment using the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated, patient-reported, heart-failure-specific QOL scale, favored the PCI group at 6 and 12 months of follow-up, the difference had diminished at 24 months.
The main strength of the REVIVED study was that it targeted a patient population with severe coronary artery disease, including left main disease and severely reduced ejection fraction, that historically have been excluded from large-scale randomized controlled studies evaluating PCI with OMT compared to OMT alone.7 However, there are several points to consider when interpreting the results of this study. First, further details of the PCI procedures are necessary. The REVIVED study recommended revascularization of all territories with viable myocardium; the anatomical revascularization index utilizing the British Cardiovascular Intervention Society (BCIS) Jeopardy Score was 71%. It is important to note that this jeopardy score was operator-reported and the core-lab adjudicated anatomical revascularization rate may be lower. Although viability testing primarily utilizing cardiac magnetic resonance imaging was performed in most patients, correlation between the revascularization territory and the viable segments has yet to be reported. Moreover, procedural details such as use of intravascular ultrasound and physiological testing, known to improve clinical outcome, need to be reported.8,9
Second, there is a high prevalence of ischemic cardiomyopathy, and it is important to note that the patients included in this study were highly selected from daily clinical practice, as evidenced by the prolonged enrollment period (8 years). Individuals were largely stable patients with less complex coronary anatomy as evidenced by the median interval from angiography to randomization of 80 days. Taking into consideration the degree of left ventricular dysfunction for patients included in the trial, only 14% of the patients had left main disease and half of the patients only had 2-vessel disease. The severity of the left main disease also needs to be clarified as it is likely that patients the operator determined to be critical were not enrolled in the study. Furthermore, the standard of care based on the STICH trial is to refer patients with severe multivessel coronary artery disease to CABG, making it more likely that patients with more severe and complex disease were not included in this trial. It is also important to note that this study enrolled patients with stable ischemic heart disease, and the data do not apply to patients presenting with acute coronary syndrome.
Third, although the primary outcome was similar between the groups, the secondary outcome of unplanned revascularization was lower in the PCI group. In addition, the rate of acute myocardial infarction (MI) was similar between the 2 groups, but the rate of spontaneous MI was lower in the PCI group compared to the OMT group (5.2% vs 9.3%) as 40% of MI cases in the PCI group were periprocedural MIs. The correlation between periprocedural MI and long-term outcomes has been modest compared to spontaneous MI. Moreover, with the longer follow-up, the number of spontaneous MI cases is expected to rise while the number of periprocedural MI cases is not. Extending the follow-up period is also important, as the STICH extension trial showed a statistically significant difference at 10-year follow up despite negative results at the time of the original publication.
Fourth, the REVIVED trial randomized a significantly lower number of patients compared to the STICH trial, and the authors reported fewer primary-outcome events than the estimated number needed to achieve the power to assess the primary hypothesis. In addition, significant improvements in medical treatment for heart failure with reduced ejection fraction since the STICH trial make comparison of PCI vs CABG in this patient population unfeasible.
Finally, although severe angina was not an exclusion criterion, two-thirds of the patients enrolled had no angina, and only 2% of the patients had baseline severe angina. This is important to consider when interpreting the results of the patient-reported health status as previous studies have shown that patients with worse angina at baseline derive the largest improvement in their QOL,10,11 and symptom improvement is the main indication for PCI in patients with stable ischemic heart disease.
Applications for Clinical Practice and System Implementation
In patients with severe left ventricular systolic dysfunction and multivessel stable ischemic heart disease who are well compensated and have little or no angina at baseline, OMT alone as an initial strategy may be considered against the addition of PCI after careful risk and benefit discussion. Further details about revascularization and extended follow-up data from the REVIVED trial are necessary.
Practice Points
- Patients with ischemic cardiomyopathy with reduced ejection fraction have been an understudied population in previous studies.
- Further studies are necessary to understand the benefits of revascularization and the role of viability testing in this population.
