User login
Hospital Medicine Has a Specialty Code. Is the Memo Still in the Mail?
In recognizing the importance of Hospital Medicine (HM) and its practitioners, the Centers for Medicare and Medicaid Services (CMS) awarded the field a specialty designation in 2016. The code is self-selected by hospitalists and used by the CMS for programmatic and claims processing purposes. The HM code (“C6”), submitted to the CMS by the provider or their designee through the Provider Enrollment Chain and Ownership System (PECOS), in turn links to the National Provider Identification provider data.
The Society of Hospital Medicine® sought the designation given the growth of hospitalists practicing nationally, their impact on the practice of medicine in the inpatient setting,1 and their secondary effects on global care.2 In fact, early efforts by the CMS to transition physician payments to the value-based payment used specialty designations to create benchmarks in cost metrics, heightening the importance for hospitalists to be able to assess their performance. The need to identify any shifts in resource utilization and workforce mix in the broader context of health reforms necessitated action. Essentially, to understand the “why’s” of hospital medicine, the field required an accounting of the “who’s” and “where’s.”
The CMS granted the C6 designation in 2016, and it went live in April 2017. Despite the code’s brief two-year tenure, calls for its creation long predated its existence. As such, the new modifier requires an initial look to help steer the role of HM in any future CMS and managed care organization (MCO) quality, payment, or practice improvement activities.
METHODS
We analyzed publicly available 2017 Medicare Part B utilization data3 to explore the rates of Evaluation & Management (E&M) codes used across specialties, using the C6 designation to identify hospitalists.
To try to estimate the percentage of hospitalists who were likely billing under the C6 designation, we then compared the rates of C6 billing to expected rates of hospitalist E&M billing based on an analysis of hospitalist prevalence in the 2012 Medicare physician payment data. Prior work to identify hospitalists before the implementation of the C6 designation relied on thresholds of inpatient codes for various inpatient E&M services.4,5 We used our previously published approach of a threshold of 60% of inpatient E&M hospital services to differentiate hospitalists from their parent specialties.6 We also calculated the expected rates of E&M billing for other select specialty services by applying the 2012 E&M coding trends to the 2017 data.
RESULTS
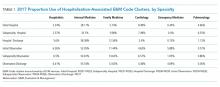
Table 1 shows the distribution of inpatient E&M codes billed by hospitalists using the C6 identification, as well as the use of those codes by other specialists. Hospitalists identified by the C6 designation billed only 2%-5% of inpatient and 6% of observation codes. As an example, in 2017, discharge CPT codes 99238 and 99239 were used 7,872,323 times. However, C6-identified hospitalists accounted for only 441,420 of these codes.
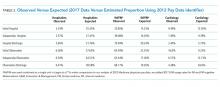
Table 2 compares the observed billing rates by specialty using the C6 designation to identify hospitalists with what would be the expected rates with the 2012 threshold-based specialty billing designation applied to the 2017 data. This comparison demonstrates that hospitalist billing based on the C6 modifier use is approximately one-tenth of what would have been their expected volume of E&M services.
DISCUSSION
We examined the patterns of hospitalist billing using the C6 hospital medicine specialty modifier, comparing billing patterns with what we would expect hospitalist activity to be if we had used a threshold-based approach. The difference between the C6 and the threshold-based approaches to assessing hospitalist activity suggests that as few as 10% of hospitalists have adopted the C6 code.
Why is the adoption of the C6 modifier so low? Although administrative data do not allow us to identify the reasons why providers chose to disregard the C6 designation, we can speculate on causes. There are, to date, low direct risks and recognized benefits with using the code. We hypothesize that several factors could be impeding whether providers use the modifier to bring about potential gains. The first may be knowledge-related; ie, hospitalists might not be familiar with the specialty code or unaware of the importance of accurately capturing hospitalist practice patterns. They may also wrongly assume that their practices are aware of the revision or have submitted the appropriate paperwork. Similarly, practice personnel may lack knowledge regarding the code or the importance of its use. The second factor may be logistical; ie, administrative barriers such as difficulty accessing the Provider Enrollment, Chain and Ownership System (PECOS) and out-of-date paper registration forms impede fast uptake. The final reason might be related to professionals whose tenures as hospitalists will be brief, and their unease of carrying an identifier into their next non-HM position prompts hesitation. Providers may have a misperception that using the C6 code may somehow impact or limit their future scope of practice, when, in fact, they may change their Medicare specialty designation at any time.
Changes in reimbursement models, including the Bundled Payments for Care Improvement Advanced (BPCI-A) and other value-based initiatives, heighten the need for a more accurate identification of the specialty. Classifying individual providers and groups to make valid performance comparisons is relevant for the same reasons. The CMS continues to advance cost and efficiency measures in its publicly accessible physiciancompare.gov website.7 Without an improved ability to identify services provided by hospitalists—by both CMS and commercial entities—the potential benefits delivered by hospitalists in terms of improved care quality, safety, or efficiency could go undetected by payers and policymakers. Moreover, C6 may be used in other ways by the CMS throughout its payment systems and programmatic efforts that use specialty to differentiate between Medicare providers.8 Finally, the C6 is an identifier for the Medicare fee-for-service system; state programs and MCOs may not identify hospitalists in the same manner, or at all. Therefore, it may make it more difficult for those groups and HM researchers to study the trends in care delivery changes. The specialty needs to engage with these other payers to assist in revising their information systems to better account for how hospitalists care for their insured populations.
Although we would expect a natural increase in C6 adoption over time, optimally meeting stakeholders’ data needs requires more rapid uptake. Our analysis is limited by our assumption that specialty patterns of code use remain similar from 2012 to 2017. Regardless, the magnitude of the difference between the estimate of hospitalists using the C6 versus billing thresholds strongly suggests underuse of the C6 designation. The CMS and MCOs have an increasing need for valid and representative data, and C6 can be used to assess “HM-adjusted” resource utilization, relative value units (RVUs), and performance evaluations. Therefore, hospitalists may see more incentives to use the C6 specialty code in a manner consistent with other recognized subspecialties.
Disclaimer
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, and the Health Services Research and Development Service. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
1. Wachter RM, Goldman L. Zero to 50,000—The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
2. Quinn R. HM 2016: A year in review. The Hospitalist. 2016;12. https://www.the-hospitalist.org/hospitalist/article/121419/everything-you-need-know-about-bundled-payments-care-improvement
3. Centers for Medicare and Medicaid Services. Medicare Utilization for Part B. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicarefeeforsvcpartsab/medicareutilizationforpartb.html. Accessed June 14, 2019.
4. Saint S, Christakis DA, Baldwin L-M, Rosenblatt R. Is hospitalism new? An analysis of Medicare data from Washington State in 1994. Eff Clin Pract. 2000;3(1):35-39.
5. Welch WP, Stearns SC, Cuellar AE, Bindman AB. Use of hospitalists by Medicare beneficiaries: a national picture. Medicare Medicaid Res Rev. 2014;4(2). https://doi.org/10.5600/mmrr2014-004-02-b01.
6. Lapps J, Flansbaum B, Leykum L, Boswell J, Haines L. Updating threshold-based identification of hospitalists in 2012 medicare pay data. J Hosp Med. 2016;11(1):45-47. https://doi.org/10.1002/jhm.2480.
7. Centers for Medicare & Medicaid Services. Physician Compare Initiative. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/physician-compare-initiative/index.html. Accessed June 14, 2019.
8. Centers for Medicare & Medicaid Services. Revisions to Payment Policies under the Medicare Physician Fee Schedule, Quality Payment Program and Other Revisions to Part B for CY 2020 (CMS-1715-P). Accessed prior to publishing in the Federal Register through www.regulations.gov.
In recognizing the importance of Hospital Medicine (HM) and its practitioners, the Centers for Medicare and Medicaid Services (CMS) awarded the field a specialty designation in 2016. The code is self-selected by hospitalists and used by the CMS for programmatic and claims processing purposes. The HM code (“C6”), submitted to the CMS by the provider or their designee through the Provider Enrollment Chain and Ownership System (PECOS), in turn links to the National Provider Identification provider data.
The Society of Hospital Medicine® sought the designation given the growth of hospitalists practicing nationally, their impact on the practice of medicine in the inpatient setting,1 and their secondary effects on global care.2 In fact, early efforts by the CMS to transition physician payments to the value-based payment used specialty designations to create benchmarks in cost metrics, heightening the importance for hospitalists to be able to assess their performance. The need to identify any shifts in resource utilization and workforce mix in the broader context of health reforms necessitated action. Essentially, to understand the “why’s” of hospital medicine, the field required an accounting of the “who’s” and “where’s.”
The CMS granted the C6 designation in 2016, and it went live in April 2017. Despite the code’s brief two-year tenure, calls for its creation long predated its existence. As such, the new modifier requires an initial look to help steer the role of HM in any future CMS and managed care organization (MCO) quality, payment, or practice improvement activities.
METHODS
We analyzed publicly available 2017 Medicare Part B utilization data3 to explore the rates of Evaluation & Management (E&M) codes used across specialties, using the C6 designation to identify hospitalists.
To try to estimate the percentage of hospitalists who were likely billing under the C6 designation, we then compared the rates of C6 billing to expected rates of hospitalist E&M billing based on an analysis of hospitalist prevalence in the 2012 Medicare physician payment data. Prior work to identify hospitalists before the implementation of the C6 designation relied on thresholds of inpatient codes for various inpatient E&M services.4,5 We used our previously published approach of a threshold of 60% of inpatient E&M hospital services to differentiate hospitalists from their parent specialties.6 We also calculated the expected rates of E&M billing for other select specialty services by applying the 2012 E&M coding trends to the 2017 data.
RESULTS
Table 1 shows the distribution of inpatient E&M codes billed by hospitalists using the C6 identification, as well as the use of those codes by other specialists. Hospitalists identified by the C6 designation billed only 2%-5% of inpatient and 6% of observation codes. As an example, in 2017, discharge CPT codes 99238 and 99239 were used 7,872,323 times. However, C6-identified hospitalists accounted for only 441,420 of these codes.
Table 2 compares the observed billing rates by specialty using the C6 designation to identify hospitalists with what would be the expected rates with the 2012 threshold-based specialty billing designation applied to the 2017 data. This comparison demonstrates that hospitalist billing based on the C6 modifier use is approximately one-tenth of what would have been their expected volume of E&M services.
DISCUSSION
We examined the patterns of hospitalist billing using the C6 hospital medicine specialty modifier, comparing billing patterns with what we would expect hospitalist activity to be if we had used a threshold-based approach. The difference between the C6 and the threshold-based approaches to assessing hospitalist activity suggests that as few as 10% of hospitalists have adopted the C6 code.
Why is the adoption of the C6 modifier so low? Although administrative data do not allow us to identify the reasons why providers chose to disregard the C6 designation, we can speculate on causes. There are, to date, low direct risks and recognized benefits with using the code. We hypothesize that several factors could be impeding whether providers use the modifier to bring about potential gains. The first may be knowledge-related; ie, hospitalists might not be familiar with the specialty code or unaware of the importance of accurately capturing hospitalist practice patterns. They may also wrongly assume that their practices are aware of the revision or have submitted the appropriate paperwork. Similarly, practice personnel may lack knowledge regarding the code or the importance of its use. The second factor may be logistical; ie, administrative barriers such as difficulty accessing the Provider Enrollment, Chain and Ownership System (PECOS) and out-of-date paper registration forms impede fast uptake. The final reason might be related to professionals whose tenures as hospitalists will be brief, and their unease of carrying an identifier into their next non-HM position prompts hesitation. Providers may have a misperception that using the C6 code may somehow impact or limit their future scope of practice, when, in fact, they may change their Medicare specialty designation at any time.
Changes in reimbursement models, including the Bundled Payments for Care Improvement Advanced (BPCI-A) and other value-based initiatives, heighten the need for a more accurate identification of the specialty. Classifying individual providers and groups to make valid performance comparisons is relevant for the same reasons. The CMS continues to advance cost and efficiency measures in its publicly accessible physiciancompare.gov website.7 Without an improved ability to identify services provided by hospitalists—by both CMS and commercial entities—the potential benefits delivered by hospitalists in terms of improved care quality, safety, or efficiency could go undetected by payers and policymakers. Moreover, C6 may be used in other ways by the CMS throughout its payment systems and programmatic efforts that use specialty to differentiate between Medicare providers.8 Finally, the C6 is an identifier for the Medicare fee-for-service system; state programs and MCOs may not identify hospitalists in the same manner, or at all. Therefore, it may make it more difficult for those groups and HM researchers to study the trends in care delivery changes. The specialty needs to engage with these other payers to assist in revising their information systems to better account for how hospitalists care for their insured populations.
Although we would expect a natural increase in C6 adoption over time, optimally meeting stakeholders’ data needs requires more rapid uptake. Our analysis is limited by our assumption that specialty patterns of code use remain similar from 2012 to 2017. Regardless, the magnitude of the difference between the estimate of hospitalists using the C6 versus billing thresholds strongly suggests underuse of the C6 designation. The CMS and MCOs have an increasing need for valid and representative data, and C6 can be used to assess “HM-adjusted” resource utilization, relative value units (RVUs), and performance evaluations. Therefore, hospitalists may see more incentives to use the C6 specialty code in a manner consistent with other recognized subspecialties.
Disclaimer
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, and the Health Services Research and Development Service. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
In recognizing the importance of Hospital Medicine (HM) and its practitioners, the Centers for Medicare and Medicaid Services (CMS) awarded the field a specialty designation in 2016. The code is self-selected by hospitalists and used by the CMS for programmatic and claims processing purposes. The HM code (“C6”), submitted to the CMS by the provider or their designee through the Provider Enrollment Chain and Ownership System (PECOS), in turn links to the National Provider Identification provider data.
The Society of Hospital Medicine® sought the designation given the growth of hospitalists practicing nationally, their impact on the practice of medicine in the inpatient setting,1 and their secondary effects on global care.2 In fact, early efforts by the CMS to transition physician payments to the value-based payment used specialty designations to create benchmarks in cost metrics, heightening the importance for hospitalists to be able to assess their performance. The need to identify any shifts in resource utilization and workforce mix in the broader context of health reforms necessitated action. Essentially, to understand the “why’s” of hospital medicine, the field required an accounting of the “who’s” and “where’s.”
