User login
ED docs are cleaning up the messes of medical tourism
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
It was a typical, busy evening shift in the emergency department (ED) when Steve Carroll, DO, an emergency medicine physician in the Philadelphia area, noticed an odd listing on the tracking board. In the waiting room, there was someone whose chief complaint was that she needed to have surgical drains pulled.
According to the woman’s chart, she’d undergone liposuction in Miami a week before. The surgeon had effectively relinquished all follow-up care to the woman’s local ED.
Dr. Carroll searched the name of her surgeon and found that his site “specifically advertised medical tourism,” Dr. Carroll said. The site lured patients with the idea of recovering by the beach and that a local nurse would come to their room every day.
But when Dr. Carroll told the patient that her surgeon should be the one who removes the drains, she became concerned. She didn’t know that her surgeon wasn’t providing the standard of care, he said. Somewhat appalled that a board-certified plastic surgeon would place the burden of follow-up care on an ED doctor hundreds of miles away, Dr. Carroll posted the case to Twitter and several Facebook groups.
“Yes I could refuse to take [the drains] out but that’s not patient-centered care,” Dr. Carroll wrote in a Twitter thread. “It’s unfairly shifting routine outpatient surgical followup (and liability) onto me and extra cost to [the patient].” Comments from ED physicians and sympathetic surgeons across the country flowed in. Dr. Carroll quickly realized his situation was part of a much larger problem than he’d thought.
Dr. Carroll’s patient told him that the Miami surgery cost less than undergoing the surgery locally; that’s why she’d made the trip. She’s not alone. Traveling to get the lowest price for a plastic surgery procedure has been a rising phenomenon since the early 2000s, according to the American Society of Plastic Surgeons (ASPS). Many countries are actively fostering their medical tourism industries, as are states such as Florida.
People have long traveled to get the best medical care. But “medical tourism is completely different,” said Alan Matarasso, MD, FACS, a Manhattan-based plastic surgeon and member of the ASPS Executive Committee. “People [are] traveling to get a simultaneous vacation or lower cost,” he said.
Choosing facilities on the basis of these criteria comes with myriad problems, and the quality of medical care may be lower. It’s difficult to verify the credentials of the surgeons, anesthesiologists, and facilities involved. Medical records can be in a different language, and traveling immediately after surgery increases the risk for pulmonary embolism and death, not to mention the added complications of traveling and being a surgical patient during the COVID-19 pandemic, he said.
Typically, surgeons are protective of their patients. But Murtaza Akhter, MD, an emergency medicine physician based in Miami, says it’s the opposite with the medical tourism surgeons whose patients regularly end up in his ED. “There’s almost no ownership,” he said. “Every time, [the patients] say, ‘My doctor isn’t responding,’ or they said go to the ER.” And that’s before they’ve even made it out of Miami.
The most common cosmetic surgery complications Dr. Akhter sees occur in patients who’ve undergone so-called Brazilian butt lifts. They show up in his ED face down, suffering from severe blood loss. He has them undergo a transfusion and maybe some imaging, but if they need a higher degree of care, they have to be transferred. “There’s a reason it’s cheaper,” he said.
Medical tourism mishaps are such a regular occurrence in Miami that no one flinches when the patients show up in the ED, Dr. Akhter said. He had begun to think he was overreacting to the problem until he saw Dr. Carroll’s Twitter thread.
“Since it’s daily, I just thought maybe I had gone crazy and that it’s considered normal for plastic surgeons to do this. Thanks for making me feel sane again,” Dr. Akhter tweeted in a reply to Dr. Carroll.
There are no reliable data as to of how often or where such surgeries are occurring or of patients’ outcomes. But Nicholas Genes, MD, an ED physician in Manhattan, says he sees far more postsurgical patients who traveled for their procedures than ones who underwent surgery locally. He can’t say for certain whether that’s because procedures performed by doctors in New York City have fewer complications or the physicians just handle postprocedure problems themselves.
In a 2021 systematic review of aesthetic breast surgeries performed through medical tourism, researchers found that of 171 patients who traveled for surgery, 88 (51%) had a total of 106 complications that required returning to the operating room and undergoing general anesthesia. They also found that 39% of breast augmentation implant surgeries required either a unilateral or bilateral explantation procedure after patients returned home.
The rate of complications was higher than the study authors had expected. “These are totally elective procedures,” Dr. Matarasso said. “They should be optimized.” And high rates of complications come with hefty price tags.
The cost of managing these complications, which falls to the home healthcare system or the patient themselves, can range from $5,500 (determined on the basis of data from a 2019 study in the United Kingdom) to as much as $123,000, researchers in New York City calculated, if the patient develops a complicated mycobacterium infection.
“In your effort to get a good deal or around the system, you could still end up with a lot of extensive medical bills if something goes wrong,” Dr. Genes said.
The liability dilemma
Many of the ED physicians Dr. Carroll heard from said that they wouldn’t have treated the woman who needed to have drains removed. Unlike the Brazilian-butt-lifts-gone-wrong in Miami or the complications Dr. Genes sees in New York City, Dr. Carroll’s patient wasn’t in a state of emergency. Most ED physicians said they would have sent her on her way to find a surgeon.
“In general, we shouldn’t be doing things we aren’t trained to do. It’s sort of a slippery slope,” Dr. Genes said. He’s comfortable with removing stitches, but for surgical drains and plastic apparatuses, “I don’t feel particularly well trained. I’d have to consult a colleague in general surgery,” he said. When he does get one of these patients, he works the phones to find a plastic surgeon who will see the patient, something he says their original plastic surgeon should have done.
“Sitting there with the patient, I felt a little bad for her,” Dr. Carroll said. “I knew if I didn’t do it, it would be weeks while she bounced around to urgent care, primary care, and finally found a surgeon.” But by removing the drains, he did shift some of the liability to himself. “If she developed a wound infection, then I’m on the hook for [that],” he said. “If I send her away, I have less liability but didn’t quite do the right thing for the patient.”
In replies to Dr. Carroll’s thread, some doctors debated whether these types of cases, particularly those in which surgeons forgo follow-up care, could be considered medical abandonment. Legal experts say that’s not exactly the case, at least it would not be the case with Dr. Carroll’s patient.
“I don’t think they’ve abandoned the patient; I think they’ve abandoned care,” said Michael Flynn, JD, professor of personal injury law at Nova Southeastern University, in Fort Lauderdale–Davie, Fla. “And that abandonment of follow-up care, if it falls below the standard of what medical professionals should do, then it’s malpractice.”
“The doctor didn’t just walk away and become unreachable,” said Bernard Black, JD, a medical malpractice attorney and law professor at Northwestern University, in Evanston, Ill. Technically, the surgeon referred the patient to the ED. Mr. Black agreed that it sounds more like a question of malpractice, “but without real damages, there’s no claim.”
Even if not illegal, sending these patients to the ED is still highly unethical, Dr. Carroll said. The authors of a 2014 article in Aesthetic Plastic Surgery concur: “It is the duty and ethical responsibility of plastic surgeons to prevent unnecessary complications following tourism medicine by adequately counseling patients, defining perioperative treatment protocols, and reporting complications to regional and specialty-specific governing bodies,” they write.
Sometimes patients need to travel, Dr. Matarasso said. Recently, three out-of-state patients came to him for procedures. Two stayed in Manhattan until their follow-up care was finished; he arranged care elsewhere for the third. It’s the operating surgeon’s job to connect patients with someone who can provide follow-up care when they go home, Dr. Matarasso said. If a surgeon doesn’t have a connection in a patient’s home city, the ASPS has a referral service to help, he said.
“My frustration was never with the patient,” Dr. Carroll said. “No one should feel bad about coming to an ED for literally anything, and I mean that. My frustration is with the surgeon who didn’t go the one extra step to arrange her follow-up.”
A version of this article first appeared on Medscape.com.
Injectable monoclonal antibodies prevent COVID-19 in trial
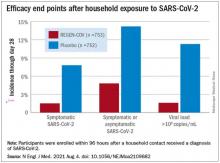
according to results of a randomized, double-blind, placebo-controlled clinical trial published online August 4, 2021, in the New England Journal of Medicine.
The cocktail of the monoclonal antibodies casirivimab and imdevimab (REGEN-COV, Regeneron Pharmaceuticals) reduced participants’ relative risk of infection by 72%, compared with placebo within the first week. After the first week, risk reduction increased to 93%.
“Long after you would be exposed by your household, there is an enduring effect that prevents you from community spread,” said David Wohl, MD, professor of medicine in the division of infectious diseases at the University of North Carolina at Chapel Hill, who was a site investigator for the trial but not a study author.
Participants were enrolled within 96 hours after someone in their household tested positive for SARS-CoV-2. Participants were randomly assigned to receive 1,200 mg of REGEN-COV subcutaneously or a placebo. Based on serologic testing, study participants showed no evidence of current or previous SARS-CoV-2 infection. The median age of participants was 42.9, but 45% were male teenagers (ages 12-17).
In the group that received REGEN-COV, 11 out of 753 participants developed symptomatic COVID-19, compared with 59 out of 752 participants who received placebo. The relative risk reduction for the study’s 4-week period was 81.4% (P < .001). Of the participants that did develop a SARS-CoV-2 infection, those that received REGEN-COV were less likely to be symptomatic. Asymptomatic infections developed in 25 participants who received REGEN-COV versus 48 in the placebo group. The relative risk of developing any SARS-CoV-2 infection, symptomatic or asymptomatic, was reduced by 66.4% with REGEN-COV (P < .001).
Among the patients who were symptomatic, symptoms subsided within a median of 1.2 weeks for the group that received REGEN-COV, 2 weeks earlier than the placebo group. These patients also had a shorter duration of a high viral load (>104 copies/mL). Few adverse events were reported in the treatment or placebo groups. Monoclonal antibodies “seem to be incredibly safe,” Dr. Wohl said.
“These monoclonal antibodies have proven they can reduce the viral replication in the nose,” said study author Myron Cohen, MD, an infectious disease specialist and professor of epidemiology at the University of North Carolina.
The Food and Drug Administration first granted REGEN-COV emergency use authorization (EUA) in November 2020 for use in patients with mild or moderate COVID-19 who were also at high risk for progressing to severe COVID-19. At that time, the cocktail of monoclonal antibodies was delivered by a single intravenous infusion.
In January, Regeneron first announced the success of this trial of the subcutaneous injection for exposed household contacts based on early results, and in June of 2021, the FDA expanded the EUA to include a subcutaneous delivery when IV is not feasible. On July 30, the EUA was expanded again to include prophylactic use in exposed patients based on these trial results.
The U.S. government has purchased approximately 1.5 million doses of REGEN-COV from Regeneron and has agreed to make the treatments free of charge to patients.
But despite being free, available, and backed by promising data, monoclonal antibodies as a therapeutic answer to COVID-19 still hasn’t really taken off. “The problem is, it first requires knowledge and awareness,” Dr. Wohl said. “A lot [of people] don’t know this exists. To be honest, vaccination has taken up all the oxygen in the room.”
Dr. Cohen agreed. One reason for the slow uptake may be because the drug supply is owned by the government and not a pharmaceutical company. There hasn’t been a typical marketing push to make physicians and consumers aware. Additionally, “the logistics are daunting,” Dr. Cohen said. The office spaces where many physicians care for patients “often aren’t appropriate for patients who think they have SARS-CoV-2.”
“Right now, there’s not a mechanism” to administer the drug to people who could benefit from it, Dr. Wohl said. Eligible patients are either immunocompromised and unlikely to mount a sufficient immune response with vaccination, or not fully vaccinated. They should have been exposed to an infected individual or have a high likelihood of exposure due to where they live, such as in a prison or nursing home. Local doctors are unlikely to be the primary administrators of the drug, Dr. Wohl added. “How do we operationalize this for people who fit the criteria?”
There’s also an issue of timing. REGEN-COV is most effective when given early, Dr. Cohen said. “[Monoclonal antibodies] really only work well in the replication phase.” Many patients who would be eligible delay care until they’ve had symptoms for several days, when REGEN-COV would no longer have the desired effect.
Eventually, Dr. Wohl suspects demand will increase when people realize REGEN-COV can help those with COVID-19 and those who have been exposed. But before then, “we do have to think about how to integrate this into a workflow people can access without being confused.”
The trial was done before there was widespread vaccination, so it’s unclear what the results mean for people who have been vaccinated. Dr. Cohen and Dr. Wohl said there are ongoing conversations about whether monoclonal antibodies could be complementary to vaccination and if there’s potential for continued monthly use of these therapies.
Cohen and Wohl reported no relevant financial relationships. The trial was supported by Regeneron Pharmaceuticals, F. Hoffmann–La Roche, the National Institute of Allergy and Infectious Diseases, NIH, and the COVID-19 Prevention Network.
A version of this article first appeared on Medscape.com.
according to results of a randomized, double-blind, placebo-controlled clinical trial published online August 4, 2021, in the New England Journal of Medicine.
The cocktail of the monoclonal antibodies casirivimab and imdevimab (REGEN-COV, Regeneron Pharmaceuticals) reduced participants’ relative risk of infection by 72%, compared with placebo within the first week. After the first week, risk reduction increased to 93%.
“Long after you would be exposed by your household, there is an enduring effect that prevents you from community spread,” said David Wohl, MD, professor of medicine in the division of infectious diseases at the University of North Carolina at Chapel Hill, who was a site investigator for the trial but not a study author.
Participants were enrolled within 96 hours after someone in their household tested positive for SARS-CoV-2. Participants were randomly assigned to receive 1,200 mg of REGEN-COV subcutaneously or a placebo. Based on serologic testing, study participants showed no evidence of current or previous SARS-CoV-2 infection. The median age of participants was 42.9, but 45% were male teenagers (ages 12-17).
In the group that received REGEN-COV, 11 out of 753 participants developed symptomatic COVID-19, compared with 59 out of 752 participants who received placebo. The relative risk reduction for the study’s 4-week period was 81.4% (P < .001). Of the participants that did develop a SARS-CoV-2 infection, those that received REGEN-COV were less likely to be symptomatic. Asymptomatic infections developed in 25 participants who received REGEN-COV versus 48 in the placebo group. The relative risk of developing any SARS-CoV-2 infection, symptomatic or asymptomatic, was reduced by 66.4% with REGEN-COV (P < .001).
Among the patients who were symptomatic, symptoms subsided within a median of 1.2 weeks for the group that received REGEN-COV, 2 weeks earlier than the placebo group. These patients also had a shorter duration of a high viral load (>104 copies/mL). Few adverse events were reported in the treatment or placebo groups. Monoclonal antibodies “seem to be incredibly safe,” Dr. Wohl said.
“These monoclonal antibodies have proven they can reduce the viral replication in the nose,” said study author Myron Cohen, MD, an infectious disease specialist and professor of epidemiology at the University of North Carolina.
The Food and Drug Administration first granted REGEN-COV emergency use authorization (EUA) in November 2020 for use in patients with mild or moderate COVID-19 who were also at high risk for progressing to severe COVID-19. At that time, the cocktail of monoclonal antibodies was delivered by a single intravenous infusion.
In January, Regeneron first announced the success of this trial of the subcutaneous injection for exposed household contacts based on early results, and in June of 2021, the FDA expanded the EUA to include a subcutaneous delivery when IV is not feasible. On July 30, the EUA was expanded again to include prophylactic use in exposed patients based on these trial results.
The U.S. government has purchased approximately 1.5 million doses of REGEN-COV from Regeneron and has agreed to make the treatments free of charge to patients.
But despite being free, available, and backed by promising data, monoclonal antibodies as a therapeutic answer to COVID-19 still hasn’t really taken off. “The problem is, it first requires knowledge and awareness,” Dr. Wohl said. “A lot [of people] don’t know this exists. To be honest, vaccination has taken up all the oxygen in the room.”
Dr. Cohen agreed. One reason for the slow uptake may be because the drug supply is owned by the government and not a pharmaceutical company. There hasn’t been a typical marketing push to make physicians and consumers aware. Additionally, “the logistics are daunting,” Dr. Cohen said. The office spaces where many physicians care for patients “often aren’t appropriate for patients who think they have SARS-CoV-2.”
“Right now, there’s not a mechanism” to administer the drug to people who could benefit from it, Dr. Wohl said. Eligible patients are either immunocompromised and unlikely to mount a sufficient immune response with vaccination, or not fully vaccinated. They should have been exposed to an infected individual or have a high likelihood of exposure due to where they live, such as in a prison or nursing home. Local doctors are unlikely to be the primary administrators of the drug, Dr. Wohl added. “How do we operationalize this for people who fit the criteria?”
There’s also an issue of timing. REGEN-COV is most effective when given early, Dr. Cohen said. “[Monoclonal antibodies] really only work well in the replication phase.” Many patients who would be eligible delay care until they’ve had symptoms for several days, when REGEN-COV would no longer have the desired effect.
Eventually, Dr. Wohl suspects demand will increase when people realize REGEN-COV can help those with COVID-19 and those who have been exposed. But before then, “we do have to think about how to integrate this into a workflow people can access without being confused.”
The trial was done before there was widespread vaccination, so it’s unclear what the results mean for people who have been vaccinated. Dr. Cohen and Dr. Wohl said there are ongoing conversations about whether monoclonal antibodies could be complementary to vaccination and if there’s potential for continued monthly use of these therapies.
Cohen and Wohl reported no relevant financial relationships. The trial was supported by Regeneron Pharmaceuticals, F. Hoffmann–La Roche, the National Institute of Allergy and Infectious Diseases, NIH, and the COVID-19 Prevention Network.
A version of this article first appeared on Medscape.com.
according to results of a randomized, double-blind, placebo-controlled clinical trial published online August 4, 2021, in the New England Journal of Medicine.
The cocktail of the monoclonal antibodies casirivimab and imdevimab (REGEN-COV, Regeneron Pharmaceuticals) reduced participants’ relative risk of infection by 72%, compared with placebo within the first week. After the first week, risk reduction increased to 93%.
“Long after you would be exposed by your household, there is an enduring effect that prevents you from community spread,” said David Wohl, MD, professor of medicine in the division of infectious diseases at the University of North Carolina at Chapel Hill, who was a site investigator for the trial but not a study author.
Participants were enrolled within 96 hours after someone in their household tested positive for SARS-CoV-2. Participants were randomly assigned to receive 1,200 mg of REGEN-COV subcutaneously or a placebo. Based on serologic testing, study participants showed no evidence of current or previous SARS-CoV-2 infection. The median age of participants was 42.9, but 45% were male teenagers (ages 12-17).
In the group that received REGEN-COV, 11 out of 753 participants developed symptomatic COVID-19, compared with 59 out of 752 participants who received placebo. The relative risk reduction for the study’s 4-week period was 81.4% (P < .001). Of the participants that did develop a SARS-CoV-2 infection, those that received REGEN-COV were less likely to be symptomatic. Asymptomatic infections developed in 25 participants who received REGEN-COV versus 48 in the placebo group. The relative risk of developing any SARS-CoV-2 infection, symptomatic or asymptomatic, was reduced by 66.4% with REGEN-COV (P < .001).
Among the patients who were symptomatic, symptoms subsided within a median of 1.2 weeks for the group that received REGEN-COV, 2 weeks earlier than the placebo group. These patients also had a shorter duration of a high viral load (>104 copies/mL). Few adverse events were reported in the treatment or placebo groups. Monoclonal antibodies “seem to be incredibly safe,” Dr. Wohl said.
“These monoclonal antibodies have proven they can reduce the viral replication in the nose,” said study author Myron Cohen, MD, an infectious disease specialist and professor of epidemiology at the University of North Carolina.
The Food and Drug Administration first granted REGEN-COV emergency use authorization (EUA) in November 2020 for use in patients with mild or moderate COVID-19 who were also at high risk for progressing to severe COVID-19. At that time, the cocktail of monoclonal antibodies was delivered by a single intravenous infusion.
In January, Regeneron first announced the success of this trial of the subcutaneous injection for exposed household contacts based on early results, and in June of 2021, the FDA expanded the EUA to include a subcutaneous delivery when IV is not feasible. On July 30, the EUA was expanded again to include prophylactic use in exposed patients based on these trial results.
The U.S. government has purchased approximately 1.5 million doses of REGEN-COV from Regeneron and has agreed to make the treatments free of charge to patients.
But despite being free, available, and backed by promising data, monoclonal antibodies as a therapeutic answer to COVID-19 still hasn’t really taken off. “The problem is, it first requires knowledge and awareness,” Dr. Wohl said. “A lot [of people] don’t know this exists. To be honest, vaccination has taken up all the oxygen in the room.”
