User login
Should You Report a Substance-Abusing Colleague to the State Licensing Board?
PRO
Hospitalists’ moral obligation is to protect the patient
In this era of historic budget deficits, wars, and political strife surrounding healthcare reform, one might ask if we can afford to spend valuable time and energy on the issue of reporting physicians who abuse substances.
At first glance, I certainly had skepticism about the subject, but then I dug deeper. To my surprise (and likely yours), studies indicate that physicians develop substance-abuse problems as often or more than the general population does.1 Recent reports detail horrific patient outcomes at the hands of health providers whose actions are compromised by drug use. With data showing the prevalence of substance abuse among physicians hovering around 10% to 12%, we must accept the reality that hospitalists are not exempt.2,3,4,5
As medical doctors, our promise to our patients is to provide care in an ethical manner. Even if we try to live in denial, most of us would agree that with great blessing (or power) comes great responsibility. So when the question of reporting a fellow hospitalist who is abusing substances was asked, my response was unequivocally yes.
In my opinion, this discussion can be limited to two overarching principles: First, we are compelled to put our patients first. As hospitalists, we are blessed to be caring for some of the most frail and vulnerable in our society. Fortunately, an overwhelming number of us do so with pride, skill, and integrity.
The task of providing high-quality care to an empowered patient population is difficult enough with us being physically, emotionally, and mentally exhausted. But to add substance abuse to this is just a complete and utter violation of our patients’ trust. We must agree that putting our patients’ well-being beyond reproach requires us to report any colleague who is compromised.
Second, delayed help for a colleague in trouble with substance-abuse issues could be fatal—and for more than just that single colleague. At some point, we are compelled to do more than just raise an eyebrow and shake our head. Usually at the time of discovery, months if not years of substance abuse already have gone by undetected. Deferring to the next person is just not an option. There is too much at stake. It is our moral duty to help our colleagues who are unable to realize the danger they are posing to themselves, the team, and, most importantly, the patients.
Certainly, physicians do not need another lecture about the perils of substance abuse. Whether discussing prescription drugs, alcohol, marijuana, cocaine, or the like, we all have witnessed the devastating effects of abuse. The fact is, any substance that alters our ability to perform our trusted duty must be avoided.
Colleagues, the algorithm is simple: Be vigilant, observe, confirm, and report. It is our moral and ethical imperative.
Dr. Pyke is chief medical officer of Medicus Consulting, LLC.
CON
Responsible, helpful action doesn’t always mean official involvement
Recognizing impairment in our colleagues is both difficult and ethically challenging. Despite national trends, medicine remains a largely self-regulated profession, and we have an ethical obligation to report impaired, incompetent, or unethical colleagues. Rarely are the indications for reporting or identifying a colleague clear.
As trained clinicians, we know the signs of substance abuse:6
- Frequent tardiness and absences;
- Unexplained disappearances during working hours;
- Inappropriate behavior;
- Affective lability or irritability;
- Interpersonal conflict;
- Avoidance of peers or supervisors;
- Keeping odd hours;
- Disorganized and forgetful;
- Incomplete charts and work performance;
- Heavy drinking at social functions;
- Unexplained changes in weight or energy level;
- Diminished personal hygiene;
- Slurred or rapid speech;
- Frequently dilated pupils or red, watery eyes and a runny nose;
- Defensiveness, anxiety, apathy, and manipulative behaviors; and
- Withdrawal from long-standing relationships.
Yet when it is a colleague, we are often in denial about their substance abuse. Certainly, simple seasonal allergies and allergy medications can cause a number of the above symptoms. We also are aware of and fear the potential impact of licensing board notification on a physician’s career. In fact, in a national survey of physicians, 45% of respondents who had encountered impaired or incompetent physicians had not reported them, even though 96% of those surveyed agreed that physicians should report impaired or incompetent colleagues.7
Similar to reporting child or elder abuse, you don’t want to be wrong.
At the same time, impaired physicians are disruptive. They negatively impact the lives of their patients, colleagues, and hospital staff.
It is possible to do both the responsible thing and not go directly to the licensing board. You are not responsible for diagnosing your colleagues, but rather recognizing possible impairment.
Check out the Federation of State Physician Health Programs’ website (www.fsphp.org) to identify a local physician health program. Call them and place a report of concern identifying your impaired colleague. While it’s possibly new to you, they have years of experience working with this situation. Trust these organizations, many of which are independent from licensing, to intervene responsibly and confidentially. They can evaluate your colleague and provide a treatment plan and monitoring, as needed. Their approach is rehabilitative rather than punitive, and they resist reporting to the medical board unless the physician-patient is noncompliant.
Physicians have better outcomes than the general population, with reported abstinence rates of 70% to 90% for those who complete treatment.8,9 Between 75% and 85% of physicians who complete rehabilitation and comply with close monitoring and follow-up care are able to return to work.9,10
There is hope for your impaired colleague. Contact your local physician health program.
Dr. Guerrasio is a hospitalist and director of resident and medical student remediation at the University of Colorado Denver.
References
- Hughes PH, Brandenburg N, Baldwin DC Jr., et al. Prevalence of substance use among US physicians. JAMA. 1992;267:2333-2339.
- Gold KB, Teitelbaum SA. Physicians impaired by substance abuse disorders. The Journal of Global Drug Policy and Practice website. Available at: http://www.globaldrugpolicy.org/2/2/3.php. Accessed June 27, 2011.
- Wolfgang AP. Substance abuse potential and job stress: a study of pharmacists, physicians, and nurses. J Pharm Mark Manage. 1989;3(4):97-110.
- Cicala RS. Substance abuse among physicians: What you need to know. Hosp Phys. 2003:39-46.
- Berge KH, Seppala MD, Schipper AM. Chemical dependency and the physician. Mayo Clin Proc. 2009;84(7):625-631.
- Bright RP, Krahn L. Impaired physicians: How to recognize, when to report, and where to refer. Curr Psy. 2010;9(6):11-20.
- Campbell EG, Regan S, Gruen RL, et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med. 2007;147:795-802.
- Femino J, Nirenberg TD. Treatment outcome studies on physician impairment: a review of the literature. R I Med. 1994;77:345-350.
- Alpern F, Correnti CE, Dolan TE, Llufrio MC, Sill A. A survey of recovering Maryland physicians. Md Med J. 1992;41:301-303.
- Gallegos KV, Lubin BH, Bowers C, Blevins JW, Talbott GD, Wilson PO. Relapse and recovery: five to ten year follow-up study of chemically dependent physicians—the Georgia experience. Md Med J. 1992;41:315-319.
PRO
Hospitalists’ moral obligation is to protect the patient
In this era of historic budget deficits, wars, and political strife surrounding healthcare reform, one might ask if we can afford to spend valuable time and energy on the issue of reporting physicians who abuse substances.
At first glance, I certainly had skepticism about the subject, but then I dug deeper. To my surprise (and likely yours), studies indicate that physicians develop substance-abuse problems as often or more than the general population does.1 Recent reports detail horrific patient outcomes at the hands of health providers whose actions are compromised by drug use. With data showing the prevalence of substance abuse among physicians hovering around 10% to 12%, we must accept the reality that hospitalists are not exempt.2,3,4,5
As medical doctors, our promise to our patients is to provide care in an ethical manner. Even if we try to live in denial, most of us would agree that with great blessing (or power) comes great responsibility. So when the question of reporting a fellow hospitalist who is abusing substances was asked, my response was unequivocally yes.
In my opinion, this discussion can be limited to two overarching principles: First, we are compelled to put our patients first. As hospitalists, we are blessed to be caring for some of the most frail and vulnerable in our society. Fortunately, an overwhelming number of us do so with pride, skill, and integrity.
The task of providing high-quality care to an empowered patient population is difficult enough with us being physically, emotionally, and mentally exhausted. But to add substance abuse to this is just a complete and utter violation of our patients’ trust. We must agree that putting our patients’ well-being beyond reproach requires us to report any colleague who is compromised.
Second, delayed help for a colleague in trouble with substance-abuse issues could be fatal—and for more than just that single colleague. At some point, we are compelled to do more than just raise an eyebrow and shake our head. Usually at the time of discovery, months if not years of substance abuse already have gone by undetected. Deferring to the next person is just not an option. There is too much at stake. It is our moral duty to help our colleagues who are unable to realize the danger they are posing to themselves, the team, and, most importantly, the patients.
Certainly, physicians do not need another lecture about the perils of substance abuse. Whether discussing prescription drugs, alcohol, marijuana, cocaine, or the like, we all have witnessed the devastating effects of abuse. The fact is, any substance that alters our ability to perform our trusted duty must be avoided.
Colleagues, the algorithm is simple: Be vigilant, observe, confirm, and report. It is our moral and ethical imperative.
Dr. Pyke is chief medical officer of Medicus Consulting, LLC.
CON
Responsible, helpful action doesn’t always mean official involvement
Recognizing impairment in our colleagues is both difficult and ethically challenging. Despite national trends, medicine remains a largely self-regulated profession, and we have an ethical obligation to report impaired, incompetent, or unethical colleagues. Rarely are the indications for reporting or identifying a colleague clear.
As trained clinicians, we know the signs of substance abuse:6
- Frequent tardiness and absences;
- Unexplained disappearances during working hours;
- Inappropriate behavior;
- Affective lability or irritability;
- Interpersonal conflict;
- Avoidance of peers or supervisors;
- Keeping odd hours;
- Disorganized and forgetful;
- Incomplete charts and work performance;
- Heavy drinking at social functions;
- Unexplained changes in weight or energy level;
- Diminished personal hygiene;
- Slurred or rapid speech;
- Frequently dilated pupils or red, watery eyes and a runny nose;
- Defensiveness, anxiety, apathy, and manipulative behaviors; and
- Withdrawal from long-standing relationships.
Yet when it is a colleague, we are often in denial about their substance abuse. Certainly, simple seasonal allergies and allergy medications can cause a number of the above symptoms. We also are aware of and fear the potential impact of licensing board notification on a physician’s career. In fact, in a national survey of physicians, 45% of respondents who had encountered impaired or incompetent physicians had not reported them, even though 96% of those surveyed agreed that physicians should report impaired or incompetent colleagues.7
Similar to reporting child or elder abuse, you don’t want to be wrong.
At the same time, impaired physicians are disruptive. They negatively impact the lives of their patients, colleagues, and hospital staff.
It is possible to do both the responsible thing and not go directly to the licensing board. You are not responsible for diagnosing your colleagues, but rather recognizing possible impairment.
Check out the Federation of State Physician Health Programs’ website (www.fsphp.org) to identify a local physician health program. Call them and place a report of concern identifying your impaired colleague. While it’s possibly new to you, they have years of experience working with this situation. Trust these organizations, many of which are independent from licensing, to intervene responsibly and confidentially. They can evaluate your colleague and provide a treatment plan and monitoring, as needed. Their approach is rehabilitative rather than punitive, and they resist reporting to the medical board unless the physician-patient is noncompliant.
Physicians have better outcomes than the general population, with reported abstinence rates of 70% to 90% for those who complete treatment.8,9 Between 75% and 85% of physicians who complete rehabilitation and comply with close monitoring and follow-up care are able to return to work.9,10
There is hope for your impaired colleague. Contact your local physician health program.
Dr. Guerrasio is a hospitalist and director of resident and medical student remediation at the University of Colorado Denver.
References
- Hughes PH, Brandenburg N, Baldwin DC Jr., et al. Prevalence of substance use among US physicians. JAMA. 1992;267:2333-2339.
- Gold KB, Teitelbaum SA. Physicians impaired by substance abuse disorders. The Journal of Global Drug Policy and Practice website. Available at: http://www.globaldrugpolicy.org/2/2/3.php. Accessed June 27, 2011.
- Wolfgang AP. Substance abuse potential and job stress: a study of pharmacists, physicians, and nurses. J Pharm Mark Manage. 1989;3(4):97-110.
- Cicala RS. Substance abuse among physicians: What you need to know. Hosp Phys. 2003:39-46.
- Berge KH, Seppala MD, Schipper AM. Chemical dependency and the physician. Mayo Clin Proc. 2009;84(7):625-631.
- Bright RP, Krahn L. Impaired physicians: How to recognize, when to report, and where to refer. Curr Psy. 2010;9(6):11-20.
- Campbell EG, Regan S, Gruen RL, et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med. 2007;147:795-802.
- Femino J, Nirenberg TD. Treatment outcome studies on physician impairment: a review of the literature. R I Med. 1994;77:345-350.
- Alpern F, Correnti CE, Dolan TE, Llufrio MC, Sill A. A survey of recovering Maryland physicians. Md Med J. 1992;41:301-303.
- Gallegos KV, Lubin BH, Bowers C, Blevins JW, Talbott GD, Wilson PO. Relapse and recovery: five to ten year follow-up study of chemically dependent physicians—the Georgia experience. Md Med J. 1992;41:315-319.
PRO
Hospitalists’ moral obligation is to protect the patient
In this era of historic budget deficits, wars, and political strife surrounding healthcare reform, one might ask if we can afford to spend valuable time and energy on the issue of reporting physicians who abuse substances.
At first glance, I certainly had skepticism about the subject, but then I dug deeper. To my surprise (and likely yours), studies indicate that physicians develop substance-abuse problems as often or more than the general population does.1 Recent reports detail horrific patient outcomes at the hands of health providers whose actions are compromised by drug use. With data showing the prevalence of substance abuse among physicians hovering around 10% to 12%, we must accept the reality that hospitalists are not exempt.2,3,4,5
As medical doctors, our promise to our patients is to provide care in an ethical manner. Even if we try to live in denial, most of us would agree that with great blessing (or power) comes great responsibility. So when the question of reporting a fellow hospitalist who is abusing substances was asked, my response was unequivocally yes.
In my opinion, this discussion can be limited to two overarching principles: First, we are compelled to put our patients first. As hospitalists, we are blessed to be caring for some of the most frail and vulnerable in our society. Fortunately, an overwhelming number of us do so with pride, skill, and integrity.
The task of providing high-quality care to an empowered patient population is difficult enough with us being physically, emotionally, and mentally exhausted. But to add substance abuse to this is just a complete and utter violation of our patients’ trust. We must agree that putting our patients’ well-being beyond reproach requires us to report any colleague who is compromised.
Second, delayed help for a colleague in trouble with substance-abuse issues could be fatal—and for more than just that single colleague. At some point, we are compelled to do more than just raise an eyebrow and shake our head. Usually at the time of discovery, months if not years of substance abuse already have gone by undetected. Deferring to the next person is just not an option. There is too much at stake. It is our moral duty to help our colleagues who are unable to realize the danger they are posing to themselves, the team, and, most importantly, the patients.
Certainly, physicians do not need another lecture about the perils of substance abuse. Whether discussing prescription drugs, alcohol, marijuana, cocaine, or the like, we all have witnessed the devastating effects of abuse. The fact is, any substance that alters our ability to perform our trusted duty must be avoided.
Colleagues, the algorithm is simple: Be vigilant, observe, confirm, and report. It is our moral and ethical imperative.
Dr. Pyke is chief medical officer of Medicus Consulting, LLC.
CON
Responsible, helpful action doesn’t always mean official involvement
Recognizing impairment in our colleagues is both difficult and ethically challenging. Despite national trends, medicine remains a largely self-regulated profession, and we have an ethical obligation to report impaired, incompetent, or unethical colleagues. Rarely are the indications for reporting or identifying a colleague clear.
As trained clinicians, we know the signs of substance abuse:6
- Frequent tardiness and absences;
- Unexplained disappearances during working hours;
- Inappropriate behavior;
- Affective lability or irritability;
- Interpersonal conflict;
- Avoidance of peers or supervisors;
- Keeping odd hours;
- Disorganized and forgetful;
- Incomplete charts and work performance;
- Heavy drinking at social functions;
- Unexplained changes in weight or energy level;
- Diminished personal hygiene;
- Slurred or rapid speech;
- Frequently dilated pupils or red, watery eyes and a runny nose;
- Defensiveness, anxiety, apathy, and manipulative behaviors; and
- Withdrawal from long-standing relationships.
Yet when it is a colleague, we are often in denial about their substance abuse. Certainly, simple seasonal allergies and allergy medications can cause a number of the above symptoms. We also are aware of and fear the potential impact of licensing board notification on a physician’s career. In fact, in a national survey of physicians, 45% of respondents who had encountered impaired or incompetent physicians had not reported them, even though 96% of those surveyed agreed that physicians should report impaired or incompetent colleagues.7
Similar to reporting child or elder abuse, you don’t want to be wrong.
At the same time, impaired physicians are disruptive. They negatively impact the lives of their patients, colleagues, and hospital staff.
It is possible to do both the responsible thing and not go directly to the licensing board. You are not responsible for diagnosing your colleagues, but rather recognizing possible impairment.
Check out the Federation of State Physician Health Programs’ website (www.fsphp.org) to identify a local physician health program. Call them and place a report of concern identifying your impaired colleague. While it’s possibly new to you, they have years of experience working with this situation. Trust these organizations, many of which are independent from licensing, to intervene responsibly and confidentially. They can evaluate your colleague and provide a treatment plan and monitoring, as needed. Their approach is rehabilitative rather than punitive, and they resist reporting to the medical board unless the physician-patient is noncompliant.
Physicians have better outcomes than the general population, with reported abstinence rates of 70% to 90% for those who complete treatment.8,9 Between 75% and 85% of physicians who complete rehabilitation and comply with close monitoring and follow-up care are able to return to work.9,10
There is hope for your impaired colleague. Contact your local physician health program.
Dr. Guerrasio is a hospitalist and director of resident and medical student remediation at the University of Colorado Denver.
References
- Hughes PH, Brandenburg N, Baldwin DC Jr., et al. Prevalence of substance use among US physicians. JAMA. 1992;267:2333-2339.
- Gold KB, Teitelbaum SA. Physicians impaired by substance abuse disorders. The Journal of Global Drug Policy and Practice website. Available at: http://www.globaldrugpolicy.org/2/2/3.php. Accessed June 27, 2011.
- Wolfgang AP. Substance abuse potential and job stress: a study of pharmacists, physicians, and nurses. J Pharm Mark Manage. 1989;3(4):97-110.
- Cicala RS. Substance abuse among physicians: What you need to know. Hosp Phys. 2003:39-46.
- Berge KH, Seppala MD, Schipper AM. Chemical dependency and the physician. Mayo Clin Proc. 2009;84(7):625-631.
- Bright RP, Krahn L. Impaired physicians: How to recognize, when to report, and where to refer. Curr Psy. 2010;9(6):11-20.
- Campbell EG, Regan S, Gruen RL, et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med. 2007;147:795-802.
- Femino J, Nirenberg TD. Treatment outcome studies on physician impairment: a review of the literature. R I Med. 1994;77:345-350.
- Alpern F, Correnti CE, Dolan TE, Llufrio MC, Sill A. A survey of recovering Maryland physicians. Md Med J. 1992;41:301-303.
- Gallegos KV, Lubin BH, Bowers C, Blevins JW, Talbott GD, Wilson PO. Relapse and recovery: five to ten year follow-up study of chemically dependent physicians—the Georgia experience. Md Med J. 1992;41:315-319.
Hospitalist‐Run Acute Care for Elderly
For the frail older patient, hospitalization marks a period of high risk of poor outcomes and adverse events including functional decline, delirium, pressure ulcers, adverse drug events, nosocomial infections, and falls.1, 2 Physician recognition of elderly patients at risk for adverse outcomes is poor, making it difficult to intervene to prevent them.3, 4 Among frail, elderly inpatients at an urban academic medical center, doctors documented cognitive assessments in only 5% of patients. Functional assessments are appropriately documented in 40%80% of inpatients.3, 5
The Acute Care for Elders (ACE) unit is one of several models of comprehensive inpatient geriatric care that have been developed by geriatrician researchers to address the adverse events and functional decline that often accompany hospitalization.6 The ACE unit model generally incorporates: 1) a modified hospital environment, 2) early assessment and intensive management to minimize the adverse effects of hospital care, 3) early discharge planning, 4) patient centered care protocols, and 5) a consistent nursing staff.7 Two randomized, controlled trials have shown the ACE unit model to be successful in reducing functional decline among frail older inpatients during and after hospitalization.7, 8 While meta‐analyses data also suggests the ACE unit model reduces functional decline and future institutionalization, significant impact on other outcomes is not proven.9, 10
Several barriers have prevented the successful dissemination of the ACE unit model. The chief limitations are the upfront resources required to create and maintain a modified, dedicated unit, as well as the lack of a geriatrics trained workforce.7, 1113 The rapid growth of hospital medicine presents opportunities for innovation in the care of older patients. Still, a 2006 census demonstrated that few hospitalist groups had identified geriatric care as a priority.14
In response to these challenges, the University of Colorado Hospital Medicine Group created a hospitalist‐run inpatient medical service designed for the care of the frail older patient. This Hospitalist‐Acute Care for the Elderly (Hospitalist‐ACE) unit is a hybrid of a general medical service and an inpatient geriatrics unit.7 The goals of the Hospitalist‐ACE service are to provide high quality care tailored to older inpatients, thus minimizing the risks of functional decline and adverse events associate with hospitalization, and to provide a clinical geriatrics teaching experience for Hospitalist Training Track Residents within the Internal Medicine Residency Training Program and medical students at the University of Colorado Denver School of Medicine. The Hospitalist‐ACE unit is staffed with a core group of hospitalist attendings who have, at a minimum, attended an intensive mini‐course in inpatient geriatrics. The service employs interdisciplinary rounds; a brief, standardized geriatric assessment including screens of function, cognition, and mood; a clinical focus on mitigating the hazards of hospitalization, early discharge planning; and a novel geriatric educational curriculum for medicine residents and medical students.
This article will: 1) describe the creation of the Hospitalist‐ACE service at the University of Colorado Hospital; and 2) summarize the evaluation of the Hospitalist‐ACE service in a quasi‐randomized, controlled manner during its first year. We hypothesized that, when compared to patients receiving usual care, patients cared for on the Hospitalist‐ACE service would have increased recognition of abnormal functional status; recognition of abnormal cognitive status and delirium; equivalent lengths of stay and hospital charges; and decreased falls, 30‐day readmissions, and restraint use.
METHODS
Design
We performed a quasi‐randomized, controlled study of the Hospitalist‐ACE service.
Setting
The study setting was the inpatient general medical services of the Anschutz Inpatient Pavilion (AIP) of the University of Colorado Hospital (UCH). The AIP is a 425‐bed tertiary care hospital that is the major teaching affiliate of the University of Colorado School of Medicine and a regional referral center. The control services, hereafter referred to as usual care, were comprised of the four inpatient general medicine teaching services that take admissions on a four‐day rotation (in general, two were staffed by outpatient general internists and medical subspecialists, and two were staffed by academic hospitalists). The Hospitalist‐ACE service was a novel hospitalist teaching service that began in July 2007. Hospitalist‐ACE patients were admitted to a single 12‐bed medical unit (12 West) when beds were available; 12 West is similar to the other medical/surgical units at UCH and did not have any modifications to the rooms, equipment, or common areas for the intervention. The nursing staff on this unit had no formal geriatric nursing training. The Hospitalist‐ACE team admitted patients daily (between 7 AM and 3 PM MondayFriday; between 7 AM and 12 noon Saturday and Sunday). Patients assigned to the Hospitalist‐ACE service after hours were admitted by the internal medicine resident on call for the usual care services and handed off to the Hospitalist‐ACE team at 7 AM the next morning.
Study Subjects
Eligible subjects were inpatients age 70 years admitted to the usual care or Hospitalist‐ACE services at the AIP from November 2, 2007 to April 15, 2008. All patients age 70 years were randomized to the Hospitalist‐ACE service or usual care on a general internal medicine service by the last digit of the medical record number (odd numbers admitted to the Hospitalist‐ACE service and even numbers admitted to usual care). Patients followed by the Hospitalist‐ACE service but not admitted to 12 West were included in the study. To isolate the impact of the intervention, patients admitted to a medicine subspecialty service (such as cardiology, pulmonary, or oncology), or transferred to or from the Hospitalist‐ACE or control services to another service (eg, intensive care unit [ICU] or orthopedic surgery service) were excluded from the study.
Intervention
The Hospitalist‐ACE unit implemented an interdisciplinary team approach to identify and address geriatric syndromes in patients aged 70 and over. The Hospitalist‐ACE model of care consisted of clinical care provided by a hospitalist attending with additional training in geriatric medicine, administration of standardized geriatric screens assessing function, cognition, and mood, 15 minute daily (MondayFriday) interdisciplinary rounds focusing on recognition and management of geriatric syndromes and early discharge planning, and a standardized educational curriculum for medical residents and medical students addressing hazards of hospitalization.
The Hospitalist‐ACE service was a unique rotation within the Hospitalist Training Track of the Internal Medicine Residency that was developed with the support of the University of Colorado Hospital and the Internal Medicine Residency Training Program, and input from the Geriatrics Division at the University of Colorado Denver. The director received additional training from the Donald W. Reynolds FoundationUCLA Faculty Development to Advance Geriatric Education Mini‐Fellowship for hospitalist faculty. The mission of the service was to excel at educating the next generation of hospitalists while providing a model for excellence of care for hospitalized elderly patients. Important stakeholders were identified, and a leadership teamincluding representatives from nursing, physical and occupational therapy, pharmacy, social work, case management, and later, volunteer servicescreated the model daily interdisciplinary rounds. As geographic concentration was essential for the viability of interdisciplinary rounds, one unit (12 West) within the hospital was designated as the preferred location for patients admitted to the Hospitalist‐ACE service.