– Taishi Hirai MD, and Ziad Sayed Ahmad, MD
University of Missouri, Columbia, MO
1. Nowbar AN, Gitto M, Howard JP, et al. Mortality from ischemic heart disease. Circ Cardiovasc Qual Outcomes. 2019;12(6):e005375. doi:10.1161/CIRCOUTCOMES
2. Velazquez EJ, Lee KL, Deja MA, et al; for the STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364(17):1607-1616. doi:10.1056/NEJMoa1100356
3. Velazquez EJ, Lee KL, Jones RH, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511-1520. doi:10.1056/NEJMoa1602001
4. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(2):e21-e129. doi:10.1016/j.jacc.2021.09.006
5. Kirtane AJ, Doshi D, Leon MB, et al. Treatment of higher-risk patients with an indication for revascularization: evolution within the field of contemporary percutaneous coronary intervention. Circulation. 2016;134(5):422-431. doi:10.1161/CIRCULATIONAHA
6. Perera D, Clayton T, O’Kane PD, et al. Percutaneous revascularization for ischemic left ventricular dysfunction. N Engl J Med. 2022;387(15):1351-1360. doi:10.1056/NEJMoa2206606
7. Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. Circulation. 2020;142(18):1725-1735. doi:10.1161/CIRCULATIONAHA
8. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991-1001. doi:10.1056/NEJMoa1205361
9. Zhang J, Gao X, Kan J, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: The ULTIMATE trial. J Am Coll Cardiol. 2018;72(24):3126-3137. doi:10.1016/j.jacc.2018.09.013
10. Spertus JA, Jones PG, Maron DJ, et al. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med. 2020;382(15):1408-1419. doi:10.1056/NEJMoa1916370
11. Hirai T, Grantham JA, Sapontis J, et al. Quality of life changes after chronic total occlusion angioplasty in patients with baseline refractory angina. Circ Cardiovasc Interv. 2019;12:e007558. doi:10.1161/CIRCINTERVENTIONS.118.007558
Study 1 Overview (STICHES Investigators)
Objective: To assess the survival benefit of coronary-artery bypass grafting (CABG) added to guideline-directed medical therapy, compared to optimal medical therapy (OMT) alone, in patients with coronary artery disease, heart failure, and severe left ventricular dysfunction. Design: Multicenter, randomized, prospective study with extended follow-up (median duration of 9.8 years).
Setting and participants: A total of 1212 patients with left ventricular ejection fraction (LVEF) of 35% or less and coronary artery disease were randomized to medical therapy plus CABG or OMT alone at 127 clinical sites in 26 countries.
Main outcome measures: The primary endpoint was death from any cause. Main secondary endpoints were death from cardiovascular causes and a composite outcome of death from any cause or hospitalization for cardiovascular causes.
Main results: There were 359 primary outcome all-cause deaths (58.9%) in the CABG group and 398 (66.1%) in the medical therapy group (hazard ratio [HR], 0.84; 95% CI, 0.73-0.97; P = .02). Death from cardiovascular causes was reported in 247 patients (40.5%) in the CABG group and 297 patients (49.3%) in the medical therapy group (HR, 0.79; 95% CI, 0.66-0.93; P < .01). The composite outcome of death from any cause or hospitalization for cardiovascular causes occurred in 467 patients (76.6%) in the CABG group and 467 patients (87.0%) in the medical therapy group (HR, 0.72; 95% CI, 0.64-0.82; P < .01).
Conclusion: Over a median follow-up of 9.8 years in patients with ischemic cardiomyopathy with severely reduced ejection fraction, the rates of death from any cause, death from cardiovascular causes, and the composite of death from any cause or hospitalization for cardiovascular causes were significantly lower in patients undergoing CABG than in patients receiving medical therapy alone.
Study 2 Overview (REVIVED BCIS Trial Group)
Objective: To assess whether percutaneous coronary intervention (PCI) can improve survival and left ventricular function in patients with severe left ventricular systolic dysfunction as compared to OMT alone.
Design: Multicenter, randomized, prospective study.
