User login
Improving Patient Safety and Quality of Care
Patient safety and improved quality of care have become priority issues in the American healthcare system. The potential for medical errors was highlighted in 1999 when the Quality of Health Care in America Committee of the Institute of Medicine (IOM) published its first report, To Err is Human: Building a Safer Health System. The committee estimated that between 44,000 and 98,000 people die annually from inpatient medical errors. The eighth leading cause of death in this country, preventable medical errors, cost the U.S. approximately $17 billion annually in direct and indirect costs (IOM). These alarming statistics in the IOM report ignited the patient safety movement (I).
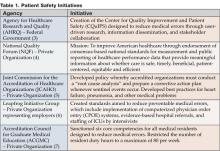
The IOM report made a series of recommendations that included the creation of a center for patient safety, the development of a national public reporting system, the establishment of oversight agencies, and the incorporation of safety principles into monitoring systems. Public and private agencies have responded with a series of initiatives that address these recommendations (See Table 1).
One healthcare expert describes three reasons as to why the potential for medical errors has increased. First, technology has created a sophisticated array of test, x-rays, laboratory procedures, and diagnostic tools. Second, pharmaceutical research has introduced thousands of new medications to the marketplace. Finally, specialization has led to experts, both physician and non-physician, in a wide range of body systems, diseases, settings, procedures, and therapies. Hospital medicine represents a new type of medical specialty that has the potential to address this increased complexity and sophistication and to improve patient care in the hospital inpatient environment (2).
Hospitalists as Team Coordinators
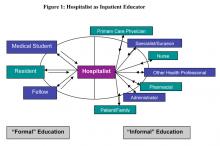
To achieve maximum positive outcomes in the complex inpatient environment, a qualified coordinator must educate others and facilitate activity revolving around patient care. Hospitalists as inpatient experts possess the necessary qualifications to integrate hospital systems and maximize efforts to enhance patient safety by monitoring medication distribution, chairing pharmaceuticals and therapeutics (P&T) committees, overseeing computerized physician order entry (CPOE), directing quality/performance improvement projects, and collaborating with discharge planning and case management.
Lakshmi Halasyamani, MD, is vice chair of the department of Internal Medicine at St. Joseph Mercy Hospital in Michigan and chairperson of the Society of Hospital Medicine (SHM) Hospital Quality and Patient Safety Committee. She says, Hospitalists have a ‘lens of understanding the systems under which they care for patients.’ They take care of patients in the hospital every single day so they can examine the processes with which they work. Hospitalists have an ideal perspective from which to reform ineffective systems.”
In spite of all the guidelines established by federal agencies and expert groups, Dr. Halasyamani points out that implementation barriers exist that prevent well-intentioned protocols and best practices from being carried out. Part of the challenge is the performance of a critical piece of the infrastructure—the multidisciplinary team. The very nature of healthcare demands an inherent need to coordinate and communicate. “Treating the patient is not the responsibility of one single individual,” says Halasyamani. “This is a team effort. The hospitalist recognizes that he is part of that team.” By elevating the ideals of teamwork, hospitalists can deliver to the patients the essential care that patients need, both while in the hospital and after they are discharged. In managing hospital inpatients, physicians must cope with high intensity of illness, pressures to reduce length of stay (LOS), and the coordination of handoffs among many specialists. According to Halasyamani, this can be a “recipe for disaster.”
Halasyamani acknowledges the vital role of protocols in reducing medical errors and improving quality of care. The training, education, and experience a hospitalist has acquired enables him to optimize communication and implement protocols, thus facilitating the practice of delivering safe and consistent care to all patients. In fact, with this smaller core group of inpatient physicians, the development and implementation of protocols can potentially be more effective because it targets a smaller group of physicians than the traditional inpatient model (8).
Kaveh C. Shojania, MD, is assistant professor of medicine at the University of Ottawa and co-author of Internal Bleeding: The Terrifying Truth Behind America's Epidemic Medical Mistakes. He points out that the current inpatient medical landscape involves a significant number of clinicians who practice at the hospital but not all their activity is centered there. “From a clinical perspective, no one has ownership,” he says. “On the other hand, hospitalists are based in a single hospital and have a vested interest in that particular hospital.” Typically generalists, hospitalists tend to interact with all specialists and therefore have a good sense of all interests.
Medical errors occur most often during transition times, from the ICU to the floor or from inpatient to outpatient status. There is the potential for a loss of clinical information during these transfers. According to Shojania, a significant portion of the hospitalist’s time is spent managing these transitions and overseeing patients as they are relocated from floor to floor and discharge to home, rehabilitation facility, or nursing home. He notes that the regulatory agencies have begun to acknowledge the importance of hospitalists. “The JCAHO (Joint Commission for the Accreditation of Healthcare Organizations) recognizes hospitalists as a resource because they are always in the hospital and have a vested interest,” he says (9).
Stakeholder Analysis
Patients stand to gain the most benefit from hospitalists insofar as safety and quality of care is concerned. Through the efforts and oversight of hospitalists, patients may experience reduced medical errors and lower mortality rates. For primary care physicians and hospitals, this lower rate of medical error means fewer medical malpractice cases, the potential for lower insurance premiums and, as a result, enhanced reputations. When hospitals are run more efficiently and provide a greater sense of trust and efficient management practices, society in general becomes the benefactor.
Clinical Trials
To date, few research studies measuring the impact of hospitalists on patient safety and quality of care have been conducted. Quality of care has been assessed largely through the surrogate markers of mortality and readmission rates. One study showed decreased in-hospital and 1-year mortality rates for hospitalist patients (10), and another indicated a decrease in 30-day readmission rates (11).
In addition, data from individual programs demonstrate positive findings. For example, Stacy Goldsholl, MD, medical director of the Covenant Healthcare hospital medicine program in Michigan, reports a 17% decrease in the expected mortality rate in the first year of the hospital medicine program. The information was drawn from the Michigan Hospital Association (MHA) databank and matched for severity and diagnosis (See Table 2). “This was significant when compared to the internal medicine comparison group with similar case mix index (CMI),” says Goldsholl. “In the first half of our second year, we have demonstrated a 46% decrease in expected mortality, while internal medicine had a 4% increase” (12).
Additionally, Goldsholl reports that Covenant initiated a Code Blue and emergency consult service to improve patient outcome and experienced a marked increase in efficiency. Table 3 represents elementary data collected during the first 6 months pre- and post-initiation of the hospital medicine program at Covenant (12).
Conclusion
Patient safety and quality of care in the hospital require a team of dedicated people to effect change. Orchestrating the team effectively is the responsibility of an attending physician. With the numerous “handoffs” that take place during hospitalization, the potential for medical errors increases exponentially. Federal mandates requiring the conversion to electronic medical records, which includes basic health information as well as critical data regarding medications, procedures, and surgeries, further complicates efficient and safe patient management. According to Robert Wachter, “Those doctors with the best outcomes were those who tended to treat similar patients with similar problems using similar techniques.” By definition, the hospitalist is a “physician who focuses his practice on the care, coordination, and safety of hospitalized patients.” Who better to stand at the center of the issue of reduced medical errors, improved patient care, and enhanced quality of care than hospitalists (13)?
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
References
- To Err is Human: Building a Safer Health System, Institute of Medicine, November 1999.
- Wachter R. The end of the beginning: patient safety five years after ‘To Err Is Human.’ Health Affairs. November 30, 2004.
- Mission Statement: Center for Quality Improvement and Patient Safety. February 2004. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/about/cquips/cquipsmiss.htm.
- Safe Practices for Better Healthcare: a Consensus. The National Quality Forum, 2003.
- Joint Commission for Accreditation of Healthcare Organizations (JCAHO), www.jcaho.org.
- Leapfrog Group, www.leapfroggroup.org.
- Accreditation Council for Graduate Medical Education (ACGME), www.acgme.org.
- Halasyamani L. Telephone interview. February 7, 2005.
- Shojania KG. Assistant professor of medicine, University of Ottawa. Telephone interview. January 31, 2005.
- Auerbach AD, Wachter RM, Katz P. et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859-65.
- Kulaga ME, Charney P, O’Mahoney SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Goldsholl S. Medical director. Covenant Healthcare hospital medicine program, Saginaw, Michigan, email interview. January 31, 2005.
- Wachter R, Shojania K. Internal bleeding: the truth behind America’s terrifying epidemic of medical mistakes. Rugged Land, LLC, 2004.
Patient safety and improved quality of care have become priority issues in the American healthcare system. The potential for medical errors was highlighted in 1999 when the Quality of Health Care in America Committee of the Institute of Medicine (IOM) published its first report, To Err is Human: Building a Safer Health System. The committee estimated that between 44,000 and 98,000 people die annually from inpatient medical errors. The eighth leading cause of death in this country, preventable medical errors, cost the U.S. approximately $17 billion annually in direct and indirect costs (IOM). These alarming statistics in the IOM report ignited the patient safety movement (I).
The IOM report made a series of recommendations that included the creation of a center for patient safety, the development of a national public reporting system, the establishment of oversight agencies, and the incorporation of safety principles into monitoring systems. Public and private agencies have responded with a series of initiatives that address these recommendations (See Table 1).
One healthcare expert describes three reasons as to why the potential for medical errors has increased. First, technology has created a sophisticated array of test, x-rays, laboratory procedures, and diagnostic tools. Second, pharmaceutical research has introduced thousands of new medications to the marketplace. Finally, specialization has led to experts, both physician and non-physician, in a wide range of body systems, diseases, settings, procedures, and therapies. Hospital medicine represents a new type of medical specialty that has the potential to address this increased complexity and sophistication and to improve patient care in the hospital inpatient environment (2).
Hospitalists as Team Coordinators
To achieve maximum positive outcomes in the complex inpatient environment, a qualified coordinator must educate others and facilitate activity revolving around patient care. Hospitalists as inpatient experts possess the necessary qualifications to integrate hospital systems and maximize efforts to enhance patient safety by monitoring medication distribution, chairing pharmaceuticals and therapeutics (P&T) committees, overseeing computerized physician order entry (CPOE), directing quality/performance improvement projects, and collaborating with discharge planning and case management.
Lakshmi Halasyamani, MD, is vice chair of the department of Internal Medicine at St. Joseph Mercy Hospital in Michigan and chairperson of the Society of Hospital Medicine (SHM) Hospital Quality and Patient Safety Committee. She says, Hospitalists have a ‘lens of understanding the systems under which they care for patients.’ They take care of patients in the hospital every single day so they can examine the processes with which they work. Hospitalists have an ideal perspective from which to reform ineffective systems.”
In spite of all the guidelines established by federal agencies and expert groups, Dr. Halasyamani points out that implementation barriers exist that prevent well-intentioned protocols and best practices from being carried out. Part of the challenge is the performance of a critical piece of the infrastructure—the multidisciplinary team. The very nature of healthcare demands an inherent need to coordinate and communicate. “Treating the patient is not the responsibility of one single individual,” says Halasyamani. “This is a team effort. The hospitalist recognizes that he is part of that team.” By elevating the ideals of teamwork, hospitalists can deliver to the patients the essential care that patients need, both while in the hospital and after they are discharged. In managing hospital inpatients, physicians must cope with high intensity of illness, pressures to reduce length of stay (LOS), and the coordination of handoffs among many specialists. According to Halasyamani, this can be a “recipe for disaster.”
Halasyamani acknowledges the vital role of protocols in reducing medical errors and improving quality of care. The training, education, and experience a hospitalist has acquired enables him to optimize communication and implement protocols, thus facilitating the practice of delivering safe and consistent care to all patients. In fact, with this smaller core group of inpatient physicians, the development and implementation of protocols can potentially be more effective because it targets a smaller group of physicians than the traditional inpatient model (8).
Kaveh C. Shojania, MD, is assistant professor of medicine at the University of Ottawa and co-author of Internal Bleeding: The Terrifying Truth Behind America's Epidemic Medical Mistakes. He points out that the current inpatient medical landscape involves a significant number of clinicians who practice at the hospital but not all their activity is centered there. “From a clinical perspective, no one has ownership,” he says. “On the other hand, hospitalists are based in a single hospital and have a vested interest in that particular hospital.” Typically generalists, hospitalists tend to interact with all specialists and therefore have a good sense of all interests.
Medical errors occur most often during transition times, from the ICU to the floor or from inpatient to outpatient status. There is the potential for a loss of clinical information during these transfers. According to Shojania, a significant portion of the hospitalist’s time is spent managing these transitions and overseeing patients as they are relocated from floor to floor and discharge to home, rehabilitation facility, or nursing home. He notes that the regulatory agencies have begun to acknowledge the importance of hospitalists. “The JCAHO (Joint Commission for the Accreditation of Healthcare Organizations) recognizes hospitalists as a resource because they are always in the hospital and have a vested interest,” he says (9).
