User login
Visual impairment more common in minority youth
Race, ethnicity, and socioeconomic status are closely associated with visual impairment in adolescents in the United States, researchers have found.
The study showed that adolescents who identified as Black, Mexican-American, of low income, or as non–U.S. citizens were two to three times more likely than White adolescents to report vision problems and to perform worse on objective tests of visual acuity.
Although disparities in visual impairment with respect to ethnic, racial, and socioeconomic status have been described among adults, little research has explored the adolescent population, according to the researchers, whose findings appear in JAMA Ophthalmology.
“The primary motivation behind trying to figure out exactly when these disparities emerge is that it gives us an opportunity to come up with ideas for interventions that can potentially address them before they manifest in a way that they are no longer treatable,” said Isdin Oke, MD, an instructor in ophthalmology at Harvard Medical School, Boston, who led the latest study.
Dr. Oke and his colleagues analyzed the records of 2,833 children and adolescents aged 12 through 18 years (mean, 15.5 years; 49% female) in the National Health and Nutrition Examination Survey. All the participants had completed a visual function questionnaire and had undergone an eye examination. The primary outcomes of the study were subjective (self-reported) poor vision and objective measures of visual function (visual acuity worse than 20/40 in the better-seeing eye).
Of the study participants, 14% were non-Hispanic Black, 11% were Mexican-American, 63% were non-Hispanic White, and 11% were of other race and ethnicity. Five percent of participants were not U.S. citizens, and 19% had a family income below the poverty threshold.
After accounting for potential confounders, self-reported poor vision was more common among Black (odds ratio, 2.85; 95% CI, 2.00-4.05; P < .001), Mexican-American (OR, 2.83; 95% CI, 1.70-4.73; P < .001), and low-income youth (OR, 2.44; 95% CI, 1.63-3.65; P < .001), the researchers report.
The study also found increased odds of visual acuity below 20/40 in the better-seeing eye among Black (OR, 2.13; 95% CI, 1.41-3.24; P = .001) and Mexican-American adolescents (OR, 2.13; 95% CI, 1.39-3.26; P = .001) and non–U.S. citizens (OR, 1.96; 95% CI, 1.10-3.49; P = .02).
Black and Mexican-American adolescents were almost three times more likely to suffer poor subjective visual function and twice as likely to have low objective visual acuity than non-Hispanic White youth, according to the researchers.
“I think it’s something that health care providers, and even the population as a whole, should be more aware of,” Dr. Oke said.
Opportunities for intervention
Dr. Oke said the findings likely reflect the underlying inequities in access to vision care experienced by these persons.
“There are a lot of opportunities for early intervention, whether it’s through vision screening or improving access to vision services for children and adolescents that can really make a big difference over the long term,” he told this news organization.
Michael F. Chiang, MD, director of the National Eye Institute at the National Institutes of Health, Bethesda, Md., agreed that more steps need to be taken to improve access to vision care for all Americans.
“There are good data showing that we don’t have a sufficient number of eye care providers and health-services clinical researchers who come from backgrounds that are currently underrepresented in medicine and science,” Dr. Chiang said. “Therefore, we need to find ways to inspire, recruit, and train a larger number of people to strengthen our vision workforce.”
Other ways to address these gaps in care, he added, include improving understanding of the social determinants of vision health as well as developing ways to improve access to eye care.
“That may include new models of eye care, like telehealth to improve outreach, and will likely need to include what we call implementation science, so clinicians can better adopt these measures,” he said.
Dr. Oke and Dr. Chiang reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Race, ethnicity, and socioeconomic status are closely associated with visual impairment in adolescents in the United States, researchers have found.
The study showed that adolescents who identified as Black, Mexican-American, of low income, or as non–U.S. citizens were two to three times more likely than White adolescents to report vision problems and to perform worse on objective tests of visual acuity.
Although disparities in visual impairment with respect to ethnic, racial, and socioeconomic status have been described among adults, little research has explored the adolescent population, according to the researchers, whose findings appear in JAMA Ophthalmology.
“The primary motivation behind trying to figure out exactly when these disparities emerge is that it gives us an opportunity to come up with ideas for interventions that can potentially address them before they manifest in a way that they are no longer treatable,” said Isdin Oke, MD, an instructor in ophthalmology at Harvard Medical School, Boston, who led the latest study.
Dr. Oke and his colleagues analyzed the records of 2,833 children and adolescents aged 12 through 18 years (mean, 15.5 years; 49% female) in the National Health and Nutrition Examination Survey. All the participants had completed a visual function questionnaire and had undergone an eye examination. The primary outcomes of the study were subjective (self-reported) poor vision and objective measures of visual function (visual acuity worse than 20/40 in the better-seeing eye).
Of the study participants, 14% were non-Hispanic Black, 11% were Mexican-American, 63% were non-Hispanic White, and 11% were of other race and ethnicity. Five percent of participants were not U.S. citizens, and 19% had a family income below the poverty threshold.
After accounting for potential confounders, self-reported poor vision was more common among Black (odds ratio, 2.85; 95% CI, 2.00-4.05; P < .001), Mexican-American (OR, 2.83; 95% CI, 1.70-4.73; P < .001), and low-income youth (OR, 2.44; 95% CI, 1.63-3.65; P < .001), the researchers report.
The study also found increased odds of visual acuity below 20/40 in the better-seeing eye among Black (OR, 2.13; 95% CI, 1.41-3.24; P = .001) and Mexican-American adolescents (OR, 2.13; 95% CI, 1.39-3.26; P = .001) and non–U.S. citizens (OR, 1.96; 95% CI, 1.10-3.49; P = .02).
Black and Mexican-American adolescents were almost three times more likely to suffer poor subjective visual function and twice as likely to have low objective visual acuity than non-Hispanic White youth, according to the researchers.
“I think it’s something that health care providers, and even the population as a whole, should be more aware of,” Dr. Oke said.
Opportunities for intervention
Dr. Oke said the findings likely reflect the underlying inequities in access to vision care experienced by these persons.
“There are a lot of opportunities for early intervention, whether it’s through vision screening or improving access to vision services for children and adolescents that can really make a big difference over the long term,” he told this news organization.
Michael F. Chiang, MD, director of the National Eye Institute at the National Institutes of Health, Bethesda, Md., agreed that more steps need to be taken to improve access to vision care for all Americans.
“There are good data showing that we don’t have a sufficient number of eye care providers and health-services clinical researchers who come from backgrounds that are currently underrepresented in medicine and science,” Dr. Chiang said. “Therefore, we need to find ways to inspire, recruit, and train a larger number of people to strengthen our vision workforce.”
Other ways to address these gaps in care, he added, include improving understanding of the social determinants of vision health as well as developing ways to improve access to eye care.
“That may include new models of eye care, like telehealth to improve outreach, and will likely need to include what we call implementation science, so clinicians can better adopt these measures,” he said.
Dr. Oke and Dr. Chiang reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Race, ethnicity, and socioeconomic status are closely associated with visual impairment in adolescents in the United States, researchers have found.
The study showed that adolescents who identified as Black, Mexican-American, of low income, or as non–U.S. citizens were two to three times more likely than White adolescents to report vision problems and to perform worse on objective tests of visual acuity.
Although disparities in visual impairment with respect to ethnic, racial, and socioeconomic status have been described among adults, little research has explored the adolescent population, according to the researchers, whose findings appear in JAMA Ophthalmology.
“The primary motivation behind trying to figure out exactly when these disparities emerge is that it gives us an opportunity to come up with ideas for interventions that can potentially address them before they manifest in a way that they are no longer treatable,” said Isdin Oke, MD, an instructor in ophthalmology at Harvard Medical School, Boston, who led the latest study.
Dr. Oke and his colleagues analyzed the records of 2,833 children and adolescents aged 12 through 18 years (mean, 15.5 years; 49% female) in the National Health and Nutrition Examination Survey. All the participants had completed a visual function questionnaire and had undergone an eye examination. The primary outcomes of the study were subjective (self-reported) poor vision and objective measures of visual function (visual acuity worse than 20/40 in the better-seeing eye).
Of the study participants, 14% were non-Hispanic Black, 11% were Mexican-American, 63% were non-Hispanic White, and 11% were of other race and ethnicity. Five percent of participants were not U.S. citizens, and 19% had a family income below the poverty threshold.
After accounting for potential confounders, self-reported poor vision was more common among Black (odds ratio, 2.85; 95% CI, 2.00-4.05; P < .001), Mexican-American (OR, 2.83; 95% CI, 1.70-4.73; P < .001), and low-income youth (OR, 2.44; 95% CI, 1.63-3.65; P < .001), the researchers report.
The study also found increased odds of visual acuity below 20/40 in the better-seeing eye among Black (OR, 2.13; 95% CI, 1.41-3.24; P = .001) and Mexican-American adolescents (OR, 2.13; 95% CI, 1.39-3.26; P = .001) and non–U.S. citizens (OR, 1.96; 95% CI, 1.10-3.49; P = .02).
Black and Mexican-American adolescents were almost three times more likely to suffer poor subjective visual function and twice as likely to have low objective visual acuity than non-Hispanic White youth, according to the researchers.
“I think it’s something that health care providers, and even the population as a whole, should be more aware of,” Dr. Oke said.
