User login
Are Energy Drinks Causing This Man's Shortness of Breath?
ANSWER
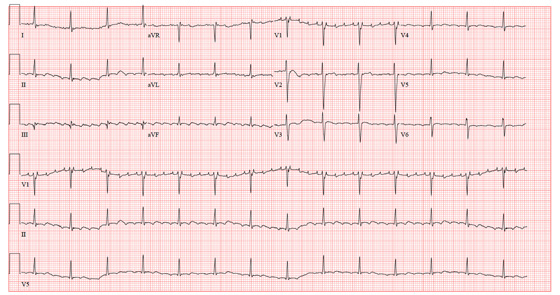
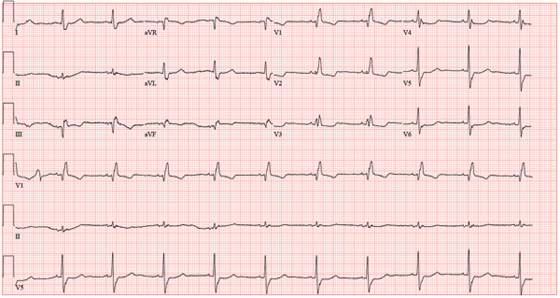
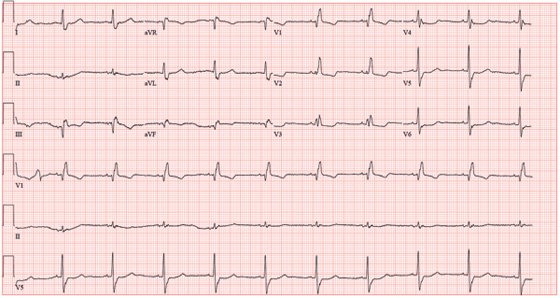
The ECG reveals atrial flutter with a nonspecific T-wave abnormality. The atrial rate is 300 beats/min. The ventricular rate is 84 beats/min; hence the atrial flutter occurs in a 4:1 pattern. (This is best seen in lead V1, where one of the atrial beats is “hidden” in the QRS complex.) The PR interval of 208 ms on the computerized analysis is misleading and illustrates the risk of relying on the computer for a diagnosis. The nonspecific T-wave abnormalities are best seen in leads V2 and V3 and are of no consequence.
While there are no definitive studies that prove that combining energy drinks containing taurine with beverages containing caffeine increases the risk for arrhythmias, there are several anecdotal case reports. In addition to consumption of taurine- and caffeine-containing beverages, this patient is under a significant amount of stress, producing a large catecholaminergic response.
The patient has no prior cardiac history of arrhythmias and no prior cardiac workup. He underwent synchronized cardioversion to restore normal sinus rhythm and was scheduled for an outpatient workup for structural heart disease.
ANSWER
The ECG reveals atrial flutter with a nonspecific T-wave abnormality. The atrial rate is 300 beats/min. The ventricular rate is 84 beats/min; hence the atrial flutter occurs in a 4:1 pattern. (This is best seen in lead V1, where one of the atrial beats is “hidden” in the QRS complex.) The PR interval of 208 ms on the computerized analysis is misleading and illustrates the risk of relying on the computer for a diagnosis. The nonspecific T-wave abnormalities are best seen in leads V2 and V3 and are of no consequence.
While there are no definitive studies that prove that combining energy drinks containing taurine with beverages containing caffeine increases the risk for arrhythmias, there are several anecdotal case reports. In addition to consumption of taurine- and caffeine-containing beverages, this patient is under a significant amount of stress, producing a large catecholaminergic response.
The patient has no prior cardiac history of arrhythmias and no prior cardiac workup. He underwent synchronized cardioversion to restore normal sinus rhythm and was scheduled for an outpatient workup for structural heart disease.
ANSWER
The ECG reveals atrial flutter with a nonspecific T-wave abnormality. The atrial rate is 300 beats/min. The ventricular rate is 84 beats/min; hence the atrial flutter occurs in a 4:1 pattern. (This is best seen in lead V1, where one of the atrial beats is “hidden” in the QRS complex.) The PR interval of 208 ms on the computerized analysis is misleading and illustrates the risk of relying on the computer for a diagnosis. The nonspecific T-wave abnormalities are best seen in leads V2 and V3 and are of no consequence.
While there are no definitive studies that prove that combining energy drinks containing taurine with beverages containing caffeine increases the risk for arrhythmias, there are several anecdotal case reports. In addition to consumption of taurine- and caffeine-containing beverages, this patient is under a significant amount of stress, producing a large catecholaminergic response.
The patient has no prior cardiac history of arrhythmias and no prior cardiac workup. He underwent synchronized cardioversion to restore normal sinus rhythm and was scheduled for an outpatient workup for structural heart disease.
A business professional, age 39, presents with shortness of breath that abruptly began two hours ago. He states he has been under a significant amount of stress at work during the past six months. He is approaching a deadline on a very important contract, which he says will “make or break” his career. As a result, he has been working long hours and often consumes eight to 10 cups of coffee as well as three to five energy drinks per day. After getting only three hours of sleep last night, he had two cups of coffee with a “two–energy-drink chaser.” About one hour after his last energy drink, he felt several palpitations and abruptly became short of breath. There is no history of pulmonary or cardiac illness. The patient’s medical history is unremarkable, with the exception of childhood cases of chickenpox and mumps. He has never had a surgical procedure. He takes ibuprofen on occasion after playing sports and has no known drug allergies. During college, he smoked one pack of cigarettes per day, ceasing at graduation. In response to work-related stress, he has started smoking again and is up to half a pack per day. His alcohol consumption consists of two cocktails in the evening and a 12-pack of beer on the weekends. He denies illicit drug use. The review of systems is remarkable for heartburn, bloating, and frequent indigestion. He denies nausea, vomiting, diarrhea, or constipation. The physical examination reveals a well-developed, anxious male in mild distress. His weight is 174 lb and his height is 74 in. Vital signs include a blood pressure of 90/58 mm Hg; pulse, 88 beats/min; respiratory rate, 18 breaths/min; and temperature, 98°F. His O2 saturation is 99% on room air. The HEENT exam is normal. There is no thyromegaly. The mucous membranes are pink and moist. The chest is clear to auscultation in all lung fields with excellent diaphragmatic excursion. The pulse is regular. There are no murmurs, rubs, clicks, or extra heart sounds. The abdomen is soft and nontender. The liver and spleen are not palpable. The pulses are equal and strong bilaterally. The neurologic exam is unremarkable. A chest x-ray, blood chemistry, complete blood count, and electrocardiogram are ordered. You are handed an ECG tracing that reveals the following: a ventricular rate of 84 beats/min; PR interval, 208 ms; QRS duration, 102 ms; QT/QTc interval, 358/423 ms; R axis, 20°; and T axis, 29°. What is your interpretation of this ECG?
