User login
Hospital Observation Care
Observation hospitalization is a growing phenomenon in the United States healthcare system.[1] For Medicare beneficiaries, observation encounters increased 33.6% from 2004 to 2011, with inpatient encounters decreasing by 7.8% over the same period.[2]
Observation length of stay has also increased. Medicare states that observation care should typically last <24 hours, and in only rare and exceptional cases exceed 48 hours. We and others have showed that observation stays, on average, do not meet this definition.[1, 3] At our institution, historically less than half of observation encounters discharge in under 24 hours, and 1 in 6 stay longer than 48 hours.[3]
The Centers for Medicare and Medicaid Services (CMS) issued a rules change effective October 1, 2013, in response to concern about recent increases in the length of time that CMS beneficiaries spend as hospital outpatients receiving observation services.[4] These rules shifted observation determination from clinical criteria, such as InterQual,[5] to a time‐based rule that hinges on a 2‐midnight cut point. Patients staying <2 midnights, with few exceptions, are now observation, and those staying 2 midnights are inpatients. This is important, as patients hospitalized as observation are technically outpatients, not covered by Medicare Part A hospital insurance, and ineligible for skilled nursing facility benefits.[3, 6]
Although challenges with observation status in general are well described,[1, 3, 7] the potential impact of the 2‐midnight rule is not fully known. The purpose of our descriptive study was to examine how the new rules, retrospectively applied to recent encounters, would affect our hospital encounters, with a separate analysis of Medicare encounters and adult general medicine encounters. First, as CMS predicted a net shift from outpatient to inpatient stays[8] under the new rule, we attempted to determine whether this rule would actually reduce observation encounter frequency. Second, as CMS has cited persistently large improper payment rates in short‐stay hospital inpatient claims[4] and intends to audit <2‐midnight inpatient encounters under the assumption that many are misclassified observation stays,[4, 8, 9] we sought to determine if short‐stay inpatient and observation encounters were truly the same. Third, as insurance coverage will change based on the 2‐midnight cut point, we sought to determine whether 2 midnights separated distinct clinical populations within observation status, making the rule logical and fair. Finally, we sought to determine whether external factors, such as time of admission, day of week of admission, and transfer to our institution would impact how patients may be classified under the new rule.
METHODS
Study Population
Our methods have been described previously[3] with the exception of the updated dates of inclusion. Briefly, we analyzed all observation and inpatient encounters at University of Wisconsin Hospital and Clinics (UWHC) and the adjacent American Family Children's Hospital, a tertiary care referral academic medical center in Madison, Wisconsin,[10] with start date between January 1, 2012 and February 28, 2013. Six encounters with length of stay (LOS) >6 months were censored as they were not discharged by the time of data abstraction, and 3 encounters were removed due to erroneous encounter discharge dates. Patients with all insurance types were included in anticipation that commercial payors will follow Medicare rules changes. The University of Wisconsin (UW) Health Sciences Institutional Review Board approved the study.
Data Sources
Data were abstracted from the UW Health Sciences electronic medical record and ancillary data systems by the UWHC Business Planning and Analysis Department. Variables included demographics (age, sex, ethnicity), insurance type, and characteristics of hospitalization (admission service, day of week encounter began, acute/unscheduled presentation, International Classification of Diseases, 9th Revision [ICD‐9] codes, LOS, transfer from other hospital). We considered inpatient admission start time to be departure from the emergency department (ED) or arrival at our hospital if the encounter was a transfer from another facility. Observation start time also hinged on arrival at our hospital if the encounter was transferred from another facility, but for observation encounters arriving from the ED, the ED rooming time was used as the encounter start based on conservative interpretation of CMS rules for observation start time under the 2‐midnight rule.[11] Discharge time for all encounters was considered physical discharge from the ward. Observation status decisions were made by the admitting physician, with as‐needed guidance by case management staff and utilization review physicians using InterQual Criteria (McKesson Corp, San Francisco, CA),[5] a reference historically used by CMS auditors to determine status.
Evaluation of the 2‐Midnight Rule
All encounters were stratified based on a stay of <2 midnights or 2 midnights. Because general medicine patients comprise the bulk of observation patients,[3] the subset of encounters occurring on the hospital's 4 hospitalist medicine services, 3 general medicine resident services, and 1 adult nonobstetrics family medicine service, collectively termed adult general medicine, were also evaluated separately. Medicare encounters were also evaluated separately.
We first specifically compared <2‐midnight inpatient encounters and 2‐midnight observation encounters during the study period to determine the net number of encounters that would lose inpatient status (<2‐midnight inpatient encounters) and that would gain inpatient status (2‐midnight observation encounters) under the new rules. Subtracting the absolute number of <2‐midnight inpatient encounters from the 2‐midnight observation encounters results in the net loss or gain of inpatient encounters, assuming LOS does not change. Second, we compared ICD‐9 codes between <2‐midnight inpatient encounters and observation encounters to determine if these 2 groups were clinically distinguishable. Third, we compared diagnosis codes between observation encounters lasting <2 midnights and 2 midnights to establish whether the 2‐midnight cut point defines distinct patient groups within observation. Finally, we evaluated all observation encounters to determine whether the time of admission, the day of admission (weekday vs weekend), or whether the encounter had been transferred from another facility impacted encounter categorization under the new rules.
Statistical Methods
Descriptive statistics were used in this study, with data largely summarized as number and percent. When appropriate, mean and standard deviation were used to describe central tendency and dispersion.
RESULTS
Characteristics of Inpatient and Observation Encounters
Of the 36,193 total hospital encounters during the study period, 4769 (13.2%) were classified as observation encounters. Of 8510 adult general medicine encounters, 2443 (28.7%) were observation. Adult general medicine observation encounters accounted for 51.2% of all observation encounters for the hospital. A total of 9.0% of our observation encounters were transferred from another institution (Table 1).
| Inpatient, n=31,424 (86.8%) | Observation, n=4,769 (13.2%) | |
|---|---|---|
| ||
| Demographics | ||
| Female | 15,083 (48.0%) | 2,321 (48.7%) |
| Age, y, mean (SD) | 49.2 (23.6) | 49.4 (25.4) |
| Has primary care provider | 27,378 (87.1%) | 4,152 (87.1%) |
| Ethnicity | ||
| Caucasian | 27,145 (86.4%) | 3,880 (81.4%) |
| Non‐Caucasian | 3,478 (11.1%) | 739 (15.5%) |
| Unknown | 801 (2.5%) | 150 (3.1%) |
| Characteristics of hospitalization | ||
| Day of admission | ||
| Weekend (SaturdaySunday) | 5,058 (16.1%) | 1,129 (23.7%) |
| Weekday (MondayFriday) | 26,360 (83.9%) | 3,640 (76.3%) |
| Transfer from other institution | 6,191 (19.7%) | 427 (9.0%) |
| Acute/unscheduled | 21,150 (67.3%) | 4,479 (93.9%) |
| Service of admission | ||
| Adult general medicine | 6,067 (19.3%) | 2,443 (51.2%) |
| Adult surgery | 13,625 (43.4%) | 856 (17.9%) |
| Adult subspecialty nonsurgery | 7,432 (23.7%) | 802 (16.8%) |
| Pediatrics | 4,300 (13.7%) | 668 (14.0%) |
| Insurance | ||
| Medicare | 11,719 (37.3%) | 1,846 (38.7%) |
| Medicaid | 3,642 (11.6%) | 658 (13.8%) |
| Commercial | 13,321 (42.4%) | 1,817 (38.1%) |
| Other | 1,665 (5.3%) | 184 (3.9%) |
| None | 1,077 (3.4%) | 264 (5.5%) |
A total of 1442 (4.0%) encounters changed status during the study period, with 606 (42.0%) having changed from inpatient to observation and considered observation, and 836 (58.0%) having changed from observation to inpatient and considered inpatient.
Impact of the 2‐Midnight Rule on Number of Observation and Inpatient Encounters
Among all encounters, the 2‐midnight rule would result in a net transition of 14.9% of inpatient encounters to observation. Considering only Medicare encounters, the net transition would be 7.4% inpatient encounters to observation. Within adult general medicine patients, the parallel changes would be 2.2% (all insurance types) and a gain of 2.4% (Medicare only) (Table 2).
| Inpatient, n=31,424 (86.8%) | Observation, n=4,769 (13.2%) | |
|---|---|---|
| ||
| All encounters, n=36,193 | ||
| <2 Midnights | 6,723* (21.4%) | 3,454 (72.4%) |
| 2 Midnights | 24,701 (78.6%) | 1,315* (27.6%) |
| Net change inpatient encounters | 5,408 (14.9%) | |
| Medicare encounters, n=13,565 | ||
| <2 Midnights | 1,728* (14.7%) | 1,127 (61.1%) |
| 2 Midnights | 9,991 (85.3%) | 719* (38.9%) |
| Net change inpatient encounters | 1,009 (7.4%) | |
| All general medicine, n=8,510 | ||
| <2 Midnights | 1,114* (18.4%) | 1,512 (61.9%) |
| 2 Midnights | 4,953 (81.6%) | 931* (38.1%) |
| Net change inpatient encounters | 183 (2.2%) | |
| Medicare general medicine, n=4,571 | ||
| <2 Midnights | 472* (14.3%) | 690 (54.2%) |
| 2 Midnights | 2,827 (85.7%) | 582* (45.8%) |
| Net change inpatient encounters | 110 (2.4%) | |
Encounters including surgical procedures on the so‐called inpatient‐only list will remain inpatient regardless of LOS. As we could not identify such encounters, we tested removal of all surgical stays under the overly conservative assumption that all short stay surgical patients would remain inpatient. Of 21,712 nonsurgical encounters that remained, there were 4074 <2‐midnight inpatient encounters and 1146 2‐midnight observation encounters, yielding a net transition of 2928 (13.5%) inpatient encounters to observation encounters. Medicare encounters accounted for 8240 of these 21,712 (38.0%) nonsurgical encounters, with 1105 <2‐midnight inpatient encounters and 653 2‐midnight observation encounters, yielding a net reclassification of 452 (5.5%) Medicare nonsurgical inpatient encounters to observation encounters.
Length of Stay and Diagnoses After Application of the 2‐Midnight Rule to Inpatient and Observation Encounters
Only 1 of the top 5 ICD‐9 codes (code 427: cardiac dysrhythmias) was shared between the 2‐midnight inpatient encounters and any observation encounter group. When the same criteria were applied to adult general medicine encounters, none of the top 5 ICD‐9 codes were shared (Table 3).
| All Encounters, n=36,193 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Inpatient Stays Shorter Than 2 Midnights, n=6,723 (21.4%) | Inpatient Stays 2 Midnights, n=24,701 (78.6%) | Observation Stays Shorter Than 2 Midnights, n=3,454 (72.4%) | Observation Stays 2 Midnights n=1,315 (27.6%) | |||||
| ||||||||
| Day of admission | ||||||||
| Weekend (Saturday Sunday) | 1,026 (15.3%) | 4,032 (16.3%) | 781 (22.6%) | 348 (26.5%) | ||||
| Weekday (MondayFriday) | 5,697 (84.7%) | 20,669 (83.7%) | 2,673 (77.4%) | 967 (73.5%) | ||||
| Transfer from another institution | 986 (14.7%) | 5,205 (21.1%) | 297 (8.6%) | 130 (9.9%) | ||||
| Top diagnosis codes | ||||||||
| ICD‐9 #1 | 996: Complications peculiar to specific procedure | 200 (3.0%) | 996: Complications peculiar to specific procedure | 1,355 (5.5%) | 786: Symptoms involving respiratory/other chest | 531 (15.4%) | 780: General symptoms | 124 (9.4%) |
| ICD‐9 #2 | 427: Cardiac dysrhythmias | 195 (2.9%) | 715: Osteoarthrosis and allied disorders | 917 (3.7%) | 780: General symptoms | 235 (6.8%) | 786: Symptoms involving respiratory/other chest | 80 (6.1%) |
| ICD‐9 #3 | 722: Intervertebral disk disorder | 182 (2.7%) | 038: Septicemia | 689 (2.8%) | 427: Cardiac dysrhythmias | 103 (3.0%) | 789: Other symptoms involving abdomen/pelvis | 48 (3.7%) |
| ICD‐9 #4 | 540: Acute appendicitis | 179 (2.7%) | 296: Episodic mood disorder | 619 (2.5%) | 789: Other symptoms involving abdomen/pelvis | 89 (2.6%) | 787: Symptoms involving digestive system | 38 (2.9%) |
| ICD‐9 #5 | V58: Encounter for other and unspecified procedures | 176 (2.6%) | 998: Other complications of procedures not elsewhere classified | 516 (2.1%) | 787: Symptoms involving digestive system | 56 (1.6%) | 599: Other disorders of urethra/urinary tract | 35 (2.7%) |
| Adult General Medicine Encounters, n=8,510 | ||||||||
| Inpatient Stays Shorter Than 2 Midnights, n=1,114 (18.4%) | Inpatient Stays 2 Midnights, n=4,953 (81.6%) | Observation Stays Shorter Than 2 Midnights, n=1,512 (61.9%) | Observation Stays 2 Midnights, n=931 (38.1%) | |||||
| Day of admission | ||||||||
| Weekend (Saturday Sunday) | 253 (22.7%) | 1,189 (24.0%) | 318 (21.0%) | 261 (28.0%) | ||||
| Weekday (MondayFriday) | 861 (77.3%) | 3,764 (76.0%) | 1,194 (79.0%) | 670 (72.0%) | ||||
| Transfer from another institution | 89 (8.0%) | 1,193 (24.1%) | 61 (4.0%) | 75 (8.1%) | ||||
| Top diagnosis codes | ||||||||
| ICD‐9 #1 | 415: Acute pulmonary heart disease | 57 (5.1%) | 038: Septicemia | 423 (8.5%) | 786: Symptoms involving respiratory/other chest | 315 (20.8%) | 780: General symptoms | 99 (10.6%) |
| ICD‐9 #2 | 276: Disorders of fluid/electrolyte, acid/base | 51 (4.6%) | 486: Pneumonia | 206 (4.2%) | 780: General symptoms | 138 (9.1%) | 786: Symptoms involving respiratory/other chest | 51 (5.5%) |
| ICD‐9 #3 | 682: Other cellulitis and abscess | 47 (4.2%) | 584: Acute kidney failure | 181 (3.7%) | 789: Other symptoms involving abdomen/pelvis | 47 (3.1%) | 789: Other symptoms involving abdomen/pelvis | 37 (4.0%) |
| ICD‐9 #4 | 427: Cardiac dysrhythmias | 43 (3.9%) | 577: Diseases of the pancreas | 181 (3.7%) | 787: Symptoms involving digestive system | 35 (2.3%) | 599: Other disorders of urethra/urinary tract | 30 (3.2%) |
| ICD‐9 #5 | 250: Diabetes mellitus | 40 (3.6%) | 682: Other cellulitis and abscess | 175 (3.5%) | 305: Nondependent abuse of drugs | 32 (2.1%) | 787: Symptoms involving digestive system | 28 (3.0%) |
Including all observation encounters across LOS, 4 of the 5 top ICD‐9 codes were the same for stays <2 midnights and 2 midnights. The same was true for short‐ and long‐stay general medicine observation encounters (Table 3).
For all observation encounters, 26.5% (348/1315) of 2‐midnight encounters started on a weekend compared to 22.6% (781/3454) of <2‐midnight encounters. For adult medicine observation, 28.0% (261/931) of 2‐midnight encounters started on a weekend compared to 21.0% (318/1512) of <2‐midnight encounters (Table 3).