Stakeholder Analysis
Patients stand to gain the most benefit from hospitalists insofar as safety and quality of care is concerned. Through the efforts and oversight of hospitalists, patients may experience reduced medical errors and lower mortality rates. For primary care physicians and hospitals, this lower rate of medical error means fewer medical malpractice cases, the potential for lower insurance premiums and, as a result, enhanced reputations. When hospitals are run more efficiently and provide a greater sense of trust and efficient management practices, society in general becomes the benefactor.
Clinical Trials
To date, few research studies measuring the impact of hospitalists on patient safety and quality of care have been conducted. Quality of care has been assessed largely through the surrogate markers of mortality and readmission rates. One study showed decreased in-hospital and 1-year mortality rates for hospitalist patients (10), and another indicated a decrease in 30-day readmission rates (11).
In addition, data from individual programs demonstrate positive findings. For example, Stacy Goldsholl, MD, medical director of the Covenant Healthcare hospital medicine program in Michigan, reports a 17% decrease in the expected mortality rate in the first year of the hospital medicine program. The information was drawn from the Michigan Hospital Association (MHA) databank and matched for severity and diagnosis (See Table 2). “This was significant when compared to the internal medicine comparison group with similar case mix index (CMI),” says Goldsholl. “In the first half of our second year, we have demonstrated a 46% decrease in expected mortality, while internal medicine had a 4% increase” (12).
Additionally, Goldsholl reports that Covenant initiated a Code Blue and emergency consult service to improve patient outcome and experienced a marked increase in efficiency. Table 3 represents elementary data collected during the first 6 months pre- and post-initiation of the hospital medicine program at Covenant (12).
Conclusion
Patient safety and quality of care in the hospital require a team of dedicated people to effect change. Orchestrating the team effectively is the responsibility of an attending physician. With the numerous “handoffs” that take place during hospitalization, the potential for medical errors increases exponentially. Federal mandates requiring the conversion to electronic medical records, which includes basic health information as well as critical data regarding medications, procedures, and surgeries, further complicates efficient and safe patient management. According to Robert Wachter, “Those doctors with the best outcomes were those who tended to treat similar patients with similar problems using similar techniques.” By definition, the hospitalist is a “physician who focuses his practice on the care, coordination, and safety of hospitalized patients.” Who better to stand at the center of the issue of reduced medical errors, improved patient care, and enhanced quality of care than hospitalists (13)?
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
References
- To Err is Human: Building a Safer Health System, Institute of Medicine, November 1999.
- Wachter R. The end of the beginning: patient safety five years after ‘To Err Is Human.’ Health Affairs. November 30, 2004.
- Mission Statement: Center for Quality Improvement and Patient Safety. February 2004. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/about/cquips/cquipsmiss.htm.
- Safe Practices for Better Healthcare: a Consensus. The National Quality Forum, 2003.
- Joint Commission for Accreditation of Healthcare Organizations (JCAHO), www.jcaho.org.
- Leapfrog Group, www.leapfroggroup.org.
- Accreditation Council for Graduate Medical Education (ACGME), www.acgme.org.
- Halasyamani L. Telephone interview. February 7, 2005.
- Shojania KG. Assistant professor of medicine, University of Ottawa. Telephone interview. January 31, 2005.
- Auerbach AD, Wachter RM, Katz P. et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859-65.
- Kulaga ME, Charney P, O’Mahoney SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Goldsholl S. Medical director. Covenant Healthcare hospital medicine program, Saginaw, Michigan, email interview. January 31, 2005.
- Wachter R, Shojania K. Internal bleeding: the truth behind America’s terrifying epidemic of medical mistakes. Rugged Land, LLC, 2004.
Patient safety and improved quality of care have become priority issues in the American healthcare system. The potential for medical errors was highlighted in 1999 when the Quality of Health Care in America Committee of the Institute of Medicine (IOM) published its first report, To Err is Human: Building a Safer Health System. The committee estimated that between 44,000 and 98,000 people die annually from inpatient medical errors. The eighth leading cause of death in this country, preventable medical errors, cost the U.S. approximately $17 billion annually in direct and indirect costs (IOM). These alarming statistics in the IOM report ignited the patient safety movement (I).
The IOM report made a series of recommendations that included the creation of a center for patient safety, the development of a national public reporting system, the establishment of oversight agencies, and the incorporation of safety principles into monitoring systems. Public and private agencies have responded with a series of initiatives that address these recommendations (See Table 1).
One healthcare expert describes three reasons as to why the potential for medical errors has increased. First, technology has created a sophisticated array of test, x-rays, laboratory procedures, and diagnostic tools. Second, pharmaceutical research has introduced thousands of new medications to the marketplace. Finally, specialization has led to experts, both physician and non-physician, in a wide range of body systems, diseases, settings, procedures, and therapies. Hospital medicine represents a new type of medical specialty that has the potential to address this increased complexity and sophistication and to improve patient care in the hospital inpatient environment (2).
Hospitalists as Team Coordinators
To achieve maximum positive outcomes in the complex inpatient environment, a qualified coordinator must educate others and facilitate activity revolving around patient care. Hospitalists as inpatient experts possess the necessary qualifications to integrate hospital systems and maximize efforts to enhance patient safety by monitoring medication distribution, chairing pharmaceuticals and therapeutics (P&T) committees, overseeing computerized physician order entry (CPOE), directing quality/performance improvement projects, and collaborating with discharge planning and case management.
Lakshmi Halasyamani, MD, is vice chair of the department of Internal Medicine at St. Joseph Mercy Hospital in Michigan and chairperson of the Society of Hospital Medicine (SHM) Hospital Quality and Patient Safety Committee. She says, Hospitalists have a ‘lens of understanding the systems under which they care for patients.’ They take care of patients in the hospital every single day so they can examine the processes with which they work. Hospitalists have an ideal perspective from which to reform ineffective systems.”
In spite of all the guidelines established by federal agencies and expert groups, Dr. Halasyamani points out that implementation barriers exist that prevent well-intentioned protocols and best practices from being carried out. Part of the challenge is the performance of a critical piece of the infrastructure—the multidisciplinary team. The very nature of healthcare demands an inherent need to coordinate and communicate. “Treating the patient is not the responsibility of one single individual,” says Halasyamani. “This is a team effort. The hospitalist recognizes that he is part of that team.” By elevating the ideals of teamwork, hospitalists can deliver to the patients the essential care that patients need, both while in the hospital and after they are discharged. In managing hospital inpatients, physicians must cope with high intensity of illness, pressures to reduce length of stay (LOS), and the coordination of handoffs among many specialists. According to Halasyamani, this can be a “recipe for disaster.”
Halasyamani acknowledges the vital role of protocols in reducing medical errors and improving quality of care. The training, education, and experience a hospitalist has acquired enables him to optimize communication and implement protocols, thus facilitating the practice of delivering safe and consistent care to all patients. In fact, with this smaller core group of inpatient physicians, the development and implementation of protocols can potentially be more effective because it targets a smaller group of physicians than the traditional inpatient model (8).
Kaveh C. Shojania, MD, is assistant professor of medicine at the University of Ottawa and co-author of Internal Bleeding: The Terrifying Truth Behind America's Epidemic Medical Mistakes. He points out that the current inpatient medical landscape involves a significant number of clinicians who practice at the hospital but not all their activity is centered there. “From a clinical perspective, no one has ownership,” he says. “On the other hand, hospitalists are based in a single hospital and have a vested interest in that particular hospital.” Typically generalists, hospitalists tend to interact with all specialists and therefore have a good sense of all interests.
Medical errors occur most often during transition times, from the ICU to the floor or from inpatient to outpatient status. There is the potential for a loss of clinical information during these transfers. According to Shojania, a significant portion of the hospitalist’s time is spent managing these transitions and overseeing patients as they are relocated from floor to floor and discharge to home, rehabilitation facility, or nursing home. He notes that the regulatory agencies have begun to acknowledge the importance of hospitalists. “The JCAHO (Joint Commission for the Accreditation of Healthcare Organizations) recognizes hospitalists as a resource because they are always in the hospital and have a vested interest,” he says (9).
Stakeholder Analysis
Patients stand to gain the most benefit from hospitalists insofar as safety and quality of care is concerned. Through the efforts and oversight of hospitalists, patients may experience reduced medical errors and lower mortality rates. For primary care physicians and hospitals, this lower rate of medical error means fewer medical malpractice cases, the potential for lower insurance premiums and, as a result, enhanced reputations. When hospitals are run more efficiently and provide a greater sense of trust and efficient management practices, society in general becomes the benefactor.
Clinical Trials
To date, few research studies measuring the impact of hospitalists on patient safety and quality of care have been conducted. Quality of care has been assessed largely through the surrogate markers of mortality and readmission rates. One study showed decreased in-hospital and 1-year mortality rates for hospitalist patients (10), and another indicated a decrease in 30-day readmission rates (11).
In addition, data from individual programs demonstrate positive findings. For example, Stacy Goldsholl, MD, medical director of the Covenant Healthcare hospital medicine program in Michigan, reports a 17% decrease in the expected mortality rate in the first year of the hospital medicine program. The information was drawn from the Michigan Hospital Association (MHA) databank and matched for severity and diagnosis (See Table 2). “This was significant when compared to the internal medicine comparison group with similar case mix index (CMI),” says Goldsholl. “In the first half of our second year, we have demonstrated a 46% decrease in expected mortality, while internal medicine had a 4% increase” (12).
Additionally, Goldsholl reports that Covenant initiated a Code Blue and emergency consult service to improve patient outcome and experienced a marked increase in efficiency. Table 3 represents elementary data collected during the first 6 months pre- and post-initiation of the hospital medicine program at Covenant (12).
Conclusion
Patient safety and quality of care in the hospital require a team of dedicated people to effect change. Orchestrating the team effectively is the responsibility of an attending physician. With the numerous “handoffs” that take place during hospitalization, the potential for medical errors increases exponentially. Federal mandates requiring the conversion to electronic medical records, which includes basic health information as well as critical data regarding medications, procedures, and surgeries, further complicates efficient and safe patient management. According to Robert Wachter, “Those doctors with the best outcomes were those who tended to treat similar patients with similar problems using similar techniques.” By definition, the hospitalist is a “physician who focuses his practice on the care, coordination, and safety of hospitalized patients.” Who better to stand at the center of the issue of reduced medical errors, improved patient care, and enhanced quality of care than hospitalists (13)?
Dr. Pak can be contacted at mhp@medicine.wisc.edu.
References
- To Err is Human: Building a Safer Health System, Institute of Medicine, November 1999.
- Wachter R. The end of the beginning: patient safety five years after ‘To Err Is Human.’ Health Affairs. November 30, 2004.
- Mission Statement: Center for Quality Improvement and Patient Safety. February 2004. Agency for Healthcare Research and Quality, Rockville, MD. www.ahrq.gov/about/cquips/cquipsmiss.htm.
- Safe Practices for Better Healthcare: a Consensus. The National Quality Forum, 2003.
- Joint Commission for Accreditation of Healthcare Organizations (JCAHO), www.jcaho.org.
- Leapfrog Group, www.leapfroggroup.org.
- Accreditation Council for Graduate Medical Education (ACGME), www.acgme.org.
- Halasyamani L. Telephone interview. February 7, 2005.
- Shojania KG. Assistant professor of medicine, University of Ottawa. Telephone interview. January 31, 2005.
- Auerbach AD, Wachter RM, Katz P. et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137:859-65.
- Kulaga ME, Charney P, O’Mahoney SP, et al. The positive impact of initiation of hospitalist clinician educators. J Gen Intern Med. 2004;19:293-301.
- Goldsholl S. Medical director. Covenant Healthcare hospital medicine program, Saginaw, Michigan, email interview. January 31, 2005.
- Wachter R, Shojania K. Internal bleeding: the truth behind America’s terrifying epidemic of medical mistakes. Rugged Land, LLC, 2004.
Other Literature of Interest
1. Annane D, Bellissant E, Briegel J, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and metaanalysis. BMJ. 2004;329:480.
Severe sepsis is a common cause of ICU admissions and continues to have mortality rates as high as 30%. As research has evolved, the role of corticosteroids in sepsis has changed. Annane and colleagues systematically reviewed corticosteroid treatment for severe sepsis and septic shock. The authors found 15 randomized trials that evaluated their main outcome of all-cause mortality at 28 days. When these results were pooled there was no significant improvement in mortality (RR 0.98; 0.87 to 1.10). However, the analysis showed very significant heterogeneity, so the authors appropriately performed a sensitivity analysis based on an a priori hypothesis that low-dose, long-course steroids (≤ 300 mg hydrocortisone/day and ≥ 5 days) would provide greater benefit than short-course, high-dose corticosteroids. The sensitivity analysis of five studies with low-dose, long-course corticosteroids showed a clear reduction in 28-day mortality (RR 0.80; 0.67 to 0.95) with no heterogeneity. There was no statistically significant difference in GI bleeds, superinfections, and hyperglycemia.