The CMS granted the C6 designation in 2016, and it went live in April 2017. Despite the code’s brief two-year tenure, calls for its creation long predated its existence. As such, the new modifier requires an initial look to help steer the role of HM in any future CMS and managed care organization (MCO) quality, payment, or practice improvement activities.
METHODS
We analyzed publicly available 2017 Medicare Part B utilization data3 to explore the rates of Evaluation & Management (E&M) codes used across specialties, using the C6 designation to identify hospitalists.
To try to estimate the percentage of hospitalists who were likely billing under the C6 designation, we then compared the rates of C6 billing to expected rates of hospitalist E&M billing based on an analysis of hospitalist prevalence in the 2012 Medicare physician payment data. Prior work to identify hospitalists before the implementation of the C6 designation relied on thresholds of inpatient codes for various inpatient E&M services.4,5 We used our previously published approach of a threshold of 60% of inpatient E&M hospital services to differentiate hospitalists from their parent specialties.6 We also calculated the expected rates of E&M billing for other select specialty services by applying the 2012 E&M coding trends to the 2017 data.
RESULTS
Table 1 shows the distribution of inpatient E&M codes billed by hospitalists using the C6 identification, as well as the use of those codes by other specialists. Hospitalists identified by the C6 designation billed only 2%-5% of inpatient and 6% of observation codes. As an example, in 2017, discharge CPT codes 99238 and 99239 were used 7,872,323 times. However, C6-identified hospitalists accounted for only 441,420 of these codes.
Table 2 compares the observed billing rates by specialty using the C6 designation to identify hospitalists with what would be the expected rates with the 2012 threshold-based specialty billing designation applied to the 2017 data. This comparison demonstrates that hospitalist billing based on the C6 modifier use is approximately one-tenth of what would have been their expected volume of E&M services.
DISCUSSION
We examined the patterns of hospitalist billing using the C6 hospital medicine specialty modifier, comparing billing patterns with what we would expect hospitalist activity to be if we had used a threshold-based approach. The difference between the C6 and the threshold-based approaches to assessing hospitalist activity suggests that as few as 10% of hospitalists have adopted the C6 code.
Why is the adoption of the C6 modifier so low? Although administrative data do not allow us to identify the reasons why providers chose to disregard the C6 designation, we can speculate on causes. There are, to date, low direct risks and recognized benefits with using the code. We hypothesize that several factors could be impeding whether providers use the modifier to bring about potential gains. The first may be knowledge-related; ie, hospitalists might not be familiar with the specialty code or unaware of the importance of accurately capturing hospitalist practice patterns. They may also wrongly assume that their practices are aware of the revision or have submitted the appropriate paperwork. Similarly, practice personnel may lack knowledge regarding the code or the importance of its use. The second factor may be logistical; ie, administrative barriers such as difficulty accessing the Provider Enrollment, Chain and Ownership System (PECOS) and out-of-date paper registration forms impede fast uptake. The final reason might be related to professionals whose tenures as hospitalists will be brief, and their unease of carrying an identifier into their next non-HM position prompts hesitation. Providers may have a misperception that using the C6 code may somehow impact or limit their future scope of practice, when, in fact, they may change their Medicare specialty designation at any time.
Changes in reimbursement models, including the Bundled Payments for Care Improvement Advanced (BPCI-A) and other value-based initiatives, heighten the need for a more accurate identification of the specialty. Classifying individual providers and groups to make valid performance comparisons is relevant for the same reasons. The CMS continues to advance cost and efficiency measures in its publicly accessible physiciancompare.gov website.7 Without an improved ability to identify services provided by hospitalists—by both CMS and commercial entities—the potential benefits delivered by hospitalists in terms of improved care quality, safety, or efficiency could go undetected by payers and policymakers. Moreover, C6 may be used in other ways by the CMS throughout its payment systems and programmatic efforts that use specialty to differentiate between Medicare providers.8 Finally, the C6 is an identifier for the Medicare fee-for-service system; state programs and MCOs may not identify hospitalists in the same manner, or at all. Therefore, it may make it more difficult for those groups and HM researchers to study the trends in care delivery changes. The specialty needs to engage with these other payers to assist in revising their information systems to better account for how hospitalists care for their insured populations.
Although we would expect a natural increase in C6 adoption over time, optimally meeting stakeholders’ data needs requires more rapid uptake. Our analysis is limited by our assumption that specialty patterns of code use remain similar from 2012 to 2017. Regardless, the magnitude of the difference between the estimate of hospitalists using the C6 versus billing thresholds strongly suggests underuse of the C6 designation. The CMS and MCOs have an increasing need for valid and representative data, and C6 can be used to assess “HM-adjusted” resource utilization, relative value units (RVUs), and performance evaluations. Therefore, hospitalists may see more incentives to use the C6 specialty code in a manner consistent with other recognized subspecialties.
Disclaimer
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, and the Health Services Research and Development Service. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
1. Wachter RM, Goldman L. Zero to 50,000—The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
2. Quinn R. HM 2016: A year in review. The Hospitalist. 2016;12. https://www.the-hospitalist.org/hospitalist/article/121419/everything-you-need-know-about-bundled-payments-care-improvement
3. Centers for Medicare and Medicaid Services. Medicare Utilization for Part B. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicarefeeforsvcpartsab/medicareutilizationforpartb.html. Accessed June 14, 2019.
4. Saint S, Christakis DA, Baldwin L-M, Rosenblatt R. Is hospitalism new? An analysis of Medicare data from Washington State in 1994. Eff Clin Pract. 2000;3(1):35-39.
5. Welch WP, Stearns SC, Cuellar AE, Bindman AB. Use of hospitalists by Medicare beneficiaries: a national picture. Medicare Medicaid Res Rev. 2014;4(2). https://doi.org/10.5600/mmrr2014-004-02-b01.
6. Lapps J, Flansbaum B, Leykum L, Boswell J, Haines L. Updating threshold-based identification of hospitalists in 2012 medicare pay data. J Hosp Med. 2016;11(1):45-47. https://doi.org/10.1002/jhm.2480.
7. Centers for Medicare & Medicaid Services. Physician Compare Initiative. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/physician-compare-initiative/index.html. Accessed June 14, 2019.
8. Centers for Medicare & Medicaid Services. Revisions to Payment Policies under the Medicare Physician Fee Schedule, Quality Payment Program and Other Revisions to Part B for CY 2020 (CMS-1715-P). Accessed prior to publishing in the Federal Register through www.regulations.gov.
1. Wachter RM, Goldman L. Zero to 50,000—The 20th Anniversary of the Hospitalist. N Engl J Med. 2016;375(11):1009-1011. https://doi.org/10.1056/NEJMp1607958.
2. Quinn R. HM 2016: A year in review. The Hospitalist. 2016;12. https://www.the-hospitalist.org/hospitalist/article/121419/everything-you-need-know-about-bundled-payments-care-improvement
3. Centers for Medicare and Medicaid Services. Medicare Utilization for Part B. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicarefeeforsvcpartsab/medicareutilizationforpartb.html. Accessed June 14, 2019.
4. Saint S, Christakis DA, Baldwin L-M, Rosenblatt R. Is hospitalism new? An analysis of Medicare data from Washington State in 1994. Eff Clin Pract. 2000;3(1):35-39.
5. Welch WP, Stearns SC, Cuellar AE, Bindman AB. Use of hospitalists by Medicare beneficiaries: a national picture. Medicare Medicaid Res Rev. 2014;4(2). https://doi.org/10.5600/mmrr2014-004-02-b01.
6. Lapps J, Flansbaum B, Leykum L, Boswell J, Haines L. Updating threshold-based identification of hospitalists in 2012 medicare pay data. J Hosp Med. 2016;11(1):45-47. https://doi.org/10.1002/jhm.2480.
7. Centers for Medicare & Medicaid Services. Physician Compare Initiative. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/physician-compare-initiative/index.html. Accessed June 14, 2019.
8. Centers for Medicare & Medicaid Services. Revisions to Payment Policies under the Medicare Physician Fee Schedule, Quality Payment Program and Other Revisions to Part B for CY 2020 (CMS-1715-P). Accessed prior to publishing in the Federal Register through www.regulations.gov.
© 2019 Society of Hospital Medicine
The Critical Role of Hospitalists for Successful Hospital-SNF Integration Hospitalists and Hospital/SNF Integration
In 2015, the Centers for Medicare and Medicaid Services (CMS) tied 42% of Medicare payments to a value-based model of care.1 Many of these models are designed to expand the scope of hospitals’ accountability to include care provided to patients postdischarge (eg, readmission penalties, bundled payments, accountable care organizations). With such a significant change in organizational incentives, one would expect to see activity as it relates to hospital-skilled nursing facility (SNF) integration, potentially including shared risk among providers.2,3
Hospitals can choose from several different strategies when contemplating SNF integration, such as vertical integration with SNFs, which would involve acquiring and owning SNFs. However, despite the high level of incentive alignment and financial integration achieved through SNF acquisition, this strategy has not been widely adopted. Perhaps this is because hospitals can often attain a shorter length of stay and lower readmission rates without taking on the additional risk of owning a facility, except under particular market conditions.4 Hospitals can alternatively pursue virtual integration by developing preferred provider networks through contractual relationships or other formal processes, attempting to direct patients to SNF providers that have met predefined criteria, as described by Conway and colleagues in this issue of the Journal of Hospital Medicine®.5 While hospitals have adopted this form of integration more widely than vertical integration, only those with additional financial motivations, such as those employing bundled payments, engaged in accountable care organizations (ACOs) or forward-thinking organizations preparing for looming global models of payment, have implemented such action. Finally, hospitals can focus on relational coordination through informal person-to-person communication and transition management. Given the high number of patients discharged to SNFs, the strategies above are not mutually exclusive, and enhanced relational coordination is most likely going to occur regardless of the type of—and perhaps even without—organizational-level integration.
For those hospitals choosing not to pursue integration with SNFs, there are several reasons to maintain the status quo. First, hospitals have different interpretations of provider choice (“beneficiary freedom to choose”), whereby many do not believe they can provide information to patients outside of facility names and addresses. As such, they will refrain from developing a SNF network due to their interpretation of hazy federal rules.6 Second, it is possible that the incremental benefit of establishing a network is viewed by many hospitals as not worth the cost, measured by the time and effort required and the potential risk of not adhering to choice requirements. This could be especially true for hospitals without additional financial motivations, such as participation in an ACO or bundled payment program.
As the landscape continues to evolve, more successful systems will embrace a more concordant partnership with local and regional SNF providers, and several market factors will support the trend. First, the Medicare Payment Advisory Commission (MedPAC) is discussing the idea of choice in the context of postacute discharge, potentially leading to hospitals relaxing their strict interpretations of choice and the level of information provided to patients.7 Second, the evidence supports better patient outcomes when hospitals develop SNF networks.8,9 Finally, continued penetration of value-based payment models combined with CMS decisions regarding choice will continue to provide the additional motivation hospitals may need to change the cost-benefit calculation in favor of developing a network.
IMPLICATIONS FOR HOSPITALISTS
Traditionally, primary care physicians followed their patients through the acute- and postacute care continuum, but a variety of changes led to the growth of hospital medicine as fewer primary care physicians saw patients in the hospital.10,11 This shift has challenged efforts to ensure continuity of care across settings, especially since most hospitalists have ceded control of postdischarge placement to case managers and therapists. Further, there has been little incentive to connect hospitalists to any other component or provider along the range of care, and compensation models rarely, if at all, consider any accountability for patient outcomes outside the hospital. Several factors can change this reality for hospitalists.
First, as more providers adopt team-based care approaches and as alternative payment models expand the scope of accountability, hospitalists will become an even more central component of the risk evaluation process for hospitalized patients as it relates to their discharge profile. This could mean that hospitalists are more involved in the postdischarge follow-up of patients sent home, to make sure patients adhere to discharge instructions. Alternatively, hospitalists may need to increase the level of physician-to-physician communication with SNF medical directors for patients discharged to SNF. This, in turn, could result in an increasing number of hospitalist groups recruiting SNFists to join their group or potentially assigning existing hospitalists or physician assistants to round on patients in the SNF. The 2018 Society of Hospital Medicine report showed an increase in activity among hospital medicine groups performing services in postacute-care facilities outside the hospital from 13% in 2016 to 25% in 2018.12 Similarly, a 2017 study in JAMA Internal Medicine reported a 48.2% increase in the number of physicians classified as SNFists from 2007 to 2014.13
Second, hospitalists will be more involved in the discharge planning process through internal interdisciplinary team communications. Whereas case managers and therapists owned the discharge planning process historically, new teams will include hospitalists, case managers, physical therapists, and pharmacists. System leaders will task them with identifying the appropriate discharge destination (eg, SNF, home health), finalizing the medication reconciliation, scheduling follow-up appointments, and completing a warm handoff.
Finally, as the field matures and hospitalists learn more about postacute-care connections, they will continue to be held more accountable for patient outcomes postdischarge. Many hospitalists have already connected to community providers through checklists and use evidence-based discharge programs like ProjectRed or Project BOOST.14,15 Organizations will need a similar strategy for SNFs, developing process measures, with the input of hospitalists, around those noteworthy areas that hospitalists can control. This will require greater alignment among constituents around overall organizational goals and, more importantly, entail the hospitalist to be attuned to overall patient goals beyond the care provided in the hospital setting.
As payment and care models continue to evolve, the status quo cannot be sustained. We anticipate that hospitalists will become more integrated into the patient discharge process, especially as it relates to discharge to SNFs before patients reconnect to their community physicians. Hospital systems will accelerate integration through the development of preferred SNF networks, and hospitalists stand to play a critical role in the success of these arrangements by enriching the benefits they create through these outward relationships.
For organizations engaged in embedded networks, they can realize gains via incentive alignment, trust, information transfer, mutual support, and coordination through virtual integration, without requiring vertical ownership.3,16Thus, the opportunity exists for hospitalists to be critical drivers of network success, serving as intermediaries from which information, collaboration, and shared problem-solving flow between hospitals, SNFs, patients, and the entire care team. Opportunities to rebuild our system are long past; however, like all changing sectors in healthcare, the disaggregate acute and postacute settings must move in lockstep. Hospitals and postacute care facilities must find ways to alter their thinking to eradicate the obstructive and injurious invisible wall.
Disclosures
The authors have nothing to disclose.
