User login
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
How to Handle Medicare Documentation Audits
The recent announcement of a settlement by a physician firm should cause the HM community to pause and take inventory. The settlement “addressed allegations that, between 2004 and 2012, [the firm] knowingly submitted to federal health benefits programs inflated claims on behalf of its hospitalist employees for higher and more expensive levels of service than were documented by hospitalists in patient medical records.”1
This civil settlement highlights the vigilance being exercised against healthcare fraud and demonstrates the coordinated efforts in place to tackle the issue. To put the weight of this case in perspective, consider the breadth of legal entities involved: the U.S. Department of Justice; the U.S. Attorney’s Office; the U.S. Department of Health and Human Services; the U.S. Department of Defense; the U.S. Office of Personnel Management; the U.S. Department of Veterans’ Affairs; and the TRICARE Management Activity Office of General Counsel.1
The underlying factor in the settlement is a common issue routinely identified by Medicare-initiated review programs such as CERT (Comprehensive Error Rate Testing). CERT selects a stratified, random sample of approximately 40,000 claims submitted to Part A/B Medicare Administrative Contractors (MACs) and Durable Medical Equipment MACs (DME MACs) during each reporting period and allows the Centers for Medicare and Medicaid Services (CMS) to calculate a national improper payment rate and contractor- and service-specific improper payment rates.2 The CERT-determined improper payment rate identifies services that have not satisfied Medicare requirements, but it cannot label a claim fraudulent.2
Incorrect coding errors involving hospitalists are related to inpatient evaluation and management (E/M) services that do not adequately reflect the documentation in the medical record. For example, WPS Medicare identified the following error rates for claims submitted 7/1/11 to 6/30/12: 45% of 99223 (initial hospital care, per day, for the evaluation and management of a patient, which requires these three key components: a comprehensive history, a comprehensive exam, and medical decision-making of high complexity); and 34% of 99233 (subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least two of these three key components: a detailed interval history, a detailed examination, and medical decision-making of high complexity).3,4 More recent WPS Medicare data in first quarter of FY2013 reveals a continuing problem but an improved error rate.5 Novitas Solutions offers additional support of these findings.6
Based on efforts that identify improper payments, MACs are encouraged to initiate targeted service-specific prepayment review to prevent improper payments for services identified by CERT or recovery audit contractors (RACs) as problem areas, as well as problem areas identified by their own data analysis.7 For this reason, hospitalists may see prepayment requests for documentation by Medicare for services that are most “problematic” (e.g., 99223 and 99233). This occurs when a claim involving these services is submitted to Medicare. The MAC suspends all or part of a claim so that a trained clinician or claims analyst can review the claim and associated documentation in order to make determinations about coverage and payment.7 Responding to these requests in a timely manner is crucial in preventing claim denials.
Responding to Requests
When documentation is requested by the payor, take note of the date and the provider for whom the service is requested. Be certain to include all pertinent information in support of the claim. The payor request letter will typically include a generic list of items that should be submitted with the documentation request. Consider these particular items when submitting documentation for targeted services typically provided by hospitalists:
- Initial Hospital Care (99223)
- Physician notes (including resident, nurse practitioner, or physician assistant notes);
- Identify any referenced sources of information (e.g., physician referencing a family history documented in the ED record);
- Dictations, when performed;
- Admitting orders; and
- Labs or diagnostic test reports performed on admission.
- Subsequent Hospital Care (99233)
- Physician notes (including resident, nurse practitioner, or physician assistant notes);
- Identify multiple encounters/entries recorded on a given date;
- Physician orders; and
- Labs or diagnostic test reports performed on the requested date.
Documentation Tips
Because it is the primary communication tool for providers involved in the patient’s care, documentation must be entered in a timely manner and must be decipherable to members of the healthcare team as well as other individuals who may need to review the information (e.g., auditors). Proper credit cannot be given for documentation that is difficult to read.
Information should include historical review of past/interim events, a physical exam, medical decision-making as related to the patient’s progress/response to intervention, and modification of the care plan (as necessary). The reason for the encounter should be evident to support the medical necessity of the service. Because various specialists may participate in patient care, documentation for each provider’s encounter should demonstrate personalized and non-duplicative care.
Each individual provider must exhibit a personal contribution to the case to prevent payors from viewing the documentation as overlapping and indistinguishable from care already provided by another physician. Each entry should be dated and signed with a legible identifier (i.e., signature with a printed name).
The next several articles will address each of the key components (history, exam, and decision-making) and serve as a “documentation refresher” for providers who wish to compare their documentation to current standards.
References
- Department of Justice, Office of Public Affairs. Tacoma, Wash., Medical Firm to Pay $14.5 Million to Settle Overbilling Allegations. Available at: www.justice.gov/opa/pr/2013/July/13-civ-758.html. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Comprehensive Error Rate Testing (CERT). Available at: www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/CERT/index.html?redirect=/cert. Accessed September 20, 2013.
- WPS Medicare, Legacy Part B. Are you billing these evaluation and management (e/m) services correctly? Available at: http://www.wpsmedicare.com/j5macpartb/departments/cert/2011-0912-billemservices.shtml. Accessed September 20, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis, L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012:15-17.
- WPS Medicare, Legacy Part B. 1st Qtr. 2013 (Jan. - Mar.) - CERT Error Summary. Available at: http://www.wpsmedicare.com/j5macpartb/departments/cert/2013-1st-quarter-summary.shtml. Accessed September 20, 2013.
- Novitas Solutions. Analysis of JL Part B Comprehensive Error Rate Testing (CERT) Data - January thru March 2013. Available at: https://www.novitas-solutions.com/cert/errors/2013/b-jan-mar-j12.html. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Medicare Program Integrity Manual, Chapter 3, Section 3.2. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c03.pdf. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual, Chapter 11, Section 40.1.2 Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed September 20, 2013.
The recent announcement of a settlement by a physician firm should cause the HM community to pause and take inventory. The settlement “addressed allegations that, between 2004 and 2012, [the firm] knowingly submitted to federal health benefits programs inflated claims on behalf of its hospitalist employees for higher and more expensive levels of service than were documented by hospitalists in patient medical records.”1
This civil settlement highlights the vigilance being exercised against healthcare fraud and demonstrates the coordinated efforts in place to tackle the issue. To put the weight of this case in perspective, consider the breadth of legal entities involved: the U.S. Department of Justice; the U.S. Attorney’s Office; the U.S. Department of Health and Human Services; the U.S. Department of Defense; the U.S. Office of Personnel Management; the U.S. Department of Veterans’ Affairs; and the TRICARE Management Activity Office of General Counsel.1
The underlying factor in the settlement is a common issue routinely identified by Medicare-initiated review programs such as CERT (Comprehensive Error Rate Testing). CERT selects a stratified, random sample of approximately 40,000 claims submitted to Part A/B Medicare Administrative Contractors (MACs) and Durable Medical Equipment MACs (DME MACs) during each reporting period and allows the Centers for Medicare and Medicaid Services (CMS) to calculate a national improper payment rate and contractor- and service-specific improper payment rates.2 The CERT-determined improper payment rate identifies services that have not satisfied Medicare requirements, but it cannot label a claim fraudulent.2
Incorrect coding errors involving hospitalists are related to inpatient evaluation and management (E/M) services that do not adequately reflect the documentation in the medical record. For example, WPS Medicare identified the following error rates for claims submitted 7/1/11 to 6/30/12: 45% of 99223 (initial hospital care, per day, for the evaluation and management of a patient, which requires these three key components: a comprehensive history, a comprehensive exam, and medical decision-making of high complexity); and 34% of 99233 (subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least two of these three key components: a detailed interval history, a detailed examination, and medical decision-making of high complexity).3,4 More recent WPS Medicare data in first quarter of FY2013 reveals a continuing problem but an improved error rate.5 Novitas Solutions offers additional support of these findings.6
Based on efforts that identify improper payments, MACs are encouraged to initiate targeted service-specific prepayment review to prevent improper payments for services identified by CERT or recovery audit contractors (RACs) as problem areas, as well as problem areas identified by their own data analysis.7 For this reason, hospitalists may see prepayment requests for documentation by Medicare for services that are most “problematic” (e.g., 99223 and 99233). This occurs when a claim involving these services is submitted to Medicare. The MAC suspends all or part of a claim so that a trained clinician or claims analyst can review the claim and associated documentation in order to make determinations about coverage and payment.7 Responding to these requests in a timely manner is crucial in preventing claim denials.
Responding to Requests
When documentation is requested by the payor, take note of the date and the provider for whom the service is requested. Be certain to include all pertinent information in support of the claim. The payor request letter will typically include a generic list of items that should be submitted with the documentation request. Consider these particular items when submitting documentation for targeted services typically provided by hospitalists:
- Initial Hospital Care (99223)
- Physician notes (including resident, nurse practitioner, or physician assistant notes);
- Identify any referenced sources of information (e.g., physician referencing a family history documented in the ED record);
- Dictations, when performed;
- Admitting orders; and
- Labs or diagnostic test reports performed on admission.
- Subsequent Hospital Care (99233)
- Physician notes (including resident, nurse practitioner, or physician assistant notes);
- Identify multiple encounters/entries recorded on a given date;
- Physician orders; and
- Labs or diagnostic test reports performed on the requested date.
Documentation Tips
Because it is the primary communication tool for providers involved in the patient’s care, documentation must be entered in a timely manner and must be decipherable to members of the healthcare team as well as other individuals who may need to review the information (e.g., auditors). Proper credit cannot be given for documentation that is difficult to read.
Information should include historical review of past/interim events, a physical exam, medical decision-making as related to the patient’s progress/response to intervention, and modification of the care plan (as necessary). The reason for the encounter should be evident to support the medical necessity of the service. Because various specialists may participate in patient care, documentation for each provider’s encounter should demonstrate personalized and non-duplicative care.
Each individual provider must exhibit a personal contribution to the case to prevent payors from viewing the documentation as overlapping and indistinguishable from care already provided by another physician. Each entry should be dated and signed with a legible identifier (i.e., signature with a printed name).
The next several articles will address each of the key components (history, exam, and decision-making) and serve as a “documentation refresher” for providers who wish to compare their documentation to current standards.
