User login
The Bad Hire
Hospital medicine groups depend on camaraderie and expertise to carry them through long days and heavy workloads. Group cohesiveness—often fragile—depends on recruiting and keeping hard-working doctors who pull their weight professionally and boost the group’s chemistry.
In a field with five job openings for every qualified candidate, and average annual turnover at 12%, hospital medicine groups can ill afford a bad hire. Whether that person is a practice killer, a cipher who blends into the wallpaper while collecting a paycheck, or a doctor marking time until a fellowship or something better comes along, the group leader must quickly limit a bad hire’s negative impact.
Recognizing that competition to hire hospitalists is fierce, it may seem that avoiding or axing a bad hire—the physician who either doesn’t mesh with your team, is a professional and/or personal train wreck, or has a blue-ribbon pedigree, but performs poorly—is a luxury hospitalist groups can’t afford.
But as Per Danielsson, MD, medical director of Seattle-based Swedish Medical Center’s adult hospitalist program has learned the hard way: “No doctor is better than the wrong doctor. I don’t sugarcoat the demands of our program with prospects. We’re a seasoned hospitalist program, we work hard, and, if we have a position vacant, we’ll work even harder for short periods of time until we find the right person.”
With a hospitalist group of 25 providers, Dr. Danielsson spends more time than he’d like recruiting and interviewing candidates, but he considers it time well spent. “The CV and interview are important, but I’ve devised a list of 12 personality traits that I consider important,” he says. “I share the list with candidates to see if we have a good fit.”
Chris Nussbaum, MD, CEO of Synergy Medical Group, based in Brandon, Fla., says: “They don’t make doctors the way they used to. I don’t see why some hospitalists think seeing 20 to 25 patients a day is such a big deal. I’ve had several tell me that 20 patients a day is no problem—and then they only last one day.” When that happens, Synergy cuts its losses, not allowing a bad hire to linger.
Dr. Nussbaum didn’t think twice about firing one new hire—a physician with an impressive resume who, while writing chart notes at a nursing station, watched a nurse have a seizure, gathered his notes and left the room. “He expected an endocrinologist standing nearby to help out, but it’s outrageous that any hospitalist wouldn’t respond appropriately,” he says. Such callous behavior would send shock waves through any group, and that physician was fired on the spot.
Another organizational disrupter, briefly employed by IPC-the Hospitalist Company (North Hollywood, Calif.) made inflammatory remarks about a hospital’s pre-eminent specialist and other referring physicians. He was fired. Several hospitalist leaders report hiring physicians with stellar pedigrees whose hands consistently strayed to nurses’ derrieres. Those doctors were quickly shown the door.
Robin Ryan, a career coach from Newcastle, Wash., who has prepared office-based physicians for professional moves to hospitalist careers, says the new career path can be confusing. When a physician and a hospitalist group have made a mistake, Ryan says most groups cut their losses by terminating someone who doesn’t fit. “Contracts often require a hefty severance fee, but it’s often the road that groups take,” she says.
Probing Personality
To weed out potential bad hires, employees long have used personality tests. Such tests also help job candidates clarify what matters most to them professionally. The SHM’s Career Satisfaction Task Force has developed a framework for hospitalists to do that. The self-test rests on four pillars of job satisfaction: reward/recognition, workload/schedule, autonomy/control, and community/environment (to view, go to www.hospitalmedicine.org and click “Career Satisfaction White Paper”).
Sylvia McKean, MD, medical director, the Brigham & Women’s Hospital/Faulkner Hospitalist Program in Boston and the task force’s co-chair, urges hospitalists to complete the self-test to maximize a potential job fit.
“All jobs have unpleasant side effects,” says Dr. McKean. “People get sick at bad times. There is high stress and sometimes high error rates. It’s important for a hospitalist to analyze what your needs are and to find an environment that best suits them.”
Dr. McKean also offers wisdom from the other side of desk, having interviewed candidates for coveted spots at Brigham & Women’s hospitalist program. “I’ve interviewed doctors who aren’t interested in hospitalist medicine but view our program as a stepping stone to the job they really want here,’’ she says. “We hired and fired someone who wanted her own way all the time. She left for another prestigious hospital. Then there are others who don’t want to teach, but choose a teaching hospital.”
Dr. McKean hopes SHM’s self-assessment tools will help job candidates focus on what they want from a hospital medicine group and avoid the “pebbles” that erode job satisfaction.
IPC, which employs 600 physicians in 100 practices in 24 markets, tried personality testing then discarded it. IPC hired a psychometric firm to devise a psychological profile of “best” and “worst” performing hospitalists. The testers created a test measuring seven key characteristics relating to temperament, intelligence, and clinical skills.
IPC’s CEO Adam Singer, MD, says: “We tested all candidates but found the test ineffective because nearly everyone, including me, got five or better.” He dropped the test, relying instead on extensive interviews. Dr. Singer reviews 2,500 to 3,000 physician resumes annually and spends significant resources on avoiding bad hires. All that hard work doesn’t avoid the occasional mistake.
“I’ve seen everything—the brilliant doctor who can’t function on a team, aloofness, temper tantrums, rudeness, and always pushing responsibility on someone else,” says Dr. Singer. “When something’s wrong, 90% of the time we terminate them ASAP. The other 10% we salvage by finding what’s stressing them, relieving the pressure, and mentoring them into proper behavior.”
Cynthia Stamer, a Dallas-based attorney at Glast, Phillips & Murray, P.C., works extensively with physicians and hospitals and sees young physicians straight from residency joining hospitalist programs “just looking for a job and not focused on whether or not there’s a good personality fit.” She urges job candidates and hirers to better probe the fit.
Stamer finds good hospitalists to be stress jockeys who thrive on the intensity of hospital work. “I think they’re born and not bred,” she says. “They tend to be bored or disruptive in office practices, and to enjoy a pattern of work hard, play hard. The ability to throw the ‘on’ switch and be intense for block scheduling, then be ‘off’ for a block suits them,” she says.
Not That Bad
In a field where an extra pair of hands can make the difference between taking night call or the freedom to take several days off for emergencies, a mediocre team member might seem better than none. Some hospitalist groups would rather pull a bigger load temporarily than tolerate a laggard; others stomach imperfection.
Spotting problems during the hiring process can turn a bad hire into a proper fit. For example, offering a permanent part-time position to someone with young children who can’t commit to full-time employment avoids potential problems. Or, asking enough probing questions might help you discover a physician has a year before a coveted fellowship begins; tailoring a one-year contract for that person optimizes fit. Eliminating managerial tasks for a pure clinician who eschews the leadership fast track works, too.
What to do with the mediocre performer rather than the egregious misfit? Perhaps she consistently arrives to work late, doesn’t complete her charts, and tries to avoid admissions or challenging assignments. A group leader may salvage the situation through mentoring and tying pay to performance. Dr. Singer says: “Underperformers usually don’t understand their impact on the group. We teach them healthcare economics and the flow of dollars. We train them to get the relationship between pay and performance, and hope for results.”
Stamer urges hospitalist leaders to build termination procedures into employment contracts, to document poor performance, and to give severance pay or buy out a contract with a bad hire. “People get testy around disengagement, but if you can take the heat out of the process, it’s better in the long run,” she concludes.
As hospitalist supply approaches demand, avoiding bad hires should be easier. For now, most groups prefer pulling together and working harder rather than abide an outlier. It comes with the territory. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Hospital medicine groups depend on camaraderie and expertise to carry them through long days and heavy workloads. Group cohesiveness—often fragile—depends on recruiting and keeping hard-working doctors who pull their weight professionally and boost the group’s chemistry.
In a field with five job openings for every qualified candidate, and average annual turnover at 12%, hospital medicine groups can ill afford a bad hire. Whether that person is a practice killer, a cipher who blends into the wallpaper while collecting a paycheck, or a doctor marking time until a fellowship or something better comes along, the group leader must quickly limit a bad hire’s negative impact.
Recognizing that competition to hire hospitalists is fierce, it may seem that avoiding or axing a bad hire—the physician who either doesn’t mesh with your team, is a professional and/or personal train wreck, or has a blue-ribbon pedigree, but performs poorly—is a luxury hospitalist groups can’t afford.
But as Per Danielsson, MD, medical director of Seattle-based Swedish Medical Center’s adult hospitalist program has learned the hard way: “No doctor is better than the wrong doctor. I don’t sugarcoat the demands of our program with prospects. We’re a seasoned hospitalist program, we work hard, and, if we have a position vacant, we’ll work even harder for short periods of time until we find the right person.”
With a hospitalist group of 25 providers, Dr. Danielsson spends more time than he’d like recruiting and interviewing candidates, but he considers it time well spent. “The CV and interview are important, but I’ve devised a list of 12 personality traits that I consider important,” he says. “I share the list with candidates to see if we have a good fit.”
Chris Nussbaum, MD, CEO of Synergy Medical Group, based in Brandon, Fla., says: “They don’t make doctors the way they used to. I don’t see why some hospitalists think seeing 20 to 25 patients a day is such a big deal. I’ve had several tell me that 20 patients a day is no problem—and then they only last one day.” When that happens, Synergy cuts its losses, not allowing a bad hire to linger.
Dr. Nussbaum didn’t think twice about firing one new hire—a physician with an impressive resume who, while writing chart notes at a nursing station, watched a nurse have a seizure, gathered his notes and left the room. “He expected an endocrinologist standing nearby to help out, but it’s outrageous that any hospitalist wouldn’t respond appropriately,” he says. Such callous behavior would send shock waves through any group, and that physician was fired on the spot.
Another organizational disrupter, briefly employed by IPC-the Hospitalist Company (North Hollywood, Calif.) made inflammatory remarks about a hospital’s pre-eminent specialist and other referring physicians. He was fired. Several hospitalist leaders report hiring physicians with stellar pedigrees whose hands consistently strayed to nurses’ derrieres. Those doctors were quickly shown the door.
Robin Ryan, a career coach from Newcastle, Wash., who has prepared office-based physicians for professional moves to hospitalist careers, says the new career path can be confusing. When a physician and a hospitalist group have made a mistake, Ryan says most groups cut their losses by terminating someone who doesn’t fit. “Contracts often require a hefty severance fee, but it’s often the road that groups take,” she says.
Probing Personality
To weed out potential bad hires, employees long have used personality tests. Such tests also help job candidates clarify what matters most to them professionally. The SHM’s Career Satisfaction Task Force has developed a framework for hospitalists to do that. The self-test rests on four pillars of job satisfaction: reward/recognition, workload/schedule, autonomy/control, and community/environment (to view, go to www.hospitalmedicine.org and click “Career Satisfaction White Paper”).
Sylvia McKean, MD, medical director, the Brigham & Women’s Hospital/Faulkner Hospitalist Program in Boston and the task force’s co-chair, urges hospitalists to complete the self-test to maximize a potential job fit.
“All jobs have unpleasant side effects,” says Dr. McKean. “People get sick at bad times. There is high stress and sometimes high error rates. It’s important for a hospitalist to analyze what your needs are and to find an environment that best suits them.”
Dr. McKean also offers wisdom from the other side of desk, having interviewed candidates for coveted spots at Brigham & Women’s hospitalist program. “I’ve interviewed doctors who aren’t interested in hospitalist medicine but view our program as a stepping stone to the job they really want here,’’ she says. “We hired and fired someone who wanted her own way all the time. She left for another prestigious hospital. Then there are others who don’t want to teach, but choose a teaching hospital.”
Dr. McKean hopes SHM’s self-assessment tools will help job candidates focus on what they want from a hospital medicine group and avoid the “pebbles” that erode job satisfaction.
IPC, which employs 600 physicians in 100 practices in 24 markets, tried personality testing then discarded it. IPC hired a psychometric firm to devise a psychological profile of “best” and “worst” performing hospitalists. The testers created a test measuring seven key characteristics relating to temperament, intelligence, and clinical skills.
IPC’s CEO Adam Singer, MD, says: “We tested all candidates but found the test ineffective because nearly everyone, including me, got five or better.” He dropped the test, relying instead on extensive interviews. Dr. Singer reviews 2,500 to 3,000 physician resumes annually and spends significant resources on avoiding bad hires. All that hard work doesn’t avoid the occasional mistake.
“I’ve seen everything—the brilliant doctor who can’t function on a team, aloofness, temper tantrums, rudeness, and always pushing responsibility on someone else,” says Dr. Singer. “When something’s wrong, 90% of the time we terminate them ASAP. The other 10% we salvage by finding what’s stressing them, relieving the pressure, and mentoring them into proper behavior.”
Cynthia Stamer, a Dallas-based attorney at Glast, Phillips & Murray, P.C., works extensively with physicians and hospitals and sees young physicians straight from residency joining hospitalist programs “just looking for a job and not focused on whether or not there’s a good personality fit.” She urges job candidates and hirers to better probe the fit.
Stamer finds good hospitalists to be stress jockeys who thrive on the intensity of hospital work. “I think they’re born and not bred,” she says. “They tend to be bored or disruptive in office practices, and to enjoy a pattern of work hard, play hard. The ability to throw the ‘on’ switch and be intense for block scheduling, then be ‘off’ for a block suits them,” she says.
Not That Bad
In a field where an extra pair of hands can make the difference between taking night call or the freedom to take several days off for emergencies, a mediocre team member might seem better than none. Some hospitalist groups would rather pull a bigger load temporarily than tolerate a laggard; others stomach imperfection.
Spotting problems during the hiring process can turn a bad hire into a proper fit. For example, offering a permanent part-time position to someone with young children who can’t commit to full-time employment avoids potential problems. Or, asking enough probing questions might help you discover a physician has a year before a coveted fellowship begins; tailoring a one-year contract for that person optimizes fit. Eliminating managerial tasks for a pure clinician who eschews the leadership fast track works, too.
What to do with the mediocre performer rather than the egregious misfit? Perhaps she consistently arrives to work late, doesn’t complete her charts, and tries to avoid admissions or challenging assignments. A group leader may salvage the situation through mentoring and tying pay to performance. Dr. Singer says: “Underperformers usually don’t understand their impact on the group. We teach them healthcare economics and the flow of dollars. We train them to get the relationship between pay and performance, and hope for results.”
Stamer urges hospitalist leaders to build termination procedures into employment contracts, to document poor performance, and to give severance pay or buy out a contract with a bad hire. “People get testy around disengagement, but if you can take the heat out of the process, it’s better in the long run,” she concludes.
As hospitalist supply approaches demand, avoiding bad hires should be easier. For now, most groups prefer pulling together and working harder rather than abide an outlier. It comes with the territory. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Hospital medicine groups depend on camaraderie and expertise to carry them through long days and heavy workloads. Group cohesiveness—often fragile—depends on recruiting and keeping hard-working doctors who pull their weight professionally and boost the group’s chemistry.
In a field with five job openings for every qualified candidate, and average annual turnover at 12%, hospital medicine groups can ill afford a bad hire. Whether that person is a practice killer, a cipher who blends into the wallpaper while collecting a paycheck, or a doctor marking time until a fellowship or something better comes along, the group leader must quickly limit a bad hire’s negative impact.
Recognizing that competition to hire hospitalists is fierce, it may seem that avoiding or axing a bad hire—the physician who either doesn’t mesh with your team, is a professional and/or personal train wreck, or has a blue-ribbon pedigree, but performs poorly—is a luxury hospitalist groups can’t afford.
But as Per Danielsson, MD, medical director of Seattle-based Swedish Medical Center’s adult hospitalist program has learned the hard way: “No doctor is better than the wrong doctor. I don’t sugarcoat the demands of our program with prospects. We’re a seasoned hospitalist program, we work hard, and, if we have a position vacant, we’ll work even harder for short periods of time until we find the right person.”
With a hospitalist group of 25 providers, Dr. Danielsson spends more time than he’d like recruiting and interviewing candidates, but he considers it time well spent. “The CV and interview are important, but I’ve devised a list of 12 personality traits that I consider important,” he says. “I share the list with candidates to see if we have a good fit.”
Chris Nussbaum, MD, CEO of Synergy Medical Group, based in Brandon, Fla., says: “They don’t make doctors the way they used to. I don’t see why some hospitalists think seeing 20 to 25 patients a day is such a big deal. I’ve had several tell me that 20 patients a day is no problem—and then they only last one day.” When that happens, Synergy cuts its losses, not allowing a bad hire to linger.
Dr. Nussbaum didn’t think twice about firing one new hire—a physician with an impressive resume who, while writing chart notes at a nursing station, watched a nurse have a seizure, gathered his notes and left the room. “He expected an endocrinologist standing nearby to help out, but it’s outrageous that any hospitalist wouldn’t respond appropriately,” he says. Such callous behavior would send shock waves through any group, and that physician was fired on the spot.
Another organizational disrupter, briefly employed by IPC-the Hospitalist Company (North Hollywood, Calif.) made inflammatory remarks about a hospital’s pre-eminent specialist and other referring physicians. He was fired. Several hospitalist leaders report hiring physicians with stellar pedigrees whose hands consistently strayed to nurses’ derrieres. Those doctors were quickly shown the door.
Robin Ryan, a career coach from Newcastle, Wash., who has prepared office-based physicians for professional moves to hospitalist careers, says the new career path can be confusing. When a physician and a hospitalist group have made a mistake, Ryan says most groups cut their losses by terminating someone who doesn’t fit. “Contracts often require a hefty severance fee, but it’s often the road that groups take,” she says.
Probing Personality
To weed out potential bad hires, employees long have used personality tests. Such tests also help job candidates clarify what matters most to them professionally. The SHM’s Career Satisfaction Task Force has developed a framework for hospitalists to do that. The self-test rests on four pillars of job satisfaction: reward/recognition, workload/schedule, autonomy/control, and community/environment (to view, go to www.hospitalmedicine.org and click “Career Satisfaction White Paper”).
Sylvia McKean, MD, medical director, the Brigham & Women’s Hospital/Faulkner Hospitalist Program in Boston and the task force’s co-chair, urges hospitalists to complete the self-test to maximize a potential job fit.
“All jobs have unpleasant side effects,” says Dr. McKean. “People get sick at bad times. There is high stress and sometimes high error rates. It’s important for a hospitalist to analyze what your needs are and to find an environment that best suits them.”
Dr. McKean also offers wisdom from the other side of desk, having interviewed candidates for coveted spots at Brigham & Women’s hospitalist program. “I’ve interviewed doctors who aren’t interested in hospitalist medicine but view our program as a stepping stone to the job they really want here,’’ she says. “We hired and fired someone who wanted her own way all the time. She left for another prestigious hospital. Then there are others who don’t want to teach, but choose a teaching hospital.”
Dr. McKean hopes SHM’s self-assessment tools will help job candidates focus on what they want from a hospital medicine group and avoid the “pebbles” that erode job satisfaction.
IPC, which employs 600 physicians in 100 practices in 24 markets, tried personality testing then discarded it. IPC hired a psychometric firm to devise a psychological profile of “best” and “worst” performing hospitalists. The testers created a test measuring seven key characteristics relating to temperament, intelligence, and clinical skills.
IPC’s CEO Adam Singer, MD, says: “We tested all candidates but found the test ineffective because nearly everyone, including me, got five or better.” He dropped the test, relying instead on extensive interviews. Dr. Singer reviews 2,500 to 3,000 physician resumes annually and spends significant resources on avoiding bad hires. All that hard work doesn’t avoid the occasional mistake.
“I’ve seen everything—the brilliant doctor who can’t function on a team, aloofness, temper tantrums, rudeness, and always pushing responsibility on someone else,” says Dr. Singer. “When something’s wrong, 90% of the time we terminate them ASAP. The other 10% we salvage by finding what’s stressing them, relieving the pressure, and mentoring them into proper behavior.”
Cynthia Stamer, a Dallas-based attorney at Glast, Phillips & Murray, P.C., works extensively with physicians and hospitals and sees young physicians straight from residency joining hospitalist programs “just looking for a job and not focused on whether or not there’s a good personality fit.” She urges job candidates and hirers to better probe the fit.
Stamer finds good hospitalists to be stress jockeys who thrive on the intensity of hospital work. “I think they’re born and not bred,” she says. “They tend to be bored or disruptive in office practices, and to enjoy a pattern of work hard, play hard. The ability to throw the ‘on’ switch and be intense for block scheduling, then be ‘off’ for a block suits them,” she says.
Not That Bad
In a field where an extra pair of hands can make the difference between taking night call or the freedom to take several days off for emergencies, a mediocre team member might seem better than none. Some hospitalist groups would rather pull a bigger load temporarily than tolerate a laggard; others stomach imperfection.
Spotting problems during the hiring process can turn a bad hire into a proper fit. For example, offering a permanent part-time position to someone with young children who can’t commit to full-time employment avoids potential problems. Or, asking enough probing questions might help you discover a physician has a year before a coveted fellowship begins; tailoring a one-year contract for that person optimizes fit. Eliminating managerial tasks for a pure clinician who eschews the leadership fast track works, too.
What to do with the mediocre performer rather than the egregious misfit? Perhaps she consistently arrives to work late, doesn’t complete her charts, and tries to avoid admissions or challenging assignments. A group leader may salvage the situation through mentoring and tying pay to performance. Dr. Singer says: “Underperformers usually don’t understand their impact on the group. We teach them healthcare economics and the flow of dollars. We train them to get the relationship between pay and performance, and hope for results.”
Stamer urges hospitalist leaders to build termination procedures into employment contracts, to document poor performance, and to give severance pay or buy out a contract with a bad hire. “People get testy around disengagement, but if you can take the heat out of the process, it’s better in the long run,” she concludes.
As hospitalist supply approaches demand, avoiding bad hires should be easier. For now, most groups prefer pulling together and working harder rather than abide an outlier. It comes with the territory. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
VTE Studies Win Grants
Two pharmacist-hospitalist teams each won $50,000 grants June 12 from the American Society of Health-System Pharmacists (ASHP) Research and Education Foundation (Bethesda, Md.) to support development of screening tools and order sets to prevent and treat hospital-acquired venous thromboembolism (VTE).
The grant winners and lead co-investigators from each team:
- Robert Weibert, PharmD, health sciences clinical professor and director of the Anticoagulation Clinic, School of Pharmacy, and Gregory Maynard, MD, MS, head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego (UCSD); and
- Rachel Hroncich, PharmD, pharmacy clinical coordinator of Presbyterian Healthcare Service, and Randle Adair, DO, PhD, a PMG hospitalist in adult medicine from Albuquerque, N.M.
The ASHP, a nonprofit organization, fosters safe medication use.
“We are thrilled that our grant application was selected by the ASHP and excited about the opportunity for our research to improve patient care,” says Dr. Hroncich.
The ASHP Research and Education Foundation grant program, sponsored by Sanofi-Aventis, supports research by hospitalists and hospital pharmacists to treat VTE, with a focus on hospitalized patients and post-discharge follow-up. The grants are geared to help hospitalists and pharmacists reduce hospital-acquired VTE, a significant cause of morbidity and mortality in hospitals.
VTE-related treatment costs $1.5 billion a year, according to researchers at the University of Washington School of Pharmacy in Seattle. ASHP statistics indicate VTE affects more than 450,000 hospitalized patients annually. The condition—an amalgam of deep vein thrombosis (DVT) and pulmonary embolism (PE)—affects a range of hospitalized patients. Gynecologic, orthopedic, urologic, vascular, trauma, and cancer patients all are at risk—as are those with other medical conditions such as congestive heart failure, severe respiratory disease, and obesity, or those who are bedridden.
The ASHP grants help pharmacist-hospitalist teams find tools to screen for VTE. Such tools let clinicians intervene early with at-risk patients. Better screening and intervention requires sound clinical, administrative, and IT processes.
The trick is to encourage busy hospitalists to use a consensus-based VTE screening tool for all hospitalized patients.
While most VTE research involves retrospective chart review of diagnostic codes, Drs. Weibert and Maynard’s grant research goes beyond such studies by identifying patients at risk concurrent with their hospitalizations. Dr. Maynard says the need is urgent: “Hospitals grossly underestimate the risk of VTE. In a 300-bed hospital, at least 150 patients are at risk of hospital-acquired VTE at any time.”
The UCSD team hopes to improve VTE screening by integrating an order set into the hospital’s computer physician order entry (CPOE) system. “The literature points to a bundle of best practices for VTE,” says Dr. Maynard, “including baseline lab work, use of compression stockings, using heparin for an optimal time period, patient education for those on anticoagulants, timely follow-up post discharge, the Society of Hospital Medicine collaborative, etc.”
Based on that body of knowledge and the input of its 15 full-time equivalent hospitalists, UCSD stakeholders in VTE screening debate what is practical and workable, conduct small, paper-based pilot projects, and fine-tune the protocol to integrate it with patient flow through admissions. “As we transition fully to a CPOE in our health system, we will incorporate a VTE order set that is doable and user-friendly,” adds Dr. Maynard.
UCSD’s pharmacist-hospitalist collaboration also encourages residents from both disciplines to work together on integrating protocols into clinical care processes. The team hopes that the VTE protocol will go beyond the inpatient stay by wrapping the protocol into the discharge plan. Dr. Weibert’s anticoagulation and pulmonary embolism clinics also help “build on our strengths,” he says.
The second team is led by newcomers to the grant winner’s circle, Drs. Hroncich (pharmacist) and Adair (hospitalist) from Presbyterian Healthcare Services, Albuquerque, N.M. They base their research on this question: Is it more efficient for the system’s 34 hospitalists to screen out those at low risk of VTE than to screen everyone for high risk?
The investigators have been collecting baseline data on compliance with VTE screening since 2003. Hospitalist use of a VTE screening tool on admissions was 60%, improving to 88% with reminders. “The implication is that 12% of the hospitalists didn’t use the screening tool,” says Dr. Adair. “We found that they were resistant to another piece of paper.” PHS data also showed that seven out of 10 patients had some VTE risk, that co-morbidities and hospitalization increase VTE risk, and that the age at which patients fall prey to VTE is dropping to between 50 and 60.
For the ASHP grant, Drs. Hroncich and Adair will monitor VTE screening on admission to all PHS general medical units. All patients 18 or older admitted to those units during a three-month period will be routinely screened on admission for VTE risk. Drs. Hroncich and Adair will make two VTE-related admission order sets available to hospitalists to complete. The current screening tool is designed to identify patients at risk of developing a VTE based on the presence of risk factors. The second, shorter admission order set will contain a screening tool that assumes that all patients need VTE prophylaxis, except low-risk patients and those with VTE prophylaxis contraindications. “The shorter tool should take only one or two minutes to complete,” says Dr. Hroncich.
The PHS team hopes that the shorter screening tool will overcome resistance to VTE screening. Dr. Hroncich says there are many barriers to VTE screening. They include lack of consensus on the best screening tool on admission, the misperception that VTE isn’t a big problem, lack of reliable processes so at-risk patients don’t fall through the cracks, and a misperception that anti-coagulant therapy is dangerous.
“It’s one thing to treat COPD and heart failure,” adds Dr. Adair, “but if I can prevent VTE with less than a 60-second screening, I can prevent a disease state from happening.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Two pharmacist-hospitalist teams each won $50,000 grants June 12 from the American Society of Health-System Pharmacists (ASHP) Research and Education Foundation (Bethesda, Md.) to support development of screening tools and order sets to prevent and treat hospital-acquired venous thromboembolism (VTE).
The grant winners and lead co-investigators from each team:
- Robert Weibert, PharmD, health sciences clinical professor and director of the Anticoagulation Clinic, School of Pharmacy, and Gregory Maynard, MD, MS, head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego (UCSD); and
- Rachel Hroncich, PharmD, pharmacy clinical coordinator of Presbyterian Healthcare Service, and Randle Adair, DO, PhD, a PMG hospitalist in adult medicine from Albuquerque, N.M.
The ASHP, a nonprofit organization, fosters safe medication use.
“We are thrilled that our grant application was selected by the ASHP and excited about the opportunity for our research to improve patient care,” says Dr. Hroncich.
The ASHP Research and Education Foundation grant program, sponsored by Sanofi-Aventis, supports research by hospitalists and hospital pharmacists to treat VTE, with a focus on hospitalized patients and post-discharge follow-up. The grants are geared to help hospitalists and pharmacists reduce hospital-acquired VTE, a significant cause of morbidity and mortality in hospitals.
VTE-related treatment costs $1.5 billion a year, according to researchers at the University of Washington School of Pharmacy in Seattle. ASHP statistics indicate VTE affects more than 450,000 hospitalized patients annually. The condition—an amalgam of deep vein thrombosis (DVT) and pulmonary embolism (PE)—affects a range of hospitalized patients. Gynecologic, orthopedic, urologic, vascular, trauma, and cancer patients all are at risk—as are those with other medical conditions such as congestive heart failure, severe respiratory disease, and obesity, or those who are bedridden.
The ASHP grants help pharmacist-hospitalist teams find tools to screen for VTE. Such tools let clinicians intervene early with at-risk patients. Better screening and intervention requires sound clinical, administrative, and IT processes.
The trick is to encourage busy hospitalists to use a consensus-based VTE screening tool for all hospitalized patients.
While most VTE research involves retrospective chart review of diagnostic codes, Drs. Weibert and Maynard’s grant research goes beyond such studies by identifying patients at risk concurrent with their hospitalizations. Dr. Maynard says the need is urgent: “Hospitals grossly underestimate the risk of VTE. In a 300-bed hospital, at least 150 patients are at risk of hospital-acquired VTE at any time.”
The UCSD team hopes to improve VTE screening by integrating an order set into the hospital’s computer physician order entry (CPOE) system. “The literature points to a bundle of best practices for VTE,” says Dr. Maynard, “including baseline lab work, use of compression stockings, using heparin for an optimal time period, patient education for those on anticoagulants, timely follow-up post discharge, the Society of Hospital Medicine collaborative, etc.”
Based on that body of knowledge and the input of its 15 full-time equivalent hospitalists, UCSD stakeholders in VTE screening debate what is practical and workable, conduct small, paper-based pilot projects, and fine-tune the protocol to integrate it with patient flow through admissions. “As we transition fully to a CPOE in our health system, we will incorporate a VTE order set that is doable and user-friendly,” adds Dr. Maynard.
UCSD’s pharmacist-hospitalist collaboration also encourages residents from both disciplines to work together on integrating protocols into clinical care processes. The team hopes that the VTE protocol will go beyond the inpatient stay by wrapping the protocol into the discharge plan. Dr. Weibert’s anticoagulation and pulmonary embolism clinics also help “build on our strengths,” he says.
The second team is led by newcomers to the grant winner’s circle, Drs. Hroncich (pharmacist) and Adair (hospitalist) from Presbyterian Healthcare Services, Albuquerque, N.M. They base their research on this question: Is it more efficient for the system’s 34 hospitalists to screen out those at low risk of VTE than to screen everyone for high risk?
The investigators have been collecting baseline data on compliance with VTE screening since 2003. Hospitalist use of a VTE screening tool on admissions was 60%, improving to 88% with reminders. “The implication is that 12% of the hospitalists didn’t use the screening tool,” says Dr. Adair. “We found that they were resistant to another piece of paper.” PHS data also showed that seven out of 10 patients had some VTE risk, that co-morbidities and hospitalization increase VTE risk, and that the age at which patients fall prey to VTE is dropping to between 50 and 60.