1. Catalyst for Payment Reform. CPR Scorecard on Medicare Payment Reform 2015.
2. Mick S, Shay P. Accountable care organizations and transaction cost economics. Med Care Res Rev. 2016;73(6):649-659. doi: 10.1177/1077558716640411. PubMed
3. Shay P, Mick S. Post-acute care and vertical integration after the Patient Protection and Affordable Care Act. J Healthc Manag. 2013;58(1):15-27. PubMed
4. McHugh J, Zinn J, Shield R, et al. Strategy and risk-sharing in hospital-postacute care integration. Health Care Manage Rev. 2018. doi: 10.1097/HMR.0000000000000204. PubMed
5. Conway S, Parekh A, Hughes A, et al. Post-acute care transitions: developing a skilled nursing facility collaborative within an academic health system. J Hosp Med. 2019;14(3):174-177. doi: 10.12788/jhm.3117. PubMed
6. Tyler D, Gadbois E, McHugh J, Shield R, Winblad U, Mor V. Patients are not given quality-of-care data about skilled nursing facilities when discharged from hospitals. Health Aff. 2017;36(8):1385-1391. doi: 10.1377/hlthaff.2017.0155. PubMed
7. Medicare Payment Advisory Commission. Encouraging Medicare Beneficiaries to Use Higher Quality Post-Acute Care Providers. Washington, DC: MedPAC; 2018.
8. McHugh J, Foster A, Mor V, et al. Reducing hospital readmissions through preferred networks of skilled nursing facilities. Health Aff. 2017;36(9):1591-1598. doi: 10.1377/hlthaff.2017.0211. PubMed
9. Rahman M, Foster A, Grabowski D, Zinn J, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013;48(6):1898-1919. doi: 10.1111/1475-6773.12112. PubMed
10. Wachter R, Goldman L. Zero to 50,000 - The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. doi: 10.1056/NEJMp1607958. PubMed
11. Kripalani S, Jackson A, Schnipper J, Coleman E. Promoting effective transitions of care at hopsital discharge: A review of key issues for hospitalists. J Hosp Med. 2007;2(5):314-323. doi: 10.1002/jhm.228. PubMed
12. Society of Hospital Medicine. 2018 State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine; 2018. 2018 SHM Report.
13. Teno J, Gozalo P, Trivedi A, Mitchell S, Bunker J, Mor V. Temporal trends in the numbers of skilled nursing facility specialists from 2007 through 2014. JAMA Intern Med. 2017;177(9):1376-1378. doi: 10.1001/jamainternmed.2017.2136. PubMed
14. Boston University Medical Center. Project RED Re-Engineered Discharge. Project RED. Available at: https://www.bu.edu/fammed/projectred/. Accessed Dec 9, 2018.
15. Hansen L, Greenwald J, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8:421-427. doi: 10.1002/jhm.2054. PubMed
16. Uzzi B. The sources and consequences of embeddedness for the economic performance of organizations: the network effect. Am Sociol Rev. 1996:674-698. doi: 10.2307/2096399.
In 2015, the Centers for Medicare and Medicaid Services (CMS) tied 42% of Medicare payments to a value-based model of care.1 Many of these models are designed to expand the scope of hospitals’ accountability to include care provided to patients postdischarge (eg, readmission penalties, bundled payments, accountable care organizations). With such a significant change in organizational incentives, one would expect to see activity as it relates to hospital-skilled nursing facility (SNF) integration, potentially including shared risk among providers.2,3
Hospitals can choose from several different strategies when contemplating SNF integration, such as vertical integration with SNFs, which would involve acquiring and owning SNFs. However, despite the high level of incentive alignment and financial integration achieved through SNF acquisition, this strategy has not been widely adopted. Perhaps this is because hospitals can often attain a shorter length of stay and lower readmission rates without taking on the additional risk of owning a facility, except under particular market conditions.4 Hospitals can alternatively pursue virtual integration by developing preferred provider networks through contractual relationships or other formal processes, attempting to direct patients to SNF providers that have met predefined criteria, as described by Conway and colleagues in this issue of the Journal of Hospital Medicine®.5 While hospitals have adopted this form of integration more widely than vertical integration, only those with additional financial motivations, such as those employing bundled payments, engaged in accountable care organizations (ACOs) or forward-thinking organizations preparing for looming global models of payment, have implemented such action. Finally, hospitals can focus on relational coordination through informal person-to-person communication and transition management. Given the high number of patients discharged to SNFs, the strategies above are not mutually exclusive, and enhanced relational coordination is most likely going to occur regardless of the type of—and perhaps even without—organizational-level integration.
For those hospitals choosing not to pursue integration with SNFs, there are several reasons to maintain the status quo. First, hospitals have different interpretations of provider choice (“beneficiary freedom to choose”), whereby many do not believe they can provide information to patients outside of facility names and addresses. As such, they will refrain from developing a SNF network due to their interpretation of hazy federal rules.6 Second, it is possible that the incremental benefit of establishing a network is viewed by many hospitals as not worth the cost, measured by the time and effort required and the potential risk of not adhering to choice requirements. This could be especially true for hospitals without additional financial motivations, such as participation in an ACO or bundled payment program.
As the landscape continues to evolve, more successful systems will embrace a more concordant partnership with local and regional SNF providers, and several market factors will support the trend. First, the Medicare Payment Advisory Commission (MedPAC) is discussing the idea of choice in the context of postacute discharge, potentially leading to hospitals relaxing their strict interpretations of choice and the level of information provided to patients.7 Second, the evidence supports better patient outcomes when hospitals develop SNF networks.8,9 Finally, continued penetration of value-based payment models combined with CMS decisions regarding choice will continue to provide the additional motivation hospitals may need to change the cost-benefit calculation in favor of developing a network.
IMPLICATIONS FOR HOSPITALISTS
Traditionally, primary care physicians followed their patients through the acute- and postacute care continuum, but a variety of changes led to the growth of hospital medicine as fewer primary care physicians saw patients in the hospital.10,11 This shift has challenged efforts to ensure continuity of care across settings, especially since most hospitalists have ceded control of postdischarge placement to case managers and therapists. Further, there has been little incentive to connect hospitalists to any other component or provider along the range of care, and compensation models rarely, if at all, consider any accountability for patient outcomes outside the hospital. Several factors can change this reality for hospitalists.
First, as more providers adopt team-based care approaches and as alternative payment models expand the scope of accountability, hospitalists will become an even more central component of the risk evaluation process for hospitalized patients as it relates to their discharge profile. This could mean that hospitalists are more involved in the postdischarge follow-up of patients sent home, to make sure patients adhere to discharge instructions. Alternatively, hospitalists may need to increase the level of physician-to-physician communication with SNF medical directors for patients discharged to SNF. This, in turn, could result in an increasing number of hospitalist groups recruiting SNFists to join their group or potentially assigning existing hospitalists or physician assistants to round on patients in the SNF. The 2018 Society of Hospital Medicine report showed an increase in activity among hospital medicine groups performing services in postacute-care facilities outside the hospital from 13% in 2016 to 25% in 2018.12 Similarly, a 2017 study in JAMA Internal Medicine reported a 48.2% increase in the number of physicians classified as SNFists from 2007 to 2014.13
Second, hospitalists will be more involved in the discharge planning process through internal interdisciplinary team communications. Whereas case managers and therapists owned the discharge planning process historically, new teams will include hospitalists, case managers, physical therapists, and pharmacists. System leaders will task them with identifying the appropriate discharge destination (eg, SNF, home health), finalizing the medication reconciliation, scheduling follow-up appointments, and completing a warm handoff.
Finally, as the field matures and hospitalists learn more about postacute-care connections, they will continue to be held more accountable for patient outcomes postdischarge. Many hospitalists have already connected to community providers through checklists and use evidence-based discharge programs like ProjectRed or Project BOOST.14,15 Organizations will need a similar strategy for SNFs, developing process measures, with the input of hospitalists, around those noteworthy areas that hospitalists can control. This will require greater alignment among constituents around overall organizational goals and, more importantly, entail the hospitalist to be attuned to overall patient goals beyond the care provided in the hospital setting.
As payment and care models continue to evolve, the status quo cannot be sustained. We anticipate that hospitalists will become more integrated into the patient discharge process, especially as it relates to discharge to SNFs before patients reconnect to their community physicians. Hospital systems will accelerate integration through the development of preferred SNF networks, and hospitalists stand to play a critical role in the success of these arrangements by enriching the benefits they create through these outward relationships.
For organizations engaged in embedded networks, they can realize gains via incentive alignment, trust, information transfer, mutual support, and coordination through virtual integration, without requiring vertical ownership.3,16Thus, the opportunity exists for hospitalists to be critical drivers of network success, serving as intermediaries from which information, collaboration, and shared problem-solving flow between hospitals, SNFs, patients, and the entire care team. Opportunities to rebuild our system are long past; however, like all changing sectors in healthcare, the disaggregate acute and postacute settings must move in lockstep. Hospitals and postacute care facilities must find ways to alter their thinking to eradicate the obstructive and injurious invisible wall.
Disclosures
The authors have nothing to disclose.
In 2015, the Centers for Medicare and Medicaid Services (CMS) tied 42% of Medicare payments to a value-based model of care.1 Many of these models are designed to expand the scope of hospitals’ accountability to include care provided to patients postdischarge (eg, readmission penalties, bundled payments, accountable care organizations). With such a significant change in organizational incentives, one would expect to see activity as it relates to hospital-skilled nursing facility (SNF) integration, potentially including shared risk among providers.2,3
Hospitals can choose from several different strategies when contemplating SNF integration, such as vertical integration with SNFs, which would involve acquiring and owning SNFs. However, despite the high level of incentive alignment and financial integration achieved through SNF acquisition, this strategy has not been widely adopted. Perhaps this is because hospitals can often attain a shorter length of stay and lower readmission rates without taking on the additional risk of owning a facility, except under particular market conditions.4 Hospitals can alternatively pursue virtual integration by developing preferred provider networks through contractual relationships or other formal processes, attempting to direct patients to SNF providers that have met predefined criteria, as described by Conway and colleagues in this issue of the Journal of Hospital Medicine®.5 While hospitals have adopted this form of integration more widely than vertical integration, only those with additional financial motivations, such as those employing bundled payments, engaged in accountable care organizations (ACOs) or forward-thinking organizations preparing for looming global models of payment, have implemented such action. Finally, hospitals can focus on relational coordination through informal person-to-person communication and transition management. Given the high number of patients discharged to SNFs, the strategies above are not mutually exclusive, and enhanced relational coordination is most likely going to occur regardless of the type of—and perhaps even without—organizational-level integration.
For those hospitals choosing not to pursue integration with SNFs, there are several reasons to maintain the status quo. First, hospitals have different interpretations of provider choice (“beneficiary freedom to choose”), whereby many do not believe they can provide information to patients outside of facility names and addresses. As such, they will refrain from developing a SNF network due to their interpretation of hazy federal rules.6 Second, it is possible that the incremental benefit of establishing a network is viewed by many hospitals as not worth the cost, measured by the time and effort required and the potential risk of not adhering to choice requirements. This could be especially true for hospitals without additional financial motivations, such as participation in an ACO or bundled payment program.
As the landscape continues to evolve, more successful systems will embrace a more concordant partnership with local and regional SNF providers, and several market factors will support the trend. First, the Medicare Payment Advisory Commission (MedPAC) is discussing the idea of choice in the context of postacute discharge, potentially leading to hospitals relaxing their strict interpretations of choice and the level of information provided to patients.7 Second, the evidence supports better patient outcomes when hospitals develop SNF networks.8,9 Finally, continued penetration of value-based payment models combined with CMS decisions regarding choice will continue to provide the additional motivation hospitals may need to change the cost-benefit calculation in favor of developing a network.
IMPLICATIONS FOR HOSPITALISTS
Traditionally, primary care physicians followed their patients through the acute- and postacute care continuum, but a variety of changes led to the growth of hospital medicine as fewer primary care physicians saw patients in the hospital.10,11 This shift has challenged efforts to ensure continuity of care across settings, especially since most hospitalists have ceded control of postdischarge placement to case managers and therapists. Further, there has been little incentive to connect hospitalists to any other component or provider along the range of care, and compensation models rarely, if at all, consider any accountability for patient outcomes outside the hospital. Several factors can change this reality for hospitalists.
First, as more providers adopt team-based care approaches and as alternative payment models expand the scope of accountability, hospitalists will become an even more central component of the risk evaluation process for hospitalized patients as it relates to their discharge profile. This could mean that hospitalists are more involved in the postdischarge follow-up of patients sent home, to make sure patients adhere to discharge instructions. Alternatively, hospitalists may need to increase the level of physician-to-physician communication with SNF medical directors for patients discharged to SNF. This, in turn, could result in an increasing number of hospitalist groups recruiting SNFists to join their group or potentially assigning existing hospitalists or physician assistants to round on patients in the SNF. The 2018 Society of Hospital Medicine report showed an increase in activity among hospital medicine groups performing services in postacute-care facilities outside the hospital from 13% in 2016 to 25% in 2018.12 Similarly, a 2017 study in JAMA Internal Medicine reported a 48.2% increase in the number of physicians classified as SNFists from 2007 to 2014.13
Second, hospitalists will be more involved in the discharge planning process through internal interdisciplinary team communications. Whereas case managers and therapists owned the discharge planning process historically, new teams will include hospitalists, case managers, physical therapists, and pharmacists. System leaders will task them with identifying the appropriate discharge destination (eg, SNF, home health), finalizing the medication reconciliation, scheduling follow-up appointments, and completing a warm handoff.
Finally, as the field matures and hospitalists learn more about postacute-care connections, they will continue to be held more accountable for patient outcomes postdischarge. Many hospitalists have already connected to community providers through checklists and use evidence-based discharge programs like ProjectRed or Project BOOST.14,15 Organizations will need a similar strategy for SNFs, developing process measures, with the input of hospitalists, around those noteworthy areas that hospitalists can control. This will require greater alignment among constituents around overall organizational goals and, more importantly, entail the hospitalist to be attuned to overall patient goals beyond the care provided in the hospital setting.
As payment and care models continue to evolve, the status quo cannot be sustained. We anticipate that hospitalists will become more integrated into the patient discharge process, especially as it relates to discharge to SNFs before patients reconnect to their community physicians. Hospital systems will accelerate integration through the development of preferred SNF networks, and hospitalists stand to play a critical role in the success of these arrangements by enriching the benefits they create through these outward relationships.