This is a very well-done review, which included an exhaustive search for all available evidence. The authors conclude based on the findings of an individual study in the review that patients with septic shock should undergo adrenal insufficiency testing prior to starting empiric therapy with low-dose hydrocortisone (200-300 mg/day). Hydrocortisone should then be stopped if there is no evidence of adrenal insufficiency. However, none of the studies in this review were limited to patients with adrenal insufficiency. Also, although none of the studies individually showed a statistically significant improvement with corticosteroids, they all favored the steroid treatment group with RRs < 1. Although there is good evidence that septic shock patients with adrenal insufficiency should be treated with corticosteroids, it remains unclear if therapy should be generalized to all septic patients. The ongoing European CORTICUS trial should help answer some of these questions.
2. Baddour L.,Yu, V. and the International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Resp Crit Care Med; 2004;170:440-444.
Three retrospective studies indicate that patients with pneumococcal bacteremia are less likely to die if treated with combination antibiotics. The combination of a beta-lactam and a macrolide appear to be especially protective. Based upon this soft data, multiple societies now recommend combination antibiotic therapy with a beta-lactam and a macrolide as first-line therapy for hospitalized patients with CAP. This large, multi-center, prospective observational study analyzed outcomes for all patients with pneumococcal bacteremia. Critically ill patients were eight times more likely to die than non-critically ill patients (mortality: 54.6% vs. 7.3%, p=0.0001). Combination therapy was defined as any two or more antibiotics used concurrently: multiple different regimens were used. The 14-day mortality difference between pneumococcal bacteremic patients receiving monotherapy vs. those receiving combination therapy was not significant (10.4 vs. 11.5%, p-value not disclosed) However, in critically ill patients, combination antibiotic therapy was associated with a marked decrease in mortality (23.4 vs. 55.3%, p=0.0015).
This study has significant limitations. It is not randomized, combination therapy was broadly defined as any two or more antibiotics, and 16% of critically ill patients received only one antibiotic, a major deviation from the standard of care. Nonetheless, this is the first prospective trial that attempts to ascertain which patients with pneumococcal bacteremia benefit from combination therapy. The marked mortality reduction in critically ill patients who received combination therapy reinforces the current recommendation that septic patients with pneumococcal bacteremia should receive combination therapy. However, these findings also underscore the fact that current guidelines for the treatment of an exceedingly common and serious disease are based upon weak retrospective data. Further randomized prospective trials are needed to determine which patients with pneumococcal pneumonia may actually benefit from combination antimicrobial therapy and what combination is most efficacious.
3. Fernandez-Avilles F, Alsonso J, Castro-Beivas A, et al, on behalf of the GRACIA (Grupo de Analisis de la Cardiopatio Isquemica Aguda) Group. Routine invasive strategy within 24 hours of thrombolysis versus ischemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1). Lancet;2004;364:045-1053
In the last ACC/AHA guidelines for acute myocardial infarction (1999), angioplasty soon after thrombolysis is strongly discouraged (class III) because studies to date showed no significant difference in outcomes and propensity for adverse events, i.e. bleeding. However, as stated in these last recommendations, the benefits of early post-thrombolysis percutaneous transluminal coronary angioplasty (PTCA) with stenting should be reassessed as interventional strategies mature. In the current era of stents and newer antiplatelet therapies, it looks as if now is the time to take another look.
The GRACIA-1 was a randomized, multi-centered trial to assess early intervention following thrombolysis in ST-elevation myocardial infarction (STEMI). Five hundred patients were enrolled and randomized to receive either fibrin-specific thrombolytics alone in the conservative group or thrombolysis combined with early PTCA. The primary endpoint was a combined rate of death, non-fatal reinfarction, or ischemia-induced revascularization at 1 year. Pre-discharge PTCA and stenting in those demonstrating recurrent ischemia in the conservative group (n=52) was analyzed as a secondary endpoint. One-year follow-up was completed in 98% of patients. Both groups had similar major cardiac events at 30 days, with the one-year endpoint demonstrating no difference in mortality. Significant differences were seen in the primary endpoint at one year [23 (9%) in the invasive group vs. 51 (21%) in the conservative group (RR-0.44, 95% CI 0.28-0.70 p=0.00008)].
A major limitation of this study was the low-risk profile of its patients, and the fact that it was not powered to differentiate between mortality and reinfarction. It will be interesting to see if these results are replicated in future studies (CARESS-2005) and their clinical impact on the management of acute myocardial infarction in centers without interventional support.
4. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med.2004;19:732-739.
Falls in hospital patients are common and persistent problems in hospitals across the country, with significant impact on patient safety, morbidity, and health care cost. Previous studies have reported up to 30% of inpatient falls result in injury, with 4-6% resulting in serious injury. Most studies on falls are retrospective reviews. This paper detailed a prospective observational study designed to identify and analyze the patient characteristics or the circumstances that contribute to falls. Using an online adverse event reporting system, patient falls were identified. Once identified, additional data sources, including the patients’ medical records, electronic nursing records, and interviews with patient or family members and nurses, were used to collect information. A total of 183 patients fell during the study period, with 85% of the falls occurring in the patient’s room.
Half of the falls involved bowel or bladder elimination and were more likely to occur in patients over 65 years in age (adjusted odds ratio 2.4; 95% confidence interval 1.1 to 5.3). Most of the falls (59%) occurred during the evening/overnight. 58% of the patients who fell had received agents with central nervous system activity in the 24 hours prior to a fall. 12% of the patients who fell received sedative-hypnotics. Repeat fallers were more likely to be men than women (11/86 [13%] vs 4/97 [4%]; p=0.03). 42% of the falls resulted in some type of injury, ranging from pain/swelling (34%) to cardiac arrest/death (0.5%). In multivariate analysis, only elimination-related falls remained a significant predictor of being injured from a fall (aOR , 2.4; 95% CI 1.1 to 5.3). Interestingly, patients who were confused or disoriented were less likely to be injured than alert and oriented patients (crude OR, 0.5; 95% CI, 0.3 to 0.98). When examined by services, medicine and neurology had the highest fall rate at 6.12 falls per 1000 patient days and had the highest patient-to-nurse ratio of 6.5 and 5.3, respectively.
While specific independent risk factors for prevention of falls could not be determined in this study due to a lack of a control group, their findings are consistent with previously identified risk factors for falling, including weakness, poor cognitive status including medication-related changes, and altered elimination. Potential interventions to prevent falls include toileting schedules for high-risk elderly patients and review of medication lists to minimize centrally acting, psychotropic, or sedating agents.
5. Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med; 2004;164:2044-2050
Elderly patients are increasingly likely to require long-term anticoagulation. Despite this, physicians often withhold long-term anticoagulation due to perceived risk factors for bleeding, including age, comorbidity, and cognitive or functional impairment.
This combination retrospective and prospective observational study evaluated the safety and quality of anticoagulation in elderly patients. Over a three-year span, 323 elderly patients were discharged on warfarin from a large Israeli hospital. These patients were frail and potentially “at risk”; 54% were older than age 80, 81% were uneducated, and 84% had low income. 47% were considered cognitively intact (according to MMSE) and only 34% were functionally independent. Using a multivariate analysis, the authors determined that only poor quality of anticoagulation education (OR: 8.83; 95% CI: 2.0-50.2), polypharmacy (OR: 6.14; 95% CI 1.2-42.4) and INR >3 (OR: 1.08; 95% CI 1.03-1.14) were associated with major bleeding.
This study of a “real world” population of frail, at-risk elderly patients provides important insights into risks for major bleeding resulting from warfarin therapy. Surprisingly, advanced age, cognitive impairment and markers for frailty did not confer elevated risk for major bleeding. Importantly, the study did not explicitly address patient fall risk, an often-cited reason for withholding anticoagulation therapy. Supratherapeutic anticoagulation is associated with a statistically but not clinically significant bleeding risk. Polypharmacy is increasingly unavoidable in elderly patients. However, appropriate anticoagulation therapy should be the standard of care. This study makes it clear that we need to focus our efforts on ensuring that elderly patients and their caregivers receive appropriate anticoagulation education prior to discharge from the hospital.
6. Prinssen M, Verhoeven E, Buth J, et al. A Randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607-18.
Endovascular repair of abdominal aortic aneurysm, which involves percutaneous introduction of a graft to bridge an aortic aneurysm, has been available since the early 1990s. This procedure was initially used in patients who were felt to be at high risk for the traditional open procedure. This selection bias may have affected the outcome of earlier studies. Therefore, the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial was designed to assess outcomes in patients deemed fit to undergo either open or endovascular repair. The study was conducted at 24 centers in the Netherlands and four centers in Belgium. Three hundred and forty-five patients had abdominal aortic aneurysms of at least 5 cm and were considered eligible for either open or endovascular repair. Patients were then randomized to undergo one procedure or the other.
Surgeons experienced in both endovascular and open repair performed the procedures. Primary outcomes were 30-day mortality (defined as death during the primary hospital admission or within 30 days), severe complications, and the combination of the two. The operative mortality rate was 4.6% in the open-repair group and 1.2% in the endovascular repair group, with a risk ratio of 3.9 (95% CI, 0.9-32.9). The combined endpoint of mortality and severe complication was 9.8% in the open-repair group and 4.7% in the endovascular repair group, with a risk ratio of 2.1 (95% CI, 0.9 to 5.4). It should be noted that 90% of study patients were men. These findings indicate that endovascular repair of aortic aneurysm results in less short-term morbidity and mortality than open repair. Larger studies with longer follow up are indicated.
7. Spargias K, Alexopoulos E, Kyrzopoulos S. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation.110(18)2837-42
In this study, a team of Greek researchers studied the use of vitamin C in patients with renal insufficiency (creatinine >1.2) undergoing coronary catheterization or intervention to determine if it prevented contrast-mediated nephropathy (CMN). Although the etiology of CMN is unknown, ischemic insults to the renal medulla and free radical release have been implicated. Since vitamin C has been shown in animal studies to attenuate nephropathy when administered with known renal toxins, a similar effect was postulated when administered with IV contrast.
Two hundred and twenty patients electively admitted for coronary catheterization or intervention were randomized to placebo or to receive 3 grams of vitamin C 2 hours prior to the dye load followed by 2 gm that night and the morning after. The two groups were balanced for presence of hypertension, diabetes, tobacco use, and use of commonly prescribed medications. Intravenous hydration was given to all at variable rates depending on left ventricular ejection fraction. The catheterization team chose the type of contrast agent. Creatinine was measured at baseline (up to 3 months prior to dye load) and 2-5 days afterwards. CMN was defined as a rise in total serum creatinine by 0.5 mg/dL or by 25%. Using these criteria, 9% of the vitamin C group developed CMN as opposed to 20% in the controls (NNT 9; 95% CI: 5-53). Logistical regression was performed to account for differences in age, initial serum creatinine, or both, and always yielded significant differences. The treatment group was slightly older, had higher rates of isoosmolar contrast administration (reno-protective), and had slightly higher baseline creatinines, so the true protective effect was thought even higher than reported.
This study is limited by small sample size, an overwhelmingly male patient base (90%), and the suspected presence of atherosclerotic heart disease in all patients. The amount and rate of delivery of contrast was not noted. The vitamin C preparation used was not described, implying that all preparations were bioequivalent. No mention was made of whether these results could be extrapolated to other procedures involving contrast. Given the low cost and high tolerability of vitamin C, however, further studies would certainly be welcome.
8. Yadav J, Wholey M, Kuntz R, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. NEJM.2004;351:1493-1501.
Carotid angioplasty has been available for the past decade, but, due to possible complications such as plaque embolization and stent compression, the procedure had been limited to patients unsuitable for surgical endarterectomy. Recently, the introduction of crush-resistant nitinol stents and emboli protection devices has made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year.
1. Annane D, Bellissant E, Briegel J, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and metaanalysis. BMJ. 2004;329:480.
Severe sepsis is a common cause of ICU admissions and continues to have mortality rates as high as 30%. As research has evolved, the role of corticosteroids in sepsis has changed. Annane and colleagues systematically reviewed corticosteroid treatment for severe sepsis and septic shock. The authors found 15 randomized trials that evaluated their main outcome of all-cause mortality at 28 days. When these results were pooled there was no significant improvement in mortality (RR 0.98; 0.87 to 1.10). However, the analysis showed very significant heterogeneity, so the authors appropriately performed a sensitivity analysis based on an a priori hypothesis that low-dose, long-course steroids (≤ 300 mg hydrocortisone/day and ≥ 5 days) would provide greater benefit than short-course, high-dose corticosteroids. The sensitivity analysis of five studies with low-dose, long-course corticosteroids showed a clear reduction in 28-day mortality (RR 0.80; 0.67 to 0.95) with no heterogeneity. There was no statistically significant difference in GI bleeds, superinfections, and hyperglycemia.