References
- Department of Justice, Office of Public Affairs. Tacoma, Wash., Medical Firm to Pay $14.5 Million to Settle Overbilling Allegations. Available at: www.justice.gov/opa/pr/2013/July/13-civ-758.html. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Comprehensive Error Rate Testing (CERT). Available at: www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/CERT/index.html?redirect=/cert. Accessed September 20, 2013.
- WPS Medicare, Legacy Part B. Are you billing these evaluation and management (e/m) services correctly? Available at: http://www.wpsmedicare.com/j5macpartb/departments/cert/2011-0912-billemservices.shtml. Accessed September 20, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis, L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012:15-17.
- WPS Medicare, Legacy Part B. 1st Qtr. 2013 (Jan. - Mar.) - CERT Error Summary. Available at: http://www.wpsmedicare.com/j5macpartb/departments/cert/2013-1st-quarter-summary.shtml. Accessed September 20, 2013.
- Novitas Solutions. Analysis of JL Part B Comprehensive Error Rate Testing (CERT) Data - January thru March 2013. Available at: https://www.novitas-solutions.com/cert/errors/2013/b-jan-mar-j12.html. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Medicare Program Integrity Manual, Chapter 3, Section 3.2. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c03.pdf. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual, Chapter 11, Section 40.1.2 Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed September 20, 2013.
The recent announcement of a settlement by a physician firm should cause the HM community to pause and take inventory. The settlement “addressed allegations that, between 2004 and 2012, [the firm] knowingly submitted to federal health benefits programs inflated claims on behalf of its hospitalist employees for higher and more expensive levels of service than were documented by hospitalists in patient medical records.”1
This civil settlement highlights the vigilance being exercised against healthcare fraud and demonstrates the coordinated efforts in place to tackle the issue. To put the weight of this case in perspective, consider the breadth of legal entities involved: the U.S. Department of Justice; the U.S. Attorney’s Office; the U.S. Department of Health and Human Services; the U.S. Department of Defense; the U.S. Office of Personnel Management; the U.S. Department of Veterans’ Affairs; and the TRICARE Management Activity Office of General Counsel.1
The underlying factor in the settlement is a common issue routinely identified by Medicare-initiated review programs such as CERT (Comprehensive Error Rate Testing). CERT selects a stratified, random sample of approximately 40,000 claims submitted to Part A/B Medicare Administrative Contractors (MACs) and Durable Medical Equipment MACs (DME MACs) during each reporting period and allows the Centers for Medicare and Medicaid Services (CMS) to calculate a national improper payment rate and contractor- and service-specific improper payment rates.2 The CERT-determined improper payment rate identifies services that have not satisfied Medicare requirements, but it cannot label a claim fraudulent.2
Incorrect coding errors involving hospitalists are related to inpatient evaluation and management (E/M) services that do not adequately reflect the documentation in the medical record. For example, WPS Medicare identified the following error rates for claims submitted 7/1/11 to 6/30/12: 45% of 99223 (initial hospital care, per day, for the evaluation and management of a patient, which requires these three key components: a comprehensive history, a comprehensive exam, and medical decision-making of high complexity); and 34% of 99233 (subsequent hospital care, per day, for the evaluation and management of a patient, which requires at least two of these three key components: a detailed interval history, a detailed examination, and medical decision-making of high complexity).3,4 More recent WPS Medicare data in first quarter of FY2013 reveals a continuing problem but an improved error rate.5 Novitas Solutions offers additional support of these findings.6
Based on efforts that identify improper payments, MACs are encouraged to initiate targeted service-specific prepayment review to prevent improper payments for services identified by CERT or recovery audit contractors (RACs) as problem areas, as well as problem areas identified by their own data analysis.7 For this reason, hospitalists may see prepayment requests for documentation by Medicare for services that are most “problematic” (e.g., 99223 and 99233). This occurs when a claim involving these services is submitted to Medicare. The MAC suspends all or part of a claim so that a trained clinician or claims analyst can review the claim and associated documentation in order to make determinations about coverage and payment.7 Responding to these requests in a timely manner is crucial in preventing claim denials.
Responding to Requests
When documentation is requested by the payor, take note of the date and the provider for whom the service is requested. Be certain to include all pertinent information in support of the claim. The payor request letter will typically include a generic list of items that should be submitted with the documentation request. Consider these particular items when submitting documentation for targeted services typically provided by hospitalists:
- Initial Hospital Care (99223)
- Physician notes (including resident, nurse practitioner, or physician assistant notes);
- Identify any referenced sources of information (e.g., physician referencing a family history documented in the ED record);
- Dictations, when performed;
- Admitting orders; and
- Labs or diagnostic test reports performed on admission.
- Subsequent Hospital Care (99233)
- Physician notes (including resident, nurse practitioner, or physician assistant notes);
- Identify multiple encounters/entries recorded on a given date;
- Physician orders; and
- Labs or diagnostic test reports performed on the requested date.
Documentation Tips
Because it is the primary communication tool for providers involved in the patient’s care, documentation must be entered in a timely manner and must be decipherable to members of the healthcare team as well as other individuals who may need to review the information (e.g., auditors). Proper credit cannot be given for documentation that is difficult to read.
Information should include historical review of past/interim events, a physical exam, medical decision-making as related to the patient’s progress/response to intervention, and modification of the care plan (as necessary). The reason for the encounter should be evident to support the medical necessity of the service. Because various specialists may participate in patient care, documentation for each provider’s encounter should demonstrate personalized and non-duplicative care.
Each individual provider must exhibit a personal contribution to the case to prevent payors from viewing the documentation as overlapping and indistinguishable from care already provided by another physician. Each entry should be dated and signed with a legible identifier (i.e., signature with a printed name).
The next several articles will address each of the key components (history, exam, and decision-making) and serve as a “documentation refresher” for providers who wish to compare their documentation to current standards.
References
- Department of Justice, Office of Public Affairs. Tacoma, Wash., Medical Firm to Pay $14.5 Million to Settle Overbilling Allegations. Available at: www.justice.gov/opa/pr/2013/July/13-civ-758.html. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Comprehensive Error Rate Testing (CERT). Available at: www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/CERT/index.html?redirect=/cert. Accessed September 20, 2013.
- WPS Medicare, Legacy Part B. Are you billing these evaluation and management (e/m) services correctly? Available at: http://www.wpsmedicare.com/j5macpartb/departments/cert/2011-0912-billemservices.shtml. Accessed September 20, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis, L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012:15-17.
- WPS Medicare, Legacy Part B. 1st Qtr. 2013 (Jan. - Mar.) - CERT Error Summary. Available at: http://www.wpsmedicare.com/j5macpartb/departments/cert/2013-1st-quarter-summary.shtml. Accessed September 20, 2013.
- Novitas Solutions. Analysis of JL Part B Comprehensive Error Rate Testing (CERT) Data - January thru March 2013. Available at: https://www.novitas-solutions.com/cert/errors/2013/b-jan-mar-j12.html. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Medicare Program Integrity Manual, Chapter 3, Section 3.2. Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/pim83c03.pdf. Accessed September 20, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual, Chapter 11, Section 40.1.2 Available at: www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed September 20, 2013.
How To Avoid Medicare Denials for Critical-Care Billing
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
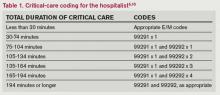
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Are your critical-care claims at risk for denial or repayment upon review? Several payors have identified increased potential for critical-care reporting discrepancies, which has resulted in targeted prepayment reviews of this code.1 Some payors have implemented 100% review when critical care is reported in settings other than inpatient hospitals, outpatient hospitals, or emergency departments.2 To ensure a successful outcome, make sure the documentation meets the basic principles of the critical-care guidelines.
Defining Critical Illness/Injury
CPT and the Centers for Medicare & Medicaid Services (CMS) define “critical illness or injury” as a condition that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition (e.g. central-nervous-system failure; circulatory failure; shock; renal, hepatic, metabolic, and/or respiratory failure).3 The provider’s time must be solely directed toward the critically ill patient. Highly complex decision-making and interventions of high intensity are required to prevent the patient’s inevitable decline if left untreated. Payment may be made for critical-care services provided in any reasonable location, as long as the care provided meets the definition of critical care. Critical-care services cannot be reported for a patient who is not critically ill but happens to be in a critical-care unit, or when a particular physician is only treating one of the patient’s conditions that is not considered the critical illness.4
Examples of patients who may not satisfy Medicare medical-necessity criteria, do not meet critical-care criteria, or who do not have a critical-care illness or injury and therefore are not eligible for critical-care payment:
- Patients admitted to a critical-care unit because no other hospital beds were available;
- Patients admitted to a critical-care unit for close nursing observation and/or frequent monitoring of vital signs (e.g. drug toxicity or overdose);
- Patients admitted to a critical-care unit because hospital rules require certain treatments (e.g. insulin infusions) to be administered in the critical-care unit; and
- Care of only a chronic illness in the absence of caring for a critical illness (e.g. daily management of a chronic ventilator patient; management of or care related to dialysis for an ESRD).
These circumstances would require using subsequent hospital care codes (99231-99233), initial hospital care codes (99221-99223), or hospital consultation codes (99251-99255) when applicable.3,5
Because critical-care time is a cumulative service, providers keep track of their total time throughout a single calendar day. For each date and encounter entry, the physician’s progress notes shall document the total time that critical-care services were provided (e.g. 45 minutes).4 Some payors impose the notation of “start-and-stop time” per encounter (e.g. 10 to 10:45 a.m.).
Code This Case
Consider the following scenario: A hospitalist admits a 75-year-old patient to the ICU with acute respiratory failure. He spends 45 minutes in critical-care time. The patient’s family arrives soon thereafter to discuss the patient’s condition with a second hospitalist. The discussion lasts an additional 20 minutes, and the decision regarding the patient’s DNR status is made.
Family meetings must take place at the bedside or on the patient’s unit/floor. The patient must participate, unless they are medically unable or clinically incompetent to participate. A notation in the chart should indicate the patient’s inability to participate and the reason. Meeting time can only involve obtaining a medical history and/or discussing treatment options or the limitations of treatment. The conversation must bear directly on patient management.5,6 Meetings that take place for family grief counseling (90846, 90847, 90849) are not included in critical-care time and cannot be billed separately.