For organizations engaged in embedded networks, they can realize gains via incentive alignment, trust, information transfer, mutual support, and coordination through virtual integration, without requiring vertical ownership.3,16Thus, the opportunity exists for hospitalists to be critical drivers of network success, serving as intermediaries from which information, collaboration, and shared problem-solving flow between hospitals, SNFs, patients, and the entire care team. Opportunities to rebuild our system are long past; however, like all changing sectors in healthcare, the disaggregate acute and postacute settings must move in lockstep. Hospitals and postacute care facilities must find ways to alter their thinking to eradicate the obstructive and injurious invisible wall.
Disclosures
The authors have nothing to disclose.
1. Catalyst for Payment Reform. CPR Scorecard on Medicare Payment Reform 2015.
2. Mick S, Shay P. Accountable care organizations and transaction cost economics. Med Care Res Rev. 2016;73(6):649-659. doi: 10.1177/1077558716640411. PubMed
3. Shay P, Mick S. Post-acute care and vertical integration after the Patient Protection and Affordable Care Act. J Healthc Manag. 2013;58(1):15-27. PubMed
4. McHugh J, Zinn J, Shield R, et al. Strategy and risk-sharing in hospital-postacute care integration. Health Care Manage Rev. 2018. doi: 10.1097/HMR.0000000000000204. PubMed
5. Conway S, Parekh A, Hughes A, et al. Post-acute care transitions: developing a skilled nursing facility collaborative within an academic health system. J Hosp Med. 2019;14(3):174-177. doi: 10.12788/jhm.3117. PubMed
6. Tyler D, Gadbois E, McHugh J, Shield R, Winblad U, Mor V. Patients are not given quality-of-care data about skilled nursing facilities when discharged from hospitals. Health Aff. 2017;36(8):1385-1391. doi: 10.1377/hlthaff.2017.0155. PubMed
7. Medicare Payment Advisory Commission. Encouraging Medicare Beneficiaries to Use Higher Quality Post-Acute Care Providers. Washington, DC: MedPAC; 2018.
8. McHugh J, Foster A, Mor V, et al. Reducing hospital readmissions through preferred networks of skilled nursing facilities. Health Aff. 2017;36(9):1591-1598. doi: 10.1377/hlthaff.2017.0211. PubMed
9. Rahman M, Foster A, Grabowski D, Zinn J, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013;48(6):1898-1919. doi: 10.1111/1475-6773.12112. PubMed
10. Wachter R, Goldman L. Zero to 50,000 - The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. doi: 10.1056/NEJMp1607958. PubMed
11. Kripalani S, Jackson A, Schnipper J, Coleman E. Promoting effective transitions of care at hopsital discharge: A review of key issues for hospitalists. J Hosp Med. 2007;2(5):314-323. doi: 10.1002/jhm.228. PubMed
12. Society of Hospital Medicine. 2018 State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine; 2018. 2018 SHM Report.
13. Teno J, Gozalo P, Trivedi A, Mitchell S, Bunker J, Mor V. Temporal trends in the numbers of skilled nursing facility specialists from 2007 through 2014. JAMA Intern Med. 2017;177(9):1376-1378. doi: 10.1001/jamainternmed.2017.2136. PubMed
14. Boston University Medical Center. Project RED Re-Engineered Discharge. Project RED. Available at: https://www.bu.edu/fammed/projectred/. Accessed Dec 9, 2018.
15. Hansen L, Greenwald J, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8:421-427. doi: 10.1002/jhm.2054. PubMed
16. Uzzi B. The sources and consequences of embeddedness for the economic performance of organizations: the network effect. Am Sociol Rev. 1996:674-698. doi: 10.2307/2096399.
1. Catalyst for Payment Reform. CPR Scorecard on Medicare Payment Reform 2015.
2. Mick S, Shay P. Accountable care organizations and transaction cost economics. Med Care Res Rev. 2016;73(6):649-659. doi: 10.1177/1077558716640411. PubMed
3. Shay P, Mick S. Post-acute care and vertical integration after the Patient Protection and Affordable Care Act. J Healthc Manag. 2013;58(1):15-27. PubMed
4. McHugh J, Zinn J, Shield R, et al. Strategy and risk-sharing in hospital-postacute care integration. Health Care Manage Rev. 2018. doi: 10.1097/HMR.0000000000000204. PubMed
5. Conway S, Parekh A, Hughes A, et al. Post-acute care transitions: developing a skilled nursing facility collaborative within an academic health system. J Hosp Med. 2019;14(3):174-177. doi: 10.12788/jhm.3117. PubMed
6. Tyler D, Gadbois E, McHugh J, Shield R, Winblad U, Mor V. Patients are not given quality-of-care data about skilled nursing facilities when discharged from hospitals. Health Aff. 2017;36(8):1385-1391. doi: 10.1377/hlthaff.2017.0155. PubMed
7. Medicare Payment Advisory Commission. Encouraging Medicare Beneficiaries to Use Higher Quality Post-Acute Care Providers. Washington, DC: MedPAC; 2018.
8. McHugh J, Foster A, Mor V, et al. Reducing hospital readmissions through preferred networks of skilled nursing facilities. Health Aff. 2017;36(9):1591-1598. doi: 10.1377/hlthaff.2017.0211. PubMed
9. Rahman M, Foster A, Grabowski D, Zinn J, Mor V. Effect of hospital-SNF referral linkages on rehospitalization. Health Serv Res. 2013;48(6):1898-1919. doi: 10.1111/1475-6773.12112. PubMed
10. Wachter R, Goldman L. Zero to 50,000 - The 20th anniversary of the hospitalist. N Engl J Med. 2016;375(11):1009-1011. doi: 10.1056/NEJMp1607958. PubMed
11. Kripalani S, Jackson A, Schnipper J, Coleman E. Promoting effective transitions of care at hopsital discharge: A review of key issues for hospitalists. J Hosp Med. 2007;2(5):314-323. doi: 10.1002/jhm.228. PubMed
12. Society of Hospital Medicine. 2018 State of Hospital Medicine Report. Philadelphia: Society of Hospital Medicine; 2018. 2018 SHM Report.
13. Teno J, Gozalo P, Trivedi A, Mitchell S, Bunker J, Mor V. Temporal trends in the numbers of skilled nursing facility specialists from 2007 through 2014. JAMA Intern Med. 2017;177(9):1376-1378. doi: 10.1001/jamainternmed.2017.2136. PubMed
14. Boston University Medical Center. Project RED Re-Engineered Discharge. Project RED. Available at: https://www.bu.edu/fammed/projectred/. Accessed Dec 9, 2018.
15. Hansen L, Greenwald J, Budnitz T, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8:421-427. doi: 10.1002/jhm.2054. PubMed
16. Uzzi B. The sources and consequences of embeddedness for the economic performance of organizations: the network effect. Am Sociol Rev. 1996:674-698. doi: 10.2307/2096399.
© 2019 Society of Hospital Medicine
Sneak Peek: The Hospital Leader blog – Oct. 2017
You Have Lowered Length of Stay. Congratulations: You’re Fired.
For several decades, providers working within hospitals have had incentives to reduce stay durations and keep patient flow tip-top. Diagnosis Related Group (DRG)–based and capitated payments expedited that shift.
Accompanying the change, physicians became more aware of the potential repercussions of sicker and quicker discharges. They began to monitor their care and, as best as possible, use what measures they could as a proxy for quality (readmissions and hospital-acquired conditions). Providers balanced the harms of a continued stay with the benefits of added days, not to mention the need for cost savings.
I recognize this because of the cognitive dissonance providers now experience because of the mixed messages delivered by hospital leaders.
On the one hand, the DRG-driven system that we have binds the hospital’s bottom line – and that is not going away. On the other, we are paying more attention to excessive costs in post-acute settings, that is, subacute facilities when home health will do or more intense acute rehabilitation rather than the subacute route.
Making determinations as to whether a certain course is proper, whether a patient will be safe, whether families can provide adequate agency and backing, and whether we can avail community services takes time. Sicker and quicker; mindful of short-term outcomes; worked when we had postdischarge blinders on. As we remove such obstacles, and payment incentives change to cover broader intervals of time, we have to adapt. And that means leadership must realize that the practices that held hospitals in sound financial stead in years past are heading toward extinction – or, at best, falling out of favor.
Compare the costs of routine hospital care with the added expense of post-acute care, then multiply that extra expense times an aging, dependent population, and you add billions of dollars to the recovery tab. Some of these expenses are necessary, and some are not; a stay at a skilled nursing facility, for example, doubles the cost of an episode.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
- Why 7 On/7 Off Doesn’t Meet the Needs of Long-Stay Hospital Patients by Lauren Doctoroff, MD, FHM
- Is It Time for Health Policy M&Ms? by Chris Moriates, MD
- George Carlin Predicts Hospital Planning Strategy by Jordan Messler, MD, SFHM
- Many Paths to a Richer Job by Leslie Flores, MHA, MPH, SFHM
- A New Face for Online Modules by Chris Moriates, MD
You Have Lowered Length of Stay. Congratulations: You’re Fired.
For several decades, providers working within hospitals have had incentives to reduce stay durations and keep patient flow tip-top. Diagnosis Related Group (DRG)–based and capitated payments expedited that shift.
Accompanying the change, physicians became more aware of the potential repercussions of sicker and quicker discharges. They began to monitor their care and, as best as possible, use what measures they could as a proxy for quality (readmissions and hospital-acquired conditions). Providers balanced the harms of a continued stay with the benefits of added days, not to mention the need for cost savings.
I recognize this because of the cognitive dissonance providers now experience because of the mixed messages delivered by hospital leaders.
On the one hand, the DRG-driven system that we have binds the hospital’s bottom line – and that is not going away. On the other, we are paying more attention to excessive costs in post-acute settings, that is, subacute facilities when home health will do or more intense acute rehabilitation rather than the subacute route.
Making determinations as to whether a certain course is proper, whether a patient will be safe, whether families can provide adequate agency and backing, and whether we can avail community services takes time. Sicker and quicker; mindful of short-term outcomes; worked when we had postdischarge blinders on. As we remove such obstacles, and payment incentives change to cover broader intervals of time, we have to adapt. And that means leadership must realize that the practices that held hospitals in sound financial stead in years past are heading toward extinction – or, at best, falling out of favor.
Compare the costs of routine hospital care with the added expense of post-acute care, then multiply that extra expense times an aging, dependent population, and you add billions of dollars to the recovery tab. Some of these expenses are necessary, and some are not; a stay at a skilled nursing facility, for example, doubles the cost of an episode.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
- Why 7 On/7 Off Doesn’t Meet the Needs of Long-Stay Hospital Patients by Lauren Doctoroff, MD, FHM
- Is It Time for Health Policy M&Ms? by Chris Moriates, MD
- George Carlin Predicts Hospital Planning Strategy by Jordan Messler, MD, SFHM
- Many Paths to a Richer Job by Leslie Flores, MHA, MPH, SFHM
- A New Face for Online Modules by Chris Moriates, MD
You Have Lowered Length of Stay. Congratulations: You’re Fired.
For several decades, providers working within hospitals have had incentives to reduce stay durations and keep patient flow tip-top. Diagnosis Related Group (DRG)–based and capitated payments expedited that shift.
Accompanying the change, physicians became more aware of the potential repercussions of sicker and quicker discharges. They began to monitor their care and, as best as possible, use what measures they could as a proxy for quality (readmissions and hospital-acquired conditions). Providers balanced the harms of a continued stay with the benefits of added days, not to mention the need for cost savings.
I recognize this because of the cognitive dissonance providers now experience because of the mixed messages delivered by hospital leaders.
On the one hand, the DRG-driven system that we have binds the hospital’s bottom line – and that is not going away. On the other, we are paying more attention to excessive costs in post-acute settings, that is, subacute facilities when home health will do or more intense acute rehabilitation rather than the subacute route.
Making determinations as to whether a certain course is proper, whether a patient will be safe, whether families can provide adequate agency and backing, and whether we can avail community services takes time. Sicker and quicker; mindful of short-term outcomes; worked when we had postdischarge blinders on. As we remove such obstacles, and payment incentives change to cover broader intervals of time, we have to adapt. And that means leadership must realize that the practices that held hospitals in sound financial stead in years past are heading toward extinction – or, at best, falling out of favor.
Compare the costs of routine hospital care with the added expense of post-acute care, then multiply that extra expense times an aging, dependent population, and you add billions of dollars to the recovery tab. Some of these expenses are necessary, and some are not; a stay at a skilled nursing facility, for example, doubles the cost of an episode.
Read the full post at hospitalleader.org.
Also on The Hospital Leader …
- Why 7 On/7 Off Doesn’t Meet the Needs of Long-Stay Hospital Patients by Lauren Doctoroff, MD, FHM
- Is It Time for Health Policy M&Ms? by Chris Moriates, MD
- George Carlin Predicts Hospital Planning Strategy by Jordan Messler, MD, SFHM
- Many Paths to a Richer Job by Leslie Flores, MHA, MPH, SFHM
- A New Face for Online Modules by Chris Moriates, MD
Identification of Hospitalists
A seminal 1996 New England Journal of Medicine article introduced the term hospitalist to describe the emerging trend of primary care physicians practicing in inpatient hospital settings.[1] Although physicians had practice patterns akin to hospitalists prior to the introduction of the term,[2] the field continues to grow and formalize as a unique specialty in medicine.
There is currently no board certification or specialty billing code associated with hospitalists. In 2009, the American Board of Internal Medicine and American Board of Family Medicine introduced a Focused Practice in Hospital Medicine optional recertification pathway.[3] However, absent a unique identifier, it remains difficult to identify the number of hospitalists practicing today. Issues with identification notwithstanding, published data consistently suggest that the number of hospitalists has grown dramatically over the last 2 decades.[4, 5, 6]
The Centers for Medicare and Medicaid Services (CMS), along with other payers, classify hospitalists based on their board certificationmost commonly internal medicine or family practice. Other approaches for more precise assessment utilized billing data or hospital designation. Saint et al. identified hospital‐based providers practicing in Washington State in 1994 using variable thresholds of billing for inpatient services.[2] In 2011, Welch et al. identified 25,787 hospitalists nationwide, using a 90% threshold of billing inpatient services in Medicare data.[6] That same year, an American Hospital Association survey identified 34,411 hospitalists based on self‐reporting.[4]
Building on the work of previous researchers, we applied an updated threshold of inpatient services in publicly available 2012 Medicare Provider Utilization and Payment Data to identify a range of hospitalists practicing in the United States. We also examine the codes billed by providers identified in different decile billing thresholds to assess the validity of using lower thresholds to identify hospitalists.