Pruritic Rash on Both Soles
ANSWER
The correct answer is a form of psoriasis (choice “a”)—in this case, pustular psoriasis, which is seen mostly on hands and feet.
As in many such cases, biopsy was necessary; it successfully ruled out several items in the differential, in particular contact dermatitis (choice “b”). Ringworm and athlete’s foot (choice “c” and “d,” respectively) are archaic lay terms for fungal infection, which was not only ruled out by its absence in the biopsy specimen, but was unlikely given the lack of response to multiple antifungal medications.
DISCUSSION
Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
Biopsy was deemed necessary to clarify the diagnosis and gain confidence in the therapeutic process, which can be difficult with this problem.
The patient was urged to consult her psychiatrist about finding a substitute for her lithium. At the time of this description, she is currently applying clobetasol cream under occlusion for three weeks, at the conclusion of which she will be re-evaluated. Many such patients go on to require the use of other medications, such as methotrexate or acetretin.
ANSWER
The correct answer is a form of psoriasis (choice “a”)—in this case, pustular psoriasis, which is seen mostly on hands and feet.
As in many such cases, biopsy was necessary; it successfully ruled out several items in the differential, in particular contact dermatitis (choice “b”). Ringworm and athlete’s foot (choice “c” and “d,” respectively) are archaic lay terms for fungal infection, which was not only ruled out by its absence in the biopsy specimen, but was unlikely given the lack of response to multiple antifungal medications.
DISCUSSION
Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
Biopsy was deemed necessary to clarify the diagnosis and gain confidence in the therapeutic process, which can be difficult with this problem.
The patient was urged to consult her psychiatrist about finding a substitute for her lithium. At the time of this description, she is currently applying clobetasol cream under occlusion for three weeks, at the conclusion of which she will be re-evaluated. Many such patients go on to require the use of other medications, such as methotrexate or acetretin.
ANSWER
The correct answer is a form of psoriasis (choice “a”)—in this case, pustular psoriasis, which is seen mostly on hands and feet.
As in many such cases, biopsy was necessary; it successfully ruled out several items in the differential, in particular contact dermatitis (choice “b”). Ringworm and athlete’s foot (choice “c” and “d,” respectively) are archaic lay terms for fungal infection, which was not only ruled out by its absence in the biopsy specimen, but was unlikely given the lack of response to multiple antifungal medications.
DISCUSSION
Palmoplantar pustulosis is the term most often used to describe a fairly common form of psoriasis typified by this case. Many patients are genetically predisposed to psoriasis, but they may require a trigger to set it off, such as strep infection or occasionally, medication. Notable among the latter are the b-blockers and lithium. Stress is often involved as well.
The bilateral symmetrical involvement of both insteps is highly suggestive of this diagnosis, which often also affects either peripheral or central palms. A secondary form of neurodermatitis (itch–scratch–itch cycle) can follow, complicating the picture and perpetuating the problem.
Biopsy was deemed necessary to clarify the diagnosis and gain confidence in the therapeutic process, which can be difficult with this problem.
The patient was urged to consult her psychiatrist about finding a substitute for her lithium. At the time of this description, she is currently applying clobetasol cream under occlusion for three weeks, at the conclusion of which she will be re-evaluated. Many such patients go on to require the use of other medications, such as methotrexate or acetretin.

A 62-year-old woman is referred to dermatology for evaluation of a pruritic rash that has been present on both soles for more than two years. Attempts to treat it with different OTC topical creams (eg, clotrimazole, miconazole), prescription antifungal creams (oxiconazole and nystatin), and even a combination cream (clotrimazole/betamethasone) have been unsuccessful. The last eased her symptoms but yielded no lasting relief. Her primary care provider had prescribed a month-long course of oral terbinafine (250 mg/d). When that did not help, a two-week course of oral antibiotic (cephalexin 500 mg qid) was tried. Neither had any salutary effect, so the patient was referred first to a podiatrist, who quickly sent her to dermatology. Complaining bitterly of itching on these areas, she explains that the condition began with tiny pustules, then tiny blisters that gradually covered both insteps. She denies having any such rash elsewhere (eg, on elbows or knees or in the scalp). There is no known family history of skin problems, and no personal history of arthritis. Just prior to the onset of this problem, she had received a diagnosis of bipolar affective disorder, which forced her to leave her job and start taking lithium. Although the lithium has helped, she remains unable to work. On examination, the skin of both insteps is covered with discrete and confluent papules and tiny pustules on an erythematous and hyperpigmented (brown), sharply demarcated, and highly symmetrical base. As the patient said, her skin, nails, and scalp elsewhere are free of any such lesions. Given her Hispanic ancestry, her skin is phototype IV/VI. Punch biopsy is performed and shows almost no spongiosis or edema, relatively tortuous capillary loops, and collections of neutrophils above foci of parakeratosis. Special stain for fungal elements fails to identify any sign of that family of organisms.
Man Run Over By Vehicle
ANSWER
The radiograph shows some deformity within the mid-to-distal diaphysis of both the radius and ulna; however, no acute fracture is seen. This is most likely related to remote trauma.