This is a very well-done review, which included an exhaustive search for all available evidence. The authors conclude based on the findings of an individual study in the review that patients with septic shock should undergo adrenal insufficiency testing prior to starting empiric therapy with low-dose hydrocortisone (200-300 mg/day). Hydrocortisone should then be stopped if there is no evidence of adrenal insufficiency. However, none of the studies in this review were limited to patients with adrenal insufficiency. Also, although none of the studies individually showed a statistically significant improvement with corticosteroids, they all favored the steroid treatment group with RRs < 1. Although there is good evidence that septic shock patients with adrenal insufficiency should be treated with corticosteroids, it remains unclear if therapy should be generalized to all septic patients. The ongoing European CORTICUS trial should help answer some of these questions.
2. Baddour L.,Yu, V. and the International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Resp Crit Care Med; 2004;170:440-444.
Three retrospective studies indicate that patients with pneumococcal bacteremia are less likely to die if treated with combination antibiotics. The combination of a beta-lactam and a macrolide appear to be especially protective. Based upon this soft data, multiple societies now recommend combination antibiotic therapy with a beta-lactam and a macrolide as first-line therapy for hospitalized patients with CAP. This large, multi-center, prospective observational study analyzed outcomes for all patients with pneumococcal bacteremia. Critically ill patients were eight times more likely to die than non-critically ill patients (mortality: 54.6% vs. 7.3%, p=0.0001). Combination therapy was defined as any two or more antibiotics used concurrently: multiple different regimens were used. The 14-day mortality difference between pneumococcal bacteremic patients receiving monotherapy vs. those receiving combination therapy was not significant (10.4 vs. 11.5%, p-value not disclosed) However, in critically ill patients, combination antibiotic therapy was associated with a marked decrease in mortality (23.4 vs. 55.3%, p=0.0015).
This study has significant limitations. It is not randomized, combination therapy was broadly defined as any two or more antibiotics, and 16% of critically ill patients received only one antibiotic, a major deviation from the standard of care. Nonetheless, this is the first prospective trial that attempts to ascertain which patients with pneumococcal bacteremia benefit from combination therapy. The marked mortality reduction in critically ill patients who received combination therapy reinforces the current recommendation that septic patients with pneumococcal bacteremia should receive combination therapy. However, these findings also underscore the fact that current guidelines for the treatment of an exceedingly common and serious disease are based upon weak retrospective data. Further randomized prospective trials are needed to determine which patients with pneumococcal pneumonia may actually benefit from combination antimicrobial therapy and what combination is most efficacious.
3. Fernandez-Avilles F, Alsonso J, Castro-Beivas A, et al, on behalf of the GRACIA (Grupo de Analisis de la Cardiopatio Isquemica Aguda) Group. Routine invasive strategy within 24 hours of thrombolysis versus ischemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1). Lancet;2004;364:045-1053
In the last ACC/AHA guidelines for acute myocardial infarction (1999), angioplasty soon after thrombolysis is strongly discouraged (class III) because studies to date showed no significant difference in outcomes and propensity for adverse events, i.e. bleeding. However, as stated in these last recommendations, the benefits of early post-thrombolysis percutaneous transluminal coronary angioplasty (PTCA) with stenting should be reassessed as interventional strategies mature. In the current era of stents and newer antiplatelet therapies, it looks as if now is the time to take another look.
The GRACIA-1 was a randomized, multi-centered trial to assess early intervention following thrombolysis in ST-elevation myocardial infarction (STEMI). Five hundred patients were enrolled and randomized to receive either fibrin-specific thrombolytics alone in the conservative group or thrombolysis combined with early PTCA. The primary endpoint was a combined rate of death, non-fatal reinfarction, or ischemia-induced revascularization at 1 year. Pre-discharge PTCA and stenting in those demonstrating recurrent ischemia in the conservative group (n=52) was analyzed as a secondary endpoint. One-year follow-up was completed in 98% of patients. Both groups had similar major cardiac events at 30 days, with the one-year endpoint demonstrating no difference in mortality. Significant differences were seen in the primary endpoint at one year [23 (9%) in the invasive group vs. 51 (21%) in the conservative group (RR-0.44, 95% CI 0.28-0.70 p=0.00008)].
A major limitation of this study was the low-risk profile of its patients, and the fact that it was not powered to differentiate between mortality and reinfarction. It will be interesting to see if these results are replicated in future studies (CARESS-2005) and their clinical impact on the management of acute myocardial infarction in centers without interventional support.
4. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med.2004;19:732-739.
Falls in hospital patients are common and persistent problems in hospitals across the country, with significant impact on patient safety, morbidity, and health care cost. Previous studies have reported up to 30% of inpatient falls result in injury, with 4-6% resulting in serious injury. Most studies on falls are retrospective reviews. This paper detailed a prospective observational study designed to identify and analyze the patient characteristics or the circumstances that contribute to falls. Using an online adverse event reporting system, patient falls were identified. Once identified, additional data sources, including the patients’ medical records, electronic nursing records, and interviews with patient or family members and nurses, were used to collect information. A total of 183 patients fell during the study period, with 85% of the falls occurring in the patient’s room.
Half of the falls involved bowel or bladder elimination and were more likely to occur in patients over 65 years in age (adjusted odds ratio 2.4; 95% confidence interval 1.1 to 5.3). Most of the falls (59%) occurred during the evening/overnight. 58% of the patients who fell had received agents with central nervous system activity in the 24 hours prior to a fall. 12% of the patients who fell received sedative-hypnotics. Repeat fallers were more likely to be men than women (11/86 [13%] vs 4/97 [4%]; p=0.03). 42% of the falls resulted in some type of injury, ranging from pain/swelling (34%) to cardiac arrest/death (0.5%). In multivariate analysis, only elimination-related falls remained a significant predictor of being injured from a fall (aOR , 2.4; 95% CI 1.1 to 5.3). Interestingly, patients who were confused or disoriented were less likely to be injured than alert and oriented patients (crude OR, 0.5; 95% CI, 0.3 to 0.98). When examined by services, medicine and neurology had the highest fall rate at 6.12 falls per 1000 patient days and had the highest patient-to-nurse ratio of 6.5 and 5.3, respectively.
While specific independent risk factors for prevention of falls could not be determined in this study due to a lack of a control group, their findings are consistent with previously identified risk factors for falling, including weakness, poor cognitive status including medication-related changes, and altered elimination. Potential interventions to prevent falls include toileting schedules for high-risk elderly patients and review of medication lists to minimize centrally acting, psychotropic, or sedating agents.
5. Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med; 2004;164:2044-2050
Elderly patients are increasingly likely to require long-term anticoagulation. Despite this, physicians often withhold long-term anticoagulation due to perceived risk factors for bleeding, including age, comorbidity, and cognitive or functional impairment.
This combination retrospective and prospective observational study evaluated the safety and quality of anticoagulation in elderly patients. Over a three-year span, 323 elderly patients were discharged on warfarin from a large Israeli hospital. These patients were frail and potentially “at risk”; 54% were older than age 80, 81% were uneducated, and 84% had low income. 47% were considered cognitively intact (according to MMSE) and only 34% were functionally independent. Using a multivariate analysis, the authors determined that only poor quality of anticoagulation education (OR: 8.83; 95% CI: 2.0-50.2), polypharmacy (OR: 6.14; 95% CI 1.2-42.4) and INR >3 (OR: 1.08; 95% CI 1.03-1.14) were associated with major bleeding.
This study of a “real world” population of frail, at-risk elderly patients provides important insights into risks for major bleeding resulting from warfarin therapy. Surprisingly, advanced age, cognitive impairment and markers for frailty did not confer elevated risk for major bleeding. Importantly, the study did not explicitly address patient fall risk, an often-cited reason for withholding anticoagulation therapy. Supratherapeutic anticoagulation is associated with a statistically but not clinically significant bleeding risk. Polypharmacy is increasingly unavoidable in elderly patients. However, appropriate anticoagulation therapy should be the standard of care. This study makes it clear that we need to focus our efforts on ensuring that elderly patients and their caregivers receive appropriate anticoagulation education prior to discharge from the hospital.
6. Prinssen M, Verhoeven E, Buth J, et al. A Randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607-18.
Endovascular repair of abdominal aortic aneurysm, which involves percutaneous introduction of a graft to bridge an aortic aneurysm, has been available since the early 1990s. This procedure was initially used in patients who were felt to be at high risk for the traditional open procedure. This selection bias may have affected the outcome of earlier studies. Therefore, the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial was designed to assess outcomes in patients deemed fit to undergo either open or endovascular repair. The study was conducted at 24 centers in the Netherlands and four centers in Belgium. Three hundred and forty-five patients had abdominal aortic aneurysms of at least 5 cm and were considered eligible for either open or endovascular repair. Patients were then randomized to undergo one procedure or the other.
Surgeons experienced in both endovascular and open repair performed the procedures. Primary outcomes were 30-day mortality (defined as death during the primary hospital admission or within 30 days), severe complications, and the combination of the two. The operative mortality rate was 4.6% in the open-repair group and 1.2% in the endovascular repair group, with a risk ratio of 3.9 (95% CI, 0.9-32.9). The combined endpoint of mortality and severe complication was 9.8% in the open-repair group and 4.7% in the endovascular repair group, with a risk ratio of 2.1 (95% CI, 0.9 to 5.4). It should be noted that 90% of study patients were men. These findings indicate that endovascular repair of aortic aneurysm results in less short-term morbidity and mortality than open repair. Larger studies with longer follow up are indicated.
7. Spargias K, Alexopoulos E, Kyrzopoulos S. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation.110(18)2837-42
In this study, a team of Greek researchers studied the use of vitamin C in patients with renal insufficiency (creatinine >1.2) undergoing coronary catheterization or intervention to determine if it prevented contrast-mediated nephropathy (CMN). Although the etiology of CMN is unknown, ischemic insults to the renal medulla and free radical release have been implicated. Since vitamin C has been shown in animal studies to attenuate nephropathy when administered with known renal toxins, a similar effect was postulated when administered with IV contrast.
Two hundred and twenty patients electively admitted for coronary catheterization or intervention were randomized to placebo or to receive 3 grams of vitamin C 2 hours prior to the dye load followed by 2 gm that night and the morning after. The two groups were balanced for presence of hypertension, diabetes, tobacco use, and use of commonly prescribed medications. Intravenous hydration was given to all at variable rates depending on left ventricular ejection fraction. The catheterization team chose the type of contrast agent. Creatinine was measured at baseline (up to 3 months prior to dye load) and 2-5 days afterwards. CMN was defined as a rise in total serum creatinine by 0.5 mg/dL or by 25%. Using these criteria, 9% of the vitamin C group developed CMN as opposed to 20% in the controls (NNT 9; 95% CI: 5-53). Logistical regression was performed to account for differences in age, initial serum creatinine, or both, and always yielded significant differences. The treatment group was slightly older, had higher rates of isoosmolar contrast administration (reno-protective), and had slightly higher baseline creatinines, so the true protective effect was thought even higher than reported.
This study is limited by small sample size, an overwhelmingly male patient base (90%), and the suspected presence of atherosclerotic heart disease in all patients. The amount and rate of delivery of contrast was not noted. The vitamin C preparation used was not described, implying that all preparations were bioequivalent. No mention was made of whether these results could be extrapolated to other procedures involving contrast. Given the low cost and high tolerability of vitamin C, however, further studies would certainly be welcome.
8. Yadav J, Wholey M, Kuntz R, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. NEJM.2004;351:1493-1501.
Carotid angioplasty has been available for the past decade, but, due to possible complications such as plaque embolization and stent compression, the procedure had been limited to patients unsuitable for surgical endarterectomy. Recently, the introduction of crush-resistant nitinol stents and emboli protection devices has made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year.
1. Annane D, Bellissant E, Briegel J, et al. Corticosteroids for severe sepsis and septic shock: a systematic review and metaanalysis. BMJ. 2004;329:480.
