User login
Adhesive Tape to Guide Injection Depth of Botulinum Toxin for Axillary Hyperhidrosis
Practice Gap
OnabotulinumtoxinA is a US Food and Drug Administration–approved second-line treatment of axillary hyperhidrosis, with a long-term success rate greater than 80% and minimal adverse effects.1 The recommended depth and angle of injection of onabotulinumtoxinA for most cases of primary hyperhidrosis is 2 to 3 mm at a 45° angle to the skin surface.2 This small depth is difficult to accurately estimate once the needle tip is in the skin.
Injection Technique
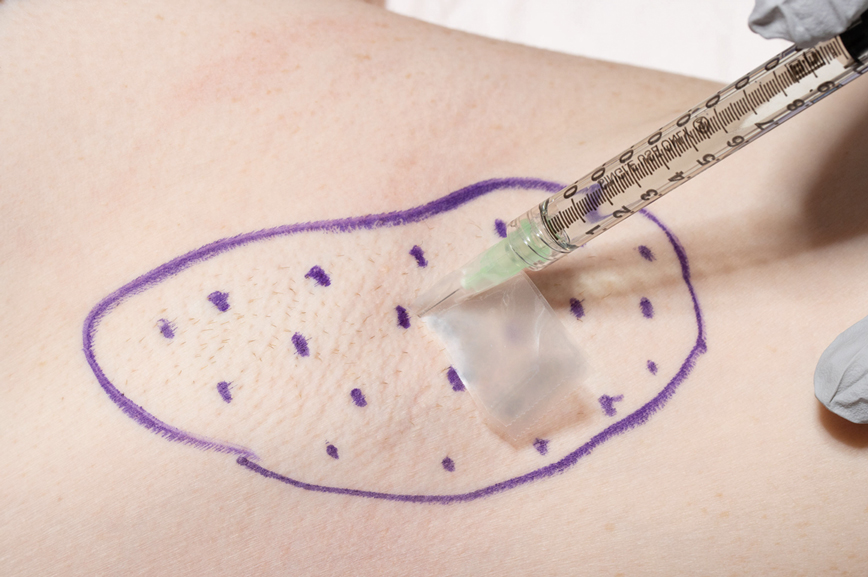
We have found that measuring 2 to 3 mm on the needle tip and then wrapping a piece of adhesive tape at that point acts as a depth guide (Figure 1). The flag shape of the tape acts as a physical barrier to prevent the needle tip from penetrating too deeply (Figure 2). This barrier also allows the injector to inject quickly to reduce the amount of pain that the patient experiences.
Practice Implications
Applying adhesive tape to a needle tip at a premeasured distance is a fast, inexpensive, and effective tool to aid accurate depth of injection for both experienced clinicians and clinicians in-training. The tape is a common office supply and the amount of tape used for a patient costs a fraction of a cent. Additionally, applying the tape takes less than 1 minute. This technique is useful for axillary hyperhidrosis injection (Figures 1 and 2) but could be used in palmar and plantar hyperhidrosis injections as well as injections other than onabotulinumtoxinA that require a specific fixed depth.
- Naumann M, Lowe NJ, Kumar CR, et al; Hyperhidrosis Clinical Investigators Group. Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003;139:731-736. doi:10.1001/archderm.139.6.731
- Botox. Prescribing information. Allergan Pharmaceuticals Ireland;2011. Accessed May 12, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/103000s5236lbl.pdf
Practice Gap
OnabotulinumtoxinA is a US Food and Drug Administration–approved second-line treatment of axillary hyperhidrosis, with a long-term success rate greater than 80% and minimal adverse effects.1 The recommended depth and angle of injection of onabotulinumtoxinA for most cases of primary hyperhidrosis is 2 to 3 mm at a 45° angle to the skin surface.2 This small depth is difficult to accurately estimate once the needle tip is in the skin.
Injection Technique
We have found that measuring 2 to 3 mm on the needle tip and then wrapping a piece of adhesive tape at that point acts as a depth guide (Figure 1). The flag shape of the tape acts as a physical barrier to prevent the needle tip from penetrating too deeply (Figure 2). This barrier also allows the injector to inject quickly to reduce the amount of pain that the patient experiences.
Practice Implications
Applying adhesive tape to a needle tip at a premeasured distance is a fast, inexpensive, and effective tool to aid accurate depth of injection for both experienced clinicians and clinicians in-training. The tape is a common office supply and the amount of tape used for a patient costs a fraction of a cent. Additionally, applying the tape takes less than 1 minute. This technique is useful for axillary hyperhidrosis injection (Figures 1 and 2) but could be used in palmar and plantar hyperhidrosis injections as well as injections other than onabotulinumtoxinA that require a specific fixed depth.
