User login
Dandruff Provides Clue for Rash
ANSWER
The correct answer is seborrhea (choice “c”), aka seborrheic dermatitis, a papulosquamous condition known to affect a variety of areas, including the groin and axillae. This patient could have had a close cousin of seborrhea, psoriasis (choice “a”), but he was missing corroborative involvement of his elbows, knees, and nails.
Groin rashes are often misdiagnosed as “yeast infections” (choice “b”); however, candidal involvement of the groin is actually quite unusual in men, and it would almost certainly have responded well to the imidazoles the patient had tried.
Eczema (choice “d”) is certainly common enough, but it is almost invariably highly pruritic and seldom affects the groin exclusively. It is therefore an unlikely choice.
DISCUSSION
This case nicely illustrates several useful points. One is that the differential for groin rashes is extensive (18 items long!) and demands careful thought, since cancer (eg, cutaneous T-cell lymphoma and extramammary Paget’s disease) can present as a rashlike eruption in the groin. The lack of response to the “usual and customary” treatments is precisely what should prompt further consideration.
Another learning point to be gleaned from this case is: When stumped, look elsewhere. Can’t figure out the groin rash? Look elsewhere, anywhere, for clues, when puzzled. In this case, finding signs of seborrhea elsewhere raised that possibility in the groin as well. Corroboration was also provided by the history of antecedent stress, a well-known trigger for flares of seborrhea, and by the relative lack of symptoms.
Treatment in this case entailed hydrocortisone 2.5% cream, but the real “cure” will only come with serious reduction of the patient’s stress level. His topical steroid use will be limited to no more than five consecutive days, with a break for two consecutive days per week.
Our real contribution to this patient’s well-being is in establishing the correct diagnosis and “selling” it to the patient, optimizing his confidence in the benignancy and self-limiting nature of his problem.
ANSWER
The correct answer is seborrhea (choice “c”), aka seborrheic dermatitis, a papulosquamous condition known to affect a variety of areas, including the groin and axillae. This patient could have had a close cousin of seborrhea, psoriasis (choice “a”), but he was missing corroborative involvement of his elbows, knees, and nails.
Groin rashes are often misdiagnosed as “yeast infections” (choice “b”); however, candidal involvement of the groin is actually quite unusual in men, and it would almost certainly have responded well to the imidazoles the patient had tried.
Eczema (choice “d”) is certainly common enough, but it is almost invariably highly pruritic and seldom affects the groin exclusively. It is therefore an unlikely choice.
DISCUSSION
This case nicely illustrates several useful points. One is that the differential for groin rashes is extensive (18 items long!) and demands careful thought, since cancer (eg, cutaneous T-cell lymphoma and extramammary Paget’s disease) can present as a rashlike eruption in the groin. The lack of response to the “usual and customary” treatments is precisely what should prompt further consideration.
Another learning point to be gleaned from this case is: When stumped, look elsewhere. Can’t figure out the groin rash? Look elsewhere, anywhere, for clues, when puzzled. In this case, finding signs of seborrhea elsewhere raised that possibility in the groin as well. Corroboration was also provided by the history of antecedent stress, a well-known trigger for flares of seborrhea, and by the relative lack of symptoms.
Treatment in this case entailed hydrocortisone 2.5% cream, but the real “cure” will only come with serious reduction of the patient’s stress level. His topical steroid use will be limited to no more than five consecutive days, with a break for two consecutive days per week.
Our real contribution to this patient’s well-being is in establishing the correct diagnosis and “selling” it to the patient, optimizing his confidence in the benignancy and self-limiting nature of his problem.
ANSWER
The correct answer is seborrhea (choice “c”), aka seborrheic dermatitis, a papulosquamous condition known to affect a variety of areas, including the groin and axillae. This patient could have had a close cousin of seborrhea, psoriasis (choice “a”), but he was missing corroborative involvement of his elbows, knees, and nails.
Groin rashes are often misdiagnosed as “yeast infections” (choice “b”); however, candidal involvement of the groin is actually quite unusual in men, and it would almost certainly have responded well to the imidazoles the patient had tried.
Eczema (choice “d”) is certainly common enough, but it is almost invariably highly pruritic and seldom affects the groin exclusively. It is therefore an unlikely choice.
DISCUSSION
This case nicely illustrates several useful points. One is that the differential for groin rashes is extensive (18 items long!) and demands careful thought, since cancer (eg, cutaneous T-cell lymphoma and extramammary Paget’s disease) can present as a rashlike eruption in the groin. The lack of response to the “usual and customary” treatments is precisely what should prompt further consideration.
Another learning point to be gleaned from this case is: When stumped, look elsewhere. Can’t figure out the groin rash? Look elsewhere, anywhere, for clues, when puzzled. In this case, finding signs of seborrhea elsewhere raised that possibility in the groin as well. Corroboration was also provided by the history of antecedent stress, a well-known trigger for flares of seborrhea, and by the relative lack of symptoms.
Treatment in this case entailed hydrocortisone 2.5% cream, but the real “cure” will only come with serious reduction of the patient’s stress level. His topical steroid use will be limited to no more than five consecutive days, with a break for two consecutive days per week.
Our real contribution to this patient’s well-being is in establishing the correct diagnosis and “selling” it to the patient, optimizing his confidence in the benignancy and self-limiting nature of his problem.

