User login
The Challenge of Surgeon Self-Improvement
At the end of a journey 3,650 days long, there is a path leading into the wilderness. From the first day of medical school until the last day of fellowship, we safely follow the well-paved and often-traveled road of medical education with its preset and regimented responsibilities, objectives, and milestones. We become comfortable in the academic routine of newly prescribed goals and responsibilities every year of training. We continually push forward with the stated desire of completing our education, beginning our dream job, and discovering our personas as physicians and human beings along the way. Balance, while an ideal to aspire to, is often put aside for the perceived greater glory of practical knowledge, competition, and the finish line. The assumption all along is that happiness is preordained by this path. However, when the routine comes to an end and we take our first steps into life as an attending surgeon, we can come face to face with an inexplicable void.
It is often said that the best period of training is the first years of practice. We spend those initial years drinking from the fire hose that is the attending surgeon learning curve, but that learning curve often too quickly plateaus. We can be paralyzed by the uncertainty of what the future may bring and of our roles in it. At that moment we have a profound new choice to make: to relish the freedom to reinvent ourselves and create new adventures, or to succumb to the unhealthy temptations and outside influences that abound. Bad decisions are inevitable if we never spend any time reflecting on what actually makes us happy. The sesquipedalian prose of self-improvement books often belabors the fact that we are all at risk of becoming clichés. To fight the cliché, we believe the essence of healthy success in practice after training lies in 3 principles: reinvention, passion, and inspiration. The rest is filler.
Reinvent yourself within medicine. As physicians, part of our identities is built upon our abilities to compassionately care for patients and effectively treat disease. However, the vast majority of procedures and skills we acquire during training will be obsolete in a decade or less. Therefore, it is imperative that we change with time, or else we will become stagnant. If we choose to compare ourselves only to those around us and similar to us, we can be unaware of our standing still as the world moves forward. Medicine as a career can remain exciting if we persistently demand that we improve every day in some way, no matter how small. Previous training cannot limit future learning, and we must strive to never give in to excuses and constantly seek out new skills. Research, teaching, administration, society involvement, politics, governance, and business can all serve as catalysts in our work lives to instigate meaningful change and discover new challenges. The pursuit of new experiences in medicine is the lifeblood of our future careers and constant reinvention is the heartbeat that sustains it. No talented person in the business or technology sectors would ever be asked to do the exact same job for an entire career. Therefore, why should we? Reinvention every 5 to 7 years is a must.
Find passion outside of medicine. Our interests outside of medicine are assets no different than finances, property, and material goods. As such, we need a plan for asset allocation and diversification that involves more than just numbers and percentages. We need healthy passions that evoke emotions and solidify memories. A busy practice can be a jealous mistress. Therefore, be careful to allocate time in your calendar to develop your identity outside of the practice environment. The overwhelming urge is to ignore the lack of attention to life outside medicine because it’s not as comfortable as seeing familiar patients who need your help. As ignoring an infection can be deadly for patients, this approach can pull us inescapably far away from the things and people that we love. While a simple hike in the woods, a dinner with friends, or quiet conversation with family can seem trivial and easily pushed aside for clinics and cases, these are the anchors in our lives that will prevent us from going astray. As we develop healthy passions in our personal lives outside of medicine, we in turn create more anchors, keeping us grounded and true to ourselves and to those around us. When we decide what is important in our personal lives we must ensure that our schedules diligently protect the time devoted to these priorities. Control your schedule or your schedule will control you.
Create your own inspiration. To put it simply and honestly as Andy Dufresne once did in the film The Shawshank Redemption, we have to “get busy living or get busy dying.” There is a widely held misconception that by completing our training and graduating for the final time, we will be imbued with a sense of purpose to guide us for the rest of our careers. However, the reality is that, if we do the same thing every day for years, medicine can become simply a job, and the world around us can lose some of its luster. Inspiration is hard to come by, which is why we must create our own in the moments we can. Nothing should be taken for granted, as inspiration has no prerequisite size or form. It can be as simple as a novel observation or as grandiose as a revolutionary treatment. It can be as guileless as a beloved child’s success or a spouse’s love. Actively sharing ideas with mentors, colleagues, friends, and patients empowers each of us with a voice to create change. However, what matters more than the final outcome is our perception of the process and how we lead it. The constant and deliberate pursuit of new sources of motivation is paramount to staying excited and engaged in our work and our lives. Enjoy the journey—it can be well worth it.
In the end, if we change nothing, nothing will ever change. This adage is harder to follow than any surgical skill we perform. We can never give up on our personal growth in and out of medicine, as both are vitally important for our mental, spiritual, and physical health. A vibrant optimism is contagious and good for patients and physicians alike. As we travel deeper into the wilderness, remember that failures need not be daunting and perilous. They can be embraced and lead to learning and success that make us stronger and more hopeful than we ever thought possible. Be bold, be brave, and commit to fighting the cliché for your entire unique career. ◾
At the end of a journey 3,650 days long, there is a path leading into the wilderness. From the first day of medical school until the last day of fellowship, we safely follow the well-paved and often-traveled road of medical education with its preset and regimented responsibilities, objectives, and milestones. We become comfortable in the academic routine of newly prescribed goals and responsibilities every year of training. We continually push forward with the stated desire of completing our education, beginning our dream job, and discovering our personas as physicians and human beings along the way. Balance, while an ideal to aspire to, is often put aside for the perceived greater glory of practical knowledge, competition, and the finish line. The assumption all along is that happiness is preordained by this path. However, when the routine comes to an end and we take our first steps into life as an attending surgeon, we can come face to face with an inexplicable void.
It is often said that the best period of training is the first years of practice. We spend those initial years drinking from the fire hose that is the attending surgeon learning curve, but that learning curve often too quickly plateaus. We can be paralyzed by the uncertainty of what the future may bring and of our roles in it. At that moment we have a profound new choice to make: to relish the freedom to reinvent ourselves and create new adventures, or to succumb to the unhealthy temptations and outside influences that abound. Bad decisions are inevitable if we never spend any time reflecting on what actually makes us happy. The sesquipedalian prose of self-improvement books often belabors the fact that we are all at risk of becoming clichés. To fight the cliché, we believe the essence of healthy success in practice after training lies in 3 principles: reinvention, passion, and inspiration. The rest is filler.
Reinvent yourself within medicine. As physicians, part of our identities is built upon our abilities to compassionately care for patients and effectively treat disease. However, the vast majority of procedures and skills we acquire during training will be obsolete in a decade or less. Therefore, it is imperative that we change with time, or else we will become stagnant. If we choose to compare ourselves only to those around us and similar to us, we can be unaware of our standing still as the world moves forward. Medicine as a career can remain exciting if we persistently demand that we improve every day in some way, no matter how small. Previous training cannot limit future learning, and we must strive to never give in to excuses and constantly seek out new skills. Research, teaching, administration, society involvement, politics, governance, and business can all serve as catalysts in our work lives to instigate meaningful change and discover new challenges. The pursuit of new experiences in medicine is the lifeblood of our future careers and constant reinvention is the heartbeat that sustains it. No talented person in the business or technology sectors would ever be asked to do the exact same job for an entire career. Therefore, why should we? Reinvention every 5 to 7 years is a must.
Find passion outside of medicine. Our interests outside of medicine are assets no different than finances, property, and material goods. As such, we need a plan for asset allocation and diversification that involves more than just numbers and percentages. We need healthy passions that evoke emotions and solidify memories. A busy practice can be a jealous mistress. Therefore, be careful to allocate time in your calendar to develop your identity outside of the practice environment. The overwhelming urge is to ignore the lack of attention to life outside medicine because it’s not as comfortable as seeing familiar patients who need your help. As ignoring an infection can be deadly for patients, this approach can pull us inescapably far away from the things and people that we love. While a simple hike in the woods, a dinner with friends, or quiet conversation with family can seem trivial and easily pushed aside for clinics and cases, these are the anchors in our lives that will prevent us from going astray. As we develop healthy passions in our personal lives outside of medicine, we in turn create more anchors, keeping us grounded and true to ourselves and to those around us. When we decide what is important in our personal lives we must ensure that our schedules diligently protect the time devoted to these priorities. Control your schedule or your schedule will control you.
Create your own inspiration. To put it simply and honestly as Andy Dufresne once did in the film The Shawshank Redemption, we have to “get busy living or get busy dying.” There is a widely held misconception that by completing our training and graduating for the final time, we will be imbued with a sense of purpose to guide us for the rest of our careers. However, the reality is that, if we do the same thing every day for years, medicine can become simply a job, and the world around us can lose some of its luster. Inspiration is hard to come by, which is why we must create our own in the moments we can. Nothing should be taken for granted, as inspiration has no prerequisite size or form. It can be as simple as a novel observation or as grandiose as a revolutionary treatment. It can be as guileless as a beloved child’s success or a spouse’s love. Actively sharing ideas with mentors, colleagues, friends, and patients empowers each of us with a voice to create change. However, what matters more than the final outcome is our perception of the process and how we lead it. The constant and deliberate pursuit of new sources of motivation is paramount to staying excited and engaged in our work and our lives. Enjoy the journey—it can be well worth it.
In the end, if we change nothing, nothing will ever change. This adage is harder to follow than any surgical skill we perform. We can never give up on our personal growth in and out of medicine, as both are vitally important for our mental, spiritual, and physical health. A vibrant optimism is contagious and good for patients and physicians alike. As we travel deeper into the wilderness, remember that failures need not be daunting and perilous. They can be embraced and lead to learning and success that make us stronger and more hopeful than we ever thought possible. Be bold, be brave, and commit to fighting the cliché for your entire unique career. ◾
At the end of a journey 3,650 days long, there is a path leading into the wilderness. From the first day of medical school until the last day of fellowship, we safely follow the well-paved and often-traveled road of medical education with its preset and regimented responsibilities, objectives, and milestones. We become comfortable in the academic routine of newly prescribed goals and responsibilities every year of training. We continually push forward with the stated desire of completing our education, beginning our dream job, and discovering our personas as physicians and human beings along the way. Balance, while an ideal to aspire to, is often put aside for the perceived greater glory of practical knowledge, competition, and the finish line. The assumption all along is that happiness is preordained by this path. However, when the routine comes to an end and we take our first steps into life as an attending surgeon, we can come face to face with an inexplicable void.
It is often said that the best period of training is the first years of practice. We spend those initial years drinking from the fire hose that is the attending surgeon learning curve, but that learning curve often too quickly plateaus. We can be paralyzed by the uncertainty of what the future may bring and of our roles in it. At that moment we have a profound new choice to make: to relish the freedom to reinvent ourselves and create new adventures, or to succumb to the unhealthy temptations and outside influences that abound. Bad decisions are inevitable if we never spend any time reflecting on what actually makes us happy. The sesquipedalian prose of self-improvement books often belabors the fact that we are all at risk of becoming clichés. To fight the cliché, we believe the essence of healthy success in practice after training lies in 3 principles: reinvention, passion, and inspiration. The rest is filler.
Reinvent yourself within medicine. As physicians, part of our identities is built upon our abilities to compassionately care for patients and effectively treat disease. However, the vast majority of procedures and skills we acquire during training will be obsolete in a decade or less. Therefore, it is imperative that we change with time, or else we will become stagnant. If we choose to compare ourselves only to those around us and similar to us, we can be unaware of our standing still as the world moves forward. Medicine as a career can remain exciting if we persistently demand that we improve every day in some way, no matter how small. Previous training cannot limit future learning, and we must strive to never give in to excuses and constantly seek out new skills. Research, teaching, administration, society involvement, politics, governance, and business can all serve as catalysts in our work lives to instigate meaningful change and discover new challenges. The pursuit of new experiences in medicine is the lifeblood of our future careers and constant reinvention is the heartbeat that sustains it. No talented person in the business or technology sectors would ever be asked to do the exact same job for an entire career. Therefore, why should we? Reinvention every 5 to 7 years is a must.
Find passion outside of medicine. Our interests outside of medicine are assets no different than finances, property, and material goods. As such, we need a plan for asset allocation and diversification that involves more than just numbers and percentages. We need healthy passions that evoke emotions and solidify memories. A busy practice can be a jealous mistress. Therefore, be careful to allocate time in your calendar to develop your identity outside of the practice environment. The overwhelming urge is to ignore the lack of attention to life outside medicine because it’s not as comfortable as seeing familiar patients who need your help. As ignoring an infection can be deadly for patients, this approach can pull us inescapably far away from the things and people that we love. While a simple hike in the woods, a dinner with friends, or quiet conversation with family can seem trivial and easily pushed aside for clinics and cases, these are the anchors in our lives that will prevent us from going astray. As we develop healthy passions in our personal lives outside of medicine, we in turn create more anchors, keeping us grounded and true to ourselves and to those around us. When we decide what is important in our personal lives we must ensure that our schedules diligently protect the time devoted to these priorities. Control your schedule or your schedule will control you.
Create your own inspiration. To put it simply and honestly as Andy Dufresne once did in the film The Shawshank Redemption, we have to “get busy living or get busy dying.” There is a widely held misconception that by completing our training and graduating for the final time, we will be imbued with a sense of purpose to guide us for the rest of our careers. However, the reality is that, if we do the same thing every day for years, medicine can become simply a job, and the world around us can lose some of its luster. Inspiration is hard to come by, which is why we must create our own in the moments we can. Nothing should be taken for granted, as inspiration has no prerequisite size or form. It can be as simple as a novel observation or as grandiose as a revolutionary treatment. It can be as guileless as a beloved child’s success or a spouse’s love. Actively sharing ideas with mentors, colleagues, friends, and patients empowers each of us with a voice to create change. However, what matters more than the final outcome is our perception of the process and how we lead it. The constant and deliberate pursuit of new sources of motivation is paramount to staying excited and engaged in our work and our lives. Enjoy the journey—it can be well worth it.
In the end, if we change nothing, nothing will ever change. This adage is harder to follow than any surgical skill we perform. We can never give up on our personal growth in and out of medicine, as both are vitally important for our mental, spiritual, and physical health. A vibrant optimism is contagious and good for patients and physicians alike. As we travel deeper into the wilderness, remember that failures need not be daunting and perilous. They can be embraced and lead to learning and success that make us stronger and more hopeful than we ever thought possible. Be bold, be brave, and commit to fighting the cliché for your entire unique career. ◾
Metal Ion Levels in Maternal and Placental Blood After Metal-on-Metal Total Hip Arthroplasty
Serum metal ion levels are increased after primary total hip arthroplasty (THA) with all types of head-liner bearing surfaces.1-4 In recent years, there has been increasing concern regarding elevated metal ion levels and adverse local and systemic effects, in particular, from metal-on-metal (MOM) implants.5 There have been reports of adverse local tissue reactions (ALTR) and systemic effects associated with elevated metal ion levels from MOM THA.6-10 MOM hip resurfacings have been advocated in the literature for use in select patient populations, such as young, active individuals.11,12 Purported benefits of MOM-bearing surfaces in this patient population include reduced wear and the prevention of osteolysis.13 While the incidence of ALTR has been reported to be approximately 1% within 5 years after MOM hip resurfacing, the prevalence of ALTR at long-term follow-up is unknown.14 Adverse local tissue reactions in hip resurfacing are related in part to femoral head coverage by the acetabular cup, as well as component design and orientation. The risk for ALTR with MOM THA has been reported to correlate with the level of serum metal ion levels because of the bearing surface, along with taper corrosion and corrosion secondary to the large surface area of the femoral head.13-15 The overall clinical and prognostic value of metal ion levels in cases of MOM bearings remains controversial and without clear cut-off values.15
The long-term physiologic response to elevated serum metal ion levels from THA implants remains unknown and is of particular concern in pregnant women because of potential transplacental transfer. Several studies have shown that DNA (deoxyribonucleic acid) and chromosomal changes can occur in patients with both MOM and non-MOM hip implants.16-18 Techniques to accurately measure the levels of metal ions, including cobalt, chromium, and titanium in the serum, have improved substantially in recent years and have been used successfully in clinical applications with low detection limits.2,4,19,20 Evidence shows that pregnancy-related complications in women with well-functioning cemented, hybrid, or uncemented metal-on-polyethylene THA are not different from those in healthy women.21 However, it is unclear if metal ions can cross the placenta and negatively affect the development of a fetus in mothers with MOM-bearing THAs.22 We conducted this study to determine if metal ions can traverse the placenta by measuring serum metal ion concentrations in mothers with and without MOM THA and the corresponding levels in umbilical cord blood samples.