METHODS
Approach to Identifying Hospitalists
In April 2014, CMS publicly released Medicare Provider Utilization and Payment data from all 880,000 providers who billed Medicare Part B in 2012. The dataset included services charged for 2012 Medicare Part B fee‐for‐service claims. The data omitted claims billed by a unique National Provider Identifier (NPI) for fewer than 10 Medicare beneficiaries. CMS assigned a specialty designation to each provider in the pay data based on the Medicare specialty billing code listed most frequently on his or her claims.
We explored the number of hospitalists in the 2012 Medicare pay data using specialty designation in combination with patterns of billing data. We first grouped physicians with specialty designations of internal medicine and family practice (IM/FP), the most common board certifications for hospitalists. We then selected 4 Healthcare Common Procedure Coding System (HCPCS) code clusters commonly associated with hospitalist practice: acute inpatient (HCPCS codes 9922199223, 9923199233, and 9923899239), observation (9921899220, 9922499226, and 99217), observation/emnpatient same day (9923499236), and critical care (9929199292). We included observation services codes given the significant role hospitalists play in their use[7, 8] and CMS incorporation of observation services for a threshold to identify and exempt hospital‐based providers in meaningful use.[9]
Analysis of Billing Thresholds and Other Codes Billed by Hospitalists
We examined the numbers of hospitalists who would be identified using a 50%, 60%, 70%, 80%, or 90% threshold, and compared the level of change in the size of the group with each change in decile.
We then analyzed the services billed by hospitalists who billed our threshold codes between 60% and 70% of the time. We looked at all codes billed with a frequency of greater than 0.1%, grouping clusters of similar services to identify patterns of clinical activity performed by these physicians.
RESULTS
The 2012 Medicare pay data included 664,253 physicians with unique NPIs. Of these, 169,317 had IM/FP specialty designations, whereas just under half (46.25%) of those physicians billed any of the inpatient HCPCS codes associated with our threshold.
Table 1 describes the range of number of hospitalists identified by varying the threshold of inpatient services. A total of 28,473 providers bill the threshold‐associated inpatient codes almost exclusively, whereas each descending decile increases in size by an average of 7.29%.
| Threshold (%) | Unique NPIs | % of IM/FP Physicians | % of All Physicians |
|---|---|---|---|
| |||
| 90 | 28,473 | 16.8 | 4.3 |
| 80 | 30,866 | 18.2 | 4.6 |
| 70 | 32,834 | 19.4 | 4.9 |
| 60 | 35,116 | 20.7 | 5.3 |
| 50 | 37,646 | 22.2 | 5.7 |
We also analyzed billing patterns of a subset of physicians who billed our threshold codes between 60% and 70% of the time to better characterize the remainder of clinical work they perform. This group included 2282 physicians and only 56 unique HCPCS codes with frequencies greater than 0.1%. After clustering related codes, we identified 4 common code groups that account for the majority of the remaining billing beyond inpatient threshold codes (Table 2).
| Clinical Service Cluster | HCPCS Codes Included | % |
|---|---|---|
| ||
| Threshold codes | 99217, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239, 99291 | 64.5 |
| Office visit (new and established) | 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215 | 15.3 |
| SNF care (initial and subsequent) | 99305, 99306, 99307, 99308, 99309, 99310, 99315 | 7.1 |
| ECG‐related codes | 93000, 93010, 93042 | 2.5 |
| Routine venipuncture | 36415 | 1.0 |
| Other codes with f>0.1%* | 25 codes | 5.1 |
| Codes with f<0.1% | 439 codes | 4.5 |
| Total | 495 codes | 100.0 |
DISCUSSION
Hospitalists make up approximately 5% of the practicing physicians nationwide, performing a critical role caring for hospitalized patients. Saint et al. defined a pure hospitalist as a physician who meets a 90% threshold of inpatient services.[2] This approach has been replicated in subsequent studies that used a 90% threshold to identify hospitalists.[5, 6] Our results with the same threshold reveal more than 28,000 hospitalists with nearly uniform practice patterns, a 10% growth in the number of hospitalists from the Welch et al. analysis in 2011.[6]
A threshold is not a perfect tool for identifying groups of practicing physicians, as it creates an arbitrary cutoff within a dataset. Undoubtedly our analysis could include providers who would not consider themselves hospitalists, or alternatively, appear to have a hospital‐based practice when they do not. Our results suggest that a 90% threshold may identify a majority of practicing hospitalists, but excludes providers who likely identify as hospitalists albeit with divergent practice and billing patterns.
A lower threshold may be more inclusive of the current realities of hospitalist practice, accounting for the myriad other services provided during, immediately prior to, or following a hospitalization. With hospitalists commonly practicing in diverse facility settings, rotating through rehabilitation or nursing home facilities, discharge clinics, and preoperative medicine practices, the continued use of a 90% threshold appears to exclude a sizable number of practicing hospitalists.
In the absence of a formal identifier, developing identification methodologies that account for the diversity of hospitalist practice is crucial. As physician payment transitions to value‐based reimbursement, systems must have the ability to account for and allocate the most efficient mix of providers for their patient populations. Because provider alignment and coordination are structural features of these programs, these systems‐based changes in effect require accurate identification of hospitalists, yet currently lack the tools to do so.
Disclosures
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration. Investigator salary support is provided through the South Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors report no conflicts of interest.
A seminal 1996 New England Journal of Medicine article introduced the term hospitalist to describe the emerging trend of primary care physicians practicing in inpatient hospital settings.[1] Although physicians had practice patterns akin to hospitalists prior to the introduction of the term,[2] the field continues to grow and formalize as a unique specialty in medicine.
There is currently no board certification or specialty billing code associated with hospitalists. In 2009, the American Board of Internal Medicine and American Board of Family Medicine introduced a Focused Practice in Hospital Medicine optional recertification pathway.[3] However, absent a unique identifier, it remains difficult to identify the number of hospitalists practicing today. Issues with identification notwithstanding, published data consistently suggest that the number of hospitalists has grown dramatically over the last 2 decades.[4, 5, 6]
The Centers for Medicare and Medicaid Services (CMS), along with other payers, classify hospitalists based on their board certificationmost commonly internal medicine or family practice. Other approaches for more precise assessment utilized billing data or hospital designation. Saint et al. identified hospital‐based providers practicing in Washington State in 1994 using variable thresholds of billing for inpatient services.[2] In 2011, Welch et al. identified 25,787 hospitalists nationwide, using a 90% threshold of billing inpatient services in Medicare data.[6] That same year, an American Hospital Association survey identified 34,411 hospitalists based on self‐reporting.[4]
Building on the work of previous researchers, we applied an updated threshold of inpatient services in publicly available 2012 Medicare Provider Utilization and Payment Data to identify a range of hospitalists practicing in the United States. We also examine the codes billed by providers identified in different decile billing thresholds to assess the validity of using lower thresholds to identify hospitalists.
METHODS
Approach to Identifying Hospitalists
In April 2014, CMS publicly released Medicare Provider Utilization and Payment data from all 880,000 providers who billed Medicare Part B in 2012. The dataset included services charged for 2012 Medicare Part B fee‐for‐service claims. The data omitted claims billed by a unique National Provider Identifier (NPI) for fewer than 10 Medicare beneficiaries. CMS assigned a specialty designation to each provider in the pay data based on the Medicare specialty billing code listed most frequently on his or her claims.
We explored the number of hospitalists in the 2012 Medicare pay data using specialty designation in combination with patterns of billing data. We first grouped physicians with specialty designations of internal medicine and family practice (IM/FP), the most common board certifications for hospitalists. We then selected 4 Healthcare Common Procedure Coding System (HCPCS) code clusters commonly associated with hospitalist practice: acute inpatient (HCPCS codes 9922199223, 9923199233, and 9923899239), observation (9921899220, 9922499226, and 99217), observation/emnpatient same day (9923499236), and critical care (9929199292). We included observation services codes given the significant role hospitalists play in their use[7, 8] and CMS incorporation of observation services for a threshold to identify and exempt hospital‐based providers in meaningful use.[9]
Analysis of Billing Thresholds and Other Codes Billed by Hospitalists
We examined the numbers of hospitalists who would be identified using a 50%, 60%, 70%, 80%, or 90% threshold, and compared the level of change in the size of the group with each change in decile.
We then analyzed the services billed by hospitalists who billed our threshold codes between 60% and 70% of the time. We looked at all codes billed with a frequency of greater than 0.1%, grouping clusters of similar services to identify patterns of clinical activity performed by these physicians.
RESULTS
The 2012 Medicare pay data included 664,253 physicians with unique NPIs. Of these, 169,317 had IM/FP specialty designations, whereas just under half (46.25%) of those physicians billed any of the inpatient HCPCS codes associated with our threshold.
Table 1 describes the range of number of hospitalists identified by varying the threshold of inpatient services. A total of 28,473 providers bill the threshold‐associated inpatient codes almost exclusively, whereas each descending decile increases in size by an average of 7.29%.
| Threshold (%) | Unique NPIs | % of IM/FP Physicians | % of All Physicians |
|---|---|---|---|
| |||
| 90 | 28,473 | 16.8 | 4.3 |
| 80 | 30,866 | 18.2 | 4.6 |
| 70 | 32,834 | 19.4 | 4.9 |
| 60 | 35,116 | 20.7 | 5.3 |
| 50 | 37,646 | 22.2 | 5.7 |
We also analyzed billing patterns of a subset of physicians who billed our threshold codes between 60% and 70% of the time to better characterize the remainder of clinical work they perform. This group included 2282 physicians and only 56 unique HCPCS codes with frequencies greater than 0.1%. After clustering related codes, we identified 4 common code groups that account for the majority of the remaining billing beyond inpatient threshold codes (Table 2).
| Clinical Service Cluster | HCPCS Codes Included | % |
|---|---|---|
| ||
| Threshold codes | 99217, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239, 99291 | 64.5 |
| Office visit (new and established) | 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215 | 15.3 |
| SNF care (initial and subsequent) | 99305, 99306, 99307, 99308, 99309, 99310, 99315 | 7.1 |
| ECG‐related codes | 93000, 93010, 93042 | 2.5 |
| Routine venipuncture | 36415 | 1.0 |
| Other codes with f>0.1%* | 25 codes | 5.1 |
| Codes with f<0.1% | 439 codes | 4.5 |
| Total | 495 codes | 100.0 |
DISCUSSION
Hospitalists make up approximately 5% of the practicing physicians nationwide, performing a critical role caring for hospitalized patients. Saint et al. defined a pure hospitalist as a physician who meets a 90% threshold of inpatient services.[2] This approach has been replicated in subsequent studies that used a 90% threshold to identify hospitalists.[5, 6] Our results with the same threshold reveal more than 28,000 hospitalists with nearly uniform practice patterns, a 10% growth in the number of hospitalists from the Welch et al. analysis in 2011.[6]
A threshold is not a perfect tool for identifying groups of practicing physicians, as it creates an arbitrary cutoff within a dataset. Undoubtedly our analysis could include providers who would not consider themselves hospitalists, or alternatively, appear to have a hospital‐based practice when they do not. Our results suggest that a 90% threshold may identify a majority of practicing hospitalists, but excludes providers who likely identify as hospitalists albeit with divergent practice and billing patterns.
A lower threshold may be more inclusive of the current realities of hospitalist practice, accounting for the myriad other services provided during, immediately prior to, or following a hospitalization. With hospitalists commonly practicing in diverse facility settings, rotating through rehabilitation or nursing home facilities, discharge clinics, and preoperative medicine practices, the continued use of a 90% threshold appears to exclude a sizable number of practicing hospitalists.
In the absence of a formal identifier, developing identification methodologies that account for the diversity of hospitalist practice is crucial. As physician payment transitions to value‐based reimbursement, systems must have the ability to account for and allocate the most efficient mix of providers for their patient populations. Because provider alignment and coordination are structural features of these programs, these systems‐based changes in effect require accurate identification of hospitalists, yet currently lack the tools to do so.
Disclosures
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration. Investigator salary support is provided through the South Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors report no conflicts of interest.
A seminal 1996 New England Journal of Medicine article introduced the term hospitalist to describe the emerging trend of primary care physicians practicing in inpatient hospital settings.[1] Although physicians had practice patterns akin to hospitalists prior to the introduction of the term,[2] the field continues to grow and formalize as a unique specialty in medicine.
There is currently no board certification or specialty billing code associated with hospitalists. In 2009, the American Board of Internal Medicine and American Board of Family Medicine introduced a Focused Practice in Hospital Medicine optional recertification pathway.[3] However, absent a unique identifier, it remains difficult to identify the number of hospitalists practicing today. Issues with identification notwithstanding, published data consistently suggest that the number of hospitalists has grown dramatically over the last 2 decades.[4, 5, 6]
The Centers for Medicare and Medicaid Services (CMS), along with other payers, classify hospitalists based on their board certificationmost commonly internal medicine or family practice. Other approaches for more precise assessment utilized billing data or hospital designation. Saint et al. identified hospital‐based providers practicing in Washington State in 1994 using variable thresholds of billing for inpatient services.[2] In 2011, Welch et al. identified 25,787 hospitalists nationwide, using a 90% threshold of billing inpatient services in Medicare data.[6] That same year, an American Hospital Association survey identified 34,411 hospitalists based on self‐reporting.[4]
Building on the work of previous researchers, we applied an updated threshold of inpatient services in publicly available 2012 Medicare Provider Utilization and Payment Data to identify a range of hospitalists practicing in the United States. We also examine the codes billed by providers identified in different decile billing thresholds to assess the validity of using lower thresholds to identify hospitalists.
METHODS
Approach to Identifying Hospitalists
In April 2014, CMS publicly released Medicare Provider Utilization and Payment data from all 880,000 providers who billed Medicare Part B in 2012. The dataset included services charged for 2012 Medicare Part B fee‐for‐service claims. The data omitted claims billed by a unique National Provider Identifier (NPI) for fewer than 10 Medicare beneficiaries. CMS assigned a specialty designation to each provider in the pay data based on the Medicare specialty billing code listed most frequently on his or her claims.