A 64-year-old man self-refers to dermatology for evaluation of an asymptomatic rash that has been present on his groin for more than a year. He has tried a number of topical antifungal creams (terbinafine, tolnaftate, and miconazole) and oral antifungal medications (terbinafine and ketoconazole), none of which produced any beneficial effect. The rash, which has been constant and limited to the groin, started around the same time his mother became ill. She eventually succumbed to cancer, leaving a number of stressful tasks for the patient to complete. As a result, the patient had to leave his job and spend a good deal of time away from home, repairing and then selling his mother’s home and possessions. At his first visit to dermatology, the groin rash is bright orange-red, covers both crural areas, and exhibits sharply defined margins that are faintly scaly. However, a KOH prep fails to demonstrate fungal elements, and since a number of antifungal treatments have already been tried without success, a provisional diagnosis of erythrasma is made. The patient is given topical clindamycin solution and oral cephalexin (500 mg tid for a week). Neither of these treatments changes the rash at all, so the man returns for a second visit. Since the rash is asymptomatic, you are not inclined to biopsy it. Clearly, the rash is neither fungal nor bacterial in origin, but in an effort to try something, you go to the supply room seeking samples of a mild steroid cream. When you return to the exam room, you find the man’s wife closely examining his scalp. When you ask what she is looking at, she says she is checking his dandruff, which has been flaring for months. When you look, you see that he does indeed have a brisk case of dandruff. Checking elsewhere, you notice that his external auditory meati are scaly and red, as are the eyebrow, postauricular sulci, and perinasilar areas. There are focally scaly, salmon-pink sites in his beard.
Man with History of Intense Sun Exposure
ANSWER
The correct answer is Poikiloderma of Civatte (POC; choice “a”), a consequence of extensive and poorly tolerated sun exposure. Although it is the result of multiple sunburns, POC is permanently fixed to affected skin, not merely a temporary phenomenon like sunburn—so choice “b” is incorrect.
Some forms of lupus (choice “c”) present with redness, but it tends to be of acute onset (in the beginning at least) and will usually involve epidermal disturbance (eg, scaling or erosions). The condition often manifests as discrete and confluent lesions with clearing centers.
Rosacea (choice “d”) can affect the neck and face. However, it will typically wax and wane, and will often involve papules and pustules as well. By contrast, POC is basically unchanging and has no palpable component.
DISCUSSION
POC is one of many indices of dermatoheliosis (chronic sun damage) and is reportedly more common in women, although it is not at all unusual in men with a history of overexposure to ultraviolet light sources. As this case demonstrates, POC often develops so gradually that even patients with pronounced involvement of several years’ duration may not be aware of their condition until it is pointed out to them.
The history of overexposure to the sun, the photodistribution of the erythema, and the distinct sparing provided by the chin all serve to confirm the nature of the problem. So too does the presence of multiple other indices of dermatoheliosis, such as actinic keratoses, solar lentigines, weathering, and the stellate scars on the dorsal arms of older patients.
Affected patients need a thorough skin check for possible malignancies at the time of the initial visit, with arrangements made for ongoing periodic checks. Patient education on the need for better sun protection can be reinforced by providing samples of sunscreen products. The diagnosis of POC is often a shock to patients, but the occasion provides the perfect opportunity to educate them about the effects of chronic overexposure to the sun.
For pronounced cases such as this one, ablation with the appropriate laser is, by far, the most effective option. But since POC is not truly a disease, most patients are content to learn the nature of their diagnosis and their role in limiting its worsening.
ANSWER
The correct answer is Poikiloderma of Civatte (POC; choice “a”), a consequence of extensive and poorly tolerated sun exposure. Although it is the result of multiple sunburns, POC is permanently fixed to affected skin, not merely a temporary phenomenon like sunburn—so choice “b” is incorrect.
Some forms of lupus (choice “c”) present with redness, but it tends to be of acute onset (in the beginning at least) and will usually involve epidermal disturbance (eg, scaling or erosions). The condition often manifests as discrete and confluent lesions with clearing centers.
Rosacea (choice “d”) can affect the neck and face. However, it will typically wax and wane, and will often involve papules and pustules as well. By contrast, POC is basically unchanging and has no palpable component.
DISCUSSION
POC is one of many indices of dermatoheliosis (chronic sun damage) and is reportedly more common in women, although it is not at all unusual in men with a history of overexposure to ultraviolet light sources. As this case demonstrates, POC often develops so gradually that even patients with pronounced involvement of several years’ duration may not be aware of their condition until it is pointed out to them.
The history of overexposure to the sun, the photodistribution of the erythema, and the distinct sparing provided by the chin all serve to confirm the nature of the problem. So too does the presence of multiple other indices of dermatoheliosis, such as actinic keratoses, solar lentigines, weathering, and the stellate scars on the dorsal arms of older patients.
Affected patients need a thorough skin check for possible malignancies at the time of the initial visit, with arrangements made for ongoing periodic checks. Patient education on the need for better sun protection can be reinforced by providing samples of sunscreen products. The diagnosis of POC is often a shock to patients, but the occasion provides the perfect opportunity to educate them about the effects of chronic overexposure to the sun.
For pronounced cases such as this one, ablation with the appropriate laser is, by far, the most effective option. But since POC is not truly a disease, most patients are content to learn the nature of their diagnosis and their role in limiting its worsening.
ANSWER
The correct answer is Poikiloderma of Civatte (POC; choice “a”), a consequence of extensive and poorly tolerated sun exposure. Although it is the result of multiple sunburns, POC is permanently fixed to affected skin, not merely a temporary phenomenon like sunburn—so choice “b” is incorrect.
Some forms of lupus (choice “c”) present with redness, but it tends to be of acute onset (in the beginning at least) and will usually involve epidermal disturbance (eg, scaling or erosions). The condition often manifests as discrete and confluent lesions with clearing centers.
Rosacea (choice “d”) can affect the neck and face. However, it will typically wax and wane, and will often involve papules and pustules as well. By contrast, POC is basically unchanging and has no palpable component.
DISCUSSION
POC is one of many indices of dermatoheliosis (chronic sun damage) and is reportedly more common in women, although it is not at all unusual in men with a history of overexposure to ultraviolet light sources. As this case demonstrates, POC often develops so gradually that even patients with pronounced involvement of several years’ duration may not be aware of their condition until it is pointed out to them.
