User login
Discharge Summary Quality
Hospitalized patients are often cared for by physicians who do not follow them in the community, creating a discontinuity of care that must be bridged through communication. This communication between inpatient and outpatient physicians occurs, in part via a discharge summary, which is intended to summarize events during hospitalization and prepare the outpatient physician to resume care of the patient. Yet, this form of communication has long been problematic.[1, 2, 3] In a 1960 study, only 30% of discharge letters were received by the primary care physician within 48 hours of discharge.[1]
More recent studies have shown little improvement. Direct communication between hospital and outpatient physicians is rare, and discharge summaries are still largely unavailable at the time of follow‐up.[4] In 1 study, primary care physicians were unaware of 62% of laboratory tests or study results that were pending on discharge,[5] in part because this information is missing from most discharge summaries.[6] Deficits such as these persist despite the fact that the rate of postdischarge completion of recommended tests, referrals, or procedures is significantly increased when the recommendation is included in the discharge summary.[7]
Regulatory mandates for discharge summaries from the Centers for Medicare and Medicaid Services[8] and from The Joint Commission[9] appear to be generally met[10, 11]; however, these mandates have no requirements for timeliness stricter than 30 days, do not require that summaries be transmitted to outpatient physicians, and do not require several content elements that might be useful to outside physicians such as condition of the patient at discharge, cognitive and functional status, goals of care, or pending studies. Expert opinion guidelines have more comprehensive recommendations,[12, 13] but it is uncertain how widely they are followed.
The existence of a discharge summary does not necessarily mean it serves a patient well in the transitional period.[11, 14, 15] Discharge summaries are a complex intervention, and we do not yet understand the best ways discharge summaries may fulfill needs specific to transitional care. Furthermore, it is uncertain what factors improve aspects of discharge summary quality as defined by timeliness, transmission, and content.[6, 16]
The goal of the DIagnosing Systemic failures, Complexities and HARm in GEriatric discharges study (DISCHARGE) was to comprehensively assess the discharge process for older patients discharged to the community. In this article we examine discharge summaries of patients enrolled in the study to determine the timeliness, transmission to outside physicians, and content of the summaries. We further examine the effect of provider training level and timeliness of dictation on discharge summary quality.
METHODS
Study Cohort
The DISCHARGE study was a prospective, observational cohort study of patients 65 years or older discharged to home from YaleNew Haven Hospital (YNHH) who were admitted with acute coronary syndrome (ACS), community‐acquired pneumonia, or heart failure (HF). Patients were screened by physicians for eligibility within 24 hours of admission using specialty society guidelines[17, 18, 19, 20] and were enrolled by telephone within 1 week of discharge. Additional inclusion criteria included speaking English or Spanish, and ability of the patient or caregiver to participate in a telephone interview. Patients enrolled in hospice were excluded, as were patients who failed the Mini‐Cog mental status screen (3‐item recall and a clock draw)[21] while in the hospital or appeared confused or delirious during the telephone interview. Caregivers of cognitively impaired patients were eligible for enrollment instead if the patient provided permission.
Study Setting
YNHH is a 966‐bed urban tertiary care hospital with statistically lower than the national average mortality for acute myocardial infarction, HF, and pneumonia but statistically higher than the national average for 30‐day readmission rates for HF and pneumonia at the time this study was conducted. Advanced practice registered nurses (APRNs) working under the supervision of private or university cardiologists provided care for cardiology service patients. Housestaff under the supervision of university or hospitalist attending physicians, or physician assistants or APRNs under the supervision of hospitalist attending physicians provided care for patients on medical services. Discharge summaries were typically dictated by APRNs for cardiology patients, by 2nd‐ or 3rd‐year residents for housestaff patients, and by hospitalists for hospitalist patients. A dictation guideline was provided to housestaff and hospitalists (see Supporting Information, Appendix 1, in the online version of this article); this guideline suggested including basic demographic information, disposition and diagnoses, the admission history and physical, hospital course, discharge medications, and follow‐up appointments. Additionally, housestaff received a lecture about discharge summaries at the start of their 2nd year. Discharge instructions including medications and follow‐up appointment information were automatically appended to the discharge summaries. Summaries were sent by the medical records department only to physicians in the system who were listed by the dictating physician as needing to receive a copy of the summary; no summary was automatically sent (ie, to the primary care physician) if not requested by the dictating physician.
Data Collection
Experienced registered nurses trained in chart abstraction conducted explicit reviews of medical charts using a standardized review tool. The tool included 24 questions about the discharge summary applicable to all 3 conditions, with 7 additional questions for patients with HF and 1 additional question for patients with ACS. These questions included the 6 elements required by The Joint Commission for all discharge summaries (reason for hospitalization, significant findings, procedures and treatment provided, patient's discharge condition, patient and family instructions, and attending physician's signature)[9] as well as the 7 elements (principal diagnosis and problem list, medication list, transferring physician name and contact information, cognitive status of the patient, test results, and pending test results) recommended by the Transitions of Care Consensus Conference (TOCCC), a recent consensus statement produced by 6 major medical societies.[13] Each content element is shown in (see Supporting Information, Appendix 2, in the online version of this article), which also indicates the elements included in the 2 guidelines.
Main Measures
We assessed quality in 3 main domains: timeliness, transmission, and content. We defined timeliness as days between discharge date and dictation date (not final signature date, which may occur later), and measured both median timeliness and proportion of discharge summaries completed on the day of discharge. We defined transmission as successful fax or mail of the discharge summary to an outside physician as reported by the medical records department, and measured the proportion of discharge summaries sent to any outside physician as well as the median number of physicians per discharge summary who were scheduled to follow‐up with the patient postdischarge but who did not receive a copy of the summary. We defined 21 individual content items and assessed the frequency of each individual content item. We also measured compliance with The Joint Commission mandates and TOCCC recommendations, which included several of the individual content items.
To measure compliance with The Joint Commission requirements, we created a composite score in which 1 point was provided for the presence of each of the 6 required elements (maximum score=6). Every discharge summary received 1 point for attending physician signature, because all discharge summaries were electronically signed. Discharge instructions to family/patients were automatically appended to every discharge summary; however, we gave credit for patient and family instructions only to those that included any information about signs and symptoms to monitor for at home. We defined discharge condition as any information about functional status, cognitive status, physical exam, or laboratory findings at discharge.
To measure compliance with specialty society recommendations for discharge summaries, we created a composite score in which 1 point was provided for the presence of each of the 7 recommended elements (maximum score=7). Every discharge summary received 1 point for discharge medications, because these are automatically appended.
We obtained data on age, race, gender, and length of stay from hospital administrative databases. The study was approved by the Yale Human Investigation Committee, and verbal informed consent was obtained from all study participants.
Statistical Analysis
Characteristics of the sample are described with counts and percentages or means and standard deviations. Medians and interquartile ranges (IQRs) or counts and percentages were calculated for summary measures of timeliness, transmission, and content. We assessed differences in quality measures between APRNs, housestaff, and hospitalists using 2 tests. We conducted multivariable logistic regression analyses for timeliness and for transmission to any outside physician. All discharge summaries included at least 4 of The Joint Commission elements; consequently, we coded this content outcome as an ordinal variable with 3 levels indicating inclusion of 4, 5, or 6 of The Joint Commission elements. We coded the TOCCC content outcome as a 3‐level variable indicating <4, 4, or >4 elements satisfied. Accordingly, proportional odds models were used, in which the reported odds ratios (ORs) can be interpreted as the average effect of the explanatory variable on the odds of having more recommendations, for any dichotomization of the outcome. Residual analysis and goodness‐of‐fit statistics were used to assess model fit; the proportional odds assumption was tested. Statistical analyses were conducted with SAS 9.2 (SAS Institute, Cary, NC). P values <0.05 were interpreted as statistically significant for 2‐sided tests.
RESULTS
Enrollment and Study Sample
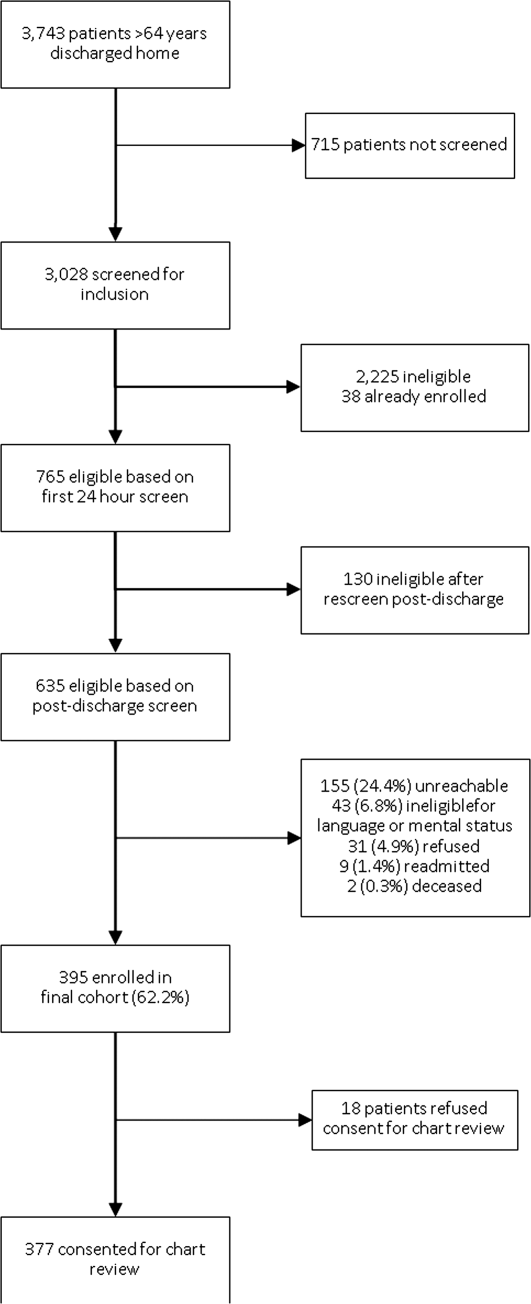
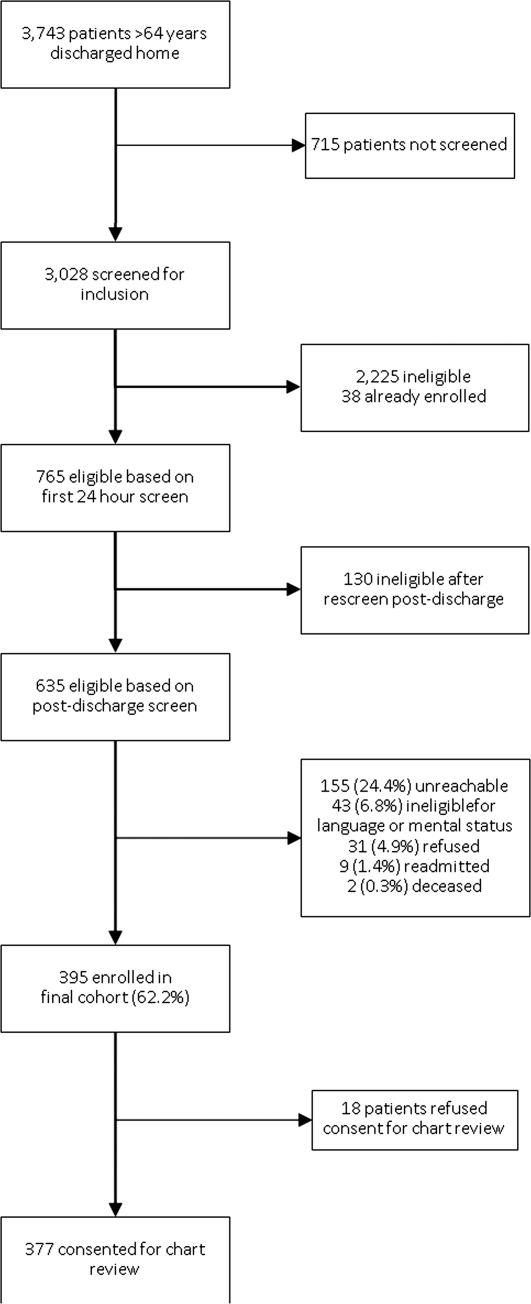
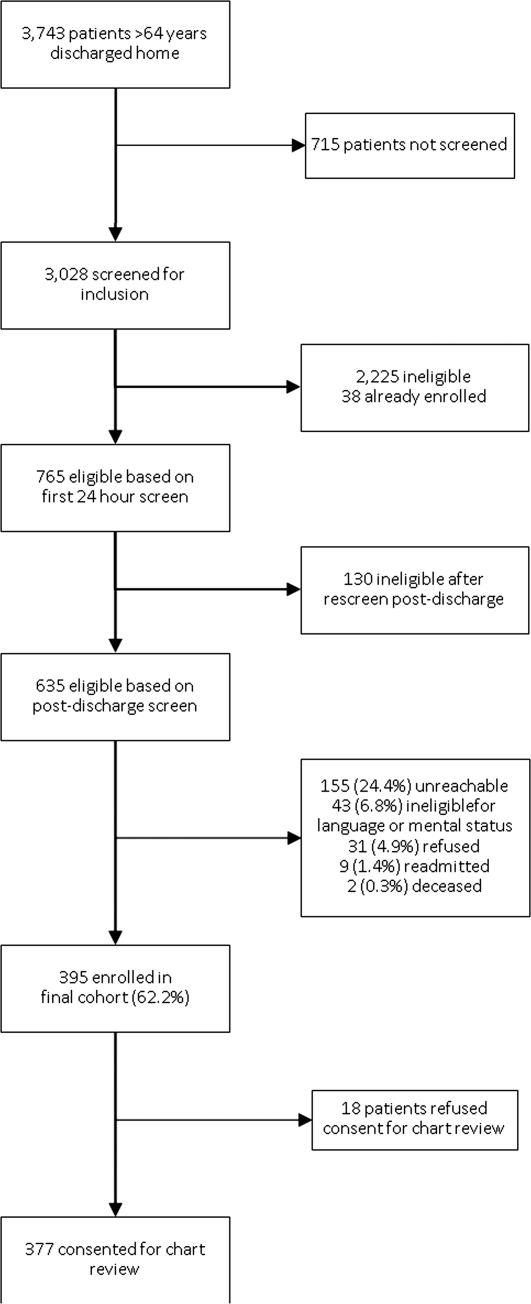
A total of 3743 patients over 64 years old were discharged home from the medical service at YNHH during the study period; 3028 patients were screened for eligibility within 24 hours of admission. We identified 635 eligible admissions and enrolled 395 patients (62.2%) in the study. Of these, 377 granted permission for chart review and were included in this analysis (Figure 1).
The study sample had a mean age of 77.1 years (standard deviation: 7.8); 205 (54.4%) were male and 310 (82.5%) were non‐Hispanic white. A total of 195 (51.7%) had ACS, 91 (24.1%) had pneumonia, and 146 (38.7%) had HF; 54 (14.3%) patients had more than 1 qualifying condition. There were similar numbers of patients on the cardiology, medicine housestaff, and medicine hospitalist teams (Table 1).
| Characteristic | N (%) or Mean (SD) |
|---|---|
| |
| Condition | |
| Acute coronary syndrome | 195 (51.7) |
| Community‐acquired pneumonia | 91 (24.1) |
| Heart failure | 146 (38.7) |
| Training level of summary dictator | |
| APRN | 140 (37.1) |
| House staff | 123 (32.6) |
| Hospitalist | 114 (30.2) |
| Length of stay, mean, d | 3.5 (2.5) |
| Total number of medications | 8.9 (3.3) |
| Identify a usual source of care | 360 (96.0) |
| Age, mean, y | 77.1 (7.8) |
| Male | 205 (54.4) |
| English‐speaking | 366 (98.1) |
| Race/ethnicity | |
| Non‐Hispanic white | 310 (82.5) |
| Non‐Hispanic black | 44 (11.7) |
| Hispanic | 15 (4.0) |
| Other | 7 (1.9) |
| High school graduate or GED Admission source | 268 (73.4) |
| Emergency department | 248 (66.0) |
| Direct transfer from hospital or nursing facility | 94 (25.0) |
| Direct admission from office | 34 (9.0) |
Timeliness
Discharge summaries were completed for 376/377 patients, of which 174 (46.3%) were dictated on the day of discharge. However, 122 (32.4%) summaries were dictated more than 48 hours after discharge, including 93 (24.7%) that were dictated more than 1 week after discharge (see Supporting Information, Appendix 3, in the online version of this article).
Summaries dictated by hospitalists were most likely to be done on the day of discharge (35.3% APRNs, 38.2% housestaff, 68.4% hospitalists, P<0.001). After adjustment for diagnosis and length of stay, hospitalists were still significantly more likely to produce a timely discharge summary than APRNs (OR: 2.82; 95% confidence interval [CI]: 1.56‐5.09), whereas housestaff were no different than APRNs (OR: 0.84; 95% CI: 0.48‐1.46).
Transmission
A total of 144 (38.3%) discharge summaries were not sent to any physician besides the inpatient attending, and 209/374 (55.9%) were not sent to at least 1 physician listed as having a follow‐up appointment planned with the patient. Each discharge summary was sent to a median of 1 physician besides the dictating physician (IQR: 01). However, for each summary, a median of 1 physician (IQR: 01) who had a scheduled follow‐up with the patient did not receive the summary. Summaries dictated by hospitalists were most likely to be sent to at least 1 outside physician (54.7% APRNs, 58.5% housestaff, 73.7% hospitalists, P=0.006). Summaries dictated on the day of discharge were more likely than delayed summaries to be sent to at least 1 outside physician (75.9% vs 49.5%, P<0.001). After adjustment for diagnosis and length of stay, there was no longer a difference in likelihood of transmitting a discharge summary to any outpatient physician according to training level; however, dictations completed on the day of discharge remained significantly more likely to be transmitted to an outside physician (OR: 3.05; 95% CI: 1.88‐4.93) (Table 2).
| Explanatory Variable | Proportion Transmitted to at Least 1 Outside Physician | OR for Transmission to Any Outside Physician (95% CI) | Adjusted P Value |
|---|---|---|---|
| |||
| Training level | 0.52 | ||
| APRN | 54.7% | REF | |
| Housestaff | 58.5% | 1.17 (0.66‐2.06) | |
| Hospitalist | 73.7% | 1.46 (0.76‐2.79) | |
| Timeliness | |||
| Dictated after discharge | 49.5% | REF | <0.001 |
| Dictated day of discharge | 75.9% | 3.05 (1.88‐4.93) | |
| Acute coronary syndrome vs nota | 52.1 % | 1.05 (0.49‐2.26) | 0.89 |
| Pneumonia vs nota | 69.2 % | 1.59 (0.66‐3.79) | 0.30 |
| Heart failure vs nota | 74.7 % | 3.32 (1.61‐6.84) | 0.001 |
| Length of stay, d | 0.91 (0.83‐1.00) | 0.06 | |
Content
Rate of inclusion of each content element is shown in Table 3, overall and by training level. Nearly every discharge summary included information about admitting diagnosis, hospital course, and procedures or tests performed during the hospitalization. However, few summaries included information about the patient's condition at discharge. Less than half included discharge laboratory results; less than one‐third included functional capacity, cognitive capacity, or discharge physical exam. Only 4.1% overall of discharge summaries for patients with HF included the patient's weight at discharge; best were hospitalists who still included this information in only 7.7% of summaries. Information about postdischarge care, including home social support, pending tests, or recommended follow‐up tests/procedures was also rarely specified. Last, only 6.2% of discharge summaries included the name and contact number of the inpatient physician; this information was least likely to be provided by housestaff (1.6%) and most likely to be provided by hospitalists (15.2%) (P<0.001).
| Discharge Summary Component | Overall, n=377, n (%) | APRN, n=140, n (%) | Housestaff, n=123, n (%) | Hospitalist, n=114, n (%) | P Value |
|---|---|---|---|---|---|
| |||||
| Diagnosisab | 368 (97.9) | 136 (97.8) | 120 (97.6) | 112 (98.3) | 1.00 |
| Discharge second diagnosisb | 289 (76.9) | 100 (71.9) | 89 (72.4) | 100 (87.7) | <0.001 |
| Hospital coursea | 375 (100.0) | 138 (100) | 123 (100) | 114 (100) | N/A |
| Procedures/tests performed during admissionab | 374 (99.7) | 138 (99.3) | 123 (100) | 113 (100) | N/A |
| Patient and family instructionsa | 371 (98.4) | 136 (97.1) | 122 (99.2) | 113 (99.1) | .43 |
| Social support or living situation of patient | 148 (39.5) | 18 (12.9) | 62 (50.4) | 68 (60.2) | <0.001 |
| Functional capacity at dischargea | 99 (26.4) | 37 (26.6) | 32 (26.0) | 30 (26.6) | 0.99 |
| Cognitive capacity at dischargeab | 30 (8.0) | 6 (4.4) | 11 (8.9) | 13 (11.5) | 0.10 |
| Physical exam at dischargea | 62 (16.7) | 19 (13.8) | 16 (13.1) | 27 (24.1) | 0.04 |
| Laboratory results at time of dischargea | 164 (43.9) | 63 (45.3) | 50 (40.7) | 51 (45.5) | 0.68 |
| Back to baseline or other nonspecific remark about discharge statusa | 71 (19.0) | 30 (21.6) | 18 (14.8) | 23 (20.4) | 0.34 |
| Any test or result still pending or specific comment that nothing is pendingb | 46 (12.2) | 9 (6.4) | 20 (16.3) | 17 (14.9) | 0.03 |
| Recommendation for follow‐up tests/procedures | 157 (41.9) | 43 (30.9) | 54 (43.9) | 60 (53.1) | 0.002 |
| Call‐back number of responsible in‐house physicianb | 23 (6.2) | 4 (2.9) | 2 (1.6) | 17 (15.2) | <0.001 |
| Resuscitation status | 27 (7.7) | 2 (1.5) | 18 (15.4) | 7 (6.7) | <0.001 |
| Etiology of heart failurec | 120 (82.8) | 44 (81.5) | 34 (87.2) | 42 (80.8) | 0.69 |
| Reason/trigger for exacerbationc | 86 (58.9) | 30 (55.6) | 27 (67.5) | 29 (55.8) | 0.43 |
| Ejection fractionc | 107 (73.3) | 40 (74.1) | 32 (80.0) | 35 (67.3) | 0.39 |
| Discharge weightc | 6 (4.1) | 1 (1.9) | 1 (2.5) | 4 (7.7) | 0.33 |
| Target weight rangec | 5 (3.4) | 0 (0) | 2 (5.0) | 3 (5.8) | 0.22 |
| Discharge creatinine or GFRc | 34 (23.3) | 14 (25.9) | 10 (25.0) | 10 (19.2) | 0.69 |
| If stent placed, whether drug‐eluting or notd | 89 (81.7) | 58 (87.9) | 27 (81.8) | 4 (40.0) | 0.001 |
On average, summaries included 5.6 of the 6 Joint Commission elements and 4.0 of the 7 TOCCC elements. A total of 63.0% of discharge summaries included all 6 elements required by The Joint Commission, whereas no discharge summary included all 7 TOCCC elements.