Percentage of Observation Encounters Reaching 2 Midnights Based on Time of Hospitalization
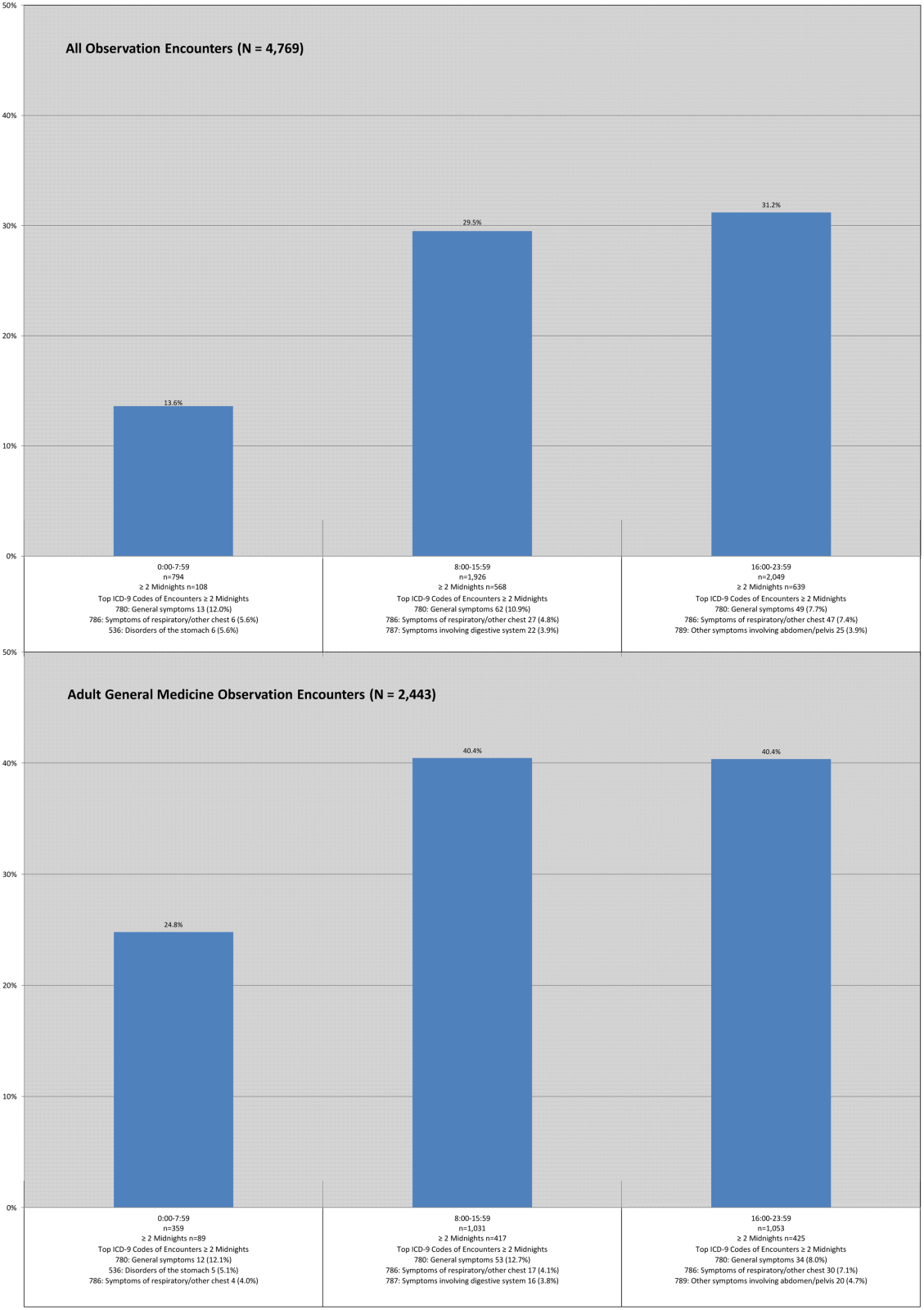
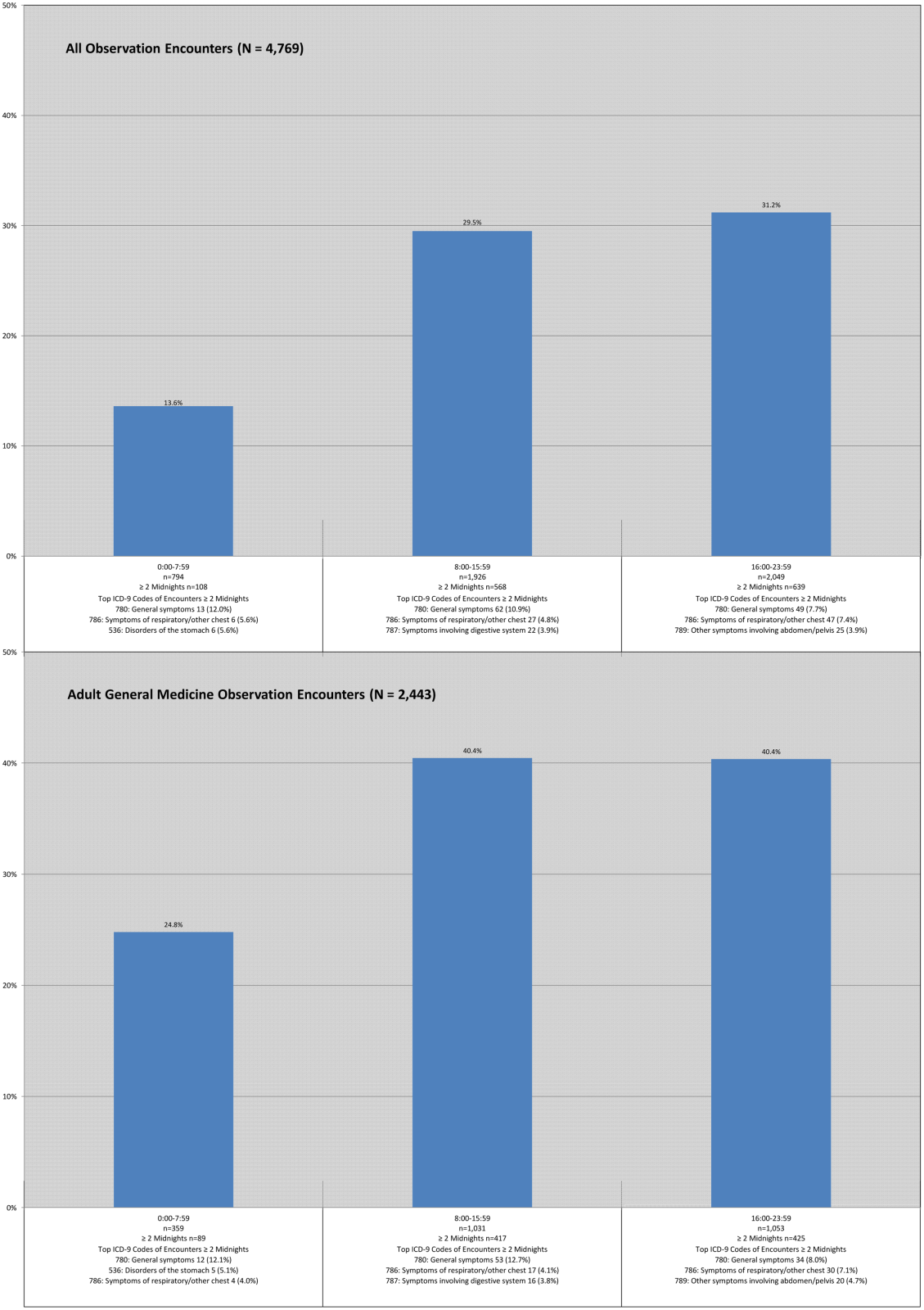
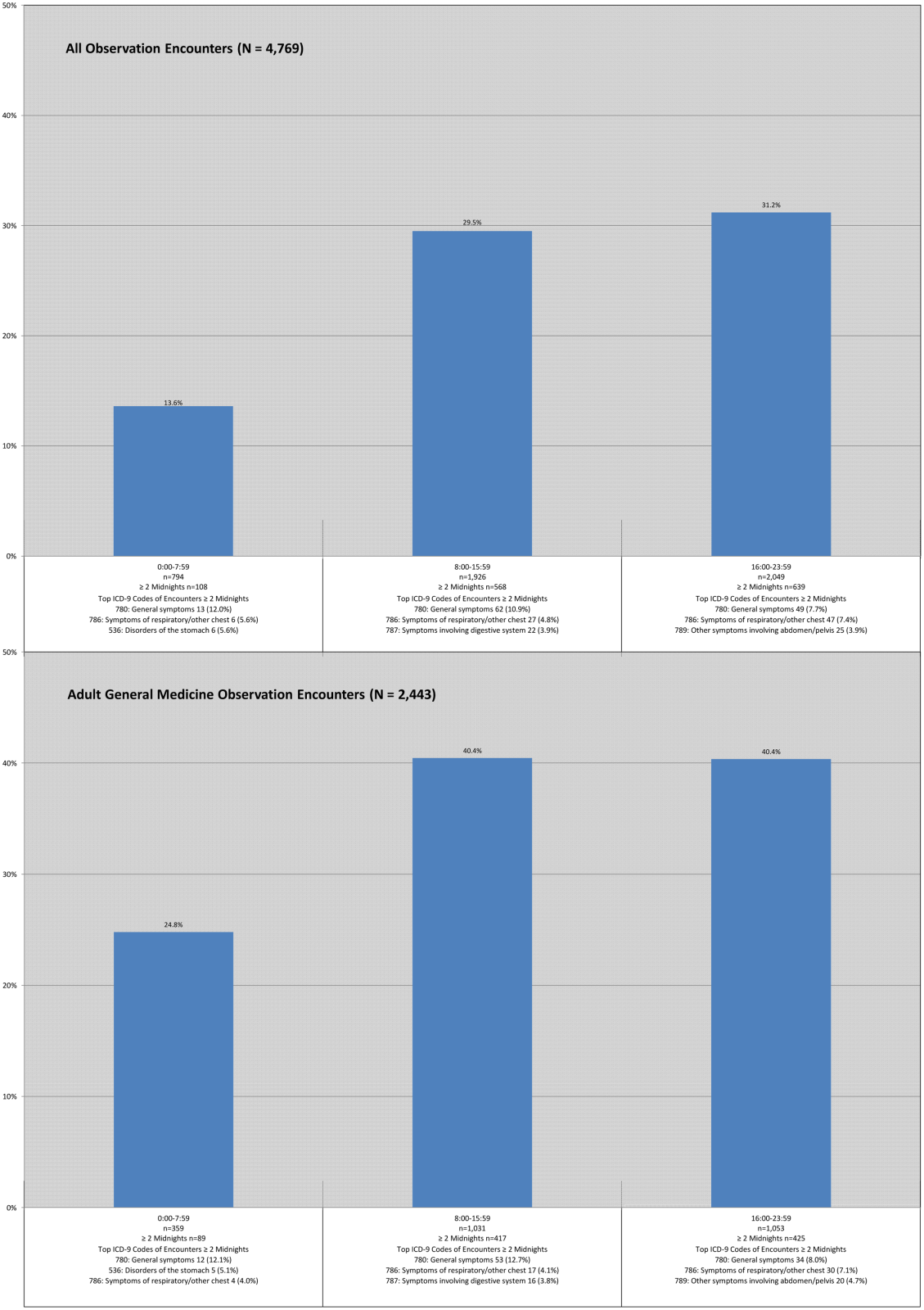
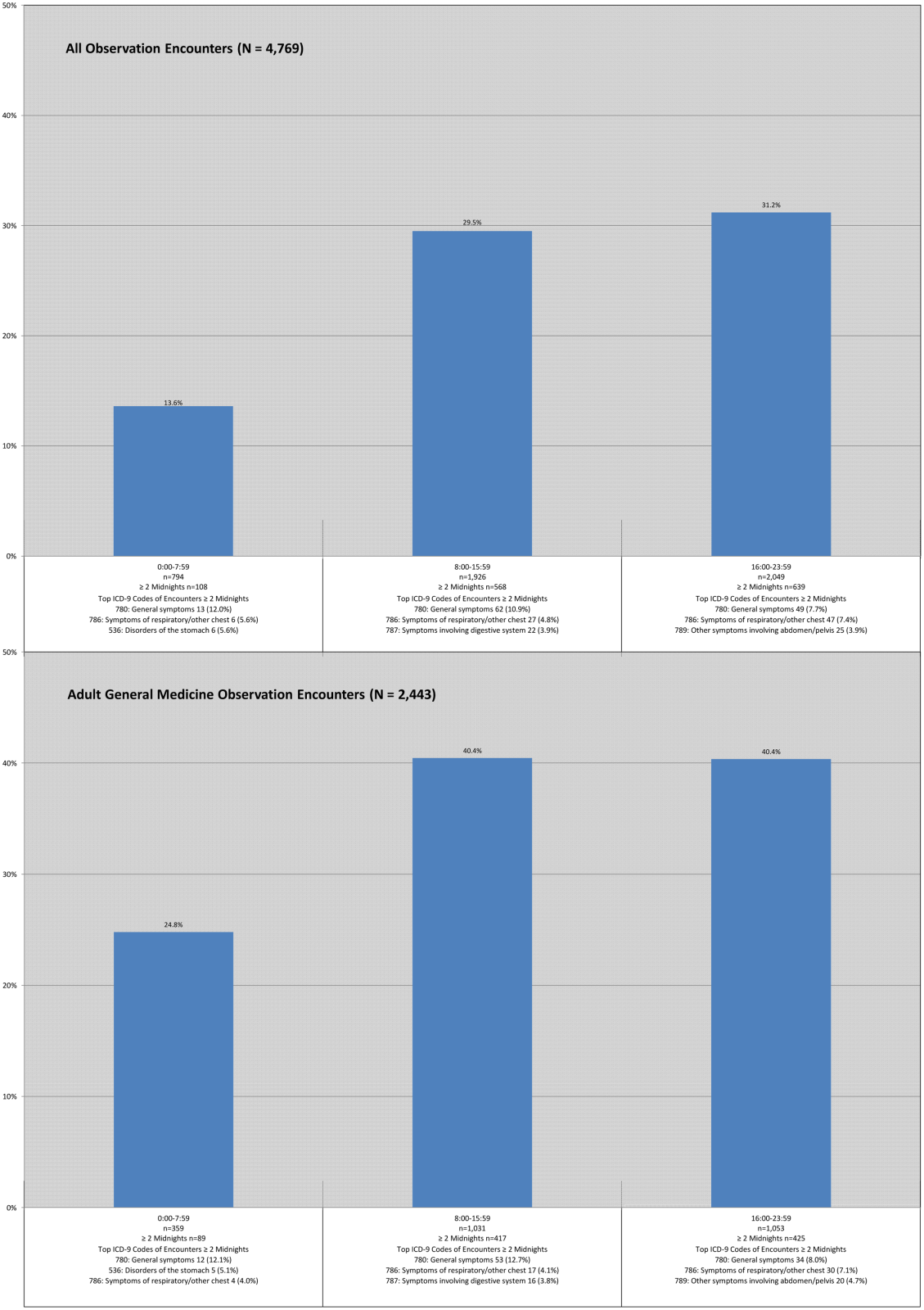
Observation encounters starting before 8:00 am spanned 2 midnights 13.6% of the time, and those encounters starting after 4:00 pm crossed 2 midnights 31.2% of the time. Two of the 3 top ICD‐9 codes were the same across LOS, with similar findings for the adult general medicine‐only group (Figure 1).
DISCUSSION
Although CMS predicts that more patients will be classified as inpatients under the new rule, we determined the opposite, consistent with a recent report generated by the Office of the Inspector General (OIG) for 2012 Medicare beneficiaries.[8] Our results did not change when we excluded all surgical encounters to account for possible exclusions based on the surgical inpatient‐only list. Although a small percentage of Medicare adult general medicine patients may be reclassified as inpatients under the new rules, the net effect would be that many more hospital encounters will be billed under observation rather than inpatient status. These findings assume overall length of stay will remain unchanged under these rules, an assumption that may not hold true given the financial losses we predicted hospitals may face under this rule,[12] and potential pressures on individual physicians providing patient care.
Medicare has prioritized auditing <2‐midnight inpatient encounters under the assumption that many short inpatient encounters are actually misclassified observation encounters,[4, 8, 9] prompting us to investigate whether this was the case in our patient population. Although it did not use ICD‐9 diagnosis codes, the OIG report suggested that short‐stay inpatients and observation patients may be clinically similar.[8, 13] Using ICD‐9 codes, we found no overlap between the top ICD‐9 codes for adult general medicine <2‐midnight inpatient and observation encounters, and only 1 of 5 shared codes for these encounters across all service lines. These findings are counter to the OIG report, and suggest that <2‐midnight inpatients are different from observation patients at our institution, and that <2‐midnight inpatients should not be arbitrarily reclassified as observation based solely upon LOS.
We also found that the majority of top ICD‐9 codes within observation were the same regardless of LOS, suggesting that LOS does not reliably differentiate clinically different observation populations that merit different insurance coverage (Medicare Part A for 2‐midnight encounters, Medicare Part B for <2‐midnight encounters). This lack of a clear cut point may drive an overall increase in LOS to achieve 2 midnights, as common diagnosis codes can be justified for both <2‐midnight or 2‐midnight observation stays.
Finally, we found that external factors, such as the time of day and specific day (weekday vs weekend) of hospitalization, impact the likelihood of achieving a 2‐midnight stay. Patients hospitalized earlier in the day were less likely to span 2 midnights compared to later‐day encounters, suggesting that use of a full working day as the day of presentation is harmful to a patient's chance of gaining inpatient status. Observation hospitalizations starting on a weekend day were more likely to achieve 2 midnights, which likely reflects different resource allocation and hospital efficiency on weekends, yet it is unlikely that weekend midnights, if associated with any delay in care, will be counted toward a patient's cumulative 2‐midnight total. The CMS has further indicated that midnights accrued prior to transfer from 1 hospital to another will not count toward a cumulative 2‐midnight stay. Although it would seem likely that patients requiring transfer to a tertiary care center would meet inpatient criteria, 9% of our observation encounters were transferred from other acute care hospitals, and many will have lost attributable midnights accrued prior to transfer to our hospital. Taken together, our findings strongly suggest that issues entirely unrelated to diagnosis or clinical status will impact whether hospitalized patients will be classified as inpatient or observation under the new rule.
This study has several limitations. Our data were limited to a single Midwestern tertiary care academic medical center, and may not be applicable to other healthcare settings. Second, 1.5% (466) of our inpatient stays and 56 (1.2%) of our observation encounters lacked a referral source in our administrative database, although these deficiencies would not likely change the conclusions. Finally, the total number of observation encounters starting before 8:00 am and staying 2 midnights was small and therefore potentially subject to confounding. However, despite the fact that encounters beginning in the early morning hours may be different in ways unable to be measured in this study, encounter ICD‐9 codes were similar regardless of time of day.
Despite these limitations, our study raises concerns about the impact of CMS's new time‐driven observation rules on hospital practice patterns. We found distinctly different <2‐midnight inpatient ICD‐9 codes as compared to those for observation encounters. Reclassifying <2‐midnight inpatients as observation may inappropriately shift the financial burden of acute hospitalizations to patients who were previously eligible to receive Medicare inpatient benefits. We also demonstrated a decrease in billable inpatient encounters under the new rules, which may be countered by changes in hospital and provider practice to drive more admissions over the 2‐midnight threshold to avoid financial losses. These changes should be defensible under audit given the ambiguities of the rule we found in this study surrounding time of day of admission, weekend and transfer hospitalizations, and the fact that common observation ICD‐9 codes are similar across LOS. Ironically, the unintended consequence of the new rule may be to drive up hospital LOS, reduce efficiency, and increase the overall cost of care.