The history of overexposure to the sun, the photodistribution of the erythema, and the distinct sparing provided by the chin all serve to confirm the nature of the problem. So too does the presence of multiple other indices of dermatoheliosis, such as actinic keratoses, solar lentigines, weathering, and the stellate scars on the dorsal arms of older patients.
Affected patients need a thorough skin check for possible malignancies at the time of the initial visit, with arrangements made for ongoing periodic checks. Patient education on the need for better sun protection can be reinforced by providing samples of sunscreen products. The diagnosis of POC is often a shock to patients, but the occasion provides the perfect opportunity to educate them about the effects of chronic overexposure to the sun.
For pronounced cases such as this one, ablation with the appropriate laser is, by far, the most effective option. But since POC is not truly a disease, most patients are content to learn the nature of their diagnosis and their role in limiting its worsening.
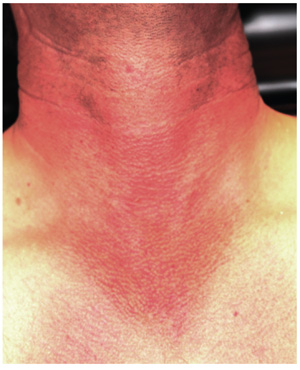
A 36-year-old man urgently self-refers to dermatology for evaluation of skin changes that a friend recently noticed and promptly insisted he seek care for. The patient denies symptoms and has never had any previous medical provider comment on his skin.
He has a long history of overexposure to the sun, as an oil field worker and as a professional bass fisherman on weekends. “If the sun is up, chances are I’m out in it, seven days a week,” is how the patient puts it, adding that he knows he needs sunscreen but has just never bothered with it. At work, he is required to wear a hardhat; in his leisure time, he wears short sleeves and a ball cap, if anything, on his head.
Overall, the patient looks easily 10 years older than his stated age, with splotchy, weathered skin and a very red face on which multiple actinic keratoses are readily noted. With the patient’s shirt off, the primary reason for his visit is apparent: an intensely red, sharply demarcated, blanchable macular V-shaped patch of skin that roughly coincides with the area not usually covered by his shirt. This same process extends onto his anterior neck and cheeks, becoming slightly less intense on posterior neck skin. The U-shaped area of his anterior neck (directly under his chin) is spared, with sharply defined margins between red and white skin.
Examination with 10x magnification reveals a dense mat of fine telangiectatic, blanchable blood vessels comprising the bulk of the erythema. On both sides of the anterolateral neck, rows of sharply defined, 1- to 1.5-mm whitish yellow papules can be seen, virtually covering the area. These gradually thin out, then end, as normal skin is encountered on the upper chest.
Man Gets Burning Sensation in Chest During an Argument
ANSWER
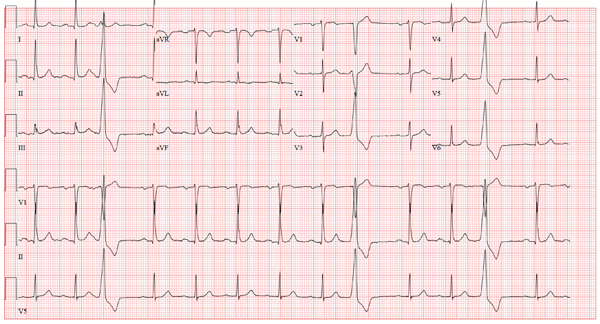
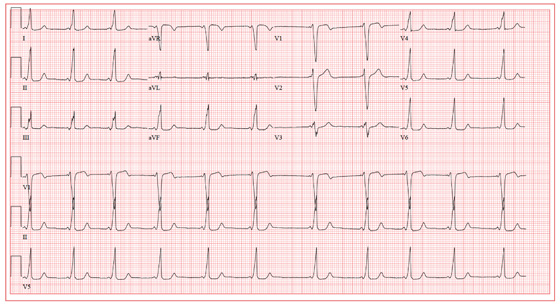
The ECG shows normal sinus rhythm with a first-degree atrioventricular block with frequent premature ventricular complexes. There is no evidence of ongoing ischemia or recent myocardial injury or infarction.
First-degree atrioventricular block occurs when atrial activation and conduction are always transmitted to the ventricles, albeit with an unusual delay at or below the atrioventricular node. It is characterized by a PR interval greater than 200 ms.
Three premature ventricular complexes are also seen (see beats 3, 9, and 12). These are characterized by wide complexes originating in the ventricle, which do not occur within the conduction atrioventricular node or the His–Purkinje system. Premature ventricular complexes are not preceded by a P wave, and the QRS complex is wider than 100 ms. They do not affect atrial conduction unless they are conducted retrograde up the atrioventricular node or an accessory pathway into the right atrium.
ANSWER
The ECG shows normal sinus rhythm with a first-degree atrioventricular block with frequent premature ventricular complexes. There is no evidence of ongoing ischemia or recent myocardial injury or infarction.
First-degree atrioventricular block occurs when atrial activation and conduction are always transmitted to the ventricles, albeit with an unusual delay at or below the atrioventricular node. It is characterized by a PR interval greater than 200 ms.
Three premature ventricular complexes are also seen (see beats 3, 9, and 12). These are characterized by wide complexes originating in the ventricle, which do not occur within the conduction atrioventricular node or the His–Purkinje system. Premature ventricular complexes are not preceded by a P wave, and the QRS complex is wider than 100 ms. They do not affect atrial conduction unless they are conducted retrograde up the atrioventricular node or an accessory pathway into the right atrium.
ANSWER
The ECG shows normal sinus rhythm with a first-degree atrioventricular block with frequent premature ventricular complexes. There is no evidence of ongoing ischemia or recent myocardial injury or infarction.
First-degree atrioventricular block occurs when atrial activation and conduction are always transmitted to the ventricles, albeit with an unusual delay at or below the atrioventricular node. It is characterized by a PR interval greater than 200 ms.