For the ASHP grant, Drs. Hroncich and Adair will monitor VTE screening on admission to all PHS general medical units. All patients 18 or older admitted to those units during a three-month period will be routinely screened on admission for VTE risk. Drs. Hroncich and Adair will make two VTE-related admission order sets available to hospitalists to complete. The current screening tool is designed to identify patients at risk of developing a VTE based on the presence of risk factors. The second, shorter admission order set will contain a screening tool that assumes that all patients need VTE prophylaxis, except low-risk patients and those with VTE prophylaxis contraindications. “The shorter tool should take only one or two minutes to complete,” says Dr. Hroncich.
The PHS team hopes that the shorter screening tool will overcome resistance to VTE screening. Dr. Hroncich says there are many barriers to VTE screening. They include lack of consensus on the best screening tool on admission, the misperception that VTE isn’t a big problem, lack of reliable processes so at-risk patients don’t fall through the cracks, and a misperception that anti-coagulant therapy is dangerous.
“It’s one thing to treat COPD and heart failure,” adds Dr. Adair, “but if I can prevent VTE with less than a 60-second screening, I can prevent a disease state from happening.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Two pharmacist-hospitalist teams each won $50,000 grants June 12 from the American Society of Health-System Pharmacists (ASHP) Research and Education Foundation (Bethesda, Md.) to support development of screening tools and order sets to prevent and treat hospital-acquired venous thromboembolism (VTE).
The grant winners and lead co-investigators from each team:
- Robert Weibert, PharmD, health sciences clinical professor and director of the Anticoagulation Clinic, School of Pharmacy, and Gregory Maynard, MD, MS, head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California-San Diego (UCSD); and
- Rachel Hroncich, PharmD, pharmacy clinical coordinator of Presbyterian Healthcare Service, and Randle Adair, DO, PhD, a PMG hospitalist in adult medicine from Albuquerque, N.M.
The ASHP, a nonprofit organization, fosters safe medication use.
“We are thrilled that our grant application was selected by the ASHP and excited about the opportunity for our research to improve patient care,” says Dr. Hroncich.
The ASHP Research and Education Foundation grant program, sponsored by Sanofi-Aventis, supports research by hospitalists and hospital pharmacists to treat VTE, with a focus on hospitalized patients and post-discharge follow-up. The grants are geared to help hospitalists and pharmacists reduce hospital-acquired VTE, a significant cause of morbidity and mortality in hospitals.
VTE-related treatment costs $1.5 billion a year, according to researchers at the University of Washington School of Pharmacy in Seattle. ASHP statistics indicate VTE affects more than 450,000 hospitalized patients annually. The condition—an amalgam of deep vein thrombosis (DVT) and pulmonary embolism (PE)—affects a range of hospitalized patients. Gynecologic, orthopedic, urologic, vascular, trauma, and cancer patients all are at risk—as are those with other medical conditions such as congestive heart failure, severe respiratory disease, and obesity, or those who are bedridden.
The ASHP grants help pharmacist-hospitalist teams find tools to screen for VTE. Such tools let clinicians intervene early with at-risk patients. Better screening and intervention requires sound clinical, administrative, and IT processes.
The trick is to encourage busy hospitalists to use a consensus-based VTE screening tool for all hospitalized patients.
While most VTE research involves retrospective chart review of diagnostic codes, Drs. Weibert and Maynard’s grant research goes beyond such studies by identifying patients at risk concurrent with their hospitalizations. Dr. Maynard says the need is urgent: “Hospitals grossly underestimate the risk of VTE. In a 300-bed hospital, at least 150 patients are at risk of hospital-acquired VTE at any time.”
The UCSD team hopes to improve VTE screening by integrating an order set into the hospital’s computer physician order entry (CPOE) system. “The literature points to a bundle of best practices for VTE,” says Dr. Maynard, “including baseline lab work, use of compression stockings, using heparin for an optimal time period, patient education for those on anticoagulants, timely follow-up post discharge, the Society of Hospital Medicine collaborative, etc.”
Based on that body of knowledge and the input of its 15 full-time equivalent hospitalists, UCSD stakeholders in VTE screening debate what is practical and workable, conduct small, paper-based pilot projects, and fine-tune the protocol to integrate it with patient flow through admissions. “As we transition fully to a CPOE in our health system, we will incorporate a VTE order set that is doable and user-friendly,” adds Dr. Maynard.
UCSD’s pharmacist-hospitalist collaboration also encourages residents from both disciplines to work together on integrating protocols into clinical care processes. The team hopes that the VTE protocol will go beyond the inpatient stay by wrapping the protocol into the discharge plan. Dr. Weibert’s anticoagulation and pulmonary embolism clinics also help “build on our strengths,” he says.
The second team is led by newcomers to the grant winner’s circle, Drs. Hroncich (pharmacist) and Adair (hospitalist) from Presbyterian Healthcare Services, Albuquerque, N.M. They base their research on this question: Is it more efficient for the system’s 34 hospitalists to screen out those at low risk of VTE than to screen everyone for high risk?
The investigators have been collecting baseline data on compliance with VTE screening since 2003. Hospitalist use of a VTE screening tool on admissions was 60%, improving to 88% with reminders. “The implication is that 12% of the hospitalists didn’t use the screening tool,” says Dr. Adair. “We found that they were resistant to another piece of paper.” PHS data also showed that seven out of 10 patients had some VTE risk, that co-morbidities and hospitalization increase VTE risk, and that the age at which patients fall prey to VTE is dropping to between 50 and 60.
For the ASHP grant, Drs. Hroncich and Adair will monitor VTE screening on admission to all PHS general medical units. All patients 18 or older admitted to those units during a three-month period will be routinely screened on admission for VTE risk. Drs. Hroncich and Adair will make two VTE-related admission order sets available to hospitalists to complete. The current screening tool is designed to identify patients at risk of developing a VTE based on the presence of risk factors. The second, shorter admission order set will contain a screening tool that assumes that all patients need VTE prophylaxis, except low-risk patients and those with VTE prophylaxis contraindications. “The shorter tool should take only one or two minutes to complete,” says Dr. Hroncich.
The PHS team hopes that the shorter screening tool will overcome resistance to VTE screening. Dr. Hroncich says there are many barriers to VTE screening. They include lack of consensus on the best screening tool on admission, the misperception that VTE isn’t a big problem, lack of reliable processes so at-risk patients don’t fall through the cracks, and a misperception that anti-coagulant therapy is dangerous.
“It’s one thing to treat COPD and heart failure,” adds Dr. Adair, “but if I can prevent VTE with less than a 60-second screening, I can prevent a disease state from happening.” TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Efficiency Rules
While nationwide demand for hospitalists outstrips supply, hospitals across the country are looking at how their hospitalists and their hospital medicine groups weigh in on efficiency.
The notion of efficiency at a time of rapid growth may seem counterintuitive, but healthcare dollars are always hotly contested, and an efficient hospitalist program has a better chance of capturing them than a less-efficient one.
Even the definition of efficiency is being refined. Stakeholders scrutinizing compensation packages, key clinical indicators, productivity and quality metrics, scheduling, average daily census, and patient handoffs to gauge whether or not their group has a competitive edge over others. And hospital medicine group (HMG) leaders are scrutinizing themselves because they know hospitals increasingly are inviting more than one HMG to work under their roofs—the better to serve different populations and compare one with another.
How to Measure Efficiency
An evolving medical discipline that aspires to specialize in internal medicine, hospital medicine is in the process of developing a consensus definition of efficiency for itself. Major variables included in the calculation are obvious: average daily census, length of stay (LOS), case mix-adjusted costs, severity, and readmission rates. Other, harder-to-quantify dimensions include how a hospitalist group practice affects mortality, and how scheduling, variable costs, hospitalist group type, subsidies, and level of expertise play out.
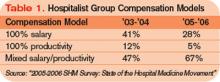
The foundation on which hospitalist groups build their efficiencies is the group type. In itself, how a hospitalist group chooses to organize itself reflects a maturing marketplace. SHM’s 2005-2006 productivity survey shows an increase in multistate hospitalist groups, up from 9% in ’03-’04 to 19% in the latest survey. Local private hospitalist groups fell from 20% in ’03-’04 to 12% in ’05-’06. The percentage of academic hospitalist groups rose from 16% to 20% in the same period.
It’s unclear how to interpret the shift from local to multistate hospitalist groups and the increase in academic medical center programs, but these trends bear watching. Comparison of the two most recent SHM surveys shows compensation models are also growing up, reflecting the need to balance base salary with productivity.
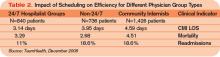
A major indicator of hospital group efficiency is the performance of groups with hospitalists on duty 24 hours a day, seven days a week. Although hospital administrators and hospitalist leaders struggle with the economics of providing night coverage when admissions are slow, such coverage pays off in quality and efficiency.
Stacy Goldsholl, MD, president of TeamHealth Hospital Medicine, a healthcare outsourcing firm based in Knoxville, Tenn., has long advocated 24/7 coverage as a crucial element in HMG efficiency. Even though she estimates that night coverage adds approximately $10,000 in subsidies to an average compensation package for a full-time hospitalist, such coverage improves efficiency in length of stay adjusted for severity and in readmissions. Full coverage allows hospitalists to be better integrated into the hospital in a way that fewer hours don’t.
“How hospitalists who cover 24/7 are used varies,” says Dr. Goldsholl. “Doing night admissions for community doctors, [working] as intensivist extenders, helping with ED [emergency department] throughput, being on rapid response teams—all are important contributors to improved efficiency,” says Dr. Goldsholl.
For Dr. Goldsholl, who has at least one academic medical center—Good Samaritan in Los Angeles at the University of Southern California Keck School of Medicine—on her roster, hospitalist group efficiency and productivity are major concerns for academic and community hospital administrators footing the bill for such services.
“Usually, TeamHealth is the exclusive hospitalist medicine provider contracting with a community hospital,” she explains. “Once we have been in a hospital for a while, we tend to see a progression in our responsibilities. Mostly we start with unassigned patients, then we expand to cover private primary care physicians’ patients. Then we co-manage complex cases with sub-specialists.”
Despite operating mostly in community hospitals, Dr. Goldsholl has fielded more queries from academic medical centers (AMCs) in the past several years.
“We’re definitely getting more interest from AMCs,” Dr. Goldsholl notes. “The work-hours restriction on residents—faculty who are uninterested in being hospitalists—whatever is driving their interest, they’re looking for solutions for handling their unassigned patients and beyond. To outsource to a private hospitalist company, an academic medical center would have to be in some pain, but interest is definitely picking up.”
Cogent Healthcare’s June 2006 contract with Temple University Hospital (TUH), Philadelphia, to provide a 24/7 hospitalist program of teaching and non-teaching services is another example of hospitals striving for efficiency. To better reach its clinical, economic, and regulatory goals, TUH switched from its own academic hospitalist group to partner with Cogent to manage its adult medical/surgical population. It’s too soon to gauge the results.
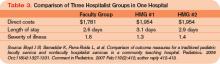
Despite stakeholders’ need to know more about which hospitalist group structure is most efficient, there’s little published data on AMC versus private group efficiency. One important study, published in the American Journal of Medicine (AJM) in May 2005, compared an academic hospitalist group with a private hospitalist group and community internists on several efficiency measures. The academic hospitalists’ patients had a 13% shorter LOS than those patients cared for by other groups and academic hospitalists had lowered costs by $173 per case, versus $109 for the private hospitalist group. The academic hospitalists also had a 20% relative risk reduction for severity of illness over the community physicians.
Lakshmi Halasyamani, MD, the AJM study’s lead author and chair of the Hospital Quality and Patient Safety Committee for SHM, speculated that the academic hospitalist groups’ efficiency resulted from fewer handoffs and that academic hospitalists’ relationships with their hospitals were more aligned than those of outsiders, both from financial and quality perspectives. Additionally, the academic hospitalist group used the hospital’s computerized physician order entry system and followed its protocols for clinical pathways and core measures. Scheduling also made a difference. The academic group worked in half-month blocks for an average of 14 weeks, while the private hospitalists worked from 8 a.m. to 6 p.m. on weekdays and some nights and weekends, leaving moonlighters to cover 75% of nights, weekends, and holidays and providing for rockier handoffs.
Another study comparing a traditional pediatric faculty group with two private hospitalist groups at St. Joseph’s Hospital and Medical Center of Phoenix showed that the faculty group outperformed the private hospitalists on all measures.
The authors concluded that faculty models can be as efficient as or more efficient than private groups in terms of direct costs and LOS.
Fine Tuning
Although academic hospitalist groups have been thought of as less efficient than private hospitalist groups because the former tend to use salaried employees while the latter tend to compensate employees based more on performance, the data cited above indicate academic hospitalist groups may have a competitive edge with regard to efficiency. What may account for the difference is that academic hospitalists are familiar with and often products of their hospital’s culture and mores. Unlike physicians working for private hospitalist groups with their own structure and culture, academic hospitalists are of a piece with their hospital. It’s common to find academic hospitalists who return to their medical school alma mater after a stint in an office-based practice. Some never left, joining the academic hospitalist group directly from residency.
For the chief of a hospitalist program, being so attuned to the hospital’s rhythms can be a mixed blessing.
Pat Cawley, MD, is the hospitalist program director and founder of the academic hospitalist group at the Charleston-based Medical University of South Carolina’s Hospital. He has a hard time focusing on hospitalist group efficiency, though, when he’s still flat-out recruiting.
“Demand for hospitalists is still way outstripping supply,” says Dr. Cawley. “We currently have nine hospitalists and plan to add five more this year, but we could actually use 10 more.”
The South Carolina market is competitive, with other hospitals planning to establish hospitalist medicine programs and vying with Dr. Cawley’s program for fresh physicians. Medical University Hospital’s hospitalist group started in July 2003 with four physicians and has kept growing. The hospitalists spend most of their time functioning as a teaching service and also cover a long-term acute-care facility at another hospital.
Defining efficiency in South Carolina’s booming market is secondary to recruiting and incorporating new physicians as team members. Dr. Cawley uses average daily census (ADC) as an efficiency benchmark: 15-20 patients per hospitalist is productive, although many doctors are comfortable at 12.
“We looked at our learning curve, about 10-12,” points out Dr. Cawley. “We think 15-20 is better, although some places are reporting an ADC of 22. But after a certain point, performance doesn’t appear to improve.”
A big problem with improving hospitalist group efficiency, according to Dr. Cawley, is hospital inefficiency: “Lack of IT to get lab results quickly, not enough nursing and secretarial support for admissions and discharges, policies on contacting the primary doc versus having a standing order for a procedure—all decrease efficiency.”
He’d also like his hospital administrators to allow nurses to pronounce death (common in community hospitals but less so in AMCs). “The power of hospitalists is to challenge the hospital’s inefficiencies, to break down the barriers to more efficient practices,” adds Dr. Cawley. “Many institutions need huge culture change, and hospitalists must lead the way.”
A close watcher of hospitalist performance, Scott Oxenhandler, MD, medical director of the Memorial Hospitalist Group in Hollywood, Fla., heads a hospitalist group he started in June 2004 that now has 23 physicians and two nurse practitioners. Memorial Hospital also has two other private hospitalist groups. While Dr. Oxenhandler’s group handles unassigned patients (55%) and Medicaid/Medicare patients (45%), the other hospitalist groups have captured the more lucrative business of managed care and other commercially insured patients.
—Per Danielsson, MD, medical director, Swedish Medical Center Adult Hospitalist Program, Seattle
Dr. Oxenhandler says efficiency is a complicated issue involving several key components. “Following evidence-based medicine protocols and CMS core measures are fairly straightforward [ideas] for all of us,” he says, “but financial measures are more complex.”
He has taken aim at adjusted variable costs per discharge on lab tests, pharmacy, and radiology, “three areas where I know that our group can improve,” he adds.
As for how hard and how efficiently a hospitalist works, Dr. Oxenhandler is taking a closer look at that as his group and the field mature. “We know that average daily census can be deceiving and RVUs [relative value units] are more relevant to efficiency but not perfect,” he says. “Another factor is tenure with the hospitalist group. For the physician to excel and to mature clinically, he or she needs to stay with a hospitalist group long enough to improve readmission rates and to get a sense of how to better manage clinical resources.’’
Dr. Oxenhandler describes a patient presenting with heart failure and anemia to show how a hospitalist’s clinical skills might mature. After several days of repeated hemoglobin studies indicating anemia, the hospitalist might refer the patient—once stabilized and discharged—to his primary physician for an outpatient work-up for possible colon cancer—rather than do so during the hospitalization.
Dr. Oxenhandler has contemplated pursuing managed care contracts but hesitates because his hospitalist group’s clinical and cost performance is equal to that of the hospitalist group that currently holds such contracts. “Why should they switch to us unless we can outperform the other group?” he muses. “Plus, there would be added cost for us in more paperwork and administration, and we’d have to improve our efficiency to make it worthwhile.”
Per Danielsson, MD, Swedish Medical Center’s Adult Hospitalist Program’s medical director, has hospitalists rotating among the First Hill, Cherry Hill, and Ballard campuses in Seattle, Wash. Demand for hospitalist services at the sites keeps growing, and Dr. Danielsson sees no end in sight. “Today’s hospital stays are getting shorter, and the patients are sicker, and there is increasing pressure for greater efficiency here,” he says.
Overall, clinicians, administrators, and researchers need to zero in on the organizational factors of hospitalist groups—from scheduling to 24/7 coverage, handoffs, and use of in-hospital resources—to improve efficiency. At present, academic hospitalist groups appear to have a slight edge because they’re tied more closely to hospital personnel, technology, and care pathways than private groups that come from outside the hospital. But there isn’t enough data either way to say which group type is the most efficient. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
While nationwide demand for hospitalists outstrips supply, hospitals across the country are looking at how their hospitalists and their hospital medicine groups weigh in on efficiency.
The notion of efficiency at a time of rapid growth may seem counterintuitive, but healthcare dollars are always hotly contested, and an efficient hospitalist program has a better chance of capturing them than a less-efficient one.
Even the definition of efficiency is being refined. Stakeholders scrutinizing compensation packages, key clinical indicators, productivity and quality metrics, scheduling, average daily census, and patient handoffs to gauge whether or not their group has a competitive edge over others. And hospital medicine group (HMG) leaders are scrutinizing themselves because they know hospitals increasingly are inviting more than one HMG to work under their roofs—the better to serve different populations and compare one with another.
How to Measure Efficiency
An evolving medical discipline that aspires to specialize in internal medicine, hospital medicine is in the process of developing a consensus definition of efficiency for itself. Major variables included in the calculation are obvious: average daily census, length of stay (LOS), case mix-adjusted costs, severity, and readmission rates. Other, harder-to-quantify dimensions include how a hospitalist group practice affects mortality, and how scheduling, variable costs, hospitalist group type, subsidies, and level of expertise play out.
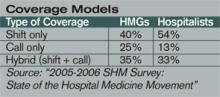
The foundation on which hospitalist groups build their efficiencies is the group type. In itself, how a hospitalist group chooses to organize itself reflects a maturing marketplace. SHM’s 2005-2006 productivity survey shows an increase in multistate hospitalist groups, up from 9% in ’03-’04 to 19% in the latest survey. Local private hospitalist groups fell from 20% in ’03-’04 to 12% in ’05-’06. The percentage of academic hospitalist groups rose from 16% to 20% in the same period.
It’s unclear how to interpret the shift from local to multistate hospitalist groups and the increase in academic medical center programs, but these trends bear watching. Comparison of the two most recent SHM surveys shows compensation models are also growing up, reflecting the need to balance base salary with productivity.
A major indicator of hospital group efficiency is the performance of groups with hospitalists on duty 24 hours a day, seven days a week. Although hospital administrators and hospitalist leaders struggle with the economics of providing night coverage when admissions are slow, such coverage pays off in quality and efficiency.
Stacy Goldsholl, MD, president of TeamHealth Hospital Medicine, a healthcare outsourcing firm based in Knoxville, Tenn., has long advocated 24/7 coverage as a crucial element in HMG efficiency. Even though she estimates that night coverage adds approximately $10,000 in subsidies to an average compensation package for a full-time hospitalist, such coverage improves efficiency in length of stay adjusted for severity and in readmissions. Full coverage allows hospitalists to be better integrated into the hospital in a way that fewer hours don’t.
“How hospitalists who cover 24/7 are used varies,” says Dr. Goldsholl. “Doing night admissions for community doctors, [working] as intensivist extenders, helping with ED [emergency department] throughput, being on rapid response teams—all are important contributors to improved efficiency,” says Dr. Goldsholl.
For Dr. Goldsholl, who has at least one academic medical center—Good Samaritan in Los Angeles at the University of Southern California Keck School of Medicine—on her roster, hospitalist group efficiency and productivity are major concerns for academic and community hospital administrators footing the bill for such services.
“Usually, TeamHealth is the exclusive hospitalist medicine provider contracting with a community hospital,” she explains. “Once we have been in a hospital for a while, we tend to see a progression in our responsibilities. Mostly we start with unassigned patients, then we expand to cover private primary care physicians’ patients. Then we co-manage complex cases with sub-specialists.”
Despite operating mostly in community hospitals, Dr. Goldsholl has fielded more queries from academic medical centers (AMCs) in the past several years.
“We’re definitely getting more interest from AMCs,” Dr. Goldsholl notes. “The work-hours restriction on residents—faculty who are uninterested in being hospitalists—whatever is driving their interest, they’re looking for solutions for handling their unassigned patients and beyond. To outsource to a private hospitalist company, an academic medical center would have to be in some pain, but interest is definitely picking up.”
Cogent Healthcare’s June 2006 contract with Temple University Hospital (TUH), Philadelphia, to provide a 24/7 hospitalist program of teaching and non-teaching services is another example of hospitals striving for efficiency. To better reach its clinical, economic, and regulatory goals, TUH switched from its own academic hospitalist group to partner with Cogent to manage its adult medical/surgical population. It’s too soon to gauge the results.
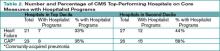
Despite stakeholders’ need to know more about which hospitalist group structure is most efficient, there’s little published data on AMC versus private group efficiency. One important study, published in the American Journal of Medicine (AJM) in May 2005, compared an academic hospitalist group with a private hospitalist group and community internists on several efficiency measures. The academic hospitalists’ patients had a 13% shorter LOS than those patients cared for by other groups and academic hospitalists had lowered costs by $173 per case, versus $109 for the private hospitalist group. The academic hospitalists also had a 20% relative risk reduction for severity of illness over the community physicians.
Lakshmi Halasyamani, MD, the AJM study’s lead author and chair of the Hospital Quality and Patient Safety Committee for SHM, speculated that the academic hospitalist groups’ efficiency resulted from fewer handoffs and that academic hospitalists’ relationships with their hospitals were more aligned than those of outsiders, both from financial and quality perspectives. Additionally, the academic hospitalist group used the hospital’s computerized physician order entry system and followed its protocols for clinical pathways and core measures. Scheduling also made a difference. The academic group worked in half-month blocks for an average of 14 weeks, while the private hospitalists worked from 8 a.m. to 6 p.m. on weekdays and some nights and weekends, leaving moonlighters to cover 75% of nights, weekends, and holidays and providing for rockier handoffs.
Another study comparing a traditional pediatric faculty group with two private hospitalist groups at St. Joseph’s Hospital and Medical Center of Phoenix showed that the faculty group outperformed the private hospitalists on all measures.
The authors concluded that faculty models can be as efficient as or more efficient than private groups in terms of direct costs and LOS.
Fine Tuning
Although academic hospitalist groups have been thought of as less efficient than private hospitalist groups because the former tend to use salaried employees while the latter tend to compensate employees based more on performance, the data cited above indicate academic hospitalist groups may have a competitive edge with regard to efficiency. What may account for the difference is that academic hospitalists are familiar with and often products of their hospital’s culture and mores. Unlike physicians working for private hospitalist groups with their own structure and culture, academic hospitalists are of a piece with their hospital. It’s common to find academic hospitalists who return to their medical school alma mater after a stint in an office-based practice. Some never left, joining the academic hospitalist group directly from residency.
For the chief of a hospitalist program, being so attuned to the hospital’s rhythms can be a mixed blessing.
Pat Cawley, MD, is the hospitalist program director and founder of the academic hospitalist group at the Charleston-based Medical University of South Carolina’s Hospital. He has a hard time focusing on hospitalist group efficiency, though, when he’s still flat-out recruiting.
“Demand for hospitalists is still way outstripping supply,” says Dr. Cawley. “We currently have nine hospitalists and plan to add five more this year, but we could actually use 10 more.”
The South Carolina market is competitive, with other hospitals planning to establish hospitalist medicine programs and vying with Dr. Cawley’s program for fresh physicians. Medical University Hospital’s hospitalist group started in July 2003 with four physicians and has kept growing. The hospitalists spend most of their time functioning as a teaching service and also cover a long-term acute-care facility at another hospital.
Defining efficiency in South Carolina’s booming market is secondary to recruiting and incorporating new physicians as team members. Dr. Cawley uses average daily census (ADC) as an efficiency benchmark: 15-20 patients per hospitalist is productive, although many doctors are comfortable at 12.
“We looked at our learning curve, about 10-12,” points out Dr. Cawley. “We think 15-20 is better, although some places are reporting an ADC of 22. But after a certain point, performance doesn’t appear to improve.”
A big problem with improving hospitalist group efficiency, according to Dr. Cawley, is hospital inefficiency: “Lack of IT to get lab results quickly, not enough nursing and secretarial support for admissions and discharges, policies on contacting the primary doc versus having a standing order for a procedure—all decrease efficiency.”
He’d also like his hospital administrators to allow nurses to pronounce death (common in community hospitals but less so in AMCs). “The power of hospitalists is to challenge the hospital’s inefficiencies, to break down the barriers to more efficient practices,” adds Dr. Cawley. “Many institutions need huge culture change, and hospitalists must lead the way.”
A close watcher of hospitalist performance, Scott Oxenhandler, MD, medical director of the Memorial Hospitalist Group in Hollywood, Fla., heads a hospitalist group he started in June 2004 that now has 23 physicians and two nurse practitioners. Memorial Hospital also has two other private hospitalist groups. While Dr. Oxenhandler’s group handles unassigned patients (55%) and Medicaid/Medicare patients (45%), the other hospitalist groups have captured the more lucrative business of managed care and other commercially insured patients.
—Per Danielsson, MD, medical director, Swedish Medical Center Adult Hospitalist Program, Seattle
Dr. Oxenhandler says efficiency is a complicated issue involving several key components. “Following evidence-based medicine protocols and CMS core measures are fairly straightforward [ideas] for all of us,” he says, “but financial measures are more complex.”
He has taken aim at adjusted variable costs per discharge on lab tests, pharmacy, and radiology, “three areas where I know that our group can improve,” he adds.
As for how hard and how efficiently a hospitalist works, Dr. Oxenhandler is taking a closer look at that as his group and the field mature. “We know that average daily census can be deceiving and RVUs [relative value units] are more relevant to efficiency but not perfect,” he says. “Another factor is tenure with the hospitalist group. For the physician to excel and to mature clinically, he or she needs to stay with a hospitalist group long enough to improve readmission rates and to get a sense of how to better manage clinical resources.’’
Dr. Oxenhandler describes a patient presenting with heart failure and anemia to show how a hospitalist’s clinical skills might mature. After several days of repeated hemoglobin studies indicating anemia, the hospitalist might refer the patient—once stabilized and discharged—to his primary physician for an outpatient work-up for possible colon cancer—rather than do so during the hospitalization.
Dr. Oxenhandler has contemplated pursuing managed care contracts but hesitates because his hospitalist group’s clinical and cost performance is equal to that of the hospitalist group that currently holds such contracts. “Why should they switch to us unless we can outperform the other group?” he muses. “Plus, there would be added cost for us in more paperwork and administration, and we’d have to improve our efficiency to make it worthwhile.”
Per Danielsson, MD, Swedish Medical Center’s Adult Hospitalist Program’s medical director, has hospitalists rotating among the First Hill, Cherry Hill, and Ballard campuses in Seattle, Wash. Demand for hospitalist services at the sites keeps growing, and Dr. Danielsson sees no end in sight. “Today’s hospital stays are getting shorter, and the patients are sicker, and there is increasing pressure for greater efficiency here,” he says.
Overall, clinicians, administrators, and researchers need to zero in on the organizational factors of hospitalist groups—from scheduling to 24/7 coverage, handoffs, and use of in-hospital resources—to improve efficiency. At present, academic hospitalist groups appear to have a slight edge because they’re tied more closely to hospital personnel, technology, and care pathways than private groups that come from outside the hospital. But there isn’t enough data either way to say which group type is the most efficient. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
While nationwide demand for hospitalists outstrips supply, hospitals across the country are looking at how their hospitalists and their hospital medicine groups weigh in on efficiency.
The notion of efficiency at a time of rapid growth may seem counterintuitive, but healthcare dollars are always hotly contested, and an efficient hospitalist program has a better chance of capturing them than a less-efficient one.
Even the definition of efficiency is being refined. Stakeholders scrutinizing compensation packages, key clinical indicators, productivity and quality metrics, scheduling, average daily census, and patient handoffs to gauge whether or not their group has a competitive edge over others. And hospital medicine group (HMG) leaders are scrutinizing themselves because they know hospitals increasingly are inviting more than one HMG to work under their roofs—the better to serve different populations and compare one with another.
How to Measure Efficiency
An evolving medical discipline that aspires to specialize in internal medicine, hospital medicine is in the process of developing a consensus definition of efficiency for itself. Major variables included in the calculation are obvious: average daily census, length of stay (LOS), case mix-adjusted costs, severity, and readmission rates. Other, harder-to-quantify dimensions include how a hospitalist group practice affects mortality, and how scheduling, variable costs, hospitalist group type, subsidies, and level of expertise play out.
The foundation on which hospitalist groups build their efficiencies is the group type. In itself, how a hospitalist group chooses to organize itself reflects a maturing marketplace. SHM’s 2005-2006 productivity survey shows an increase in multistate hospitalist groups, up from 9% in ’03-’04 to 19% in the latest survey. Local private hospitalist groups fell from 20% in ’03-’04 to 12% in ’05-’06. The percentage of academic hospitalist groups rose from 16% to 20% in the same period.
It’s unclear how to interpret the shift from local to multistate hospitalist groups and the increase in academic medical center programs, but these trends bear watching. Comparison of the two most recent SHM surveys shows compensation models are also growing up, reflecting the need to balance base salary with productivity.
A major indicator of hospital group efficiency is the performance of groups with hospitalists on duty 24 hours a day, seven days a week. Although hospital administrators and hospitalist leaders struggle with the economics of providing night coverage when admissions are slow, such coverage pays off in quality and efficiency.
Stacy Goldsholl, MD, president of TeamHealth Hospital Medicine, a healthcare outsourcing firm based in Knoxville, Tenn., has long advocated 24/7 coverage as a crucial element in HMG efficiency. Even though she estimates that night coverage adds approximately $10,000 in subsidies to an average compensation package for a full-time hospitalist, such coverage improves efficiency in length of stay adjusted for severity and in readmissions. Full coverage allows hospitalists to be better integrated into the hospital in a way that fewer hours don’t.
“How hospitalists who cover 24/7 are used varies,” says Dr. Goldsholl. “Doing night admissions for community doctors, [working] as intensivist extenders, helping with ED [emergency department] throughput, being on rapid response teams—all are important contributors to improved efficiency,” says Dr. Goldsholl.
For Dr. Goldsholl, who has at least one academic medical center—Good Samaritan in Los Angeles at the University of Southern California Keck School of Medicine—on her roster, hospitalist group efficiency and productivity are major concerns for academic and community hospital administrators footing the bill for such services.