Dr. Cohen agreed. One reason for the slow uptake may be because the drug supply is owned by the government and not a pharmaceutical company. There hasn’t been a typical marketing push to make physicians and consumers aware. Additionally, “the logistics are daunting,” Dr. Cohen said. The office spaces where many physicians care for patients “often aren’t appropriate for patients who think they have SARS-CoV-2.”
“Right now, there’s not a mechanism” to administer the drug to people who could benefit from it, Dr. Wohl said. Eligible patients are either immunocompromised and unlikely to mount a sufficient immune response with vaccination, or not fully vaccinated. They should have been exposed to an infected individual or have a high likelihood of exposure due to where they live, such as in a prison or nursing home. Local doctors are unlikely to be the primary administrators of the drug, Dr. Wohl added. “How do we operationalize this for people who fit the criteria?”
There’s also an issue of timing. REGEN-COV is most effective when given early, Dr. Cohen said. “[Monoclonal antibodies] really only work well in the replication phase.” Many patients who would be eligible delay care until they’ve had symptoms for several days, when REGEN-COV would no longer have the desired effect.
Eventually, Dr. Wohl suspects demand will increase when people realize REGEN-COV can help those with COVID-19 and those who have been exposed. But before then, “we do have to think about how to integrate this into a workflow people can access without being confused.”
The trial was done before there was widespread vaccination, so it’s unclear what the results mean for people who have been vaccinated. Dr. Cohen and Dr. Wohl said there are ongoing conversations about whether monoclonal antibodies could be complementary to vaccination and if there’s potential for continued monthly use of these therapies.
Cohen and Wohl reported no relevant financial relationships. The trial was supported by Regeneron Pharmaceuticals, F. Hoffmann–La Roche, the National Institute of Allergy and Infectious Diseases, NIH, and the COVID-19 Prevention Network.
A version of this article first appeared on Medscape.com.
Midodrine reduces fainting in young patients
.
Vasovagal syncope is the most common cause of fainting and is often triggered by dehydration and upright posture, according to Johns Hopkins Medicine. But it can also be caused by stimuli like the sight of blood or sudden emotional distress. The stimulus causes the heart rate and blood pressure to drop rapidly, according to the Mayo Clinic.
The randomized, placebo-controlled, double-blind trial included 133 patients with recurrent vasovagal syncope and was published in Annals of Internal Medicine. Those that received midodrine were less likely to have one syncope episode (28 of 66 [42%]), compared with those that took the placebo (41 of 67 [61%]). The absolute risk reduction for vasovagal syncope was 19 percentage points (95% confidence interval, 2-36 percentage points).
The study included patients from 25 university hospitals in Canada, the United States, Mexico, and the United Kingdom, who were followed for 12 months. The trial participants were highly symptomatic for vasovagal syncope, having experienced a median of 23 episodes in their lifetime and 5 syncope episodes in the last year, and they had no comorbid conditions.
“We don’t have many arrows in our quiver,” said Robert Sheldon, MD, PhD, a cardiologist at University of Calgary (Alta.) and lead author of the study, referring to the lack of evidence-based treatments for syncope.
For 20 years Dr. Sheldon’s lab has been testing drugs that showed some potential. While a previous study of fludrocortisone (Florinef ) showed some benefit, “[midodrine] was the first to be unequivocally, slam-dunk positive,” he said in an interview.
Earlier trials of midodrine
Other studies have shown midodrine to prevent syncope on tilt tests. There have been two randomized trials where midodrine significantly reduced vasovagal syncope, but one of these was short and in children, and the other one was open label with no placebo control.
“Risk reduction was very high in previous studies,” Dr. Sheldon said in an interview. But, because they were open label, there was a huge placebo effect, he noted.
“There were no adequately done, adequately powered [studies] that have been positive,” Dr. Sheldon added.
New study methods and outcomes
The study published in Annals of Internal Medicine this week included patients over 18 years of age with a Calgary Syncope Symptom Score of at least 2. All were educated on lifestyle measures that can prevent syncopes before beginning to take 5 mg of study drug or placebo three times daily, 4 hours apart.
In these cases, the study authors wrote, “taking medication three times a day seems worth the effort.” But in patients with a lower frequency of episodes, midodrine might not have an adequate payoff.
These results are “impressive,” said Roopinder K. Sandhu, MD, MPH, clinical electrophysiologist at Cedar-Sinai in Los Angeles. “This study demonstrated that midodrine is the first medical therapy, in addition to education and lifestyle measures, to unequivocally pass the scrutiny of an international, placebo-controlled, RCT to show a significant reduction in syncope recurrence in a younger population with frequent syncope events.”
“[Taking midodrine] doesn’t carry the long-term consequence of pacemakers,” she added.
Study limitations
Limitations of the new study include its small size and short observation period, the authors wrote. Additionally, a large proportion of patients enrolled were also from a single center in Calgary that specializes in syncope care. Twenty-seven patients in the trial stopped taking their assigned medication during the year observation period, but the authors concluded these participants “likely would bias the results against midodrine.”
For doctors considering midodrine for their patients, it’s critical to confirm the diagnosis and to try patient education first, Dr. Sheldon advised.
Lifestyle factors like hydration, adequate sodium intake, and squatting or lying down when the syncope is coming on can sufficiently suppress syncopes in two-thirds of patients, he noted.
This is a treatment for young people, Dr. Sandhu said. The median age in the trial was 35, so patients taking midodrine should be younger than 50. Midodrine is also not effective in patients with high blood pressure or heart failure, she said.
“[Midodrine] is easy to use but kind of a pain at first,” Dr. Sheldon noted. Every patient should start out taking 5 mg doses, three times a day – during waking hours. But then you have to adjust the dosage, “and it’s tricky,” he said.
If a patient experiences goosebumps or the sensation of worms crawling in the hair, the dose might be too much, Dr. Sheldon noted.
If the patient is still fainting, first consider when they are fainting, he said. If it’s around the time they should take another dose, it might be trough effect.
Dr. Sandhu was not involved in the study, but Cedar Sinai was a participating center, and she considers Dr. Sheldon to be a mentor. Dr. Sandhu also noted that she has published papers with Dr. Sheldon, who reported no conflicts.
.
Vasovagal syncope is the most common cause of fainting and is often triggered by dehydration and upright posture, according to Johns Hopkins Medicine. But it can also be caused by stimuli like the sight of blood or sudden emotional distress. The stimulus causes the heart rate and blood pressure to drop rapidly, according to the Mayo Clinic.
The randomized, placebo-controlled, double-blind trial included 133 patients with recurrent vasovagal syncope and was published in Annals of Internal Medicine. Those that received midodrine were less likely to have one syncope episode (28 of 66 [42%]), compared with those that took the placebo (41 of 67 [61%]). The absolute risk reduction for vasovagal syncope was 19 percentage points (95% confidence interval, 2-36 percentage points).
The study included patients from 25 university hospitals in Canada, the United States, Mexico, and the United Kingdom, who were followed for 12 months. The trial participants were highly symptomatic for vasovagal syncope, having experienced a median of 23 episodes in their lifetime and 5 syncope episodes in the last year, and they had no comorbid conditions.
“We don’t have many arrows in our quiver,” said Robert Sheldon, MD, PhD, a cardiologist at University of Calgary (Alta.) and lead author of the study, referring to the lack of evidence-based treatments for syncope.
For 20 years Dr. Sheldon’s lab has been testing drugs that showed some potential. While a previous study of fludrocortisone (Florinef ) showed some benefit, “[midodrine] was the first to be unequivocally, slam-dunk positive,” he said in an interview.
Earlier trials of midodrine
Other studies have shown midodrine to prevent syncope on tilt tests. There have been two randomized trials where midodrine significantly reduced vasovagal syncope, but one of these was short and in children, and the other one was open label with no placebo control.
“Risk reduction was very high in previous studies,” Dr. Sheldon said in an interview. But, because they were open label, there was a huge placebo effect, he noted.
“There were no adequately done, adequately powered [studies] that have been positive,” Dr. Sheldon added.
New study methods and outcomes
The study published in Annals of Internal Medicine this week included patients over 18 years of age with a Calgary Syncope Symptom Score of at least 2. All were educated on lifestyle measures that can prevent syncopes before beginning to take 5 mg of study drug or placebo three times daily, 4 hours apart.
In these cases, the study authors wrote, “taking medication three times a day seems worth the effort.” But in patients with a lower frequency of episodes, midodrine might not have an adequate payoff.
These results are “impressive,” said Roopinder K. Sandhu, MD, MPH, clinical electrophysiologist at Cedar-Sinai in Los Angeles. “This study demonstrated that midodrine is the first medical therapy, in addition to education and lifestyle measures, to unequivocally pass the scrutiny of an international, placebo-controlled, RCT to show a significant reduction in syncope recurrence in a younger population with frequent syncope events.”
“[Taking midodrine] doesn’t carry the long-term consequence of pacemakers,” she added.
Study limitations
Limitations of the new study include its small size and short observation period, the authors wrote. Additionally, a large proportion of patients enrolled were also from a single center in Calgary that specializes in syncope care. Twenty-seven patients in the trial stopped taking their assigned medication during the year observation period, but the authors concluded these participants “likely would bias the results against midodrine.”
For doctors considering midodrine for their patients, it’s critical to confirm the diagnosis and to try patient education first, Dr. Sheldon advised.
Lifestyle factors like hydration, adequate sodium intake, and squatting or lying down when the syncope is coming on can sufficiently suppress syncopes in two-thirds of patients, he noted.
This is a treatment for young people, Dr. Sandhu said. The median age in the trial was 35, so patients taking midodrine should be younger than 50. Midodrine is also not effective in patients with high blood pressure or heart failure, she said.
“[Midodrine] is easy to use but kind of a pain at first,” Dr. Sheldon noted. Every patient should start out taking 5 mg doses, three times a day – during waking hours. But then you have to adjust the dosage, “and it’s tricky,” he said.
If a patient experiences goosebumps or the sensation of worms crawling in the hair, the dose might be too much, Dr. Sheldon noted.
If the patient is still fainting, first consider when they are fainting, he said. If it’s around the time they should take another dose, it might be trough effect.
Dr. Sandhu was not involved in the study, but Cedar Sinai was a participating center, and she considers Dr. Sheldon to be a mentor. Dr. Sandhu also noted that she has published papers with Dr. Sheldon, who reported no conflicts.
.
Vasovagal syncope is the most common cause of fainting and is often triggered by dehydration and upright posture, according to Johns Hopkins Medicine. But it can also be caused by stimuli like the sight of blood or sudden emotional distress. The stimulus causes the heart rate and blood pressure to drop rapidly, according to the Mayo Clinic.
The randomized, placebo-controlled, double-blind trial included 133 patients with recurrent vasovagal syncope and was published in Annals of Internal Medicine. Those that received midodrine were less likely to have one syncope episode (28 of 66 [42%]), compared with those that took the placebo (41 of 67 [61%]). The absolute risk reduction for vasovagal syncope was 19 percentage points (95% confidence interval, 2-36 percentage points).
The study included patients from 25 university hospitals in Canada, the United States, Mexico, and the United Kingdom, who were followed for 12 months. The trial participants were highly symptomatic for vasovagal syncope, having experienced a median of 23 episodes in their lifetime and 5 syncope episodes in the last year, and they had no comorbid conditions.
“We don’t have many arrows in our quiver,” said Robert Sheldon, MD, PhD, a cardiologist at University of Calgary (Alta.) and lead author of the study, referring to the lack of evidence-based treatments for syncope.
For 20 years Dr. Sheldon’s lab has been testing drugs that showed some potential. While a previous study of fludrocortisone (Florinef ) showed some benefit, “[midodrine] was the first to be unequivocally, slam-dunk positive,” he said in an interview.
Earlier trials of midodrine
Other studies have shown midodrine to prevent syncope on tilt tests. There have been two randomized trials where midodrine significantly reduced vasovagal syncope, but one of these was short and in children, and the other one was open label with no placebo control.
“Risk reduction was very high in previous studies,” Dr. Sheldon said in an interview. But, because they were open label, there was a huge placebo effect, he noted.
“There were no adequately done, adequately powered [studies] that have been positive,” Dr. Sheldon added.
New study methods and outcomes
The study published in Annals of Internal Medicine this week included patients over 18 years of age with a Calgary Syncope Symptom Score of at least 2. All were educated on lifestyle measures that can prevent syncopes before beginning to take 5 mg of study drug or placebo three times daily, 4 hours apart.
In these cases, the study authors wrote, “taking medication three times a day seems worth the effort.” But in patients with a lower frequency of episodes, midodrine might not have an adequate payoff.
These results are “impressive,” said Roopinder K. Sandhu, MD, MPH, clinical electrophysiologist at Cedar-Sinai in Los Angeles. “This study demonstrated that midodrine is the first medical therapy, in addition to education and lifestyle measures, to unequivocally pass the scrutiny of an international, placebo-controlled, RCT to show a significant reduction in syncope recurrence in a younger population with frequent syncope events.”
“[Taking midodrine] doesn’t carry the long-term consequence of pacemakers,” she added.
Study limitations
Limitations of the new study include its small size and short observation period, the authors wrote. Additionally, a large proportion of patients enrolled were also from a single center in Calgary that specializes in syncope care. Twenty-seven patients in the trial stopped taking their assigned medication during the year observation period, but the authors concluded these participants “likely would bias the results against midodrine.”
For doctors considering midodrine for their patients, it’s critical to confirm the diagnosis and to try patient education first, Dr. Sheldon advised.
Lifestyle factors like hydration, adequate sodium intake, and squatting or lying down when the syncope is coming on can sufficiently suppress syncopes in two-thirds of patients, he noted.
This is a treatment for young people, Dr. Sandhu said. The median age in the trial was 35, so patients taking midodrine should be younger than 50. Midodrine is also not effective in patients with high blood pressure or heart failure, she said.
“[Midodrine] is easy to use but kind of a pain at first,” Dr. Sheldon noted. Every patient should start out taking 5 mg doses, three times a day – during waking hours. But then you have to adjust the dosage, “and it’s tricky,” he said.
If a patient experiences goosebumps or the sensation of worms crawling in the hair, the dose might be too much, Dr. Sheldon noted.
If the patient is still fainting, first consider when they are fainting, he said. If it’s around the time they should take another dose, it might be trough effect.
Dr. Sandhu was not involved in the study, but Cedar Sinai was a participating center, and she considers Dr. Sheldon to be a mentor. Dr. Sandhu also noted that she has published papers with Dr. Sheldon, who reported no conflicts.
FROM ANNALS OF INTERNAL MEDICINE
Married docs remove girl’s lethal facial tumor in ‘excruciatingly difficult’ procedure
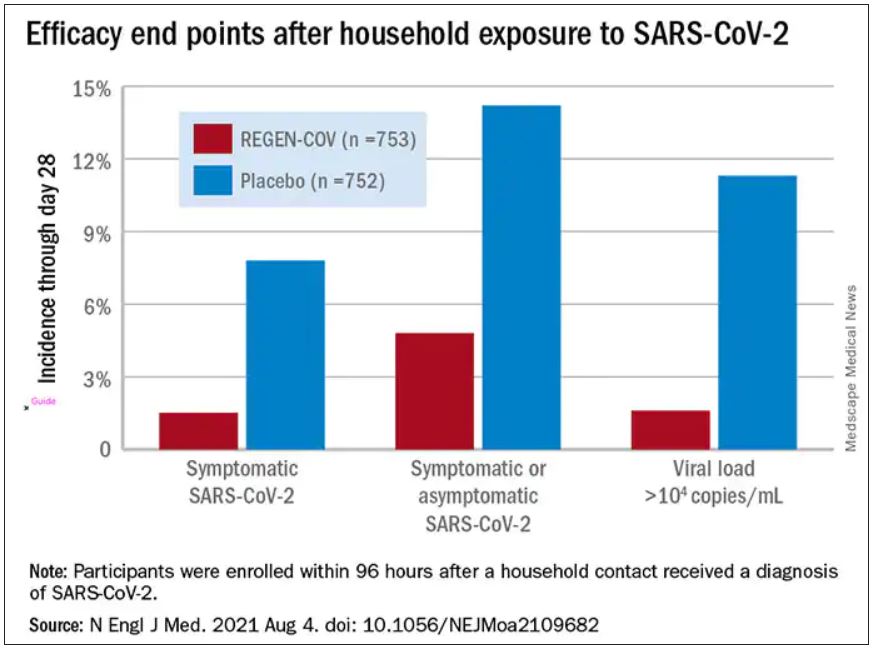
In 2019, doctors in London saw a 5-year old girl from rural Ethiopia with an enormous tumor extending from her cheek to her lower jaw. Her name was Negalem and the tumor was a vascular malformation, a life-threatening web of tangled blood vessels.
Surgery to remove it was impossible, the doctors told the foundation advocating for the girl. The child would never make it off the operating table. After a closer examination, the London group still declined to do the procedure, but told the child’s parents and advocates that if anyone was going to attempt this, they’d need to get the little girl to New York.
In New York City, on 64th St. in Manhattan, is the Vascular Birthmark Institute, founded by Milton Waner, MD, who has exclusively treated hemangiomas and vascular malformations for the last 30 years. “I’m the only person in the [United] States whose practice is exclusively [treating] vascular anomalies,” Dr. Waner said in an interview.
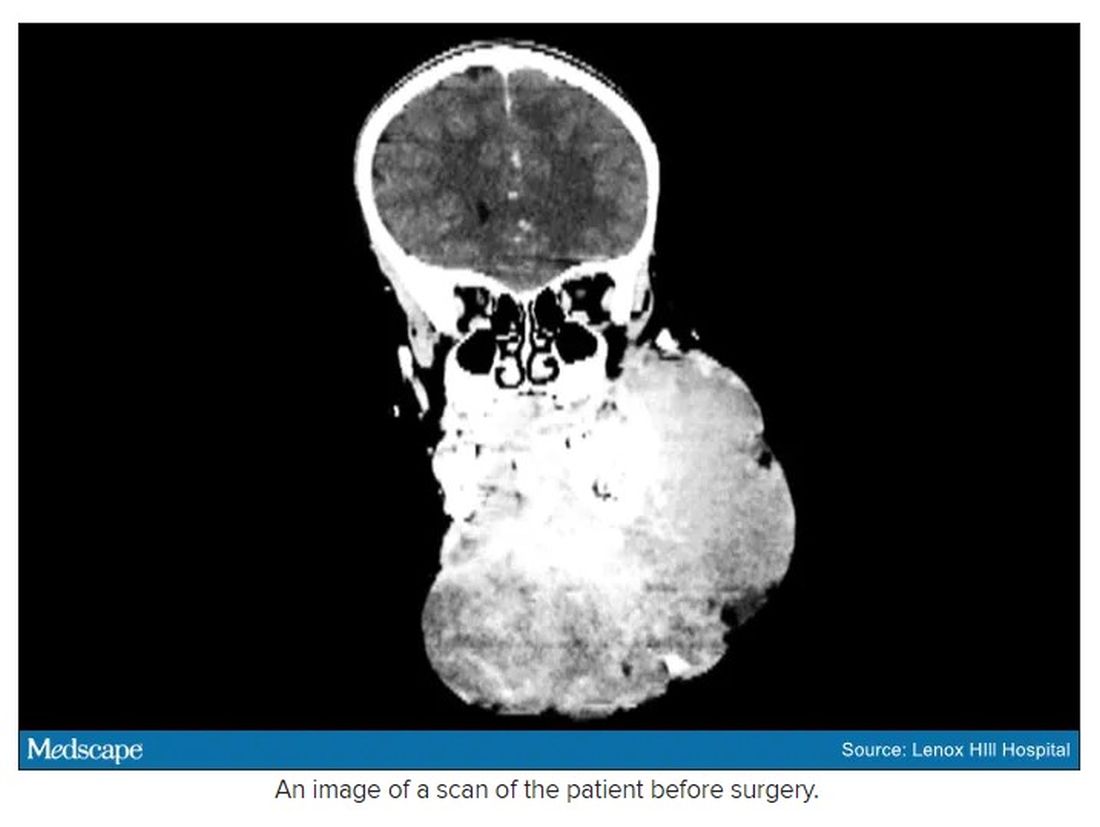
Dr. Waner has assembled a multidisciplinary team of experts at the institute’s offices in Lenox Hill – including his wife Teresa O, MD, a facial plastic and reconstructive surgeon and neurospecialist. “People often ask how the hell do you spend so much time with your spouse?” Dr. Waner says. “We work extremely well together. We complement each other.”
Dr. O and Dr. Waner each manage half of the cases at VBI. And in January they received an email about Negalem. After corresponding with the child’s advocate and reviewing images,
The challenge with vascular malformations in children, Dr. Waner said, is that they have a fraction of the blood an adult has. Where adults have an average of 5 L of blood, a child this age has only 1 L. To lose 200 or 300 mL of blood, “that’s 20% or 30% of their blood volume,” Dr. Waner said. So the removal of such a mass, which requires a meticulous dissection around many blood vessels, carries a high risk of the child bleeding out.