Severe sepsis is a common cause of ICU admissions and continues to have mortality rates as high as 30%. As research has evolved, the role of corticosteroids in sepsis has changed. Annane and colleagues systematically reviewed corticosteroid treatment for severe sepsis and septic shock. The authors found 15 randomized trials that evaluated their main outcome of all-cause mortality at 28 days. When these results were pooled there was no significant improvement in mortality (RR 0.98; 0.87 to 1.10). However, the analysis showed very significant heterogeneity, so the authors appropriately performed a sensitivity analysis based on an a priori hypothesis that low-dose, long-course steroids (≤ 300 mg hydrocortisone/day and ≥ 5 days) would provide greater benefit than short-course, high-dose corticosteroids. The sensitivity analysis of five studies with low-dose, long-course corticosteroids showed a clear reduction in 28-day mortality (RR 0.80; 0.67 to 0.95) with no heterogeneity. There was no statistically significant difference in GI bleeds, superinfections, and hyperglycemia.
This is a very well-done review, which included an exhaustive search for all available evidence. The authors conclude based on the findings of an individual study in the review that patients with septic shock should undergo adrenal insufficiency testing prior to starting empiric therapy with low-dose hydrocortisone (200-300 mg/day). Hydrocortisone should then be stopped if there is no evidence of adrenal insufficiency. However, none of the studies in this review were limited to patients with adrenal insufficiency. Also, although none of the studies individually showed a statistically significant improvement with corticosteroids, they all favored the steroid treatment group with RRs < 1. Although there is good evidence that septic shock patients with adrenal insufficiency should be treated with corticosteroids, it remains unclear if therapy should be generalized to all septic patients. The ongoing European CORTICUS trial should help answer some of these questions.
2. Baddour L.,Yu, V. and the International Pneumococcal Study Group. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Resp Crit Care Med; 2004;170:440-444.
Three retrospective studies indicate that patients with pneumococcal bacteremia are less likely to die if treated with combination antibiotics. The combination of a beta-lactam and a macrolide appear to be especially protective. Based upon this soft data, multiple societies now recommend combination antibiotic therapy with a beta-lactam and a macrolide as first-line therapy for hospitalized patients with CAP. This large, multi-center, prospective observational study analyzed outcomes for all patients with pneumococcal bacteremia. Critically ill patients were eight times more likely to die than non-critically ill patients (mortality: 54.6% vs. 7.3%, p=0.0001). Combination therapy was defined as any two or more antibiotics used concurrently: multiple different regimens were used. The 14-day mortality difference between pneumococcal bacteremic patients receiving monotherapy vs. those receiving combination therapy was not significant (10.4 vs. 11.5%, p-value not disclosed) However, in critically ill patients, combination antibiotic therapy was associated with a marked decrease in mortality (23.4 vs. 55.3%, p=0.0015).
This study has significant limitations. It is not randomized, combination therapy was broadly defined as any two or more antibiotics, and 16% of critically ill patients received only one antibiotic, a major deviation from the standard of care. Nonetheless, this is the first prospective trial that attempts to ascertain which patients with pneumococcal bacteremia benefit from combination therapy. The marked mortality reduction in critically ill patients who received combination therapy reinforces the current recommendation that septic patients with pneumococcal bacteremia should receive combination therapy. However, these findings also underscore the fact that current guidelines for the treatment of an exceedingly common and serious disease are based upon weak retrospective data. Further randomized prospective trials are needed to determine which patients with pneumococcal pneumonia may actually benefit from combination antimicrobial therapy and what combination is most efficacious.
3. Fernandez-Avilles F, Alsonso J, Castro-Beivas A, et al, on behalf of the GRACIA (Grupo de Analisis de la Cardiopatio Isquemica Aguda) Group. Routine invasive strategy within 24 hours of thrombolysis versus ischemia-guided conservative approach for acute myocardial infarction with ST-segment elevation (GRACIA-1). Lancet;2004;364:045-1053
In the last ACC/AHA guidelines for acute myocardial infarction (1999), angioplasty soon after thrombolysis is strongly discouraged (class III) because studies to date showed no significant difference in outcomes and propensity for adverse events, i.e. bleeding. However, as stated in these last recommendations, the benefits of early post-thrombolysis percutaneous transluminal coronary angioplasty (PTCA) with stenting should be reassessed as interventional strategies mature. In the current era of stents and newer antiplatelet therapies, it looks as if now is the time to take another look.
The GRACIA-1 was a randomized, multi-centered trial to assess early intervention following thrombolysis in ST-elevation myocardial infarction (STEMI). Five hundred patients were enrolled and randomized to receive either fibrin-specific thrombolytics alone in the conservative group or thrombolysis combined with early PTCA. The primary endpoint was a combined rate of death, non-fatal reinfarction, or ischemia-induced revascularization at 1 year. Pre-discharge PTCA and stenting in those demonstrating recurrent ischemia in the conservative group (n=52) was analyzed as a secondary endpoint. One-year follow-up was completed in 98% of patients. Both groups had similar major cardiac events at 30 days, with the one-year endpoint demonstrating no difference in mortality. Significant differences were seen in the primary endpoint at one year [23 (9%) in the invasive group vs. 51 (21%) in the conservative group (RR-0.44, 95% CI 0.28-0.70 p=0.00008)].
A major limitation of this study was the low-risk profile of its patients, and the fact that it was not powered to differentiate between mortality and reinfarction. It will be interesting to see if these results are replicated in future studies (CARESS-2005) and their clinical impact on the management of acute myocardial infarction in centers without interventional support.
4. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med.2004;19:732-739.
Falls in hospital patients are common and persistent problems in hospitals across the country, with significant impact on patient safety, morbidity, and health care cost. Previous studies have reported up to 30% of inpatient falls result in injury, with 4-6% resulting in serious injury. Most studies on falls are retrospective reviews. This paper detailed a prospective observational study designed to identify and analyze the patient characteristics or the circumstances that contribute to falls. Using an online adverse event reporting system, patient falls were identified. Once identified, additional data sources, including the patients’ medical records, electronic nursing records, and interviews with patient or family members and nurses, were used to collect information. A total of 183 patients fell during the study period, with 85% of the falls occurring in the patient’s room.
Half of the falls involved bowel or bladder elimination and were more likely to occur in patients over 65 years in age (adjusted odds ratio 2.4; 95% confidence interval 1.1 to 5.3). Most of the falls (59%) occurred during the evening/overnight. 58% of the patients who fell had received agents with central nervous system activity in the 24 hours prior to a fall. 12% of the patients who fell received sedative-hypnotics. Repeat fallers were more likely to be men than women (11/86 [13%] vs 4/97 [4%]; p=0.03). 42% of the falls resulted in some type of injury, ranging from pain/swelling (34%) to cardiac arrest/death (0.5%). In multivariate analysis, only elimination-related falls remained a significant predictor of being injured from a fall (aOR , 2.4; 95% CI 1.1 to 5.3). Interestingly, patients who were confused or disoriented were less likely to be injured than alert and oriented patients (crude OR, 0.5; 95% CI, 0.3 to 0.98). When examined by services, medicine and neurology had the highest fall rate at 6.12 falls per 1000 patient days and had the highest patient-to-nurse ratio of 6.5 and 5.3, respectively.
While specific independent risk factors for prevention of falls could not be determined in this study due to a lack of a control group, their findings are consistent with previously identified risk factors for falling, including weakness, poor cognitive status including medication-related changes, and altered elimination. Potential interventions to prevent falls include toileting schedules for high-risk elderly patients and review of medication lists to minimize centrally acting, psychotropic, or sedating agents.
5. Kagansky N, Knobler H, Rimon E, Ozer Z, Levy S. Safety of anticoagulation therapy in well-informed older patients. Arch Intern Med; 2004;164:2044-2050
Elderly patients are increasingly likely to require long-term anticoagulation. Despite this, physicians often withhold long-term anticoagulation due to perceived risk factors for bleeding, including age, comorbidity, and cognitive or functional impairment.
This combination retrospective and prospective observational study evaluated the safety and quality of anticoagulation in elderly patients. Over a three-year span, 323 elderly patients were discharged on warfarin from a large Israeli hospital. These patients were frail and potentially “at risk”; 54% were older than age 80, 81% were uneducated, and 84% had low income. 47% were considered cognitively intact (according to MMSE) and only 34% were functionally independent. Using a multivariate analysis, the authors determined that only poor quality of anticoagulation education (OR: 8.83; 95% CI: 2.0-50.2), polypharmacy (OR: 6.14; 95% CI 1.2-42.4) and INR >3 (OR: 1.08; 95% CI 1.03-1.14) were associated with major bleeding.
This study of a “real world” population of frail, at-risk elderly patients provides important insights into risks for major bleeding resulting from warfarin therapy. Surprisingly, advanced age, cognitive impairment and markers for frailty did not confer elevated risk for major bleeding. Importantly, the study did not explicitly address patient fall risk, an often-cited reason for withholding anticoagulation therapy. Supratherapeutic anticoagulation is associated with a statistically but not clinically significant bleeding risk. Polypharmacy is increasingly unavoidable in elderly patients. However, appropriate anticoagulation therapy should be the standard of care. This study makes it clear that we need to focus our efforts on ensuring that elderly patients and their caregivers receive appropriate anticoagulation education prior to discharge from the hospital.
6. Prinssen M, Verhoeven E, Buth J, et al. A Randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. NEJM. 2004;351:1607-18.
Endovascular repair of abdominal aortic aneurysm, which involves percutaneous introduction of a graft to bridge an aortic aneurysm, has been available since the early 1990s. This procedure was initially used in patients who were felt to be at high risk for the traditional open procedure. This selection bias may have affected the outcome of earlier studies. Therefore, the Dutch Randomized Endovascular Aneurysm Management (DREAM) trial was designed to assess outcomes in patients deemed fit to undergo either open or endovascular repair. The study was conducted at 24 centers in the Netherlands and four centers in Belgium. Three hundred and forty-five patients had abdominal aortic aneurysms of at least 5 cm and were considered eligible for either open or endovascular repair. Patients were then randomized to undergo one procedure or the other.
Surgeons experienced in both endovascular and open repair performed the procedures. Primary outcomes were 30-day mortality (defined as death during the primary hospital admission or within 30 days), severe complications, and the combination of the two. The operative mortality rate was 4.6% in the open-repair group and 1.2% in the endovascular repair group, with a risk ratio of 3.9 (95% CI, 0.9-32.9). The combined endpoint of mortality and severe complication was 9.8% in the open-repair group and 4.7% in the endovascular repair group, with a risk ratio of 2.1 (95% CI, 0.9 to 5.4). It should be noted that 90% of study patients were men. These findings indicate that endovascular repair of aortic aneurysm results in less short-term morbidity and mortality than open repair. Larger studies with longer follow up are indicated.
7. Spargias K, Alexopoulos E, Kyrzopoulos S. Ascorbic acid prevents contrast-mediated nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. Circulation.110(18)2837-42
In this study, a team of Greek researchers studied the use of vitamin C in patients with renal insufficiency (creatinine >1.2) undergoing coronary catheterization or intervention to determine if it prevented contrast-mediated nephropathy (CMN). Although the etiology of CMN is unknown, ischemic insults to the renal medulla and free radical release have been implicated. Since vitamin C has been shown in animal studies to attenuate nephropathy when administered with known renal toxins, a similar effect was postulated when administered with IV contrast.
Two hundred and twenty patients electively admitted for coronary catheterization or intervention were randomized to placebo or to receive 3 grams of vitamin C 2 hours prior to the dye load followed by 2 gm that night and the morning after. The two groups were balanced for presence of hypertension, diabetes, tobacco use, and use of commonly prescribed medications. Intravenous hydration was given to all at variable rates depending on left ventricular ejection fraction. The catheterization team chose the type of contrast agent. Creatinine was measured at baseline (up to 3 months prior to dye load) and 2-5 days afterwards. CMN was defined as a rise in total serum creatinine by 0.5 mg/dL or by 25%. Using these criteria, 9% of the vitamin C group developed CMN as opposed to 20% in the controls (NNT 9; 95% CI: 5-53). Logistical regression was performed to account for differences in age, initial serum creatinine, or both, and always yielded significant differences. The treatment group was slightly older, had higher rates of isoosmolar contrast administration (reno-protective), and had slightly higher baseline creatinines, so the true protective effect was thought even higher than reported.
This study is limited by small sample size, an overwhelmingly male patient base (90%), and the suspected presence of atherosclerotic heart disease in all patients. The amount and rate of delivery of contrast was not noted. The vitamin C preparation used was not described, implying that all preparations were bioequivalent. No mention was made of whether these results could be extrapolated to other procedures involving contrast. Given the low cost and high tolerability of vitamin C, however, further studies would certainly be welcome.