Materials and Methods
Ten patients were prospectively enrolled in this study, which was approved by the institutional review boards at all 3 participating hospitals prior to initiation. All patients provided informed consent and agreed to maternal and umbilical cord blood sampling. Seven of the 10 patients did not have any metallic implants and served as controls. The remaining 3 patients had either a MOM unilateral primary THA (1 patient) or unilateral MOM hip-resurfacing arthroplasty (2 patients) with no other metal implants in the body. For all subjects, maternal and umbilical cord blood was obtained at the time of delivery.
Group Demographics
The 3 women in the implant group had a mean age of 32.3 years (range, 23-39 years) at time of delivery. The first patient had posttraumatic osteoarthritis and underwent right THA using a modular MOM 60-mm acetabular component, a 36-mm cobalt chrome head, and a cementless, titanium proximally porous-coated femoral component (Pinnacle Total Hip System and Summit Total Hip System; DePuy Synthes, Warsaw, Indiana). Her infant was born 2 years after index THA. The second patient had a diagnosis of degenerative osteoarthritis secondary to developmental dysplasia of the hip and underwent a hybrid MOM hip resurfacing with a monoblock 50-mm cup and 40-mm cobalt chrome head (Conserve Plus; Wright Medical Technology, Arlington, Tennessee). She gave birth to her infant 6 years after her hip resurfacing. The third patient also had a diagnosis of degenerative osteoarthritis secondary to developmental dysplasia of the hip and underwent hip resurfacing with a 54-mm monoblock cup and 44-mm cobalt chrome head (Conserve Plus). Her infant was born 4 years after her resurfacing arthroplasty. All of the infants were born healthy, and the deliveries were uneventful and without complications. Seven women with a mean age of 32.1 years (range, 24-37 years) and their infants served as controls at the time of delivery. None of the women in the control group had a history of renal impairment, inherited genetic disorders, or metal implants.
Serum Metal Ion Analysis
Blood samples were collected using S-Monovette polypropylene syringes (Sarstedt, Princeton, New Jersey), a multi-adapter, and infusion set following an established technique.1 All vessels and utensils used for specimen collection were verified to be free of metal contamination. Three 10-mL syringes were drawn, and each syringe was labeled to indicate the sequence of collection. The first 10 mL were drawn to rinse the needle and adapter. Blood was then allowed to clot naturally and centrifuged at 1850 rpm for 30 minutes, separating samples into cell and serum fractions that were stored in labeled vials at -80ºC. All specimen manipulations after collection were carried out in a class-100 environment using a SterilGARD Biological Safety Cabinet (Baker, Sanford, Maine) and class-100 gloves (Oak Technical, Ravenna, Ohio) to minimize atmospheric and manual contamination. Maternal and umbilical cord blood metal ion levels were tested using high-resolution sector-field inductively-coupled plasma-mass spectrometry (HR-SF-ICPMS) (Element 2; Thermo Fisher Scientific, Bremen, Germany) following the method of additions as described previously.23 The HR-SF-ICPMS machine was equipped with an SC-E2 autosampler, Teflon nebulizer and spray chamber, sapphire injector (Elemental Scientific, Omaha, Nebraska) and platinum cones. All calibration and internal standard solutions were prepared by gradual dilutions of single-element standard solutions (1000 μg/mL from High Purity Standards, Charleston, South Carolina). The certified reference material, Seronorm Trace Elements Serum (SERO, Billingstad, Norway), were routinely analyzed with samples. The serum concentrations of cobalt, chromium, titanium, and nickel were measured with detection limits in ng/mL (parts per billion) of 0.04 for cobalt, 0.015 for chromium, 0.2 for titanium, and 0.17 for nickel.4 Concentrations below the detection limit were approximated as one-half of the detection limit by convention to calculate means.
Statistical Analysis
The data reported are the means for each group for each of the metal ion levels analyzed. Intergroup comparisons were made with the Mann-Whitney-Wilcoxon test using SPSS statistics software (SPSS Science Inc, Chicago, Illinois) to compare implant and control groups in regards to serum metal ion levels. Intragroup comparisons were made using the Friedman test with significance set at P < .05. Spearman rank-order correlation tests were used to investigate relationships between maternal and infant serum metal ion levels.
Results
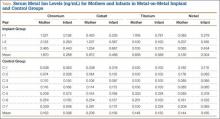
The Table shows the mean serum metal ion levels of chromium, cobalt, titanium, and nickel for both groups. The implant-group mothers had significantly higher chromium and cobalt levels than the control-group mothers, with mean chromium levels of 1.87 ng/mL vs 0.16 ng/mL (P = .01) and mean cobalt levels of 0.97 ng/mL vs 0.20 ng/mL (P = .01), respectively. All control-group maternal chromium and cobalt levels were lower than the implant group. There were no significant differences detected between the implant-group and control-group mothers with respect to serum titanium or nickel levels.
The implant-group cord blood samples also had significantly higher chromium and cobalt levels than did the control-group infants with mean chromium levels of 0.29 ng/mL vs 0.10 ng/mL (P = .03) and mean cobalt levels of 0.49 ng/mL vs 0.16 ng/mL (P = .01), respectively. All but 1 of the control-group infants had chromium levels that were lower than the implant-group infant chromium levels. All of the control-group infant cobalt levels were lower than the implant-group infant cobalt levels. In the mother (I-1) who had a titanium-containing implant, her titanium level was 1.77 ng/mL and her cord blood level was 0.78 ng/mL. In contrast, the other 2 patients did not have titanium-containing implants and had corresponding metal levels of 0.10 ng/mL and cord blood levels either below the detection limit or just slightly above it. No statistically significant differences were found between the implant- and control-group infants with respect to serum titanium or nickel levels.
Considering the implant and control groups separately, we found no statistically significant differences between the maternal and infant titanium levels or the maternal and infant nickel levels. In the implant group, the mother’s chromium level was always higher than her infant’s chromium level, and the mother’s cobalt level was always higher than her infant’s cobalt level (P= .08). In the control group, there was no correlation between the maternal and infant chromium levels, or between the maternal and infant cobalt levels. In the implant group, the maternal and infant chromium levels were highly correlated (r = 1), as were the maternal and infant cobalt levels (r = 1).
When infants’ chromium levels were expressed as a percentage of their mothers’ chromium levels, the mean was 15.4% (range, 12.3%-18%) for the implant group and 58.9% (range, 13.5%-165.7%) for the control group (P = .05). The mean infant cobalt level, expressed as percentage of maternal cobalt level, was 50% (range, 45.8%-53.1%) for the implant group and 76.6% (range, 59.1%-150.8%) for the control group (P = .01).
Discussion
Cobalt and chromium serum metal ion levels obtained from mothers with MOM implants and umbilical cord samples were significantly elevated in comparison with controls. There was also a strong correlation between implant-group maternal cobalt and chromium levels and implant-group infant cobalt and chromium levels; however, no such correlation existed in the control group. Our results suggest that cobalt and chromium cross the placental barrier. Implant mothers had higher chromium and cobalt levels compared with implant babies, and these babies had approximately 15% of the level of chromium and 50% of the level of cobalt when compared to implant maternal levels. This finding suggests that the placenta modulates the transfer of chromium and cobalt to the fetus.
Two studies have reported chromium and cobalt levels in maternal and umbilical cord sera after MOM THA.5,24 Brodner and colleagues5 determined the maternal serum levels of cobalt and chromium in 3 women 3.8 years after MOM THA and compared those to cobalt and chromium levels obtained from umbilical cord blood. At the time of delivery, the maternal chromium concentrations in the 3 patients were 1.6 ng/mL, 0.5 ng/mL, and 0.9 ng/mL, and the cobalt concentrations were 1 ng/mL in 1 patient and below the detection limit in the other 2 patients. Cobalt and chromium concentrations of the 3 umbilical cord sera were below the detection limit. The authors concluded that cobalt and chromium did not cross the placenta based on their laboratory detection limits. Metal ion levels were measured using atomic absorption spectrometry with relatively high detection limits of 0.3 ng/mL, which is not as sensitive as the HR-SF-ICPMS technique used in the present study that has detection limits of 0.04 ng/mL for cobalt and 0.015 ng/mL for chromium. The relatively high detection limits of atomic absorption spectrometry were likely responsible for the authors’ inability to detect elevated chromium and cobalt levels in umbilical cord sera.
Ziaee and colleagues24 used HR-SF-ICPMS, as we did in this study, to measure the mean concentrations of cobalt and chromium ion levels in 10 maternal and umbilical cord blood samples in women with Birmingham MOM hip-resurfacing prostheses (Smith & Nephew, Warwick, United Kingdom). Nine of those patients had a unilateral resurfacing and 1 patient had bilateral-resurfacing prostheses. The mean maternal age was 31 years, and mean duration between hip resurfacing and delivery was 53 months. Ten normal controls were also tested with a mean maternal age of 30.9 years. The authors found that the mean cord blood level of cobalt in the study patients was 0.83 ng/mL, significantly higher (P < .01) than cobalt levels in the control group, which measured 0.33 ng/mL. The mean cord blood levels of chromium in the study and control groups were 0.37 ng/mL and 0.19 ng/mL, respectively. No children were reported to have evidence of congenital anomalies. Similar to our findings, they noted a modulatory effect on the transfer of metal ions across the placenta in patients with MOM prostheses.24 They reported the relative levels of cobalt and chromium in offspring to be 60.4% and 29.4% of the maternal ion levels, respectively. Control-group infants had mean cobalt and chromium levels that were 98.5% and 97.2% of mean maternal levels, respectively.
The transfer of metal ions across the placenta in control subjects is an expected finding because cobalt and chromium are essential trace elements required by the developing fetus. Rudge and colleagues25 estimated a transplacental transfer rate of 45% for cobalt in a series of 62 paired samples of maternal and cord blood. DeSouza and coauthors26 reported a series of 3 patients with MOM hip resurfacings who had the prosthesis in situ during pregnancy and found no teratogenic effects of metal ion transfer across the placenta. Umbilical cord blood chromium levels were less than 25% of the maternal serum levels and cord blood cobalt levels were approximately 50% that of maternal blood.26 In an animal experiment, Wallach and Verch18 also reported that maternal chromium levels can be decreased because of placental uptake.
Ziaee and colleagues24 tested metal ion levels using whole blood in contrast to serum, as we did in the present study. Daniel and coauthors16, who reported on the validity of serum levels as a surrogate measure of systemic exposure to metal ions in hip replacement, suggested that serum and whole blood metal ion levels cannot be interconverted because metal within cells are not in dynamic equilibrium with extracellular levels. They concluded that serum metal ion concentrations are not a useful surrogate measure of systemic metal ion exposure based on the wide variability seen in normalized and Bland-Altman scatterplots.16 However, it is important to note that Bland-Altman plots are user-dependent in determining significance, and results can vary based on the parameters tested. A high correlation does not automatically imply that there is a good agreement between 2 methods because a widespread sample could influence results. Whole blood analysis requires more processing steps, thus providing an increased chance of contamination and variability compared with serum metal level analysis. In our experiences, serum metal ion analysis has been shown to have accurate and reproducible results in clinical situations.2,4
While there is insufficient literature that specifically studies the effects of elevated metal ion levels on maternal and fetal subjects, there have been no reported negative effects in human babies even when maternal ion levels are elevated enough to be associated with ALTR. A case report by Fritzsche and colleagues27 reported a mother with bilateral MOM THA, a recurrent pseudotumor, and high blood levels of chromium (39 ng/mL) and cobalt (138 ng/mL) at 12 weeks gestation. The child was born at 38 weeks gestation with cord blood chromium and cobalt levels of 2.1 ng/mL and 75 ng/mL, respectively. The infant’s metal ion levels remained elevated at age 8 weeks with a chromium level of 2.5 ng/mL and cobalt level of 13 ng/mL and no signs of toxicity by age 14 weeks. In an animal model, Saxena and colleagues28 found that chromium in the hexavalent form passed through the placenta in mice and rats that were fed high doses of potassium dichromate. Trivalent chromium was not found to cross the placenta. In a follow-up study, Junaid and coauthors29 investigated the effects of elevated chromium levels in female mice given potassium dichromate in drinking water on days 14 to 19 of pregnancy. Animals receiving high-dose chromium had significantly higher incidences of postimplantation loss along with subdermal hemorrhagic patches and reduced ossification.29 Cobalt has not been shown to be teratogenic or cause fetotoxicity in a rat animal model given daily doses of as much as 100 mg/kg cobalt (II) chloride on days 6 to 15 of gestation.30
It is important to recognize that rodent data are limited and may not provide accurate translational insight into the effects of metal ions in human maternal and fetal subjects. Mammalian species have significant heterogeneity in the structure and function of their placentas. Rurak31 has shown that rodents have an additional persisting yolk sac placenta that allows the transfer of maternal immunoglobulins to the fetus. Humans, on the other hand, have a yolk sac placenta that regresses early in pregnancy. Differing placental biologic function makes it difficult to extrapolate the effects of metal ions in rodents to human subjects.
It is also important to note that serum levels of cobalt, chromium, and titanium can remain persistently elevated in well-functioning metal-on-polyethylene THA for several years and that elevated metal ion levels are not confined to MOM bearings.2 Levine and colleagues4 reported that serum levels of cobalt, chromium, and titanium remain persistently elevated after 10 years in a cohort of 27 well-functioning primary metal-on-polyethylene THA (hybrid, cobalt-chrome, titanium). Cobalt concentrations were elevated in all implants compared with controls at all follow-up periods through 10 years with absolute values less than 1 ng/mL. The authors noted that metal release at the modular femoral head-neck junctions was likely the dominant source of serum cobalt and chromium rather than passive dissolution. Hsu and colleagues32 have also shown that patients undergoing a second metal-on-polyethylene THA after primary THA have elevated serum metal ion levels (cobalt, chromium, titanium) up to 6 years after second surgery. Reported cobalt concentrations in patients with unilateral THA reached a maximum of 0.5 ng/mL during the follow-up course compared with 1.5 ng/mL for patients with bilateral THA. It is unknown what the potential metal ion transfer load would be in mothers with metal-on-polyethylene THA and associated taper corrosion to their infants.