There were some logistical hurdles, but the patient arrived in Manhattan in mid-June, at no cost to her family. The medical visa was organized by a volunteer who also work for USAID. Healing the Children Northeast paid for her travel and the Waner Kids Foundation paid for her hotel stay. Lenox Hill Hospital and Northwell Health covered all hospital costs and postsurgery care. And Dr. O and Dr. Waner did the planning, consult visits, and procedure pro bono.
The surgery was possible because of the generosity of several organizations, but the two surgeons still had a limited time to remove the mass. Under different circumstances, and with the luxury of more time, the patient would have undergone several rounds of sclerotherapy. This procedure, done by interventional radiologists, involves injecting a toxin into the blood vessels, which causes them to clot. Done prior to surgery it can help limit bleeding risk.
On June 23, the morning of the surgery, the patient underwent one round of sclerotherapy. However, it didn’t have the intended effect, Dr. Waner said, “because the lesion was just so massive.”
The team had planned several of their moves ahead of time. But this isn’t the sort of surgery you’d find in a textbook. Because it’s such a unique field, Dr. Waner and Dr. O have developed many of their own techniques along the way. This patient was much like the cases they treat every day, only “several orders of magnitudes greater,” Dr. Waner said. “On a scale of 1 to 10 she was a 12.”
The morning of the surgery, “I was very apprehensive,” Dr. Waner recalled. He vividly remembers the girl’s father repeatedly kissing her to say goodbye as she lay on the operating table, fully aware that this procedure was a life-threatening one. And from the beginning there were challenges, like getting her under anesthesia when the anatomy of her mouth, deformed by the tumor, didn’t allow the anesthesiologists to use their typical tubing. Then, once the skin was removed, it became clear how dilated and tangled the involved blood vessels were. There were many vital structures tangled in the anomaly. “The jugular vein was right there. The carotid artery was right there,” Dr. Waner said. It was extremely difficult to delineate and preserve them, he said.
“That’s why we really took our time. We just went very slowly and deliberately,” Dr. O said. The blood vessels were so dilated that their only option was to move painstakingly slow – otherwise a small nick could be devastating.
But even with the slow pace the surgery was “excruciatingly difficult,” Dr. Waner said. And early on in the dissection he wasn’t quite sure they’d make it out. The sclerotherapy hadn’t done much to prevent bleeding. “At one point every millimeter or 2 that we advanced we got into some bleeding,” Dr. Waner said. “Brisk bleeding.”
Once they got into the surgery they also realized that the growth had adhered to the jaw bone. “There were vessels traversing into the bone, which were hard to control,” Dr. O said.
But finally, both doctors realized they’d be able to remove it. With the lesion removed they began the work of reconstruction and reanimation.
The child’s jaw and cheek bone had grown beyond their normal size to support the growth. They had to shave them down to achieve facial symmetry. The tumor had also inhibited much of the child’s facial nerve control. With it gone, Dr. O began the work of finding all the facial nerve branches and assembling them to reanimate the child’s face.
Before medicine, Dr. O trained as an architect, which, according to Dr. Waner, has equipped her with very good spatial awareness – a valuable skill in the surgical reconstruction phase. After seeing a lecture by Dr. Waner, she immediately saw a fit for her unique interest and skill set. She did fellowship training with Dr. Waner in vascular anomalies, and then went on to specialize in facial nerve reanimation. The proof of Dr. O’s expertise is Negalem’s new, beautiful smile, Dr. Waner said.
The surgery drew out over 8 hours, as long as a day of surgeries for the two doctors. When Dr. O finally walked into the waiting room to inform the family of the success, the first words out of the father’s mouth were: “Is my daughter alive?”
A growth like Negalem had is not compatible with a normal life. Dr. Waner’s mantra is that every child has the right to look normal. But this case went beyond aesthetics. If the growth hadn’t been removed, the child was expected to live only 4-6 more years, Dr. Waner said. Without the surgery, she could have suffocated, starved without the ability to swallow, or suffered a fatal bleed.

Dr. O and Dr. Waner are uniquely equipped to do this kind of work, but both are adamant that treating vascular anomalies is a multidisciplinary, multimodal approach. Specialties in anesthesiology, radiology, lasers, facial nerves – they are all critical to these procedures. And often patients with these kinds of lesions require medical and radiologic interventions in addition to surgery. In this particular case, from logistics to post op, “it was a lot of teamwork,” Dr. O said, “a lot of international teams coming together.”
Though extremely difficult, “in the end the result was exactly what we wanted,” Dr. Waner said. Negalem can live a normal life. And as for the surgical duo, both feel very fortunate to do this work. Dr. O said, “I’m honored to have found this specialty and to be able to train with and work with Milton. I’m so happy to do what I do every day.”
A version of this article first appeared on Medscape.com.
In 2019, doctors in London saw a 5-year old girl from rural Ethiopia with an enormous tumor extending from her cheek to her lower jaw. Her name was Negalem and the tumor was a vascular malformation, a life-threatening web of tangled blood vessels.
Surgery to remove it was impossible, the doctors told the foundation advocating for the girl. The child would never make it off the operating table. After a closer examination, the London group still declined to do the procedure, but told the child’s parents and advocates that if anyone was going to attempt this, they’d need to get the little girl to New York.
In New York City, on 64th St. in Manhattan, is the Vascular Birthmark Institute, founded by Milton Waner, MD, who has exclusively treated hemangiomas and vascular malformations for the last 30 years. “I’m the only person in the [United] States whose practice is exclusively [treating] vascular anomalies,” Dr. Waner said in an interview.
Dr. Waner has assembled a multidisciplinary team of experts at the institute’s offices in Lenox Hill – including his wife Teresa O, MD, a facial plastic and reconstructive surgeon and neurospecialist. “People often ask how the hell do you spend so much time with your spouse?” Dr. Waner says. “We work extremely well together. We complement each other.”
Dr. O and Dr. Waner each manage half of the cases at VBI. And in January they received an email about Negalem. After corresponding with the child’s advocate and reviewing images,
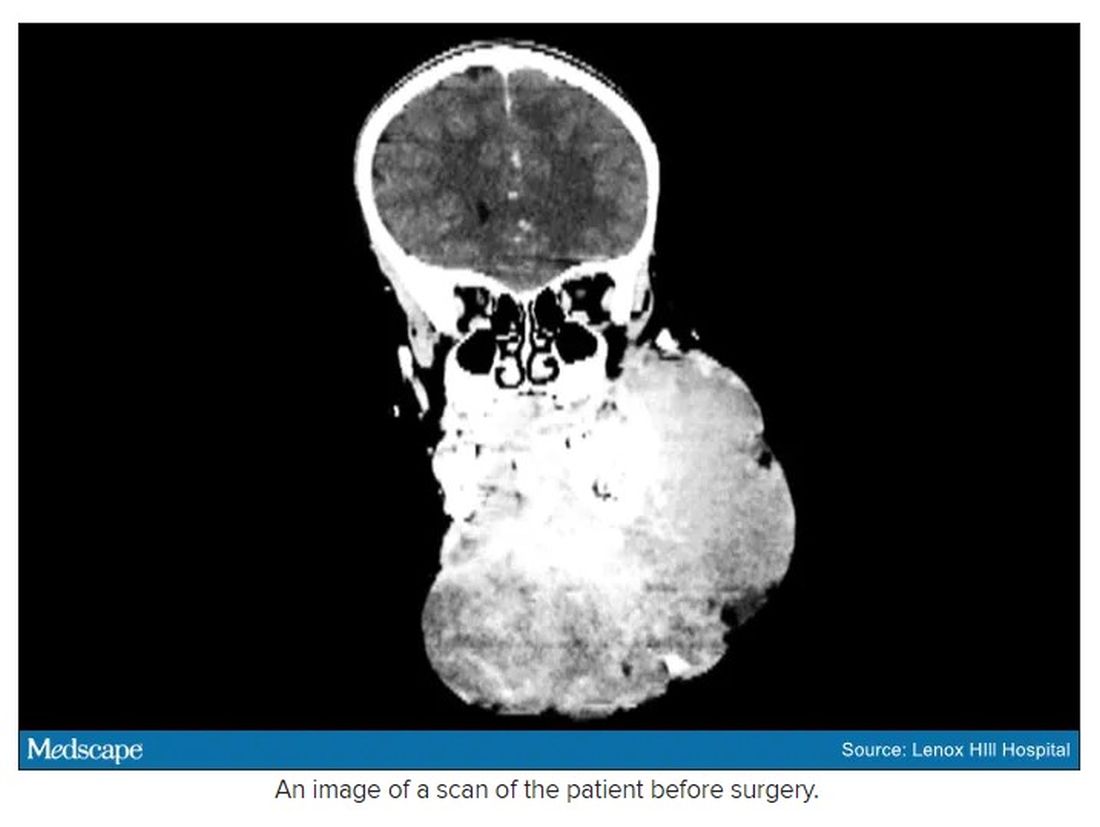
The challenge with vascular malformations in children, Dr. Waner said, is that they have a fraction of the blood an adult has. Where adults have an average of 5 L of blood, a child this age has only 1 L. To lose 200 or 300 mL of blood, “that’s 20% or 30% of their blood volume,” Dr. Waner said. So the removal of such a mass, which requires a meticulous dissection around many blood vessels, carries a high risk of the child bleeding out.
There were some logistical hurdles, but the patient arrived in Manhattan in mid-June, at no cost to her family. The medical visa was organized by a volunteer who also work for USAID. Healing the Children Northeast paid for her travel and the Waner Kids Foundation paid for her hotel stay. Lenox Hill Hospital and Northwell Health covered all hospital costs and postsurgery care. And Dr. O and Dr. Waner did the planning, consult visits, and procedure pro bono.
The surgery was possible because of the generosity of several organizations, but the two surgeons still had a limited time to remove the mass. Under different circumstances, and with the luxury of more time, the patient would have undergone several rounds of sclerotherapy. This procedure, done by interventional radiologists, involves injecting a toxin into the blood vessels, which causes them to clot. Done prior to surgery it can help limit bleeding risk.
On June 23, the morning of the surgery, the patient underwent one round of sclerotherapy. However, it didn’t have the intended effect, Dr. Waner said, “because the lesion was just so massive.”
The team had planned several of their moves ahead of time. But this isn’t the sort of surgery you’d find in a textbook. Because it’s such a unique field, Dr. Waner and Dr. O have developed many of their own techniques along the way. This patient was much like the cases they treat every day, only “several orders of magnitudes greater,” Dr. Waner said. “On a scale of 1 to 10 she was a 12.”
The morning of the surgery, “I was very apprehensive,” Dr. Waner recalled. He vividly remembers the girl’s father repeatedly kissing her to say goodbye as she lay on the operating table, fully aware that this procedure was a life-threatening one. And from the beginning there were challenges, like getting her under anesthesia when the anatomy of her mouth, deformed by the tumor, didn’t allow the anesthesiologists to use their typical tubing. Then, once the skin was removed, it became clear how dilated and tangled the involved blood vessels were. There were many vital structures tangled in the anomaly. “The jugular vein was right there. The carotid artery was right there,” Dr. Waner said. It was extremely difficult to delineate and preserve them, he said.
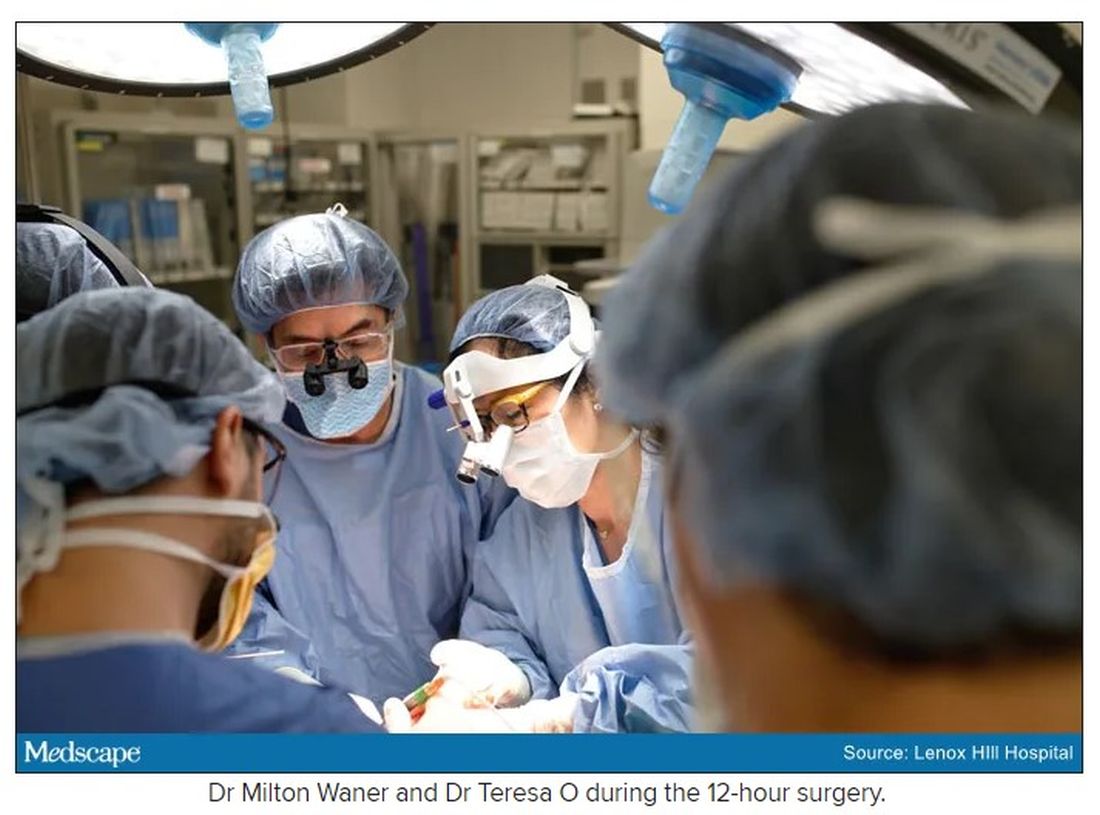
“That’s why we really took our time. We just went very slowly and deliberately,” Dr. O said. The blood vessels were so dilated that their only option was to move painstakingly slow – otherwise a small nick could be devastating.
But even with the slow pace the surgery was “excruciatingly difficult,” Dr. Waner said. And early on in the dissection he wasn’t quite sure they’d make it out. The sclerotherapy hadn’t done much to prevent bleeding. “At one point every millimeter or 2 that we advanced we got into some bleeding,” Dr. Waner said. “Brisk bleeding.”
Once they got into the surgery they also realized that the growth had adhered to the jaw bone. “There were vessels traversing into the bone, which were hard to control,” Dr. O said.
But finally, both doctors realized they’d be able to remove it. With the lesion removed they began the work of reconstruction and reanimation.
The child’s jaw and cheek bone had grown beyond their normal size to support the growth. They had to shave them down to achieve facial symmetry. The tumor had also inhibited much of the child’s facial nerve control. With it gone, Dr. O began the work of finding all the facial nerve branches and assembling them to reanimate the child’s face.
Before medicine, Dr. O trained as an architect, which, according to Dr. Waner, has equipped her with very good spatial awareness – a valuable skill in the surgical reconstruction phase. After seeing a lecture by Dr. Waner, she immediately saw a fit for her unique interest and skill set. She did fellowship training with Dr. Waner in vascular anomalies, and then went on to specialize in facial nerve reanimation. The proof of Dr. O’s expertise is Negalem’s new, beautiful smile, Dr. Waner said.
The surgery drew out over 8 hours, as long as a day of surgeries for the two doctors. When Dr. O finally walked into the waiting room to inform the family of the success, the first words out of the father’s mouth were: “Is my daughter alive?”
A growth like Negalem had is not compatible with a normal life. Dr. Waner’s mantra is that every child has the right to look normal. But this case went beyond aesthetics. If the growth hadn’t been removed, the child was expected to live only 4-6 more years, Dr. Waner said. Without the surgery, she could have suffocated, starved without the ability to swallow, or suffered a fatal bleed.

Dr. O and Dr. Waner are uniquely equipped to do this kind of work, but both are adamant that treating vascular anomalies is a multidisciplinary, multimodal approach. Specialties in anesthesiology, radiology, lasers, facial nerves – they are all critical to these procedures. And often patients with these kinds of lesions require medical and radiologic interventions in addition to surgery. In this particular case, from logistics to post op, “it was a lot of teamwork,” Dr. O said, “a lot of international teams coming together.”
Though extremely difficult, “in the end the result was exactly what we wanted,” Dr. Waner said. Negalem can live a normal life. And as for the surgical duo, both feel very fortunate to do this work. Dr. O said, “I’m honored to have found this specialty and to be able to train with and work with Milton. I’m so happy to do what I do every day.”
A version of this article first appeared on Medscape.com.
In 2019, doctors in London saw a 5-year old girl from rural Ethiopia with an enormous tumor extending from her cheek to her lower jaw. Her name was Negalem and the tumor was a vascular malformation, a life-threatening web of tangled blood vessels.
Surgery to remove it was impossible, the doctors told the foundation advocating for the girl. The child would never make it off the operating table. After a closer examination, the London group still declined to do the procedure, but told the child’s parents and advocates that if anyone was going to attempt this, they’d need to get the little girl to New York.
In New York City, on 64th St. in Manhattan, is the Vascular Birthmark Institute, founded by Milton Waner, MD, who has exclusively treated hemangiomas and vascular malformations for the last 30 years. “I’m the only person in the [United] States whose practice is exclusively [treating] vascular anomalies,” Dr. Waner said in an interview.
Dr. Waner has assembled a multidisciplinary team of experts at the institute’s offices in Lenox Hill – including his wife Teresa O, MD, a facial plastic and reconstructive surgeon and neurospecialist. “People often ask how the hell do you spend so much time with your spouse?” Dr. Waner says. “We work extremely well together. We complement each other.”
Dr. O and Dr. Waner each manage half of the cases at VBI. And in January they received an email about Negalem. After corresponding with the child’s advocate and reviewing images,
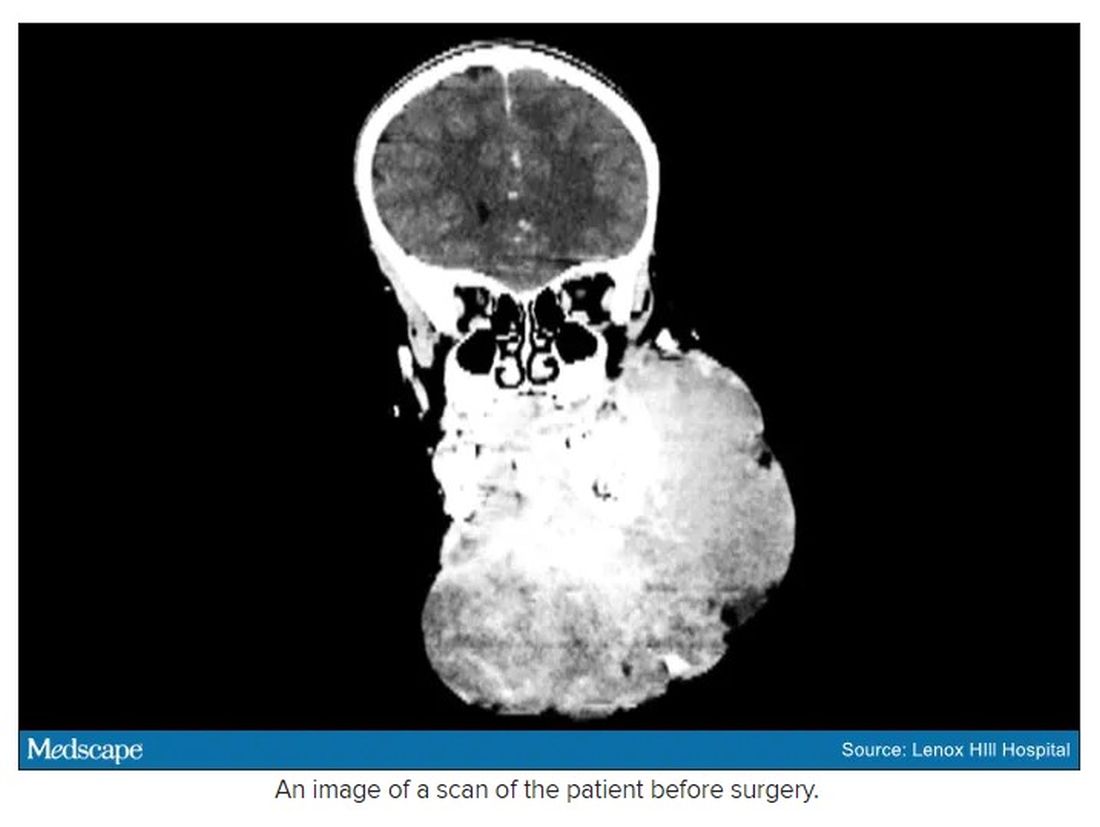
The challenge with vascular malformations in children, Dr. Waner said, is that they have a fraction of the blood an adult has. Where adults have an average of 5 L of blood, a child this age has only 1 L. To lose 200 or 300 mL of blood, “that’s 20% or 30% of their blood volume,” Dr. Waner said. So the removal of such a mass, which requires a meticulous dissection around many blood vessels, carries a high risk of the child bleeding out.