APRNs, housestaff and hospitalists included the same average number of The Joint Commission elements (5.6 each), but hospitalists on average included slightly more TOCCC elements (4.3) than did housestaff (4.0) or APRNs (3.8) (P<0.001). Summaries dictated on the day of discharge included an average of 4.2 TOCCC elements, compared to 3.9 TOCCC elements in delayed discharge. In multivariable analyses adjusted for diagnosis and length of stay, there was still no difference by training level in presence of The Joint Commission elements, but hospitalists were significantly more likely to include more TOCCC elements than APRNs (OR: 2.70; 95% CI: 1.49‐4.90) (Table 4). Summaries dictated on the day of discharge were significantly more likely to include more TOCCC elements (OR: 1.92; 95% CI: 1.23‐2.99).
| Explanatory Variable | Average Number of TOCCC Elements Included | OR (95% CI) | Adjusted P Value |
|---|---|---|---|
| |||
| Training level | 0.004 | ||
| APRN | 3.8 | REF | |
| Housestaff | 4.0 | 1.54 (0.90‐2.62) | |
| Hospitalist | 4.3 | 2.70 (1.49‐4.90) | |
| Timeliness | |||
| Dictated after discharge | 3.9 | REF | |
| Dictated day of discharge | 4.2 | 1.92 (1.23‐2.99) | 0.004 |
| Acute coronary syndrome vs nota | 3.9 | 0.72 (0.37‐1.39) | 0.33 |
| Pneumonia vs nota | 4.2 | 1.02 (0.49‐2.14) | 0.95 |
| Heart failure vs nota | 4.1 | 1.49 (0.80‐2.78) | 0.21 |
| Length of stay, d | 0.99 (0.90‐1.07) | 0.73 | |
No discharge summary included all 7 TOCCC‐endorsed content elements, was dictated on the day of discharge, and was sent to an outside physician.
DISCUSSION
In this prospective single‐site study of medical patients with 3 common conditions, we found that discharge summaries were completed relatively promptly, but were often not sent to the appropriate outpatient physicians. We also found that summaries were uniformly excellent at providing details of the hospitalization, but less reliable at providing details relevant to transitional care such as the patient's condition on discharge or existence of pending tests. On average, summaries included 57% of the elements included in consensus guidelines by 6 major medical societies. The content of discharge summaries dictated by hospitalists was slightly more comprehensive than that of APRNs and trainees, but no group exhibited high performance. In fact, not one discharge summary fully met all 3 quality criteria of timeliness, transmission, and content.
Our study, unlike most in the field, focused on multiple dimensions of discharge summary quality simultaneously. For instance, previous studies have found that timely receipt of a discharge summary does not reduce readmission rates.[11, 14, 15] Yet, if the content of the discharge summary is inadequate for postdischarge care, the summary may not be useful even if it is received by the follow‐up visit. Conversely, high‐quality content is ineffective if the summary is not sent to the outpatient physician.
This study suggests several avenues for improving summary quality. Timely discharge summaries in this study were more likely to include key content and to be transmitted to the appropriate physician. Strategies to improve discharge summary quality should therefore prioritize timely summaries, which can be expected to have downstream benefits for other aspects of quality. Some studies have found that templates improve discharge summary content.[22] In our institution, a template exists, but it favors a hospitalization‐focused rather than transition‐focused approach to the discharge summary. For instance, it includes instructions to dictate the admission exam, but not the discharge exam. Thus, designing templates specifically for transitional care is key. Maximizing capabilities of electronic records may help; many content elements that were commonly missing (e.g., pending results, discharge vitals, discharge weight) could be automatically inserted from electronic records. Likewise, automatic transmission of the summary to care providers listed in the electronic record might ameliorate many transmission failures. Some efforts have been made to convert existing electronic data into discharge summaries.[23, 24, 25] However, these activities are very preliminary, and some studies have found the quality of electronic summaries to be lower than dictated or handwritten summaries.[26] As with all automated or electronic applications, it will be essential to consider workflow, readability, and ability to synthesize information prior to adoption.
Hospitalists consistently produced highest‐quality summaries, even though they did not receive explicit training, suggesting experience may be beneficial,[27, 28, 29] or that the hospitalist community focus on transitional care has been effective. In addition, hospitalists at our institution explicitly prioritize timely and comprehensive discharge dictations, because their business relies on maintaining good relationships with outpatient physicians who contract for their services. Housestaff and APRNs have no such incentives or policies; rather, they typically consider discharge summaries to be a useful source of patient history at the time of an admission or readmission. Other academic centers have found similar results.[6, 16] Nonetheless, even though hospitalists had slightly better performance in our study, large gaps in the quality of summaries remained for all groups including hospitalists.
This study has several limitations. First, as a single‐site study at an academic hospital, it may not be generalizable to other hospitals or other settings. It is noteworthy, however, that the average time to dictation in this study was much lower than that of other studies,[4, 14, 30, 31, 32] suggesting that practices at this institution are at least no worse and possibly better than elsewhere. Second, although there are some mandates and expert opinion‐based guidelines for discharge summary content, there is no validated evidence base to confirm what content ought to be present in discharge summaries to improve patient outcomes. Third, we had too few readmissions in the dataset to have enough power to determine whether discharge summary content, timeliness, or transmission predicts readmission. Fourth, we did not determine whether the information in discharge summaries was accurate or complete; we merely assessed whether it was present. For example, we gave every discharge summary full credit for including discharge medications because they are automatically appended. Yet medication reconciliation errors at discharge are common.[33, 34] In fact, in the DISCHARGE study cohort, more than a quarter of discharge medication lists contained a suspected error.[35]
In summary, this study demonstrated the inadequacy of the contemporary discharge summary for conveying information that is critical to the transition from hospital to home. It may be that hospital culture treats hospitalizations as discrete and self‐contained events rather than as components of a larger episode of care. As interest in reducing readmissions rises, reframing the discharge summary to serve as a transitional tool and targeting it for quality assessment will likely be necessary.
Acknowledgments
The authors would like to acknowledge Amy Browning and the staff of the Center for Outcomes Research and Evaluation Follow‐Up Center for conducting patient interviews, Mark Abroms and Katherine Herman for patient recruitment and screening, and Peter Charpentier for Web site development.
Disclosures
At the time this study was conducted, Dr. Horwitz was supported by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research, and was a Centers of Excellence Scholar in Geriatric Medicine by the John A. Hartford Foundation and the American Federation for Aging Research. Dr. Horwitz is now supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. This work was also supported by a grant from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (P30AG021342 NIH/NIA). Dr. Krumholz is supported by grant U01 HL105270‐01 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. No funding source had any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging, the National Center for Advancing Translational Sciences, the National Institutes of Health, The John A. Hartford Foundation, the National Heart, Lung, and Blood Institute, or the American Federation for Aging Research. Dr. Horwitz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. An earlier version of this work was presented as an oral presentation at the Society of General Internal Medicine Annual Meeting in Orlando, Florida on May 12, 2012. Dr. Krumholz chairs a cardiac scientific advisory board for UnitedHealth. Dr. Krumholz receives support from the Centers of Medicare and Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting, including readmission measures.
APPENDIX
A
Dictation guidelines provided to house staff and hospitalists
DICTATION GUIDELINES
FORMAT OF DISCHARGE SUMMARY
- Your name(spell it out), andPatient name(spell it out as well)
- Medical record number, date of admission, date of discharge
- Attending physician
- Disposition
- Principal and other diagnoses, Principal and other operations/procedures
- Copies to be sent to other physicians
- Begin narrative: CC, HPI, PMHx, Medications on admit, Social, Family Hx, Physical exam on admission, Data (labs on admission, plus labs relevant to workup, significant changes at discharge, admission EKG, radiologic and other data),Hospital course by problem, discharge meds, follow‐up appointments
APPENDIX
B
| Diagnosis |
| Discharge Second Diagnosis |
| Hospital course |
| Procedures/tests performed during admission |
| Patient and Family Instructions |
| Social support or living situation of patient |
| Functional capacity at discharge |
| Cognitive capacity at discharge |
| Physical exam at discharge |
| Laboratory results at time of discharge |
| Back to baseline or other nonspecific remark about discharge status |
| Any test or result still pending |
| Specific comment that nothing is pending |
| Recommendation for follow up tests/procedures |
| Call back number of responsible in‐house physician |
| Resuscitation status |
| Etiology of heart failure |
| Reason/trigger for exacerbation |
| Ejection fraction |
| Discharge weight |
| Target weight range |
| Discharge creatinine or GFR |
| If stent placed, whether drug‐eluting or not |
| Composite element | Data elements abstracted that qualify as meeting measure |
|---|---|
| Reason for hospitalization | Diagnosis |
| Significant findings | Hospital course |
| Procedures and treatment provided | Procedures/tests performed during admission |
| Patient's discharge condition | Functional capacity at discharge, Cognitive capacity at discharge, Physical exam at discharge, Laboratory results at time of discharge, Back to baseline or other nonspecific remark about discharge status |
| Patient and family instructions | Signs and symptoms to monitor at home |
| Attending physician's signature | Attending signature |
| Composite element | Data elements abstracted that qualify as meeting measure |
|---|---|
| Principal diagnosis | Diagnosis |
| Problem list | Discharge second diagnosis |
| Medication list | [Automatically appended; full credit to every summary] |
| Transferring physician name and contact information | Call back number of responsible in‐house physician |
| Cognitive status of the patient | Cognitive capacity at discharge |
| Test results | Procedures/tests performed during admission |
| Pending test results | Any test or result still pending or specific comment that nothing is pending |
APPENDIX
C
Histogram of days between discharge and dictation
- , , . Value of the specialist's report. Br Med J. 1960;2(5213):1663–1664.
- , . Communications between general practitioners and consultants. Br Med J. 1974;4(5942):456–459.
- , , . A functional hospital discharge summary. J Pediatr. 1975;86(1):97–98.
- , , , , , . Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128.
- , , , et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow‐up providers. J Gen Intern Med. 2009;24(9):1002–1006.
- , , . Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305–1311.
- Centers for Medicare and Medicaid Services. Condition of participation: medical record services. 42. Vol 482.C.F.R. § 482.24 (2012).
- Joint Commission on Accreditation of Healthcare Organizations. Hospital Accreditation Standards. Standard IM 6.10 EP 7–9. Oakbrook Terrace, IL: The Joint Commission; 2008.
- , . Documentation of mandated discharge summary components in transitions from acute to subacute care. In: Agency for Healthcare Research and Quality, ed. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 2: Culture and Redesign. AHRQ Publication No. 08-0034‐2. Rockville, MD: Agency for Healthcare Research and Quality; 2008:179–188.
- , , , et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20(9):773–778.
- , , , et al. Transition of care for hospitalized elderly patients‐development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354–360.
- , , , et al. Transitions of Care Consensus Policy Statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971–976.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , . Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , . Provider characteristics, clinical‐work processes and their relationship to discharge summary quality for sub‐acute care patients. J Gen Intern Med. 2012;27(1):78–84.
- , , , et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50(7):e1–e157.
- , , . Universal definition of myocardial infarction. Eur Heart J. 2007;28(20):2525–2538.
- , , , et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–989.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- , , , et al. Clock drawing in Alzheimer's disease. A novel measure of dementia severity. J Am Geriatr Soc. 1989;37(8):725–729.
- , , , , . Assessing quality and efficiency of discharge summaries. Am J Med Qual. 2005;20(6):337–343.
- , , , et al. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Intern Med. 2009;24(9):995–1001.
- , , , . Dictated versus database‐generated discharge summaries: a randomized clinical trial. CMAJ. 1999;160(3):319–326.
- , , , , . Computerised updating of clinical summaries: new opportunities for clinical practice and research? BMJ. 1988;297(6662):1504–1506.
- , , . Evaluation of electronic discharge summaries: a comparison of documentation in electronic and handwritten discharge summaries. Int J Med Inform. 2008;77(9):613–620.
- , , , , . Did I do as best as the system would let me? Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , , . Learning by doing—resident perspectives on developing competency in high‐quality discharge care. J Gen Intern Med. 2012;27(9):1188–1194.
- , , , , . Out of sight, out of mind: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381.
- , , . Dissemination of discharge summaries. Not reaching follow‐up physicians. Can Fam Physician. 2002;48:737–742.
- , , , . Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , . General practitioner‐hospital communications: a review of discharge summaries. J Qual Clin Pract. 2001;21(4):104–108.
- , , . Accuracy of information on medicines in hospital discharge summaries. Intern Med J. 2006;36(4):221–225.
- , , . Accuracy of medication documentation in hospital discharge summaries: A retrospective analysis of medication transcription errors in manual and electronic discharge summaries. Int J Med Inform. 2010;79(1):58–64.
- , , , . Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012;27(11):1513–1520.
Hospitalized patients are often cared for by physicians who do not follow them in the community, creating a discontinuity of care that must be bridged through communication. This communication between inpatient and outpatient physicians occurs, in part via a discharge summary, which is intended to summarize events during hospitalization and prepare the outpatient physician to resume care of the patient. Yet, this form of communication has long been problematic.[1, 2, 3] In a 1960 study, only 30% of discharge letters were received by the primary care physician within 48 hours of discharge.[1]
More recent studies have shown little improvement. Direct communication between hospital and outpatient physicians is rare, and discharge summaries are still largely unavailable at the time of follow‐up.[4] In 1 study, primary care physicians were unaware of 62% of laboratory tests or study results that were pending on discharge,[5] in part because this information is missing from most discharge summaries.[6] Deficits such as these persist despite the fact that the rate of postdischarge completion of recommended tests, referrals, or procedures is significantly increased when the recommendation is included in the discharge summary.[7]
Regulatory mandates for discharge summaries from the Centers for Medicare and Medicaid Services[8] and from The Joint Commission[9] appear to be generally met[10, 11]; however, these mandates have no requirements for timeliness stricter than 30 days, do not require that summaries be transmitted to outpatient physicians, and do not require several content elements that might be useful to outside physicians such as condition of the patient at discharge, cognitive and functional status, goals of care, or pending studies. Expert opinion guidelines have more comprehensive recommendations,[12, 13] but it is uncertain how widely they are followed.
The existence of a discharge summary does not necessarily mean it serves a patient well in the transitional period.[11, 14, 15] Discharge summaries are a complex intervention, and we do not yet understand the best ways discharge summaries may fulfill needs specific to transitional care. Furthermore, it is uncertain what factors improve aspects of discharge summary quality as defined by timeliness, transmission, and content.[6, 16]
The goal of the DIagnosing Systemic failures, Complexities and HARm in GEriatric discharges study (DISCHARGE) was to comprehensively assess the discharge process for older patients discharged to the community. In this article we examine discharge summaries of patients enrolled in the study to determine the timeliness, transmission to outside physicians, and content of the summaries. We further examine the effect of provider training level and timeliness of dictation on discharge summary quality.
METHODS
Study Cohort
The DISCHARGE study was a prospective, observational cohort study of patients 65 years or older discharged to home from YaleNew Haven Hospital (YNHH) who were admitted with acute coronary syndrome (ACS), community‐acquired pneumonia, or heart failure (HF). Patients were screened by physicians for eligibility within 24 hours of admission using specialty society guidelines[17, 18, 19, 20] and were enrolled by telephone within 1 week of discharge. Additional inclusion criteria included speaking English or Spanish, and ability of the patient or caregiver to participate in a telephone interview. Patients enrolled in hospice were excluded, as were patients who failed the Mini‐Cog mental status screen (3‐item recall and a clock draw)[21] while in the hospital or appeared confused or delirious during the telephone interview. Caregivers of cognitively impaired patients were eligible for enrollment instead if the patient provided permission.
Study Setting
YNHH is a 966‐bed urban tertiary care hospital with statistically lower than the national average mortality for acute myocardial infarction, HF, and pneumonia but statistically higher than the national average for 30‐day readmission rates for HF and pneumonia at the time this study was conducted. Advanced practice registered nurses (APRNs) working under the supervision of private or university cardiologists provided care for cardiology service patients. Housestaff under the supervision of university or hospitalist attending physicians, or physician assistants or APRNs under the supervision of hospitalist attending physicians provided care for patients on medical services. Discharge summaries were typically dictated by APRNs for cardiology patients, by 2nd‐ or 3rd‐year residents for housestaff patients, and by hospitalists for hospitalist patients. A dictation guideline was provided to housestaff and hospitalists (see Supporting Information, Appendix 1, in the online version of this article); this guideline suggested including basic demographic information, disposition and diagnoses, the admission history and physical, hospital course, discharge medications, and follow‐up appointments. Additionally, housestaff received a lecture about discharge summaries at the start of their 2nd year. Discharge instructions including medications and follow‐up appointment information were automatically appended to the discharge summaries. Summaries were sent by the medical records department only to physicians in the system who were listed by the dictating physician as needing to receive a copy of the summary; no summary was automatically sent (ie, to the primary care physician) if not requested by the dictating physician.
Data Collection
Experienced registered nurses trained in chart abstraction conducted explicit reviews of medical charts using a standardized review tool. The tool included 24 questions about the discharge summary applicable to all 3 conditions, with 7 additional questions for patients with HF and 1 additional question for patients with ACS. These questions included the 6 elements required by The Joint Commission for all discharge summaries (reason for hospitalization, significant findings, procedures and treatment provided, patient's discharge condition, patient and family instructions, and attending physician's signature)[9] as well as the 7 elements (principal diagnosis and problem list, medication list, transferring physician name and contact information, cognitive status of the patient, test results, and pending test results) recommended by the Transitions of Care Consensus Conference (TOCCC), a recent consensus statement produced by 6 major medical societies.[13] Each content element is shown in (see Supporting Information, Appendix 2, in the online version of this article), which also indicates the elements included in the 2 guidelines.
Main Measures
We assessed quality in 3 main domains: timeliness, transmission, and content. We defined timeliness as days between discharge date and dictation date (not final signature date, which may occur later), and measured both median timeliness and proportion of discharge summaries completed on the day of discharge. We defined transmission as successful fax or mail of the discharge summary to an outside physician as reported by the medical records department, and measured the proportion of discharge summaries sent to any outside physician as well as the median number of physicians per discharge summary who were scheduled to follow‐up with the patient postdischarge but who did not receive a copy of the summary. We defined 21 individual content items and assessed the frequency of each individual content item. We also measured compliance with The Joint Commission mandates and TOCCC recommendations, which included several of the individual content items.
To measure compliance with The Joint Commission requirements, we created a composite score in which 1 point was provided for the presence of each of the 6 required elements (maximum score=6). Every discharge summary received 1 point for attending physician signature, because all discharge summaries were electronically signed. Discharge instructions to family/patients were automatically appended to every discharge summary; however, we gave credit for patient and family instructions only to those that included any information about signs and symptoms to monitor for at home. We defined discharge condition as any information about functional status, cognitive status, physical exam, or laboratory findings at discharge.
To measure compliance with specialty society recommendations for discharge summaries, we created a composite score in which 1 point was provided for the presence of each of the 7 recommended elements (maximum score=7). Every discharge summary received 1 point for discharge medications, because these are automatically appended.
We obtained data on age, race, gender, and length of stay from hospital administrative databases. The study was approved by the Yale Human Investigation Committee, and verbal informed consent was obtained from all study participants.
Statistical Analysis
Characteristics of the sample are described with counts and percentages or means and standard deviations. Medians and interquartile ranges (IQRs) or counts and percentages were calculated for summary measures of timeliness, transmission, and content. We assessed differences in quality measures between APRNs, housestaff, and hospitalists using 2 tests. We conducted multivariable logistic regression analyses for timeliness and for transmission to any outside physician. All discharge summaries included at least 4 of The Joint Commission elements; consequently, we coded this content outcome as an ordinal variable with 3 levels indicating inclusion of 4, 5, or 6 of The Joint Commission elements. We coded the TOCCC content outcome as a 3‐level variable indicating <4, 4, or >4 elements satisfied. Accordingly, proportional odds models were used, in which the reported odds ratios (ORs) can be interpreted as the average effect of the explanatory variable on the odds of having more recommendations, for any dichotomization of the outcome. Residual analysis and goodness‐of‐fit statistics were used to assess model fit; the proportional odds assumption was tested. Statistical analyses were conducted with SAS 9.2 (SAS Institute, Cary, NC). P values <0.05 were interpreted as statistically significant for 2‐sided tests.