Of note, closer to the elbow, there are some small avulsion fractures near the area of the lateral epicondyle. The patient was treated with a posterior splint and referred to orthopedics.
ANSWER
The radiograph shows some deformity within the mid-to-distal diaphysis of both the radius and ulna; however, no acute fracture is seen. This is most likely related to remote trauma.
Of note, closer to the elbow, there are some small avulsion fractures near the area of the lateral epicondyle. The patient was treated with a posterior splint and referred to orthopedics.
ANSWER
The radiograph shows some deformity within the mid-to-distal diaphysis of both the radius and ulna; however, no acute fracture is seen. This is most likely related to remote trauma.
Of note, closer to the elbow, there are some small avulsion fractures near the area of the lateral epicondyle. The patient was treated with a posterior splint and referred to orthopedics.

After accidentally being run over by a vehicle, a 54-year-old man presents to the emergency department for evaluation of pain in his elbow and left arm. He was leaning down behind the vehicle and was not seen when the driver backed up. The patient states that one of the tires went over his left shoulder and arm. Primary complaint is pain and decreased range of motion. He denies any significant medical history, except for medication-controlled hypertension and gallbladder surgery. His vital signs are stable. Exammination of the left arm demonstrates some abrasions and contusions over the shoulder and forearm, as well as some swelling over the elbow. The patient has good color, distal pulses, and sensation. There is localized tenderness over the elbow and midforearm. Flexion of the elbow is somewhat limited secondary to pain. Radiograph of the forearm is obtained and shown. What is your impression?
Man with Debilitating Back Pain
ANSWER
The radiograph demonstrates generalized degenerative changes. Of note are fairly significant destructive changes in the endplate at the L3-4 level. Such changes are generally consistent with osteomyelitis and diskitis.
On further questioning, the patient reported that when he was admitted previously, he was told that he had an “infection in his back” and was treated with IV antibiotics. This patient was again admitted for additional workup and treatment.
ANSWER
The radiograph demonstrates generalized degenerative changes. Of note are fairly significant destructive changes in the endplate at the L3-4 level. Such changes are generally consistent with osteomyelitis and diskitis.
On further questioning, the patient reported that when he was admitted previously, he was told that he had an “infection in his back” and was treated with IV antibiotics. This patient was again admitted for additional workup and treatment.
ANSWER
The radiograph demonstrates generalized degenerative changes. Of note are fairly significant destructive changes in the endplate at the L3-4 level. Such changes are generally consistent with osteomyelitis and diskitis.
On further questioning, the patient reported that when he was admitted previously, he was told that he had an “infection in his back” and was treated with IV antibiotics. This patient was again admitted for additional workup and treatment.

A 54-year-old man presents with a complaint of a two-week history of severe low back pain. He denies any injury or trauma. The pain is so severe that it limits his ability to walk. He states he had similar episodes earlier this year, some of which required him to be admitted to the hospital. His medical history is significant for hypertension, diabetes, and coronary artery disease. He admits to recently having subjective fever and chills, as well as some nausea. Physical exam shows a deconditioned male who is uncomfortable but in no obvious distress. He is afebrile, with a blood pressure of 92/57 mm Hg, a heart rate of 97 beats/min, and a respiratory rate of 20 breaths/min. He has mild tenderness to his lumbosacral area; no deformity, step-off, or crepitus is appreciated. He does have decreased range of motion in his lower extremities, although this may be a consequence of his back pain. While trying to pull up his previous medical records, you order some basic labwork and lumbar spine radiographs. Lateral lumbar spine radiograph is shown; what is your impression?
Ederly Woman Experiences Chest Pain While Knitting
ANSWER
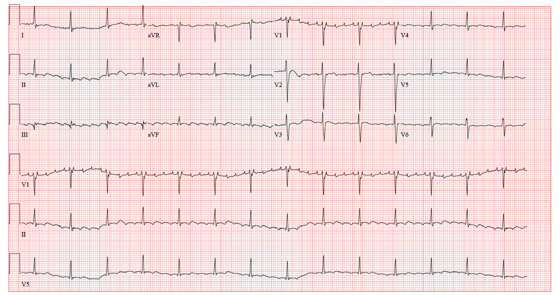
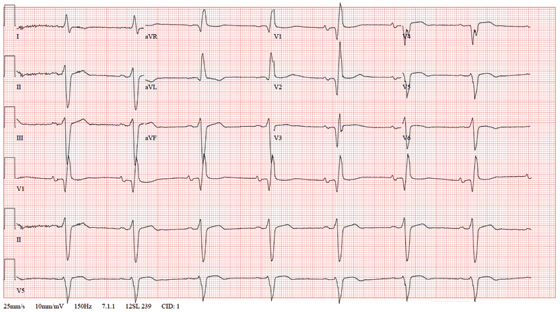
The ECG shows normal sinus rhythm with a short PR interval, right bundle branch block, and an inferior myocardial infarction. The PR interval may vary based on age and heart rate, but is generally accepted as ranging between 120 and 200 ms.
Criteria for a right bundle branch include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. An inferior wall myocardial infarction is evidenced by significant Q waves and T-wave inversions in the inferior leads II, III, and aVF.
This case illustrates that an ECG may be of little value in the setting of an ascending aortic dissection. This patient succumbed to rupture of her aortic dissection shortly after admission.
ANSWER
The ECG shows normal sinus rhythm with a short PR interval, right bundle branch block, and an inferior myocardial infarction. The PR interval may vary based on age and heart rate, but is generally accepted as ranging between 120 and 200 ms.
Criteria for a right bundle branch include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. An inferior wall myocardial infarction is evidenced by significant Q waves and T-wave inversions in the inferior leads II, III, and aVF.
This case illustrates that an ECG may be of little value in the setting of an ascending aortic dissection. This patient succumbed to rupture of her aortic dissection shortly after admission.