Opportunities for intervention
Dr. Oke said the findings likely reflect the underlying inequities in access to vision care experienced by these persons.
“There are a lot of opportunities for early intervention, whether it’s through vision screening or improving access to vision services for children and adolescents that can really make a big difference over the long term,” he told this news organization.
Michael F. Chiang, MD, director of the National Eye Institute at the National Institutes of Health, Bethesda, Md., agreed that more steps need to be taken to improve access to vision care for all Americans.
“There are good data showing that we don’t have a sufficient number of eye care providers and health-services clinical researchers who come from backgrounds that are currently underrepresented in medicine and science,” Dr. Chiang said. “Therefore, we need to find ways to inspire, recruit, and train a larger number of people to strengthen our vision workforce.”
Other ways to address these gaps in care, he added, include improving understanding of the social determinants of vision health as well as developing ways to improve access to eye care.
“That may include new models of eye care, like telehealth to improve outreach, and will likely need to include what we call implementation science, so clinicians can better adopt these measures,” he said.
Dr. Oke and Dr. Chiang reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Trauma rates with operative vaginal delivery unexpectedly high, study finds
A new investigation has found that rates of physical trauma following operative vaginal delivery (OVD) in Canada are higher than previously reported.
The cohort study of more than 1.3 million deliveries in the country found trauma rates were highest with forceps delivery, with more than 1 in 4 pregnancies resulting in maternal trauma and 1 in 105 infants experiencing neonatal trauma. Maternal and neonatal trauma following vacuum deliveries was less common, occurring in 1 in 8 pregnancies and 1 in 104 infants, according to the researchers, who reported their findings in the Canadian Medical Association Journal .
“The rates of trauma following OVD in Canada are higher than previously reported, irrespective of region, level of obstetric care, and volume of instrument use among hospitals,” lead author Giulia Muraca, PhD, MPH, assistant professor of obstetrics and gynecology at McMaster University, Hamilton, Ont., said in an interview. “While OVDs may be associated with low rates of morbidity in carefully selected circumstances, the uniformly high rates of trauma among forceps and vacuum deliveries documented across regions, levels of obstetric care, and hospitals show that such conditions do not apply to routine obstetric practice in Canada.”
The American College of Obstetricians and Gynecologists considers OVD a way to reduce the rate of cesarean deliveries. However, the group has also pointed to a decline in familiarity with the procedures among clinicians new to the field.
Current reports also show that while OVD accounts for up to 15% of deliveries in Canada, Australia, and the United Kingdom, the risks associated with the approach are heavily dependent on the expertise of the provider. Declining use of OVD in favor of cesarean delivery has reduced opportunities for clinicians to acquire proficiency in performing these deliveries, according to the researchers.
Given these various factors, the investigators said the consensus on the safety of OVD is under scrutiny.
“An examination of maternal and neonatal trauma among OVD in contemporary practice is necessary to ensure that health care providers, policy makers, and pregnant individuals are informed regarding the risks of OVD typically experienced in routine obstetric practice, rather than those encountered under ideal conditions,” Dr. Muraca said.
Over 1 million deliveries studied
Dr. Muraca and colleagues looked at 1,326,191 deliveries occurring across Canada (except Quebec) between April 2013 and March 2019. The researchers included all singleton, term (≥37 weeks), in-hospital deliveries to women who had not undergone a previous cesarean delivery.
The study’s primary outcome measures were composite maternal trauma and composite neonatal trauma. Maternal trauma included obstetric anal sphincter injury (OASI); cervical or high vaginal laceration; pelvic hematoma; obstetric injury to the pelvic organs, pelvic joints, or ligaments; injury to the bladder or urethra; and other pelvic trauma. Neonatal trauma comprised intracranial hemorrhage and laceration, skull fracture, severe injury to the central or peripheral nervous system, fracture of the long bones, injury to the liver or spleen, seizures, and neonatal death.
The analysis found that 38,500 (2.9%) of the cases involved attempted forceps deliveries while 110,987 (8.4%) were attempted vacuum deliveries. Of the attempted forceps deliveries, 1,606 (4.2%) failed, while 8,791 (7.9%) of attempted vacuum deliveries failed.
Maternal trauma was observed in 25.3% of all forceps deliveries (n = 9,728) and 13.2% of all vacuum deliveries (n = 14,614), the researchers reported. The most common form of maternal trauma was OASI, which was observed in 21.52% of women undergoing forceps delivery and 11.67% of those undergoing vacuum delivery. The rates of all other forms of maternal trauma were higher among patients undergoing attempted forceps delivery than among their counterparts undergoing attempted vacuum delivery.
After adjusting for possible confounders, rates of maternal trauma remained higher with forceps than with vacuum deliveries (adjusted rate ratio, 1.70).
The rate of neonatal trauma was comparable for forceps (9.56/1,000 live births) and vacuum deliveries (9.58/1,000 live births). In these cases, damage to the peripheral nervous system was the most common form of neonatal trauma, occurring in 4.85/1,000 live births with forceps delivery and 3.41/1,000 live births for vacuum delivery, the researchers found.
Consider morbidity following OVD against potential alternatives, authors say
According to Dr. Muraca, the rates of maternal trauma in her study – along with accumulating evidence of the severe long-term consequences of these injuries – demonstrates the importance of reporting timely, empirically derived risk measures that accurately reflect those that pregnant individuals may encounter in typical obstetric practice.
“Although there is merit in understanding the estimates of risk that can be achieved when conditions are optimal, the interpretation of these estimates can be misleading, especially given secular shifts in patterns of practice,” she said. “The failure to do so compromises women’s autonomy in making evidence-informed decisions regarding childbirth interventions, such as evaluating the short- and long-term risks of OVD and cesarean delivery.
Her group recommended that morbidity following OVD be weighed against potential alternatives to such procedures, which carry their own risks. “This includes an extended second stage of labor and a spontaneous vaginal delivery, or a second-stage cesarean delivery, both of which are associated with significant morbidity,” Dr. Muraca said. “However, a comprehensive consideration of high population rates of OVD morbidity also prompts questions about choice of instrument, obstetrician training in OVD use, and for recognizing cases that would benefit from a cesarean delivery earlier in labor.”
Alan Peaceman, MD, professor of obstetrics and gynecology at Northwestern University, Chicago, said he was not surprised by the rates of sphincter injury, but that the rate of severe neonatal injury rate was higher than he expected. However, he added, “I don’t think clinicians should change their approach based on a single study. They should continue with the approach that they are most skilled at and is appropriate for the clinical circumstances.”
The study was funded by a grant from the Canadian Institutes of Health Research. Dr. Muraca and Dr. Peaceman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new investigation has found that rates of physical trauma following operative vaginal delivery (OVD) in Canada are higher than previously reported.
The cohort study of more than 1.3 million deliveries in the country found trauma rates were highest with forceps delivery, with more than 1 in 4 pregnancies resulting in maternal trauma and 1 in 105 infants experiencing neonatal trauma. Maternal and neonatal trauma following vacuum deliveries was less common, occurring in 1 in 8 pregnancies and 1 in 104 infants, according to the researchers, who reported their findings in the Canadian Medical Association Journal .
“The rates of trauma following OVD in Canada are higher than previously reported, irrespective of region, level of obstetric care, and volume of instrument use among hospitals,” lead author Giulia Muraca, PhD, MPH, assistant professor of obstetrics and gynecology at McMaster University, Hamilton, Ont., said in an interview. “While OVDs may be associated with low rates of morbidity in carefully selected circumstances, the uniformly high rates of trauma among forceps and vacuum deliveries documented across regions, levels of obstetric care, and hospitals show that such conditions do not apply to routine obstetric practice in Canada.”
The American College of Obstetricians and Gynecologists considers OVD a way to reduce the rate of cesarean deliveries. However, the group has also pointed to a decline in familiarity with the procedures among clinicians new to the field.
Current reports also show that while OVD accounts for up to 15% of deliveries in Canada, Australia, and the United Kingdom, the risks associated with the approach are heavily dependent on the expertise of the provider. Declining use of OVD in favor of cesarean delivery has reduced opportunities for clinicians to acquire proficiency in performing these deliveries, according to the researchers.
Given these various factors, the investigators said the consensus on the safety of OVD is under scrutiny.
“An examination of maternal and neonatal trauma among OVD in contemporary practice is necessary to ensure that health care providers, policy makers, and pregnant individuals are informed regarding the risks of OVD typically experienced in routine obstetric practice, rather than those encountered under ideal conditions,” Dr. Muraca said.
Over 1 million deliveries studied
Dr. Muraca and colleagues looked at 1,326,191 deliveries occurring across Canada (except Quebec) between April 2013 and March 2019. The researchers included all singleton, term (≥37 weeks), in-hospital deliveries to women who had not undergone a previous cesarean delivery.
The study’s primary outcome measures were composite maternal trauma and composite neonatal trauma. Maternal trauma included obstetric anal sphincter injury (OASI); cervical or high vaginal laceration; pelvic hematoma; obstetric injury to the pelvic organs, pelvic joints, or ligaments; injury to the bladder or urethra; and other pelvic trauma. Neonatal trauma comprised intracranial hemorrhage and laceration, skull fracture, severe injury to the central or peripheral nervous system, fracture of the long bones, injury to the liver or spleen, seizures, and neonatal death.