The Hospitalist‐ACE unit team consisted of one attending hospitalist, one resident, one intern, and medical students. The attending was one of five hospitalists, with additional training in geriatric medicine, who rotated attending responsibilities on the service. One of the hospitalists was board certified in geriatric medicine. Each of the other four hospitalists attended the Reynolds FoundationUCLA mini‐fellowship in geriatric medicine. Hospitalist‐ACE attendings rotated on a variety of other hospitalist services throughout the academic year, including the usual care services.
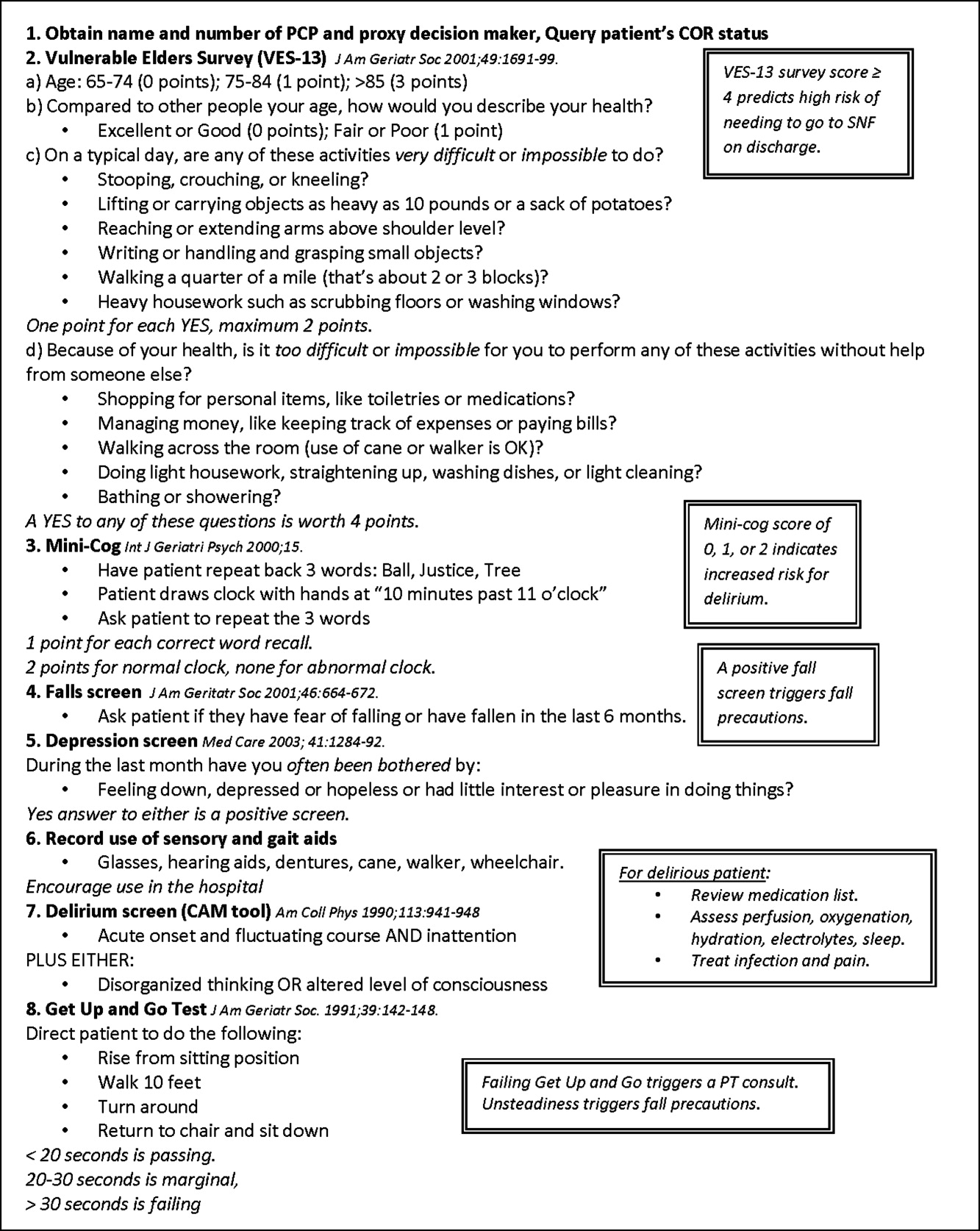
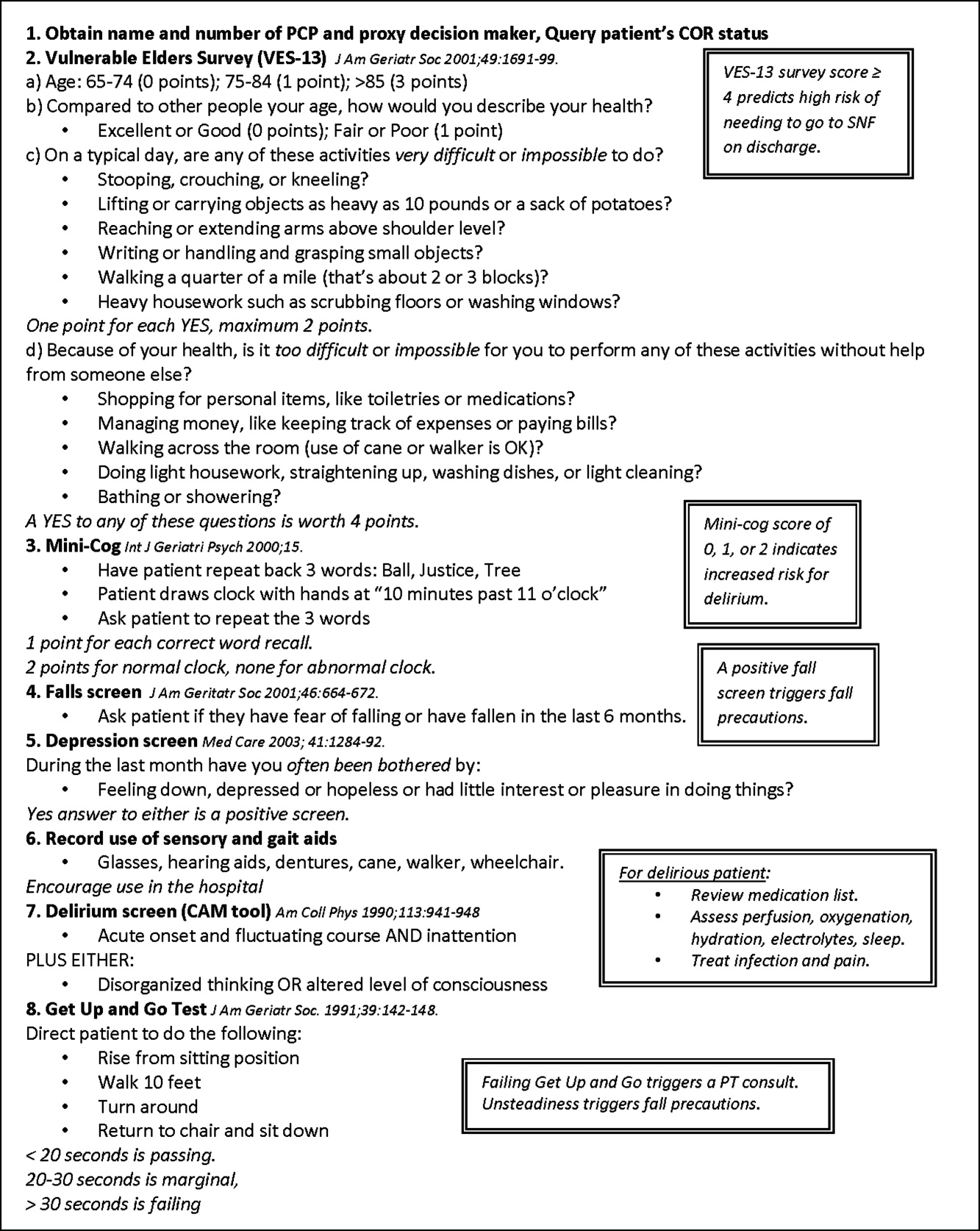
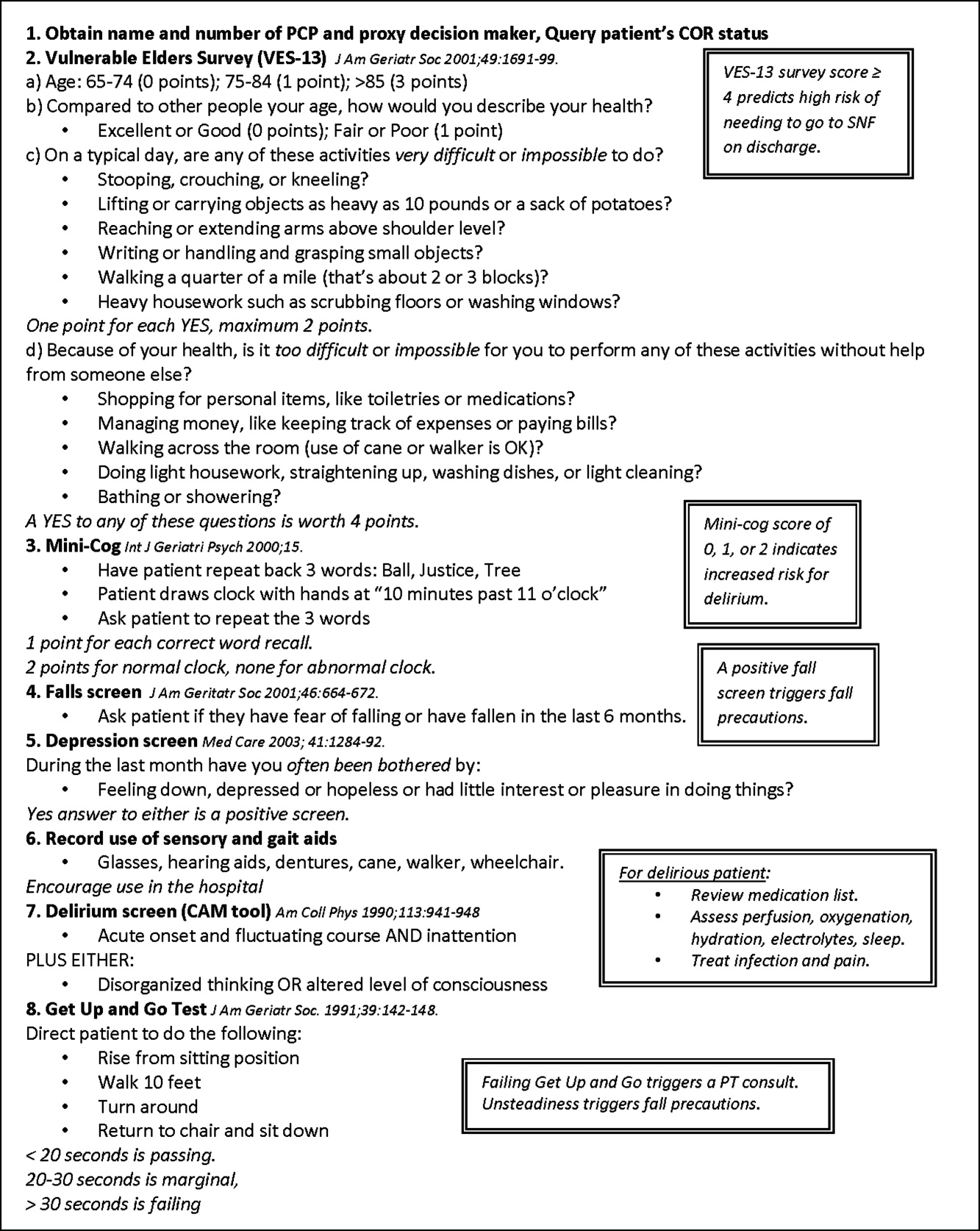
The brief standardized geriatric assessment consisted of six validated instruments, and was completed by house staff or medical students on admission, following instruction by the attending physician. The complete assessment tool is shown in Figure 1. The cognitive items included the Mini‐Cog,15 a two‐item depression screen,16 and the Confusion Assessment Method.17 The functional items included the Vulnerable Elders Survey (VES‐13),18 the Timed Get Up and Go test,19 and a two‐question falls screen.20 The elements of the assessment tool were selected by the Hospitalist‐ACE attendings for brevity and the potential to inform clinical management. To standardize the clinical and educational approach, the Hospitalist‐ACE attendings regularly discussed appropriate orders recommended in response to each positive screen, but no templated order sets were used during the study period.
Interdisciplinary rounds were attended by Hospitalist‐ACE physicians, nurses, case managers, social workers, physical or occupational therapists, pharmacists, and volunteers. Rounds were led by the attending or medical resident.
The educational curriculum encompassed 13 modules created by the attending faculty that cover delirium, falls, dementia, pressure ulcers, physiology of aging, movement disorders, medication safety, end of life care, advance directives, care transitions, financing of health care for the elderly, and ethical conundrums in the care of the elderly. A full table of contents appears in online Appendix 1. Additionally, portions of the curriculum have been published online.21, 22 Topic selection was guided by the Accreditation Council for Graduate Medical Education (ACGME) core geriatrics topics determined most relevant for the inpatient setting. Formal instruction of 3045 minutes duration occurred three to four days a week and was presented in addition to routine internal medicine educational conferences. Attendings coordinated teaching to ensure that each trainee was exposed to all of the content during the course of their four‐week rotation.
In contrast to the Hospitalist‐ACE service, usual care on the control general medical services consisted of either a hospitalist, a general internist, or an internal medicine subspecialist attending physician, with one medical resident, one intern, and medical students admitting every fourth day. The general medical teams attended daily discharge planning rounds with a discharge planner and social worker focused exclusively on discharge planning. The content of teaching rounds on the general medical services was largely left to the discretion of the attending physician.
This program evaluation of the Hospitalist‐ACE service was granted a waiver of consent and Health Insurance Portability and Accountability Act (HIPAA) by the Colorado Multiple Institutional Review Board.
Measures
Primary Outcome
The primary outcome for the study was the recognition of abnormal functional status by the primary team. Recognition of abnormal functional status was determined from chart review and consisted of both the physician's detection of abnormal functional status and evidence of a corresponding treatment plan identified in the notes or orders of a physician member of the primary team (Table 1).
| Measure | Criterion | Source | Content Examples |
|---|---|---|---|
| |||
| Recognition of abnormal functional status* | 1) Detection | MD's documentation of history | Presentation with change in function (new gait instability); use of gait aides (wheelchair) |
| OR | |||
| MD's documentation of physical exam | Observation of abnormal gait (eg, unsteady, wide‐based, shuffling) and/or balance Abnormal Get Up and Go test | ||
| AND | |||
| 2) Treatment | MD's order | PT/OT consult; home safety evaluation | |
| OR | |||
| MD's documentation assessment/plan | Inclusion of functional status (rehabilitation, PT/OT needs) on the MD's problem list | ||
| Recognition of abnormal cognitive status | Any of the following: | ||
| Delirium | 1) Detection | MD's history | Presentation of confusion or altered mental status |
| OR | |||
| MD's physical exam | Abnormal confusion assessment method | ||
| AND | |||
| 2) Treatment | MD's order | Sitter, reorienting communication, new halperidol order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of delirium on the problem list | ||
| OR | |||
| Dementia | 1) Detection | MD's history | Dementia in medical history |
| OR | OR | ||
| MD's physical exam | Abnormal Folstein Mini‐Mental Status Exam or Mini‐Cog | ||
| AND | |||
| 2) Treatment | MD's order | Cholinesterase inhibitor ordered | |
| OR | OR | ||
| MD's documentation of assessment/plan | Inclusion of dementia on the problem list | ||
| OR | |||
| Depression | 1) Detection | MD's history | Depression in medical history |
| OR | OR | ||
| MD's physical exam | Positive depression screen | ||
| AND | |||
| 2) Treatment | MD's order | New antidepressant order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of depression on the problem list | ||
Secondary Outcomes
Recognition of abnormal cognitive status was determined from chart review and consisted of both the physician's detection of dementia, depression, or delirium, and evidence of a corresponding treatment plan for any of the documented conditions identified in the notes or orders of a physician member of the primary team (Table 1). Additionally, we measured recognition and treatment of delirium alone.
Falls were determined from mandatory event reporting collected by the hospital on the University Hospitals Consortium Patient Safety Net web‐based reporting system and based on clinical assessment as reported by the nursing staff. The reports are validated by the appropriate clinical managers within 45 days of the event according to standard procedure.
Physical restraint use (type of restraint and duration) was determined from query of mandatory clinical documentation in the electronic medical record. Use of sleep aids was determined from review of the physician's order sheets in the medical record. The chart review captured any of 39 commonly prescribed hypnotic medications ordered at hour of sleep or for insomnia. The sleep medication list was compiled with the assistance of a pharmacist for an earlier chart review and included non‐benzodiazepine hypnotics, benzodiazepines, antidepressants, antihistamines, and antipsychotics.23
Length of stay, hospital charges, 30‐day readmissions to UCH (calculated from date of discharge), and discharge location were determined from administrative data.
Additional Descriptive Variables
Name, medical record number, gender, date of birth, date of admission and discharge, and primary diagnosis were obtained from the medical record. The Case Mix Index for each group of patients was determined from the average Medicare Severity‐adjusted Diagnosis Related Group (MS‐DRG) weight obtained from administrative data.
Data Collection
A two‐step, retrospective chart abstraction was employed. A professional research assistant (P.R.A.) hand‐abstracted process measures from the paper medical chart onto a data collection form designed for this study. A physician investigator performed a secondary review (H.L.W.). Discrepancies were resolved by the physician reviewer.
Data Analysis
Descriptive statistics were performed on intervention and control subjects. Means and standard deviations (age) or frequencies (gender, primary diagnoses) were calculated as appropriate. T tests were used for continuous variables, chi‐square tests for gender, and the Wilcoxon rank sum test for categorical variables.
Outcomes were reported as means and standard deviations for continuous variables (length of stay and charges) and frequencies for categorical variables (all other outcomes). T tests were used for continuous variables, Fisher's exact test for restraint use, and chi‐square tests were used for categorical variable to compare the impact of the intervention between intervention and control patients. For falls, confidence intervals were calculated for the incidence rate differences based on Poisson approximations.
Sample Size Considerations
An a priori sample size calculation was performed. A 2001 study showed that functional status is poorly documented in at least 60% of hospital charts of elderly patients.5 Given an estimated sample size of 120 per group and a power of 80%, this study was powered to be able to detect an absolute difference in the documentation of functional status of as little as 18%.
RESULTS
Two hundred seventeen patients met the study entry criteria (Table 2): 122 were admitted to the Hospitalist‐ACE service, and 95 were admitted to usual care on the general medical services. The average age of the study patients was 80.5 years, 55.3% were female. Twenty‐eight percent of subjects were admitted for pulmonary diagnoses. The two groups of patients were similar with respect to age, gender, and distribution of primary diagnoses. The Hospitalist‐ACE patients had a mean MS‐DRG weight of 1.15, which was slightly higher than that of usual care patients at 1.05 (P = 0.06). Typically, 70% of Hospitalist‐ACE patients are admitted to the designated ACE medical unit (12 West).
| Characteristic | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Age (years), mean (SD) | 80.5 (6.5) | 80.7 (7.0) | 0.86 |
| Gender (% female) | 52.5 | 59 | 0.34 |
| Case Mix Index (mean MS‐DRG weight [SD]) | 1.15 (0.43) | 1.05 (0.31) | 0.06 |
| Primary ICD‐9 diagnosis (%) | 0.59 | ||
| Pulmonary | 27.9 | 28.4 | |
| General medicine | 15.6 | 11.6 | |
| Surgery | 13.9 | 11.6 | |
| Cardiology | 9.8 | 6.3 | |
| Nephrology | 8.2 | 7.4 | |
Processes of Care
Processes of care for older patients are displayed in Table 3. Patients on the Hospitalist‐ACE service had recognition and treatment of abnormal functional status at a rate that was nearly double that of patients on the usual care services (68.9% vs 35.8%, P < 0.0001). In addition, patients on the Hospitalist‐ACE service were significantly more likely to have had recognition and treatment of any abnormal cognitive status (55.7% vs 40.0%, P = 0.02). When delirium was evaluated alone, the Hospitalist‐ACE patients were also more likely to have had recognition and treatment of delirium (27.1% vs 17.0%, P = 0.08), although this finding did not reach statistical significance.
| Measure | Percent of Hospitalist‐ACE Patients | Percent of Usual Care Patients | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Recognition and treatment of abnormal functional status | 68.9 | 35.8 | <0.0001 |
| Recognition and treatment of abnormal cognitive status* | 55.7 | 40.0 | 0.02 |
| Recognition and treatment of delirium | 27.1 | 17.0 | 0.08 |
| Documentation of resuscitation preferences | 95.1 | 91.6 | 0.3 |
| Do Not Attempt Resuscitation orders | 39.3 | 26.3 | 0.04 |
| Use of sleep medications | 28.1 | 27.4 | 0.91 |
| Use of physical restraints | 2.5 | 0 | 0.26 |
While patients on the Hospitalist‐ACE and usual care services had similar percentages of documentation of resuscitation preferences (95.1% vs 91.6%, P = 0.3), the percentage of Hospitalist‐ACE patients who had Do Not Attempt Resuscitation (DNAR) orders was significantly greater than that of the usual care patients (39.3% vs 26.3%, P = 0.04).
There were no differences in the use of physical restraints or sleep medications for Hospitalist‐ACE patients as compared to usual care patients, although the types of sleep mediations used on each service were markedly different: trazadone was employed as the first‐line sleep agent on the Hospitalist‐ACE service (77.7%), and non‐benzodiazepine hypnotics (primarily zolpidem) were employed most commonly on the usual care services (35%). There were no differences noted in the percentage of patients with benzodiazepines prescribed as sleep aids.
Outcomes
Resource utilization outcomes are reported in Table 4. Of note, there were no significant differences between Hospitalist‐ACE discharges and usual care discharges in mean length of stay (3.4 2.7 days vs 3.1 2.7 days, P = 0.52), mean charges ($24,617 15,828 vs $21,488 13,407, P = 0.12), or 30‐day readmissions to UCH (12.3% vs 9.5%, P = 0.51). Hospitalist‐ACE discharges and usual care patients were equally likely to be discharged to home (68.6% vs 67.4%, P = 0.84), with a similar proportion of Hospitalist‐ACE discharges receiving home health care or home hospice services (14.1% vs 7.4%, P = 12).
| Measure | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Length of stay in days (mean [SD]) | 3.4 (2.7) | 3.1 (2.7) | 0.52 |
| Charges in dollars (mean [SD]) | 24,617 (15,828) | 21,488 (13,407) | 0.12 |
| 30‐Day readmissions to UCH (%) | 12.3 | 9.5 | 0.51 |
| Discharges to home (%) | 68.8* | 67.4 | 0.84 |
| Discharges to home with services (%) | 14%* | 7.4% | 0.12 |
In addition, the fall rate for Hospitalist‐ACE patients was not significantly different from the fall rate for usual care patients (4.8 falls/1000 patient days vs 6.7 falls/1000 patient days, 95% confidence interval 9.613.3).
DISCUSSION
We report the implementation and evaluation of a medical service tailored to the care of the acutely ill older patient that draws from elements of the hospitalist model and the ACE unit model.7, 14, 24 For this Hospitalist‐ACE service, we developed a specialized hospitalist workforce, assembled a brief geriatric assessment tailored to the inpatient setting, instituted an interdisciplinary rounding model, and created a novel inpatient geriatrics curriculum.
During the study period, we improved performance of important processes of care for hospitalized elders, including recognition of abnormal cognitive and functional status; maintained comparable resource use; and implemented a novel, inpatient‐focused geriatric medicine educational experience. We were unable to demonstrate an impact on key clinical outcomes such as falls, physical restraint use, and readmissions. Nonetheless, there is evidence that the performance of selected processes of care is associated with improved three‐year survival status in the community‐dwelling vulnerable older patient, and may also be associated with a mortality benefit in the hospitalized vulnerable older patient.25, 26 Therefore, methods to improve the performance of these processes of care may be of clinical importance.
The finding of increased use of DNAR orders in the face of equivalent documentation of code status is of interest and generates hypotheses for further study. It is possible that the educational experience and use of geriatric assessment provides a more complete context for the code status discussion (one that incorporates the patient's social, physical, and cognitive function). However, we do not know if the patients on the ACE service had improved concordance between their code status and their goals of care.
We believe that there was no difference in key clinical outcomes between Hospitalist‐ACE and control patients because the population in this study was relatively low acuity and, therefore, the occurrence of falls and the use of physical restraints were quite low in the study population. In particular, the readmission rate was much lower than is typical for the Medicare population at our hospital, making it challenging to draw conclusions about the impact of the intervention on readmissions, however, we cannot rule out the possibility that our early discharge planning did not address the determinants of readmission for this population.