ANSWER
The ECG shows normal sinus rhythm with a short PR interval, right bundle branch block, and an inferior myocardial infarction. The PR interval may vary based on age and heart rate, but is generally accepted as ranging between 120 and 200 ms.
Criteria for a right bundle branch include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. An inferior wall myocardial infarction is evidenced by significant Q waves and T-wave inversions in the inferior leads II, III, and aVF.
This case illustrates that an ECG may be of little value in the setting of an ascending aortic dissection. This patient succumbed to rupture of her aortic dissection shortly after admission.
An 84-year-old woman presents with left-sided chest pain radiating to the back and neck. The pain began about four hours ago, while she was knitting. She describes it as a “dull ache” that quickly progressed to a “sharp, sticking” pain on a scale of 8/10. She has never experienced pain like this before. She denies nausea, vomiting, diaphoresis, headache, palpitations, orthopnea, or dyspnea on exertion. Her medical history is remarkable for Crohn’s disease, atrial fibrillation, hypertension, and myxomatous mitral valve disease. Surgical history is remarkable for a myocardial infarction 10 years ago, two separate catheter ablations for atrial fibrillation (successful on the second attempt), a mitral valve replacement (bioprosthetic) one year ago, and a hysterectomy/oophorectomy in the remote past. The patient has no known drug allergies. Her medications include atenolol, aspirin, furosemide, estradiol, ferrous sulfate, mesalamine, omeprazole, warfarin, and lisinopril. She is a retired teacher, married, who has never smoked and rarely drinks alcohol. Her family history is remarkable for heart disease in her father and diabetes in her mother. The review of systems is negative, with the exception of frequent episodes of nonbloody diarrhea and abdominal pain associated with her Crohn’s disease. Physical exam reveals a blood pressure of 208/120 mm Hg; pulse, 60 beats/min; respiratory rate, 22 breaths/min-1; temperature, 97.8°F; and O2 saturation, 96% on 2L oxygen. She appears anxious, restless, and unable to find a comfortable position. Pertinent physical findings include jugular venous distention to the angle of the jaw, a regular heart rate with a harsh III/VI systolic murmur at the left upper sternal border, and a soft II/VI diastolic murmur radiating to the apex. Peripheral pulses are brisk and equal bilaterally. There are no neurologic deficits. Laboratory data include a normal complete blood count, an INR of 2.2, normal blood chemistries, normal liver function studies, and negative troponin levels. CT reveals a 5.5-cm dissection of the ascending aorta. An ECG shows the following: a ventricular rate of 61 beats/min; PR interval, 108 ms; QRS duration, 132 ms; QT/QTc interval, 478/481 ms; P axis, 19°; R axis, 0°; and T axis, –13°. What is your interpretation of this ECG?
Is A Common Illness The Cause of This Man's Rash?
ANSWER
The correct answer is erythema annulare centrifugum (EAC; choice “c”), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis.
Dermatophytosis (choice “a”), a superficial fungal infection, would likely have demonstrated KOH positivity at its scaly leading edge.
Subacute cutaneous lupus (choice “b”) has many morphologic presentations, including annular scaly lesions with clearing centers, but definite signs (interface dermatitis, increased mucin or apoptosis) would have been seen on biopsy.
Cutaneous T-cell lymphoma (choice “d”) is one of a handful of malignancies that can present as a “rash,” but the biopsy effectively ruled it out.
DISCUSSION
First described by Darier in 1916, EAC exhibits a pathognomic feature called “trailing scale.” With dermatophytosis, for example, the bulk of the scaling is found at the leading edge of the lesion. By contrast, with EAC, the scaling lags behind the leading erythematous border and is thus said to “trail” the edge. Since EAC so closely resembles dermatophytosis, this feature serves to distinguish the two.
EAC lesions can be large, appear in multiples, and spare only palms and soles.
EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
A brisk inflammatory tinea can set it off, complicating the clinical picture by presenting with two different types of annular lesions. Treating the fungal infection or other trigger effectively cures the EAC. In such cases, a careful history will show which rash came first.
When the cause is not immediately obvious, potential triggers that should be investigated include: occult malignancy, tuberculosis, sarcoidosis, and pregnancy. Examination of skin distant from the obviously affected areas is often necessary, with special attention to the feet, groin, and scalp. Laboratory studies should include a complete blood count, liver function tests, rapid plasma reagin test, urinalysis, and chest x-ray for completeness.
EAC is treated, as mentioned earlier, by finding and eliminating the underlying cause. That often proves impossible, so steroid therapy (oral or topical) is often employed with some effect (though it will not prevent recurrences of the condition). Empiric use of oral antibiotics has produced mixed results. The condition can persist for years but is seldom significantly symptomatic.
ANSWER
The correct answer is erythema annulare centrifugum (EAC; choice “c”), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis.
Dermatophytosis (choice “a”), a superficial fungal infection, would likely have demonstrated KOH positivity at its scaly leading edge.
Subacute cutaneous lupus (choice “b”) has many morphologic presentations, including annular scaly lesions with clearing centers, but definite signs (interface dermatitis, increased mucin or apoptosis) would have been seen on biopsy.
Cutaneous T-cell lymphoma (choice “d”) is one of a handful of malignancies that can present as a “rash,” but the biopsy effectively ruled it out.
DISCUSSION
First described by Darier in 1916, EAC exhibits a pathognomic feature called “trailing scale.” With dermatophytosis, for example, the bulk of the scaling is found at the leading edge of the lesion. By contrast, with EAC, the scaling lags behind the leading erythematous border and is thus said to “trail” the edge. Since EAC so closely resembles dermatophytosis, this feature serves to distinguish the two.
EAC lesions can be large, appear in multiples, and spare only palms and soles.
EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
A brisk inflammatory tinea can set it off, complicating the clinical picture by presenting with two different types of annular lesions. Treating the fungal infection or other trigger effectively cures the EAC. In such cases, a careful history will show which rash came first.