The analysis found that 38,500 (2.9%) of the cases involved attempted forceps deliveries while 110,987 (8.4%) were attempted vacuum deliveries. Of the attempted forceps deliveries, 1,606 (4.2%) failed, while 8,791 (7.9%) of attempted vacuum deliveries failed.
Maternal trauma was observed in 25.3% of all forceps deliveries (n = 9,728) and 13.2% of all vacuum deliveries (n = 14,614), the researchers reported. The most common form of maternal trauma was OASI, which was observed in 21.52% of women undergoing forceps delivery and 11.67% of those undergoing vacuum delivery. The rates of all other forms of maternal trauma were higher among patients undergoing attempted forceps delivery than among their counterparts undergoing attempted vacuum delivery.
After adjusting for possible confounders, rates of maternal trauma remained higher with forceps than with vacuum deliveries (adjusted rate ratio, 1.70).
The rate of neonatal trauma was comparable for forceps (9.56/1,000 live births) and vacuum deliveries (9.58/1,000 live births). In these cases, damage to the peripheral nervous system was the most common form of neonatal trauma, occurring in 4.85/1,000 live births with forceps delivery and 3.41/1,000 live births for vacuum delivery, the researchers found.
Consider morbidity following OVD against potential alternatives, authors say
According to Dr. Muraca, the rates of maternal trauma in her study – along with accumulating evidence of the severe long-term consequences of these injuries – demonstrates the importance of reporting timely, empirically derived risk measures that accurately reflect those that pregnant individuals may encounter in typical obstetric practice.
“Although there is merit in understanding the estimates of risk that can be achieved when conditions are optimal, the interpretation of these estimates can be misleading, especially given secular shifts in patterns of practice,” she said. “The failure to do so compromises women’s autonomy in making evidence-informed decisions regarding childbirth interventions, such as evaluating the short- and long-term risks of OVD and cesarean delivery.
Her group recommended that morbidity following OVD be weighed against potential alternatives to such procedures, which carry their own risks. “This includes an extended second stage of labor and a spontaneous vaginal delivery, or a second-stage cesarean delivery, both of which are associated with significant morbidity,” Dr. Muraca said. “However, a comprehensive consideration of high population rates of OVD morbidity also prompts questions about choice of instrument, obstetrician training in OVD use, and for recognizing cases that would benefit from a cesarean delivery earlier in labor.”
Alan Peaceman, MD, professor of obstetrics and gynecology at Northwestern University, Chicago, said he was not surprised by the rates of sphincter injury, but that the rate of severe neonatal injury rate was higher than he expected. However, he added, “I don’t think clinicians should change their approach based on a single study. They should continue with the approach that they are most skilled at and is appropriate for the clinical circumstances.”
The study was funded by a grant from the Canadian Institutes of Health Research. Dr. Muraca and Dr. Peaceman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new investigation has found that rates of physical trauma following operative vaginal delivery (OVD) in Canada are higher than previously reported.
The cohort study of more than 1.3 million deliveries in the country found trauma rates were highest with forceps delivery, with more than 1 in 4 pregnancies resulting in maternal trauma and 1 in 105 infants experiencing neonatal trauma. Maternal and neonatal trauma following vacuum deliveries was less common, occurring in 1 in 8 pregnancies and 1 in 104 infants, according to the researchers, who reported their findings in the Canadian Medical Association Journal .
“The rates of trauma following OVD in Canada are higher than previously reported, irrespective of region, level of obstetric care, and volume of instrument use among hospitals,” lead author Giulia Muraca, PhD, MPH, assistant professor of obstetrics and gynecology at McMaster University, Hamilton, Ont., said in an interview. “While OVDs may be associated with low rates of morbidity in carefully selected circumstances, the uniformly high rates of trauma among forceps and vacuum deliveries documented across regions, levels of obstetric care, and hospitals show that such conditions do not apply to routine obstetric practice in Canada.”
The American College of Obstetricians and Gynecologists considers OVD a way to reduce the rate of cesarean deliveries. However, the group has also pointed to a decline in familiarity with the procedures among clinicians new to the field.
Current reports also show that while OVD accounts for up to 15% of deliveries in Canada, Australia, and the United Kingdom, the risks associated with the approach are heavily dependent on the expertise of the provider. Declining use of OVD in favor of cesarean delivery has reduced opportunities for clinicians to acquire proficiency in performing these deliveries, according to the researchers.
Given these various factors, the investigators said the consensus on the safety of OVD is under scrutiny.
“An examination of maternal and neonatal trauma among OVD in contemporary practice is necessary to ensure that health care providers, policy makers, and pregnant individuals are informed regarding the risks of OVD typically experienced in routine obstetric practice, rather than those encountered under ideal conditions,” Dr. Muraca said.
Over 1 million deliveries studied
Dr. Muraca and colleagues looked at 1,326,191 deliveries occurring across Canada (except Quebec) between April 2013 and March 2019. The researchers included all singleton, term (≥37 weeks), in-hospital deliveries to women who had not undergone a previous cesarean delivery.
The study’s primary outcome measures were composite maternal trauma and composite neonatal trauma. Maternal trauma included obstetric anal sphincter injury (OASI); cervical or high vaginal laceration; pelvic hematoma; obstetric injury to the pelvic organs, pelvic joints, or ligaments; injury to the bladder or urethra; and other pelvic trauma. Neonatal trauma comprised intracranial hemorrhage and laceration, skull fracture, severe injury to the central or peripheral nervous system, fracture of the long bones, injury to the liver or spleen, seizures, and neonatal death.
The analysis found that 38,500 (2.9%) of the cases involved attempted forceps deliveries while 110,987 (8.4%) were attempted vacuum deliveries. Of the attempted forceps deliveries, 1,606 (4.2%) failed, while 8,791 (7.9%) of attempted vacuum deliveries failed.
Maternal trauma was observed in 25.3% of all forceps deliveries (n = 9,728) and 13.2% of all vacuum deliveries (n = 14,614), the researchers reported. The most common form of maternal trauma was OASI, which was observed in 21.52% of women undergoing forceps delivery and 11.67% of those undergoing vacuum delivery. The rates of all other forms of maternal trauma were higher among patients undergoing attempted forceps delivery than among their counterparts undergoing attempted vacuum delivery.
After adjusting for possible confounders, rates of maternal trauma remained higher with forceps than with vacuum deliveries (adjusted rate ratio, 1.70).
The rate of neonatal trauma was comparable for forceps (9.56/1,000 live births) and vacuum deliveries (9.58/1,000 live births). In these cases, damage to the peripheral nervous system was the most common form of neonatal trauma, occurring in 4.85/1,000 live births with forceps delivery and 3.41/1,000 live births for vacuum delivery, the researchers found.
Consider morbidity following OVD against potential alternatives, authors say
According to Dr. Muraca, the rates of maternal trauma in her study – along with accumulating evidence of the severe long-term consequences of these injuries – demonstrates the importance of reporting timely, empirically derived risk measures that accurately reflect those that pregnant individuals may encounter in typical obstetric practice.
“Although there is merit in understanding the estimates of risk that can be achieved when conditions are optimal, the interpretation of these estimates can be misleading, especially given secular shifts in patterns of practice,” she said. “The failure to do so compromises women’s autonomy in making evidence-informed decisions regarding childbirth interventions, such as evaluating the short- and long-term risks of OVD and cesarean delivery.
Her group recommended that morbidity following OVD be weighed against potential alternatives to such procedures, which carry their own risks. “This includes an extended second stage of labor and a spontaneous vaginal delivery, or a second-stage cesarean delivery, both of which are associated with significant morbidity,” Dr. Muraca said. “However, a comprehensive consideration of high population rates of OVD morbidity also prompts questions about choice of instrument, obstetrician training in OVD use, and for recognizing cases that would benefit from a cesarean delivery earlier in labor.”
Alan Peaceman, MD, professor of obstetrics and gynecology at Northwestern University, Chicago, said he was not surprised by the rates of sphincter injury, but that the rate of severe neonatal injury rate was higher than he expected. However, he added, “I don’t think clinicians should change their approach based on a single study. They should continue with the approach that they are most skilled at and is appropriate for the clinical circumstances.”
The study was funded by a grant from the Canadian Institutes of Health Research. Dr. Muraca and Dr. Peaceman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
Workplace mistreatment common among emergency medicine residents
published online Aug. 19 in JAMA Network Open.
The survey of more than 6,000 residents found that almost 1 in 2 respondents had been exposed to some form of workplace mistreatment in the previous year, including gender and racial discrimination, physical abuse, or sexual harassment.
“The last study on mistreatment in EM residency training in the United States occurred more than 25 years ago,” said Michelle D. Lall, MD, associate professor of medicine at Emory University, Atlanta. “These findings provide a current look. Mistreatment occurs frequently in EM residency training nationally, and it occurs more frequently in women, racial/ethnic minorities, and those who identify as LGBTQ+,” Dr. Lall added. “Additionally, we found an association between experiencing mistreatment at least a few times per month and having suicidal thoughts.”