“Usually, TeamHealth is the exclusive hospitalist medicine provider contracting with a community hospital,” she explains. “Once we have been in a hospital for a while, we tend to see a progression in our responsibilities. Mostly we start with unassigned patients, then we expand to cover private primary care physicians’ patients. Then we co-manage complex cases with sub-specialists.”
Despite operating mostly in community hospitals, Dr. Goldsholl has fielded more queries from academic medical centers (AMCs) in the past several years.
“We’re definitely getting more interest from AMCs,” Dr. Goldsholl notes. “The work-hours restriction on residents—faculty who are uninterested in being hospitalists—whatever is driving their interest, they’re looking for solutions for handling their unassigned patients and beyond. To outsource to a private hospitalist company, an academic medical center would have to be in some pain, but interest is definitely picking up.”
Cogent Healthcare’s June 2006 contract with Temple University Hospital (TUH), Philadelphia, to provide a 24/7 hospitalist program of teaching and non-teaching services is another example of hospitals striving for efficiency. To better reach its clinical, economic, and regulatory goals, TUH switched from its own academic hospitalist group to partner with Cogent to manage its adult medical/surgical population. It’s too soon to gauge the results.
Despite stakeholders’ need to know more about which hospitalist group structure is most efficient, there’s little published data on AMC versus private group efficiency. One important study, published in the American Journal of Medicine (AJM) in May 2005, compared an academic hospitalist group with a private hospitalist group and community internists on several efficiency measures. The academic hospitalists’ patients had a 13% shorter LOS than those patients cared for by other groups and academic hospitalists had lowered costs by $173 per case, versus $109 for the private hospitalist group. The academic hospitalists also had a 20% relative risk reduction for severity of illness over the community physicians.
Lakshmi Halasyamani, MD, the AJM study’s lead author and chair of the Hospital Quality and Patient Safety Committee for SHM, speculated that the academic hospitalist groups’ efficiency resulted from fewer handoffs and that academic hospitalists’ relationships with their hospitals were more aligned than those of outsiders, both from financial and quality perspectives. Additionally, the academic hospitalist group used the hospital’s computerized physician order entry system and followed its protocols for clinical pathways and core measures. Scheduling also made a difference. The academic group worked in half-month blocks for an average of 14 weeks, while the private hospitalists worked from 8 a.m. to 6 p.m. on weekdays and some nights and weekends, leaving moonlighters to cover 75% of nights, weekends, and holidays and providing for rockier handoffs.
Another study comparing a traditional pediatric faculty group with two private hospitalist groups at St. Joseph’s Hospital and Medical Center of Phoenix showed that the faculty group outperformed the private hospitalists on all measures.
The authors concluded that faculty models can be as efficient as or more efficient than private groups in terms of direct costs and LOS.
Fine Tuning
Although academic hospitalist groups have been thought of as less efficient than private hospitalist groups because the former tend to use salaried employees while the latter tend to compensate employees based more on performance, the data cited above indicate academic hospitalist groups may have a competitive edge with regard to efficiency. What may account for the difference is that academic hospitalists are familiar with and often products of their hospital’s culture and mores. Unlike physicians working for private hospitalist groups with their own structure and culture, academic hospitalists are of a piece with their hospital. It’s common to find academic hospitalists who return to their medical school alma mater after a stint in an office-based practice. Some never left, joining the academic hospitalist group directly from residency.
For the chief of a hospitalist program, being so attuned to the hospital’s rhythms can be a mixed blessing.
Pat Cawley, MD, is the hospitalist program director and founder of the academic hospitalist group at the Charleston-based Medical University of South Carolina’s Hospital. He has a hard time focusing on hospitalist group efficiency, though, when he’s still flat-out recruiting.
“Demand for hospitalists is still way outstripping supply,” says Dr. Cawley. “We currently have nine hospitalists and plan to add five more this year, but we could actually use 10 more.”
The South Carolina market is competitive, with other hospitals planning to establish hospitalist medicine programs and vying with Dr. Cawley’s program for fresh physicians. Medical University Hospital’s hospitalist group started in July 2003 with four physicians and has kept growing. The hospitalists spend most of their time functioning as a teaching service and also cover a long-term acute-care facility at another hospital.
Defining efficiency in South Carolina’s booming market is secondary to recruiting and incorporating new physicians as team members. Dr. Cawley uses average daily census (ADC) as an efficiency benchmark: 15-20 patients per hospitalist is productive, although many doctors are comfortable at 12.
“We looked at our learning curve, about 10-12,” points out Dr. Cawley. “We think 15-20 is better, although some places are reporting an ADC of 22. But after a certain point, performance doesn’t appear to improve.”
A big problem with improving hospitalist group efficiency, according to Dr. Cawley, is hospital inefficiency: “Lack of IT to get lab results quickly, not enough nursing and secretarial support for admissions and discharges, policies on contacting the primary doc versus having a standing order for a procedure—all decrease efficiency.”
He’d also like his hospital administrators to allow nurses to pronounce death (common in community hospitals but less so in AMCs). “The power of hospitalists is to challenge the hospital’s inefficiencies, to break down the barriers to more efficient practices,” adds Dr. Cawley. “Many institutions need huge culture change, and hospitalists must lead the way.”
A close watcher of hospitalist performance, Scott Oxenhandler, MD, medical director of the Memorial Hospitalist Group in Hollywood, Fla., heads a hospitalist group he started in June 2004 that now has 23 physicians and two nurse practitioners. Memorial Hospital also has two other private hospitalist groups. While Dr. Oxenhandler’s group handles unassigned patients (55%) and Medicaid/Medicare patients (45%), the other hospitalist groups have captured the more lucrative business of managed care and other commercially insured patients.
—Per Danielsson, MD, medical director, Swedish Medical Center Adult Hospitalist Program, Seattle
Dr. Oxenhandler says efficiency is a complicated issue involving several key components. “Following evidence-based medicine protocols and CMS core measures are fairly straightforward [ideas] for all of us,” he says, “but financial measures are more complex.”
He has taken aim at adjusted variable costs per discharge on lab tests, pharmacy, and radiology, “three areas where I know that our group can improve,” he adds.
As for how hard and how efficiently a hospitalist works, Dr. Oxenhandler is taking a closer look at that as his group and the field mature. “We know that average daily census can be deceiving and RVUs [relative value units] are more relevant to efficiency but not perfect,” he says. “Another factor is tenure with the hospitalist group. For the physician to excel and to mature clinically, he or she needs to stay with a hospitalist group long enough to improve readmission rates and to get a sense of how to better manage clinical resources.’’
Dr. Oxenhandler describes a patient presenting with heart failure and anemia to show how a hospitalist’s clinical skills might mature. After several days of repeated hemoglobin studies indicating anemia, the hospitalist might refer the patient—once stabilized and discharged—to his primary physician for an outpatient work-up for possible colon cancer—rather than do so during the hospitalization.
Dr. Oxenhandler has contemplated pursuing managed care contracts but hesitates because his hospitalist group’s clinical and cost performance is equal to that of the hospitalist group that currently holds such contracts. “Why should they switch to us unless we can outperform the other group?” he muses. “Plus, there would be added cost for us in more paperwork and administration, and we’d have to improve our efficiency to make it worthwhile.”
Per Danielsson, MD, Swedish Medical Center’s Adult Hospitalist Program’s medical director, has hospitalists rotating among the First Hill, Cherry Hill, and Ballard campuses in Seattle, Wash. Demand for hospitalist services at the sites keeps growing, and Dr. Danielsson sees no end in sight. “Today’s hospital stays are getting shorter, and the patients are sicker, and there is increasing pressure for greater efficiency here,” he says.
Overall, clinicians, administrators, and researchers need to zero in on the organizational factors of hospitalist groups—from scheduling to 24/7 coverage, handoffs, and use of in-hospital resources—to improve efficiency. At present, academic hospitalist groups appear to have a slight edge because they’re tied more closely to hospital personnel, technology, and care pathways than private groups that come from outside the hospital. But there isn’t enough data either way to say which group type is the most efficient. TH
Marlene Piturro is a frequent contributor to The Hospitalist.
Homegrown Health
Tucked away in the University of Florida (UF), which is—with 50,000 students—the state’s largest university and the nation’s fourth largest, is its School of Medicine’s Community Health and Family Medicine (CHFM) department, along with that department’s hospital medicine program. The department remains a touchstone for its graduates, past and present, and has created hospitalist leaders to be proud of. Much of that pride emanates from R. Whit Curry Jr., MD, CHFM’s department chairman, who is a friend and mentor to several generations of family medicine physicians.
In late 2001, after a private hospital medicine group headed by John Nelson, MD, a UF graduate, SHM co-founder and columnist for this publication, it was natural for Shands Alachua General Hospital (SAGH) to turn to Dr. Curry to start a hospitalist program. Dr. Curry, who says wryly, “If you’ve seen one hospitalist program, you’ve seen one hospitalist program,” knew he could build a unique team of family medicine physicians into a cohesive hospital medicine group.
UF’s CHFM department had staffed SAGH with residents for years before the hospital asked Dr. Curry to start the hospitalist program. The group’s coverage had been limited to inpatient care for about 20 primary care physicians, with a similar arrangement for a for-profit HCA community hospital across town. SAGH needed a more ambitious hospitalist program, one that would cover unassigned patients as well as inpatient care for local doctors. At that point, SAGH issued a request for proposals (RFP) for a hospital medicine group, accepting UF’s CHFM proposal to fill the vacuum left by the departing group. Initially, SAGH would handle the 20 private physicians’ inpatients covered by the existing group, the overflow of unassigned patients from residency workload restrictions, and admitting and co-management for specialists.
Dr. Curry started building his team with Elizabeth Chmelik, MD, recruiting her as the program’s director straight from CHFM residency. The program’s first year—2002—was whirlwind hectic. Fortunately for the group, Marcia Miller, MD, a 1988 graduate of UF’s CHFM department, had burned herself out running a local private practice with two partners. She turned to Dr. Curry, her mentor and confidant. “I called him, told him I needed a job, and he hired me as the hospitalist program’s co-director,” says Dr. Miller. Her community-based partners endorsed her new career path, and she joined Dr. Chmelik in working every day of the program’s first year. “It was challenging,” she says, “but, with inpatient medicine, I became the doctor I was trained to be.”
Sherri Swilley, the department’s coordinator of administrative affairs, recalls the patient census growing so fast that she struggled to keep up with getting doctors temporary privileges while pursuing credentialing for the permanent staff. “The hospitalists had a fierce work ethic that carried us through those early years,” says Swilley.
Gainesville’s Medical Community
In spring 2003, the program added a local physician eager to exit private practice and a family medicine graduate who had worked in SAGH’s emergency department (ED) for 12 years. In June, they snagged two stellar family medicine graduates and a nocturnist. The nocturnist represents the program’s only turnover; her nightly 12 to 20 admissions proved too much to handle.
UF’s homegrown bunch of family physicians shaped this distinctive hospital medicine program. Dr. Chmelik, assistant professor and co-director of the UF College of Medicine’s hospitalist program at SAGH, says that although family physicians are outnumbered by internal medicine hospitalist physicians they add something special to the role.
“We want to go beyond the stereotype of the internal-medicine trained physician drudging through the hospital as an eternal extension of residency,” says Dr. Chmelik. “Family physicians excel at end-of-life issues and the biopsychosocial model of healthcare, both of which are very important in a hospital.”
Another addition to Dr. Chmelik’s black bag is her expert consulting on obstetric and pediatric patients; she can easily handle issues such as hypertension in a postpartum patient or post-appendectomy asthma in a child.
The Financial Tightrope
The University of Florida’s CHFM is closely tied to SAGH, a 75-year-old, 367-bed community hospital that serves as its training ground for residents and hospitalist fellows. Although SAGH is a vital part of Gainesville’s medical scene, its financial status has been shaky for some time.
In 2002, Moody’s Investor Service gave SAGH a negative rating, which was upgraded to stable in 2003.The upgrade of SAGH’s $312 million of outstanding debt issued by Alachua County Health Facilities Authority kept the wolf from the door temporarily. Talk persists that SAGH is in trouble, however, and a Gainesville group, the Health Care Is a Human Right Coalition, asserted in July 2006 that the hospital lacked leadership and that “there are no published plans to keep SAGH open beyond 2010.” SAGH spokesman Ralph Ives says, “Nothing could be further from the truth.” He points to SAGH’s investment in an 82-bed pediatric hospital in a renovated wing with its own hospital medicine group as an affirmation of the institution’s future.
Like other hospitals struggling with public payers and lots of unassigned patients, SAGH’s hospitalist program improves the hospital’s financial health by serving large numbers of patients cost-effectively. Conversely, hospitalist programs can sink because of inattention to financial basics. Early in SAGH’s history, the hospitalists were overwhelmed with a burgeoning census, leaving coding and billing for clerical staff to figure out at day’s end. This delayed billing and often failed to capture the correct diagnostic codes and level of severity for each patient encounter. As the program matured, the hospitalists and hospital administration agreed that physicians would do the coding themselves as they rounded. That change saved on the back end of clerical work and got the charges in promptly.
Each month, Swilley and the hospitalists review individual and group coding patterns, payer mix, the amount billed to each carrier, the amount of time bills spend in accounts receivable, and the services that have been denied. Hospitalists also receive daily reports on their charges and tips on improving coding. For example, if they’ve reviewed documents, Swilley reminds them to code that activity, just as she does a hospitalist who was swamped in the ED at 10 p.m. and left coding his encounters until 1 a.m., thereby losing one day of service. “A hospital is a business. Our hospitalists work hard; I teach them to work smarter and to pay attention to the bottom line,” says Swilley.
Being diligent about financial productivity matters greatly when it’s time for the CHFM department to negotiate with the hospital for its annual subsidy, which Dr. Curry says is about $500,000.
“When we present our budget, we include billing expenses, overhead, salary, and fringe benefits,” says Swilley. “The more detail we have on the number of patient encounters, [our] productivity, and the revenues we generate, the better position we’re in to get support.”
Like most other hospitals, SAGH struggles with tight reimbursement versus the need for an attractive physical plant. To that end, in 1998 it became the first hospital in Florida to adopt the Planetree model, which advocates patient-driven healthcare, serving body, mind, and spirit. “We’ve always been a deeply compassionate hospital,” says Lynne Mercadante, RN, SAGH’s director of Medical Staff Services, “and Planetree is a natural extension of our looking into our hearts and minds about treating the whole person.”
The hospitalists are deeply connected to the community, knowing when to bring in pastoral care or family therapy, as well as joining in celebrations for weddings and anniversaries.
SAGH has made typical Planetree physical changes, including remodeling one floor into six-patient nursing pods versus one nursing station for 42 patients, along with adding meditation rooms, libraries, a piano in the lobby, and a fish tank. Physicians, patients, and visitors are treated to Brahms’ Lullaby over the loudspeaker system every time a baby is born and can experience pet visitations and aromatherapy.
The Schedule
UF’s hospitalists initially adopted a rotation of seven days on, seven days off. When the group’s nocturnist left because of the heavy burden of night admissions, the nine hospitalists decided to cover call themselves instead of hiring a replacement nocturnist. Every ninth week, a hospitalist takes call Monday through Thursday, with residents carrying the weekend. It isn’t ideal, but it distributes call evenly and ensures hospitalists two free weekends a month.
Like most hospital medicine groups, UF’s hospitalists are trying to tinker with the schedule to make it more flexible. They had some give for Scott Medley, MD, who retired from his large Gainesville private practice of 10 physicians, 65 employees, five offices, and 40,000 patients in 2002 at age 55.
“My private [practice] kept me busy seven days a week. I had been there, done that, got the T-shirt,” says Dr. Medley. “I had enough of private practice, but I didn’t want to leave medicine. On reflection, I realized that what I enjoyed most is taking care of really sick patients, so I contacted Whit Curry, and he hired me as a hospitalist Monday through Friday mornings.”
Dr. Medley loves being an employee, doesn’t mind covering for younger colleagues on holidays, and is now collaborating with specialists who have been his friends and colleagues for 25 years. “I also enjoy teaching younger docs both the art and the economics of medicine—and not having to worry where my next paycheck is coming from,” he says.
Looking ahead, Dr. Miller relishes being a hospitalist at age 47, but wonders what the pace will feel like another decade out. To be more flexible, the group is considering allowing physicians to work more days but fewer hours, initiating job sharing, and recruiting more retirees like Dr. Medley, who can work shorter days and are willing to pinch-hit when coverage is tight. They are working toward consensus on maximizing flexibility while maintaining coverage. Still, there’s no easy solution to fluctuations in census, and Dr. Curry notes that some days span 7:30 a.m. to 3:30 p.m., while others stretch into the night. “We haven’t found a better solution yet to providing care 24 hours a day, 365 days a year,” concludes Dr. Medley.
Creating Value
Looking back at her quarter century at SAGH, Mercadante analyzes how the hospitalist medicine program improved things. “Without hospitalists, whoever was on call covered everyone in the ED, so you had neurologists treating patients with pneumonia. There was little continuity of care, unlike with the hospitalists who meet every morning discussing cases.”
In addition, the medical staff feel they have their lives back because call is covered, and they can count on the hospitalists to co-manage complicated cases. “When specialty physicians are in high demand and short supply, knowing that someone’s covering their hospitalized patients for chronic conditions is so important,” concludes Mercadante.
Looking to the future, UF’s hospitalists plan to build on their cohesiveness, collegiality, and emphasis on family medicine. With alumni of their school at the ready, they know where to turn to continue to grow the program. TH
Marlene Piturro also writes about scheduling in this issue.
Tucked away in the University of Florida (UF), which is—with 50,000 students—the state’s largest university and the nation’s fourth largest, is its School of Medicine’s Community Health and Family Medicine (CHFM) department, along with that department’s hospital medicine program. The department remains a touchstone for its graduates, past and present, and has created hospitalist leaders to be proud of. Much of that pride emanates from R. Whit Curry Jr., MD, CHFM’s department chairman, who is a friend and mentor to several generations of family medicine physicians.
In late 2001, after a private hospital medicine group headed by John Nelson, MD, a UF graduate, SHM co-founder and columnist for this publication, it was natural for Shands Alachua General Hospital (SAGH) to turn to Dr. Curry to start a hospitalist program. Dr. Curry, who says wryly, “If you’ve seen one hospitalist program, you’ve seen one hospitalist program,” knew he could build a unique team of family medicine physicians into a cohesive hospital medicine group.
UF’s CHFM department had staffed SAGH with residents for years before the hospital asked Dr. Curry to start the hospitalist program. The group’s coverage had been limited to inpatient care for about 20 primary care physicians, with a similar arrangement for a for-profit HCA community hospital across town. SAGH needed a more ambitious hospitalist program, one that would cover unassigned patients as well as inpatient care for local doctors. At that point, SAGH issued a request for proposals (RFP) for a hospital medicine group, accepting UF’s CHFM proposal to fill the vacuum left by the departing group. Initially, SAGH would handle the 20 private physicians’ inpatients covered by the existing group, the overflow of unassigned patients from residency workload restrictions, and admitting and co-management for specialists.
Dr. Curry started building his team with Elizabeth Chmelik, MD, recruiting her as the program’s director straight from CHFM residency. The program’s first year—2002—was whirlwind hectic. Fortunately for the group, Marcia Miller, MD, a 1988 graduate of UF’s CHFM department, had burned herself out running a local private practice with two partners. She turned to Dr. Curry, her mentor and confidant. “I called him, told him I needed a job, and he hired me as the hospitalist program’s co-director,” says Dr. Miller. Her community-based partners endorsed her new career path, and she joined Dr. Chmelik in working every day of the program’s first year. “It was challenging,” she says, “but, with inpatient medicine, I became the doctor I was trained to be.”
Sherri Swilley, the department’s coordinator of administrative affairs, recalls the patient census growing so fast that she struggled to keep up with getting doctors temporary privileges while pursuing credentialing for the permanent staff. “The hospitalists had a fierce work ethic that carried us through those early years,” says Swilley.
Gainesville’s Medical Community
In spring 2003, the program added a local physician eager to exit private practice and a family medicine graduate who had worked in SAGH’s emergency department (ED) for 12 years. In June, they snagged two stellar family medicine graduates and a nocturnist. The nocturnist represents the program’s only turnover; her nightly 12 to 20 admissions proved too much to handle.
UF’s homegrown bunch of family physicians shaped this distinctive hospital medicine program. Dr. Chmelik, assistant professor and co-director of the UF College of Medicine’s hospitalist program at SAGH, says that although family physicians are outnumbered by internal medicine hospitalist physicians they add something special to the role.
“We want to go beyond the stereotype of the internal-medicine trained physician drudging through the hospital as an eternal extension of residency,” says Dr. Chmelik. “Family physicians excel at end-of-life issues and the biopsychosocial model of healthcare, both of which are very important in a hospital.”
Another addition to Dr. Chmelik’s black bag is her expert consulting on obstetric and pediatric patients; she can easily handle issues such as hypertension in a postpartum patient or post-appendectomy asthma in a child.
The Financial Tightrope
The University of Florida’s CHFM is closely tied to SAGH, a 75-year-old, 367-bed community hospital that serves as its training ground for residents and hospitalist fellows. Although SAGH is a vital part of Gainesville’s medical scene, its financial status has been shaky for some time.
In 2002, Moody’s Investor Service gave SAGH a negative rating, which was upgraded to stable in 2003.The upgrade of SAGH’s $312 million of outstanding debt issued by Alachua County Health Facilities Authority kept the wolf from the door temporarily. Talk persists that SAGH is in trouble, however, and a Gainesville group, the Health Care Is a Human Right Coalition, asserted in July 2006 that the hospital lacked leadership and that “there are no published plans to keep SAGH open beyond 2010.” SAGH spokesman Ralph Ives says, “Nothing could be further from the truth.” He points to SAGH’s investment in an 82-bed pediatric hospital in a renovated wing with its own hospital medicine group as an affirmation of the institution’s future.
Like other hospitals struggling with public payers and lots of unassigned patients, SAGH’s hospitalist program improves the hospital’s financial health by serving large numbers of patients cost-effectively. Conversely, hospitalist programs can sink because of inattention to financial basics. Early in SAGH’s history, the hospitalists were overwhelmed with a burgeoning census, leaving coding and billing for clerical staff to figure out at day’s end. This delayed billing and often failed to capture the correct diagnostic codes and level of severity for each patient encounter. As the program matured, the hospitalists and hospital administration agreed that physicians would do the coding themselves as they rounded. That change saved on the back end of clerical work and got the charges in promptly.
Each month, Swilley and the hospitalists review individual and group coding patterns, payer mix, the amount billed to each carrier, the amount of time bills spend in accounts receivable, and the services that have been denied. Hospitalists also receive daily reports on their charges and tips on improving coding. For example, if they’ve reviewed documents, Swilley reminds them to code that activity, just as she does a hospitalist who was swamped in the ED at 10 p.m. and left coding his encounters until 1 a.m., thereby losing one day of service. “A hospital is a business. Our hospitalists work hard; I teach them to work smarter and to pay attention to the bottom line,” says Swilley.
Being diligent about financial productivity matters greatly when it’s time for the CHFM department to negotiate with the hospital for its annual subsidy, which Dr. Curry says is about $500,000.
“When we present our budget, we include billing expenses, overhead, salary, and fringe benefits,” says Swilley. “The more detail we have on the number of patient encounters, [our] productivity, and the revenues we generate, the better position we’re in to get support.”
Like most other hospitals, SAGH struggles with tight reimbursement versus the need for an attractive physical plant. To that end, in 1998 it became the first hospital in Florida to adopt the Planetree model, which advocates patient-driven healthcare, serving body, mind, and spirit. “We’ve always been a deeply compassionate hospital,” says Lynne Mercadante, RN, SAGH’s director of Medical Staff Services, “and Planetree is a natural extension of our looking into our hearts and minds about treating the whole person.”
The hospitalists are deeply connected to the community, knowing when to bring in pastoral care or family therapy, as well as joining in celebrations for weddings and anniversaries.
SAGH has made typical Planetree physical changes, including remodeling one floor into six-patient nursing pods versus one nursing station for 42 patients, along with adding meditation rooms, libraries, a piano in the lobby, and a fish tank. Physicians, patients, and visitors are treated to Brahms’ Lullaby over the loudspeaker system every time a baby is born and can experience pet visitations and aromatherapy.
The Schedule
UF’s hospitalists initially adopted a rotation of seven days on, seven days off. When the group’s nocturnist left because of the heavy burden of night admissions, the nine hospitalists decided to cover call themselves instead of hiring a replacement nocturnist. Every ninth week, a hospitalist takes call Monday through Thursday, with residents carrying the weekend. It isn’t ideal, but it distributes call evenly and ensures hospitalists two free weekends a month.
Like most hospital medicine groups, UF’s hospitalists are trying to tinker with the schedule to make it more flexible. They had some give for Scott Medley, MD, who retired from his large Gainesville private practice of 10 physicians, 65 employees, five offices, and 40,000 patients in 2002 at age 55.
“My private [practice] kept me busy seven days a week. I had been there, done that, got the T-shirt,” says Dr. Medley. “I had enough of private practice, but I didn’t want to leave medicine. On reflection, I realized that what I enjoyed most is taking care of really sick patients, so I contacted Whit Curry, and he hired me as a hospitalist Monday through Friday mornings.”
Dr. Medley loves being an employee, doesn’t mind covering for younger colleagues on holidays, and is now collaborating with specialists who have been his friends and colleagues for 25 years. “I also enjoy teaching younger docs both the art and the economics of medicine—and not having to worry where my next paycheck is coming from,” he says.
Looking ahead, Dr. Miller relishes being a hospitalist at age 47, but wonders what the pace will feel like another decade out. To be more flexible, the group is considering allowing physicians to work more days but fewer hours, initiating job sharing, and recruiting more retirees like Dr. Medley, who can work shorter days and are willing to pinch-hit when coverage is tight. They are working toward consensus on maximizing flexibility while maintaining coverage. Still, there’s no easy solution to fluctuations in census, and Dr. Curry notes that some days span 7:30 a.m. to 3:30 p.m., while others stretch into the night. “We haven’t found a better solution yet to providing care 24 hours a day, 365 days a year,” concludes Dr. Medley.
Creating Value
Looking back at her quarter century at SAGH, Mercadante analyzes how the hospitalist medicine program improved things. “Without hospitalists, whoever was on call covered everyone in the ED, so you had neurologists treating patients with pneumonia. There was little continuity of care, unlike with the hospitalists who meet every morning discussing cases.”
In addition, the medical staff feel they have their lives back because call is covered, and they can count on the hospitalists to co-manage complicated cases. “When specialty physicians are in high demand and short supply, knowing that someone’s covering their hospitalized patients for chronic conditions is so important,” concludes Mercadante.
Looking to the future, UF’s hospitalists plan to build on their cohesiveness, collegiality, and emphasis on family medicine. With alumni of their school at the ready, they know where to turn to continue to grow the program. TH
Marlene Piturro also writes about scheduling in this issue.
Tucked away in the University of Florida (UF), which is—with 50,000 students—the state’s largest university and the nation’s fourth largest, is its School of Medicine’s Community Health and Family Medicine (CHFM) department, along with that department’s hospital medicine program. The department remains a touchstone for its graduates, past and present, and has created hospitalist leaders to be proud of. Much of that pride emanates from R. Whit Curry Jr., MD, CHFM’s department chairman, who is a friend and mentor to several generations of family medicine physicians.
In late 2001, after a private hospital medicine group headed by John Nelson, MD, a UF graduate, SHM co-founder and columnist for this publication, it was natural for Shands Alachua General Hospital (SAGH) to turn to Dr. Curry to start a hospitalist program. Dr. Curry, who says wryly, “If you’ve seen one hospitalist program, you’ve seen one hospitalist program,” knew he could build a unique team of family medicine physicians into a cohesive hospital medicine group.
UF’s CHFM department had staffed SAGH with residents for years before the hospital asked Dr. Curry to start the hospitalist program. The group’s coverage had been limited to inpatient care for about 20 primary care physicians, with a similar arrangement for a for-profit HCA community hospital across town. SAGH needed a more ambitious hospitalist program, one that would cover unassigned patients as well as inpatient care for local doctors. At that point, SAGH issued a request for proposals (RFP) for a hospital medicine group, accepting UF’s CHFM proposal to fill the vacuum left by the departing group. Initially, SAGH would handle the 20 private physicians’ inpatients covered by the existing group, the overflow of unassigned patients from residency workload restrictions, and admitting and co-management for specialists.
Dr. Curry started building his team with Elizabeth Chmelik, MD, recruiting her as the program’s director straight from CHFM residency. The program’s first year—2002—was whirlwind hectic. Fortunately for the group, Marcia Miller, MD, a 1988 graduate of UF’s CHFM department, had burned herself out running a local private practice with two partners. She turned to Dr. Curry, her mentor and confidant. “I called him, told him I needed a job, and he hired me as the hospitalist program’s co-director,” says Dr. Miller. Her community-based partners endorsed her new career path, and she joined Dr. Chmelik in working every day of the program’s first year. “It was challenging,” she says, “but, with inpatient medicine, I became the doctor I was trained to be.”
Sherri Swilley, the department’s coordinator of administrative affairs, recalls the patient census growing so fast that she struggled to keep up with getting doctors temporary privileges while pursuing credentialing for the permanent staff. “The hospitalists had a fierce work ethic that carried us through those early years,” says Swilley.
Gainesville’s Medical Community
In spring 2003, the program added a local physician eager to exit private practice and a family medicine graduate who had worked in SAGH’s emergency department (ED) for 12 years. In June, they snagged two stellar family medicine graduates and a nocturnist. The nocturnist represents the program’s only turnover; her nightly 12 to 20 admissions proved too much to handle.
UF’s homegrown bunch of family physicians shaped this distinctive hospital medicine program. Dr. Chmelik, assistant professor and co-director of the UF College of Medicine’s hospitalist program at SAGH, says that although family physicians are outnumbered by internal medicine hospitalist physicians they add something special to the role.
“We want to go beyond the stereotype of the internal-medicine trained physician drudging through the hospital as an eternal extension of residency,” says Dr. Chmelik. “Family physicians excel at end-of-life issues and the biopsychosocial model of healthcare, both of which are very important in a hospital.”
Another addition to Dr. Chmelik’s black bag is her expert consulting on obstetric and pediatric patients; she can easily handle issues such as hypertension in a postpartum patient or post-appendectomy asthma in a child.
The Financial Tightrope
The University of Florida’s CHFM is closely tied to SAGH, a 75-year-old, 367-bed community hospital that serves as its training ground for residents and hospitalist fellows. Although SAGH is a vital part of Gainesville’s medical scene, its financial status has been shaky for some time.
In 2002, Moody’s Investor Service gave SAGH a negative rating, which was upgraded to stable in 2003.The upgrade of SAGH’s $312 million of outstanding debt issued by Alachua County Health Facilities Authority kept the wolf from the door temporarily. Talk persists that SAGH is in trouble, however, and a Gainesville group, the Health Care Is a Human Right Coalition, asserted in July 2006 that the hospital lacked leadership and that “there are no published plans to keep SAGH open beyond 2010.” SAGH spokesman Ralph Ives says, “Nothing could be further from the truth.” He points to SAGH’s investment in an 82-bed pediatric hospital in a renovated wing with its own hospital medicine group as an affirmation of the institution’s future.