RESULTS
Enrollment and Study Sample
A total of 3743 patients over 64 years old were discharged home from the medical service at YNHH during the study period; 3028 patients were screened for eligibility within 24 hours of admission. We identified 635 eligible admissions and enrolled 395 patients (62.2%) in the study. Of these, 377 granted permission for chart review and were included in this analysis (Figure 1).
The study sample had a mean age of 77.1 years (standard deviation: 7.8); 205 (54.4%) were male and 310 (82.5%) were non‐Hispanic white. A total of 195 (51.7%) had ACS, 91 (24.1%) had pneumonia, and 146 (38.7%) had HF; 54 (14.3%) patients had more than 1 qualifying condition. There were similar numbers of patients on the cardiology, medicine housestaff, and medicine hospitalist teams (Table 1).
| Characteristic | N (%) or Mean (SD) |
|---|---|
| |
| Condition | |
| Acute coronary syndrome | 195 (51.7) |
| Community‐acquired pneumonia | 91 (24.1) |
| Heart failure | 146 (38.7) |
| Training level of summary dictator | |
| APRN | 140 (37.1) |
| House staff | 123 (32.6) |
| Hospitalist | 114 (30.2) |
| Length of stay, mean, d | 3.5 (2.5) |
| Total number of medications | 8.9 (3.3) |
| Identify a usual source of care | 360 (96.0) |
| Age, mean, y | 77.1 (7.8) |
| Male | 205 (54.4) |
| English‐speaking | 366 (98.1) |
| Race/ethnicity | |
| Non‐Hispanic white | 310 (82.5) |
| Non‐Hispanic black | 44 (11.7) |
| Hispanic | 15 (4.0) |
| Other | 7 (1.9) |
| High school graduate or GED Admission source | 268 (73.4) |
| Emergency department | 248 (66.0) |
| Direct transfer from hospital or nursing facility | 94 (25.0) |
| Direct admission from office | 34 (9.0) |
Timeliness
Discharge summaries were completed for 376/377 patients, of which 174 (46.3%) were dictated on the day of discharge. However, 122 (32.4%) summaries were dictated more than 48 hours after discharge, including 93 (24.7%) that were dictated more than 1 week after discharge (see Supporting Information, Appendix 3, in the online version of this article).
Summaries dictated by hospitalists were most likely to be done on the day of discharge (35.3% APRNs, 38.2% housestaff, 68.4% hospitalists, P<0.001). After adjustment for diagnosis and length of stay, hospitalists were still significantly more likely to produce a timely discharge summary than APRNs (OR: 2.82; 95% confidence interval [CI]: 1.56‐5.09), whereas housestaff were no different than APRNs (OR: 0.84; 95% CI: 0.48‐1.46).
Transmission
A total of 144 (38.3%) discharge summaries were not sent to any physician besides the inpatient attending, and 209/374 (55.9%) were not sent to at least 1 physician listed as having a follow‐up appointment planned with the patient. Each discharge summary was sent to a median of 1 physician besides the dictating physician (IQR: 01). However, for each summary, a median of 1 physician (IQR: 01) who had a scheduled follow‐up with the patient did not receive the summary. Summaries dictated by hospitalists were most likely to be sent to at least 1 outside physician (54.7% APRNs, 58.5% housestaff, 73.7% hospitalists, P=0.006). Summaries dictated on the day of discharge were more likely than delayed summaries to be sent to at least 1 outside physician (75.9% vs 49.5%, P<0.001). After adjustment for diagnosis and length of stay, there was no longer a difference in likelihood of transmitting a discharge summary to any outpatient physician according to training level; however, dictations completed on the day of discharge remained significantly more likely to be transmitted to an outside physician (OR: 3.05; 95% CI: 1.88‐4.93) (Table 2).
| Explanatory Variable | Proportion Transmitted to at Least 1 Outside Physician | OR for Transmission to Any Outside Physician (95% CI) | Adjusted P Value |
|---|---|---|---|
| |||
| Training level | 0.52 | ||
| APRN | 54.7% | REF | |
| Housestaff | 58.5% | 1.17 (0.66‐2.06) | |
| Hospitalist | 73.7% | 1.46 (0.76‐2.79) | |
| Timeliness | |||
| Dictated after discharge | 49.5% | REF | <0.001 |
| Dictated day of discharge | 75.9% | 3.05 (1.88‐4.93) | |
| Acute coronary syndrome vs nota | 52.1 % | 1.05 (0.49‐2.26) | 0.89 |
| Pneumonia vs nota | 69.2 % | 1.59 (0.66‐3.79) | 0.30 |
| Heart failure vs nota | 74.7 % | 3.32 (1.61‐6.84) | 0.001 |
| Length of stay, d | 0.91 (0.83‐1.00) | 0.06 | |
Content
Rate of inclusion of each content element is shown in Table 3, overall and by training level. Nearly every discharge summary included information about admitting diagnosis, hospital course, and procedures or tests performed during the hospitalization. However, few summaries included information about the patient's condition at discharge. Less than half included discharge laboratory results; less than one‐third included functional capacity, cognitive capacity, or discharge physical exam. Only 4.1% overall of discharge summaries for patients with HF included the patient's weight at discharge; best were hospitalists who still included this information in only 7.7% of summaries. Information about postdischarge care, including home social support, pending tests, or recommended follow‐up tests/procedures was also rarely specified. Last, only 6.2% of discharge summaries included the name and contact number of the inpatient physician; this information was least likely to be provided by housestaff (1.6%) and most likely to be provided by hospitalists (15.2%) (P<0.001).
| Discharge Summary Component | Overall, n=377, n (%) | APRN, n=140, n (%) | Housestaff, n=123, n (%) | Hospitalist, n=114, n (%) | P Value |
|---|---|---|---|---|---|
| |||||
| Diagnosisab | 368 (97.9) | 136 (97.8) | 120 (97.6) | 112 (98.3) | 1.00 |
| Discharge second diagnosisb | 289 (76.9) | 100 (71.9) | 89 (72.4) | 100 (87.7) | <0.001 |
| Hospital coursea | 375 (100.0) | 138 (100) | 123 (100) | 114 (100) | N/A |
| Procedures/tests performed during admissionab | 374 (99.7) | 138 (99.3) | 123 (100) | 113 (100) | N/A |
| Patient and family instructionsa | 371 (98.4) | 136 (97.1) | 122 (99.2) | 113 (99.1) | .43 |
| Social support or living situation of patient | 148 (39.5) | 18 (12.9) | 62 (50.4) | 68 (60.2) | <0.001 |
| Functional capacity at dischargea | 99 (26.4) | 37 (26.6) | 32 (26.0) | 30 (26.6) | 0.99 |
| Cognitive capacity at dischargeab | 30 (8.0) | 6 (4.4) | 11 (8.9) | 13 (11.5) | 0.10 |
| Physical exam at dischargea | 62 (16.7) | 19 (13.8) | 16 (13.1) | 27 (24.1) | 0.04 |
| Laboratory results at time of dischargea | 164 (43.9) | 63 (45.3) | 50 (40.7) | 51 (45.5) | 0.68 |
| Back to baseline or other nonspecific remark about discharge statusa | 71 (19.0) | 30 (21.6) | 18 (14.8) | 23 (20.4) | 0.34 |
| Any test or result still pending or specific comment that nothing is pendingb | 46 (12.2) | 9 (6.4) | 20 (16.3) | 17 (14.9) | 0.03 |
| Recommendation for follow‐up tests/procedures | 157 (41.9) | 43 (30.9) | 54 (43.9) | 60 (53.1) | 0.002 |
| Call‐back number of responsible in‐house physicianb | 23 (6.2) | 4 (2.9) | 2 (1.6) | 17 (15.2) | <0.001 |
| Resuscitation status | 27 (7.7) | 2 (1.5) | 18 (15.4) | 7 (6.7) | <0.001 |
| Etiology of heart failurec | 120 (82.8) | 44 (81.5) | 34 (87.2) | 42 (80.8) | 0.69 |
| Reason/trigger for exacerbationc | 86 (58.9) | 30 (55.6) | 27 (67.5) | 29 (55.8) | 0.43 |
| Ejection fractionc | 107 (73.3) | 40 (74.1) | 32 (80.0) | 35 (67.3) | 0.39 |
| Discharge weightc | 6 (4.1) | 1 (1.9) | 1 (2.5) | 4 (7.7) | 0.33 |
| Target weight rangec | 5 (3.4) | 0 (0) | 2 (5.0) | 3 (5.8) | 0.22 |
| Discharge creatinine or GFRc | 34 (23.3) | 14 (25.9) | 10 (25.0) | 10 (19.2) | 0.69 |
| If stent placed, whether drug‐eluting or notd | 89 (81.7) | 58 (87.9) | 27 (81.8) | 4 (40.0) | 0.001 |
On average, summaries included 5.6 of the 6 Joint Commission elements and 4.0 of the 7 TOCCC elements. A total of 63.0% of discharge summaries included all 6 elements required by The Joint Commission, whereas no discharge summary included all 7 TOCCC elements.
APRNs, housestaff and hospitalists included the same average number of The Joint Commission elements (5.6 each), but hospitalists on average included slightly more TOCCC elements (4.3) than did housestaff (4.0) or APRNs (3.8) (P<0.001). Summaries dictated on the day of discharge included an average of 4.2 TOCCC elements, compared to 3.9 TOCCC elements in delayed discharge. In multivariable analyses adjusted for diagnosis and length of stay, there was still no difference by training level in presence of The Joint Commission elements, but hospitalists were significantly more likely to include more TOCCC elements than APRNs (OR: 2.70; 95% CI: 1.49‐4.90) (Table 4). Summaries dictated on the day of discharge were significantly more likely to include more TOCCC elements (OR: 1.92; 95% CI: 1.23‐2.99).
| Explanatory Variable | Average Number of TOCCC Elements Included | OR (95% CI) | Adjusted P Value |
|---|---|---|---|
| |||
| Training level | 0.004 | ||
| APRN | 3.8 | REF | |
| Housestaff | 4.0 | 1.54 (0.90‐2.62) | |
| Hospitalist | 4.3 | 2.70 (1.49‐4.90) | |
| Timeliness | |||
| Dictated after discharge | 3.9 | REF | |
| Dictated day of discharge | 4.2 | 1.92 (1.23‐2.99) | 0.004 |
| Acute coronary syndrome vs nota | 3.9 | 0.72 (0.37‐1.39) | 0.33 |
| Pneumonia vs nota | 4.2 | 1.02 (0.49‐2.14) | 0.95 |
| Heart failure vs nota | 4.1 | 1.49 (0.80‐2.78) | 0.21 |
| Length of stay, d | 0.99 (0.90‐1.07) | 0.73 | |
No discharge summary included all 7 TOCCC‐endorsed content elements, was dictated on the day of discharge, and was sent to an outside physician.
DISCUSSION
In this prospective single‐site study of medical patients with 3 common conditions, we found that discharge summaries were completed relatively promptly, but were often not sent to the appropriate outpatient physicians. We also found that summaries were uniformly excellent at providing details of the hospitalization, but less reliable at providing details relevant to transitional care such as the patient's condition on discharge or existence of pending tests. On average, summaries included 57% of the elements included in consensus guidelines by 6 major medical societies. The content of discharge summaries dictated by hospitalists was slightly more comprehensive than that of APRNs and trainees, but no group exhibited high performance. In fact, not one discharge summary fully met all 3 quality criteria of timeliness, transmission, and content.
Our study, unlike most in the field, focused on multiple dimensions of discharge summary quality simultaneously. For instance, previous studies have found that timely receipt of a discharge summary does not reduce readmission rates.[11, 14, 15] Yet, if the content of the discharge summary is inadequate for postdischarge care, the summary may not be useful even if it is received by the follow‐up visit. Conversely, high‐quality content is ineffective if the summary is not sent to the outpatient physician.
This study suggests several avenues for improving summary quality. Timely discharge summaries in this study were more likely to include key content and to be transmitted to the appropriate physician. Strategies to improve discharge summary quality should therefore prioritize timely summaries, which can be expected to have downstream benefits for other aspects of quality. Some studies have found that templates improve discharge summary content.[22] In our institution, a template exists, but it favors a hospitalization‐focused rather than transition‐focused approach to the discharge summary. For instance, it includes instructions to dictate the admission exam, but not the discharge exam. Thus, designing templates specifically for transitional care is key. Maximizing capabilities of electronic records may help; many content elements that were commonly missing (e.g., pending results, discharge vitals, discharge weight) could be automatically inserted from electronic records. Likewise, automatic transmission of the summary to care providers listed in the electronic record might ameliorate many transmission failures. Some efforts have been made to convert existing electronic data into discharge summaries.[23, 24, 25] However, these activities are very preliminary, and some studies have found the quality of electronic summaries to be lower than dictated or handwritten summaries.[26] As with all automated or electronic applications, it will be essential to consider workflow, readability, and ability to synthesize information prior to adoption.
Hospitalists consistently produced highest‐quality summaries, even though they did not receive explicit training, suggesting experience may be beneficial,[27, 28, 29] or that the hospitalist community focus on transitional care has been effective. In addition, hospitalists at our institution explicitly prioritize timely and comprehensive discharge dictations, because their business relies on maintaining good relationships with outpatient physicians who contract for their services. Housestaff and APRNs have no such incentives or policies; rather, they typically consider discharge summaries to be a useful source of patient history at the time of an admission or readmission. Other academic centers have found similar results.[6, 16] Nonetheless, even though hospitalists had slightly better performance in our study, large gaps in the quality of summaries remained for all groups including hospitalists.
This study has several limitations. First, as a single‐site study at an academic hospital, it may not be generalizable to other hospitals or other settings. It is noteworthy, however, that the average time to dictation in this study was much lower than that of other studies,[4, 14, 30, 31, 32] suggesting that practices at this institution are at least no worse and possibly better than elsewhere. Second, although there are some mandates and expert opinion‐based guidelines for discharge summary content, there is no validated evidence base to confirm what content ought to be present in discharge summaries to improve patient outcomes. Third, we had too few readmissions in the dataset to have enough power to determine whether discharge summary content, timeliness, or transmission predicts readmission. Fourth, we did not determine whether the information in discharge summaries was accurate or complete; we merely assessed whether it was present. For example, we gave every discharge summary full credit for including discharge medications because they are automatically appended. Yet medication reconciliation errors at discharge are common.[33, 34] In fact, in the DISCHARGE study cohort, more than a quarter of discharge medication lists contained a suspected error.[35]
In summary, this study demonstrated the inadequacy of the contemporary discharge summary for conveying information that is critical to the transition from hospital to home. It may be that hospital culture treats hospitalizations as discrete and self‐contained events rather than as components of a larger episode of care. As interest in reducing readmissions rises, reframing the discharge summary to serve as a transitional tool and targeting it for quality assessment will likely be necessary.
Acknowledgments
The authors would like to acknowledge Amy Browning and the staff of the Center for Outcomes Research and Evaluation Follow‐Up Center for conducting patient interviews, Mark Abroms and Katherine Herman for patient recruitment and screening, and Peter Charpentier for Web site development.
Disclosures
At the time this study was conducted, Dr. Horwitz was supported by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research, and was a Centers of Excellence Scholar in Geriatric Medicine by the John A. Hartford Foundation and the American Federation for Aging Research. Dr. Horwitz is now supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. This work was also supported by a grant from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (P30AG021342 NIH/NIA). Dr. Krumholz is supported by grant U01 HL105270‐01 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. No funding source had any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging, the National Center for Advancing Translational Sciences, the National Institutes of Health, The John A. Hartford Foundation, the National Heart, Lung, and Blood Institute, or the American Federation for Aging Research. Dr. Horwitz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. An earlier version of this work was presented as an oral presentation at the Society of General Internal Medicine Annual Meeting in Orlando, Florida on May 12, 2012. Dr. Krumholz chairs a cardiac scientific advisory board for UnitedHealth. Dr. Krumholz receives support from the Centers of Medicare and Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting, including readmission measures.
APPENDIX
A
Dictation guidelines provided to house staff and hospitalists
DICTATION GUIDELINES
FORMAT OF DISCHARGE SUMMARY
- Your name(spell it out), andPatient name(spell it out as well)
- Medical record number, date of admission, date of discharge
- Attending physician
- Disposition
- Principal and other diagnoses, Principal and other operations/procedures
- Copies to be sent to other physicians
- Begin narrative: CC, HPI, PMHx, Medications on admit, Social, Family Hx, Physical exam on admission, Data (labs on admission, plus labs relevant to workup, significant changes at discharge, admission EKG, radiologic and other data),Hospital course by problem, discharge meds, follow‐up appointments
APPENDIX
B
| Diagnosis |
| Discharge Second Diagnosis |
| Hospital course |
| Procedures/tests performed during admission |
| Patient and Family Instructions |
| Social support or living situation of patient |
| Functional capacity at discharge |
| Cognitive capacity at discharge |
| Physical exam at discharge |
| Laboratory results at time of discharge |
| Back to baseline or other nonspecific remark about discharge status |
| Any test or result still pending |
| Specific comment that nothing is pending |
| Recommendation for follow up tests/procedures |
| Call back number of responsible in‐house physician |
| Resuscitation status |
| Etiology of heart failure |
| Reason/trigger for exacerbation |
| Ejection fraction |
| Discharge weight |
| Target weight range |
| Discharge creatinine or GFR |
| If stent placed, whether drug‐eluting or not |
| Composite element | Data elements abstracted that qualify as meeting measure |
|---|---|
| Reason for hospitalization | Diagnosis |
| Significant findings | Hospital course |
| Procedures and treatment provided | Procedures/tests performed during admission |
| Patient's discharge condition | Functional capacity at discharge, Cognitive capacity at discharge, Physical exam at discharge, Laboratory results at time of discharge, Back to baseline or other nonspecific remark about discharge status |
| Patient and family instructions | Signs and symptoms to monitor at home |
| Attending physician's signature | Attending signature |
| Composite element | Data elements abstracted that qualify as meeting measure |
|---|---|
| Principal diagnosis | Diagnosis |
| Problem list | Discharge second diagnosis |
| Medication list | [Automatically appended; full credit to every summary] |
| Transferring physician name and contact information | Call back number of responsible in‐house physician |
| Cognitive status of the patient | Cognitive capacity at discharge |
| Test results | Procedures/tests performed during admission |
| Pending test results | Any test or result still pending or specific comment that nothing is pending |
APPENDIX
C
Histogram of days between discharge and dictation
Hospitalized patients are often cared for by physicians who do not follow them in the community, creating a discontinuity of care that must be bridged through communication. This communication between inpatient and outpatient physicians occurs, in part via a discharge summary, which is intended to summarize events during hospitalization and prepare the outpatient physician to resume care of the patient. Yet, this form of communication has long been problematic.[1, 2, 3] In a 1960 study, only 30% of discharge letters were received by the primary care physician within 48 hours of discharge.[1]
More recent studies have shown little improvement. Direct communication between hospital and outpatient physicians is rare, and discharge summaries are still largely unavailable at the time of follow‐up.[4] In 1 study, primary care physicians were unaware of 62% of laboratory tests or study results that were pending on discharge,[5] in part because this information is missing from most discharge summaries.[6] Deficits such as these persist despite the fact that the rate of postdischarge completion of recommended tests, referrals, or procedures is significantly increased when the recommendation is included in the discharge summary.[7]
Regulatory mandates for discharge summaries from the Centers for Medicare and Medicaid Services[8] and from The Joint Commission[9] appear to be generally met[10, 11]; however, these mandates have no requirements for timeliness stricter than 30 days, do not require that summaries be transmitted to outpatient physicians, and do not require several content elements that might be useful to outside physicians such as condition of the patient at discharge, cognitive and functional status, goals of care, or pending studies. Expert opinion guidelines have more comprehensive recommendations,[12, 13] but it is uncertain how widely they are followed.
The existence of a discharge summary does not necessarily mean it serves a patient well in the transitional period.[11, 14, 15] Discharge summaries are a complex intervention, and we do not yet understand the best ways discharge summaries may fulfill needs specific to transitional care. Furthermore, it is uncertain what factors improve aspects of discharge summary quality as defined by timeliness, transmission, and content.[6, 16]
The goal of the DIagnosing Systemic failures, Complexities and HARm in GEriatric discharges study (DISCHARGE) was to comprehensively assess the discharge process for older patients discharged to the community. In this article we examine discharge summaries of patients enrolled in the study to determine the timeliness, transmission to outside physicians, and content of the summaries. We further examine the effect of provider training level and timeliness of dictation on discharge summary quality.
METHODS
Study Cohort
The DISCHARGE study was a prospective, observational cohort study of patients 65 years or older discharged to home from YaleNew Haven Hospital (YNHH) who were admitted with acute coronary syndrome (ACS), community‐acquired pneumonia, or heart failure (HF). Patients were screened by physicians for eligibility within 24 hours of admission using specialty society guidelines[17, 18, 19, 20] and were enrolled by telephone within 1 week of discharge. Additional inclusion criteria included speaking English or Spanish, and ability of the patient or caregiver to participate in a telephone interview. Patients enrolled in hospice were excluded, as were patients who failed the Mini‐Cog mental status screen (3‐item recall and a clock draw)[21] while in the hospital or appeared confused or delirious during the telephone interview. Caregivers of cognitively impaired patients were eligible for enrollment instead if the patient provided permission.