8. Yadav J, Wholey M, Kuntz R, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. NEJM.2004;351:1493-1501.
Carotid angioplasty has been available for the past decade, but, due to possible complications such as plaque embolization and stent compression, the procedure had been limited to patients unsuitable for surgical endarterectomy. Recently, the introduction of crush-resistant nitinol stents and emboli protection devices has made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year made the procedure safer. This study was designed to test the hypothesis that angioplasty and stenting is not inferior to endarterectomy. Three hundred and thirty-four patients at 29 centers had either a symptomatic carotid lesion greater than 50% or asymptomatic lesion greater than 80% and were deemed to be suitable candidates for either carotid endarterectomy or angioplasty. Patients were then randomized to one of the treatment groups. Surgeons, cardiologists, or interventional radiologists performed angioplasty. The primary endpoint was a composite of death, stroke, or MI within 30 days of the procedure, or death or stroke between 31 days and one year.
Secondary endpoints were the need for revascularization and cranial-nerve palsy at one year. During the first month after procedure, 4.8% of patients in the stent group and 9.8% of patients in the surgical group reached the primary endpoint. In the subsequent year, 12.2% of stent patients and 20.1% of surgical patients reached the primary endpoint (absolute risk reduction of 7.9, CI 0.7-16.4 and NNT 14). Cranial nerve palsy at one year was 0% vs. 4.9% in the stent vs. surgical group. Need for revascularization at one year was 0.6% vs. 4.3% for stent vs. surgical group. Although this study was designed to show the non-inferiority of angioplasty vs. carotid endarterectomy in patients deemed suitable for either procedure, it actually was statistically significant for superiority of stenting. It also implied a lower complication rate in terms of cranial nerve palsy and the need for revascularization at one year.
Education: Hospitalists Add Value to Formal and Informal Learning Processes
Type a medical condition or term into a search engine and watch what happens. A search on the words “diabetes” yields more than 13 million Web pages, and “pneumonia” produces another 1.65 million. In 1998, the Internet hosted approximately 5000 health-related Web sites; two years later that number quadrupled (1). Between 30,000 and 45,000 medical articles on various drug therapies are published annually. The Patent and Trademark Office issued between 2000 and 4200 drug patents each year between 1979 and 1989 (2). The National Library of Medicine reports that it adds more than 2000 journal article citations to its MEDLINE database on a daily basis. In 2003, more than 460,000 citations were entered.
Deciphering and applying this myriad of changing information is a critical activity in the medical field. Without disseminating new knowledge through ongoing education, medical practices and procedures would become outdated, and uninformed medical professionals and patients would continue to operate under misinformation that might be detrimental to health or worse.
Hospitalists as Inpatient Experts
In an inpatient setting, hospitalists are uniquely qualified to play the role of educator. They analyze and interpret a wide range of medical information to treat their patients and provide updated information to patients and their families, residents, interns, nursing staff, other health care professionals, and hospital administrators. The hospitalist can be viewed as the “hub” of educational activities in the inpatient environment, absorbing, synthesizing, and disseminating information. They are “inpatient experts” in the following five spheres of knowledge:
- patient management
- clinical knowledge
- clinical skills
- health care industry issues
- research and management/leadership (3)
Hospitalists are uniquely qualified in the sphere of patient management, efficiently and effectively guiding the patient through the mazelike inpatient environment. Most hospitalists are quite familiar with critical hospital functions and activities, including treatment in the emergency department, the admissions process, bedside care on the medical floor, treatment in the intensive care unit, and the discharge process. Hospitalists, because they understand “how to get things done” by ancillary departments, including diagnostic and therapeutic services, often find themselves as conductors of inpatient care. Many hospitalists have developed unique proficiency in co-managing surgical cases due to expertise in peri-operative evaluation and care. Hospitalists are recognized as inpatient team leaders, facilitating and coordinating a range of support services needed to treat the patient, including nursing, case management, pharmacy, occupational/physical therapy, and social work. Hospitalists must also be effective in managing relationships with health care personnel external to the inpatient environment, including community physicians, homecare providers, extended care facilities, and visiting nurse services. Finally, hospitalists are oaen well informed about hospital processes, procedures, rules, regulations, and information systems.
As inpatient generalists, hospitalists continually treat the most common reasons for admission and have exceptional clinical knowledge of these conditions. These conditions include pneumonia, deep vein thrombosis (DVT), congestive heart failure (CHF), diabetes, end-of-life care, and other medical diagnoses. Since they treat many elderly patients, hospitalists are considered experts in managing patients with multiple co-morbidities. A related area of expertise is clinical guidelines/pathways, quality of care metrics, and practice standards. Since they spend nearly all of their time treating inpatients, hospitalists develop extraordinary familiarity with the clinical rules and tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have the experience and expertise to teach inpatient clinical skills. These skills include diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination, and oversight. Also, most hospitalists are familiar with a range of technical procedures, including insertion of central lines and arterial lines, lumbar puncture, arthrocentesis, paracentesis, and thoracentesis.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of health care industry issues. These include comprehension of the payer/insurance regulations regarding medication formularies, utilization review requirements, and other care policies. Their expertise may extend to knowledge of state and federal regulations, public health initiatives, and recently enacted or pending health care legislation. Finally, hospitalists also are often conversant in the field of health care economics, especially regarding the financial impact on hospitals of reimbursement policies, legislative initiatives, technology, etc.
The fifth sphere of hospitalist expertise combines several knowledge domains. Individual hospitalists have specialized expertise in particular fields related to hospital medicine. Some hospitalists, mostly affiliated with academic institutions, are researchers who may develop research protocols, gather data, perform statistical analyses, and write papers that may potentially become the basis of improved patient care. Other hospitalists are exceptionally experienced in management/leadership. A hospitalist may be highly qualified to manage projects (e.g., computer-based physician order entry systems, throughput initiatives, etc.),or a hospitalist could be a strategic thinker who is viewed as a key clinical member of the hospital’s management team.
As a growing specialty, hospitalists have established a proficiency in a range of disciplines and intellectual domains. They are well positioned to assume the role of educator in the hospital environment. Given the exceptional knowledge and skills needed to be a hospitalist, the Society of Hospital Medicine (SHM) is pursing an effort to standardize education and lend greater credibility to the hospitalist profession. The “core curriculum” project is currently formalizing training that will provide a solid foundation for effective clinical practice in the field of hospital medicine.
Dual Educational Tracks
As depicted in Figure 1 below, medical education activity and the ways in which knowledge is imparted fall into two categories: formal and informal. Although some overlap may occur, there are distinct characteristics attributable to both classifications.
“Formal”
Formal education refers to the traditional “teacher-learner” roles in medicine. The learner can be a medical student, resident, or fellow. Education is typically transmitted from teacher to learner (as depicted in the diagram by a solid line), with some reciprocal feedback from the learner to the teacher (dotted line). It should be noted that as the importance and value of hospital medicine programs gain recognition, fellowship programs focusing on this specialty have been established. As of August 2004, eight active hospital medicine fellowship programs exist in the United States: three in California, two in Minnesota, and one each in Ohio, Illinois, and Texas. There are also pediatric hospital medicine fellowship programs in Boston, Washington DC, Houston, and San Diego. Each program enrolls one or two fellows annually (4).
Formal education can take place in both academic medical centers and community hospitals. By definition, academic medical centers provide supervised practical training for medical students, student nurses, and/or other health care professionals, as well as residents and fellows. In many academic medical centers throughout the country, hospitalists are emerging as core teachers of inpatient medicine. A prime example is the University of California, San Francisco. In 2002, 15 faculty hospitalists served as staff for approximately two-thirds of ward-attending months, as well as all medical consults (5).
By the same token, community hospitals that have residency programs also incorporate education to some degree into their daily operations. Today, medical education places a significant burden on residents and on the professionals charged with teaching students to absorb and understand vast amounts of science and medical information. On July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) revised the regulations governing the number of resident duty hours. These changes have forced residency programs to find viable options for imparting the required knowledge and hands-on experience to residents in fewer hours. Many consider hospitalists, by virtue of their “superior clinical and educational skills,” as representative of “the solution to the residency work duty problem.” In addition to providing excellence in teaching, hospitalists, known for their “superior clinical and educational skills,” may lead the way in creating and leading a clinical research agenda, which presents as the ultimate pedagogical experience (6).
In 2002, ACGME required six general competencies to be incorporated into residency curriculum and evaluation: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Hospitalists, because their practice already incorporates many aspects of these competencies, may be more effective at teaching these concepts to residents.
In the formal capacity of teacher, hospitalists can participate in attending/teaching rounds and in didactic patient-specific sessions presented in a case-based format, which provides residents with basic knowledge. As teaching supervisors, they can oversee the full range of clinical processes and procedures from the admission stage to post-discharge. Hospitalist teachers can also serve as mentors, providing a role model to residents who may be searching for direction regarding future plans. Through career counseling, hospitalists may steer learners into appropriate areas of study and training. Table 1 summarizes a series of research studies that document the positive impact hospitalists have achieved as educators in the academic environment.
Hospitalists may also have formal responsibility for developing curricula for learners in the academic environment. Whether the focus is on teaching medical students, residents, or hospitalist fellows, there is a need to determine the topics and material to be covered, incorporate them into a cogent curriculum, and update regularly to reflect the changing standards of care.
“Informal”
Informal education can be viewed as an exchange of information among stakeholders in the health care industry attempting to improve outcomes. Figure 1 depicts this as a two-way information exchange (solid arrows in both directions). As hospitalists impart knowledge to primary care physicians (PCPs), specialists/surgeons, other health care professionals (including nurses and pharmacists), patients, families, and hospital administrators, they reap benefits as well. These stakeholders stand to profit from the knowledge hospitalists can impart in daily interactions within the hospital and in less formal settings.
By working together with nurses, emergency room physicians, medical specialists, and PCPs, hospitalists can help achieve efficient and effective processes of care. The use of available software programs enables health care professionals to cooperatively exchange reliable information regarding patient management. Ongoing conversations regarding diagnoses, treatment, medications, and procedures serve to keep each member of the team educated and informed, thus ensuring more efficient delivery of care (12).
Alpesh Amin, MD, executive director of the hospitalist program at the University of California, Irvine, and chair of SHM’s Education Committee, points out that hospitalists frequently have opportunities to act as educators during case-by-case interactions with PCPs and other health care providers. “Every time you talk to a doctor about admitting or discharging a patient, it’s an opportunity to educate,” he says. In addition, “the hospitalist can apply and/or develop critical pathways and algorithms to educate others.” In the course of managing care, criteria can be developed for previously unaddressed medical issues.
This same opportunity for education extends to the hospital floor where team building serves to enlighten each member of the group providing patient care. In a reciprocal environment, both hospitalists and their medical professional “teammates” benefit from each other’s knowledge. Amin points out that specialists typically focus on one condition, while hospitalists consider the entire patient. By openly receiving the specialist’s input and advice, processing it, and then applying it to the patient, the hospitalist can develop a comprehensive approach to disease management. By considering co-morbidities and long-term care, the health care team should base decisions on “patient-centered education (13).”
Hospitalists can initiate informal in-house educational outreach, such as informational programs about medical breakthroughs, new medications, explanations of existing medical legislation, and other relevant topics. These programs can enlighten nurses, case managers, pharmacists, and other health care professionals about issues important to managing patients and/or achieving quality outcomes. The format for these programs may be one-on-one interactions (either in-person or by telephone) relating to one specific patient; formal in-service lectures; “Lunch and Learns”; pharmaceutically funded drug- or-disease-management seminars; committee or departmental meetings, and/or random written communications (sent electronically or by interoffice mail) that incorporate history and physical findings, consultations, discharge summaries, or hard-copy articles (12).
Conclusion
Because they spend so much time in the hospital, hospitalists are experts on all aspects of inpatient care: clinical, administrative, patient flow, and health care industry issues. Published research shows that academic institutions that employ hospitalists will have more satisfied and better-educated students. Common sense suggests that nurses and other stakeholders who work with hospitalists will be more informed and better-educated team members in the patient care process. Hospitalists can be the key ingredient and centerpiece in effective inpatient medical education.
References
- Yale New Haven Hospital Report, March 2004.
- Ward, Michael R. “Drug approval overregulation.” Regulation: the Review of Business and Government. Cato Institute, September 27, 2004.
- Pak, MH. Associate Professor of Medicine, Hospitalist, Director, General Medicine Consultation Service, University of Wisconsin School of Medicine, Madison, WI.
- Ranji S, Rosenman D. “Hospital medicine fellowship update.” The Hospitalist. 2004; 8 (5): 39.
- Wachter RM, Goldman L. “The hospitalist movement five years later.” JAMA.2002; 287(4): 487-94.
- Saint S, Flanders SA. “Hospitalists in teaching hospitals: opportunities but not without danger.” J Gen Intern Med. 2004; 19: 392-3.
- Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. “Resident satisfaction on an academic hospitalist service: time to teach.” Am J Med. 2002; 112: 597-601.