Negative sequelae from workplace mistreatment
Dr. Lall explained that workplace mistreatment and institutional responses to such behaviors have been linked to hostile work environments for physicians. In previous research, workplace mistreatment has been found to negatively affect individuals’ sense of self, a phenomenon that not only hindered professional productivity but also increased a variety of other negative factors, such as stress, job dissatisfaction, negative workplace behaviors, and turnover. Perhaps not surprisingly, workplace discrimination has also been shown to have negative effects on physical and mental health.
Despite such findings, little is known about the current state of workplace mistreatment among EM residents. This led the investigators to examine the prevalence, types, and sources of such perceived treatment during their training. In addition, the researchers assessed the association between mistreatment and suicidal ideation. Insights into these problems, they say, may spur leaders in the field to develop and implement strategies to help new physicians maintain their well-being throughout their careers.
“A 2019 study by Yue-Yung Hu and associates looked at discrimination, abuse, harassment, and burnout in surgical residents, and they found that mistreatment occurs frequently among general surgery residents, especially women,” Dr. Lall said. “Our study group felt it was important to look at the rates of mistreatment among EM residents nationally in order to obtain baseline data and to use this data to identify and promote educational interventions to reduce workplace mistreatment.”
Emergency residents surveyed
To achieve these ends, Dr. Lall and colleagues sent a survey to all individuals enrolled in EM residencies accredited by the Accreditation Council for Graduate Medical Education who had participated in the 2020 American Board of Emergency Medicine in-training examination. The 35-item multiple-choice survey asked residents to self-report the frequency, sources, and types of mistreatment they had experienced during their training. Suicidal thoughts were assessed by asking residents whether they had considered taking their own life.
Respondents categorized the frequency of mistreatment as never having occurred, having occurred a few times a year, a few times a month, a few times a week, or every day. The investigators created a composite indicator for the study’s primary comparisons that represented the maximum reported frequency of any single exposure. Responses were categorized according to the frequency of mistreatment exposure as either no exposure, exposures a few times per year, or exposures a few times or more per month (including a few times per week or every day).
Almost half report mistreatment
The survey was sent to 8,162 eligible residents in EM. Of those, 6,503 (79.7%) completed the entire survey. Respondents were primarily male (62.1%) and non-Hispanic White (64.0%); 2,620 residents (34.1%) were from other racial/ethnic groups. Of the respondents, 483 residents (6.6%) identified as lesbian, gay, bisexual, transgender, queer, or other (LGBTQ+); 5,951 residents (77.5%) were married or in a relationship.
It was found that 3,463 (45.1%) of participants reported having been exposed to some sort of workplace mistreatment during the most recent academic year. A common source of mistreatment was patients and/or their families. These caused a total of 1,234 events.
Gender discrimination was reported by 2,104 residents (29.5%), 1,635 of whom were women. The most common source of such discrimination was patients or patients’ family members (1,027 women; 184 men). Other sources included nurses or staff (331 women; 59 men).
Racial discrimination was common. It was reported by 1,284 residents; 907 residents were from racial/ethnic groups other than White. Among non-White racial/ethnic groups, 248 residents reported being exposed to racial discrimination at least a few times per month. The most common source of racial discrimination was patients or their family members.
Discrimination based on sexual orientation or gender identity was reported by 220 residents. Once again, the majority of LGBTQ+ residents indicated that patients or their families were the primary source. More than 1,000 residents (n = 1047) reported sexual harassment; among these residents, 721 were women. Patients and/or patients’ family members were the most common source of such discrimination, followed by nurses and staff.
A total of 2,069 residents reported verbal or emotional abuse, including 806 women and 1,212 men. Patients/patients’ family members were the most common source, followed by attending physicians. Physical abuse was reported by 331 respondents. Physical abuse was primarily attributed to patients/patients’ families.
Suicidal thoughts were reported by 178 residents; the prevalence was comparable with respect to gender (2.4% men; 2.4% women) and race/ethnicity (2.4% non-Hispanic White; 2.7% other racial/ethnic groups). Adjusted models revealed that the prevalence for suicidal thoughts was greater among residents who identified as LGBTQ+ (odds ratio [OR], 2.04; 99% confidence interval, 1.04-3.99). An association was found between suicidal thoughts and having experienced mistreatment at least a few times each month (OR, 5.83; 99% CI, 3.70-9.20).
Identifying sources key to stemming mistreatment
These findings, the researchers say, demonstrate the alarming frequency with which workplace mistreatment occurs for EM residents. The survey also found that such mistreatment was more common among residents from racial/ethnic minority populations, women, and residents who identify as LGBTQ+. Perhaps most disturbingly, the occurrence of workplace mistreatment was found to be associated with suicidal thoughts.
The researchers say that although it is likely that residents in many medical specialties experience similar mistreatment to some degree, such treatment should never be considered acceptable. Indeed, Dr. Lall said that identifying sources of mistreatment may help both institutions and individuals determine interventions necessary for improving the well-being of EM residents.
“The first step is recognizing, based on our data, that mistreatment is experienced frequently in EM training in the United States,” she said. “Future qualitative studies of residents and program leaders may help identify which systems, programs, or cultural factors were associated with lower rates of mistreatment in some institutions and higher rates in others.
“Identifying these factors and developing and promoting best practices to minimize workplace mistreatment during residency may help optimize the professional career experience and improve the personal and professional well-being of physicians throughout their lives,” Dr. Lall added.
Commenting on the findings for this article, Karl Y. Bilimoria, MD, of Northwestern University, Chicago, noted that these surveys clearly lay out actionable opportunities to improve trainee mistreatment. “Given that much of the mistreatment of EM residents comes from patients and families, the solutions must be appropriately tailored to address those sources,” Dr. Bilimoria noted.
“Programs need to actively work even more to protect their trainees and faculty from this mistreatment, as it has severe effects and often leads to, or worsens, burnout,” he added.
Funding for statistical analysis was provided by the American Board of Emergency Medicine. Dr. Lall and Dr. Bilimoria reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
published online Aug. 19 in JAMA Network Open.
The survey of more than 6,000 residents found that almost 1 in 2 respondents had been exposed to some form of workplace mistreatment in the previous year, including gender and racial discrimination, physical abuse, or sexual harassment.
“The last study on mistreatment in EM residency training in the United States occurred more than 25 years ago,” said Michelle D. Lall, MD, associate professor of medicine at Emory University, Atlanta. “These findings provide a current look. Mistreatment occurs frequently in EM residency training nationally, and it occurs more frequently in women, racial/ethnic minorities, and those who identify as LGBTQ+,” Dr. Lall added. “Additionally, we found an association between experiencing mistreatment at least a few times per month and having suicidal thoughts.”
Negative sequelae from workplace mistreatment
Dr. Lall explained that workplace mistreatment and institutional responses to such behaviors have been linked to hostile work environments for physicians. In previous research, workplace mistreatment has been found to negatively affect individuals’ sense of self, a phenomenon that not only hindered professional productivity but also increased a variety of other negative factors, such as stress, job dissatisfaction, negative workplace behaviors, and turnover. Perhaps not surprisingly, workplace discrimination has also been shown to have negative effects on physical and mental health.
Despite such findings, little is known about the current state of workplace mistreatment among EM residents. This led the investigators to examine the prevalence, types, and sources of such perceived treatment during their training. In addition, the researchers assessed the association between mistreatment and suicidal ideation. Insights into these problems, they say, may spur leaders in the field to develop and implement strategies to help new physicians maintain their well-being throughout their careers.
“A 2019 study by Yue-Yung Hu and associates looked at discrimination, abuse, harassment, and burnout in surgical residents, and they found that mistreatment occurs frequently among general surgery residents, especially women,” Dr. Lall said. “Our study group felt it was important to look at the rates of mistreatment among EM residents nationally in order to obtain baseline data and to use this data to identify and promote educational interventions to reduce workplace mistreatment.”
Emergency residents surveyed
To achieve these ends, Dr. Lall and colleagues sent a survey to all individuals enrolled in EM residencies accredited by the Accreditation Council for Graduate Medical Education who had participated in the 2020 American Board of Emergency Medicine in-training examination. The 35-item multiple-choice survey asked residents to self-report the frequency, sources, and types of mistreatment they had experienced during their training. Suicidal thoughts were assessed by asking residents whether they had considered taking their own life.
Respondents categorized the frequency of mistreatment as never having occurred, having occurred a few times a year, a few times a month, a few times a week, or every day. The investigators created a composite indicator for the study’s primary comparisons that represented the maximum reported frequency of any single exposure. Responses were categorized according to the frequency of mistreatment exposure as either no exposure, exposures a few times per year, or exposures a few times or more per month (including a few times per week or every day).
Almost half report mistreatment
The survey was sent to 8,162 eligible residents in EM. Of those, 6,503 (79.7%) completed the entire survey. Respondents were primarily male (62.1%) and non-Hispanic White (64.0%); 2,620 residents (34.1%) were from other racial/ethnic groups. Of the respondents, 483 residents (6.6%) identified as lesbian, gay, bisexual, transgender, queer, or other (LGBTQ+); 5,951 residents (77.5%) were married or in a relationship.
It was found that 3,463 (45.1%) of participants reported having been exposed to some sort of workplace mistreatment during the most recent academic year. A common source of mistreatment was patients and/or their families. These caused a total of 1,234 events.