Conclusion
Mothers with MOM-bearing implants and their children have higher cobalt and chromium levels than control subjects, demonstrating that the placenta is not a complete barrier to metal ion transport, although it seems to have a modulating effect. Physicians and women of child-bearing age should be aware of these findings when considering the use of MOM-bearing couples for THA. The effects of metal ions on long-term maternal and fetal health require research through serial clinical exams and metal ion level testing in prospective studies of different THA-bearing surfaces.
1. Jacobs JJ, Skipor AK, Black J, Urban R, Galante JO. Release and excretion of metal in patients who have a total hip-replacement component made of titanium-base alloy. J Bone Joint Surg Am. 1991;73(10):1475-1486.
2. Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80(10):1447-1458.
3. Jacobs JJ, Skipor AK, Urban RM, Black J, Manion LM, Galante JO. Transport of metal degradation products of titanium alloy total hip replacements to reticuloendothelial organs. An autopsy study. Trans Soc Biomater. 1994;18:318-325.
4. Levine BR, Hsu AR, Skipor AK, et al. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty: a concise follow-up of a previous report. J Bone Joint Surg Am. 2013;95(6):512-518.
5. Brodner W, Grohs JG, Bancher-Todesca D, et al. Does the placenta inhibit the passage of chromium and cobalt after metal-on-metal total hip arthroplasty? J Arthroplasty. 2004;19(8 suppl 3):102-106.
6. Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop. 2012;41(9):422-426.
7. Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(17):2847-2851.
8. Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Black J, Peoc’h M. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82(4):457-476.
9. Watters TS, Eward WC, Hallows RK, Dodd LG, Wellman SS, Bolognesi MP. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(7):1666-1669.
10. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87(1):28-36.
11. Nunley RM, Della Valle CJ, Barrack RL. Is patient selection important for hip resurfacing? Clin Orthop. 2009;467(1):56-65.
12. Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87(2):167-170.
13. Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation. Four to seven-year results. J Bone Joint Surg Am. 2000;82(6):789-798.
14. Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90(7):847-851.
15. Hartmann A, Hannemann F, Lutzner J, et al. Metal ion concentrations in body fluids after implantation of hip replacements with metal-on-metal bearing--systematic review of clinical and epidemiological studies. PLoS One. 2013;8(8):e70359.
16. Daniel J, Ziaee H, Pynsent PB, McMinn DJ. The validity of serum levels as a surrogate measure of systemic exposure to metal ions in hip replacement. J Bone Joint Surg Br. 2007;89(6):736-741.
17. Merritt K, Brown SA. Release of hexavalent chromium from corrosion of stainless steel and cobalt-chromium alloys. J Biomed Mater Res. 1995;29(5):627-633.
18. Wallach S, Verch RL. Placental transport of chromium. J Am Coll Nutr. 1984;3(1):69-74.
19. Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80(2):268-282.
20. Van Der Straeten C, Grammatopoulos G, Gill HS, Calistri A, Campbell P, De Smet KA. The 2012 Otto Aufranc Award: The interpretation of metal ion levels in unilateral and bilateral hip resurfacing. Clin Orthop. 2013;471(2):377-385.
21. Sierra RJ, Trousdale RT, Cabanela ME. Pregnancy and childbirth after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(1):21-24.
22. Antoniou J, Zukor DJ, Mwale F, Minarik W, Petit A, Huk OL. Metal ion levels in the blood of patients after hip resurfacing: a comparison between twenty-eight and thirty-six-millimeter-head metal-on-metal prostheses. J Bone Joint Surg Am. 2008;90(Suppl 3):142-148.
23. Iavicoli I, Falcone G, Alessandrelli M, et al. The release of metals from metal-on-metal surface arthroplasty of the hip. J Trace Elem Med Biol. 2006;20(1):25-31.
24. Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJ. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: a controlled study. J Bone Joint Surg Br. 2007;89(3):301-305.
25. Rudge CV, Rollin HB, Nogueira CM, Thomassen Y, Rudge MC, Odland JO. The placenta as a barrier for toxic and essential elements in paired maternal and cord blood samples of South African delivering women. J Environ Monit. 2009;11(7):1322-1330.
26. deSouza RM, Wallace D, Costa ML, Krikler SJ. Transplacental passage of metal ions in women with hip resurfacing: no teratogenic effects observed. Hip Int. 2012;22(1):96-99.
27. Fritzsche J, Borisch C, Schaefer C. Case report: High chromium and cobalt levels in a pregnant patient with bilateral metal-on-metal hip arthroplasties. Clin Orthop. 2012;470(8):2325-2331.
28. Saxena DK, Murthy RC, Jain VK, Chandra SV. Fetoplacental-maternal uptake of hexavalent chromium administered orally in rats and mice. Bull Environ Contam Toxicol. 1990;45(3):430-435.
29. Junaid M, Murthy RC, Saxena DK. Chromium fetotoxicity in mice during late pregnancy. Vet Hum Toxicol. 1995;37(4):320-323.
30. Paternain JL, Domingo JL, Corbella J. Developmental toxicity of cobalt in the rat. J Toxicol Environ Health. 1988;24(2):193-200.
31. Rurak DW. Development and function of the placenta. In: Harding R, Bocking AD, eds. Fetal Growth and Development. Cambridge, UK: Cambridge University Press; 2001.
32. Hsu AR, Levine BR, Skipor AK, Hallab NJ, Paprosky WG, Jacobs JJ. Effect of a second joint arthroplasty on metal ion levels after primary total hip arthroplasty. Am J Orthop. 2013;42(10):E84-E87.
Serum metal ion levels are increased after primary total hip arthroplasty (THA) with all types of head-liner bearing surfaces.1-4 In recent years, there has been increasing concern regarding elevated metal ion levels and adverse local and systemic effects, in particular, from metal-on-metal (MOM) implants.5 There have been reports of adverse local tissue reactions (ALTR) and systemic effects associated with elevated metal ion levels from MOM THA.6-10 MOM hip resurfacings have been advocated in the literature for use in select patient populations, such as young, active individuals.11,12 Purported benefits of MOM-bearing surfaces in this patient population include reduced wear and the prevention of osteolysis.13 While the incidence of ALTR has been reported to be approximately 1% within 5 years after MOM hip resurfacing, the prevalence of ALTR at long-term follow-up is unknown.14 Adverse local tissue reactions in hip resurfacing are related in part to femoral head coverage by the acetabular cup, as well as component design and orientation. The risk for ALTR with MOM THA has been reported to correlate with the level of serum metal ion levels because of the bearing surface, along with taper corrosion and corrosion secondary to the large surface area of the femoral head.13-15 The overall clinical and prognostic value of metal ion levels in cases of MOM bearings remains controversial and without clear cut-off values.15
The long-term physiologic response to elevated serum metal ion levels from THA implants remains unknown and is of particular concern in pregnant women because of potential transplacental transfer. Several studies have shown that DNA (deoxyribonucleic acid) and chromosomal changes can occur in patients with both MOM and non-MOM hip implants.16-18 Techniques to accurately measure the levels of metal ions, including cobalt, chromium, and titanium in the serum, have improved substantially in recent years and have been used successfully in clinical applications with low detection limits.2,4,19,20 Evidence shows that pregnancy-related complications in women with well-functioning cemented, hybrid, or uncemented metal-on-polyethylene THA are not different from those in healthy women.21 However, it is unclear if metal ions can cross the placenta and negatively affect the development of a fetus in mothers with MOM-bearing THAs.22 We conducted this study to determine if metal ions can traverse the placenta by measuring serum metal ion concentrations in mothers with and without MOM THA and the corresponding levels in umbilical cord blood samples.
Materials and Methods
Ten patients were prospectively enrolled in this study, which was approved by the institutional review boards at all 3 participating hospitals prior to initiation. All patients provided informed consent and agreed to maternal and umbilical cord blood sampling. Seven of the 10 patients did not have any metallic implants and served as controls. The remaining 3 patients had either a MOM unilateral primary THA (1 patient) or unilateral MOM hip-resurfacing arthroplasty (2 patients) with no other metal implants in the body. For all subjects, maternal and umbilical cord blood was obtained at the time of delivery.
Group Demographics
The 3 women in the implant group had a mean age of 32.3 years (range, 23-39 years) at time of delivery. The first patient had posttraumatic osteoarthritis and underwent right THA using a modular MOM 60-mm acetabular component, a 36-mm cobalt chrome head, and a cementless, titanium proximally porous-coated femoral component (Pinnacle Total Hip System and Summit Total Hip System; DePuy Synthes, Warsaw, Indiana). Her infant was born 2 years after index THA. The second patient had a diagnosis of degenerative osteoarthritis secondary to developmental dysplasia of the hip and underwent a hybrid MOM hip resurfacing with a monoblock 50-mm cup and 40-mm cobalt chrome head (Conserve Plus; Wright Medical Technology, Arlington, Tennessee). She gave birth to her infant 6 years after her hip resurfacing. The third patient also had a diagnosis of degenerative osteoarthritis secondary to developmental dysplasia of the hip and underwent hip resurfacing with a 54-mm monoblock cup and 44-mm cobalt chrome head (Conserve Plus). Her infant was born 4 years after her resurfacing arthroplasty. All of the infants were born healthy, and the deliveries were uneventful and without complications. Seven women with a mean age of 32.1 years (range, 24-37 years) and their infants served as controls at the time of delivery. None of the women in the control group had a history of renal impairment, inherited genetic disorders, or metal implants.
Serum Metal Ion Analysis
Blood samples were collected using S-Monovette polypropylene syringes (Sarstedt, Princeton, New Jersey), a multi-adapter, and infusion set following an established technique.1 All vessels and utensils used for specimen collection were verified to be free of metal contamination. Three 10-mL syringes were drawn, and each syringe was labeled to indicate the sequence of collection. The first 10 mL were drawn to rinse the needle and adapter. Blood was then allowed to clot naturally and centrifuged at 1850 rpm for 30 minutes, separating samples into cell and serum fractions that were stored in labeled vials at -80ºC. All specimen manipulations after collection were carried out in a class-100 environment using a SterilGARD Biological Safety Cabinet (Baker, Sanford, Maine) and class-100 gloves (Oak Technical, Ravenna, Ohio) to minimize atmospheric and manual contamination. Maternal and umbilical cord blood metal ion levels were tested using high-resolution sector-field inductively-coupled plasma-mass spectrometry (HR-SF-ICPMS) (Element 2; Thermo Fisher Scientific, Bremen, Germany) following the method of additions as described previously.23 The HR-SF-ICPMS machine was equipped with an SC-E2 autosampler, Teflon nebulizer and spray chamber, sapphire injector (Elemental Scientific, Omaha, Nebraska) and platinum cones. All calibration and internal standard solutions were prepared by gradual dilutions of single-element standard solutions (1000 μg/mL from High Purity Standards, Charleston, South Carolina). The certified reference material, Seronorm Trace Elements Serum (SERO, Billingstad, Norway), were routinely analyzed with samples. The serum concentrations of cobalt, chromium, titanium, and nickel were measured with detection limits in ng/mL (parts per billion) of 0.04 for cobalt, 0.015 for chromium, 0.2 for titanium, and 0.17 for nickel.4 Concentrations below the detection limit were approximated as one-half of the detection limit by convention to calculate means.
Statistical Analysis
The data reported are the means for each group for each of the metal ion levels analyzed. Intergroup comparisons were made with the Mann-Whitney-Wilcoxon test using SPSS statistics software (SPSS Science Inc, Chicago, Illinois) to compare implant and control groups in regards to serum metal ion levels. Intragroup comparisons were made using the Friedman test with significance set at P < .05. Spearman rank-order correlation tests were used to investigate relationships between maternal and infant serum metal ion levels.
Results
The Table shows the mean serum metal ion levels of chromium, cobalt, titanium, and nickel for both groups. The implant-group mothers had significantly higher chromium and cobalt levels than the control-group mothers, with mean chromium levels of 1.87 ng/mL vs 0.16 ng/mL (P = .01) and mean cobalt levels of 0.97 ng/mL vs 0.20 ng/mL (P = .01), respectively. All control-group maternal chromium and cobalt levels were lower than the implant group. There were no significant differences detected between the implant-group and control-group mothers with respect to serum titanium or nickel levels.
The implant-group cord blood samples also had significantly higher chromium and cobalt levels than did the control-group infants with mean chromium levels of 0.29 ng/mL vs 0.10 ng/mL (P = .03) and mean cobalt levels of 0.49 ng/mL vs 0.16 ng/mL (P = .01), respectively. All but 1 of the control-group infants had chromium levels that were lower than the implant-group infant chromium levels. All of the control-group infant cobalt levels were lower than the implant-group infant cobalt levels. In the mother (I-1) who had a titanium-containing implant, her titanium level was 1.77 ng/mL and her cord blood level was 0.78 ng/mL. In contrast, the other 2 patients did not have titanium-containing implants and had corresponding metal levels of 0.10 ng/mL and cord blood levels either below the detection limit or just slightly above it. No statistically significant differences were found between the implant- and control-group infants with respect to serum titanium or nickel levels.
Considering the implant and control groups separately, we found no statistically significant differences between the maternal and infant titanium levels or the maternal and infant nickel levels. In the implant group, the mother’s chromium level was always higher than her infant’s chromium level, and the mother’s cobalt level was always higher than her infant’s cobalt level (P= .08). In the control group, there was no correlation between the maternal and infant chromium levels, or between the maternal and infant cobalt levels. In the implant group, the maternal and infant chromium levels were highly correlated (r = 1), as were the maternal and infant cobalt levels (r = 1).
When infants’ chromium levels were expressed as a percentage of their mothers’ chromium levels, the mean was 15.4% (range, 12.3%-18%) for the implant group and 58.9% (range, 13.5%-165.7%) for the control group (P = .05). The mean infant cobalt level, expressed as percentage of maternal cobalt level, was 50% (range, 45.8%-53.1%) for the implant group and 76.6% (range, 59.1%-150.8%) for the control group (P = .01).
Discussion
Cobalt and chromium serum metal ion levels obtained from mothers with MOM implants and umbilical cord samples were significantly elevated in comparison with controls. There was also a strong correlation between implant-group maternal cobalt and chromium levels and implant-group infant cobalt and chromium levels; however, no such correlation existed in the control group. Our results suggest that cobalt and chromium cross the placental barrier. Implant mothers had higher chromium and cobalt levels compared with implant babies, and these babies had approximately 15% of the level of chromium and 50% of the level of cobalt when compared to implant maternal levels. This finding suggests that the placenta modulates the transfer of chromium and cobalt to the fetus.
Two studies have reported chromium and cobalt levels in maternal and umbilical cord sera after MOM THA.5,24 Brodner and colleagues5 determined the maternal serum levels of cobalt and chromium in 3 women 3.8 years after MOM THA and compared those to cobalt and chromium levels obtained from umbilical cord blood. At the time of delivery, the maternal chromium concentrations in the 3 patients were 1.6 ng/mL, 0.5 ng/mL, and 0.9 ng/mL, and the cobalt concentrations were 1 ng/mL in 1 patient and below the detection limit in the other 2 patients. Cobalt and chromium concentrations of the 3 umbilical cord sera were below the detection limit. The authors concluded that cobalt and chromium did not cross the placenta based on their laboratory detection limits. Metal ion levels were measured using atomic absorption spectrometry with relatively high detection limits of 0.3 ng/mL, which is not as sensitive as the HR-SF-ICPMS technique used in the present study that has detection limits of 0.04 ng/mL for cobalt and 0.015 ng/mL for chromium. The relatively high detection limits of atomic absorption spectrometry were likely responsible for the authors’ inability to detect elevated chromium and cobalt levels in umbilical cord sera.