Study Setting
YNHH is a 966‐bed urban tertiary care hospital with statistically lower than the national average mortality for acute myocardial infarction, HF, and pneumonia but statistically higher than the national average for 30‐day readmission rates for HF and pneumonia at the time this study was conducted. Advanced practice registered nurses (APRNs) working under the supervision of private or university cardiologists provided care for cardiology service patients. Housestaff under the supervision of university or hospitalist attending physicians, or physician assistants or APRNs under the supervision of hospitalist attending physicians provided care for patients on medical services. Discharge summaries were typically dictated by APRNs for cardiology patients, by 2nd‐ or 3rd‐year residents for housestaff patients, and by hospitalists for hospitalist patients. A dictation guideline was provided to housestaff and hospitalists (see Supporting Information, Appendix 1, in the online version of this article); this guideline suggested including basic demographic information, disposition and diagnoses, the admission history and physical, hospital course, discharge medications, and follow‐up appointments. Additionally, housestaff received a lecture about discharge summaries at the start of their 2nd year. Discharge instructions including medications and follow‐up appointment information were automatically appended to the discharge summaries. Summaries were sent by the medical records department only to physicians in the system who were listed by the dictating physician as needing to receive a copy of the summary; no summary was automatically sent (ie, to the primary care physician) if not requested by the dictating physician.
Data Collection
Experienced registered nurses trained in chart abstraction conducted explicit reviews of medical charts using a standardized review tool. The tool included 24 questions about the discharge summary applicable to all 3 conditions, with 7 additional questions for patients with HF and 1 additional question for patients with ACS. These questions included the 6 elements required by The Joint Commission for all discharge summaries (reason for hospitalization, significant findings, procedures and treatment provided, patient's discharge condition, patient and family instructions, and attending physician's signature)[9] as well as the 7 elements (principal diagnosis and problem list, medication list, transferring physician name and contact information, cognitive status of the patient, test results, and pending test results) recommended by the Transitions of Care Consensus Conference (TOCCC), a recent consensus statement produced by 6 major medical societies.[13] Each content element is shown in (see Supporting Information, Appendix 2, in the online version of this article), which also indicates the elements included in the 2 guidelines.
Main Measures
We assessed quality in 3 main domains: timeliness, transmission, and content. We defined timeliness as days between discharge date and dictation date (not final signature date, which may occur later), and measured both median timeliness and proportion of discharge summaries completed on the day of discharge. We defined transmission as successful fax or mail of the discharge summary to an outside physician as reported by the medical records department, and measured the proportion of discharge summaries sent to any outside physician as well as the median number of physicians per discharge summary who were scheduled to follow‐up with the patient postdischarge but who did not receive a copy of the summary. We defined 21 individual content items and assessed the frequency of each individual content item. We also measured compliance with The Joint Commission mandates and TOCCC recommendations, which included several of the individual content items.
To measure compliance with The Joint Commission requirements, we created a composite score in which 1 point was provided for the presence of each of the 6 required elements (maximum score=6). Every discharge summary received 1 point for attending physician signature, because all discharge summaries were electronically signed. Discharge instructions to family/patients were automatically appended to every discharge summary; however, we gave credit for patient and family instructions only to those that included any information about signs and symptoms to monitor for at home. We defined discharge condition as any information about functional status, cognitive status, physical exam, or laboratory findings at discharge.
To measure compliance with specialty society recommendations for discharge summaries, we created a composite score in which 1 point was provided for the presence of each of the 7 recommended elements (maximum score=7). Every discharge summary received 1 point for discharge medications, because these are automatically appended.
We obtained data on age, race, gender, and length of stay from hospital administrative databases. The study was approved by the Yale Human Investigation Committee, and verbal informed consent was obtained from all study participants.
Statistical Analysis
Characteristics of the sample are described with counts and percentages or means and standard deviations. Medians and interquartile ranges (IQRs) or counts and percentages were calculated for summary measures of timeliness, transmission, and content. We assessed differences in quality measures between APRNs, housestaff, and hospitalists using 2 tests. We conducted multivariable logistic regression analyses for timeliness and for transmission to any outside physician. All discharge summaries included at least 4 of The Joint Commission elements; consequently, we coded this content outcome as an ordinal variable with 3 levels indicating inclusion of 4, 5, or 6 of The Joint Commission elements. We coded the TOCCC content outcome as a 3‐level variable indicating <4, 4, or >4 elements satisfied. Accordingly, proportional odds models were used, in which the reported odds ratios (ORs) can be interpreted as the average effect of the explanatory variable on the odds of having more recommendations, for any dichotomization of the outcome. Residual analysis and goodness‐of‐fit statistics were used to assess model fit; the proportional odds assumption was tested. Statistical analyses were conducted with SAS 9.2 (SAS Institute, Cary, NC). P values <0.05 were interpreted as statistically significant for 2‐sided tests.
RESULTS
Enrollment and Study Sample
A total of 3743 patients over 64 years old were discharged home from the medical service at YNHH during the study period; 3028 patients were screened for eligibility within 24 hours of admission. We identified 635 eligible admissions and enrolled 395 patients (62.2%) in the study. Of these, 377 granted permission for chart review and were included in this analysis (Figure 1).
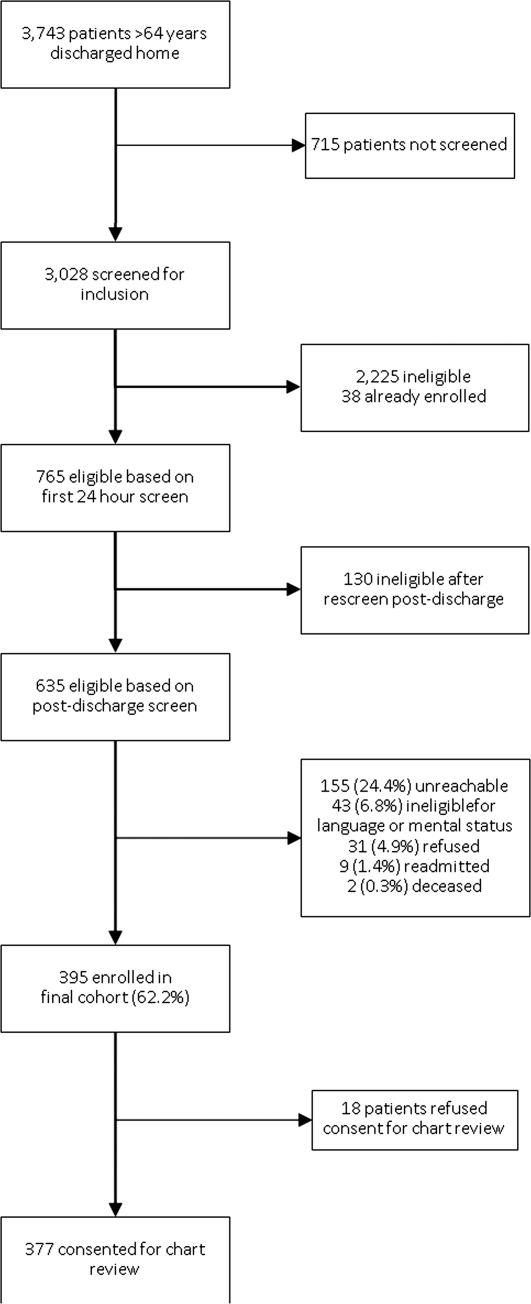
The study sample had a mean age of 77.1 years (standard deviation: 7.8); 205 (54.4%) were male and 310 (82.5%) were non‐Hispanic white. A total of 195 (51.7%) had ACS, 91 (24.1%) had pneumonia, and 146 (38.7%) had HF; 54 (14.3%) patients had more than 1 qualifying condition. There were similar numbers of patients on the cardiology, medicine housestaff, and medicine hospitalist teams (Table 1).
| Characteristic | N (%) or Mean (SD) |
|---|---|
| |
| Condition | |
| Acute coronary syndrome | 195 (51.7) |
| Community‐acquired pneumonia | 91 (24.1) |
| Heart failure | 146 (38.7) |
| Training level of summary dictator | |
| APRN | 140 (37.1) |
| House staff | 123 (32.6) |
| Hospitalist | 114 (30.2) |
| Length of stay, mean, d | 3.5 (2.5) |
| Total number of medications | 8.9 (3.3) |
| Identify a usual source of care | 360 (96.0) |
| Age, mean, y | 77.1 (7.8) |
| Male | 205 (54.4) |
| English‐speaking | 366 (98.1) |
| Race/ethnicity | |
| Non‐Hispanic white | 310 (82.5) |
| Non‐Hispanic black | 44 (11.7) |
| Hispanic | 15 (4.0) |
| Other | 7 (1.9) |
| High school graduate or GED Admission source | 268 (73.4) |
| Emergency department | 248 (66.0) |
| Direct transfer from hospital or nursing facility | 94 (25.0) |
| Direct admission from office | 34 (9.0) |
Timeliness
Discharge summaries were completed for 376/377 patients, of which 174 (46.3%) were dictated on the day of discharge. However, 122 (32.4%) summaries were dictated more than 48 hours after discharge, including 93 (24.7%) that were dictated more than 1 week after discharge (see Supporting Information, Appendix 3, in the online version of this article).
Summaries dictated by hospitalists were most likely to be done on the day of discharge (35.3% APRNs, 38.2% housestaff, 68.4% hospitalists, P<0.001). After adjustment for diagnosis and length of stay, hospitalists were still significantly more likely to produce a timely discharge summary than APRNs (OR: 2.82; 95% confidence interval [CI]: 1.56‐5.09), whereas housestaff were no different than APRNs (OR: 0.84; 95% CI: 0.48‐1.46).
Transmission
A total of 144 (38.3%) discharge summaries were not sent to any physician besides the inpatient attending, and 209/374 (55.9%) were not sent to at least 1 physician listed as having a follow‐up appointment planned with the patient. Each discharge summary was sent to a median of 1 physician besides the dictating physician (IQR: 01). However, for each summary, a median of 1 physician (IQR: 01) who had a scheduled follow‐up with the patient did not receive the summary. Summaries dictated by hospitalists were most likely to be sent to at least 1 outside physician (54.7% APRNs, 58.5% housestaff, 73.7% hospitalists, P=0.006). Summaries dictated on the day of discharge were more likely than delayed summaries to be sent to at least 1 outside physician (75.9% vs 49.5%, P<0.001). After adjustment for diagnosis and length of stay, there was no longer a difference in likelihood of transmitting a discharge summary to any outpatient physician according to training level; however, dictations completed on the day of discharge remained significantly more likely to be transmitted to an outside physician (OR: 3.05; 95% CI: 1.88‐4.93) (Table 2).
| Explanatory Variable | Proportion Transmitted to at Least 1 Outside Physician | OR for Transmission to Any Outside Physician (95% CI) | Adjusted P Value |
|---|---|---|---|
| |||
| Training level | 0.52 | ||
| APRN | 54.7% | REF | |
| Housestaff | 58.5% | 1.17 (0.66‐2.06) | |
| Hospitalist | 73.7% | 1.46 (0.76‐2.79) | |
| Timeliness | |||
| Dictated after discharge | 49.5% | REF | <0.001 |
| Dictated day of discharge | 75.9% | 3.05 (1.88‐4.93) | |
| Acute coronary syndrome vs nota | 52.1 % | 1.05 (0.49‐2.26) | 0.89 |
| Pneumonia vs nota | 69.2 % | 1.59 (0.66‐3.79) | 0.30 |
| Heart failure vs nota | 74.7 % | 3.32 (1.61‐6.84) | 0.001 |
| Length of stay, d | 0.91 (0.83‐1.00) | 0.06 | |
Content
Rate of inclusion of each content element is shown in Table 3, overall and by training level. Nearly every discharge summary included information about admitting diagnosis, hospital course, and procedures or tests performed during the hospitalization. However, few summaries included information about the patient's condition at discharge. Less than half included discharge laboratory results; less than one‐third included functional capacity, cognitive capacity, or discharge physical exam. Only 4.1% overall of discharge summaries for patients with HF included the patient's weight at discharge; best were hospitalists who still included this information in only 7.7% of summaries. Information about postdischarge care, including home social support, pending tests, or recommended follow‐up tests/procedures was also rarely specified. Last, only 6.2% of discharge summaries included the name and contact number of the inpatient physician; this information was least likely to be provided by housestaff (1.6%) and most likely to be provided by hospitalists (15.2%) (P<0.001).
| Discharge Summary Component | Overall, n=377, n (%) | APRN, n=140, n (%) | Housestaff, n=123, n (%) | Hospitalist, n=114, n (%) | P Value |
|---|---|---|---|---|---|
| |||||
| Diagnosisab | 368 (97.9) | 136 (97.8) | 120 (97.6) | 112 (98.3) | 1.00 |
| Discharge second diagnosisb | 289 (76.9) | 100 (71.9) | 89 (72.4) | 100 (87.7) | <0.001 |
| Hospital coursea | 375 (100.0) | 138 (100) | 123 (100) | 114 (100) | N/A |
| Procedures/tests performed during admissionab | 374 (99.7) | 138 (99.3) | 123 (100) | 113 (100) | N/A |
| Patient and family instructionsa | 371 (98.4) | 136 (97.1) | 122 (99.2) | 113 (99.1) | .43 |
| Social support or living situation of patient | 148 (39.5) | 18 (12.9) | 62 (50.4) | 68 (60.2) | <0.001 |
| Functional capacity at dischargea | 99 (26.4) | 37 (26.6) | 32 (26.0) | 30 (26.6) | 0.99 |
| Cognitive capacity at dischargeab | 30 (8.0) | 6 (4.4) | 11 (8.9) | 13 (11.5) | 0.10 |
| Physical exam at dischargea | 62 (16.7) | 19 (13.8) | 16 (13.1) | 27 (24.1) | 0.04 |
| Laboratory results at time of dischargea | 164 (43.9) | 63 (45.3) | 50 (40.7) | 51 (45.5) | 0.68 |
| Back to baseline or other nonspecific remark about discharge statusa | 71 (19.0) | 30 (21.6) | 18 (14.8) | 23 (20.4) | 0.34 |
| Any test or result still pending or specific comment that nothing is pendingb | 46 (12.2) | 9 (6.4) | 20 (16.3) | 17 (14.9) | 0.03 |
| Recommendation for follow‐up tests/procedures | 157 (41.9) | 43 (30.9) | 54 (43.9) | 60 (53.1) | 0.002 |
| Call‐back number of responsible in‐house physicianb | 23 (6.2) | 4 (2.9) | 2 (1.6) | 17 (15.2) | <0.001 |
| Resuscitation status | 27 (7.7) | 2 (1.5) | 18 (15.4) | 7 (6.7) | <0.001 |
| Etiology of heart failurec | 120 (82.8) | 44 (81.5) | 34 (87.2) | 42 (80.8) | 0.69 |
| Reason/trigger for exacerbationc | 86 (58.9) | 30 (55.6) | 27 (67.5) | 29 (55.8) | 0.43 |
| Ejection fractionc | 107 (73.3) | 40 (74.1) | 32 (80.0) | 35 (67.3) | 0.39 |
| Discharge weightc | 6 (4.1) | 1 (1.9) | 1 (2.5) | 4 (7.7) | 0.33 |
| Target weight rangec | 5 (3.4) | 0 (0) | 2 (5.0) | 3 (5.8) | 0.22 |
| Discharge creatinine or GFRc | 34 (23.3) | 14 (25.9) | 10 (25.0) | 10 (19.2) | 0.69 |
| If stent placed, whether drug‐eluting or notd | 89 (81.7) | 58 (87.9) | 27 (81.8) | 4 (40.0) | 0.001 |
On average, summaries included 5.6 of the 6 Joint Commission elements and 4.0 of the 7 TOCCC elements. A total of 63.0% of discharge summaries included all 6 elements required by The Joint Commission, whereas no discharge summary included all 7 TOCCC elements.
APRNs, housestaff and hospitalists included the same average number of The Joint Commission elements (5.6 each), but hospitalists on average included slightly more TOCCC elements (4.3) than did housestaff (4.0) or APRNs (3.8) (P<0.001). Summaries dictated on the day of discharge included an average of 4.2 TOCCC elements, compared to 3.9 TOCCC elements in delayed discharge. In multivariable analyses adjusted for diagnosis and length of stay, there was still no difference by training level in presence of The Joint Commission elements, but hospitalists were significantly more likely to include more TOCCC elements than APRNs (OR: 2.70; 95% CI: 1.49‐4.90) (Table 4). Summaries dictated on the day of discharge were significantly more likely to include more TOCCC elements (OR: 1.92; 95% CI: 1.23‐2.99).
| Explanatory Variable | Average Number of TOCCC Elements Included | OR (95% CI) | Adjusted P Value |
|---|---|---|---|
| |||
| Training level | 0.004 | ||
| APRN | 3.8 | REF | |
| Housestaff | 4.0 | 1.54 (0.90‐2.62) | |
| Hospitalist | 4.3 | 2.70 (1.49‐4.90) | |
| Timeliness | |||
| Dictated after discharge | 3.9 | REF | |
| Dictated day of discharge | 4.2 | 1.92 (1.23‐2.99) | 0.004 |
| Acute coronary syndrome vs nota | 3.9 | 0.72 (0.37‐1.39) | 0.33 |
| Pneumonia vs nota | 4.2 | 1.02 (0.49‐2.14) | 0.95 |
| Heart failure vs nota | 4.1 | 1.49 (0.80‐2.78) | 0.21 |
| Length of stay, d | 0.99 (0.90‐1.07) | 0.73 | |
No discharge summary included all 7 TOCCC‐endorsed content elements, was dictated on the day of discharge, and was sent to an outside physician.
DISCUSSION
In this prospective single‐site study of medical patients with 3 common conditions, we found that discharge summaries were completed relatively promptly, but were often not sent to the appropriate outpatient physicians. We also found that summaries were uniformly excellent at providing details of the hospitalization, but less reliable at providing details relevant to transitional care such as the patient's condition on discharge or existence of pending tests. On average, summaries included 57% of the elements included in consensus guidelines by 6 major medical societies. The content of discharge summaries dictated by hospitalists was slightly more comprehensive than that of APRNs and trainees, but no group exhibited high performance. In fact, not one discharge summary fully met all 3 quality criteria of timeliness, transmission, and content.
Our study, unlike most in the field, focused on multiple dimensions of discharge summary quality simultaneously. For instance, previous studies have found that timely receipt of a discharge summary does not reduce readmission rates.[11, 14, 15] Yet, if the content of the discharge summary is inadequate for postdischarge care, the summary may not be useful even if it is received by the follow‐up visit. Conversely, high‐quality content is ineffective if the summary is not sent to the outpatient physician.
This study suggests several avenues for improving summary quality. Timely discharge summaries in this study were more likely to include key content and to be transmitted to the appropriate physician. Strategies to improve discharge summary quality should therefore prioritize timely summaries, which can be expected to have downstream benefits for other aspects of quality. Some studies have found that templates improve discharge summary content.[22] In our institution, a template exists, but it favors a hospitalization‐focused rather than transition‐focused approach to the discharge summary. For instance, it includes instructions to dictate the admission exam, but not the discharge exam. Thus, designing templates specifically for transitional care is key. Maximizing capabilities of electronic records may help; many content elements that were commonly missing (e.g., pending results, discharge vitals, discharge weight) could be automatically inserted from electronic records. Likewise, automatic transmission of the summary to care providers listed in the electronic record might ameliorate many transmission failures. Some efforts have been made to convert existing electronic data into discharge summaries.[23, 24, 25] However, these activities are very preliminary, and some studies have found the quality of electronic summaries to be lower than dictated or handwritten summaries.[26] As with all automated or electronic applications, it will be essential to consider workflow, readability, and ability to synthesize information prior to adoption.
Hospitalists consistently produced highest‐quality summaries, even though they did not receive explicit training, suggesting experience may be beneficial,[27, 28, 29] or that the hospitalist community focus on transitional care has been effective. In addition, hospitalists at our institution explicitly prioritize timely and comprehensive discharge dictations, because their business relies on maintaining good relationships with outpatient physicians who contract for their services. Housestaff and APRNs have no such incentives or policies; rather, they typically consider discharge summaries to be a useful source of patient history at the time of an admission or readmission. Other academic centers have found similar results.[6, 16] Nonetheless, even though hospitalists had slightly better performance in our study, large gaps in the quality of summaries remained for all groups including hospitalists.
This study has several limitations. First, as a single‐site study at an academic hospital, it may not be generalizable to other hospitals or other settings. It is noteworthy, however, that the average time to dictation in this study was much lower than that of other studies,[4, 14, 30, 31, 32] suggesting that practices at this institution are at least no worse and possibly better than elsewhere. Second, although there are some mandates and expert opinion‐based guidelines for discharge summary content, there is no validated evidence base to confirm what content ought to be present in discharge summaries to improve patient outcomes. Third, we had too few readmissions in the dataset to have enough power to determine whether discharge summary content, timeliness, or transmission predicts readmission. Fourth, we did not determine whether the information in discharge summaries was accurate or complete; we merely assessed whether it was present. For example, we gave every discharge summary full credit for including discharge medications because they are automatically appended. Yet medication reconciliation errors at discharge are common.[33, 34] In fact, in the DISCHARGE study cohort, more than a quarter of discharge medication lists contained a suspected error.[35]
In summary, this study demonstrated the inadequacy of the contemporary discharge summary for conveying information that is critical to the transition from hospital to home. It may be that hospital culture treats hospitalizations as discrete and self‐contained events rather than as components of a larger episode of care. As interest in reducing readmissions rises, reframing the discharge summary to serve as a transitional tool and targeting it for quality assessment will likely be necessary.