Gender discrimination was reported by 2,104 residents (29.5%), 1,635 of whom were women. The most common source of such discrimination was patients or patients’ family members (1,027 women; 184 men). Other sources included nurses or staff (331 women; 59 men).
Racial discrimination was common. It was reported by 1,284 residents; 907 residents were from racial/ethnic groups other than White. Among non-White racial/ethnic groups, 248 residents reported being exposed to racial discrimination at least a few times per month. The most common source of racial discrimination was patients or their family members.
Discrimination based on sexual orientation or gender identity was reported by 220 residents. Once again, the majority of LGBTQ+ residents indicated that patients or their families were the primary source. More than 1,000 residents (n = 1047) reported sexual harassment; among these residents, 721 were women. Patients and/or patients’ family members were the most common source of such discrimination, followed by nurses and staff.
A total of 2,069 residents reported verbal or emotional abuse, including 806 women and 1,212 men. Patients/patients’ family members were the most common source, followed by attending physicians. Physical abuse was reported by 331 respondents. Physical abuse was primarily attributed to patients/patients’ families.
Suicidal thoughts were reported by 178 residents; the prevalence was comparable with respect to gender (2.4% men; 2.4% women) and race/ethnicity (2.4% non-Hispanic White; 2.7% other racial/ethnic groups). Adjusted models revealed that the prevalence for suicidal thoughts was greater among residents who identified as LGBTQ+ (odds ratio [OR], 2.04; 99% confidence interval, 1.04-3.99). An association was found between suicidal thoughts and having experienced mistreatment at least a few times each month (OR, 5.83; 99% CI, 3.70-9.20).
Identifying sources key to stemming mistreatment
These findings, the researchers say, demonstrate the alarming frequency with which workplace mistreatment occurs for EM residents. The survey also found that such mistreatment was more common among residents from racial/ethnic minority populations, women, and residents who identify as LGBTQ+. Perhaps most disturbingly, the occurrence of workplace mistreatment was found to be associated with suicidal thoughts.
The researchers say that although it is likely that residents in many medical specialties experience similar mistreatment to some degree, such treatment should never be considered acceptable. Indeed, Dr. Lall said that identifying sources of mistreatment may help both institutions and individuals determine interventions necessary for improving the well-being of EM residents.
“The first step is recognizing, based on our data, that mistreatment is experienced frequently in EM training in the United States,” she said. “Future qualitative studies of residents and program leaders may help identify which systems, programs, or cultural factors were associated with lower rates of mistreatment in some institutions and higher rates in others.
“Identifying these factors and developing and promoting best practices to minimize workplace mistreatment during residency may help optimize the professional career experience and improve the personal and professional well-being of physicians throughout their lives,” Dr. Lall added.
Commenting on the findings for this article, Karl Y. Bilimoria, MD, of Northwestern University, Chicago, noted that these surveys clearly lay out actionable opportunities to improve trainee mistreatment. “Given that much of the mistreatment of EM residents comes from patients and families, the solutions must be appropriately tailored to address those sources,” Dr. Bilimoria noted.
“Programs need to actively work even more to protect their trainees and faculty from this mistreatment, as it has severe effects and often leads to, or worsens, burnout,” he added.
Funding for statistical analysis was provided by the American Board of Emergency Medicine. Dr. Lall and Dr. Bilimoria reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
published online Aug. 19 in JAMA Network Open.
The survey of more than 6,000 residents found that almost 1 in 2 respondents had been exposed to some form of workplace mistreatment in the previous year, including gender and racial discrimination, physical abuse, or sexual harassment.
“The last study on mistreatment in EM residency training in the United States occurred more than 25 years ago,” said Michelle D. Lall, MD, associate professor of medicine at Emory University, Atlanta. “These findings provide a current look. Mistreatment occurs frequently in EM residency training nationally, and it occurs more frequently in women, racial/ethnic minorities, and those who identify as LGBTQ+,” Dr. Lall added. “Additionally, we found an association between experiencing mistreatment at least a few times per month and having suicidal thoughts.”
Negative sequelae from workplace mistreatment
Dr. Lall explained that workplace mistreatment and institutional responses to such behaviors have been linked to hostile work environments for physicians. In previous research, workplace mistreatment has been found to negatively affect individuals’ sense of self, a phenomenon that not only hindered professional productivity but also increased a variety of other negative factors, such as stress, job dissatisfaction, negative workplace behaviors, and turnover. Perhaps not surprisingly, workplace discrimination has also been shown to have negative effects on physical and mental health.
Despite such findings, little is known about the current state of workplace mistreatment among EM residents. This led the investigators to examine the prevalence, types, and sources of such perceived treatment during their training. In addition, the researchers assessed the association between mistreatment and suicidal ideation. Insights into these problems, they say, may spur leaders in the field to develop and implement strategies to help new physicians maintain their well-being throughout their careers.
“A 2019 study by Yue-Yung Hu and associates looked at discrimination, abuse, harassment, and burnout in surgical residents, and they found that mistreatment occurs frequently among general surgery residents, especially women,” Dr. Lall said. “Our study group felt it was important to look at the rates of mistreatment among EM residents nationally in order to obtain baseline data and to use this data to identify and promote educational interventions to reduce workplace mistreatment.”
Emergency residents surveyed
To achieve these ends, Dr. Lall and colleagues sent a survey to all individuals enrolled in EM residencies accredited by the Accreditation Council for Graduate Medical Education who had participated in the 2020 American Board of Emergency Medicine in-training examination. The 35-item multiple-choice survey asked residents to self-report the frequency, sources, and types of mistreatment they had experienced during their training. Suicidal thoughts were assessed by asking residents whether they had considered taking their own life.
Respondents categorized the frequency of mistreatment as never having occurred, having occurred a few times a year, a few times a month, a few times a week, or every day. The investigators created a composite indicator for the study’s primary comparisons that represented the maximum reported frequency of any single exposure. Responses were categorized according to the frequency of mistreatment exposure as either no exposure, exposures a few times per year, or exposures a few times or more per month (including a few times per week or every day).
Almost half report mistreatment
The survey was sent to 8,162 eligible residents in EM. Of those, 6,503 (79.7%) completed the entire survey. Respondents were primarily male (62.1%) and non-Hispanic White (64.0%); 2,620 residents (34.1%) were from other racial/ethnic groups. Of the respondents, 483 residents (6.6%) identified as lesbian, gay, bisexual, transgender, queer, or other (LGBTQ+); 5,951 residents (77.5%) were married or in a relationship.
It was found that 3,463 (45.1%) of participants reported having been exposed to some sort of workplace mistreatment during the most recent academic year. A common source of mistreatment was patients and/or their families. These caused a total of 1,234 events.
Gender discrimination was reported by 2,104 residents (29.5%), 1,635 of whom were women. The most common source of such discrimination was patients or patients’ family members (1,027 women; 184 men). Other sources included nurses or staff (331 women; 59 men).
Racial discrimination was common. It was reported by 1,284 residents; 907 residents were from racial/ethnic groups other than White. Among non-White racial/ethnic groups, 248 residents reported being exposed to racial discrimination at least a few times per month. The most common source of racial discrimination was patients or their family members.
Discrimination based on sexual orientation or gender identity was reported by 220 residents. Once again, the majority of LGBTQ+ residents indicated that patients or their families were the primary source. More than 1,000 residents (n = 1047) reported sexual harassment; among these residents, 721 were women. Patients and/or patients’ family members were the most common source of such discrimination, followed by nurses and staff.
A total of 2,069 residents reported verbal or emotional abuse, including 806 women and 1,212 men. Patients/patients’ family members were the most common source, followed by attending physicians. Physical abuse was reported by 331 respondents. Physical abuse was primarily attributed to patients/patients’ families.
Suicidal thoughts were reported by 178 residents; the prevalence was comparable with respect to gender (2.4% men; 2.4% women) and race/ethnicity (2.4% non-Hispanic White; 2.7% other racial/ethnic groups). Adjusted models revealed that the prevalence for suicidal thoughts was greater among residents who identified as LGBTQ+ (odds ratio [OR], 2.04; 99% confidence interval, 1.04-3.99). An association was found between suicidal thoughts and having experienced mistreatment at least a few times each month (OR, 5.83; 99% CI, 3.70-9.20).
Identifying sources key to stemming mistreatment
These findings, the researchers say, demonstrate the alarming frequency with which workplace mistreatment occurs for EM residents. The survey also found that such mistreatment was more common among residents from racial/ethnic minority populations, women, and residents who identify as LGBTQ+. Perhaps most disturbingly, the occurrence of workplace mistreatment was found to be associated with suicidal thoughts.
The researchers say that although it is likely that residents in many medical specialties experience similar mistreatment to some degree, such treatment should never be considered acceptable. Indeed, Dr. Lall said that identifying sources of mistreatment may help both institutions and individuals determine interventions necessary for improving the well-being of EM residents.
“The first step is recognizing, based on our data, that mistreatment is experienced frequently in EM training in the United States,” she said. “Future qualitative studies of residents and program leaders may help identify which systems, programs, or cultural factors were associated with lower rates of mistreatment in some institutions and higher rates in others.