Ziaee and colleagues24 used HR-SF-ICPMS, as we did in this study, to measure the mean concentrations of cobalt and chromium ion levels in 10 maternal and umbilical cord blood samples in women with Birmingham MOM hip-resurfacing prostheses (Smith & Nephew, Warwick, United Kingdom). Nine of those patients had a unilateral resurfacing and 1 patient had bilateral-resurfacing prostheses. The mean maternal age was 31 years, and mean duration between hip resurfacing and delivery was 53 months. Ten normal controls were also tested with a mean maternal age of 30.9 years. The authors found that the mean cord blood level of cobalt in the study patients was 0.83 ng/mL, significantly higher (P < .01) than cobalt levels in the control group, which measured 0.33 ng/mL. The mean cord blood levels of chromium in the study and control groups were 0.37 ng/mL and 0.19 ng/mL, respectively. No children were reported to have evidence of congenital anomalies. Similar to our findings, they noted a modulatory effect on the transfer of metal ions across the placenta in patients with MOM prostheses.24 They reported the relative levels of cobalt and chromium in offspring to be 60.4% and 29.4% of the maternal ion levels, respectively. Control-group infants had mean cobalt and chromium levels that were 98.5% and 97.2% of mean maternal levels, respectively.
The transfer of metal ions across the placenta in control subjects is an expected finding because cobalt and chromium are essential trace elements required by the developing fetus. Rudge and colleagues25 estimated a transplacental transfer rate of 45% for cobalt in a series of 62 paired samples of maternal and cord blood. DeSouza and coauthors26 reported a series of 3 patients with MOM hip resurfacings who had the prosthesis in situ during pregnancy and found no teratogenic effects of metal ion transfer across the placenta. Umbilical cord blood chromium levels were less than 25% of the maternal serum levels and cord blood cobalt levels were approximately 50% that of maternal blood.26 In an animal experiment, Wallach and Verch18 also reported that maternal chromium levels can be decreased because of placental uptake.
Ziaee and colleagues24 tested metal ion levels using whole blood in contrast to serum, as we did in the present study. Daniel and coauthors16, who reported on the validity of serum levels as a surrogate measure of systemic exposure to metal ions in hip replacement, suggested that serum and whole blood metal ion levels cannot be interconverted because metal within cells are not in dynamic equilibrium with extracellular levels. They concluded that serum metal ion concentrations are not a useful surrogate measure of systemic metal ion exposure based on the wide variability seen in normalized and Bland-Altman scatterplots.16 However, it is important to note that Bland-Altman plots are user-dependent in determining significance, and results can vary based on the parameters tested. A high correlation does not automatically imply that there is a good agreement between 2 methods because a widespread sample could influence results. Whole blood analysis requires more processing steps, thus providing an increased chance of contamination and variability compared with serum metal level analysis. In our experiences, serum metal ion analysis has been shown to have accurate and reproducible results in clinical situations.2,4
While there is insufficient literature that specifically studies the effects of elevated metal ion levels on maternal and fetal subjects, there have been no reported negative effects in human babies even when maternal ion levels are elevated enough to be associated with ALTR. A case report by Fritzsche and colleagues27 reported a mother with bilateral MOM THA, a recurrent pseudotumor, and high blood levels of chromium (39 ng/mL) and cobalt (138 ng/mL) at 12 weeks gestation. The child was born at 38 weeks gestation with cord blood chromium and cobalt levels of 2.1 ng/mL and 75 ng/mL, respectively. The infant’s metal ion levels remained elevated at age 8 weeks with a chromium level of 2.5 ng/mL and cobalt level of 13 ng/mL and no signs of toxicity by age 14 weeks. In an animal model, Saxena and colleagues28 found that chromium in the hexavalent form passed through the placenta in mice and rats that were fed high doses of potassium dichromate. Trivalent chromium was not found to cross the placenta. In a follow-up study, Junaid and coauthors29 investigated the effects of elevated chromium levels in female mice given potassium dichromate in drinking water on days 14 to 19 of pregnancy. Animals receiving high-dose chromium had significantly higher incidences of postimplantation loss along with subdermal hemorrhagic patches and reduced ossification.29 Cobalt has not been shown to be teratogenic or cause fetotoxicity in a rat animal model given daily doses of as much as 100 mg/kg cobalt (II) chloride on days 6 to 15 of gestation.30
It is important to recognize that rodent data are limited and may not provide accurate translational insight into the effects of metal ions in human maternal and fetal subjects. Mammalian species have significant heterogeneity in the structure and function of their placentas. Rurak31 has shown that rodents have an additional persisting yolk sac placenta that allows the transfer of maternal immunoglobulins to the fetus. Humans, on the other hand, have a yolk sac placenta that regresses early in pregnancy. Differing placental biologic function makes it difficult to extrapolate the effects of metal ions in rodents to human subjects.
It is also important to note that serum levels of cobalt, chromium, and titanium can remain persistently elevated in well-functioning metal-on-polyethylene THA for several years and that elevated metal ion levels are not confined to MOM bearings.2 Levine and colleagues4 reported that serum levels of cobalt, chromium, and titanium remain persistently elevated after 10 years in a cohort of 27 well-functioning primary metal-on-polyethylene THA (hybrid, cobalt-chrome, titanium). Cobalt concentrations were elevated in all implants compared with controls at all follow-up periods through 10 years with absolute values less than 1 ng/mL. The authors noted that metal release at the modular femoral head-neck junctions was likely the dominant source of serum cobalt and chromium rather than passive dissolution. Hsu and colleagues32 have also shown that patients undergoing a second metal-on-polyethylene THA after primary THA have elevated serum metal ion levels (cobalt, chromium, titanium) up to 6 years after second surgery. Reported cobalt concentrations in patients with unilateral THA reached a maximum of 0.5 ng/mL during the follow-up course compared with 1.5 ng/mL for patients with bilateral THA. It is unknown what the potential metal ion transfer load would be in mothers with metal-on-polyethylene THA and associated taper corrosion to their infants.
Conclusion
Mothers with MOM-bearing implants and their children have higher cobalt and chromium levels than control subjects, demonstrating that the placenta is not a complete barrier to metal ion transport, although it seems to have a modulating effect. Physicians and women of child-bearing age should be aware of these findings when considering the use of MOM-bearing couples for THA. The effects of metal ions on long-term maternal and fetal health require research through serial clinical exams and metal ion level testing in prospective studies of different THA-bearing surfaces.
Serum metal ion levels are increased after primary total hip arthroplasty (THA) with all types of head-liner bearing surfaces.1-4 In recent years, there has been increasing concern regarding elevated metal ion levels and adverse local and systemic effects, in particular, from metal-on-metal (MOM) implants.5 There have been reports of adverse local tissue reactions (ALTR) and systemic effects associated with elevated metal ion levels from MOM THA.6-10 MOM hip resurfacings have been advocated in the literature for use in select patient populations, such as young, active individuals.11,12 Purported benefits of MOM-bearing surfaces in this patient population include reduced wear and the prevention of osteolysis.13 While the incidence of ALTR has been reported to be approximately 1% within 5 years after MOM hip resurfacing, the prevalence of ALTR at long-term follow-up is unknown.14 Adverse local tissue reactions in hip resurfacing are related in part to femoral head coverage by the acetabular cup, as well as component design and orientation. The risk for ALTR with MOM THA has been reported to correlate with the level of serum metal ion levels because of the bearing surface, along with taper corrosion and corrosion secondary to the large surface area of the femoral head.13-15 The overall clinical and prognostic value of metal ion levels in cases of MOM bearings remains controversial and without clear cut-off values.15
The long-term physiologic response to elevated serum metal ion levels from THA implants remains unknown and is of particular concern in pregnant women because of potential transplacental transfer. Several studies have shown that DNA (deoxyribonucleic acid) and chromosomal changes can occur in patients with both MOM and non-MOM hip implants.16-18 Techniques to accurately measure the levels of metal ions, including cobalt, chromium, and titanium in the serum, have improved substantially in recent years and have been used successfully in clinical applications with low detection limits.2,4,19,20 Evidence shows that pregnancy-related complications in women with well-functioning cemented, hybrid, or uncemented metal-on-polyethylene THA are not different from those in healthy women.21 However, it is unclear if metal ions can cross the placenta and negatively affect the development of a fetus in mothers with MOM-bearing THAs.22 We conducted this study to determine if metal ions can traverse the placenta by measuring serum metal ion concentrations in mothers with and without MOM THA and the corresponding levels in umbilical cord blood samples.
Materials and Methods
Ten patients were prospectively enrolled in this study, which was approved by the institutional review boards at all 3 participating hospitals prior to initiation. All patients provided informed consent and agreed to maternal and umbilical cord blood sampling. Seven of the 10 patients did not have any metallic implants and served as controls. The remaining 3 patients had either a MOM unilateral primary THA (1 patient) or unilateral MOM hip-resurfacing arthroplasty (2 patients) with no other metal implants in the body. For all subjects, maternal and umbilical cord blood was obtained at the time of delivery.
Group Demographics
The 3 women in the implant group had a mean age of 32.3 years (range, 23-39 years) at time of delivery. The first patient had posttraumatic osteoarthritis and underwent right THA using a modular MOM 60-mm acetabular component, a 36-mm cobalt chrome head, and a cementless, titanium proximally porous-coated femoral component (Pinnacle Total Hip System and Summit Total Hip System; DePuy Synthes, Warsaw, Indiana). Her infant was born 2 years after index THA. The second patient had a diagnosis of degenerative osteoarthritis secondary to developmental dysplasia of the hip and underwent a hybrid MOM hip resurfacing with a monoblock 50-mm cup and 40-mm cobalt chrome head (Conserve Plus; Wright Medical Technology, Arlington, Tennessee). She gave birth to her infant 6 years after her hip resurfacing. The third patient also had a diagnosis of degenerative osteoarthritis secondary to developmental dysplasia of the hip and underwent hip resurfacing with a 54-mm monoblock cup and 44-mm cobalt chrome head (Conserve Plus). Her infant was born 4 years after her resurfacing arthroplasty. All of the infants were born healthy, and the deliveries were uneventful and without complications. Seven women with a mean age of 32.1 years (range, 24-37 years) and their infants served as controls at the time of delivery. None of the women in the control group had a history of renal impairment, inherited genetic disorders, or metal implants.
Serum Metal Ion Analysis
Blood samples were collected using S-Monovette polypropylene syringes (Sarstedt, Princeton, New Jersey), a multi-adapter, and infusion set following an established technique.1 All vessels and utensils used for specimen collection were verified to be free of metal contamination. Three 10-mL syringes were drawn, and each syringe was labeled to indicate the sequence of collection. The first 10 mL were drawn to rinse the needle and adapter. Blood was then allowed to clot naturally and centrifuged at 1850 rpm for 30 minutes, separating samples into cell and serum fractions that were stored in labeled vials at -80ºC. All specimen manipulations after collection were carried out in a class-100 environment using a SterilGARD Biological Safety Cabinet (Baker, Sanford, Maine) and class-100 gloves (Oak Technical, Ravenna, Ohio) to minimize atmospheric and manual contamination. Maternal and umbilical cord blood metal ion levels were tested using high-resolution sector-field inductively-coupled plasma-mass spectrometry (HR-SF-ICPMS) (Element 2; Thermo Fisher Scientific, Bremen, Germany) following the method of additions as described previously.23 The HR-SF-ICPMS machine was equipped with an SC-E2 autosampler, Teflon nebulizer and spray chamber, sapphire injector (Elemental Scientific, Omaha, Nebraska) and platinum cones. All calibration and internal standard solutions were prepared by gradual dilutions of single-element standard solutions (1000 μg/mL from High Purity Standards, Charleston, South Carolina). The certified reference material, Seronorm Trace Elements Serum (SERO, Billingstad, Norway), were routinely analyzed with samples. The serum concentrations of cobalt, chromium, titanium, and nickel were measured with detection limits in ng/mL (parts per billion) of 0.04 for cobalt, 0.015 for chromium, 0.2 for titanium, and 0.17 for nickel.4 Concentrations below the detection limit were approximated as one-half of the detection limit by convention to calculate means.
Statistical Analysis
The data reported are the means for each group for each of the metal ion levels analyzed. Intergroup comparisons were made with the Mann-Whitney-Wilcoxon test using SPSS statistics software (SPSS Science Inc, Chicago, Illinois) to compare implant and control groups in regards to serum metal ion levels. Intragroup comparisons were made using the Friedman test with significance set at P < .05. Spearman rank-order correlation tests were used to investigate relationships between maternal and infant serum metal ion levels.
Results
The Table shows the mean serum metal ion levels of chromium, cobalt, titanium, and nickel for both groups. The implant-group mothers had significantly higher chromium and cobalt levels than the control-group mothers, with mean chromium levels of 1.87 ng/mL vs 0.16 ng/mL (P = .01) and mean cobalt levels of 0.97 ng/mL vs 0.20 ng/mL (P = .01), respectively. All control-group maternal chromium and cobalt levels were lower than the implant group. There were no significant differences detected between the implant-group and control-group mothers with respect to serum titanium or nickel levels.
The implant-group cord blood samples also had significantly higher chromium and cobalt levels than did the control-group infants with mean chromium levels of 0.29 ng/mL vs 0.10 ng/mL (P = .03) and mean cobalt levels of 0.49 ng/mL vs 0.16 ng/mL (P = .01), respectively. All but 1 of the control-group infants had chromium levels that were lower than the implant-group infant chromium levels. All of the control-group infant cobalt levels were lower than the implant-group infant cobalt levels. In the mother (I-1) who had a titanium-containing implant, her titanium level was 1.77 ng/mL and her cord blood level was 0.78 ng/mL. In contrast, the other 2 patients did not have titanium-containing implants and had corresponding metal levels of 0.10 ng/mL and cord blood levels either below the detection limit or just slightly above it. No statistically significant differences were found between the implant- and control-group infants with respect to serum titanium or nickel levels.
Considering the implant and control groups separately, we found no statistically significant differences between the maternal and infant titanium levels or the maternal and infant nickel levels. In the implant group, the mother’s chromium level was always higher than her infant’s chromium level, and the mother’s cobalt level was always higher than her infant’s cobalt level (P= .08). In the control group, there was no correlation between the maternal and infant chromium levels, or between the maternal and infant cobalt levels. In the implant group, the maternal and infant chromium levels were highly correlated (r = 1), as were the maternal and infant cobalt levels (r = 1).
When infants’ chromium levels were expressed as a percentage of their mothers’ chromium levels, the mean was 15.4% (range, 12.3%-18%) for the implant group and 58.9% (range, 13.5%-165.7%) for the control group (P = .05). The mean infant cobalt level, expressed as percentage of maternal cobalt level, was 50% (range, 45.8%-53.1%) for the implant group and 76.6% (range, 59.1%-150.8%) for the control group (P = .01).
Discussion
Cobalt and chromium serum metal ion levels obtained from mothers with MOM implants and umbilical cord samples were significantly elevated in comparison with controls. There was also a strong correlation between implant-group maternal cobalt and chromium levels and implant-group infant cobalt and chromium levels; however, no such correlation existed in the control group. Our results suggest that cobalt and chromium cross the placental barrier. Implant mothers had higher chromium and cobalt levels compared with implant babies, and these babies had approximately 15% of the level of chromium and 50% of the level of cobalt when compared to implant maternal levels. This finding suggests that the placenta modulates the transfer of chromium and cobalt to the fetus.