Our findings suggest that CMS should define observation care per its original intent: as a means to determine if a patient can safely return home after a short period of additional care.[6] Patients whose conditions necessitate an intensity and level of service beyond this narrow scope should be classified as full inpatients irrespective of LOS, whether that LOS is <2 midnights or 2 midnights. Policies that fail to reflect the original intent of observation status are unlikely to achieve the intended outcome of defining 2 distinct patient populations that merit different services and reimbursement.
Acknowledgements
The authors thank Andrew LaRocque and Dan Dexter for their assistance with the data. Without their help, this article would not have been possible.
Disclosures: Dr. Graf reports receiving royalties from Smith & Nephew for patents he has assigned to them involving orthopedic implants. This is unrelated to the topic or content of this manuscript. The authors report no other conflicts of interest.
Editor's Note: On February 24, 2014, after this manuscript was published, CMS issued a rules clarification allowing midnights spent at a referral hospital prior to transfer to be counted in the cumulative 2 midnight tally to determine inpatient status.
- , , . Sharp rise in Medicare enrollees being held hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251–1259.
- MedPAC report to Congress: hospital inpatient and outpatient services. Available at: http://www.medpac.gov/chapters/Mar13_Ch03.pdf. Accessed September 29, 2013.
- , , , et al. Hospitalized but not admitted: characteristics of patients with “Observation Status” at an academic medical center. JAMA Intern Med. 2013;173(21):1991–1998.
- Centers for Medicare and Medicaid Services inpatient prospective payment system 1599‐F. Fiscal year 2014 final rule. Available at: http://www.gpo.gov/fdsys/pkg/FR‐2013‐08‐19/pdf/2013–18956.pdf. Accessed December 22, 2013.
- McKesson Interqual. Available at: http://www.mckesson.com/en_us/McKesson.com/Payers/Decision%2BManagement/InterQual%2BEvidence‐Based%2BClinical%2BContent/InterQual%2BEvidence‐Based%2BClinical%2BContent.html. Accessed October 3, 2013.
- Medicare benefit policy manual. Chapter 6. Hospital services covered under Part B. Available at: https://www.cms.gov/transmittals/downloads/R42BP.pdf. Accessed December 22, 2013.
- . Thinking of admitting this patient? Think again: how observation care is complicating life for you (and your patients). Today's Hospitalist. Available at: http://www.todayshospitalist.com/index.php?b=articles_read173(21):2004–2006.
- Kaiser Health News. HHS Inspector General scrutinizes Medicare observation care policy. Available at: http://www.kaiserhealthnews.org/stories/2013/july/30/ig‐report‐observation‐care.aspx. Accessed October 3, 2013.
Observation hospitalization is a growing phenomenon in the United States healthcare system.[1] For Medicare beneficiaries, observation encounters increased 33.6% from 2004 to 2011, with inpatient encounters decreasing by 7.8% over the same period.[2]
Observation length of stay has also increased. Medicare states that observation care should typically last <24 hours, and in only rare and exceptional cases exceed 48 hours. We and others have showed that observation stays, on average, do not meet this definition.[1, 3] At our institution, historically less than half of observation encounters discharge in under 24 hours, and 1 in 6 stay longer than 48 hours.[3]
The Centers for Medicare and Medicaid Services (CMS) issued a rules change effective October 1, 2013, in response to concern about recent increases in the length of time that CMS beneficiaries spend as hospital outpatients receiving observation services.[4] These rules shifted observation determination from clinical criteria, such as InterQual,[5] to a time‐based rule that hinges on a 2‐midnight cut point. Patients staying <2 midnights, with few exceptions, are now observation, and those staying 2 midnights are inpatients. This is important, as patients hospitalized as observation are technically outpatients, not covered by Medicare Part A hospital insurance, and ineligible for skilled nursing facility benefits.[3, 6]
Although challenges with observation status in general are well described,[1, 3, 7] the potential impact of the 2‐midnight rule is not fully known. The purpose of our descriptive study was to examine how the new rules, retrospectively applied to recent encounters, would affect our hospital encounters, with a separate analysis of Medicare encounters and adult general medicine encounters. First, as CMS predicted a net shift from outpatient to inpatient stays[8] under the new rule, we attempted to determine whether this rule would actually reduce observation encounter frequency. Second, as CMS has cited persistently large improper payment rates in short‐stay hospital inpatient claims[4] and intends to audit <2‐midnight inpatient encounters under the assumption that many are misclassified observation stays,[4, 8, 9] we sought to determine if short‐stay inpatient and observation encounters were truly the same. Third, as insurance coverage will change based on the 2‐midnight cut point, we sought to determine whether 2 midnights separated distinct clinical populations within observation status, making the rule logical and fair. Finally, we sought to determine whether external factors, such as time of admission, day of week of admission, and transfer to our institution would impact how patients may be classified under the new rule.
METHODS
Study Population
Our methods have been described previously[3] with the exception of the updated dates of inclusion. Briefly, we analyzed all observation and inpatient encounters at University of Wisconsin Hospital and Clinics (UWHC) and the adjacent American Family Children's Hospital, a tertiary care referral academic medical center in Madison, Wisconsin,[10] with start date between January 1, 2012 and February 28, 2013. Six encounters with length of stay (LOS) >6 months were censored as they were not discharged by the time of data abstraction, and 3 encounters were removed due to erroneous encounter discharge dates. Patients with all insurance types were included in anticipation that commercial payors will follow Medicare rules changes. The University of Wisconsin (UW) Health Sciences Institutional Review Board approved the study.
Data Sources
Data were abstracted from the UW Health Sciences electronic medical record and ancillary data systems by the UWHC Business Planning and Analysis Department. Variables included demographics (age, sex, ethnicity), insurance type, and characteristics of hospitalization (admission service, day of week encounter began, acute/unscheduled presentation, International Classification of Diseases, 9th Revision [ICD‐9] codes, LOS, transfer from other hospital). We considered inpatient admission start time to be departure from the emergency department (ED) or arrival at our hospital if the encounter was a transfer from another facility. Observation start time also hinged on arrival at our hospital if the encounter was transferred from another facility, but for observation encounters arriving from the ED, the ED rooming time was used as the encounter start based on conservative interpretation of CMS rules for observation start time under the 2‐midnight rule.[11] Discharge time for all encounters was considered physical discharge from the ward. Observation status decisions were made by the admitting physician, with as‐needed guidance by case management staff and utilization review physicians using InterQual Criteria (McKesson Corp, San Francisco, CA),[5] a reference historically used by CMS auditors to determine status.
Evaluation of the 2‐Midnight Rule
All encounters were stratified based on a stay of <2 midnights or 2 midnights. Because general medicine patients comprise the bulk of observation patients,[3] the subset of encounters occurring on the hospital's 4 hospitalist medicine services, 3 general medicine resident services, and 1 adult nonobstetrics family medicine service, collectively termed adult general medicine, were also evaluated separately. Medicare encounters were also evaluated separately.
We first specifically compared <2‐midnight inpatient encounters and 2‐midnight observation encounters during the study period to determine the net number of encounters that would lose inpatient status (<2‐midnight inpatient encounters) and that would gain inpatient status (2‐midnight observation encounters) under the new rules. Subtracting the absolute number of <2‐midnight inpatient encounters from the 2‐midnight observation encounters results in the net loss or gain of inpatient encounters, assuming LOS does not change. Second, we compared ICD‐9 codes between <2‐midnight inpatient encounters and observation encounters to determine if these 2 groups were clinically distinguishable. Third, we compared diagnosis codes between observation encounters lasting <2 midnights and 2 midnights to establish whether the 2‐midnight cut point defines distinct patient groups within observation. Finally, we evaluated all observation encounters to determine whether the time of admission, the day of admission (weekday vs weekend), or whether the encounter had been transferred from another facility impacted encounter categorization under the new rules.
Statistical Methods
Descriptive statistics were used in this study, with data largely summarized as number and percent. When appropriate, mean and standard deviation were used to describe central tendency and dispersion.
RESULTS
Characteristics of Inpatient and Observation Encounters
Of the 36,193 total hospital encounters during the study period, 4769 (13.2%) were classified as observation encounters. Of 8510 adult general medicine encounters, 2443 (28.7%) were observation. Adult general medicine observation encounters accounted for 51.2% of all observation encounters for the hospital. A total of 9.0% of our observation encounters were transferred from another institution (Table 1).
| Inpatient, n=31,424 (86.8%) | Observation, n=4,769 (13.2%) | |
|---|---|---|
| ||
| Demographics | ||
| Female | 15,083 (48.0%) | 2,321 (48.7%) |
| Age, y, mean (SD) | 49.2 (23.6) | 49.4 (25.4) |
| Has primary care provider | 27,378 (87.1%) | 4,152 (87.1%) |
| Ethnicity | ||
| Caucasian | 27,145 (86.4%) | 3,880 (81.4%) |
| Non‐Caucasian | 3,478 (11.1%) | 739 (15.5%) |
| Unknown | 801 (2.5%) | 150 (3.1%) |
| Characteristics of hospitalization | ||
| Day of admission | ||
| Weekend (SaturdaySunday) | 5,058 (16.1%) | 1,129 (23.7%) |
| Weekday (MondayFriday) | 26,360 (83.9%) | 3,640 (76.3%) |
| Transfer from other institution | 6,191 (19.7%) | 427 (9.0%) |
| Acute/unscheduled | 21,150 (67.3%) | 4,479 (93.9%) |
| Service of admission | ||
| Adult general medicine | 6,067 (19.3%) | 2,443 (51.2%) |
| Adult surgery | 13,625 (43.4%) | 856 (17.9%) |
| Adult subspecialty nonsurgery | 7,432 (23.7%) | 802 (16.8%) |
| Pediatrics | 4,300 (13.7%) | 668 (14.0%) |
| Insurance | ||
| Medicare | 11,719 (37.3%) | 1,846 (38.7%) |
| Medicaid | 3,642 (11.6%) | 658 (13.8%) |
| Commercial | 13,321 (42.4%) | 1,817 (38.1%) |
| Other | 1,665 (5.3%) | 184 (3.9%) |
| None | 1,077 (3.4%) | 264 (5.5%) |
A total of 1442 (4.0%) encounters changed status during the study period, with 606 (42.0%) having changed from inpatient to observation and considered observation, and 836 (58.0%) having changed from observation to inpatient and considered inpatient.
Impact of the 2‐Midnight Rule on Number of Observation and Inpatient Encounters
Among all encounters, the 2‐midnight rule would result in a net transition of 14.9% of inpatient encounters to observation. Considering only Medicare encounters, the net transition would be 7.4% inpatient encounters to observation. Within adult general medicine patients, the parallel changes would be 2.2% (all insurance types) and a gain of 2.4% (Medicare only) (Table 2).
| Inpatient, n=31,424 (86.8%) | Observation, n=4,769 (13.2%) | |
|---|---|---|
| ||
| All encounters, n=36,193 | ||
| <2 Midnights | 6,723* (21.4%) | 3,454 (72.4%) |
| 2 Midnights | 24,701 (78.6%) | 1,315* (27.6%) |
| Net change inpatient encounters | 5,408 (14.9%) | |
| Medicare encounters, n=13,565 | ||
| <2 Midnights | 1,728* (14.7%) | 1,127 (61.1%) |
| 2 Midnights | 9,991 (85.3%) | 719* (38.9%) |
| Net change inpatient encounters | 1,009 (7.4%) | |
| All general medicine, n=8,510 | ||
| <2 Midnights | 1,114* (18.4%) | 1,512 (61.9%) |
| 2 Midnights | 4,953 (81.6%) | 931* (38.1%) |
| Net change inpatient encounters | 183 (2.2%) | |
| Medicare general medicine, n=4,571 | ||
| <2 Midnights | 472* (14.3%) | 690 (54.2%) |
| 2 Midnights | 2,827 (85.7%) | 582* (45.8%) |
| Net change inpatient encounters | 110 (2.4%) | |
Encounters including surgical procedures on the so‐called inpatient‐only list will remain inpatient regardless of LOS. As we could not identify such encounters, we tested removal of all surgical stays under the overly conservative assumption that all short stay surgical patients would remain inpatient. Of 21,712 nonsurgical encounters that remained, there were 4074 <2‐midnight inpatient encounters and 1146 2‐midnight observation encounters, yielding a net transition of 2928 (13.5%) inpatient encounters to observation encounters. Medicare encounters accounted for 8240 of these 21,712 (38.0%) nonsurgical encounters, with 1105 <2‐midnight inpatient encounters and 653 2‐midnight observation encounters, yielding a net reclassification of 452 (5.5%) Medicare nonsurgical inpatient encounters to observation encounters.
Length of Stay and Diagnoses After Application of the 2‐Midnight Rule to Inpatient and Observation Encounters
Only 1 of the top 5 ICD‐9 codes (code 427: cardiac dysrhythmias) was shared between the 2‐midnight inpatient encounters and any observation encounter group. When the same criteria were applied to adult general medicine encounters, none of the top 5 ICD‐9 codes were shared (Table 3).
| All Encounters, n=36,193 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Inpatient Stays Shorter Than 2 Midnights, n=6,723 (21.4%) | Inpatient Stays 2 Midnights, n=24,701 (78.6%) | Observation Stays Shorter Than 2 Midnights, n=3,454 (72.4%) | Observation Stays 2 Midnights n=1,315 (27.6%) | |||||
| ||||||||
| Day of admission | ||||||||
| Weekend (Saturday Sunday) | 1,026 (15.3%) | 4,032 (16.3%) | 781 (22.6%) | 348 (26.5%) | ||||
| Weekday (MondayFriday) | 5,697 (84.7%) | 20,669 (83.7%) | 2,673 (77.4%) | 967 (73.5%) | ||||
| Transfer from another institution | 986 (14.7%) | 5,205 (21.1%) | 297 (8.6%) | 130 (9.9%) | ||||
| Top diagnosis codes | ||||||||
| ICD‐9 #1 | 996: Complications peculiar to specific procedure | 200 (3.0%) | 996: Complications peculiar to specific procedure | 1,355 (5.5%) | 786: Symptoms involving respiratory/other chest | 531 (15.4%) | 780: General symptoms | 124 (9.4%) |
| ICD‐9 #2 | 427: Cardiac dysrhythmias | 195 (2.9%) | 715: Osteoarthrosis and allied disorders | 917 (3.7%) | 780: General symptoms | 235 (6.8%) | 786: Symptoms involving respiratory/other chest | 80 (6.1%) |
| ICD‐9 #3 | 722: Intervertebral disk disorder | 182 (2.7%) | 038: Septicemia | 689 (2.8%) | 427: Cardiac dysrhythmias | 103 (3.0%) | 789: Other symptoms involving abdomen/pelvis | 48 (3.7%) |
| ICD‐9 #4 | 540: Acute appendicitis | 179 (2.7%) | 296: Episodic mood disorder | 619 (2.5%) | 789: Other symptoms involving abdomen/pelvis | 89 (2.6%) | 787: Symptoms involving digestive system | 38 (2.9%) |
| ICD‐9 #5 | V58: Encounter for other and unspecified procedures | 176 (2.6%) | 998: Other complications of procedures not elsewhere classified | 516 (2.1%) | 787: Symptoms involving digestive system | 56 (1.6%) | 599: Other disorders of urethra/urinary tract | 35 (2.7%) |
| Adult General Medicine Encounters, n=8,510 | ||||||||
| Inpatient Stays Shorter Than 2 Midnights, n=1,114 (18.4%) | Inpatient Stays 2 Midnights, n=4,953 (81.6%) | Observation Stays Shorter Than 2 Midnights, n=1,512 (61.9%) | Observation Stays 2 Midnights, n=931 (38.1%) | |||||
| Day of admission | ||||||||
| Weekend (Saturday Sunday) | 253 (22.7%) | 1,189 (24.0%) | 318 (21.0%) | 261 (28.0%) | ||||
| Weekday (MondayFriday) | 861 (77.3%) | 3,764 (76.0%) | 1,194 (79.0%) | 670 (72.0%) | ||||
| Transfer from another institution | 89 (8.0%) | 1,193 (24.1%) | 61 (4.0%) | 75 (8.1%) | ||||
| Top diagnosis codes | ||||||||
| ICD‐9 #1 | 415: Acute pulmonary heart disease | 57 (5.1%) | 038: Septicemia | 423 (8.5%) | 786: Symptoms involving respiratory/other chest | 315 (20.8%) | 780: General symptoms | 99 (10.6%) |
| ICD‐9 #2 | 276: Disorders of fluid/electrolyte, acid/base | 51 (4.6%) | 486: Pneumonia | 206 (4.2%) | 780: General symptoms | 138 (9.1%) | 786: Symptoms involving respiratory/other chest | 51 (5.5%) |
| ICD‐9 #3 | 682: Other cellulitis and abscess | 47 (4.2%) | 584: Acute kidney failure | 181 (3.7%) | 789: Other symptoms involving abdomen/pelvis | 47 (3.1%) | 789: Other symptoms involving abdomen/pelvis | 37 (4.0%) |
| ICD‐9 #4 | 427: Cardiac dysrhythmias | 43 (3.9%) | 577: Diseases of the pancreas | 181 (3.7%) | 787: Symptoms involving digestive system | 35 (2.3%) | 599: Other disorders of urethra/urinary tract | 30 (3.2%) |
| ICD‐9 #5 | 250: Diabetes mellitus | 40 (3.6%) | 682: Other cellulitis and abscess | 175 (3.5%) | 305: Nondependent abuse of drugs | 32 (2.1%) | 787: Symptoms involving digestive system | 28 (3.0%) |
Including all observation encounters across LOS, 4 of the 5 top ICD‐9 codes were the same for stays <2 midnights and 2 midnights. The same was true for short‐ and long‐stay general medicine observation encounters (Table 3).