“Identifying these factors and developing and promoting best practices to minimize workplace mistreatment during residency may help optimize the professional career experience and improve the personal and professional well-being of physicians throughout their lives,” Dr. Lall added.
Commenting on the findings for this article, Karl Y. Bilimoria, MD, of Northwestern University, Chicago, noted that these surveys clearly lay out actionable opportunities to improve trainee mistreatment. “Given that much of the mistreatment of EM residents comes from patients and families, the solutions must be appropriately tailored to address those sources,” Dr. Bilimoria noted.
“Programs need to actively work even more to protect their trainees and faculty from this mistreatment, as it has severe effects and often leads to, or worsens, burnout,” he added.
Funding for statistical analysis was provided by the American Board of Emergency Medicine. Dr. Lall and Dr. Bilimoria reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An international trip: Global experts weigh in on psychedelics
In 1967, when the United Nations Convention on Drugs classified psychedelics as schedule I substances, it effectively ended research into these agents as potential therapeutics for psychiatric disorders.
Psychedelics induce altered states of perception. They bind to the 5-hydroxytryptamine 2A (5-HT2A) receptor and include psilocybin, which is derived from “magic mushrooms”; N,N-dimethyltryptamine (DMT), a component of ayahuasca and mescaline (peyote cactus); and the synthesized compound D-lysergic acid diethylamide (LSD). Other agents, such as ketamine and 3,4-methylenedioxymethamphetamine (MDMA), also known as ecstasy, are sometimes considered psychedelics as well.
Before they were classified as schedule I agents, psychedelics had been shown to be particularly beneficial for patients with treatment-resistant conditions, including depression and posttraumatic stress disorder (PTSD), especially when administered in a supportive, therapeutic setting.
Now, after a hiatus of almost 50 years, there is renewed global interest in the scientific investigation of psychedelics. The attention was spurred in part by several exploratory studies of DMT in humans conducted in the 1990s by Rick Strassman, MD, and colleagues at the University of New Mexico, Albuquerque.
Around the same time, Franz X. Vollenweider, MD, and colleagues at the University of Zürich began researching psilocybin and its effects on human behavior. However, it was a 2006 study of psilocybin by a team of researchers at Johns Hopkins University, Baltimore, that is widely cited as a catalyst for the current renaissance in psychedelic research.
To provide a broad-based, international perspective on these agents, including their current legal status and indications, treatment regimens, safety, efficacy, and future considerations, this news organization interviewed nine expert researchers from around the globe.
Global legal status
In most, if not all, countries, it is still illegal to prescribe psychedelics in other than a research setting.
They can be used in research, but only with approval from the Food and Drug Administration under licensure from the Drug Enforcement Administration.
France lists all synthetic hallucinogens and hallucinogenic mushrooms as narcotic. As a result, possession, use, transportation, and collection are subject to criminal sanctions.
In France, NMDA antagonists such as ketamine and nitrous oxide are regarded as psychedelic molecules and can be used off label for various conditions or as part of research protocols authorized by the French public health code.
Although psychedelics are illegal under Mexican law, they are commonly used in indigenous communities as part of traditional rituals.
“The line between traditional consumption and psychedelic tourism is very thin,” José J. Mendoza Velásquez, MD, professor in the department of mental health, National Autonomous University of Mexico, Mexico City, said in an interview.
Psychedelics also are illegal in the United Kingdom, although government agencies have recently allowed research groups to investigate them. Psychedelics cannot be prescribed in Germany, Spain, or Italy. However, investigators in these countries can request permission from regulatory agencies to conduct research.
Brazil allows psychedelic substances to be researched, particularly ayahuasca, which has long traditional and religious roots in the country.
However, as in other countries, none of the classic psychedelics is regulated for therapeutic use in Brazil. It is widely expected that the Brazilian government will approve MDMA sometime in 2024 for use in the treatment of PTSD.
Potential indications
Psychedelics are currently under investigation as potential treatments for major depression, treatment-resistant depression, PTSD, pain management, and anorexia, among other conditions.
In France, Florian Ferreri, MD, PhD, at Hospital Saint-Antoine, Paris, is researching ketamine for treatment of patients with suicidal crisis/ideation and treatment-resistant depression.
In the United Kingdom, David Nutt, FMedSci, Edmond J. Safra Professor of Neuropsychopharmacology at Imperial College London, and his team have conducted studies of the use of psychedelics in conjunction with psychological support for patients with treatment-resistant depression, and they are currently exploring their use in the treatment of anorexia and various pain syndromes.
In Germany, Gerhard Gründer, MD, professor of psychiatry at the Central Institute of Mental Health, in Mannheim, noted that a study of psilocybin for treatment-resistant depression will launch sometime in 2021. In Italy, current research is focusing on MDMA and ketamine in the laboratory environment and in animal models for treating depression and drug abuse.
Researcher Helen Dolengevich-Segal, MD, a psychiatrist at Hospital Universitario del Henares, Madrid, noted that although research on esketamine for the treatment of severe depressive disorder with suicidal thoughts is underway, there is very limited published research from that country into the use of classic psychedelics for various psychiatric disorders, given their current illegal status.
Mexico’s Dr. Velásquez noted that although he is prohibited from prescribing psychedelics, he does have patients who take the drugs to augment medical treatment. For instance, he said, his patients frequently use psilocybin to help with severe depression, pain, and insomnia.
Environment is key
Most researchers agree that for psychedelics to be safe and effective, patient education and administration in a controlled environment by experienced clinicians are key to successful treatment.
Roland R. Griffiths, PhD, director of the Center for Psychedelic and Consciousness Research at Johns Hopkins, said that ongoing U.S. psilocybin research – primarily in major depressive disorder and psychological distress associated with life-threatening illness, drug addiction, anorexia nervosa, obsessive-compulsive disorder, and headache – generally includes one or two treatment sessions, each of which lasts 6-8 hours.
Such sessions typically involve oral administration of a moderately high dose of a psychedelic under what he characterizes as “psychologically supported conditions.”
For Dr. Griffiths, there are serious potential risks associated with the use of psilocybin and other psychedelics outside such environments.
“When taken in uncontrolled conditions, classic psychedelics can produce confusion and disorientation resulting in behavior dangerous to the participant and others, including life-threatening risk,” he said.
Dr. Gründer agreed.
“At the moment, I cannot imagine that you would go to the pharmacy with a prescription for psilocybin and get yourself a pill and then take it in a quiet little room,” he said. Dr. Dolengevich-Segal and Dr. Velásquez echoed these sentiments, noting the optimal location for administration is one that is quiet and secure and where patients feel safe.
Luís Fernando Tófoli, MD, PhD, professor of medical psychology and psychiatry at the University of Campinas, and Eduardo Schenberg, PhD, founder and CEO of Instituto Phaneros in São Paulo, Brazil, said more research is needed to determine the optimal therapeutic environment for individual agents.
“Most studies have a low number of participants (around 20 or 30), especially in neuroimaging, with high unblinding rates,” Dr. Schenberg said. “Therefore, novel methodological approaches are also necessary, as these substances do not easily fit into the traditional pharmacology epistemic model.”
Risks, abuse potential
The abuse potential of psychedelics is an ongoing concern for the public, researchers, and regulators, but the consensus among nearly all of these experts is that when administered by medical professionals in controlled settings, these drugs are associated with extremely low risk.
It is recreational use that presents an abuse concern, said Dr. Ferreri, but with the low doses used in psychiatry, the risk is “very limited or even nonexistent.”
Dr. Nutt said the abuse potential of psychedelics is so low that they can be used to treat addiction.
“Functionally, psychedelics are antiaddictive,” Dr. Nutt said. “The fact is, if you take them repeatedly, you develop tolerance, and the effect disappears. You can’t overcome it. But everyone believes they’re addictive because they’re scheduled drugs.”
Dr. Velásquez is something of an outlier. He believes the abuse potential with psychedelics is poorly understood and that some patients may develop tolerance, which is a potential gateway to dependence.
“Such is the case with LSD,” he said, “where this substance also favors tolerance to other psychedelic drugs such as psilocybin.”
Dosing also seems to play a key role in mitigating potential abuse, said Luca Pani, MD, professor of pharmacology and psychiatry at the University of Modena, Italy. Dr. Pani explained that with low doses and microdoses of psychedelics, the potential for abuse is eliminated.
Dr. Nutt, Dr. Pani, and Dr. Ferreri also noted the importance of medical supervision. For instance, said Dr. Ferreri, when administering ketamine, his team closely monitors both mental and physical parameters – heart rate and blood pressure, in particular – because the drug can have hypertensive effects.
Dr. Schenberg noted that ibogaine, a naturally occurring psychedelic frequently used by traditional communities in Africa in rituals and for healing purposes, could cause potentially fatal arrhythmias, so it’s critical that the treatment is administered in a hospital setting that has a cardiac unit.
Dr. Pani said there is a need for more research, especially regarding the molecular mechanisms behind the behavioral effects of low-dose psychedelic therapy and the potential risks of multiple treatments with the drugs.
“Although extensive toxicology has been conducted on a single active dose of psilocybin, which has been proven to be safe, further research is required to understand better the possible health risks, especially in relation to cardiac and lung tissue,” he said.