- Landrigan CP, Muret-Wagstaff S, Chiang VW, Nigrin DJ, Goldmann DA, Finkelstein JA. “Effect of a pediatric hospitalist system on housestaff education and experience.” Arch Ped Adoles Med. 2002; 156 (9): 877-83.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. “Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations.” Acad Med. 2004; 79:78-82.
- 10. Kulaga, ME. “The positive impact of initiation of hospitalist clinician educators.” J Gen Intern Med.2004; 19(4): 293-301.
- Hauer K, Wachter R, McCulloch C, Woo G, Auerbach A. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004; 164: 1866-71.
- Jones T, DO. Director of Medical Affairs, IPC, The Hospitalist Company, Mesa, AZ.
- Amin A, MD, MBA, FACP, executive director, Hospitalist Program, University of California, Irvine. Chair, Education Committee, Society of Hospital Medicine. Personal interview. October 7, 2004.
Type a medical condition or term into a search engine and watch what happens. A search on the words “diabetes” yields more than 13 million Web pages, and “pneumonia” produces another 1.65 million. In 1998, the Internet hosted approximately 5000 health-related Web sites; two years later that number quadrupled (1). Between 30,000 and 45,000 medical articles on various drug therapies are published annually. The Patent and Trademark Office issued between 2000 and 4200 drug patents each year between 1979 and 1989 (2). The National Library of Medicine reports that it adds more than 2000 journal article citations to its MEDLINE database on a daily basis. In 2003, more than 460,000 citations were entered.
Deciphering and applying this myriad of changing information is a critical activity in the medical field. Without disseminating new knowledge through ongoing education, medical practices and procedures would become outdated, and uninformed medical professionals and patients would continue to operate under misinformation that might be detrimental to health or worse.
Hospitalists as Inpatient Experts
In an inpatient setting, hospitalists are uniquely qualified to play the role of educator. They analyze and interpret a wide range of medical information to treat their patients and provide updated information to patients and their families, residents, interns, nursing staff, other health care professionals, and hospital administrators. The hospitalist can be viewed as the “hub” of educational activities in the inpatient environment, absorbing, synthesizing, and disseminating information. They are “inpatient experts” in the following five spheres of knowledge:
- patient management
- clinical knowledge
- clinical skills
- health care industry issues
- research and management/leadership (3)
Hospitalists are uniquely qualified in the sphere of patient management, efficiently and effectively guiding the patient through the mazelike inpatient environment. Most hospitalists are quite familiar with critical hospital functions and activities, including treatment in the emergency department, the admissions process, bedside care on the medical floor, treatment in the intensive care unit, and the discharge process. Hospitalists, because they understand “how to get things done” by ancillary departments, including diagnostic and therapeutic services, often find themselves as conductors of inpatient care. Many hospitalists have developed unique proficiency in co-managing surgical cases due to expertise in peri-operative evaluation and care. Hospitalists are recognized as inpatient team leaders, facilitating and coordinating a range of support services needed to treat the patient, including nursing, case management, pharmacy, occupational/physical therapy, and social work. Hospitalists must also be effective in managing relationships with health care personnel external to the inpatient environment, including community physicians, homecare providers, extended care facilities, and visiting nurse services. Finally, hospitalists are oaen well informed about hospital processes, procedures, rules, regulations, and information systems.
As inpatient generalists, hospitalists continually treat the most common reasons for admission and have exceptional clinical knowledge of these conditions. These conditions include pneumonia, deep vein thrombosis (DVT), congestive heart failure (CHF), diabetes, end-of-life care, and other medical diagnoses. Since they treat many elderly patients, hospitalists are considered experts in managing patients with multiple co-morbidities. A related area of expertise is clinical guidelines/pathways, quality of care metrics, and practice standards. Since they spend nearly all of their time treating inpatients, hospitalists develop extraordinary familiarity with the clinical rules and tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have the experience and expertise to teach inpatient clinical skills. These skills include diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination, and oversight. Also, most hospitalists are familiar with a range of technical procedures, including insertion of central lines and arterial lines, lumbar puncture, arthrocentesis, paracentesis, and thoracentesis.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of health care industry issues. These include comprehension of the payer/insurance regulations regarding medication formularies, utilization review requirements, and other care policies. Their expertise may extend to knowledge of state and federal regulations, public health initiatives, and recently enacted or pending health care legislation. Finally, hospitalists also are often conversant in the field of health care economics, especially regarding the financial impact on hospitals of reimbursement policies, legislative initiatives, technology, etc.
The fifth sphere of hospitalist expertise combines several knowledge domains. Individual hospitalists have specialized expertise in particular fields related to hospital medicine. Some hospitalists, mostly affiliated with academic institutions, are researchers who may develop research protocols, gather data, perform statistical analyses, and write papers that may potentially become the basis of improved patient care. Other hospitalists are exceptionally experienced in management/leadership. A hospitalist may be highly qualified to manage projects (e.g., computer-based physician order entry systems, throughput initiatives, etc.),or a hospitalist could be a strategic thinker who is viewed as a key clinical member of the hospital’s management team.
As a growing specialty, hospitalists have established a proficiency in a range of disciplines and intellectual domains. They are well positioned to assume the role of educator in the hospital environment. Given the exceptional knowledge and skills needed to be a hospitalist, the Society of Hospital Medicine (SHM) is pursing an effort to standardize education and lend greater credibility to the hospitalist profession. The “core curriculum” project is currently formalizing training that will provide a solid foundation for effective clinical practice in the field of hospital medicine.
Dual Educational Tracks
As depicted in Figure 1 below, medical education activity and the ways in which knowledge is imparted fall into two categories: formal and informal. Although some overlap may occur, there are distinct characteristics attributable to both classifications.
“Formal”
Formal education refers to the traditional “teacher-learner” roles in medicine. The learner can be a medical student, resident, or fellow. Education is typically transmitted from teacher to learner (as depicted in the diagram by a solid line), with some reciprocal feedback from the learner to the teacher (dotted line). It should be noted that as the importance and value of hospital medicine programs gain recognition, fellowship programs focusing on this specialty have been established. As of August 2004, eight active hospital medicine fellowship programs exist in the United States: three in California, two in Minnesota, and one each in Ohio, Illinois, and Texas. There are also pediatric hospital medicine fellowship programs in Boston, Washington DC, Houston, and San Diego. Each program enrolls one or two fellows annually (4).
Formal education can take place in both academic medical centers and community hospitals. By definition, academic medical centers provide supervised practical training for medical students, student nurses, and/or other health care professionals, as well as residents and fellows. In many academic medical centers throughout the country, hospitalists are emerging as core teachers of inpatient medicine. A prime example is the University of California, San Francisco. In 2002, 15 faculty hospitalists served as staff for approximately two-thirds of ward-attending months, as well as all medical consults (5).
By the same token, community hospitals that have residency programs also incorporate education to some degree into their daily operations. Today, medical education places a significant burden on residents and on the professionals charged with teaching students to absorb and understand vast amounts of science and medical information. On July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) revised the regulations governing the number of resident duty hours. These changes have forced residency programs to find viable options for imparting the required knowledge and hands-on experience to residents in fewer hours. Many consider hospitalists, by virtue of their “superior clinical and educational skills,” as representative of “the solution to the residency work duty problem.” In addition to providing excellence in teaching, hospitalists, known for their “superior clinical and educational skills,” may lead the way in creating and leading a clinical research agenda, which presents as the ultimate pedagogical experience (6).
In 2002, ACGME required six general competencies to be incorporated into residency curriculum and evaluation: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Hospitalists, because their practice already incorporates many aspects of these competencies, may be more effective at teaching these concepts to residents.
In the formal capacity of teacher, hospitalists can participate in attending/teaching rounds and in didactic patient-specific sessions presented in a case-based format, which provides residents with basic knowledge. As teaching supervisors, they can oversee the full range of clinical processes and procedures from the admission stage to post-discharge. Hospitalist teachers can also serve as mentors, providing a role model to residents who may be searching for direction regarding future plans. Through career counseling, hospitalists may steer learners into appropriate areas of study and training. Table 1 summarizes a series of research studies that document the positive impact hospitalists have achieved as educators in the academic environment.
Hospitalists may also have formal responsibility for developing curricula for learners in the academic environment. Whether the focus is on teaching medical students, residents, or hospitalist fellows, there is a need to determine the topics and material to be covered, incorporate them into a cogent curriculum, and update regularly to reflect the changing standards of care.
“Informal”
Informal education can be viewed as an exchange of information among stakeholders in the health care industry attempting to improve outcomes. Figure 1 depicts this as a two-way information exchange (solid arrows in both directions). As hospitalists impart knowledge to primary care physicians (PCPs), specialists/surgeons, other health care professionals (including nurses and pharmacists), patients, families, and hospital administrators, they reap benefits as well. These stakeholders stand to profit from the knowledge hospitalists can impart in daily interactions within the hospital and in less formal settings.
By working together with nurses, emergency room physicians, medical specialists, and PCPs, hospitalists can help achieve efficient and effective processes of care. The use of available software programs enables health care professionals to cooperatively exchange reliable information regarding patient management. Ongoing conversations regarding diagnoses, treatment, medications, and procedures serve to keep each member of the team educated and informed, thus ensuring more efficient delivery of care (12).
Alpesh Amin, MD, executive director of the hospitalist program at the University of California, Irvine, and chair of SHM’s Education Committee, points out that hospitalists frequently have opportunities to act as educators during case-by-case interactions with PCPs and other health care providers. “Every time you talk to a doctor about admitting or discharging a patient, it’s an opportunity to educate,” he says. In addition, “the hospitalist can apply and/or develop critical pathways and algorithms to educate others.” In the course of managing care, criteria can be developed for previously unaddressed medical issues.
This same opportunity for education extends to the hospital floor where team building serves to enlighten each member of the group providing patient care. In a reciprocal environment, both hospitalists and their medical professional “teammates” benefit from each other’s knowledge. Amin points out that specialists typically focus on one condition, while hospitalists consider the entire patient. By openly receiving the specialist’s input and advice, processing it, and then applying it to the patient, the hospitalist can develop a comprehensive approach to disease management. By considering co-morbidities and long-term care, the health care team should base decisions on “patient-centered education (13).”
Hospitalists can initiate informal in-house educational outreach, such as informational programs about medical breakthroughs, new medications, explanations of existing medical legislation, and other relevant topics. These programs can enlighten nurses, case managers, pharmacists, and other health care professionals about issues important to managing patients and/or achieving quality outcomes. The format for these programs may be one-on-one interactions (either in-person or by telephone) relating to one specific patient; formal in-service lectures; “Lunch and Learns”; pharmaceutically funded drug- or-disease-management seminars; committee or departmental meetings, and/or random written communications (sent electronically or by interoffice mail) that incorporate history and physical findings, consultations, discharge summaries, or hard-copy articles (12).
Conclusion
Because they spend so much time in the hospital, hospitalists are experts on all aspects of inpatient care: clinical, administrative, patient flow, and health care industry issues. Published research shows that academic institutions that employ hospitalists will have more satisfied and better-educated students. Common sense suggests that nurses and other stakeholders who work with hospitalists will be more informed and better-educated team members in the patient care process. Hospitalists can be the key ingredient and centerpiece in effective inpatient medical education.
References
- Yale New Haven Hospital Report, March 2004.
- Ward, Michael R. “Drug approval overregulation.” Regulation: the Review of Business and Government. Cato Institute, September 27, 2004.
- Pak, MH. Associate Professor of Medicine, Hospitalist, Director, General Medicine Consultation Service, University of Wisconsin School of Medicine, Madison, WI.
- Ranji S, Rosenman D. “Hospital medicine fellowship update.” The Hospitalist. 2004; 8 (5): 39.
- Wachter RM, Goldman L. “The hospitalist movement five years later.” JAMA.2002; 287(4): 487-94.
- Saint S, Flanders SA. “Hospitalists in teaching hospitals: opportunities but not without danger.” J Gen Intern Med. 2004; 19: 392-3.
- Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. “Resident satisfaction on an academic hospitalist service: time to teach.” Am J Med. 2002; 112: 597-601.
- Landrigan CP, Muret-Wagstaff S, Chiang VW, Nigrin DJ, Goldmann DA, Finkelstein JA. “Effect of a pediatric hospitalist system on housestaff education and experience.” Arch Ped Adoles Med. 2002; 156 (9): 877-83.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. “Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations.” Acad Med. 2004; 79:78-82.
- 10. Kulaga, ME. “The positive impact of initiation of hospitalist clinician educators.” J Gen Intern Med.2004; 19(4): 293-301.
- Hauer K, Wachter R, McCulloch C, Woo G, Auerbach A. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004; 164: 1866-71.
- Jones T, DO. Director of Medical Affairs, IPC, The Hospitalist Company, Mesa, AZ.