Three premature ventricular complexes are also seen (see beats 3, 9, and 12). These are characterized by wide complexes originating in the ventricle, which do not occur within the conduction atrioventricular node or the His–Purkinje system. Premature ventricular complexes are not preceded by a P wave, and the QRS complex is wider than 100 ms. They do not affect atrial conduction unless they are conducted retrograde up the atrioventricular node or an accessory pathway into the right atrium.
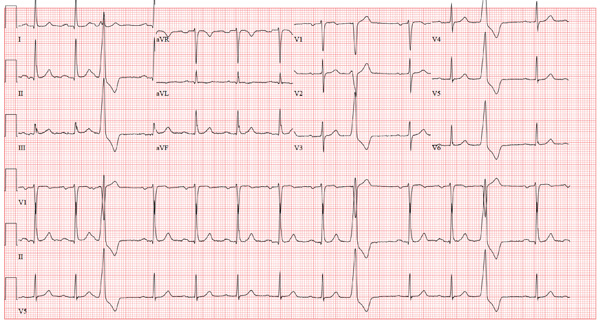
An 80-year-old man presents to your office after having two separate episodes of chest pain. The first occurred two weeks ago, while the patient was arguing with his home health nurse. He describes the pain as a “burning” sensation deep in his chest—similar to that from his long-standing history of esophageal reflux, with the exception that the onset and resolution were much quicker. A second, similar episode occurred two days ago, again during an argument with his nurse. He did not disclose either episode to the nurse. However, he was sufficiently concerned about the possibility of a cardiac cause that he decided to see you. When questioning him about his chest pain, you learn that there was no associated diaphoresis, shortness of breath, or pain radiation to the neck or arm. He denies symptoms of bradycardia, tachycardia, or palpitations. When you question him about the argument with his nurse, you learn that he has been eating chips and salsa, which you have previously advised against, given his history of esophageal reflux, Barrett’s esophagus, and endoscopic confirmation of esophageal dysplasia. The medical history is also significant for bilateral below-knee amputations from trauma sustained during army service in the Korean War. He has had multiple bilateral stump revisions, such that he can no longer wear prostheses and is wheelchair bound. Adenomatous colonic polyps, iron-deficiency anemia, hypothyroidism, asthma, benign prostatic hypertrophy, glaucoma, and Parkinson’s disease complete the medical history. The family history is remarkable for a father who died of a hemorrhagic stroke and a mother who died of renal failure. The patient, a widower, resides at home with a live-in nurse and a housekeeper. His medication list includes aspirin, lisinopril, levothyroxine, carbidopa/levodopa, and travoprost and timolol eye drops. He is allergic to sulfa. The review of symptoms is remarkable for urinary retention and recent resolution of diarrhea. Pertinent physical findings in this pleasant elderly man include audible wheezing and a raspy voice. The lungs are diffusely wheezy on expiration, and there is no conversational dyspnea or accessory muscle use. The neck veins are flat, and while heart sounds are distant, there are no murmurs, rubs, or extra heart sounds. The abdomen is soft and nontender. A low-amplitude tremor is present in both hands, and there is no cogwheeling. Serum B-type natriuretic peptide is 190 pg/mL and serum troponin levels are negative. An ECG reveals the following: a ventricular rate of 79 beats/min; PR interval, 212 ms; QRS duration, 92 ms; QT/QTc interval, 358/410 ms; P axis, 35°; R axis, 47°; and T axis, 69°. What is your interpretation of this ECG?
Woman with Malaise, Cough, and Shoulder Pain
ANSWER
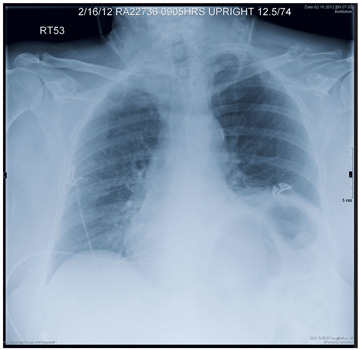
The radiograph demonstrates a slightly elevated left hemidiaphragm, which is nonspecific, as well as normal to slightly increased lung markings. There is no definite infiltrate or consolidation noted.
Of note, there is a displaced fracture of the mid-distal left clavicle, which may be partially healed. There appears to be a focal lytic lesion within that area. The surrounding bone is extremely osteopenic as well.
These findings, especially in the absence of injury or trauma, raise the question of a pathologic fracture, and further workup is warranted. Subsequent workup on this patient demonstrated a large renal mass, which was felt to be, most likely, a metastatic lesion.
ANSWER
The radiograph demonstrates a slightly elevated left hemidiaphragm, which is nonspecific, as well as normal to slightly increased lung markings. There is no definite infiltrate or consolidation noted.
Of note, there is a displaced fracture of the mid-distal left clavicle, which may be partially healed. There appears to be a focal lytic lesion within that area. The surrounding bone is extremely osteopenic as well.
These findings, especially in the absence of injury or trauma, raise the question of a pathologic fracture, and further workup is warranted. Subsequent workup on this patient demonstrated a large renal mass, which was felt to be, most likely, a metastatic lesion.
ANSWER
The radiograph demonstrates a slightly elevated left hemidiaphragm, which is nonspecific, as well as normal to slightly increased lung markings. There is no definite infiltrate or consolidation noted.
Of note, there is a displaced fracture of the mid-distal left clavicle, which may be partially healed. There appears to be a focal lytic lesion within that area. The surrounding bone is extremely osteopenic as well.
These findings, especially in the absence of injury or trauma, raise the question of a pathologic fracture, and further workup is warranted. Subsequent workup on this patient demonstrated a large renal mass, which was felt to be, most likely, a metastatic lesion.