Psychologically challenging
The experts note that given the relative lack of experience with psychedelic therapy, preparing patients for potential adverse effects is paramount. This is particularly relevant in the research setting and highlights the need for adequate patient screening and aftercare.
Dr. Gründer and Dr. Dolengevich-Segal emphasized the importance of having qualified personnel available in the event that patients experience adverse psychological events during treatment.
For Dr. Gründer, the potential for psilocybin to cause patients to lose control, experience psychotic symptoms, or become paranoid warrants considerable preparation by treating physicians.
Patients occasionally experience fear and anxiety during treatment, though it’s usually short-lived, said Dr. Griffiths. Nevertheless, these experiences may open the door to greater insight. “A number of people report that these psychologically challenging states are a valuable part of the overall experience,” he said.
The situation is similar in Spain, where Dr. Dolengevich-Segal noted that typical treatment regimens have a strong focus on the patient’s experience as a therapeutic tool. As in the United Kingdom and the United States, her team guides patients to what they call a “peak experience,” which allows them to gain a better understanding of the trauma underlying their mental health problems.
Dr. Nutt said that in the United Kingdom, they haven’t seen adverse reactions in patients receiving psychedelic therapy, although sedatives such as benzodiazepines could be used to manage them. He added that at his center, two therapists are present at every treatment session, and all personnel are “trained medics or psychologists.”
Patient education
Preparing and educating patients about the therapy are critical, said Dr. Gründer, especially given the intense response psychedelic treatment often invokes.
Echoing Dr. Gründer, Dr. Tófoli said explaining the nature of psychedelic treatment to potential patients helps ease anxiety.
Dr. Griffiths noted that in the United States, study participants are not only educated about the potential effects of psychedelic agents but also undergo several hours of psychological preparation in advance of their first treatment session and are provided with psychological support after treatment.
There is also a strong emphasis on patient preparation and education in the United Kingdom, where patients meet with therapists before and after treatment. During these posttreatment debriefings, clinicians use the patients’ experience with psychedelics to help them gain insight into the underlying cause of their depression.
Dr. Schenberg noted that at his institution in São Paulo, there are online courses to teach clinicians about psychedelic therapy for psychiatric disorders. Next year, he added, a new training program in MDMA-assisted psychotherapy will begin.
Working out treatment protocols
Treatment protocols for psychedelics vary by agent and indication from country to country. For instance, Dr. Pani noted that current psychedelic research in Italy predominantly focuses more on microdosing, which involves administering 1% of the pharmacologically active dose to a maximum of 100 mcg, in contrast to low dosing or full dosing.
Therapeutic regimens in Brazil, said Dr. Schenberg, also differ by agent but share common elements. For instance, psychedelics are always administered in a research setting, and sessions include concomitant psychotherapy.
In Germany, investigators are working to determine optimal treatment regimen for psilocybin for resistant depression in a randomized three-arm study planned for 2021.
For Mexico’s Dr. Velásquez, treatment regimens are complex and varied. Either way, he said, patients always require long-term follow-up.
With ketamine therapy, Dr. Ferreri said his team administers the drug in 45- to 60-minute intravenous infusion sessions in a hospital room without light or sound stimulation. Regardless of the drug’s immediate effect, he said, the protocol is repeated within a 6-month period.
The question of the duration of treatment effect is important. Dr. Griffiths said research suggests that the positive effects of psilocybin are long lasting and that most individuals report positive changes in mood, attitude, and behavior that endure for months or even years after the session.
“Our research has shown that the benefits of these experiences can last as long as 14 months, often longer, and that many participants characterize their psilocybin experience as among the most profound and personally meaningful experiences of their lives,” said Dr. Griffiths.
Dr. Nutt agreed, noting that a single intense “trip” can improve mood for weeks, months, or even years. Nevertheless, he said, in his experience, approximately three-quarters of patients treated with psychedelics for major depression relapse within 3-9 months.
“Most get better,” he said, “but the majority of depression comes back over a period of months.”
Given the current illegal status of the drugs, he said it’s nearly impossible to provide patients with regular, subsequent treatment with psychedelics over time.
“My suspicion is that you might well have to dose four or five times over a couple of years to get people to escape from very severe depression,” said Dr. Nutt. “The longer they’ve been depressed, the harder it is for them to make a full recovery, because it’s more entrenched in the brain.”
All experts agree that exciting times are ahead for psychedelics as therapeutics for a wide range of psychiatric disorders.
“We can look forward to continued growth and expansion of this research,” said Dr. Griffiths, “including the refinement of protocols for a variety of therapeutic indications and to the development of a variety of new classic psychedelic compounds.”
A version of this article first appeared on Medscape.com.
In 1967, when the United Nations Convention on Drugs classified psychedelics as schedule I substances, it effectively ended research into these agents as potential therapeutics for psychiatric disorders.
Psychedelics induce altered states of perception. They bind to the 5-hydroxytryptamine 2A (5-HT2A) receptor and include psilocybin, which is derived from “magic mushrooms”; N,N-dimethyltryptamine (DMT), a component of ayahuasca and mescaline (peyote cactus); and the synthesized compound D-lysergic acid diethylamide (LSD). Other agents, such as ketamine and 3,4-methylenedioxymethamphetamine (MDMA), also known as ecstasy, are sometimes considered psychedelics as well.
Before they were classified as schedule I agents, psychedelics had been shown to be particularly beneficial for patients with treatment-resistant conditions, including depression and posttraumatic stress disorder (PTSD), especially when administered in a supportive, therapeutic setting.
Now, after a hiatus of almost 50 years, there is renewed global interest in the scientific investigation of psychedelics. The attention was spurred in part by several exploratory studies of DMT in humans conducted in the 1990s by Rick Strassman, MD, and colleagues at the University of New Mexico, Albuquerque.
Around the same time, Franz X. Vollenweider, MD, and colleagues at the University of Zürich began researching psilocybin and its effects on human behavior. However, it was a 2006 study of psilocybin by a team of researchers at Johns Hopkins University, Baltimore, that is widely cited as a catalyst for the current renaissance in psychedelic research.
To provide a broad-based, international perspective on these agents, including their current legal status and indications, treatment regimens, safety, efficacy, and future considerations, this news organization interviewed nine expert researchers from around the globe.
Global legal status
In most, if not all, countries, it is still illegal to prescribe psychedelics in other than a research setting.
They can be used in research, but only with approval from the Food and Drug Administration under licensure from the Drug Enforcement Administration.
France lists all synthetic hallucinogens and hallucinogenic mushrooms as narcotic. As a result, possession, use, transportation, and collection are subject to criminal sanctions.
In France, NMDA antagonists such as ketamine and nitrous oxide are regarded as psychedelic molecules and can be used off label for various conditions or as part of research protocols authorized by the French public health code.
Although psychedelics are illegal under Mexican law, they are commonly used in indigenous communities as part of traditional rituals.
“The line between traditional consumption and psychedelic tourism is very thin,” José J. Mendoza Velásquez, MD, professor in the department of mental health, National Autonomous University of Mexico, Mexico City, said in an interview.
Psychedelics also are illegal in the United Kingdom, although government agencies have recently allowed research groups to investigate them. Psychedelics cannot be prescribed in Germany, Spain, or Italy. However, investigators in these countries can request permission from regulatory agencies to conduct research.
Brazil allows psychedelic substances to be researched, particularly ayahuasca, which has long traditional and religious roots in the country.
However, as in other countries, none of the classic psychedelics is regulated for therapeutic use in Brazil. It is widely expected that the Brazilian government will approve MDMA sometime in 2024 for use in the treatment of PTSD.
Potential indications
Psychedelics are currently under investigation as potential treatments for major depression, treatment-resistant depression, PTSD, pain management, and anorexia, among other conditions.
In France, Florian Ferreri, MD, PhD, at Hospital Saint-Antoine, Paris, is researching ketamine for treatment of patients with suicidal crisis/ideation and treatment-resistant depression.
In the United Kingdom, David Nutt, FMedSci, Edmond J. Safra Professor of Neuropsychopharmacology at Imperial College London, and his team have conducted studies of the use of psychedelics in conjunction with psychological support for patients with treatment-resistant depression, and they are currently exploring their use in the treatment of anorexia and various pain syndromes.
In Germany, Gerhard Gründer, MD, professor of psychiatry at the Central Institute of Mental Health, in Mannheim, noted that a study of psilocybin for treatment-resistant depression will launch sometime in 2021. In Italy, current research is focusing on MDMA and ketamine in the laboratory environment and in animal models for treating depression and drug abuse.
Researcher Helen Dolengevich-Segal, MD, a psychiatrist at Hospital Universitario del Henares, Madrid, noted that although research on esketamine for the treatment of severe depressive disorder with suicidal thoughts is underway, there is very limited published research from that country into the use of classic psychedelics for various psychiatric disorders, given their current illegal status.
Mexico’s Dr. Velásquez noted that although he is prohibited from prescribing psychedelics, he does have patients who take the drugs to augment medical treatment. For instance, he said, his patients frequently use psilocybin to help with severe depression, pain, and insomnia.
Environment is key
Most researchers agree that for psychedelics to be safe and effective, patient education and administration in a controlled environment by experienced clinicians are key to successful treatment.