Two studies have reported chromium and cobalt levels in maternal and umbilical cord sera after MOM THA.5,24 Brodner and colleagues5 determined the maternal serum levels of cobalt and chromium in 3 women 3.8 years after MOM THA and compared those to cobalt and chromium levels obtained from umbilical cord blood. At the time of delivery, the maternal chromium concentrations in the 3 patients were 1.6 ng/mL, 0.5 ng/mL, and 0.9 ng/mL, and the cobalt concentrations were 1 ng/mL in 1 patient and below the detection limit in the other 2 patients. Cobalt and chromium concentrations of the 3 umbilical cord sera were below the detection limit. The authors concluded that cobalt and chromium did not cross the placenta based on their laboratory detection limits. Metal ion levels were measured using atomic absorption spectrometry with relatively high detection limits of 0.3 ng/mL, which is not as sensitive as the HR-SF-ICPMS technique used in the present study that has detection limits of 0.04 ng/mL for cobalt and 0.015 ng/mL for chromium. The relatively high detection limits of atomic absorption spectrometry were likely responsible for the authors’ inability to detect elevated chromium and cobalt levels in umbilical cord sera.
Ziaee and colleagues24 used HR-SF-ICPMS, as we did in this study, to measure the mean concentrations of cobalt and chromium ion levels in 10 maternal and umbilical cord blood samples in women with Birmingham MOM hip-resurfacing prostheses (Smith & Nephew, Warwick, United Kingdom). Nine of those patients had a unilateral resurfacing and 1 patient had bilateral-resurfacing prostheses. The mean maternal age was 31 years, and mean duration between hip resurfacing and delivery was 53 months. Ten normal controls were also tested with a mean maternal age of 30.9 years. The authors found that the mean cord blood level of cobalt in the study patients was 0.83 ng/mL, significantly higher (P < .01) than cobalt levels in the control group, which measured 0.33 ng/mL. The mean cord blood levels of chromium in the study and control groups were 0.37 ng/mL and 0.19 ng/mL, respectively. No children were reported to have evidence of congenital anomalies. Similar to our findings, they noted a modulatory effect on the transfer of metal ions across the placenta in patients with MOM prostheses.24 They reported the relative levels of cobalt and chromium in offspring to be 60.4% and 29.4% of the maternal ion levels, respectively. Control-group infants had mean cobalt and chromium levels that were 98.5% and 97.2% of mean maternal levels, respectively.
The transfer of metal ions across the placenta in control subjects is an expected finding because cobalt and chromium are essential trace elements required by the developing fetus. Rudge and colleagues25 estimated a transplacental transfer rate of 45% for cobalt in a series of 62 paired samples of maternal and cord blood. DeSouza and coauthors26 reported a series of 3 patients with MOM hip resurfacings who had the prosthesis in situ during pregnancy and found no teratogenic effects of metal ion transfer across the placenta. Umbilical cord blood chromium levels were less than 25% of the maternal serum levels and cord blood cobalt levels were approximately 50% that of maternal blood.26 In an animal experiment, Wallach and Verch18 also reported that maternal chromium levels can be decreased because of placental uptake.
Ziaee and colleagues24 tested metal ion levels using whole blood in contrast to serum, as we did in the present study. Daniel and coauthors16, who reported on the validity of serum levels as a surrogate measure of systemic exposure to metal ions in hip replacement, suggested that serum and whole blood metal ion levels cannot be interconverted because metal within cells are not in dynamic equilibrium with extracellular levels. They concluded that serum metal ion concentrations are not a useful surrogate measure of systemic metal ion exposure based on the wide variability seen in normalized and Bland-Altman scatterplots.16 However, it is important to note that Bland-Altman plots are user-dependent in determining significance, and results can vary based on the parameters tested. A high correlation does not automatically imply that there is a good agreement between 2 methods because a widespread sample could influence results. Whole blood analysis requires more processing steps, thus providing an increased chance of contamination and variability compared with serum metal level analysis. In our experiences, serum metal ion analysis has been shown to have accurate and reproducible results in clinical situations.2,4
While there is insufficient literature that specifically studies the effects of elevated metal ion levels on maternal and fetal subjects, there have been no reported negative effects in human babies even when maternal ion levels are elevated enough to be associated with ALTR. A case report by Fritzsche and colleagues27 reported a mother with bilateral MOM THA, a recurrent pseudotumor, and high blood levels of chromium (39 ng/mL) and cobalt (138 ng/mL) at 12 weeks gestation. The child was born at 38 weeks gestation with cord blood chromium and cobalt levels of 2.1 ng/mL and 75 ng/mL, respectively. The infant’s metal ion levels remained elevated at age 8 weeks with a chromium level of 2.5 ng/mL and cobalt level of 13 ng/mL and no signs of toxicity by age 14 weeks. In an animal model, Saxena and colleagues28 found that chromium in the hexavalent form passed through the placenta in mice and rats that were fed high doses of potassium dichromate. Trivalent chromium was not found to cross the placenta. In a follow-up study, Junaid and coauthors29 investigated the effects of elevated chromium levels in female mice given potassium dichromate in drinking water on days 14 to 19 of pregnancy. Animals receiving high-dose chromium had significantly higher incidences of postimplantation loss along with subdermal hemorrhagic patches and reduced ossification.29 Cobalt has not been shown to be teratogenic or cause fetotoxicity in a rat animal model given daily doses of as much as 100 mg/kg cobalt (II) chloride on days 6 to 15 of gestation.30
It is important to recognize that rodent data are limited and may not provide accurate translational insight into the effects of metal ions in human maternal and fetal subjects. Mammalian species have significant heterogeneity in the structure and function of their placentas. Rurak31 has shown that rodents have an additional persisting yolk sac placenta that allows the transfer of maternal immunoglobulins to the fetus. Humans, on the other hand, have a yolk sac placenta that regresses early in pregnancy. Differing placental biologic function makes it difficult to extrapolate the effects of metal ions in rodents to human subjects.
It is also important to note that serum levels of cobalt, chromium, and titanium can remain persistently elevated in well-functioning metal-on-polyethylene THA for several years and that elevated metal ion levels are not confined to MOM bearings.2 Levine and colleagues4 reported that serum levels of cobalt, chromium, and titanium remain persistently elevated after 10 years in a cohort of 27 well-functioning primary metal-on-polyethylene THA (hybrid, cobalt-chrome, titanium). Cobalt concentrations were elevated in all implants compared with controls at all follow-up periods through 10 years with absolute values less than 1 ng/mL. The authors noted that metal release at the modular femoral head-neck junctions was likely the dominant source of serum cobalt and chromium rather than passive dissolution. Hsu and colleagues32 have also shown that patients undergoing a second metal-on-polyethylene THA after primary THA have elevated serum metal ion levels (cobalt, chromium, titanium) up to 6 years after second surgery. Reported cobalt concentrations in patients with unilateral THA reached a maximum of 0.5 ng/mL during the follow-up course compared with 1.5 ng/mL for patients with bilateral THA. It is unknown what the potential metal ion transfer load would be in mothers with metal-on-polyethylene THA and associated taper corrosion to their infants.
Conclusion
Mothers with MOM-bearing implants and their children have higher cobalt and chromium levels than control subjects, demonstrating that the placenta is not a complete barrier to metal ion transport, although it seems to have a modulating effect. Physicians and women of child-bearing age should be aware of these findings when considering the use of MOM-bearing couples for THA. The effects of metal ions on long-term maternal and fetal health require research through serial clinical exams and metal ion level testing in prospective studies of different THA-bearing surfaces.
1. Jacobs JJ, Skipor AK, Black J, Urban R, Galante JO. Release and excretion of metal in patients who have a total hip-replacement component made of titanium-base alloy. J Bone Joint Surg Am. 1991;73(10):1475-1486.
2. Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80(10):1447-1458.
3. Jacobs JJ, Skipor AK, Urban RM, Black J, Manion LM, Galante JO. Transport of metal degradation products of titanium alloy total hip replacements to reticuloendothelial organs. An autopsy study. Trans Soc Biomater. 1994;18:318-325.
4. Levine BR, Hsu AR, Skipor AK, et al. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty: a concise follow-up of a previous report. J Bone Joint Surg Am. 2013;95(6):512-518.
5. Brodner W, Grohs JG, Bancher-Todesca D, et al. Does the placenta inhibit the passage of chromium and cobalt after metal-on-metal total hip arthroplasty? J Arthroplasty. 2004;19(8 suppl 3):102-106.
6. Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop. 2012;41(9):422-426.
7. Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(17):2847-2851.
8. Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Black J, Peoc’h M. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82(4):457-476.
9. Watters TS, Eward WC, Hallows RK, Dodd LG, Wellman SS, Bolognesi MP. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(7):1666-1669.
10. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87(1):28-36.
11. Nunley RM, Della Valle CJ, Barrack RL. Is patient selection important for hip resurfacing? Clin Orthop. 2009;467(1):56-65.
12. Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87(2):167-170.
13. Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation. Four to seven-year results. J Bone Joint Surg Am. 2000;82(6):789-798.
14. Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90(7):847-851.
15. Hartmann A, Hannemann F, Lutzner J, et al. Metal ion concentrations in body fluids after implantation of hip replacements with metal-on-metal bearing--systematic review of clinical and epidemiological studies. PLoS One. 2013;8(8):e70359.
16. Daniel J, Ziaee H, Pynsent PB, McMinn DJ. The validity of serum levels as a surrogate measure of systemic exposure to metal ions in hip replacement. J Bone Joint Surg Br. 2007;89(6):736-741.
17. Merritt K, Brown SA. Release of hexavalent chromium from corrosion of stainless steel and cobalt-chromium alloys. J Biomed Mater Res. 1995;29(5):627-633.
18. Wallach S, Verch RL. Placental transport of chromium. J Am Coll Nutr. 1984;3(1):69-74.
19. Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80(2):268-282.
20. Van Der Straeten C, Grammatopoulos G, Gill HS, Calistri A, Campbell P, De Smet KA. The 2012 Otto Aufranc Award: The interpretation of metal ion levels in unilateral and bilateral hip resurfacing. Clin Orthop. 2013;471(2):377-385.
21. Sierra RJ, Trousdale RT, Cabanela ME. Pregnancy and childbirth after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(1):21-24.
22. Antoniou J, Zukor DJ, Mwale F, Minarik W, Petit A, Huk OL. Metal ion levels in the blood of patients after hip resurfacing: a comparison between twenty-eight and thirty-six-millimeter-head metal-on-metal prostheses. J Bone Joint Surg Am. 2008;90(Suppl 3):142-148.
23. Iavicoli I, Falcone G, Alessandrelli M, et al. The release of metals from metal-on-metal surface arthroplasty of the hip. J Trace Elem Med Biol. 2006;20(1):25-31.
24. Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJ. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: a controlled study. J Bone Joint Surg Br. 2007;89(3):301-305.
25. Rudge CV, Rollin HB, Nogueira CM, Thomassen Y, Rudge MC, Odland JO. The placenta as a barrier for toxic and essential elements in paired maternal and cord blood samples of South African delivering women. J Environ Monit. 2009;11(7):1322-1330.
26. deSouza RM, Wallace D, Costa ML, Krikler SJ. Transplacental passage of metal ions in women with hip resurfacing: no teratogenic effects observed. Hip Int. 2012;22(1):96-99.
27. Fritzsche J, Borisch C, Schaefer C. Case report: High chromium and cobalt levels in a pregnant patient with bilateral metal-on-metal hip arthroplasties. Clin Orthop. 2012;470(8):2325-2331.
28. Saxena DK, Murthy RC, Jain VK, Chandra SV. Fetoplacental-maternal uptake of hexavalent chromium administered orally in rats and mice. Bull Environ Contam Toxicol. 1990;45(3):430-435.
29. Junaid M, Murthy RC, Saxena DK. Chromium fetotoxicity in mice during late pregnancy. Vet Hum Toxicol. 1995;37(4):320-323.
30. Paternain JL, Domingo JL, Corbella J. Developmental toxicity of cobalt in the rat. J Toxicol Environ Health. 1988;24(2):193-200.
31. Rurak DW. Development and function of the placenta. In: Harding R, Bocking AD, eds. Fetal Growth and Development. Cambridge, UK: Cambridge University Press; 2001.
32. Hsu AR, Levine BR, Skipor AK, Hallab NJ, Paprosky WG, Jacobs JJ. Effect of a second joint arthroplasty on metal ion levels after primary total hip arthroplasty. Am J Orthop. 2013;42(10):E84-E87.
1. Jacobs JJ, Skipor AK, Black J, Urban R, Galante JO. Release and excretion of metal in patients who have a total hip-replacement component made of titanium-base alloy. J Bone Joint Surg Am. 1991;73(10):1475-1486.
2. Jacobs JJ, Skipor AK, Patterson LM, et al. Metal release in patients who have had a primary total hip arthroplasty. A prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80(10):1447-1458.
3. Jacobs JJ, Skipor AK, Urban RM, Black J, Manion LM, Galante JO. Transport of metal degradation products of titanium alloy total hip replacements to reticuloendothelial organs. An autopsy study. Trans Soc Biomater. 1994;18:318-325.
4. Levine BR, Hsu AR, Skipor AK, et al. Ten-year outcome of serum metal ion levels after primary total hip arthroplasty: a concise follow-up of a previous report. J Bone Joint Surg Am. 2013;95(6):512-518.
5. Brodner W, Grohs JG, Bancher-Todesca D, et al. Does the placenta inhibit the passage of chromium and cobalt after metal-on-metal total hip arthroplasty? J Arthroplasty. 2004;19(8 suppl 3):102-106.
6. Hsu AR, Gross CE, Levine BR. Pseudotumor from modular neck corrosion after ceramic-on-polyethylene total hip arthroplasty. Am J Orthop. 2012;41(9):422-426.
7. Tower SS. Arthroprosthetic cobaltism: neurological and cardiac manifestations in two patients with metal-on-metal arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(17):2847-2851.
8. Urban RM, Jacobs JJ, Tomlinson MJ, Gavrilovic J, Black J, Peoc’h M. Dissemination of wear particles to the liver, spleen, and abdominal lymph nodes of patients with hip or knee replacement. J Bone Joint Surg Am. 2000;82(4):457-476.
9. Watters TS, Eward WC, Hallows RK, Dodd LG, Wellman SS, Bolognesi MP. Pseudotumor with superimposed periprosthetic infection following metal-on-metal total hip arthroplasty: a case report. J Bone Joint Surg Am. 2010;92(7):1666-1669.
10. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87(1):28-36.
11. Nunley RM, Della Valle CJ, Barrack RL. Is patient selection important for hip resurfacing? Clin Orthop. 2009;467(1):56-65.
12. Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87(2):167-170.
13. Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation. Four to seven-year results. J Bone Joint Surg Am. 2000;82(6):789-798.
14. Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90(7):847-851.
15. Hartmann A, Hannemann F, Lutzner J, et al. Metal ion concentrations in body fluids after implantation of hip replacements with metal-on-metal bearing--systematic review of clinical and epidemiological studies. PLoS One. 2013;8(8):e70359.
16. Daniel J, Ziaee H, Pynsent PB, McMinn DJ. The validity of serum levels as a surrogate measure of systemic exposure to metal ions in hip replacement. J Bone Joint Surg Br. 2007;89(6):736-741.