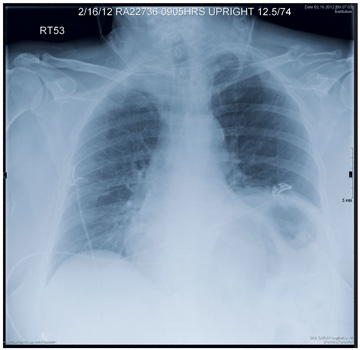
A 63-year-old woman presents to your clinic with complaints of general malaise, weakness, and occasional cough—symptoms that started a couple of days ago. Also, her left shoulder has been hurting her “more than usual.” She denies any fever, chills, nausea, or vomiting. She admits to smoking two packs of cigarettes per day and having hypertension. Otherwise, her medical history is unremarkable. During the physical exam, you observe that the patient is an older female in no obvious distress. She is afebrile, and the rest of her vital signs, including pulse oximetry, are normal. Her breath sounds demonstrate scattered rhonchi but overall are clear. She does have localized tenderness over her left shoulder, with decreased range of motion in that arm secondary to the pain and stiffness in it. You send a blood sample to the lab to check her complete blood count and obtain a chest radiograph, which is shown. What is your impression?
Woman Goes Gray - Not Her Hair, Her Face
ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.
ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.
ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.
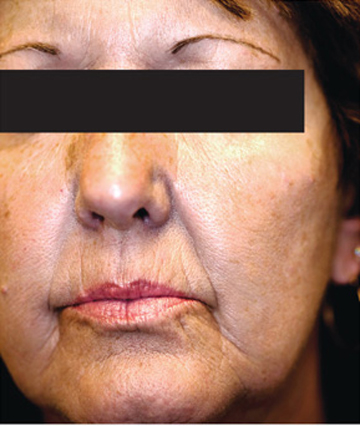
A 61-year-old woman presents with marked changes in her skin that she first noted several months ago. These have become so noticeable that friends and family, growing alarmed, urged her to seek medical evaluation. The patient, who is a hospital nurse, denies taking any prescription medicines (eg, minocycline, amiodarone) during this time. She further denies having any accompanying symptoms in her facial skin. On examination, the patient’s face and neck are markedly discolored—a uniform shade of slate gray. The problem affects her whole body, but is more evident in sun-exposed areas. The discoloration is not blanchable, nor can it be removed by scrubbing the skin with an alcohol-soaked pad. Oral mucosal surfaces, including the gums, are also affected, but less so than the facial skin. These findings prompt additional history taking, with a particular focus on nonprescription medications. As a result, the patient recalls taking an oral colloidal silver–containing solution from the health food store for several months, for reasons she cannot recall.
Man Fell Off Roof
ANSWER
The radiograph shows a comminuted fracture of the os calcis, as well as a comminuted fracture of the navicular bone. CT on this patient was pending to further assess for additional fractures, and the patient will likely undergo open reduction and internal fixation for definitive treatment.
ANSWER
The radiograph shows a comminuted fracture of the os calcis, as well as a comminuted fracture of the navicular bone. CT on this patient was pending to further assess for additional fractures, and the patient will likely undergo open reduction and internal fixation for definitive treatment.
ANSWER
The radiograph shows a comminuted fracture of the os calcis, as well as a comminuted fracture of the navicular bone. CT on this patient was pending to further assess for additional fractures, and the patient will likely undergo open reduction and internal fixation for definitive treatment.

A 51-year-old man is brought to your facility for evaluation of right foot pain after sustaining a fall. He was working on top of his house when he lost his balance and fell approximately 15 to 20 feet. He states he landed on his feet and has the above complaint. His medical history is significant for hypertension and heart disease. He regularly works as a truck driver and smokes one to two packs of cigarettes per day. His exam shows a middle-aged male who is uncomfortable but in no obvious distress. Primary survey is normal. His right foot shows no obvious deformity. There is some swelling and moderate tenderness over the dorsal aspect, as well as in the area of the heel. Pulses are present, sensation is intact, and good capillary refill time is noted. Portable radiograph of the right foot is obtained. What is your impression?
Woman Faints During Concert
ANSWER
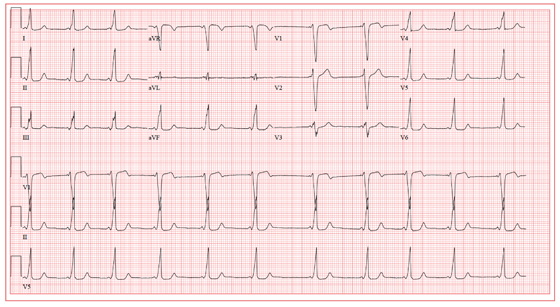
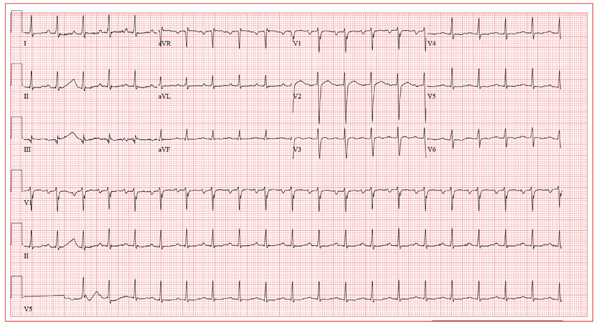
The ECG shows a sinus rhythm with a sinus arrhythmia and a short PR interval with ventricular pre-excitation, consistent with Wolff-Parkinson-White syndrome.
Ventricular pre-excitation occurs when conduction proceeds from the atria to the ventricles via an accessory pathway without involving the atrioventricular node, and is evident from a short PR interval and a delta wave immediately preceding the QRS complex. The delta wave illustrates conduction down the accessory pathway.
Careful examination reveals positive delta waves in the limb leads and the precordial leads, with an R-wave transition occurring in lead V4. This suggests the location of the accessory pathway to be on the tricuspid annulus (right sided) in an anteroseptal location. This location was confirmed by electrophysiology study, as was the pathway’s participation in an orthodromic reentry tachycardia responsible for the patient’s episodes of near-syncope and syncope. It was successfully ablated.