Do not count time associated with periodic condition updates to the family or answering questions about the patient’s condition that are unrelated to decision-making.
Family discussions can take place via phone as long as the physician is calling from the patient’s unit/floor and the conversation involves the same criterion identified for face-to-face family meetings.6
Critically ill patients often require the care of multiple providers.3 Payors implement code logic in their systems that allow reimbursement for 99291 once per day when reported by physicians of the same group and specialty.8 Physicians of different specialties can separately report critical-care hours. Documentation must demonstrate that care is not duplicative of other specialists and does not overlap the same time period of any other physician reporting critical-care services.
Same-specialty physicians (two hospitalists from the same group practice) bill and are paid as one physician. The initial critical-care hour (99291) must be met by a single physician. Medically necessary critical-care time beyond the first hour (99292) may be met individually by the same physician or collectively with another physician from the same group. Cumulative physician time should be reported under one provider number on a single invoice in order to prevent denials from billing 99292 independently (see “Critical-Care Services: Time Reminders,”).
When a physician and a nurse practitioner (NP) see a patient on the same calendar day, critical-care reporting is handled differently. A single unit of critical-care time cannot be split or shared between a physician and a qualified NP. One individual must meet the entire time requirement of the reported service code.
More specifically, the hospitalist must individually meet the criteria for the first critical-care hour before reporting 99291, and the NP must individually meet the criteria for an additional 30 minutes of critical care before reporting 99292. The same is true if the NP provided the initial hour while the hospitalist provided the additional critical-care time.
Payors who recognize NPs as independent billing providers (e.g. Medicare and Aetna) require a “split” invoice: an invoice for 99291 with the hospitalist NPI and an invoice for 99292 with the NP’s NPI.9 This ensures reimbursement-rate accuracy, as the physician receives 100% of the allowable rate while the NP receives 85%. If the 99292 invoice is denied due to the payor’s system edits disallowing separate invoicing of add-on codes, appeal with documentation by both the hospitalist and NP to identify the circumstances and reclaim payment.
References
- Cahaba Government Benefit Administrators LLC. Widespread prepayment targeted review notification—CPT 99291. Cahaba Government Benefit Administrators LLC website. Available at: http://www.cahabagba.com/news/widespread-prepayment-targeted-review-notification-part-b/. Accessed May 4, 2013.
- First Coast Service Options Inc. Prepayment edit of evaluation and management (E/M) code 99291. First Coast Service Options Inc. website. Available at: http://medicare.fcso.com/Medical_documentation/249650.asp. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12B. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 5, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12E. Centers for Medicare and Medicaid Services website. Available at http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 6, 2013.
- Abraham M, Ahlman J, Boudreau A, Connelly J, Levreau-Davis L. Current Procedural Terminology 2013 Professional Edition. Chicago: American Medical Association Press; 2012.
- Novitas Solutions Inc. Evaluation & management: service-specific coding instructions. Novitas Solutions Inc. website. Available at: http://www.novitas-solutions.com/em/coding.html. Accessed May 7, 2013.
- United Healthcare. Same day same service policy—adding edits. United Healthcare website. Available at: http://www.unitedhealthcareonline.com/ccmcontent/ ProviderII/ UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/News/Network_Bulletin_November _2012_Volume_52.pdf. Accessed May 7, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12I. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 10, 2013.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.12G. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed May 4, 2013.
Documentation, CMS-Approved Language Key to Getting Paid for Hospitalist Teaching Services
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
When hospitalists work in academic centers, medical and surgical services are furnished, in part, by a resident within the scope of the hospitalists’ training program. A resident is “an individual who participates in an approved graduate medical education (GME) program or a physician who is not in an approved GME program but who is authorized to practice only in a hospital setting.”1 Resident services are covered by Centers for Medicare & Medicaid Services (CMS) and paid by the Fiscal Intermediary through direct GME and Indirect Medical Education (IME) payments. These services are not billed or paid using the Medicare Physician Fee Schedule. The teaching physician is responsible for supervising the resident’s health-care delivery but is not paid for the resident’s work. The teaching physician is paid for their personal and medically necessary service in providing patient care. The teaching physician has the option to perform the entire service, or perform the self-determined critical or key portion(s) of the service.
Comprehensive Service
Teaching physicians independently see the patient and perform all required elements to support the visit level (e.g. 99233: subsequent hospital care, per day, which requires at least two of the following three key components: a detailed interval history, a detailed examination, or high-complexity medical decision-making).2 The teaching physician writes a note independent of a resident encounter with the patient or documentation. The teaching physician note “stands alone” and does not rely on the resident’s documentation. If the resident saw the patient and documented the encounter, the teaching physician might choose to “link to” the resident note in lieu of personally documenting the entire service. The linking statement must demonstrate teaching physician involvement in the patient encounter and participation in patient management. Use of CMS-approved statements is best to meet these requirements. Statement examples include:3
- “I performed a history and physical examination of the patient and discussed his management with the resident. I reviewed the resident’s note and agree with the documented findings and plan of care.”
- “I saw and evaluated the patient. I agree with the findings and the plan of care as documented in the resident’s note.”
- “I saw and examined the patient. I agree with the resident’s note, except the heart murmur is louder, so I will obtain an echo to evaluate.”
Each of these statements meets the minimum requirements for billing. However, teaching physicians should offer more information in support of other clinical, quality, and regulatory initiatives and mandates, better exemplified in the last example. The reported visit level will be supported by the combined documentation (teaching physician and resident).
The teaching physician submits a claim in their name and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99223-GC). This alerts the Medicare contractor that services were provided under teaching physician rules. Requests for documentation should include a response with medical record entries from the teaching physician and resident.
Critical/Key Portion
“Supervised” service: The resident and teaching physician can round together; they can see the patient at the same time. The teaching physician observes the resident’s performance during the patient encounter, or personally performs self-determined elements of patient care. The resident documents their patient care. The attending must still note their presence in the medical record, performance of the critical or key portions of the service, and involvement in patient management. CMS-accepted statements include:3
- “I was present with the resident during the history and exam. I discussed the case with the resident and agree with the findings and plan as documented in the resident’s note.”
- “I saw the patient with the resident and agree with the resident’s findings and plan.”
Although these statements demonstrate acceptable billing language, they lack patient-specific details that support the teaching physician’s personal contribution to patient care and the quality of their expertise. The teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99232-GC).
“Shared” service: The resident sees the patient unaccompanied and documents the corresponding care provided. The teaching physician sees the patient at a different time but performs only the critical or key portions of the service. The case is subsequently discussed with the resident. The teaching physician must document their presence and performance of the critical or key portions of the service, along with any patient management. Using CMS-quoted statements ensures regulatory compliance:3
- “I saw and evaluated the patient. I reviewed the resident’s note and agree, except that the picture is more consistent with pericarditis than myocardial ischemia. Will begin NSAIDs.”
- “I saw and evaluated the patient. Discussed with resident and agree with resident’s findings and plan as documented in the resident’s note.”
- “See resident’s note for details. I saw and evaluated the patient and agree with the resident’s finding and plans as written.”
- “I saw and evaluated the patient. Agree with resident’s note, but lower extremities are weaker, now 3/5; MRI of L/S spine today.”
Once again, the teaching physician selects the visit level that represents the combined documentation and, if it is a Medicare claim, appends modifier GC to the selected visit level (e.g. 99233-GC).
EHR Considerations
When seeing patients independent of one another, the timing of the teaching physician and resident encounters does not impact billing. However, the time that the resident encounter is documented in the medical record can significantly impact the payment when reviewed by external auditors. When the resident note is dated and timed later than the teaching physician’s entry, the teaching physician cannot consider the resident’s note for visit-level selection. The teaching physician should not “link to” a resident note that is viewed as “not having been written” prior to the teaching physician note. This would not fulfill the requirements represented in the CMS-approved language “I reviewed the resident’s note and agree.”
Electronic health record (EHR) systems sometimes hinder compliance. If the resident completes the note but does not “finalize” or “close” the encounter until after the teaching physician documents their own note, it can falsely appear that the resident note did not exist at the time the teaching physician created their entry. Because an auditor can only view the finalized entries, the timing of each entry might be erroneously represented. Proper training and closing of encounters can diminish these issues.
Additionally, scribing the attestation is not permitted. Residents cannot document the teaching physician attestation on behalf of the physician under any circumstance. CMS rules require the teaching physician to document their presence, participation, and management of the patient. In an EHR, the teaching physician must document this entry under his/her own log-in and password, which is not to be shared with anyone.
Students
CMS defines student as “an individual who participates in an accredited educational program [e.g. a medical school] that is not an approved GME program.”1 A student is not regarded as a “physician in training,” and the service is not eligible for reimbursement consideration under the teaching physician rules.
Per CMS guidelines, students can document services in the medical record, but the teaching physician may only refer to the student’s systems review and past/family/social history entries. The teaching physician must verify and redocument the history of present illness. A student’s physical exam findings or medical decision-making are not suitable for tethering, and the teaching physician must personally perform and redocument the physical exam and medical decision-making. The visit level reflects only the teaching physician’s personally performed and documented service.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare and Medicaid Services. Guidelines for Teaching Physicians, Interns, Residents. CMS website. Available at: http://www.cms.gov/MLNProducts/downloads/gdelinesteachgresfctsht.pdf. Accessed Jan. 8, 2013.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare and Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 100. CMS website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan. 8, 2013.
- Centers for Medicare and Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 30.2. CMS website. Available at: http://www.cms.hhs.gov/manuals/Downloads/bp102c15.pdf. Accessed Jan. 8, 2013.
Medicare Billing Regulations for Nonphysician Providers Vary by State, Facility
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Nurse practitioners (NPs) and physician assistants (PAs), referred to as nonphysician providers (NPPs) in billing policy, provide many different services in the hospital setting. Roles include:
- Rounding independently and following patients of varying acuity with physician supervision. The NPP may ask the physician to see the patient, as necessary, if a change in the patient’s condition arises and warrants physician evaluation.
- Providing prompt consultative
- services when the physician is not
- readily available.
- Rounding alongside the physician and expediting the work of admission services through a combined effort.
Hospitalist programs may elect one model over another, or utilize NPPs according to existing need and shifting census. Employers must be aware of state and federal regulations, facility-imposed standards of care, and billing requirements surrounding NPP services.