When the cause is not immediately obvious, potential triggers that should be investigated include: occult malignancy, tuberculosis, sarcoidosis, and pregnancy. Examination of skin distant from the obviously affected areas is often necessary, with special attention to the feet, groin, and scalp. Laboratory studies should include a complete blood count, liver function tests, rapid plasma reagin test, urinalysis, and chest x-ray for completeness.
EAC is treated, as mentioned earlier, by finding and eliminating the underlying cause. That often proves impossible, so steroid therapy (oral or topical) is often employed with some effect (though it will not prevent recurrences of the condition). Empiric use of oral antibiotics has produced mixed results. The condition can persist for years but is seldom significantly symptomatic.
ANSWER
The correct answer is erythema annulare centrifugum (EAC; choice “c”), one of the so-called “reactive erythemas,” which have several potential causes including streptococcal infections. The clinical picture and classic histologic pattern seen on biopsy effectively ruled out the other items in the differential diagnosis.
Dermatophytosis (choice “a”), a superficial fungal infection, would likely have demonstrated KOH positivity at its scaly leading edge.
Subacute cutaneous lupus (choice “b”) has many morphologic presentations, including annular scaly lesions with clearing centers, but definite signs (interface dermatitis, increased mucin or apoptosis) would have been seen on biopsy.
Cutaneous T-cell lymphoma (choice “d”) is one of a handful of malignancies that can present as a “rash,” but the biopsy effectively ruled it out.
DISCUSSION
First described by Darier in 1916, EAC exhibits a pathognomic feature called “trailing scale.” With dermatophytosis, for example, the bulk of the scaling is found at the leading edge of the lesion. By contrast, with EAC, the scaling lags behind the leading erythematous border and is thus said to “trail” the edge. Since EAC so closely resembles dermatophytosis, this feature serves to distinguish the two.
EAC lesions can be large, appear in multiples, and spare only palms and soles.
EAC is most often idiopathic. However, there are many reported triggers, including drugs (eg, gold, antimalarials, penicillin, and aspirin), infections (such as strep and dermatophytosis), and malignancies.
A brisk inflammatory tinea can set it off, complicating the clinical picture by presenting with two different types of annular lesions. Treating the fungal infection or other trigger effectively cures the EAC. In such cases, a careful history will show which rash came first.
When the cause is not immediately obvious, potential triggers that should be investigated include: occult malignancy, tuberculosis, sarcoidosis, and pregnancy. Examination of skin distant from the obviously affected areas is often necessary, with special attention to the feet, groin, and scalp. Laboratory studies should include a complete blood count, liver function tests, rapid plasma reagin test, urinalysis, and chest x-ray for completeness.
EAC is treated, as mentioned earlier, by finding and eliminating the underlying cause. That often proves impossible, so steroid therapy (oral or topical) is often employed with some effect (though it will not prevent recurrences of the condition). Empiric use of oral antibiotics has produced mixed results. The condition can persist for years but is seldom significantly symptomatic.

A 44-year-old man presents with an asymptomatic rash that manifested several weeks ago. His primary care provider called it “ringworm,” but it has been unresponsive to topical antifungal creams, including clotrimazole and tolnaftate. The patient also sought evaluation in an urgent care setting, where the provider diagnosed “psoriasis” and prescribed triamcinolone, which didn’t seem to help. Additional history taking reveals that, two weeks before the lesions appeared, the patient received a diagnosis of strep throat and subsequently was treated with amoxicillin. The patient is otherwise healthy, taking no medications regularly. On examination, the rash is quite striking—brightly erythematous, with annular margins on which the skin is red. But just behind the advancing margin is a parallel band of scaling. At its largest dimension, the papulosquamous patch is slightly in excess of 8 cm. Microscopic examination of scrapings from the lesion’s scale is negative for fungal elements. The rest of the patient’s skin, with particular attention to the feet and groin, is well within normal limits. Punch biopsy of the lesion shows intense lymphohistiocytic cuffing around superficial and deep dermal vessels, with no epidermal involvement. Stains for fungal elements are negative.
Woman with Foot Pain After Neurosurgery Service
ANSWER
The radiograph demonstrates mild soft-tissue swelling and an oblique, mildly displaced fracture of the distal fibula. In addition, there is a small bone density adjacent to the medial malleolus, which could represent either an unfused accessory ossification center or a sequela of prior trauma.
On closer questioning, the patient acknowledged that a few months prior, she had stepped in a hole and been treated for a “broken bone.” She had been in a cast for an undisclosed period of time; at a follow-up appointment, the cast had been removed and the bone had been declared “healed.”
A new orthopedic consultation was obtained prior to the patient’s discharge from the hospital, which resulted in placement of a short leg cast.
ANSWER
The radiograph demonstrates mild soft-tissue swelling and an oblique, mildly displaced fracture of the distal fibula. In addition, there is a small bone density adjacent to the medial malleolus, which could represent either an unfused accessory ossification center or a sequela of prior trauma.
On closer questioning, the patient acknowledged that a few months prior, she had stepped in a hole and been treated for a “broken bone.” She had been in a cast for an undisclosed period of time; at a follow-up appointment, the cast had been removed and the bone had been declared “healed.”
A new orthopedic consultation was obtained prior to the patient’s discharge from the hospital, which resulted in placement of a short leg cast.
ANSWER
The radiograph demonstrates mild soft-tissue swelling and an oblique, mildly displaced fracture of the distal fibula. In addition, there is a small bone density adjacent to the medial malleolus, which could represent either an unfused accessory ossification center or a sequela of prior trauma.
On closer questioning, the patient acknowledged that a few months prior, she had stepped in a hole and been treated for a “broken bone.” She had been in a cast for an undisclosed period of time; at a follow-up appointment, the cast had been removed and the bone had been declared “healed.”
A new orthopedic consultation was obtained prior to the patient’s discharge from the hospital, which resulted in placement of a short leg cast.