We explored the number of hospitalists in the 2012 Medicare pay data using specialty designation in combination with patterns of billing data. We first grouped physicians with specialty designations of internal medicine and family practice (IM/FP), the most common board certifications for hospitalists. We then selected 4 Healthcare Common Procedure Coding System (HCPCS) code clusters commonly associated with hospitalist practice: acute inpatient (HCPCS codes 9922199223, 9923199233, and 9923899239), observation (9921899220, 9922499226, and 99217), observation/emnpatient same day (9923499236), and critical care (9929199292). We included observation services codes given the significant role hospitalists play in their use[7, 8] and CMS incorporation of observation services for a threshold to identify and exempt hospital‐based providers in meaningful use.[9]
Analysis of Billing Thresholds and Other Codes Billed by Hospitalists
We examined the numbers of hospitalists who would be identified using a 50%, 60%, 70%, 80%, or 90% threshold, and compared the level of change in the size of the group with each change in decile.
We then analyzed the services billed by hospitalists who billed our threshold codes between 60% and 70% of the time. We looked at all codes billed with a frequency of greater than 0.1%, grouping clusters of similar services to identify patterns of clinical activity performed by these physicians.
RESULTS
The 2012 Medicare pay data included 664,253 physicians with unique NPIs. Of these, 169,317 had IM/FP specialty designations, whereas just under half (46.25%) of those physicians billed any of the inpatient HCPCS codes associated with our threshold.
Table 1 describes the range of number of hospitalists identified by varying the threshold of inpatient services. A total of 28,473 providers bill the threshold‐associated inpatient codes almost exclusively, whereas each descending decile increases in size by an average of 7.29%.
| Threshold (%) | Unique NPIs | % of IM/FP Physicians | % of All Physicians |
|---|---|---|---|
| |||
| 90 | 28,473 | 16.8 | 4.3 |
| 80 | 30,866 | 18.2 | 4.6 |
| 70 | 32,834 | 19.4 | 4.9 |
| 60 | 35,116 | 20.7 | 5.3 |
| 50 | 37,646 | 22.2 | 5.7 |
We also analyzed billing patterns of a subset of physicians who billed our threshold codes between 60% and 70% of the time to better characterize the remainder of clinical work they perform. This group included 2282 physicians and only 56 unique HCPCS codes with frequencies greater than 0.1%. After clustering related codes, we identified 4 common code groups that account for the majority of the remaining billing beyond inpatient threshold codes (Table 2).
| Clinical Service Cluster | HCPCS Codes Included | % |
|---|---|---|
| ||
| Threshold codes | 99217, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99238, 99239, 99291 | 64.5 |
| Office visit (new and established) | 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215 | 15.3 |
| SNF care (initial and subsequent) | 99305, 99306, 99307, 99308, 99309, 99310, 99315 | 7.1 |
| ECG‐related codes | 93000, 93010, 93042 | 2.5 |
| Routine venipuncture | 36415 | 1.0 |
| Other codes with f>0.1%* | 25 codes | 5.1 |
| Codes with f<0.1% | 439 codes | 4.5 |
| Total | 495 codes | 100.0 |
DISCUSSION
Hospitalists make up approximately 5% of the practicing physicians nationwide, performing a critical role caring for hospitalized patients. Saint et al. defined a pure hospitalist as a physician who meets a 90% threshold of inpatient services.[2] This approach has been replicated in subsequent studies that used a 90% threshold to identify hospitalists.[5, 6] Our results with the same threshold reveal more than 28,000 hospitalists with nearly uniform practice patterns, a 10% growth in the number of hospitalists from the Welch et al. analysis in 2011.[6]
A threshold is not a perfect tool for identifying groups of practicing physicians, as it creates an arbitrary cutoff within a dataset. Undoubtedly our analysis could include providers who would not consider themselves hospitalists, or alternatively, appear to have a hospital‐based practice when they do not. Our results suggest that a 90% threshold may identify a majority of practicing hospitalists, but excludes providers who likely identify as hospitalists albeit with divergent practice and billing patterns.
A lower threshold may be more inclusive of the current realities of hospitalist practice, accounting for the myriad other services provided during, immediately prior to, or following a hospitalization. With hospitalists commonly practicing in diverse facility settings, rotating through rehabilitation or nursing home facilities, discharge clinics, and preoperative medicine practices, the continued use of a 90% threshold appears to exclude a sizable number of practicing hospitalists.
In the absence of a formal identifier, developing identification methodologies that account for the diversity of hospitalist practice is crucial. As physician payment transitions to value‐based reimbursement, systems must have the ability to account for and allocate the most efficient mix of providers for their patient populations. Because provider alignment and coordination are structural features of these programs, these systems‐based changes in effect require accurate identification of hospitalists, yet currently lack the tools to do so.
Disclosures
The research reported here was supported by the Department of Veterans Affairs, Veterans Health Administration. Investigator salary support is provided through the South Texas Veterans Health Care System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors report no conflicts of interest.
Letter to the Editor
I read with great interest the article by McAlister and colleagues[1] on weekend versus weekday discharge outcomes.
The authors addressed length of stay (LOS) as a potential confounder in their inquiry. They ran regressions with and without LOS as a control and stated their results did not change; the findings imply LOS did not rest in the causal pathway between calendar day of discharge and outcomes.
I would like to highlight a recent article in which the authors found the reverse. Bartel et al.[2] applied a clever instrumental analysischoosing admission day (Sunday and Monday vs Tuesday through Saturday) as the instrumentto determine outcomes based on LOS. The investigators also ran a number of convincing falsification tests to verify their study design. They found an inverse association between greater length of hospital stay and readmissions and mortality.
Although Bartel et al. used a narrower spectrum of diagnoses and analyzed Medicare beneficiaries only, the results illuminate the difficulty in understanding the relationship between time in house and the day of discharge. If LOS influences mortality and readmission rates, overlooking its effect may obscure physician efforts to reduce LOS, for the laudatory goal of lessening return hospital trips and death.
The book on LOS impact remains open. We must remain uncertain of the interplay between days in house, mortality, readmission, and the weekend effect until further studies can elucidate how these variables interact.
- , , , . Similar outcomes among general medicine patients discharged on weekends. J Hosp Med. 2015;10(2):69–74.
- , , . Should hospitals keep their patients longer? The role of inpatient and outpatient care in reducing readmissions. NBER working paper no. 20499. National Bureau of Economic Research website. Available at: http://www.nber.org/papers/w20499. Published September 2014. Accessed December 26, 2014.
I read with great interest the article by McAlister and colleagues[1] on weekend versus weekday discharge outcomes.
The authors addressed length of stay (LOS) as a potential confounder in their inquiry. They ran regressions with and without LOS as a control and stated their results did not change; the findings imply LOS did not rest in the causal pathway between calendar day of discharge and outcomes.
I would like to highlight a recent article in which the authors found the reverse. Bartel et al.[2] applied a clever instrumental analysischoosing admission day (Sunday and Monday vs Tuesday through Saturday) as the instrumentto determine outcomes based on LOS. The investigators also ran a number of convincing falsification tests to verify their study design. They found an inverse association between greater length of hospital stay and readmissions and mortality.
Although Bartel et al. used a narrower spectrum of diagnoses and analyzed Medicare beneficiaries only, the results illuminate the difficulty in understanding the relationship between time in house and the day of discharge. If LOS influences mortality and readmission rates, overlooking its effect may obscure physician efforts to reduce LOS, for the laudatory goal of lessening return hospital trips and death.
The book on LOS impact remains open. We must remain uncertain of the interplay between days in house, mortality, readmission, and the weekend effect until further studies can elucidate how these variables interact.
I read with great interest the article by McAlister and colleagues[1] on weekend versus weekday discharge outcomes.
The authors addressed length of stay (LOS) as a potential confounder in their inquiry. They ran regressions with and without LOS as a control and stated their results did not change; the findings imply LOS did not rest in the causal pathway between calendar day of discharge and outcomes.
I would like to highlight a recent article in which the authors found the reverse. Bartel et al.[2] applied a clever instrumental analysischoosing admission day (Sunday and Monday vs Tuesday through Saturday) as the instrumentto determine outcomes based on LOS. The investigators also ran a number of convincing falsification tests to verify their study design. They found an inverse association between greater length of hospital stay and readmissions and mortality.
Although Bartel et al. used a narrower spectrum of diagnoses and analyzed Medicare beneficiaries only, the results illuminate the difficulty in understanding the relationship between time in house and the day of discharge. If LOS influences mortality and readmission rates, overlooking its effect may obscure physician efforts to reduce LOS, for the laudatory goal of lessening return hospital trips and death.
The book on LOS impact remains open. We must remain uncertain of the interplay between days in house, mortality, readmission, and the weekend effect until further studies can elucidate how these variables interact.
- , , , . Similar outcomes among general medicine patients discharged on weekends. J Hosp Med. 2015;10(2):69–74.
- , , . Should hospitals keep their patients longer? The role of inpatient and outpatient care in reducing readmissions. NBER working paper no. 20499. National Bureau of Economic Research website. Available at: http://www.nber.org/papers/w20499. Published September 2014. Accessed December 26, 2014.
- , , , . Similar outcomes among general medicine patients discharged on weekends. J Hosp Med. 2015;10(2):69–74.
- , , . Should hospitals keep their patients longer? The role of inpatient and outpatient care in reducing readmissions. NBER working paper no. 20499. National Bureau of Economic Research website. Available at: http://www.nber.org/papers/w20499. Published September 2014. Accessed December 26, 2014.
Members should “pony up” and run a 21st-century medical society
It was a propitious step to hear from Jeff Weise, MD, SFHM, current president of SHM, speaking in favor of increased transparency for our organization (see “To Err is Human,” October 2010, p. 42).
Encouragingly, when SHM has misstepped, we have corrected our transgressions. We have adopted rigorous conflict-of-interest policies, and we now disclose affiliations rapidly as a consequence—both for our board and for ranking members.
However, I do not believe, as Jeff states, we are the leaders in this domain. SHM still accepts large sums of money from industry, the exact amounts of which remain undisclosed on our website. Additionally, we underwrite our national meetings with corporate contributions, while other organizations have moved forward and shunned this process.1 Corporate sponsorship via branded logos are prominent on our website.
Granted, we are far from alone in this endeavor. Nevertheless, even with full disclosure, the appearance of purity is far from assured, as an outstanding essay commenting on AAFP’s acceptance of monies from Coca-Cola conveys.2
Calls to reform professional medical society practices are increasing, and the new healthcare legislation will begin to mandate recording, and then reporting, of physician-industry affiliations.3
Whether our organization will continue to “lead” on this front is unknown, and a question we must ask is, “Are our members prepared to pay full freight and pony up the costs of running our society in lieu of outside dollars?” I hope at some point the answer is “Yes.”
I for one would welcome full SHM disclosure, front and center, at our next national meeting. Similar to consumer-directed healthcare plan (CDHP) uptake lagging in the presence of opaque transaction costs at hospitals, we cannot change unless as members we know exactly what percentage of our activity others remunerate.
The “others,” as you can guess, are not physicians.
Bradley Flansbaum, DO, MPH, SFHM,
director, hospitalist services,
Lenox Hill Hospital, New York
References
- The American Psychiatric Association phases out industry-supported symposia. American Psychiatric Association website. Available at: http://psych.org/MainMenu/Newsroom/NewsReleases/2009NewsReleases/APAPhasesOutISS.aspx. Accessed Sept. 21, 2010.
- Brody H. Professional medical organizations and commercial conflicts of interest: ethical issues. Ann Fam Med. 2010;8(4):354-358.
- Rothman DJ, McDonald WJ, Berkowitz CD, et al. Professional medical associations and their relationships with industry: a proposal for controlling conflict of interest. JAMA. 2009;301(13):1367-1372.
It was a propitious step to hear from Jeff Weise, MD, SFHM, current president of SHM, speaking in favor of increased transparency for our organization (see “To Err is Human,” October 2010, p. 42).
Encouragingly, when SHM has misstepped, we have corrected our transgressions. We have adopted rigorous conflict-of-interest policies, and we now disclose affiliations rapidly as a consequence—both for our board and for ranking members.
However, I do not believe, as Jeff states, we are the leaders in this domain. SHM still accepts large sums of money from industry, the exact amounts of which remain undisclosed on our website. Additionally, we underwrite our national meetings with corporate contributions, while other organizations have moved forward and shunned this process.1 Corporate sponsorship via branded logos are prominent on our website.
Granted, we are far from alone in this endeavor. Nevertheless, even with full disclosure, the appearance of purity is far from assured, as an outstanding essay commenting on AAFP’s acceptance of monies from Coca-Cola conveys.2
Calls to reform professional medical society practices are increasing, and the new healthcare legislation will begin to mandate recording, and then reporting, of physician-industry affiliations.3
Whether our organization will continue to “lead” on this front is unknown, and a question we must ask is, “Are our members prepared to pay full freight and pony up the costs of running our society in lieu of outside dollars?” I hope at some point the answer is “Yes.”
I for one would welcome full SHM disclosure, front and center, at our next national meeting. Similar to consumer-directed healthcare plan (CDHP) uptake lagging in the presence of opaque transaction costs at hospitals, we cannot change unless as members we know exactly what percentage of our activity others remunerate.
The “others,” as you can guess, are not physicians.
Bradley Flansbaum, DO, MPH, SFHM,
director, hospitalist services,
Lenox Hill Hospital, New York
References
- The American Psychiatric Association phases out industry-supported symposia. American Psychiatric Association website. Available at: http://psych.org/MainMenu/Newsroom/NewsReleases/2009NewsReleases/APAPhasesOutISS.aspx. Accessed Sept. 21, 2010.
- Brody H. Professional medical organizations and commercial conflicts of interest: ethical issues. Ann Fam Med. 2010;8(4):354-358.
- Rothman DJ, McDonald WJ, Berkowitz CD, et al. Professional medical associations and their relationships with industry: a proposal for controlling conflict of interest. JAMA. 2009;301(13):1367-1372.
It was a propitious step to hear from Jeff Weise, MD, SFHM, current president of SHM, speaking in favor of increased transparency for our organization (see “To Err is Human,” October 2010, p. 42).
Encouragingly, when SHM has misstepped, we have corrected our transgressions. We have adopted rigorous conflict-of-interest policies, and we now disclose affiliations rapidly as a consequence—both for our board and for ranking members.