Acknowledgments
The authors would like to acknowledge Amy Browning and the staff of the Center for Outcomes Research and Evaluation Follow‐Up Center for conducting patient interviews, Mark Abroms and Katherine Herman for patient recruitment and screening, and Peter Charpentier for Web site development.
Disclosures
At the time this study was conducted, Dr. Horwitz was supported by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research, and was a Centers of Excellence Scholar in Geriatric Medicine by the John A. Hartford Foundation and the American Federation for Aging Research. Dr. Horwitz is now supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. This work was also supported by a grant from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (P30AG021342 NIH/NIA). Dr. Krumholz is supported by grant U01 HL105270‐01 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. No funding source had any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging, the National Center for Advancing Translational Sciences, the National Institutes of Health, The John A. Hartford Foundation, the National Heart, Lung, and Blood Institute, or the American Federation for Aging Research. Dr. Horwitz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. An earlier version of this work was presented as an oral presentation at the Society of General Internal Medicine Annual Meeting in Orlando, Florida on May 12, 2012. Dr. Krumholz chairs a cardiac scientific advisory board for UnitedHealth. Dr. Krumholz receives support from the Centers of Medicare and Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting, including readmission measures.
APPENDIX
A
Dictation guidelines provided to house staff and hospitalists
DICTATION GUIDELINES
FORMAT OF DISCHARGE SUMMARY
- Your name(spell it out), andPatient name(spell it out as well)
- Medical record number, date of admission, date of discharge
- Attending physician
- Disposition
- Principal and other diagnoses, Principal and other operations/procedures
- Copies to be sent to other physicians
- Begin narrative: CC, HPI, PMHx, Medications on admit, Social, Family Hx, Physical exam on admission, Data (labs on admission, plus labs relevant to workup, significant changes at discharge, admission EKG, radiologic and other data),Hospital course by problem, discharge meds, follow‐up appointments
APPENDIX
B
| Diagnosis |
| Discharge Second Diagnosis |
| Hospital course |
| Procedures/tests performed during admission |
| Patient and Family Instructions |
| Social support or living situation of patient |
| Functional capacity at discharge |
| Cognitive capacity at discharge |
| Physical exam at discharge |
| Laboratory results at time of discharge |
| Back to baseline or other nonspecific remark about discharge status |
| Any test or result still pending |
| Specific comment that nothing is pending |
| Recommendation for follow up tests/procedures |
| Call back number of responsible in‐house physician |
| Resuscitation status |
| Etiology of heart failure |
| Reason/trigger for exacerbation |
| Ejection fraction |
| Discharge weight |
| Target weight range |
| Discharge creatinine or GFR |
| If stent placed, whether drug‐eluting or not |
| Composite element | Data elements abstracted that qualify as meeting measure |
|---|---|
| Reason for hospitalization | Diagnosis |
| Significant findings | Hospital course |
| Procedures and treatment provided | Procedures/tests performed during admission |
| Patient's discharge condition | Functional capacity at discharge, Cognitive capacity at discharge, Physical exam at discharge, Laboratory results at time of discharge, Back to baseline or other nonspecific remark about discharge status |
| Patient and family instructions | Signs and symptoms to monitor at home |
| Attending physician's signature | Attending signature |
| Composite element | Data elements abstracted that qualify as meeting measure |
|---|---|
| Principal diagnosis | Diagnosis |
| Problem list | Discharge second diagnosis |
| Medication list | [Automatically appended; full credit to every summary] |
| Transferring physician name and contact information | Call back number of responsible in‐house physician |
| Cognitive status of the patient | Cognitive capacity at discharge |
| Test results | Procedures/tests performed during admission |
| Pending test results | Any test or result still pending or specific comment that nothing is pending |
APPENDIX
C
Histogram of days between discharge and dictation
- , , . Value of the specialist's report. Br Med J. 1960;2(5213):1663–1664.
- , . Communications between general practitioners and consultants. Br Med J. 1974;4(5942):456–459.
- , , . A functional hospital discharge summary. J Pediatr. 1975;86(1):97–98.
- , , , , , . Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128.
- , , , et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow‐up providers. J Gen Intern Med. 2009;24(9):1002–1006.
- , , . Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305–1311.
- Centers for Medicare and Medicaid Services. Condition of participation: medical record services. 42. Vol 482.C.F.R. § 482.24 (2012).
- Joint Commission on Accreditation of Healthcare Organizations. Hospital Accreditation Standards. Standard IM 6.10 EP 7–9. Oakbrook Terrace, IL: The Joint Commission; 2008.
- , . Documentation of mandated discharge summary components in transitions from acute to subacute care. In: Agency for Healthcare Research and Quality, ed. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 2: Culture and Redesign. AHRQ Publication No. 08-0034‐2. Rockville, MD: Agency for Healthcare Research and Quality; 2008:179–188.
- , , , et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20(9):773–778.
- , , , et al. Transition of care for hospitalized elderly patients‐development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354–360.
- , , , et al. Transitions of Care Consensus Policy Statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971–976.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , . Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , . Provider characteristics, clinical‐work processes and their relationship to discharge summary quality for sub‐acute care patients. J Gen Intern Med. 2012;27(1):78–84.
- , , , et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50(7):e1–e157.
- , , . Universal definition of myocardial infarction. Eur Heart J. 2007;28(20):2525–2538.
- , , , et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–989.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- , , , et al. Clock drawing in Alzheimer's disease. A novel measure of dementia severity. J Am Geriatr Soc. 1989;37(8):725–729.
- , , , , . Assessing quality and efficiency of discharge summaries. Am J Med Qual. 2005;20(6):337–343.
- , , , et al. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Intern Med. 2009;24(9):995–1001.
- , , , . Dictated versus database‐generated discharge summaries: a randomized clinical trial. CMAJ. 1999;160(3):319–326.
- , , , , . Computerised updating of clinical summaries: new opportunities for clinical practice and research? BMJ. 1988;297(6662):1504–1506.
- , , . Evaluation of electronic discharge summaries: a comparison of documentation in electronic and handwritten discharge summaries. Int J Med Inform. 2008;77(9):613–620.
- , , , , . Did I do as best as the system would let me? Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , , . Learning by doing—resident perspectives on developing competency in high‐quality discharge care. J Gen Intern Med. 2012;27(9):1188–1194.
- , , , , . Out of sight, out of mind: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381.
- , , . Dissemination of discharge summaries. Not reaching follow‐up physicians. Can Fam Physician. 2002;48:737–742.
- , , , . Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , . General practitioner‐hospital communications: a review of discharge summaries. J Qual Clin Pract. 2001;21(4):104–108.
- , , . Accuracy of information on medicines in hospital discharge summaries. Intern Med J. 2006;36(4):221–225.
- , , . Accuracy of medication documentation in hospital discharge summaries: A retrospective analysis of medication transcription errors in manual and electronic discharge summaries. Int J Med Inform. 2010;79(1):58–64.
- , , , . Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012;27(11):1513–1520.
- , , . Value of the specialist's report. Br Med J. 1960;2(5213):1663–1664.
- , . Communications between general practitioners and consultants. Br Med J. 1974;4(5942):456–459.
- , , . A functional hospital discharge summary. J Pediatr. 1975;86(1):97–98.
- , , , , , . Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med. 2005;143(2):121–128.
- , , , et al. Adequacy of hospital discharge summaries in documenting tests with pending results and outpatient follow‐up providers. J Gen Intern Med. 2009;24(9):1002–1006.
- , , . Tying up loose ends: discharging patients with unresolved medical issues. Arch Intern Med. 2007;167(12):1305–1311.
- Centers for Medicare and Medicaid Services. Condition of participation: medical record services. 42. Vol 482.C.F.R. § 482.24 (2012).
- Joint Commission on Accreditation of Healthcare Organizations. Hospital Accreditation Standards. Standard IM 6.10 EP 7–9. Oakbrook Terrace, IL: The Joint Commission; 2008.
- , . Documentation of mandated discharge summary components in transitions from acute to subacute care. In: Agency for Healthcare Research and Quality, ed. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 2: Culture and Redesign. AHRQ Publication No. 08-0034‐2. Rockville, MD: Agency for Healthcare Research and Quality; 2008:179–188.
- , , , et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf. 2011;20(9):773–778.
- , , , et al. Transition of care for hospitalized elderly patients‐development of a discharge checklist for hospitalists. J Hosp Med. 2006;1(6):354–360.
- , , , et al. Transitions of Care Consensus Policy Statement American College of Physicians‐Society of General Internal Medicine‐Society of Hospital Medicine‐American Geriatrics Society‐American College of Emergency Physicians‐Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971–976.
- , , , et al. Association of communication between hospital‐based physicians and primary care providers with patient outcomes. J Gen Intern Med. 2009;24(3):381–386.
- , , , . Effect of discharge summary availability during post‐discharge visits on hospital readmission. J Gen Intern Med. 2002;17(3):186–192.
- , , , , . Provider characteristics, clinical‐work processes and their relationship to discharge summary quality for sub‐acute care patients. J Gen Intern Med. 2012;27(1):78–84.
- , , , et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non‐ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non‐ST‐Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50(7):e1–e157.
- , , . Universal definition of myocardial infarction. Eur Heart J. 2007;28(20):2525–2538.
- , , , et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–989.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- , , , et al. Clock drawing in Alzheimer's disease. A novel measure of dementia severity. J Am Geriatr Soc. 1989;37(8):725–729.
- , , , , . Assessing quality and efficiency of discharge summaries. Am J Med Qual. 2005;20(6):337–343.
- , , , et al. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Intern Med. 2009;24(9):995–1001.
- , , , . Dictated versus database‐generated discharge summaries: a randomized clinical trial. CMAJ. 1999;160(3):319–326.
- , , , , . Computerised updating of clinical summaries: new opportunities for clinical practice and research? BMJ. 1988;297(6662):1504–1506.
- , , . Evaluation of electronic discharge summaries: a comparison of documentation in electronic and handwritten discharge summaries. Int J Med Inform. 2008;77(9):613–620.
- , , , , . Did I do as best as the system would let me? Healthcare professional views on hospital to home care transitions. J Gen Intern Med. 2012;27(12):1649–1656.
- , , , , . Learning by doing—resident perspectives on developing competency in high‐quality discharge care. J Gen Intern Med. 2012;27(9):1188–1194.
- , , , , . Out of sight, out of mind: housestaff perceptions of quality‐limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381.
- , , . Dissemination of discharge summaries. Not reaching follow‐up physicians. Can Fam Physician. 2002;48:737–742.
- , , , . Primary care physician attitudes regarding communication with hospitalists. Am J Med. 2001;111(9B):15S–20S.
- , , , . General practitioner‐hospital communications: a review of discharge summaries. J Qual Clin Pract. 2001;21(4):104–108.
- , , . Accuracy of information on medicines in hospital discharge summaries. Intern Med J. 2006;36(4):221–225.
- , , . Accuracy of medication documentation in hospital discharge summaries: A retrospective analysis of medication transcription errors in manual and electronic discharge summaries. Int J Med Inform. 2010;79(1):58–64.
- , , , . Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med. 2012;27(11):1513–1520.
Copyright © 2013 Society of Hospital Medicine
Patient Dissatisfaction
The United States spends more money per capita on healthcare than any other industrialized nation,1 yet patients are the least satisfied with their care.2 Patient satisfaction is associated in both cross‐sectional3 and longitudinal studies4 with improved physical and mental health outcomes. Conversely, dissatisfaction with care hampers future medical interactions, prevents sharing of information, and impairs the building of trust.5 The increasing recognition that a patient's experience of care affects patient outcomes has furthered efforts to evaluate satisfaction with care.6, 7
However, patient satisfaction is challenging to define and understand. Even the definition of satisfaction is ambiguous, for to satisfy can mean both to make happy and the lesser, to be adequate. To dissatisfy is to displease or disappoint, but dissatisfaction is not the opposite of satisfaction: qualitative studies give little if any indication that patients evaluate satisfaction on a continuum ranging from dissatisfied at one end to very satisfied at the other.8 Instead, it appears that satisfaction and dissatisfaction are different constructs, such that patients may simultaneously be both satisfied and dissatisfied.9, 10 Patients often express overall satisfaction with a service or encounter while also reporting specific criticisms about its shortcomings.11, 12 Alternatively, consumers may be generally satisfied unless something unpleasant or improper happens.13 Thus, dissatisfaction and satisfaction may require different methods of measurement.
The most common model for measuring patient satisfaction is a quantitative survey of patients' experiences in specific predetermined domains. Of 54 hospital satisfaction surveys in common use, only 11 included patient input in their development,14 casting doubt on the relevance of these attributes to patients' priorities of care. Since it is well recognized that patient expectations influence satisfaction,8, 13, 15 it is important to identify patient expectations and priorities up front. However, these have not been clearly established. Furthermore, focusing purely on satisfaction with particular domains of care may miss the separate but illuminating construct of patient dissatisfaction.
In this study we therefore aim to understand patient dissatisfaction with hospitalization more fully as a means of elucidating implicit expectations for hospital care. Using qualitative techniques, we analyzed a large volume of patient responses to a single open‐ended study question to identify determinants and patterns of patient dissatisfaction.
Methods
Study Design
We conducted a qualitative analysis of telephone survey data obtained from adults recently discharged after an acute care hospitalization. Survey participants were asked five questions, including: If there was one thing we could have done to improve your experience in the hospital, what would it have been? Answers to this open‐ended question were included in this study.
Setting and Participants
The hospital is a 944‐bed, urban academic medical center. Patients or patient representatives were routinely surveyed in a telephone interview conducted by trained hospital staff 1‐5 days after hospital discharge. Calls were attempted to 90% of adult discharged patients, and approximately 50% of them were reached. For this study, we included patients who were age 18 or older, spoke English, and were discharged to home from a medical, surgical, gynecology‐oncology, neurology, neurosurgery, or intensive care unit. Of those patients, we randomly selected 10% of those surveyed between July 1, 2007 and June 30, 2008 for inclusion.
Primary Data Analysis
Qualitative data analysis was used to classify patient suggestions. The study team included internal medicine physicians (J.P.M., L.I.H.), a medical student (A.V.L.), and a recent college graduate (C.P.B.). Codes were generated using a mixed inductive and deductive approach by reading and rereading the primary data.16 A set of 100 interview responses were first read individually by three investigators (J.P.M., A.V.L., C.P.B.), after which investigators met to discuss themes and ideas. A preliminary list of coding categories was then generated. Each investigator then assigned these coding categories to additional survey responses in sets of 100. Subsequent meetings were held to refine codes using the constant comparative method.16 Disagreements were resolved by negotiated consensus. The full study group met periodically to review the code structure for logic and breadth. Once thematic saturation was achieved, the entire dataset was recoded by two investigators using the final coding structure. The final coding structure contained 42 unique codes organized into six broader themes. We used descriptive statistics to characterize the coding category results. The score for intercoder reliability was 0.91.
This study was approved by the Yale Human Investigation Committee, which granted a waiver of informed consent.
Results
A total of 976 surveys was randomly selected from 9,764 postdischarge phone interviews completed between July 1, 2007 and June 30, 2008. A total of 56.3% of patients was female. Nearly half the patients were discharged from medical units (Table 1). Of the 976 patients, 439 (45.0%) gave at least one suggestion for improvement, yielding a total of 579 suggestions. Patients also offered numerous positive comments about their care, but these comments were not included in the analysis.
| No. | % of Total Surveyed | |
|---|---|---|
| Total surveys | 976 | |
| Male | 427 | 43.7 |
| Female | 549 | 56.3 |
| Discharge Unit | ||
| Medical | 434 | 44.5 |
| Surgical | 303 | 31.0 |
| Gynecology/Oncology | 103 | 10.6 |
| ICU/CCU/Step‐down | 71 | 7.3 |
| Neurology/Neurosurgery | 65 | 6.6 |
| No suggestions for improvement | 537 | 55.0 |
| At least one suggestion for improvement | 439 | 45.0 |
Through qualitative analysis, we assigned suggestions for improvement to six major categories of dissatisfaction: 1) ineptitude, 2) disrespect, 3) prolonged waits, 4) ineffective communication, 5) lack of environmental control, and 6) substandard amenities. We considered the inverse of these problems to represent six implicit expectations of good hospital care: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities (Table 2). The number of patient suggestions related to each domain is detailed in Table 3.
| Domain of Dissatisfaction | Implicit Expectations | Example |
|---|---|---|
| Ineptitude | Safety | The only thing was that when I was getting ready to get discharged, one of Dr. H*'s associates came in and said, We have to readmit you for a further procedure. I said, Well, that's strange because Dr. H* put in a stent yesterday, and I'm supposed to leave today. Well, he checked, and he had the wrong guy. I'm glad I said something or else they probably would have hauled me off. |
| Disrespect | Treatment with respect and dignity | Transport was rude due to me being a heavy person. They were saying they didn't want to move me and snickering. |
| Prolonged waits | Prompt and efficient care | I called for someone because I had to use the bathroom really bad, but I had those things stuck to my legs and needed help walking to the bathroom but no one came. Well, I had to go so bad that I had a panic attack. Then all these people came rushing in to help. I felt so embarrassed. |
| Ineffective communication | Successful exchange of information | There were a few days that [were] a little confusing to me. I didn't know if I was going to have surgery or go home. The communication wasn't that great. |
| Lack of environmental control | Environmental autonomy and control | I was put in a room with a man who had many issues. He was loud and yelling all night. It was a very disturbing experience. |
| Substandard amenities | High‐quality amenities | In that ICU they should put a TV on the ceiling for when you're lying flat on your back looking at the ceiling tiles for 4 days. |
| Domain of Dissatisfaction | No. (N = 579 suggestionsa) | % of Total Surveyed | % Within Domain |
|---|---|---|---|
| |||
| Perceived ineptitude | 75 | 7.7 | 100 |
| Adverse events | 18 | 1.8 | 24.0 |
| Cleanliness | 36 | 3.7 | 48.0 |
| Perceived lack of knowledge/skill | 12 | 1.2 | 16.0 |
| Rushed out | 9 | 0.9 | 12.0 |
| Disrespect | 59 | 6.0 | 100 |
| Unprofessional staff behavior | 55 | 5.6 | 93.2 |
| Lack of privacy/confidentiality | 4 | 0.4 | 6.8 |
| Prolonged waits | 154 | 15.8 | 100 |
| Response to call bell | |||
| Bathing/toileting/distress | 24 | 2.5 | 15.6 |
| General | 41 | 4.2 | 26.6 |
| Wait for physician | 12 | 1.2 | 7.8 |
| Wait for admission bed | 29 | 3.0 | 18.8 |
| Wait for transport | 16 | 1.6 | 10.4 |
| Wait for food | 7 | 0.7 | 4.6 |
| Wait for medication | 11 | 1.1 | 7.1 |
| Wait for diagnostic test/procedures | 6 | 0.6 | 3.9 |
| Wait for discharge | 8 | 0.8 | 5.2 |
| Ineffective communication | 72 | 7.4 | 100 |
| Communication with patients | 33 | 3.4 | 45.8 |
| Communication with family | 3 | 0.3 | 4.2 |
| Translation | 2 | 0.2 | 2.8 |
| Communication between providers | 13 | 1.3 | 18.1 |
| Coordination of care (inpatient) | 11 | 1.1 | 15.3 |
| Medication reconciliation | 5 | 0.5 | 6.9 |
| Continuity inpatient to outpatient | 5 | 0.5 | 6.9 |
| Lack of environmental control | 152 | 15.6 | 100 |
| Physical environment | |||
| Roommates | 38 | 3.9 | 25.0 |
| Noise | 24 | 2.5 | 15.8 |
| Temperature | 12 | 1.2 | 7.9 |
| Smell | 1 | 0.1 | 0.7 |
| Interruption by staff | 15 | 1.5 | 9.9 |
| Lighting | 2 | 0.2 | 1.3 |
| Chaos/hectic | 4 | 0.4 | 2.6 |
| Shorter Stay | 8 | 0.8 | 5.3 |
| General | 3 | 0.3 | 2.0 |
| Facilities | |||
| Pain control | 10 | 1.0 | 6.6 |
| Painful procedures | 17 | 1.7 | 11.2 |
| Facilities | |||
| Bathrooms | 7 | 0.7 | 4.6 |
| Maintenance response | 5 | 0.5 | 3.3 |
| Traffic/parking | 6 | 0.6 | 3.9 |
| Substandard amenities | 67 | 6.9 | 100 |
| Food quality | 26 | 2.7 | 38.8 |
| Food variety | 5 | 0.5 | 7.5 |
| Food service | 16 | 1.6 | 23.9 |
| TV | 8 | 0.8 | 11.9 |
| Beds | 8 | 0.8 | 11.9 |
| Gowns | 4 | 0.4 | 6.0 |
Ineptitude
A total of 7.7% of interviewed patients reported experiencing a situation that made them feel unsafe. Dissatisfaction with safety included adverse events or near misses, uncleanliness, and a perceived lack of knowledge or skill. The implicit expectation that emerged from this domain was that the hospital would be safe, and that medical staff would be knowledgeable and skillful.
Adverse events or near misses were experienced in several areas, including diet, medication administration, patient identification, and equipment. Patients were particularly troubled when they or a family member caught the error:
There was one male nurse in training, C*, who was about to give my mother an injection. I asked what he was doing because she was about to go into surgery. He said he thought she was going home. He looked at the chart again and it turns out he was holding her roommate's chart. I don't know what would have happened if I wasn't there.