Setting and participants: A total of 700 patients with LVEF <35% with severe coronary artery disease amendable to PCI and demonstrable myocardial viability were randomly assigned to either PCI plus optimal medical therapy (PCI group) or OMT alone (OMT group).
Main outcome measures: The primary outcome was death from any cause or hospitalization for heart failure. The main secondary outcomes were LVEF at 6 and 12 months and quality of life (QOL) scores.
Main results: Over a median follow-up of 41 months, the primary outcome was reported in 129 patients (37.2%) in the PCI group and in 134 patients (38.0%) in the OMT group (HR, 0.99; 95% CI, 0.78-1.27; P = .96). The LVEF was similar in the 2 groups at 6 months (mean difference, –1.6 percentage points; 95% CI, –3.7 to 0.5) and at 12 months (mean difference, 0.9 percentage points; 95% CI, –1.7 to 3.4). QOL scores at 6 and 12 months favored the PCI group, but the difference had diminished at 24 months.
Conclusion: In patients with severe ischemic cardiomyopathy, revascularization by PCI in addition to OMT did not result in a lower incidence of death from any cause or hospitalization from heart failure.
Commentary
Coronary artery disease is the most common cause of heart failure with reduced ejection fraction and an important cause of mortality.1 Patients with ischemic cardiomyopathy with reduced ejection fraction are often considered for revascularization in addition to OMT and device therapies. Although there have been multiple retrospective studies and registries suggesting that cardiac outcomes and LVEF improve with revascularization, the number of large-scale prospective studies that assessed this clinical question and randomized patients to revascularization plus OMT compared to OMT alone has been limited.
In the Surgical Treatment for Ischemic Heart Failure (STICH) study,2,3 eligible patients had coronary artery disease amendable to CABG and a LVEF of 35% or less. Patients (N = 1212) were randomly assigned to CABG plus OMT or OMT alone between July 2002 and May 2007. The original study, with a median follow-up of 5 years, did not show survival benefit, but the investigators reported that the primary outcome of death from any cause was significantly lower in the CABG group compared to OMT alone when follow-up of the same study population was extended to 9.8 years (58.9% vs 66.1%, P = .02). The findings from this study led to a class I guideline recommendation of CABG over medical therapy in patients with multivessel disease and low ejection fraction.4
Since the STICH trial was designed, there have been significant improvements in devices and techniques used for PCI, and the procedure is now widely performed in patients with multivessel disease.5 The advantages of PCI over CABG include shorter recovery times and lower risk of immediate complications. In this context, the recently reported Revascularization for Ischemic Ventricular Dysfunction (REVIVED) study assessed clinical outcomes in patients with severe coronary artery disease and reduced ejection fraction by randomizing patients to either PCI with OMT or OMT alone.6 At a median follow-up of 3.5 years, the investigators found no difference in the primary outcome of death from any cause or hospitalization for heart failure (37.2% vs 38.0%; 95% CI, 0.78-1.28; P = .96). Moreover, the degree of LVEF improvement, assessed by follow-up echocardiogram read by the core lab, showed no difference in the degree of LVEF improvement between groups at 6 and 12 months. Finally, although results of the QOL assessment using the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated, patient-reported, heart-failure-specific QOL scale, favored the PCI group at 6 and 12 months of follow-up, the difference had diminished at 24 months.