The ACE unit paradigmcharacterized by 1) closed, modified hospital units; 2) staffing by geriatricians and nurses with geriatrics training; 3) employing geriatric nursing care protocolsrequires significant resources and is not feasible for all settings.6 There is a need for alternative models of comprehensive care for hospitalized elders that require fewer resources in the form of dedicated units and specialist personnel, and can be more responsive to institutional needs. For example, in a 2005 report, one institution reported the creation of a geriatric medicine service that utilized a geriatrician and hospitalist co‐attending model.14 More recently, a large geriatrics program replaced its inpatient geriatrics unit with a mobile inpatient geriatrics service staffed by an attending geriatricianhospitalist, a geriatrics fellow, and a nurse practitioner.27 While these innovative models have eliminated the dedicated unit, they rely on board certified geriatricians, a group in short supply nationally.28 Hospitalists are a rapidly growing provider group that, with appropriate training and building on the work of geriatricians, is poised to provide leadership in acute geriatric care.29, 30
In contrast to the comprehensive inpatient geriatric care models described above, the Hospitalist‐ACE service uses a specialized hospitalist workforce and is not dependent on continuous staffing by geriatricians. Although geographic concentration is important for the success of interdisciplinary rounds, the Hospitalist‐ACE service does not require a closed or modified unit. The nursing staff caring for Hospitalist‐ACE patients have generalist nursing training and, at the time of the study, did not utilize geriatric‐care protocols. Our results need to be interpreted in the light of these differences from the ACE unit model which is a significantly more intensive intervention than the Hospitalist‐ACE service. In addition, the current practice environment is quite different from the mid‐1990s when ACE units were developed and studied. Development and maintenance of models of comprehensive inpatient geriatric care require demonstration of both value as well as return on investment. The alignment of financial and regulatory incentives for programs that provide comprehensive care to complex patients, such as those anticipated by the Affordable Care Act, may encourage the growth of such models.
These data represent findings from a six‐month evaluation of a novel inpatient service in the middle of its first year. There are several limitations related to our study design. First, the results of this small study at a single academic medical center may be of limited generalizability to other settings. Second, the program was evaluated only three months after its inception; we did not capture further improvements in methods, training, and outcomes expected as the program matured. Third, most of the Hospitalist‐ACE service attendings and residents rotate on the UCH general medical services throughout the year. Consequently, we were unable to eliminate the possibility of contamination of the control group, and we were unable to blind the physicians to the study. Fourth, the study population had a relatively low severity of illnessthe average MS‐DRG weight was near 1and low rates of important adverse events such falls and restraint use. This may have occurred because we excluded patients transferred from the ICUs and other services. It is possible that the Hospitalist‐ACE intervention might have demonstrated a larger benefit in a sicker population that would have presented greater opportunities for reductions in length of stay, costs, and adverse events. Fifth, given the retrospective nature of the data collection, we were not able to prospectively assess the incidence of important geriatric outcomes such as delirium and functional decline, nor can we make conclusions about changes in function during the hospitalization.
While the outcome measures we used are conceptually similar to several measures developed by RAND's Assessing Care of Vulnerable Elders (ACOVE) project, this study did not explicitly rely on those constructs.31 To do so would have required prospective screening by clinical staff independent from the care team for vulnerability that was beyond the scope of this project. In addition, the ACOVE measures of interest for functional and cognitive decline are limited to documentation of cognitive or functional assessments in the medical record. The ACE service's adoption of a brief standardized geriatric assessment was almost certain to meet that documentation requirement. While documentation is important, it is not clear that documentation, in and of itself, improves outcomes. Therefore, we expanded upon the ACOVE constructs to include the need for the additional evidence of a treatment plan when abnormal physical or cognitive function was documented. These constructs are important process of care for vulnerable elders. While we demonstrated improvements in several of these important processes of care for elderly patients, we are unable to draw conclusions about the impact of these differences in care on important clinical outcomes such as development of delirium, long‐term institutionalization, or mortality.
CONCLUSIONS
The risks of hospitalization for older persons are numerous, and present challenges and opportunities for inpatient physicians. As the hospitalized population agesmirroring national demographic trends and trends in use of acute care hospitalsthe challenge of avoiding harm in the older hospitalized patient will intensify. Innovations in care to improve the experience and outcomes of hospitalization for older patients are needed in the face of limited geriatrics‐trained workforce and few discretionary funds for unit redesign. The Hospitalist‐ACE service is a promising strategy for hospitalist programs with sufficient numbers of older patients and hospitalists with interest in improving clinical care for older adults. It provides a model for hospitalists to employ geriatrics principles targeted at reducing harm to their most vulnerable patients. Hospitalist‐run geriatric care models offer great promise for improving the care of acutely ill elderly patients. Future investigation should focus on demonstrating the impact of such care on important clinical outcomes between admission and discharge; on model refinement and adaptation, such as determining what components of comprehensive geriatric care are essential to success; and on how complementary interventions, such as the use of templated orders for the hospitalized elderly, impact outcomes. Additional research is needed, with a focus on demonstrating value with regard to an array of outcomes including cost, readmissions, and preventable harms of care.
Acknowledgements
Jean Kutner, MD, MSPH; Daniel Sandy, MPH; Shelly Limon, RN; nurses of 12 West; the UCH staff on the interdisciplinary team; and ACE patients and their families.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,.Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care.Am J Med.1999;106:565–573.
- ,,, et al.Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders.J Am Geriatr Soc.2007;55(11):1705–1711.
- ,,, et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5:69–75.
- ,,,,.What does the medical record reveal about functional status? A comparison of medical record and interview data.J Gen Intern Med.2001;16(11):728–736.
- ,,,,,.Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's “Retooling for an Aging America” report.J Am Geriatr Soc.2009;57(12):2328–2337.
- ,,,,.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1581.
- ,,, et al.The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta‐analysis.J Am Geriatr Soc.2010;58:83–92.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.A randomized, controlled clinical trial of a geriatrics consultation team: compliance with recommendations.JAMA.1986;255:2617–2621.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Dissemination and characteristics of Acute Care of Elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19:220–227.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,,,.The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- ,,.The Patient Health Questionnaire‐2: validity of a two‐item depression screener.Med Care.2003;41:1284–1292.
- ,,,,,.Clarifying confusion: the Confusion Assessment Method.Ann Intern Med.1990;113(12):941–948.
- ,,, et al.The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am Geriatr Soc.2001;49:1691–1699.
- ,.The timed “Up and Go”: a test of basic functional mobility for frail elderly persons.J Am Geriatr Soc.1991;39:142–148.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention.Guideline for the prevention of falls in older persons.J Am Geriatr Soc.2001;49:664–672.
- . Falls for the inpatient physician. Translating knowledge into action. The Portal of Online Geriatric Education (POGOe). 6–19‐2008. Available at: http://www.pogoe.org/productid/20212.
- ,,,. Incontinence and urinary catheters for the inpatient physician. The Portal of Online Geriatric Education (POGOe). 11–27‐0008. Available at: http://www.pogoe.org/productid/20296.
- ,,,.Use of medications for insomnia in the hospitalized geriatric population.J Am Geriatr Soc.2008;56(3):579–581.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130(4 pt 2):343–349.
- ,,, et al.Quality of care associated with survival in vulnerable older patients.Ann Intern Med.2005;143:274–281.
- ,,, et al.Higher quality of care for hosptialized frail older adults is associated with improved survival one year after discharge.J Hosp Med.2009;4(S1):24.
- ,,,.Operational and quality outcomes of a novel mobile acute care for the elderly service.J Am Geriatr Soc.2009;57:S1.
- Institute of Medicine (IOM).Retooling for an Aging America: Building the Health Care Workforce.Washington, DC:The National Academies Press;2008.
- ,,.Alternative solutions to the geriatric workforce deficit.Am J Med.2008;121:e23.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,.Assessing care of vulnerable elders: ACOVE project overview.Ann Intern Med.2001;135(8 pt 2):642–646.
For the frail older patient, hospitalization marks a period of high risk of poor outcomes and adverse events including functional decline, delirium, pressure ulcers, adverse drug events, nosocomial infections, and falls.1, 2 Physician recognition of elderly patients at risk for adverse outcomes is poor, making it difficult to intervene to prevent them.3, 4 Among frail, elderly inpatients at an urban academic medical center, doctors documented cognitive assessments in only 5% of patients. Functional assessments are appropriately documented in 40%80% of inpatients.3, 5
The Acute Care for Elders (ACE) unit is one of several models of comprehensive inpatient geriatric care that have been developed by geriatrician researchers to address the adverse events and functional decline that often accompany hospitalization.6 The ACE unit model generally incorporates: 1) a modified hospital environment, 2) early assessment and intensive management to minimize the adverse effects of hospital care, 3) early discharge planning, 4) patient centered care protocols, and 5) a consistent nursing staff.7 Two randomized, controlled trials have shown the ACE unit model to be successful in reducing functional decline among frail older inpatients during and after hospitalization.7, 8 While meta‐analyses data also suggests the ACE unit model reduces functional decline and future institutionalization, significant impact on other outcomes is not proven.9, 10
Several barriers have prevented the successful dissemination of the ACE unit model. The chief limitations are the upfront resources required to create and maintain a modified, dedicated unit, as well as the lack of a geriatrics trained workforce.7, 1113 The rapid growth of hospital medicine presents opportunities for innovation in the care of older patients. Still, a 2006 census demonstrated that few hospitalist groups had identified geriatric care as a priority.14
In response to these challenges, the University of Colorado Hospital Medicine Group created a hospitalist‐run inpatient medical service designed for the care of the frail older patient. This Hospitalist‐Acute Care for the Elderly (Hospitalist‐ACE) unit is a hybrid of a general medical service and an inpatient geriatrics unit.7 The goals of the Hospitalist‐ACE service are to provide high quality care tailored to older inpatients, thus minimizing the risks of functional decline and adverse events associate with hospitalization, and to provide a clinical geriatrics teaching experience for Hospitalist Training Track Residents within the Internal Medicine Residency Training Program and medical students at the University of Colorado Denver School of Medicine. The Hospitalist‐ACE unit is staffed with a core group of hospitalist attendings who have, at a minimum, attended an intensive mini‐course in inpatient geriatrics. The service employs interdisciplinary rounds; a brief, standardized geriatric assessment including screens of function, cognition, and mood; a clinical focus on mitigating the hazards of hospitalization, early discharge planning; and a novel geriatric educational curriculum for medicine residents and medical students.
This article will: 1) describe the creation of the Hospitalist‐ACE service at the University of Colorado Hospital; and 2) summarize the evaluation of the Hospitalist‐ACE service in a quasi‐randomized, controlled manner during its first year. We hypothesized that, when compared to patients receiving usual care, patients cared for on the Hospitalist‐ACE service would have increased recognition of abnormal functional status; recognition of abnormal cognitive status and delirium; equivalent lengths of stay and hospital charges; and decreased falls, 30‐day readmissions, and restraint use.
METHODS
Design
We performed a quasi‐randomized, controlled study of the Hospitalist‐ACE service.
Setting
The study setting was the inpatient general medical services of the Anschutz Inpatient Pavilion (AIP) of the University of Colorado Hospital (UCH). The AIP is a 425‐bed tertiary care hospital that is the major teaching affiliate of the University of Colorado School of Medicine and a regional referral center. The control services, hereafter referred to as usual care, were comprised of the four inpatient general medicine teaching services that take admissions on a four‐day rotation (in general, two were staffed by outpatient general internists and medical subspecialists, and two were staffed by academic hospitalists). The Hospitalist‐ACE service was a novel hospitalist teaching service that began in July 2007. Hospitalist‐ACE patients were admitted to a single 12‐bed medical unit (12 West) when beds were available; 12 West is similar to the other medical/surgical units at UCH and did not have any modifications to the rooms, equipment, or common areas for the intervention. The nursing staff on this unit had no formal geriatric nursing training. The Hospitalist‐ACE team admitted patients daily (between 7 AM and 3 PM MondayFriday; between 7 AM and 12 noon Saturday and Sunday). Patients assigned to the Hospitalist‐ACE service after hours were admitted by the internal medicine resident on call for the usual care services and handed off to the Hospitalist‐ACE team at 7 AM the next morning.
Study Subjects
Eligible subjects were inpatients age 70 years admitted to the usual care or Hospitalist‐ACE services at the AIP from November 2, 2007 to April 15, 2008. All patients age 70 years were randomized to the Hospitalist‐ACE service or usual care on a general internal medicine service by the last digit of the medical record number (odd numbers admitted to the Hospitalist‐ACE service and even numbers admitted to usual care). Patients followed by the Hospitalist‐ACE service but not admitted to 12 West were included in the study. To isolate the impact of the intervention, patients admitted to a medicine subspecialty service (such as cardiology, pulmonary, or oncology), or transferred to or from the Hospitalist‐ACE or control services to another service (eg, intensive care unit [ICU] or orthopedic surgery service) were excluded from the study.
Intervention
The Hospitalist‐ACE unit implemented an interdisciplinary team approach to identify and address geriatric syndromes in patients aged 70 and over. The Hospitalist‐ACE model of care consisted of clinical care provided by a hospitalist attending with additional training in geriatric medicine, administration of standardized geriatric screens assessing function, cognition, and mood, 15 minute daily (MondayFriday) interdisciplinary rounds focusing on recognition and management of geriatric syndromes and early discharge planning, and a standardized educational curriculum for medical residents and medical students addressing hazards of hospitalization.
The Hospitalist‐ACE service was a unique rotation within the Hospitalist Training Track of the Internal Medicine Residency that was developed with the support of the University of Colorado Hospital and the Internal Medicine Residency Training Program, and input from the Geriatrics Division at the University of Colorado Denver. The director received additional training from the Donald W. Reynolds FoundationUCLA Faculty Development to Advance Geriatric Education Mini‐Fellowship for hospitalist faculty. The mission of the service was to excel at educating the next generation of hospitalists while providing a model for excellence of care for hospitalized elderly patients. Important stakeholders were identified, and a leadership teamincluding representatives from nursing, physical and occupational therapy, pharmacy, social work, case management, and later, volunteer servicescreated the model daily interdisciplinary rounds. As geographic concentration was essential for the viability of interdisciplinary rounds, one unit (12 West) within the hospital was designated as the preferred location for patients admitted to the Hospitalist‐ACE service.
The Hospitalist‐ACE unit team consisted of one attending hospitalist, one resident, one intern, and medical students. The attending was one of five hospitalists, with additional training in geriatric medicine, who rotated attending responsibilities on the service. One of the hospitalists was board certified in geriatric medicine. Each of the other four hospitalists attended the Reynolds FoundationUCLA mini‐fellowship in geriatric medicine. Hospitalist‐ACE attendings rotated on a variety of other hospitalist services throughout the academic year, including the usual care services.
The brief standardized geriatric assessment consisted of six validated instruments, and was completed by house staff or medical students on admission, following instruction by the attending physician. The complete assessment tool is shown in Figure 1. The cognitive items included the Mini‐Cog,15 a two‐item depression screen,16 and the Confusion Assessment Method.17 The functional items included the Vulnerable Elders Survey (VES‐13),18 the Timed Get Up and Go test,19 and a two‐question falls screen.20 The elements of the assessment tool were selected by the Hospitalist‐ACE attendings for brevity and the potential to inform clinical management. To standardize the clinical and educational approach, the Hospitalist‐ACE attendings regularly discussed appropriate orders recommended in response to each positive screen, but no templated order sets were used during the study period.
Interdisciplinary rounds were attended by Hospitalist‐ACE physicians, nurses, case managers, social workers, physical or occupational therapists, pharmacists, and volunteers. Rounds were led by the attending or medical resident.
The educational curriculum encompassed 13 modules created by the attending faculty that cover delirium, falls, dementia, pressure ulcers, physiology of aging, movement disorders, medication safety, end of life care, advance directives, care transitions, financing of health care for the elderly, and ethical conundrums in the care of the elderly. A full table of contents appears in online Appendix 1. Additionally, portions of the curriculum have been published online.21, 22 Topic selection was guided by the Accreditation Council for Graduate Medical Education (ACGME) core geriatrics topics determined most relevant for the inpatient setting. Formal instruction of 3045 minutes duration occurred three to four days a week and was presented in addition to routine internal medicine educational conferences. Attendings coordinated teaching to ensure that each trainee was exposed to all of the content during the course of their four‐week rotation.
In contrast to the Hospitalist‐ACE service, usual care on the control general medical services consisted of either a hospitalist, a general internist, or an internal medicine subspecialist attending physician, with one medical resident, one intern, and medical students admitting every fourth day. The general medical teams attended daily discharge planning rounds with a discharge planner and social worker focused exclusively on discharge planning. The content of teaching rounds on the general medical services was largely left to the discretion of the attending physician.
This program evaluation of the Hospitalist‐ACE service was granted a waiver of consent and Health Insurance Portability and Accountability Act (HIPAA) by the Colorado Multiple Institutional Review Board.
Measures
Primary Outcome
The primary outcome for the study was the recognition of abnormal functional status by the primary team. Recognition of abnormal functional status was determined from chart review and consisted of both the physician's detection of abnormal functional status and evidence of a corresponding treatment plan identified in the notes or orders of a physician member of the primary team (Table 1).
| Measure | Criterion | Source | Content Examples |
|---|---|---|---|
| |||
| Recognition of abnormal functional status* | 1) Detection | MD's documentation of history | Presentation with change in function (new gait instability); use of gait aides (wheelchair) |
| OR | |||
| MD's documentation of physical exam | Observation of abnormal gait (eg, unsteady, wide‐based, shuffling) and/or balance Abnormal Get Up and Go test | ||
| AND | |||
| 2) Treatment | MD's order | PT/OT consult; home safety evaluation | |
| OR | |||
| MD's documentation assessment/plan | Inclusion of functional status (rehabilitation, PT/OT needs) on the MD's problem list | ||
| Recognition of abnormal cognitive status | Any of the following: | ||
| Delirium | 1) Detection | MD's history | Presentation of confusion or altered mental status |
| OR | |||
| MD's physical exam | Abnormal confusion assessment method | ||
| AND | |||
| 2) Treatment | MD's order | Sitter, reorienting communication, new halperidol order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of delirium on the problem list | ||
| OR | |||
| Dementia | 1) Detection | MD's history | Dementia in medical history |
| OR | OR | ||
| MD's physical exam | Abnormal Folstein Mini‐Mental Status Exam or Mini‐Cog | ||
| AND | |||
| 2) Treatment | MD's order | Cholinesterase inhibitor ordered | |
| OR | OR | ||
| MD's documentation of assessment/plan | Inclusion of dementia on the problem list | ||
| OR | |||
| Depression | 1) Detection | MD's history | Depression in medical history |
| OR | OR | ||
| MD's physical exam | Positive depression screen | ||
| AND | |||
| 2) Treatment | MD's order | New antidepressant order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of depression on the problem list | ||
Secondary Outcomes
Recognition of abnormal cognitive status was determined from chart review and consisted of both the physician's detection of dementia, depression, or delirium, and evidence of a corresponding treatment plan for any of the documented conditions identified in the notes or orders of a physician member of the primary team (Table 1). Additionally, we measured recognition and treatment of delirium alone.
Falls were determined from mandatory event reporting collected by the hospital on the University Hospitals Consortium Patient Safety Net web‐based reporting system and based on clinical assessment as reported by the nursing staff. The reports are validated by the appropriate clinical managers within 45 days of the event according to standard procedure.
Physical restraint use (type of restraint and duration) was determined from query of mandatory clinical documentation in the electronic medical record. Use of sleep aids was determined from review of the physician's order sheets in the medical record. The chart review captured any of 39 commonly prescribed hypnotic medications ordered at hour of sleep or for insomnia. The sleep medication list was compiled with the assistance of a pharmacist for an earlier chart review and included non‐benzodiazepine hypnotics, benzodiazepines, antidepressants, antihistamines, and antipsychotics.23
Length of stay, hospital charges, 30‐day readmissions to UCH (calculated from date of discharge), and discharge location were determined from administrative data.
Additional Descriptive Variables
Name, medical record number, gender, date of birth, date of admission and discharge, and primary diagnosis were obtained from the medical record. The Case Mix Index for each group of patients was determined from the average Medicare Severity‐adjusted Diagnosis Related Group (MS‐DRG) weight obtained from administrative data.
Data Collection
A two‐step, retrospective chart abstraction was employed. A professional research assistant (P.R.A.) hand‐abstracted process measures from the paper medical chart onto a data collection form designed for this study. A physician investigator performed a secondary review (H.L.W.). Discrepancies were resolved by the physician reviewer.
Data Analysis
Descriptive statistics were performed on intervention and control subjects. Means and standard deviations (age) or frequencies (gender, primary diagnoses) were calculated as appropriate. T tests were used for continuous variables, chi‐square tests for gender, and the Wilcoxon rank sum test for categorical variables.
Outcomes were reported as means and standard deviations for continuous variables (length of stay and charges) and frequencies for categorical variables (all other outcomes). T tests were used for continuous variables, Fisher's exact test for restraint use, and chi‐square tests were used for categorical variable to compare the impact of the intervention between intervention and control patients. For falls, confidence intervals were calculated for the incidence rate differences based on Poisson approximations.
Sample Size Considerations
An a priori sample size calculation was performed. A 2001 study showed that functional status is poorly documented in at least 60% of hospital charts of elderly patients.5 Given an estimated sample size of 120 per group and a power of 80%, this study was powered to be able to detect an absolute difference in the documentation of functional status of as little as 18%.
RESULTS
Two hundred seventeen patients met the study entry criteria (Table 2): 122 were admitted to the Hospitalist‐ACE service, and 95 were admitted to usual care on the general medical services. The average age of the study patients was 80.5 years, 55.3% were female. Twenty‐eight percent of subjects were admitted for pulmonary diagnoses. The two groups of patients were similar with respect to age, gender, and distribution of primary diagnoses. The Hospitalist‐ACE patients had a mean MS‐DRG weight of 1.15, which was slightly higher than that of usual care patients at 1.05 (P = 0.06). Typically, 70% of Hospitalist‐ACE patients are admitted to the designated ACE medical unit (12 West).
| Characteristic | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Age (years), mean (SD) | 80.5 (6.5) | 80.7 (7.0) | 0.86 |
| Gender (% female) | 52.5 | 59 | 0.34 |
| Case Mix Index (mean MS‐DRG weight [SD]) | 1.15 (0.43) | 1.05 (0.31) | 0.06 |
| Primary ICD‐9 diagnosis (%) | 0.59 | ||
| Pulmonary | 27.9 | 28.4 | |
| General medicine | 15.6 | 11.6 | |
| Surgery | 13.9 | 11.6 | |
| Cardiology | 9.8 | 6.3 | |
| Nephrology | 8.2 | 7.4 | |
Processes of Care
Processes of care for older patients are displayed in Table 3. Patients on the Hospitalist‐ACE service had recognition and treatment of abnormal functional status at a rate that was nearly double that of patients on the usual care services (68.9% vs 35.8%, P < 0.0001). In addition, patients on the Hospitalist‐ACE service were significantly more likely to have had recognition and treatment of any abnormal cognitive status (55.7% vs 40.0%, P = 0.02). When delirium was evaluated alone, the Hospitalist‐ACE patients were also more likely to have had recognition and treatment of delirium (27.1% vs 17.0%, P = 0.08), although this finding did not reach statistical significance.
| Measure | Percent of Hospitalist‐ACE Patients | Percent of Usual Care Patients | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Recognition and treatment of abnormal functional status | 68.9 | 35.8 | <0.0001 |
| Recognition and treatment of abnormal cognitive status* | 55.7 | 40.0 | 0.02 |
| Recognition and treatment of delirium | 27.1 | 17.0 | 0.08 |
| Documentation of resuscitation preferences | 95.1 | 91.6 | 0.3 |
| Do Not Attempt Resuscitation orders | 39.3 | 26.3 | 0.04 |
| Use of sleep medications | 28.1 | 27.4 | 0.91 |
| Use of physical restraints | 2.5 | 0 | 0.26 |
While patients on the Hospitalist‐ACE and usual care services had similar percentages of documentation of resuscitation preferences (95.1% vs 91.6%, P = 0.3), the percentage of Hospitalist‐ACE patients who had Do Not Attempt Resuscitation (DNAR) orders was significantly greater than that of the usual care patients (39.3% vs 26.3%, P = 0.04).
There were no differences in the use of physical restraints or sleep medications for Hospitalist‐ACE patients as compared to usual care patients, although the types of sleep mediations used on each service were markedly different: trazadone was employed as the first‐line sleep agent on the Hospitalist‐ACE service (77.7%), and non‐benzodiazepine hypnotics (primarily zolpidem) were employed most commonly on the usual care services (35%). There were no differences noted in the percentage of patients with benzodiazepines prescribed as sleep aids.
Outcomes
Resource utilization outcomes are reported in Table 4. Of note, there were no significant differences between Hospitalist‐ACE discharges and usual care discharges in mean length of stay (3.4 2.7 days vs 3.1 2.7 days, P = 0.52), mean charges ($24,617 15,828 vs $21,488 13,407, P = 0.12), or 30‐day readmissions to UCH (12.3% vs 9.5%, P = 0.51). Hospitalist‐ACE discharges and usual care patients were equally likely to be discharged to home (68.6% vs 67.4%, P = 0.84), with a similar proportion of Hospitalist‐ACE discharges receiving home health care or home hospice services (14.1% vs 7.4%, P = 12).
| Measure | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Length of stay in days (mean [SD]) | 3.4 (2.7) | 3.1 (2.7) | 0.52 |
| Charges in dollars (mean [SD]) | 24,617 (15,828) | 21,488 (13,407) | 0.12 |
| 30‐Day readmissions to UCH (%) | 12.3 | 9.5 | 0.51 |
| Discharges to home (%) | 68.8* | 67.4 | 0.84 |
| Discharges to home with services (%) | 14%* | 7.4% | 0.12 |
In addition, the fall rate for Hospitalist‐ACE patients was not significantly different from the fall rate for usual care patients (4.8 falls/1000 patient days vs 6.7 falls/1000 patient days, 95% confidence interval 9.613.3).
DISCUSSION
We report the implementation and evaluation of a medical service tailored to the care of the acutely ill older patient that draws from elements of the hospitalist model and the ACE unit model.7, 14, 24 For this Hospitalist‐ACE service, we developed a specialized hospitalist workforce, assembled a brief geriatric assessment tailored to the inpatient setting, instituted an interdisciplinary rounding model, and created a novel inpatient geriatrics curriculum.