Like other hospitals struggling with public payers and lots of unassigned patients, SAGH’s hospitalist program improves the hospital’s financial health by serving large numbers of patients cost-effectively. Conversely, hospitalist programs can sink because of inattention to financial basics. Early in SAGH’s history, the hospitalists were overwhelmed with a burgeoning census, leaving coding and billing for clerical staff to figure out at day’s end. This delayed billing and often failed to capture the correct diagnostic codes and level of severity for each patient encounter. As the program matured, the hospitalists and hospital administration agreed that physicians would do the coding themselves as they rounded. That change saved on the back end of clerical work and got the charges in promptly.
Each month, Swilley and the hospitalists review individual and group coding patterns, payer mix, the amount billed to each carrier, the amount of time bills spend in accounts receivable, and the services that have been denied. Hospitalists also receive daily reports on their charges and tips on improving coding. For example, if they’ve reviewed documents, Swilley reminds them to code that activity, just as she does a hospitalist who was swamped in the ED at 10 p.m. and left coding his encounters until 1 a.m., thereby losing one day of service. “A hospital is a business. Our hospitalists work hard; I teach them to work smarter and to pay attention to the bottom line,” says Swilley.
Being diligent about financial productivity matters greatly when it’s time for the CHFM department to negotiate with the hospital for its annual subsidy, which Dr. Curry says is about $500,000.
“When we present our budget, we include billing expenses, overhead, salary, and fringe benefits,” says Swilley. “The more detail we have on the number of patient encounters, [our] productivity, and the revenues we generate, the better position we’re in to get support.”
Like most other hospitals, SAGH struggles with tight reimbursement versus the need for an attractive physical plant. To that end, in 1998 it became the first hospital in Florida to adopt the Planetree model, which advocates patient-driven healthcare, serving body, mind, and spirit. “We’ve always been a deeply compassionate hospital,” says Lynne Mercadante, RN, SAGH’s director of Medical Staff Services, “and Planetree is a natural extension of our looking into our hearts and minds about treating the whole person.”
The hospitalists are deeply connected to the community, knowing when to bring in pastoral care or family therapy, as well as joining in celebrations for weddings and anniversaries.
SAGH has made typical Planetree physical changes, including remodeling one floor into six-patient nursing pods versus one nursing station for 42 patients, along with adding meditation rooms, libraries, a piano in the lobby, and a fish tank. Physicians, patients, and visitors are treated to Brahms’ Lullaby over the loudspeaker system every time a baby is born and can experience pet visitations and aromatherapy.
The Schedule
UF’s hospitalists initially adopted a rotation of seven days on, seven days off. When the group’s nocturnist left because of the heavy burden of night admissions, the nine hospitalists decided to cover call themselves instead of hiring a replacement nocturnist. Every ninth week, a hospitalist takes call Monday through Thursday, with residents carrying the weekend. It isn’t ideal, but it distributes call evenly and ensures hospitalists two free weekends a month.
Like most hospital medicine groups, UF’s hospitalists are trying to tinker with the schedule to make it more flexible. They had some give for Scott Medley, MD, who retired from his large Gainesville private practice of 10 physicians, 65 employees, five offices, and 40,000 patients in 2002 at age 55.
“My private [practice] kept me busy seven days a week. I had been there, done that, got the T-shirt,” says Dr. Medley. “I had enough of private practice, but I didn’t want to leave medicine. On reflection, I realized that what I enjoyed most is taking care of really sick patients, so I contacted Whit Curry, and he hired me as a hospitalist Monday through Friday mornings.”
Dr. Medley loves being an employee, doesn’t mind covering for younger colleagues on holidays, and is now collaborating with specialists who have been his friends and colleagues for 25 years. “I also enjoy teaching younger docs both the art and the economics of medicine—and not having to worry where my next paycheck is coming from,” he says.
Looking ahead, Dr. Miller relishes being a hospitalist at age 47, but wonders what the pace will feel like another decade out. To be more flexible, the group is considering allowing physicians to work more days but fewer hours, initiating job sharing, and recruiting more retirees like Dr. Medley, who can work shorter days and are willing to pinch-hit when coverage is tight. They are working toward consensus on maximizing flexibility while maintaining coverage. Still, there’s no easy solution to fluctuations in census, and Dr. Curry notes that some days span 7:30 a.m. to 3:30 p.m., while others stretch into the night. “We haven’t found a better solution yet to providing care 24 hours a day, 365 days a year,” concludes Dr. Medley.
Creating Value
Looking back at her quarter century at SAGH, Mercadante analyzes how the hospitalist medicine program improved things. “Without hospitalists, whoever was on call covered everyone in the ED, so you had neurologists treating patients with pneumonia. There was little continuity of care, unlike with the hospitalists who meet every morning discussing cases.”
In addition, the medical staff feel they have their lives back because call is covered, and they can count on the hospitalists to co-manage complicated cases. “When specialty physicians are in high demand and short supply, knowing that someone’s covering their hospitalized patients for chronic conditions is so important,” concludes Mercadante.
Looking to the future, UF’s hospitalists plan to build on their cohesiveness, collegiality, and emphasis on family medicine. With alumni of their school at the ready, they know where to turn to continue to grow the program. TH
Marlene Piturro also writes about scheduling in this issue.
Scheduling Strategies
The media often make complex issues sound simple—10 tips for this, the best eight ways to do that. Vexing problems are neatly addressed in a page or two, ending with bullet points lest the reader misunderstand the sage advice offered. While The Hospitalist would not presume that a task as fraught as hospitalist scheduling could be approached using tips similar to those suggested for soothing toddler temper tantrums, we lightly present some collective wisdom on scheduling.
Before sharing how several hospitalist medicine groups (HMGs) previously profiled in The Hospitalist attacked their toughest scheduling issues, we looked at the “2005-2006 SHM Survey: State of the Hospital Medicine Movement” of 2,550 hospitalists in 396 HMGs for insights about how hospitalists spend their time and how they struggle to balance work and personal lives. This background information provides a context for scheduling.
Here’s what the data say. For starters, the average hospitalist is not fresh out of residency. The SHM survey says the average HMG leader is 41, with 5.1 years of hospitalist experience. Non-leader hospitalists are, on average, 37 and have been hospitalists for an average of three years. Hospitalist physician staffing levels increased from 8.49 to 8.81 physicians, while non-physician staffing decreased from 3.10 to 1.09 FTEs.
Hospitalists spend 10% of their time in non-clinical activities, and that 10% is divided as follows: committee work, 92%; quality improvement, 86%; developing practice guidelines, 72%; and teaching medical students, 51%. New since the last survey is the fact that 52% of HMGs became involved in rapid response teams, while 19% of HMGs spend time on computerized physician order entry (CPOE) systems.
Scheduling’s impact on hospitalists’ lives remains a big issue. Forty-two percent of HMG leaders cited balancing work hours and personal life balance as problematic, 29% were concerned about their daily workloads, 23% said that expectations and demands on hospitalists were increasing, 15% worried about career sustainability and retaining hospitalists, while 11% cited scheduling per se as challenging.
Coverage arrangements changed significantly from the 2003-2004 survey. More HMGs now use hybrid (shift + call) coverage (35% in ’05-’06 versus 27% in ’03-’04) and fewer use call only (25% in ’05-’06 versus 36% in ’03-’04).
SHM’s survey shows that hospitalists working shift-only schedules average 187 shifts, 10.8 hours a day. Call-only hospitalists average 150 days on call, for 15.7-hour days. Hybrid schedules average 206 days, with each day spanning 8.9 hours; of those days, 82 are 12.8-hour on-call days.
For the thorny issue of night call, of the hospitalists who do cover call, 41% cover call from home, 51% are on site, and 8% of HMGs don’t cover call. About one-quarter of HMGs provide an on-site nocturnist, but most practices can’t justify the compensation package for the one or two admits and patient visits they have during the average night. To fill gaps, 24% of HMGs used moonlighters; 11% rely on residents; and 5% and 4%, respectively, use physician assistants and nurse practitioners.
In summary, HMG staffing has increased slightly, more groups are using hybrid shift/call arrangements, most hospitalists work long hours compressed into approximately 180 days per year, and scheduling for work/personal life balance remains a major issue for HMG leaders and their hospitalists.
Common Sense
Hospitalist schedules have evolved from what doctors know best—shift work or office-based practice hours. Most HMGs organize hospitalist shifts into blocks, with the most popular block still the seven days on/seven days off schedule. Block scheduling becomes easier as HMGs grow to six to 10 physicians.
While the seven on/seven off schedule has become popular, many find that it is stressful and can lead to burnout. The on days’ long hours can make it hard to recover on days off. John Nelson, MD, director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., SHM co-founder, and “Practice Management” columnist for The Hospitalist, contends in published writings that the seven on/seven off schedule squeezes a full-time job into only 182.5 days; the stress that such intensity entails—both personally and professionally—is tremendous. Compressed schedules, in trying to shoehorn the average workload into too few days, can also lead to below average relative value units (RVUs) and other productivity measures.
Dr. Nelson advises reducing the daily workload by spreading the work over 210 to 220 days annually. While that doesn’t afford the luxury of seven consecutive days off, it allows the doctors to titrate their work out over more days so that the average day will be less busy. He also advises flexibility in starting and stopping times for individual shifts, allowing HMGs to adjust to changes in patient volume and workload. Scheduling elasticity lets doctors adapt to a day’s ebbs and flows, perhaps taking a lunch hour or driving a child to soccer practice. That may mean early evening hospital time to finish up, but variety keeps life interesting.
About patient volume (another scheduling headache) Dr. Nelson says that capping individual physician workloads makes sense because overwhelmed physicians tend to make mistakes. But capping a practice’s volume looks unprofessional and can limit a group’s earnings. Several HMGs we profiled disagree with Dr. Nelson. (See below.) Most didn’t actually cap patient volume, but instead restricted the number of physicians transferring inpatients to the HMG, adding more referral sources only as patient volume stabilized or new hospitalists came on board to handle growing volume.
Some of the best-functioning HMGs we encountered have lured well-known office-based doctors ready for a change. Eager to shed a practice’s financial and administrative burden, as well as regular office hours, these physicians relish the chance to return to hospital work—their first career love. They also remember what it’s like to have to work Thanksgiving, Christmas, and New Year’s, and the more generous among them volunteer for those shifts so that younger hospitalists can spend holidays with their families.
Awards for Struggling through Scheduling Issues
Data on where the average HMG stands on scheduling are important, but every successful group has physician leaders who craft schedules based on a broad and subtle understanding of their medical communities. They factor in whether the areas surrounding their hospitals are stable, growing, or shrinking; the patient mix they’re likely to see; their hospital’s corporate culture and those of the referring office practices. For recruiting, they think about whether their location offers an attractive lifestyle or how they can sweeten the pot if it doesn’t. If they’re at an academic medical center, they’ll have a lower average daily census (ADC) and different expectations about productivity than if they’re a private HMG at a community hospital. Chemistry, meaning whether or not a new hospitalist who looks great on paper and interviews well will gel with the group or upset the apple cart, is a tantalizing unknown.
So here’s our list of HMGs that wrestled successfully with their scheduling challenges:
The “Are We Good, or What? Award” goes to Health Partners of Minneapolis, Minn. These hospitalists have won numerous SHM awards for clinical excellence, reflecting their high standards and competence. The 25 physicians and two nurse practitioners can choose between two block schedules: seven days on/seven days off or 14 days on/14 days off. They also work two night shifts a month—6 p.m. to 8 a.m.—backing up residents. Key to avoiding burnout on this schedule is geographical deployment. Hospitalists work only in one or two units, rather than covering the entire seven-floor hospital.
The “Go Gators Award” goes to Sage Alachua General Hospital of Gainesville, Fla. Whenever possible, these hospitalists attend the home football games of their beloved Florida Gators, 2007 Bowl Championship Series winners. This reflects their strong ties to the University of Florida Medical School—also Dr. Nelson’s alma mater—and the many physicians who come from or settle in the Gainesville area. The group started with three hospitalists on a seven on/seven off schedule, backed up by a nocturnist who quit due to the heavy volume of night admissions. They now have nine hospitalists—all family practice physicians—working a seven/seven schedule. Each one covers Monday through Thursday night call every nine weeks, with residents handling Friday through Sunday. An internist who retired from his office practice works Monday through Friday mornings and occasionally covers holiday shifts for his younger colleagues.
The “He’s Not Heavy, He’s My Colleague Award” goes to Nashua, N.H.-based Southern New Hampshire Medical Center (SNHMC) hospitalists: Stewart Fulton, DO, SNHMC’s solo hospitalist for more than a year, answered call 24/7, with help from the community doctors whose inpatients he was following. Though he was joined eventually by the group’s second hospitalist, Suneetha Kammila, MD, chaos reigned for the next year. They hired a third hospitalist and eventually grew to five physicians and moved from call to shifts. By the third year, SNHMC had 10 hospitalists—two teams of five—and moved to the seven days on/seven days off schedule everyone wanted. The tenacity of HMG leaders Dr. Fulton and Dr. Kammila allowed the group to survive its early scheduling hardships.
The “If We Were Cars, We’d Be Benzes or Beemers Award” goes to the Colorado Kaiser-Permanente hospitalists in Denver. Part of an organization that prides itself on perfecting processes and improving transparency in healthcare, this group had all the tools to get their scheduling right. They started with the widely used seven on/seven off schedule but found it dissatisfying both personally and professionally. Through consensus, they arrived at a schedule of six consecutive eight-hour days of rounding with one triage physician handling after-hours call. There are two hospitalists on-site, 24 hours a day, seven days a week, and they admit and cross-cover after 4 p.m.
The “Planning Is Everything Award” goes to the Brockie Hospitalist Group in York, Pa. Both the hospital and the city of York are in a sustained growth mode. There are several large outpatient practices waiting for Brockie’s hospitalist group to assume their inpatients. The 18 hospitalists have wisely demurred, allowing their office-based colleagues to turn over the inpatient work only when the hospitalists can handle the additional load. Hospitalists choose either a 132-hour or a 147-hour schedule that is divided into blocks over three weeks, with a productivity/incentive program that changes as the increasing workload dictates.
The “Scheduling Is a Piece of Cake Award” goes out to Scott Oxenhandler, MD, chief hospitalist at Hollywood Memorial Hospital in Florida. Dr. Oxenhandler left an office practice for the hospitalist’s chance to practice acute care medicine with good compensation and benefits, reduced paperwork, and a great schedule. He recruited 21 hospitalists. Most work an 8 a.m. to 5 p.m. schedule, while a nocturnist covers the hours from 8 p.m. to 8 a.m. Ten physicians handle the 5 to 8 p.m. “short call” four times a month. The large number of hospitalists allows flexibility in scheduling to accommodate individual needs.
The “We Grew Past Our Mistakes Award” has been earned by Presbyterian Inpatient Care Systems in Charlotte, N.C. This program started as a two-physician, 5 p.m. to 7 a.m. admitting service for community physicians too busy to cover call. The hospitalists quit, wanting more out of medicine than an admitting service. Four hospitalists who were committed to providing inpatient care replaced them, with better results. The group now has more than 30 physicians working 12-hour shifts and co-managing, with sub-specialists, complex care. A nocturnist, working an eight-hour shift instead of the 12-hour shift that burned out a predecessor, covers night admissions and call.
Tighter Times?
Could the days of hospitalists fretting about work/life balance and optimal schedules be drawing to an end, as hospitals cast a jaundiced eye on the value hospitalists create versus what they cost? Chris Nussbaum, MD, CEO of Synergy Medical Group, based in Brandon, Fla., thinks so. He employs 10 hospitalists who cover six Tampa-area hospitals located within 15 minutes of each other. The group just switched from call to a 7 a.m. to 7 p.m. shift schedule. Dr. Nussbaum deploys hospitalists based on each hospital’s average daily census, so a doctor could cover several hospitals a day.
On an average day, eight hospitalists work days, one works the night shift, and one is off. Dr. Nussbaum’s rationale: “We’re very aggressive about time management. Our first year docs earn a base salary of $200,000, with $40,000 in productivity bonuses.” He adds, “I believe hospitalist medicine is moving in the direction we’ve taken. Scheduling is critical, and hospitalists need to work harder and be entrepreneurial. … In today’s market, prima donna docs command high salaries and have an ADC of 10 patients. That will change soon as supply catches up with demand.” TH
Marlene Piturro regularly profiles HMGs and trends in hospital medicine for The Hospitalist.
The media often make complex issues sound simple—10 tips for this, the best eight ways to do that. Vexing problems are neatly addressed in a page or two, ending with bullet points lest the reader misunderstand the sage advice offered. While The Hospitalist would not presume that a task as fraught as hospitalist scheduling could be approached using tips similar to those suggested for soothing toddler temper tantrums, we lightly present some collective wisdom on scheduling.
Before sharing how several hospitalist medicine groups (HMGs) previously profiled in The Hospitalist attacked their toughest scheduling issues, we looked at the “2005-2006 SHM Survey: State of the Hospital Medicine Movement” of 2,550 hospitalists in 396 HMGs for insights about how hospitalists spend their time and how they struggle to balance work and personal lives. This background information provides a context for scheduling.
Here’s what the data say. For starters, the average hospitalist is not fresh out of residency. The SHM survey says the average HMG leader is 41, with 5.1 years of hospitalist experience. Non-leader hospitalists are, on average, 37 and have been hospitalists for an average of three years. Hospitalist physician staffing levels increased from 8.49 to 8.81 physicians, while non-physician staffing decreased from 3.10 to 1.09 FTEs.
Hospitalists spend 10% of their time in non-clinical activities, and that 10% is divided as follows: committee work, 92%; quality improvement, 86%; developing practice guidelines, 72%; and teaching medical students, 51%. New since the last survey is the fact that 52% of HMGs became involved in rapid response teams, while 19% of HMGs spend time on computerized physician order entry (CPOE) systems.
Scheduling’s impact on hospitalists’ lives remains a big issue. Forty-two percent of HMG leaders cited balancing work hours and personal life balance as problematic, 29% were concerned about their daily workloads, 23% said that expectations and demands on hospitalists were increasing, 15% worried about career sustainability and retaining hospitalists, while 11% cited scheduling per se as challenging.
Coverage arrangements changed significantly from the 2003-2004 survey. More HMGs now use hybrid (shift + call) coverage (35% in ’05-’06 versus 27% in ’03-’04) and fewer use call only (25% in ’05-’06 versus 36% in ’03-’04).
SHM’s survey shows that hospitalists working shift-only schedules average 187 shifts, 10.8 hours a day. Call-only hospitalists average 150 days on call, for 15.7-hour days. Hybrid schedules average 206 days, with each day spanning 8.9 hours; of those days, 82 are 12.8-hour on-call days.
For the thorny issue of night call, of the hospitalists who do cover call, 41% cover call from home, 51% are on site, and 8% of HMGs don’t cover call. About one-quarter of HMGs provide an on-site nocturnist, but most practices can’t justify the compensation package for the one or two admits and patient visits they have during the average night. To fill gaps, 24% of HMGs used moonlighters; 11% rely on residents; and 5% and 4%, respectively, use physician assistants and nurse practitioners.
In summary, HMG staffing has increased slightly, more groups are using hybrid shift/call arrangements, most hospitalists work long hours compressed into approximately 180 days per year, and scheduling for work/personal life balance remains a major issue for HMG leaders and their hospitalists.
Common Sense
Hospitalist schedules have evolved from what doctors know best—shift work or office-based practice hours. Most HMGs organize hospitalist shifts into blocks, with the most popular block still the seven days on/seven days off schedule. Block scheduling becomes easier as HMGs grow to six to 10 physicians.
While the seven on/seven off schedule has become popular, many find that it is stressful and can lead to burnout. The on days’ long hours can make it hard to recover on days off. John Nelson, MD, director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., SHM co-founder, and “Practice Management” columnist for The Hospitalist, contends in published writings that the seven on/seven off schedule squeezes a full-time job into only 182.5 days; the stress that such intensity entails—both personally and professionally—is tremendous. Compressed schedules, in trying to shoehorn the average workload into too few days, can also lead to below average relative value units (RVUs) and other productivity measures.
Dr. Nelson advises reducing the daily workload by spreading the work over 210 to 220 days annually. While that doesn’t afford the luxury of seven consecutive days off, it allows the doctors to titrate their work out over more days so that the average day will be less busy. He also advises flexibility in starting and stopping times for individual shifts, allowing HMGs to adjust to changes in patient volume and workload. Scheduling elasticity lets doctors adapt to a day’s ebbs and flows, perhaps taking a lunch hour or driving a child to soccer practice. That may mean early evening hospital time to finish up, but variety keeps life interesting.
About patient volume (another scheduling headache) Dr. Nelson says that capping individual physician workloads makes sense because overwhelmed physicians tend to make mistakes. But capping a practice’s volume looks unprofessional and can limit a group’s earnings. Several HMGs we profiled disagree with Dr. Nelson. (See below.) Most didn’t actually cap patient volume, but instead restricted the number of physicians transferring inpatients to the HMG, adding more referral sources only as patient volume stabilized or new hospitalists came on board to handle growing volume.
Some of the best-functioning HMGs we encountered have lured well-known office-based doctors ready for a change. Eager to shed a practice’s financial and administrative burden, as well as regular office hours, these physicians relish the chance to return to hospital work—their first career love. They also remember what it’s like to have to work Thanksgiving, Christmas, and New Year’s, and the more generous among them volunteer for those shifts so that younger hospitalists can spend holidays with their families.
Awards for Struggling through Scheduling Issues
Data on where the average HMG stands on scheduling are important, but every successful group has physician leaders who craft schedules based on a broad and subtle understanding of their medical communities. They factor in whether the areas surrounding their hospitals are stable, growing, or shrinking; the patient mix they’re likely to see; their hospital’s corporate culture and those of the referring office practices. For recruiting, they think about whether their location offers an attractive lifestyle or how they can sweeten the pot if it doesn’t. If they’re at an academic medical center, they’ll have a lower average daily census (ADC) and different expectations about productivity than if they’re a private HMG at a community hospital. Chemistry, meaning whether or not a new hospitalist who looks great on paper and interviews well will gel with the group or upset the apple cart, is a tantalizing unknown.
So here’s our list of HMGs that wrestled successfully with their scheduling challenges:
The “Are We Good, or What? Award” goes to Health Partners of Minneapolis, Minn. These hospitalists have won numerous SHM awards for clinical excellence, reflecting their high standards and competence. The 25 physicians and two nurse practitioners can choose between two block schedules: seven days on/seven days off or 14 days on/14 days off. They also work two night shifts a month—6 p.m. to 8 a.m.—backing up residents. Key to avoiding burnout on this schedule is geographical deployment. Hospitalists work only in one or two units, rather than covering the entire seven-floor hospital.
The “Go Gators Award” goes to Sage Alachua General Hospital of Gainesville, Fla. Whenever possible, these hospitalists attend the home football games of their beloved Florida Gators, 2007 Bowl Championship Series winners. This reflects their strong ties to the University of Florida Medical School—also Dr. Nelson’s alma mater—and the many physicians who come from or settle in the Gainesville area. The group started with three hospitalists on a seven on/seven off schedule, backed up by a nocturnist who quit due to the heavy volume of night admissions. They now have nine hospitalists—all family practice physicians—working a seven/seven schedule. Each one covers Monday through Thursday night call every nine weeks, with residents handling Friday through Sunday. An internist who retired from his office practice works Monday through Friday mornings and occasionally covers holiday shifts for his younger colleagues.
The “He’s Not Heavy, He’s My Colleague Award” goes to Nashua, N.H.-based Southern New Hampshire Medical Center (SNHMC) hospitalists: Stewart Fulton, DO, SNHMC’s solo hospitalist for more than a year, answered call 24/7, with help from the community doctors whose inpatients he was following. Though he was joined eventually by the group’s second hospitalist, Suneetha Kammila, MD, chaos reigned for the next year. They hired a third hospitalist and eventually grew to five physicians and moved from call to shifts. By the third year, SNHMC had 10 hospitalists—two teams of five—and moved to the seven days on/seven days off schedule everyone wanted. The tenacity of HMG leaders Dr. Fulton and Dr. Kammila allowed the group to survive its early scheduling hardships.
The “If We Were Cars, We’d Be Benzes or Beemers Award” goes to the Colorado Kaiser-Permanente hospitalists in Denver. Part of an organization that prides itself on perfecting processes and improving transparency in healthcare, this group had all the tools to get their scheduling right. They started with the widely used seven on/seven off schedule but found it dissatisfying both personally and professionally. Through consensus, they arrived at a schedule of six consecutive eight-hour days of rounding with one triage physician handling after-hours call. There are two hospitalists on-site, 24 hours a day, seven days a week, and they admit and cross-cover after 4 p.m.
The “Planning Is Everything Award” goes to the Brockie Hospitalist Group in York, Pa. Both the hospital and the city of York are in a sustained growth mode. There are several large outpatient practices waiting for Brockie’s hospitalist group to assume their inpatients. The 18 hospitalists have wisely demurred, allowing their office-based colleagues to turn over the inpatient work only when the hospitalists can handle the additional load. Hospitalists choose either a 132-hour or a 147-hour schedule that is divided into blocks over three weeks, with a productivity/incentive program that changes as the increasing workload dictates.
The “Scheduling Is a Piece of Cake Award” goes out to Scott Oxenhandler, MD, chief hospitalist at Hollywood Memorial Hospital in Florida. Dr. Oxenhandler left an office practice for the hospitalist’s chance to practice acute care medicine with good compensation and benefits, reduced paperwork, and a great schedule. He recruited 21 hospitalists. Most work an 8 a.m. to 5 p.m. schedule, while a nocturnist covers the hours from 8 p.m. to 8 a.m. Ten physicians handle the 5 to 8 p.m. “short call” four times a month. The large number of hospitalists allows flexibility in scheduling to accommodate individual needs.
The “We Grew Past Our Mistakes Award” has been earned by Presbyterian Inpatient Care Systems in Charlotte, N.C. This program started as a two-physician, 5 p.m. to 7 a.m. admitting service for community physicians too busy to cover call. The hospitalists quit, wanting more out of medicine than an admitting service. Four hospitalists who were committed to providing inpatient care replaced them, with better results. The group now has more than 30 physicians working 12-hour shifts and co-managing, with sub-specialists, complex care. A nocturnist, working an eight-hour shift instead of the 12-hour shift that burned out a predecessor, covers night admissions and call.
Tighter Times?
Could the days of hospitalists fretting about work/life balance and optimal schedules be drawing to an end, as hospitals cast a jaundiced eye on the value hospitalists create versus what they cost? Chris Nussbaum, MD, CEO of Synergy Medical Group, based in Brandon, Fla., thinks so. He employs 10 hospitalists who cover six Tampa-area hospitals located within 15 minutes of each other. The group just switched from call to a 7 a.m. to 7 p.m. shift schedule. Dr. Nussbaum deploys hospitalists based on each hospital’s average daily census, so a doctor could cover several hospitals a day.
On an average day, eight hospitalists work days, one works the night shift, and one is off. Dr. Nussbaum’s rationale: “We’re very aggressive about time management. Our first year docs earn a base salary of $200,000, with $40,000 in productivity bonuses.” He adds, “I believe hospitalist medicine is moving in the direction we’ve taken. Scheduling is critical, and hospitalists need to work harder and be entrepreneurial. … In today’s market, prima donna docs command high salaries and have an ADC of 10 patients. That will change soon as supply catches up with demand.” TH
Marlene Piturro regularly profiles HMGs and trends in hospital medicine for The Hospitalist.
The media often make complex issues sound simple—10 tips for this, the best eight ways to do that. Vexing problems are neatly addressed in a page or two, ending with bullet points lest the reader misunderstand the sage advice offered. While The Hospitalist would not presume that a task as fraught as hospitalist scheduling could be approached using tips similar to those suggested for soothing toddler temper tantrums, we lightly present some collective wisdom on scheduling.
Before sharing how several hospitalist medicine groups (HMGs) previously profiled in The Hospitalist attacked their toughest scheduling issues, we looked at the “2005-2006 SHM Survey: State of the Hospital Medicine Movement” of 2,550 hospitalists in 396 HMGs for insights about how hospitalists spend their time and how they struggle to balance work and personal lives. This background information provides a context for scheduling.
Here’s what the data say. For starters, the average hospitalist is not fresh out of residency. The SHM survey says the average HMG leader is 41, with 5.1 years of hospitalist experience. Non-leader hospitalists are, on average, 37 and have been hospitalists for an average of three years. Hospitalist physician staffing levels increased from 8.49 to 8.81 physicians, while non-physician staffing decreased from 3.10 to 1.09 FTEs.
Hospitalists spend 10% of their time in non-clinical activities, and that 10% is divided as follows: committee work, 92%; quality improvement, 86%; developing practice guidelines, 72%; and teaching medical students, 51%. New since the last survey is the fact that 52% of HMGs became involved in rapid response teams, while 19% of HMGs spend time on computerized physician order entry (CPOE) systems.
Scheduling’s impact on hospitalists’ lives remains a big issue. Forty-two percent of HMG leaders cited balancing work hours and personal life balance as problematic, 29% were concerned about their daily workloads, 23% said that expectations and demands on hospitalists were increasing, 15% worried about career sustainability and retaining hospitalists, while 11% cited scheduling per se as challenging.
Coverage arrangements changed significantly from the 2003-2004 survey. More HMGs now use hybrid (shift + call) coverage (35% in ’05-’06 versus 27% in ’03-’04) and fewer use call only (25% in ’05-’06 versus 36% in ’03-’04).
SHM’s survey shows that hospitalists working shift-only schedules average 187 shifts, 10.8 hours a day. Call-only hospitalists average 150 days on call, for 15.7-hour days. Hybrid schedules average 206 days, with each day spanning 8.9 hours; of those days, 82 are 12.8-hour on-call days.
For the thorny issue of night call, of the hospitalists who do cover call, 41% cover call from home, 51% are on site, and 8% of HMGs don’t cover call. About one-quarter of HMGs provide an on-site nocturnist, but most practices can’t justify the compensation package for the one or two admits and patient visits they have during the average night. To fill gaps, 24% of HMGs used moonlighters; 11% rely on residents; and 5% and 4%, respectively, use physician assistants and nurse practitioners.
In summary, HMG staffing has increased slightly, more groups are using hybrid shift/call arrangements, most hospitalists work long hours compressed into approximately 180 days per year, and scheduling for work/personal life balance remains a major issue for HMG leaders and their hospitalists.
Common Sense
Hospitalist schedules have evolved from what doctors know best—shift work or office-based practice hours. Most HMGs organize hospitalist shifts into blocks, with the most popular block still the seven days on/seven days off schedule. Block scheduling becomes easier as HMGs grow to six to 10 physicians.
While the seven on/seven off schedule has become popular, many find that it is stressful and can lead to burnout. The on days’ long hours can make it hard to recover on days off. John Nelson, MD, director of the hospitalist practice at Overlake Hospital in Bellevue, Wash., SHM co-founder, and “Practice Management” columnist for The Hospitalist, contends in published writings that the seven on/seven off schedule squeezes a full-time job into only 182.5 days; the stress that such intensity entails—both personally and professionally—is tremendous. Compressed schedules, in trying to shoehorn the average workload into too few days, can also lead to below average relative value units (RVUs) and other productivity measures.