Medicare Enrollment and Billing Eligibility
Certified PAs and NPs may provide covered services to Medicare beneficiaries in accordance with their state scope of practice under state law and corresponding supervision/collaboration requirements. They can submit claims for these services, providing they meet enrollment qualifications.1
PAs must have:
- Graduated from a PA educational program accredited by the Accreditation Review Commission on Education for the Physician Assistant (or its predecessor agencies, the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Committee on Allied Health Education and Accreditation (CAHEA); or
- Passed the national certification examination administered by the National Commission on Certification of Physician Assistants (NCCPA); and
- A license as a PA in the practicing state.
NPs must:
- Be a registered nurse who is authorized and licensed by the state to practice as a nurse practitioner by Dec. 31, 2000; or
- After Jan. 1, 2001, be a registered nurse who is authorized and licensed by the state to practice as an NP and be certified by a recognized national certifying body that has established standards for NPs (e.g. American Academy of Nurse Practitioners, American Nurses Credentialing Center, AACN Certification Corp., or National Board on Certification of Hospice and Palliative Nurses); and
- Possess a master’s degree in nursing.
Independent Billing
NPPs can see patients in any setting without the presence of a physician. The physician is not required to see the patient but must be available by phone or beeper in accordance with supervisory/collaborative guidelines. Physician cosignature is not required unless mandated by state law or the facility.
NPPs document and report their services according to the Centers for Medicare & Medicaid Services (CMS) Documentation Guidelines (available at www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/EMDOC.html). The NPP should be listed as the rendering provider on the claim form. Currently, insurance programs Medicare and Aetna Inc. consistently enroll and recognize NPPs as billing providers and reimburse these services at 85% of the allowable physician rate.2
Shared/Split Billing
When two providers (a physician and NPP) from the same group (direct employment or a lease arrangement contractually linking the providers) perform a service for the same patient on the same calendar day, CMS allows the combined services to be reported under a single provider’s name.
Allowable services. NPPs are only limited by the state scope of practice under state law, and the facility rules in which the NPPs practice. Services must be performed under the appropriate level of supervision or collaboration. Medicare reimburses reasonable and necessary services not otherwise excluded from coverage.
However, shared/split rules restrict the services reported under this billing model, recognizing only evaluation and management (E/M) services (and not procedures) provided in the ED, outpatient hospital clinics, or inpatient hospital (i.e. facility-based services). Shared/split rules do not involve all types of E/M services. For hospitalist programs, critical-care services (99291-99292) are excluded.3
Physician requirement. Shared/split rules require a face-to-face patient encounter by each provider on the same calendar day. There are no billing mandates requiring the NPP to see the patient before the physician does, although practice style might govern this decision.4 CMS does not specify the extent of provider involvement, but it could be established by local Medicare contractor requirements. Some contractors reference physician participation as a “substantive” service without further elaboration on specific parameters. Therefore, the physician determines the critical or key portion of his/her personal service. Minimalistic documentation can be problematic for quality or medicolegal aspects of patient care, and physicians might benefit from a more detailed notation of participation.
Documentation. Physician documentation must include an attestation that supports the physician encounter (e.g. “Patient seen and examined by me”), the individual with whom the service is shared (e.g. “Agree with note by X”), their portion of the rendered service (e.g. “Pulse oximetry 94% on room air. Audible rhonchi at bilateral lung bases. Start O2 2L nasal cannula. Obtain CXR”), the date, and a legible signature. NPP documentation should include as similar reference to the physician with whom the service is being shared for better charge capture. It alerts coders, auditors, and payor representatives to consider both notes in support of the billed service and ensures that the correct notes are sent to the payor in the event of claim denial and subsequent appeal.
Although the visit level is supported by both provider services, only one claim may be submitted for a shared/split service. The rendering provider listed on the claim can be the physician (reimbursed at 100% of the Medicare allowable physician rate) or the NPP (reimbursed at 85% of the allowable physician rate).
Non-Medicare Claims
Shared/split billing policy only applies to Medicare beneficiaries, while independent billing policy applies to Medicare and Aetna. Excessive costs prevent most other non-Medicare insurers from credentialing and enrollment NPPs. Absence of payor policy does not disqualify reimbursement for shared services, but it does require additional measures to establish recognition of NPP services and a corresponding reimbursement model.
After determining payor mix, develop a reasonable guideline for those payors who do not enroll NPPs. Delineate, in writing, a predetermined time frame for guideline implementation unless the payor can provide an alternate billing option. Some experts suggest physician groups outline the following key issues when structuring a billing option5:
- Type of NPPs involved in patient care;
- Category of services provided;
- Service location(s);
- Physician involvement;
- Mechanism for reporting services; and
- Documentation requirements.
Guidelines can be developed for any of the billing options (independent, “incident-to,” shared/split). Be sure to obtain written payor response before initiating the billing process.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Benefit Policy Manual: Chapter 15, Section 190-200. Centers for Medicare & Medicaid website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c15.pdf. Accessed Nov. 5, 2012.
- Aetna Inc. Aetna office links updates. Reminder: Reimbursement change for mid-level practitioners. Aetna Inc. website. Available at www.aetna.com/provider/data/OLU_MA_JUN2010_final.pdf. Accessed Nov. 6, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 30.6.1B. Centers for Medicare & Medicaid website. Available at: http://www.cms.hhs.gov/manuals/downloads/clm104c12.pdf. Accessed Jan 21, 2013.
- Pohlig, C. Nonphysician Providers in Your Practice. In: Coding for Chest Medicine 2011. Northbrook, Ill.: American College of Chest Physicians, 2010.
Host of Factors Play Into Hospitalist Billing for Patient Transfers
Patient Transfers
Hospitalist billing depends on several factors. Know your role and avoid common mistakes Patient transfers can occur for many reasons: advanced technological services required, health insurance coverage, or a change in the level of care, to name a few. Patient care that is provided in the acute-care setting does not always terminate with discharge to home. Frequently, hospitalists are involved in patient transfers to another location to receive additional services: intrafacility (a different unit or related facility within the same physical plant) or interfacility (geographically separate facilities). The hospitalist must identify his or her role in the transfer and the patient’s new environment.
Physician billing in the transferred setting depends upon several factors:1
- Shared or merged medical record;
- The attending of record in each setting;
- The requirements for care rendered by the hospitalist in each setting; and
- Service dates.
Intrafacility Initial Service
Let’s examine a common example: A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for an 83-year-old female with hypertension and diabetes who sustained a left hip fracture. The hospitalist plans to discharge the patient to the rehabilitation unit. After transfer, the rehabilitation physician becomes the attending of record, and the hospitalist might be asked to provide ongoing care for the patient’s hypertension and diabetes.
What should the hospitalist report for the initial post-transfer service? The typical options to consider are:2
- Inpatient consultation (99251-99255);
- Initial hospital care (99221-99223); and
- Subsequent hospital care (99231-99233).
Report a consultation only if the rehab attending requests an opinion or advice for an unrelated, new condition instead of previously treated conditions, and the requesting physician’s intent is for opinion or advice on management options rather than the a priori intent for the hospitalist to assume the patient’s medical care. If these requirements are met, the hospitalist may report an inpatient consultation code (99251-99255). Alternatively, if the intent or need represents a continuity of medical care provided during the acute episode of care, report the most appropriate subsequent hospital care code (99231-99233) for the hospitalist’s initial rehab visit and all follow-up services.
Initial hospital care (99221-99223) codes can only be reported for Medicare beneficiaries in place of consultation codes (99251-99255), as Medicare ceased to reimburse consultation codes.3 Most other payors who do not recognize consultation services only allow one initial hospital care code per hospitalization, reserved for the attending of record.
Interfacility Initial Service
Hospitalist groups provide patient care and coverage in many different types of facilities. Confusion often arises when the “attending of record” during acute care and the “subacute” setting (e.g. long-term acute-care hospital) are two different hospitalists from the same group practice. The hospitalist receiving the patient in the transfer facility may decide to report subsequent hospital care (99231-99233), because the group has been providing ongoing care to this patient. In this scenario, the hospitalist group could be losing revenue if an admission service (99221-99223) was not reported.
An initial hospital care service (99221-99223) is permitted when the transfer is between:
- Different hospitals;
- Different facilities under common ownership which do not have merged records; or
- Between the acute-care hospital and a PPS (prospective payment system)-exempt unit within the same hospital when there are no merged records (e.g. Medicare Part A-covered inpatient care in psychiatric, rehabilitation, critical access, and long-term care hospitals).4
In all other transfer circumstances not meeting the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Do not equate “merged records” to commonly accessible charts via an electronic medical record system or an electronic storage system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
Billing Two Services on Day of Transfer
Whether the transfer is classified as intrafacility or interfacility, an individual hospitalist or two separate hospitalists from the same group practice may provide the acute-care discharge and the transfer admission. A hospital discharge day management service (99238-99239) and an initial hospital care service (99221-99223) can only be reported if they do not occur on the same day.1 Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician; if more than one evaluation and management (face to face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported.5
The Exception
CMS will allow a single hospitalist or two hospitalists from the same group practice to report a discharge day management service on the same day as an admission service. When they are billed by the same physician or group with the same date of service, contractors are instructed to pay the hospital discharge day management code (99238-99239) in addition to a nursing facility admission code (99304-99306).6
Conversely, if the patient is admitted to a hospital (99221-99223) following a nursing facility discharge (99315-99316) on the same date by the same physician/group, insurers will only reimburse the initial hospital care code. Payment for the initial hospital care service includes all work performed by the physician/group in all sites of service on that date.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References available online at the-hospitalist.org
Patient Transfers
Hospitalist billing depends on several factors. Know your role and avoid common mistakes Patient transfers can occur for many reasons: advanced technological services required, health insurance coverage, or a change in the level of care, to name a few. Patient care that is provided in the acute-care setting does not always terminate with discharge to home. Frequently, hospitalists are involved in patient transfers to another location to receive additional services: intrafacility (a different unit or related facility within the same physical plant) or interfacility (geographically separate facilities). The hospitalist must identify his or her role in the transfer and the patient’s new environment.
Physician billing in the transferred setting depends upon several factors:1
- Shared or merged medical record;
- The attending of record in each setting;
- The requirements for care rendered by the hospitalist in each setting; and
- Service dates.