The sinus arrhythmia seen on the ECG is a normal variant.
ANSWER
The ECG shows a sinus rhythm with a sinus arrhythmia and a short PR interval with ventricular pre-excitation, consistent with Wolff-Parkinson-White syndrome.
Ventricular pre-excitation occurs when conduction proceeds from the atria to the ventricles via an accessory pathway without involving the atrioventricular node, and is evident from a short PR interval and a delta wave immediately preceding the QRS complex. The delta wave illustrates conduction down the accessory pathway.
Careful examination reveals positive delta waves in the limb leads and the precordial leads, with an R-wave transition occurring in lead V4. This suggests the location of the accessory pathway to be on the tricuspid annulus (right sided) in an anteroseptal location. This location was confirmed by electrophysiology study, as was the pathway’s participation in an orthodromic reentry tachycardia responsible for the patient’s episodes of near-syncope and syncope. It was successfully ablated.
The sinus arrhythmia seen on the ECG is a normal variant.
ANSWER
The ECG shows a sinus rhythm with a sinus arrhythmia and a short PR interval with ventricular pre-excitation, consistent with Wolff-Parkinson-White syndrome.
Ventricular pre-excitation occurs when conduction proceeds from the atria to the ventricles via an accessory pathway without involving the atrioventricular node, and is evident from a short PR interval and a delta wave immediately preceding the QRS complex. The delta wave illustrates conduction down the accessory pathway.
Careful examination reveals positive delta waves in the limb leads and the precordial leads, with an R-wave transition occurring in lead V4. This suggests the location of the accessory pathway to be on the tricuspid annulus (right sided) in an anteroseptal location. This location was confirmed by electrophysiology study, as was the pathway’s participation in an orthodromic reentry tachycardia responsible for the patient’s episodes of near-syncope and syncope. It was successfully ablated.
The sinus arrhythmia seen on the ECG is a normal variant.
A19-year-old woman is referred from the emergency department (ED) for follow-up. While attending a concert last weekend, she experienced an episode of syncope, was promptly resuscitated by EMTs on site, and was taken by friends to the ED for evaluation. On arrival, she was alert and oriented, albeit embarrassed that she was responsible for her friends missing the remainder of the concert. She admitted having a couple of beers and thought she may have been dehydrated. Following a history, physical exam, lab work, and an ECG, she was discharged in stable condition and asked to follow up in your clinic. As you ask her to remember the episode, she does not recall becoming light-headed or dizzy, and denies having chest pain or palpitations. She says her medical history is unremarkable; however, upon careful questioning, she admits having had several episodes of near-syncope beginning at age 16, with the most recent occurring six months ago. She is a freshman at a local community college and works as a barista at a local coffeehouse. She has no drug allergies and is currently taking no medications. She drinks socially although she is underage, does not smoke, and denies recreational drug use. Her review of systems is negative, and her physical exam is within normal limits for her gender and age. Her last menstrual period was two weeks ago. Reviewing the medical records from the ED, you discover the blood alcohol content was 0.08 and the toxicology screen was negative. A serum beta human chorionic gonadotropin (β-HCG) for pregnancy was negative as well. The ECG reveals a ventricular rate of 64 beats/min; PR interval, 64 ms; QRS duration, 146 ms; QT/QTc interval, 454/468 ms; P axis, unmeasurable; R axis, 60°; and T axis, 92°. What is your interpretation of this ECG, and what do you suspect is the cause of her syncope?
Woman with Abdominal Pain Following Severe Car Crash
ANSWER
The radiograph shows a comminuted fracture at the midshaft of the tibia. In addition, there is a comminuted fracture of the proximal tibial metaphysis extending to the tibia plateau. Also noted is a comminuted fracture of the distal femur metaphysis extending to the intercondylar notch
ANSWER
The radiograph shows a comminuted fracture at the midshaft of the tibia. In addition, there is a comminuted fracture of the proximal tibial metaphysis extending to the tibia plateau. Also noted is a comminuted fracture of the distal femur metaphysis extending to the intercondylar notch
ANSWER
The radiograph shows a comminuted fracture at the midshaft of the tibia. In addition, there is a comminuted fracture of the proximal tibial metaphysis extending to the tibia plateau. Also noted is a comminuted fracture of the distal femur metaphysis extending to the intercondylar notch

A 43-year-old woman is airlifted to your facility from an outlying area following a severe motor vehicle collision. Details are unclear, but there were known fatalities at the scene. Her primary complaints are abdominal pain and noted deformities of the lower extremities, according to the transporting medical personnel. On arrival, she is noted to be semi-arousable and is moving distal portions of all four extremities. Her heart rate is 150 beats/min, with a blood pressure of 80/40 mm Hg. She responds to initial fluid and volume resuscitation. She has no pertinent medical history. Her response to the fluid resuscitation is sufficient to stabilize her for transport to the CT scanner for additional imaging. Prior to the transfer, though, a portable radiograph of her right tibia is obtained. What is your impression?
Patient's Condition is "All Thumbs"
ANSWER
The correct answer is habit-tic deformity (choice “d”), a relatively common self-inflicted condition relegated to thumbnails.
Chronic candidal paronychia (choice “a”) has certain similarities to habit-tic deformity (eg, loss of connection between cuticle and nail plate) but it also has an inflammatory aspect that manifests as chronic focal tenderness, redness, and swelling of the adjacent perionychial tissue.
The clinical picture and total lack of response to antifungal medications made a diagnosis of onychomycosis (choice “b”) quite unlikely. Canaliformis defect (choice “c”) involves a central longitudinal linear concave defect in the affected nails and is therefore incorrect.
DISCUSSION
Fungal infection in fingernails, while not unknown, is about 18 times less likely than the same condition in toenails. Nonetheless, onychomycosis continues to be vastly overdiagnosed by clinicians whose differential diagnoses are lacking.