A 60-year-old woman is admitted electively to the neurosurgery service for a multilevel posterior cervical decompression and fusion. The procedure is completed uneventfully and without complication. The patient is admitted to the neurosurgical floor. In the middle of the night, you receive a call from the nurse stating that the patient is complaining of moderate pain and swelling in her left ankle and foot, which occurred after she got up to use the bathroom. The patient denies injuring herself. She complains of pain with weight-bearing. Since the pain is tolerable and pain medication has already been given, it is decided to assess the complaint later in the morning. On evaluation, the left foot and ankle are mildly swollen, with tenderness on the lateral aspect. There is minimal tenderness on the foot. Distal pulses and color are good. The calf is nontender. The patient’s medical history is significant only for mild hypertension. Radiographs of the left ankle are obtained. What is your impression?
Widower Experiencing Fatigue
ANSWER
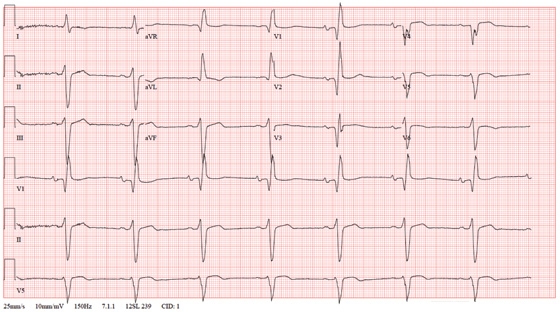
The correct interpretation of this ECG includes marked sinus bradycardia, left atrial enlargement, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy, and an old anteroseptal myocardial infarction.
Marked sinus bradycardia is represented by a heart rate of 46 beats/min. Left atrial enlargement is evident from P waves ≥ 110 ms in lead I (difficult to see in this ECG) and a terminally negative P wave in lead V1 ≥ 1 mm2 (easier to see in this ECG).
Findings of a right bundle branch block include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. (In this ECG, the RSR’ complex is not obvious.)
A left anterior fascicular block is indicated by S waves > R waves in leads II, III, and aVF with marked left-axis deviation (R axis, –77°). Left ventricular hypertrophy is evident if the sum of the R wave in lead I and the S wave in III ≥ 25 mm or if the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm.
Finally, the diagnosis of an old anteroseptal myocardial infarction is evidenced by Q waves in leads V1 through V3 and a QS pattern in lead V4.
The patient’s bradycardia was responsible for his symptoms of fatigue. Careful questioning revealed that he had inadvertently doubled his dose of atenolol for the preceding two weeks. Upon correction of his dose, his heart rate increased and his symptoms resolved.
ANSWER
The correct interpretation of this ECG includes marked sinus bradycardia, left atrial enlargement, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy, and an old anteroseptal myocardial infarction.
Marked sinus bradycardia is represented by a heart rate of 46 beats/min. Left atrial enlargement is evident from P waves ≥ 110 ms in lead I (difficult to see in this ECG) and a terminally negative P wave in lead V1 ≥ 1 mm2 (easier to see in this ECG).
Findings of a right bundle branch block include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. (In this ECG, the RSR’ complex is not obvious.)
A left anterior fascicular block is indicated by S waves > R waves in leads II, III, and aVF with marked left-axis deviation (R axis, –77°). Left ventricular hypertrophy is evident if the sum of the R wave in lead I and the S wave in III ≥ 25 mm or if the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm.
Finally, the diagnosis of an old anteroseptal myocardial infarction is evidenced by Q waves in leads V1 through V3 and a QS pattern in lead V4.
The patient’s bradycardia was responsible for his symptoms of fatigue. Careful questioning revealed that he had inadvertently doubled his dose of atenolol for the preceding two weeks. Upon correction of his dose, his heart rate increased and his symptoms resolved.
ANSWER
The correct interpretation of this ECG includes marked sinus bradycardia, left atrial enlargement, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy, and an old anteroseptal myocardial infarction.
Marked sinus bradycardia is represented by a heart rate of 46 beats/min. Left atrial enlargement is evident from P waves ≥ 110 ms in lead I (difficult to see in this ECG) and a terminally negative P wave in lead V1 ≥ 1 mm2 (easier to see in this ECG).
Findings of a right bundle branch block include a QRS complex > 120 ms, a terminal broad S wave in lead I, and an RSR’ complex in lead V1. (In this ECG, the RSR’ complex is not obvious.)
A left anterior fascicular block is indicated by S waves > R waves in leads II, III, and aVF with marked left-axis deviation (R axis, –77°). Left ventricular hypertrophy is evident if the sum of the R wave in lead I and the S wave in III ≥ 25 mm or if the sum of the S wave in V1 and the R wave in either V5 or V6 is ≥ 35 mm.
Finally, the diagnosis of an old anteroseptal myocardial infarction is evidenced by Q waves in leads V1 through V3 and a QS pattern in lead V4.
The patient’s bradycardia was responsible for his symptoms of fatigue. Careful questioning revealed that he had inadvertently doubled his dose of atenolol for the preceding two weeks. Upon correction of his dose, his heart rate increased and his symptoms resolved.