Intrafacility Initial Service
Let’s examine a common example: A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for an 83-year-old female with hypertension and diabetes who sustained a left hip fracture. The hospitalist plans to discharge the patient to the rehabilitation unit. After transfer, the rehabilitation physician becomes the attending of record, and the hospitalist might be asked to provide ongoing care for the patient’s hypertension and diabetes.
What should the hospitalist report for the initial post-transfer service? The typical options to consider are:2
- Inpatient consultation (99251-99255);
- Initial hospital care (99221-99223); and
- Subsequent hospital care (99231-99233).
Report a consultation only if the rehab attending requests an opinion or advice for an unrelated, new condition instead of previously treated conditions, and the requesting physician’s intent is for opinion or advice on management options rather than the a priori intent for the hospitalist to assume the patient’s medical care. If these requirements are met, the hospitalist may report an inpatient consultation code (99251-99255). Alternatively, if the intent or need represents a continuity of medical care provided during the acute episode of care, report the most appropriate subsequent hospital care code (99231-99233) for the hospitalist’s initial rehab visit and all follow-up services.
Initial hospital care (99221-99223) codes can only be reported for Medicare beneficiaries in place of consultation codes (99251-99255), as Medicare ceased to reimburse consultation codes.3 Most other payors who do not recognize consultation services only allow one initial hospital care code per hospitalization, reserved for the attending of record.
Interfacility Initial Service
Hospitalist groups provide patient care and coverage in many different types of facilities. Confusion often arises when the “attending of record” during acute care and the “subacute” setting (e.g. long-term acute-care hospital) are two different hospitalists from the same group practice. The hospitalist receiving the patient in the transfer facility may decide to report subsequent hospital care (99231-99233), because the group has been providing ongoing care to this patient. In this scenario, the hospitalist group could be losing revenue if an admission service (99221-99223) was not reported.
An initial hospital care service (99221-99223) is permitted when the transfer is between:
- Different hospitals;
- Different facilities under common ownership which do not have merged records; or
- Between the acute-care hospital and a PPS (prospective payment system)-exempt unit within the same hospital when there are no merged records (e.g. Medicare Part A-covered inpatient care in psychiatric, rehabilitation, critical access, and long-term care hospitals).4
In all other transfer circumstances not meeting the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Do not equate “merged records” to commonly accessible charts via an electronic medical record system or an electronic storage system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
Billing Two Services on Day of Transfer
Whether the transfer is classified as intrafacility or interfacility, an individual hospitalist or two separate hospitalists from the same group practice may provide the acute-care discharge and the transfer admission. A hospital discharge day management service (99238-99239) and an initial hospital care service (99221-99223) can only be reported if they do not occur on the same day.1 Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician; if more than one evaluation and management (face to face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported.5
The Exception
CMS will allow a single hospitalist or two hospitalists from the same group practice to report a discharge day management service on the same day as an admission service. When they are billed by the same physician or group with the same date of service, contractors are instructed to pay the hospital discharge day management code (99238-99239) in addition to a nursing facility admission code (99304-99306).6
Conversely, if the patient is admitted to a hospital (99221-99223) following a nursing facility discharge (99315-99316) on the same date by the same physician/group, insurers will only reimburse the initial hospital care code. Payment for the initial hospital care service includes all work performed by the physician/group in all sites of service on that date.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References available online at the-hospitalist.org
Patient Transfers
Hospitalist billing depends on several factors. Know your role and avoid common mistakes Patient transfers can occur for many reasons: advanced technological services required, health insurance coverage, or a change in the level of care, to name a few. Patient care that is provided in the acute-care setting does not always terminate with discharge to home. Frequently, hospitalists are involved in patient transfers to another location to receive additional services: intrafacility (a different unit or related facility within the same physical plant) or interfacility (geographically separate facilities). The hospitalist must identify his or her role in the transfer and the patient’s new environment.
Physician billing in the transferred setting depends upon several factors:1
- Shared or merged medical record;
- The attending of record in each setting;
- The requirements for care rendered by the hospitalist in each setting; and
- Service dates.
Intrafacility Initial Service
Let’s examine a common example: A hospitalist serves as the “attending of record” in an inpatient hospital where acute care is required for an 83-year-old female with hypertension and diabetes who sustained a left hip fracture. The hospitalist plans to discharge the patient to the rehabilitation unit. After transfer, the rehabilitation physician becomes the attending of record, and the hospitalist might be asked to provide ongoing care for the patient’s hypertension and diabetes.
What should the hospitalist report for the initial post-transfer service? The typical options to consider are:2
- Inpatient consultation (99251-99255);
- Initial hospital care (99221-99223); and
- Subsequent hospital care (99231-99233).
Report a consultation only if the rehab attending requests an opinion or advice for an unrelated, new condition instead of previously treated conditions, and the requesting physician’s intent is for opinion or advice on management options rather than the a priori intent for the hospitalist to assume the patient’s medical care. If these requirements are met, the hospitalist may report an inpatient consultation code (99251-99255). Alternatively, if the intent or need represents a continuity of medical care provided during the acute episode of care, report the most appropriate subsequent hospital care code (99231-99233) for the hospitalist’s initial rehab visit and all follow-up services.
Initial hospital care (99221-99223) codes can only be reported for Medicare beneficiaries in place of consultation codes (99251-99255), as Medicare ceased to reimburse consultation codes.3 Most other payors who do not recognize consultation services only allow one initial hospital care code per hospitalization, reserved for the attending of record.
Interfacility Initial Service
Hospitalist groups provide patient care and coverage in many different types of facilities. Confusion often arises when the “attending of record” during acute care and the “subacute” setting (e.g. long-term acute-care hospital) are two different hospitalists from the same group practice. The hospitalist receiving the patient in the transfer facility may decide to report subsequent hospital care (99231-99233), because the group has been providing ongoing care to this patient. In this scenario, the hospitalist group could be losing revenue if an admission service (99221-99223) was not reported.
An initial hospital care service (99221-99223) is permitted when the transfer is between:
- Different hospitals;
- Different facilities under common ownership which do not have merged records; or
- Between the acute-care hospital and a PPS (prospective payment system)-exempt unit within the same hospital when there are no merged records (e.g. Medicare Part A-covered inpatient care in psychiatric, rehabilitation, critical access, and long-term care hospitals).4
In all other transfer circumstances not meeting the elements noted above, the physician should bill only the appropriate level of subsequent hospital care (99231-99233) for the date of transfer.1 Do not equate “merged records” to commonly accessible charts via an electronic medical record system or an electronic storage system. If the medical record for the patient’s acute stay is “closed” and the patient is given a separate medical record and registration for the stay in the transferred facility, consider the transfer stay as a separate admission.
Billing Two Services on Day of Transfer
Whether the transfer is classified as intrafacility or interfacility, an individual hospitalist or two separate hospitalists from the same group practice may provide the acute-care discharge and the transfer admission. A hospital discharge day management service (99238-99239) and an initial hospital care service (99221-99223) can only be reported if they do not occur on the same day.1 Physicians in the same group practice who are in the same specialty must bill and be paid as though they were a single physician; if more than one evaluation and management (face to face) service is provided on the same day to the same patient by the same physician or more than one physician in the same specialty in the same group, only one evaluation and management service may be reported.5
The Exception
CMS will allow a single hospitalist or two hospitalists from the same group practice to report a discharge day management service on the same day as an admission service. When they are billed by the same physician or group with the same date of service, contractors are instructed to pay the hospital discharge day management code (99238-99239) in addition to a nursing facility admission code (99304-99306).6
Conversely, if the patient is admitted to a hospital (99221-99223) following a nursing facility discharge (99315-99316) on the same date by the same physician/group, insurers will only reimburse the initial hospital care code. Payment for the initial hospital care service includes all work performed by the physician/group in all sites of service on that date.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References available online at the-hospitalist.org
Medical Coding: Hospice Care vs. Palliative Care
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Response: Properly Coding an Uncertain Diagnosis
Dr. Pinson:
Thank you for your inquiry to my June column, which outlined physician reporting of ICD-9-CM diagnoses. Confusion arises because there are two mechanisms for reporting facility-based claims: the professional (physician) bill and the facility bill. ICD-9-CM has been adopted under HIPAA for all healthcare settings. Several components of the ICD-9-CM manual offer instructions on its use. “How to Use the ICD-9-CM for Physicians (Volumes 1&2)” identifies “10 Steps to Correct Coding.”2,3 Step 1 explicitly denotes the inability to use “rule out,” “suspected,” “probable,” or “questionable” diagnoses, and applies to all professional claims submitted on CMS1500 or electronic equivalent.3
The “ICD-9-CM Official Guidelines for Coding and Reporting” are a set of rules developed to accompany and complement the official conventions and instructions provided within ICD-9-CM and approved by the four organizations that make up the Cooperating Parties for the ICD-9-CM: the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), the Centers for Medicare & Medicaid Services (CMS), and NCHS. These guidelines are included on the official government version of the ICD-9-CM, and also appear in “Coding Clinic for ICD-9-CM” published by the AHA.3
While Section I of these guidelines applies to all locations, Sections II and III refer to the selection of the principal diagnosis (the condition established after study to be chiefly responsible for the admission) reported by facilities for DRG payment on CMS1450 or its electronic equivalent.2 Since DRG payment is based on the average resources used to treat inpatients, it is allowable to code a properly documented, “uncertain” condition as if it existed or was established. It does not apply to the outpatient setting. Outpatient, facility-based (Section IV) claims follow the same standards as professional claims, which should not list any diagnosis documented as “probable,” “suspected,” “questionable,” “rule out” or “working diagnosis,” or other similar terms indicating uncertainty.
Carol Pohlig, BSN, RN, CPC, ACS, is a contributing writer to The Hospitalist.
References
- Hart AC, Stegman MS, Ford B, eds. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page vi.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual. Chapter 23, Section 10A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c23.pdf. Accessed July 24, 2012.
- Hart AC, Stegman MS, Ford B. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page 1.