Dr. Nelson advises reducing the daily workload by spreading the work over 210 to 220 days annually. While that doesn’t afford the luxury of seven consecutive days off, it allows the doctors to titrate their work out over more days so that the average day will be less busy. He also advises flexibility in starting and stopping times for individual shifts, allowing HMGs to adjust to changes in patient volume and workload. Scheduling elasticity lets doctors adapt to a day’s ebbs and flows, perhaps taking a lunch hour or driving a child to soccer practice. That may mean early evening hospital time to finish up, but variety keeps life interesting.
About patient volume (another scheduling headache) Dr. Nelson says that capping individual physician workloads makes sense because overwhelmed physicians tend to make mistakes. But capping a practice’s volume looks unprofessional and can limit a group’s earnings. Several HMGs we profiled disagree with Dr. Nelson. (See below.) Most didn’t actually cap patient volume, but instead restricted the number of physicians transferring inpatients to the HMG, adding more referral sources only as patient volume stabilized or new hospitalists came on board to handle growing volume.
Some of the best-functioning HMGs we encountered have lured well-known office-based doctors ready for a change. Eager to shed a practice’s financial and administrative burden, as well as regular office hours, these physicians relish the chance to return to hospital work—their first career love. They also remember what it’s like to have to work Thanksgiving, Christmas, and New Year’s, and the more generous among them volunteer for those shifts so that younger hospitalists can spend holidays with their families.
Awards for Struggling through Scheduling Issues
Data on where the average HMG stands on scheduling are important, but every successful group has physician leaders who craft schedules based on a broad and subtle understanding of their medical communities. They factor in whether the areas surrounding their hospitals are stable, growing, or shrinking; the patient mix they’re likely to see; their hospital’s corporate culture and those of the referring office practices. For recruiting, they think about whether their location offers an attractive lifestyle or how they can sweeten the pot if it doesn’t. If they’re at an academic medical center, they’ll have a lower average daily census (ADC) and different expectations about productivity than if they’re a private HMG at a community hospital. Chemistry, meaning whether or not a new hospitalist who looks great on paper and interviews well will gel with the group or upset the apple cart, is a tantalizing unknown.
So here’s our list of HMGs that wrestled successfully with their scheduling challenges:
The “Are We Good, or What? Award” goes to Health Partners of Minneapolis, Minn. These hospitalists have won numerous SHM awards for clinical excellence, reflecting their high standards and competence. The 25 physicians and two nurse practitioners can choose between two block schedules: seven days on/seven days off or 14 days on/14 days off. They also work two night shifts a month—6 p.m. to 8 a.m.—backing up residents. Key to avoiding burnout on this schedule is geographical deployment. Hospitalists work only in one or two units, rather than covering the entire seven-floor hospital.
The “Go Gators Award” goes to Sage Alachua General Hospital of Gainesville, Fla. Whenever possible, these hospitalists attend the home football games of their beloved Florida Gators, 2007 Bowl Championship Series winners. This reflects their strong ties to the University of Florida Medical School—also Dr. Nelson’s alma mater—and the many physicians who come from or settle in the Gainesville area. The group started with three hospitalists on a seven on/seven off schedule, backed up by a nocturnist who quit due to the heavy volume of night admissions. They now have nine hospitalists—all family practice physicians—working a seven/seven schedule. Each one covers Monday through Thursday night call every nine weeks, with residents handling Friday through Sunday. An internist who retired from his office practice works Monday through Friday mornings and occasionally covers holiday shifts for his younger colleagues.
The “He’s Not Heavy, He’s My Colleague Award” goes to Nashua, N.H.-based Southern New Hampshire Medical Center (SNHMC) hospitalists: Stewart Fulton, DO, SNHMC’s solo hospitalist for more than a year, answered call 24/7, with help from the community doctors whose inpatients he was following. Though he was joined eventually by the group’s second hospitalist, Suneetha Kammila, MD, chaos reigned for the next year. They hired a third hospitalist and eventually grew to five physicians and moved from call to shifts. By the third year, SNHMC had 10 hospitalists—two teams of five—and moved to the seven days on/seven days off schedule everyone wanted. The tenacity of HMG leaders Dr. Fulton and Dr. Kammila allowed the group to survive its early scheduling hardships.
The “If We Were Cars, We’d Be Benzes or Beemers Award” goes to the Colorado Kaiser-Permanente hospitalists in Denver. Part of an organization that prides itself on perfecting processes and improving transparency in healthcare, this group had all the tools to get their scheduling right. They started with the widely used seven on/seven off schedule but found it dissatisfying both personally and professionally. Through consensus, they arrived at a schedule of six consecutive eight-hour days of rounding with one triage physician handling after-hours call. There are two hospitalists on-site, 24 hours a day, seven days a week, and they admit and cross-cover after 4 p.m.
The “Planning Is Everything Award” goes to the Brockie Hospitalist Group in York, Pa. Both the hospital and the city of York are in a sustained growth mode. There are several large outpatient practices waiting for Brockie’s hospitalist group to assume their inpatients. The 18 hospitalists have wisely demurred, allowing their office-based colleagues to turn over the inpatient work only when the hospitalists can handle the additional load. Hospitalists choose either a 132-hour or a 147-hour schedule that is divided into blocks over three weeks, with a productivity/incentive program that changes as the increasing workload dictates.
The “Scheduling Is a Piece of Cake Award” goes out to Scott Oxenhandler, MD, chief hospitalist at Hollywood Memorial Hospital in Florida. Dr. Oxenhandler left an office practice for the hospitalist’s chance to practice acute care medicine with good compensation and benefits, reduced paperwork, and a great schedule. He recruited 21 hospitalists. Most work an 8 a.m. to 5 p.m. schedule, while a nocturnist covers the hours from 8 p.m. to 8 a.m. Ten physicians handle the 5 to 8 p.m. “short call” four times a month. The large number of hospitalists allows flexibility in scheduling to accommodate individual needs.
The “We Grew Past Our Mistakes Award” has been earned by Presbyterian Inpatient Care Systems in Charlotte, N.C. This program started as a two-physician, 5 p.m. to 7 a.m. admitting service for community physicians too busy to cover call. The hospitalists quit, wanting more out of medicine than an admitting service. Four hospitalists who were committed to providing inpatient care replaced them, with better results. The group now has more than 30 physicians working 12-hour shifts and co-managing, with sub-specialists, complex care. A nocturnist, working an eight-hour shift instead of the 12-hour shift that burned out a predecessor, covers night admissions and call.
Tighter Times?
Could the days of hospitalists fretting about work/life balance and optimal schedules be drawing to an end, as hospitals cast a jaundiced eye on the value hospitalists create versus what they cost? Chris Nussbaum, MD, CEO of Synergy Medical Group, based in Brandon, Fla., thinks so. He employs 10 hospitalists who cover six Tampa-area hospitals located within 15 minutes of each other. The group just switched from call to a 7 a.m. to 7 p.m. shift schedule. Dr. Nussbaum deploys hospitalists based on each hospital’s average daily census, so a doctor could cover several hospitals a day.
On an average day, eight hospitalists work days, one works the night shift, and one is off. Dr. Nussbaum’s rationale: “We’re very aggressive about time management. Our first year docs earn a base salary of $200,000, with $40,000 in productivity bonuses.” He adds, “I believe hospitalist medicine is moving in the direction we’ve taken. Scheduling is critical, and hospitalists need to work harder and be entrepreneurial. … In today’s market, prima donna docs command high salaries and have an ADC of 10 patients. That will change soon as supply catches up with demand.” TH
Marlene Piturro regularly profiles HMGs and trends in hospital medicine for The Hospitalist.
Score!
Deciding to measure performance—whether by test scores or clinical indicators—is step one to improve what you’re measuring. So when the Centers for Medicare and Medicaid Services (CMS) awarded $8.85 million in incentives to hospitals that showed measurable care improvements in 2005, it was no surprise that industry stakeholders took notice. Top decile hospitals received a 3% bonus, while second decile winners received 1%; bonuses were based on the achievement of specific clinical quality indicators. CMS improved care quality in five targeted clinical areas by the percentages indicated: community-acquired pneumonia (CAP) by 10%, heart failure by 9%, hip/knee replacement and coronary artery bypass graft (CABG) by 5% each, and acute myocardial infarction (AMI) by 4%.
CMS’ core measures project encourages winners to tout their achievements to consumers, recruitable physicians, payers, and anyone else who will listen. Like any program based on achieving scores rather than identifying the processes necessary to achieve success, though, insiders can speculate about what variables are responsible for positive outcomes. In the case of CMS’ core measures, if hospitalist stakeholders can demonstrate that having hospitalists increases a hospital’s CMS core measure performance, they’ve earned important marketing and clinical leverage. Stacy Goldsholl, MD, of Wilmington, N.C.-based TeamHealth, estimates that more than 70% of TeamHealth’s potential clients now ask for her firm’s data on CMS core measures.
The Hospitalist’s Measures
To explore the relationship between a hospital’s position in the top two deciles on core measures with its hospitalist program, The Hospitalist extrapolated data from the CMS/Premier Hospital Quality Incentive Demonstration Project (www.premierinc.com/quality-safety) and SHM’s membership list, a proxy for a comprehensive list of hospitalist programs. All 44 hospitals in the top two deciles for heart failure core measures and the 49 hospitals listed for CAP were checked against the SHM list, as were their Web sites, for mention of a hospitalist program.
We compared data on two of the five core measures: heart failure and CAP. We expected a higher correlation for CAP because hospitalists are more likely to have primary inpatient responsibility for CAP patients than they are for heart failure patients, for whom cardiologists often have primary accountability. Here are the results of The Hospitalist’s analysis.
Hospitals in the top 10% for heart failure core measures are St. Helena Hospital (Calif.), Homestead Hospital (Fla.), Kootenai Medical Center (Idaho), Mission Hospital (N.C.), Staten Island University Hospital (N.Y.), Harris Methodist Fort Worth (Texas), and Harris Methodist Southwest (Texas).
Top decile performers in CAP are Methodist Medical Center of Illinois (Ill.), St. Vincent Memorial Hospital (Ill.), Heartland Regional Medical Center (Mo.), Stanly Memorial Hospital (N.C.), Alegent Health Immanuel Medical Center (Neb.), Staten Island University Hospital (N.Y.), Presbyterian Hospital of Kaufman (Texas), and Aurora Medical Center (Wis.).
Hospitals with some form of hospitalist program performed well, particularly on the second decile of the two core measures The Hospitalist examined: heart failure (44%) and community-acquired pneumonia (58%).
Complex Issues
Hospitalists expressed varied reactions to The Hospitalist’s correlation between a hospital’s core measures performance and its use of hospitalists. Adam Singer, MD, CEO of IPC-The Hospitalist Company of North Hollywood, Calif., scanned The Hospitalist’s lists and found a number of top-performing hospitals on its roster, including Methodist Forth Worth and Methodist Southwest in Texas.
According to Dr. Singer, none of IPC’s 105 hospitalist practices tie core measures to the group’s incentives, and prospective clients haven’t made core measures a top priority. Still, the firm has invested substantially in information technology (IT) infrastructure for hospitalists to track core measures compliance and other clinical indicators.
“In a pay-for-performance world, you need IT tools to help with core measures and DRG [diagnosis-related group] documentation, which will improve clinical and financial results dramatically.”
Ron Greeno, MD, CMO of Cogent Healthcare in Los Angeles, is dubious about tying core measures compliance to the presence of hospitalists. “The core measures are CMS’ attempt to devise a statistical representation of everything clinically relevant that a doctor does,” he says. “It’s like a quiz at school. You can memorize answers to the quiz without learning the subject … . It’s measuring quality by proxy.”
The fact that “hospitalist program” applies to a wide range of programs—from one emergency department doctor admitting patients to full-blown, highly organized, and well-resourced hospital medicine groups, also muddies the waters. “Comparing them on core measure compliance is not science,” concludes Dr. Greeno.
Team Health’s Dr. Goldsholl says that while hospitalists enhance core measures compliance many hospitals throw other resources at improving core measures compliance without much to show for it.
“Some hospitals have case managers telling doctors that they can’t discharge a patient without documenting core measure compliance, or [they] have hired one case manager per core measure,” she explains. “Others issue MD report cards. Some [hospitals] without strong quality improvement departments and strong governance aren’t sure what to do.”
Dr. Goldsholl points out that hospitalists, who routinely incorporate core measures compliance along with their other duties, give hospitals greater value for money spent than hiring case managers just for core measure compliance.
Then there are problems with the core measures themselves, as a recent JAMA study shows. Fonarow and colleagues examined the correlation between heart failure-related 60- to 90-day mortality and re-hospitalizations and CMS core measures.1 They concluded that “current heart failure performance measures, aside from prescription of an ACE inhibitor or angiotensin receptor blocker at discharge, have little relationship to mortality and combined mortality/rehospitalizations … post-hospitalization.” The authors urge the adoption of additional measures and better methods for identifying and validating heart failure performance measures.
More to Come
Core measure weakness notwithstanding, Dr. Greeno believes CMS core measures represent a major salvo in the pay-for-performance movement. “They’re the first step in changing the entire reimbursement system,” he says. “To succeed, a hospital will need the right doctors trained to work together as a team, with consensus on order sets, care protocols, excellent communication with primary care physicians, and statistical identification of obstacles to achieving quality within the hospitals.” TH
Marlene Piturro is a regular contributor to The Hospitalist.
Reference
- Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70.
Deciding to measure performance—whether by test scores or clinical indicators—is step one to improve what you’re measuring. So when the Centers for Medicare and Medicaid Services (CMS) awarded $8.85 million in incentives to hospitals that showed measurable care improvements in 2005, it was no surprise that industry stakeholders took notice. Top decile hospitals received a 3% bonus, while second decile winners received 1%; bonuses were based on the achievement of specific clinical quality indicators. CMS improved care quality in five targeted clinical areas by the percentages indicated: community-acquired pneumonia (CAP) by 10%, heart failure by 9%, hip/knee replacement and coronary artery bypass graft (CABG) by 5% each, and acute myocardial infarction (AMI) by 4%.
CMS’ core measures project encourages winners to tout their achievements to consumers, recruitable physicians, payers, and anyone else who will listen. Like any program based on achieving scores rather than identifying the processes necessary to achieve success, though, insiders can speculate about what variables are responsible for positive outcomes. In the case of CMS’ core measures, if hospitalist stakeholders can demonstrate that having hospitalists increases a hospital’s CMS core measure performance, they’ve earned important marketing and clinical leverage. Stacy Goldsholl, MD, of Wilmington, N.C.-based TeamHealth, estimates that more than 70% of TeamHealth’s potential clients now ask for her firm’s data on CMS core measures.
The Hospitalist’s Measures
To explore the relationship between a hospital’s position in the top two deciles on core measures with its hospitalist program, The Hospitalist extrapolated data from the CMS/Premier Hospital Quality Incentive Demonstration Project (www.premierinc.com/quality-safety) and SHM’s membership list, a proxy for a comprehensive list of hospitalist programs. All 44 hospitals in the top two deciles for heart failure core measures and the 49 hospitals listed for CAP were checked against the SHM list, as were their Web sites, for mention of a hospitalist program.
We compared data on two of the five core measures: heart failure and CAP. We expected a higher correlation for CAP because hospitalists are more likely to have primary inpatient responsibility for CAP patients than they are for heart failure patients, for whom cardiologists often have primary accountability. Here are the results of The Hospitalist’s analysis.
Hospitals in the top 10% for heart failure core measures are St. Helena Hospital (Calif.), Homestead Hospital (Fla.), Kootenai Medical Center (Idaho), Mission Hospital (N.C.), Staten Island University Hospital (N.Y.), Harris Methodist Fort Worth (Texas), and Harris Methodist Southwest (Texas).
Top decile performers in CAP are Methodist Medical Center of Illinois (Ill.), St. Vincent Memorial Hospital (Ill.), Heartland Regional Medical Center (Mo.), Stanly Memorial Hospital (N.C.), Alegent Health Immanuel Medical Center (Neb.), Staten Island University Hospital (N.Y.), Presbyterian Hospital of Kaufman (Texas), and Aurora Medical Center (Wis.).
Hospitals with some form of hospitalist program performed well, particularly on the second decile of the two core measures The Hospitalist examined: heart failure (44%) and community-acquired pneumonia (58%).
Complex Issues
Hospitalists expressed varied reactions to The Hospitalist’s correlation between a hospital’s core measures performance and its use of hospitalists. Adam Singer, MD, CEO of IPC-The Hospitalist Company of North Hollywood, Calif., scanned The Hospitalist’s lists and found a number of top-performing hospitals on its roster, including Methodist Forth Worth and Methodist Southwest in Texas.
According to Dr. Singer, none of IPC’s 105 hospitalist practices tie core measures to the group’s incentives, and prospective clients haven’t made core measures a top priority. Still, the firm has invested substantially in information technology (IT) infrastructure for hospitalists to track core measures compliance and other clinical indicators.
“In a pay-for-performance world, you need IT tools to help with core measures and DRG [diagnosis-related group] documentation, which will improve clinical and financial results dramatically.”
Ron Greeno, MD, CMO of Cogent Healthcare in Los Angeles, is dubious about tying core measures compliance to the presence of hospitalists. “The core measures are CMS’ attempt to devise a statistical representation of everything clinically relevant that a doctor does,” he says. “It’s like a quiz at school. You can memorize answers to the quiz without learning the subject … . It’s measuring quality by proxy.”
The fact that “hospitalist program” applies to a wide range of programs—from one emergency department doctor admitting patients to full-blown, highly organized, and well-resourced hospital medicine groups, also muddies the waters. “Comparing them on core measure compliance is not science,” concludes Dr. Greeno.
Team Health’s Dr. Goldsholl says that while hospitalists enhance core measures compliance many hospitals throw other resources at improving core measures compliance without much to show for it.
“Some hospitals have case managers telling doctors that they can’t discharge a patient without documenting core measure compliance, or [they] have hired one case manager per core measure,” she explains. “Others issue MD report cards. Some [hospitals] without strong quality improvement departments and strong governance aren’t sure what to do.”
Dr. Goldsholl points out that hospitalists, who routinely incorporate core measures compliance along with their other duties, give hospitals greater value for money spent than hiring case managers just for core measure compliance.
Then there are problems with the core measures themselves, as a recent JAMA study shows. Fonarow and colleagues examined the correlation between heart failure-related 60- to 90-day mortality and re-hospitalizations and CMS core measures.1 They concluded that “current heart failure performance measures, aside from prescription of an ACE inhibitor or angiotensin receptor blocker at discharge, have little relationship to mortality and combined mortality/rehospitalizations … post-hospitalization.” The authors urge the adoption of additional measures and better methods for identifying and validating heart failure performance measures.
More to Come
Core measure weakness notwithstanding, Dr. Greeno believes CMS core measures represent a major salvo in the pay-for-performance movement. “They’re the first step in changing the entire reimbursement system,” he says. “To succeed, a hospital will need the right doctors trained to work together as a team, with consensus on order sets, care protocols, excellent communication with primary care physicians, and statistical identification of obstacles to achieving quality within the hospitals.” TH
Marlene Piturro is a regular contributor to The Hospitalist.
Reference
- Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70.
Deciding to measure performance—whether by test scores or clinical indicators—is step one to improve what you’re measuring. So when the Centers for Medicare and Medicaid Services (CMS) awarded $8.85 million in incentives to hospitals that showed measurable care improvements in 2005, it was no surprise that industry stakeholders took notice. Top decile hospitals received a 3% bonus, while second decile winners received 1%; bonuses were based on the achievement of specific clinical quality indicators. CMS improved care quality in five targeted clinical areas by the percentages indicated: community-acquired pneumonia (CAP) by 10%, heart failure by 9%, hip/knee replacement and coronary artery bypass graft (CABG) by 5% each, and acute myocardial infarction (AMI) by 4%.
CMS’ core measures project encourages winners to tout their achievements to consumers, recruitable physicians, payers, and anyone else who will listen. Like any program based on achieving scores rather than identifying the processes necessary to achieve success, though, insiders can speculate about what variables are responsible for positive outcomes. In the case of CMS’ core measures, if hospitalist stakeholders can demonstrate that having hospitalists increases a hospital’s CMS core measure performance, they’ve earned important marketing and clinical leverage. Stacy Goldsholl, MD, of Wilmington, N.C.-based TeamHealth, estimates that more than 70% of TeamHealth’s potential clients now ask for her firm’s data on CMS core measures.
The Hospitalist’s Measures
To explore the relationship between a hospital’s position in the top two deciles on core measures with its hospitalist program, The Hospitalist extrapolated data from the CMS/Premier Hospital Quality Incentive Demonstration Project (www.premierinc.com/quality-safety) and SHM’s membership list, a proxy for a comprehensive list of hospitalist programs. All 44 hospitals in the top two deciles for heart failure core measures and the 49 hospitals listed for CAP were checked against the SHM list, as were their Web sites, for mention of a hospitalist program.
We compared data on two of the five core measures: heart failure and CAP. We expected a higher correlation for CAP because hospitalists are more likely to have primary inpatient responsibility for CAP patients than they are for heart failure patients, for whom cardiologists often have primary accountability. Here are the results of The Hospitalist’s analysis.
Hospitals in the top 10% for heart failure core measures are St. Helena Hospital (Calif.), Homestead Hospital (Fla.), Kootenai Medical Center (Idaho), Mission Hospital (N.C.), Staten Island University Hospital (N.Y.), Harris Methodist Fort Worth (Texas), and Harris Methodist Southwest (Texas).
Top decile performers in CAP are Methodist Medical Center of Illinois (Ill.), St. Vincent Memorial Hospital (Ill.), Heartland Regional Medical Center (Mo.), Stanly Memorial Hospital (N.C.), Alegent Health Immanuel Medical Center (Neb.), Staten Island University Hospital (N.Y.), Presbyterian Hospital of Kaufman (Texas), and Aurora Medical Center (Wis.).
Hospitals with some form of hospitalist program performed well, particularly on the second decile of the two core measures The Hospitalist examined: heart failure (44%) and community-acquired pneumonia (58%).
Complex Issues
Hospitalists expressed varied reactions to The Hospitalist’s correlation between a hospital’s core measures performance and its use of hospitalists. Adam Singer, MD, CEO of IPC-The Hospitalist Company of North Hollywood, Calif., scanned The Hospitalist’s lists and found a number of top-performing hospitals on its roster, including Methodist Forth Worth and Methodist Southwest in Texas.
According to Dr. Singer, none of IPC’s 105 hospitalist practices tie core measures to the group’s incentives, and prospective clients haven’t made core measures a top priority. Still, the firm has invested substantially in information technology (IT) infrastructure for hospitalists to track core measures compliance and other clinical indicators.
“In a pay-for-performance world, you need IT tools to help with core measures and DRG [diagnosis-related group] documentation, which will improve clinical and financial results dramatically.”
Ron Greeno, MD, CMO of Cogent Healthcare in Los Angeles, is dubious about tying core measures compliance to the presence of hospitalists. “The core measures are CMS’ attempt to devise a statistical representation of everything clinically relevant that a doctor does,” he says. “It’s like a quiz at school. You can memorize answers to the quiz without learning the subject … . It’s measuring quality by proxy.”
The fact that “hospitalist program” applies to a wide range of programs—from one emergency department doctor admitting patients to full-blown, highly organized, and well-resourced hospital medicine groups, also muddies the waters. “Comparing them on core measure compliance is not science,” concludes Dr. Greeno.
Team Health’s Dr. Goldsholl says that while hospitalists enhance core measures compliance many hospitals throw other resources at improving core measures compliance without much to show for it.
“Some hospitals have case managers telling doctors that they can’t discharge a patient without documenting core measure compliance, or [they] have hired one case manager per core measure,” she explains. “Others issue MD report cards. Some [hospitals] without strong quality improvement departments and strong governance aren’t sure what to do.”
Dr. Goldsholl points out that hospitalists, who routinely incorporate core measures compliance along with their other duties, give hospitals greater value for money spent than hiring case managers just for core measure compliance.
Then there are problems with the core measures themselves, as a recent JAMA study shows. Fonarow and colleagues examined the correlation between heart failure-related 60- to 90-day mortality and re-hospitalizations and CMS core measures.1 They concluded that “current heart failure performance measures, aside from prescription of an ACE inhibitor or angiotensin receptor blocker at discharge, have little relationship to mortality and combined mortality/rehospitalizations … post-hospitalization.” The authors urge the adoption of additional measures and better methods for identifying and validating heart failure performance measures.
More to Come
Core measure weakness notwithstanding, Dr. Greeno believes CMS core measures represent a major salvo in the pay-for-performance movement. “They’re the first step in changing the entire reimbursement system,” he says. “To succeed, a hospital will need the right doctors trained to work together as a team, with consensus on order sets, care protocols, excellent communication with primary care physicians, and statistical identification of obstacles to achieving quality within the hospitals.” TH
Marlene Piturro is a regular contributor to The Hospitalist.
Reference
- Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. JAMA. 2007 Jan 3;297(1):61-70.
A Pennsylvania Practice
More than 20 years before the term hospitalist was coined, the Brockie Medical Group, a strong internal medicine practice led by Benjamin Hoover, MD, relished its hospital work at York Hospital in York, Pa. Back then, the doctors didn’t call themselves hospitalists, but the time they spent on hospital duties made them the forebears of today’s hospitalists.
According to John McConville, MD, chairman of York Hospital’s department of medicine and a hospital fixture since 1976, some of Brockie Internal Medicine group’s physicians devoted 60% to 70% of their practice time to inpatient tasks. “That was the culture when I arrived on the scene,” he recounts. Shortly thereafter, the group grew stronger when The Brockie Internal Medicine Group’s main competition—a sizable family practice group—fell apart. Brockie absorbed its like-minded physicians.
York, pa.
The Brockie Internal Medical Group is firmly anchored in York, Pa., home to factories that produce barbells and Harley-Davidson motorcycles. York has a soft side, though—it produced the first Peppermint Pattie, a mint-chocolate candy. It is an affordable, rapidly growing suburb, a place where commuters to Philadelphia, Baltimore, and Washington, D.C., can have a comfortable lifestyle without big city housing prices and the hassles of urban life.
The medical community is close-knit, described by Jonathan Whitney, MD, a Brockie hospitalist leader, as “a collegial environment with a growing population and plenty of patients, so there’s not a sense of competition among physicians.” Dr. Whitney, along with William “Tex” Landis, MD, and Michael Lamanteer, MD, form the Brockie Hospitalist Group’s executive committee, elected decision makers who deal with WellSpan Health and York Hospital on behalf of their colleagues.
WellSpan’s Role
As York grew, so did the Brockie Internal Medical Group. Then came managed care in the 1980s and 1990s, and Brockie’s internists were not happy. “We saw the medical landscape changing everywhere, and we didn’t want managed care pushing us around,” explains Dr. Landis, a Lancaster, Pa., native and now the Brockie Hospitalist Group’s lead physician. “Analyzing how medicine was changing, we felt vulnerable as a single specialty group. We considered various scenarios for becoming a multi-specialty practice, but decided that wasn’t right for us.”
So, in 1995, five group partners decided to sell the practice to WellSpan Health, an integrated nonprofit healthcare system located in South Central Pennsylvania. Their expectation? That WellSpan’s administrative support and financial muscle would protect them against managed care’s encroachment.
Affiliating with WellSpan Health aligned Brockie with the medical services line of York Hospital, providing the administrative support they needed to grow and thrive. Working together, Brockie’s medical leaders and WellSpan administrators oversee the following areas: strategic planning; budgeting, compensation, benefits, and incentives; collections and coding; care management and performance improvement; recruiting and other personnel issues; and scheduling and coverage.
The Hospitalist Program
York Hospital and its surrounding community continued to grow, as did the need for more office-based and inpatient physician services. By 2001, York Hospital’s top executives recognized that a dedicated hospitalist group was the best solution for its overflowing emergency department (ED), booming admissions, and climbing average daily census. As specialists in internal medicine already heavily involved in inpatient care, the Brockie Internal Medical Group was York Hospital’s obvious choice to pioneer a hospital medicine program. Five Brockie physicians chose to join the newly minted inpatient hospital group (the Brockie Hospitalist Group), with four others continuing outpatient care. Over time, seven more hospitalists came on board, with more anticipated in late 2006 through mid-2007.
Part of the York Hospital mindset is that the demand for inpatient services would keep climbing as the community continued to attract newcomers. An unanticipated consequence of having a hospital medicine program was that outpatient practices quickly grew by 20% because they had offloaded their hospital work, in turn generating more hospital admissions. Brockie and York leaders, recognizing the possibility of stress and burnout on hospitalists as their volume of work grew, took steps to avert problems. “We’re in a sustained growth mode and we need the hospitalists to be satisfied with their compensation and schedules to be able to recruit new physicians,” says Dr. McConville. “Hospital administration underwrites the hospitalist program’s shortfall so that we can pay [the hospitalists] a salary commensurate with MGMA [Medical Group Management Association] guidelines plus productivity. It’s a substantial amount annually and well worth it,” he adds.
Unlike many hospitalist programs, York Hospital’s did not arise because physicians wanted to avoid driving to the hospital to make rounds. “Some groups are five minutes away and they gave us their inpatient work, while a group that’s 45 minutes away still does hospital rounds. What drives physicians here is their view of continuity of care,” says Dr. McConville.
Brockie is York’s only hospitalist group, although three other medical groups have hired two doctors to handle their inpatient work. “It’s not a problem for us. We don’t have a sense of competition,” says Dr. Whitney.
The Nuts and Bolts
Perhaps it’s Brockie’s long tenure as a medical group, its acquisition by WellSpan and the performance expectations that such an acquisition denotes, the thoroughness of its hospitalist leaders, or some combination of the above, but the hospitalists have their schedules and compensation calculations down pat.
Dr. Lamanteer spends much time and thought on the hospitalists’ compensation package. He studies national salary data and factors them into a sophisticated system of relative value units (RVUs) and case-based data to maintain a “competitive compensation package that provides incentives for both our physicians and the hospital to balance productivity with keeping length of stay in check,” he says. That’s not as easy as he makes it sound, because bumping up RVUs and volume has to be balanced with a length of stay that is both efficient and safe for patients.
Compensation begins with base salary—either Level I for 132 hours or Level II for 147 hours over three weeks. Productivity bonuses start with one point awarded for each admission, discharge, consult, and ED evaluation. Point values are then adjusted for average professional revenue generated per patient. The threshold for bonus pay is 806 points. Additionally, three clinical performance criteria, chosen annually, impact the bonus. For example, recent targets include ordering a tentative discharge time one or more days in advance (>65%), abiding by the “do not use” abbreviation list created by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (>90%), and complying with diagnostic coding rules (>75% accuracy).
The hospitalists’ schedule is challenging, particularly for doctors way past residency, involving 8 a.m. to 10 p.m. shifts on a three-week cycle that starts on a Friday. Physicians work eight 14-hour days, followed by a weekend off, then five days on (Monday-Friday) and six days off (Saturday-Thursday). The hospitalists don’t routinely cover night call. A full-time nocturnist, who started in 1992, and moonlighters cover the 10 p.m. to 8 a.m. shift seven days a week, with hospitalists covering only for major emergencies.
Avoiding Burnout
York Hospital’s ED and a cap on residents’ hours keep the Brockie hospitalists busy. But, early in 2005, it looked as if the workload had reached a plateau. Although Dr. Whitney suspected that the breather wouldn’t last, the group had no evidence that the tempo would increase and voted to maintain the number of hospitalists. The tempo picked up.