For all observation encounters, 26.5% (348/1315) of 2‐midnight encounters started on a weekend compared to 22.6% (781/3454) of <2‐midnight encounters. For adult medicine observation, 28.0% (261/931) of 2‐midnight encounters started on a weekend compared to 21.0% (318/1512) of <2‐midnight encounters (Table 3).
Percentage of Observation Encounters Reaching 2 Midnights Based on Time of Hospitalization
Observation encounters starting before 8:00 am spanned 2 midnights 13.6% of the time, and those encounters starting after 4:00 pm crossed 2 midnights 31.2% of the time. Two of the 3 top ICD‐9 codes were the same across LOS, with similar findings for the adult general medicine‐only group (Figure 1).
DISCUSSION
Although CMS predicts that more patients will be classified as inpatients under the new rule, we determined the opposite, consistent with a recent report generated by the Office of the Inspector General (OIG) for 2012 Medicare beneficiaries.[8] Our results did not change when we excluded all surgical encounters to account for possible exclusions based on the surgical inpatient‐only list. Although a small percentage of Medicare adult general medicine patients may be reclassified as inpatients under the new rules, the net effect would be that many more hospital encounters will be billed under observation rather than inpatient status. These findings assume overall length of stay will remain unchanged under these rules, an assumption that may not hold true given the financial losses we predicted hospitals may face under this rule,[12] and potential pressures on individual physicians providing patient care.
Medicare has prioritized auditing <2‐midnight inpatient encounters under the assumption that many short inpatient encounters are actually misclassified observation encounters,[4, 8, 9] prompting us to investigate whether this was the case in our patient population. Although it did not use ICD‐9 diagnosis codes, the OIG report suggested that short‐stay inpatients and observation patients may be clinically similar.[8, 13] Using ICD‐9 codes, we found no overlap between the top ICD‐9 codes for adult general medicine <2‐midnight inpatient and observation encounters, and only 1 of 5 shared codes for these encounters across all service lines. These findings are counter to the OIG report, and suggest that <2‐midnight inpatients are different from observation patients at our institution, and that <2‐midnight inpatients should not be arbitrarily reclassified as observation based solely upon LOS.
We also found that the majority of top ICD‐9 codes within observation were the same regardless of LOS, suggesting that LOS does not reliably differentiate clinically different observation populations that merit different insurance coverage (Medicare Part A for 2‐midnight encounters, Medicare Part B for <2‐midnight encounters). This lack of a clear cut point may drive an overall increase in LOS to achieve 2 midnights, as common diagnosis codes can be justified for both <2‐midnight or 2‐midnight observation stays.
Finally, we found that external factors, such as the time of day and specific day (weekday vs weekend) of hospitalization, impact the likelihood of achieving a 2‐midnight stay. Patients hospitalized earlier in the day were less likely to span 2 midnights compared to later‐day encounters, suggesting that use of a full working day as the day of presentation is harmful to a patient's chance of gaining inpatient status. Observation hospitalizations starting on a weekend day were more likely to achieve 2 midnights, which likely reflects different resource allocation and hospital efficiency on weekends, yet it is unlikely that weekend midnights, if associated with any delay in care, will be counted toward a patient's cumulative 2‐midnight total. The CMS has further indicated that midnights accrued prior to transfer from 1 hospital to another will not count toward a cumulative 2‐midnight stay. Although it would seem likely that patients requiring transfer to a tertiary care center would meet inpatient criteria, 9% of our observation encounters were transferred from other acute care hospitals, and many will have lost attributable midnights accrued prior to transfer to our hospital. Taken together, our findings strongly suggest that issues entirely unrelated to diagnosis or clinical status will impact whether hospitalized patients will be classified as inpatient or observation under the new rule.
This study has several limitations. Our data were limited to a single Midwestern tertiary care academic medical center, and may not be applicable to other healthcare settings. Second, 1.5% (466) of our inpatient stays and 56 (1.2%) of our observation encounters lacked a referral source in our administrative database, although these deficiencies would not likely change the conclusions. Finally, the total number of observation encounters starting before 8:00 am and staying 2 midnights was small and therefore potentially subject to confounding. However, despite the fact that encounters beginning in the early morning hours may be different in ways unable to be measured in this study, encounter ICD‐9 codes were similar regardless of time of day.
Despite these limitations, our study raises concerns about the impact of CMS's new time‐driven observation rules on hospital practice patterns. We found distinctly different <2‐midnight inpatient ICD‐9 codes as compared to those for observation encounters. Reclassifying <2‐midnight inpatients as observation may inappropriately shift the financial burden of acute hospitalizations to patients who were previously eligible to receive Medicare inpatient benefits. We also demonstrated a decrease in billable inpatient encounters under the new rules, which may be countered by changes in hospital and provider practice to drive more admissions over the 2‐midnight threshold to avoid financial losses. These changes should be defensible under audit given the ambiguities of the rule we found in this study surrounding time of day of admission, weekend and transfer hospitalizations, and the fact that common observation ICD‐9 codes are similar across LOS. Ironically, the unintended consequence of the new rule may be to drive up hospital LOS, reduce efficiency, and increase the overall cost of care.
Our findings suggest that CMS should define observation care per its original intent: as a means to determine if a patient can safely return home after a short period of additional care.[6] Patients whose conditions necessitate an intensity and level of service beyond this narrow scope should be classified as full inpatients irrespective of LOS, whether that LOS is <2 midnights or 2 midnights. Policies that fail to reflect the original intent of observation status are unlikely to achieve the intended outcome of defining 2 distinct patient populations that merit different services and reimbursement.
Acknowledgements
The authors thank Andrew LaRocque and Dan Dexter for their assistance with the data. Without their help, this article would not have been possible.
Disclosures: Dr. Graf reports receiving royalties from Smith & Nephew for patents he has assigned to them involving orthopedic implants. This is unrelated to the topic or content of this manuscript. The authors report no other conflicts of interest.
Editor's Note: On February 24, 2014, after this manuscript was published, CMS issued a rules clarification allowing midnights spent at a referral hospital prior to transfer to be counted in the cumulative 2 midnight tally to determine inpatient status.
Observation hospitalization is a growing phenomenon in the United States healthcare system.[1] For Medicare beneficiaries, observation encounters increased 33.6% from 2004 to 2011, with inpatient encounters decreasing by 7.8% over the same period.[2]
Observation length of stay has also increased. Medicare states that observation care should typically last <24 hours, and in only rare and exceptional cases exceed 48 hours. We and others have showed that observation stays, on average, do not meet this definition.[1, 3] At our institution, historically less than half of observation encounters discharge in under 24 hours, and 1 in 6 stay longer than 48 hours.[3]
The Centers for Medicare and Medicaid Services (CMS) issued a rules change effective October 1, 2013, in response to concern about recent increases in the length of time that CMS beneficiaries spend as hospital outpatients receiving observation services.[4] These rules shifted observation determination from clinical criteria, such as InterQual,[5] to a time‐based rule that hinges on a 2‐midnight cut point. Patients staying <2 midnights, with few exceptions, are now observation, and those staying 2 midnights are inpatients. This is important, as patients hospitalized as observation are technically outpatients, not covered by Medicare Part A hospital insurance, and ineligible for skilled nursing facility benefits.[3, 6]
Although challenges with observation status in general are well described,[1, 3, 7] the potential impact of the 2‐midnight rule is not fully known. The purpose of our descriptive study was to examine how the new rules, retrospectively applied to recent encounters, would affect our hospital encounters, with a separate analysis of Medicare encounters and adult general medicine encounters. First, as CMS predicted a net shift from outpatient to inpatient stays[8] under the new rule, we attempted to determine whether this rule would actually reduce observation encounter frequency. Second, as CMS has cited persistently large improper payment rates in short‐stay hospital inpatient claims[4] and intends to audit <2‐midnight inpatient encounters under the assumption that many are misclassified observation stays,[4, 8, 9] we sought to determine if short‐stay inpatient and observation encounters were truly the same. Third, as insurance coverage will change based on the 2‐midnight cut point, we sought to determine whether 2 midnights separated distinct clinical populations within observation status, making the rule logical and fair. Finally, we sought to determine whether external factors, such as time of admission, day of week of admission, and transfer to our institution would impact how patients may be classified under the new rule.
METHODS
Study Population
Our methods have been described previously[3] with the exception of the updated dates of inclusion. Briefly, we analyzed all observation and inpatient encounters at University of Wisconsin Hospital and Clinics (UWHC) and the adjacent American Family Children's Hospital, a tertiary care referral academic medical center in Madison, Wisconsin,[10] with start date between January 1, 2012 and February 28, 2013. Six encounters with length of stay (LOS) >6 months were censored as they were not discharged by the time of data abstraction, and 3 encounters were removed due to erroneous encounter discharge dates. Patients with all insurance types were included in anticipation that commercial payors will follow Medicare rules changes. The University of Wisconsin (UW) Health Sciences Institutional Review Board approved the study.
Data Sources
Data were abstracted from the UW Health Sciences electronic medical record and ancillary data systems by the UWHC Business Planning and Analysis Department. Variables included demographics (age, sex, ethnicity), insurance type, and characteristics of hospitalization (admission service, day of week encounter began, acute/unscheduled presentation, International Classification of Diseases, 9th Revision [ICD‐9] codes, LOS, transfer from other hospital). We considered inpatient admission start time to be departure from the emergency department (ED) or arrival at our hospital if the encounter was a transfer from another facility. Observation start time also hinged on arrival at our hospital if the encounter was transferred from another facility, but for observation encounters arriving from the ED, the ED rooming time was used as the encounter start based on conservative interpretation of CMS rules for observation start time under the 2‐midnight rule.[11] Discharge time for all encounters was considered physical discharge from the ward. Observation status decisions were made by the admitting physician, with as‐needed guidance by case management staff and utilization review physicians using InterQual Criteria (McKesson Corp, San Francisco, CA),[5] a reference historically used by CMS auditors to determine status.
Evaluation of the 2‐Midnight Rule
All encounters were stratified based on a stay of <2 midnights or 2 midnights. Because general medicine patients comprise the bulk of observation patients,[3] the subset of encounters occurring on the hospital's 4 hospitalist medicine services, 3 general medicine resident services, and 1 adult nonobstetrics family medicine service, collectively termed adult general medicine, were also evaluated separately. Medicare encounters were also evaluated separately.
We first specifically compared <2‐midnight inpatient encounters and 2‐midnight observation encounters during the study period to determine the net number of encounters that would lose inpatient status (<2‐midnight inpatient encounters) and that would gain inpatient status (2‐midnight observation encounters) under the new rules. Subtracting the absolute number of <2‐midnight inpatient encounters from the 2‐midnight observation encounters results in the net loss or gain of inpatient encounters, assuming LOS does not change. Second, we compared ICD‐9 codes between <2‐midnight inpatient encounters and observation encounters to determine if these 2 groups were clinically distinguishable. Third, we compared diagnosis codes between observation encounters lasting <2 midnights and 2 midnights to establish whether the 2‐midnight cut point defines distinct patient groups within observation. Finally, we evaluated all observation encounters to determine whether the time of admission, the day of admission (weekday vs weekend), or whether the encounter had been transferred from another facility impacted encounter categorization under the new rules.
Statistical Methods
Descriptive statistics were used in this study, with data largely summarized as number and percent. When appropriate, mean and standard deviation were used to describe central tendency and dispersion.
RESULTS
Characteristics of Inpatient and Observation Encounters
Of the 36,193 total hospital encounters during the study period, 4769 (13.2%) were classified as observation encounters. Of 8510 adult general medicine encounters, 2443 (28.7%) were observation. Adult general medicine observation encounters accounted for 51.2% of all observation encounters for the hospital. A total of 9.0% of our observation encounters were transferred from another institution (Table 1).
| Inpatient, n=31,424 (86.8%) | Observation, n=4,769 (13.2%) | |
|---|---|---|
| ||
| Demographics | ||
| Female | 15,083 (48.0%) | 2,321 (48.7%) |
| Age, y, mean (SD) | 49.2 (23.6) | 49.4 (25.4) |
| Has primary care provider | 27,378 (87.1%) | 4,152 (87.1%) |
| Ethnicity | ||
| Caucasian | 27,145 (86.4%) | 3,880 (81.4%) |
| Non‐Caucasian | 3,478 (11.1%) | 739 (15.5%) |
| Unknown | 801 (2.5%) | 150 (3.1%) |
| Characteristics of hospitalization | ||
| Day of admission | ||
| Weekend (SaturdaySunday) | 5,058 (16.1%) | 1,129 (23.7%) |
| Weekday (MondayFriday) | 26,360 (83.9%) | 3,640 (76.3%) |
| Transfer from other institution | 6,191 (19.7%) | 427 (9.0%) |
| Acute/unscheduled | 21,150 (67.3%) | 4,479 (93.9%) |
| Service of admission | ||
| Adult general medicine | 6,067 (19.3%) | 2,443 (51.2%) |
| Adult surgery | 13,625 (43.4%) | 856 (17.9%) |
| Adult subspecialty nonsurgery | 7,432 (23.7%) | 802 (16.8%) |
| Pediatrics | 4,300 (13.7%) | 668 (14.0%) |
| Insurance | ||
| Medicare | 11,719 (37.3%) | 1,846 (38.7%) |
| Medicaid | 3,642 (11.6%) | 658 (13.8%) |
| Commercial | 13,321 (42.4%) | 1,817 (38.1%) |
| Other | 1,665 (5.3%) | 184 (3.9%) |
| None | 1,077 (3.4%) | 264 (5.5%) |
A total of 1442 (4.0%) encounters changed status during the study period, with 606 (42.0%) having changed from inpatient to observation and considered observation, and 836 (58.0%) having changed from observation to inpatient and considered inpatient.
Impact of the 2‐Midnight Rule on Number of Observation and Inpatient Encounters
Among all encounters, the 2‐midnight rule would result in a net transition of 14.9% of inpatient encounters to observation. Considering only Medicare encounters, the net transition would be 7.4% inpatient encounters to observation. Within adult general medicine patients, the parallel changes would be 2.2% (all insurance types) and a gain of 2.4% (Medicare only) (Table 2).
| Inpatient, n=31,424 (86.8%) | Observation, n=4,769 (13.2%) | |
|---|---|---|
| ||
| All encounters, n=36,193 | ||
| <2 Midnights | 6,723* (21.4%) | 3,454 (72.4%) |
| 2 Midnights | 24,701 (78.6%) | 1,315* (27.6%) |
| Net change inpatient encounters | 5,408 (14.9%) | |
| Medicare encounters, n=13,565 | ||
| <2 Midnights | 1,728* (14.7%) | 1,127 (61.1%) |
| 2 Midnights | 9,991 (85.3%) | 719* (38.9%) |
| Net change inpatient encounters | 1,009 (7.4%) | |
| All general medicine, n=8,510 | ||
| <2 Midnights | 1,114* (18.4%) | 1,512 (61.9%) |
| 2 Midnights | 4,953 (81.6%) | 931* (38.1%) |
| Net change inpatient encounters | 183 (2.2%) | |
| Medicare general medicine, n=4,571 | ||
| <2 Midnights | 472* (14.3%) | 690 (54.2%) |
| 2 Midnights | 2,827 (85.7%) | 582* (45.8%) |
| Net change inpatient encounters | 110 (2.4%) | |
Encounters including surgical procedures on the so‐called inpatient‐only list will remain inpatient regardless of LOS. As we could not identify such encounters, we tested removal of all surgical stays under the overly conservative assumption that all short stay surgical patients would remain inpatient. Of 21,712 nonsurgical encounters that remained, there were 4074 <2‐midnight inpatient encounters and 1146 2‐midnight observation encounters, yielding a net transition of 2928 (13.5%) inpatient encounters to observation encounters. Medicare encounters accounted for 8240 of these 21,712 (38.0%) nonsurgical encounters, with 1105 <2‐midnight inpatient encounters and 653 2‐midnight observation encounters, yielding a net reclassification of 452 (5.5%) Medicare nonsurgical inpatient encounters to observation encounters.