Habit-tic deformity is a perfect example of this phenomenon. Also called onychotillomania, habit-tic is actually caused by chronic picking of the cuticles; over time, this results in the creation of transverse parallel grooves that persist for the 4 to 4.5 months it takes for the nail plate to grow out. It rarely occurs on fingernails other than the thumbnails. Habit-tic, as in this case, can also involve modest traumatically induced subungual bleeding, seen as brownish discoloration.
Many patients have good insight into their causative role, but just as many pick their cuticle unconsciously. The obvious solution is to stop the offending behavior and/or put a barrier on the nails, but neither measure has met with much success. One potential remedy (see “Suggested Reading”) is to fill the cuticular sulcus with protective acrylate glue and let it dry. This, in effect, creates a barrier while the cuticle heals and reattaches to the nail plate (although the potential for contact dermatitis may become a concern). Hypnosis and other behavior modification have also been tried.
For many patients, just knowing what they don’t have is quite helpful. For providers, it is helpful to develop a differential for conditions that involve nail dystrophy, including the incorrect answer choices offered here. If fungal infection were truly a possibility, the best way to confirm that diagnosis would be to send a nail clipping to pathology, either for sectioning and identification of fungal elements or an actual fungal culture.
SUGGESTED READING
Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146(11):1222-1223.
ANSWER
The correct answer is habit-tic deformity (choice “d”), a relatively common self-inflicted condition relegated to thumbnails.
Chronic candidal paronychia (choice “a”) has certain similarities to habit-tic deformity (eg, loss of connection between cuticle and nail plate) but it also has an inflammatory aspect that manifests as chronic focal tenderness, redness, and swelling of the adjacent perionychial tissue.
The clinical picture and total lack of response to antifungal medications made a diagnosis of onychomycosis (choice “b”) quite unlikely. Canaliformis defect (choice “c”) involves a central longitudinal linear concave defect in the affected nails and is therefore incorrect.
DISCUSSION
Fungal infection in fingernails, while not unknown, is about 18 times less likely than the same condition in toenails. Nonetheless, onychomycosis continues to be vastly overdiagnosed by clinicians whose differential diagnoses are lacking.
Habit-tic deformity is a perfect example of this phenomenon. Also called onychotillomania, habit-tic is actually caused by chronic picking of the cuticles; over time, this results in the creation of transverse parallel grooves that persist for the 4 to 4.5 months it takes for the nail plate to grow out. It rarely occurs on fingernails other than the thumbnails. Habit-tic, as in this case, can also involve modest traumatically induced subungual bleeding, seen as brownish discoloration.
Many patients have good insight into their causative role, but just as many pick their cuticle unconsciously. The obvious solution is to stop the offending behavior and/or put a barrier on the nails, but neither measure has met with much success. One potential remedy (see “Suggested Reading”) is to fill the cuticular sulcus with protective acrylate glue and let it dry. This, in effect, creates a barrier while the cuticle heals and reattaches to the nail plate (although the potential for contact dermatitis may become a concern). Hypnosis and other behavior modification have also been tried.
For many patients, just knowing what they don’t have is quite helpful. For providers, it is helpful to develop a differential for conditions that involve nail dystrophy, including the incorrect answer choices offered here. If fungal infection were truly a possibility, the best way to confirm that diagnosis would be to send a nail clipping to pathology, either for sectioning and identification of fungal elements or an actual fungal culture.
SUGGESTED READING
Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146(11):1222-1223.
ANSWER
The correct answer is habit-tic deformity (choice “d”), a relatively common self-inflicted condition relegated to thumbnails.
Chronic candidal paronychia (choice “a”) has certain similarities to habit-tic deformity (eg, loss of connection between cuticle and nail plate) but it also has an inflammatory aspect that manifests as chronic focal tenderness, redness, and swelling of the adjacent perionychial tissue.
The clinical picture and total lack of response to antifungal medications made a diagnosis of onychomycosis (choice “b”) quite unlikely. Canaliformis defect (choice “c”) involves a central longitudinal linear concave defect in the affected nails and is therefore incorrect.
DISCUSSION
Fungal infection in fingernails, while not unknown, is about 18 times less likely than the same condition in toenails. Nonetheless, onychomycosis continues to be vastly overdiagnosed by clinicians whose differential diagnoses are lacking.
Habit-tic deformity is a perfect example of this phenomenon. Also called onychotillomania, habit-tic is actually caused by chronic picking of the cuticles; over time, this results in the creation of transverse parallel grooves that persist for the 4 to 4.5 months it takes for the nail plate to grow out. It rarely occurs on fingernails other than the thumbnails. Habit-tic, as in this case, can also involve modest traumatically induced subungual bleeding, seen as brownish discoloration.
Many patients have good insight into their causative role, but just as many pick their cuticle unconsciously. The obvious solution is to stop the offending behavior and/or put a barrier on the nails, but neither measure has met with much success. One potential remedy (see “Suggested Reading”) is to fill the cuticular sulcus with protective acrylate glue and let it dry. This, in effect, creates a barrier while the cuticle heals and reattaches to the nail plate (although the potential for contact dermatitis may become a concern). Hypnosis and other behavior modification have also been tried.
For many patients, just knowing what they don’t have is quite helpful. For providers, it is helpful to develop a differential for conditions that involve nail dystrophy, including the incorrect answer choices offered here. If fungal infection were truly a possibility, the best way to confirm that diagnosis would be to send a nail clipping to pathology, either for sectioning and identification of fungal elements or an actual fungal culture.
SUGGESTED READING
Ring DS. Inexpensive solution for habit-tic deformity. Arch Dermatol. 2010;146(11):1222-1223.