There were some logistical hurdles, but the patient arrived in Manhattan in mid-June, at no cost to her family. The medical visa was organized by a volunteer who also work for USAID. Healing the Children Northeast paid for her travel and the Waner Kids Foundation paid for her hotel stay. Lenox Hill Hospital and Northwell Health covered all hospital costs and postsurgery care. And Dr. O and Dr. Waner did the planning, consult visits, and procedure pro bono.
The surgery was possible because of the generosity of several organizations, but the two surgeons still had a limited time to remove the mass. Under different circumstances, and with the luxury of more time, the patient would have undergone several rounds of sclerotherapy. This procedure, done by interventional radiologists, involves injecting a toxin into the blood vessels, which causes them to clot. Done prior to surgery it can help limit bleeding risk.
On June 23, the morning of the surgery, the patient underwent one round of sclerotherapy. However, it didn’t have the intended effect, Dr. Waner said, “because the lesion was just so massive.”
The team had planned several of their moves ahead of time. But this isn’t the sort of surgery you’d find in a textbook. Because it’s such a unique field, Dr. Waner and Dr. O have developed many of their own techniques along the way. This patient was much like the cases they treat every day, only “several orders of magnitudes greater,” Dr. Waner said. “On a scale of 1 to 10 she was a 12.”
The morning of the surgery, “I was very apprehensive,” Dr. Waner recalled. He vividly remembers the girl’s father repeatedly kissing her to say goodbye as she lay on the operating table, fully aware that this procedure was a life-threatening one. And from the beginning there were challenges, like getting her under anesthesia when the anatomy of her mouth, deformed by the tumor, didn’t allow the anesthesiologists to use their typical tubing. Then, once the skin was removed, it became clear how dilated and tangled the involved blood vessels were. There were many vital structures tangled in the anomaly. “The jugular vein was right there. The carotid artery was right there,” Dr. Waner said. It was extremely difficult to delineate and preserve them, he said.
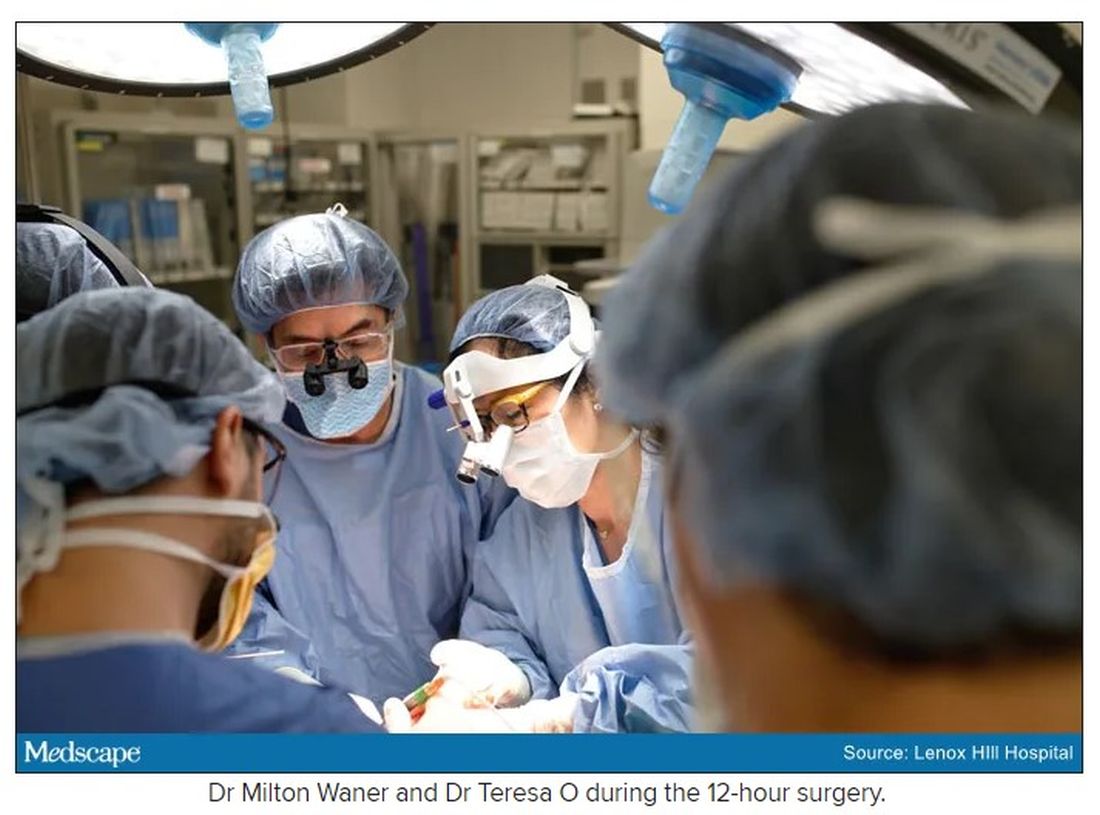
“That’s why we really took our time. We just went very slowly and deliberately,” Dr. O said. The blood vessels were so dilated that their only option was to move painstakingly slow – otherwise a small nick could be devastating.
But even with the slow pace the surgery was “excruciatingly difficult,” Dr. Waner said. And early on in the dissection he wasn’t quite sure they’d make it out. The sclerotherapy hadn’t done much to prevent bleeding. “At one point every millimeter or 2 that we advanced we got into some bleeding,” Dr. Waner said. “Brisk bleeding.”
Once they got into the surgery they also realized that the growth had adhered to the jaw bone. “There were vessels traversing into the bone, which were hard to control,” Dr. O said.
But finally, both doctors realized they’d be able to remove it. With the lesion removed they began the work of reconstruction and reanimation.
The child’s jaw and cheek bone had grown beyond their normal size to support the growth. They had to shave them down to achieve facial symmetry. The tumor had also inhibited much of the child’s facial nerve control. With it gone, Dr. O began the work of finding all the facial nerve branches and assembling them to reanimate the child’s face.
Before medicine, Dr. O trained as an architect, which, according to Dr. Waner, has equipped her with very good spatial awareness – a valuable skill in the surgical reconstruction phase. After seeing a lecture by Dr. Waner, she immediately saw a fit for her unique interest and skill set. She did fellowship training with Dr. Waner in vascular anomalies, and then went on to specialize in facial nerve reanimation. The proof of Dr. O’s expertise is Negalem’s new, beautiful smile, Dr. Waner said.
The surgery drew out over 8 hours, as long as a day of surgeries for the two doctors. When Dr. O finally walked into the waiting room to inform the family of the success, the first words out of the father’s mouth were: “Is my daughter alive?”
A growth like Negalem had is not compatible with a normal life. Dr. Waner’s mantra is that every child has the right to look normal. But this case went beyond aesthetics. If the growth hadn’t been removed, the child was expected to live only 4-6 more years, Dr. Waner said. Without the surgery, she could have suffocated, starved without the ability to swallow, or suffered a fatal bleed.

Dr. O and Dr. Waner are uniquely equipped to do this kind of work, but both are adamant that treating vascular anomalies is a multidisciplinary, multimodal approach. Specialties in anesthesiology, radiology, lasers, facial nerves – they are all critical to these procedures. And often patients with these kinds of lesions require medical and radiologic interventions in addition to surgery. In this particular case, from logistics to post op, “it was a lot of teamwork,” Dr. O said, “a lot of international teams coming together.”
Though extremely difficult, “in the end the result was exactly what we wanted,” Dr. Waner said. Negalem can live a normal life. And as for the surgical duo, both feel very fortunate to do this work. Dr. O said, “I’m honored to have found this specialty and to be able to train with and work with Milton. I’m so happy to do what I do every day.”
A version of this article first appeared on Medscape.com.
Conflicting medical opinions: Black lungs, Big Coal, and bias
In 2008, the U.S. Department of Labor (DOL) paid for Tony Adams, a 48-year-old coal miner, to have a chest x-ray. His doctor found stage I black lung disease. Yet Mr. Adams’ claim for medical benefits was denied. This was because the insurance group that represented his employer hired a different – more credentialed – doctor as its medical expert. That doctor said he saw no such evidence. The judge ruled in favor of the mining company on the basis of the latter’s “expertise.”
Before he died 5 years later, at age 53, Mr. Adams went through this process again. In fact, he did it four more times. Each time, his doctor found evidence of black lung, but the company’s medical expert did not. He died without receiving benefits. Among the causes of death listed on his autopsy were cardiopulmonary arrest and coal worker’s pneumoconiosis (CWP): black lung.
Since his death in 2013, two judges have awarded Mr. Adams’ benefits to his widow, Linda. Both times, the mining company appealed the decision, most recently in December 2020. She’s not giving up. “Two weeks before he died, he told me, ‘I’m going to die of black lung,’ ” Linda recalled. “‘But I don’t want you to give up on black lung. There are too many people screwing these miners out of what they deserve.’”
There has long been suspicion among miners and their advocates that doctors used by coal companies to fight claims like Mr. Adams’ are in the pocket of “Big Coal.” At the very least, some say these physicians are swayed by their client’s preference when reading a coal miner’s chest x-ray. A recent study published in Annals of the American Thoracic Society provides empirical evidence that these doctors’ conflict of interest – namely, that parties representing coal companies hired them – appears to influence their medical opinion.
Proof of a ‘broken system’
The Annals study examined 63,780 radiograph classifications made by 264 physicians – all certified as B-readers, a certification by the National Institute for Occupational Safety and Health (NIOSH) for physicians who demonstrate proficiency in classifying radiographs of pneumoconiosis. The results showed that doctors hired by miners identified black lung 49% of the time; those hired by coal companies identified black lung only 15% of the time.
The study also found that B-readers contracted by employers read results differently for different clients. The same doctors were significantly less likely to say a miner’s lungs were negative for CWP when they were hired by the DOL (77.2%) than when they were hired by a coal company or its insurers (90.2%).
The bias does appear to work both ways: B-readers hired by miners and miners’ attorneys were more likely to find evidence of black lung when they worked with plaintiffs. However, a much higher number of doctors appeared to be biased in favor of the companies. “There were 3X more B-readers providing 8X more classifications among those affiliated with employers compared to those affiliated with miners,” the study concluded.
The authors suggest that one reason for this was the difference in pay. Some company-hired doctors made as much as $750 per reading, about 10 times what miner-hired doctors were paid.
“We knew [about the potential bias] from our work over the decades taking care of these guys,” said Robert A. Cohen, MD, a pulmonologist and the study’s senior author. “But then you see it with P values that are incredibly statistically significant ...”
The study finally put numbers to a problem that many working with black lung claims had always assumed. Those within the system are accustomed to seeing names of the same doctors on documents and reports, with little to no overlap between those hired by the defense and the plaintiffs.
“The vast majority of the time, we know what a report will say based on the doctor’s name,” said Evan Smith, JD, advocacy director at AppalReD Legal Aid, in Prestonsburg, Ky.. It is far more surprising, he said, when a defense-hired doctor agrees with a miner-hired doctor.
Over the years, Katherine DePonte, MD, a radiologist and B-reader in West Virginia, has often seen an “almost textbook appearance” of CWP, only to later learn that “another radiologist read it as negative.” She explained, “They would use some other term, like ‘old granulomatous disease.’”
Employer-hired doctors often do acknowledge the same lung damage on the radiograph as miner-hired docs; they simply don’t attribute it to coal dust. Common “alternative diagnoses” include chronic obstructive pulmonary disease or histoplasmosis. “I know a number don’t believe this disease of coal worker pneumoconiosis exists [at all],” Dr. DePonte said.
What’s inarguable is that, even as coal mining in Appalachia is on the decline, black lung disease is on the rise. NIOSH now estimates that it affects over 20% of long-term (25+ years) coal workers in central Appalachia. That’s the highest prevalence in a quarter of a century.
Mr. Smith said that at its most basic level, these doctors’ conflicts of interest “lead to people who have the disease that these benefits are for, having them denied.” People like Tony Adams. Whether the doctors involved are complicit or just conservative, critics say they have become a fixture of a broken system.
Financial bias or difference of opinion?
Broken system or not, evidence suggests that the problem can’t be blamed solely on medical experts. Dr. DePonte primarily reads for the DOL and miners. “Not that I necessarily chose that,” she said. “You get pigeonholed.”
Some say that the bias demonstrated by the Annals study is at least partially driven by the litigation process itself. It is an adversarial system. As such, attorneys on both sides are naturally inclined to seek out doctors who will best support their clients’ cases. Doctors with a legitimately conservative perspective on what constitutes black lung are more sought after by the coal companies’ attorneys.
“It can often be impossible to tell whether the money is driving a change in the behavior or if the behavior is causing them to be sought out,” said Matt McCoy, PhD, a medical ethicist who specializes in conflicts of interest at the University of Pennsylvania, Philadelphia.
Although some believe that certain doctors are driven purely by financial incentive and offer a specific reading to secure repeat business, B-readers can end up working exclusively for companies because of other reasons. Wes Addington, JD, an attorney at the Appalachian Citizens’ Law Center, Whitesburg, Ky., said some doctors appear to have an authentically different – often antiquated – view of the disease.
Perhaps the most extreme example is Paul Wheeler, MD, a highly credentialed Johns Hopkins radiologist who was exposed for false medical testimony in Chris Hamby’s 2013 Pulitzer Prize reporting. In 1,500 readings, Dr. Wheeler never diagnosed a single case of severe black lung. And yet, Dr. Cohen, Mr. Addington, Mr. Smith, and other experts all agree that Dr. Wheeler appeared to wholeheartedly believe that his view of black lung was accurate. That made him a valuable asset to mining companies.
Since Dr. Wheeler’s exposure, there has been a greater sense of accountability among B-readers, said John Cline, JD, a West Virginia–based attorney who represents miners with federal black lung claims. “Radiologists were thinking, ‘Somebody could be watching me.’ Even if they thought they were doing this in the shadows, it made people more cautious,” he said.
The data used in the Annals study predate Mr. Hamby’s investigation, going back to 2000. Thus, it is possible that, as Mr. Cline argues, things may be different now. However, Lee S. Friedman, PhD, associate professor at the University of Illinois at Chicago, who is the lead author of the study, remains skeptical.
“While the Wheeler case might have dampened some physicians [who were] completely skewing their readings always negative, I think it’s premature or incorrect” to say it resolved the issue, he said. “Did they all change their behavior the morning after? It doesn’t seem likely, given the evidence of financial conflicts of interest and behavior that’s been demonstrated.”
Skewing the evidence?
Mr. Hamby’s 2013 reporting also revealed that even when company-hired doctors did diagnose CWP, law firms were burying those readings. In 2016, the DOL attempted to stop this practice. The agency made suppression of written evidence illegal – emphasis on written.
Law firms can’t hide positive reports, but they can prevent them. Dr. Cohen explained that now, “a doctor on the phone says, ‘I will read this as positive.’ Then the company says, ‘No, thank you,’ we will send you a check.”
This practice was confirmed by Kim Adcock, MD, a retired radiologist and B-reader in Littleton, Colo., who primarily reads for 26 law firms. Some of his clients want a report no matter how he reads the radiograph. However, some want him to call them first if he’s going to read the radiograph as positive. Dr. Adcock said this practice skews the dataset to make company-hired docs appear to read more negatively than they actually do.
Because the dataset used in the study is from the Federal Black Lung Program (FBLP), it includes only readings that made it to court. Dr. Adcock said he reads approximately 2,000 radiographs a year, although only a few of his readings appeared in the study’s dataset, according to a search by Dr. Friedman. This difference is likely because the study evaluated only readings between 2000 and 2013, the year Dr. Adcock started B-reading.
“I think it’s important to get a message that, to a certain extent, contravenes this paper. Yes, we should have some reservations about the conclusions,” Dr. Adcock explained. “There are people out there attempting to do the best job they could do.”
Law firms shopping for the reading they want and censoring the ones they don’t might alter the FBLP data, but experts say that doesn’t change the underlying problem. “In any case like this, where you’re looking at individuals going up against corporations,” Dr. McCoy said, “[corporations] are able to marshal their resources and hire more officials in a way claimants can’t, and that’s a baseline concern here.”
Battling bias
Admitting bias is notoriously difficult; thus, it isn’t surprising that many doctors involved refuse to believe they are influenced by money, incentives, or other biases. Dr. DePonte said she’s not swayed by money, nor does she actively take a pro-miner stance. She views herself as more of an advocate for accuracy. However, she did say that it has traditionally been far more difficult for miners to prove their cases, a problem that has improved with new regulations in recent years.
In Colorado, Dr. Adcock’s approach is to stay as far removed from the litigation process as possible. He said he has limited understanding of how his reports are used or how claims are filed and awarded. He leans heavily on his initial – almost instantaneous – impression of a chest x-ray.
Dr. DePonte and Dr. Adcock were both hired as experts on Tony Adams’ case. In 2008, Dr. DePonte read his chest x-ray as positive for early-stage black lung (1/0). Dr. Adcock also read two of Adams’ four chest x-rays, one in 2009 and the other in 2013. He read them as negative. When asked about the case, which autopsy confirmed as black lung, Dr. Adcock explained that positive histopathology doesn’t mean the radiograph reading was wrong, only that the disease didn’t show on that radiograph. He said his “highest ambition” is to be “an objective finder of fact” and that he trusts the process to work out the truth.
That process didn’t work in time for Tony Adams. Dr. Friedman argues that people who provide expert testimony have an ethical responsibility to know how their testimony is being used; to do otherwise, he says, is “willful ignorance.” Still, the Annals study authors, along with Dr. DePonte, Mr. Cline, and West Virginia attorney Sam Petsonk, say that the process is getting fairer, thanks to new policies developed over the past 5 years by the DOL.
“The DOL has worked very hard to reconcile the final award rate (around 30%) with the incidence of disease in the population (between 20% and 25%),” Mr. Petsonk said. Although the study calls into question the integrity of the system and the doctors within it, it’s critical for miners to know that the system is working and that they can get benefits, he explained. Many fear that cynicism about the system drives miners away and causes them to resort to Social Security or long-term disability.
Fixing what’s broken
The Annals study’s authors propose some solutions to the problems they quantified. The first is a sort of “super panel” that collectively evaluates readings. Although a completely unbiased panel would be nice, such impartiality is likely unsustainable, Mr. Smith said. He believes that over time, the panel would become vulnerable to politics and would work in favor of the companies.
Even without a panel, a method to provide greater transparency could be a great start, some suggest. The DOL could make the entire FBLP database public and analyze it annually. The authors also propose a flat fee for readings. Even now, Dr. Adcock said he doesn’t make anywhere close to the upper limit of $750 per readings. “My understanding is around $125 is a pretty characteristic fee [for reading a chest x-ray],” he elaborated. “Everyone I’ve had a conversation with is within 25 bucks [of that].”
That said, Dr. Adcock is not currently listed among the heavy readers who appear in the data used for the study; it’s possible that his experience is not representative. Some readers who were included in that dataset read more than 10 times the average number of classifications per reader – the average was 242 classifications – and read 95% of chest x-rays as negative, according to Dr. Friedman. This news organization obtained the names of two doctors whose readings were 95% negative on a high volume of cases. Neither agreed to an interview.
It’s possible that if the dataset had included readings from more recent years, Dr. Adcock would have appeared more frequently, given his personal estimates. That’s why the study authors recommend that the DOL conduct this kind of analysis annually in order to get an accurate picture of who is contributing to these cases, in what way, and how often. By doing so, readers who appear biased could be identified and addressed with more regularity, Dr. Friedman said.
Even if the rate were more consistent and the data were more frequently analyzed, the very nature of the adversarial system will put any potential solution at risk. “I’m not sure there’s a foolproof system that can be devised that can’t be corrupted in time,” Mr. Cline said.
A version of this article first appeared on Medscape.com.