The main strength of the REVIVED study was that it targeted a patient population with severe coronary artery disease, including left main disease and severely reduced ejection fraction, that historically have been excluded from large-scale randomized controlled studies evaluating PCI with OMT compared to OMT alone.7 However, there are several points to consider when interpreting the results of this study. First, further details of the PCI procedures are necessary. The REVIVED study recommended revascularization of all territories with viable myocardium; the anatomical revascularization index utilizing the British Cardiovascular Intervention Society (BCIS) Jeopardy Score was 71%. It is important to note that this jeopardy score was operator-reported and the core-lab adjudicated anatomical revascularization rate may be lower. Although viability testing primarily utilizing cardiac magnetic resonance imaging was performed in most patients, correlation between the revascularization territory and the viable segments has yet to be reported. Moreover, procedural details such as use of intravascular ultrasound and physiological testing, known to improve clinical outcome, need to be reported.8,9
Second, there is a high prevalence of ischemic cardiomyopathy, and it is important to note that the patients included in this study were highly selected from daily clinical practice, as evidenced by the prolonged enrollment period (8 years). Individuals were largely stable patients with less complex coronary anatomy as evidenced by the median interval from angiography to randomization of 80 days. Taking into consideration the degree of left ventricular dysfunction for patients included in the trial, only 14% of the patients had left main disease and half of the patients only had 2-vessel disease. The severity of the left main disease also needs to be clarified as it is likely that patients the operator determined to be critical were not enrolled in the study. Furthermore, the standard of care based on the STICH trial is to refer patients with severe multivessel coronary artery disease to CABG, making it more likely that patients with more severe and complex disease were not included in this trial. It is also important to note that this study enrolled patients with stable ischemic heart disease, and the data do not apply to patients presenting with acute coronary syndrome.
Third, although the primary outcome was similar between the groups, the secondary outcome of unplanned revascularization was lower in the PCI group. In addition, the rate of acute myocardial infarction (MI) was similar between the 2 groups, but the rate of spontaneous MI was lower in the PCI group compared to the OMT group (5.2% vs 9.3%) as 40% of MI cases in the PCI group were periprocedural MIs. The correlation between periprocedural MI and long-term outcomes has been modest compared to spontaneous MI. Moreover, with the longer follow-up, the number of spontaneous MI cases is expected to rise while the number of periprocedural MI cases is not. Extending the follow-up period is also important, as the STICH extension trial showed a statistically significant difference at 10-year follow up despite negative results at the time of the original publication.
Fourth, the REVIVED trial randomized a significantly lower number of patients compared to the STICH trial, and the authors reported fewer primary-outcome events than the estimated number needed to achieve the power to assess the primary hypothesis. In addition, significant improvements in medical treatment for heart failure with reduced ejection fraction since the STICH trial make comparison of PCI vs CABG in this patient population unfeasible.
Finally, although severe angina was not an exclusion criterion, two-thirds of the patients enrolled had no angina, and only 2% of the patients had baseline severe angina. This is important to consider when interpreting the results of the patient-reported health status as previous studies have shown that patients with worse angina at baseline derive the largest improvement in their QOL,10,11 and symptom improvement is the main indication for PCI in patients with stable ischemic heart disease.
Applications for Clinical Practice and System Implementation
In patients with severe left ventricular systolic dysfunction and multivessel stable ischemic heart disease who are well compensated and have little or no angina at baseline, OMT alone as an initial strategy may be considered against the addition of PCI after careful risk and benefit discussion. Further details about revascularization and extended follow-up data from the REVIVED trial are necessary.
Practice Points
- Patients with ischemic cardiomyopathy with reduced ejection fraction have been an understudied population in previous studies.
- Further studies are necessary to understand the benefits of revascularization and the role of viability testing in this population.
– Taishi Hirai MD, and Ziad Sayed Ahmad, MD
University of Missouri, Columbia, MO
Study 1 Overview (STICHES Investigators)
Objective: To assess the survival benefit of coronary-artery bypass grafting (CABG) added to guideline-directed medical therapy, compared to optimal medical therapy (OMT) alone, in patients with coronary artery disease, heart failure, and severe left ventricular dysfunction. Design: Multicenter, randomized, prospective study with extended follow-up (median duration of 9.8 years).
Setting and participants: A total of 1212 patients with left ventricular ejection fraction (LVEF) of 35% or less and coronary artery disease were randomized to medical therapy plus CABG or OMT alone at 127 clinical sites in 26 countries.
Main outcome measures: The primary endpoint was death from any cause. Main secondary endpoints were death from cardiovascular causes and a composite outcome of death from any cause or hospitalization for cardiovascular causes.