During the study period, we improved performance of important processes of care for hospitalized elders, including recognition of abnormal cognitive and functional status; maintained comparable resource use; and implemented a novel, inpatient‐focused geriatric medicine educational experience. We were unable to demonstrate an impact on key clinical outcomes such as falls, physical restraint use, and readmissions. Nonetheless, there is evidence that the performance of selected processes of care is associated with improved three‐year survival status in the community‐dwelling vulnerable older patient, and may also be associated with a mortality benefit in the hospitalized vulnerable older patient.25, 26 Therefore, methods to improve the performance of these processes of care may be of clinical importance.
The finding of increased use of DNAR orders in the face of equivalent documentation of code status is of interest and generates hypotheses for further study. It is possible that the educational experience and use of geriatric assessment provides a more complete context for the code status discussion (one that incorporates the patient's social, physical, and cognitive function). However, we do not know if the patients on the ACE service had improved concordance between their code status and their goals of care.
We believe that there was no difference in key clinical outcomes between Hospitalist‐ACE and control patients because the population in this study was relatively low acuity and, therefore, the occurrence of falls and the use of physical restraints were quite low in the study population. In particular, the readmission rate was much lower than is typical for the Medicare population at our hospital, making it challenging to draw conclusions about the impact of the intervention on readmissions, however, we cannot rule out the possibility that our early discharge planning did not address the determinants of readmission for this population.
The ACE unit paradigmcharacterized by 1) closed, modified hospital units; 2) staffing by geriatricians and nurses with geriatrics training; 3) employing geriatric nursing care protocolsrequires significant resources and is not feasible for all settings.6 There is a need for alternative models of comprehensive care for hospitalized elders that require fewer resources in the form of dedicated units and specialist personnel, and can be more responsive to institutional needs. For example, in a 2005 report, one institution reported the creation of a geriatric medicine service that utilized a geriatrician and hospitalist co‐attending model.14 More recently, a large geriatrics program replaced its inpatient geriatrics unit with a mobile inpatient geriatrics service staffed by an attending geriatricianhospitalist, a geriatrics fellow, and a nurse practitioner.27 While these innovative models have eliminated the dedicated unit, they rely on board certified geriatricians, a group in short supply nationally.28 Hospitalists are a rapidly growing provider group that, with appropriate training and building on the work of geriatricians, is poised to provide leadership in acute geriatric care.29, 30
In contrast to the comprehensive inpatient geriatric care models described above, the Hospitalist‐ACE service uses a specialized hospitalist workforce and is not dependent on continuous staffing by geriatricians. Although geographic concentration is important for the success of interdisciplinary rounds, the Hospitalist‐ACE service does not require a closed or modified unit. The nursing staff caring for Hospitalist‐ACE patients have generalist nursing training and, at the time of the study, did not utilize geriatric‐care protocols. Our results need to be interpreted in the light of these differences from the ACE unit model which is a significantly more intensive intervention than the Hospitalist‐ACE service. In addition, the current practice environment is quite different from the mid‐1990s when ACE units were developed and studied. Development and maintenance of models of comprehensive inpatient geriatric care require demonstration of both value as well as return on investment. The alignment of financial and regulatory incentives for programs that provide comprehensive care to complex patients, such as those anticipated by the Affordable Care Act, may encourage the growth of such models.
These data represent findings from a six‐month evaluation of a novel inpatient service in the middle of its first year. There are several limitations related to our study design. First, the results of this small study at a single academic medical center may be of limited generalizability to other settings. Second, the program was evaluated only three months after its inception; we did not capture further improvements in methods, training, and outcomes expected as the program matured. Third, most of the Hospitalist‐ACE service attendings and residents rotate on the UCH general medical services throughout the year. Consequently, we were unable to eliminate the possibility of contamination of the control group, and we were unable to blind the physicians to the study. Fourth, the study population had a relatively low severity of illnessthe average MS‐DRG weight was near 1and low rates of important adverse events such falls and restraint use. This may have occurred because we excluded patients transferred from the ICUs and other services. It is possible that the Hospitalist‐ACE intervention might have demonstrated a larger benefit in a sicker population that would have presented greater opportunities for reductions in length of stay, costs, and adverse events. Fifth, given the retrospective nature of the data collection, we were not able to prospectively assess the incidence of important geriatric outcomes such as delirium and functional decline, nor can we make conclusions about changes in function during the hospitalization.
While the outcome measures we used are conceptually similar to several measures developed by RAND's Assessing Care of Vulnerable Elders (ACOVE) project, this study did not explicitly rely on those constructs.31 To do so would have required prospective screening by clinical staff independent from the care team for vulnerability that was beyond the scope of this project. In addition, the ACOVE measures of interest for functional and cognitive decline are limited to documentation of cognitive or functional assessments in the medical record. The ACE service's adoption of a brief standardized geriatric assessment was almost certain to meet that documentation requirement. While documentation is important, it is not clear that documentation, in and of itself, improves outcomes. Therefore, we expanded upon the ACOVE constructs to include the need for the additional evidence of a treatment plan when abnormal physical or cognitive function was documented. These constructs are important process of care for vulnerable elders. While we demonstrated improvements in several of these important processes of care for elderly patients, we are unable to draw conclusions about the impact of these differences in care on important clinical outcomes such as development of delirium, long‐term institutionalization, or mortality.
CONCLUSIONS
The risks of hospitalization for older persons are numerous, and present challenges and opportunities for inpatient physicians. As the hospitalized population agesmirroring national demographic trends and trends in use of acute care hospitalsthe challenge of avoiding harm in the older hospitalized patient will intensify. Innovations in care to improve the experience and outcomes of hospitalization for older patients are needed in the face of limited geriatrics‐trained workforce and few discretionary funds for unit redesign. The Hospitalist‐ACE service is a promising strategy for hospitalist programs with sufficient numbers of older patients and hospitalists with interest in improving clinical care for older adults. It provides a model for hospitalists to employ geriatrics principles targeted at reducing harm to their most vulnerable patients. Hospitalist‐run geriatric care models offer great promise for improving the care of acutely ill elderly patients. Future investigation should focus on demonstrating the impact of such care on important clinical outcomes between admission and discharge; on model refinement and adaptation, such as determining what components of comprehensive geriatric care are essential to success; and on how complementary interventions, such as the use of templated orders for the hospitalized elderly, impact outcomes. Additional research is needed, with a focus on demonstrating value with regard to an array of outcomes including cost, readmissions, and preventable harms of care.
Acknowledgements
Jean Kutner, MD, MSPH; Daniel Sandy, MPH; Shelly Limon, RN; nurses of 12 West; the UCH staff on the interdisciplinary team; and ACE patients and their families.
For the frail older patient, hospitalization marks a period of high risk of poor outcomes and adverse events including functional decline, delirium, pressure ulcers, adverse drug events, nosocomial infections, and falls.1, 2 Physician recognition of elderly patients at risk for adverse outcomes is poor, making it difficult to intervene to prevent them.3, 4 Among frail, elderly inpatients at an urban academic medical center, doctors documented cognitive assessments in only 5% of patients. Functional assessments are appropriately documented in 40%80% of inpatients.3, 5
The Acute Care for Elders (ACE) unit is one of several models of comprehensive inpatient geriatric care that have been developed by geriatrician researchers to address the adverse events and functional decline that often accompany hospitalization.6 The ACE unit model generally incorporates: 1) a modified hospital environment, 2) early assessment and intensive management to minimize the adverse effects of hospital care, 3) early discharge planning, 4) patient centered care protocols, and 5) a consistent nursing staff.7 Two randomized, controlled trials have shown the ACE unit model to be successful in reducing functional decline among frail older inpatients during and after hospitalization.7, 8 While meta‐analyses data also suggests the ACE unit model reduces functional decline and future institutionalization, significant impact on other outcomes is not proven.9, 10
Several barriers have prevented the successful dissemination of the ACE unit model. The chief limitations are the upfront resources required to create and maintain a modified, dedicated unit, as well as the lack of a geriatrics trained workforce.7, 1113 The rapid growth of hospital medicine presents opportunities for innovation in the care of older patients. Still, a 2006 census demonstrated that few hospitalist groups had identified geriatric care as a priority.14
In response to these challenges, the University of Colorado Hospital Medicine Group created a hospitalist‐run inpatient medical service designed for the care of the frail older patient. This Hospitalist‐Acute Care for the Elderly (Hospitalist‐ACE) unit is a hybrid of a general medical service and an inpatient geriatrics unit.7 The goals of the Hospitalist‐ACE service are to provide high quality care tailored to older inpatients, thus minimizing the risks of functional decline and adverse events associate with hospitalization, and to provide a clinical geriatrics teaching experience for Hospitalist Training Track Residents within the Internal Medicine Residency Training Program and medical students at the University of Colorado Denver School of Medicine. The Hospitalist‐ACE unit is staffed with a core group of hospitalist attendings who have, at a minimum, attended an intensive mini‐course in inpatient geriatrics. The service employs interdisciplinary rounds; a brief, standardized geriatric assessment including screens of function, cognition, and mood; a clinical focus on mitigating the hazards of hospitalization, early discharge planning; and a novel geriatric educational curriculum for medicine residents and medical students.
This article will: 1) describe the creation of the Hospitalist‐ACE service at the University of Colorado Hospital; and 2) summarize the evaluation of the Hospitalist‐ACE service in a quasi‐randomized, controlled manner during its first year. We hypothesized that, when compared to patients receiving usual care, patients cared for on the Hospitalist‐ACE service would have increased recognition of abnormal functional status; recognition of abnormal cognitive status and delirium; equivalent lengths of stay and hospital charges; and decreased falls, 30‐day readmissions, and restraint use.
METHODS
Design
We performed a quasi‐randomized, controlled study of the Hospitalist‐ACE service.
Setting
The study setting was the inpatient general medical services of the Anschutz Inpatient Pavilion (AIP) of the University of Colorado Hospital (UCH). The AIP is a 425‐bed tertiary care hospital that is the major teaching affiliate of the University of Colorado School of Medicine and a regional referral center. The control services, hereafter referred to as usual care, were comprised of the four inpatient general medicine teaching services that take admissions on a four‐day rotation (in general, two were staffed by outpatient general internists and medical subspecialists, and two were staffed by academic hospitalists). The Hospitalist‐ACE service was a novel hospitalist teaching service that began in July 2007. Hospitalist‐ACE patients were admitted to a single 12‐bed medical unit (12 West) when beds were available; 12 West is similar to the other medical/surgical units at UCH and did not have any modifications to the rooms, equipment, or common areas for the intervention. The nursing staff on this unit had no formal geriatric nursing training. The Hospitalist‐ACE team admitted patients daily (between 7 AM and 3 PM MondayFriday; between 7 AM and 12 noon Saturday and Sunday). Patients assigned to the Hospitalist‐ACE service after hours were admitted by the internal medicine resident on call for the usual care services and handed off to the Hospitalist‐ACE team at 7 AM the next morning.
Study Subjects
Eligible subjects were inpatients age 70 years admitted to the usual care or Hospitalist‐ACE services at the AIP from November 2, 2007 to April 15, 2008. All patients age 70 years were randomized to the Hospitalist‐ACE service or usual care on a general internal medicine service by the last digit of the medical record number (odd numbers admitted to the Hospitalist‐ACE service and even numbers admitted to usual care). Patients followed by the Hospitalist‐ACE service but not admitted to 12 West were included in the study. To isolate the impact of the intervention, patients admitted to a medicine subspecialty service (such as cardiology, pulmonary, or oncology), or transferred to or from the Hospitalist‐ACE or control services to another service (eg, intensive care unit [ICU] or orthopedic surgery service) were excluded from the study.
Intervention
The Hospitalist‐ACE unit implemented an interdisciplinary team approach to identify and address geriatric syndromes in patients aged 70 and over. The Hospitalist‐ACE model of care consisted of clinical care provided by a hospitalist attending with additional training in geriatric medicine, administration of standardized geriatric screens assessing function, cognition, and mood, 15 minute daily (MondayFriday) interdisciplinary rounds focusing on recognition and management of geriatric syndromes and early discharge planning, and a standardized educational curriculum for medical residents and medical students addressing hazards of hospitalization.
The Hospitalist‐ACE service was a unique rotation within the Hospitalist Training Track of the Internal Medicine Residency that was developed with the support of the University of Colorado Hospital and the Internal Medicine Residency Training Program, and input from the Geriatrics Division at the University of Colorado Denver. The director received additional training from the Donald W. Reynolds FoundationUCLA Faculty Development to Advance Geriatric Education Mini‐Fellowship for hospitalist faculty. The mission of the service was to excel at educating the next generation of hospitalists while providing a model for excellence of care for hospitalized elderly patients. Important stakeholders were identified, and a leadership teamincluding representatives from nursing, physical and occupational therapy, pharmacy, social work, case management, and later, volunteer servicescreated the model daily interdisciplinary rounds. As geographic concentration was essential for the viability of interdisciplinary rounds, one unit (12 West) within the hospital was designated as the preferred location for patients admitted to the Hospitalist‐ACE service.
The Hospitalist‐ACE unit team consisted of one attending hospitalist, one resident, one intern, and medical students. The attending was one of five hospitalists, with additional training in geriatric medicine, who rotated attending responsibilities on the service. One of the hospitalists was board certified in geriatric medicine. Each of the other four hospitalists attended the Reynolds FoundationUCLA mini‐fellowship in geriatric medicine. Hospitalist‐ACE attendings rotated on a variety of other hospitalist services throughout the academic year, including the usual care services.
The brief standardized geriatric assessment consisted of six validated instruments, and was completed by house staff or medical students on admission, following instruction by the attending physician. The complete assessment tool is shown in Figure 1. The cognitive items included the Mini‐Cog,15 a two‐item depression screen,16 and the Confusion Assessment Method.17 The functional items included the Vulnerable Elders Survey (VES‐13),18 the Timed Get Up and Go test,19 and a two‐question falls screen.20 The elements of the assessment tool were selected by the Hospitalist‐ACE attendings for brevity and the potential to inform clinical management. To standardize the clinical and educational approach, the Hospitalist‐ACE attendings regularly discussed appropriate orders recommended in response to each positive screen, but no templated order sets were used during the study period.
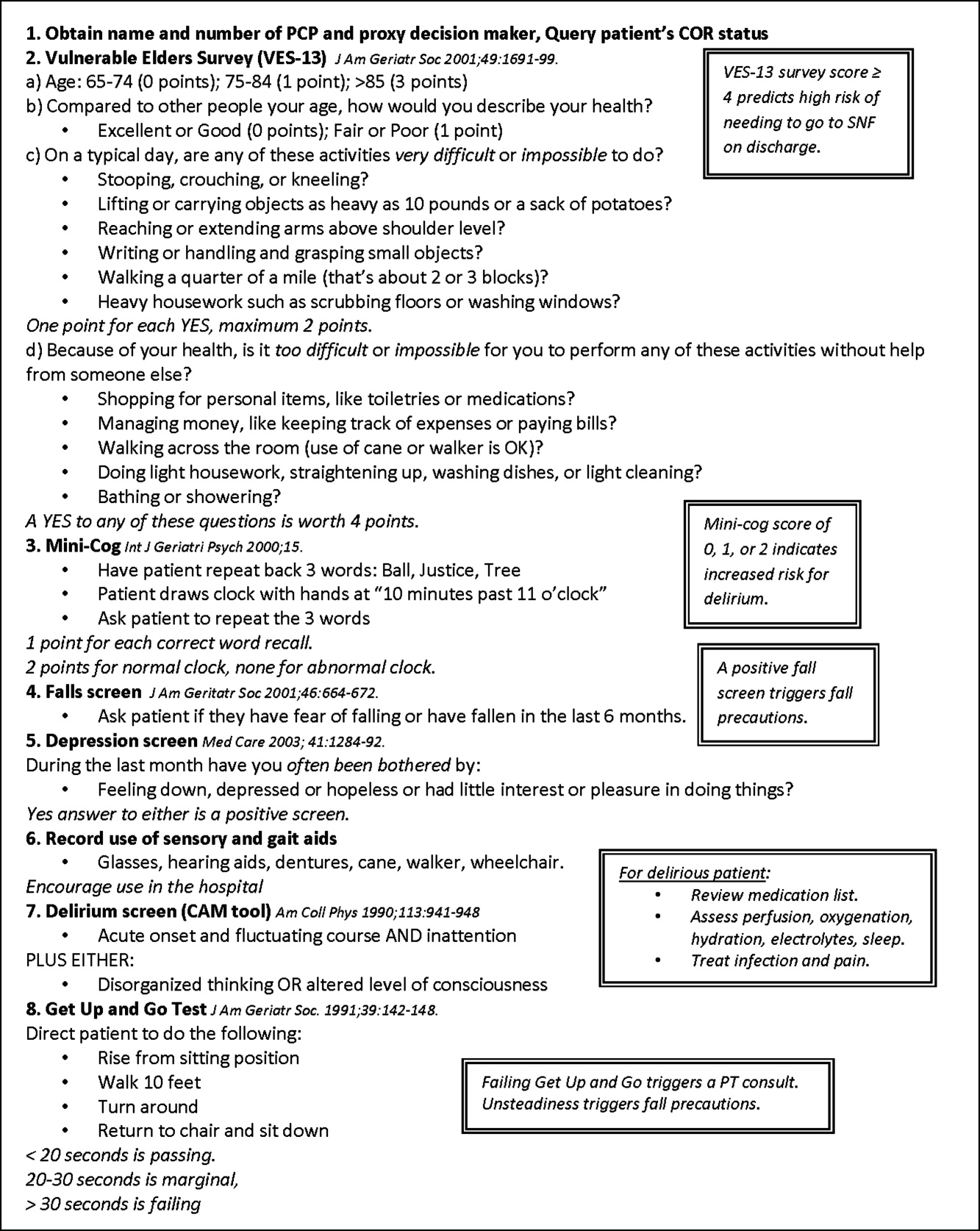
Interdisciplinary rounds were attended by Hospitalist‐ACE physicians, nurses, case managers, social workers, physical or occupational therapists, pharmacists, and volunteers. Rounds were led by the attending or medical resident.
The educational curriculum encompassed 13 modules created by the attending faculty that cover delirium, falls, dementia, pressure ulcers, physiology of aging, movement disorders, medication safety, end of life care, advance directives, care transitions, financing of health care for the elderly, and ethical conundrums in the care of the elderly. A full table of contents appears in online Appendix 1. Additionally, portions of the curriculum have been published online.21, 22 Topic selection was guided by the Accreditation Council for Graduate Medical Education (ACGME) core geriatrics topics determined most relevant for the inpatient setting. Formal instruction of 3045 minutes duration occurred three to four days a week and was presented in addition to routine internal medicine educational conferences. Attendings coordinated teaching to ensure that each trainee was exposed to all of the content during the course of their four‐week rotation.
In contrast to the Hospitalist‐ACE service, usual care on the control general medical services consisted of either a hospitalist, a general internist, or an internal medicine subspecialist attending physician, with one medical resident, one intern, and medical students admitting every fourth day. The general medical teams attended daily discharge planning rounds with a discharge planner and social worker focused exclusively on discharge planning. The content of teaching rounds on the general medical services was largely left to the discretion of the attending physician.
This program evaluation of the Hospitalist‐ACE service was granted a waiver of consent and Health Insurance Portability and Accountability Act (HIPAA) by the Colorado Multiple Institutional Review Board.
Measures
Primary Outcome
The primary outcome for the study was the recognition of abnormal functional status by the primary team. Recognition of abnormal functional status was determined from chart review and consisted of both the physician's detection of abnormal functional status and evidence of a corresponding treatment plan identified in the notes or orders of a physician member of the primary team (Table 1).
| Measure | Criterion | Source | Content Examples |
|---|---|---|---|
| |||
| Recognition of abnormal functional status* | 1) Detection | MD's documentation of history | Presentation with change in function (new gait instability); use of gait aides (wheelchair) |
| OR | |||
| MD's documentation of physical exam | Observation of abnormal gait (eg, unsteady, wide‐based, shuffling) and/or balance Abnormal Get Up and Go test | ||
| AND | |||
| 2) Treatment | MD's order | PT/OT consult; home safety evaluation | |
| OR | |||
| MD's documentation assessment/plan | Inclusion of functional status (rehabilitation, PT/OT needs) on the MD's problem list | ||
| Recognition of abnormal cognitive status | Any of the following: | ||
| Delirium | 1) Detection | MD's history | Presentation of confusion or altered mental status |
| OR | |||
| MD's physical exam | Abnormal confusion assessment method | ||
| AND | |||
| 2) Treatment | MD's order | Sitter, reorienting communication, new halperidol order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of delirium on the problem list | ||
| OR | |||
| Dementia | 1) Detection | MD's history | Dementia in medical history |
| OR | OR | ||
| MD's physical exam | Abnormal Folstein Mini‐Mental Status Exam or Mini‐Cog | ||
| AND | |||
| 2) Treatment | MD's order | Cholinesterase inhibitor ordered | |
| OR | OR | ||
| MD's documentation of assessment/plan | Inclusion of dementia on the problem list | ||
| OR | |||
| Depression | 1) Detection | MD's history | Depression in medical history |
| OR | OR | ||
| MD's physical exam | Positive depression screen | ||
| AND | |||
| 2) Treatment | MD's order | New antidepressant order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of depression on the problem list | ||
Secondary Outcomes
Recognition of abnormal cognitive status was determined from chart review and consisted of both the physician's detection of dementia, depression, or delirium, and evidence of a corresponding treatment plan for any of the documented conditions identified in the notes or orders of a physician member of the primary team (Table 1). Additionally, we measured recognition and treatment of delirium alone.
Falls were determined from mandatory event reporting collected by the hospital on the University Hospitals Consortium Patient Safety Net web‐based reporting system and based on clinical assessment as reported by the nursing staff. The reports are validated by the appropriate clinical managers within 45 days of the event according to standard procedure.
Physical restraint use (type of restraint and duration) was determined from query of mandatory clinical documentation in the electronic medical record. Use of sleep aids was determined from review of the physician's order sheets in the medical record. The chart review captured any of 39 commonly prescribed hypnotic medications ordered at hour of sleep or for insomnia. The sleep medication list was compiled with the assistance of a pharmacist for an earlier chart review and included non‐benzodiazepine hypnotics, benzodiazepines, antidepressants, antihistamines, and antipsychotics.23
Length of stay, hospital charges, 30‐day readmissions to UCH (calculated from date of discharge), and discharge location were determined from administrative data.
Additional Descriptive Variables
Name, medical record number, gender, date of birth, date of admission and discharge, and primary diagnosis were obtained from the medical record. The Case Mix Index for each group of patients was determined from the average Medicare Severity‐adjusted Diagnosis Related Group (MS‐DRG) weight obtained from administrative data.
Data Collection
A two‐step, retrospective chart abstraction was employed. A professional research assistant (P.R.A.) hand‐abstracted process measures from the paper medical chart onto a data collection form designed for this study. A physician investigator performed a secondary review (H.L.W.). Discrepancies were resolved by the physician reviewer.
Data Analysis
Descriptive statistics were performed on intervention and control subjects. Means and standard deviations (age) or frequencies (gender, primary diagnoses) were calculated as appropriate. T tests were used for continuous variables, chi‐square tests for gender, and the Wilcoxon rank sum test for categorical variables.
Outcomes were reported as means and standard deviations for continuous variables (length of stay and charges) and frequencies for categorical variables (all other outcomes). T tests were used for continuous variables, Fisher's exact test for restraint use, and chi‐square tests were used for categorical variable to compare the impact of the intervention between intervention and control patients. For falls, confidence intervals were calculated for the incidence rate differences based on Poisson approximations.
Sample Size Considerations
An a priori sample size calculation was performed. A 2001 study showed that functional status is poorly documented in at least 60% of hospital charts of elderly patients.5 Given an estimated sample size of 120 per group and a power of 80%, this study was powered to be able to detect an absolute difference in the documentation of functional status of as little as 18%.
RESULTS
Two hundred seventeen patients met the study entry criteria (Table 2): 122 were admitted to the Hospitalist‐ACE service, and 95 were admitted to usual care on the general medical services. The average age of the study patients was 80.5 years, 55.3% were female. Twenty‐eight percent of subjects were admitted for pulmonary diagnoses. The two groups of patients were similar with respect to age, gender, and distribution of primary diagnoses. The Hospitalist‐ACE patients had a mean MS‐DRG weight of 1.15, which was slightly higher than that of usual care patients at 1.05 (P = 0.06). Typically, 70% of Hospitalist‐ACE patients are admitted to the designated ACE medical unit (12 West).
| Characteristic | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Age (years), mean (SD) | 80.5 (6.5) | 80.7 (7.0) | 0.86 |
| Gender (% female) | 52.5 | 59 | 0.34 |
| Case Mix Index (mean MS‐DRG weight [SD]) | 1.15 (0.43) | 1.05 (0.31) | 0.06 |
| Primary ICD‐9 diagnosis (%) | 0.59 | ||
| Pulmonary | 27.9 | 28.4 | |
| General medicine | 15.6 | 11.6 | |
| Surgery | 13.9 | 11.6 | |
| Cardiology | 9.8 | 6.3 | |
| Nephrology | 8.2 | 7.4 | |
Processes of Care
Processes of care for older patients are displayed in Table 3. Patients on the Hospitalist‐ACE service had recognition and treatment of abnormal functional status at a rate that was nearly double that of patients on the usual care services (68.9% vs 35.8%, P < 0.0001). In addition, patients on the Hospitalist‐ACE service were significantly more likely to have had recognition and treatment of any abnormal cognitive status (55.7% vs 40.0%, P = 0.02). When delirium was evaluated alone, the Hospitalist‐ACE patients were also more likely to have had recognition and treatment of delirium (27.1% vs 17.0%, P = 0.08), although this finding did not reach statistical significance.
| Measure | Percent of Hospitalist‐ACE Patients | Percent of Usual Care Patients | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Recognition and treatment of abnormal functional status | 68.9 | 35.8 | <0.0001 |
| Recognition and treatment of abnormal cognitive status* | 55.7 | 40.0 | 0.02 |
| Recognition and treatment of delirium | 27.1 | 17.0 | 0.08 |
| Documentation of resuscitation preferences | 95.1 | 91.6 | 0.3 |
| Do Not Attempt Resuscitation orders | 39.3 | 26.3 | 0.04 |
| Use of sleep medications | 28.1 | 27.4 | 0.91 |
| Use of physical restraints | 2.5 | 0 | 0.26 |
While patients on the Hospitalist‐ACE and usual care services had similar percentages of documentation of resuscitation preferences (95.1% vs 91.6%, P = 0.3), the percentage of Hospitalist‐ACE patients who had Do Not Attempt Resuscitation (DNAR) orders was significantly greater than that of the usual care patients (39.3% vs 26.3%, P = 0.04).