- Amin A, MD, MBA, FACP, executive director, Hospitalist Program, University of California, Irvine. Chair, Education Committee, Society of Hospital Medicine. Personal interview. October 7, 2004.
Type a medical condition or term into a search engine and watch what happens. A search on the words “diabetes” yields more than 13 million Web pages, and “pneumonia” produces another 1.65 million. In 1998, the Internet hosted approximately 5000 health-related Web sites; two years later that number quadrupled (1). Between 30,000 and 45,000 medical articles on various drug therapies are published annually. The Patent and Trademark Office issued between 2000 and 4200 drug patents each year between 1979 and 1989 (2). The National Library of Medicine reports that it adds more than 2000 journal article citations to its MEDLINE database on a daily basis. In 2003, more than 460,000 citations were entered.
Deciphering and applying this myriad of changing information is a critical activity in the medical field. Without disseminating new knowledge through ongoing education, medical practices and procedures would become outdated, and uninformed medical professionals and patients would continue to operate under misinformation that might be detrimental to health or worse.
Hospitalists as Inpatient Experts
In an inpatient setting, hospitalists are uniquely qualified to play the role of educator. They analyze and interpret a wide range of medical information to treat their patients and provide updated information to patients and their families, residents, interns, nursing staff, other health care professionals, and hospital administrators. The hospitalist can be viewed as the “hub” of educational activities in the inpatient environment, absorbing, synthesizing, and disseminating information. They are “inpatient experts” in the following five spheres of knowledge:
- patient management
- clinical knowledge
- clinical skills
- health care industry issues
- research and management/leadership (3)
Hospitalists are uniquely qualified in the sphere of patient management, efficiently and effectively guiding the patient through the mazelike inpatient environment. Most hospitalists are quite familiar with critical hospital functions and activities, including treatment in the emergency department, the admissions process, bedside care on the medical floor, treatment in the intensive care unit, and the discharge process. Hospitalists, because they understand “how to get things done” by ancillary departments, including diagnostic and therapeutic services, often find themselves as conductors of inpatient care. Many hospitalists have developed unique proficiency in co-managing surgical cases due to expertise in peri-operative evaluation and care. Hospitalists are recognized as inpatient team leaders, facilitating and coordinating a range of support services needed to treat the patient, including nursing, case management, pharmacy, occupational/physical therapy, and social work. Hospitalists must also be effective in managing relationships with health care personnel external to the inpatient environment, including community physicians, homecare providers, extended care facilities, and visiting nurse services. Finally, hospitalists are oaen well informed about hospital processes, procedures, rules, regulations, and information systems.
As inpatient generalists, hospitalists continually treat the most common reasons for admission and have exceptional clinical knowledge of these conditions. These conditions include pneumonia, deep vein thrombosis (DVT), congestive heart failure (CHF), diabetes, end-of-life care, and other medical diagnoses. Since they treat many elderly patients, hospitalists are considered experts in managing patients with multiple co-morbidities. A related area of expertise is clinical guidelines/pathways, quality of care metrics, and practice standards. Since they spend nearly all of their time treating inpatients, hospitalists develop extraordinary familiarity with the clinical rules and tools supporting the patient care process.
In addition to clinical knowledge, hospitalists have the experience and expertise to teach inpatient clinical skills. These skills include diagnosis, physical examination, discharge planning, medical chart recording, family meeting coordination, and oversight. Also, most hospitalists are familiar with a range of technical procedures, including insertion of central lines and arterial lines, lumbar puncture, arthrocentesis, paracentesis, and thoracentesis.
Hospitalists often are the most knowledgeable inpatient clinicians with regard to a wide range of health care industry issues. These include comprehension of the payer/insurance regulations regarding medication formularies, utilization review requirements, and other care policies. Their expertise may extend to knowledge of state and federal regulations, public health initiatives, and recently enacted or pending health care legislation. Finally, hospitalists also are often conversant in the field of health care economics, especially regarding the financial impact on hospitals of reimbursement policies, legislative initiatives, technology, etc.
The fifth sphere of hospitalist expertise combines several knowledge domains. Individual hospitalists have specialized expertise in particular fields related to hospital medicine. Some hospitalists, mostly affiliated with academic institutions, are researchers who may develop research protocols, gather data, perform statistical analyses, and write papers that may potentially become the basis of improved patient care. Other hospitalists are exceptionally experienced in management/leadership. A hospitalist may be highly qualified to manage projects (e.g., computer-based physician order entry systems, throughput initiatives, etc.),or a hospitalist could be a strategic thinker who is viewed as a key clinical member of the hospital’s management team.
As a growing specialty, hospitalists have established a proficiency in a range of disciplines and intellectual domains. They are well positioned to assume the role of educator in the hospital environment. Given the exceptional knowledge and skills needed to be a hospitalist, the Society of Hospital Medicine (SHM) is pursing an effort to standardize education and lend greater credibility to the hospitalist profession. The “core curriculum” project is currently formalizing training that will provide a solid foundation for effective clinical practice in the field of hospital medicine.
Dual Educational Tracks
As depicted in Figure 1 below, medical education activity and the ways in which knowledge is imparted fall into two categories: formal and informal. Although some overlap may occur, there are distinct characteristics attributable to both classifications.
“Formal”
Formal education refers to the traditional “teacher-learner” roles in medicine. The learner can be a medical student, resident, or fellow. Education is typically transmitted from teacher to learner (as depicted in the diagram by a solid line), with some reciprocal feedback from the learner to the teacher (dotted line). It should be noted that as the importance and value of hospital medicine programs gain recognition, fellowship programs focusing on this specialty have been established. As of August 2004, eight active hospital medicine fellowship programs exist in the United States: three in California, two in Minnesota, and one each in Ohio, Illinois, and Texas. There are also pediatric hospital medicine fellowship programs in Boston, Washington DC, Houston, and San Diego. Each program enrolls one or two fellows annually (4).
Formal education can take place in both academic medical centers and community hospitals. By definition, academic medical centers provide supervised practical training for medical students, student nurses, and/or other health care professionals, as well as residents and fellows. In many academic medical centers throughout the country, hospitalists are emerging as core teachers of inpatient medicine. A prime example is the University of California, San Francisco. In 2002, 15 faculty hospitalists served as staff for approximately two-thirds of ward-attending months, as well as all medical consults (5).
By the same token, community hospitals that have residency programs also incorporate education to some degree into their daily operations. Today, medical education places a significant burden on residents and on the professionals charged with teaching students to absorb and understand vast amounts of science and medical information. On July 1, 2003, the Accreditation Council for Graduate Medical Education (ACGME) revised the regulations governing the number of resident duty hours. These changes have forced residency programs to find viable options for imparting the required knowledge and hands-on experience to residents in fewer hours. Many consider hospitalists, by virtue of their “superior clinical and educational skills,” as representative of “the solution to the residency work duty problem.” In addition to providing excellence in teaching, hospitalists, known for their “superior clinical and educational skills,” may lead the way in creating and leading a clinical research agenda, which presents as the ultimate pedagogical experience (6).
In 2002, ACGME required six general competencies to be incorporated into residency curriculum and evaluation: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice. Hospitalists, because their practice already incorporates many aspects of these competencies, may be more effective at teaching these concepts to residents.
In the formal capacity of teacher, hospitalists can participate in attending/teaching rounds and in didactic patient-specific sessions presented in a case-based format, which provides residents with basic knowledge. As teaching supervisors, they can oversee the full range of clinical processes and procedures from the admission stage to post-discharge. Hospitalist teachers can also serve as mentors, providing a role model to residents who may be searching for direction regarding future plans. Through career counseling, hospitalists may steer learners into appropriate areas of study and training. Table 1 summarizes a series of research studies that document the positive impact hospitalists have achieved as educators in the academic environment.
Hospitalists may also have formal responsibility for developing curricula for learners in the academic environment. Whether the focus is on teaching medical students, residents, or hospitalist fellows, there is a need to determine the topics and material to be covered, incorporate them into a cogent curriculum, and update regularly to reflect the changing standards of care.
“Informal”
Informal education can be viewed as an exchange of information among stakeholders in the health care industry attempting to improve outcomes. Figure 1 depicts this as a two-way information exchange (solid arrows in both directions). As hospitalists impart knowledge to primary care physicians (PCPs), specialists/surgeons, other health care professionals (including nurses and pharmacists), patients, families, and hospital administrators, they reap benefits as well. These stakeholders stand to profit from the knowledge hospitalists can impart in daily interactions within the hospital and in less formal settings.
By working together with nurses, emergency room physicians, medical specialists, and PCPs, hospitalists can help achieve efficient and effective processes of care. The use of available software programs enables health care professionals to cooperatively exchange reliable information regarding patient management. Ongoing conversations regarding diagnoses, treatment, medications, and procedures serve to keep each member of the team educated and informed, thus ensuring more efficient delivery of care (12).
Alpesh Amin, MD, executive director of the hospitalist program at the University of California, Irvine, and chair of SHM’s Education Committee, points out that hospitalists frequently have opportunities to act as educators during case-by-case interactions with PCPs and other health care providers. “Every time you talk to a doctor about admitting or discharging a patient, it’s an opportunity to educate,” he says. In addition, “the hospitalist can apply and/or develop critical pathways and algorithms to educate others.” In the course of managing care, criteria can be developed for previously unaddressed medical issues.
This same opportunity for education extends to the hospital floor where team building serves to enlighten each member of the group providing patient care. In a reciprocal environment, both hospitalists and their medical professional “teammates” benefit from each other’s knowledge. Amin points out that specialists typically focus on one condition, while hospitalists consider the entire patient. By openly receiving the specialist’s input and advice, processing it, and then applying it to the patient, the hospitalist can develop a comprehensive approach to disease management. By considering co-morbidities and long-term care, the health care team should base decisions on “patient-centered education (13).”
Hospitalists can initiate informal in-house educational outreach, such as informational programs about medical breakthroughs, new medications, explanations of existing medical legislation, and other relevant topics. These programs can enlighten nurses, case managers, pharmacists, and other health care professionals about issues important to managing patients and/or achieving quality outcomes. The format for these programs may be one-on-one interactions (either in-person or by telephone) relating to one specific patient; formal in-service lectures; “Lunch and Learns”; pharmaceutically funded drug- or-disease-management seminars; committee or departmental meetings, and/or random written communications (sent electronically or by interoffice mail) that incorporate history and physical findings, consultations, discharge summaries, or hard-copy articles (12).
Conclusion
Because they spend so much time in the hospital, hospitalists are experts on all aspects of inpatient care: clinical, administrative, patient flow, and health care industry issues. Published research shows that academic institutions that employ hospitalists will have more satisfied and better-educated students. Common sense suggests that nurses and other stakeholders who work with hospitalists will be more informed and better-educated team members in the patient care process. Hospitalists can be the key ingredient and centerpiece in effective inpatient medical education.
References
- Yale New Haven Hospital Report, March 2004.
- Ward, Michael R. “Drug approval overregulation.” Regulation: the Review of Business and Government. Cato Institute, September 27, 2004.
- Pak, MH. Associate Professor of Medicine, Hospitalist, Director, General Medicine Consultation Service, University of Wisconsin School of Medicine, Madison, WI.
- Ranji S, Rosenman D. “Hospital medicine fellowship update.” The Hospitalist. 2004; 8 (5): 39.
- Wachter RM, Goldman L. “The hospitalist movement five years later.” JAMA.2002; 287(4): 487-94.
- Saint S, Flanders SA. “Hospitalists in teaching hospitals: opportunities but not without danger.” J Gen Intern Med. 2004; 19: 392-3.
- Chung P, Morrison J, Jin L, Levinson W, Humphrey H, Meltzer D. “Resident satisfaction on an academic hospitalist service: time to teach.” Am J Med. 2002; 112: 597-601.
- Landrigan CP, Muret-Wagstaff S, Chiang VW, Nigrin DJ, Goldmann DA, Finkelstein JA. “Effect of a pediatric hospitalist system on housestaff education and experience.” Arch Ped Adoles Med. 2002; 156 (9): 877-83.
- Hunter AJ, Desai SS, Harrison RA, Chan BK. “Medical student evaluation of the quality of hospitalist and non-hospitalist teaching faculty on inpatient medicine rotations.” Acad Med. 2004; 79:78-82.
- 10. Kulaga, ME. “The positive impact of initiation of hospitalist clinician educators.” J Gen Intern Med.2004; 19(4): 293-301.
- Hauer K, Wachter R, McCulloch C, Woo G, Auerbach A. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004; 164: 1866-71.
- Jones T, DO. Director of Medical Affairs, IPC, The Hospitalist Company, Mesa, AZ.
- Amin A, MD, MBA, FACP, executive director, Hospitalist Program, University of California, Irvine. Chair, Education Committee, Society of Hospital Medicine. Personal interview. October 7, 2004.