However, I do not believe, as Jeff states, we are the leaders in this domain. SHM still accepts large sums of money from industry, the exact amounts of which remain undisclosed on our website. Additionally, we underwrite our national meetings with corporate contributions, while other organizations have moved forward and shunned this process.1 Corporate sponsorship via branded logos are prominent on our website.
Granted, we are far from alone in this endeavor. Nevertheless, even with full disclosure, the appearance of purity is far from assured, as an outstanding essay commenting on AAFP’s acceptance of monies from Coca-Cola conveys.2
Calls to reform professional medical society practices are increasing, and the new healthcare legislation will begin to mandate recording, and then reporting, of physician-industry affiliations.3
Whether our organization will continue to “lead” on this front is unknown, and a question we must ask is, “Are our members prepared to pay full freight and pony up the costs of running our society in lieu of outside dollars?” I hope at some point the answer is “Yes.”
I for one would welcome full SHM disclosure, front and center, at our next national meeting. Similar to consumer-directed healthcare plan (CDHP) uptake lagging in the presence of opaque transaction costs at hospitals, we cannot change unless as members we know exactly what percentage of our activity others remunerate.
The “others,” as you can guess, are not physicians.
Bradley Flansbaum, DO, MPH, SFHM,
director, hospitalist services,
Lenox Hill Hospital, New York
References
- The American Psychiatric Association phases out industry-supported symposia. American Psychiatric Association website. Available at: http://psych.org/MainMenu/Newsroom/NewsReleases/2009NewsReleases/APAPhasesOutISS.aspx. Accessed Sept. 21, 2010.
- Brody H. Professional medical organizations and commercial conflicts of interest: ethical issues. Ann Fam Med. 2010;8(4):354-358.
- Rothman DJ, McDonald WJ, Berkowitz CD, et al. Professional medical associations and their relationships with industry: a proposal for controlling conflict of interest. JAMA. 2009;301(13):1367-1372.
Welcome to My World
Is hospital medicine a bona fide specialty? Do something long enough, and as Justice Potter Stewart said when defining a certain taboo carnal subject many years ago, I know it when I see it. Although working groups may struggle to conceive a master set of core competencies for hospitalists, I will tell you this: no texts are needed, and you know that you are on to something when 2 hospitalists practicing 3000 miles apart shoot each other a knowing glance and, without words, just understand what the other is thinking. After 10 years of practice in several hospitals, I have had enough mind melds to last a lifetime. Who needs science after all? I mean, how many of us can keep a straight face when asked if we have ever heard this line: Ah, yes, Dr. Flansbaum, umm, I am Dr. Smith from the surgical ICU, and we have a patient hospital day 34 status post Whipple that is no longer surgically active. See, you are smiling already. Do I have to finish the sentence for you?
What follows is a collective experience of things that I call the grind: things so small, so inconsequential, that no one will ever cite them individually as the deal breakers of the day. Collectively, they are the fabric of who we are and that little sore on the inside of our cheek that we just have to touch every few minutes in order to remind ourselves of why dermatologists always look so happy. Any accompanying sage lessons are also free of charge.
-
Why at the end of the day, always on a weekend after you have found a comfortable seat as far away from the nurse's station as possible, do you open up the chart and see 1 line of open space left on the last page of the progress notepaper? Even better, why is the note above it a follow‐up from vascular surgery, written in font size 24, in a form of Sanskrit that not even Steven Hawkings would recognize?
-
Okay, how about this: For patients with loooong lengths of stay, how many creative ways can you write Awaiting placement, afebrile, no complaints (in compliance with billing rules of course)? The correct answer is between 16 and 23. A thesaurus helps for word number 1try stable to startand change your pen from fine point to medium point on odd days. Then add tolerated breakfast on Monday, lunch on Tuesday, and dinner on Wednesday. Voila! Who said this was tough?
-
Okay, this one boggles my mind. You wish to auscultate a set of lungs. The patient is sitting on his gown. You attempt to lift the gown, and instead of raising his tush, the patient continues to sit while you tug away. Is this just me? It happens every week.
-
The medical students are great. They are ambitious and make teaching fun. Why though, at 9:59 AM, with an upcoming meeting with your chief at 10, are there no PC terminals at the station available except for the MSIII on MySpace.com with the chart you could not find (for 5 minutes) underneath his clipboard? Yes, Virginia, make me remember those days.
-
Clearly, this is one of the more helpful lines you can get from a consult: Patient needs to be medically optimized, and consider head MRI. Consider? Is not that why I called the consult in the first place? Let us consider not to use the word consider any more. Consider that. I feel better.
-
While we are on the topic of consultants, a dollar goes to you if this has never happened during your time on the wards: (1) the consultant visits, (2) the consultant evaluates, (3) you speak with the consultant, (4) all of you agree that the patient can go home, and (5) you then read the consult after the patient is dressed and his IV is out. Umm, a head CT before discharge and please have the neurosurgery clear the patient before discharge? Am I working in a parallel universe? Too much caffeine? Lord, give me strength.
-
Your beeper goes off at 2:57 PM. At 2:57 PM plus 5 seconds, you call the number you were paged from and no one answers. Does the word ponderous come to mind? This invariably happens every day, of course, typically when I am in the midst of multitasking 4 conversations. However, I extract some form of perverse cosmic revenge when I need to make a call and pick up an open extension from a ringing multiline phone. Invariably, I click the button to engage a line and, oops, good bye caller. I am only kidding; that never happens (is my nose really growing?). Just think, I could have been the one screaming, Is Laverne here?
-
You get an admission, a patient whom you have never met, and his room is listed as 428. You walk in, and the patient nearest to you is a well‐groomed middle‐age individual with a welcoming smile. The patient next to him is breathing fire, screaming at an imaginary executioner, and claiming that you are the guilty party and need to die. Which patient do you think is yours?
-
Those of you who work with housestaff will appreciate this one (file it under systems issue: fix next week): You have a discussion with a patient regarding his PM discharge at 11 AM. You arrange the follow‐up, you review the new medications, you discuss who will pick him up after dinner, and so forth. You get that warm and fuzzy feeling that you have done your job and all is right in the universe. Naturally, you also tell the resident that the patient can go home. Lo and behold, you look at your census the following morning, and the name of the aforementioned patient radiates like a beacon from the screen. You then poke your head into the room, feeling assured that it is merely an error, and the aforementioned patient is lying in bed, smiling and happy to see you. You ask, What happened? The reply, I don't know. Didn't your son come last night to pick you up? The response is yes. After the penetrating ulcer in your stomach bores a little deeper, you discover the official discharge order did not occur, and the patient was content eating chipped beef and sleeping on said contoured mattress 1 more night. Serenity now, serenity now.
-
The fifth vital sign? Is that the new black? Heck, number 5, I think we are up to 11 or 12 these days. Need a new metric installed? You guessed it: add it to the list!
-
Do you ever get LOS fatigue with a particular patient that is so severe you go to bed the previous night and have problems falling asleep? Really, what do you say to a person when his hospital stay exceeds, say, 5 months? Yes, I actually think of topics and issues that I can incorporate into the conversation which will spice up the relationship. New bed sheets, a fresh coat of paint? It would make a good Seinfeld episode, no?
-
Is it me, or is having 2 patients in the same room like being a flight attendant wheeling around the beverage cart? Get one the peanuts, and then the other wants the pretzels. For sure, add 10 minutes to your time in room 728 tomorrow.
-
If a patient is unable to leave the hospital for reasons unrelated to discharge planning (locked out of his house, the child is out of town until the next morning, etc.), why do I feel so naughty when I get off the phone with the MCO medical director after offering explanations? I do not get it. You think that the hospital employs a battery of runners to padlock homes and steal patient's clothing. Who wrote this playbook?
-
I love my consultants. Really, I do. I am not picking on them today. The high points of my day are the exchanges that I have with my subspecialty colleagues. However, the myopia that pervades some sign off notes give me pause. For example, a patient admitted for gastrointestinal bleed, s/p EGD, and stable at 72 hours post arrival receives a consultant note as follows: if patient eating and ambulating, can be discharged home as per PMD. Surely, when the level of transferred oversight shifts to the level of caloric ingestion and sneaker use, well, let us just say that I am all for some new E&M codes. They did not tell me about this in hospitalist school.
-
Don't you love the feeling of your beeper going off, and 30 seconds after the first page, boom, it goes off againboth to the same extension? I mean really, I am a nice guy, but do you really want to rile me up this early in the morning?
-
The nurse pages you from 1 floor away10 seconds from where you are standing. You recognize that number, you knew that it was coming, and for sure, waiting on the other end is that family member who hails from a foreboding place. How quickly does your brain do the computationdo I use the phone and let my fingers do the talking, or make that stroll and have that face‐to‐face summit? No sarcastic comment is needed. I see us now, hands joined, joyfully singing Kumbaya in a loving embrace.
-
Gee, it is not busy today. Say that on the wards and you get a leering glance. However, say that in the emergency room and you will meet your death. There is something about that phrase and the emergency department. The nurses there do not forget, although a Starbucks cappuccino does put a nice salve on the wound.
-
On your day off, do you ever notice that your beeper vibrates on your belt and you are not wearing it? I am not kidding.
-
An irony of life: I have developed an immunity to cigarette smoke in hospital bathrooms. Why is that? It is like peanut butter and jelly. They just seem so happy together.
-
Do you want to transfer that patient to psychiatry? No, no, no, you silly hospitalistdid you not notice that abnormal BUN and atypical lymphocyte on the peripheral smear? Hey, Dr. Freud, can you write me for some of that Prozac too!
-
We need to consult a rulebook on chair ownership. Did you ever notice (a tinge of Andy Rooney here) that case managers own their seats? I know that the world is not quite right when a case manager shoots me that dastardly glare, as if to say, Flee, you silly physician, I live at this station, you are merely my guest! As far as that chair is concerned, perhaps if a small plaque is added to the backrest with a suitable donation, my legs will finally get their deserved daily rest.
-
Finally, do you want to become invisible? Go to the reading board and stand behind a radiologist at 10:30 AM. Do it long enough, and after a few days, you will be saying I'm Good Enough, I'm Smart Enough, and Doggone It, People Like Me! Do you want to disappear completely? Try it on a Friday.
Okay, okay, I will stop there. It is funny, though; this stuff really happens. Despite the aggravation, I see these commonalities as the glue that binds us, assists in building the esprit de corps in our profession, and adds a little levity to the work place. Outside the hospital (not inside, of course), I can confidently state that these routines are part of who I am. After all, it is all about the knowing glance that I mentioned previously. The humorous part is that we are certainly on someone else's list. Probably a nurse, an emergency room doctor, or maybe a physician's assistant is scribing away at this minute, and we are number 7: Those hospitalists really tick me off.
EPILOGUE
Note to selflook in the mirror occasionally; you might learn something.
I apologize to all my nonhospitalist colleagues if you sneered. I love all of you. Today.
Is hospital medicine a bona fide specialty? Do something long enough, and as Justice Potter Stewart said when defining a certain taboo carnal subject many years ago, I know it when I see it. Although working groups may struggle to conceive a master set of core competencies for hospitalists, I will tell you this: no texts are needed, and you know that you are on to something when 2 hospitalists practicing 3000 miles apart shoot each other a knowing glance and, without words, just understand what the other is thinking. After 10 years of practice in several hospitals, I have had enough mind melds to last a lifetime. Who needs science after all? I mean, how many of us can keep a straight face when asked if we have ever heard this line: Ah, yes, Dr. Flansbaum, umm, I am Dr. Smith from the surgical ICU, and we have a patient hospital day 34 status post Whipple that is no longer surgically active. See, you are smiling already. Do I have to finish the sentence for you?
What follows is a collective experience of things that I call the grind: things so small, so inconsequential, that no one will ever cite them individually as the deal breakers of the day. Collectively, they are the fabric of who we are and that little sore on the inside of our cheek that we just have to touch every few minutes in order to remind ourselves of why dermatologists always look so happy. Any accompanying sage lessons are also free of charge.
-
Why at the end of the day, always on a weekend after you have found a comfortable seat as far away from the nurse's station as possible, do you open up the chart and see 1 line of open space left on the last page of the progress notepaper? Even better, why is the note above it a follow‐up from vascular surgery, written in font size 24, in a form of Sanskrit that not even Steven Hawkings would recognize?
-
Okay, how about this: For patients with loooong lengths of stay, how many creative ways can you write Awaiting placement, afebrile, no complaints (in compliance with billing rules of course)? The correct answer is between 16 and 23. A thesaurus helps for word number 1try stable to startand change your pen from fine point to medium point on odd days. Then add tolerated breakfast on Monday, lunch on Tuesday, and dinner on Wednesday. Voila! Who said this was tough?
-
Okay, this one boggles my mind. You wish to auscultate a set of lungs. The patient is sitting on his gown. You attempt to lift the gown, and instead of raising his tush, the patient continues to sit while you tug away. Is this just me? It happens every week.
-
The medical students are great. They are ambitious and make teaching fun. Why though, at 9:59 AM, with an upcoming meeting with your chief at 10, are there no PC terminals at the station available except for the MSIII on MySpace.com with the chart you could not find (for 5 minutes) underneath his clipboard? Yes, Virginia, make me remember those days.
-
Clearly, this is one of the more helpful lines you can get from a consult: Patient needs to be medically optimized, and consider head MRI. Consider? Is not that why I called the consult in the first place? Let us consider not to use the word consider any more. Consider that. I feel better.
-
While we are on the topic of consultants, a dollar goes to you if this has never happened during your time on the wards: (1) the consultant visits, (2) the consultant evaluates, (3) you speak with the consultant, (4) all of you agree that the patient can go home, and (5) you then read the consult after the patient is dressed and his IV is out. Umm, a head CT before discharge and please have the neurosurgery clear the patient before discharge? Am I working in a parallel universe? Too much caffeine? Lord, give me strength.
-
Your beeper goes off at 2:57 PM. At 2:57 PM plus 5 seconds, you call the number you were paged from and no one answers. Does the word ponderous come to mind? This invariably happens every day, of course, typically when I am in the midst of multitasking 4 conversations. However, I extract some form of perverse cosmic revenge when I need to make a call and pick up an open extension from a ringing multiline phone. Invariably, I click the button to engage a line and, oops, good bye caller. I am only kidding; that never happens (is my nose really growing?). Just think, I could have been the one screaming, Is Laverne here?