There were no differences in the use of physical restraints or sleep medications for Hospitalist‐ACE patients as compared to usual care patients, although the types of sleep mediations used on each service were markedly different: trazadone was employed as the first‐line sleep agent on the Hospitalist‐ACE service (77.7%), and non‐benzodiazepine hypnotics (primarily zolpidem) were employed most commonly on the usual care services (35%). There were no differences noted in the percentage of patients with benzodiazepines prescribed as sleep aids.
Outcomes
Resource utilization outcomes are reported in Table 4. Of note, there were no significant differences between Hospitalist‐ACE discharges and usual care discharges in mean length of stay (3.4 2.7 days vs 3.1 2.7 days, P = 0.52), mean charges ($24,617 15,828 vs $21,488 13,407, P = 0.12), or 30‐day readmissions to UCH (12.3% vs 9.5%, P = 0.51). Hospitalist‐ACE discharges and usual care patients were equally likely to be discharged to home (68.6% vs 67.4%, P = 0.84), with a similar proportion of Hospitalist‐ACE discharges receiving home health care or home hospice services (14.1% vs 7.4%, P = 12).
| Measure | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Length of stay in days (mean [SD]) | 3.4 (2.7) | 3.1 (2.7) | 0.52 |
| Charges in dollars (mean [SD]) | 24,617 (15,828) | 21,488 (13,407) | 0.12 |
| 30‐Day readmissions to UCH (%) | 12.3 | 9.5 | 0.51 |
| Discharges to home (%) | 68.8* | 67.4 | 0.84 |
| Discharges to home with services (%) | 14%* | 7.4% | 0.12 |
In addition, the fall rate for Hospitalist‐ACE patients was not significantly different from the fall rate for usual care patients (4.8 falls/1000 patient days vs 6.7 falls/1000 patient days, 95% confidence interval 9.613.3).
DISCUSSION
We report the implementation and evaluation of a medical service tailored to the care of the acutely ill older patient that draws from elements of the hospitalist model and the ACE unit model.7, 14, 24 For this Hospitalist‐ACE service, we developed a specialized hospitalist workforce, assembled a brief geriatric assessment tailored to the inpatient setting, instituted an interdisciplinary rounding model, and created a novel inpatient geriatrics curriculum.
During the study period, we improved performance of important processes of care for hospitalized elders, including recognition of abnormal cognitive and functional status; maintained comparable resource use; and implemented a novel, inpatient‐focused geriatric medicine educational experience. We were unable to demonstrate an impact on key clinical outcomes such as falls, physical restraint use, and readmissions. Nonetheless, there is evidence that the performance of selected processes of care is associated with improved three‐year survival status in the community‐dwelling vulnerable older patient, and may also be associated with a mortality benefit in the hospitalized vulnerable older patient.25, 26 Therefore, methods to improve the performance of these processes of care may be of clinical importance.
The finding of increased use of DNAR orders in the face of equivalent documentation of code status is of interest and generates hypotheses for further study. It is possible that the educational experience and use of geriatric assessment provides a more complete context for the code status discussion (one that incorporates the patient's social, physical, and cognitive function). However, we do not know if the patients on the ACE service had improved concordance between their code status and their goals of care.
We believe that there was no difference in key clinical outcomes between Hospitalist‐ACE and control patients because the population in this study was relatively low acuity and, therefore, the occurrence of falls and the use of physical restraints were quite low in the study population. In particular, the readmission rate was much lower than is typical for the Medicare population at our hospital, making it challenging to draw conclusions about the impact of the intervention on readmissions, however, we cannot rule out the possibility that our early discharge planning did not address the determinants of readmission for this population.
The ACE unit paradigmcharacterized by 1) closed, modified hospital units; 2) staffing by geriatricians and nurses with geriatrics training; 3) employing geriatric nursing care protocolsrequires significant resources and is not feasible for all settings.6 There is a need for alternative models of comprehensive care for hospitalized elders that require fewer resources in the form of dedicated units and specialist personnel, and can be more responsive to institutional needs. For example, in a 2005 report, one institution reported the creation of a geriatric medicine service that utilized a geriatrician and hospitalist co‐attending model.14 More recently, a large geriatrics program replaced its inpatient geriatrics unit with a mobile inpatient geriatrics service staffed by an attending geriatricianhospitalist, a geriatrics fellow, and a nurse practitioner.27 While these innovative models have eliminated the dedicated unit, they rely on board certified geriatricians, a group in short supply nationally.28 Hospitalists are a rapidly growing provider group that, with appropriate training and building on the work of geriatricians, is poised to provide leadership in acute geriatric care.29, 30
In contrast to the comprehensive inpatient geriatric care models described above, the Hospitalist‐ACE service uses a specialized hospitalist workforce and is not dependent on continuous staffing by geriatricians. Although geographic concentration is important for the success of interdisciplinary rounds, the Hospitalist‐ACE service does not require a closed or modified unit. The nursing staff caring for Hospitalist‐ACE patients have generalist nursing training and, at the time of the study, did not utilize geriatric‐care protocols. Our results need to be interpreted in the light of these differences from the ACE unit model which is a significantly more intensive intervention than the Hospitalist‐ACE service. In addition, the current practice environment is quite different from the mid‐1990s when ACE units were developed and studied. Development and maintenance of models of comprehensive inpatient geriatric care require demonstration of both value as well as return on investment. The alignment of financial and regulatory incentives for programs that provide comprehensive care to complex patients, such as those anticipated by the Affordable Care Act, may encourage the growth of such models.
These data represent findings from a six‐month evaluation of a novel inpatient service in the middle of its first year. There are several limitations related to our study design. First, the results of this small study at a single academic medical center may be of limited generalizability to other settings. Second, the program was evaluated only three months after its inception; we did not capture further improvements in methods, training, and outcomes expected as the program matured. Third, most of the Hospitalist‐ACE service attendings and residents rotate on the UCH general medical services throughout the year. Consequently, we were unable to eliminate the possibility of contamination of the control group, and we were unable to blind the physicians to the study. Fourth, the study population had a relatively low severity of illnessthe average MS‐DRG weight was near 1and low rates of important adverse events such falls and restraint use. This may have occurred because we excluded patients transferred from the ICUs and other services. It is possible that the Hospitalist‐ACE intervention might have demonstrated a larger benefit in a sicker population that would have presented greater opportunities for reductions in length of stay, costs, and adverse events. Fifth, given the retrospective nature of the data collection, we were not able to prospectively assess the incidence of important geriatric outcomes such as delirium and functional decline, nor can we make conclusions about changes in function during the hospitalization.
While the outcome measures we used are conceptually similar to several measures developed by RAND's Assessing Care of Vulnerable Elders (ACOVE) project, this study did not explicitly rely on those constructs.31 To do so would have required prospective screening by clinical staff independent from the care team for vulnerability that was beyond the scope of this project. In addition, the ACOVE measures of interest for functional and cognitive decline are limited to documentation of cognitive or functional assessments in the medical record. The ACE service's adoption of a brief standardized geriatric assessment was almost certain to meet that documentation requirement. While documentation is important, it is not clear that documentation, in and of itself, improves outcomes. Therefore, we expanded upon the ACOVE constructs to include the need for the additional evidence of a treatment plan when abnormal physical or cognitive function was documented. These constructs are important process of care for vulnerable elders. While we demonstrated improvements in several of these important processes of care for elderly patients, we are unable to draw conclusions about the impact of these differences in care on important clinical outcomes such as development of delirium, long‐term institutionalization, or mortality.
CONCLUSIONS
The risks of hospitalization for older persons are numerous, and present challenges and opportunities for inpatient physicians. As the hospitalized population agesmirroring national demographic trends and trends in use of acute care hospitalsthe challenge of avoiding harm in the older hospitalized patient will intensify. Innovations in care to improve the experience and outcomes of hospitalization for older patients are needed in the face of limited geriatrics‐trained workforce and few discretionary funds for unit redesign. The Hospitalist‐ACE service is a promising strategy for hospitalist programs with sufficient numbers of older patients and hospitalists with interest in improving clinical care for older adults. It provides a model for hospitalists to employ geriatrics principles targeted at reducing harm to their most vulnerable patients. Hospitalist‐run geriatric care models offer great promise for improving the care of acutely ill elderly patients. Future investigation should focus on demonstrating the impact of such care on important clinical outcomes between admission and discharge; on model refinement and adaptation, such as determining what components of comprehensive geriatric care are essential to success; and on how complementary interventions, such as the use of templated orders for the hospitalized elderly, impact outcomes. Additional research is needed, with a focus on demonstrating value with regard to an array of outcomes including cost, readmissions, and preventable harms of care.
Acknowledgements
Jean Kutner, MD, MSPH; Daniel Sandy, MPH; Shelly Limon, RN; nurses of 12 West; the UCH staff on the interdisciplinary team; and ACE patients and their families.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,.Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care.Am J Med.1999;106:565–573.
- ,,, et al.Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders.J Am Geriatr Soc.2007;55(11):1705–1711.
- ,,, et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5:69–75.
- ,,,,.What does the medical record reveal about functional status? A comparison of medical record and interview data.J Gen Intern Med.2001;16(11):728–736.
- ,,,,,.Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's “Retooling for an Aging America” report.J Am Geriatr Soc.2009;57(12):2328–2337.
- ,,,,.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1581.
- ,,, et al.The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta‐analysis.J Am Geriatr Soc.2010;58:83–92.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.A randomized, controlled clinical trial of a geriatrics consultation team: compliance with recommendations.JAMA.1986;255:2617–2621.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Dissemination and characteristics of Acute Care of Elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19:220–227.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,,,.The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- ,,.The Patient Health Questionnaire‐2: validity of a two‐item depression screener.Med Care.2003;41:1284–1292.
- ,,,,,.Clarifying confusion: the Confusion Assessment Method.Ann Intern Med.1990;113(12):941–948.
- ,,, et al.The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am Geriatr Soc.2001;49:1691–1699.
- ,.The timed “Up and Go”: a test of basic functional mobility for frail elderly persons.J Am Geriatr Soc.1991;39:142–148.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention.Guideline for the prevention of falls in older persons.J Am Geriatr Soc.2001;49:664–672.
- . Falls for the inpatient physician. Translating knowledge into action. The Portal of Online Geriatric Education (POGOe). 6–19‐2008. Available at: http://www.pogoe.org/productid/20212.
- ,,,. Incontinence and urinary catheters for the inpatient physician. The Portal of Online Geriatric Education (POGOe). 11–27‐0008. Available at: http://www.pogoe.org/productid/20296.
- ,,,.Use of medications for insomnia in the hospitalized geriatric population.J Am Geriatr Soc.2008;56(3):579–581.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130(4 pt 2):343–349.
- ,,, et al.Quality of care associated with survival in vulnerable older patients.Ann Intern Med.2005;143:274–281.
- ,,, et al.Higher quality of care for hosptialized frail older adults is associated with improved survival one year after discharge.J Hosp Med.2009;4(S1):24.
- ,,,.Operational and quality outcomes of a novel mobile acute care for the elderly service.J Am Geriatr Soc.2009;57:S1.
- Institute of Medicine (IOM).Retooling for an Aging America: Building the Health Care Workforce.Washington, DC:The National Academies Press;2008.
- ,,.Alternative solutions to the geriatric workforce deficit.Am J Med.2008;121:e23.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,.Assessing care of vulnerable elders: ACOVE project overview.Ann Intern Med.2001;135(8 pt 2):642–646.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,.Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care.Am J Med.1999;106:565–573.
- ,,, et al.Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders.J Am Geriatr Soc.2007;55(11):1705–1711.
- ,,, et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5:69–75.
- ,,,,.What does the medical record reveal about functional status? A comparison of medical record and interview data.J Gen Intern Med.2001;16(11):728–736.
- ,,,,,.Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's “Retooling for an Aging America” report.J Am Geriatr Soc.2009;57(12):2328–2337.
- ,,,,.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1581.
- ,,, et al.The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta‐analysis.J Am Geriatr Soc.2010;58:83–92.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.A randomized, controlled clinical trial of a geriatrics consultation team: compliance with recommendations.JAMA.1986;255:2617–2621.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Dissemination and characteristics of Acute Care of Elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19:220–227.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,,,.The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- ,,.The Patient Health Questionnaire‐2: validity of a two‐item depression screener.Med Care.2003;41:1284–1292.
- ,,,,,.Clarifying confusion: the Confusion Assessment Method.Ann Intern Med.1990;113(12):941–948.
- ,,, et al.The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am Geriatr Soc.2001;49:1691–1699.
- ,.The timed “Up and Go”: a test of basic functional mobility for frail elderly persons.J Am Geriatr Soc.1991;39:142–148.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention.Guideline for the prevention of falls in older persons.J Am Geriatr Soc.2001;49:664–672.
- . Falls for the inpatient physician. Translating knowledge into action. The Portal of Online Geriatric Education (POGOe). 6–19‐2008. Available at: http://www.pogoe.org/productid/20212.
- ,,,. Incontinence and urinary catheters for the inpatient physician. The Portal of Online Geriatric Education (POGOe). 11–27‐0008. Available at: http://www.pogoe.org/productid/20296.
- ,,,.Use of medications for insomnia in the hospitalized geriatric population.J Am Geriatr Soc.2008;56(3):579–581.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130(4 pt 2):343–349.
- ,,, et al.Quality of care associated with survival in vulnerable older patients.Ann Intern Med.2005;143:274–281.
- ,,, et al.Higher quality of care for hosptialized frail older adults is associated with improved survival one year after discharge.J Hosp Med.2009;4(S1):24.
- ,,,.Operational and quality outcomes of a novel mobile acute care for the elderly service.J Am Geriatr Soc.2009;57:S1.
- Institute of Medicine (IOM).Retooling for an Aging America: Building the Health Care Workforce.Washington, DC:The National Academies Press;2008.
- ,,.Alternative solutions to the geriatric workforce deficit.Am J Med.2008;121:e23.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,.Assessing care of vulnerable elders: ACOVE project overview.Ann Intern Med.2001;135(8 pt 2):642–646.
Copyright © 2011 Society of Hospital Medicine
In the Literature
In This Edition
Literature at a Glance
A guide to this month’s studies
- PE and COPD exacerbations.
- Care bundles and readmission rates.
- Family history and VTE risk.
- Vasopressor choice and mortality in sepsis.
- Vitamin K use in overanticoagulation.
- Appropriate treatment of asymptomatic bacteriuria.
- Guideline adherence in thrombocytopenia.
Pulmonary Embolism Frequently Complicates COPD Exacerbations
Clinical question: What percentage of patients with acute chronic obstructive pulmonary disease (COPD) exacerbations has pulmonary emboli?
Background: As many as 30% of COPD exacerbations have no apparent precipitating event. Even in patients with evidence of a precipitating event, such as an upper-respiratory illness or increased environmental irritants, pulmonary emboli (PE) may coexist and warrant evaluation.
Study design: Literature review.
Setting: Multiple studies in Europe and the U.S.
Synopsis: This literature review included five studies to estimate the rate of PE in patients with a COPD exacerbation. Overall incidence of PE in COPD exacerbations was 19.9%, but of those patients requiring hospitalization, the incidence was as high as 25.5%. Incidence estimates varied based on interpretation of data that were missing or inconsistent between studies. Patients most commonly present with dyspnea, chest pain, hemoptysis, cough, and palpitations. Six percent of PE patients presented with syncope; no patients with an exacerbation without a PE presented with syncope.
Risk of mortality from PE is almost twice as high in patients with a COPD exacerbation compared with PE in other settings. A significant number of patients have PE without history or evidence of DVT, so in situ thrombosis is a significant factor. The interpretation of these results is limited by the heterogeneity of the study designs, and by the relatively low number of cases. Larger trials are necessary.
Bottom line: Pulmonary emboli are present in as many as 25% of all COPD exacerbations. Delay in diagnosis of PE in COPD patients affects morbidity and mortality. PE should be a consideration in many COPD exacerbations.
Citation: Rizkallah J, Man SF, Din DD. Prevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2009;135(3):786-793.
Targeted-Care Bundle Can Reduce ED Visits and Readmission Rates in High-Risk Elderly Patients
Clinical question: Can a care coordination bundle reduce length of stay (LOS), ED visits, or readmissions within 30 days of a hospital admission?
Background: Hospital-based care coordination interventions have shown mixed results in affecting LOS, post-discharge ED visits, and readmission rates. Although there has been some success with particular interventions, no consistent benefit has been demonstrated. Most notably, a recent meta-analysis of several different interventions showed no improvement in mortality, LOS, or readmission rates.
Study design: A randomized, controlled trial of select high-risk elderly patients.
Setting: A large teaching hospital at Baylor University Medical Center.
Synopsis: A “targeted-care bundle” was implemented with high-risk elderly patients to try to reduce LOS, readmissions, and ED visits. High-risk patients were identified by age, diagnosis-related group (DRG), number of medications at admission, comorbid conditions, and need for assistance in activities of daily living. Subjects were randomized to usual care or to receive a targeted-care bundle. The targeted-care bundle included multiple interventions. A study care coordinator provided daily patient education, including condition-specific teaching, discharge teaching and planning, and a follow-up phone call at five to seven days after discharge. A clinical pharmacist intervened for medication reconciliation at admission and discharge, medication teaching, and a follow-up phone call at five to seven days after discharge. Structured documents, including a personal health record and supplemental discharge form, were implemented.
The study had low enrollment, largely due to the requirement to obtain informed consent from all participants. Therefore, the study was underpowered to detect such target endpoints as LOS. A significant decrease in 30-day readmission rates/ED visits was noticed, but there was no persistent effect at 60 days.
The intervention was designed to use existing hospital staff in order to be practical for broad utilization. Future studies need to focus on increased enrollment to demonstrate beneficial effect.
Bottom line: Targeted health interventions focusing on education and coordination of care might effect some significant outcomes, most notably readmissions or ED visits within 30 days, but the nature of the clinical problem makes rigorous testing of interventions a challenge.
Citation: Kohler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Family History Is a Risk Factor for Venous Thrombosis
Clinical question: Is family history of additional value in predicting an individual’s risk of venous thrombosis once a genetic risk factor is identified?
Background: A positive family history of venous thrombosis might suggest the presence of genetic risk factors in a given family. However, it is not known whether family history is of additional significance—once a risk factor is identified—in predicting an individual’s risk for venous thrombosis.
Study design: Population-based, case-control study.
Setting: Participants in the Multiple Environmental and Genetic Assessment (MEGA) of risk factors for venous thrombosis study.
Synopsis: Recruitment, data collection, and blood samples were obtained from individuals in the MEGA study. Participants completed a questionnaire about risk factors for venous thrombosis and family history. A positive family history more than doubled the risk of venous thrombosis, and when more than one family member was affected, the risk increased fourfold. The risk for venous thrombosis increased 64 times for individuals who had a family history, genetic risk factor, and environmental risk factor when compared with those with a negative family history and no known risk factors.
The underreporting or overestimation of the prevalence of a positive family history might limit this study.
Bottom line: Family history is a risk indictor for a first venous thrombosis, despite the presence of other risk factors.
Citation: Bezemer ID, van der Meer FJ, Eikenboom JC, Rosendaal FR, Doggen CJ. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med. 2009;169(6):610-615.
Vasopressor Choice Predicts Mortality in Septic Shock
Clinical question: Does vasopressor choice affect mortality in patients with community-acquired septic shock?
Background: Community-acquired septic shock is a common illness and, despite aggressive care, a leading cause of death. Randomized clinical control trials evaluating the efficacy and safety of different adrenergic supportive agents are lacking. Thus, both norepinephrine and dopamine are recommended as first-line agents in the treatment of septic shock by the Surviving Sepsis Campaign guidelines.
Study design: Multicenter, cohort observational study.
Setting: Seventeen intensive-care units in Portugal.
Synopsis: In adjusted analysis controlling for Simplified Acute Physiology Score (SAPS) II, use of norepinephrine in community-acquired septic shock was associated with higher hospital mortality and lower 28-day survival when compared with dopamine. Specifically, patients treated with norepinephrine had a statistically significant higher hospital mortality rate than those treated with dopamine (52% and 38.5%, respectively, P=0.002) and a lower 28-day survival (log rank=22.6; P<0.001). While this data is valuable, the nonrandomized, observational study design limits firm conclusions regarding vasopressor choice. Further results from three large trials comparing vasopressor use in septic shock should continue to shed light on this debate.
Bottom line: Norepinephrine administration is associated with higher hospital mortality and lower 28-day survival when compared with dopamine in patients with community-acquired septic shock.
Citation: Póvoa PR, Carneiro AH, Ribeiro OS, Pereira AC, Portuguese Community-Acquired Sepsis Study Group. Influence of vasopressor agent in septic shock mortality. Results from the Portuguese Community-Acquired Sepsis Study (SACiUCI study). Crit Care Med. 2009;37(2):410-416.
Oral Vitamin K Versus Placebo to Correct Excess Anticoagulation in Warfarin Patients
Clinical question: In nonbleeding patients with warfarin-associated coagulopathy, does oral vitamin K reduce bleeding events when compared to placebo?
Background: Warfarin is a common drug for primary and secondary prevention of thromboembolism, but it requires continued monitoring of the international normalized ratio (INR) value. INR values >4.0 are associated with an increase in bleeding complications, with specific concern for intracranial bleeding when INR values exceed 4.5. Small, randomized trials have shown that single, low-dose administration of oral vitamin K effectively reduces the INR in nonbleeding, overanticoagulated patients.
However, these studies have not shown if vitamin K reduces risk for bleeding without increasing the risk for thromboembolism.
Study design: Randomized, placebo-controlled trial.
Setting: Fourteen anticoagulation clinics in Canada, Italy, and the U.S.
Synopsis: Nonbleeding patients with supratherapeutic INR values between 4.5 and 10.0 were randomly assigned to receive 1.25 mg of oral vitamin K or placebo, then evaluated for all forms of bleeding for 90 days. Bleeding events were defined as “major bleeding,” “minor bleeding,” and “trivial bleeding.”
Though patients who received oral vitamin K had a significantly more rapid INR decrease, there were no differences between the two groups with regard to all bleeding events, thromboembolism, or death. The study was underpowered to detect differences in major bleeding.
Bottom line: Low-dose oral vitamin K leads to more rapid correction of the INR in overanticoagulated patients on warfarin therapy, but has little effect on clinical outcomes at 90 days.
Citation: Crowther MA, Ageno W, Garcia D, et al. Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin: a randomized trial. Ann Intern Med. 2009;150(5):293-300.
Inappropriate Treatment of Catheter-Associated Asymptomatic Bacteriuria
Clinical question: Are hospitalized patients with urinary catheters inappropriately treated with antibiotics for asymptomatic bacteriuria?
Background: Persons with catheters acquire bacteriuria at the rate of 3% to 10% per day, but in the majority of cases, no symptoms or secondary complications occur. Evidenced-based guidelines state that asymptomatic bacteriuria is not a clinically significant infection, and numerous studies have shown that treatment is unlikely to confer clinical benefit.
Study design: Retrospective cohort study.
Setting: A single-site Veterans Affairs hospital.
Synopsis: Using urine culture results over a three-month period from a single VA medical center, 280 cases were analyzed: 164 catheter-associated asymptomatic bacteriuria and 116 catheter-associated urinary tract infections (UTIs). A UTI was defined as having one or more of these symptoms: fever, urgency, frequency, dysuria, suprapubic tenderness, altered mental status, or hypotension in a patient without another recognized infection and a positive urine culture. Of the asymptomatic bacteriuria cases, 68% were managed appropriately with no antibiotic treatment; 32% were inappropriately treated with antibiotics.
In multivariate analysis, older patient age, predominance of gram-negative bacteria, and higher urine white blood cell count were significantly associated with inappropriate treatment.
This study highlights the fact that antibiotics continue to be used inappropriately in patients with catheters. Current guidelines do not distinguish well between asymptomatic bacteriuria and UTI, so there might be a knowledge gap. This study was based on urine culture data, not urinalysis of all patients with a catheter, so the symptomatic patients were likely over-represented.
An associated editorial observes that the study extrapolates data from studies that involved patients with uncomplicated UTIs and, therefore, might reach erroneous conclusions. Further, viewing catheter-associated symptomatic UTIs and catheter-associated asymptomatic bactiuria as dichotomous and warranting inherently different management fails to encompass a number of clinical factors, including co-infection, and further fails to acknowledge that removal of the catheter is the first step in treatment. However, the finding that antibiotics continue to be used inappropriately is useful.