Dr. Pinson:
Thank you for your inquiry to my June column, which outlined physician reporting of ICD-9-CM diagnoses. Confusion arises because there are two mechanisms for reporting facility-based claims: the professional (physician) bill and the facility bill. ICD-9-CM has been adopted under HIPAA for all healthcare settings. Several components of the ICD-9-CM manual offer instructions on its use. “How to Use the ICD-9-CM for Physicians (Volumes 1&2)” identifies “10 Steps to Correct Coding.”2,3 Step 1 explicitly denotes the inability to use “rule out,” “suspected,” “probable,” or “questionable” diagnoses, and applies to all professional claims submitted on CMS1500 or electronic equivalent.3
The “ICD-9-CM Official Guidelines for Coding and Reporting” are a set of rules developed to accompany and complement the official conventions and instructions provided within ICD-9-CM and approved by the four organizations that make up the Cooperating Parties for the ICD-9-CM: the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), the Centers for Medicare & Medicaid Services (CMS), and NCHS. These guidelines are included on the official government version of the ICD-9-CM, and also appear in “Coding Clinic for ICD-9-CM” published by the AHA.3
While Section I of these guidelines applies to all locations, Sections II and III refer to the selection of the principal diagnosis (the condition established after study to be chiefly responsible for the admission) reported by facilities for DRG payment on CMS1450 or its electronic equivalent.2 Since DRG payment is based on the average resources used to treat inpatients, it is allowable to code a properly documented, “uncertain” condition as if it existed or was established. It does not apply to the outpatient setting. Outpatient, facility-based (Section IV) claims follow the same standards as professional claims, which should not list any diagnosis documented as “probable,” “suspected,” “questionable,” “rule out” or “working diagnosis,” or other similar terms indicating uncertainty.
Carol Pohlig, BSN, RN, CPC, ACS, is a contributing writer to The Hospitalist.
References
- Hart AC, Stegman MS, Ford B, eds. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page vi.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual. Chapter 23, Section 10A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c23.pdf. Accessed July 24, 2012.
- Hart AC, Stegman MS, Ford B. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page 1.
Dr. Pinson:
Thank you for your inquiry to my June column, which outlined physician reporting of ICD-9-CM diagnoses. Confusion arises because there are two mechanisms for reporting facility-based claims: the professional (physician) bill and the facility bill. ICD-9-CM has been adopted under HIPAA for all healthcare settings. Several components of the ICD-9-CM manual offer instructions on its use. “How to Use the ICD-9-CM for Physicians (Volumes 1&2)” identifies “10 Steps to Correct Coding.”2,3 Step 1 explicitly denotes the inability to use “rule out,” “suspected,” “probable,” or “questionable” diagnoses, and applies to all professional claims submitted on CMS1500 or electronic equivalent.3
The “ICD-9-CM Official Guidelines for Coding and Reporting” are a set of rules developed to accompany and complement the official conventions and instructions provided within ICD-9-CM and approved by the four organizations that make up the Cooperating Parties for the ICD-9-CM: the American Hospital Association (AHA), the American Health Information Management Association (AHIMA), the Centers for Medicare & Medicaid Services (CMS), and NCHS. These guidelines are included on the official government version of the ICD-9-CM, and also appear in “Coding Clinic for ICD-9-CM” published by the AHA.3
While Section I of these guidelines applies to all locations, Sections II and III refer to the selection of the principal diagnosis (the condition established after study to be chiefly responsible for the admission) reported by facilities for DRG payment on CMS1450 or its electronic equivalent.2 Since DRG payment is based on the average resources used to treat inpatients, it is allowable to code a properly documented, “uncertain” condition as if it existed or was established. It does not apply to the outpatient setting. Outpatient, facility-based (Section IV) claims follow the same standards as professional claims, which should not list any diagnosis documented as “probable,” “suspected,” “questionable,” “rule out” or “working diagnosis,” or other similar terms indicating uncertainty.
Carol Pohlig, BSN, RN, CPC, ACS, is a contributing writer to The Hospitalist.
References
- Hart AC, Stegman MS, Ford B, eds. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page vi.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual. Chapter 23, Section 10A. Centers for Medicare and Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c23.pdf. Accessed July 24, 2012.
- Hart AC, Stegman MS, Ford B. ICD-9-CM for Physicians Volumes 1 & 2 2012 Expert Edition. OptimumInsight; 2011. Page 1.
Know Surgical Package Requirements before Billing Postoperative Care
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Hospitalists often are involved in the postoperative care of the surgical patient. However, HM is emerging in the admitting/attending role for procedural patients. Confusion can arise as to the nature of the hospitalist service, and whether it is deemed billable. Knowing the surgical package requirements can help hospitalists consider the issues.
Global Surgical Package Period1
Surgical procedures, categorized as major or minor surgery, are reimbursed for pre-, intra-, and postoperative care. Postoperative care varies according to the procedure’s assigned global period, which designates zero, 10, or 90 postoperative days. (Physicians can review the global period for any given CPT code in the Medicare Physician Fee Schedule, available at www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx.)
Services classified with “XXX” do not have the global period concept. “ZZZ” services denote an “add-on” procedure code that must always be reported with a primary procedure code and assumes the global period assigned to the primary procedure performed.
Major surgery allocates a 90-day global period in which the surgeon is responsible for all related surgical care one day before surgery through 90 postoperative days with no additional charge. Minor surgery, including endoscopy, appoints a zero-day or 10-day postoperative period. The zero-day global period encompasses only services provided on the surgical day, whereas 10-day global periods include services on the surgical day through 10 postoperative days.
Global Surgical Package Components2
The global surgical package comprises a host of responsibilities that include standard facility requirements of filling out all necessary paperwork involved in surgical cases (e.g. preoperative H&P, operative consent forms, preoperative orders). Additionally, the surgeon’s packaged payment includes (at no extra charge):
- Preoperative visits after making the decision for surgery beginning one day prior to surgery;
- All additional postoperative medical or surgical services provided by the surgeon related to complications but not requiring additional trips to the operating room;
- Postoperative visits by the surgeon related to recovery from surgery, including but not limited to dressing changes; local incisional care; removal of cutaneous sutures and staples; line removals; changes and removal of tracheostomy tubes; and discharge services; and
- Postoperative pain management provided by the surgeon.
- Examples of services that are not included in the global surgical package, (i.e. are separately billable and may require an appropriate modifier) are:
- The initial consultation or evaluation of the problem by the surgeon to determine the need for surgery;
- Services of other physicians except where the other physicians are providing coverage for the surgeon or agree on a transfer of care (i.e. a formal agreement in the form of a letter or an annotation in the discharge summary, hospital record, or ASC record);
- Postoperative visits by the surgeon unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery;
- Diagnostic tests and procedures, including diagnostic radiological procedures;
- Clearly distinct surgical procedures during the postoperative period that do not result in repeat operations or treatment for complications;
- Treatment for postoperative complications that requires a return trip to the operating room (OR), catheterization lab or endoscopy suite;
- Immunosuppressive therapy for organ transplants; and
- Critical-care services (CPT codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the surgeon.
Classification of “Surgeon”
For billing purposes, the “surgeon” is a qualified physician who can perform “surgical” services within their scope of practice. All physicians with the same specialty designation in the same group practice as the “surgeon” (i.e. reporting services under the same tax identification number) are considered a single entity and must adhere to the global period billing rules initiated by the “surgeon.”
Alternately, physicians with different specialty designations in the same group practice (e.g. a hospitalist and a cardiologist in a multispecialty group who report services under the same tax identification number) or different group practices can perform and separately report medically necessary services during the surgeon’s global period, as long as a formal (mutually agreed-upon) transfer of care did not occur.
Medical Necessity
With the growth of HM programs and the admission/attending role expansion, involvement in surgical cases comes under scrutiny for medical necessity. Admitting a patient who has active medical conditions (e.g. hypertension, diabetes, emphysema) is reasonable and necessary because the patient has a well-defined need for medical management by the hospitalist. Participation in the care of these patients is separately billable from the surgeon’s global period package.
Alternatively, a hospitalist might be required to admit and follow surgical patients who have no other identifiable chronic or acute conditions aside from the surgical problem. In these cases, hospitalist involvement may satisfy facility policy (quality of care, risk reduction, etc.) and administrative functions (discharge services or coordination of care) rather than active clinical management. This “medical management” will not be considered “medically necessary” by the payor, and may be denied as incidental to the surgeon’s perioperative services. Erroneous payment can occur, which will result in refund requests, as payors do not want to pay twice for duplicate services. Hospitalists can attempt to negotiate other terms with facilities to account for the unpaid time and effort directed toward these types of cases.
Consider the Case
A patient with numerous medical comorbidities is admitted to the hospitalist service for stabilization prior to surgery, which will occur the next day. The hospitalist can report the appropriate admission code (99221-99223) without need for modifiers because the hospitalist is the attending of record and in a different specialty group. If a private insurer denies the claim as inclusive to the surgical service, the hospitalist can appeal with notes and a cover letter, along with the Medicare guidelines for global surgical package. The hospitalist may continue to provide postoperative daily care, as needed, to manage the patient’s chronic conditions, and report each service as subsequent hospital care (99231-99233) without modifier until the day of discharge (99238-99239). Again, if a payor issues a denial (inclusive to surgery), appealing with notes might be necessary.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 12, Section 40. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c12.pdf. Accessed May 5, 2012.
- Centers for Medicare & Medicaid Services. ICD-10: HHS proposes one-year delay of ICD-10 compliance date. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Medicare/Coding/ICD10/index.html?redirect=/ICD10. Accessed May 5, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
Efficacy, Diagnoses, Frequency Play Parts in Coverage Limitations
Under Section 1862(a)(1)(A) of the Social Security Act, the Medicare program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).1 Coverage limitations include:2
- Proven clinical efficacy. For example, Medicare deems acupuncture “experimental/investigational” in the diagnosis or treatment of illness or injury;
- Diagnoses. As an example, vitamin B-12 injections are covered, but only for such diagnoses as pernicious anemia and dementias secondary to vitamin B-12 deficiency; and
- Frequency/utilization parameters. For example, a screening colonoscopy (G0105) can be paid once every 24 months for beneficiaries who are at high risk for colorectal cancer; otherwise the service is limited to once every 10 years.
Beyond these factors, individual consideration might be granted. Supportive and unambiguous documentation (medical records, clinical studies, etc.) must be submitted when the clinical circumstances do not appear to support the medical necessity for the service.