Main results: There were 359 primary outcome all-cause deaths (58.9%) in the CABG group and 398 (66.1%) in the medical therapy group (hazard ratio [HR], 0.84; 95% CI, 0.73-0.97; P = .02). Death from cardiovascular causes was reported in 247 patients (40.5%) in the CABG group and 297 patients (49.3%) in the medical therapy group (HR, 0.79; 95% CI, 0.66-0.93; P < .01). The composite outcome of death from any cause or hospitalization for cardiovascular causes occurred in 467 patients (76.6%) in the CABG group and 467 patients (87.0%) in the medical therapy group (HR, 0.72; 95% CI, 0.64-0.82; P < .01).
Conclusion: Over a median follow-up of 9.8 years in patients with ischemic cardiomyopathy with severely reduced ejection fraction, the rates of death from any cause, death from cardiovascular causes, and the composite of death from any cause or hospitalization for cardiovascular causes were significantly lower in patients undergoing CABG than in patients receiving medical therapy alone.
Study 2 Overview (REVIVED BCIS Trial Group)
Objective: To assess whether percutaneous coronary intervention (PCI) can improve survival and left ventricular function in patients with severe left ventricular systolic dysfunction as compared to OMT alone.
Design: Multicenter, randomized, prospective study.
Setting and participants: A total of 700 patients with LVEF <35% with severe coronary artery disease amendable to PCI and demonstrable myocardial viability were randomly assigned to either PCI plus optimal medical therapy (PCI group) or OMT alone (OMT group).
Main outcome measures: The primary outcome was death from any cause or hospitalization for heart failure. The main secondary outcomes were LVEF at 6 and 12 months and quality of life (QOL) scores.
Main results: Over a median follow-up of 41 months, the primary outcome was reported in 129 patients (37.2%) in the PCI group and in 134 patients (38.0%) in the OMT group (HR, 0.99; 95% CI, 0.78-1.27; P = .96). The LVEF was similar in the 2 groups at 6 months (mean difference, –1.6 percentage points; 95% CI, –3.7 to 0.5) and at 12 months (mean difference, 0.9 percentage points; 95% CI, –1.7 to 3.4). QOL scores at 6 and 12 months favored the PCI group, but the difference had diminished at 24 months.
Conclusion: In patients with severe ischemic cardiomyopathy, revascularization by PCI in addition to OMT did not result in a lower incidence of death from any cause or hospitalization from heart failure.
Commentary
Coronary artery disease is the most common cause of heart failure with reduced ejection fraction and an important cause of mortality.1 Patients with ischemic cardiomyopathy with reduced ejection fraction are often considered for revascularization in addition to OMT and device therapies. Although there have been multiple retrospective studies and registries suggesting that cardiac outcomes and LVEF improve with revascularization, the number of large-scale prospective studies that assessed this clinical question and randomized patients to revascularization plus OMT compared to OMT alone has been limited.
In the Surgical Treatment for Ischemic Heart Failure (STICH) study,2,3 eligible patients had coronary artery disease amendable to CABG and a LVEF of 35% or less. Patients (N = 1212) were randomly assigned to CABG plus OMT or OMT alone between July 2002 and May 2007. The original study, with a median follow-up of 5 years, did not show survival benefit, but the investigators reported that the primary outcome of death from any cause was significantly lower in the CABG group compared to OMT alone when follow-up of the same study population was extended to 9.8 years (58.9% vs 66.1%, P = .02). The findings from this study led to a class I guideline recommendation of CABG over medical therapy in patients with multivessel disease and low ejection fraction.4
Since the STICH trial was designed, there have been significant improvements in devices and techniques used for PCI, and the procedure is now widely performed in patients with multivessel disease.5 The advantages of PCI over CABG include shorter recovery times and lower risk of immediate complications. In this context, the recently reported Revascularization for Ischemic Ventricular Dysfunction (REVIVED) study assessed clinical outcomes in patients with severe coronary artery disease and reduced ejection fraction by randomizing patients to either PCI with OMT or OMT alone.6 At a median follow-up of 3.5 years, the investigators found no difference in the primary outcome of death from any cause or hospitalization for heart failure (37.2% vs 38.0%; 95% CI, 0.78-1.28; P = .96). Moreover, the degree of LVEF improvement, assessed by follow-up echocardiogram read by the core lab, showed no difference in the degree of LVEF improvement between groups at 6 and 12 months. Finally, although results of the QOL assessment using the Kansas City Cardiomyopathy Questionnaire (KCCQ), a validated, patient-reported, heart-failure-specific QOL scale, favored the PCI group at 6 and 12 months of follow-up, the difference had diminished at 24 months.