Bottom line: A clinical determination of whether a patient with a catheter really has a symptomatic UTI/urosepsis or only has asymptomatic bacteriuria should precede starting antibiotics in hospitalized patients.
Citations: Cope M, Cevallos ME, Cadle RM, Darouiche RO, Musher DM, Trautner BW. Inappropriate treatment of catheter-associated asymptomatic bateriuria in a tertiary care hospital. Clin Infect Dis. 2009;48(9):1182-1188.
Kunin CM. Catheter-associated urinary tract infections: a syllogism compounded by a questionable dichotomy. Clin Infect Dis. 2009;48:1189-1190.
Current Practices in the Evaluation and Management of Thrombocytopenia in Heparin Patients
Clinical question: Are the current American College of Chest Physicians (ACCP) guidelines for the recognition, treatment, and prevention of heparin-induced thrombocytopenia (HIT) being followed?
Background: Heparin-based anticoagulation is frequently given to hospitalized patients, and approximately 1% to 5% of these patients develop HIT. In 2004, the ACCP published a consensus statement on the evaluation, management, and prevention of HIT.
Study design: Prospective, observational study.
Setting: Forty-eight U.S. hospitals in the Complications After Thrombocytopenia Caused by Heparin (CATCH) registry.
Synopsis: The CATCH trial enrolled patients receiving any form of heparin for >96 hours (n=2,420), cardiac-care-unit patients treated with heparin (n=1,090), and patients who had an HIT antibody assay performed (n=449), for a total of 3,536 total patients. The study included patients on unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH). Thrombocytopenia was defined at a platelet count <150,000, or a decrease of 50% when compared with admission.
In the prolonged heparin group, 36.4% of patients developed thrombocytopenia; however, HIT was suspected in only 19.8% of these high-risk patients. While physicians were more likely to consider HIT in the cardiac-care patients (37.6%), the diagnosis was considered>24 hours after the thrombocytopenia developed. Physicians often waited until after a thromboembolic complication occurred before evaluating for HIT. More often than not, preventive measures were missed (e.g., failing to check for HIT antibodies, continuing heparin after HIT was suspected).
Bottom line: Thrombocytopenia is a common occurrence in patients receiving heparin and, despite the risk of devastating complications from HIT, treatment infrequently conforms to the established guidelines.
Citation: Crespo EM, Oliveira GBF, Honeycutt EF, et al. Evaluation and management of thrombocytopenia and suspected heparin-induced thrombocytopenia in hospitalized patients: The Complications After Thrombocytopenia Caused by Heparin (CATCH) registry. Am Heart J. 2009;157(4):651-657. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- PE and COPD exacerbations.
- Care bundles and readmission rates.
- Family history and VTE risk.
- Vasopressor choice and mortality in sepsis.
- Vitamin K use in overanticoagulation.
- Appropriate treatment of asymptomatic bacteriuria.
- Guideline adherence in thrombocytopenia.
Pulmonary Embolism Frequently Complicates COPD Exacerbations
Clinical question: What percentage of patients with acute chronic obstructive pulmonary disease (COPD) exacerbations has pulmonary emboli?
Background: As many as 30% of COPD exacerbations have no apparent precipitating event. Even in patients with evidence of a precipitating event, such as an upper-respiratory illness or increased environmental irritants, pulmonary emboli (PE) may coexist and warrant evaluation.
Study design: Literature review.
Setting: Multiple studies in Europe and the U.S.
Synopsis: This literature review included five studies to estimate the rate of PE in patients with a COPD exacerbation. Overall incidence of PE in COPD exacerbations was 19.9%, but of those patients requiring hospitalization, the incidence was as high as 25.5%. Incidence estimates varied based on interpretation of data that were missing or inconsistent between studies. Patients most commonly present with dyspnea, chest pain, hemoptysis, cough, and palpitations. Six percent of PE patients presented with syncope; no patients with an exacerbation without a PE presented with syncope.
Risk of mortality from PE is almost twice as high in patients with a COPD exacerbation compared with PE in other settings. A significant number of patients have PE without history or evidence of DVT, so in situ thrombosis is a significant factor. The interpretation of these results is limited by the heterogeneity of the study designs, and by the relatively low number of cases. Larger trials are necessary.
Bottom line: Pulmonary emboli are present in as many as 25% of all COPD exacerbations. Delay in diagnosis of PE in COPD patients affects morbidity and mortality. PE should be a consideration in many COPD exacerbations.
Citation: Rizkallah J, Man SF, Din DD. Prevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2009;135(3):786-793.
Targeted-Care Bundle Can Reduce ED Visits and Readmission Rates in High-Risk Elderly Patients
Clinical question: Can a care coordination bundle reduce length of stay (LOS), ED visits, or readmissions within 30 days of a hospital admission?
Background: Hospital-based care coordination interventions have shown mixed results in affecting LOS, post-discharge ED visits, and readmission rates. Although there has been some success with particular interventions, no consistent benefit has been demonstrated. Most notably, a recent meta-analysis of several different interventions showed no improvement in mortality, LOS, or readmission rates.
Study design: A randomized, controlled trial of select high-risk elderly patients.
Setting: A large teaching hospital at Baylor University Medical Center.
Synopsis: A “targeted-care bundle” was implemented with high-risk elderly patients to try to reduce LOS, readmissions, and ED visits. High-risk patients were identified by age, diagnosis-related group (DRG), number of medications at admission, comorbid conditions, and need for assistance in activities of daily living. Subjects were randomized to usual care or to receive a targeted-care bundle. The targeted-care bundle included multiple interventions. A study care coordinator provided daily patient education, including condition-specific teaching, discharge teaching and planning, and a follow-up phone call at five to seven days after discharge. A clinical pharmacist intervened for medication reconciliation at admission and discharge, medication teaching, and a follow-up phone call at five to seven days after discharge. Structured documents, including a personal health record and supplemental discharge form, were implemented.
The study had low enrollment, largely due to the requirement to obtain informed consent from all participants. Therefore, the study was underpowered to detect such target endpoints as LOS. A significant decrease in 30-day readmission rates/ED visits was noticed, but there was no persistent effect at 60 days.
The intervention was designed to use existing hospital staff in order to be practical for broad utilization. Future studies need to focus on increased enrollment to demonstrate beneficial effect.
Bottom line: Targeted health interventions focusing on education and coordination of care might effect some significant outcomes, most notably readmissions or ED visits within 30 days, but the nature of the clinical problem makes rigorous testing of interventions a challenge.
Citation: Kohler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Family History Is a Risk Factor for Venous Thrombosis
Clinical question: Is family history of additional value in predicting an individual’s risk of venous thrombosis once a genetic risk factor is identified?
Background: A positive family history of venous thrombosis might suggest the presence of genetic risk factors in a given family. However, it is not known whether family history is of additional significance—once a risk factor is identified—in predicting an individual’s risk for venous thrombosis.
Study design: Population-based, case-control study.
Setting: Participants in the Multiple Environmental and Genetic Assessment (MEGA) of risk factors for venous thrombosis study.
Synopsis: Recruitment, data collection, and blood samples were obtained from individuals in the MEGA study. Participants completed a questionnaire about risk factors for venous thrombosis and family history. A positive family history more than doubled the risk of venous thrombosis, and when more than one family member was affected, the risk increased fourfold. The risk for venous thrombosis increased 64 times for individuals who had a family history, genetic risk factor, and environmental risk factor when compared with those with a negative family history and no known risk factors.
The underreporting or overestimation of the prevalence of a positive family history might limit this study.
Bottom line: Family history is a risk indictor for a first venous thrombosis, despite the presence of other risk factors.
Citation: Bezemer ID, van der Meer FJ, Eikenboom JC, Rosendaal FR, Doggen CJ. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med. 2009;169(6):610-615.
Vasopressor Choice Predicts Mortality in Septic Shock
Clinical question: Does vasopressor choice affect mortality in patients with community-acquired septic shock?
Background: Community-acquired septic shock is a common illness and, despite aggressive care, a leading cause of death. Randomized clinical control trials evaluating the efficacy and safety of different adrenergic supportive agents are lacking. Thus, both norepinephrine and dopamine are recommended as first-line agents in the treatment of septic shock by the Surviving Sepsis Campaign guidelines.
Study design: Multicenter, cohort observational study.
Setting: Seventeen intensive-care units in Portugal.
Synopsis: In adjusted analysis controlling for Simplified Acute Physiology Score (SAPS) II, use of norepinephrine in community-acquired septic shock was associated with higher hospital mortality and lower 28-day survival when compared with dopamine. Specifically, patients treated with norepinephrine had a statistically significant higher hospital mortality rate than those treated with dopamine (52% and 38.5%, respectively, P=0.002) and a lower 28-day survival (log rank=22.6; P<0.001). While this data is valuable, the nonrandomized, observational study design limits firm conclusions regarding vasopressor choice. Further results from three large trials comparing vasopressor use in septic shock should continue to shed light on this debate.
Bottom line: Norepinephrine administration is associated with higher hospital mortality and lower 28-day survival when compared with dopamine in patients with community-acquired septic shock.
Citation: Póvoa PR, Carneiro AH, Ribeiro OS, Pereira AC, Portuguese Community-Acquired Sepsis Study Group. Influence of vasopressor agent in septic shock mortality. Results from the Portuguese Community-Acquired Sepsis Study (SACiUCI study). Crit Care Med. 2009;37(2):410-416.
Oral Vitamin K Versus Placebo to Correct Excess Anticoagulation in Warfarin Patients
Clinical question: In nonbleeding patients with warfarin-associated coagulopathy, does oral vitamin K reduce bleeding events when compared to placebo?
Background: Warfarin is a common drug for primary and secondary prevention of thromboembolism, but it requires continued monitoring of the international normalized ratio (INR) value. INR values >4.0 are associated with an increase in bleeding complications, with specific concern for intracranial bleeding when INR values exceed 4.5. Small, randomized trials have shown that single, low-dose administration of oral vitamin K effectively reduces the INR in nonbleeding, overanticoagulated patients.
However, these studies have not shown if vitamin K reduces risk for bleeding without increasing the risk for thromboembolism.
Study design: Randomized, placebo-controlled trial.
Setting: Fourteen anticoagulation clinics in Canada, Italy, and the U.S.
Synopsis: Nonbleeding patients with supratherapeutic INR values between 4.5 and 10.0 were randomly assigned to receive 1.25 mg of oral vitamin K or placebo, then evaluated for all forms of bleeding for 90 days. Bleeding events were defined as “major bleeding,” “minor bleeding,” and “trivial bleeding.”
Though patients who received oral vitamin K had a significantly more rapid INR decrease, there were no differences between the two groups with regard to all bleeding events, thromboembolism, or death. The study was underpowered to detect differences in major bleeding.
Bottom line: Low-dose oral vitamin K leads to more rapid correction of the INR in overanticoagulated patients on warfarin therapy, but has little effect on clinical outcomes at 90 days.
Citation: Crowther MA, Ageno W, Garcia D, et al. Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin: a randomized trial. Ann Intern Med. 2009;150(5):293-300.
Inappropriate Treatment of Catheter-Associated Asymptomatic Bacteriuria
Clinical question: Are hospitalized patients with urinary catheters inappropriately treated with antibiotics for asymptomatic bacteriuria?
Background: Persons with catheters acquire bacteriuria at the rate of 3% to 10% per day, but in the majority of cases, no symptoms or secondary complications occur. Evidenced-based guidelines state that asymptomatic bacteriuria is not a clinically significant infection, and numerous studies have shown that treatment is unlikely to confer clinical benefit.
Study design: Retrospective cohort study.
Setting: A single-site Veterans Affairs hospital.
Synopsis: Using urine culture results over a three-month period from a single VA medical center, 280 cases were analyzed: 164 catheter-associated asymptomatic bacteriuria and 116 catheter-associated urinary tract infections (UTIs). A UTI was defined as having one or more of these symptoms: fever, urgency, frequency, dysuria, suprapubic tenderness, altered mental status, or hypotension in a patient without another recognized infection and a positive urine culture. Of the asymptomatic bacteriuria cases, 68% were managed appropriately with no antibiotic treatment; 32% were inappropriately treated with antibiotics.
In multivariate analysis, older patient age, predominance of gram-negative bacteria, and higher urine white blood cell count were significantly associated with inappropriate treatment.
This study highlights the fact that antibiotics continue to be used inappropriately in patients with catheters. Current guidelines do not distinguish well between asymptomatic bacteriuria and UTI, so there might be a knowledge gap. This study was based on urine culture data, not urinalysis of all patients with a catheter, so the symptomatic patients were likely over-represented.
An associated editorial observes that the study extrapolates data from studies that involved patients with uncomplicated UTIs and, therefore, might reach erroneous conclusions. Further, viewing catheter-associated symptomatic UTIs and catheter-associated asymptomatic bactiuria as dichotomous and warranting inherently different management fails to encompass a number of clinical factors, including co-infection, and further fails to acknowledge that removal of the catheter is the first step in treatment. However, the finding that antibiotics continue to be used inappropriately is useful.
Bottom line: A clinical determination of whether a patient with a catheter really has a symptomatic UTI/urosepsis or only has asymptomatic bacteriuria should precede starting antibiotics in hospitalized patients.
Citations: Cope M, Cevallos ME, Cadle RM, Darouiche RO, Musher DM, Trautner BW. Inappropriate treatment of catheter-associated asymptomatic bateriuria in a tertiary care hospital. Clin Infect Dis. 2009;48(9):1182-1188.
Kunin CM. Catheter-associated urinary tract infections: a syllogism compounded by a questionable dichotomy. Clin Infect Dis. 2009;48:1189-1190.
Current Practices in the Evaluation and Management of Thrombocytopenia in Heparin Patients
Clinical question: Are the current American College of Chest Physicians (ACCP) guidelines for the recognition, treatment, and prevention of heparin-induced thrombocytopenia (HIT) being followed?
Background: Heparin-based anticoagulation is frequently given to hospitalized patients, and approximately 1% to 5% of these patients develop HIT. In 2004, the ACCP published a consensus statement on the evaluation, management, and prevention of HIT.
Study design: Prospective, observational study.
Setting: Forty-eight U.S. hospitals in the Complications After Thrombocytopenia Caused by Heparin (CATCH) registry.
Synopsis: The CATCH trial enrolled patients receiving any form of heparin for >96 hours (n=2,420), cardiac-care-unit patients treated with heparin (n=1,090), and patients who had an HIT antibody assay performed (n=449), for a total of 3,536 total patients. The study included patients on unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH). Thrombocytopenia was defined at a platelet count <150,000, or a decrease of 50% when compared with admission.
In the prolonged heparin group, 36.4% of patients developed thrombocytopenia; however, HIT was suspected in only 19.8% of these high-risk patients. While physicians were more likely to consider HIT in the cardiac-care patients (37.6%), the diagnosis was considered>24 hours after the thrombocytopenia developed. Physicians often waited until after a thromboembolic complication occurred before evaluating for HIT. More often than not, preventive measures were missed (e.g., failing to check for HIT antibodies, continuing heparin after HIT was suspected).
Bottom line: Thrombocytopenia is a common occurrence in patients receiving heparin and, despite the risk of devastating complications from HIT, treatment infrequently conforms to the established guidelines.
Citation: Crespo EM, Oliveira GBF, Honeycutt EF, et al. Evaluation and management of thrombocytopenia and suspected heparin-induced thrombocytopenia in hospitalized patients: The Complications After Thrombocytopenia Caused by Heparin (CATCH) registry. Am Heart J. 2009;157(4):651-657. TH
In This Edition
Literature at a Glance
A guide to this month’s studies
- PE and COPD exacerbations.
- Care bundles and readmission rates.
- Family history and VTE risk.
- Vasopressor choice and mortality in sepsis.
- Vitamin K use in overanticoagulation.
- Appropriate treatment of asymptomatic bacteriuria.
- Guideline adherence in thrombocytopenia.
Pulmonary Embolism Frequently Complicates COPD Exacerbations
Clinical question: What percentage of patients with acute chronic obstructive pulmonary disease (COPD) exacerbations has pulmonary emboli?
Background: As many as 30% of COPD exacerbations have no apparent precipitating event. Even in patients with evidence of a precipitating event, such as an upper-respiratory illness or increased environmental irritants, pulmonary emboli (PE) may coexist and warrant evaluation.
Study design: Literature review.
Setting: Multiple studies in Europe and the U.S.
Synopsis: This literature review included five studies to estimate the rate of PE in patients with a COPD exacerbation. Overall incidence of PE in COPD exacerbations was 19.9%, but of those patients requiring hospitalization, the incidence was as high as 25.5%. Incidence estimates varied based on interpretation of data that were missing or inconsistent between studies. Patients most commonly present with dyspnea, chest pain, hemoptysis, cough, and palpitations. Six percent of PE patients presented with syncope; no patients with an exacerbation without a PE presented with syncope.
Risk of mortality from PE is almost twice as high in patients with a COPD exacerbation compared with PE in other settings. A significant number of patients have PE without history or evidence of DVT, so in situ thrombosis is a significant factor. The interpretation of these results is limited by the heterogeneity of the study designs, and by the relatively low number of cases. Larger trials are necessary.
Bottom line: Pulmonary emboli are present in as many as 25% of all COPD exacerbations. Delay in diagnosis of PE in COPD patients affects morbidity and mortality. PE should be a consideration in many COPD exacerbations.
Citation: Rizkallah J, Man SF, Din DD. Prevalence of pulmonary embolism in acute exacerbations of COPD: a systematic review and metaanalysis. Chest. 2009;135(3):786-793.
Targeted-Care Bundle Can Reduce ED Visits and Readmission Rates in High-Risk Elderly Patients
Clinical question: Can a care coordination bundle reduce length of stay (LOS), ED visits, or readmissions within 30 days of a hospital admission?
Background: Hospital-based care coordination interventions have shown mixed results in affecting LOS, post-discharge ED visits, and readmission rates. Although there has been some success with particular interventions, no consistent benefit has been demonstrated. Most notably, a recent meta-analysis of several different interventions showed no improvement in mortality, LOS, or readmission rates.
Study design: A randomized, controlled trial of select high-risk elderly patients.
Setting: A large teaching hospital at Baylor University Medical Center.
Synopsis: A “targeted-care bundle” was implemented with high-risk elderly patients to try to reduce LOS, readmissions, and ED visits. High-risk patients were identified by age, diagnosis-related group (DRG), number of medications at admission, comorbid conditions, and need for assistance in activities of daily living. Subjects were randomized to usual care or to receive a targeted-care bundle. The targeted-care bundle included multiple interventions. A study care coordinator provided daily patient education, including condition-specific teaching, discharge teaching and planning, and a follow-up phone call at five to seven days after discharge. A clinical pharmacist intervened for medication reconciliation at admission and discharge, medication teaching, and a follow-up phone call at five to seven days after discharge. Structured documents, including a personal health record and supplemental discharge form, were implemented.
The study had low enrollment, largely due to the requirement to obtain informed consent from all participants. Therefore, the study was underpowered to detect such target endpoints as LOS. A significant decrease in 30-day readmission rates/ED visits was noticed, but there was no persistent effect at 60 days.
The intervention was designed to use existing hospital staff in order to be practical for broad utilization. Future studies need to focus on increased enrollment to demonstrate beneficial effect.
Bottom line: Targeted health interventions focusing on education and coordination of care might effect some significant outcomes, most notably readmissions or ED visits within 30 days, but the nature of the clinical problem makes rigorous testing of interventions a challenge.
Citation: Kohler BE, Richter KM, Youngblood L, et al. Reduction of 30-day postdischarge hospital readmission or emergency department (ED) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J Hosp Med. 2009;4(4):211-218.
Family History Is a Risk Factor for Venous Thrombosis
Clinical question: Is family history of additional value in predicting an individual’s risk of venous thrombosis once a genetic risk factor is identified?
Background: A positive family history of venous thrombosis might suggest the presence of genetic risk factors in a given family. However, it is not known whether family history is of additional significance—once a risk factor is identified—in predicting an individual’s risk for venous thrombosis.
Study design: Population-based, case-control study.
Setting: Participants in the Multiple Environmental and Genetic Assessment (MEGA) of risk factors for venous thrombosis study.
Synopsis: Recruitment, data collection, and blood samples were obtained from individuals in the MEGA study. Participants completed a questionnaire about risk factors for venous thrombosis and family history. A positive family history more than doubled the risk of venous thrombosis, and when more than one family member was affected, the risk increased fourfold. The risk for venous thrombosis increased 64 times for individuals who had a family history, genetic risk factor, and environmental risk factor when compared with those with a negative family history and no known risk factors.
The underreporting or overestimation of the prevalence of a positive family history might limit this study.
Bottom line: Family history is a risk indictor for a first venous thrombosis, despite the presence of other risk factors.
Citation: Bezemer ID, van der Meer FJ, Eikenboom JC, Rosendaal FR, Doggen CJ. The value of family history as a risk indicator for venous thrombosis. Arch Intern Med. 2009;169(6):610-615.
Vasopressor Choice Predicts Mortality in Septic Shock
Clinical question: Does vasopressor choice affect mortality in patients with community-acquired septic shock?
Background: Community-acquired septic shock is a common illness and, despite aggressive care, a leading cause of death. Randomized clinical control trials evaluating the efficacy and safety of different adrenergic supportive agents are lacking. Thus, both norepinephrine and dopamine are recommended as first-line agents in the treatment of septic shock by the Surviving Sepsis Campaign guidelines.
Study design: Multicenter, cohort observational study.
Setting: Seventeen intensive-care units in Portugal.
Synopsis: In adjusted analysis controlling for Simplified Acute Physiology Score (SAPS) II, use of norepinephrine in community-acquired septic shock was associated with higher hospital mortality and lower 28-day survival when compared with dopamine. Specifically, patients treated with norepinephrine had a statistically significant higher hospital mortality rate than those treated with dopamine (52% and 38.5%, respectively, P=0.002) and a lower 28-day survival (log rank=22.6; P<0.001). While this data is valuable, the nonrandomized, observational study design limits firm conclusions regarding vasopressor choice. Further results from three large trials comparing vasopressor use in septic shock should continue to shed light on this debate.
Bottom line: Norepinephrine administration is associated with higher hospital mortality and lower 28-day survival when compared with dopamine in patients with community-acquired septic shock.
Citation: Póvoa PR, Carneiro AH, Ribeiro OS, Pereira AC, Portuguese Community-Acquired Sepsis Study Group. Influence of vasopressor agent in septic shock mortality. Results from the Portuguese Community-Acquired Sepsis Study (SACiUCI study). Crit Care Med. 2009;37(2):410-416.
Oral Vitamin K Versus Placebo to Correct Excess Anticoagulation in Warfarin Patients
Clinical question: In nonbleeding patients with warfarin-associated coagulopathy, does oral vitamin K reduce bleeding events when compared to placebo?
Background: Warfarin is a common drug for primary and secondary prevention of thromboembolism, but it requires continued monitoring of the international normalized ratio (INR) value. INR values >4.0 are associated with an increase in bleeding complications, with specific concern for intracranial bleeding when INR values exceed 4.5. Small, randomized trials have shown that single, low-dose administration of oral vitamin K effectively reduces the INR in nonbleeding, overanticoagulated patients.
However, these studies have not shown if vitamin K reduces risk for bleeding without increasing the risk for thromboembolism.
Study design: Randomized, placebo-controlled trial.
Setting: Fourteen anticoagulation clinics in Canada, Italy, and the U.S.
Synopsis: Nonbleeding patients with supratherapeutic INR values between 4.5 and 10.0 were randomly assigned to receive 1.25 mg of oral vitamin K or placebo, then evaluated for all forms of bleeding for 90 days. Bleeding events were defined as “major bleeding,” “minor bleeding,” and “trivial bleeding.”
Though patients who received oral vitamin K had a significantly more rapid INR decrease, there were no differences between the two groups with regard to all bleeding events, thromboembolism, or death. The study was underpowered to detect differences in major bleeding.
Bottom line: Low-dose oral vitamin K leads to more rapid correction of the INR in overanticoagulated patients on warfarin therapy, but has little effect on clinical outcomes at 90 days.
Citation: Crowther MA, Ageno W, Garcia D, et al. Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin: a randomized trial. Ann Intern Med. 2009;150(5):293-300.
Inappropriate Treatment of Catheter-Associated Asymptomatic Bacteriuria
Clinical question: Are hospitalized patients with urinary catheters inappropriately treated with antibiotics for asymptomatic bacteriuria?
Background: Persons with catheters acquire bacteriuria at the rate of 3% to 10% per day, but in the majority of cases, no symptoms or secondary complications occur. Evidenced-based guidelines state that asymptomatic bacteriuria is not a clinically significant infection, and numerous studies have shown that treatment is unlikely to confer clinical benefit.
Study design: Retrospective cohort study.
Setting: A single-site Veterans Affairs hospital.
Synopsis: Using urine culture results over a three-month period from a single VA medical center, 280 cases were analyzed: 164 catheter-associated asymptomatic bacteriuria and 116 catheter-associated urinary tract infections (UTIs). A UTI was defined as having one or more of these symptoms: fever, urgency, frequency, dysuria, suprapubic tenderness, altered mental status, or hypotension in a patient without another recognized infection and a positive urine culture. Of the asymptomatic bacteriuria cases, 68% were managed appropriately with no antibiotic treatment; 32% were inappropriately treated with antibiotics.
In multivariate analysis, older patient age, predominance of gram-negative bacteria, and higher urine white blood cell count were significantly associated with inappropriate treatment.