In 2008, the U.S. Department of Labor (DOL) paid for Tony Adams, a 48-year-old coal miner, to have a chest x-ray. His doctor found stage I black lung disease. Yet Mr. Adams’ claim for medical benefits was denied. This was because the insurance group that represented his employer hired a different – more credentialed – doctor as its medical expert. That doctor said he saw no such evidence. The judge ruled in favor of the mining company on the basis of the latter’s “expertise.”
Before he died 5 years later, at age 53, Mr. Adams went through this process again. In fact, he did it four more times. Each time, his doctor found evidence of black lung, but the company’s medical expert did not. He died without receiving benefits. Among the causes of death listed on his autopsy were cardiopulmonary arrest and coal worker’s pneumoconiosis (CWP): black lung.
Since his death in 2013, two judges have awarded Mr. Adams’ benefits to his widow, Linda. Both times, the mining company appealed the decision, most recently in December 2020. She’s not giving up. “Two weeks before he died, he told me, ‘I’m going to die of black lung,’ ” Linda recalled. “‘But I don’t want you to give up on black lung. There are too many people screwing these miners out of what they deserve.’”
There has long been suspicion among miners and their advocates that doctors used by coal companies to fight claims like Mr. Adams’ are in the pocket of “Big Coal.” At the very least, some say these physicians are swayed by their client’s preference when reading a coal miner’s chest x-ray. A recent study published in Annals of the American Thoracic Society provides empirical evidence that these doctors’ conflict of interest – namely, that parties representing coal companies hired them – appears to influence their medical opinion.
Proof of a ‘broken system’
The Annals study examined 63,780 radiograph classifications made by 264 physicians – all certified as B-readers, a certification by the National Institute for Occupational Safety and Health (NIOSH) for physicians who demonstrate proficiency in classifying radiographs of pneumoconiosis. The results showed that doctors hired by miners identified black lung 49% of the time; those hired by coal companies identified black lung only 15% of the time.
The study also found that B-readers contracted by employers read results differently for different clients. The same doctors were significantly less likely to say a miner’s lungs were negative for CWP when they were hired by the DOL (77.2%) than when they were hired by a coal company or its insurers (90.2%).
The bias does appear to work both ways: B-readers hired by miners and miners’ attorneys were more likely to find evidence of black lung when they worked with plaintiffs. However, a much higher number of doctors appeared to be biased in favor of the companies. “There were 3X more B-readers providing 8X more classifications among those affiliated with employers compared to those affiliated with miners,” the study concluded.
The authors suggest that one reason for this was the difference in pay. Some company-hired doctors made as much as $750 per reading, about 10 times what miner-hired doctors were paid.
“We knew [about the potential bias] from our work over the decades taking care of these guys,” said Robert A. Cohen, MD, a pulmonologist and the study’s senior author. “But then you see it with P values that are incredibly statistically significant ...”
The study finally put numbers to a problem that many working with black lung claims had always assumed. Those within the system are accustomed to seeing names of the same doctors on documents and reports, with little to no overlap between those hired by the defense and the plaintiffs.
“The vast majority of the time, we know what a report will say based on the doctor’s name,” said Evan Smith, JD, advocacy director at AppalReD Legal Aid, in Prestonsburg, Ky.. It is far more surprising, he said, when a defense-hired doctor agrees with a miner-hired doctor.
Over the years, Katherine DePonte, MD, a radiologist and B-reader in West Virginia, has often seen an “almost textbook appearance” of CWP, only to later learn that “another radiologist read it as negative.” She explained, “They would use some other term, like ‘old granulomatous disease.’”
Employer-hired doctors often do acknowledge the same lung damage on the radiograph as miner-hired docs; they simply don’t attribute it to coal dust. Common “alternative diagnoses” include chronic obstructive pulmonary disease or histoplasmosis. “I know a number don’t believe this disease of coal worker pneumoconiosis exists [at all],” Dr. DePonte said.
What’s inarguable is that, even as coal mining in Appalachia is on the decline, black lung disease is on the rise. NIOSH now estimates that it affects over 20% of long-term (25+ years) coal workers in central Appalachia. That’s the highest prevalence in a quarter of a century.
Mr. Smith said that at its most basic level, these doctors’ conflicts of interest “lead to people who have the disease that these benefits are for, having them denied.” People like Tony Adams. Whether the doctors involved are complicit or just conservative, critics say they have become a fixture of a broken system.
Financial bias or difference of opinion?
Broken system or not, evidence suggests that the problem can’t be blamed solely on medical experts. Dr. DePonte primarily reads for the DOL and miners. “Not that I necessarily chose that,” she said. “You get pigeonholed.”
Some say that the bias demonstrated by the Annals study is at least partially driven by the litigation process itself. It is an adversarial system. As such, attorneys on both sides are naturally inclined to seek out doctors who will best support their clients’ cases. Doctors with a legitimately conservative perspective on what constitutes black lung are more sought after by the coal companies’ attorneys.
“It can often be impossible to tell whether the money is driving a change in the behavior or if the behavior is causing them to be sought out,” said Matt McCoy, PhD, a medical ethicist who specializes in conflicts of interest at the University of Pennsylvania, Philadelphia.
Although some believe that certain doctors are driven purely by financial incentive and offer a specific reading to secure repeat business, B-readers can end up working exclusively for companies because of other reasons. Wes Addington, JD, an attorney at the Appalachian Citizens’ Law Center, Whitesburg, Ky., said some doctors appear to have an authentically different – often antiquated – view of the disease.
Perhaps the most extreme example is Paul Wheeler, MD, a highly credentialed Johns Hopkins radiologist who was exposed for false medical testimony in Chris Hamby’s 2013 Pulitzer Prize reporting. In 1,500 readings, Dr. Wheeler never diagnosed a single case of severe black lung. And yet, Dr. Cohen, Mr. Addington, Mr. Smith, and other experts all agree that Dr. Wheeler appeared to wholeheartedly believe that his view of black lung was accurate. That made him a valuable asset to mining companies.
Since Dr. Wheeler’s exposure, there has been a greater sense of accountability among B-readers, said John Cline, JD, a West Virginia–based attorney who represents miners with federal black lung claims. “Radiologists were thinking, ‘Somebody could be watching me.’ Even if they thought they were doing this in the shadows, it made people more cautious,” he said.
The data used in the Annals study predate Mr. Hamby’s investigation, going back to 2000. Thus, it is possible that, as Mr. Cline argues, things may be different now. However, Lee S. Friedman, PhD, associate professor at the University of Illinois at Chicago, who is the lead author of the study, remains skeptical.
“While the Wheeler case might have dampened some physicians [who were] completely skewing their readings always negative, I think it’s premature or incorrect” to say it resolved the issue, he said. “Did they all change their behavior the morning after? It doesn’t seem likely, given the evidence of financial conflicts of interest and behavior that’s been demonstrated.”
Skewing the evidence?
Mr. Hamby’s 2013 reporting also revealed that even when company-hired doctors did diagnose CWP, law firms were burying those readings. In 2016, the DOL attempted to stop this practice. The agency made suppression of written evidence illegal – emphasis on written.
Law firms can’t hide positive reports, but they can prevent them. Dr. Cohen explained that now, “a doctor on the phone says, ‘I will read this as positive.’ Then the company says, ‘No, thank you,’ we will send you a check.”
This practice was confirmed by Kim Adcock, MD, a retired radiologist and B-reader in Littleton, Colo., who primarily reads for 26 law firms. Some of his clients want a report no matter how he reads the radiograph. However, some want him to call them first if he’s going to read the radiograph as positive. Dr. Adcock said this practice skews the dataset to make company-hired docs appear to read more negatively than they actually do.
Because the dataset used in the study is from the Federal Black Lung Program (FBLP), it includes only readings that made it to court. Dr. Adcock said he reads approximately 2,000 radiographs a year, although only a few of his readings appeared in the study’s dataset, according to a search by Dr. Friedman. This difference is likely because the study evaluated only readings between 2000 and 2013, the year Dr. Adcock started B-reading.
“I think it’s important to get a message that, to a certain extent, contravenes this paper. Yes, we should have some reservations about the conclusions,” Dr. Adcock explained. “There are people out there attempting to do the best job they could do.”
Law firms shopping for the reading they want and censoring the ones they don’t might alter the FBLP data, but experts say that doesn’t change the underlying problem. “In any case like this, where you’re looking at individuals going up against corporations,” Dr. McCoy said, “[corporations] are able to marshal their resources and hire more officials in a way claimants can’t, and that’s a baseline concern here.”
Battling bias
Admitting bias is notoriously difficult; thus, it isn’t surprising that many doctors involved refuse to believe they are influenced by money, incentives, or other biases. Dr. DePonte said she’s not swayed by money, nor does she actively take a pro-miner stance. She views herself as more of an advocate for accuracy. However, she did say that it has traditionally been far more difficult for miners to prove their cases, a problem that has improved with new regulations in recent years.
In Colorado, Dr. Adcock’s approach is to stay as far removed from the litigation process as possible. He said he has limited understanding of how his reports are used or how claims are filed and awarded. He leans heavily on his initial – almost instantaneous – impression of a chest x-ray.
Dr. DePonte and Dr. Adcock were both hired as experts on Tony Adams’ case. In 2008, Dr. DePonte read his chest x-ray as positive for early-stage black lung (1/0). Dr. Adcock also read two of Adams’ four chest x-rays, one in 2009 and the other in 2013. He read them as negative. When asked about the case, which autopsy confirmed as black lung, Dr. Adcock explained that positive histopathology doesn’t mean the radiograph reading was wrong, only that the disease didn’t show on that radiograph. He said his “highest ambition” is to be “an objective finder of fact” and that he trusts the process to work out the truth.
That process didn’t work in time for Tony Adams. Dr. Friedman argues that people who provide expert testimony have an ethical responsibility to know how their testimony is being used; to do otherwise, he says, is “willful ignorance.” Still, the Annals study authors, along with Dr. DePonte, Mr. Cline, and West Virginia attorney Sam Petsonk, say that the process is getting fairer, thanks to new policies developed over the past 5 years by the DOL.
“The DOL has worked very hard to reconcile the final award rate (around 30%) with the incidence of disease in the population (between 20% and 25%),” Mr. Petsonk said. Although the study calls into question the integrity of the system and the doctors within it, it’s critical for miners to know that the system is working and that they can get benefits, he explained. Many fear that cynicism about the system drives miners away and causes them to resort to Social Security or long-term disability.
Fixing what’s broken
The Annals study’s authors propose some solutions to the problems they quantified. The first is a sort of “super panel” that collectively evaluates readings. Although a completely unbiased panel would be nice, such impartiality is likely unsustainable, Mr. Smith said. He believes that over time, the panel would become vulnerable to politics and would work in favor of the companies.
Even without a panel, a method to provide greater transparency could be a great start, some suggest. The DOL could make the entire FBLP database public and analyze it annually. The authors also propose a flat fee for readings. Even now, Dr. Adcock said he doesn’t make anywhere close to the upper limit of $750 per readings. “My understanding is around $125 is a pretty characteristic fee [for reading a chest x-ray],” he elaborated. “Everyone I’ve had a conversation with is within 25 bucks [of that].”
That said, Dr. Adcock is not currently listed among the heavy readers who appear in the data used for the study; it’s possible that his experience is not representative. Some readers who were included in that dataset read more than 10 times the average number of classifications per reader – the average was 242 classifications – and read 95% of chest x-rays as negative, according to Dr. Friedman. This news organization obtained the names of two doctors whose readings were 95% negative on a high volume of cases. Neither agreed to an interview.
It’s possible that if the dataset had included readings from more recent years, Dr. Adcock would have appeared more frequently, given his personal estimates. That’s why the study authors recommend that the DOL conduct this kind of analysis annually in order to get an accurate picture of who is contributing to these cases, in what way, and how often. By doing so, readers who appear biased could be identified and addressed with more regularity, Dr. Friedman said.
Even if the rate were more consistent and the data were more frequently analyzed, the very nature of the adversarial system will put any potential solution at risk. “I’m not sure there’s a foolproof system that can be devised that can’t be corrupted in time,” Mr. Cline said.
A version of this article first appeared on Medscape.com.
In 2008, the U.S. Department of Labor (DOL) paid for Tony Adams, a 48-year-old coal miner, to have a chest x-ray. His doctor found stage I black lung disease. Yet Mr. Adams’ claim for medical benefits was denied. This was because the insurance group that represented his employer hired a different – more credentialed – doctor as its medical expert. That doctor said he saw no such evidence. The judge ruled in favor of the mining company on the basis of the latter’s “expertise.”
Before he died 5 years later, at age 53, Mr. Adams went through this process again. In fact, he did it four more times. Each time, his doctor found evidence of black lung, but the company’s medical expert did not. He died without receiving benefits. Among the causes of death listed on his autopsy were cardiopulmonary arrest and coal worker’s pneumoconiosis (CWP): black lung.
Since his death in 2013, two judges have awarded Mr. Adams’ benefits to his widow, Linda. Both times, the mining company appealed the decision, most recently in December 2020. She’s not giving up. “Two weeks before he died, he told me, ‘I’m going to die of black lung,’ ” Linda recalled. “‘But I don’t want you to give up on black lung. There are too many people screwing these miners out of what they deserve.’”
There has long been suspicion among miners and their advocates that doctors used by coal companies to fight claims like Mr. Adams’ are in the pocket of “Big Coal.” At the very least, some say these physicians are swayed by their client’s preference when reading a coal miner’s chest x-ray. A recent study published in Annals of the American Thoracic Society provides empirical evidence that these doctors’ conflict of interest – namely, that parties representing coal companies hired them – appears to influence their medical opinion.
Proof of a ‘broken system’
The Annals study examined 63,780 radiograph classifications made by 264 physicians – all certified as B-readers, a certification by the National Institute for Occupational Safety and Health (NIOSH) for physicians who demonstrate proficiency in classifying radiographs of pneumoconiosis. The results showed that doctors hired by miners identified black lung 49% of the time; those hired by coal companies identified black lung only 15% of the time.
The study also found that B-readers contracted by employers read results differently for different clients. The same doctors were significantly less likely to say a miner’s lungs were negative for CWP when they were hired by the DOL (77.2%) than when they were hired by a coal company or its insurers (90.2%).
The bias does appear to work both ways: B-readers hired by miners and miners’ attorneys were more likely to find evidence of black lung when they worked with plaintiffs. However, a much higher number of doctors appeared to be biased in favor of the companies. “There were 3X more B-readers providing 8X more classifications among those affiliated with employers compared to those affiliated with miners,” the study concluded.
The authors suggest that one reason for this was the difference in pay. Some company-hired doctors made as much as $750 per reading, about 10 times what miner-hired doctors were paid.
“We knew [about the potential bias] from our work over the decades taking care of these guys,” said Robert A. Cohen, MD, a pulmonologist and the study’s senior author. “But then you see it with P values that are incredibly statistically significant ...”
The study finally put numbers to a problem that many working with black lung claims had always assumed. Those within the system are accustomed to seeing names of the same doctors on documents and reports, with little to no overlap between those hired by the defense and the plaintiffs.
“The vast majority of the time, we know what a report will say based on the doctor’s name,” said Evan Smith, JD, advocacy director at AppalReD Legal Aid, in Prestonsburg, Ky.. It is far more surprising, he said, when a defense-hired doctor agrees with a miner-hired doctor.
Over the years, Katherine DePonte, MD, a radiologist and B-reader in West Virginia, has often seen an “almost textbook appearance” of CWP, only to later learn that “another radiologist read it as negative.” She explained, “They would use some other term, like ‘old granulomatous disease.’”
Employer-hired doctors often do acknowledge the same lung damage on the radiograph as miner-hired docs; they simply don’t attribute it to coal dust. Common “alternative diagnoses” include chronic obstructive pulmonary disease or histoplasmosis. “I know a number don’t believe this disease of coal worker pneumoconiosis exists [at all],” Dr. DePonte said.
What’s inarguable is that, even as coal mining in Appalachia is on the decline, black lung disease is on the rise. NIOSH now estimates that it affects over 20% of long-term (25+ years) coal workers in central Appalachia. That’s the highest prevalence in a quarter of a century.
Mr. Smith said that at its most basic level, these doctors’ conflicts of interest “lead to people who have the disease that these benefits are for, having them denied.” People like Tony Adams. Whether the doctors involved are complicit or just conservative, critics say they have become a fixture of a broken system.
Financial bias or difference of opinion?
Broken system or not, evidence suggests that the problem can’t be blamed solely on medical experts. Dr. DePonte primarily reads for the DOL and miners. “Not that I necessarily chose that,” she said. “You get pigeonholed.”
Some say that the bias demonstrated by the Annals study is at least partially driven by the litigation process itself. It is an adversarial system. As such, attorneys on both sides are naturally inclined to seek out doctors who will best support their clients’ cases. Doctors with a legitimately conservative perspective on what constitutes black lung are more sought after by the coal companies’ attorneys.
“It can often be impossible to tell whether the money is driving a change in the behavior or if the behavior is causing them to be sought out,” said Matt McCoy, PhD, a medical ethicist who specializes in conflicts of interest at the University of Pennsylvania, Philadelphia.
Although some believe that certain doctors are driven purely by financial incentive and offer a specific reading to secure repeat business, B-readers can end up working exclusively for companies because of other reasons. Wes Addington, JD, an attorney at the Appalachian Citizens’ Law Center, Whitesburg, Ky., said some doctors appear to have an authentically different – often antiquated – view of the disease.
Perhaps the most extreme example is Paul Wheeler, MD, a highly credentialed Johns Hopkins radiologist who was exposed for false medical testimony in Chris Hamby’s 2013 Pulitzer Prize reporting. In 1,500 readings, Dr. Wheeler never diagnosed a single case of severe black lung. And yet, Dr. Cohen, Mr. Addington, Mr. Smith, and other experts all agree that Dr. Wheeler appeared to wholeheartedly believe that his view of black lung was accurate. That made him a valuable asset to mining companies.
Since Dr. Wheeler’s exposure, there has been a greater sense of accountability among B-readers, said John Cline, JD, a West Virginia–based attorney who represents miners with federal black lung claims. “Radiologists were thinking, ‘Somebody could be watching me.’ Even if they thought they were doing this in the shadows, it made people more cautious,” he said.
The data used in the Annals study predate Mr. Hamby’s investigation, going back to 2000. Thus, it is possible that, as Mr. Cline argues, things may be different now. However, Lee S. Friedman, PhD, associate professor at the University of Illinois at Chicago, who is the lead author of the study, remains skeptical.
“While the Wheeler case might have dampened some physicians [who were] completely skewing their readings always negative, I think it’s premature or incorrect” to say it resolved the issue, he said. “Did they all change their behavior the morning after? It doesn’t seem likely, given the evidence of financial conflicts of interest and behavior that’s been demonstrated.”
Skewing the evidence?
Mr. Hamby’s 2013 reporting also revealed that even when company-hired doctors did diagnose CWP, law firms were burying those readings. In 2016, the DOL attempted to stop this practice. The agency made suppression of written evidence illegal – emphasis on written.
Law firms can’t hide positive reports, but they can prevent them. Dr. Cohen explained that now, “a doctor on the phone says, ‘I will read this as positive.’ Then the company says, ‘No, thank you,’ we will send you a check.”
This practice was confirmed by Kim Adcock, MD, a retired radiologist and B-reader in Littleton, Colo., who primarily reads for 26 law firms. Some of his clients want a report no matter how he reads the radiograph. However, some want him to call them first if he’s going to read the radiograph as positive. Dr. Adcock said this practice skews the dataset to make company-hired docs appear to read more negatively than they actually do.
Because the dataset used in the study is from the Federal Black Lung Program (FBLP), it includes only readings that made it to court. Dr. Adcock said he reads approximately 2,000 radiographs a year, although only a few of his readings appeared in the study’s dataset, according to a search by Dr. Friedman. This difference is likely because the study evaluated only readings between 2000 and 2013, the year Dr. Adcock started B-reading.
“I think it’s important to get a message that, to a certain extent, contravenes this paper. Yes, we should have some reservations about the conclusions,” Dr. Adcock explained. “There are people out there attempting to do the best job they could do.”
Law firms shopping for the reading they want and censoring the ones they don’t might alter the FBLP data, but experts say that doesn’t change the underlying problem. “In any case like this, where you’re looking at individuals going up against corporations,” Dr. McCoy said, “[corporations] are able to marshal their resources and hire more officials in a way claimants can’t, and that’s a baseline concern here.”
Battling bias
Admitting bias is notoriously difficult; thus, it isn’t surprising that many doctors involved refuse to believe they are influenced by money, incentives, or other biases. Dr. DePonte said she’s not swayed by money, nor does she actively take a pro-miner stance. She views herself as more of an advocate for accuracy. However, she did say that it has traditionally been far more difficult for miners to prove their cases, a problem that has improved with new regulations in recent years.