A 56-year-old man is referred to dermatology for evaluation of a “fungal infection” that has affected both thumbnails for at least 20 years. While the condition produces no symptoms, it has nonetheless been a source of constant embarrassment to him. He denies having any such problems with his toenails. Furthermore, he says the problem has persisted despite the use of numerous topical and oral medications, including topical miconazole, clotrimazole, oil of eucalyptus, bleach, and the oral antifungals terbinafine and griseofulvin. None of these has had any effect. Additional history taking reveals that the patient is highly allergy-prone; he had seasonal allergies and asthma as a child. He also has a history of extremely dry and sensitive skin. On examination, the problems with the patient’s thumbnails are obvious, with traumatic absence of cuticles, widening and deepening of the cuticular sulcus, and deep parallel transverse lines involving the entire visible nail plates. Scattered subungual patches of brown discoloration are also seen beneath the lines. None of the patient’s other nails are abnormal in any way.
Atrial Flutter Follow-up
ANSWER
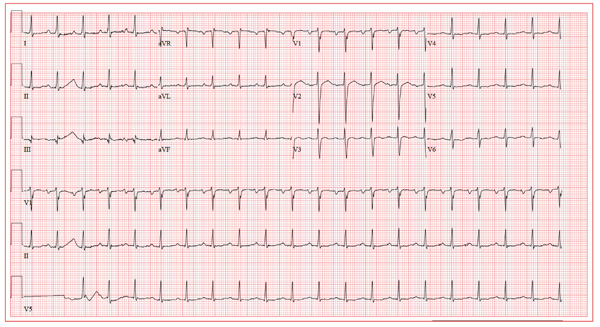
The ECG reveals sinus tachycardia with possible left atrial enlargement and a nonspecific T-wave abnormality. Sinus tachycardia is evidenced by a sinus rate > 100 beats/min, with one corresponding QRS complex for each P wave.
The criteria for left atrial enlargement include a P-wave duration ≥ 0.12 s in lead II, notched P waves in the limb leads, and a biphasic P wave in lead V1, with the terminal portion of the P wave (corresponding to the left atrium) being negative with a duration of ≥ 0.04 s and a depth ≥ 1 mm. (The echocardiogram shows a left atrial measurement at the upper limits of normal.)
Nonspecific T-wave changes are again seen in the precordial leads. Based on these findings, there is no structural disease to suggest a cause for this patient’s episode of atrial flutter.
ANSWER
The ECG reveals sinus tachycardia with possible left atrial enlargement and a nonspecific T-wave abnormality. Sinus tachycardia is evidenced by a sinus rate > 100 beats/min, with one corresponding QRS complex for each P wave.
The criteria for left atrial enlargement include a P-wave duration ≥ 0.12 s in lead II, notched P waves in the limb leads, and a biphasic P wave in lead V1, with the terminal portion of the P wave (corresponding to the left atrium) being negative with a duration of ≥ 0.04 s and a depth ≥ 1 mm. (The echocardiogram shows a left atrial measurement at the upper limits of normal.)
Nonspecific T-wave changes are again seen in the precordial leads. Based on these findings, there is no structural disease to suggest a cause for this patient’s episode of atrial flutter.
ANSWER
The ECG reveals sinus tachycardia with possible left atrial enlargement and a nonspecific T-wave abnormality. Sinus tachycardia is evidenced by a sinus rate > 100 beats/min, with one corresponding QRS complex for each P wave.
The criteria for left atrial enlargement include a P-wave duration ≥ 0.12 s in lead II, notched P waves in the limb leads, and a biphasic P wave in lead V1, with the terminal portion of the P wave (corresponding to the left atrium) being negative with a duration of ≥ 0.04 s and a depth ≥ 1 mm. (The echocardiogram shows a left atrial measurement at the upper limits of normal.)
Nonspecific T-wave changes are again seen in the precordial leads. Based on these findings, there is no structural disease to suggest a cause for this patient’s episode of atrial flutter.
A 39-year-old business professional returns to your clinic for follow-up one month after a synchronized cardioversion to treat abrupt-onset atrial flutter (see January 2012 ECG Challenge). He is slightly short of breath, he says, because he ran up six flights of stairs to see you in clinic after undergoing an echocardiogram. Briefly, he developed atrial flutter presumably as a result of consuming a large quantity of caffeinated coffee along with several energy drinks containing taurine. He has been under a significant amount of stress at work for the past six months, working on a project that he predicted would play a major role in his career. The deadline has come and gone, and his business transaction was a success. He has taken your advice to avoid energy drinks, consume coffee in moderation, stop smoking, get plenty of rest, and exercise. His affect is much improved. He is pleasant, jovial, and relieved that he has had no subsequent episodes of atrial flutter. His medical history is remarkable for that single episode of atrial flutter, as well as childhood cases of chickenpox and mumps. He is taking ibuprofen for a sore knee as a result of “too much basketball.” He has no known drug allergies. Following his cardioversion, his alcohol consumption decreased from two cocktails in the evening and a 12-pack of beer on the weekends to an occasional cocktail during the week and two to four beers on the weekends. He denies illicit drug use. The review of systems is unremarkable. The physical exam reveals a thin, well-developed man in no distress. His weight is 170 lb and his height, 74”. Vital statistics include a blood pressure of 128/72 mm Hg; pulse, 110 beats/min; respiratory rate, 16 breaths/min; temperature, 98.4°F; and O2 saturation, 100% on room air. The chest is clear to auscultation in all lung fields. There are no murmurs, rubs, clicks, or extra heart sounds. The abdomen is soft and nontender. The pulses are equal and bounding bilaterally. The neurologic exam is benign. The echocardiogram performed earlier shows a left ventricular ejection fraction of 68%, normal left and right ventricular volumes and function, normal valvular function, and a left atrial measurement of 3.8 cm (normal, 1.6 to 4.0 cm). An ECG performed just before you entered the exam room reveals the following: a ventricular rate of 122 beats/min; PR interval, 184 ms; QRS duration, 90 ms; QT/QTc interval, 282/401 ms; P axis, 24°; R axis, 28°; and T axis, –45°. What is your interpretation of this ECG?