Dissatisfaction with the cleanliness of the hospital environment was also frequently expressed as a safety concern:
The rooms are dirtyThe floors are dirty. They don't sweep unless you ask them to. It took three different people to come and clean the bathroom right. I have to come back for surgery and I'm scared to death with all that bacteria and uncleanliness.
In this category, patients also described care by not too knowledgeable trainees or other staff as a safety hazard.
Disrespect
A total of 6.0% of surveyed patients suggested improvements that reflected disrespectful treatment, including poor work ethic, lack of warmth, rudeness, and a lack of attention to privacy and confidentiality. This type of dissatisfaction suggested an implicit expectation for treatment with respect and dignity that was clearly distinct from the expectation of technical quality:
[Hospital name] has always been like [this] since I started going there in 1982. They're very good technically but their bedside manner kind of sucks. You survive but you don't walk away with a warm fuzzy feeling.
Underprivileged patients were particularly sensitive to the need for respect:
I feel like the doctor that saw me that last night there was trying to get me out of there as fast as possible, saying not in so many words that it was because I don't have any insurance. I just feel like they treated me like an animal.
Violations of privacy and confidentiality were not only perceived as disrespectful, but also as a direct impediment to high‐quality care:
In the ER, I didn't like that I had no privacy especially talking with the doctor because I was in the hallway. I didn't have any privacy therefore I wasn't completely truthful with the doctor because everyone could hear.
Prolonged Waits
A total of 15.8% of patients noted dissatisfaction with wait times in the hospital. Waits for admission, transport, or discharge were frequently cited as anxiety‐provoking or frustrating:
The ER wait is too long. I was there from 8:00 AM to 2:00 AM the next day. I was there the whole day and night. When someone is in pain, they just want to be taken care of, not waiting around.
Waits related to receiving patient care, for example the inability to access nurses or physicians, more often caused feelings of fear and abandonment:
Every patient is different, I understand, but when you're there at night it can be a little scary. I was not only scared but in pain. The nurse tried to get a hold of the doctor that was on call, but the doctor took hours to respond. That was very scary.
It was also distressing to patients to watch roommates experience a delay in help for urgent needs:
The lady next to me was an elderly woman with a brace on her neck, and she couldn't speak very well. She had diarrhea at night and she would ask for a bedpan. The nurses would take forever bringing it to her. I just think when there are elderly people they should be more attentive to them because they tend to not be as vocal, you know?
Together, these comments represented an implicit expectation for prompt and efficient care.
Ineffective Communication
Communication during hospitalization was a source of dissatisfaction in 7.4% of surveyed patients. Communication failures occurred in several areas. Most common was the ineffective transfer of medical information to patients:
For days I thought I was having surgery on Friday. So all that day I ate and drank nothing and got prepped for surgery. Finally later that night I was told I was going to have it on Saturday. Saturday comes and still nothing. I never saw a surgeon or talked to anyone. Then later after that I was told I'm not having the surgery. That was the most frustrating thing.
Patients were also dissatisfied with their ability to communicate with their doctors:
I was sent home on a Friday and was sent right back on Friday night because my blood count was low and I ended up needing a blood transfusion. I tried to tell them this but they didn't listen. They need to listen to the patients.
Failed communication between care providers in the hospital was a third inadequacy noted by patients:
The only problem I had was all the different doctors coming in and out. There's so many that it confuses the patient, and a lot of them would contradict each other. One doctor said I could go home and another doctor said, No, you need to stay.
Finally, patients were dissatisfied when there was ineffective communication between inpatient and outpatient providers.
They said the VNA [Visiting Nurse Association] is supposed to come. The nurse hasn't come to see me and she hasn't called. My daughter and I have been waiting.
Thus, patients had an implicit expectation for effective communication between all parties in the hospital and were dissatisfied when any type of communication was inadequate.
Lack of Environmental Control
A total of 15.4% of surveyed patients reported dissatisfaction with the inability to control the physical environment. The inability to control noise levels, roommate behavior, temperature, smells, pain, lighting, staff interruptions, food service, smoking, and even humidity were all anxiety‐producing for different patients. The feeling of being imposed upon by an uncomfortable physical environment also extended to hospital facilities such as inaccessible bathrooms, traffic, and parking. Dissatisfaction with rooming arrangements was common:
I was in a triple room and one of my roommates had at least six visitors in the room at a time every day including two infant twins. Someone really should have said something about that. It became very disturbing, and I even left a day early because of that.
An expectation for quiet, especially during the night, was also repeatedly expressed:
The night shift could have been more considerate of people trying to rest. There was a lot of noise and bangs. I know people have to laugh and have fun but it could have been a little more quiet.
Related was the inability to control interruptions by staff members:
It's hard enough to get sleep, but then those blood suckers come in the middle of the night.
This category of dissatisfaction reflected an implicit expectation for autonomy and control over the environment so that it was conducive to rest and healing.
Substandard Amenities
A total of 6.9% of surveyed patients suggested improvements to amenities such as food, bedding, gowns, and television. Moving beyond the expectation of having peaceful surroundings, these comments reflected an expectation of a well‐appointed hospital environment with high‐quality amenities. A typical example was this comment about the food and service:
You never get what you order from the kitchen. Your tray either has something missing from it or it's the wrong tray or not the right diet. It's very frustrating and hard to get the orders the way you want.
Discussion
We analyzed 439 patient suggestions for improving hospital care and found that dissatisfaction resulted from six categories of negative experiences: 1) ineptitude, 2) disrespect, 3) prolonged wait times, 4) ineffective communication, 5) lack of environmental control, and 6) substandard amenities. These domains represented a corresponding set of implicit patient expectations for: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities. Each of these categories suggests avenues by which both the assessment and provision of hospital care can be made more patient‐centered.
The most widely used patient satisfaction survey in use in the United States today is the Hospital Consumer Assessment of Healthcare Providers & Systems (HCAHPS), which includes eight domains: communication with doctors, communication with nurses, responsiveness of hospital staff, pain management, communication about medicines, discharge information, cleanliness of the hospital environment, and quietness of the hospital environment.17 The dissatisfaction domains found in this study closely overlap the HCAHPS satisfaction domains, but with a few key differences.
First, dissatisfaction with ineptitude in our study encompassed concerns over adverse events and near misses, in addition to the cleanliness of the environment. Other research has shown that dissatisfaction with hospitalization can be predicted by the number of reported problems18 and the perception of receiving incorrect treatment.19 While elaborate methods have been devised to assess and compare the hospital quality and safety, patient satisfaction surveys including the HCAHPS survey often fail to ask patients directly about their perceptions of safety. In fact, this study and others20, 21 show that patients are able to recognize adverse events during hospitalization. Patient report may be a useful adjunct to other methods of adverse event case finding and outcomes reporting.
Second, while HCAHPS and others identify warmth, courtesy, concern, and respect as dimensions of patient‐centered care,14, 17, 22, 23 the ability of quantitative satisfaction surveys to capture the experience of disrespectful treatment may be limited, especially during hospitalization. Most respondents who commented on feeling disrespected identified only a single encounter, which can be masked by otherwise satisfying interactions with numerous care providers. Directly asking patients whether any experience during hospitalization caused them to feel disrespected, and allowing room for explanation, might more efficiently identify problem areas. This is particularly important because even one episode of disrespectful treatment, particularly when perceived to be racially motivated, increases the likelihood of not following a doctor's advice or putting off care.24
Third, HCAHPS emphasizes two aspects of communication: that between patients and doctors, and that between patients and nurses. Our patients confirmed that these are important, but they also noted a third dimension of communication contributing to dissatisfaction: provider‐provider communication. Communication and coordination failures among providers are key contributors to adverse events or near misses,2528 but their influence on patient satisfaction has not been widely assessed. Furthermore, patient input is rarely utilized to identify poor interprovider communication. Our study suggests that, just as patients can identify adverse events, they are also able to recognize poor provider‐provider communication.
Patients' reports of dissatisfying events also highlight areas in which small changes in hospital practice might greatly improve the patient experience. For instance, concerns over environment, food, sleep, hygiene, and pain appeared to be representative of a broader dissatisfaction with loss of autonomy and control. Hospitalized patients are often obliged to room with strangers, are subject to noise and interruptions, and cede control of their medication management at a time when they are feeling particularly vulnerable. The importance of this lack of autonomy to patients suggests a variety of small interventions that could improve satisfaction, such as individual control of noise and temperature, a visible commitment to a quiet hospital environment, and minimized interruptions and sleep disturbance.2932 Single‐occupancy hospital rooms have been associated with lower rates of nosocomial infection, medication errors, and patient stress, as well as increased privacy, rest, visitor involvement, and doctor‐patient communication.33, 34 The most sophisticated intervention, acuity‐adaptable private hospital rooms, allows hospitals to maintain patients in the same private hospital room during an entire admission, regardless of changes to level of acuity.35
In‐depth analysis of suggestions for improvement, as gathered by telephone surveys of recently discharged patients, was a particularly well‐suited approach to identifying explicit expectations for care that were violated by dissatisfying incidents. When allowed to express dissatisfaction in terms of suggestions for improvement, patients talked freely about specific dissatisfying experiences. Using telephone interviews allowed a large volume of patient responses to be included, unlike smaller focus groups. Our study was oral and did not rely on the literacy level of patients. Additionally, the open‐ended nature of questioning avoided some of the usual pitfalls of satisfaction surveys. We did not rely on predetermined satisfaction categories or presume the inherent value of particular attributes of care. Nonetheless, our study does have important limitations.
Patient perceptions were not compared with chart data or clinician report. Caregivers were allowed to participate in lieu of patients, which may have reduced identification of some dissatisfying events. Likewise, patients discharged to nursing homes or who were not English or Spanish speaking were excluded and may have had different dissatisfying experiences. Interviews were brief and dissatisfying events were not explored in detail. Although nearly half of respondents reported dissatisfying events, some patients may have been reluctant to criticize their care directly to a hospital representative. Finally, patients generally confined their comments to one or two dissatisfying events, even though there may have been others. We therefore cannot draw any conclusions about the relative frequency of dissatisfying events by domain.
Conclusions
All hospitalized patients bring expectations for their hospital experience. While specific expectations vary between patients, expectations for: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities were found in this study to encompass core expectations for hospitalization. It may be useful to ensure that postdischarge surveys explicitly address these expectations. Efforts to address and manage these core expectations of hospital care may help to reduce patient dissatisfaction with hospitalization and improve the delivery and quality of hospital care.
- ,.Multinational Comparisons of Health Systems Data, 2006.Washington, DC:The Commonwealth Fund;2007.
- ,,,,,.Toward higher‐performance health systems: Adults' health care experiences in seven countries, 2007.Health Aff.2007;26:w717–734.
- ,,, et al.Patient satisfaction and its relationship with clinical quality and inpatient mortality in acute myocardial infarction.Circ Cardiovasc Qual Outcomes.2010;3:188–195.
- ,.A longitudinal analysis of patient satisfaction and subsequent quality of life in Hong Kong Chinese breast and nasopharyngeal cancer patients.Med Care.2009;47:875–881.
- .Understanding dissatisfied users: developing a framework for comprehending criticisms of health care work.J Adv Nurs.1999;30:723–731.
- ,.Patient satisfaction: a review of issues and concepts.Soc Sci Med.1997;45:1829–1843.
- Institute of Medicine.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- .Patient satisfaction: a valid concept?Soc Sci Med.1994;38:509–516.
- .Exploring the meaning of ‘dissatisfaction’ with health care: the importance of ‘personal identity threat’.Sociol Health Illn.1999;21:95–123.
- ,.Pathways, pyramids and icebergs? Mapping the links between dissatisfaction and complaints.Sociol Health Illn.1998;20:825–847.
- ,.Convergence and divergence: assessing criteria of consumer satisfaction across general practice, dental and hospital care settings.Soc Sci Med.1991;33:707–716.
- ,,,,,.National survey of hospital patients [see comment].BMJ.1994;309:1542–1546.
- ,,, et al.The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.Health Technol Assess.2002;6:1–244.
- ,,,.Review of the literature on survey instruments used to collect data on hospital patients' perceptions of care.Health Serv Res.2005;40:1996–2017.
- ,,.Satisfying solutions? A review of some unresolved issues in the measurement of patient satisfaction.J Adv Nurs.1995;22:316–322.
- ,.The Discovery of Grounded Theory: Strategies for Qualitative Research.Chicago, IL:Aldine;1967.
- Hospital Consumer Assessment of Healthcare Providers 25:25–36.
- ,,,.Patient experiences in relation to respondent and health service delivery characteristics: a survey of 26,938 patients attending 62 hospitals throughout Norway.Scand J Public Health.2007;35:70–77.
- ,,, et al.What can hospitalized patients tell us about adverse events? Learning from patient‐reported incidents.J Gen Intern Med.2005;20:830–836.
- .A hospitalization from hell: a patient's perspective on quality.Ann Intern Med.2003;138:33–39.
- ,,,.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco, CA:Jossey‐Bass;1993.
- ,,,,.What do consumers want to know about the quality of care in hospitals?Health Serv Res.2005;40:2018–2036.
- ,.R‐e‐s‐p‐e‐c‐t: patient reports of disrespect in the health care setting and its impact on care.J Fam Pract.2004;53:721–730.
- ,,,,.Perceived information needs and communication difficulties of inpatient physicians and nurses.J Am Med Inform Assoc.2002;9(6 suppl 1):S64–S69.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13:i85–i90.
- ,,,,.Consequences of inadequate sign‐out for patient care.Arch Intern Med.2008;168:1755–1760.
- ,,,,,.Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care.Ann Emerg Med.2009;53:701–710 e704.
- ,.Interactive relationships between hospital patients' noise‐induced stress and other stress with sleep.Heart Lung.2001;30:237–243.
- .The influence of subjective reactions to noise on health effects of the noise.Environ Int.1996;22:93–104.
- .A novel PACU design for noise reduction.J Perianesth Nurs.2008;23:226–229.
- ,,,.The Planetree Model Hospital Project: an example of the patient as partner. (Pacific Presbyterian Medical Center, San Francisco).Hosp Health Serv Admin.1990;35:591–601.
- ,,.Physician‐patient communication in single‐bedded versus four‐bedded hospital rooms.Patient Educ Couns.2008;73:215–219.
- ,,.Advantages and disadvantages of single‐versus multiple‐occupancy rooms in acute care environments: a review and analysis of the literature.Environ Behav.2005;37:760–786.
- ,.Impacting patient outcomes through design: acuity adaptable care/universal room design.Crit Care Nurs Q.2006;29:326–341.
The United States spends more money per capita on healthcare than any other industrialized nation,1 yet patients are the least satisfied with their care.2 Patient satisfaction is associated in both cross‐sectional3 and longitudinal studies4 with improved physical and mental health outcomes. Conversely, dissatisfaction with care hampers future medical interactions, prevents sharing of information, and impairs the building of trust.5 The increasing recognition that a patient's experience of care affects patient outcomes has furthered efforts to evaluate satisfaction with care.6, 7
However, patient satisfaction is challenging to define and understand. Even the definition of satisfaction is ambiguous, for to satisfy can mean both to make happy and the lesser, to be adequate. To dissatisfy is to displease or disappoint, but dissatisfaction is not the opposite of satisfaction: qualitative studies give little if any indication that patients evaluate satisfaction on a continuum ranging from dissatisfied at one end to very satisfied at the other.8 Instead, it appears that satisfaction and dissatisfaction are different constructs, such that patients may simultaneously be both satisfied and dissatisfied.9, 10 Patients often express overall satisfaction with a service or encounter while also reporting specific criticisms about its shortcomings.11, 12 Alternatively, consumers may be generally satisfied unless something unpleasant or improper happens.13 Thus, dissatisfaction and satisfaction may require different methods of measurement.
The most common model for measuring patient satisfaction is a quantitative survey of patients' experiences in specific predetermined domains. Of 54 hospital satisfaction surveys in common use, only 11 included patient input in their development,14 casting doubt on the relevance of these attributes to patients' priorities of care. Since it is well recognized that patient expectations influence satisfaction,8, 13, 15 it is important to identify patient expectations and priorities up front. However, these have not been clearly established. Furthermore, focusing purely on satisfaction with particular domains of care may miss the separate but illuminating construct of patient dissatisfaction.
In this study we therefore aim to understand patient dissatisfaction with hospitalization more fully as a means of elucidating implicit expectations for hospital care. Using qualitative techniques, we analyzed a large volume of patient responses to a single open‐ended study question to identify determinants and patterns of patient dissatisfaction.
Methods
Study Design
We conducted a qualitative analysis of telephone survey data obtained from adults recently discharged after an acute care hospitalization. Survey participants were asked five questions, including: If there was one thing we could have done to improve your experience in the hospital, what would it have been? Answers to this open‐ended question were included in this study.
Setting and Participants
The hospital is a 944‐bed, urban academic medical center. Patients or patient representatives were routinely surveyed in a telephone interview conducted by trained hospital staff 1‐5 days after hospital discharge. Calls were attempted to 90% of adult discharged patients, and approximately 50% of them were reached. For this study, we included patients who were age 18 or older, spoke English, and were discharged to home from a medical, surgical, gynecology‐oncology, neurology, neurosurgery, or intensive care unit. Of those patients, we randomly selected 10% of those surveyed between July 1, 2007 and June 30, 2008 for inclusion.
Primary Data Analysis
Qualitative data analysis was used to classify patient suggestions. The study team included internal medicine physicians (J.P.M., L.I.H.), a medical student (A.V.L.), and a recent college graduate (C.P.B.). Codes were generated using a mixed inductive and deductive approach by reading and rereading the primary data.16 A set of 100 interview responses were first read individually by three investigators (J.P.M., A.V.L., C.P.B.), after which investigators met to discuss themes and ideas. A preliminary list of coding categories was then generated. Each investigator then assigned these coding categories to additional survey responses in sets of 100. Subsequent meetings were held to refine codes using the constant comparative method.16 Disagreements were resolved by negotiated consensus. The full study group met periodically to review the code structure for logic and breadth. Once thematic saturation was achieved, the entire dataset was recoded by two investigators using the final coding structure. The final coding structure contained 42 unique codes organized into six broader themes. We used descriptive statistics to characterize the coding category results. The score for intercoder reliability was 0.91.
This study was approved by the Yale Human Investigation Committee, which granted a waiver of informed consent.
Results
A total of 976 surveys was randomly selected from 9,764 postdischarge phone interviews completed between July 1, 2007 and June 30, 2008. A total of 56.3% of patients was female. Nearly half the patients were discharged from medical units (Table 1). Of the 976 patients, 439 (45.0%) gave at least one suggestion for improvement, yielding a total of 579 suggestions. Patients also offered numerous positive comments about their care, but these comments were not included in the analysis.
| No. | % of Total Surveyed | |
|---|---|---|
| Total surveys | 976 | |
| Male | 427 | 43.7 |
| Female | 549 | 56.3 |
| Discharge Unit | ||
| Medical | 434 | 44.5 |
| Surgical | 303 | 31.0 |
| Gynecology/Oncology | 103 | 10.6 |
| ICU/CCU/Step‐down | 71 | 7.3 |
| Neurology/Neurosurgery | 65 | 6.6 |
| No suggestions for improvement | 537 | 55.0 |
| At least one suggestion for improvement | 439 | 45.0 |
Through qualitative analysis, we assigned suggestions for improvement to six major categories of dissatisfaction: 1) ineptitude, 2) disrespect, 3) prolonged waits, 4) ineffective communication, 5) lack of environmental control, and 6) substandard amenities. We considered the inverse of these problems to represent six implicit expectations of good hospital care: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities (Table 2). The number of patient suggestions related to each domain is detailed in Table 3.
| Domain of Dissatisfaction | Implicit Expectations | Example |
|---|---|---|
| Ineptitude | Safety | The only thing was that when I was getting ready to get discharged, one of Dr. H*'s associates came in and said, We have to readmit you for a further procedure. I said, Well, that's strange because Dr. H* put in a stent yesterday, and I'm supposed to leave today. Well, he checked, and he had the wrong guy. I'm glad I said something or else they probably would have hauled me off. |
| Disrespect | Treatment with respect and dignity | Transport was rude due to me being a heavy person. They were saying they didn't want to move me and snickering. |
| Prolonged waits | Prompt and efficient care | I called for someone because I had to use the bathroom really bad, but I had those things stuck to my legs and needed help walking to the bathroom but no one came. Well, I had to go so bad that I had a panic attack. Then all these people came rushing in to help. I felt so embarrassed. |
| Ineffective communication | Successful exchange of information | There were a few days that [were] a little confusing to me. I didn't know if I was going to have surgery or go home. The communication wasn't that great. |
| Lack of environmental control | Environmental autonomy and control | I was put in a room with a man who had many issues. He was loud and yelling all night. It was a very disturbing experience. |
| Substandard amenities | High‐quality amenities | In that ICU they should put a TV on the ceiling for when you're lying flat on your back looking at the ceiling tiles for 4 days. |
| Domain of Dissatisfaction | No. (N = 579 suggestionsa) | % of Total Surveyed | % Within Domain |
|---|---|---|---|
| |||
| Perceived ineptitude | 75 | 7.7 | 100 |
| Adverse events | 18 | 1.8 | 24.0 |
| Cleanliness | 36 | 3.7 | 48.0 |
| Perceived lack of knowledge/skill | 12 | 1.2 | 16.0 |
| Rushed out | 9 | 0.9 | 12.0 |
| Disrespect | 59 | 6.0 | 100 |
| Unprofessional staff behavior | 55 | 5.6 | 93.2 |
| Lack of privacy/confidentiality | 4 | 0.4 | 6.8 |
| Prolonged waits | 154 | 15.8 | 100 |
| Response to call bell | |||
| Bathing/toileting/distress | 24 | 2.5 | 15.6 |
| General | 41 | 4.2 | 26.6 |
| Wait for physician | 12 | 1.2 | 7.8 |
| Wait for admission bed | 29 | 3.0 | 18.8 |
| Wait for transport | 16 | 1.6 | 10.4 |
| Wait for food | 7 | 0.7 | 4.6 |
| Wait for medication | 11 | 1.1 | 7.1 |
| Wait for diagnostic test/procedures | 6 | 0.6 | 3.9 |
| Wait for discharge | 8 | 0.8 | 5.2 |
| Ineffective communication | 72 | 7.4 | 100 |
| Communication with patients | 33 | 3.4 | 45.8 |
| Communication with family | 3 | 0.3 | 4.2 |
| Translation | 2 | 0.2 | 2.8 |
| Communication between providers | 13 | 1.3 | 18.1 |
| Coordination of care (inpatient) | 11 | 1.1 | 15.3 |
| Medication reconciliation | 5 | 0.5 | 6.9 |
| Continuity inpatient to outpatient | 5 | 0.5 | 6.9 |
| Lack of environmental control | 152 | 15.6 | 100 |
| Physical environment | |||
| Roommates | 38 | 3.9 | 25.0 |
| Noise | 24 | 2.5 | 15.8 |
| Temperature | 12 | 1.2 | 7.9 |
| Smell | 1 | 0.1 | 0.7 |
| Interruption by staff | 15 | 1.5 | 9.9 |
| Lighting | 2 | 0.2 | 1.3 |
| Chaos/hectic | 4 | 0.4 | 2.6 |
| Shorter Stay | 8 | 0.8 | 5.3 |
| General | 3 | 0.3 | 2.0 |
| Facilities | |||
| Pain control | 10 | 1.0 | 6.6 |
| Painful procedures | 17 | 1.7 | 11.2 |
| Facilities | |||
| Bathrooms | 7 | 0.7 | 4.6 |
| Maintenance response | 5 | 0.5 | 3.3 |
| Traffic/parking | 6 | 0.6 | 3.9 |
| Substandard amenities | 67 | 6.9 | 100 |
| Food quality | 26 | 2.7 | 38.8 |
| Food variety | 5 | 0.5 | 7.5 |
| Food service | 16 | 1.6 | 23.9 |
| TV | 8 | 0.8 | 11.9 |
| Beds | 8 | 0.8 | 11.9 |
| Gowns | 4 | 0.4 | 6.0 |
Ineptitude
A total of 7.7% of interviewed patients reported experiencing a situation that made them feel unsafe. Dissatisfaction with safety included adverse events or near misses, uncleanliness, and a perceived lack of knowledge or skill. The implicit expectation that emerged from this domain was that the hospital would be safe, and that medical staff would be knowledgeable and skillful.