In Colorado, Dr. Adcock’s approach is to stay as far removed from the litigation process as possible. He said he has limited understanding of how his reports are used or how claims are filed and awarded. He leans heavily on his initial – almost instantaneous – impression of a chest x-ray.
Dr. DePonte and Dr. Adcock were both hired as experts on Tony Adams’ case. In 2008, Dr. DePonte read his chest x-ray as positive for early-stage black lung (1/0). Dr. Adcock also read two of Adams’ four chest x-rays, one in 2009 and the other in 2013. He read them as negative. When asked about the case, which autopsy confirmed as black lung, Dr. Adcock explained that positive histopathology doesn’t mean the radiograph reading was wrong, only that the disease didn’t show on that radiograph. He said his “highest ambition” is to be “an objective finder of fact” and that he trusts the process to work out the truth.
That process didn’t work in time for Tony Adams. Dr. Friedman argues that people who provide expert testimony have an ethical responsibility to know how their testimony is being used; to do otherwise, he says, is “willful ignorance.” Still, the Annals study authors, along with Dr. DePonte, Mr. Cline, and West Virginia attorney Sam Petsonk, say that the process is getting fairer, thanks to new policies developed over the past 5 years by the DOL.
“The DOL has worked very hard to reconcile the final award rate (around 30%) with the incidence of disease in the population (between 20% and 25%),” Mr. Petsonk said. Although the study calls into question the integrity of the system and the doctors within it, it’s critical for miners to know that the system is working and that they can get benefits, he explained. Many fear that cynicism about the system drives miners away and causes them to resort to Social Security or long-term disability.
Fixing what’s broken
The Annals study’s authors propose some solutions to the problems they quantified. The first is a sort of “super panel” that collectively evaluates readings. Although a completely unbiased panel would be nice, such impartiality is likely unsustainable, Mr. Smith said. He believes that over time, the panel would become vulnerable to politics and would work in favor of the companies.
Even without a panel, a method to provide greater transparency could be a great start, some suggest. The DOL could make the entire FBLP database public and analyze it annually. The authors also propose a flat fee for readings. Even now, Dr. Adcock said he doesn’t make anywhere close to the upper limit of $750 per readings. “My understanding is around $125 is a pretty characteristic fee [for reading a chest x-ray],” he elaborated. “Everyone I’ve had a conversation with is within 25 bucks [of that].”
That said, Dr. Adcock is not currently listed among the heavy readers who appear in the data used for the study; it’s possible that his experience is not representative. Some readers who were included in that dataset read more than 10 times the average number of classifications per reader – the average was 242 classifications – and read 95% of chest x-rays as negative, according to Dr. Friedman. This news organization obtained the names of two doctors whose readings were 95% negative on a high volume of cases. Neither agreed to an interview.
It’s possible that if the dataset had included readings from more recent years, Dr. Adcock would have appeared more frequently, given his personal estimates. That’s why the study authors recommend that the DOL conduct this kind of analysis annually in order to get an accurate picture of who is contributing to these cases, in what way, and how often. By doing so, readers who appear biased could be identified and addressed with more regularity, Dr. Friedman said.
Even if the rate were more consistent and the data were more frequently analyzed, the very nature of the adversarial system will put any potential solution at risk. “I’m not sure there’s a foolproof system that can be devised that can’t be corrupted in time,” Mr. Cline said.
A version of this article first appeared on Medscape.com.
The pandemic is making periods unbearable for some women
Stories of how the pandemic has disrupted women’s periods reverberated across the Internet. Here’s what docs can do to help.
Following a recent article in the Guardian, the Internet has erupted with tales of periods gone awry. The stress and loss of normalcy over the last year appears to have altered cycles and amplified the premenstrual syndrome (PMS) symptoms many women experience. And after the piece published, many responded on social media with the same sentiment: “So, it’s not just me?”
Women have experienced the loss of their period, excessive and prolonged bleeding, severe mood swings, and irritability, according to the Guardian article. London-based gynecologist Anita Mitra, MBChB, PhD, took an informal survey and found that 65% of 5,677 respondents had noticed a change in their menstrual cycle, the Guardian reported. Another survey, which was posted on medRxiv but hasn’t been peer reviewed yet, found 53% of the 749 respondents had noticed a change in their menstrual cycle, including increased cycle length.
“The pandemic in itself has made more stress for women,” said Karen Carlson, MD, obstetrician and gynecologist at Nebraska Medicine. There’s preliminary evidence that the cycling progesterone and estrogen experienced by reproductive age women actually offers a protective effect against COVID-19, which is good news. But Dr. Carlson said that because they are less likely than men and the elderly to become seriously ill, many women have taken on a lot of the additional responsibilities brought on by the pandemic. They often juggle homeschooling and elder care in addition to the ubiquitous stressors of isolation and concerns around personal health.
“Abnormal bleeding is the most common reason people present to the gynecologist,” Dr. Carlson said in an interview. But in recent months, Dr. Carlson said she’s seen a slight uptick in these issues, and there might have been even more women presenting to their physicians if the pandemic hadn’t also suppressed access to care.
Stress, or rather the cortisol it causes the body to produce, is the culprit for disrupted cycles. It can suppress pituitary hormones that stimulate ovulation. “Some women don’t feel right because they are stuck in the one phase of the cycle,” Dr. Carlson said. They may go months without a period and when they do eventually shed their uterine lining the bleeding goes on for a while.
Some irregularity in a person’s cycle is a normal response to stress and even likely, given the last year. However, bleeding for more than 2 weeks or irregularity for more than 3 months could point to something more serious like an infection or cancer, Dr. Carlson said. Getting a clear history so you know when you need to do blood and hormone workups is critical.
Anxiety and depression amplified
For some women it’s not bleeding that’s a problem, rather their PMS has become crippling. And some of their significant others have noticed drastic changes in their mood. In the Guardian article, one woman said she’d gone from feeling withdrawn during her period to being totally unreachable and experiencing intense anxiety.
Maureen Whelihan, MD, a gynecologist in Palm Beach, Fla., said that, for the majority of her patients under 39 years of age, these feelings aren’t a hormone issue, but a stress and neuroreceptor issue. She says she’s seen approximately a 30% increase in mood disorders since the start of the pandemic. Even though many of her patients are cycling relatively normally, their anxiety and depression have been amplified.
Caroline Gurvich, PhD, a neuroscientist at Monash University in Melbourne, attributes this to the loss of typical coping mechanisms. “Having changes to the support system and routine and things that would keep them mentally healthy can exacerbate PMS,” she said in an interview. Dr. Gurvich’s advice is to build routines into the pandemic lifestyle. Normal wake and sleep times, healthy eating, and practices that bring happiness can be “crucial to keeping those PMS systems as controlled as possible.”
Telehealth has made it much easier to access some patients struggling with PMS and offer them the medication or counseling they need, Dr. Carlson said. But that approach doesn’t work for everyone. “I feel like there are a lot of silent sufferers,” she said.
This is where screening practices like the Patient Health Questionnaire-9 are so critical, according to Dr. Whelihan, who screens every patient as part of their routine iPad check-in process. Even in a normal year, “I think one-third of gynecology is psychiatry,” she said in an interview. She finds many of the patients struggling with excessive PMS symptoms, both during the pandemic and before, benefit from a child-sized dose of antidepressant. This may allow them to get to a place where they can make impactful routine decisions about exercise or sleep, and then taper off the antidepressant.
It may also be important for clinicians to help patients make the initial connection between their worsening mood or cognitive function and their period. Knowing their feelings of stress, irritability, fogginess, or being withdrawn are linked to their hormone cycle and possibly worsened by the stress of the pandemic can be helpful, Dr. Gurvich said. “If they become conscious of how they are feeling it can be helpful for management of these stressful symptoms,” she said.
Stories of how the pandemic has disrupted women’s periods reverberated across the Internet. Here’s what docs can do to help.
Stories of how the pandemic has disrupted women’s periods reverberated across the Internet. Here’s what docs can do to help.
Following a recent article in the Guardian, the Internet has erupted with tales of periods gone awry. The stress and loss of normalcy over the last year appears to have altered cycles and amplified the premenstrual syndrome (PMS) symptoms many women experience. And after the piece published, many responded on social media with the same sentiment: “So, it’s not just me?”
Women have experienced the loss of their period, excessive and prolonged bleeding, severe mood swings, and irritability, according to the Guardian article. London-based gynecologist Anita Mitra, MBChB, PhD, took an informal survey and found that 65% of 5,677 respondents had noticed a change in their menstrual cycle, the Guardian reported. Another survey, which was posted on medRxiv but hasn’t been peer reviewed yet, found 53% of the 749 respondents had noticed a change in their menstrual cycle, including increased cycle length.
“The pandemic in itself has made more stress for women,” said Karen Carlson, MD, obstetrician and gynecologist at Nebraska Medicine. There’s preliminary evidence that the cycling progesterone and estrogen experienced by reproductive age women actually offers a protective effect against COVID-19, which is good news. But Dr. Carlson said that because they are less likely than men and the elderly to become seriously ill, many women have taken on a lot of the additional responsibilities brought on by the pandemic. They often juggle homeschooling and elder care in addition to the ubiquitous stressors of isolation and concerns around personal health.
“Abnormal bleeding is the most common reason people present to the gynecologist,” Dr. Carlson said in an interview. But in recent months, Dr. Carlson said she’s seen a slight uptick in these issues, and there might have been even more women presenting to their physicians if the pandemic hadn’t also suppressed access to care.
Stress, or rather the cortisol it causes the body to produce, is the culprit for disrupted cycles. It can suppress pituitary hormones that stimulate ovulation. “Some women don’t feel right because they are stuck in the one phase of the cycle,” Dr. Carlson said. They may go months without a period and when they do eventually shed their uterine lining the bleeding goes on for a while.
Some irregularity in a person’s cycle is a normal response to stress and even likely, given the last year. However, bleeding for more than 2 weeks or irregularity for more than 3 months could point to something more serious like an infection or cancer, Dr. Carlson said. Getting a clear history so you know when you need to do blood and hormone workups is critical.
Anxiety and depression amplified
For some women it’s not bleeding that’s a problem, rather their PMS has become crippling. And some of their significant others have noticed drastic changes in their mood. In the Guardian article, one woman said she’d gone from feeling withdrawn during her period to being totally unreachable and experiencing intense anxiety.
Maureen Whelihan, MD, a gynecologist in Palm Beach, Fla., said that, for the majority of her patients under 39 years of age, these feelings aren’t a hormone issue, but a stress and neuroreceptor issue. She says she’s seen approximately a 30% increase in mood disorders since the start of the pandemic. Even though many of her patients are cycling relatively normally, their anxiety and depression have been amplified.
Caroline Gurvich, PhD, a neuroscientist at Monash University in Melbourne, attributes this to the loss of typical coping mechanisms. “Having changes to the support system and routine and things that would keep them mentally healthy can exacerbate PMS,” she said in an interview. Dr. Gurvich’s advice is to build routines into the pandemic lifestyle. Normal wake and sleep times, healthy eating, and practices that bring happiness can be “crucial to keeping those PMS systems as controlled as possible.”
Telehealth has made it much easier to access some patients struggling with PMS and offer them the medication or counseling they need, Dr. Carlson said. But that approach doesn’t work for everyone. “I feel like there are a lot of silent sufferers,” she said.
This is where screening practices like the Patient Health Questionnaire-9 are so critical, according to Dr. Whelihan, who screens every patient as part of their routine iPad check-in process. Even in a normal year, “I think one-third of gynecology is psychiatry,” she said in an interview. She finds many of the patients struggling with excessive PMS symptoms, both during the pandemic and before, benefit from a child-sized dose of antidepressant. This may allow them to get to a place where they can make impactful routine decisions about exercise or sleep, and then taper off the antidepressant.
It may also be important for clinicians to help patients make the initial connection between their worsening mood or cognitive function and their period. Knowing their feelings of stress, irritability, fogginess, or being withdrawn are linked to their hormone cycle and possibly worsened by the stress of the pandemic can be helpful, Dr. Gurvich said. “If they become conscious of how they are feeling it can be helpful for management of these stressful symptoms,” she said.
Following a recent article in the Guardian, the Internet has erupted with tales of periods gone awry. The stress and loss of normalcy over the last year appears to have altered cycles and amplified the premenstrual syndrome (PMS) symptoms many women experience. And after the piece published, many responded on social media with the same sentiment: “So, it’s not just me?”
Women have experienced the loss of their period, excessive and prolonged bleeding, severe mood swings, and irritability, according to the Guardian article. London-based gynecologist Anita Mitra, MBChB, PhD, took an informal survey and found that 65% of 5,677 respondents had noticed a change in their menstrual cycle, the Guardian reported. Another survey, which was posted on medRxiv but hasn’t been peer reviewed yet, found 53% of the 749 respondents had noticed a change in their menstrual cycle, including increased cycle length.
“The pandemic in itself has made more stress for women,” said Karen Carlson, MD, obstetrician and gynecologist at Nebraska Medicine. There’s preliminary evidence that the cycling progesterone and estrogen experienced by reproductive age women actually offers a protective effect against COVID-19, which is good news. But Dr. Carlson said that because they are less likely than men and the elderly to become seriously ill, many women have taken on a lot of the additional responsibilities brought on by the pandemic. They often juggle homeschooling and elder care in addition to the ubiquitous stressors of isolation and concerns around personal health.
“Abnormal bleeding is the most common reason people present to the gynecologist,” Dr. Carlson said in an interview. But in recent months, Dr. Carlson said she’s seen a slight uptick in these issues, and there might have been even more women presenting to their physicians if the pandemic hadn’t also suppressed access to care.
Stress, or rather the cortisol it causes the body to produce, is the culprit for disrupted cycles. It can suppress pituitary hormones that stimulate ovulation. “Some women don’t feel right because they are stuck in the one phase of the cycle,” Dr. Carlson said. They may go months without a period and when they do eventually shed their uterine lining the bleeding goes on for a while.
Some irregularity in a person’s cycle is a normal response to stress and even likely, given the last year. However, bleeding for more than 2 weeks or irregularity for more than 3 months could point to something more serious like an infection or cancer, Dr. Carlson said. Getting a clear history so you know when you need to do blood and hormone workups is critical.
Anxiety and depression amplified
For some women it’s not bleeding that’s a problem, rather their PMS has become crippling. And some of their significant others have noticed drastic changes in their mood. In the Guardian article, one woman said she’d gone from feeling withdrawn during her period to being totally unreachable and experiencing intense anxiety.
Maureen Whelihan, MD, a gynecologist in Palm Beach, Fla., said that, for the majority of her patients under 39 years of age, these feelings aren’t a hormone issue, but a stress and neuroreceptor issue. She says she’s seen approximately a 30% increase in mood disorders since the start of the pandemic. Even though many of her patients are cycling relatively normally, their anxiety and depression have been amplified.
Caroline Gurvich, PhD, a neuroscientist at Monash University in Melbourne, attributes this to the loss of typical coping mechanisms. “Having changes to the support system and routine and things that would keep them mentally healthy can exacerbate PMS,” she said in an interview. Dr. Gurvich’s advice is to build routines into the pandemic lifestyle. Normal wake and sleep times, healthy eating, and practices that bring happiness can be “crucial to keeping those PMS systems as controlled as possible.”
Telehealth has made it much easier to access some patients struggling with PMS and offer them the medication or counseling they need, Dr. Carlson said. But that approach doesn’t work for everyone. “I feel like there are a lot of silent sufferers,” she said.
This is where screening practices like the Patient Health Questionnaire-9 are so critical, according to Dr. Whelihan, who screens every patient as part of their routine iPad check-in process. Even in a normal year, “I think one-third of gynecology is psychiatry,” she said in an interview. She finds many of the patients struggling with excessive PMS symptoms, both during the pandemic and before, benefit from a child-sized dose of antidepressant. This may allow them to get to a place where they can make impactful routine decisions about exercise or sleep, and then taper off the antidepressant.
It may also be important for clinicians to help patients make the initial connection between their worsening mood or cognitive function and their period. Knowing their feelings of stress, irritability, fogginess, or being withdrawn are linked to their hormone cycle and possibly worsened by the stress of the pandemic can be helpful, Dr. Gurvich said. “If they become conscious of how they are feeling it can be helpful for management of these stressful symptoms,” she said.
Doctors search for missing link between COVID-19 and ITP
Hospitalist Sarah Stone, MD, arrived for her day shift at Sharp Chula Vista one day in late December. The ICU and hospital wards were still overflowing with COVID-19 patients. But over the previous couple of months, she’d also seen more and more recovered patients presenting with a myriad of symptoms: pulmonary emboli, cardiomyopathy, a shocking case of aspergillosis, and those rare cases of “long COVID,” the patients who just can’t get better.
This morning it was a woman in her 30s. She felt fine, but 2 weeks after recovering from COVID-19, she had unexplained bruising on her arm, a petechiae rash on her legs, and her gums were bleeding. Once admitted to the emergency department, her platelet count of 5000/mm3 was a dead giveaway of immune thrombocytopenic purpura (ITP).
In Dr. Stone’s experience, new and otherwise unexplained symptoms so soon post COVID-19 can’t be written off as a coincidence without some additional consideration. But a quick preliminary search of the literature during her rounds came up almost empty. She found one report with three cases of post-COVID-19 ITP. But other online resources made no mention of it. Kenneth Johnson, MD, the hematologist/oncologist consulting on the new case, told Dr. Stone he’d seen one other case of post-COVID-19 ITP only earlier that month. Dr. Stone called a sister hospital. They’d seen one other case just weeks before.
“I was surprised to find just three cases in the literature when we had seen three among us in a matter of weeks,” Dr. Stone said in an interview. Something was missing.
A missing link
ITP is caused by an immune reaction against a patient’s own platelets.
“We know that infections like influenza can cause ITP, so in this light, [COVID-19-associated ITP] might not be surprising,” Gerard Jansen, MD, PhD, an internist and hematologist in Rotterdam, the Netherlands, said in an interview.
Dr. Jansen and colleagues recorded three cases of post-COVID-19 ITP in May 2020 – the report Dr. Stone had found during her shift. Two patients developed ITP several weeks after COVID-19 and responded to treatment with corticosteroids and intravenous immunoglobulin G (IVIG). The third patient, however, died of intracerebral bleeding while still battling COVID-19. He was retrospectively diagnosed with COVID-19-associated ITP.
A deeper dive into the literature uncovers additional case reports from India, France, the United Kingdom, Turkey, and one from China as early as January 2020. A September 2020 review of ITP secondary to COVID-19 included 23 papers and a total of 45 patients. The review authors noted that more than 70% of cases occurred in patients who were aged over 50 years and 75% had had moderate to severe COVID-19 infections. However, the sample size of 45 is too small to definitively describe what’s happening in the overall population.
ITP’s link to COVID-19 gained a media spotlight after the Miami obstetrician, Gregory Michael, MD, developed ITP days after getting the Pfizer COVID-19 vaccine. In early January, after 2 weeks in the ICU, Dr. Michael died of a hemorrhagic stroke caused by the low platelet count.
Pfizer said in a statement that the company is “actively investigating” the case, “but we don’t believe at this time that there is any direct connection to the vaccine.” Other experts have said the timing, particularly in a relatively young and healthy man, means a link to the vaccine is possible or even likely, but final results won›t be known until the Centers for Disease Control and Prevention finishes its investigation.
But “it is quite unusual to die from ITP,” San Diego hematologist Dr. Johnson said in an interview. In his more than 20 years of practice, he has never had a patient die from the condition.
For his part, Dr. Jansen, the hematologist in Rotterdam, said that at this point we just don’t know if there’s a link between the vaccine and ITP. Both infection and drugs are well established causes of ITP, so with that general mechanism or pathology in mind it makes sense that COVID-19 and the vaccine could instigate ITP. But it would be very difficult to prove in just one instance, he said. And considering the millions who have thus far received the vaccine without incident, and the known risks and dangers of COVID-19, “we still advise to vaccinate,” he said.
The number of cases is underestimated
Since his original case report in May, Dr. Jansen has seen five or so additional cases. But the causal link between the coronavirus and the hematologic symptoms is still undefined. “We don’t know much about platelet counts in COVID-19 at all,” he said. It could be that COVID-19 somehow inhibits platelet production or that it kills existing platelets. Whatever the exact relationship to the virus, Dr. Jansen expects that the true number of COVID-19-related ITP cases is higher than current estimates suggest.
One reason it isn’t coming up more often, Dr. Jansen said, may be that the cause of ITP in COVID-19 patients is hard to pin down. In the case report from May, Dr. Jansen and colleagues wrote: “And there are numerous other factors that can cause thrombocytopenia where COVID is concerned. For instance the coagulation activation by COVID‐19 infection leading to disseminated intravascular coagulation (DIC) and subsequent thrombocytopenia. Also, treatments for COVID‐19, including heparin, azithromycin and hydroxychloroquine, may lead to thrombocytopenia.”