“We had estimated an 11 percent growth in RVUs, which actually grew by 23 percent last year,” says Dr. Whitney. Then a large primary care group agreed to shift its inpatient work to Brockie in 2006. Dr. Whitney estimated that assuming that practice’s hospital patients would add 5,000 RVUs and 600 more admissions.
“We realized we could approach a point of stress and burnout with the increased workload, so we recruited two new hospitalists,” says Dr. Whitney.
Still, the hospitalists face a balancing act of census peaks and valleys. “The variations with census and admissions go well beyond the bell curve,” says Whitney, who prepares for crunches by finding volunteers among the hospitalists to cover unexpected peaks.
If Brockie sounds like a Harvard case study on hospitalist medicine, it should. Its long tenure, physician leadership, and administrative support have shaped the business practices that facilitated the program’s growth. For one, the sophisticated compensation/productivity scheme didn’t come about by accident. Dr. McConville, a representative of WellSpan’s medical service line, meets with three Brockie hospitalists to fine-tune the program’s metrics. QI measures that are newly written each year, regular individual feedback, and inclusion of evidence-based guidelines contribute to measures and practices that address many of hospital medicine’s problems.
A Big Step to Little Things
But Brockie isn’t perfect. The responsibility of 24/7 coverage and 14-hour days allows little things to fall through the cracks—things like finding the time to promote the hospitalist service on the Web site, getting new formulary updates out quickly, and immediately informing all of those concerned that a patient has died. Brockie has addressed those and other issues that are the mortar to the bricks of a hospitalist practice by hiring David Orskey, an ex-Navy corpsman, as its senior practice manager in July 2006.
Orskey, co-chair of the medical group’s process improvement committee, sees his work as finding efficiencies, working for better care, and increasing patient satisfaction, plus attending to the budget and human resources issues and networking with outpatient practices.
“Twenty-one years in Navy medicine prepared me for this job,” says Orskey. “I’m enjoying this community, which has everything from farmland to executive homes and an influx of Hispanic migrants.”
He’s able to focus on both the details and the big picture, such as making sure that everyone works toward implementing and using the electronic medical record and improving after-hours answering services, as well as refining credentialing and risk management.
LTAC Unit
Brockie’s hospitalists also serve Mechanicsburg, Pa.,-based Select Medical Corporation’s long-term acute care (LTAC) unit, a 30-bed unit within York Hospital that supports patients needing a bridge between an acute hospital and skilled nursing care. The patients run the gamut in their needs—some have pulmonary/ventilator issues; others present medically complex situations such as heart failure, multi-system organ impairment, and cancer; some are neurosurgical/post trauma; and others need specialized wound care.
Dr. Whitney explains that all Brockie hospitalists add the LTAC to their rounds, usually leaving them for the end of the day, when the physicians can better attend to their complex situations. “Many of these patients are older, have been in the ICU with complicated medical issues, and face weeks of care in the LTAC before they can go to a nursing home or another long-term care setting,” he says. “It’s a whole different LOS, and it’s good that we have the LTAC because it reduces the hospital’s burden of caring for them as acute patients, when they really need what the LTAC offers.”
Conclusion
Dr. Lamanteer keeps an eye on the Brockie hospitalists’ future. “It’s clear that we benefit patients, that we provide excellent care, and that we need a large subsidy to do it,” he says. And the big picture means keeping focused on the peaks and valleys of admissions and wondering how volume will grow in the next ten years. He’d like to limit the number of 14-hour shifts to help physicians avoid burnout and to limit weekend duty to one out of three (sustainable) or one out of four (heaven). TH
Marlene Piturro is based in New York.
More than 20 years before the term hospitalist was coined, the Brockie Medical Group, a strong internal medicine practice led by Benjamin Hoover, MD, relished its hospital work at York Hospital in York, Pa. Back then, the doctors didn’t call themselves hospitalists, but the time they spent on hospital duties made them the forebears of today’s hospitalists.
According to John McConville, MD, chairman of York Hospital’s department of medicine and a hospital fixture since 1976, some of Brockie Internal Medicine group’s physicians devoted 60% to 70% of their practice time to inpatient tasks. “That was the culture when I arrived on the scene,” he recounts. Shortly thereafter, the group grew stronger when The Brockie Internal Medicine Group’s main competition—a sizable family practice group—fell apart. Brockie absorbed its like-minded physicians.
York, pa.
The Brockie Internal Medical Group is firmly anchored in York, Pa., home to factories that produce barbells and Harley-Davidson motorcycles. York has a soft side, though—it produced the first Peppermint Pattie, a mint-chocolate candy. It is an affordable, rapidly growing suburb, a place where commuters to Philadelphia, Baltimore, and Washington, D.C., can have a comfortable lifestyle without big city housing prices and the hassles of urban life.
The medical community is close-knit, described by Jonathan Whitney, MD, a Brockie hospitalist leader, as “a collegial environment with a growing population and plenty of patients, so there’s not a sense of competition among physicians.” Dr. Whitney, along with William “Tex” Landis, MD, and Michael Lamanteer, MD, form the Brockie Hospitalist Group’s executive committee, elected decision makers who deal with WellSpan Health and York Hospital on behalf of their colleagues.
WellSpan’s Role
As York grew, so did the Brockie Internal Medical Group. Then came managed care in the 1980s and 1990s, and Brockie’s internists were not happy. “We saw the medical landscape changing everywhere, and we didn’t want managed care pushing us around,” explains Dr. Landis, a Lancaster, Pa., native and now the Brockie Hospitalist Group’s lead physician. “Analyzing how medicine was changing, we felt vulnerable as a single specialty group. We considered various scenarios for becoming a multi-specialty practice, but decided that wasn’t right for us.”
So, in 1995, five group partners decided to sell the practice to WellSpan Health, an integrated nonprofit healthcare system located in South Central Pennsylvania. Their expectation? That WellSpan’s administrative support and financial muscle would protect them against managed care’s encroachment.
Affiliating with WellSpan Health aligned Brockie with the medical services line of York Hospital, providing the administrative support they needed to grow and thrive. Working together, Brockie’s medical leaders and WellSpan administrators oversee the following areas: strategic planning; budgeting, compensation, benefits, and incentives; collections and coding; care management and performance improvement; recruiting and other personnel issues; and scheduling and coverage.
The Hospitalist Program
York Hospital and its surrounding community continued to grow, as did the need for more office-based and inpatient physician services. By 2001, York Hospital’s top executives recognized that a dedicated hospitalist group was the best solution for its overflowing emergency department (ED), booming admissions, and climbing average daily census. As specialists in internal medicine already heavily involved in inpatient care, the Brockie Internal Medical Group was York Hospital’s obvious choice to pioneer a hospital medicine program. Five Brockie physicians chose to join the newly minted inpatient hospital group (the Brockie Hospitalist Group), with four others continuing outpatient care. Over time, seven more hospitalists came on board, with more anticipated in late 2006 through mid-2007.
Part of the York Hospital mindset is that the demand for inpatient services would keep climbing as the community continued to attract newcomers. An unanticipated consequence of having a hospital medicine program was that outpatient practices quickly grew by 20% because they had offloaded their hospital work, in turn generating more hospital admissions. Brockie and York leaders, recognizing the possibility of stress and burnout on hospitalists as their volume of work grew, took steps to avert problems. “We’re in a sustained growth mode and we need the hospitalists to be satisfied with their compensation and schedules to be able to recruit new physicians,” says Dr. McConville. “Hospital administration underwrites the hospitalist program’s shortfall so that we can pay [the hospitalists] a salary commensurate with MGMA [Medical Group Management Association] guidelines plus productivity. It’s a substantial amount annually and well worth it,” he adds.
Unlike many hospitalist programs, York Hospital’s did not arise because physicians wanted to avoid driving to the hospital to make rounds. “Some groups are five minutes away and they gave us their inpatient work, while a group that’s 45 minutes away still does hospital rounds. What drives physicians here is their view of continuity of care,” says Dr. McConville.
Brockie is York’s only hospitalist group, although three other medical groups have hired two doctors to handle their inpatient work. “It’s not a problem for us. We don’t have a sense of competition,” says Dr. Whitney.
The Nuts and Bolts
Perhaps it’s Brockie’s long tenure as a medical group, its acquisition by WellSpan and the performance expectations that such an acquisition denotes, the thoroughness of its hospitalist leaders, or some combination of the above, but the hospitalists have their schedules and compensation calculations down pat.
Dr. Lamanteer spends much time and thought on the hospitalists’ compensation package. He studies national salary data and factors them into a sophisticated system of relative value units (RVUs) and case-based data to maintain a “competitive compensation package that provides incentives for both our physicians and the hospital to balance productivity with keeping length of stay in check,” he says. That’s not as easy as he makes it sound, because bumping up RVUs and volume has to be balanced with a length of stay that is both efficient and safe for patients.
Compensation begins with base salary—either Level I for 132 hours or Level II for 147 hours over three weeks. Productivity bonuses start with one point awarded for each admission, discharge, consult, and ED evaluation. Point values are then adjusted for average professional revenue generated per patient. The threshold for bonus pay is 806 points. Additionally, three clinical performance criteria, chosen annually, impact the bonus. For example, recent targets include ordering a tentative discharge time one or more days in advance (>65%), abiding by the “do not use” abbreviation list created by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (>90%), and complying with diagnostic coding rules (>75% accuracy).
The hospitalists’ schedule is challenging, particularly for doctors way past residency, involving 8 a.m. to 10 p.m. shifts on a three-week cycle that starts on a Friday. Physicians work eight 14-hour days, followed by a weekend off, then five days on (Monday-Friday) and six days off (Saturday-Thursday). The hospitalists don’t routinely cover night call. A full-time nocturnist, who started in 1992, and moonlighters cover the 10 p.m. to 8 a.m. shift seven days a week, with hospitalists covering only for major emergencies.
Avoiding Burnout
York Hospital’s ED and a cap on residents’ hours keep the Brockie hospitalists busy. But, early in 2005, it looked as if the workload had reached a plateau. Although Dr. Whitney suspected that the breather wouldn’t last, the group had no evidence that the tempo would increase and voted to maintain the number of hospitalists. The tempo picked up.
“We had estimated an 11 percent growth in RVUs, which actually grew by 23 percent last year,” says Dr. Whitney. Then a large primary care group agreed to shift its inpatient work to Brockie in 2006. Dr. Whitney estimated that assuming that practice’s hospital patients would add 5,000 RVUs and 600 more admissions.
“We realized we could approach a point of stress and burnout with the increased workload, so we recruited two new hospitalists,” says Dr. Whitney.
Still, the hospitalists face a balancing act of census peaks and valleys. “The variations with census and admissions go well beyond the bell curve,” says Whitney, who prepares for crunches by finding volunteers among the hospitalists to cover unexpected peaks.
If Brockie sounds like a Harvard case study on hospitalist medicine, it should. Its long tenure, physician leadership, and administrative support have shaped the business practices that facilitated the program’s growth. For one, the sophisticated compensation/productivity scheme didn’t come about by accident. Dr. McConville, a representative of WellSpan’s medical service line, meets with three Brockie hospitalists to fine-tune the program’s metrics. QI measures that are newly written each year, regular individual feedback, and inclusion of evidence-based guidelines contribute to measures and practices that address many of hospital medicine’s problems.
A Big Step to Little Things
But Brockie isn’t perfect. The responsibility of 24/7 coverage and 14-hour days allows little things to fall through the cracks—things like finding the time to promote the hospitalist service on the Web site, getting new formulary updates out quickly, and immediately informing all of those concerned that a patient has died. Brockie has addressed those and other issues that are the mortar to the bricks of a hospitalist practice by hiring David Orskey, an ex-Navy corpsman, as its senior practice manager in July 2006.
Orskey, co-chair of the medical group’s process improvement committee, sees his work as finding efficiencies, working for better care, and increasing patient satisfaction, plus attending to the budget and human resources issues and networking with outpatient practices.
“Twenty-one years in Navy medicine prepared me for this job,” says Orskey. “I’m enjoying this community, which has everything from farmland to executive homes and an influx of Hispanic migrants.”
He’s able to focus on both the details and the big picture, such as making sure that everyone works toward implementing and using the electronic medical record and improving after-hours answering services, as well as refining credentialing and risk management.
LTAC Unit
Brockie’s hospitalists also serve Mechanicsburg, Pa.,-based Select Medical Corporation’s long-term acute care (LTAC) unit, a 30-bed unit within York Hospital that supports patients needing a bridge between an acute hospital and skilled nursing care. The patients run the gamut in their needs—some have pulmonary/ventilator issues; others present medically complex situations such as heart failure, multi-system organ impairment, and cancer; some are neurosurgical/post trauma; and others need specialized wound care.
Dr. Whitney explains that all Brockie hospitalists add the LTAC to their rounds, usually leaving them for the end of the day, when the physicians can better attend to their complex situations. “Many of these patients are older, have been in the ICU with complicated medical issues, and face weeks of care in the LTAC before they can go to a nursing home or another long-term care setting,” he says. “It’s a whole different LOS, and it’s good that we have the LTAC because it reduces the hospital’s burden of caring for them as acute patients, when they really need what the LTAC offers.”
Conclusion
Dr. Lamanteer keeps an eye on the Brockie hospitalists’ future. “It’s clear that we benefit patients, that we provide excellent care, and that we need a large subsidy to do it,” he says. And the big picture means keeping focused on the peaks and valleys of admissions and wondering how volume will grow in the next ten years. He’d like to limit the number of 14-hour shifts to help physicians avoid burnout and to limit weekend duty to one out of three (sustainable) or one out of four (heaven). TH
Marlene Piturro is based in New York.
More than 20 years before the term hospitalist was coined, the Brockie Medical Group, a strong internal medicine practice led by Benjamin Hoover, MD, relished its hospital work at York Hospital in York, Pa. Back then, the doctors didn’t call themselves hospitalists, but the time they spent on hospital duties made them the forebears of today’s hospitalists.
According to John McConville, MD, chairman of York Hospital’s department of medicine and a hospital fixture since 1976, some of Brockie Internal Medicine group’s physicians devoted 60% to 70% of their practice time to inpatient tasks. “That was the culture when I arrived on the scene,” he recounts. Shortly thereafter, the group grew stronger when The Brockie Internal Medicine Group’s main competition—a sizable family practice group—fell apart. Brockie absorbed its like-minded physicians.
York, pa.
The Brockie Internal Medical Group is firmly anchored in York, Pa., home to factories that produce barbells and Harley-Davidson motorcycles. York has a soft side, though—it produced the first Peppermint Pattie, a mint-chocolate candy. It is an affordable, rapidly growing suburb, a place where commuters to Philadelphia, Baltimore, and Washington, D.C., can have a comfortable lifestyle without big city housing prices and the hassles of urban life.
The medical community is close-knit, described by Jonathan Whitney, MD, a Brockie hospitalist leader, as “a collegial environment with a growing population and plenty of patients, so there’s not a sense of competition among physicians.” Dr. Whitney, along with William “Tex” Landis, MD, and Michael Lamanteer, MD, form the Brockie Hospitalist Group’s executive committee, elected decision makers who deal with WellSpan Health and York Hospital on behalf of their colleagues.
WellSpan’s Role
As York grew, so did the Brockie Internal Medical Group. Then came managed care in the 1980s and 1990s, and Brockie’s internists were not happy. “We saw the medical landscape changing everywhere, and we didn’t want managed care pushing us around,” explains Dr. Landis, a Lancaster, Pa., native and now the Brockie Hospitalist Group’s lead physician. “Analyzing how medicine was changing, we felt vulnerable as a single specialty group. We considered various scenarios for becoming a multi-specialty practice, but decided that wasn’t right for us.”
So, in 1995, five group partners decided to sell the practice to WellSpan Health, an integrated nonprofit healthcare system located in South Central Pennsylvania. Their expectation? That WellSpan’s administrative support and financial muscle would protect them against managed care’s encroachment.
Affiliating with WellSpan Health aligned Brockie with the medical services line of York Hospital, providing the administrative support they needed to grow and thrive. Working together, Brockie’s medical leaders and WellSpan administrators oversee the following areas: strategic planning; budgeting, compensation, benefits, and incentives; collections and coding; care management and performance improvement; recruiting and other personnel issues; and scheduling and coverage.
The Hospitalist Program
York Hospital and its surrounding community continued to grow, as did the need for more office-based and inpatient physician services. By 2001, York Hospital’s top executives recognized that a dedicated hospitalist group was the best solution for its overflowing emergency department (ED), booming admissions, and climbing average daily census. As specialists in internal medicine already heavily involved in inpatient care, the Brockie Internal Medical Group was York Hospital’s obvious choice to pioneer a hospital medicine program. Five Brockie physicians chose to join the newly minted inpatient hospital group (the Brockie Hospitalist Group), with four others continuing outpatient care. Over time, seven more hospitalists came on board, with more anticipated in late 2006 through mid-2007.
Part of the York Hospital mindset is that the demand for inpatient services would keep climbing as the community continued to attract newcomers. An unanticipated consequence of having a hospital medicine program was that outpatient practices quickly grew by 20% because they had offloaded their hospital work, in turn generating more hospital admissions. Brockie and York leaders, recognizing the possibility of stress and burnout on hospitalists as their volume of work grew, took steps to avert problems. “We’re in a sustained growth mode and we need the hospitalists to be satisfied with their compensation and schedules to be able to recruit new physicians,” says Dr. McConville. “Hospital administration underwrites the hospitalist program’s shortfall so that we can pay [the hospitalists] a salary commensurate with MGMA [Medical Group Management Association] guidelines plus productivity. It’s a substantial amount annually and well worth it,” he adds.
Unlike many hospitalist programs, York Hospital’s did not arise because physicians wanted to avoid driving to the hospital to make rounds. “Some groups are five minutes away and they gave us their inpatient work, while a group that’s 45 minutes away still does hospital rounds. What drives physicians here is their view of continuity of care,” says Dr. McConville.
Brockie is York’s only hospitalist group, although three other medical groups have hired two doctors to handle their inpatient work. “It’s not a problem for us. We don’t have a sense of competition,” says Dr. Whitney.
The Nuts and Bolts
Perhaps it’s Brockie’s long tenure as a medical group, its acquisition by WellSpan and the performance expectations that such an acquisition denotes, the thoroughness of its hospitalist leaders, or some combination of the above, but the hospitalists have their schedules and compensation calculations down pat.
Dr. Lamanteer spends much time and thought on the hospitalists’ compensation package. He studies national salary data and factors them into a sophisticated system of relative value units (RVUs) and case-based data to maintain a “competitive compensation package that provides incentives for both our physicians and the hospital to balance productivity with keeping length of stay in check,” he says. That’s not as easy as he makes it sound, because bumping up RVUs and volume has to be balanced with a length of stay that is both efficient and safe for patients.
Compensation begins with base salary—either Level I for 132 hours or Level II for 147 hours over three weeks. Productivity bonuses start with one point awarded for each admission, discharge, consult, and ED evaluation. Point values are then adjusted for average professional revenue generated per patient. The threshold for bonus pay is 806 points. Additionally, three clinical performance criteria, chosen annually, impact the bonus. For example, recent targets include ordering a tentative discharge time one or more days in advance (>65%), abiding by the “do not use” abbreviation list created by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) (>90%), and complying with diagnostic coding rules (>75% accuracy).
The hospitalists’ schedule is challenging, particularly for doctors way past residency, involving 8 a.m. to 10 p.m. shifts on a three-week cycle that starts on a Friday. Physicians work eight 14-hour days, followed by a weekend off, then five days on (Monday-Friday) and six days off (Saturday-Thursday). The hospitalists don’t routinely cover night call. A full-time nocturnist, who started in 1992, and moonlighters cover the 10 p.m. to 8 a.m. shift seven days a week, with hospitalists covering only for major emergencies.
Avoiding Burnout
York Hospital’s ED and a cap on residents’ hours keep the Brockie hospitalists busy. But, early in 2005, it looked as if the workload had reached a plateau. Although Dr. Whitney suspected that the breather wouldn’t last, the group had no evidence that the tempo would increase and voted to maintain the number of hospitalists. The tempo picked up.
“We had estimated an 11 percent growth in RVUs, which actually grew by 23 percent last year,” says Dr. Whitney. Then a large primary care group agreed to shift its inpatient work to Brockie in 2006. Dr. Whitney estimated that assuming that practice’s hospital patients would add 5,000 RVUs and 600 more admissions.
“We realized we could approach a point of stress and burnout with the increased workload, so we recruited two new hospitalists,” says Dr. Whitney.
Still, the hospitalists face a balancing act of census peaks and valleys. “The variations with census and admissions go well beyond the bell curve,” says Whitney, who prepares for crunches by finding volunteers among the hospitalists to cover unexpected peaks.
If Brockie sounds like a Harvard case study on hospitalist medicine, it should. Its long tenure, physician leadership, and administrative support have shaped the business practices that facilitated the program’s growth. For one, the sophisticated compensation/productivity scheme didn’t come about by accident. Dr. McConville, a representative of WellSpan’s medical service line, meets with three Brockie hospitalists to fine-tune the program’s metrics. QI measures that are newly written each year, regular individual feedback, and inclusion of evidence-based guidelines contribute to measures and practices that address many of hospital medicine’s problems.
A Big Step to Little Things
But Brockie isn’t perfect. The responsibility of 24/7 coverage and 14-hour days allows little things to fall through the cracks—things like finding the time to promote the hospitalist service on the Web site, getting new formulary updates out quickly, and immediately informing all of those concerned that a patient has died. Brockie has addressed those and other issues that are the mortar to the bricks of a hospitalist practice by hiring David Orskey, an ex-Navy corpsman, as its senior practice manager in July 2006.
Orskey, co-chair of the medical group’s process improvement committee, sees his work as finding efficiencies, working for better care, and increasing patient satisfaction, plus attending to the budget and human resources issues and networking with outpatient practices.
“Twenty-one years in Navy medicine prepared me for this job,” says Orskey. “I’m enjoying this community, which has everything from farmland to executive homes and an influx of Hispanic migrants.”
He’s able to focus on both the details and the big picture, such as making sure that everyone works toward implementing and using the electronic medical record and improving after-hours answering services, as well as refining credentialing and risk management.
LTAC Unit
Brockie’s hospitalists also serve Mechanicsburg, Pa.,-based Select Medical Corporation’s long-term acute care (LTAC) unit, a 30-bed unit within York Hospital that supports patients needing a bridge between an acute hospital and skilled nursing care. The patients run the gamut in their needs—some have pulmonary/ventilator issues; others present medically complex situations such as heart failure, multi-system organ impairment, and cancer; some are neurosurgical/post trauma; and others need specialized wound care.
Dr. Whitney explains that all Brockie hospitalists add the LTAC to their rounds, usually leaving them for the end of the day, when the physicians can better attend to their complex situations. “Many of these patients are older, have been in the ICU with complicated medical issues, and face weeks of care in the LTAC before they can go to a nursing home or another long-term care setting,” he says. “It’s a whole different LOS, and it’s good that we have the LTAC because it reduces the hospital’s burden of caring for them as acute patients, when they really need what the LTAC offers.”
Conclusion
Dr. Lamanteer keeps an eye on the Brockie hospitalists’ future. “It’s clear that we benefit patients, that we provide excellent care, and that we need a large subsidy to do it,” he says. And the big picture means keeping focused on the peaks and valleys of admissions and wondering how volume will grow in the next ten years. He’d like to limit the number of 14-hour shifts to help physicians avoid burnout and to limit weekend duty to one out of three (sustainable) or one out of four (heaven). TH
Marlene Piturro is based in New York.
A Work in Progress
Most hospitalist programs start when hospital administrators realize that having physicians dedicated exclusively to inpatient care is a great idea. Administrators then recruit a lead hospitalist—perhaps a stellar performer straight from residency, a community doctor closing his office, or a doctor located through a specialty staffing group.
Colorado Permanente Medical Group (CPMG), backed by a brand as powerful as Starbucks or Nordstrom, did things differently. So imbued with the Permanente culture are its physicians that its hospitalist group arose organically from physicians serving Denver’s Exempla St. Joseph Hospital and Boulder Community Hospital. (See “Kaiser Permanente Culture,” below.)
“Thirty years ago Permanente explored building their own versus finding a cost-effective hospital. They chose us, and their clinic doctors rounded on what grew to 70% of our department of medicine patients,” says Robert Gibbons, MD, St. Joseph’s residency program director. “Then they saw they needed to provide full-time inpatient coverage—the advent of the hospitalist program. Soon many CPMG clinic doctors disappeared, but the quality of medicine remained the same.”
Regional Department Chief Lauren Fraser, MD, oversees the now-mature hospitalist program, which keeps growing in size, complexity, and competence. “We’re always a work in progress, and that’s good,” she says.
According to Joe Heaton, MD, currently a Good Samaritan hospitalist and formerly CPMG regional department chief, CPMG’s primary care departments targeted three areas for better care early in 1995: streamlining patient scheduling, developing a centralized call center, and starting a hospitalist program.
The hospitalist program aimed for cost neutrality by limiting staffing at both hospitals to the same full-time equivalents (FTEs). To avoid forcing physicians into unwelcome assignments, the department offered its 70 internal medicine and 30 family practice doctors four tracks:
- Track A meant full-time hospital work;
- Track B offered a 50-50 hospital-clinic split;
- Track C provided for a 70% clinic, 30% hospital schedule; and
- Track D was full-time clinic work.
The family medicine department opted out of hospital duty, while the internists tracked themselves as follows: eight each for full-time hospital and half-time hospital duty, 34 for 30% hospital time, and 20 for full-time clinic. Fortunately, the tracks chosen matched the hospitals’ needs, and the program was off and running by July 1995.
“At the time, our group’s size created one of the largest hospitalist programs, allowing us to provide 24/7 coverage with at least two physicians on site,” says Dr. Heaton of the launch.
The hospitalist program had immediate measurable impact. Average length of stay dropped by 15%, and Track A and C physicians had similar utilization measures, suggesting that the model of care delivery was the key driver—rather than the amount of time physicians spent in the hospital. Dr. Gibbons was impressed with the hospitalist group’s results, noting that St. Joseph’s average reduced length of stay of 0.7 to one full day was consistent with national benchmarks. Because CPMG sees only Permanente patients, St. Joseph eventually contracted with two other hospitalist groups: the Exempla Faculty Inpatient Team, which covers half of its unassigned patients, and Midtown Inpatient Medicine, private internists who cover the other half of the unassigned patients, co-manage with orthopedic surgeons, and cover for internal medicine groups that no longer make hospital rounds.
CPMG hospitalists also covered Boulder Community Hospital in Denver’s rapidly expanding suburbs until 2005, when CPMG’s contract expired. All six hospitalists moved to nearby Exempla’s new Good Samaritan Hospital, where patient volume grew quickly from 25-30 patients a day to 80; 90% of the patients are Permanente members. Hospitalist staffing jumped to 13 FTEs (19 physicians). “We recruited very aggressively, including lots of locum tenens and moonlighters to cover the booming volume,” explains Brian Thom, MD, assistant regional department chief, Good Samaritan Hospital.
More Measures
In addition to length of stay, CPMG tracks the percentage of patients discharged in less than 24 hours, readmission rates, and disease-specific mortality by provider. All hospitalists get regular reports of department averages and statistical analyses of individual physicians. “This may be controversial, but we must look at outliers to see if [the problem is] case mix, such as many hospice patients, or something else,” says Dr. Heaton.
Striving for high levels of clinical expertise and consistency is a CPMG hallmark. Working for a medical behemoth in the Denver area, CPMG doctors—whether clinic-based or hospitalists—have a huge opportunity to integrate care and to co-manage many conditions with their colleagues. Hospitalists also staff the ICUs. In 2000, William Kinnard, MD, CPMG’s ICU co-director, commented that the group’s use of data-driven protocols allowed hospitalists to practice effectively in ICUs.
As for patient satisfaction, Dr. Heaton admits to “struggling for good measures,” noting that CPMG tackled it head-on in 1999 when Executive Medical Director Jack Cochran, MD, addressed the level of patient tenacity it took to navigate CPMG. Physician career satisfaction was sinking from long chaotic workdays that left both patients and doctors frustrated. By re-engineering scheduling and visit processes, Dr. Cochran made things run more smoothly. Other initiatives included an eight-hour physician-patient interaction course, video vignettes starring CPMG doctors illustrating communication techniques, and formal physician-to-physician coaching. Dr. Fraser still sends new hires to the course, recognizing that good communication satisfies both patients and physicians.
Scheduling: Every Program’s Mt. Everest
Because of the hospitalist program’s size and longevity, physicians have experimented extensively with scheduling. As do many groups, it started with seven 12-hour days on/seven days off blocks, which proved dissatisfying both personally and professionally.
“We experimented with scheduling to find what was sustainable for physicians and provided patient continuity,” says Dr. Fraser. “We’ve found that six eight-hour days in a row of rounding works best.”
Scheduling has evolved to the point that hospitalists provide the following to meet the hospitalist’s, the group’s, and the hospital’s needs: a dedicated triage physician 24/7 to handle calls from all sources of patient flow, two hospitalists on site at all times, eight-hour rounding days, and call physicians who admit and cross-cover after 4 p.m. Average daily census (ADC) is 10-12, plus one or two admissions. While that appears low, if CPMG hospitalists worked 12-hour shifts, their ADC would be 13-16, consistent with national norms.
“Dropping to eight-hour, as opposed to 12-hour, days keeps the job sustainable and helps doctors avoid burnout,” says Dr. Fraser. “However, we work more days per month, an average of 20-22.”
Overall, the scheduling strategy is working. “The majority of physicians who started over a decade ago remain, including many mid-life hospitalists in their 40s and 50s,” she adds. Physicians, rather than administrators, handle scheduling. Dr. Fraser has found that physicians can accept that third triage shift in a month (or an extra night shift when they’re short-handed) when another physician is filling the slots.
Other Features
All CPMG hospitalists can participate in St. Joseph’s residency program as “teaching attendings” for one month. From them, residents learn to co-manage care and participate in interdisciplinary rounds with nurses and social workers. Physicians note that residents make a hospitalist’s life smoother.
“At Good Sam, we do all our own procedures, unlike St. Joe’s, where they have residents. With our patient volumes, there’s little breathing room, especially when we have to cover non-Kaiser patients,” says Dr. Thom. Eventually, residents will rotate through Good Samaritan as well as St. Joseph.
One of the advantages of working in a brand-new hospital like Good Samaritan is establishing systems from scratch. That includes the new hospital’s electronic medical record (EMR), which is integrated with CPMG’s outpatient EMR. “We set up our own systems, complete with order sets and protocols,” explains Dr. Thom. “Considering that 90% of our patients are CPMG members, this gives us a high level of integration, clinically and electronically.”
Challenges Ahead
Despite CPMG’s size and stellar track record, challenges remain. Dr. Fraser identifies them as salaries that rank last within the group, making recruiting difficult; a hard time providing adequate back-up if a physician is unexpectedly absent; adjustments to fluctuations in patient census; time pressures of hospital committee work; and identification of an optimal scheduling model that fosters continuity of care yet provides a sustainable work life.
The group’s size has drawbacks, which Dr. Heaton identifies as the potential for a physician to not feel mission critical or to hide, and that communication and face-to-face meetings get complicated.