17. Merritt K, Brown SA. Release of hexavalent chromium from corrosion of stainless steel and cobalt-chromium alloys. J Biomed Mater Res. 1995;29(5):627-633.
18. Wallach S, Verch RL. Placental transport of chromium. J Am Coll Nutr. 1984;3(1):69-74.
19. Jacobs JJ, Gilbert JL, Urban RM. Corrosion of metal orthopaedic implants. J Bone Joint Surg Am. 1998;80(2):268-282.
20. Van Der Straeten C, Grammatopoulos G, Gill HS, Calistri A, Campbell P, De Smet KA. The 2012 Otto Aufranc Award: The interpretation of metal ion levels in unilateral and bilateral hip resurfacing. Clin Orthop. 2013;471(2):377-385.
21. Sierra RJ, Trousdale RT, Cabanela ME. Pregnancy and childbirth after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(1):21-24.
22. Antoniou J, Zukor DJ, Mwale F, Minarik W, Petit A, Huk OL. Metal ion levels in the blood of patients after hip resurfacing: a comparison between twenty-eight and thirty-six-millimeter-head metal-on-metal prostheses. J Bone Joint Surg Am. 2008;90(Suppl 3):142-148.
23. Iavicoli I, Falcone G, Alessandrelli M, et al. The release of metals from metal-on-metal surface arthroplasty of the hip. J Trace Elem Med Biol. 2006;20(1):25-31.
24. Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJ. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: a controlled study. J Bone Joint Surg Br. 2007;89(3):301-305.
25. Rudge CV, Rollin HB, Nogueira CM, Thomassen Y, Rudge MC, Odland JO. The placenta as a barrier for toxic and essential elements in paired maternal and cord blood samples of South African delivering women. J Environ Monit. 2009;11(7):1322-1330.
26. deSouza RM, Wallace D, Costa ML, Krikler SJ. Transplacental passage of metal ions in women with hip resurfacing: no teratogenic effects observed. Hip Int. 2012;22(1):96-99.
27. Fritzsche J, Borisch C, Schaefer C. Case report: High chromium and cobalt levels in a pregnant patient with bilateral metal-on-metal hip arthroplasties. Clin Orthop. 2012;470(8):2325-2331.
28. Saxena DK, Murthy RC, Jain VK, Chandra SV. Fetoplacental-maternal uptake of hexavalent chromium administered orally in rats and mice. Bull Environ Contam Toxicol. 1990;45(3):430-435.
29. Junaid M, Murthy RC, Saxena DK. Chromium fetotoxicity in mice during late pregnancy. Vet Hum Toxicol. 1995;37(4):320-323.
30. Paternain JL, Domingo JL, Corbella J. Developmental toxicity of cobalt in the rat. J Toxicol Environ Health. 1988;24(2):193-200.
31. Rurak DW. Development and function of the placenta. In: Harding R, Bocking AD, eds. Fetal Growth and Development. Cambridge, UK: Cambridge University Press; 2001.
32. Hsu AR, Levine BR, Skipor AK, Hallab NJ, Paprosky WG, Jacobs JJ. Effect of a second joint arthroplasty on metal ion levels after primary total hip arthroplasty. Am J Orthop. 2013;42(10):E84-E87.
Large Solitary Glomus Tumor of the Wrist Involving the Radial Artery
Glomus tumors are neoplasms that originate from normal glomus bodies in the skin and are most commonly found in the subungual areas of the digits.1 Glomus bodies are neuromyoarterial structures in the reticular dermis that serve as specialized arteriovenous anastomoses. These bodies contain afferent arterioles and efferent veins with multiple connections, and glomus cells have contractile properties because of their similarity to smooth muscle cells.1,2 Glomus bodies help regulate blood flow and temperature of the skin and are found in their largest concentration in the fingertips, palms of the hands, and soles of the feet.3,4
Glomus tumors represent hyperplastic glomus bodies and make up 1% to 4.5% of upper extremity neoplasms, with approximately 75% in the hand and 50% in the subungual area.1,5,6 These tumors can also present in multiple locations at once and can occur in atypical and ectopic locations.3 Although generally benign, glomus tumors can also exhibit malignant and metastatic potential in rare cases.7,8 They can also be locally aggressive with bony destruction of the distal phalynx.2,9,10 Tumors typically present as painful solitary soft-tissue lesions that are exquisitely tender to palpation, dark red-purple or bluish, and hypersensitive to cold.5,10 Van Geertruyden and colleagues10 reported that the diagnosis of glomus tumor can be made clinically in 90% of cases. However, glomus tumors can easily be mistaken for other lesions, such as hemangiomas, angiomas, neuromas, neurofibromas, lipomas, and ganglion cysts. An inaccurate or incomplete workup can result in persistent pain and symptoms along with intraoperative complications.3 Magnetic resonance imaging (MRI), the most sensitive imaging modality for detecting glomus tumors of the hand, can assist in the workup.3,11,12
Extradigital glomus tumors are difficult to diagnose because of their rarity and unspecific symptoms and presentation.13 Misdiagnosis and delayed diagnosis can result in significant chronic pain, disuse syndromes, and disability.1,10 Correct diagnosis and surgical resection are generally curative with complete resolution of symptoms.
In this article, we report a case of a large atypical glomus tumor that occurred on the wrist and involved the radial artery. This tumor was successfully treated with surgical excision. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 63-year-old man presented to clinic with an extremely tender soft-tissue mass on his nondominant, left wrist. The mass had been increasing in size for a year. It was painless at rest but very painful to light palpation, with referred pain proximally up to the shoulder.
The patient did not recall any traumatic or inciting event, had not undergone any prior workup or treatment for symptoms, and had no history of masses elsewhere on the body. Past medical history was significant for type 2 diabetes and colon and prostate cancer, which had been treated with chemotherapy and was now in remission.
Physical examination revealed a 2×2.5-cm well-circumscribed soft-tissue mass on the volar-radial aspect of the left wrist proximal to the thenar eminence and radial to the flexor carpi radialis tendon (Figure 1). The mass was soft, mobile, and nonfluctuant and did not transilluminate. The overlying skin was normal in color and appearance—no discoloration, erythema, wounds, or drainage. The radial artery was palpable, and the mass did not pulsate or have a bruit. The patient had normal wrist range of motion limited by pain on compression of the mass with motor and sensation intact throughout the hand. Plain radiographs of the wrist showed no bony pathology or involvement from the mass. A soft-tissue shadow was visible around the wrist without calcifications. A wrist MRI was performed to better evaluate the mass, and the T2-weighted images showed a heterogeneous subcutaneous mass adjacent to the radial artery with increased signal intensity from surrounding feeding vessels (Figure 2).
Given the clinical and imaging findings, there was concern for a possible vascular tumor. Therefore, excisional biopsy was recommended over needle biopsy because of the bleeding risk. With the patient under general anesthesia, and a tourniquet used without exsanguination, a Brunner-type zigzag incision was made centered over the mass with elevated skin flaps. The 2.7×2.6×1.1-cm mass was superficial and involved the radial artery (Figure 3). After the radial artery was dissected proximally and distally, 2 perforating vessels were found entering the mass. These vessels were ligated, which allowed the mass to be peeled completely off the artery. Histology with hematoxylin-eosin staining showed solid sheets of uniform round cells with interspersed capillaries and centrally placed nuclei without evidence of malignancy (Figure 4).
The tourniquet was released before skin closure, and adequate hemostasis was obtained. The wound was closed, and the patient was placed in a volar wrist splint for immobilization. Pain relief after excision of the mass was immediate, and the postoperative course uneventful. After surgery, immunohistochemistry of the mass showed minimal mitotic activity, with a positive immunoperoxidase stain for smooth muscle actin confirming a diagnosis of glomus tumor (Figure 5). At 3-year follow-up, the patient had no pain, symptoms, or tumor recurrence.
Discussion
Glomus tumors are an established cause of pain in the subungual areas of the hand; numerous cases have been reported.1,5,10,14 However, extradigital glomus tumors, particularly those involving the wrist, are rare, and only a few have been described. Given the lack of consistent findings and presentations, diagnosis is difficult. Case series have documented an overall 2:1 female-to-male predominance of glomus tumors,6 but extradigital tumors are more common in men (4.6:1 male-to-female ratio).3 Extradigital glomus tumors are commonly diagnosed between ages 40 and 80 years. Classic symptoms of subungual tumors include pain, localized tenderness, and cold hypersensitivity,1,10 but symptoms are much more variable with extradigital locations. Previous trauma or injury to the lesion area is reported in 20% to 30% of cases before symptom onset.3,15 Intravascular locations of glomus tumors are extremely rare; only 4 cases of tumors involving venous structures have been reported.16-19 In the present case, the patient’s main complaints were pain and localized tenderness associated with a progressively increasing mass without any history of trauma. The large size of his mass (~2.5 cm in diameter) on examination was unique, as was involvement of the radial artery.
Misdiagnosis and delayed diagnosis of extradigital glomus tumors are common, and symptoms such as chronic pain typically persist for 7 to 11 years before the correct diagnosis is made.1,10 On average, 2.5 physician consultants (including psychiatrists) evaluate the patient before glomus tumor is identified.10 There are other reports of atypical or ectopic glomus tumors taking 5 to 25 years to be diagnosed.20-22 The differential diagnosis for glomus tumors includes hemangiomas, cellular or cavernous hemangiomas, vascular tumors, neuromas, neurofibromas, lipomas, paragangliomas, ganglion cysts, pigmented nevi, Pacinian corpuscle hyperplasia, and foreign bodies. A key element of clinical diagnosis is the disproportionate amount of pain and localized tenderness caused by the lesion relative to its size. The hypersensitivity of this tumor is thought to result from enlargement of the tumor and impingement on nearby Pacinian corpuscles, nerve endings in the skin that are responsible for sensitivity to vibration and pressure.2,9
Plain radiographs can be useful in detecting glomus tumors of the hand but are less helpful with extradigital tumors, with identification rates of 24% in certain series.3 MRI is the most sensitive imaging modality for diagnosing glomus tumors of the hand; a detection rate of 80% to 100% has been reported in various case series.3,11,12 Specificity of MRI for glomus tumors has been reported at 50%.11,23 Placement of a radiographic marker directly over the area of most pain can assist in tumor localization.3 Glomus tumors typically have decreased signal intensity on T1-weighted images and increased intensity on T2-weighted images, but signal patterns are variable and particularly difficult to differentiate with small tumors. MRI is useful in the setting of recurrent glomus tumors, where incomplete excision is possible. In 24 cases of continued pain after glomus tumor excision, Theumann and colleagues24 used MRI to identify a nodule consistent with recurrent glomus tumor in all patients. Three-dimensional contrast-enhanced magnetic resonance angiography (MRA) can also help diagnose glomus tumors while providing valuable information regarding size and location for surgical planning.25,26 With MRA, it is crucial to evaluate the arterial or arteriovenous phase of imaging, as the glomus tumor is richly vascularized and shows contrast enhancement after intravenous injection of gadolinium.27 Angiography, ultrasonography, thermography, and scintigraphy have all been used to diagnose glomus tumors but have shown limited utility and accuracy.11
Treatment of glomus tumors is complete surgical excision because of their relatively small size and subcutaneous location. Resection success rates are consistently higher than 95%, with resolution of all symptoms.1,10,14 Local recurrence of tumors after excision occurs in 1% to 33% of cases, depending on series, and may be immediate or delayed, with immediate recurrence commonly caused by inadequate excision.1,10,15,28 Delayed recurrence is less common and presents several years after excision, typically with a new growth near the previous excision.10 Recurrence years after surgery may also represent multiple tumors unrecognized during initial workup and can be treated with repeat excision or radiotherapy.
Robert and colleagues29 recently reported the case of a glomus tumor, on the dorsal aspect of the wrist, discovered incidentally in a 71-year-old patient and treated with surgical excision. Several years earlier, Chim and colleagues30 described a similar case, of a large wrist glomus tumor worked up with MRI. In a retrospective review of all extradigital glomus tumors seen over a 20-year period, Schiefer and colleagues3 reported 4 glomus tumors of the wrist out of 56 tumors total. The most common sites were forearm (11 cases) and knee (10 cases), and the majority of patients presented with pain and localized tenderness. Mean tumor size was 0.66 cm (range, 0.1-0.3 cm), with 77% of tumors less than 1 cm. Our patient’s 2.7×2.6×1.1-cm tumor was large for a glomus tumor. Its involvement with the radial artery feeding vessels likely contributed to its large and progressively increasing size. It is worth noting that, in the series by Schiefer and colleagues,3 the only patient with symptoms persisting after excision had a large (3 cm in diameter) deep tumor of the foot; the entire tumor was removed, and there was no recurrence by 10-year follow-up. Folpe and colleagues7 suggested that deep tumors larger than 2 cm should be at higher suspicion for malignancy. Joseph and Posner21 reported 3 cases of glomus tumors, on the ulnar side of the wrist, diagnosed with help of a provocative test using ethyl chloride spray.
Conclusion
Overall, glomus tumors are rare and challenging to diagnosis and should be in the differential in any symptomatic patient with a painful soft-tissue mass of the wrist. Advanced imaging studies, such as MRI, can assist in localization, diagnosis, and preoperative planning. Histology and immunohistochemistry are essential to differentiate glomus tumor from other vascular tumors, and complete excision is necessary to prevent local recurrence.
1. Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972;54(4):691-703.
2. Riddell DH, Martin RS. Glomus tumor of unusual size; case report. Ann Surg. 1951;133(3):401-403.
3. Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81(10):1337-1344.
4. Tuncali D, Yilmaz AC, Terzioglu A, Aslan G. Multiple occurrences of different histologic types of the glomus tumor. J Hand Surg Am. 2005;30(1):161-164.
5. Greene RG. Soft tissue tumors of the hand and wrist. A 10 year survey. J Med Soc N J. 1964;61:495-498.
6. Maxwell GP, Curtis RM, Wilgis EF. Multiple digital glomus tumors. J Hand Surg Am. 1979;4(4):363-367.
7. Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25(1):1-12.
8. De Chiara A, Apice G, Mori S, et al. Malignant glomus tumour: a case report and review of the literature. Sarcoma. 2003;7(2):87-91.
9. Riveros M, Pack GT. The glomus tumor; report of 20 cases. Ann Surg. 1951;133(3):394-400.
10. Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21(2):257-260.
11. Al-Qattan MM, Al-Namla A, Al-Thunayan A, Al-Subhi F, El-Shayeb AF. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30(5):535-540.
12. Drape JL, Idy-Peretti I, Goettmann S, et al. Subungual glomus tumors: evaluation with MR imaging. Radiology. 1995;195(2):507-515.
13. Heys SD, Brittenden J, Atkinson P, Eremin O. Glomus tumour: an analysis of 43 patients and review of the literature. Br J Surg. 1992;79(4):345-347.
14. Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br. 2002;27(3):229-231.
15. Rettig AC, Strickland JW. Glomus tumor of the digits. J Hand Surg Am. 1977;2(4):261-265.
16. Beham A, Fletcher CD. Intravascular glomus tumour: a previously undescribed phenomenon. Virchows Arch A Pathol Anat Histopathol. 1991;418(2):175-177.
17. Googe PB, Griffin WC. Intravenous glomus tumor of the forearm. J Cutan Pathol. 1993;20(4):359-363.
18. Koibuchi H, Fujii Y, Taniguchi N. An unusual case of a glomus tumor developing in a subcutaneous vein of the wrist. J Clin Ultrasound. 2008;36(6):369-370.