Length of Stay and Diagnoses After Application of the 2‐Midnight Rule to Inpatient and Observation Encounters
Only 1 of the top 5 ICD‐9 codes (code 427: cardiac dysrhythmias) was shared between the 2‐midnight inpatient encounters and any observation encounter group. When the same criteria were applied to adult general medicine encounters, none of the top 5 ICD‐9 codes were shared (Table 3).
| All Encounters, n=36,193 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Inpatient Stays Shorter Than 2 Midnights, n=6,723 (21.4%) | Inpatient Stays 2 Midnights, n=24,701 (78.6%) | Observation Stays Shorter Than 2 Midnights, n=3,454 (72.4%) | Observation Stays 2 Midnights n=1,315 (27.6%) | |||||
| ||||||||
| Day of admission | ||||||||
| Weekend (Saturday Sunday) | 1,026 (15.3%) | 4,032 (16.3%) | 781 (22.6%) | 348 (26.5%) | ||||
| Weekday (MondayFriday) | 5,697 (84.7%) | 20,669 (83.7%) | 2,673 (77.4%) | 967 (73.5%) | ||||
| Transfer from another institution | 986 (14.7%) | 5,205 (21.1%) | 297 (8.6%) | 130 (9.9%) | ||||
| Top diagnosis codes | ||||||||
| ICD‐9 #1 | 996: Complications peculiar to specific procedure | 200 (3.0%) | 996: Complications peculiar to specific procedure | 1,355 (5.5%) | 786: Symptoms involving respiratory/other chest | 531 (15.4%) | 780: General symptoms | 124 (9.4%) |
| ICD‐9 #2 | 427: Cardiac dysrhythmias | 195 (2.9%) | 715: Osteoarthrosis and allied disorders | 917 (3.7%) | 780: General symptoms | 235 (6.8%) | 786: Symptoms involving respiratory/other chest | 80 (6.1%) |
| ICD‐9 #3 | 722: Intervertebral disk disorder | 182 (2.7%) | 038: Septicemia | 689 (2.8%) | 427: Cardiac dysrhythmias | 103 (3.0%) | 789: Other symptoms involving abdomen/pelvis | 48 (3.7%) |
| ICD‐9 #4 | 540: Acute appendicitis | 179 (2.7%) | 296: Episodic mood disorder | 619 (2.5%) | 789: Other symptoms involving abdomen/pelvis | 89 (2.6%) | 787: Symptoms involving digestive system | 38 (2.9%) |
| ICD‐9 #5 | V58: Encounter for other and unspecified procedures | 176 (2.6%) | 998: Other complications of procedures not elsewhere classified | 516 (2.1%) | 787: Symptoms involving digestive system | 56 (1.6%) | 599: Other disorders of urethra/urinary tract | 35 (2.7%) |
| Adult General Medicine Encounters, n=8,510 | ||||||||
| Inpatient Stays Shorter Than 2 Midnights, n=1,114 (18.4%) | Inpatient Stays 2 Midnights, n=4,953 (81.6%) | Observation Stays Shorter Than 2 Midnights, n=1,512 (61.9%) | Observation Stays 2 Midnights, n=931 (38.1%) | |||||
| Day of admission | ||||||||
| Weekend (Saturday Sunday) | 253 (22.7%) | 1,189 (24.0%) | 318 (21.0%) | 261 (28.0%) | ||||
| Weekday (MondayFriday) | 861 (77.3%) | 3,764 (76.0%) | 1,194 (79.0%) | 670 (72.0%) | ||||
| Transfer from another institution | 89 (8.0%) | 1,193 (24.1%) | 61 (4.0%) | 75 (8.1%) | ||||
| Top diagnosis codes | ||||||||
| ICD‐9 #1 | 415: Acute pulmonary heart disease | 57 (5.1%) | 038: Septicemia | 423 (8.5%) | 786: Symptoms involving respiratory/other chest | 315 (20.8%) | 780: General symptoms | 99 (10.6%) |
| ICD‐9 #2 | 276: Disorders of fluid/electrolyte, acid/base | 51 (4.6%) | 486: Pneumonia | 206 (4.2%) | 780: General symptoms | 138 (9.1%) | 786: Symptoms involving respiratory/other chest | 51 (5.5%) |
| ICD‐9 #3 | 682: Other cellulitis and abscess | 47 (4.2%) | 584: Acute kidney failure | 181 (3.7%) | 789: Other symptoms involving abdomen/pelvis | 47 (3.1%) | 789: Other symptoms involving abdomen/pelvis | 37 (4.0%) |
| ICD‐9 #4 | 427: Cardiac dysrhythmias | 43 (3.9%) | 577: Diseases of the pancreas | 181 (3.7%) | 787: Symptoms involving digestive system | 35 (2.3%) | 599: Other disorders of urethra/urinary tract | 30 (3.2%) |
| ICD‐9 #5 | 250: Diabetes mellitus | 40 (3.6%) | 682: Other cellulitis and abscess | 175 (3.5%) | 305: Nondependent abuse of drugs | 32 (2.1%) | 787: Symptoms involving digestive system | 28 (3.0%) |
Including all observation encounters across LOS, 4 of the 5 top ICD‐9 codes were the same for stays <2 midnights and 2 midnights. The same was true for short‐ and long‐stay general medicine observation encounters (Table 3).
For all observation encounters, 26.5% (348/1315) of 2‐midnight encounters started on a weekend compared to 22.6% (781/3454) of <2‐midnight encounters. For adult medicine observation, 28.0% (261/931) of 2‐midnight encounters started on a weekend compared to 21.0% (318/1512) of <2‐midnight encounters (Table 3).
Percentage of Observation Encounters Reaching 2 Midnights Based on Time of Hospitalization
Observation encounters starting before 8:00 am spanned 2 midnights 13.6% of the time, and those encounters starting after 4:00 pm crossed 2 midnights 31.2% of the time. Two of the 3 top ICD‐9 codes were the same across LOS, with similar findings for the adult general medicine‐only group (Figure 1).
DISCUSSION
Although CMS predicts that more patients will be classified as inpatients under the new rule, we determined the opposite, consistent with a recent report generated by the Office of the Inspector General (OIG) for 2012 Medicare beneficiaries.[8] Our results did not change when we excluded all surgical encounters to account for possible exclusions based on the surgical inpatient‐only list. Although a small percentage of Medicare adult general medicine patients may be reclassified as inpatients under the new rules, the net effect would be that many more hospital encounters will be billed under observation rather than inpatient status. These findings assume overall length of stay will remain unchanged under these rules, an assumption that may not hold true given the financial losses we predicted hospitals may face under this rule,[12] and potential pressures on individual physicians providing patient care.
Medicare has prioritized auditing <2‐midnight inpatient encounters under the assumption that many short inpatient encounters are actually misclassified observation encounters,[4, 8, 9] prompting us to investigate whether this was the case in our patient population. Although it did not use ICD‐9 diagnosis codes, the OIG report suggested that short‐stay inpatients and observation patients may be clinically similar.[8, 13] Using ICD‐9 codes, we found no overlap between the top ICD‐9 codes for adult general medicine <2‐midnight inpatient and observation encounters, and only 1 of 5 shared codes for these encounters across all service lines. These findings are counter to the OIG report, and suggest that <2‐midnight inpatients are different from observation patients at our institution, and that <2‐midnight inpatients should not be arbitrarily reclassified as observation based solely upon LOS.
We also found that the majority of top ICD‐9 codes within observation were the same regardless of LOS, suggesting that LOS does not reliably differentiate clinically different observation populations that merit different insurance coverage (Medicare Part A for 2‐midnight encounters, Medicare Part B for <2‐midnight encounters). This lack of a clear cut point may drive an overall increase in LOS to achieve 2 midnights, as common diagnosis codes can be justified for both <2‐midnight or 2‐midnight observation stays.
Finally, we found that external factors, such as the time of day and specific day (weekday vs weekend) of hospitalization, impact the likelihood of achieving a 2‐midnight stay. Patients hospitalized earlier in the day were less likely to span 2 midnights compared to later‐day encounters, suggesting that use of a full working day as the day of presentation is harmful to a patient's chance of gaining inpatient status. Observation hospitalizations starting on a weekend day were more likely to achieve 2 midnights, which likely reflects different resource allocation and hospital efficiency on weekends, yet it is unlikely that weekend midnights, if associated with any delay in care, will be counted toward a patient's cumulative 2‐midnight total. The CMS has further indicated that midnights accrued prior to transfer from 1 hospital to another will not count toward a cumulative 2‐midnight stay. Although it would seem likely that patients requiring transfer to a tertiary care center would meet inpatient criteria, 9% of our observation encounters were transferred from other acute care hospitals, and many will have lost attributable midnights accrued prior to transfer to our hospital. Taken together, our findings strongly suggest that issues entirely unrelated to diagnosis or clinical status will impact whether hospitalized patients will be classified as inpatient or observation under the new rule.
This study has several limitations. Our data were limited to a single Midwestern tertiary care academic medical center, and may not be applicable to other healthcare settings. Second, 1.5% (466) of our inpatient stays and 56 (1.2%) of our observation encounters lacked a referral source in our administrative database, although these deficiencies would not likely change the conclusions. Finally, the total number of observation encounters starting before 8:00 am and staying 2 midnights was small and therefore potentially subject to confounding. However, despite the fact that encounters beginning in the early morning hours may be different in ways unable to be measured in this study, encounter ICD‐9 codes were similar regardless of time of day.
Despite these limitations, our study raises concerns about the impact of CMS's new time‐driven observation rules on hospital practice patterns. We found distinctly different <2‐midnight inpatient ICD‐9 codes as compared to those for observation encounters. Reclassifying <2‐midnight inpatients as observation may inappropriately shift the financial burden of acute hospitalizations to patients who were previously eligible to receive Medicare inpatient benefits. We also demonstrated a decrease in billable inpatient encounters under the new rules, which may be countered by changes in hospital and provider practice to drive more admissions over the 2‐midnight threshold to avoid financial losses. These changes should be defensible under audit given the ambiguities of the rule we found in this study surrounding time of day of admission, weekend and transfer hospitalizations, and the fact that common observation ICD‐9 codes are similar across LOS. Ironically, the unintended consequence of the new rule may be to drive up hospital LOS, reduce efficiency, and increase the overall cost of care.
Our findings suggest that CMS should define observation care per its original intent: as a means to determine if a patient can safely return home after a short period of additional care.[6] Patients whose conditions necessitate an intensity and level of service beyond this narrow scope should be classified as full inpatients irrespective of LOS, whether that LOS is <2 midnights or 2 midnights. Policies that fail to reflect the original intent of observation status are unlikely to achieve the intended outcome of defining 2 distinct patient populations that merit different services and reimbursement.
Acknowledgements
The authors thank Andrew LaRocque and Dan Dexter for their assistance with the data. Without their help, this article would not have been possible.
Disclosures: Dr. Graf reports receiving royalties from Smith & Nephew for patents he has assigned to them involving orthopedic implants. This is unrelated to the topic or content of this manuscript. The authors report no other conflicts of interest.
Editor's Note: On February 24, 2014, after this manuscript was published, CMS issued a rules clarification allowing midnights spent at a referral hospital prior to transfer to be counted in the cumulative 2 midnight tally to determine inpatient status.
- , , . Sharp rise in Medicare enrollees being held hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251–1259.
- MedPAC report to Congress: hospital inpatient and outpatient services. Available at: http://www.medpac.gov/chapters/Mar13_Ch03.pdf. Accessed September 29, 2013.
- , , , et al. Hospitalized but not admitted: characteristics of patients with “Observation Status” at an academic medical center. JAMA Intern Med. 2013;173(21):1991–1998.
- Centers for Medicare and Medicaid Services inpatient prospective payment system 1599‐F. Fiscal year 2014 final rule. Available at: http://www.gpo.gov/fdsys/pkg/FR‐2013‐08‐19/pdf/2013–18956.pdf. Accessed December 22, 2013.
- McKesson Interqual. Available at: http://www.mckesson.com/en_us/McKesson.com/Payers/Decision%2BManagement/InterQual%2BEvidence‐Based%2BClinical%2BContent/InterQual%2BEvidence‐Based%2BClinical%2BContent.html. Accessed October 3, 2013.
- Medicare benefit policy manual. Chapter 6. Hospital services covered under Part B. Available at: https://www.cms.gov/transmittals/downloads/R42BP.pdf. Accessed December 22, 2013.
- . Thinking of admitting this patient? Think again: how observation care is complicating life for you (and your patients). Today's Hospitalist. Available at: http://www.todayshospitalist.com/index.php?b=articles_read173(21):2004–2006.
- Kaiser Health News. HHS Inspector General scrutinizes Medicare observation care policy. Available at: http://www.kaiserhealthnews.org/stories/2013/july/30/ig‐report‐observation‐care.aspx. Accessed October 3, 2013.
- , , . Sharp rise in Medicare enrollees being held hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood). 2012;31(6):1251–1259.
- MedPAC report to Congress: hospital inpatient and outpatient services. Available at: http://www.medpac.gov/chapters/Mar13_Ch03.pdf. Accessed September 29, 2013.
- , , , et al. Hospitalized but not admitted: characteristics of patients with “Observation Status” at an academic medical center. JAMA Intern Med. 2013;173(21):1991–1998.
- Centers for Medicare and Medicaid Services inpatient prospective payment system 1599‐F. Fiscal year 2014 final rule. Available at: http://www.gpo.gov/fdsys/pkg/FR‐2013‐08‐19/pdf/2013–18956.pdf. Accessed December 22, 2013.
- McKesson Interqual. Available at: http://www.mckesson.com/en_us/McKesson.com/Payers/Decision%2BManagement/InterQual%2BEvidence‐Based%2BClinical%2BContent/InterQual%2BEvidence‐Based%2BClinical%2BContent.html. Accessed October 3, 2013.
- Medicare benefit policy manual. Chapter 6. Hospital services covered under Part B. Available at: https://www.cms.gov/transmittals/downloads/R42BP.pdf. Accessed December 22, 2013.
- . Thinking of admitting this patient? Think again: how observation care is complicating life for you (and your patients). Today's Hospitalist. Available at: http://www.todayshospitalist.com/index.php?b=articles_read173(21):2004–2006.
- Kaiser Health News. HHS Inspector General scrutinizes Medicare observation care policy. Available at: http://www.kaiserhealthnews.org/stories/2013/july/30/ig‐report‐observation‐care.aspx. Accessed October 3, 2013.
© 2014 Society of Hospital Medicine
Update from the Public Policy Committee
One of SHM’s missions is to advocate policies and positions that support hospital medicine, hospitalists, and our patients. SHM also engages broader issues impacting the delivery, quality, and safety of medical care and lobbies for policies that ensure public health and safety. Legislators, payers, and healthcare administrators use SHM’s policy statements to guide their understanding of and expectations for hospital medicine and its practitioners.
The Public Policy Committee (PPC) is SHM’s primary resource for researching and recommending policy and advocacy positions to the Board of Directors. We respond to issues raised by SHM members, federal and state healthcare legislation, and hospital and health plan policies that affect hospital medicine, hospitalists, and patients.
- In 1999, SHM stood firmly against health plans mandating PCP referral to hospitalists. Our stance defused concerns about hospital medicine raised by primary care physicians and helped to fuel the rapid growth of hospital medicine.
- In 2001, some hospitalists were having hospital privileges withheld because of their designation as hospitalists. The SHM condemned this practice and insisted that hospitalists should be subject to the same privileging and credentialing process as other physicians practicing inpatient medicine.
Recently, SHM members raised concerns over hospitals’ mandating that hospitalists maintain responsibility for patient follow-up after discharge. Based upon the PPC’s research and recommendation, the SHM Board approved a policy clarifying the role of the hospitalist in the continuum of care. (“The Hospitalist,” May/June 2005) This policy will clarify expectations for hospital medicine practices as they develop care management arrangements with hospitals, physicians, and payers.
Currently, the PPC is spearheading several initiatives:
- We are coordinating SHM’s participation in CMS’s 5-year review of valuation of E&M codes.
- In conjunction with a respected health policy analysis firm, we are developing a “hospital medicine White Paper,” which will serve as the definitive description of what hospital medicine is and document its potential to change health care. It will serve as our primary tool to communicate with legislators, policy makers, third-party payers, and healthcare leaders to further the mission and values of hospital medicine as a specialty.
- Finally, the PPC is leveraging our Washington, DC, venue for the 2006 Annual Meeting to organize a “hospital medicine Legislative Day.” At this event, hospitalists will visit legislators to discuss issues of importance to hospital medicine, such as patient safety and allocation of healthcare resources. We hope that this event will further raise awareness of hospital medicine and spur hospitalists to become politically active on behalf of our specialty.
Finally, on behalf of the members of the PPC, I want to thank Mary Jo Gorman for her 2-year stewardship of the Public Policy Committee. Her drive, vision, and enthusiasm were key to many of the successes described above.
More Information
- Visit www.hospitalmedicine.org > Click on “About SHM” > Click on “Committees > Scroll down to view “Public Policy Committee”
- Visit www.hospitalmedicine.org > Click on “Advocacy & Policy”
One of SHM’s missions is to advocate policies and positions that support hospital medicine, hospitalists, and our patients. SHM also engages broader issues impacting the delivery, quality, and safety of medical care and lobbies for policies that ensure public health and safety. Legislators, payers, and healthcare administrators use SHM’s policy statements to guide their understanding of and expectations for hospital medicine and its practitioners.
The Public Policy Committee (PPC) is SHM’s primary resource for researching and recommending policy and advocacy positions to the Board of Directors. We respond to issues raised by SHM members, federal and state healthcare legislation, and hospital and health plan policies that affect hospital medicine, hospitalists, and patients.
- In 1999, SHM stood firmly against health plans mandating PCP referral to hospitalists. Our stance defused concerns about hospital medicine raised by primary care physicians and helped to fuel the rapid growth of hospital medicine.
- In 2001, some hospitalists were having hospital privileges withheld because of their designation as hospitalists. The SHM condemned this practice and insisted that hospitalists should be subject to the same privileging and credentialing process as other physicians practicing inpatient medicine.
Recently, SHM members raised concerns over hospitals’ mandating that hospitalists maintain responsibility for patient follow-up after discharge. Based upon the PPC’s research and recommendation, the SHM Board approved a policy clarifying the role of the hospitalist in the continuum of care. (“The Hospitalist,” May/June 2005) This policy will clarify expectations for hospital medicine practices as they develop care management arrangements with hospitals, physicians, and payers.
Currently, the PPC is spearheading several initiatives:
- We are coordinating SHM’s participation in CMS’s 5-year review of valuation of E&M codes.