Adverse events or near misses were experienced in several areas, including diet, medication administration, patient identification, and equipment. Patients were particularly troubled when they or a family member caught the error:
There was one male nurse in training, C*, who was about to give my mother an injection. I asked what he was doing because she was about to go into surgery. He said he thought she was going home. He looked at the chart again and it turns out he was holding her roommate's chart. I don't know what would have happened if I wasn't there.
Dissatisfaction with the cleanliness of the hospital environment was also frequently expressed as a safety concern:
The rooms are dirtyThe floors are dirty. They don't sweep unless you ask them to. It took three different people to come and clean the bathroom right. I have to come back for surgery and I'm scared to death with all that bacteria and uncleanliness.
In this category, patients also described care by not too knowledgeable trainees or other staff as a safety hazard.
Disrespect
A total of 6.0% of surveyed patients suggested improvements that reflected disrespectful treatment, including poor work ethic, lack of warmth, rudeness, and a lack of attention to privacy and confidentiality. This type of dissatisfaction suggested an implicit expectation for treatment with respect and dignity that was clearly distinct from the expectation of technical quality:
[Hospital name] has always been like [this] since I started going there in 1982. They're very good technically but their bedside manner kind of sucks. You survive but you don't walk away with a warm fuzzy feeling.
Underprivileged patients were particularly sensitive to the need for respect:
I feel like the doctor that saw me that last night there was trying to get me out of there as fast as possible, saying not in so many words that it was because I don't have any insurance. I just feel like they treated me like an animal.
Violations of privacy and confidentiality were not only perceived as disrespectful, but also as a direct impediment to high‐quality care:
In the ER, I didn't like that I had no privacy especially talking with the doctor because I was in the hallway. I didn't have any privacy therefore I wasn't completely truthful with the doctor because everyone could hear.
Prolonged Waits
A total of 15.8% of patients noted dissatisfaction with wait times in the hospital. Waits for admission, transport, or discharge were frequently cited as anxiety‐provoking or frustrating:
The ER wait is too long. I was there from 8:00 AM to 2:00 AM the next day. I was there the whole day and night. When someone is in pain, they just want to be taken care of, not waiting around.
Waits related to receiving patient care, for example the inability to access nurses or physicians, more often caused feelings of fear and abandonment:
Every patient is different, I understand, but when you're there at night it can be a little scary. I was not only scared but in pain. The nurse tried to get a hold of the doctor that was on call, but the doctor took hours to respond. That was very scary.
It was also distressing to patients to watch roommates experience a delay in help for urgent needs:
The lady next to me was an elderly woman with a brace on her neck, and she couldn't speak very well. She had diarrhea at night and she would ask for a bedpan. The nurses would take forever bringing it to her. I just think when there are elderly people they should be more attentive to them because they tend to not be as vocal, you know?
Together, these comments represented an implicit expectation for prompt and efficient care.
Ineffective Communication
Communication during hospitalization was a source of dissatisfaction in 7.4% of surveyed patients. Communication failures occurred in several areas. Most common was the ineffective transfer of medical information to patients:
For days I thought I was having surgery on Friday. So all that day I ate and drank nothing and got prepped for surgery. Finally later that night I was told I was going to have it on Saturday. Saturday comes and still nothing. I never saw a surgeon or talked to anyone. Then later after that I was told I'm not having the surgery. That was the most frustrating thing.
Patients were also dissatisfied with their ability to communicate with their doctors:
I was sent home on a Friday and was sent right back on Friday night because my blood count was low and I ended up needing a blood transfusion. I tried to tell them this but they didn't listen. They need to listen to the patients.
Failed communication between care providers in the hospital was a third inadequacy noted by patients:
The only problem I had was all the different doctors coming in and out. There's so many that it confuses the patient, and a lot of them would contradict each other. One doctor said I could go home and another doctor said, No, you need to stay.
Finally, patients were dissatisfied when there was ineffective communication between inpatient and outpatient providers.
They said the VNA [Visiting Nurse Association] is supposed to come. The nurse hasn't come to see me and she hasn't called. My daughter and I have been waiting.
Thus, patients had an implicit expectation for effective communication between all parties in the hospital and were dissatisfied when any type of communication was inadequate.
Lack of Environmental Control
A total of 15.4% of surveyed patients reported dissatisfaction with the inability to control the physical environment. The inability to control noise levels, roommate behavior, temperature, smells, pain, lighting, staff interruptions, food service, smoking, and even humidity were all anxiety‐producing for different patients. The feeling of being imposed upon by an uncomfortable physical environment also extended to hospital facilities such as inaccessible bathrooms, traffic, and parking. Dissatisfaction with rooming arrangements was common:
I was in a triple room and one of my roommates had at least six visitors in the room at a time every day including two infant twins. Someone really should have said something about that. It became very disturbing, and I even left a day early because of that.
An expectation for quiet, especially during the night, was also repeatedly expressed:
The night shift could have been more considerate of people trying to rest. There was a lot of noise and bangs. I know people have to laugh and have fun but it could have been a little more quiet.
Related was the inability to control interruptions by staff members:
It's hard enough to get sleep, but then those blood suckers come in the middle of the night.
This category of dissatisfaction reflected an implicit expectation for autonomy and control over the environment so that it was conducive to rest and healing.
Substandard Amenities
A total of 6.9% of surveyed patients suggested improvements to amenities such as food, bedding, gowns, and television. Moving beyond the expectation of having peaceful surroundings, these comments reflected an expectation of a well‐appointed hospital environment with high‐quality amenities. A typical example was this comment about the food and service:
You never get what you order from the kitchen. Your tray either has something missing from it or it's the wrong tray or not the right diet. It's very frustrating and hard to get the orders the way you want.
Discussion
We analyzed 439 patient suggestions for improving hospital care and found that dissatisfaction resulted from six categories of negative experiences: 1) ineptitude, 2) disrespect, 3) prolonged wait times, 4) ineffective communication, 5) lack of environmental control, and 6) substandard amenities. These domains represented a corresponding set of implicit patient expectations for: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities. Each of these categories suggests avenues by which both the assessment and provision of hospital care can be made more patient‐centered.
The most widely used patient satisfaction survey in use in the United States today is the Hospital Consumer Assessment of Healthcare Providers & Systems (HCAHPS), which includes eight domains: communication with doctors, communication with nurses, responsiveness of hospital staff, pain management, communication about medicines, discharge information, cleanliness of the hospital environment, and quietness of the hospital environment.17 The dissatisfaction domains found in this study closely overlap the HCAHPS satisfaction domains, but with a few key differences.
First, dissatisfaction with ineptitude in our study encompassed concerns over adverse events and near misses, in addition to the cleanliness of the environment. Other research has shown that dissatisfaction with hospitalization can be predicted by the number of reported problems18 and the perception of receiving incorrect treatment.19 While elaborate methods have been devised to assess and compare the hospital quality and safety, patient satisfaction surveys including the HCAHPS survey often fail to ask patients directly about their perceptions of safety. In fact, this study and others20, 21 show that patients are able to recognize adverse events during hospitalization. Patient report may be a useful adjunct to other methods of adverse event case finding and outcomes reporting.
Second, while HCAHPS and others identify warmth, courtesy, concern, and respect as dimensions of patient‐centered care,14, 17, 22, 23 the ability of quantitative satisfaction surveys to capture the experience of disrespectful treatment may be limited, especially during hospitalization. Most respondents who commented on feeling disrespected identified only a single encounter, which can be masked by otherwise satisfying interactions with numerous care providers. Directly asking patients whether any experience during hospitalization caused them to feel disrespected, and allowing room for explanation, might more efficiently identify problem areas. This is particularly important because even one episode of disrespectful treatment, particularly when perceived to be racially motivated, increases the likelihood of not following a doctor's advice or putting off care.24
Third, HCAHPS emphasizes two aspects of communication: that between patients and doctors, and that between patients and nurses. Our patients confirmed that these are important, but they also noted a third dimension of communication contributing to dissatisfaction: provider‐provider communication. Communication and coordination failures among providers are key contributors to adverse events or near misses,2528 but their influence on patient satisfaction has not been widely assessed. Furthermore, patient input is rarely utilized to identify poor interprovider communication. Our study suggests that, just as patients can identify adverse events, they are also able to recognize poor provider‐provider communication.
Patients' reports of dissatisfying events also highlight areas in which small changes in hospital practice might greatly improve the patient experience. For instance, concerns over environment, food, sleep, hygiene, and pain appeared to be representative of a broader dissatisfaction with loss of autonomy and control. Hospitalized patients are often obliged to room with strangers, are subject to noise and interruptions, and cede control of their medication management at a time when they are feeling particularly vulnerable. The importance of this lack of autonomy to patients suggests a variety of small interventions that could improve satisfaction, such as individual control of noise and temperature, a visible commitment to a quiet hospital environment, and minimized interruptions and sleep disturbance.2932 Single‐occupancy hospital rooms have been associated with lower rates of nosocomial infection, medication errors, and patient stress, as well as increased privacy, rest, visitor involvement, and doctor‐patient communication.33, 34 The most sophisticated intervention, acuity‐adaptable private hospital rooms, allows hospitals to maintain patients in the same private hospital room during an entire admission, regardless of changes to level of acuity.35
In‐depth analysis of suggestions for improvement, as gathered by telephone surveys of recently discharged patients, was a particularly well‐suited approach to identifying explicit expectations for care that were violated by dissatisfying incidents. When allowed to express dissatisfaction in terms of suggestions for improvement, patients talked freely about specific dissatisfying experiences. Using telephone interviews allowed a large volume of patient responses to be included, unlike smaller focus groups. Our study was oral and did not rely on the literacy level of patients. Additionally, the open‐ended nature of questioning avoided some of the usual pitfalls of satisfaction surveys. We did not rely on predetermined satisfaction categories or presume the inherent value of particular attributes of care. Nonetheless, our study does have important limitations.
Patient perceptions were not compared with chart data or clinician report. Caregivers were allowed to participate in lieu of patients, which may have reduced identification of some dissatisfying events. Likewise, patients discharged to nursing homes or who were not English or Spanish speaking were excluded and may have had different dissatisfying experiences. Interviews were brief and dissatisfying events were not explored in detail. Although nearly half of respondents reported dissatisfying events, some patients may have been reluctant to criticize their care directly to a hospital representative. Finally, patients generally confined their comments to one or two dissatisfying events, even though there may have been others. We therefore cannot draw any conclusions about the relative frequency of dissatisfying events by domain.
Conclusions
All hospitalized patients bring expectations for their hospital experience. While specific expectations vary between patients, expectations for: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities were found in this study to encompass core expectations for hospitalization. It may be useful to ensure that postdischarge surveys explicitly address these expectations. Efforts to address and manage these core expectations of hospital care may help to reduce patient dissatisfaction with hospitalization and improve the delivery and quality of hospital care.
The United States spends more money per capita on healthcare than any other industrialized nation,1 yet patients are the least satisfied with their care.2 Patient satisfaction is associated in both cross‐sectional3 and longitudinal studies4 with improved physical and mental health outcomes. Conversely, dissatisfaction with care hampers future medical interactions, prevents sharing of information, and impairs the building of trust.5 The increasing recognition that a patient's experience of care affects patient outcomes has furthered efforts to evaluate satisfaction with care.6, 7
However, patient satisfaction is challenging to define and understand. Even the definition of satisfaction is ambiguous, for to satisfy can mean both to make happy and the lesser, to be adequate. To dissatisfy is to displease or disappoint, but dissatisfaction is not the opposite of satisfaction: qualitative studies give little if any indication that patients evaluate satisfaction on a continuum ranging from dissatisfied at one end to very satisfied at the other.8 Instead, it appears that satisfaction and dissatisfaction are different constructs, such that patients may simultaneously be both satisfied and dissatisfied.9, 10 Patients often express overall satisfaction with a service or encounter while also reporting specific criticisms about its shortcomings.11, 12 Alternatively, consumers may be generally satisfied unless something unpleasant or improper happens.13 Thus, dissatisfaction and satisfaction may require different methods of measurement.
The most common model for measuring patient satisfaction is a quantitative survey of patients' experiences in specific predetermined domains. Of 54 hospital satisfaction surveys in common use, only 11 included patient input in their development,14 casting doubt on the relevance of these attributes to patients' priorities of care. Since it is well recognized that patient expectations influence satisfaction,8, 13, 15 it is important to identify patient expectations and priorities up front. However, these have not been clearly established. Furthermore, focusing purely on satisfaction with particular domains of care may miss the separate but illuminating construct of patient dissatisfaction.
In this study we therefore aim to understand patient dissatisfaction with hospitalization more fully as a means of elucidating implicit expectations for hospital care. Using qualitative techniques, we analyzed a large volume of patient responses to a single open‐ended study question to identify determinants and patterns of patient dissatisfaction.
Methods
Study Design
We conducted a qualitative analysis of telephone survey data obtained from adults recently discharged after an acute care hospitalization. Survey participants were asked five questions, including: If there was one thing we could have done to improve your experience in the hospital, what would it have been? Answers to this open‐ended question were included in this study.
Setting and Participants
The hospital is a 944‐bed, urban academic medical center. Patients or patient representatives were routinely surveyed in a telephone interview conducted by trained hospital staff 1‐5 days after hospital discharge. Calls were attempted to 90% of adult discharged patients, and approximately 50% of them were reached. For this study, we included patients who were age 18 or older, spoke English, and were discharged to home from a medical, surgical, gynecology‐oncology, neurology, neurosurgery, or intensive care unit. Of those patients, we randomly selected 10% of those surveyed between July 1, 2007 and June 30, 2008 for inclusion.
Primary Data Analysis
Qualitative data analysis was used to classify patient suggestions. The study team included internal medicine physicians (J.P.M., L.I.H.), a medical student (A.V.L.), and a recent college graduate (C.P.B.). Codes were generated using a mixed inductive and deductive approach by reading and rereading the primary data.16 A set of 100 interview responses were first read individually by three investigators (J.P.M., A.V.L., C.P.B.), after which investigators met to discuss themes and ideas. A preliminary list of coding categories was then generated. Each investigator then assigned these coding categories to additional survey responses in sets of 100. Subsequent meetings were held to refine codes using the constant comparative method.16 Disagreements were resolved by negotiated consensus. The full study group met periodically to review the code structure for logic and breadth. Once thematic saturation was achieved, the entire dataset was recoded by two investigators using the final coding structure. The final coding structure contained 42 unique codes organized into six broader themes. We used descriptive statistics to characterize the coding category results. The score for intercoder reliability was 0.91.
This study was approved by the Yale Human Investigation Committee, which granted a waiver of informed consent.
Results
A total of 976 surveys was randomly selected from 9,764 postdischarge phone interviews completed between July 1, 2007 and June 30, 2008. A total of 56.3% of patients was female. Nearly half the patients were discharged from medical units (Table 1). Of the 976 patients, 439 (45.0%) gave at least one suggestion for improvement, yielding a total of 579 suggestions. Patients also offered numerous positive comments about their care, but these comments were not included in the analysis.
| No. | % of Total Surveyed | |
|---|---|---|
| Total surveys | 976 | |
| Male | 427 | 43.7 |
| Female | 549 | 56.3 |
| Discharge Unit | ||
| Medical | 434 | 44.5 |
| Surgical | 303 | 31.0 |
| Gynecology/Oncology | 103 | 10.6 |
| ICU/CCU/Step‐down | 71 | 7.3 |
| Neurology/Neurosurgery | 65 | 6.6 |
| No suggestions for improvement | 537 | 55.0 |
| At least one suggestion for improvement | 439 | 45.0 |
Through qualitative analysis, we assigned suggestions for improvement to six major categories of dissatisfaction: 1) ineptitude, 2) disrespect, 3) prolonged waits, 4) ineffective communication, 5) lack of environmental control, and 6) substandard amenities. We considered the inverse of these problems to represent six implicit expectations of good hospital care: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities (Table 2). The number of patient suggestions related to each domain is detailed in Table 3.
| Domain of Dissatisfaction | Implicit Expectations | Example |
|---|---|---|
| Ineptitude | Safety | The only thing was that when I was getting ready to get discharged, one of Dr. H*'s associates came in and said, We have to readmit you for a further procedure. I said, Well, that's strange because Dr. H* put in a stent yesterday, and I'm supposed to leave today. Well, he checked, and he had the wrong guy. I'm glad I said something or else they probably would have hauled me off. |
| Disrespect | Treatment with respect and dignity | Transport was rude due to me being a heavy person. They were saying they didn't want to move me and snickering. |
| Prolonged waits | Prompt and efficient care | I called for someone because I had to use the bathroom really bad, but I had those things stuck to my legs and needed help walking to the bathroom but no one came. Well, I had to go so bad that I had a panic attack. Then all these people came rushing in to help. I felt so embarrassed. |
| Ineffective communication | Successful exchange of information | There were a few days that [were] a little confusing to me. I didn't know if I was going to have surgery or go home. The communication wasn't that great. |
| Lack of environmental control | Environmental autonomy and control | I was put in a room with a man who had many issues. He was loud and yelling all night. It was a very disturbing experience. |
| Substandard amenities | High‐quality amenities | In that ICU they should put a TV on the ceiling for when you're lying flat on your back looking at the ceiling tiles for 4 days. |
| Domain of Dissatisfaction | No. (N = 579 suggestionsa) | % of Total Surveyed | % Within Domain |
|---|---|---|---|
| |||
| Perceived ineptitude | 75 | 7.7 | 100 |
| Adverse events | 18 | 1.8 | 24.0 |
| Cleanliness | 36 | 3.7 | 48.0 |
| Perceived lack of knowledge/skill | 12 | 1.2 | 16.0 |
| Rushed out | 9 | 0.9 | 12.0 |
| Disrespect | 59 | 6.0 | 100 |
| Unprofessional staff behavior | 55 | 5.6 | 93.2 |
| Lack of privacy/confidentiality | 4 | 0.4 | 6.8 |
| Prolonged waits | 154 | 15.8 | 100 |
| Response to call bell | |||
| Bathing/toileting/distress | 24 | 2.5 | 15.6 |
| General | 41 | 4.2 | 26.6 |
| Wait for physician | 12 | 1.2 | 7.8 |
| Wait for admission bed | 29 | 3.0 | 18.8 |
| Wait for transport | 16 | 1.6 | 10.4 |
| Wait for food | 7 | 0.7 | 4.6 |
| Wait for medication | 11 | 1.1 | 7.1 |
| Wait for diagnostic test/procedures | 6 | 0.6 | 3.9 |
| Wait for discharge | 8 | 0.8 | 5.2 |
| Ineffective communication | 72 | 7.4 | 100 |
| Communication with patients | 33 | 3.4 | 45.8 |
| Communication with family | 3 | 0.3 | 4.2 |
| Translation | 2 | 0.2 | 2.8 |
| Communication between providers | 13 | 1.3 | 18.1 |
| Coordination of care (inpatient) | 11 | 1.1 | 15.3 |
| Medication reconciliation | 5 | 0.5 | 6.9 |
| Continuity inpatient to outpatient | 5 | 0.5 | 6.9 |
| Lack of environmental control | 152 | 15.6 | 100 |
| Physical environment | |||
| Roommates | 38 | 3.9 | 25.0 |
| Noise | 24 | 2.5 | 15.8 |
| Temperature | 12 | 1.2 | 7.9 |
| Smell | 1 | 0.1 | 0.7 |
| Interruption by staff | 15 | 1.5 | 9.9 |
| Lighting | 2 | 0.2 | 1.3 |
| Chaos/hectic | 4 | 0.4 | 2.6 |
| Shorter Stay | 8 | 0.8 | 5.3 |
| General | 3 | 0.3 | 2.0 |
| Facilities | |||
| Pain control | 10 | 1.0 | 6.6 |
| Painful procedures | 17 | 1.7 | 11.2 |
| Facilities | |||
| Bathrooms | 7 | 0.7 | 4.6 |
| Maintenance response | 5 | 0.5 | 3.3 |
| Traffic/parking | 6 | 0.6 | 3.9 |
| Substandard amenities | 67 | 6.9 | 100 |
| Food quality | 26 | 2.7 | 38.8 |
| Food variety | 5 | 0.5 | 7.5 |
| Food service | 16 | 1.6 | 23.9 |
| TV | 8 | 0.8 | 11.9 |
| Beds | 8 | 0.8 | 11.9 |
| Gowns | 4 | 0.4 | 6.0 |
Ineptitude
A total of 7.7% of interviewed patients reported experiencing a situation that made them feel unsafe. Dissatisfaction with safety included adverse events or near misses, uncleanliness, and a perceived lack of knowledge or skill. The implicit expectation that emerged from this domain was that the hospital would be safe, and that medical staff would be knowledgeable and skillful.