Tracking and understanding COVID-19-associated ITP first requires the extensive process of elimination needed to diagnose it.
In addition, drugs used to treat COVID-19 could be masking COVID-19-related ITP. “Dexamethasone is a mainstay of COVID treatment. And it’s how we treat ITP,” Dr. Johnson said, which means physicians may be treating ITP without even registering it. And that’s one hypothesis for why Dr. Stone and Dr. Johnson didn’t see a case until 9 months into the pandemic.
Treating COVID-19-associated ITP also has its challenges, particularly in patients who develop it during an acute COVID-19 infection and are at risk for both internal bleeding and thrombosis. This was the case for the third patient in Dr. Jansen’s case report. The patient developed a pulmonary embolism and had a falling platelet count. He was given a platelet infusion and then an anticoagulant for the thrombosis. But a retrospective look at the case revealed the transfusion “did not increase numbers at all – which suggests ITP,” Dr. Jansen said. Intracerebral bleeding was the cause of death.
That’s why “it’s important to be aware of this phenomenon,” Dr. Jansen said of COVID-19-associated ITP. If a transfusion is unsuccessful, consider that the patient may have ITP and adjust. Dr. Johnson hasn’t had to treat a patient battling both complications simultaneously but says the ideal course of action would be to raise platelets with steroids and IVIG and then give the anticoagulant once the platelet count is higher. But reality is rarely ideal. Often these two treatments will have to be given concurrently since the patient faces two life-threatening risks, he said. “It’s a very challenging situation,” he said.
The good news is that standard treatments for ITP seem to work for COVID-19-associated ITP. The 30-year-old patient of Dr. Stone and Dr. Johnson responded so well to intravenous steroids that IVIG was unnecessary. She’s now on a slow prednisone taper and maintains platelet counts at 114,000/mm3 at her weekly follow-up appointments with Dr. Johnson.
Meanwhile, Dr. Jansen’s two other patients, now nearly a year out of treatment, require no additional medication. One of the patients is fully recovered and, though the other still has lower than normal platelet counts, she has no bleeding symptoms and her platelet counts remain stable. Still, Dr. Jansen is anxious for more data looking at the platelet counts in every COVID-19 patient and to combine findings from existing COVID-19-associated ITP patients.
For Dr. Stone, she says she’s added one COVID-19-associated complication to her belt. One less aftereffect will catch her off guard. And she wants others to have the same information.
“It’s just a little bit daunting. We don’t know how bad post-COVID will be,” she said. “There’s so many levels to this disease. Some people deal with it for so long and some people just get better and move on – we think ... so far.”
A version of this article first appeared on Medscape.com.
Hospitalist Sarah Stone, MD, arrived for her day shift at Sharp Chula Vista one day in late December. The ICU and hospital wards were still overflowing with COVID-19 patients. But over the previous couple of months, she’d also seen more and more recovered patients presenting with a myriad of symptoms: pulmonary emboli, cardiomyopathy, a shocking case of aspergillosis, and those rare cases of “long COVID,” the patients who just can’t get better.
This morning it was a woman in her 30s. She felt fine, but 2 weeks after recovering from COVID-19, she had unexplained bruising on her arm, a petechiae rash on her legs, and her gums were bleeding. Once admitted to the emergency department, her platelet count of 5000/mm3 was a dead giveaway of immune thrombocytopenic purpura (ITP).
In Dr. Stone’s experience, new and otherwise unexplained symptoms so soon post COVID-19 can’t be written off as a coincidence without some additional consideration. But a quick preliminary search of the literature during her rounds came up almost empty. She found one report with three cases of post-COVID-19 ITP. But other online resources made no mention of it. Kenneth Johnson, MD, the hematologist/oncologist consulting on the new case, told Dr. Stone he’d seen one other case of post-COVID-19 ITP only earlier that month. Dr. Stone called a sister hospital. They’d seen one other case just weeks before.
“I was surprised to find just three cases in the literature when we had seen three among us in a matter of weeks,” Dr. Stone said in an interview. Something was missing.
A missing link
ITP is caused by an immune reaction against a patient’s own platelets.
“We know that infections like influenza can cause ITP, so in this light, [COVID-19-associated ITP] might not be surprising,” Gerard Jansen, MD, PhD, an internist and hematologist in Rotterdam, the Netherlands, said in an interview.
Dr. Jansen and colleagues recorded three cases of post-COVID-19 ITP in May 2020 – the report Dr. Stone had found during her shift. Two patients developed ITP several weeks after COVID-19 and responded to treatment with corticosteroids and intravenous immunoglobulin G (IVIG). The third patient, however, died of intracerebral bleeding while still battling COVID-19. He was retrospectively diagnosed with COVID-19-associated ITP.
A deeper dive into the literature uncovers additional case reports from India, France, the United Kingdom, Turkey, and one from China as early as January 2020. A September 2020 review of ITP secondary to COVID-19 included 23 papers and a total of 45 patients. The review authors noted that more than 70% of cases occurred in patients who were aged over 50 years and 75% had had moderate to severe COVID-19 infections. However, the sample size of 45 is too small to definitively describe what’s happening in the overall population.
ITP’s link to COVID-19 gained a media spotlight after the Miami obstetrician, Gregory Michael, MD, developed ITP days after getting the Pfizer COVID-19 vaccine. In early January, after 2 weeks in the ICU, Dr. Michael died of a hemorrhagic stroke caused by the low platelet count.
Pfizer said in a statement that the company is “actively investigating” the case, “but we don’t believe at this time that there is any direct connection to the vaccine.” Other experts have said the timing, particularly in a relatively young and healthy man, means a link to the vaccine is possible or even likely, but final results won›t be known until the Centers for Disease Control and Prevention finishes its investigation.
But “it is quite unusual to die from ITP,” San Diego hematologist Dr. Johnson said in an interview. In his more than 20 years of practice, he has never had a patient die from the condition.
For his part, Dr. Jansen, the hematologist in Rotterdam, said that at this point we just don’t know if there’s a link between the vaccine and ITP. Both infection and drugs are well established causes of ITP, so with that general mechanism or pathology in mind it makes sense that COVID-19 and the vaccine could instigate ITP. But it would be very difficult to prove in just one instance, he said. And considering the millions who have thus far received the vaccine without incident, and the known risks and dangers of COVID-19, “we still advise to vaccinate,” he said.
The number of cases is underestimated
Since his original case report in May, Dr. Jansen has seen five or so additional cases. But the causal link between the coronavirus and the hematologic symptoms is still undefined. “We don’t know much about platelet counts in COVID-19 at all,” he said. It could be that COVID-19 somehow inhibits platelet production or that it kills existing platelets. Whatever the exact relationship to the virus, Dr. Jansen expects that the true number of COVID-19-related ITP cases is higher than current estimates suggest.
One reason it isn’t coming up more often, Dr. Jansen said, may be that the cause of ITP in COVID-19 patients is hard to pin down. In the case report from May, Dr. Jansen and colleagues wrote: “And there are numerous other factors that can cause thrombocytopenia where COVID is concerned. For instance the coagulation activation by COVID‐19 infection leading to disseminated intravascular coagulation (DIC) and subsequent thrombocytopenia. Also, treatments for COVID‐19, including heparin, azithromycin and hydroxychloroquine, may lead to thrombocytopenia.”
Tracking and understanding COVID-19-associated ITP first requires the extensive process of elimination needed to diagnose it.
In addition, drugs used to treat COVID-19 could be masking COVID-19-related ITP. “Dexamethasone is a mainstay of COVID treatment. And it’s how we treat ITP,” Dr. Johnson said, which means physicians may be treating ITP without even registering it. And that’s one hypothesis for why Dr. Stone and Dr. Johnson didn’t see a case until 9 months into the pandemic.
Treating COVID-19-associated ITP also has its challenges, particularly in patients who develop it during an acute COVID-19 infection and are at risk for both internal bleeding and thrombosis. This was the case for the third patient in Dr. Jansen’s case report. The patient developed a pulmonary embolism and had a falling platelet count. He was given a platelet infusion and then an anticoagulant for the thrombosis. But a retrospective look at the case revealed the transfusion “did not increase numbers at all – which suggests ITP,” Dr. Jansen said. Intracerebral bleeding was the cause of death.
That’s why “it’s important to be aware of this phenomenon,” Dr. Jansen said of COVID-19-associated ITP. If a transfusion is unsuccessful, consider that the patient may have ITP and adjust. Dr. Johnson hasn’t had to treat a patient battling both complications simultaneously but says the ideal course of action would be to raise platelets with steroids and IVIG and then give the anticoagulant once the platelet count is higher. But reality is rarely ideal. Often these two treatments will have to be given concurrently since the patient faces two life-threatening risks, he said. “It’s a very challenging situation,” he said.
The good news is that standard treatments for ITP seem to work for COVID-19-associated ITP. The 30-year-old patient of Dr. Stone and Dr. Johnson responded so well to intravenous steroids that IVIG was unnecessary. She’s now on a slow prednisone taper and maintains platelet counts at 114,000/mm3 at her weekly follow-up appointments with Dr. Johnson.
Meanwhile, Dr. Jansen’s two other patients, now nearly a year out of treatment, require no additional medication. One of the patients is fully recovered and, though the other still has lower than normal platelet counts, she has no bleeding symptoms and her platelet counts remain stable. Still, Dr. Jansen is anxious for more data looking at the platelet counts in every COVID-19 patient and to combine findings from existing COVID-19-associated ITP patients.
For Dr. Stone, she says she’s added one COVID-19-associated complication to her belt. One less aftereffect will catch her off guard. And she wants others to have the same information.
“It’s just a little bit daunting. We don’t know how bad post-COVID will be,” she said. “There’s so many levels to this disease. Some people deal with it for so long and some people just get better and move on – we think ... so far.”
A version of this article first appeared on Medscape.com.
Hospitalist Sarah Stone, MD, arrived for her day shift at Sharp Chula Vista one day in late December. The ICU and hospital wards were still overflowing with COVID-19 patients. But over the previous couple of months, she’d also seen more and more recovered patients presenting with a myriad of symptoms: pulmonary emboli, cardiomyopathy, a shocking case of aspergillosis, and those rare cases of “long COVID,” the patients who just can’t get better.
This morning it was a woman in her 30s. She felt fine, but 2 weeks after recovering from COVID-19, she had unexplained bruising on her arm, a petechiae rash on her legs, and her gums were bleeding. Once admitted to the emergency department, her platelet count of 5000/mm3 was a dead giveaway of immune thrombocytopenic purpura (ITP).
In Dr. Stone’s experience, new and otherwise unexplained symptoms so soon post COVID-19 can’t be written off as a coincidence without some additional consideration. But a quick preliminary search of the literature during her rounds came up almost empty. She found one report with three cases of post-COVID-19 ITP. But other online resources made no mention of it. Kenneth Johnson, MD, the hematologist/oncologist consulting on the new case, told Dr. Stone he’d seen one other case of post-COVID-19 ITP only earlier that month. Dr. Stone called a sister hospital. They’d seen one other case just weeks before.
“I was surprised to find just three cases in the literature when we had seen three among us in a matter of weeks,” Dr. Stone said in an interview. Something was missing.
A missing link
ITP is caused by an immune reaction against a patient’s own platelets.
“We know that infections like influenza can cause ITP, so in this light, [COVID-19-associated ITP] might not be surprising,” Gerard Jansen, MD, PhD, an internist and hematologist in Rotterdam, the Netherlands, said in an interview.
Dr. Jansen and colleagues recorded three cases of post-COVID-19 ITP in May 2020 – the report Dr. Stone had found during her shift. Two patients developed ITP several weeks after COVID-19 and responded to treatment with corticosteroids and intravenous immunoglobulin G (IVIG). The third patient, however, died of intracerebral bleeding while still battling COVID-19. He was retrospectively diagnosed with COVID-19-associated ITP.
A deeper dive into the literature uncovers additional case reports from India, France, the United Kingdom, Turkey, and one from China as early as January 2020. A September 2020 review of ITP secondary to COVID-19 included 23 papers and a total of 45 patients. The review authors noted that more than 70% of cases occurred in patients who were aged over 50 years and 75% had had moderate to severe COVID-19 infections. However, the sample size of 45 is too small to definitively describe what’s happening in the overall population.
ITP’s link to COVID-19 gained a media spotlight after the Miami obstetrician, Gregory Michael, MD, developed ITP days after getting the Pfizer COVID-19 vaccine. In early January, after 2 weeks in the ICU, Dr. Michael died of a hemorrhagic stroke caused by the low platelet count.
Pfizer said in a statement that the company is “actively investigating” the case, “but we don’t believe at this time that there is any direct connection to the vaccine.” Other experts have said the timing, particularly in a relatively young and healthy man, means a link to the vaccine is possible or even likely, but final results won›t be known until the Centers for Disease Control and Prevention finishes its investigation.
But “it is quite unusual to die from ITP,” San Diego hematologist Dr. Johnson said in an interview. In his more than 20 years of practice, he has never had a patient die from the condition.
For his part, Dr. Jansen, the hematologist in Rotterdam, said that at this point we just don’t know if there’s a link between the vaccine and ITP. Both infection and drugs are well established causes of ITP, so with that general mechanism or pathology in mind it makes sense that COVID-19 and the vaccine could instigate ITP. But it would be very difficult to prove in just one instance, he said. And considering the millions who have thus far received the vaccine without incident, and the known risks and dangers of COVID-19, “we still advise to vaccinate,” he said.
The number of cases is underestimated
Since his original case report in May, Dr. Jansen has seen five or so additional cases. But the causal link between the coronavirus and the hematologic symptoms is still undefined. “We don’t know much about platelet counts in COVID-19 at all,” he said. It could be that COVID-19 somehow inhibits platelet production or that it kills existing platelets. Whatever the exact relationship to the virus, Dr. Jansen expects that the true number of COVID-19-related ITP cases is higher than current estimates suggest.
One reason it isn’t coming up more often, Dr. Jansen said, may be that the cause of ITP in COVID-19 patients is hard to pin down. In the case report from May, Dr. Jansen and colleagues wrote: “And there are numerous other factors that can cause thrombocytopenia where COVID is concerned. For instance the coagulation activation by COVID‐19 infection leading to disseminated intravascular coagulation (DIC) and subsequent thrombocytopenia. Also, treatments for COVID‐19, including heparin, azithromycin and hydroxychloroquine, may lead to thrombocytopenia.”
Tracking and understanding COVID-19-associated ITP first requires the extensive process of elimination needed to diagnose it.
In addition, drugs used to treat COVID-19 could be masking COVID-19-related ITP. “Dexamethasone is a mainstay of COVID treatment. And it’s how we treat ITP,” Dr. Johnson said, which means physicians may be treating ITP without even registering it. And that’s one hypothesis for why Dr. Stone and Dr. Johnson didn’t see a case until 9 months into the pandemic.
Treating COVID-19-associated ITP also has its challenges, particularly in patients who develop it during an acute COVID-19 infection and are at risk for both internal bleeding and thrombosis. This was the case for the third patient in Dr. Jansen’s case report. The patient developed a pulmonary embolism and had a falling platelet count. He was given a platelet infusion and then an anticoagulant for the thrombosis. But a retrospective look at the case revealed the transfusion “did not increase numbers at all – which suggests ITP,” Dr. Jansen said. Intracerebral bleeding was the cause of death.
That’s why “it’s important to be aware of this phenomenon,” Dr. Jansen said of COVID-19-associated ITP. If a transfusion is unsuccessful, consider that the patient may have ITP and adjust. Dr. Johnson hasn’t had to treat a patient battling both complications simultaneously but says the ideal course of action would be to raise platelets with steroids and IVIG and then give the anticoagulant once the platelet count is higher. But reality is rarely ideal. Often these two treatments will have to be given concurrently since the patient faces two life-threatening risks, he said. “It’s a very challenging situation,” he said.
The good news is that standard treatments for ITP seem to work for COVID-19-associated ITP. The 30-year-old patient of Dr. Stone and Dr. Johnson responded so well to intravenous steroids that IVIG was unnecessary. She’s now on a slow prednisone taper and maintains platelet counts at 114,000/mm3 at her weekly follow-up appointments with Dr. Johnson.
Meanwhile, Dr. Jansen’s two other patients, now nearly a year out of treatment, require no additional medication. One of the patients is fully recovered and, though the other still has lower than normal platelet counts, she has no bleeding symptoms and her platelet counts remain stable. Still, Dr. Jansen is anxious for more data looking at the platelet counts in every COVID-19 patient and to combine findings from existing COVID-19-associated ITP patients.
For Dr. Stone, she says she’s added one COVID-19-associated complication to her belt. One less aftereffect will catch her off guard. And she wants others to have the same information.
“It’s just a little bit daunting. We don’t know how bad post-COVID will be,” she said. “There’s so many levels to this disease. Some people deal with it for so long and some people just get better and move on – we think ... so far.”
A version of this article first appeared on Medscape.com.
Patient health suffers amid pandemic health care shortages
More than half (56%) of responding clinicians reported seeing a decline in patient health because of delayed or inaccessible care amid the pandemic, according to the results of the latest survey by the Larry A. Green Center and the Primary Care Collaborative. The survey was conducted in mid-October and the results were published online Nov. 17.
In addition, 37% of respondents said their patients with chronic conditions showed “noticeably worse health resulting from the pandemic.” And a resounding 85% said patient mental health had worsened.
“I think it’s worse than we thought,” said Rebecca Etz, PhD, codirector of the Larry Green Center. “It’s the outcome of not sufficiently sending resources to primary care either before or during the pandemic.” According to Dr. Etz, survey respondents noted substantial increases in patient weight gain as well as weight loss, anxiety and depression, sleep issues, domestic abuse, and poor oral and eye health, among others.
One clinician from Pennsylvania wrote: “Patients are becoming sicker during the pandemic. I’m seeing more uncontrolled [diabetes]and new [patients with diabetes]. They prefer telehealth yet [have] no access to glucose monitoring or a blood pressure cuff. I am concerned about patients’ isolation and mental health. People are delaying care.”
Now, with COVID numbers peaking across much of the country, many clinicians are trying to close the gap in care with telehealth – something they’re more prepared to do now than they were in March. Over two-thirds of practices are using telehealth for visits to keep up with patients who have stable chronic conditions, according to the survey.
Over 60% of physicians report using telehealth for mental health visits. But a much smaller number – only 16% of respondents – said their practice had added staff to help manage the rising number of behavioral and mental health cases. About one-third (35%) of practices say they’re not financially able to take on new staff.
“We’ve been looking for more ways for patients to do self-support. A big part of chronic disease is health behaviors,” Alex Krist, MD, MPH, a family doctor in Fairfax, Va., and chairperson of the U.S. Preventive Services Task Force, said in an interview. And unfortunately, on top of limited access to basic care, healthy habits that are essential to managing many chronic conditions have become more difficult and less consistent during the pandemic.
The survey – the 22nd iteration in a series of surveys the Green Center and the Primary Care Collaborative have conducted – received 580 respondents from 47 states and Guam. Over two-thirds of respondents were primary care physicians (MDs and DOs). Over half were owners, partners, or employees of a private practice, 66% of which were family medicine practices. And one fifth of respondents provided care in a rural area.
Funding and support for primary care has been wildly insufficient, Dr. Etz said in an interview. If that doesn’t change, patient health, clinic staffing, and public health strategies amid the pandemic will continue to suffer.
“When you think of the COVID vaccine, who do you think is going to be sending that out?” Dr. Etz asked. “If we don’t bolster primary care now how are they going to handle that.”
A version of this article originally appeared on Medscape.com.
More than half (56%) of responding clinicians reported seeing a decline in patient health because of delayed or inaccessible care amid the pandemic, according to the results of the latest survey by the Larry A. Green Center and the Primary Care Collaborative. The survey was conducted in mid-October and the results were published online Nov. 17.
In addition, 37% of respondents said their patients with chronic conditions showed “noticeably worse health resulting from the pandemic.” And a resounding 85% said patient mental health had worsened.
“I think it’s worse than we thought,” said Rebecca Etz, PhD, codirector of the Larry Green Center. “It’s the outcome of not sufficiently sending resources to primary care either before or during the pandemic.” According to Dr. Etz, survey respondents noted substantial increases in patient weight gain as well as weight loss, anxiety and depression, sleep issues, domestic abuse, and poor oral and eye health, among others.
One clinician from Pennsylvania wrote: “Patients are becoming sicker during the pandemic. I’m seeing more uncontrolled [diabetes]and new [patients with diabetes]. They prefer telehealth yet [have] no access to glucose monitoring or a blood pressure cuff. I am concerned about patients’ isolation and mental health. People are delaying care.”