- In conjunction with a respected health policy analysis firm, we are developing a “hospital medicine White Paper,” which will serve as the definitive description of what hospital medicine is and document its potential to change health care. It will serve as our primary tool to communicate with legislators, policy makers, third-party payers, and healthcare leaders to further the mission and values of hospital medicine as a specialty.
- Finally, the PPC is leveraging our Washington, DC, venue for the 2006 Annual Meeting to organize a “hospital medicine Legislative Day.” At this event, hospitalists will visit legislators to discuss issues of importance to hospital medicine, such as patient safety and allocation of healthcare resources. We hope that this event will further raise awareness of hospital medicine and spur hospitalists to become politically active on behalf of our specialty.
Finally, on behalf of the members of the PPC, I want to thank Mary Jo Gorman for her 2-year stewardship of the Public Policy Committee. Her drive, vision, and enthusiasm were key to many of the successes described above.
More Information
- Visit www.hospitalmedicine.org > Click on “About SHM” > Click on “Committees > Scroll down to view “Public Policy Committee”
- Visit www.hospitalmedicine.org > Click on “Advocacy & Policy”
One of SHM’s missions is to advocate policies and positions that support hospital medicine, hospitalists, and our patients. SHM also engages broader issues impacting the delivery, quality, and safety of medical care and lobbies for policies that ensure public health and safety. Legislators, payers, and healthcare administrators use SHM’s policy statements to guide their understanding of and expectations for hospital medicine and its practitioners.
The Public Policy Committee (PPC) is SHM’s primary resource for researching and recommending policy and advocacy positions to the Board of Directors. We respond to issues raised by SHM members, federal and state healthcare legislation, and hospital and health plan policies that affect hospital medicine, hospitalists, and patients.
- In 1999, SHM stood firmly against health plans mandating PCP referral to hospitalists. Our stance defused concerns about hospital medicine raised by primary care physicians and helped to fuel the rapid growth of hospital medicine.
- In 2001, some hospitalists were having hospital privileges withheld because of their designation as hospitalists. The SHM condemned this practice and insisted that hospitalists should be subject to the same privileging and credentialing process as other physicians practicing inpatient medicine.
Recently, SHM members raised concerns over hospitals’ mandating that hospitalists maintain responsibility for patient follow-up after discharge. Based upon the PPC’s research and recommendation, the SHM Board approved a policy clarifying the role of the hospitalist in the continuum of care. (“The Hospitalist,” May/June 2005) This policy will clarify expectations for hospital medicine practices as they develop care management arrangements with hospitals, physicians, and payers.
Currently, the PPC is spearheading several initiatives:
- We are coordinating SHM’s participation in CMS’s 5-year review of valuation of E&M codes.
- In conjunction with a respected health policy analysis firm, we are developing a “hospital medicine White Paper,” which will serve as the definitive description of what hospital medicine is and document its potential to change health care. It will serve as our primary tool to communicate with legislators, policy makers, third-party payers, and healthcare leaders to further the mission and values of hospital medicine as a specialty.
- Finally, the PPC is leveraging our Washington, DC, venue for the 2006 Annual Meeting to organize a “hospital medicine Legislative Day.” At this event, hospitalists will visit legislators to discuss issues of importance to hospital medicine, such as patient safety and allocation of healthcare resources. We hope that this event will further raise awareness of hospital medicine and spur hospitalists to become politically active on behalf of our specialty.
Finally, on behalf of the members of the PPC, I want to thank Mary Jo Gorman for her 2-year stewardship of the Public Policy Committee. Her drive, vision, and enthusiasm were key to many of the successes described above.
More Information
- Visit www.hospitalmedicine.org > Click on “About SHM” > Click on “Committees > Scroll down to view “Public Policy Committee”
- Visit www.hospitalmedicine.org > Click on “Advocacy & Policy”
Opportunity to Partner in Improving Care: The Medicare Chronic Care improvement Programs
The Medicare Modernization Act of 2003 (MMA) authorized development and testing of voluntary programs focused on improving the quality of care and quality of life for beneficiaries with multiple chronic illnesses. These Chronic Care Improvement Programs (CCIPs) represent the first large-scale chronic care improvement initiative under the Medicare fee-for-service (FFS) program. The programs also may represent an opportunity for SHM members to partner with the selected organizations.
CMS selected organizations that will offer self-care guidance and support to chronically ill beneficiaries. These organizations will help beneficiaries manage their health, adhere to their physicians’ plans of care, and assure that they seek or obtain medical care as needed to reduce their health risks. Chronic conditions are currently a leading cause of illness, disability, and death among beneficiaries and account for a disproportionate share of health care expenditures.
Each selected organization may design its own program, with the potential for a variety of unique models. Some vendors are partnering with physician groups and others may reach out to physicians in their regions. The selected regions and respective vendors are:
- Brooklyn and Queens in New York City (Visiting Nurse Service of New York in partnership with United-Healthcare Services, Inc.–Evercare)
- Chicago (Aetna Health Management)
- District of Columbia and Maryland (American Healthways, Inc.)
- Central Florida (Humana, Inc.)
- Georgia (CIGNA HealthCare)
- Mississippi (McKesson Health Solutions)
- Oklahoma (LifeMasters Supported SelfCare, Inc.)
- Pennsylvania (Health Dialog Services Corporation)
- Tennessee (XLHealth)
Performance-based contracting is one of the most important features of the CCIP design. The CCIPs will be paid based on achieving measurable improvements in clinical and financial outcomes, as well as satisfaction levels across their assigned populations. Payment is not based on services provided. CCIP organizations will be paid monthly fees, but those fees will be fully at risk. The organizations will be required to refund some or all of their fees to the federal government if they do not meet agreed-upon standards for quality improvement, savings to Medicare, and increased beneficiary satisfaction levels.
Phase I programs will collectively serve 150,000 to 300,000 chronically ill beneficiaries who are enrolled in traditional fee-for-service Medicare. This is the phase currentlyunder development, with the first programs expected to begin implementation in spring 2005. The programs are intended to help increase adherence to evidence-based care, reduce unnecessary hospital stays and emergency room visits, and help beneficiaries avoid costly and debilitating complications and comorbidities. With attention to reducing hospital costs, hospitalists may play an important role in CCIPs.
CCIPs include collaboration with participants’ providers to improve communication regarding relevant clinical information. The programs are being designed to assist beneficiaries in managing all of their health problems (not just a single disease). The programs to be tested vary in types of interventions to be used to improve outcomes. Across all programs, payments will be based on performance results.
Patient participation will be entirely voluntary. Eligible beneficiaries do not have to change plans or providers to participate, and there is no charge to the beneficiaries to participate. Once the program begins, beneficiaries may stop participating at any time. These programs may not restrict access to care. CMS will use historical claims data to identify beneficiaries by geographic area and screen them for eligibility. The selected beneficiaries will be assigned randomly to either an intervention group or a control group. Those in the intervention group will be notified of the opportunity to participate via a letter from the Medicare program. The letter will describe the CCIP and give the beneficiary the opportunity to decline to participate.
Phase II, which is the expansion of successful CCIPs, may begin within 2 to 31/2 years after Phase I. Entire CCIPs, or components of programs, may be expanded either regionally or nationally. SHM will continue to track the progress of the CCIPs and to encourage members to participate in the development and implementation of this exciting new chapter of Medicare services.
Please check the list above. If you are interested in partnering with any of the organizations, please email Lillian Higgins at lhiggins@hospitalistmedicine.org. She will provide you with contact information for the CCIP vendor.
The Medicare Modernization Act of 2003 (MMA) authorized development and testing of voluntary programs focused on improving the quality of care and quality of life for beneficiaries with multiple chronic illnesses. These Chronic Care Improvement Programs (CCIPs) represent the first large-scale chronic care improvement initiative under the Medicare fee-for-service (FFS) program. The programs also may represent an opportunity for SHM members to partner with the selected organizations.
CMS selected organizations that will offer self-care guidance and support to chronically ill beneficiaries. These organizations will help beneficiaries manage their health, adhere to their physicians’ plans of care, and assure that they seek or obtain medical care as needed to reduce their health risks. Chronic conditions are currently a leading cause of illness, disability, and death among beneficiaries and account for a disproportionate share of health care expenditures.
Each selected organization may design its own program, with the potential for a variety of unique models. Some vendors are partnering with physician groups and others may reach out to physicians in their regions. The selected regions and respective vendors are:
- Brooklyn and Queens in New York City (Visiting Nurse Service of New York in partnership with United-Healthcare Services, Inc.–Evercare)
- Chicago (Aetna Health Management)
- District of Columbia and Maryland (American Healthways, Inc.)
- Central Florida (Humana, Inc.)
- Georgia (CIGNA HealthCare)
- Mississippi (McKesson Health Solutions)
- Oklahoma (LifeMasters Supported SelfCare, Inc.)
- Pennsylvania (Health Dialog Services Corporation)
- Tennessee (XLHealth)
Performance-based contracting is one of the most important features of the CCIP design. The CCIPs will be paid based on achieving measurable improvements in clinical and financial outcomes, as well as satisfaction levels across their assigned populations. Payment is not based on services provided. CCIP organizations will be paid monthly fees, but those fees will be fully at risk. The organizations will be required to refund some or all of their fees to the federal government if they do not meet agreed-upon standards for quality improvement, savings to Medicare, and increased beneficiary satisfaction levels.
Phase I programs will collectively serve 150,000 to 300,000 chronically ill beneficiaries who are enrolled in traditional fee-for-service Medicare. This is the phase currentlyunder development, with the first programs expected to begin implementation in spring 2005. The programs are intended to help increase adherence to evidence-based care, reduce unnecessary hospital stays and emergency room visits, and help beneficiaries avoid costly and debilitating complications and comorbidities. With attention to reducing hospital costs, hospitalists may play an important role in CCIPs.
CCIPs include collaboration with participants’ providers to improve communication regarding relevant clinical information. The programs are being designed to assist beneficiaries in managing all of their health problems (not just a single disease). The programs to be tested vary in types of interventions to be used to improve outcomes. Across all programs, payments will be based on performance results.
Patient participation will be entirely voluntary. Eligible beneficiaries do not have to change plans or providers to participate, and there is no charge to the beneficiaries to participate. Once the program begins, beneficiaries may stop participating at any time. These programs may not restrict access to care. CMS will use historical claims data to identify beneficiaries by geographic area and screen them for eligibility. The selected beneficiaries will be assigned randomly to either an intervention group or a control group. Those in the intervention group will be notified of the opportunity to participate via a letter from the Medicare program. The letter will describe the CCIP and give the beneficiary the opportunity to decline to participate.
Phase II, which is the expansion of successful CCIPs, may begin within 2 to 31/2 years after Phase I. Entire CCIPs, or components of programs, may be expanded either regionally or nationally. SHM will continue to track the progress of the CCIPs and to encourage members to participate in the development and implementation of this exciting new chapter of Medicare services.
Please check the list above. If you are interested in partnering with any of the organizations, please email Lillian Higgins at lhiggins@hospitalistmedicine.org. She will provide you with contact information for the CCIP vendor.
The Medicare Modernization Act of 2003 (MMA) authorized development and testing of voluntary programs focused on improving the quality of care and quality of life for beneficiaries with multiple chronic illnesses. These Chronic Care Improvement Programs (CCIPs) represent the first large-scale chronic care improvement initiative under the Medicare fee-for-service (FFS) program. The programs also may represent an opportunity for SHM members to partner with the selected organizations.
CMS selected organizations that will offer self-care guidance and support to chronically ill beneficiaries. These organizations will help beneficiaries manage their health, adhere to their physicians’ plans of care, and assure that they seek or obtain medical care as needed to reduce their health risks. Chronic conditions are currently a leading cause of illness, disability, and death among beneficiaries and account for a disproportionate share of health care expenditures.
Each selected organization may design its own program, with the potential for a variety of unique models. Some vendors are partnering with physician groups and others may reach out to physicians in their regions. The selected regions and respective vendors are:
- Brooklyn and Queens in New York City (Visiting Nurse Service of New York in partnership with United-Healthcare Services, Inc.–Evercare)
- Chicago (Aetna Health Management)
- District of Columbia and Maryland (American Healthways, Inc.)
- Central Florida (Humana, Inc.)
- Georgia (CIGNA HealthCare)
- Mississippi (McKesson Health Solutions)
- Oklahoma (LifeMasters Supported SelfCare, Inc.)
- Pennsylvania (Health Dialog Services Corporation)
- Tennessee (XLHealth)
Performance-based contracting is one of the most important features of the CCIP design. The CCIPs will be paid based on achieving measurable improvements in clinical and financial outcomes, as well as satisfaction levels across their assigned populations. Payment is not based on services provided. CCIP organizations will be paid monthly fees, but those fees will be fully at risk. The organizations will be required to refund some or all of their fees to the federal government if they do not meet agreed-upon standards for quality improvement, savings to Medicare, and increased beneficiary satisfaction levels.
Phase I programs will collectively serve 150,000 to 300,000 chronically ill beneficiaries who are enrolled in traditional fee-for-service Medicare. This is the phase currentlyunder development, with the first programs expected to begin implementation in spring 2005. The programs are intended to help increase adherence to evidence-based care, reduce unnecessary hospital stays and emergency room visits, and help beneficiaries avoid costly and debilitating complications and comorbidities. With attention to reducing hospital costs, hospitalists may play an important role in CCIPs.
CCIPs include collaboration with participants’ providers to improve communication regarding relevant clinical information. The programs are being designed to assist beneficiaries in managing all of their health problems (not just a single disease). The programs to be tested vary in types of interventions to be used to improve outcomes. Across all programs, payments will be based on performance results.
Patient participation will be entirely voluntary. Eligible beneficiaries do not have to change plans or providers to participate, and there is no charge to the beneficiaries to participate. Once the program begins, beneficiaries may stop participating at any time. These programs may not restrict access to care. CMS will use historical claims data to identify beneficiaries by geographic area and screen them for eligibility. The selected beneficiaries will be assigned randomly to either an intervention group or a control group. Those in the intervention group will be notified of the opportunity to participate via a letter from the Medicare program. The letter will describe the CCIP and give the beneficiary the opportunity to decline to participate.
Phase II, which is the expansion of successful CCIPs, may begin within 2 to 31/2 years after Phase I. Entire CCIPs, or components of programs, may be expanded either regionally or nationally. SHM will continue to track the progress of the CCIPs and to encourage members to participate in the development and implementation of this exciting new chapter of Medicare services.
Please check the list above. If you are interested in partnering with any of the organizations, please email Lillian Higgins at lhiggins@hospitalistmedicine.org. She will provide you with contact information for the CCIP vendor.
Other Literature of Interest
1. Annane D, Bellissant E, Briegel J, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and metaanalysis. BMJ. 2004;329:480.
Severe sepsis is a common cause of ICU admissions and continues to have mortality rates as high as 30%. As research has evolved, the role of corticosteroids in sepsis has changed. Annane and colleagues systematically reviewed corticosteroid treatment for severe sepsis and septic shock. The authors found 15 randomized trials that evaluated their main outcome of all-cause mortality at 28 days. When these results were pooled there was no significant improvement in mortality (RR 0.98; 0.87 to 1.10). However, the analysis showed very significant heterogeneity, so the authors appropriately performed a sensitivity analysis based on an a priori hypothesis that low-dose, long-course steroids (≤ 300 mg hydrocortisone/day and ≥ 5 days) would provide greater benefit than short-course, high-dose corticosteroids. The sensitivity analysis of five studies with low-dose, long-course corticosteroids showed a clear reduction in 28-day mortality (RR 0.80; 0.67 to 0.95) with no heterogeneity. There was no statistically significant difference in GI bleeds, superinfections, and hyperglycemia.
This is a very well-done review, which included an exhaustive search for all available evidence. The authors conclude based on the findings of an individual study in the review that patients with septic shock should undergo adrenal insufficiency testing prior to starting empiric therapy with low-dose hydrocortisone (200-300 mg/day). Hydrocortisone should then be stopped if there is no evidence of adrenal insufficiency. However, none of the studies in this review were limited to patients with adrenal insufficiency. Also, although none of the studies individually showed a statistically significant improvement with corticosteroids, they all favored the steroid treatment group with RRs < 1. Although there is good evidence that septic shock patients with adrenal insufficiency should be treated with corticosteroids, it remains unclear if therapy should be generalized to all septic patients. The ongoing European CORTICUS trial should help answer some of these questions.
2. Baddour L.,Yu, V. and the International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Resp Crit Care Med; 2004;170:440-444.
Three retrospective studies indicate that patients with pneumococcal bacteremia are less likely to die if treated with combination antibiotics. The combination of a beta-lactam and a macrolide appear to be especially protective. Based upon this soft data, multiple societies now recommend combination antibiotic therapy with a beta-lactam and a macrolide as first-line therapy for hospitalized patients with CAP. This large, multi-center, prospective observational study analyzed outcomes for all patients with pneumococcal bacteremia. Critically ill patients were eight times more likely to die than non-critically ill patients (mortality: 54.6% vs. 7.3%, p=0.0001). Combination therapy was defined as any two or more antibiotics used concurrently: multiple different regimens were used. The 14-day mortality difference between pneumococcal bacteremic patients receiving monotherapy vs. those receiving combination therapy was not significant (10.4 vs. 11.5%, p-value not disclosed) However, in critically ill patients, combination antibiotic therapy was associated with a marked decrease in mortality (23.4 vs. 55.3%, p=0.0015).