“Overall, the program can always use fine tuning, but we love who we work with and have the ultimate respect for our colleagues, which is the true benchmark of the quality of a medical career,” concludes Dr. Fraser. TH
Marlene Piturro regularly writes “Practice Profile.”
Most hospitalist programs start when hospital administrators realize that having physicians dedicated exclusively to inpatient care is a great idea. Administrators then recruit a lead hospitalist—perhaps a stellar performer straight from residency, a community doctor closing his office, or a doctor located through a specialty staffing group.
Colorado Permanente Medical Group (CPMG), backed by a brand as powerful as Starbucks or Nordstrom, did things differently. So imbued with the Permanente culture are its physicians that its hospitalist group arose organically from physicians serving Denver’s Exempla St. Joseph Hospital and Boulder Community Hospital. (See “Kaiser Permanente Culture,” below.)
“Thirty years ago Permanente explored building their own versus finding a cost-effective hospital. They chose us, and their clinic doctors rounded on what grew to 70% of our department of medicine patients,” says Robert Gibbons, MD, St. Joseph’s residency program director. “Then they saw they needed to provide full-time inpatient coverage—the advent of the hospitalist program. Soon many CPMG clinic doctors disappeared, but the quality of medicine remained the same.”
Regional Department Chief Lauren Fraser, MD, oversees the now-mature hospitalist program, which keeps growing in size, complexity, and competence. “We’re always a work in progress, and that’s good,” she says.
According to Joe Heaton, MD, currently a Good Samaritan hospitalist and formerly CPMG regional department chief, CPMG’s primary care departments targeted three areas for better care early in 1995: streamlining patient scheduling, developing a centralized call center, and starting a hospitalist program.
The hospitalist program aimed for cost neutrality by limiting staffing at both hospitals to the same full-time equivalents (FTEs). To avoid forcing physicians into unwelcome assignments, the department offered its 70 internal medicine and 30 family practice doctors four tracks:
- Track A meant full-time hospital work;
- Track B offered a 50-50 hospital-clinic split;
- Track C provided for a 70% clinic, 30% hospital schedule; and
- Track D was full-time clinic work.
The family medicine department opted out of hospital duty, while the internists tracked themselves as follows: eight each for full-time hospital and half-time hospital duty, 34 for 30% hospital time, and 20 for full-time clinic. Fortunately, the tracks chosen matched the hospitals’ needs, and the program was off and running by July 1995.
“At the time, our group’s size created one of the largest hospitalist programs, allowing us to provide 24/7 coverage with at least two physicians on site,” says Dr. Heaton of the launch.
The hospitalist program had immediate measurable impact. Average length of stay dropped by 15%, and Track A and C physicians had similar utilization measures, suggesting that the model of care delivery was the key driver—rather than the amount of time physicians spent in the hospital. Dr. Gibbons was impressed with the hospitalist group’s results, noting that St. Joseph’s average reduced length of stay of 0.7 to one full day was consistent with national benchmarks. Because CPMG sees only Permanente patients, St. Joseph eventually contracted with two other hospitalist groups: the Exempla Faculty Inpatient Team, which covers half of its unassigned patients, and Midtown Inpatient Medicine, private internists who cover the other half of the unassigned patients, co-manage with orthopedic surgeons, and cover for internal medicine groups that no longer make hospital rounds.
CPMG hospitalists also covered Boulder Community Hospital in Denver’s rapidly expanding suburbs until 2005, when CPMG’s contract expired. All six hospitalists moved to nearby Exempla’s new Good Samaritan Hospital, where patient volume grew quickly from 25-30 patients a day to 80; 90% of the patients are Permanente members. Hospitalist staffing jumped to 13 FTEs (19 physicians). “We recruited very aggressively, including lots of locum tenens and moonlighters to cover the booming volume,” explains Brian Thom, MD, assistant regional department chief, Good Samaritan Hospital.
More Measures
In addition to length of stay, CPMG tracks the percentage of patients discharged in less than 24 hours, readmission rates, and disease-specific mortality by provider. All hospitalists get regular reports of department averages and statistical analyses of individual physicians. “This may be controversial, but we must look at outliers to see if [the problem is] case mix, such as many hospice patients, or something else,” says Dr. Heaton.
Striving for high levels of clinical expertise and consistency is a CPMG hallmark. Working for a medical behemoth in the Denver area, CPMG doctors—whether clinic-based or hospitalists—have a huge opportunity to integrate care and to co-manage many conditions with their colleagues. Hospitalists also staff the ICUs. In 2000, William Kinnard, MD, CPMG’s ICU co-director, commented that the group’s use of data-driven protocols allowed hospitalists to practice effectively in ICUs.
As for patient satisfaction, Dr. Heaton admits to “struggling for good measures,” noting that CPMG tackled it head-on in 1999 when Executive Medical Director Jack Cochran, MD, addressed the level of patient tenacity it took to navigate CPMG. Physician career satisfaction was sinking from long chaotic workdays that left both patients and doctors frustrated. By re-engineering scheduling and visit processes, Dr. Cochran made things run more smoothly. Other initiatives included an eight-hour physician-patient interaction course, video vignettes starring CPMG doctors illustrating communication techniques, and formal physician-to-physician coaching. Dr. Fraser still sends new hires to the course, recognizing that good communication satisfies both patients and physicians.
Scheduling: Every Program’s Mt. Everest
Because of the hospitalist program’s size and longevity, physicians have experimented extensively with scheduling. As do many groups, it started with seven 12-hour days on/seven days off blocks, which proved dissatisfying both personally and professionally.
“We experimented with scheduling to find what was sustainable for physicians and provided patient continuity,” says Dr. Fraser. “We’ve found that six eight-hour days in a row of rounding works best.”
Scheduling has evolved to the point that hospitalists provide the following to meet the hospitalist’s, the group’s, and the hospital’s needs: a dedicated triage physician 24/7 to handle calls from all sources of patient flow, two hospitalists on site at all times, eight-hour rounding days, and call physicians who admit and cross-cover after 4 p.m. Average daily census (ADC) is 10-12, plus one or two admissions. While that appears low, if CPMG hospitalists worked 12-hour shifts, their ADC would be 13-16, consistent with national norms.
“Dropping to eight-hour, as opposed to 12-hour, days keeps the job sustainable and helps doctors avoid burnout,” says Dr. Fraser. “However, we work more days per month, an average of 20-22.”
Overall, the scheduling strategy is working. “The majority of physicians who started over a decade ago remain, including many mid-life hospitalists in their 40s and 50s,” she adds. Physicians, rather than administrators, handle scheduling. Dr. Fraser has found that physicians can accept that third triage shift in a month (or an extra night shift when they’re short-handed) when another physician is filling the slots.
Other Features
All CPMG hospitalists can participate in St. Joseph’s residency program as “teaching attendings” for one month. From them, residents learn to co-manage care and participate in interdisciplinary rounds with nurses and social workers. Physicians note that residents make a hospitalist’s life smoother.
“At Good Sam, we do all our own procedures, unlike St. Joe’s, where they have residents. With our patient volumes, there’s little breathing room, especially when we have to cover non-Kaiser patients,” says Dr. Thom. Eventually, residents will rotate through Good Samaritan as well as St. Joseph.
One of the advantages of working in a brand-new hospital like Good Samaritan is establishing systems from scratch. That includes the new hospital’s electronic medical record (EMR), which is integrated with CPMG’s outpatient EMR. “We set up our own systems, complete with order sets and protocols,” explains Dr. Thom. “Considering that 90% of our patients are CPMG members, this gives us a high level of integration, clinically and electronically.”
Challenges Ahead
Despite CPMG’s size and stellar track record, challenges remain. Dr. Fraser identifies them as salaries that rank last within the group, making recruiting difficult; a hard time providing adequate back-up if a physician is unexpectedly absent; adjustments to fluctuations in patient census; time pressures of hospital committee work; and identification of an optimal scheduling model that fosters continuity of care yet provides a sustainable work life.
The group’s size has drawbacks, which Dr. Heaton identifies as the potential for a physician to not feel mission critical or to hide, and that communication and face-to-face meetings get complicated.
“Overall, the program can always use fine tuning, but we love who we work with and have the ultimate respect for our colleagues, which is the true benchmark of the quality of a medical career,” concludes Dr. Fraser. TH
Marlene Piturro regularly writes “Practice Profile.”
Most hospitalist programs start when hospital administrators realize that having physicians dedicated exclusively to inpatient care is a great idea. Administrators then recruit a lead hospitalist—perhaps a stellar performer straight from residency, a community doctor closing his office, or a doctor located through a specialty staffing group.
Colorado Permanente Medical Group (CPMG), backed by a brand as powerful as Starbucks or Nordstrom, did things differently. So imbued with the Permanente culture are its physicians that its hospitalist group arose organically from physicians serving Denver’s Exempla St. Joseph Hospital and Boulder Community Hospital. (See “Kaiser Permanente Culture,” below.)
“Thirty years ago Permanente explored building their own versus finding a cost-effective hospital. They chose us, and their clinic doctors rounded on what grew to 70% of our department of medicine patients,” says Robert Gibbons, MD, St. Joseph’s residency program director. “Then they saw they needed to provide full-time inpatient coverage—the advent of the hospitalist program. Soon many CPMG clinic doctors disappeared, but the quality of medicine remained the same.”
Regional Department Chief Lauren Fraser, MD, oversees the now-mature hospitalist program, which keeps growing in size, complexity, and competence. “We’re always a work in progress, and that’s good,” she says.
According to Joe Heaton, MD, currently a Good Samaritan hospitalist and formerly CPMG regional department chief, CPMG’s primary care departments targeted three areas for better care early in 1995: streamlining patient scheduling, developing a centralized call center, and starting a hospitalist program.
The hospitalist program aimed for cost neutrality by limiting staffing at both hospitals to the same full-time equivalents (FTEs). To avoid forcing physicians into unwelcome assignments, the department offered its 70 internal medicine and 30 family practice doctors four tracks:
- Track A meant full-time hospital work;
- Track B offered a 50-50 hospital-clinic split;
- Track C provided for a 70% clinic, 30% hospital schedule; and
- Track D was full-time clinic work.
The family medicine department opted out of hospital duty, while the internists tracked themselves as follows: eight each for full-time hospital and half-time hospital duty, 34 for 30% hospital time, and 20 for full-time clinic. Fortunately, the tracks chosen matched the hospitals’ needs, and the program was off and running by July 1995.
“At the time, our group’s size created one of the largest hospitalist programs, allowing us to provide 24/7 coverage with at least two physicians on site,” says Dr. Heaton of the launch.
The hospitalist program had immediate measurable impact. Average length of stay dropped by 15%, and Track A and C physicians had similar utilization measures, suggesting that the model of care delivery was the key driver—rather than the amount of time physicians spent in the hospital. Dr. Gibbons was impressed with the hospitalist group’s results, noting that St. Joseph’s average reduced length of stay of 0.7 to one full day was consistent with national benchmarks. Because CPMG sees only Permanente patients, St. Joseph eventually contracted with two other hospitalist groups: the Exempla Faculty Inpatient Team, which covers half of its unassigned patients, and Midtown Inpatient Medicine, private internists who cover the other half of the unassigned patients, co-manage with orthopedic surgeons, and cover for internal medicine groups that no longer make hospital rounds.
CPMG hospitalists also covered Boulder Community Hospital in Denver’s rapidly expanding suburbs until 2005, when CPMG’s contract expired. All six hospitalists moved to nearby Exempla’s new Good Samaritan Hospital, where patient volume grew quickly from 25-30 patients a day to 80; 90% of the patients are Permanente members. Hospitalist staffing jumped to 13 FTEs (19 physicians). “We recruited very aggressively, including lots of locum tenens and moonlighters to cover the booming volume,” explains Brian Thom, MD, assistant regional department chief, Good Samaritan Hospital.
More Measures
In addition to length of stay, CPMG tracks the percentage of patients discharged in less than 24 hours, readmission rates, and disease-specific mortality by provider. All hospitalists get regular reports of department averages and statistical analyses of individual physicians. “This may be controversial, but we must look at outliers to see if [the problem is] case mix, such as many hospice patients, or something else,” says Dr. Heaton.
Striving for high levels of clinical expertise and consistency is a CPMG hallmark. Working for a medical behemoth in the Denver area, CPMG doctors—whether clinic-based or hospitalists—have a huge opportunity to integrate care and to co-manage many conditions with their colleagues. Hospitalists also staff the ICUs. In 2000, William Kinnard, MD, CPMG’s ICU co-director, commented that the group’s use of data-driven protocols allowed hospitalists to practice effectively in ICUs.
As for patient satisfaction, Dr. Heaton admits to “struggling for good measures,” noting that CPMG tackled it head-on in 1999 when Executive Medical Director Jack Cochran, MD, addressed the level of patient tenacity it took to navigate CPMG. Physician career satisfaction was sinking from long chaotic workdays that left both patients and doctors frustrated. By re-engineering scheduling and visit processes, Dr. Cochran made things run more smoothly. Other initiatives included an eight-hour physician-patient interaction course, video vignettes starring CPMG doctors illustrating communication techniques, and formal physician-to-physician coaching. Dr. Fraser still sends new hires to the course, recognizing that good communication satisfies both patients and physicians.
Scheduling: Every Program’s Mt. Everest
Because of the hospitalist program’s size and longevity, physicians have experimented extensively with scheduling. As do many groups, it started with seven 12-hour days on/seven days off blocks, which proved dissatisfying both personally and professionally.
“We experimented with scheduling to find what was sustainable for physicians and provided patient continuity,” says Dr. Fraser. “We’ve found that six eight-hour days in a row of rounding works best.”
Scheduling has evolved to the point that hospitalists provide the following to meet the hospitalist’s, the group’s, and the hospital’s needs: a dedicated triage physician 24/7 to handle calls from all sources of patient flow, two hospitalists on site at all times, eight-hour rounding days, and call physicians who admit and cross-cover after 4 p.m. Average daily census (ADC) is 10-12, plus one or two admissions. While that appears low, if CPMG hospitalists worked 12-hour shifts, their ADC would be 13-16, consistent with national norms.
“Dropping to eight-hour, as opposed to 12-hour, days keeps the job sustainable and helps doctors avoid burnout,” says Dr. Fraser. “However, we work more days per month, an average of 20-22.”
Overall, the scheduling strategy is working. “The majority of physicians who started over a decade ago remain, including many mid-life hospitalists in their 40s and 50s,” she adds. Physicians, rather than administrators, handle scheduling. Dr. Fraser has found that physicians can accept that third triage shift in a month (or an extra night shift when they’re short-handed) when another physician is filling the slots.
Other Features
All CPMG hospitalists can participate in St. Joseph’s residency program as “teaching attendings” for one month. From them, residents learn to co-manage care and participate in interdisciplinary rounds with nurses and social workers. Physicians note that residents make a hospitalist’s life smoother.
“At Good Sam, we do all our own procedures, unlike St. Joe’s, where they have residents. With our patient volumes, there’s little breathing room, especially when we have to cover non-Kaiser patients,” says Dr. Thom. Eventually, residents will rotate through Good Samaritan as well as St. Joseph.
One of the advantages of working in a brand-new hospital like Good Samaritan is establishing systems from scratch. That includes the new hospital’s electronic medical record (EMR), which is integrated with CPMG’s outpatient EMR. “We set up our own systems, complete with order sets and protocols,” explains Dr. Thom. “Considering that 90% of our patients are CPMG members, this gives us a high level of integration, clinically and electronically.”
Challenges Ahead
Despite CPMG’s size and stellar track record, challenges remain. Dr. Fraser identifies them as salaries that rank last within the group, making recruiting difficult; a hard time providing adequate back-up if a physician is unexpectedly absent; adjustments to fluctuations in patient census; time pressures of hospital committee work; and identification of an optimal scheduling model that fosters continuity of care yet provides a sustainable work life.
The group’s size has drawbacks, which Dr. Heaton identifies as the potential for a physician to not feel mission critical or to hide, and that communication and face-to-face meetings get complicated.
“Overall, the program can always use fine tuning, but we love who we work with and have the ultimate respect for our colleagues, which is the true benchmark of the quality of a medical career,” concludes Dr. Fraser. TH
Marlene Piturro regularly writes “Practice Profile.”
A Program in Transition
We work best when we remember who hired us and why. As hospital medicine matures, the goals of those who write the paychecks will continue to shape programs, even when this basic economic truth may be obscured by a program’s fast growth. That is why the 10 hospitalists at Nashua-based Southern New Hampshire Medical Center (SNHMC) work differently than their peers in other systems. They are employed by a unique joint venture of New Hampshire’s two largest multispecialty medical groups: Foundation Medical Partners of Nashua and Lebanon-based Dartmouth-Hitchcock.
Population Growth
The SNHMC hospital medicine group filled a definite need. As Tom Wilhelmson, SNHMC’s CEO and president explains it, Nashua’s population has grown tremendously—25% in the 1980s and an additional 14% in the 1990s—thanks to an influx of young families and industries relocating to business-friendly New Hampshire. During the growth spurt the area needed doctors—particularly primary care physicians. To attract physicians, in 1992 the hospital helped form Foundation Medical Partners (FMP), a large multispecialty group. Based on a private practice model, FMP physicians now cover 22 suburbs in the primary and nine in secondary service areas that serve 225,000 people. SNHMC is FMP’s safety net, negotiating malpractice rates, giving physicians access to capital, and helping with cash flow when a big payer is slow.
The hospital and FMP grew steadily, boosting hospital market share from 40% in the 1980s to 62% today. Michael Marshall, MD, medical director of the 134-physician FMP, saw it thrive.
“We were opening offices farther and farther from the hospital,” he recalls. “In 2002, when doctors’ drive times exceeded 30 minutes, we realized that hospitalists could relieve primary care doctors from hospital work.”
Issues, Options, and Resolutions
SNHMC and FMP considered these options for starting a hospitalist program:
Issue: Starting a hospitalist program from scratch.
Options:
- Hire them as hospital employees;
- Contract with a regional or national hospitalist company;
- Encourage formation of a hospital medicine group;
- Worry about Dartmouth-Hitchcock starting a program; or
- Make hospitalists FMP partners.
Resolution: Hospitalists would be FMP partners; therefore, approach Dartmouth-Hitchcock about a joint venture hospitalist program.
At the time, Dartmouth-Hitchcock, New Hampshire’s only academic medical center and FMP’s chief competition had made significant inroads in Nashua. Dartmouth-Hitchcock embraced the joint venture along with an even split of any necessary subsidies. In 2003 Wilhelmson and Dr. Marshall hired Stewart Fulton, DO, and a second career physician straight from residency, as their hospitalist medical director.
Dr. Fulton was the solo hospitalist and had a goal of assuming hospital duties for 20+ family care physicians in his first year:
Issue: Freeing a large number of primary care physicians from hospital rounds.
Specific problems:
- Dr. Fulton’s pager went off incessantly;
- He was inundated with work;
- He routinely worked 12-hour days and longer; and
- Many FMP physicians still made hospital rounds and covered call to handle patient volume.
Resolution: Hire more hospitalists.
Suneetha Kammila, MD, straight out of residency, became FMP’s second hospitalist. “All was chaos,” recalls Dr. Kammila. “The hospital was very busy; there was no proper system to get the census or see lab work; and we ran from floor to floor. I stayed because Stewart [Fulton] and I worked well together, and I thought we’d eventually succeed.”
Issue: Adding a second hospitalist.
Potential results:
- Hospitalists could see more patients;
- Inadequate systems could not be changed this soon;
- Specialists could be enlisted to deal with the volume of patients.
Resolution: Hire more hospitalists.
Soon after Dr. Kammila’s arrival, FMP added a third hospitalist who didn’t gel. “We increased our patient volume, but the third hire wasn’t a good communicator and didn’t fit. I couldn’t leave the hospital until 8 p.m. most days and I was exhausted,” says Dr. Fulton.
Joohahn John Kim, MD, became the replacement third hospitalist and meshed with Drs. Fulton and Kammila. Soon two additional hospitalists came on board. Eighteen months into the program, there were five hospitalists—a critical mass.
Issue: Growing the hospitalist group to critical mass and beyond.
Results:
- More bodies enabled hospitalists to have defined shifts;
- The laid-back personalities of the hospitalists emerged, and they forged a strong collegiality;
- They covered several more office practices;
- They began to interact more with other hospitalists and less with specialists;
- The groundwork was set for more growth; and
- Growth to 10 hospitalists would enable the seven on/seven off coverage that everyone wanted.
Doubling the number of hospitalists so quickly raised new issues. Divided into two teams of five, each group had little contact with the other team or with their FMP partners. To bridge the divide, shortly after the hospitalist cadre grew to 10, administrators threw an after-hours cocktail party for medical staff to build camaraderie among all FMP physicians.
Issue: Communication and continuity of care were not optimal.
Specific problems:
- The two hospitalist teams didn’t work together;
- Hospitalists and their office-based colleagues didn’t know each other;
- Productivity needed to be discussed; and
- Some long-term patients were unhappy about being treated by hospitalists rather than their primary physicians.
Resolution: More networking events to bring physicians together, along with daily e-mails from hospitalists to primary care physicians.
More contact among physicians revealed other issues. Terry Buchanan, MD, an FMP family practice physician whose three-provider office is several miles from SNHMC, is relieved that hospitalists freed him from hospital work. However, he says, “Not having hospital work gives a better quality of life, but we’ve lost income [from hospitalized patients] that we’re expected to recover with more outpatients.”
Another concern is losing clinical skills associated with acute care. “I don’t feel I’d be as marketable if I wanted a career change,” he adds.
Unique Metrics
No matter what the yardstick, measuring a hospital medicine program’s value is tough, particularly one transitioning to 24/7 coverage. Still, the familiar metrics of reducing average length of stay (ALOS), cutting costs, and quality improvement are not SNHMC’s ultimate gauge. In fact, ALOS has increased, from 4.15 days in 2004 to 4.26 days in 2005. Yet FMP and Dartmouth-Hitchcock gladly continue underwriting the gap between hospitalist compensation and revenues—a gap of about $30,000 per capita annually.
Issue: Customary hospitalist metrics are not the sole drivers at SNHMC.
Specific problems:
- Average length of stay was up;
- Cost cutting was not a predominant metric;
- Volume and productivity were not chief metrics; and
- Joint venture partners continued to subsidize the hospitalist program.
Resolution: The medical groups continue to support the hospitalist program as it adjusts to 24/7, with a commitment to add four more hospitalists.
Downplaying customary metrics doesn’t mean that SNHMC’s hospitalists don’t compare favorably with their peers. They do. On CMS core measures for four congestive heart failure indicators, SNHMC outperforms its state counterparts by 73% versus 65%; on community-acquired pneumonia guidelines by 54%-46%; and on surgical infection prevention by 64%-53%. Only on the six benchmarks for treating myocardial infarction does SNHMC fall short, by 85% to the 89 for other New Hampshire hospitals.
The Growth Conundrum
Moving to 24/7 coverage has challenged SNHMC, as it has other hospitalist programs. Dead time at night, when the ED and hospital floors fall silent, has to be paid for. So do the peaks and valleys of patient load.
Issue: Patient load variability makes hospitalist programs costly.
Specific Problems:
- Admissions and discharges can bunch and create bottlenecks; and
- Hospitalists are too busy at times and not seeing enough patients at other times.
Resolution: For SNHMC, examine possible response to variability, including:
- Hire/redeploy nurses and/or secretaries for discharge paperwork;
- Create a four-hour chest pain unit staffed by physician assistants;
- Re-examine seven on/seven off staffing. Does another model work better?
- Create a convenient care center separate from the ED;
- Hire moonlighters for night shifts;
- Serve more referring physicians to boost productivity; and/or
- Enlist pulmonologists to assist with ED surges.
Having peeked beneath the surface of SNHMC’s hospitalist program’s performance what lies at the heart of its success—or of its failure? By conventional vision, it’s curious; ALOS actually increased, 30+ internists still cover their hospitalized patients, admissions peaks and valleys, and program subsidies for the foreseeable future.
None of that fazes Sue DeSocio, FMP’s president and COO, who laments the dearth of benchmarking tools that accurately reflect the impact of hospitalist programs.
“At the beginning, we were sure we had everything down pat. We’d keep the hospitalists very busy and with a complement of four, we’d break even. Not even close,” she says. But she judges the program a success, as do Dr. Marshall and Wilhelmson, because it addressed FMP’s family practice physicians’ need to focus on their outpatient practices and avoid hospital work.
Patient satisfaction and hospitalist job satisfaction are high and RN turnover is nearly 12% lower than other New Hampshire hospitals. SNHMC avoided a hospitalist turf war with a successful joint venture with its chief competitor, and, perhaps most importantly, incorporated the hospitalists into FMP’s multi-specialty practice rather than taking the easy way out with outside contracting. Or you check with Drs. Fulton and Kammila, who plunged into the chaos of a start-up, worked impossibly long days, and are still there today because they believe in how they’re practicing medicine. TH
Marlene Piturro regularly writes “Practice Profiles” for The Hospitalist.
We work best when we remember who hired us and why. As hospital medicine matures, the goals of those who write the paychecks will continue to shape programs, even when this basic economic truth may be obscured by a program’s fast growth. That is why the 10 hospitalists at Nashua-based Southern New Hampshire Medical Center (SNHMC) work differently than their peers in other systems. They are employed by a unique joint venture of New Hampshire’s two largest multispecialty medical groups: Foundation Medical Partners of Nashua and Lebanon-based Dartmouth-Hitchcock.
Population Growth
The SNHMC hospital medicine group filled a definite need. As Tom Wilhelmson, SNHMC’s CEO and president explains it, Nashua’s population has grown tremendously—25% in the 1980s and an additional 14% in the 1990s—thanks to an influx of young families and industries relocating to business-friendly New Hampshire. During the growth spurt the area needed doctors—particularly primary care physicians. To attract physicians, in 1992 the hospital helped form Foundation Medical Partners (FMP), a large multispecialty group. Based on a private practice model, FMP physicians now cover 22 suburbs in the primary and nine in secondary service areas that serve 225,000 people. SNHMC is FMP’s safety net, negotiating malpractice rates, giving physicians access to capital, and helping with cash flow when a big payer is slow.
The hospital and FMP grew steadily, boosting hospital market share from 40% in the 1980s to 62% today. Michael Marshall, MD, medical director of the 134-physician FMP, saw it thrive.
“We were opening offices farther and farther from the hospital,” he recalls. “In 2002, when doctors’ drive times exceeded 30 minutes, we realized that hospitalists could relieve primary care doctors from hospital work.”
Issues, Options, and Resolutions
SNHMC and FMP considered these options for starting a hospitalist program:
Issue: Starting a hospitalist program from scratch.
Options:
- Hire them as hospital employees;
- Contract with a regional or national hospitalist company;
- Encourage formation of a hospital medicine group;
- Worry about Dartmouth-Hitchcock starting a program; or
- Make hospitalists FMP partners.
Resolution: Hospitalists would be FMP partners; therefore, approach Dartmouth-Hitchcock about a joint venture hospitalist program.
At the time, Dartmouth-Hitchcock, New Hampshire’s only academic medical center and FMP’s chief competition had made significant inroads in Nashua. Dartmouth-Hitchcock embraced the joint venture along with an even split of any necessary subsidies. In 2003 Wilhelmson and Dr. Marshall hired Stewart Fulton, DO, and a second career physician straight from residency, as their hospitalist medical director.
Dr. Fulton was the solo hospitalist and had a goal of assuming hospital duties for 20+ family care physicians in his first year:
Issue: Freeing a large number of primary care physicians from hospital rounds.
Specific problems:
- Dr. Fulton’s pager went off incessantly;
- He was inundated with work;
- He routinely worked 12-hour days and longer; and
- Many FMP physicians still made hospital rounds and covered call to handle patient volume.
Resolution: Hire more hospitalists.
Suneetha Kammila, MD, straight out of residency, became FMP’s second hospitalist. “All was chaos,” recalls Dr. Kammila. “The hospital was very busy; there was no proper system to get the census or see lab work; and we ran from floor to floor. I stayed because Stewart [Fulton] and I worked well together, and I thought we’d eventually succeed.”
Issue: Adding a second hospitalist.
Potential results:
- Hospitalists could see more patients;
- Inadequate systems could not be changed this soon;
- Specialists could be enlisted to deal with the volume of patients.
Resolution: Hire more hospitalists.
Soon after Dr. Kammila’s arrival, FMP added a third hospitalist who didn’t gel. “We increased our patient volume, but the third hire wasn’t a good communicator and didn’t fit. I couldn’t leave the hospital until 8 p.m. most days and I was exhausted,” says Dr. Fulton.
Joohahn John Kim, MD, became the replacement third hospitalist and meshed with Drs. Fulton and Kammila. Soon two additional hospitalists came on board. Eighteen months into the program, there were five hospitalists—a critical mass.
Issue: Growing the hospitalist group to critical mass and beyond.
Results:
- More bodies enabled hospitalists to have defined shifts;
- The laid-back personalities of the hospitalists emerged, and they forged a strong collegiality;
- They covered several more office practices;
- They began to interact more with other hospitalists and less with specialists;
- The groundwork was set for more growth; and
- Growth to 10 hospitalists would enable the seven on/seven off coverage that everyone wanted.
Doubling the number of hospitalists so quickly raised new issues. Divided into two teams of five, each group had little contact with the other team or with their FMP partners. To bridge the divide, shortly after the hospitalist cadre grew to 10, administrators threw an after-hours cocktail party for medical staff to build camaraderie among all FMP physicians.
Issue: Communication and continuity of care were not optimal.
Specific problems:
- The two hospitalist teams didn’t work together;
- Hospitalists and their office-based colleagues didn’t know each other;
- Productivity needed to be discussed; and
- Some long-term patients were unhappy about being treated by hospitalists rather than their primary physicians.
Resolution: More networking events to bring physicians together, along with daily e-mails from hospitalists to primary care physicians.
More contact among physicians revealed other issues. Terry Buchanan, MD, an FMP family practice physician whose three-provider office is several miles from SNHMC, is relieved that hospitalists freed him from hospital work. However, he says, “Not having hospital work gives a better quality of life, but we’ve lost income [from hospitalized patients] that we’re expected to recover with more outpatients.”
Another concern is losing clinical skills associated with acute care. “I don’t feel I’d be as marketable if I wanted a career change,” he adds.
Unique Metrics
No matter what the yardstick, measuring a hospital medicine program’s value is tough, particularly one transitioning to 24/7 coverage. Still, the familiar metrics of reducing average length of stay (ALOS), cutting costs, and quality improvement are not SNHMC’s ultimate gauge. In fact, ALOS has increased, from 4.15 days in 2004 to 4.26 days in 2005. Yet FMP and Dartmouth-Hitchcock gladly continue underwriting the gap between hospitalist compensation and revenues—a gap of about $30,000 per capita annually.
Issue: Customary hospitalist metrics are not the sole drivers at SNHMC.
Specific problems:
- Average length of stay was up;
- Cost cutting was not a predominant metric;
- Volume and productivity were not chief metrics; and
- Joint venture partners continued to subsidize the hospitalist program.
Resolution: The medical groups continue to support the hospitalist program as it adjusts to 24/7, with a commitment to add four more hospitalists.
Downplaying customary metrics doesn’t mean that SNHMC’s hospitalists don’t compare favorably with their peers. They do. On CMS core measures for four congestive heart failure indicators, SNHMC outperforms its state counterparts by 73% versus 65%; on community-acquired pneumonia guidelines by 54%-46%; and on surgical infection prevention by 64%-53%. Only on the six benchmarks for treating myocardial infarction does SNHMC fall short, by 85% to the 89 for other New Hampshire hospitals.