Practice Gap
OnabotulinumtoxinA is a US Food and Drug Administration–approved second-line treatment of axillary hyperhidrosis, with a long-term success rate greater than 80% and minimal adverse effects.1 The recommended depth and angle of injection of onabotulinumtoxinA for most cases of primary hyperhidrosis is 2 to 3 mm at a 45° angle to the skin surface.2 This small depth is difficult to accurately estimate once the needle tip is in the skin.
Injection Technique
We have found that measuring 2 to 3 mm on the needle tip and then wrapping a piece of adhesive tape at that point acts as a depth guide (Figure 1). The flag shape of the tape acts as a physical barrier to prevent the needle tip from penetrating too deeply (Figure 2). This barrier also allows the injector to inject quickly to reduce the amount of pain that the patient experiences.
Practice Implications
Applying adhesive tape to a needle tip at a premeasured distance is a fast, inexpensive, and effective tool to aid accurate depth of injection for both experienced clinicians and clinicians in-training. The tape is a common office supply and the amount of tape used for a patient costs a fraction of a cent. Additionally, applying the tape takes less than 1 minute. This technique is useful for axillary hyperhidrosis injection (Figures 1 and 2) but could be used in palmar and plantar hyperhidrosis injections as well as injections other than onabotulinumtoxinA that require a specific fixed depth.
- Naumann M, Lowe NJ, Kumar CR, et al; Hyperhidrosis Clinical Investigators Group. Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003;139:731-736. doi:10.1001/archderm.139.6.731
- Botox. Prescribing information. Allergan Pharmaceuticals Ireland;2011. Accessed May 12, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/103000s5236lbl.pdf
- Naumann M, Lowe NJ, Kumar CR, et al; Hyperhidrosis Clinical Investigators Group. Botulinum toxin type A is a safe and effective treatment for axillary hyperhidrosis over 16 months: a prospective study. Arch Dermatol. 2003;139:731-736. doi:10.1001/archderm.139.6.731
- Botox. Prescribing information. Allergan Pharmaceuticals Ireland;2011. Accessed May 12, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/103000s5236lbl.pdf
Local Depigmentation of a Tattoo
The Diagnosis: Dermatofibroma
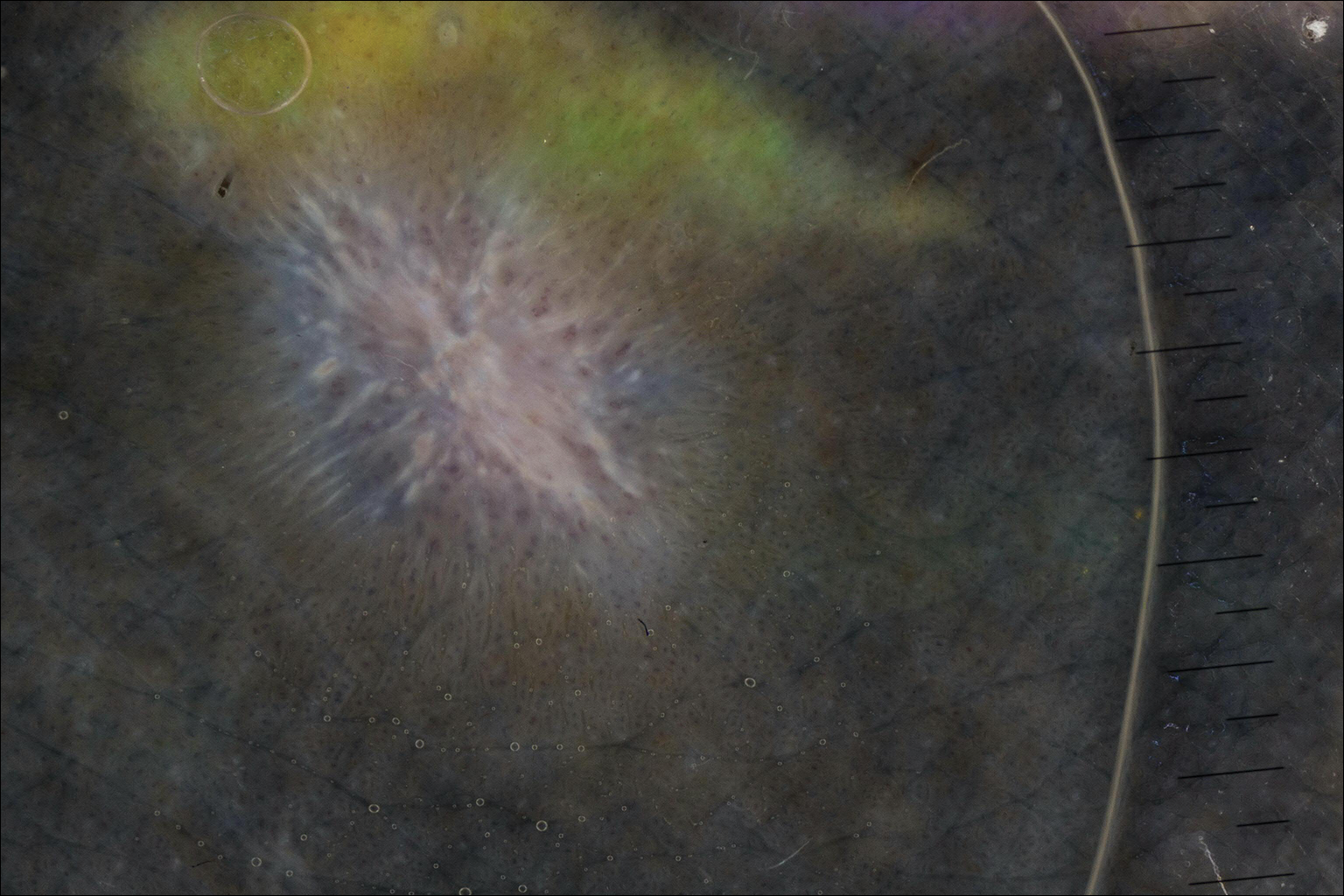
On dermoscopy, a central stellate, white, scarlike patch was seen (Figure). On both legs the patient had several additional brown 5- to 7-mm papules with similar dermoscopic features.