This study has significant limitations. It is not randomized, combination therapy was broadly defined as any two or more antibiotics, and 16% of critically ill patients received only one antibiotic, a major deviation from the standard of care. Nonetheless, this is the first prospective trial that attempts to ascertain which patients with pneumococcal bacteremia benefit from combination therapy. The marked mortality reduction in critically ill patients who received combination therapy reinforces the current recommendation that septic patients with pneumococcal bacteremia should receive combination therapy. However, these findings also underscore the fact that current guidelines for the treatment of an exceedingly common and serious disease are based upon weak retrospective data. Further randomized prospective trials are needed to determine which patients with pneumococcal pneumonia may actually benefit from combination antimicrobial therapy and what combination is most efficacious.
3. Fernandez-Avilles F, Alsonso J, Castro-Beivas A, et al, on behalf of the GRACIA (Grupo de Analisis de la Cardiopatio Isquemica Aguda) Group. Routine invasive strategy within 24 hours of thrombolysis versus ischemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1). Lancet;2004;364:045-1053
In the last ACC/AHA guidelines for acute myocardial infarction (1999), angioplasty soon after thrombolysis is strongly discouraged (class III) because studies to date showed no significant difference in outcomes and propensity for adverse events, i.e. bleeding. However, as stated in these last recommendations, the benefits of early post-thrombolysis percutaneous transluminal coronary angioplasty (PTCA) with stenting should be reassessed as interventional strategies mature. In the current era of stents and newer antiplatelet therapies, it looks as if now is the time to take another look.
The GRACIA-1 was a randomized, multi-centered trial to assess early intervention following thrombolysis in ST-elevation myocardial infarction (STEMI). Five hundred patients were enrolled and randomized to receive either fibrin-specific thrombolytics alone in the conservative group or thrombolysis combined with early PTCA. The primary endpoint was a combined rate of death, non-fatal reinfarction, or ischemia-induced revascularization at 1 year. Pre-discharge PTCA and stenting in those demonstrating recurrent ischemia in the conservative group (n=52) was analyzed as a secondary endpoint. One-year follow-up was completed in 98% of patients. Both groups had similar major cardiac events at 30 days, with the one-year endpoint demonstrating no difference in mortality. Significant differences were seen in the primary endpoint at one year [23 (9%) in the invasive group vs. 51 (21%) in the conservative group (RR-0.44, 95% CI 0.28-0.70 p=0.00008)].
A major limitation of this study was the low-risk profile of its patients, and the fact that it was not powered to differentiate between mortality and reinfarction. It will be interesting to see if these results are replicated in future studies (CARESS-2005) and their clinical impact on the management of acute myocardial infarction in centers without interventional support.
4. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med.2004;19:732-739.
Falls in hospital patients are common and persistent problems in hospitals across the country, with significant impact on patient safety, morbidity, and health care cost. Previous studies have reported up to 30% of inpatient falls result in injury, with 4-6% resulting in serious injury. Most studies on falls are retrospective reviews. This paper detailed a prospective observational study designed to identify and analyze the patient characteristics or the circumstances that contribute to falls. Using an online adverse event reporting system, patient falls were identified. Once identified, additional data sources, including the patients’ medical records, electronic nursing records, and interviews with patient or family members and nurses, were used to collect information. A total of 183 patients fell during the study period, with 85% of the falls occurring in the patient’s room.
Half of the falls involved bowel or bladder elimination and were more likely to occur in patients over 65 years in age (adjusted odds ratio 2.4; 95% confidence interval 1.1 to 5.3). Most of the falls (59%) occurred during the evening/overnight. 58% of the patients who fell had received agents with central nervous system activity in the 24 hours prior to a fall. 12% of the patients who fell received sedative-hypnotics. Repeat fallers were more likely to be men than women (11/86 [13%] vs 4/97 [4%]; p=0.03). 42% of the falls resulted in some type of injury, ranging from pain/swelling (34%) to cardiac arrest/death (0.5%). In multivariate analysis, only elimination-related falls remained a significant predictor of being injured from a fall (aOR , 2.4; 95% CI 1.1 to 5.3). Interestingly, patients who were confused or disoriented were less likely to be injured than alert and oriented patients (crude OR, 0.5; 95% CI, 0.3 to 0.98). When examined by services, medicine and neurology had the highest fall rate at 6.12 falls per 1000 patient days and had the highest patient-to-nurse ratio of 6.5 and 5.3, respectively.
While specific independent risk factors for prevention of falls could not be determined in this study due to a lack of a control group, their findings are consistent with previously identified risk factors for falling, including weakness, poor cognitive status including medication-related changes, and altered elimination. Potential interventions to prevent falls include toileting schedules for high-risk elderly patients and review of medication lists to minimize centrally acting, psychotropic, or sedating agents.
5. Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med; 2004;164:2044-2050
Elderly patients are increasingly likely to require long-term anticoagulation. Despite this, physicians often withhold long-term anticoagulation due to perceived risk factors for bleeding, including age, comorbidity, and cognitive or functional impairment.
This combination retrospective and prospective observational study evaluated the safety and quality of anticoagulation in elderly patients. Over a three-year span, 323 elderly patients were discharged on warfarin from a large Israeli hospital. These patients were frail and potentially “at risk”; 54% were older than age 80, 81% were uneducated, and 84% had low income. 47% were considered cognitively intact (according to MMSE) and only 34% were functionally independent. Using a multivariate analysis, the authors determined that only poor quality of anticoagulation education (OR: 8.83; 95% CI: 2.0-50.2), polypharmacy (OR: 6.14; 95% CI 1.2-42.4) and INR >3 (OR: 1.08; 95% CI 1.03-1.14) were associated with major bleeding.
This study of a “real world” population of frail, at-risk elderly patients provides important insights into risks for major bleeding resulting from warfarin therapy. Surprisingly, advanced age, cognitive impairment and markers for frailty did not confer elevated risk for major bleeding. Importantly, the study did not explicitly address patient fall risk, an often-cited reason for withholding anticoagulation therapy. Supratherapeutic anticoagulation is associated with a statistically but not clinically significant bleeding risk. Polypharmacy is increasingly unavoidable in elderly patients. However, appropriate anticoagulation therapy should be the standard of care. This study makes it clear that we need to focus our efforts on ensuring that elderly patients and their caregivers receive appropriate anticoagulation education prior to discharge from the hospital.
6. Prinssen M, Verhoeven E, Buth J, et al. A Randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607-18.
Endovascular repair of abdominal aortic aneurysm, which involves percutaneous introduction of a graft to bridge an aortic aneurysm, has been available since the early 1990s. This procedure was initially used in patients who were felt to be at high risk for the traditional open procedure. This selection bias may have affected the outcome of earlier studies. Therefore, the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial was designed to assess outcomes in patients deemed fit to undergo either open or endovascular repair. The study was conducted at 24 centers in the Netherlands and four centers in Belgium. Three hundred and forty-five patients had abdominal aortic aneurysms of at least 5 cm and were considered eligible for either open or endovascular repair. Patients were then randomized to undergo one procedure or the other.
Surgeons experienced in both endovascular and open repair performed the procedures. Primary outcomes were 30-day mortality (defined as death during the primary hospital admission or within 30 days), severe complications, and the combination of the two. The operative mortality rate was 4.6% in the open-repair group and 1.2% in the endovascular repair group, with a risk ratio of 3.9 (95% CI, 0.9-32.9). The combined endpoint of mortality and severe complication was 9.8% in the open-repair group and 4.7% in the endovascular repair group, with a risk ratio of 2.1 (95% CI, 0.9 to 5.4). It should be noted that 90% of study patients were men. These findings indicate that endovascular repair of aortic aneurysm results in less short-term morbidity and mortality than open repair. Larger studies with longer follow up are indicated.
7. Spargias K, Alexopoulos E, Kyrzopoulos S. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation.110(18)2837-42
In this study, a team of Greek researchers studied the use of vitamin C in patients with renal insufficiency (creatinine >1.2) undergoing coronary catheterization or intervention to determine if it prevented contrast-mediated nephropathy (CMN). Although the etiology of CMN is unknown, ischemic insults to the renal medulla and free radical release have been implicated. Since vitamin C has been shown in animal studies to attenuate nephropathy when administered with known renal toxins, a similar effect was postulated when administered with IV contrast.
Two hundred and twenty patients electively admitted for coronary catheterization or intervention were randomized to placebo or to receive 3 grams of vitamin C 2 hours prior to the dye load followed by 2 gm that night and the morning after. The two groups were balanced for presence of hypertension, diabetes, tobacco use, and use of commonly prescribed medications. Intravenous hydration was given to all at variable rates depending on left ventricular ejection fraction. The catheterization team chose the type of contrast agent. Creatinine was measured at baseline (up to 3 months prior to dye load) and 2-5 days afterwards. CMN was defined as a rise in total serum creatinine by 0.5 mg/dL or by 25%. Using these criteria, 9% of the vitamin C group developed CMN as opposed to 20% in the controls (NNT 9; 95% CI: 5-53). Logistical regression was performed to account for differences in age, initial serum creatinine, or both, and always yielded significant differences. The treatment group was slightly older, had higher rates of isoosmolar contrast administration (reno-protective), and had slightly higher baseline creatinines, so the true protective effect was thought even higher than reported.
This study is limited by small sample size, an overwhelmingly male patient base (90%), and the suspected presence of atherosclerotic heart disease in all patients. The amount and rate of delivery of contrast was not noted. The vitamin C preparation used was not described, implying that all preparations were bioequivalent. No mention was made of whether these results could be extrapolated to other procedures involving contrast. Given the low cost and high tolerability of vitamin C, however, further studies would certainly be welcome.
8. Yadav J, Wholey M, Kuntz R, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. NEJM.2004;351:1493-1501.
Carotid angioplasty has been available for the past decade, but, due to possible complications such as plaque embolization and stent compression, the procedure had been limited to patients unsuitable for surgical endarterectomy. Recently, the introduction of crush-resistant nitinol stents and emboli protection devices has made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year.
1. Annane D, Bellissant E, Briegel J, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and metaanalysis. BMJ. 2004;329:480.
Severe sepsis is a common cause of ICU admissions and continues to have mortality rates as high as 30%. As research has evolved, the role of corticosteroids in sepsis has changed. Annane and colleagues systematically reviewed corticosteroid treatment for severe sepsis and septic shock. The authors found 15 randomized trials that evaluated their main outcome of all-cause mortality at 28 days. When these results were pooled there was no significant improvement in mortality (RR 0.98; 0.87 to 1.10). However, the analysis showed very significant heterogeneity, so the authors appropriately performed a sensitivity analysis based on an a priori hypothesis that low-dose, long-course steroids (≤ 300 mg hydrocortisone/day and ≥ 5 days) would provide greater benefit than short-course, high-dose corticosteroids. The sensitivity analysis of five studies with low-dose, long-course corticosteroids showed a clear reduction in 28-day mortality (RR 0.80; 0.67 to 0.95) with no heterogeneity. There was no statistically significant difference in GI bleeds, superinfections, and hyperglycemia.
This is a very well-done review, which included an exhaustive search for all available evidence. The authors conclude based on the findings of an individual study in the review that patients with septic shock should undergo adrenal insufficiency testing prior to starting empiric therapy with low-dose hydrocortisone (200-300 mg/day). Hydrocortisone should then be stopped if there is no evidence of adrenal insufficiency. However, none of the studies in this review were limited to patients with adrenal insufficiency. Also, although none of the studies individually showed a statistically significant improvement with corticosteroids, they all favored the steroid treatment group with RRs < 1. Although there is good evidence that septic shock patients with adrenal insufficiency should be treated with corticosteroids, it remains unclear if therapy should be generalized to all septic patients. The ongoing European CORTICUS trial should help answer some of these questions.
2. Baddour L.,Yu, V. and the International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Resp Crit Care Med; 2004;170:440-444.
Three retrospective studies indicate that patients with pneumococcal bacteremia are less likely to die if treated with combination antibiotics. The combination of a beta-lactam and a macrolide appear to be especially protective. Based upon this soft data, multiple societies now recommend combination antibiotic therapy with a beta-lactam and a macrolide as first-line therapy for hospitalized patients with CAP. This large, multi-center, prospective observational study analyzed outcomes for all patients with pneumococcal bacteremia. Critically ill patients were eight times more likely to die than non-critically ill patients (mortality: 54.6% vs. 7.3%, p=0.0001). Combination therapy was defined as any two or more antibiotics used concurrently: multiple different regimens were used. The 14-day mortality difference between pneumococcal bacteremic patients receiving monotherapy vs. those receiving combination therapy was not significant (10.4 vs. 11.5%, p-value not disclosed) However, in critically ill patients, combination antibiotic therapy was associated with a marked decrease in mortality (23.4 vs. 55.3%, p=0.0015).
This study has significant limitations. It is not randomized, combination therapy was broadly defined as any two or more antibiotics, and 16% of critically ill patients received only one antibiotic, a major deviation from the standard of care. Nonetheless, this is the first prospective trial that attempts to ascertain which patients with pneumococcal bacteremia benefit from combination therapy. The marked mortality reduction in critically ill patients who received combination therapy reinforces the current recommendation that septic patients with pneumococcal bacteremia should receive combination therapy. However, these findings also underscore the fact that current guidelines for the treatment of an exceedingly common and serious disease are based upon weak retrospective data. Further randomized prospective trials are needed to determine which patients with pneumococcal pneumonia may actually benefit from combination antimicrobial therapy and what combination is most efficacious.
3. Fernandez-Avilles F, Alsonso J, Castro-Beivas A, et al, on behalf of the GRACIA (Grupo de Analisis de la Cardiopatio Isquemica Aguda) Group. Routine invasive strategy within 24 hours of thrombolysis versus ischemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1). Lancet;2004;364:045-1053
In the last ACC/AHA guidelines for acute myocardial infarction (1999), angioplasty soon after thrombolysis is strongly discouraged (class III) because studies to date showed no significant difference in outcomes and propensity for adverse events, i.e. bleeding. However, as stated in these last recommendations, the benefits of early post-thrombolysis percutaneous transluminal coronary angioplasty (PTCA) with stenting should be reassessed as interventional strategies mature. In the current era of stents and newer antiplatelet therapies, it looks as if now is the time to take another look.
The GRACIA-1 was a randomized, multi-centered trial to assess early intervention following thrombolysis in ST-elevation myocardial infarction (STEMI). Five hundred patients were enrolled and randomized to receive either fibrin-specific thrombolytics alone in the conservative group or thrombolysis combined with early PTCA. The primary endpoint was a combined rate of death, non-fatal reinfarction, or ischemia-induced revascularization at 1 year. Pre-discharge PTCA and stenting in those demonstrating recurrent ischemia in the conservative group (n=52) was analyzed as a secondary endpoint. One-year follow-up was completed in 98% of patients. Both groups had similar major cardiac events at 30 days, with the one-year endpoint demonstrating no difference in mortality. Significant differences were seen in the primary endpoint at one year [23 (9%) in the invasive group vs. 51 (21%) in the conservative group (RR-0.44, 95% CI 0.28-0.70 p=0.00008)].
A major limitation of this study was the low-risk profile of its patients, and the fact that it was not powered to differentiate between mortality and reinfarction. It will be interesting to see if these results are replicated in future studies (CARESS-2005) and their clinical impact on the management of acute myocardial infarction in centers without interventional support.
4. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med.2004;19:732-739.
Falls in hospital patients are common and persistent problems in hospitals across the country, with significant impact on patient safety, morbidity, and health care cost. Previous studies have reported up to 30% of inpatient falls result in injury, with 4-6% resulting in serious injury. Most studies on falls are retrospective reviews. This paper detailed a prospective observational study designed to identify and analyze the patient characteristics or the circumstances that contribute to falls. Using an online adverse event reporting system, patient falls were identified. Once identified, additional data sources, including the patients’ medical records, electronic nursing records, and interviews with patient or family members and nurses, were used to collect information. A total of 183 patients fell during the study period, with 85% of the falls occurring in the patient’s room.
Half of the falls involved bowel or bladder elimination and were more likely to occur in patients over 65 years in age (adjusted odds ratio 2.4; 95% confidence interval 1.1 to 5.3). Most of the falls (59%) occurred during the evening/overnight. 58% of the patients who fell had received agents with central nervous system activity in the 24 hours prior to a fall. 12% of the patients who fell received sedative-hypnotics. Repeat fallers were more likely to be men than women (11/86 [13%] vs 4/97 [4%]; p=0.03). 42% of the falls resulted in some type of injury, ranging from pain/swelling (34%) to cardiac arrest/death (0.5%). In multivariate analysis, only elimination-related falls remained a significant predictor of being injured from a fall (aOR , 2.4; 95% CI 1.1 to 5.3). Interestingly, patients who were confused or disoriented were less likely to be injured than alert and oriented patients (crude OR, 0.5; 95% CI, 0.3 to 0.98). When examined by services, medicine and neurology had the highest fall rate at 6.12 falls per 1000 patient days and had the highest patient-to-nurse ratio of 6.5 and 5.3, respectively.
While specific independent risk factors for prevention of falls could not be determined in this study due to a lack of a control group, their findings are consistent with previously identified risk factors for falling, including weakness, poor cognitive status including medication-related changes, and altered elimination. Potential interventions to prevent falls include toileting schedules for high-risk elderly patients and review of medication lists to minimize centrally acting, psychotropic, or sedating agents.
5. Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med; 2004;164:2044-2050
Elderly patients are increasingly likely to require long-term anticoagulation. Despite this, physicians often withhold long-term anticoagulation due to perceived risk factors for bleeding, including age, comorbidity, and cognitive or functional impairment.