The Growth Conundrum
Moving to 24/7 coverage has challenged SNHMC, as it has other hospitalist programs. Dead time at night, when the ED and hospital floors fall silent, has to be paid for. So do the peaks and valleys of patient load.
Issue: Patient load variability makes hospitalist programs costly.
Specific Problems:
- Admissions and discharges can bunch and create bottlenecks; and
- Hospitalists are too busy at times and not seeing enough patients at other times.
Resolution: For SNHMC, examine possible response to variability, including:
- Hire/redeploy nurses and/or secretaries for discharge paperwork;
- Create a four-hour chest pain unit staffed by physician assistants;
- Re-examine seven on/seven off staffing. Does another model work better?
- Create a convenient care center separate from the ED;
- Hire moonlighters for night shifts;
- Serve more referring physicians to boost productivity; and/or
- Enlist pulmonologists to assist with ED surges.
Having peeked beneath the surface of SNHMC’s hospitalist program’s performance what lies at the heart of its success—or of its failure? By conventional vision, it’s curious; ALOS actually increased, 30+ internists still cover their hospitalized patients, admissions peaks and valleys, and program subsidies for the foreseeable future.
None of that fazes Sue DeSocio, FMP’s president and COO, who laments the dearth of benchmarking tools that accurately reflect the impact of hospitalist programs.
“At the beginning, we were sure we had everything down pat. We’d keep the hospitalists very busy and with a complement of four, we’d break even. Not even close,” she says. But she judges the program a success, as do Dr. Marshall and Wilhelmson, because it addressed FMP’s family practice physicians’ need to focus on their outpatient practices and avoid hospital work.
Patient satisfaction and hospitalist job satisfaction are high and RN turnover is nearly 12% lower than other New Hampshire hospitals. SNHMC avoided a hospitalist turf war with a successful joint venture with its chief competitor, and, perhaps most importantly, incorporated the hospitalists into FMP’s multi-specialty practice rather than taking the easy way out with outside contracting. Or you check with Drs. Fulton and Kammila, who plunged into the chaos of a start-up, worked impossibly long days, and are still there today because they believe in how they’re practicing medicine. TH
Marlene Piturro regularly writes “Practice Profiles” for The Hospitalist.
We work best when we remember who hired us and why. As hospital medicine matures, the goals of those who write the paychecks will continue to shape programs, even when this basic economic truth may be obscured by a program’s fast growth. That is why the 10 hospitalists at Nashua-based Southern New Hampshire Medical Center (SNHMC) work differently than their peers in other systems. They are employed by a unique joint venture of New Hampshire’s two largest multispecialty medical groups: Foundation Medical Partners of Nashua and Lebanon-based Dartmouth-Hitchcock.
Population Growth
The SNHMC hospital medicine group filled a definite need. As Tom Wilhelmson, SNHMC’s CEO and president explains it, Nashua’s population has grown tremendously—25% in the 1980s and an additional 14% in the 1990s—thanks to an influx of young families and industries relocating to business-friendly New Hampshire. During the growth spurt the area needed doctors—particularly primary care physicians. To attract physicians, in 1992 the hospital helped form Foundation Medical Partners (FMP), a large multispecialty group. Based on a private practice model, FMP physicians now cover 22 suburbs in the primary and nine in secondary service areas that serve 225,000 people. SNHMC is FMP’s safety net, negotiating malpractice rates, giving physicians access to capital, and helping with cash flow when a big payer is slow.
The hospital and FMP grew steadily, boosting hospital market share from 40% in the 1980s to 62% today. Michael Marshall, MD, medical director of the 134-physician FMP, saw it thrive.
“We were opening offices farther and farther from the hospital,” he recalls. “In 2002, when doctors’ drive times exceeded 30 minutes, we realized that hospitalists could relieve primary care doctors from hospital work.”
Issues, Options, and Resolutions
SNHMC and FMP considered these options for starting a hospitalist program:
Issue: Starting a hospitalist program from scratch.
Options:
- Hire them as hospital employees;
- Contract with a regional or national hospitalist company;
- Encourage formation of a hospital medicine group;
- Worry about Dartmouth-Hitchcock starting a program; or
- Make hospitalists FMP partners.
Resolution: Hospitalists would be FMP partners; therefore, approach Dartmouth-Hitchcock about a joint venture hospitalist program.
At the time, Dartmouth-Hitchcock, New Hampshire’s only academic medical center and FMP’s chief competition had made significant inroads in Nashua. Dartmouth-Hitchcock embraced the joint venture along with an even split of any necessary subsidies. In 2003 Wilhelmson and Dr. Marshall hired Stewart Fulton, DO, and a second career physician straight from residency, as their hospitalist medical director.
Dr. Fulton was the solo hospitalist and had a goal of assuming hospital duties for 20+ family care physicians in his first year:
Issue: Freeing a large number of primary care physicians from hospital rounds.
Specific problems:
- Dr. Fulton’s pager went off incessantly;
- He was inundated with work;
- He routinely worked 12-hour days and longer; and
- Many FMP physicians still made hospital rounds and covered call to handle patient volume.
Resolution: Hire more hospitalists.
Suneetha Kammila, MD, straight out of residency, became FMP’s second hospitalist. “All was chaos,” recalls Dr. Kammila. “The hospital was very busy; there was no proper system to get the census or see lab work; and we ran from floor to floor. I stayed because Stewart [Fulton] and I worked well together, and I thought we’d eventually succeed.”
Issue: Adding a second hospitalist.
Potential results:
- Hospitalists could see more patients;
- Inadequate systems could not be changed this soon;
- Specialists could be enlisted to deal with the volume of patients.
Resolution: Hire more hospitalists.
Soon after Dr. Kammila’s arrival, FMP added a third hospitalist who didn’t gel. “We increased our patient volume, but the third hire wasn’t a good communicator and didn’t fit. I couldn’t leave the hospital until 8 p.m. most days and I was exhausted,” says Dr. Fulton.
Joohahn John Kim, MD, became the replacement third hospitalist and meshed with Drs. Fulton and Kammila. Soon two additional hospitalists came on board. Eighteen months into the program, there were five hospitalists—a critical mass.
Issue: Growing the hospitalist group to critical mass and beyond.
Results:
- More bodies enabled hospitalists to have defined shifts;
- The laid-back personalities of the hospitalists emerged, and they forged a strong collegiality;
- They covered several more office practices;
- They began to interact more with other hospitalists and less with specialists;
- The groundwork was set for more growth; and
- Growth to 10 hospitalists would enable the seven on/seven off coverage that everyone wanted.
Doubling the number of hospitalists so quickly raised new issues. Divided into two teams of five, each group had little contact with the other team or with their FMP partners. To bridge the divide, shortly after the hospitalist cadre grew to 10, administrators threw an after-hours cocktail party for medical staff to build camaraderie among all FMP physicians.
Issue: Communication and continuity of care were not optimal.
Specific problems:
- The two hospitalist teams didn’t work together;
- Hospitalists and their office-based colleagues didn’t know each other;
- Productivity needed to be discussed; and
- Some long-term patients were unhappy about being treated by hospitalists rather than their primary physicians.
Resolution: More networking events to bring physicians together, along with daily e-mails from hospitalists to primary care physicians.
More contact among physicians revealed other issues. Terry Buchanan, MD, an FMP family practice physician whose three-provider office is several miles from SNHMC, is relieved that hospitalists freed him from hospital work. However, he says, “Not having hospital work gives a better quality of life, but we’ve lost income [from hospitalized patients] that we’re expected to recover with more outpatients.”
Another concern is losing clinical skills associated with acute care. “I don’t feel I’d be as marketable if I wanted a career change,” he adds.
Unique Metrics
No matter what the yardstick, measuring a hospital medicine program’s value is tough, particularly one transitioning to 24/7 coverage. Still, the familiar metrics of reducing average length of stay (ALOS), cutting costs, and quality improvement are not SNHMC’s ultimate gauge. In fact, ALOS has increased, from 4.15 days in 2004 to 4.26 days in 2005. Yet FMP and Dartmouth-Hitchcock gladly continue underwriting the gap between hospitalist compensation and revenues—a gap of about $30,000 per capita annually.
Issue: Customary hospitalist metrics are not the sole drivers at SNHMC.
Specific problems:
- Average length of stay was up;
- Cost cutting was not a predominant metric;
- Volume and productivity were not chief metrics; and
- Joint venture partners continued to subsidize the hospitalist program.
Resolution: The medical groups continue to support the hospitalist program as it adjusts to 24/7, with a commitment to add four more hospitalists.
Downplaying customary metrics doesn’t mean that SNHMC’s hospitalists don’t compare favorably with their peers. They do. On CMS core measures for four congestive heart failure indicators, SNHMC outperforms its state counterparts by 73% versus 65%; on community-acquired pneumonia guidelines by 54%-46%; and on surgical infection prevention by 64%-53%. Only on the six benchmarks for treating myocardial infarction does SNHMC fall short, by 85% to the 89 for other New Hampshire hospitals.
The Growth Conundrum
Moving to 24/7 coverage has challenged SNHMC, as it has other hospitalist programs. Dead time at night, when the ED and hospital floors fall silent, has to be paid for. So do the peaks and valleys of patient load.
Issue: Patient load variability makes hospitalist programs costly.
Specific Problems:
- Admissions and discharges can bunch and create bottlenecks; and
- Hospitalists are too busy at times and not seeing enough patients at other times.
Resolution: For SNHMC, examine possible response to variability, including:
- Hire/redeploy nurses and/or secretaries for discharge paperwork;
- Create a four-hour chest pain unit staffed by physician assistants;
- Re-examine seven on/seven off staffing. Does another model work better?
- Create a convenient care center separate from the ED;
- Hire moonlighters for night shifts;
- Serve more referring physicians to boost productivity; and/or
- Enlist pulmonologists to assist with ED surges.
Having peeked beneath the surface of SNHMC’s hospitalist program’s performance what lies at the heart of its success—or of its failure? By conventional vision, it’s curious; ALOS actually increased, 30+ internists still cover their hospitalized patients, admissions peaks and valleys, and program subsidies for the foreseeable future.
None of that fazes Sue DeSocio, FMP’s president and COO, who laments the dearth of benchmarking tools that accurately reflect the impact of hospitalist programs.
“At the beginning, we were sure we had everything down pat. We’d keep the hospitalists very busy and with a complement of four, we’d break even. Not even close,” she says. But she judges the program a success, as do Dr. Marshall and Wilhelmson, because it addressed FMP’s family practice physicians’ need to focus on their outpatient practices and avoid hospital work.
Patient satisfaction and hospitalist job satisfaction are high and RN turnover is nearly 12% lower than other New Hampshire hospitals. SNHMC avoided a hospitalist turf war with a successful joint venture with its chief competitor, and, perhaps most importantly, incorporated the hospitalists into FMP’s multi-specialty practice rather than taking the easy way out with outside contracting. Or you check with Drs. Fulton and Kammila, who plunged into the chaos of a start-up, worked impossibly long days, and are still there today because they believe in how they’re practicing medicine. TH
Marlene Piturro regularly writes “Practice Profiles” for The Hospitalist.
Hospital Med in the Land of Rocky Top
If a busy doctor is a happy doctor, then the hospitalists in the Methodist Medical Group at Methodist Hospital in Oak Ridge, Tenn., are ecstatic. Chris Frost, MD, the hospital medicine group’s chief hospitalist and medical director, has seen the group’s average daily census climb to 70, then 90, and now 100 patients. Fortunately, the group is growing, too, from nine full-time employees in late October 2005 to 12 before year-end, a projection for 15 by first quarter 2006, and several intensivists to help by March.
The hospital itself has grown as well: It’s in the midst of a $40 million renovation and expansion started in 2004. By August 2006, Methodist Medical will have 230 new private rooms, 12 beds in a new acute care unit, and an emergency department twice the size of its predecessor.

—Chris Frost, MD
How It Started
Methodist Medical Group has been shaped by Oak Ridge’s traditions and demographics. Nestled between the Great Smokey and Cumberland Mountains, Oak Ridge was one of three research and production sites for the Manhattan Project (an effort by the United States, in conjunction with Canada and the United Kingdom to develop nuclear weapons). At its height, Oak Ridge had 75,000 inhabitants. Now its population is 28,000, with a Medicare age group that comprises 42% more of its population than the average Tennessee city. It continues as a magnet for scientists, and its physicians—both office-based and hospitalists—form a close-knit community.
Given its dynamics and demographics, when Oak Ridge’s primary care physicians asked Methodist Hospital in 1993 for help in admitting their patients, the hospital responded affirmatively. Hospital President Jan McNally, BSN, MHA, recalls how things unfolded. “Dr. Richard Dew, a highly respected primary practice physician with a busy office, wanted to change his life. His son had died and he decided to close his office, but he wanted to stay in medicine in Oak Ridge. He agreed to practice inpatient medicine at Methodist,” she explains. “The beauty of it was that he was universally respected. Barriers to the program fell because the admitting doctors and the patients all knew him.”
When Dr. Dew retired in 2002, Anthony Garton, MD, who closed his solo practice to join Dr. Dew as Methodist’s second hospitalist, stayed on. Dr. Garton became a hospitalist because “office procedures just brought me to break even financially. Only the things I did that didn’t have office overhead, such as being medical director at a nursing home and doing physicals for Boeing, made sense financially.” Dr. Garton, who worked with a nephrology group for 13 years, made a smooth transition to a hospitalist career.
From the hospitalist program’s inception, Methodist turned to Team Health, Inc., of Knoxville, an outsourcer of medical personnel, for staffing. Team Health Vice President Kenneth Burns saw a natural fit; his firm already supplied Methodist’s emergency department physicians.
“We understood the problems faced by Methodist’s ED docs,” says Burns. “Patients got stuck there and couldn’t be admitted rapidly to inpatient floors.”
He identified the hospitalist’s necessary skills as an ability to cooperate with community physicians, and an interest in improving processes to boost care quality and decrease costs. Methodist’s hospitalists have been independent contractors since the program’s inception. They receive hourly wages plus incentives based on productivity and metrics negotiated with hospital administrators.
Team Health recently rethought the model as potential recruits balked. In 2006 Methodist’s hospitalists became employees, with health benefits and defined contribution plans. Hospitalist Helen Bidawid, MD, says being employees improves recruiting because many doctors—particularly those just out of residency—find getting loans, buying health insurance, and other business associated with independent contractor status troublesome.
Symbiosis
The relationship of Methodist’s hospitalist program to Oak Ridge’s community physicians has changed over the years. Early on the group hired a hospitalist Dr. Garton describes as “very bright, knew his medicine, and would wow them in academia, but he antagonized the local docs. He left after one year and that was good because our census got low.”
Tact wasn’t that hospitalist’s long suit, and the community doctors who were uncomfortable with him didn’t refer many patients to the hospitalists. With the odd man out, hiring new hospitalists such as Joel Perkerson, MD, put the program back on track.
Dr. Perkerson left an office practice he had been in for 12 years. “I was drowning in paperwork, and it was so frustrating,” he says. “I couldn’t get my homework done or help my son, who was struggling academically.”
Having been both an office- and a hospital-based physician in Oak Ridge, he says it’s too hectic to do both. Being a hospitalist is challenging enough.
“It’s like the movie ‘Field of Dreams.’ Build it, and they will come. Demand keeps growing for our services and we all work a lot of hours,” he says, crediting the increasing load both to Dr. Frost’s leadership, which has made the subspecialists comfortable with the hospitalists’ management of medically complex patients, and to ex-TennCare patients flooding the emergency department. (See “When Politics Collide with Healthcare,” p. 38.)
Under Dr. Frost’s direction (he took over as medical director in 2003 after being recruited as assistant medical director), the hospitalist program has thrived. Dr. Frost has built relationships with Oak Ridge’s subspecialists, particularly pulmonologists, hematologists, oncologists, gastroenterologists, and orthopedists. Typical of Dr. Frost’s leadership is his response to Oak Ridge’s only pulmonary group imploding from six physicians to two. The hospitalists now admit all the group’s patients and Dr. Frost worked with Team Health to recruit intensivists for those very ill patients.
“I’m very pleased with the growth of the hospitalist program,” says Dr. Frost. “We feel empowered that more and more primary care doctors and subspecialists are allowing us to admit and take an active role in managing their patients.”
Tackling one problem that has bedeviled other hospitalist programs, Jan McNally has added a mechanism to ensure cooperation from referring doctors. She expects referring subspecialists to come for consults ASAP when a hospitalist calls.
“We must have that commitment from specialists,” she says. “We have about 15 percent who are laggards, but we will impose disciplinary action if they don’t come when called.”
Dr. Frost favors specialists willing to turn their patients over to the hospitalists in order to improve care quality. He diligently writes care guidelines, focuses on core measures, has deepened discussion of end-of-life care issues, and built such strong esprit de corps that the hospitalists willingly work long and irregular schedules until more physicians arrive. Helen Bidawid, MD, who has been a Methodist hospitalist for about a year, enjoys the hospitalist group, doesn’t mind pitching in to support her colleagues, and says “we function very well together. We watch out for all of our patients, share our responsibilities, and ask each other for help.”
Dr. Bidawid, who was in a non-supportive hospitalist group before her current position, asked herself before she arrived at Methodist: “’Will I be nurtured here or thrown to the wolves?’ Fortunately, I found a very supportive environment.”
With the course set, Dr. Frost still has challenges ahead. There’s growing patient volume, more complex cases to co-manage, carve-outs such as cardiology, neurology, and stroke care, and TennCare disenrollees to contend with.
“Our goal is to add value to Methodist Medical Center,” he says. “As a 24/7 hospitalist program, we help the medical community to be more profitable by enabling them to see more patients in the office and doing more procedures in the hospital. Better communication between physicians, patients, and their families benefits everyone and, we hope, will grow Methodist’s market share.” TH
Marlene Piturro is based in New York.
If a busy doctor is a happy doctor, then the hospitalists in the Methodist Medical Group at Methodist Hospital in Oak Ridge, Tenn., are ecstatic. Chris Frost, MD, the hospital medicine group’s chief hospitalist and medical director, has seen the group’s average daily census climb to 70, then 90, and now 100 patients. Fortunately, the group is growing, too, from nine full-time employees in late October 2005 to 12 before year-end, a projection for 15 by first quarter 2006, and several intensivists to help by March.
The hospital itself has grown as well: It’s in the midst of a $40 million renovation and expansion started in 2004. By August 2006, Methodist Medical will have 230 new private rooms, 12 beds in a new acute care unit, and an emergency department twice the size of its predecessor.

—Chris Frost, MD
How It Started
Methodist Medical Group has been shaped by Oak Ridge’s traditions and demographics. Nestled between the Great Smokey and Cumberland Mountains, Oak Ridge was one of three research and production sites for the Manhattan Project (an effort by the United States, in conjunction with Canada and the United Kingdom to develop nuclear weapons). At its height, Oak Ridge had 75,000 inhabitants. Now its population is 28,000, with a Medicare age group that comprises 42% more of its population than the average Tennessee city. It continues as a magnet for scientists, and its physicians—both office-based and hospitalists—form a close-knit community.
Given its dynamics and demographics, when Oak Ridge’s primary care physicians asked Methodist Hospital in 1993 for help in admitting their patients, the hospital responded affirmatively. Hospital President Jan McNally, BSN, MHA, recalls how things unfolded. “Dr. Richard Dew, a highly respected primary practice physician with a busy office, wanted to change his life. His son had died and he decided to close his office, but he wanted to stay in medicine in Oak Ridge. He agreed to practice inpatient medicine at Methodist,” she explains. “The beauty of it was that he was universally respected. Barriers to the program fell because the admitting doctors and the patients all knew him.”
When Dr. Dew retired in 2002, Anthony Garton, MD, who closed his solo practice to join Dr. Dew as Methodist’s second hospitalist, stayed on. Dr. Garton became a hospitalist because “office procedures just brought me to break even financially. Only the things I did that didn’t have office overhead, such as being medical director at a nursing home and doing physicals for Boeing, made sense financially.” Dr. Garton, who worked with a nephrology group for 13 years, made a smooth transition to a hospitalist career.
From the hospitalist program’s inception, Methodist turned to Team Health, Inc., of Knoxville, an outsourcer of medical personnel, for staffing. Team Health Vice President Kenneth Burns saw a natural fit; his firm already supplied Methodist’s emergency department physicians.
“We understood the problems faced by Methodist’s ED docs,” says Burns. “Patients got stuck there and couldn’t be admitted rapidly to inpatient floors.”
He identified the hospitalist’s necessary skills as an ability to cooperate with community physicians, and an interest in improving processes to boost care quality and decrease costs. Methodist’s hospitalists have been independent contractors since the program’s inception. They receive hourly wages plus incentives based on productivity and metrics negotiated with hospital administrators.
Team Health recently rethought the model as potential recruits balked. In 2006 Methodist’s hospitalists became employees, with health benefits and defined contribution plans. Hospitalist Helen Bidawid, MD, says being employees improves recruiting because many doctors—particularly those just out of residency—find getting loans, buying health insurance, and other business associated with independent contractor status troublesome.
Symbiosis
The relationship of Methodist’s hospitalist program to Oak Ridge’s community physicians has changed over the years. Early on the group hired a hospitalist Dr. Garton describes as “very bright, knew his medicine, and would wow them in academia, but he antagonized the local docs. He left after one year and that was good because our census got low.”
Tact wasn’t that hospitalist’s long suit, and the community doctors who were uncomfortable with him didn’t refer many patients to the hospitalists. With the odd man out, hiring new hospitalists such as Joel Perkerson, MD, put the program back on track.
Dr. Perkerson left an office practice he had been in for 12 years. “I was drowning in paperwork, and it was so frustrating,” he says. “I couldn’t get my homework done or help my son, who was struggling academically.”
Having been both an office- and a hospital-based physician in Oak Ridge, he says it’s too hectic to do both. Being a hospitalist is challenging enough.
“It’s like the movie ‘Field of Dreams.’ Build it, and they will come. Demand keeps growing for our services and we all work a lot of hours,” he says, crediting the increasing load both to Dr. Frost’s leadership, which has made the subspecialists comfortable with the hospitalists’ management of medically complex patients, and to ex-TennCare patients flooding the emergency department. (See “When Politics Collide with Healthcare,” p. 38.)
Under Dr. Frost’s direction (he took over as medical director in 2003 after being recruited as assistant medical director), the hospitalist program has thrived. Dr. Frost has built relationships with Oak Ridge’s subspecialists, particularly pulmonologists, hematologists, oncologists, gastroenterologists, and orthopedists. Typical of Dr. Frost’s leadership is his response to Oak Ridge’s only pulmonary group imploding from six physicians to two. The hospitalists now admit all the group’s patients and Dr. Frost worked with Team Health to recruit intensivists for those very ill patients.
“I’m very pleased with the growth of the hospitalist program,” says Dr. Frost. “We feel empowered that more and more primary care doctors and subspecialists are allowing us to admit and take an active role in managing their patients.”
Tackling one problem that has bedeviled other hospitalist programs, Jan McNally has added a mechanism to ensure cooperation from referring doctors. She expects referring subspecialists to come for consults ASAP when a hospitalist calls.
“We must have that commitment from specialists,” she says. “We have about 15 percent who are laggards, but we will impose disciplinary action if they don’t come when called.”
Dr. Frost favors specialists willing to turn their patients over to the hospitalists in order to improve care quality. He diligently writes care guidelines, focuses on core measures, has deepened discussion of end-of-life care issues, and built such strong esprit de corps that the hospitalists willingly work long and irregular schedules until more physicians arrive. Helen Bidawid, MD, who has been a Methodist hospitalist for about a year, enjoys the hospitalist group, doesn’t mind pitching in to support her colleagues, and says “we function very well together. We watch out for all of our patients, share our responsibilities, and ask each other for help.”
Dr. Bidawid, who was in a non-supportive hospitalist group before her current position, asked herself before she arrived at Methodist: “’Will I be nurtured here or thrown to the wolves?’ Fortunately, I found a very supportive environment.”
With the course set, Dr. Frost still has challenges ahead. There’s growing patient volume, more complex cases to co-manage, carve-outs such as cardiology, neurology, and stroke care, and TennCare disenrollees to contend with.
“Our goal is to add value to Methodist Medical Center,” he says. “As a 24/7 hospitalist program, we help the medical community to be more profitable by enabling them to see more patients in the office and doing more procedures in the hospital. Better communication between physicians, patients, and their families benefits everyone and, we hope, will grow Methodist’s market share.” TH
Marlene Piturro is based in New York.
If a busy doctor is a happy doctor, then the hospitalists in the Methodist Medical Group at Methodist Hospital in Oak Ridge, Tenn., are ecstatic. Chris Frost, MD, the hospital medicine group’s chief hospitalist and medical director, has seen the group’s average daily census climb to 70, then 90, and now 100 patients. Fortunately, the group is growing, too, from nine full-time employees in late October 2005 to 12 before year-end, a projection for 15 by first quarter 2006, and several intensivists to help by March.
The hospital itself has grown as well: It’s in the midst of a $40 million renovation and expansion started in 2004. By August 2006, Methodist Medical will have 230 new private rooms, 12 beds in a new acute care unit, and an emergency department twice the size of its predecessor.

—Chris Frost, MD
How It Started
Methodist Medical Group has been shaped by Oak Ridge’s traditions and demographics. Nestled between the Great Smokey and Cumberland Mountains, Oak Ridge was one of three research and production sites for the Manhattan Project (an effort by the United States, in conjunction with Canada and the United Kingdom to develop nuclear weapons). At its height, Oak Ridge had 75,000 inhabitants. Now its population is 28,000, with a Medicare age group that comprises 42% more of its population than the average Tennessee city. It continues as a magnet for scientists, and its physicians—both office-based and hospitalists—form a close-knit community.
Given its dynamics and demographics, when Oak Ridge’s primary care physicians asked Methodist Hospital in 1993 for help in admitting their patients, the hospital responded affirmatively. Hospital President Jan McNally, BSN, MHA, recalls how things unfolded. “Dr. Richard Dew, a highly respected primary practice physician with a busy office, wanted to change his life. His son had died and he decided to close his office, but he wanted to stay in medicine in Oak Ridge. He agreed to practice inpatient medicine at Methodist,” she explains. “The beauty of it was that he was universally respected. Barriers to the program fell because the admitting doctors and the patients all knew him.”
When Dr. Dew retired in 2002, Anthony Garton, MD, who closed his solo practice to join Dr. Dew as Methodist’s second hospitalist, stayed on. Dr. Garton became a hospitalist because “office procedures just brought me to break even financially. Only the things I did that didn’t have office overhead, such as being medical director at a nursing home and doing physicals for Boeing, made sense financially.” Dr. Garton, who worked with a nephrology group for 13 years, made a smooth transition to a hospitalist career.
From the hospitalist program’s inception, Methodist turned to Team Health, Inc., of Knoxville, an outsourcer of medical personnel, for staffing. Team Health Vice President Kenneth Burns saw a natural fit; his firm already supplied Methodist’s emergency department physicians.
“We understood the problems faced by Methodist’s ED docs,” says Burns. “Patients got stuck there and couldn’t be admitted rapidly to inpatient floors.”
He identified the hospitalist’s necessary skills as an ability to cooperate with community physicians, and an interest in improving processes to boost care quality and decrease costs. Methodist’s hospitalists have been independent contractors since the program’s inception. They receive hourly wages plus incentives based on productivity and metrics negotiated with hospital administrators.
Team Health recently rethought the model as potential recruits balked. In 2006 Methodist’s hospitalists became employees, with health benefits and defined contribution plans. Hospitalist Helen Bidawid, MD, says being employees improves recruiting because many doctors—particularly those just out of residency—find getting loans, buying health insurance, and other business associated with independent contractor status troublesome.
Symbiosis
The relationship of Methodist’s hospitalist program to Oak Ridge’s community physicians has changed over the years. Early on the group hired a hospitalist Dr. Garton describes as “very bright, knew his medicine, and would wow them in academia, but he antagonized the local docs. He left after one year and that was good because our census got low.”
Tact wasn’t that hospitalist’s long suit, and the community doctors who were uncomfortable with him didn’t refer many patients to the hospitalists. With the odd man out, hiring new hospitalists such as Joel Perkerson, MD, put the program back on track.
Dr. Perkerson left an office practice he had been in for 12 years. “I was drowning in paperwork, and it was so frustrating,” he says. “I couldn’t get my homework done or help my son, who was struggling academically.”
Having been both an office- and a hospital-based physician in Oak Ridge, he says it’s too hectic to do both. Being a hospitalist is challenging enough.
“It’s like the movie ‘Field of Dreams.’ Build it, and they will come. Demand keeps growing for our services and we all work a lot of hours,” he says, crediting the increasing load both to Dr. Frost’s leadership, which has made the subspecialists comfortable with the hospitalists’ management of medically complex patients, and to ex-TennCare patients flooding the emergency department. (See “When Politics Collide with Healthcare,” p. 38.)
Under Dr. Frost’s direction (he took over as medical director in 2003 after being recruited as assistant medical director), the hospitalist program has thrived. Dr. Frost has built relationships with Oak Ridge’s subspecialists, particularly pulmonologists, hematologists, oncologists, gastroenterologists, and orthopedists. Typical of Dr. Frost’s leadership is his response to Oak Ridge’s only pulmonary group imploding from six physicians to two. The hospitalists now admit all the group’s patients and Dr. Frost worked with Team Health to recruit intensivists for those very ill patients.
“I’m very pleased with the growth of the hospitalist program,” says Dr. Frost. “We feel empowered that more and more primary care doctors and subspecialists are allowing us to admit and take an active role in managing their patients.”
Tackling one problem that has bedeviled other hospitalist programs, Jan McNally has added a mechanism to ensure cooperation from referring doctors. She expects referring subspecialists to come for consults ASAP when a hospitalist calls.
“We must have that commitment from specialists,” she says. “We have about 15 percent who are laggards, but we will impose disciplinary action if they don’t come when called.”
Dr. Frost favors specialists willing to turn their patients over to the hospitalists in order to improve care quality. He diligently writes care guidelines, focuses on core measures, has deepened discussion of end-of-life care issues, and built such strong esprit de corps that the hospitalists willingly work long and irregular schedules until more physicians arrive. Helen Bidawid, MD, who has been a Methodist hospitalist for about a year, enjoys the hospitalist group, doesn’t mind pitching in to support her colleagues, and says “we function very well together. We watch out for all of our patients, share our responsibilities, and ask each other for help.”
Dr. Bidawid, who was in a non-supportive hospitalist group before her current position, asked herself before she arrived at Methodist: “’Will I be nurtured here or thrown to the wolves?’ Fortunately, I found a very supportive environment.”
With the course set, Dr. Frost still has challenges ahead. There’s growing patient volume, more complex cases to co-manage, carve-outs such as cardiology, neurology, and stroke care, and TennCare disenrollees to contend with.
“Our goal is to add value to Methodist Medical Center,” he says. “As a 24/7 hospitalist program, we help the medical community to be more profitable by enabling them to see more patients in the office and doing more procedures in the hospital. Better communication between physicians, patients, and their families benefits everyone and, we hope, will grow Methodist’s market share.” TH
Marlene Piturro is based in New York.