A 72-year-old man presents for a routine appointment. He was doing well until two months ago, when he started to notice that he fatigues easily. He is unable to go up and down stairs at home without pausing and has difficulty working in his garden. He says he does not become short of breath but just feels fatigued. The patient denies chest pain, palpitations, tachycardia, syncope, or near-syncope. He denies recent weight gain or peripheral extremity edema. He has had no recent changes to his medications, and he has not recently been ill. The man’s cardiac history is remarkable for coronary artery disease, a coronary artery bypass graft (CABG) in 2007, paroxysmal atrial fibrillation, and an ischemic cardiomyopathy. His most recent echocardiogram (six months ago) showed global left ventricular dysfunction with inferior akinesis, a left ventricular end-diastolic dimension of 8.1 cm, and a left ventricular ejection fraction of 35%. His pulmonary artery pressure was 25 to 29 mm Hg. A nuclear viability study performed at the same time showed a nonviable myocardial infarction involving the anterior and inferior septal walls of the left ventricle. A cardiac catheterization performed one year ago showed 30% stenosis of the left main coronary artery, an occluded left anterior descending (LAD) artery with myocardial perfusion supplied by right-to-left collateral vessels, 50% stenosis of the left circumflex artery, 70% stenosis of the left circumflex artery, and 70% to 80% stenosis of the mid right coronary artery (RCA). The saphenous vein grafts to the LAD, RCA, circumflex, and diagonal branches were occluded. Medical history is remarkable for dyslipidemia, arthritis, and depression. In addition to CABG, surgical history includes cholecystectomy and a left hip replacement. The patient is a retired beer distributor who has lived alone since his wife’s death three years ago. He drinks two or three glasses of wine in the evenings. Prior to quitting 10 years ago, he had a 30-pack-year history of smoking; however, he started again after his wife’s death and currently smokes half a pack of cigarettes per day. His medication list includes aspirin, atenolol, hydrochlorothiazide, lisinopril, atorvastatin, and trazodone. The review of systems is negative. Vital statistics include a blood pressure of 106/58 mm Hg; pulse, 50 beats/min; temperature, 97.5°F; and O2 saturation, 94% on room air. His weight is 172.4 lb and is unchanged from his last clinic visit. Pertinent findings on the physical exam include clear lung fields, a regular rhythm, and bradycardia with no murmurs or extra heart sounds, no bruits, no jugular venous distention, and no peripheral edema. All pulses are equal and normal. Based on the patient’s symptoms and the finding of bradycardia on physical exam, you order an ECG, which shows the following: a ventricular rate of 46 beats/min; PR interval, 202 ms; QRS duration, 200 ms; QT/QTc interval, 578/505 ms; P axis, 71°; R axis, –77°; and T axis, 109°. What is your interpretation of this ECG?
Man Continually Cuts Facial Lesion While Shaving
ANSWER
The best answer is to send the slides to a dermatopathologist (choice “a”), for reasons that will become clear in the discussion. It is true that by re-excising with margins (choice “b”), the lesion would certainly be gone, but that does nothing to address the potential pathologic implications of some of the items in the differential diagnosis for this type of lesion.
The same could be said for rechecking the lesion periodically (choice “c”), which would otherwise be an intelligent option. It is almost never wrong to consult with a supervising/collaborating physician (choice “d”), but that does not relieve the PA/NP of the ultimate responsibility for resolving the dilemma.
DISCUSSION
Odd little papules in the nasolabial fold can have implications far beyond the usual “benign versus malignant” issue. With its surface devoid of adnexal structures, and firm feel, this lesion was a bit suspicious, history of stability notwithstanding.
Generally termed skin adnexal tumors (SATs), these lesions are derived from local adnexal structures, such as eccrine or apocrine sweat glands or pilosebaceous unit tissue. But they may originate from pluripotent stem cells located in the outer root sheath of the hair follicle, residing in an area called “the bulge.”
Their final designation is based on the predominant cell type seen on pathology, but differentiation can be difficult, even for experienced pathologists. Many benign types have been described, but for every benign category, a malignant counterpart exists. The latter tend to be aggressive and involve nodes, metastasis, and generally poor outcomes.
Heredity, skin type, and UV exposure play significant roles in some types of skin cancer, but an intracellular signaling pathway is also thought to determine the ultimate differentiation of these cells. Loss of inhibition of this pathway, which normally occurs, is apparently the main deciding factor in malignant transformation.
But the importance of a precise diagnosis for an SAT is more than mere benign versus malignant considerations. These lesions can serve as markers for syndromes associated with internal malignancies, such as Cowden’s disease (trichilemmomas) or Muir-Torre syndrome (sebaceous neoplasm), to name just two.
The person most likely to be able to discriminate between these various possibilities is the dermatopathologist, who is not only an expert in what is seen microscopically, but is also typically a practicing dermatologist who regularly sees the conditions he diagnoses. The biopsying provider has an obligation to insist on a crystal-clear diagnosis, when it can be obtained. And that “diagnosis” isn’t always about what the lesion is. Sometimes it’s as much about what the lesion means.
SUGGESTED READING
Alsaad KO, Obaidat NA, Ghazarian D. Skin adnexal neoplasms—part 1: an approach to tumours of the pilosebaceous unit. J Clin Pathol. 2007;60(2):129-144.
ANSWER
The best answer is to send the slides to a dermatopathologist (choice “a”), for reasons that will become clear in the discussion. It is true that by re-excising with margins (choice “b”), the lesion would certainly be gone, but that does nothing to address the potential pathologic implications of some of the items in the differential diagnosis for this type of lesion.
The same could be said for rechecking the lesion periodically (choice “c”), which would otherwise be an intelligent option. It is almost never wrong to consult with a supervising/collaborating physician (choice “d”), but that does not relieve the PA/NP of the ultimate responsibility for resolving the dilemma.
DISCUSSION
Odd little papules in the nasolabial fold can have implications far beyond the usual “benign versus malignant” issue. With its surface devoid of adnexal structures, and firm feel, this lesion was a bit suspicious, history of stability notwithstanding.
Generally termed skin adnexal tumors (SATs), these lesions are derived from local adnexal structures, such as eccrine or apocrine sweat glands or pilosebaceous unit tissue. But they may originate from pluripotent stem cells located in the outer root sheath of the hair follicle, residing in an area called “the bulge.”
Their final designation is based on the predominant cell type seen on pathology, but differentiation can be difficult, even for experienced pathologists. Many benign types have been described, but for every benign category, a malignant counterpart exists. The latter tend to be aggressive and involve nodes, metastasis, and generally poor outcomes.
Heredity, skin type, and UV exposure play significant roles in some types of skin cancer, but an intracellular signaling pathway is also thought to determine the ultimate differentiation of these cells. Loss of inhibition of this pathway, which normally occurs, is apparently the main deciding factor in malignant transformation.
But the importance of a precise diagnosis for an SAT is more than mere benign versus malignant considerations. These lesions can serve as markers for syndromes associated with internal malignancies, such as Cowden’s disease (trichilemmomas) or Muir-Torre syndrome (sebaceous neoplasm), to name just two.