Adverse events or near misses were experienced in several areas, including diet, medication administration, patient identification, and equipment. Patients were particularly troubled when they or a family member caught the error:
There was one male nurse in training, C*, who was about to give my mother an injection. I asked what he was doing because she was about to go into surgery. He said he thought she was going home. He looked at the chart again and it turns out he was holding her roommate's chart. I don't know what would have happened if I wasn't there.
Dissatisfaction with the cleanliness of the hospital environment was also frequently expressed as a safety concern:
The rooms are dirtyThe floors are dirty. They don't sweep unless you ask them to. It took three different people to come and clean the bathroom right. I have to come back for surgery and I'm scared to death with all that bacteria and uncleanliness.
In this category, patients also described care by not too knowledgeable trainees or other staff as a safety hazard.
Disrespect
A total of 6.0% of surveyed patients suggested improvements that reflected disrespectful treatment, including poor work ethic, lack of warmth, rudeness, and a lack of attention to privacy and confidentiality. This type of dissatisfaction suggested an implicit expectation for treatment with respect and dignity that was clearly distinct from the expectation of technical quality:
[Hospital name] has always been like [this] since I started going there in 1982. They're very good technically but their bedside manner kind of sucks. You survive but you don't walk away with a warm fuzzy feeling.
Underprivileged patients were particularly sensitive to the need for respect:
I feel like the doctor that saw me that last night there was trying to get me out of there as fast as possible, saying not in so many words that it was because I don't have any insurance. I just feel like they treated me like an animal.
Violations of privacy and confidentiality were not only perceived as disrespectful, but also as a direct impediment to high‐quality care:
In the ER, I didn't like that I had no privacy especially talking with the doctor because I was in the hallway. I didn't have any privacy therefore I wasn't completely truthful with the doctor because everyone could hear.
Prolonged Waits
A total of 15.8% of patients noted dissatisfaction with wait times in the hospital. Waits for admission, transport, or discharge were frequently cited as anxiety‐provoking or frustrating:
The ER wait is too long. I was there from 8:00 AM to 2:00 AM the next day. I was there the whole day and night. When someone is in pain, they just want to be taken care of, not waiting around.
Waits related to receiving patient care, for example the inability to access nurses or physicians, more often caused feelings of fear and abandonment:
Every patient is different, I understand, but when you're there at night it can be a little scary. I was not only scared but in pain. The nurse tried to get a hold of the doctor that was on call, but the doctor took hours to respond. That was very scary.
It was also distressing to patients to watch roommates experience a delay in help for urgent needs:
The lady next to me was an elderly woman with a brace on her neck, and she couldn't speak very well. She had diarrhea at night and she would ask for a bedpan. The nurses would take forever bringing it to her. I just think when there are elderly people they should be more attentive to them because they tend to not be as vocal, you know?
Together, these comments represented an implicit expectation for prompt and efficient care.
Ineffective Communication
Communication during hospitalization was a source of dissatisfaction in 7.4% of surveyed patients. Communication failures occurred in several areas. Most common was the ineffective transfer of medical information to patients:
For days I thought I was having surgery on Friday. So all that day I ate and drank nothing and got prepped for surgery. Finally later that night I was told I was going to have it on Saturday. Saturday comes and still nothing. I never saw a surgeon or talked to anyone. Then later after that I was told I'm not having the surgery. That was the most frustrating thing.
Patients were also dissatisfied with their ability to communicate with their doctors:
I was sent home on a Friday and was sent right back on Friday night because my blood count was low and I ended up needing a blood transfusion. I tried to tell them this but they didn't listen. They need to listen to the patients.
Failed communication between care providers in the hospital was a third inadequacy noted by patients:
The only problem I had was all the different doctors coming in and out. There's so many that it confuses the patient, and a lot of them would contradict each other. One doctor said I could go home and another doctor said, No, you need to stay.
Finally, patients were dissatisfied when there was ineffective communication between inpatient and outpatient providers.
They said the VNA [Visiting Nurse Association] is supposed to come. The nurse hasn't come to see me and she hasn't called. My daughter and I have been waiting.
Thus, patients had an implicit expectation for effective communication between all parties in the hospital and were dissatisfied when any type of communication was inadequate.
Lack of Environmental Control
A total of 15.4% of surveyed patients reported dissatisfaction with the inability to control the physical environment. The inability to control noise levels, roommate behavior, temperature, smells, pain, lighting, staff interruptions, food service, smoking, and even humidity were all anxiety‐producing for different patients. The feeling of being imposed upon by an uncomfortable physical environment also extended to hospital facilities such as inaccessible bathrooms, traffic, and parking. Dissatisfaction with rooming arrangements was common:
I was in a triple room and one of my roommates had at least six visitors in the room at a time every day including two infant twins. Someone really should have said something about that. It became very disturbing, and I even left a day early because of that.
An expectation for quiet, especially during the night, was also repeatedly expressed:
The night shift could have been more considerate of people trying to rest. There was a lot of noise and bangs. I know people have to laugh and have fun but it could have been a little more quiet.
Related was the inability to control interruptions by staff members:
It's hard enough to get sleep, but then those blood suckers come in the middle of the night.
This category of dissatisfaction reflected an implicit expectation for autonomy and control over the environment so that it was conducive to rest and healing.
Substandard Amenities
A total of 6.9% of surveyed patients suggested improvements to amenities such as food, bedding, gowns, and television. Moving beyond the expectation of having peaceful surroundings, these comments reflected an expectation of a well‐appointed hospital environment with high‐quality amenities. A typical example was this comment about the food and service:
You never get what you order from the kitchen. Your tray either has something missing from it or it's the wrong tray or not the right diet. It's very frustrating and hard to get the orders the way you want.
Discussion
We analyzed 439 patient suggestions for improving hospital care and found that dissatisfaction resulted from six categories of negative experiences: 1) ineptitude, 2) disrespect, 3) prolonged wait times, 4) ineffective communication, 5) lack of environmental control, and 6) substandard amenities. These domains represented a corresponding set of implicit patient expectations for: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities. Each of these categories suggests avenues by which both the assessment and provision of hospital care can be made more patient‐centered.
The most widely used patient satisfaction survey in use in the United States today is the Hospital Consumer Assessment of Healthcare Providers & Systems (HCAHPS), which includes eight domains: communication with doctors, communication with nurses, responsiveness of hospital staff, pain management, communication about medicines, discharge information, cleanliness of the hospital environment, and quietness of the hospital environment.17 The dissatisfaction domains found in this study closely overlap the HCAHPS satisfaction domains, but with a few key differences.
First, dissatisfaction with ineptitude in our study encompassed concerns over adverse events and near misses, in addition to the cleanliness of the environment. Other research has shown that dissatisfaction with hospitalization can be predicted by the number of reported problems18 and the perception of receiving incorrect treatment.19 While elaborate methods have been devised to assess and compare the hospital quality and safety, patient satisfaction surveys including the HCAHPS survey often fail to ask patients directly about their perceptions of safety. In fact, this study and others20, 21 show that patients are able to recognize adverse events during hospitalization. Patient report may be a useful adjunct to other methods of adverse event case finding and outcomes reporting.
Second, while HCAHPS and others identify warmth, courtesy, concern, and respect as dimensions of patient‐centered care,14, 17, 22, 23 the ability of quantitative satisfaction surveys to capture the experience of disrespectful treatment may be limited, especially during hospitalization. Most respondents who commented on feeling disrespected identified only a single encounter, which can be masked by otherwise satisfying interactions with numerous care providers. Directly asking patients whether any experience during hospitalization caused them to feel disrespected, and allowing room for explanation, might more efficiently identify problem areas. This is particularly important because even one episode of disrespectful treatment, particularly when perceived to be racially motivated, increases the likelihood of not following a doctor's advice or putting off care.24
Third, HCAHPS emphasizes two aspects of communication: that between patients and doctors, and that between patients and nurses. Our patients confirmed that these are important, but they also noted a third dimension of communication contributing to dissatisfaction: provider‐provider communication. Communication and coordination failures among providers are key contributors to adverse events or near misses,2528 but their influence on patient satisfaction has not been widely assessed. Furthermore, patient input is rarely utilized to identify poor interprovider communication. Our study suggests that, just as patients can identify adverse events, they are also able to recognize poor provider‐provider communication.
Patients' reports of dissatisfying events also highlight areas in which small changes in hospital practice might greatly improve the patient experience. For instance, concerns over environment, food, sleep, hygiene, and pain appeared to be representative of a broader dissatisfaction with loss of autonomy and control. Hospitalized patients are often obliged to room with strangers, are subject to noise and interruptions, and cede control of their medication management at a time when they are feeling particularly vulnerable. The importance of this lack of autonomy to patients suggests a variety of small interventions that could improve satisfaction, such as individual control of noise and temperature, a visible commitment to a quiet hospital environment, and minimized interruptions and sleep disturbance.2932 Single‐occupancy hospital rooms have been associated with lower rates of nosocomial infection, medication errors, and patient stress, as well as increased privacy, rest, visitor involvement, and doctor‐patient communication.33, 34 The most sophisticated intervention, acuity‐adaptable private hospital rooms, allows hospitals to maintain patients in the same private hospital room during an entire admission, regardless of changes to level of acuity.35
In‐depth analysis of suggestions for improvement, as gathered by telephone surveys of recently discharged patients, was a particularly well‐suited approach to identifying explicit expectations for care that were violated by dissatisfying incidents. When allowed to express dissatisfaction in terms of suggestions for improvement, patients talked freely about specific dissatisfying experiences. Using telephone interviews allowed a large volume of patient responses to be included, unlike smaller focus groups. Our study was oral and did not rely on the literacy level of patients. Additionally, the open‐ended nature of questioning avoided some of the usual pitfalls of satisfaction surveys. We did not rely on predetermined satisfaction categories or presume the inherent value of particular attributes of care. Nonetheless, our study does have important limitations.
Patient perceptions were not compared with chart data or clinician report. Caregivers were allowed to participate in lieu of patients, which may have reduced identification of some dissatisfying events. Likewise, patients discharged to nursing homes or who were not English or Spanish speaking were excluded and may have had different dissatisfying experiences. Interviews were brief and dissatisfying events were not explored in detail. Although nearly half of respondents reported dissatisfying events, some patients may have been reluctant to criticize their care directly to a hospital representative. Finally, patients generally confined their comments to one or two dissatisfying events, even though there may have been others. We therefore cannot draw any conclusions about the relative frequency of dissatisfying events by domain.
Conclusions
All hospitalized patients bring expectations for their hospital experience. While specific expectations vary between patients, expectations for: 1) safety, 2) treatment with respect and dignity, 3) prompt and efficient care, 4) successful exchange of information, 5) environmental autonomy and control, and 6) high‐quality amenities were found in this study to encompass core expectations for hospitalization. It may be useful to ensure that postdischarge surveys explicitly address these expectations. Efforts to address and manage these core expectations of hospital care may help to reduce patient dissatisfaction with hospitalization and improve the delivery and quality of hospital care.
- ,.Multinational Comparisons of Health Systems Data, 2006.Washington, DC:The Commonwealth Fund;2007.
- ,,,,,.Toward higher‐performance health systems: Adults' health care experiences in seven countries, 2007.Health Aff.2007;26:w717–734.
- ,,, et al.Patient satisfaction and its relationship with clinical quality and inpatient mortality in acute myocardial infarction.Circ Cardiovasc Qual Outcomes.2010;3:188–195.
- ,.A longitudinal analysis of patient satisfaction and subsequent quality of life in Hong Kong Chinese breast and nasopharyngeal cancer patients.Med Care.2009;47:875–881.
- .Understanding dissatisfied users: developing a framework for comprehending criticisms of health care work.J Adv Nurs.1999;30:723–731.
- ,.Patient satisfaction: a review of issues and concepts.Soc Sci Med.1997;45:1829–1843.
- Institute of Medicine.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- .Patient satisfaction: a valid concept?Soc Sci Med.1994;38:509–516.
- .Exploring the meaning of ‘dissatisfaction’ with health care: the importance of ‘personal identity threat’.Sociol Health Illn.1999;21:95–123.
- ,.Pathways, pyramids and icebergs? Mapping the links between dissatisfaction and complaints.Sociol Health Illn.1998;20:825–847.
- ,.Convergence and divergence: assessing criteria of consumer satisfaction across general practice, dental and hospital care settings.Soc Sci Med.1991;33:707–716.
- ,,,,,.National survey of hospital patients [see comment].BMJ.1994;309:1542–1546.
- ,,, et al.The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.Health Technol Assess.2002;6:1–244.
- ,,,.Review of the literature on survey instruments used to collect data on hospital patients' perceptions of care.Health Serv Res.2005;40:1996–2017.
- ,,.Satisfying solutions? A review of some unresolved issues in the measurement of patient satisfaction.J Adv Nurs.1995;22:316–322.
- ,.The Discovery of Grounded Theory: Strategies for Qualitative Research.Chicago, IL:Aldine;1967.
- Hospital Consumer Assessment of Healthcare Providers 25:25–36.
- ,,,.Patient experiences in relation to respondent and health service delivery characteristics: a survey of 26,938 patients attending 62 hospitals throughout Norway.Scand J Public Health.2007;35:70–77.
- ,,, et al.What can hospitalized patients tell us about adverse events? Learning from patient‐reported incidents.J Gen Intern Med.2005;20:830–836.
- .A hospitalization from hell: a patient's perspective on quality.Ann Intern Med.2003;138:33–39.
- ,,,.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco, CA:Jossey‐Bass;1993.
- ,,,,.What do consumers want to know about the quality of care in hospitals?Health Serv Res.2005;40:2018–2036.
- ,.R‐e‐s‐p‐e‐c‐t: patient reports of disrespect in the health care setting and its impact on care.J Fam Pract.2004;53:721–730.
- ,,,,.Perceived information needs and communication difficulties of inpatient physicians and nurses.J Am Med Inform Assoc.2002;9(6 suppl 1):S64–S69.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13:i85–i90.
- ,,,,.Consequences of inadequate sign‐out for patient care.Arch Intern Med.2008;168:1755–1760.
- ,,,,,.Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care.Ann Emerg Med.2009;53:701–710 e704.
- ,.Interactive relationships between hospital patients' noise‐induced stress and other stress with sleep.Heart Lung.2001;30:237–243.
- .The influence of subjective reactions to noise on health effects of the noise.Environ Int.1996;22:93–104.
- .A novel PACU design for noise reduction.J Perianesth Nurs.2008;23:226–229.
- ,,,.The Planetree Model Hospital Project: an example of the patient as partner. (Pacific Presbyterian Medical Center, San Francisco).Hosp Health Serv Admin.1990;35:591–601.
- ,,.Physician‐patient communication in single‐bedded versus four‐bedded hospital rooms.Patient Educ Couns.2008;73:215–219.
- ,,.Advantages and disadvantages of single‐versus multiple‐occupancy rooms in acute care environments: a review and analysis of the literature.Environ Behav.2005;37:760–786.
- ,.Impacting patient outcomes through design: acuity adaptable care/universal room design.Crit Care Nurs Q.2006;29:326–341.
- ,.Multinational Comparisons of Health Systems Data, 2006.Washington, DC:The Commonwealth Fund;2007.
- ,,,,,.Toward higher‐performance health systems: Adults' health care experiences in seven countries, 2007.Health Aff.2007;26:w717–734.
- ,,, et al.Patient satisfaction and its relationship with clinical quality and inpatient mortality in acute myocardial infarction.Circ Cardiovasc Qual Outcomes.2010;3:188–195.
- ,.A longitudinal analysis of patient satisfaction and subsequent quality of life in Hong Kong Chinese breast and nasopharyngeal cancer patients.Med Care.2009;47:875–881.
- .Understanding dissatisfied users: developing a framework for comprehending criticisms of health care work.J Adv Nurs.1999;30:723–731.
- ,.Patient satisfaction: a review of issues and concepts.Soc Sci Med.1997;45:1829–1843.
- Institute of Medicine.Crossing the Quality Chasm: A New Health System for the 21st Century.Washington, DC:National Academy Press;2001.
- .Patient satisfaction: a valid concept?Soc Sci Med.1994;38:509–516.
- .Exploring the meaning of ‘dissatisfaction’ with health care: the importance of ‘personal identity threat’.Sociol Health Illn.1999;21:95–123.
- ,.Pathways, pyramids and icebergs? Mapping the links between dissatisfaction and complaints.Sociol Health Illn.1998;20:825–847.
- ,.Convergence and divergence: assessing criteria of consumer satisfaction across general practice, dental and hospital care settings.Soc Sci Med.1991;33:707–716.
- ,,,,,.National survey of hospital patients [see comment].BMJ.1994;309:1542–1546.
- ,,, et al.The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.Health Technol Assess.2002;6:1–244.
- ,,,.Review of the literature on survey instruments used to collect data on hospital patients' perceptions of care.Health Serv Res.2005;40:1996–2017.
- ,,.Satisfying solutions? A review of some unresolved issues in the measurement of patient satisfaction.J Adv Nurs.1995;22:316–322.
- ,.The Discovery of Grounded Theory: Strategies for Qualitative Research.Chicago, IL:Aldine;1967.
- Hospital Consumer Assessment of Healthcare Providers 25:25–36.
- ,,,.Patient experiences in relation to respondent and health service delivery characteristics: a survey of 26,938 patients attending 62 hospitals throughout Norway.Scand J Public Health.2007;35:70–77.
- ,,, et al.What can hospitalized patients tell us about adverse events? Learning from patient‐reported incidents.J Gen Intern Med.2005;20:830–836.
- .A hospitalization from hell: a patient's perspective on quality.Ann Intern Med.2003;138:33–39.
- ,,,.Through the Patient's Eyes: Understanding and Promoting Patient‐Centered Care.San Francisco, CA:Jossey‐Bass;1993.
- ,,,,.What do consumers want to know about the quality of care in hospitals?Health Serv Res.2005;40:2018–2036.
- ,.R‐e‐s‐p‐e‐c‐t: patient reports of disrespect in the health care setting and its impact on care.J Fam Pract.2004;53:721–730.
- ,,,,.Perceived information needs and communication difficulties of inpatient physicians and nurses.J Am Med Inform Assoc.2002;9(6 suppl 1):S64–S69.
- ,,.The human factor: the critical importance of effective teamwork and communication in providing safe care.Qual Saf Health Care.2004;13:i85–i90.
- ,,,,.Consequences of inadequate sign‐out for patient care.Arch Intern Med.2008;168:1755–1760.
- ,,,,,.Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care.Ann Emerg Med.2009;53:701–710 e704.
- ,.Interactive relationships between hospital patients' noise‐induced stress and other stress with sleep.Heart Lung.2001;30:237–243.
- .The influence of subjective reactions to noise on health effects of the noise.Environ Int.1996;22:93–104.
- .A novel PACU design for noise reduction.J Perianesth Nurs.2008;23:226–229.
- ,,,.The Planetree Model Hospital Project: an example of the patient as partner. (Pacific Presbyterian Medical Center, San Francisco).Hosp Health Serv Admin.1990;35:591–601.
- ,,.Physician‐patient communication in single‐bedded versus four‐bedded hospital rooms.Patient Educ Couns.2008;73:215–219.
- ,,.Advantages and disadvantages of single‐versus multiple‐occupancy rooms in acute care environments: a review and analysis of the literature.Environ Behav.2005;37:760–786.
- ,.Impacting patient outcomes through design: acuity adaptable care/universal room design.Crit Care Nurs Q.2006;29:326–341.
Copyright © 2010 Society of Hospital Medicine