Diagnoses Selection
Select the code that best represents the primary reason for the service or procedure on a given date. In the absence of a definitive diagnosis, the code may correspond to a sign or symptom. Physicians never should report a code that represents a probable, suspected, or “rule out” condition. Although facility billing might consider these unconfirmed circumstances (when necessary), physician billing prohibits this practice.
Reporting services for hospitalized patients is challenging when multiple services for the same patient are provided on the same date by the same or different physician, also known as concurrent care. Each physician manages a particular aspect while still considering the patient’s overall condition; each physician should report the corresponding diagnosis for that management. If billed correctly, each physician will have a different primary diagnosis code to justify their involvement, increasing their opportunity for payment.3
The non-primary diagnoses might also be listed on the claim if appropriately addressed in the documentation (i.e. “non-primary” conditions’ indirect role in the focused management of the primary condition). For example, a hospitalist, pulmonologist, and nephrologist manage a patient’s uncontrolled diabetes (250.02), COPD exacerbation (491.21), and CRI (585.9), respectively. Each may report subsequent hospital care (99231-99233) for medically necessary concurrent care:
- Hospitalist: 250.02, 491.21, 585.9;
- Pulmonologist: 491.21, 250.02, 585.9; and
- Nephrologist: 585.9, 492.21, 250.02.
Coverage Determinations
Code comparisons can be made after diagnosis code selection. Coverage determinations identify specific conditions (i.e. ICD-9-CM codes) for which services are considered medically necessary. They also outline the frequency interval at which services can be performed, when applicable.
For example, vascular studies (e.g. CPT 93971) are indicated for the preoperative examination (ICD-9-CM V72.83) of potential harvest vein grafts prior to bypass surgery.4 This is a covered service only when the results of the study are necessary to locate suitable graft vessels. The need for bypass surgery must be determined prior to performance of the test. V72.83 is “covered” only when reported for a unilateral study, not a bilateral study (CPT 93970). Frequency parameters allow for only one preoperative scan.4
Coverage determination can occur on two levels: national and local. The Centers for Medicare & Medicaid Services (CMS) develops national coverage determinations (NCDs) through an evidence-based process, with opportunities for public participation.5 All Medicare administrative contractors must abide by NCDs without imposing further limitations or guidelines. As example, the NCD “Consultations With a Beneficiary’s Family and Associates” permits a physician to provide counseling to family members. Family counseling services are covered only when the primary purpose of such counseling is the treatment of the patient’s condition.6
Non-Medicare payors do not have to follow federal guidelines unless the member participates in a Medicare managed-care plan.
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).5 LCDs vary by state, creating an inconsistent approach to medical coverage. The vascular study guidelines listed above do not apply to all contractors. For example, Trailblazer Health Enterprises’ policy does not reference preoperative exams being limited to unilateral studies.7 (A listing of Medicare Contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.)
Other Considerations
Investigate “medical necessity” denials. Do not take them at face value. Billing personnel often assume that the physician reported an incorrect diagnosis code. Consider the service when trying to formulate a response to the denial. Procedures (surgical or diagnostic services) may be denied for an invalid diagnosis. After reviewing the documentation to ensure that it supports the diagnosis, the claim may be resubmitted with a corrected diagnosis code, when applicable. Denials for frequency limitations can only be appealed with documentation that explicitly identifies the need for the service beyond the contractor-stated parameters.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely to be diagnosis-related. More likely, when dealing with Medicare contractors, the denial is the result of a failed response to a prepayment request for documentation. Medicare typically issues a request to review documentation prior to payment for the following inpatient E/M services: 99223, 99233, 99239, and 99292.
If the documentation is not provided to the Medicare prepayment review department within the designated time frame, the claim is automatically denied with a citation of “not deemed a medical necessity.” Acknowledge this remittance remark and do not assume that the physician assigned an incorrect diagnosis code. Although this is a possibility, it is more likely due to the failed request response. Appealing these claims requires submission of documentation to the Medicare appeals department. Reimbursement is provided once supportive documentation is received.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Social Security Administration. Exclusions from coverage and Medicare as a secondary payer. Social Security Administration website. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1862.htm. Accessed March 1, 2012.
- Highmark Medicare Services. A/B Reference Manual: Chapter 6, Medical Coverage, Medical Necessity, and Medical Policy. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/refman/chapter-6.html. Accessed March 1, 2012.
- Pohlig C. Daily care conundrums. The Hospitalist. 2008;12(12):18.
- Highmark Medicare Services. LCD L27506: Non-Invasive Peripheral Venous Studies. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/policy/mac-ab/l27506-r10.html. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare Coverage Determination Process: Overview. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare National Coverage Determination Manual: Chapter 1, Part 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed March 1, 2012.
- Trailblazer Health Enterprises. LCD 2866: Non-Invasive Venous Studies. Trailblazer Health Enterprises website. Available at: http://www.trailblazerhealth.com/Tools/LCDs.aspx?ID=2866. Accessed March 1, 2012.
Under Section 1862(a)(1)(A) of the Social Security Act, the Medicare program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).1 Coverage limitations include:2
- Proven clinical efficacy. For example, Medicare deems acupuncture “experimental/investigational” in the diagnosis or treatment of illness or injury;
- Diagnoses. As an example, vitamin B-12 injections are covered, but only for such diagnoses as pernicious anemia and dementias secondary to vitamin B-12 deficiency; and
- Frequency/utilization parameters. For example, a screening colonoscopy (G0105) can be paid once every 24 months for beneficiaries who are at high risk for colorectal cancer; otherwise the service is limited to once every 10 years.
Beyond these factors, individual consideration might be granted. Supportive and unambiguous documentation (medical records, clinical studies, etc.) must be submitted when the clinical circumstances do not appear to support the medical necessity for the service.
Diagnoses Selection
Select the code that best represents the primary reason for the service or procedure on a given date. In the absence of a definitive diagnosis, the code may correspond to a sign or symptom. Physicians never should report a code that represents a probable, suspected, or “rule out” condition. Although facility billing might consider these unconfirmed circumstances (when necessary), physician billing prohibits this practice.
Reporting services for hospitalized patients is challenging when multiple services for the same patient are provided on the same date by the same or different physician, also known as concurrent care. Each physician manages a particular aspect while still considering the patient’s overall condition; each physician should report the corresponding diagnosis for that management. If billed correctly, each physician will have a different primary diagnosis code to justify their involvement, increasing their opportunity for payment.3
The non-primary diagnoses might also be listed on the claim if appropriately addressed in the documentation (i.e. “non-primary” conditions’ indirect role in the focused management of the primary condition). For example, a hospitalist, pulmonologist, and nephrologist manage a patient’s uncontrolled diabetes (250.02), COPD exacerbation (491.21), and CRI (585.9), respectively. Each may report subsequent hospital care (99231-99233) for medically necessary concurrent care:
- Hospitalist: 250.02, 491.21, 585.9;
- Pulmonologist: 491.21, 250.02, 585.9; and
- Nephrologist: 585.9, 492.21, 250.02.
Coverage Determinations
Code comparisons can be made after diagnosis code selection. Coverage determinations identify specific conditions (i.e. ICD-9-CM codes) for which services are considered medically necessary. They also outline the frequency interval at which services can be performed, when applicable.
For example, vascular studies (e.g. CPT 93971) are indicated for the preoperative examination (ICD-9-CM V72.83) of potential harvest vein grafts prior to bypass surgery.4 This is a covered service only when the results of the study are necessary to locate suitable graft vessels. The need for bypass surgery must be determined prior to performance of the test. V72.83 is “covered” only when reported for a unilateral study, not a bilateral study (CPT 93970). Frequency parameters allow for only one preoperative scan.4
Coverage determination can occur on two levels: national and local. The Centers for Medicare & Medicaid Services (CMS) develops national coverage determinations (NCDs) through an evidence-based process, with opportunities for public participation.5 All Medicare administrative contractors must abide by NCDs without imposing further limitations or guidelines. As example, the NCD “Consultations With a Beneficiary’s Family and Associates” permits a physician to provide counseling to family members. Family counseling services are covered only when the primary purpose of such counseling is the treatment of the patient’s condition.6
Non-Medicare payors do not have to follow federal guidelines unless the member participates in a Medicare managed-care plan.
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).5 LCDs vary by state, creating an inconsistent approach to medical coverage. The vascular study guidelines listed above do not apply to all contractors. For example, Trailblazer Health Enterprises’ policy does not reference preoperative exams being limited to unilateral studies.7 (A listing of Medicare Contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.)
Other Considerations
Investigate “medical necessity” denials. Do not take them at face value. Billing personnel often assume that the physician reported an incorrect diagnosis code. Consider the service when trying to formulate a response to the denial. Procedures (surgical or diagnostic services) may be denied for an invalid diagnosis. After reviewing the documentation to ensure that it supports the diagnosis, the claim may be resubmitted with a corrected diagnosis code, when applicable. Denials for frequency limitations can only be appealed with documentation that explicitly identifies the need for the service beyond the contractor-stated parameters.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely to be diagnosis-related. More likely, when dealing with Medicare contractors, the denial is the result of a failed response to a prepayment request for documentation. Medicare typically issues a request to review documentation prior to payment for the following inpatient E/M services: 99223, 99233, 99239, and 99292.
If the documentation is not provided to the Medicare prepayment review department within the designated time frame, the claim is automatically denied with a citation of “not deemed a medical necessity.” Acknowledge this remittance remark and do not assume that the physician assigned an incorrect diagnosis code. Although this is a possibility, it is more likely due to the failed request response. Appealing these claims requires submission of documentation to the Medicare appeals department. Reimbursement is provided once supportive documentation is received.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Social Security Administration. Exclusions from coverage and Medicare as a secondary payer. Social Security Administration website. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1862.htm. Accessed March 1, 2012.
- Highmark Medicare Services. A/B Reference Manual: Chapter 6, Medical Coverage, Medical Necessity, and Medical Policy. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/refman/chapter-6.html. Accessed March 1, 2012.
- Pohlig C. Daily care conundrums. The Hospitalist. 2008;12(12):18.