The person most likely to be able to discriminate between these various possibilities is the dermatopathologist, who is not only an expert in what is seen microscopically, but is also typically a practicing dermatologist who regularly sees the conditions he diagnoses. The biopsying provider has an obligation to insist on a crystal-clear diagnosis, when it can be obtained. And that “diagnosis” isn’t always about what the lesion is. Sometimes it’s as much about what the lesion means.
SUGGESTED READING
Alsaad KO, Obaidat NA, Ghazarian D. Skin adnexal neoplasms—part 1: an approach to tumours of the pilosebaceous unit. J Clin Pathol. 2007;60(2):129-144.
ANSWER
The best answer is to send the slides to a dermatopathologist (choice “a”), for reasons that will become clear in the discussion. It is true that by re-excising with margins (choice “b”), the lesion would certainly be gone, but that does nothing to address the potential pathologic implications of some of the items in the differential diagnosis for this type of lesion.
The same could be said for rechecking the lesion periodically (choice “c”), which would otherwise be an intelligent option. It is almost never wrong to consult with a supervising/collaborating physician (choice “d”), but that does not relieve the PA/NP of the ultimate responsibility for resolving the dilemma.
DISCUSSION
Odd little papules in the nasolabial fold can have implications far beyond the usual “benign versus malignant” issue. With its surface devoid of adnexal structures, and firm feel, this lesion was a bit suspicious, history of stability notwithstanding.
Generally termed skin adnexal tumors (SATs), these lesions are derived from local adnexal structures, such as eccrine or apocrine sweat glands or pilosebaceous unit tissue. But they may originate from pluripotent stem cells located in the outer root sheath of the hair follicle, residing in an area called “the bulge.”
Their final designation is based on the predominant cell type seen on pathology, but differentiation can be difficult, even for experienced pathologists. Many benign types have been described, but for every benign category, a malignant counterpart exists. The latter tend to be aggressive and involve nodes, metastasis, and generally poor outcomes.
Heredity, skin type, and UV exposure play significant roles in some types of skin cancer, but an intracellular signaling pathway is also thought to determine the ultimate differentiation of these cells. Loss of inhibition of this pathway, which normally occurs, is apparently the main deciding factor in malignant transformation.
But the importance of a precise diagnosis for an SAT is more than mere benign versus malignant considerations. These lesions can serve as markers for syndromes associated with internal malignancies, such as Cowden’s disease (trichilemmomas) or Muir-Torre syndrome (sebaceous neoplasm), to name just two.
The person most likely to be able to discriminate between these various possibilities is the dermatopathologist, who is not only an expert in what is seen microscopically, but is also typically a practicing dermatologist who regularly sees the conditions he diagnoses. The biopsying provider has an obligation to insist on a crystal-clear diagnosis, when it can be obtained. And that “diagnosis” isn’t always about what the lesion is. Sometimes it’s as much about what the lesion means.
SUGGESTED READING
Alsaad KO, Obaidat NA, Ghazarian D. Skin adnexal neoplasms—part 1: an approach to tumours of the pilosebaceous unit. J Clin Pathol. 2007;60(2):129-144.

A 53-year-old man self-refers to dermatology for evaluation of a lesion on his left maxilla that has been basically unchanged for several years. He is concerned for two reasons: First, it is a rare day on which he fails to cut the lesion while shaving, and he is afraid this repeated trauma will “turn it into skin cancer.” Second, a co-worker who recently had a basal cell carcinoma diagnosed in the same location constantly asks the patient when he is “going to see someone about that lesion.” Additional history taking reveals that the patient has had little sun exposure in his life. He is otherwise healthy. Examination of the lesion shows a nevoid pink 6-mm intradermal nodule in the lower left nasolabial/upper maxillary area. Closer inspection reveals that the surface of the lesion is totally smooth and devoid of adnexae (pores, hairs). On palpation, the lesion is notably firmer than expected. The lesion has a slightly translucent appearance, almost as if light could pass through it. In light of the recurring trauma caused by shaving, and at his co-worker’s urging, the patient decides to have the lesion excised. The lesion is sent for pathologic examination, in this case by a general dermatologist from a laboratory of his insurance provider’s choosing. Calling the lesion a desmoplastic trichoepithelioma, the general pathologist nonetheless expressed his uncertainty, advising “clinical correlation.”
Dehydration Leads to Incidental Finding
ANSWER
The radiograph demonstrates that the nasogastric tube is within a decompressed stomach. Normal gas pattern is noted within the bowel and colon.
Of note, however, are tiny calcifications within the right upper quadrant. This finding is suggestive of cholelithiasis—in this case, likely an incidental finding.
ANSWER
The radiograph demonstrates that the nasogastric tube is within a decompressed stomach. Normal gas pattern is noted within the bowel and colon.
Of note, however, are tiny calcifications within the right upper quadrant. This finding is suggestive of cholelithiasis—in this case, likely an incidental finding.
ANSWER
The radiograph demonstrates that the nasogastric tube is within a decompressed stomach. Normal gas pattern is noted within the bowel and colon.
Of note, however, are tiny calcifications within the right upper quadrant. This finding is suggestive of cholelithiasis—in this case, likely an incidental finding.

A 57-year-old man is admitted to your facility for weakness and dehydration. His medical history is significant for rectal carcinoma, diabetes, and hypertension. His family states that his oral intake has been progressively less in the past several weeks. The patient’s vital signs are stable. Overall examination demonstrates a weak, frail-appearing man with dry mucous membranes and no other acute abnormalities. Lab work reveals that his serum sodium level and BUN/creatinine ratio are slightly elevated. To facilitate hydration, administration of medications, and nourishment, placement of a nasogastric tube is ordered; this is done just prior to your arrival at the patient’s room during rounds. As per protocol, an abdominal radiograph is obtained, and the nurses ask you to check it to confirm placement. The radiograph is shown. What is your impression?