The main strength of the REVIVED study was that it targeted a patient population with severe coronary artery disease, including left main disease and severely reduced ejection fraction, that historically have been excluded from large-scale randomized controlled studies evaluating PCI with OMT compared to OMT alone.7 However, there are several points to consider when interpreting the results of this study. First, further details of the PCI procedures are necessary. The REVIVED study recommended revascularization of all territories with viable myocardium; the anatomical revascularization index utilizing the British Cardiovascular Intervention Society (BCIS) Jeopardy Score was 71%. It is important to note that this jeopardy score was operator-reported and the core-lab adjudicated anatomical revascularization rate may be lower. Although viability testing primarily utilizing cardiac magnetic resonance imaging was performed in most patients, correlation between the revascularization territory and the viable segments has yet to be reported. Moreover, procedural details such as use of intravascular ultrasound and physiological testing, known to improve clinical outcome, need to be reported.8,9
Second, there is a high prevalence of ischemic cardiomyopathy, and it is important to note that the patients included in this study were highly selected from daily clinical practice, as evidenced by the prolonged enrollment period (8 years). Individuals were largely stable patients with less complex coronary anatomy as evidenced by the median interval from angiography to randomization of 80 days. Taking into consideration the degree of left ventricular dysfunction for patients included in the trial, only 14% of the patients had left main disease and half of the patients only had 2-vessel disease. The severity of the left main disease also needs to be clarified as it is likely that patients the operator determined to be critical were not enrolled in the study. Furthermore, the standard of care based on the STICH trial is to refer patients with severe multivessel coronary artery disease to CABG, making it more likely that patients with more severe and complex disease were not included in this trial. It is also important to note that this study enrolled patients with stable ischemic heart disease, and the data do not apply to patients presenting with acute coronary syndrome.
Third, although the primary outcome was similar between the groups, the secondary outcome of unplanned revascularization was lower in the PCI group. In addition, the rate of acute myocardial infarction (MI) was similar between the 2 groups, but the rate of spontaneous MI was lower in the PCI group compared to the OMT group (5.2% vs 9.3%) as 40% of MI cases in the PCI group were periprocedural MIs. The correlation between periprocedural MI and long-term outcomes has been modest compared to spontaneous MI. Moreover, with the longer follow-up, the number of spontaneous MI cases is expected to rise while the number of periprocedural MI cases is not. Extending the follow-up period is also important, as the STICH extension trial showed a statistically significant difference at 10-year follow up despite negative results at the time of the original publication.
Fourth, the REVIVED trial randomized a significantly lower number of patients compared to the STICH trial, and the authors reported fewer primary-outcome events than the estimated number needed to achieve the power to assess the primary hypothesis. In addition, significant improvements in medical treatment for heart failure with reduced ejection fraction since the STICH trial make comparison of PCI vs CABG in this patient population unfeasible.
Finally, although severe angina was not an exclusion criterion, two-thirds of the patients enrolled had no angina, and only 2% of the patients had baseline severe angina. This is important to consider when interpreting the results of the patient-reported health status as previous studies have shown that patients with worse angina at baseline derive the largest improvement in their QOL,10,11 and symptom improvement is the main indication for PCI in patients with stable ischemic heart disease.
Applications for Clinical Practice and System Implementation
In patients with severe left ventricular systolic dysfunction and multivessel stable ischemic heart disease who are well compensated and have little or no angina at baseline, OMT alone as an initial strategy may be considered against the addition of PCI after careful risk and benefit discussion. Further details about revascularization and extended follow-up data from the REVIVED trial are necessary.