Dermatofibromas are common benign fibrosing tumors that appear as firm papules or plaques with variable color, commonly on the legs. Typically, lateral compression of a dermatofibroma causes downward displacement, called a positive dimple sign. On histology, fibroblasts and myofibroblasts can be seen as short intersecting fascicles with variable inflammatory cells and induction of adjacent structure hyperplasia. The etiology of dermatofibromas is unclear, though some are thought to be secondary to trauma or arthropod bites.1 Because these tumors are benign, the correct diagnosis can avoid unnecessary biopsies or other procedures.
The dermoscopic features of dermatofibromas have been well established.2 As perhaps the most easily identified structure, scarlike patches were seen in as many as 92% (22/24) of dermatofibromas in one study by Ferarri et al,3 while pigment networks also are commonly seen.2 In our case, given the surrounding dense tattoo deposition, it was difficult to ascertain any pigment network. However, the scarlike central patch was clearly apparent by dermoscopy.
Because dermatofibromas are hypothesized to be secondary to trauma, presumably applying tattoos also may cause dermatofibromas. Limited cases have described dermatofibromas arising in tattoos applied several months to years prior.4-6 No prior cases utilized dermoscopy. In our case, clinical examination and dermoscopy clearly demonstrated features consistent with a dermatofibroma, and the patient had more characteristic dermatofibromas scattered elsewhere on both legs. The patient was reassured that the lesions were benign and that the depigmentation was likely secondary to the process of dermatofibroma growth. She declined any treatment.
- Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
- Zaballos P, Puig S, Llambrich A, et al. Dermoscopy of dermatofibromas: a prospective morphological study of 412 cases. Arch Dermatol. 2008;144:75-83.
- Ferrari A, Soyer HP, Peris K, et al. Central white scarlike patch: a dermatoscopic clue for the diagnosis of dermatofibroma. J Am Acad Dermatol. 2000;43:1123-1125.
- Kluger N, Cotten H, Magana C, et al. Dermatofibroma occurring within a tattoo: report of two cases. J Cutan Pathol. 2008;35:696-698.
- Lobato-Berezo A, Churruca-Grijelmo M, Martínez-Pérez M, et al. Dermatofibroma arising within a black tattoo [published online September 23, 2014]. Case Rep Dermatol Med. 2014;2014:745304.
- Bittencourt Mde J, Miranda MF, Parijós AM, et al. Dermatofibroma in a black tattoo: report of a case. An Bras Dermatol. 2013;88:614-616.
The Diagnosis: Dermatofibroma
On dermoscopy, a central stellate, white, scarlike patch was seen (Figure). On both legs the patient had several additional brown 5- to 7-mm papules with similar dermoscopic features.
Dermatofibromas are common benign fibrosing tumors that appear as firm papules or plaques with variable color, commonly on the legs. Typically, lateral compression of a dermatofibroma causes downward displacement, called a positive dimple sign. On histology, fibroblasts and myofibroblasts can be seen as short intersecting fascicles with variable inflammatory cells and induction of adjacent structure hyperplasia. The etiology of dermatofibromas is unclear, though some are thought to be secondary to trauma or arthropod bites.1 Because these tumors are benign, the correct diagnosis can avoid unnecessary biopsies or other procedures.
The dermoscopic features of dermatofibromas have been well established.2 As perhaps the most easily identified structure, scarlike patches were seen in as many as 92% (22/24) of dermatofibromas in one study by Ferarri et al,3 while pigment networks also are commonly seen.2 In our case, given the surrounding dense tattoo deposition, it was difficult to ascertain any pigment network. However, the scarlike central patch was clearly apparent by dermoscopy.