19. Acebo E, Val-Bernal JF, Arce F. Giant intravenous glomus tumor. J Cutan Pathol. 1997;24(6):384-389.
20. Ghaly RF, Ring AM. Supraclavicular glomus tumor, 20 year history of undiagnosed shoulder pain: a case report. Pain. 1999;83(2):379-382.
21. Joseph FR, Posner MA. Glomus tumors of the wrist. J Hand Surg Am. 1983;8(6):918-920.
22. Abou Jaoude JF, Roula Farah A, Sargi Z, Khairallah S, Fakih C. Glomus tumors: report on eleven cases and a review of the literature. Chir Main. 2000;19(4):243-252.
23. Jablon M, Horowitz A, Bernstein DA. Magnetic resonance imaging of a glomus tumor of the fingertip. J Hand Surg Am. 1990;15(3):507-509.
24. Theumann NH, Goettmann S, Le Viet D, et al. Recurrent glomus tumors of fingertips: MR imaging evaluation. Radiology. 2002;223(1):143-151.
25. Boudghene FP, Gouny P, Tassart M, Callard P, Le Breton C, Vayssairat M. Subungual glomus tumor: combined use of MRI and three-dimensional contrast MR angiography. J Magn Reson Imaging. 1998;8(6):1326-1328.
26. Van Ruyssevelt CE, Vranckx P. Subungual glomus tumor: emphasis on MR angiography. AJR Am J Roentgenol. 2004;182(1):263-264.
27. Connell DA, Koulouris G, Thorn DA, Potter HG. Contrast-enhanced MR angiography of the hand. Radiographics. 2002;22(3):583-599.
28. Varian JP, Cleak DK. Glomus tumours in the hand. Hand. 1980;12(3):293-299.
29. Robert G, Sawaya E, Pelissier P. Glomus tumor of the dorsal aspect of the wrist: a case report [in French]. Chir Main. 2012;31(4):214-216.
30. Chim H, Lahiri A, Chew WY. Atypical glomus tumour of the wrist: a case report. Hand Surg. 2009;14(2-3):121-123.
Glomus tumors are neoplasms that originate from normal glomus bodies in the skin and are most commonly found in the subungual areas of the digits.1 Glomus bodies are neuromyoarterial structures in the reticular dermis that serve as specialized arteriovenous anastomoses. These bodies contain afferent arterioles and efferent veins with multiple connections, and glomus cells have contractile properties because of their similarity to smooth muscle cells.1,2 Glomus bodies help regulate blood flow and temperature of the skin and are found in their largest concentration in the fingertips, palms of the hands, and soles of the feet.3,4
Glomus tumors represent hyperplastic glomus bodies and make up 1% to 4.5% of upper extremity neoplasms, with approximately 75% in the hand and 50% in the subungual area.1,5,6 These tumors can also present in multiple locations at once and can occur in atypical and ectopic locations.3 Although generally benign, glomus tumors can also exhibit malignant and metastatic potential in rare cases.7,8 They can also be locally aggressive with bony destruction of the distal phalynx.2,9,10 Tumors typically present as painful solitary soft-tissue lesions that are exquisitely tender to palpation, dark red-purple or bluish, and hypersensitive to cold.5,10 Van Geertruyden and colleagues10 reported that the diagnosis of glomus tumor can be made clinically in 90% of cases. However, glomus tumors can easily be mistaken for other lesions, such as hemangiomas, angiomas, neuromas, neurofibromas, lipomas, and ganglion cysts. An inaccurate or incomplete workup can result in persistent pain and symptoms along with intraoperative complications.3 Magnetic resonance imaging (MRI), the most sensitive imaging modality for detecting glomus tumors of the hand, can assist in the workup.3,11,12
Extradigital glomus tumors are difficult to diagnose because of their rarity and unspecific symptoms and presentation.13 Misdiagnosis and delayed diagnosis can result in significant chronic pain, disuse syndromes, and disability.1,10 Correct diagnosis and surgical resection are generally curative with complete resolution of symptoms.
In this article, we report a case of a large atypical glomus tumor that occurred on the wrist and involved the radial artery. This tumor was successfully treated with surgical excision. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 63-year-old man presented to clinic with an extremely tender soft-tissue mass on his nondominant, left wrist. The mass had been increasing in size for a year. It was painless at rest but very painful to light palpation, with referred pain proximally up to the shoulder.
The patient did not recall any traumatic or inciting event, had not undergone any prior workup or treatment for symptoms, and had no history of masses elsewhere on the body. Past medical history was significant for type 2 diabetes and colon and prostate cancer, which had been treated with chemotherapy and was now in remission.
Physical examination revealed a 2×2.5-cm well-circumscribed soft-tissue mass on the volar-radial aspect of the left wrist proximal to the thenar eminence and radial to the flexor carpi radialis tendon (Figure 1). The mass was soft, mobile, and nonfluctuant and did not transilluminate. The overlying skin was normal in color and appearance—no discoloration, erythema, wounds, or drainage. The radial artery was palpable, and the mass did not pulsate or have a bruit. The patient had normal wrist range of motion limited by pain on compression of the mass with motor and sensation intact throughout the hand. Plain radiographs of the wrist showed no bony pathology or involvement from the mass. A soft-tissue shadow was visible around the wrist without calcifications. A wrist MRI was performed to better evaluate the mass, and the T2-weighted images showed a heterogeneous subcutaneous mass adjacent to the radial artery with increased signal intensity from surrounding feeding vessels (Figure 2).
Given the clinical and imaging findings, there was concern for a possible vascular tumor. Therefore, excisional biopsy was recommended over needle biopsy because of the bleeding risk. With the patient under general anesthesia, and a tourniquet used without exsanguination, a Brunner-type zigzag incision was made centered over the mass with elevated skin flaps. The 2.7×2.6×1.1-cm mass was superficial and involved the radial artery (Figure 3). After the radial artery was dissected proximally and distally, 2 perforating vessels were found entering the mass. These vessels were ligated, which allowed the mass to be peeled completely off the artery. Histology with hematoxylin-eosin staining showed solid sheets of uniform round cells with interspersed capillaries and centrally placed nuclei without evidence of malignancy (Figure 4).
The tourniquet was released before skin closure, and adequate hemostasis was obtained. The wound was closed, and the patient was placed in a volar wrist splint for immobilization. Pain relief after excision of the mass was immediate, and the postoperative course uneventful. After surgery, immunohistochemistry of the mass showed minimal mitotic activity, with a positive immunoperoxidase stain for smooth muscle actin confirming a diagnosis of glomus tumor (Figure 5). At 3-year follow-up, the patient had no pain, symptoms, or tumor recurrence.
Discussion
Glomus tumors are an established cause of pain in the subungual areas of the hand; numerous cases have been reported.1,5,10,14 However, extradigital glomus tumors, particularly those involving the wrist, are rare, and only a few have been described. Given the lack of consistent findings and presentations, diagnosis is difficult. Case series have documented an overall 2:1 female-to-male predominance of glomus tumors,6 but extradigital tumors are more common in men (4.6:1 male-to-female ratio).3 Extradigital glomus tumors are commonly diagnosed between ages 40 and 80 years. Classic symptoms of subungual tumors include pain, localized tenderness, and cold hypersensitivity,1,10 but symptoms are much more variable with extradigital locations. Previous trauma or injury to the lesion area is reported in 20% to 30% of cases before symptom onset.3,15 Intravascular locations of glomus tumors are extremely rare; only 4 cases of tumors involving venous structures have been reported.16-19 In the present case, the patient’s main complaints were pain and localized tenderness associated with a progressively increasing mass without any history of trauma. The large size of his mass (~2.5 cm in diameter) on examination was unique, as was involvement of the radial artery.
Misdiagnosis and delayed diagnosis of extradigital glomus tumors are common, and symptoms such as chronic pain typically persist for 7 to 11 years before the correct diagnosis is made.1,10 On average, 2.5 physician consultants (including psychiatrists) evaluate the patient before glomus tumor is identified.10 There are other reports of atypical or ectopic glomus tumors taking 5 to 25 years to be diagnosed.20-22 The differential diagnosis for glomus tumors includes hemangiomas, cellular or cavernous hemangiomas, vascular tumors, neuromas, neurofibromas, lipomas, paragangliomas, ganglion cysts, pigmented nevi, Pacinian corpuscle hyperplasia, and foreign bodies. A key element of clinical diagnosis is the disproportionate amount of pain and localized tenderness caused by the lesion relative to its size. The hypersensitivity of this tumor is thought to result from enlargement of the tumor and impingement on nearby Pacinian corpuscles, nerve endings in the skin that are responsible for sensitivity to vibration and pressure.2,9
Plain radiographs can be useful in detecting glomus tumors of the hand but are less helpful with extradigital tumors, with identification rates of 24% in certain series.3 MRI is the most sensitive imaging modality for diagnosing glomus tumors of the hand; a detection rate of 80% to 100% has been reported in various case series.3,11,12 Specificity of MRI for glomus tumors has been reported at 50%.11,23 Placement of a radiographic marker directly over the area of most pain can assist in tumor localization.3 Glomus tumors typically have decreased signal intensity on T1-weighted images and increased intensity on T2-weighted images, but signal patterns are variable and particularly difficult to differentiate with small tumors. MRI is useful in the setting of recurrent glomus tumors, where incomplete excision is possible. In 24 cases of continued pain after glomus tumor excision, Theumann and colleagues24 used MRI to identify a nodule consistent with recurrent glomus tumor in all patients. Three-dimensional contrast-enhanced magnetic resonance angiography (MRA) can also help diagnose glomus tumors while providing valuable information regarding size and location for surgical planning.25,26 With MRA, it is crucial to evaluate the arterial or arteriovenous phase of imaging, as the glomus tumor is richly vascularized and shows contrast enhancement after intravenous injection of gadolinium.27 Angiography, ultrasonography, thermography, and scintigraphy have all been used to diagnose glomus tumors but have shown limited utility and accuracy.11
Treatment of glomus tumors is complete surgical excision because of their relatively small size and subcutaneous location. Resection success rates are consistently higher than 95%, with resolution of all symptoms.1,10,14 Local recurrence of tumors after excision occurs in 1% to 33% of cases, depending on series, and may be immediate or delayed, with immediate recurrence commonly caused by inadequate excision.1,10,15,28 Delayed recurrence is less common and presents several years after excision, typically with a new growth near the previous excision.10 Recurrence years after surgery may also represent multiple tumors unrecognized during initial workup and can be treated with repeat excision or radiotherapy.
Robert and colleagues29 recently reported the case of a glomus tumor, on the dorsal aspect of the wrist, discovered incidentally in a 71-year-old patient and treated with surgical excision. Several years earlier, Chim and colleagues30 described a similar case, of a large wrist glomus tumor worked up with MRI. In a retrospective review of all extradigital glomus tumors seen over a 20-year period, Schiefer and colleagues3 reported 4 glomus tumors of the wrist out of 56 tumors total. The most common sites were forearm (11 cases) and knee (10 cases), and the majority of patients presented with pain and localized tenderness. Mean tumor size was 0.66 cm (range, 0.1-0.3 cm), with 77% of tumors less than 1 cm. Our patient’s 2.7×2.6×1.1-cm tumor was large for a glomus tumor. Its involvement with the radial artery feeding vessels likely contributed to its large and progressively increasing size. It is worth noting that, in the series by Schiefer and colleagues,3 the only patient with symptoms persisting after excision had a large (3 cm in diameter) deep tumor of the foot; the entire tumor was removed, and there was no recurrence by 10-year follow-up. Folpe and colleagues7 suggested that deep tumors larger than 2 cm should be at higher suspicion for malignancy. Joseph and Posner21 reported 3 cases of glomus tumors, on the ulnar side of the wrist, diagnosed with help of a provocative test using ethyl chloride spray.
Conclusion
Overall, glomus tumors are rare and challenging to diagnosis and should be in the differential in any symptomatic patient with a painful soft-tissue mass of the wrist. Advanced imaging studies, such as MRI, can assist in localization, diagnosis, and preoperative planning. Histology and immunohistochemistry are essential to differentiate glomus tumor from other vascular tumors, and complete excision is necessary to prevent local recurrence.
Glomus tumors are neoplasms that originate from normal glomus bodies in the skin and are most commonly found in the subungual areas of the digits.1 Glomus bodies are neuromyoarterial structures in the reticular dermis that serve as specialized arteriovenous anastomoses. These bodies contain afferent arterioles and efferent veins with multiple connections, and glomus cells have contractile properties because of their similarity to smooth muscle cells.1,2 Glomus bodies help regulate blood flow and temperature of the skin and are found in their largest concentration in the fingertips, palms of the hands, and soles of the feet.3,4
Glomus tumors represent hyperplastic glomus bodies and make up 1% to 4.5% of upper extremity neoplasms, with approximately 75% in the hand and 50% in the subungual area.1,5,6 These tumors can also present in multiple locations at once and can occur in atypical and ectopic locations.3 Although generally benign, glomus tumors can also exhibit malignant and metastatic potential in rare cases.7,8 They can also be locally aggressive with bony destruction of the distal phalynx.2,9,10 Tumors typically present as painful solitary soft-tissue lesions that are exquisitely tender to palpation, dark red-purple or bluish, and hypersensitive to cold.5,10 Van Geertruyden and colleagues10 reported that the diagnosis of glomus tumor can be made clinically in 90% of cases. However, glomus tumors can easily be mistaken for other lesions, such as hemangiomas, angiomas, neuromas, neurofibromas, lipomas, and ganglion cysts. An inaccurate or incomplete workup can result in persistent pain and symptoms along with intraoperative complications.3 Magnetic resonance imaging (MRI), the most sensitive imaging modality for detecting glomus tumors of the hand, can assist in the workup.3,11,12
Extradigital glomus tumors are difficult to diagnose because of their rarity and unspecific symptoms and presentation.13 Misdiagnosis and delayed diagnosis can result in significant chronic pain, disuse syndromes, and disability.1,10 Correct diagnosis and surgical resection are generally curative with complete resolution of symptoms.
In this article, we report a case of a large atypical glomus tumor that occurred on the wrist and involved the radial artery. This tumor was successfully treated with surgical excision. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 63-year-old man presented to clinic with an extremely tender soft-tissue mass on his nondominant, left wrist. The mass had been increasing in size for a year. It was painless at rest but very painful to light palpation, with referred pain proximally up to the shoulder.
The patient did not recall any traumatic or inciting event, had not undergone any prior workup or treatment for symptoms, and had no history of masses elsewhere on the body. Past medical history was significant for type 2 diabetes and colon and prostate cancer, which had been treated with chemotherapy and was now in remission.
Physical examination revealed a 2×2.5-cm well-circumscribed soft-tissue mass on the volar-radial aspect of the left wrist proximal to the thenar eminence and radial to the flexor carpi radialis tendon (Figure 1). The mass was soft, mobile, and nonfluctuant and did not transilluminate. The overlying skin was normal in color and appearance—no discoloration, erythema, wounds, or drainage. The radial artery was palpable, and the mass did not pulsate or have a bruit. The patient had normal wrist range of motion limited by pain on compression of the mass with motor and sensation intact throughout the hand. Plain radiographs of the wrist showed no bony pathology or involvement from the mass. A soft-tissue shadow was visible around the wrist without calcifications. A wrist MRI was performed to better evaluate the mass, and the T2-weighted images showed a heterogeneous subcutaneous mass adjacent to the radial artery with increased signal intensity from surrounding feeding vessels (Figure 2).