Now, with COVID numbers peaking across much of the country, many clinicians are trying to close the gap in care with telehealth – something they’re more prepared to do now than they were in March. Over two-thirds of practices are using telehealth for visits to keep up with patients who have stable chronic conditions, according to the survey.
Over 60% of physicians report using telehealth for mental health visits. But a much smaller number – only 16% of respondents – said their practice had added staff to help manage the rising number of behavioral and mental health cases. About one-third (35%) of practices say they’re not financially able to take on new staff.
“We’ve been looking for more ways for patients to do self-support. A big part of chronic disease is health behaviors,” Alex Krist, MD, MPH, a family doctor in Fairfax, Va., and chairperson of the U.S. Preventive Services Task Force, said in an interview. And unfortunately, on top of limited access to basic care, healthy habits that are essential to managing many chronic conditions have become more difficult and less consistent during the pandemic.
The survey – the 22nd iteration in a series of surveys the Green Center and the Primary Care Collaborative have conducted – received 580 respondents from 47 states and Guam. Over two-thirds of respondents were primary care physicians (MDs and DOs). Over half were owners, partners, or employees of a private practice, 66% of which were family medicine practices. And one fifth of respondents provided care in a rural area.
Funding and support for primary care has been wildly insufficient, Dr. Etz said in an interview. If that doesn’t change, patient health, clinic staffing, and public health strategies amid the pandemic will continue to suffer.
“When you think of the COVID vaccine, who do you think is going to be sending that out?” Dr. Etz asked. “If we don’t bolster primary care now how are they going to handle that.”
A version of this article originally appeared on Medscape.com.
More than half (56%) of responding clinicians reported seeing a decline in patient health because of delayed or inaccessible care amid the pandemic, according to the results of the latest survey by the Larry A. Green Center and the Primary Care Collaborative. The survey was conducted in mid-October and the results were published online Nov. 17.
In addition, 37% of respondents said their patients with chronic conditions showed “noticeably worse health resulting from the pandemic.” And a resounding 85% said patient mental health had worsened.
“I think it’s worse than we thought,” said Rebecca Etz, PhD, codirector of the Larry Green Center. “It’s the outcome of not sufficiently sending resources to primary care either before or during the pandemic.” According to Dr. Etz, survey respondents noted substantial increases in patient weight gain as well as weight loss, anxiety and depression, sleep issues, domestic abuse, and poor oral and eye health, among others.
One clinician from Pennsylvania wrote: “Patients are becoming sicker during the pandemic. I’m seeing more uncontrolled [diabetes]and new [patients with diabetes]. They prefer telehealth yet [have] no access to glucose monitoring or a blood pressure cuff. I am concerned about patients’ isolation and mental health. People are delaying care.”
Now, with COVID numbers peaking across much of the country, many clinicians are trying to close the gap in care with telehealth – something they’re more prepared to do now than they were in March. Over two-thirds of practices are using telehealth for visits to keep up with patients who have stable chronic conditions, according to the survey.
Over 60% of physicians report using telehealth for mental health visits. But a much smaller number – only 16% of respondents – said their practice had added staff to help manage the rising number of behavioral and mental health cases. About one-third (35%) of practices say they’re not financially able to take on new staff.
“We’ve been looking for more ways for patients to do self-support. A big part of chronic disease is health behaviors,” Alex Krist, MD, MPH, a family doctor in Fairfax, Va., and chairperson of the U.S. Preventive Services Task Force, said in an interview. And unfortunately, on top of limited access to basic care, healthy habits that are essential to managing many chronic conditions have become more difficult and less consistent during the pandemic.
The survey – the 22nd iteration in a series of surveys the Green Center and the Primary Care Collaborative have conducted – received 580 respondents from 47 states and Guam. Over two-thirds of respondents were primary care physicians (MDs and DOs). Over half were owners, partners, or employees of a private practice, 66% of which were family medicine practices. And one fifth of respondents provided care in a rural area.
Funding and support for primary care has been wildly insufficient, Dr. Etz said in an interview. If that doesn’t change, patient health, clinic staffing, and public health strategies amid the pandemic will continue to suffer.
“When you think of the COVID vaccine, who do you think is going to be sending that out?” Dr. Etz asked. “If we don’t bolster primary care now how are they going to handle that.”
A version of this article originally appeared on Medscape.com.
Primary care isn’t bouncing back
published by the Primary Care Collaborative (PCC) and Larry A. Green Center.
Since mid-March these organizations have issued short weekly and biweekly surveys to U.S. primary care physicians in an attempt to find the pulse of the county’s first line of care. “There is not a federal office for primary care, and it’s been anemically funded for decades,” Rebecca Etz, PhD, said in an interview. Yet these clinics represent the front lines of U.S. health care, and it’s where most Americans go for care and COVID-19 care, said Dr. Etz, director of the Virginia-based Larry A. Green Center, which is devoted to primary care research, development, and advocacy.
The latest survey responses, collected between Sept. 4 and 6, confirm what researchers had suspected: Primary care isn’t on solid footing. Eighty-one percent of respondents disagreed emphatically that primary care has bounced back, and another 13% said things were better than earlier this year but not normal.
Meanwhile, 35% of respondents said that revenue and pay are significantly lower than they were before the pandemic and net losses threaten their practices’ viability. Almost half (49%) said their mental exhaustion from work was at an all-time high.
“Because of how our system is set up – it’s a fee-for-service model – the more patients you see, the more money you get,” said Yalda Jabbarpour, MD, medical director at the Graham Center, a leading think tank on family medicine and health care policy. But the stay-at-home order, aversion to telehealth, and fear of in-person visits have been keeping patients away – and driving primary care revenue down. Even when practices transition to and expand their telehealth, payer reimbursement is not yet on parity with in-person visits.
Right now, primary care physicians are doing fewer procedures and spending more time on video visits. “So you may have the same overhead and time investment but you’re getting paid a fraction,” Dr. Etz said. In August, 50% of primary care physicians reported they were working the same or more hours per week as they did before the pandemic but for less money, according to an earlier survey from the Green Center and the PCC. That loss of revenue is compounded by the need for expensive personal protective equipment and preparation for the upcoming flu season, Dr. Etz said.
Ongoing surveys reveal stress
Over the last 20 weeks or so, the Green Center and PCC together have disseminated weekly (through June) or biweekly surveys to 100 professional organizations. Because there isn’t an entity that represents all of primary care and claims data take years to process, these surveys are intended to get real-time feedback from clinicians who are providing a lot of patient care during the pandemic.
The sample sizes are admittedly small, with the most recent survey including 489 clinicians. Dr. Jabbarpour noted, “489 – it’s a good number, but you would want more.” Generally, for a great survey response you’d want 20%-30% of the physician population because then you could assume you’re getting a good mix of geographies, practice sizes, and settings, she said.
Respondents to the most recent survey were from 49 different states; 70% identified their practice as family medicine. One-third had between one and three physicians in their practice and 40% had 10 or more clinicians. “It’s not perfect, but it sounds pretty representative of the primary care workforce,” Dr. Jabbarpour continued.
The latest Green Center-PCC survey, published last week, also found that one in five physicians surveyed said at least one clinician in their practice had opted for early retirement or left practice as a direct result of the pandemic. These declines in clinician staffing come as school reopenings threaten to cause a resurgence of COVID-19 cases and the 2021 flu season could complicate COVID-19 care and testing.
Shortfall could cascade to other specialties
News that primary care is both struggling and shrinking doesn’t come as a surprise to those who research this area, according to Dr. Jabbarpour. Yet it matters “because primary care is where the majority of Americans get their health care.” According to the Centers for Disease Control and Prevention, primary care accounts for 50% of all office visits. But the sector only encompasses 30% of the clinician workforce, according to a 2019 study of physician supply, and accounts for just 7% of national health expenditures, according to a separate 2019 study that measured primary care investment.
If primary care doesn’t bounce back, the shortfall could overwhelm the rest of the health care system, Dr. Jabbarpour said. “If primary care shortages increase, then urgent cares, ERs, and hospitals will become overwhelmed.”
Or public health could suffer as people don’t seek care at all. A study published earlier this summer found that up to 35% of excess deaths during the pandemic were not caused by COVID-19. Instead, they can be attributed to treatable causes, like heart disease, diabetes, and Alzheimers, the researchers concluded. In Dr. Etz’s estimation, this high cost is a glimpse of what happens when there isn’t adequate access to primary care.
When asked about the frequency of the PCC/Green Center surveys, Bianca Frogner, PhD, a health economist and deputy director at the University of Washington Primary Care Innovation Lab in Seattle, said it’s unusual to have this regularity. Also, it’s unique in that it offers a constant mix of physicians. “It’s a small sample, but it still gives a voice where there isn’t one.”
Smaller weekly surveys and secondary analysis projects from the Graham Center, an American Academy of Family Physicians affiliated research center, reinforce findings of the Green Center. The Graham Center surveys also found primary care is taking a financial hit, staff is being furloughed, and patient volume is down, according to Dr. Jabbarpour, who has been involved in most of the Graham Center’s work on COVID.
Dr. Frogner, Dr. Etz, and Dr. Jabbarpour agree that, as a nation, the United States has chronically underinvested in primary care, and now the system is in crisis. The hope is that the survey data gives policymakers, state leaders, and the federal government a better idea of what’s happening on the ground.
It’s also important for researchers “keeping an eye out for the available supply of primary care for certain populations,” Dr. Frogner said. The current conditions are especially a threat to rural and underserved areas, she added.
If primary health care isn’t near recovery that’s a problem for the entire population, Dr. Etz said. And what happens if there’s another surge of COVID-19 or even a second pandemic in our lifetime? Her recommendation: Treat it like disaster recovery. Step one is “Stop the hemorrhaging – they need immediate cash flow.”
A version of this article originally appeared on Medscape.com.
published by the Primary Care Collaborative (PCC) and Larry A. Green Center.
Since mid-March these organizations have issued short weekly and biweekly surveys to U.S. primary care physicians in an attempt to find the pulse of the county’s first line of care. “There is not a federal office for primary care, and it’s been anemically funded for decades,” Rebecca Etz, PhD, said in an interview. Yet these clinics represent the front lines of U.S. health care, and it’s where most Americans go for care and COVID-19 care, said Dr. Etz, director of the Virginia-based Larry A. Green Center, which is devoted to primary care research, development, and advocacy.
The latest survey responses, collected between Sept. 4 and 6, confirm what researchers had suspected: Primary care isn’t on solid footing. Eighty-one percent of respondents disagreed emphatically that primary care has bounced back, and another 13% said things were better than earlier this year but not normal.
Meanwhile, 35% of respondents said that revenue and pay are significantly lower than they were before the pandemic and net losses threaten their practices’ viability. Almost half (49%) said their mental exhaustion from work was at an all-time high.
“Because of how our system is set up – it’s a fee-for-service model – the more patients you see, the more money you get,” said Yalda Jabbarpour, MD, medical director at the Graham Center, a leading think tank on family medicine and health care policy. But the stay-at-home order, aversion to telehealth, and fear of in-person visits have been keeping patients away – and driving primary care revenue down. Even when practices transition to and expand their telehealth, payer reimbursement is not yet on parity with in-person visits.
Right now, primary care physicians are doing fewer procedures and spending more time on video visits. “So you may have the same overhead and time investment but you’re getting paid a fraction,” Dr. Etz said. In August, 50% of primary care physicians reported they were working the same or more hours per week as they did before the pandemic but for less money, according to an earlier survey from the Green Center and the PCC. That loss of revenue is compounded by the need for expensive personal protective equipment and preparation for the upcoming flu season, Dr. Etz said.
Ongoing surveys reveal stress
Over the last 20 weeks or so, the Green Center and PCC together have disseminated weekly (through June) or biweekly surveys to 100 professional organizations. Because there isn’t an entity that represents all of primary care and claims data take years to process, these surveys are intended to get real-time feedback from clinicians who are providing a lot of patient care during the pandemic.
The sample sizes are admittedly small, with the most recent survey including 489 clinicians. Dr. Jabbarpour noted, “489 – it’s a good number, but you would want more.” Generally, for a great survey response you’d want 20%-30% of the physician population because then you could assume you’re getting a good mix of geographies, practice sizes, and settings, she said.
Respondents to the most recent survey were from 49 different states; 70% identified their practice as family medicine. One-third had between one and three physicians in their practice and 40% had 10 or more clinicians. “It’s not perfect, but it sounds pretty representative of the primary care workforce,” Dr. Jabbarpour continued.
The latest Green Center-PCC survey, published last week, also found that one in five physicians surveyed said at least one clinician in their practice had opted for early retirement or left practice as a direct result of the pandemic. These declines in clinician staffing come as school reopenings threaten to cause a resurgence of COVID-19 cases and the 2021 flu season could complicate COVID-19 care and testing.
Shortfall could cascade to other specialties
News that primary care is both struggling and shrinking doesn’t come as a surprise to those who research this area, according to Dr. Jabbarpour. Yet it matters “because primary care is where the majority of Americans get their health care.” According to the Centers for Disease Control and Prevention, primary care accounts for 50% of all office visits. But the sector only encompasses 30% of the clinician workforce, according to a 2019 study of physician supply, and accounts for just 7% of national health expenditures, according to a separate 2019 study that measured primary care investment.
If primary care doesn’t bounce back, the shortfall could overwhelm the rest of the health care system, Dr. Jabbarpour said. “If primary care shortages increase, then urgent cares, ERs, and hospitals will become overwhelmed.”
Or public health could suffer as people don’t seek care at all. A study published earlier this summer found that up to 35% of excess deaths during the pandemic were not caused by COVID-19. Instead, they can be attributed to treatable causes, like heart disease, diabetes, and Alzheimers, the researchers concluded. In Dr. Etz’s estimation, this high cost is a glimpse of what happens when there isn’t adequate access to primary care.
When asked about the frequency of the PCC/Green Center surveys, Bianca Frogner, PhD, a health economist and deputy director at the University of Washington Primary Care Innovation Lab in Seattle, said it’s unusual to have this regularity. Also, it’s unique in that it offers a constant mix of physicians. “It’s a small sample, but it still gives a voice where there isn’t one.”
Smaller weekly surveys and secondary analysis projects from the Graham Center, an American Academy of Family Physicians affiliated research center, reinforce findings of the Green Center. The Graham Center surveys also found primary care is taking a financial hit, staff is being furloughed, and patient volume is down, according to Dr. Jabbarpour, who has been involved in most of the Graham Center’s work on COVID.
Dr. Frogner, Dr. Etz, and Dr. Jabbarpour agree that, as a nation, the United States has chronically underinvested in primary care, and now the system is in crisis. The hope is that the survey data gives policymakers, state leaders, and the federal government a better idea of what’s happening on the ground.
It’s also important for researchers “keeping an eye out for the available supply of primary care for certain populations,” Dr. Frogner said. The current conditions are especially a threat to rural and underserved areas, she added.
If primary health care isn’t near recovery that’s a problem for the entire population, Dr. Etz said. And what happens if there’s another surge of COVID-19 or even a second pandemic in our lifetime? Her recommendation: Treat it like disaster recovery. Step one is “Stop the hemorrhaging – they need immediate cash flow.”
A version of this article originally appeared on Medscape.com.
published by the Primary Care Collaborative (PCC) and Larry A. Green Center.
Since mid-March these organizations have issued short weekly and biweekly surveys to U.S. primary care physicians in an attempt to find the pulse of the county’s first line of care. “There is not a federal office for primary care, and it’s been anemically funded for decades,” Rebecca Etz, PhD, said in an interview. Yet these clinics represent the front lines of U.S. health care, and it’s where most Americans go for care and COVID-19 care, said Dr. Etz, director of the Virginia-based Larry A. Green Center, which is devoted to primary care research, development, and advocacy.
The latest survey responses, collected between Sept. 4 and 6, confirm what researchers had suspected: Primary care isn’t on solid footing. Eighty-one percent of respondents disagreed emphatically that primary care has bounced back, and another 13% said things were better than earlier this year but not normal.
Meanwhile, 35% of respondents said that revenue and pay are significantly lower than they were before the pandemic and net losses threaten their practices’ viability. Almost half (49%) said their mental exhaustion from work was at an all-time high.
“Because of how our system is set up – it’s a fee-for-service model – the more patients you see, the more money you get,” said Yalda Jabbarpour, MD, medical director at the Graham Center, a leading think tank on family medicine and health care policy. But the stay-at-home order, aversion to telehealth, and fear of in-person visits have been keeping patients away – and driving primary care revenue down. Even when practices transition to and expand their telehealth, payer reimbursement is not yet on parity with in-person visits.
Right now, primary care physicians are doing fewer procedures and spending more time on video visits. “So you may have the same overhead and time investment but you’re getting paid a fraction,” Dr. Etz said. In August, 50% of primary care physicians reported they were working the same or more hours per week as they did before the pandemic but for less money, according to an earlier survey from the Green Center and the PCC. That loss of revenue is compounded by the need for expensive personal protective equipment and preparation for the upcoming flu season, Dr. Etz said.
Ongoing surveys reveal stress
Over the last 20 weeks or so, the Green Center and PCC together have disseminated weekly (through June) or biweekly surveys to 100 professional organizations. Because there isn’t an entity that represents all of primary care and claims data take years to process, these surveys are intended to get real-time feedback from clinicians who are providing a lot of patient care during the pandemic.
The sample sizes are admittedly small, with the most recent survey including 489 clinicians. Dr. Jabbarpour noted, “489 – it’s a good number, but you would want more.” Generally, for a great survey response you’d want 20%-30% of the physician population because then you could assume you’re getting a good mix of geographies, practice sizes, and settings, she said.
Respondents to the most recent survey were from 49 different states; 70% identified their practice as family medicine. One-third had between one and three physicians in their practice and 40% had 10 or more clinicians. “It’s not perfect, but it sounds pretty representative of the primary care workforce,” Dr. Jabbarpour continued.
The latest Green Center-PCC survey, published last week, also found that one in five physicians surveyed said at least one clinician in their practice had opted for early retirement or left practice as a direct result of the pandemic. These declines in clinician staffing come as school reopenings threaten to cause a resurgence of COVID-19 cases and the 2021 flu season could complicate COVID-19 care and testing.
Shortfall could cascade to other specialties
News that primary care is both struggling and shrinking doesn’t come as a surprise to those who research this area, according to Dr. Jabbarpour. Yet it matters “because primary care is where the majority of Americans get their health care.” According to the Centers for Disease Control and Prevention, primary care accounts for 50% of all office visits. But the sector only encompasses 30% of the clinician workforce, according to a 2019 study of physician supply, and accounts for just 7% of national health expenditures, according to a separate 2019 study that measured primary care investment.
If primary care doesn’t bounce back, the shortfall could overwhelm the rest of the health care system, Dr. Jabbarpour said. “If primary care shortages increase, then urgent cares, ERs, and hospitals will become overwhelmed.”
Or public health could suffer as people don’t seek care at all. A study published earlier this summer found that up to 35% of excess deaths during the pandemic were not caused by COVID-19. Instead, they can be attributed to treatable causes, like heart disease, diabetes, and Alzheimers, the researchers concluded. In Dr. Etz’s estimation, this high cost is a glimpse of what happens when there isn’t adequate access to primary care.
When asked about the frequency of the PCC/Green Center surveys, Bianca Frogner, PhD, a health economist and deputy director at the University of Washington Primary Care Innovation Lab in Seattle, said it’s unusual to have this regularity. Also, it’s unique in that it offers a constant mix of physicians. “It’s a small sample, but it still gives a voice where there isn’t one.”
Smaller weekly surveys and secondary analysis projects from the Graham Center, an American Academy of Family Physicians affiliated research center, reinforce findings of the Green Center. The Graham Center surveys also found primary care is taking a financial hit, staff is being furloughed, and patient volume is down, according to Dr. Jabbarpour, who has been involved in most of the Graham Center’s work on COVID.
Dr. Frogner, Dr. Etz, and Dr. Jabbarpour agree that, as a nation, the United States has chronically underinvested in primary care, and now the system is in crisis. The hope is that the survey data gives policymakers, state leaders, and the federal government a better idea of what’s happening on the ground.
It’s also important for researchers “keeping an eye out for the available supply of primary care for certain populations,” Dr. Frogner said. The current conditions are especially a threat to rural and underserved areas, she added.
If primary health care isn’t near recovery that’s a problem for the entire population, Dr. Etz said. And what happens if there’s another surge of COVID-19 or even a second pandemic in our lifetime? Her recommendation: Treat it like disaster recovery. Step one is “Stop the hemorrhaging – they need immediate cash flow.”
A version of this article originally appeared on Medscape.com.