This study highlights the fact that antibiotics continue to be used inappropriately in patients with catheters. Current guidelines do not distinguish well between asymptomatic bacteriuria and UTI, so there might be a knowledge gap. This study was based on urine culture data, not urinalysis of all patients with a catheter, so the symptomatic patients were likely over-represented.
An associated editorial observes that the study extrapolates data from studies that involved patients with uncomplicated UTIs and, therefore, might reach erroneous conclusions. Further, viewing catheter-associated symptomatic UTIs and catheter-associated asymptomatic bactiuria as dichotomous and warranting inherently different management fails to encompass a number of clinical factors, including co-infection, and further fails to acknowledge that removal of the catheter is the first step in treatment. However, the finding that antibiotics continue to be used inappropriately is useful.
Bottom line: A clinical determination of whether a patient with a catheter really has a symptomatic UTI/urosepsis or only has asymptomatic bacteriuria should precede starting antibiotics in hospitalized patients.
Citations: Cope M, Cevallos ME, Cadle RM, Darouiche RO, Musher DM, Trautner BW. Inappropriate treatment of catheter-associated asymptomatic bateriuria in a tertiary care hospital. Clin Infect Dis. 2009;48(9):1182-1188.
Kunin CM. Catheter-associated urinary tract infections: a syllogism compounded by a questionable dichotomy. Clin Infect Dis. 2009;48:1189-1190.
Current Practices in the Evaluation and Management of Thrombocytopenia in Heparin Patients
Clinical question: Are the current American College of Chest Physicians (ACCP) guidelines for the recognition, treatment, and prevention of heparin-induced thrombocytopenia (HIT) being followed?
Background: Heparin-based anticoagulation is frequently given to hospitalized patients, and approximately 1% to 5% of these patients develop HIT. In 2004, the ACCP published a consensus statement on the evaluation, management, and prevention of HIT.
Study design: Prospective, observational study.
Setting: Forty-eight U.S. hospitals in the Complications After Thrombocytopenia Caused by Heparin (CATCH) registry.
Synopsis: The CATCH trial enrolled patients receiving any form of heparin for >96 hours (n=2,420), cardiac-care-unit patients treated with heparin (n=1,090), and patients who had an HIT antibody assay performed (n=449), for a total of 3,536 total patients. The study included patients on unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH). Thrombocytopenia was defined at a platelet count <150,000, or a decrease of 50% when compared with admission.
In the prolonged heparin group, 36.4% of patients developed thrombocytopenia; however, HIT was suspected in only 19.8% of these high-risk patients. While physicians were more likely to consider HIT in the cardiac-care patients (37.6%), the diagnosis was considered>24 hours after the thrombocytopenia developed. Physicians often waited until after a thromboembolic complication occurred before evaluating for HIT. More often than not, preventive measures were missed (e.g., failing to check for HIT antibodies, continuing heparin after HIT was suspected).
Bottom line: Thrombocytopenia is a common occurrence in patients receiving heparin and, despite the risk of devastating complications from HIT, treatment infrequently conforms to the established guidelines.
Citation: Crespo EM, Oliveira GBF, Honeycutt EF, et al. Evaluation and management of thrombocytopenia and suspected heparin-induced thrombocytopenia in hospitalized patients: The Complications After Thrombocytopenia Caused by Heparin (CATCH) registry. Am Heart J. 2009;157(4):651-657. TH
In the Literature
In This Edition
- Cost sharing for prescription medications increases consumption of more costly healthcare services
- Community-acquired pneumonia core measures can lead to unintended consequences
- Prophylactic revascularization has no clear benefit for high-risk patients undergoing vascular surgery
- Aspirin resistance correlates with adverse clinical events
- Low-molecular-weight heparin appears to have greater efficacy as a prophylactic agent against deep-vein thrombosis and pulmonary embolism
- Antipsychotic medications appear to be associated with increased risk of death in demented patients
- Anticoagulation plus antiplatelet therapy fails to show benefit for peripheral arterial disease
- Transient atrial fibrillation following myocardial infarction increases the risk of recurrence and stroke
Do Incentives to Encourage Use of Certain Medications Affect Care?
Background: Insurers are increasingly using financial mechanisms to affect pharmaceutical usage. These practices may affect medication use and health outcomes in ways that are poorly defined and difficult to detect.
Study design: Literature review
Synopsis: There are numerous structures for drug-cost sharing, and this study evaluated co-payments, tiers/co-insurance, benefit caps, formulary limitations, and reference pricing strategies for their effect on prescription drug usage and healthcare outcomes.
Included articles varied widely in study design, making generalizable results difficult to isolate, and insurers may have instituted more than one cost-sharing mechanism simultaneously. Overall, for every 10% increase in cost sharing (via copayments or co-insurance) there was an associated 2%-6% decrease in prescription drug spending. Increasing consumer costs for medications clearly decreases usage.
Some studies demonstrated that the decrease in medication utilization was more pronounced for “nonessential” medications over “essential” medications. However, in specific chronic illnesses this is clearly associated with greater usage of inpatient and emergency medical services.
Cost sharing was also more likely to have adverse health consequences in vulnerable populations, particularly the elderly and poor. One in four Medicaid patients couldn’t fill at least one prescription in the past year, as opposed to one in 10 privately insured patients who couldn’t purchase one or more medications.
Further impact on healthcare consumption and outcomes may be masked because it is difficult to determine individual disease severity, and the effect on the more severely ill would be expected to be greater. These authors attempted to sort out a complex interaction between cost, consumption, and health, and they found important trends.
The goal of cost sharing is to align consumption more clearly with appropriate and economic products, thereby using cost sharing as a public health tool. The consequence of creating the incentives for ill patients to forego necessary treatments is a counterbalancing concern that is supported in some, but not all, of the literature.
Bottom line: Cost sharing for prescription medications decreases medication spending and utilization but disproportionately affects the disadvantaged and increases consumption of more costly healthcare services in patients with some chronic illnesses.
Citation: Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61-69.
Does Antibiotic Requirement for Suspected CAP Increase Misdiagnosis?
Background: Early administration of antibiotics in community-acquired pneumonia (CAP) improves patient outcomes. The Infectious Disease Society of America instituted guidelines that recommend initiation of antibiotics to all patients with suspected CAP within four hours of triage, and some payors are using this as a quality measure affecting reimbursement. However, this incentive may cause premature diagnosis of CAP and overuse of antibiotics.
Study design: Retrospective chart review
Setting: A large, high-volume teaching hospital with more than 500 beds and more than 112,000 annual emergency department (ED) visits
Synopsis: Charts of all patients with an admitting diagnosis of CAP were reviewed over two six-month periods. The initial review was prior to initiation of a four-hour antibiotics rule; the second was after a financial incentive to initiate antibiotics within four hours of triage was initiated.
After initiation of the four-hour rule, of the patients with an admitting diagnosis of CAP, significantly more patients received antibiotics within four hours of triage (66% versus 54%). However, the number of patients with abnormal chest X-ray findings associated with the diagnosis of CAP decreased from 28.5% to 20.6%, and the proportion of patients with a discharge diagnosis of CAP decreased from 75.9% to 58.9%.
The authors also used two diagnostic paradigms to make an independent diagnosis of CAP based on chart data. With the less rigorous independent analysis 44.7% of patients actually had CAP prior to the four-hour rule, and this fell to 36% after the four-hour rule. Using a more rigorous definition, only 32.7% of patients actually had CAP prior to initiation of the four-hour rule, and this fell to 27%.
There was no difference in length of stay or ICU transfers between the two analysis periods. The authors concluded that a four-hour rule increases premature diagnosis of CAP, presumably because providers felt compelled to initiate antibiotics before they had complete clinical data.
This tendency was associated with misuse and overuse of antibiotics, and increased laboratory testing, such as blood cultures, which had to be obtained before antibiotics were initiated. The authors emphasized the importance of reimbursement-associated quality measures creating incentives to treat the right patients for the correct diagnosis, and the potential harmful consequences of applying a quality-driven protocol to the wrong patient.
They suggest a six-hour rule would decrease the misdiagnosis of CAP. They also feel eliminating a mandatory time frame and requiring only that the first dose of antibiotics be administered in the ED will further ameliorate these effects.
Bottom line: Mandatory administration of antibiotics to patients with suspected CAP within four hours of triage increases the percentage of patients who receive antibiotics within four hours, but also increases the rate of misdiagnosis of CAP, inappropriate administration of antibiotics, and increased use of some laboratory services.
Citation: Kanwar M, Brar N, Khatib R, et al. Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4-hour antibiotic administration rule. Chest. 2007 Jun;131(6):1865-1869.
Does prophylactic cardiac revascularization benefit patients undergoing vascular surgery?
Background: American College of Cardiology/American Heart Association Guidelines recommend referral for patients with multiple cardiac risk factors for non-invasive cardiac stress testing prior to surgery and prophylactic revascularization in high-risk patients. The authors performed a pilot analysis to determine how many patients would be needed to prospectively validate this recommendation in those with more significant ischemic cardiac disease.
Study design: Randomized controlled pilot study of 1,880 consecutive patients undergoing elective vascular surgery
Setting: Brazil, Belgium, the Netherlands, Italy, Serbia, and Montenegro
Synopsis: This was a pilot study to determine the necessary power to prove or disprove the benefit of the recommendation for cardiac revascularization in high-risk patients before major vascular surgery.
Prior research had shown that prophylactic revascularization is not of demonstrable benefit in this cohort. However, the majority of the patients in this previous trial had two-vessel disease and preserved left ventricular function. This study examined a sicker cohort of patients with more significant coronary artery disease and depressed left ventricular function.
This pilot screened all patients undergoing high-risk vascular surgery. All patients with three or more risk factors underwent non-invasive evaluation for cardiac ischemia. Patients with extensive ischemia were randomized to invasive evaluation and revascularization as appropriate or non-invasive management. Both arms received optimal medical management.
Prophylactic revascularization did not improve 30-day outcome after vascular surgery, demonstrated no difference in perioperative cardiac events, and found no difference in all-cause mortality or nonfatal myocardial infarction. Similarly, there was no evidence of long-term (at one year) difference between groups. The sample size needed to definitively establish that coronary revascularization is superior to medical therapy would be 300 patients per arm. That would require screening 9,000 patients.
Bottom line: Prophylactic revascularization has no clear benefit for high-risk patients undergoing vascular surgery, but a much larger sample size would be required to definitively prove or disprove benefit.
Citation: Poldermans D, Schouten O, Vidakovic R, et al. Clinical randomized trial to evaluate the safety of a noninvasive approach in high-risk patients undergoing major vascular surgery: the DECREASE-V pilot study. J. Am Coll Cardiol. 2007;49(17):1763-1769.
How Does Aspirin Resistance Affect Patients with Coronary Artery Disease?
Background: Although aspirin is used to decrease the risk of ischemic events, up to 45% of patients do not derive adequate anti-platelet activity. Few prospective studies have used laboratory-measured aspirin resistance to assess clinical outcomes.
Study design: Blinded cohort
Setting: Patients affiliated with Queen Mary Hospital, the University of Hong Kong.
Synopsis: Aspirin-induced platelet inhibition was measured quantitatively on 468 patients with stable coronary artery disease who take 80-325 mg of aspirin per day. The study found 128 patients were aspirin resistant. Aspirin resistance was more prevalent with increased age, female gender, renal insufficiency, anemia, and with use of low-dose aspirin. At follow up, aspirin-resistant patients were more likely to develop a primary outcome event: cardiovascular deaths, myocardial infarction, stroke, transient ischemic attack, and unstable angina. Aspirin resistance was an independent risk factor for developing the aforementioned outcomes, as are diabetes, prior myocardial infarction, and low hemoglobin.
Bottom line: Aspirin resistance, as defined by an aggregation-based assay, is associated with adverse outcomes in patients with stable coronary artery disease.
Citation: Chen W, Cheng X, Lee PY, et al. Aspirin resistance and adverse clinical events in patients with coronary artery disease. Am J Med. 2007 Jul;120(7):631-635.
Which Agents Best Prevent Venous Thromboembolism?
Background: Pulmonary emboli have been linked to 10% of in-hospital deaths. There continues to be a strong emphasis on prevention. Unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), and selective factor Xa inhibitors are used for prophylaxis.
Study design: A meta-analysis of randomized controlled trials
Synopsis: The meta-analysis included 36 studies of hospitalized medical patients that compared UFH with control, LMWH with control, LMWH with UFH, and a selective factor Xa inhibitor with a placebo.
When each was compared with a control, UFH and LMWH were associated with a decreased risk of deep venous thrombosis (DVT) (risk ratio=0.33; 0.56) and pulmonary embolism (PE) (risk ratio=0.64; 0.37). Compared with control, LMWH three times daily was more effective than twice-daily dosing (risk ratio=0.27, 0.52). Through direct comparison of UFH and LMWH, LMWH was shown to have decreased DVT risk (risk ratio=0.68) and fewer injection site hematomas (risk ratio=0.47).
Neither UFH nor LMWH reduced mortality. LMWH and UFH were associated with significantly more bleeding events than control, but this increased risk was significant only for minor bleeding.
Bottom line: LMWH appears to have greater efficacy than UFH as a prophylactic agent against DVT/PE. If UFH is used, three times daily dosing is preferred.
Citation: Wein L, Wein S, Haas SJ, et al. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients. Arch Intern Med. 2007;167(14):1476-1486.
What Is the Association Between Antipsychotic Drugs and Mortality?
Background: Atypical antipsychotics prescribed off-label for problematic behaviors in dementia have been associated with risks including diabetes, stroke, and increased mortality. This resulted in the FDA placing a “black box” warning on atypical antipsychotics used for dementia. Subsequent studies have suggested that conventional antipsychotics are perhaps even more problematic.
Study Design: Retrospective cohort study
Synopsis: This trial found a small but significant increase in the risk of death in patients taking an antipsychotic medication.
The adjusted hazard ratio for death with the use of atypical antipsychotics in community dwelling patients with dementia was 1.3 (confidence interval 1.02-1.70). Similar to prior research, the authors found that conventional antipsychotics carried a higher risk than atypical agents.
Patients in long-term care settings also suffered increased risk compared with community dwelling patients. Interestingly, the increased risk of death was apparent after as little as a month of treatment.
As with all retrospective observational cohort trials, there remains the risk that an unanticipated confounding factor could skew the data and create a false association. However, the findings of this research support prior concerns that antipsychotics carry risk of increased mortality. This research bolsters the argument that these agents should not be used lightly or without full discussion of risks and benefits with the patient and/or proxy.
Bottom line: Antipsychotic agents used in patients with dementia may create increased risk of death. Potential benefit needs to be carefully weighted against this serious harm.
Citation: Gill S, Bronskill SE, Normand SL, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007 June 5;146(11):775-786.
Does Combination Therapy Help Prevent Serious Vascular Ischemic Events?
Background: Peripheral arterial disease (PAD) manifests as claudication and limb ischemia affecting 8.5 million Americans. Atherosclerotic disease in the periphery also reflects increased risk for ischemic events in the coronary and cranial circulations. Both antiplatelet agents and anticoagulation will decrease the probability of thrombus formation, although this must be weighed against bleeding risk.
Study design: Randomized, open-label, multicenter trial
Setting: Eighty centers in Europe, Asia, Australia, and North America
Synopsis: This trial randomized more than 2,000 patients with PAD to treatment with antiplatelet therapy (aspirin, ticlopidine, or clopidogrel) with or without additional anticoagulation.
During the next 3.5 years serious vascular events occurred at approximately the same rate in both combination and monotherapy groups (15.9% versus 17.4%, p=0.37). There was no significant difference between the occurrence of the composite ischemic endpoints or any of the individual endpoints. There was, however, a significantly higher rate of both moderate and life-threatening bleeding in the combination therapy group.
The 4% risk of life-threatening hemorrhage in the combination group exceeded the 1.2% rate of the monotherapy group creating a relative risk for bleeding of 3.4.
This trial demonstrates that for patients with PAD on antiplatelet therapy, the increased rate of bleeding without significant added benefit makes addition of warfarin inadvisable.1 Evidence of utility of combination therapy from studies in other arterial systems provides mixed results.2-4 Based on the results of this study, combination therapy cannot be advocated if the primary symptoms are from PAD.
Bottom line: This study provides further evidence that more is not always better when it comes to preventing thrombosis and ischemia in the peripheral arterial system. Antiplatelet agents are preferable for PAD to combination antiplatelet plus anticoagulation.
Citations:
- The Warfarin Antiplatelet Vascular Evaluation Trial Investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007 Jul 19;357(3):217-227.
- Hurlen M, Abdelnoor M, Smith P, et al. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002 Sep 26;347(13):969-974.
- Mohr JP, Thompson JL, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001 Nov 15;345(20):1444-1451.
- The ESPRIT Study Group. Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial. Lancet Neurol. 2007 Feb;6:115-124.
Does Transient Atrial Fibrillation Increase Stroke Risk After ST-Elevation Myocardial Infarction?
Background: Prior research has demonstrated that 2.1% of patients will suffer a stroke in the year following a heart attack. Persistent and paroxysmal atrial fibrillation (AF) are well recognized as risk factors for stroke, but the significance of transient ischemia-induced AF is less clear.
Study design: Retrospective cohort study
Setting: Queen Mary Hospital, Hong Kong
Synopsis: The study involved patients admitted for acute inferior ST-segment-elevation myocardial infarction (MI) with preserved left ventricular ejection fraction.
Transient AF that had converted back to normal sinus rhythm by discharge was observed in 14% of patients after the MI. Over the next three years the transient AF patients were 15 times more likely than those who remained in sinus rhythm during the index hospitalization to have recurrent AF (34% versus 2%). Despite antiplatelet therapy in both groups, ischemic stroke developed in 22% of patients who had transient AF following their MI, compared with only 4% in patients who did not (HR 5.1, confidence interval 2.4-11.2). Cerebrovascular accidents generally occurred simultaneously with recurrence of paroxysmal AF.1-2
The finding that patients with transient-ischemia-induced AF represents a group with markedly higher risk of ischemic stroke is compelling. It suggests that these patients may be candidates for combined antiplatelet and anticoagulant therapy. Trials of combined therapy following MI demonstrate that this strategy reduces the rate of recurrent cardiac ischemia, stroke, or death but does carry significantly increased risk of bleeding.3-4
Bottom line: The presence of transient AF following MI represents a significant risk factor for the development of subsequent paroxysmal AF. These patients have a five-fold increased risk of ischemic stroke over the next three years and should be considered for combined antiplatelet and anticoagulant therapy.
Citations:
- Chung-Wah S, Man-Hong J, Hee-Hwa H, et al. Transient atrial fibrillation complicating acute inferior myocardial infarction: implications for future risk of ischemic stroke. Chest. 2007 Mar 30;132(1):44-49.
- Witt BJ, Ballman KV, Brown RD Jr., Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J. Med. 2006;119(4):354 e1-9.
- Van Es RF, Jonker J, Verheugt F, et al. Aspirin and Coumadin after acute coronary syndromes (the ASPECT-2 study): a randomised controlled trial. Lancet. 2002 Jul 13;360(9327):109-113.
- Hurlen M, Abdelnoor M, Smith P, et al. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002 Sep 26;347(13):969-974. TH
In This Edition
- Cost sharing for prescription medications increases consumption of more costly healthcare services
- Community-acquired pneumonia core measures can lead to unintended consequences
- Prophylactic revascularization has no clear benefit for high-risk patients undergoing vascular surgery
- Aspirin resistance correlates with adverse clinical events
- Low-molecular-weight heparin appears to have greater efficacy as a prophylactic agent against deep-vein thrombosis and pulmonary embolism
- Antipsychotic medications appear to be associated with increased risk of death in demented patients
- Anticoagulation plus antiplatelet therapy fails to show benefit for peripheral arterial disease
- Transient atrial fibrillation following myocardial infarction increases the risk of recurrence and stroke
Do Incentives to Encourage Use of Certain Medications Affect Care?
Background: Insurers are increasingly using financial mechanisms to affect pharmaceutical usage. These practices may affect medication use and health outcomes in ways that are poorly defined and difficult to detect.
Study design: Literature review
Synopsis: There are numerous structures for drug-cost sharing, and this study evaluated co-payments, tiers/co-insurance, benefit caps, formulary limitations, and reference pricing strategies for their effect on prescription drug usage and healthcare outcomes.
Included articles varied widely in study design, making generalizable results difficult to isolate, and insurers may have instituted more than one cost-sharing mechanism simultaneously. Overall, for every 10% increase in cost sharing (via copayments or co-insurance) there was an associated 2%-6% decrease in prescription drug spending. Increasing consumer costs for medications clearly decreases usage.
Some studies demonstrated that the decrease in medication utilization was more pronounced for “nonessential” medications over “essential” medications. However, in specific chronic illnesses this is clearly associated with greater usage of inpatient and emergency medical services.
Cost sharing was also more likely to have adverse health consequences in vulnerable populations, particularly the elderly and poor. One in four Medicaid patients couldn’t fill at least one prescription in the past year, as opposed to one in 10 privately insured patients who couldn’t purchase one or more medications.
Further impact on healthcare consumption and outcomes may be masked because it is difficult to determine individual disease severity, and the effect on the more severely ill would be expected to be greater. These authors attempted to sort out a complex interaction between cost, consumption, and health, and they found important trends.
The goal of cost sharing is to align consumption more clearly with appropriate and economic products, thereby using cost sharing as a public health tool. The consequence of creating the incentives for ill patients to forego necessary treatments is a counterbalancing concern that is supported in some, but not all, of the literature.
Bottom line: Cost sharing for prescription medications decreases medication spending and utilization but disproportionately affects the disadvantaged and increases consumption of more costly healthcare services in patients with some chronic illnesses.
Citation: Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61-69.
Does Antibiotic Requirement for Suspected CAP Increase Misdiagnosis?
Background: Early administration of antibiotics in community-acquired pneumonia (CAP) improves patient outcomes. The Infectious Disease Society of America instituted guidelines that recommend initiation of antibiotics to all patients with suspected CAP within four hours of triage, and some payors are using this as a quality measure affecting reimbursement. However, this incentive may cause premature diagnosis of CAP and overuse of antibiotics.
Study design: Retrospective chart review
Setting: A large, high-volume teaching hospital with more than 500 beds and more than 112,000 annual emergency department (ED) visits
Synopsis: Charts of all patients with an admitting diagnosis of CAP were reviewed over two six-month periods. The initial review was prior to initiation of a four-hour antibiotics rule; the second was after a financial incentive to initiate antibiotics within four hours of triage was initiated.
After initiation of the four-hour rule, of the patients with an admitting diagnosis of CAP, significantly more patients received antibiotics within four hours of triage (66% versus 54%). However, the number of patients with abnormal chest X-ray findings associated with the diagnosis of CAP decreased from 28.5% to 20.6%, and the proportion of patients with a discharge diagnosis of CAP decreased from 75.9% to 58.9%.
The authors also used two diagnostic paradigms to make an independent diagnosis of CAP based on chart data. With the less rigorous independent analysis 44.7% of patients actually had CAP prior to the four-hour rule, and this fell to 36% after the four-hour rule. Using a more rigorous definition, only 32.7% of patients actually had CAP prior to initiation of the four-hour rule, and this fell to 27%.
There was no difference in length of stay or ICU transfers between the two analysis periods. The authors concluded that a four-hour rule increases premature diagnosis of CAP, presumably because providers felt compelled to initiate antibiotics before they had complete clinical data.
This tendency was associated with misuse and overuse of antibiotics, and increased laboratory testing, such as blood cultures, which had to be obtained before antibiotics were initiated. The authors emphasized the importance of reimbursement-associated quality measures creating incentives to treat the right patients for the correct diagnosis, and the potential harmful consequences of applying a quality-driven protocol to the wrong patient.
They suggest a six-hour rule would decrease the misdiagnosis of CAP. They also feel eliminating a mandatory time frame and requiring only that the first dose of antibiotics be administered in the ED will further ameliorate these effects.
Bottom line: Mandatory administration of antibiotics to patients with suspected CAP within four hours of triage increases the percentage of patients who receive antibiotics within four hours, but also increases the rate of misdiagnosis of CAP, inappropriate administration of antibiotics, and increased use of some laboratory services.
Citation: Kanwar M, Brar N, Khatib R, et al. Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4-hour antibiotic administration rule. Chest. 2007 Jun;131(6):1865-1869.
Does prophylactic cardiac revascularization benefit patients undergoing vascular surgery?
Background: American College of Cardiology/American Heart Association Guidelines recommend referral for patients with multiple cardiac risk factors for non-invasive cardiac stress testing prior to surgery and prophylactic revascularization in high-risk patients. The authors performed a pilot analysis to determine how many patients would be needed to prospectively validate this recommendation in those with more significant ischemic cardiac disease.
Study design: Randomized controlled pilot study of 1,880 consecutive patients undergoing elective vascular surgery
Setting: Brazil, Belgium, the Netherlands, Italy, Serbia, and Montenegro
Synopsis: This was a pilot study to determine the necessary power to prove or disprove the benefit of the recommendation for cardiac revascularization in high-risk patients before major vascular surgery.
Prior research had shown that prophylactic revascularization is not of demonstrable benefit in this cohort. However, the majority of the patients in this previous trial had two-vessel disease and preserved left ventricular function. This study examined a sicker cohort of patients with more significant coronary artery disease and depressed left ventricular function.
This pilot screened all patients undergoing high-risk vascular surgery. All patients with three or more risk factors underwent non-invasive evaluation for cardiac ischemia. Patients with extensive ischemia were randomized to invasive evaluation and revascularization as appropriate or non-invasive management. Both arms received optimal medical management.