- Highmark Medicare Services. LCD L27506: Non-Invasive Peripheral Venous Studies. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/policy/mac-ab/l27506-r10.html. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare Coverage Determination Process: Overview. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare National Coverage Determination Manual: Chapter 1, Part 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed March 1, 2012.
- Trailblazer Health Enterprises. LCD 2866: Non-Invasive Venous Studies. Trailblazer Health Enterprises website. Available at: http://www.trailblazerhealth.com/Tools/LCDs.aspx?ID=2866. Accessed March 1, 2012.
Under Section 1862(a)(1)(A) of the Social Security Act, the Medicare program may only pay for items and services that are “reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member,” unless there is another statutory authorization for payment (e.g. colorectal cancer screening).1 Coverage limitations include:2
- Proven clinical efficacy. For example, Medicare deems acupuncture “experimental/investigational” in the diagnosis or treatment of illness or injury;
- Diagnoses. As an example, vitamin B-12 injections are covered, but only for such diagnoses as pernicious anemia and dementias secondary to vitamin B-12 deficiency; and
- Frequency/utilization parameters. For example, a screening colonoscopy (G0105) can be paid once every 24 months for beneficiaries who are at high risk for colorectal cancer; otherwise the service is limited to once every 10 years.
Beyond these factors, individual consideration might be granted. Supportive and unambiguous documentation (medical records, clinical studies, etc.) must be submitted when the clinical circumstances do not appear to support the medical necessity for the service.
Diagnoses Selection
Select the code that best represents the primary reason for the service or procedure on a given date. In the absence of a definitive diagnosis, the code may correspond to a sign or symptom. Physicians never should report a code that represents a probable, suspected, or “rule out” condition. Although facility billing might consider these unconfirmed circumstances (when necessary), physician billing prohibits this practice.
Reporting services for hospitalized patients is challenging when multiple services for the same patient are provided on the same date by the same or different physician, also known as concurrent care. Each physician manages a particular aspect while still considering the patient’s overall condition; each physician should report the corresponding diagnosis for that management. If billed correctly, each physician will have a different primary diagnosis code to justify their involvement, increasing their opportunity for payment.3
The non-primary diagnoses might also be listed on the claim if appropriately addressed in the documentation (i.e. “non-primary” conditions’ indirect role in the focused management of the primary condition). For example, a hospitalist, pulmonologist, and nephrologist manage a patient’s uncontrolled diabetes (250.02), COPD exacerbation (491.21), and CRI (585.9), respectively. Each may report subsequent hospital care (99231-99233) for medically necessary concurrent care:
- Hospitalist: 250.02, 491.21, 585.9;
- Pulmonologist: 491.21, 250.02, 585.9; and
- Nephrologist: 585.9, 492.21, 250.02.
Coverage Determinations
Code comparisons can be made after diagnosis code selection. Coverage determinations identify specific conditions (i.e. ICD-9-CM codes) for which services are considered medically necessary. They also outline the frequency interval at which services can be performed, when applicable.
For example, vascular studies (e.g. CPT 93971) are indicated for the preoperative examination (ICD-9-CM V72.83) of potential harvest vein grafts prior to bypass surgery.4 This is a covered service only when the results of the study are necessary to locate suitable graft vessels. The need for bypass surgery must be determined prior to performance of the test. V72.83 is “covered” only when reported for a unilateral study, not a bilateral study (CPT 93970). Frequency parameters allow for only one preoperative scan.4
Coverage determination can occur on two levels: national and local. The Centers for Medicare & Medicaid Services (CMS) develops national coverage determinations (NCDs) through an evidence-based process, with opportunities for public participation.5 All Medicare administrative contractors must abide by NCDs without imposing further limitations or guidelines. As example, the NCD “Consultations With a Beneficiary’s Family and Associates” permits a physician to provide counseling to family members. Family counseling services are covered only when the primary purpose of such counseling is the treatment of the patient’s condition.6
Non-Medicare payors do not have to follow federal guidelines unless the member participates in a Medicare managed-care plan.
In the absence of a national coverage policy, an item or service may be covered at the discretion of the Medicare contractors based on a local coverage determination (LCD).5 LCDs vary by state, creating an inconsistent approach to medical coverage. The vascular study guidelines listed above do not apply to all contractors. For example, Trailblazer Health Enterprises’ policy does not reference preoperative exams being limited to unilateral studies.7 (A listing of Medicare Contractor LCDs can be found at www.cms.hhs.gov/DeterminationProcess/04_LCDs.asp.)
Other Considerations
Investigate “medical necessity” denials. Do not take them at face value. Billing personnel often assume that the physician reported an incorrect diagnosis code. Consider the service when trying to formulate a response to the denial. Procedures (surgical or diagnostic services) may be denied for an invalid diagnosis. After reviewing the documentation to ensure that it supports the diagnosis, the claim may be resubmitted with a corrected diagnosis code, when applicable. Denials for frequency limitations can only be appealed with documentation that explicitly identifies the need for the service beyond the contractor-stated parameters.
If the “medical necessity” denial involves a covered evaluation and management (E/M) visit, it is less likely to be diagnosis-related. More likely, when dealing with Medicare contractors, the denial is the result of a failed response to a prepayment request for documentation. Medicare typically issues a request to review documentation prior to payment for the following inpatient E/M services: 99223, 99233, 99239, and 99292.
If the documentation is not provided to the Medicare prepayment review department within the designated time frame, the claim is automatically denied with a citation of “not deemed a medical necessity.” Acknowledge this remittance remark and do not assume that the physician assigned an incorrect diagnosis code. Although this is a possibility, it is more likely due to the failed request response. Appealing these claims requires submission of documentation to the Medicare appeals department. Reimbursement is provided once supportive documentation is received.
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is faculty for SHM’s inpatient coding course.
References
- Social Security Administration. Exclusions from coverage and Medicare as a secondary payer. Social Security Administration website. Available at: http://www.ssa.gov/OP_Home/ssact/title18/1862.htm. Accessed March 1, 2012.
- Highmark Medicare Services. A/B Reference Manual: Chapter 6, Medical Coverage, Medical Necessity, and Medical Policy. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/refman/chapter-6.html. Accessed March 1, 2012.
- Pohlig C. Daily care conundrums. The Hospitalist. 2008;12(12):18.
- Highmark Medicare Services. LCD L27506: Non-Invasive Peripheral Venous Studies. Highmark Medicare Services website. Available at: http://www.highmarkmedicareservices.com/policy/mac-ab/l27506-r10.html. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare Coverage Determination Process: Overview. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.hhs.gov/DeterminationProcess/01_Overview.asp#TopOfPage. Accessed March 1, 2012.
- Centers for Medicare & Medicaid Services. Medicare National Coverage Determination Manual: Chapter 1, Part 1, Section 70.1. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/manuals/downloads/ncd103c1_Part1.pdf. Accessed March 1, 2012.
- Trailblazer Health Enterprises. LCD 2866: Non-Invasive Venous Studies. Trailblazer Health Enterprises website. Available at: http://www.trailblazerhealth.com/Tools/LCDs.aspx?ID=2866. Accessed March 1, 2012.
HHS Delays ICD-10 Compliance Date
According to a CMS statement regarding part of President Obama’s “commitment to reducing regulatory burden,” Health and Human Services Secretary Kathleen G. Sebelius announced that HHS will initiate a process to “postpone the date” by which certain healthcare entities have to comply with International Classification of Diseases, 10th Edition diagnosis and procedure codes (ICD-10).1
The final rule adopting ICD-10 as a standard was published in January 2009; it set a compliance date of Oct. 1, 2013 (a two-year delay from the 2008 proposed rule). HHS will announce a new compliance date moving forward.
“ICD-10 codes are important to many positive improvements in our healthcare system,” Sebelius said in the statement. “We have heard from many in the provider community who have concerns about the administrative burdens they face in the years ahead. We are committing to work with the provider community to re-examine the pace at which HHS and the nation implement these important improvements to our healthcare system.”
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the exchange of our healthcare data with that of the rest of the world, much of which has long been using ICD-10. Entities covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to use the ICD-10 diagnostic and procedure codes.
All that said, do not postpone any activities toward ICD-10 implementation until further clarification comes from CMS.
—Carol Pohlig
Reference
According to a CMS statement regarding part of President Obama’s “commitment to reducing regulatory burden,” Health and Human Services Secretary Kathleen G. Sebelius announced that HHS will initiate a process to “postpone the date” by which certain healthcare entities have to comply with International Classification of Diseases, 10th Edition diagnosis and procedure codes (ICD-10).1
The final rule adopting ICD-10 as a standard was published in January 2009; it set a compliance date of Oct. 1, 2013 (a two-year delay from the 2008 proposed rule). HHS will announce a new compliance date moving forward.
“ICD-10 codes are important to many positive improvements in our healthcare system,” Sebelius said in the statement. “We have heard from many in the provider community who have concerns about the administrative burdens they face in the years ahead. We are committing to work with the provider community to re-examine the pace at which HHS and the nation implement these important improvements to our healthcare system.”
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the exchange of our healthcare data with that of the rest of the world, much of which has long been using ICD-10. Entities covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to use the ICD-10 diagnostic and procedure codes.
All that said, do not postpone any activities toward ICD-10 implementation until further clarification comes from CMS.
—Carol Pohlig
Reference
According to a CMS statement regarding part of President Obama’s “commitment to reducing regulatory burden,” Health and Human Services Secretary Kathleen G. Sebelius announced that HHS will initiate a process to “postpone the date” by which certain healthcare entities have to comply with International Classification of Diseases, 10th Edition diagnosis and procedure codes (ICD-10).1
The final rule adopting ICD-10 as a standard was published in January 2009; it set a compliance date of Oct. 1, 2013 (a two-year delay from the 2008 proposed rule). HHS will announce a new compliance date moving forward.
“ICD-10 codes are important to many positive improvements in our healthcare system,” Sebelius said in the statement. “We have heard from many in the provider community who have concerns about the administrative burdens they face in the years ahead. We are committing to work with the provider community to re-examine the pace at which HHS and the nation implement these important improvements to our healthcare system.”
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the exchange of our healthcare data with that of the rest of the world, much of which has long been using ICD-10. Entities covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to use the ICD-10 diagnostic and procedure codes.
All that said, do not postpone any activities toward ICD-10 implementation until further clarification comes from CMS.
—Carol Pohlig