This combination retrospective and prospective observational study evaluated the safety and quality of anticoagulation in elderly patients. Over a three-year span, 323 elderly patients were discharged on warfarin from a large Israeli hospital. These patients were frail and potentially “at risk”; 54% were older than age 80, 81% were uneducated, and 84% had low income. 47% were considered cognitively intact (according to MMSE) and only 34% were functionally independent. Using a multivariate analysis, the authors determined that only poor quality of anticoagulation education (OR: 8.83; 95% CI: 2.0-50.2), polypharmacy (OR: 6.14; 95% CI 1.2-42.4) and INR >3 (OR: 1.08; 95% CI 1.03-1.14) were associated with major bleeding.
This study of a “real world” population of frail, at-risk elderly patients provides important insights into risks for major bleeding resulting from warfarin therapy. Surprisingly, advanced age, cognitive impairment and markers for frailty did not confer elevated risk for major bleeding. Importantly, the study did not explicitly address patient fall risk, an often-cited reason for withholding anticoagulation therapy. Supratherapeutic anticoagulation is associated with a statistically but not clinically significant bleeding risk. Polypharmacy is increasingly unavoidable in elderly patients. However, appropriate anticoagulation therapy should be the standard of care. This study makes it clear that we need to focus our efforts on ensuring that elderly patients and their caregivers receive appropriate anticoagulation education prior to discharge from the hospital.
6. Prinssen M, Verhoeven E, Buth J, et al. A Randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607-18.
Endovascular repair of abdominal aortic aneurysm, which involves percutaneous introduction of a graft to bridge an aortic aneurysm, has been available since the early 1990s. This procedure was initially used in patients who were felt to be at high risk for the traditional open procedure. This selection bias may have affected the outcome of earlier studies. Therefore, the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial was designed to assess outcomes in patients deemed fit to undergo either open or endovascular repair. The study was conducted at 24 centers in the Netherlands and four centers in Belgium. Three hundred and forty-five patients had abdominal aortic aneurysms of at least 5 cm and were considered eligible for either open or endovascular repair. Patients were then randomized to undergo one procedure or the other.
Surgeons experienced in both endovascular and open repair performed the procedures. Primary outcomes were 30-day mortality (defined as death during the primary hospital admission or within 30 days), severe complications, and the combination of the two. The operative mortality rate was 4.6% in the open-repair group and 1.2% in the endovascular repair group, with a risk ratio of 3.9 (95% CI, 0.9-32.9). The combined endpoint of mortality and severe complication was 9.8% in the open-repair group and 4.7% in the endovascular repair group, with a risk ratio of 2.1 (95% CI, 0.9 to 5.4). It should be noted that 90% of study patients were men. These findings indicate that endovascular repair of aortic aneurysm results in less short-term morbidity and mortality than open repair. Larger studies with longer follow up are indicated.
7. Spargias K, Alexopoulos E, Kyrzopoulos S. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation.110(18)2837-42
In this study, a team of Greek researchers studied the use of vitamin C in patients with renal insufficiency (creatinine >1.2) undergoing coronary catheterization or intervention to determine if it prevented contrast-mediated nephropathy (CMN). Although the etiology of CMN is unknown, ischemic insults to the renal medulla and free radical release have been implicated. Since vitamin C has been shown in animal studies to attenuate nephropathy when administered with known renal toxins, a similar effect was postulated when administered with IV contrast.
Two hundred and twenty patients electively admitted for coronary catheterization or intervention were randomized to placebo or to receive 3 grams of vitamin C 2 hours prior to the dye load followed by 2 gm that night and the morning after. The two groups were balanced for presence of hypertension, diabetes, tobacco use, and use of commonly prescribed medications. Intravenous hydration was given to all at variable rates depending on left ventricular ejection fraction. The catheterization team chose the type of contrast agent. Creatinine was measured at baseline (up to 3 months prior to dye load) and 2-5 days afterwards. CMN was defined as a rise in total serum creatinine by 0.5 mg/dL or by 25%. Using these criteria, 9% of the vitamin C group developed CMN as opposed to 20% in the controls (NNT 9; 95% CI: 5-53). Logistical regression was performed to account for differences in age, initial serum creatinine, or both, and always yielded significant differences. The treatment group was slightly older, had higher rates of isoosmolar contrast administration (reno-protective), and had slightly higher baseline creatinines, so the true protective effect was thought even higher than reported.
This study is limited by small sample size, an overwhelmingly male patient base (90%), and the suspected presence of atherosclerotic heart disease in all patients. The amount and rate of delivery of contrast was not noted. The vitamin C preparation used was not described, implying that all preparations were bioequivalent. No mention was made of whether these results could be extrapolated to other procedures involving contrast. Given the low cost and high tolerability of vitamin C, however, further studies would certainly be welcome.
8. Yadav J, Wholey M, Kuntz R, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. NEJM.2004;351:1493-1501.
Carotid angioplasty has been available for the past decade, but, due to possible complications such as plaque embolization and stent compression, the procedure had been limited to patients unsuitable for surgical endarterectomy. Recently, the introduction of crush-resistant nitinol stents and emboli protection devices has made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year.
1. Annane D, Bellissant E, Briegel J, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and metaanalysis. BMJ. 2004;329:480.
Severe sepsis is a common cause of ICU admissions and continues to have mortality rates as high as 30%. As research has evolved, the role of corticosteroids in sepsis has changed. Annane and colleagues systematically reviewed corticosteroid treatment for severe sepsis and septic shock. The authors found 15 randomized trials that evaluated their main outcome of all-cause mortality at 28 days. When these results were pooled there was no significant improvement in mortality (RR 0.98; 0.87 to 1.10). However, the analysis showed very significant heterogeneity, so the authors appropriately performed a sensitivity analysis based on an a priori hypothesis that low-dose, long-course steroids (≤ 300 mg hydrocortisone/day and ≥ 5 days) would provide greater benefit than short-course, high-dose corticosteroids. The sensitivity analysis of five studies with low-dose, long-course corticosteroids showed a clear reduction in 28-day mortality (RR 0.80; 0.67 to 0.95) with no heterogeneity. There was no statistically significant difference in GI bleeds, superinfections, and hyperglycemia.
This is a very well-done review, which included an exhaustive search for all available evidence. The authors conclude based on the findings of an individual study in the review that patients with septic shock should undergo adrenal insufficiency testing prior to starting empiric therapy with low-dose hydrocortisone (200-300 mg/day). Hydrocortisone should then be stopped if there is no evidence of adrenal insufficiency. However, none of the studies in this review were limited to patients with adrenal insufficiency. Also, although none of the studies individually showed a statistically significant improvement with corticosteroids, they all favored the steroid treatment group with RRs < 1. Although there is good evidence that septic shock patients with adrenal insufficiency should be treated with corticosteroids, it remains unclear if therapy should be generalized to all septic patients. The ongoing European CORTICUS trial should help answer some of these questions.
2. Baddour L.,Yu, V. and the International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Resp Crit Care Med; 2004;170:440-444.
Three retrospective studies indicate that patients with pneumococcal bacteremia are less likely to die if treated with combination antibiotics. The combination of a beta-lactam and a macrolide appear to be especially protective. Based upon this soft data, multiple societies now recommend combination antibiotic therapy with a beta-lactam and a macrolide as first-line therapy for hospitalized patients with CAP. This large, multi-center, prospective observational study analyzed outcomes for all patients with pneumococcal bacteremia. Critically ill patients were eight times more likely to die than non-critically ill patients (mortality: 54.6% vs. 7.3%, p=0.0001). Combination therapy was defined as any two or more antibiotics used concurrently: multiple different regimens were used. The 14-day mortality difference between pneumococcal bacteremic patients receiving monotherapy vs. those receiving combination therapy was not significant (10.4 vs. 11.5%, p-value not disclosed) However, in critically ill patients, combination antibiotic therapy was associated with a marked decrease in mortality (23.4 vs. 55.3%, p=0.0015).
This study has significant limitations. It is not randomized, combination therapy was broadly defined as any two or more antibiotics, and 16% of critically ill patients received only one antibiotic, a major deviation from the standard of care. Nonetheless, this is the first prospective trial that attempts to ascertain which patients with pneumococcal bacteremia benefit from combination therapy. The marked mortality reduction in critically ill patients who received combination therapy reinforces the current recommendation that septic patients with pneumococcal bacteremia should receive combination therapy. However, these findings also underscore the fact that current guidelines for the treatment of an exceedingly common and serious disease are based upon weak retrospective data. Further randomized prospective trials are needed to determine which patients with pneumococcal pneumonia may actually benefit from combination antimicrobial therapy and what combination is most efficacious.
3. Fernandez-Avilles F, Alsonso J, Castro-Beivas A, et al, on behalf of the GRACIA (Grupo de Analisis de la Cardiopatio Isquemica Aguda) Group. Routine invasive strategy within 24 hours of thrombolysis versus ischemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1). Lancet;2004;364:045-1053
In the last ACC/AHA guidelines for acute myocardial infarction (1999), angioplasty soon after thrombolysis is strongly discouraged (class III) because studies to date showed no significant difference in outcomes and propensity for adverse events, i.e. bleeding. However, as stated in these last recommendations, the benefits of early post-thrombolysis percutaneous transluminal coronary angioplasty (PTCA) with stenting should be reassessed as interventional strategies mature. In the current era of stents and newer antiplatelet therapies, it looks as if now is the time to take another look.
The GRACIA-1 was a randomized, multi-centered trial to assess early intervention following thrombolysis in ST-elevation myocardial infarction (STEMI). Five hundred patients were enrolled and randomized to receive either fibrin-specific thrombolytics alone in the conservative group or thrombolysis combined with early PTCA. The primary endpoint was a combined rate of death, non-fatal reinfarction, or ischemia-induced revascularization at 1 year. Pre-discharge PTCA and stenting in those demonstrating recurrent ischemia in the conservative group (n=52) was analyzed as a secondary endpoint. One-year follow-up was completed in 98% of patients. Both groups had similar major cardiac events at 30 days, with the one-year endpoint demonstrating no difference in mortality. Significant differences were seen in the primary endpoint at one year [23 (9%) in the invasive group vs. 51 (21%) in the conservative group (RR-0.44, 95% CI 0.28-0.70 p=0.00008)].
A major limitation of this study was the low-risk profile of its patients, and the fact that it was not powered to differentiate between mortality and reinfarction. It will be interesting to see if these results are replicated in future studies (CARESS-2005) and their clinical impact on the management of acute myocardial infarction in centers without interventional support.
4. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med.2004;19:732-739.
Falls in hospital patients are common and persistent problems in hospitals across the country, with significant impact on patient safety, morbidity, and health care cost. Previous studies have reported up to 30% of inpatient falls result in injury, with 4-6% resulting in serious injury. Most studies on falls are retrospective reviews. This paper detailed a prospective observational study designed to identify and analyze the patient characteristics or the circumstances that contribute to falls. Using an online adverse event reporting system, patient falls were identified. Once identified, additional data sources, including the patients’ medical records, electronic nursing records, and interviews with patient or family members and nurses, were used to collect information. A total of 183 patients fell during the study period, with 85% of the falls occurring in the patient’s room.
Half of the falls involved bowel or bladder elimination and were more likely to occur in patients over 65 years in age (adjusted odds ratio 2.4; 95% confidence interval 1.1 to 5.3). Most of the falls (59%) occurred during the evening/overnight. 58% of the patients who fell had received agents with central nervous system activity in the 24 hours prior to a fall. 12% of the patients who fell received sedative-hypnotics. Repeat fallers were more likely to be men than women (11/86 [13%] vs 4/97 [4%]; p=0.03). 42% of the falls resulted in some type of injury, ranging from pain/swelling (34%) to cardiac arrest/death (0.5%). In multivariate analysis, only elimination-related falls remained a significant predictor of being injured from a fall (aOR , 2.4; 95% CI 1.1 to 5.3). Interestingly, patients who were confused or disoriented were less likely to be injured than alert and oriented patients (crude OR, 0.5; 95% CI, 0.3 to 0.98). When examined by services, medicine and neurology had the highest fall rate at 6.12 falls per 1000 patient days and had the highest patient-to-nurse ratio of 6.5 and 5.3, respectively.
While specific independent risk factors for prevention of falls could not be determined in this study due to a lack of a control group, their findings are consistent with previously identified risk factors for falling, including weakness, poor cognitive status including medication-related changes, and altered elimination. Potential interventions to prevent falls include toileting schedules for high-risk elderly patients and review of medication lists to minimize centrally acting, psychotropic, or sedating agents.
5. Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med; 2004;164:2044-2050
Elderly patients are increasingly likely to require long-term anticoagulation. Despite this, physicians often withhold long-term anticoagulation due to perceived risk factors for bleeding, including age, comorbidity, and cognitive or functional impairment.
This combination retrospective and prospective observational study evaluated the safety and quality of anticoagulation in elderly patients. Over a three-year span, 323 elderly patients were discharged on warfarin from a large Israeli hospital. These patients were frail and potentially “at risk”; 54% were older than age 80, 81% were uneducated, and 84% had low income. 47% were considered cognitively intact (according to MMSE) and only 34% were functionally independent. Using a multivariate analysis, the authors determined that only poor quality of anticoagulation education (OR: 8.83; 95% CI: 2.0-50.2), polypharmacy (OR: 6.14; 95% CI 1.2-42.4) and INR >3 (OR: 1.08; 95% CI 1.03-1.14) were associated with major bleeding.
This study of a “real world” population of frail, at-risk elderly patients provides important insights into risks for major bleeding resulting from warfarin therapy. Surprisingly, advanced age, cognitive impairment and markers for frailty did not confer elevated risk for major bleeding. Importantly, the study did not explicitly address patient fall risk, an often-cited reason for withholding anticoagulation therapy. Supratherapeutic anticoagulation is associated with a statistically but not clinically significant bleeding risk. Polypharmacy is increasingly unavoidable in elderly patients. However, appropriate anticoagulation therapy should be the standard of care. This study makes it clear that we need to focus our efforts on ensuring that elderly patients and their caregivers receive appropriate anticoagulation education prior to discharge from the hospital.
6. Prinssen M, Verhoeven E, Buth J, et al. A Randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607-18.
Endovascular repair of abdominal aortic aneurysm, which involves percutaneous introduction of a graft to bridge an aortic aneurysm, has been available since the early 1990s. This procedure was initially used in patients who were felt to be at high risk for the traditional open procedure. This selection bias may have affected the outcome of earlier studies. Therefore, the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial was designed to assess outcomes in patients deemed fit to undergo either open or endovascular repair. The study was conducted at 24 centers in the Netherlands and four centers in Belgium. Three hundred and forty-five patients had abdominal aortic aneurysms of at least 5 cm and were considered eligible for either open or endovascular repair. Patients were then randomized to undergo one procedure or the other.
Surgeons experienced in both endovascular and open repair performed the procedures. Primary outcomes were 30-day mortality (defined as death during the primary hospital admission or within 30 days), severe complications, and the combination of the two. The operative mortality rate was 4.6% in the open-repair group and 1.2% in the endovascular repair group, with a risk ratio of 3.9 (95% CI, 0.9-32.9). The combined endpoint of mortality and severe complication was 9.8% in the open-repair group and 4.7% in the endovascular repair group, with a risk ratio of 2.1 (95% CI, 0.9 to 5.4). It should be noted that 90% of study patients were men. These findings indicate that endovascular repair of aortic aneurysm results in less short-term morbidity and mortality than open repair. Larger studies with longer follow up are indicated.
7. Spargias K, Alexopoulos E, Kyrzopoulos S. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation.110(18)2837-42
In this study, a team of Greek researchers studied the use of vitamin C in patients with renal insufficiency (creatinine >1.2) undergoing coronary catheterization or intervention to determine if it prevented contrast-mediated nephropathy (CMN). Although the etiology of CMN is unknown, ischemic insults to the renal medulla and free radical release have been implicated. Since vitamin C has been shown in animal studies to attenuate nephropathy when administered with known renal toxins, a similar effect was postulated when administered with IV contrast.
Two hundred and twenty patients electively admitted for coronary catheterization or intervention were randomized to placebo or to receive 3 grams of vitamin C 2 hours prior to the dye load followed by 2 gm that night and the morning after. The two groups were balanced for presence of hypertension, diabetes, tobacco use, and use of commonly prescribed medications. Intravenous hydration was given to all at variable rates depending on left ventricular ejection fraction. The catheterization team chose the type of contrast agent. Creatinine was measured at baseline (up to 3 months prior to dye load) and 2-5 days afterwards. CMN was defined as a rise in total serum creatinine by 0.5 mg/dL or by 25%. Using these criteria, 9% of the vitamin C group developed CMN as opposed to 20% in the controls (NNT 9; 95% CI: 5-53). Logistical regression was performed to account for differences in age, initial serum creatinine, or both, and always yielded significant differences. The treatment group was slightly older, had higher rates of isoosmolar contrast administration (reno-protective), and had slightly higher baseline creatinines, so the true protective effect was thought even higher than reported.
This study is limited by small sample size, an overwhelmingly male patient base (90%), and the suspected presence of atherosclerotic heart disease in all patients. The amount and rate of delivery of contrast was not noted. The vitamin C preparation used was not described, implying that all preparations were bioequivalent. No mention was made of whether these results could be extrapolated to other procedures involving contrast. Given the low cost and high tolerability of vitamin C, however, further studies would certainly be welcome.
8. Yadav J, Wholey M, Kuntz R, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. NEJM.2004;351:1493-1501.
Carotid angioplasty has been available for the past decade, but, due to possible complications such as plaque embolization and stent compression, the procedure had been limited to patients unsuitable for surgical endarterectomy. Recently, the introduction of crush-resistant nitinol stents and emboli protection devices has made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year.
Practice Guidelines for the Management of Bacterial Meningitis
Enter text here
Enter text here
Enter text here