Prophylactic revascularization did not improve 30-day outcome after vascular surgery, demonstrated no difference in perioperative cardiac events, and found no difference in all-cause mortality or nonfatal myocardial infarction. Similarly, there was no evidence of long-term (at one year) difference between groups. The sample size needed to definitively establish that coronary revascularization is superior to medical therapy would be 300 patients per arm. That would require screening 9,000 patients.
Bottom line: Prophylactic revascularization has no clear benefit for high-risk patients undergoing vascular surgery, but a much larger sample size would be required to definitively prove or disprove benefit.
Citation: Poldermans D, Schouten O, Vidakovic R, et al. Clinical randomized trial to evaluate the safety of a noninvasive approach in high-risk patients undergoing major vascular surgery: the DECREASE-V pilot study. J. Am Coll Cardiol. 2007;49(17):1763-1769.
How Does Aspirin Resistance Affect Patients with Coronary Artery Disease?
Background: Although aspirin is used to decrease the risk of ischemic events, up to 45% of patients do not derive adequate anti-platelet activity. Few prospective studies have used laboratory-measured aspirin resistance to assess clinical outcomes.
Study design: Blinded cohort
Setting: Patients affiliated with Queen Mary Hospital, the University of Hong Kong.
Synopsis: Aspirin-induced platelet inhibition was measured quantitatively on 468 patients with stable coronary artery disease who take 80-325 mg of aspirin per day. The study found 128 patients were aspirin resistant. Aspirin resistance was more prevalent with increased age, female gender, renal insufficiency, anemia, and with use of low-dose aspirin. At follow up, aspirin-resistant patients were more likely to develop a primary outcome event: cardiovascular deaths, myocardial infarction, stroke, transient ischemic attack, and unstable angina. Aspirin resistance was an independent risk factor for developing the aforementioned outcomes, as are diabetes, prior myocardial infarction, and low hemoglobin.
Bottom line: Aspirin resistance, as defined by an aggregation-based assay, is associated with adverse outcomes in patients with stable coronary artery disease.
Citation: Chen W, Cheng X, Lee PY, et al. Aspirin resistance and adverse clinical events in patients with coronary artery disease. Am J Med. 2007 Jul;120(7):631-635.
Which Agents Best Prevent Venous Thromboembolism?
Background: Pulmonary emboli have been linked to 10% of in-hospital deaths. There continues to be a strong emphasis on prevention. Unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), and selective factor Xa inhibitors are used for prophylaxis.
Study design: A meta-analysis of randomized controlled trials
Synopsis: The meta-analysis included 36 studies of hospitalized medical patients that compared UFH with control, LMWH with control, LMWH with UFH, and a selective factor Xa inhibitor with a placebo.
When each was compared with a control, UFH and LMWH were associated with a decreased risk of deep venous thrombosis (DVT) (risk ratio=0.33; 0.56) and pulmonary embolism (PE) (risk ratio=0.64; 0.37). Compared with control, LMWH three times daily was more effective than twice-daily dosing (risk ratio=0.27, 0.52). Through direct comparison of UFH and LMWH, LMWH was shown to have decreased DVT risk (risk ratio=0.68) and fewer injection site hematomas (risk ratio=0.47).
Neither UFH nor LMWH reduced mortality. LMWH and UFH were associated with significantly more bleeding events than control, but this increased risk was significant only for minor bleeding.
Bottom line: LMWH appears to have greater efficacy than UFH as a prophylactic agent against DVT/PE. If UFH is used, three times daily dosing is preferred.
Citation: Wein L, Wein S, Haas SJ, et al. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients. Arch Intern Med. 2007;167(14):1476-1486.
What Is the Association Between Antipsychotic Drugs and Mortality?
Background: Atypical antipsychotics prescribed off-label for problematic behaviors in dementia have been associated with risks including diabetes, stroke, and increased mortality. This resulted in the FDA placing a “black box” warning on atypical antipsychotics used for dementia. Subsequent studies have suggested that conventional antipsychotics are perhaps even more problematic.
Study Design: Retrospective cohort study
Synopsis: This trial found a small but significant increase in the risk of death in patients taking an antipsychotic medication.
The adjusted hazard ratio for death with the use of atypical antipsychotics in community dwelling patients with dementia was 1.3 (confidence interval 1.02-1.70). Similar to prior research, the authors found that conventional antipsychotics carried a higher risk than atypical agents.
Patients in long-term care settings also suffered increased risk compared with community dwelling patients. Interestingly, the increased risk of death was apparent after as little as a month of treatment.
As with all retrospective observational cohort trials, there remains the risk that an unanticipated confounding factor could skew the data and create a false association. However, the findings of this research support prior concerns that antipsychotics carry risk of increased mortality. This research bolsters the argument that these agents should not be used lightly or without full discussion of risks and benefits with the patient and/or proxy.
Bottom line: Antipsychotic agents used in patients with dementia may create increased risk of death. Potential benefit needs to be carefully weighted against this serious harm.
Citation: Gill S, Bronskill SE, Normand SL, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007 June 5;146(11):775-786.
Does Combination Therapy Help Prevent Serious Vascular Ischemic Events?
Background: Peripheral arterial disease (PAD) manifests as claudication and limb ischemia affecting 8.5 million Americans. Atherosclerotic disease in the periphery also reflects increased risk for ischemic events in the coronary and cranial circulations. Both antiplatelet agents and anticoagulation will decrease the probability of thrombus formation, although this must be weighed against bleeding risk.
Study design: Randomized, open-label, multicenter trial
Setting: Eighty centers in Europe, Asia, Australia, and North America
Synopsis: This trial randomized more than 2,000 patients with PAD to treatment with antiplatelet therapy (aspirin, ticlopidine, or clopidogrel) with or without additional anticoagulation.
During the next 3.5 years serious vascular events occurred at approximately the same rate in both combination and monotherapy groups (15.9% versus 17.4%, p=0.37). There was no significant difference between the occurrence of the composite ischemic endpoints or any of the individual endpoints. There was, however, a significantly higher rate of both moderate and life-threatening bleeding in the combination therapy group.
The 4% risk of life-threatening hemorrhage in the combination group exceeded the 1.2% rate of the monotherapy group creating a relative risk for bleeding of 3.4.
This trial demonstrates that for patients with PAD on antiplatelet therapy, the increased rate of bleeding without significant added benefit makes addition of warfarin inadvisable.1 Evidence of utility of combination therapy from studies in other arterial systems provides mixed results.2-4 Based on the results of this study, combination therapy cannot be advocated if the primary symptoms are from PAD.
Bottom line: This study provides further evidence that more is not always better when it comes to preventing thrombosis and ischemia in the peripheral arterial system. Antiplatelet agents are preferable for PAD to combination antiplatelet plus anticoagulation.
Citations:
- The Warfarin Antiplatelet Vascular Evaluation Trial Investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007 Jul 19;357(3):217-227.
- Hurlen M, Abdelnoor M, Smith P, et al. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002 Sep 26;347(13):969-974.
- Mohr JP, Thompson JL, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001 Nov 15;345(20):1444-1451.
- The ESPRIT Study Group. Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial. Lancet Neurol. 2007 Feb;6:115-124.
Does Transient Atrial Fibrillation Increase Stroke Risk After ST-Elevation Myocardial Infarction?
Background: Prior research has demonstrated that 2.1% of patients will suffer a stroke in the year following a heart attack. Persistent and paroxysmal atrial fibrillation (AF) are well recognized as risk factors for stroke, but the significance of transient ischemia-induced AF is less clear.
Study design: Retrospective cohort study
Setting: Queen Mary Hospital, Hong Kong
Synopsis: The study involved patients admitted for acute inferior ST-segment-elevation myocardial infarction (MI) with preserved left ventricular ejection fraction.
Transient AF that had converted back to normal sinus rhythm by discharge was observed in 14% of patients after the MI. Over the next three years the transient AF patients were 15 times more likely than those who remained in sinus rhythm during the index hospitalization to have recurrent AF (34% versus 2%). Despite antiplatelet therapy in both groups, ischemic stroke developed in 22% of patients who had transient AF following their MI, compared with only 4% in patients who did not (HR 5.1, confidence interval 2.4-11.2). Cerebrovascular accidents generally occurred simultaneously with recurrence of paroxysmal AF.1-2
The finding that patients with transient-ischemia-induced AF represents a group with markedly higher risk of ischemic stroke is compelling. It suggests that these patients may be candidates for combined antiplatelet and anticoagulant therapy. Trials of combined therapy following MI demonstrate that this strategy reduces the rate of recurrent cardiac ischemia, stroke, or death but does carry significantly increased risk of bleeding.3-4
Bottom line: The presence of transient AF following MI represents a significant risk factor for the development of subsequent paroxysmal AF. These patients have a five-fold increased risk of ischemic stroke over the next three years and should be considered for combined antiplatelet and anticoagulant therapy.
Citations:
- Chung-Wah S, Man-Hong J, Hee-Hwa H, et al. Transient atrial fibrillation complicating acute inferior myocardial infarction: implications for future risk of ischemic stroke. Chest. 2007 Mar 30;132(1):44-49.
- Witt BJ, Ballman KV, Brown RD Jr., Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J. Med. 2006;119(4):354 e1-9.
- Van Es RF, Jonker J, Verheugt F, et al. Aspirin and Coumadin after acute coronary syndromes (the ASPECT-2 study): a randomised controlled trial. Lancet. 2002 Jul 13;360(9327):109-113.
- Hurlen M, Abdelnoor M, Smith P, et al. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002 Sep 26;347(13):969-974. TH
In This Edition
- Cost sharing for prescription medications increases consumption of more costly healthcare services
- Community-acquired pneumonia core measures can lead to unintended consequences
- Prophylactic revascularization has no clear benefit for high-risk patients undergoing vascular surgery
- Aspirin resistance correlates with adverse clinical events
- Low-molecular-weight heparin appears to have greater efficacy as a prophylactic agent against deep-vein thrombosis and pulmonary embolism
- Antipsychotic medications appear to be associated with increased risk of death in demented patients
- Anticoagulation plus antiplatelet therapy fails to show benefit for peripheral arterial disease
- Transient atrial fibrillation following myocardial infarction increases the risk of recurrence and stroke
Do Incentives to Encourage Use of Certain Medications Affect Care?
Background: Insurers are increasingly using financial mechanisms to affect pharmaceutical usage. These practices may affect medication use and health outcomes in ways that are poorly defined and difficult to detect.
Study design: Literature review
Synopsis: There are numerous structures for drug-cost sharing, and this study evaluated co-payments, tiers/co-insurance, benefit caps, formulary limitations, and reference pricing strategies for their effect on prescription drug usage and healthcare outcomes.
Included articles varied widely in study design, making generalizable results difficult to isolate, and insurers may have instituted more than one cost-sharing mechanism simultaneously. Overall, for every 10% increase in cost sharing (via copayments or co-insurance) there was an associated 2%-6% decrease in prescription drug spending. Increasing consumer costs for medications clearly decreases usage.
Some studies demonstrated that the decrease in medication utilization was more pronounced for “nonessential” medications over “essential” medications. However, in specific chronic illnesses this is clearly associated with greater usage of inpatient and emergency medical services.
Cost sharing was also more likely to have adverse health consequences in vulnerable populations, particularly the elderly and poor. One in four Medicaid patients couldn’t fill at least one prescription in the past year, as opposed to one in 10 privately insured patients who couldn’t purchase one or more medications.
Further impact on healthcare consumption and outcomes may be masked because it is difficult to determine individual disease severity, and the effect on the more severely ill would be expected to be greater. These authors attempted to sort out a complex interaction between cost, consumption, and health, and they found important trends.
The goal of cost sharing is to align consumption more clearly with appropriate and economic products, thereby using cost sharing as a public health tool. The consequence of creating the incentives for ill patients to forego necessary treatments is a counterbalancing concern that is supported in some, but not all, of the literature.
Bottom line: Cost sharing for prescription medications decreases medication spending and utilization but disproportionately affects the disadvantaged and increases consumption of more costly healthcare services in patients with some chronic illnesses.
Citation: Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61-69.
Does Antibiotic Requirement for Suspected CAP Increase Misdiagnosis?
Background: Early administration of antibiotics in community-acquired pneumonia (CAP) improves patient outcomes. The Infectious Disease Society of America instituted guidelines that recommend initiation of antibiotics to all patients with suspected CAP within four hours of triage, and some payors are using this as a quality measure affecting reimbursement. However, this incentive may cause premature diagnosis of CAP and overuse of antibiotics.
Study design: Retrospective chart review
Setting: A large, high-volume teaching hospital with more than 500 beds and more than 112,000 annual emergency department (ED) visits
Synopsis: Charts of all patients with an admitting diagnosis of CAP were reviewed over two six-month periods. The initial review was prior to initiation of a four-hour antibiotics rule; the second was after a financial incentive to initiate antibiotics within four hours of triage was initiated.
After initiation of the four-hour rule, of the patients with an admitting diagnosis of CAP, significantly more patients received antibiotics within four hours of triage (66% versus 54%). However, the number of patients with abnormal chest X-ray findings associated with the diagnosis of CAP decreased from 28.5% to 20.6%, and the proportion of patients with a discharge diagnosis of CAP decreased from 75.9% to 58.9%.
The authors also used two diagnostic paradigms to make an independent diagnosis of CAP based on chart data. With the less rigorous independent analysis 44.7% of patients actually had CAP prior to the four-hour rule, and this fell to 36% after the four-hour rule. Using a more rigorous definition, only 32.7% of patients actually had CAP prior to initiation of the four-hour rule, and this fell to 27%.
There was no difference in length of stay or ICU transfers between the two analysis periods. The authors concluded that a four-hour rule increases premature diagnosis of CAP, presumably because providers felt compelled to initiate antibiotics before they had complete clinical data.
This tendency was associated with misuse and overuse of antibiotics, and increased laboratory testing, such as blood cultures, which had to be obtained before antibiotics were initiated. The authors emphasized the importance of reimbursement-associated quality measures creating incentives to treat the right patients for the correct diagnosis, and the potential harmful consequences of applying a quality-driven protocol to the wrong patient.
They suggest a six-hour rule would decrease the misdiagnosis of CAP. They also feel eliminating a mandatory time frame and requiring only that the first dose of antibiotics be administered in the ED will further ameliorate these effects.
Bottom line: Mandatory administration of antibiotics to patients with suspected CAP within four hours of triage increases the percentage of patients who receive antibiotics within four hours, but also increases the rate of misdiagnosis of CAP, inappropriate administration of antibiotics, and increased use of some laboratory services.
Citation: Kanwar M, Brar N, Khatib R, et al. Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4-hour antibiotic administration rule. Chest. 2007 Jun;131(6):1865-1869.
Does prophylactic cardiac revascularization benefit patients undergoing vascular surgery?
Background: American College of Cardiology/American Heart Association Guidelines recommend referral for patients with multiple cardiac risk factors for non-invasive cardiac stress testing prior to surgery and prophylactic revascularization in high-risk patients. The authors performed a pilot analysis to determine how many patients would be needed to prospectively validate this recommendation in those with more significant ischemic cardiac disease.
Study design: Randomized controlled pilot study of 1,880 consecutive patients undergoing elective vascular surgery
Setting: Brazil, Belgium, the Netherlands, Italy, Serbia, and Montenegro
Synopsis: This was a pilot study to determine the necessary power to prove or disprove the benefit of the recommendation for cardiac revascularization in high-risk patients before major vascular surgery.
Prior research had shown that prophylactic revascularization is not of demonstrable benefit in this cohort. However, the majority of the patients in this previous trial had two-vessel disease and preserved left ventricular function. This study examined a sicker cohort of patients with more significant coronary artery disease and depressed left ventricular function.
This pilot screened all patients undergoing high-risk vascular surgery. All patients with three or more risk factors underwent non-invasive evaluation for cardiac ischemia. Patients with extensive ischemia were randomized to invasive evaluation and revascularization as appropriate or non-invasive management. Both arms received optimal medical management.
Prophylactic revascularization did not improve 30-day outcome after vascular surgery, demonstrated no difference in perioperative cardiac events, and found no difference in all-cause mortality or nonfatal myocardial infarction. Similarly, there was no evidence of long-term (at one year) difference between groups. The sample size needed to definitively establish that coronary revascularization is superior to medical therapy would be 300 patients per arm. That would require screening 9,000 patients.
Bottom line: Prophylactic revascularization has no clear benefit for high-risk patients undergoing vascular surgery, but a much larger sample size would be required to definitively prove or disprove benefit.
Citation: Poldermans D, Schouten O, Vidakovic R, et al. Clinical randomized trial to evaluate the safety of a noninvasive approach in high-risk patients undergoing major vascular surgery: the DECREASE-V pilot study. J. Am Coll Cardiol. 2007;49(17):1763-1769.
How Does Aspirin Resistance Affect Patients with Coronary Artery Disease?
Background: Although aspirin is used to decrease the risk of ischemic events, up to 45% of patients do not derive adequate anti-platelet activity. Few prospective studies have used laboratory-measured aspirin resistance to assess clinical outcomes.
Study design: Blinded cohort
Setting: Patients affiliated with Queen Mary Hospital, the University of Hong Kong.
Synopsis: Aspirin-induced platelet inhibition was measured quantitatively on 468 patients with stable coronary artery disease who take 80-325 mg of aspirin per day. The study found 128 patients were aspirin resistant. Aspirin resistance was more prevalent with increased age, female gender, renal insufficiency, anemia, and with use of low-dose aspirin. At follow up, aspirin-resistant patients were more likely to develop a primary outcome event: cardiovascular deaths, myocardial infarction, stroke, transient ischemic attack, and unstable angina. Aspirin resistance was an independent risk factor for developing the aforementioned outcomes, as are diabetes, prior myocardial infarction, and low hemoglobin.
Bottom line: Aspirin resistance, as defined by an aggregation-based assay, is associated with adverse outcomes in patients with stable coronary artery disease.
Citation: Chen W, Cheng X, Lee PY, et al. Aspirin resistance and adverse clinical events in patients with coronary artery disease. Am J Med. 2007 Jul;120(7):631-635.
Which Agents Best Prevent Venous Thromboembolism?
Background: Pulmonary emboli have been linked to 10% of in-hospital deaths. There continues to be a strong emphasis on prevention. Unfractionated heparin (UFH), low-molecular-weight heparin (LMWH), and selective factor Xa inhibitors are used for prophylaxis.
Study design: A meta-analysis of randomized controlled trials
Synopsis: The meta-analysis included 36 studies of hospitalized medical patients that compared UFH with control, LMWH with control, LMWH with UFH, and a selective factor Xa inhibitor with a placebo.
When each was compared with a control, UFH and LMWH were associated with a decreased risk of deep venous thrombosis (DVT) (risk ratio=0.33; 0.56) and pulmonary embolism (PE) (risk ratio=0.64; 0.37). Compared with control, LMWH three times daily was more effective than twice-daily dosing (risk ratio=0.27, 0.52). Through direct comparison of UFH and LMWH, LMWH was shown to have decreased DVT risk (risk ratio=0.68) and fewer injection site hematomas (risk ratio=0.47).
Neither UFH nor LMWH reduced mortality. LMWH and UFH were associated with significantly more bleeding events than control, but this increased risk was significant only for minor bleeding.
Bottom line: LMWH appears to have greater efficacy than UFH as a prophylactic agent against DVT/PE. If UFH is used, three times daily dosing is preferred.
Citation: Wein L, Wein S, Haas SJ, et al. Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients. Arch Intern Med. 2007;167(14):1476-1486.
What Is the Association Between Antipsychotic Drugs and Mortality?
Background: Atypical antipsychotics prescribed off-label for problematic behaviors in dementia have been associated with risks including diabetes, stroke, and increased mortality. This resulted in the FDA placing a “black box” warning on atypical antipsychotics used for dementia. Subsequent studies have suggested that conventional antipsychotics are perhaps even more problematic.
Study Design: Retrospective cohort study
Synopsis: This trial found a small but significant increase in the risk of death in patients taking an antipsychotic medication.
The adjusted hazard ratio for death with the use of atypical antipsychotics in community dwelling patients with dementia was 1.3 (confidence interval 1.02-1.70). Similar to prior research, the authors found that conventional antipsychotics carried a higher risk than atypical agents.
Patients in long-term care settings also suffered increased risk compared with community dwelling patients. Interestingly, the increased risk of death was apparent after as little as a month of treatment.
As with all retrospective observational cohort trials, there remains the risk that an unanticipated confounding factor could skew the data and create a false association. However, the findings of this research support prior concerns that antipsychotics carry risk of increased mortality. This research bolsters the argument that these agents should not be used lightly or without full discussion of risks and benefits with the patient and/or proxy.
Bottom line: Antipsychotic agents used in patients with dementia may create increased risk of death. Potential benefit needs to be carefully weighted against this serious harm.
Citation: Gill S, Bronskill SE, Normand SL, et al. Antipsychotic drug use and mortality in older adults with dementia. Ann Intern Med. 2007 June 5;146(11):775-786.
Does Combination Therapy Help Prevent Serious Vascular Ischemic Events?
Background: Peripheral arterial disease (PAD) manifests as claudication and limb ischemia affecting 8.5 million Americans. Atherosclerotic disease in the periphery also reflects increased risk for ischemic events in the coronary and cranial circulations. Both antiplatelet agents and anticoagulation will decrease the probability of thrombus formation, although this must be weighed against bleeding risk.
Study design: Randomized, open-label, multicenter trial
Setting: Eighty centers in Europe, Asia, Australia, and North America
Synopsis: This trial randomized more than 2,000 patients with PAD to treatment with antiplatelet therapy (aspirin, ticlopidine, or clopidogrel) with or without additional anticoagulation.
During the next 3.5 years serious vascular events occurred at approximately the same rate in both combination and monotherapy groups (15.9% versus 17.4%, p=0.37). There was no significant difference between the occurrence of the composite ischemic endpoints or any of the individual endpoints. There was, however, a significantly higher rate of both moderate and life-threatening bleeding in the combination therapy group.
The 4% risk of life-threatening hemorrhage in the combination group exceeded the 1.2% rate of the monotherapy group creating a relative risk for bleeding of 3.4.
This trial demonstrates that for patients with PAD on antiplatelet therapy, the increased rate of bleeding without significant added benefit makes addition of warfarin inadvisable.1 Evidence of utility of combination therapy from studies in other arterial systems provides mixed results.2-4 Based on the results of this study, combination therapy cannot be advocated if the primary symptoms are from PAD.
Bottom line: This study provides further evidence that more is not always better when it comes to preventing thrombosis and ischemia in the peripheral arterial system. Antiplatelet agents are preferable for PAD to combination antiplatelet plus anticoagulation.
Citations:
- The Warfarin Antiplatelet Vascular Evaluation Trial Investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. N Engl J Med. 2007 Jul 19;357(3):217-227.
- Hurlen M, Abdelnoor M, Smith P, et al. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002 Sep 26;347(13):969-974.
- Mohr JP, Thompson JL, Lazar RM, et al. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001 Nov 15;345(20):1444-1451.
- The ESPRIT Study Group. Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial. Lancet Neurol. 2007 Feb;6:115-124.
Does Transient Atrial Fibrillation Increase Stroke Risk After ST-Elevation Myocardial Infarction?
Background: Prior research has demonstrated that 2.1% of patients will suffer a stroke in the year following a heart attack. Persistent and paroxysmal atrial fibrillation (AF) are well recognized as risk factors for stroke, but the significance of transient ischemia-induced AF is less clear.
Study design: Retrospective cohort study
Setting: Queen Mary Hospital, Hong Kong
Synopsis: The study involved patients admitted for acute inferior ST-segment-elevation myocardial infarction (MI) with preserved left ventricular ejection fraction.
Transient AF that had converted back to normal sinus rhythm by discharge was observed in 14% of patients after the MI. Over the next three years the transient AF patients were 15 times more likely than those who remained in sinus rhythm during the index hospitalization to have recurrent AF (34% versus 2%). Despite antiplatelet therapy in both groups, ischemic stroke developed in 22% of patients who had transient AF following their MI, compared with only 4% in patients who did not (HR 5.1, confidence interval 2.4-11.2). Cerebrovascular accidents generally occurred simultaneously with recurrence of paroxysmal AF.1-2
The finding that patients with transient-ischemia-induced AF represents a group with markedly higher risk of ischemic stroke is compelling. It suggests that these patients may be candidates for combined antiplatelet and anticoagulant therapy. Trials of combined therapy following MI demonstrate that this strategy reduces the rate of recurrent cardiac ischemia, stroke, or death but does carry significantly increased risk of bleeding.3-4
Bottom line: The presence of transient AF following MI represents a significant risk factor for the development of subsequent paroxysmal AF. These patients have a five-fold increased risk of ischemic stroke over the next three years and should be considered for combined antiplatelet and anticoagulant therapy.
Citations:
- Chung-Wah S, Man-Hong J, Hee-Hwa H, et al. Transient atrial fibrillation complicating acute inferior myocardial infarction: implications for future risk of ischemic stroke. Chest. 2007 Mar 30;132(1):44-49.
- Witt BJ, Ballman KV, Brown RD Jr., Meverden RA, Jacobsen SJ, Roger VL. The incidence of stroke after myocardial infarction: a meta-analysis. Am J. Med. 2006;119(4):354 e1-9.
- Van Es RF, Jonker J, Verheugt F, et al. Aspirin and Coumadin after acute coronary syndromes (the ASPECT-2 study): a randomised controlled trial. Lancet. 2002 Jul 13;360(9327):109-113.
- Hurlen M, Abdelnoor M, Smith P, et al. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002 Sep 26;347(13):969-974. TH