Practice Points
- Patients with ischemic cardiomyopathy with reduced ejection fraction have been an understudied population in previous studies.
- Further studies are necessary to understand the benefits of revascularization and the role of viability testing in this population.
– Taishi Hirai MD, and Ziad Sayed Ahmad, MD
University of Missouri, Columbia, MO
1. Nowbar AN, Gitto M, Howard JP, et al. Mortality from ischemic heart disease. Circ Cardiovasc Qual Outcomes. 2019;12(6):e005375. doi:10.1161/CIRCOUTCOMES
2. Velazquez EJ, Lee KL, Deja MA, et al; for the STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364(17):1607-1616. doi:10.1056/NEJMoa1100356
3. Velazquez EJ, Lee KL, Jones RH, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511-1520. doi:10.1056/NEJMoa1602001
4. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(2):e21-e129. doi:10.1016/j.jacc.2021.09.006
5. Kirtane AJ, Doshi D, Leon MB, et al. Treatment of higher-risk patients with an indication for revascularization: evolution within the field of contemporary percutaneous coronary intervention. Circulation. 2016;134(5):422-431. doi:10.1161/CIRCULATIONAHA
6. Perera D, Clayton T, O’Kane PD, et al. Percutaneous revascularization for ischemic left ventricular dysfunction. N Engl J Med. 2022;387(15):1351-1360. doi:10.1056/NEJMoa2206606
7. Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. Circulation. 2020;142(18):1725-1735. doi:10.1161/CIRCULATIONAHA
8. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991-1001. doi:10.1056/NEJMoa1205361
9. Zhang J, Gao X, Kan J, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: The ULTIMATE trial. J Am Coll Cardiol. 2018;72(24):3126-3137. doi:10.1016/j.jacc.2018.09.013
10. Spertus JA, Jones PG, Maron DJ, et al. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med. 2020;382(15):1408-1419. doi:10.1056/NEJMoa1916370
11. Hirai T, Grantham JA, Sapontis J, et al. Quality of life changes after chronic total occlusion angioplasty in patients with baseline refractory angina. Circ Cardiovasc Interv. 2019;12:e007558. doi:10.1161/CIRCINTERVENTIONS.118.007558
1. Nowbar AN, Gitto M, Howard JP, et al. Mortality from ischemic heart disease. Circ Cardiovasc Qual Outcomes. 2019;12(6):e005375. doi:10.1161/CIRCOUTCOMES
2. Velazquez EJ, Lee KL, Deja MA, et al; for the STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364(17):1607-1616. doi:10.1056/NEJMoa1100356
3. Velazquez EJ, Lee KL, Jones RH, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016;374(16):1511-1520. doi:10.1056/NEJMoa1602001
4. Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(2):e21-e129. doi:10.1016/j.jacc.2021.09.006
5. Kirtane AJ, Doshi D, Leon MB, et al. Treatment of higher-risk patients with an indication for revascularization: evolution within the field of contemporary percutaneous coronary intervention. Circulation. 2016;134(5):422-431. doi:10.1161/CIRCULATIONAHA
6. Perera D, Clayton T, O’Kane PD, et al. Percutaneous revascularization for ischemic left ventricular dysfunction. N Engl J Med. 2022;387(15):1351-1360. doi:10.1056/NEJMoa2206606
7. Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. Circulation. 2020;142(18):1725-1735. doi:10.1161/CIRCULATIONAHA
8. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991-1001. doi:10.1056/NEJMoa1205361
9. Zhang J, Gao X, Kan J, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: The ULTIMATE trial. J Am Coll Cardiol. 2018;72(24):3126-3137. doi:10.1016/j.jacc.2018.09.013
10. Spertus JA, Jones PG, Maron DJ, et al. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med. 2020;382(15):1408-1419. doi:10.1056/NEJMoa1916370
11. Hirai T, Grantham JA, Sapontis J, et al. Quality of life changes after chronic total occlusion angioplasty in patients with baseline refractory angina. Circ Cardiovasc Interv. 2019;12:e007558. doi:10.1161/CIRCINTERVENTIONS.118.007558