Because dermatofibromas are hypothesized to be secondary to trauma, presumably applying tattoos also may cause dermatofibromas. Limited cases have described dermatofibromas arising in tattoos applied several months to years prior.4-6 No prior cases utilized dermoscopy. In our case, clinical examination and dermoscopy clearly demonstrated features consistent with a dermatofibroma, and the patient had more characteristic dermatofibromas scattered elsewhere on both legs. The patient was reassured that the lesions were benign and that the depigmentation was likely secondary to the process of dermatofibroma growth. She declined any treatment.
The Diagnosis: Dermatofibroma
On dermoscopy, a central stellate, white, scarlike patch was seen (Figure). On both legs the patient had several additional brown 5- to 7-mm papules with similar dermoscopic features.
Dermatofibromas are common benign fibrosing tumors that appear as firm papules or plaques with variable color, commonly on the legs. Typically, lateral compression of a dermatofibroma causes downward displacement, called a positive dimple sign. On histology, fibroblasts and myofibroblasts can be seen as short intersecting fascicles with variable inflammatory cells and induction of adjacent structure hyperplasia. The etiology of dermatofibromas is unclear, though some are thought to be secondary to trauma or arthropod bites.1 Because these tumors are benign, the correct diagnosis can avoid unnecessary biopsies or other procedures.
The dermoscopic features of dermatofibromas have been well established.2 As perhaps the most easily identified structure, scarlike patches were seen in as many as 92% (22/24) of dermatofibromas in one study by Ferarri et al,3 while pigment networks also are commonly seen.2 In our case, given the surrounding dense tattoo deposition, it was difficult to ascertain any pigment network. However, the scarlike central patch was clearly apparent by dermoscopy.
Because dermatofibromas are hypothesized to be secondary to trauma, presumably applying tattoos also may cause dermatofibromas. Limited cases have described dermatofibromas arising in tattoos applied several months to years prior.4-6 No prior cases utilized dermoscopy. In our case, clinical examination and dermoscopy clearly demonstrated features consistent with a dermatofibroma, and the patient had more characteristic dermatofibromas scattered elsewhere on both legs. The patient was reassured that the lesions were benign and that the depigmentation was likely secondary to the process of dermatofibroma growth. She declined any treatment.
- Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
- Zaballos P, Puig S, Llambrich A, et al. Dermoscopy of dermatofibromas: a prospective morphological study of 412 cases. Arch Dermatol. 2008;144:75-83.
- Ferrari A, Soyer HP, Peris K, et al. Central white scarlike patch: a dermatoscopic clue for the diagnosis of dermatofibroma. J Am Acad Dermatol. 2000;43:1123-1125.
- Kluger N, Cotten H, Magana C, et al. Dermatofibroma occurring within a tattoo: report of two cases. J Cutan Pathol. 2008;35:696-698.
- Lobato-Berezo A, Churruca-Grijelmo M, Martínez-Pérez M, et al. Dermatofibroma arising within a black tattoo [published online September 23, 2014]. Case Rep Dermatol Med. 2014;2014:745304.
- Bittencourt Mde J, Miranda MF, Parijós AM, et al. Dermatofibroma in a black tattoo: report of a case. An Bras Dermatol. 2013;88:614-616.
- Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012.
- Zaballos P, Puig S, Llambrich A, et al. Dermoscopy of dermatofibromas: a prospective morphological study of 412 cases. Arch Dermatol. 2008;144:75-83.
- Ferrari A, Soyer HP, Peris K, et al. Central white scarlike patch: a dermatoscopic clue for the diagnosis of dermatofibroma. J Am Acad Dermatol. 2000;43:1123-1125.
- Kluger N, Cotten H, Magana C, et al. Dermatofibroma occurring within a tattoo: report of two cases. J Cutan Pathol. 2008;35:696-698.
- Lobato-Berezo A, Churruca-Grijelmo M, Martínez-Pérez M, et al. Dermatofibroma arising within a black tattoo [published online September 23, 2014]. Case Rep Dermatol Med. 2014;2014:745304.
- Bittencourt Mde J, Miranda MF, Parijós AM, et al. Dermatofibroma in a black tattoo: report of a case. An Bras Dermatol. 2013;88:614-616.

A 41-year-old woman presented with loss of pigment in a tattoo on the left ankle. The tattoo was initially placed several years prior to presentation. For an uncertain amount of time, she had noticed a small palpable whitish area with loss of tattoo pigment. There was no corresponding pain, pruritis, or other symptoms. Her dermatologic history was notable only for keratosis pilaris. Physical examination showed an approximately 7-mm whitish firm papule on the lateral aspect of the left ankle, clearly visible in an otherwise green-black area of the tattoo (arrow). The lesion displaced downward with lateral compression.