Given the clinical and imaging findings, there was concern for a possible vascular tumor. Therefore, excisional biopsy was recommended over needle biopsy because of the bleeding risk. With the patient under general anesthesia, and a tourniquet used without exsanguination, a Brunner-type zigzag incision was made centered over the mass with elevated skin flaps. The 2.7×2.6×1.1-cm mass was superficial and involved the radial artery (Figure 3). After the radial artery was dissected proximally and distally, 2 perforating vessels were found entering the mass. These vessels were ligated, which allowed the mass to be peeled completely off the artery. Histology with hematoxylin-eosin staining showed solid sheets of uniform round cells with interspersed capillaries and centrally placed nuclei without evidence of malignancy (Figure 4).
The tourniquet was released before skin closure, and adequate hemostasis was obtained. The wound was closed, and the patient was placed in a volar wrist splint for immobilization. Pain relief after excision of the mass was immediate, and the postoperative course uneventful. After surgery, immunohistochemistry of the mass showed minimal mitotic activity, with a positive immunoperoxidase stain for smooth muscle actin confirming a diagnosis of glomus tumor (Figure 5). At 3-year follow-up, the patient had no pain, symptoms, or tumor recurrence.
Discussion
Glomus tumors are an established cause of pain in the subungual areas of the hand; numerous cases have been reported.1,5,10,14 However, extradigital glomus tumors, particularly those involving the wrist, are rare, and only a few have been described. Given the lack of consistent findings and presentations, diagnosis is difficult. Case series have documented an overall 2:1 female-to-male predominance of glomus tumors,6 but extradigital tumors are more common in men (4.6:1 male-to-female ratio).3 Extradigital glomus tumors are commonly diagnosed between ages 40 and 80 years. Classic symptoms of subungual tumors include pain, localized tenderness, and cold hypersensitivity,1,10 but symptoms are much more variable with extradigital locations. Previous trauma or injury to the lesion area is reported in 20% to 30% of cases before symptom onset.3,15 Intravascular locations of glomus tumors are extremely rare; only 4 cases of tumors involving venous structures have been reported.16-19 In the present case, the patient’s main complaints were pain and localized tenderness associated with a progressively increasing mass without any history of trauma. The large size of his mass (~2.5 cm in diameter) on examination was unique, as was involvement of the radial artery.
Misdiagnosis and delayed diagnosis of extradigital glomus tumors are common, and symptoms such as chronic pain typically persist for 7 to 11 years before the correct diagnosis is made.1,10 On average, 2.5 physician consultants (including psychiatrists) evaluate the patient before glomus tumor is identified.10 There are other reports of atypical or ectopic glomus tumors taking 5 to 25 years to be diagnosed.20-22 The differential diagnosis for glomus tumors includes hemangiomas, cellular or cavernous hemangiomas, vascular tumors, neuromas, neurofibromas, lipomas, paragangliomas, ganglion cysts, pigmented nevi, Pacinian corpuscle hyperplasia, and foreign bodies. A key element of clinical diagnosis is the disproportionate amount of pain and localized tenderness caused by the lesion relative to its size. The hypersensitivity of this tumor is thought to result from enlargement of the tumor and impingement on nearby Pacinian corpuscles, nerve endings in the skin that are responsible for sensitivity to vibration and pressure.2,9
Plain radiographs can be useful in detecting glomus tumors of the hand but are less helpful with extradigital tumors, with identification rates of 24% in certain series.3 MRI is the most sensitive imaging modality for diagnosing glomus tumors of the hand; a detection rate of 80% to 100% has been reported in various case series.3,11,12 Specificity of MRI for glomus tumors has been reported at 50%.11,23 Placement of a radiographic marker directly over the area of most pain can assist in tumor localization.3 Glomus tumors typically have decreased signal intensity on T1-weighted images and increased intensity on T2-weighted images, but signal patterns are variable and particularly difficult to differentiate with small tumors. MRI is useful in the setting of recurrent glomus tumors, where incomplete excision is possible. In 24 cases of continued pain after glomus tumor excision, Theumann and colleagues24 used MRI to identify a nodule consistent with recurrent glomus tumor in all patients. Three-dimensional contrast-enhanced magnetic resonance angiography (MRA) can also help diagnose glomus tumors while providing valuable information regarding size and location for surgical planning.25,26 With MRA, it is crucial to evaluate the arterial or arteriovenous phase of imaging, as the glomus tumor is richly vascularized and shows contrast enhancement after intravenous injection of gadolinium.27 Angiography, ultrasonography, thermography, and scintigraphy have all been used to diagnose glomus tumors but have shown limited utility and accuracy.11
Treatment of glomus tumors is complete surgical excision because of their relatively small size and subcutaneous location. Resection success rates are consistently higher than 95%, with resolution of all symptoms.1,10,14 Local recurrence of tumors after excision occurs in 1% to 33% of cases, depending on series, and may be immediate or delayed, with immediate recurrence commonly caused by inadequate excision.1,10,15,28 Delayed recurrence is less common and presents several years after excision, typically with a new growth near the previous excision.10 Recurrence years after surgery may also represent multiple tumors unrecognized during initial workup and can be treated with repeat excision or radiotherapy.
Robert and colleagues29 recently reported the case of a glomus tumor, on the dorsal aspect of the wrist, discovered incidentally in a 71-year-old patient and treated with surgical excision. Several years earlier, Chim and colleagues30 described a similar case, of a large wrist glomus tumor worked up with MRI. In a retrospective review of all extradigital glomus tumors seen over a 20-year period, Schiefer and colleagues3 reported 4 glomus tumors of the wrist out of 56 tumors total. The most common sites were forearm (11 cases) and knee (10 cases), and the majority of patients presented with pain and localized tenderness. Mean tumor size was 0.66 cm (range, 0.1-0.3 cm), with 77% of tumors less than 1 cm. Our patient’s 2.7×2.6×1.1-cm tumor was large for a glomus tumor. Its involvement with the radial artery feeding vessels likely contributed to its large and progressively increasing size. It is worth noting that, in the series by Schiefer and colleagues,3 the only patient with symptoms persisting after excision had a large (3 cm in diameter) deep tumor of the foot; the entire tumor was removed, and there was no recurrence by 10-year follow-up. Folpe and colleagues7 suggested that deep tumors larger than 2 cm should be at higher suspicion for malignancy. Joseph and Posner21 reported 3 cases of glomus tumors, on the ulnar side of the wrist, diagnosed with help of a provocative test using ethyl chloride spray.
Conclusion
Overall, glomus tumors are rare and challenging to diagnosis and should be in the differential in any symptomatic patient with a painful soft-tissue mass of the wrist. Advanced imaging studies, such as MRI, can assist in localization, diagnosis, and preoperative planning. Histology and immunohistochemistry are essential to differentiate glomus tumor from other vascular tumors, and complete excision is necessary to prevent local recurrence.
1. Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972;54(4):691-703.
2. Riddell DH, Martin RS. Glomus tumor of unusual size; case report. Ann Surg. 1951;133(3):401-403.
3. Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81(10):1337-1344.
4. Tuncali D, Yilmaz AC, Terzioglu A, Aslan G. Multiple occurrences of different histologic types of the glomus tumor. J Hand Surg Am. 2005;30(1):161-164.
5. Greene RG. Soft tissue tumors of the hand and wrist. A 10 year survey. J Med Soc N J. 1964;61:495-498.
6. Maxwell GP, Curtis RM, Wilgis EF. Multiple digital glomus tumors. J Hand Surg Am. 1979;4(4):363-367.
7. Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25(1):1-12.
8. De Chiara A, Apice G, Mori S, et al. Malignant glomus tumour: a case report and review of the literature. Sarcoma. 2003;7(2):87-91.
9. Riveros M, Pack GT. The glomus tumor; report of 20 cases. Ann Surg. 1951;133(3):394-400.
10. Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21(2):257-260.
11. Al-Qattan MM, Al-Namla A, Al-Thunayan A, Al-Subhi F, El-Shayeb AF. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30(5):535-540.
12. Drape JL, Idy-Peretti I, Goettmann S, et al. Subungual glomus tumors: evaluation with MR imaging. Radiology. 1995;195(2):507-515.
13. Heys SD, Brittenden J, Atkinson P, Eremin O. Glomus tumour: an analysis of 43 patients and review of the literature. Br J Surg. 1992;79(4):345-347.
14. Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br. 2002;27(3):229-231.
15. Rettig AC, Strickland JW. Glomus tumor of the digits. J Hand Surg Am. 1977;2(4):261-265.
16. Beham A, Fletcher CD. Intravascular glomus tumour: a previously undescribed phenomenon. Virchows Arch A Pathol Anat Histopathol. 1991;418(2):175-177.
17. Googe PB, Griffin WC. Intravenous glomus tumor of the forearm. J Cutan Pathol. 1993;20(4):359-363.
18. Koibuchi H, Fujii Y, Taniguchi N. An unusual case of a glomus tumor developing in a subcutaneous vein of the wrist. J Clin Ultrasound. 2008;36(6):369-370.
19. Acebo E, Val-Bernal JF, Arce F. Giant intravenous glomus tumor. J Cutan Pathol. 1997;24(6):384-389.
20. Ghaly RF, Ring AM. Supraclavicular glomus tumor, 20 year history of undiagnosed shoulder pain: a case report. Pain. 1999;83(2):379-382.
21. Joseph FR, Posner MA. Glomus tumors of the wrist. J Hand Surg Am. 1983;8(6):918-920.
22. Abou Jaoude JF, Roula Farah A, Sargi Z, Khairallah S, Fakih C. Glomus tumors: report on eleven cases and a review of the literature. Chir Main. 2000;19(4):243-252.
23. Jablon M, Horowitz A, Bernstein DA. Magnetic resonance imaging of a glomus tumor of the fingertip. J Hand Surg Am. 1990;15(3):507-509.
24. Theumann NH, Goettmann S, Le Viet D, et al. Recurrent glomus tumors of fingertips: MR imaging evaluation. Radiology. 2002;223(1):143-151.
25. Boudghene FP, Gouny P, Tassart M, Callard P, Le Breton C, Vayssairat M. Subungual glomus tumor: combined use of MRI and three-dimensional contrast MR angiography. J Magn Reson Imaging. 1998;8(6):1326-1328.
26. Van Ruyssevelt CE, Vranckx P. Subungual glomus tumor: emphasis on MR angiography. AJR Am J Roentgenol. 2004;182(1):263-264.
27. Connell DA, Koulouris G, Thorn DA, Potter HG. Contrast-enhanced MR angiography of the hand. Radiographics. 2002;22(3):583-599.
28. Varian JP, Cleak DK. Glomus tumours in the hand. Hand. 1980;12(3):293-299.
29. Robert G, Sawaya E, Pelissier P. Glomus tumor of the dorsal aspect of the wrist: a case report [in French]. Chir Main. 2012;31(4):214-216.
30. Chim H, Lahiri A, Chew WY. Atypical glomus tumour of the wrist: a case report. Hand Surg. 2009;14(2-3):121-123.
1. Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972;54(4):691-703.
2. Riddell DH, Martin RS. Glomus tumor of unusual size; case report. Ann Surg. 1951;133(3):401-403.
3. Schiefer TK, Parker WL, Anakwenze OA, Amadio PC, Inwards CY, Spinner RJ. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81(10):1337-1344.
4. Tuncali D, Yilmaz AC, Terzioglu A, Aslan G. Multiple occurrences of different histologic types of the glomus tumor. J Hand Surg Am. 2005;30(1):161-164.
5. Greene RG. Soft tissue tumors of the hand and wrist. A 10 year survey. J Med Soc N J. 1964;61:495-498.
6. Maxwell GP, Curtis RM, Wilgis EF. Multiple digital glomus tumors. J Hand Surg Am. 1979;4(4):363-367.
7. Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25(1):1-12.
8. De Chiara A, Apice G, Mori S, et al. Malignant glomus tumour: a case report and review of the literature. Sarcoma. 2003;7(2):87-91.
9. Riveros M, Pack GT. The glomus tumor; report of 20 cases. Ann Surg. 1951;133(3):394-400.
10. Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21(2):257-260.
11. Al-Qattan MM, Al-Namla A, Al-Thunayan A, Al-Subhi F, El-Shayeb AF. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30(5):535-540.
12. Drape JL, Idy-Peretti I, Goettmann S, et al. Subungual glomus tumors: evaluation with MR imaging. Radiology. 1995;195(2):507-515.
13. Heys SD, Brittenden J, Atkinson P, Eremin O. Glomus tumour: an analysis of 43 patients and review of the literature. Br J Surg. 1992;79(4):345-347.
14. Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br. 2002;27(3):229-231.
15. Rettig AC, Strickland JW. Glomus tumor of the digits. J Hand Surg Am. 1977;2(4):261-265.
16. Beham A, Fletcher CD. Intravascular glomus tumour: a previously undescribed phenomenon. Virchows Arch A Pathol Anat Histopathol. 1991;418(2):175-177.
17. Googe PB, Griffin WC. Intravenous glomus tumor of the forearm. J Cutan Pathol. 1993;20(4):359-363.
18. Koibuchi H, Fujii Y, Taniguchi N. An unusual case of a glomus tumor developing in a subcutaneous vein of the wrist. J Clin Ultrasound. 2008;36(6):369-370.
19. Acebo E, Val-Bernal JF, Arce F. Giant intravenous glomus tumor. J Cutan Pathol. 1997;24(6):384-389.
20. Ghaly RF, Ring AM. Supraclavicular glomus tumor, 20 year history of undiagnosed shoulder pain: a case report. Pain. 1999;83(2):379-382.
21. Joseph FR, Posner MA. Glomus tumors of the wrist. J Hand Surg Am. 1983;8(6):918-920.
22. Abou Jaoude JF, Roula Farah A, Sargi Z, Khairallah S, Fakih C. Glomus tumors: report on eleven cases and a review of the literature. Chir Main. 2000;19(4):243-252.
23. Jablon M, Horowitz A, Bernstein DA. Magnetic resonance imaging of a glomus tumor of the fingertip. J Hand Surg Am. 1990;15(3):507-509.
24. Theumann NH, Goettmann S, Le Viet D, et al. Recurrent glomus tumors of fingertips: MR imaging evaluation. Radiology. 2002;223(1):143-151.
25. Boudghene FP, Gouny P, Tassart M, Callard P, Le Breton C, Vayssairat M. Subungual glomus tumor: combined use of MRI and three-dimensional contrast MR angiography. J Magn Reson Imaging. 1998;8(6):1326-1328.
26. Van Ruyssevelt CE, Vranckx P. Subungual glomus tumor: emphasis on MR angiography. AJR Am J Roentgenol. 2004;182(1):263-264.
27. Connell DA, Koulouris G, Thorn DA, Potter HG. Contrast-enhanced MR angiography of the hand. Radiographics. 2002;22(3):583-599.
28. Varian JP, Cleak DK. Glomus tumours in the hand. Hand. 1980;12(3):293-299.
29. Robert G, Sawaya E, Pelissier P. Glomus tumor of the dorsal aspect of the wrist: a case report [in French]. Chir Main. 2012;31(4):214-216.
30. Chim H, Lahiri A, Chew WY. Atypical glomus tumour of the wrist: a case report. Hand Surg. 2009;14(2-3):121-123.