-
You get an admission, a patient whom you have never met, and his room is listed as 428. You walk in, and the patient nearest to you is a well‐groomed middle‐age individual with a welcoming smile. The patient next to him is breathing fire, screaming at an imaginary executioner, and claiming that you are the guilty party and need to die. Which patient do you think is yours?
-
Those of you who work with housestaff will appreciate this one (file it under systems issue: fix next week): You have a discussion with a patient regarding his PM discharge at 11 AM. You arrange the follow‐up, you review the new medications, you discuss who will pick him up after dinner, and so forth. You get that warm and fuzzy feeling that you have done your job and all is right in the universe. Naturally, you also tell the resident that the patient can go home. Lo and behold, you look at your census the following morning, and the name of the aforementioned patient radiates like a beacon from the screen. You then poke your head into the room, feeling assured that it is merely an error, and the aforementioned patient is lying in bed, smiling and happy to see you. You ask, What happened? The reply, I don't know. Didn't your son come last night to pick you up? The response is yes. After the penetrating ulcer in your stomach bores a little deeper, you discover the official discharge order did not occur, and the patient was content eating chipped beef and sleeping on said contoured mattress 1 more night. Serenity now, serenity now.
-
The fifth vital sign? Is that the new black? Heck, number 5, I think we are up to 11 or 12 these days. Need a new metric installed? You guessed it: add it to the list!
-
Do you ever get LOS fatigue with a particular patient that is so severe you go to bed the previous night and have problems falling asleep? Really, what do you say to a person when his hospital stay exceeds, say, 5 months? Yes, I actually think of topics and issues that I can incorporate into the conversation which will spice up the relationship. New bed sheets, a fresh coat of paint? It would make a good Seinfeld episode, no?
-
Is it me, or is having 2 patients in the same room like being a flight attendant wheeling around the beverage cart? Get one the peanuts, and then the other wants the pretzels. For sure, add 10 minutes to your time in room 728 tomorrow.
-
If a patient is unable to leave the hospital for reasons unrelated to discharge planning (locked out of his house, the child is out of town until the next morning, etc.), why do I feel so naughty when I get off the phone with the MCO medical director after offering explanations? I do not get it. You think that the hospital employs a battery of runners to padlock homes and steal patient's clothing. Who wrote this playbook?
-
I love my consultants. Really, I do. I am not picking on them today. The high points of my day are the exchanges that I have with my subspecialty colleagues. However, the myopia that pervades some sign off notes give me pause. For example, a patient admitted for gastrointestinal bleed, s/p EGD, and stable at 72 hours post arrival receives a consultant note as follows: if patient eating and ambulating, can be discharged home as per PMD. Surely, when the level of transferred oversight shifts to the level of caloric ingestion and sneaker use, well, let us just say that I am all for some new E&M codes. They did not tell me about this in hospitalist school.
-
Don't you love the feeling of your beeper going off, and 30 seconds after the first page, boom, it goes off againboth to the same extension? I mean really, I am a nice guy, but do you really want to rile me up this early in the morning?
-
The nurse pages you from 1 floor away10 seconds from where you are standing. You recognize that number, you knew that it was coming, and for sure, waiting on the other end is that family member who hails from a foreboding place. How quickly does your brain do the computationdo I use the phone and let my fingers do the talking, or make that stroll and have that face‐to‐face summit? No sarcastic comment is needed. I see us now, hands joined, joyfully singing Kumbaya in a loving embrace.
-
Gee, it is not busy today. Say that on the wards and you get a leering glance. However, say that in the emergency room and you will meet your death. There is something about that phrase and the emergency department. The nurses there do not forget, although a Starbucks cappuccino does put a nice salve on the wound.
-
On your day off, do you ever notice that your beeper vibrates on your belt and you are not wearing it? I am not kidding.
-
An irony of life: I have developed an immunity to cigarette smoke in hospital bathrooms. Why is that? It is like peanut butter and jelly. They just seem so happy together.
-
Do you want to transfer that patient to psychiatry? No, no, no, you silly hospitalistdid you not notice that abnormal BUN and atypical lymphocyte on the peripheral smear? Hey, Dr. Freud, can you write me for some of that Prozac too!
-
We need to consult a rulebook on chair ownership. Did you ever notice (a tinge of Andy Rooney here) that case managers own their seats? I know that the world is not quite right when a case manager shoots me that dastardly glare, as if to say, Flee, you silly physician, I live at this station, you are merely my guest! As far as that chair is concerned, perhaps if a small plaque is added to the backrest with a suitable donation, my legs will finally get their deserved daily rest.
-
Finally, do you want to become invisible? Go to the reading board and stand behind a radiologist at 10:30 AM. Do it long enough, and after a few days, you will be saying I'm Good Enough, I'm Smart Enough, and Doggone It, People Like Me! Do you want to disappear completely? Try it on a Friday.
Okay, okay, I will stop there. It is funny, though; this stuff really happens. Despite the aggravation, I see these commonalities as the glue that binds us, assists in building the esprit de corps in our profession, and adds a little levity to the work place. Outside the hospital (not inside, of course), I can confidently state that these routines are part of who I am. After all, it is all about the knowing glance that I mentioned previously. The humorous part is that we are certainly on someone else's list. Probably a nurse, an emergency room doctor, or maybe a physician's assistant is scribing away at this minute, and we are number 7: Those hospitalists really tick me off.
EPILOGUE
Note to selflook in the mirror occasionally; you might learn something.
I apologize to all my nonhospitalist colleagues if you sneered. I love all of you. Today.
Is hospital medicine a bona fide specialty? Do something long enough, and as Justice Potter Stewart said when defining a certain taboo carnal subject many years ago, I know it when I see it. Although working groups may struggle to conceive a master set of core competencies for hospitalists, I will tell you this: no texts are needed, and you know that you are on to something when 2 hospitalists practicing 3000 miles apart shoot each other a knowing glance and, without words, just understand what the other is thinking. After 10 years of practice in several hospitals, I have had enough mind melds to last a lifetime. Who needs science after all? I mean, how many of us can keep a straight face when asked if we have ever heard this line: Ah, yes, Dr. Flansbaum, umm, I am Dr. Smith from the surgical ICU, and we have a patient hospital day 34 status post Whipple that is no longer surgically active. See, you are smiling already. Do I have to finish the sentence for you?
What follows is a collective experience of things that I call the grind: things so small, so inconsequential, that no one will ever cite them individually as the deal breakers of the day. Collectively, they are the fabric of who we are and that little sore on the inside of our cheek that we just have to touch every few minutes in order to remind ourselves of why dermatologists always look so happy. Any accompanying sage lessons are also free of charge.
-
Why at the end of the day, always on a weekend after you have found a comfortable seat as far away from the nurse's station as possible, do you open up the chart and see 1 line of open space left on the last page of the progress notepaper? Even better, why is the note above it a follow‐up from vascular surgery, written in font size 24, in a form of Sanskrit that not even Steven Hawkings would recognize?
-
Okay, how about this: For patients with loooong lengths of stay, how many creative ways can you write Awaiting placement, afebrile, no complaints (in compliance with billing rules of course)? The correct answer is between 16 and 23. A thesaurus helps for word number 1try stable to startand change your pen from fine point to medium point on odd days. Then add tolerated breakfast on Monday, lunch on Tuesday, and dinner on Wednesday. Voila! Who said this was tough?
-
Okay, this one boggles my mind. You wish to auscultate a set of lungs. The patient is sitting on his gown. You attempt to lift the gown, and instead of raising his tush, the patient continues to sit while you tug away. Is this just me? It happens every week.
-
The medical students are great. They are ambitious and make teaching fun. Why though, at 9:59 AM, with an upcoming meeting with your chief at 10, are there no PC terminals at the station available except for the MSIII on MySpace.com with the chart you could not find (for 5 minutes) underneath his clipboard? Yes, Virginia, make me remember those days.
-
Clearly, this is one of the more helpful lines you can get from a consult: Patient needs to be medically optimized, and consider head MRI. Consider? Is not that why I called the consult in the first place? Let us consider not to use the word consider any more. Consider that. I feel better.
-
While we are on the topic of consultants, a dollar goes to you if this has never happened during your time on the wards: (1) the consultant visits, (2) the consultant evaluates, (3) you speak with the consultant, (4) all of you agree that the patient can go home, and (5) you then read the consult after the patient is dressed and his IV is out. Umm, a head CT before discharge and please have the neurosurgery clear the patient before discharge? Am I working in a parallel universe? Too much caffeine? Lord, give me strength.
-
Your beeper goes off at 2:57 PM. At 2:57 PM plus 5 seconds, you call the number you were paged from and no one answers. Does the word ponderous come to mind? This invariably happens every day, of course, typically when I am in the midst of multitasking 4 conversations. However, I extract some form of perverse cosmic revenge when I need to make a call and pick up an open extension from a ringing multiline phone. Invariably, I click the button to engage a line and, oops, good bye caller. I am only kidding; that never happens (is my nose really growing?). Just think, I could have been the one screaming, Is Laverne here?
-
You get an admission, a patient whom you have never met, and his room is listed as 428. You walk in, and the patient nearest to you is a well‐groomed middle‐age individual with a welcoming smile. The patient next to him is breathing fire, screaming at an imaginary executioner, and claiming that you are the guilty party and need to die. Which patient do you think is yours?
-
Those of you who work with housestaff will appreciate this one (file it under systems issue: fix next week): You have a discussion with a patient regarding his PM discharge at 11 AM. You arrange the follow‐up, you review the new medications, you discuss who will pick him up after dinner, and so forth. You get that warm and fuzzy feeling that you have done your job and all is right in the universe. Naturally, you also tell the resident that the patient can go home. Lo and behold, you look at your census the following morning, and the name of the aforementioned patient radiates like a beacon from the screen. You then poke your head into the room, feeling assured that it is merely an error, and the aforementioned patient is lying in bed, smiling and happy to see you. You ask, What happened? The reply, I don't know. Didn't your son come last night to pick you up? The response is yes. After the penetrating ulcer in your stomach bores a little deeper, you discover the official discharge order did not occur, and the patient was content eating chipped beef and sleeping on said contoured mattress 1 more night. Serenity now, serenity now.
-
The fifth vital sign? Is that the new black? Heck, number 5, I think we are up to 11 or 12 these days. Need a new metric installed? You guessed it: add it to the list!
-
Do you ever get LOS fatigue with a particular patient that is so severe you go to bed the previous night and have problems falling asleep? Really, what do you say to a person when his hospital stay exceeds, say, 5 months? Yes, I actually think of topics and issues that I can incorporate into the conversation which will spice up the relationship. New bed sheets, a fresh coat of paint? It would make a good Seinfeld episode, no?
-
Is it me, or is having 2 patients in the same room like being a flight attendant wheeling around the beverage cart? Get one the peanuts, and then the other wants the pretzels. For sure, add 10 minutes to your time in room 728 tomorrow.
-
If a patient is unable to leave the hospital for reasons unrelated to discharge planning (locked out of his house, the child is out of town until the next morning, etc.), why do I feel so naughty when I get off the phone with the MCO medical director after offering explanations? I do not get it. You think that the hospital employs a battery of runners to padlock homes and steal patient's clothing. Who wrote this playbook?
-
I love my consultants. Really, I do. I am not picking on them today. The high points of my day are the exchanges that I have with my subspecialty colleagues. However, the myopia that pervades some sign off notes give me pause. For example, a patient admitted for gastrointestinal bleed, s/p EGD, and stable at 72 hours post arrival receives a consultant note as follows: if patient eating and ambulating, can be discharged home as per PMD. Surely, when the level of transferred oversight shifts to the level of caloric ingestion and sneaker use, well, let us just say that I am all for some new E&M codes. They did not tell me about this in hospitalist school.
-
Don't you love the feeling of your beeper going off, and 30 seconds after the first page, boom, it goes off againboth to the same extension? I mean really, I am a nice guy, but do you really want to rile me up this early in the morning?
-
The nurse pages you from 1 floor away10 seconds from where you are standing. You recognize that number, you knew that it was coming, and for sure, waiting on the other end is that family member who hails from a foreboding place. How quickly does your brain do the computationdo I use the phone and let my fingers do the talking, or make that stroll and have that face‐to‐face summit? No sarcastic comment is needed. I see us now, hands joined, joyfully singing Kumbaya in a loving embrace.
-
Gee, it is not busy today. Say that on the wards and you get a leering glance. However, say that in the emergency room and you will meet your death. There is something about that phrase and the emergency department. The nurses there do not forget, although a Starbucks cappuccino does put a nice salve on the wound.
-
On your day off, do you ever notice that your beeper vibrates on your belt and you are not wearing it? I am not kidding.
-
An irony of life: I have developed an immunity to cigarette smoke in hospital bathrooms. Why is that? It is like peanut butter and jelly. They just seem so happy together.
-
Do you want to transfer that patient to psychiatry? No, no, no, you silly hospitalistdid you not notice that abnormal BUN and atypical lymphocyte on the peripheral smear? Hey, Dr. Freud, can you write me for some of that Prozac too!
-
We need to consult a rulebook on chair ownership. Did you ever notice (a tinge of Andy Rooney here) that case managers own their seats? I know that the world is not quite right when a case manager shoots me that dastardly glare, as if to say, Flee, you silly physician, I live at this station, you are merely my guest! As far as that chair is concerned, perhaps if a small plaque is added to the backrest with a suitable donation, my legs will finally get their deserved daily rest.
-
Finally, do you want to become invisible? Go to the reading board and stand behind a radiologist at 10:30 AM. Do it long enough, and after a few days, you will be saying I'm Good Enough, I'm Smart Enough, and Doggone It, People Like Me! Do you want to disappear completely? Try it on a Friday.
Okay, okay, I will stop there. It is funny, though; this stuff really happens. Despite the aggravation, I see these commonalities as the glue that binds us, assists in building the esprit de corps in our profession, and adds a little levity to the work place. Outside the hospital (not inside, of course), I can confidently state that these routines are part of who I am. After all, it is all about the knowing glance that I mentioned previously. The humorous part is that we are certainly on someone else's list. Probably a nurse, an emergency room doctor, or maybe a physician's assistant is scribing away at this minute, and we are number 7: Those hospitalists really tick me off.
EPILOGUE
Note to selflook in the mirror occasionally; you might learn something.
I apologize to all my nonhospitalist colleagues if you sneered. I love all of you. Today.