Roland R. Griffiths, PhD, director of the Center for Psychedelic and Consciousness Research at Johns Hopkins, said that ongoing U.S. psilocybin research – primarily in major depressive disorder and psychological distress associated with life-threatening illness, drug addiction, anorexia nervosa, obsessive-compulsive disorder, and headache – generally includes one or two treatment sessions, each of which lasts 6-8 hours.
Such sessions typically involve oral administration of a moderately high dose of a psychedelic under what he characterizes as “psychologically supported conditions.”
For Dr. Griffiths, there are serious potential risks associated with the use of psilocybin and other psychedelics outside such environments.
“When taken in uncontrolled conditions, classic psychedelics can produce confusion and disorientation resulting in behavior dangerous to the participant and others, including life-threatening risk,” he said.
Dr. Gründer agreed.
“At the moment, I cannot imagine that you would go to the pharmacy with a prescription for psilocybin and get yourself a pill and then take it in a quiet little room,” he said. Dr. Dolengevich-Segal and Dr. Velásquez echoed these sentiments, noting the optimal location for administration is one that is quiet and secure and where patients feel safe.
Luís Fernando Tófoli, MD, PhD, professor of medical psychology and psychiatry at the University of Campinas, and Eduardo Schenberg, PhD, founder and CEO of Instituto Phaneros in São Paulo, Brazil, said more research is needed to determine the optimal therapeutic environment for individual agents.
“Most studies have a low number of participants (around 20 or 30), especially in neuroimaging, with high unblinding rates,” Dr. Schenberg said. “Therefore, novel methodological approaches are also necessary, as these substances do not easily fit into the traditional pharmacology epistemic model.”
Risks, abuse potential
The abuse potential of psychedelics is an ongoing concern for the public, researchers, and regulators, but the consensus among nearly all of these experts is that when administered by medical professionals in controlled settings, these drugs are associated with extremely low risk.
It is recreational use that presents an abuse concern, said Dr. Ferreri, but with the low doses used in psychiatry, the risk is “very limited or even nonexistent.”
Dr. Nutt said the abuse potential of psychedelics is so low that they can be used to treat addiction.
“Functionally, psychedelics are antiaddictive,” Dr. Nutt said. “The fact is, if you take them repeatedly, you develop tolerance, and the effect disappears. You can’t overcome it. But everyone believes they’re addictive because they’re scheduled drugs.”
Dr. Velásquez is something of an outlier. He believes the abuse potential with psychedelics is poorly understood and that some patients may develop tolerance, which is a potential gateway to dependence.
“Such is the case with LSD,” he said, “where this substance also favors tolerance to other psychedelic drugs such as psilocybin.”
Dosing also seems to play a key role in mitigating potential abuse, said Luca Pani, MD, professor of pharmacology and psychiatry at the University of Modena, Italy. Dr. Pani explained that with low doses and microdoses of psychedelics, the potential for abuse is eliminated.
Dr. Nutt, Dr. Pani, and Dr. Ferreri also noted the importance of medical supervision. For instance, said Dr. Ferreri, when administering ketamine, his team closely monitors both mental and physical parameters – heart rate and blood pressure, in particular – because the drug can have hypertensive effects.
Dr. Schenberg noted that ibogaine, a naturally occurring psychedelic frequently used by traditional communities in Africa in rituals and for healing purposes, could cause potentially fatal arrhythmias, so it’s critical that the treatment is administered in a hospital setting that has a cardiac unit.
Dr. Pani said there is a need for more research, especially regarding the molecular mechanisms behind the behavioral effects of low-dose psychedelic therapy and the potential risks of multiple treatments with the drugs.
“Although extensive toxicology has been conducted on a single active dose of psilocybin, which has been proven to be safe, further research is required to understand better the possible health risks, especially in relation to cardiac and lung tissue,” he said.
Psychologically challenging
The experts note that given the relative lack of experience with psychedelic therapy, preparing patients for potential adverse effects is paramount. This is particularly relevant in the research setting and highlights the need for adequate patient screening and aftercare.
Dr. Gründer and Dr. Dolengevich-Segal emphasized the importance of having qualified personnel available in the event that patients experience adverse psychological events during treatment.
For Dr. Gründer, the potential for psilocybin to cause patients to lose control, experience psychotic symptoms, or become paranoid warrants considerable preparation by treating physicians.
Patients occasionally experience fear and anxiety during treatment, though it’s usually short-lived, said Dr. Griffiths. Nevertheless, these experiences may open the door to greater insight. “A number of people report that these psychologically challenging states are a valuable part of the overall experience,” he said.
The situation is similar in Spain, where Dr. Dolengevich-Segal noted that typical treatment regimens have a strong focus on the patient’s experience as a therapeutic tool. As in the United Kingdom and the United States, her team guides patients to what they call a “peak experience,” which allows them to gain a better understanding of the trauma underlying their mental health problems.
Dr. Nutt said that in the United Kingdom, they haven’t seen adverse reactions in patients receiving psychedelic therapy, although sedatives such as benzodiazepines could be used to manage them. He added that at his center, two therapists are present at every treatment session, and all personnel are “trained medics or psychologists.”
Patient education
Preparing and educating patients about the therapy are critical, said Dr. Gründer, especially given the intense response psychedelic treatment often invokes.
Echoing Dr. Gründer, Dr. Tófoli said explaining the nature of psychedelic treatment to potential patients helps ease anxiety.
Dr. Griffiths noted that in the United States, study participants are not only educated about the potential effects of psychedelic agents but also undergo several hours of psychological preparation in advance of their first treatment session and are provided with psychological support after treatment.
There is also a strong emphasis on patient preparation and education in the United Kingdom, where patients meet with therapists before and after treatment. During these posttreatment debriefings, clinicians use the patients’ experience with psychedelics to help them gain insight into the underlying cause of their depression.
Dr. Schenberg noted that at his institution in São Paulo, there are online courses to teach clinicians about psychedelic therapy for psychiatric disorders. Next year, he added, a new training program in MDMA-assisted psychotherapy will begin.
Working out treatment protocols
Treatment protocols for psychedelics vary by agent and indication from country to country. For instance, Dr. Pani noted that current psychedelic research in Italy predominantly focuses more on microdosing, which involves administering 1% of the pharmacologically active dose to a maximum of 100 mcg, in contrast to low dosing or full dosing.
Therapeutic regimens in Brazil, said Dr. Schenberg, also differ by agent but share common elements. For instance, psychedelics are always administered in a research setting, and sessions include concomitant psychotherapy.
In Germany, investigators are working to determine optimal treatment regimen for psilocybin for resistant depression in a randomized three-arm study planned for 2021.
For Mexico’s Dr. Velásquez, treatment regimens are complex and varied. Either way, he said, patients always require long-term follow-up.
With ketamine therapy, Dr. Ferreri said his team administers the drug in 45- to 60-minute intravenous infusion sessions in a hospital room without light or sound stimulation. Regardless of the drug’s immediate effect, he said, the protocol is repeated within a 6-month period.
The question of the duration of treatment effect is important. Dr. Griffiths said research suggests that the positive effects of psilocybin are long lasting and that most individuals report positive changes in mood, attitude, and behavior that endure for months or even years after the session.
“Our research has shown that the benefits of these experiences can last as long as 14 months, often longer, and that many participants characterize their psilocybin experience as among the most profound and personally meaningful experiences of their lives,” said Dr. Griffiths.
Dr. Nutt agreed, noting that a single intense “trip” can improve mood for weeks, months, or even years. Nevertheless, he said, in his experience, approximately three-quarters of patients treated with psychedelics for major depression relapse within 3-9 months.
“Most get better,” he said, “but the majority of depression comes back over a period of months.”
Given the current illegal status of the drugs, he said it’s nearly impossible to provide patients with regular, subsequent treatment with psychedelics over time.
“My suspicion is that you might well have to dose four or five times over a couple of years to get people to escape from very severe depression,” said Dr. Nutt. “The longer they’ve been depressed, the harder it is for them to make a full recovery, because it’s more entrenched in the brain.”
All experts agree that exciting times are ahead for psychedelics as therapeutics for a wide range of psychiatric disorders.
“We can look forward to continued growth and expansion of this research,” said Dr. Griffiths, “including the refinement of protocols for a variety of therapeutic indications and to the development of a variety of new classic psychedelic compounds.”
A version of this article first appeared on Medscape.com.
In 1967, when the United Nations Convention on Drugs classified psychedelics as schedule I substances, it effectively ended research into these agents as potential therapeutics for psychiatric disorders.
Psychedelics induce altered states of perception. They bind to the 5-hydroxytryptamine 2A (5-HT2A) receptor and include psilocybin, which is derived from “magic mushrooms”; N,N-dimethyltryptamine (DMT), a component of ayahuasca and mescaline (peyote cactus); and the synthesized compound D-lysergic acid diethylamide (LSD). Other agents, such as ketamine and 3,4-methylenedioxymethamphetamine (MDMA), also known as ecstasy, are sometimes considered psychedelics as well.
Before they were classified as schedule I agents, psychedelics had been shown to be particularly beneficial for patients with treatment-resistant conditions, including depression and posttraumatic stress disorder (PTSD), especially when administered in a supportive, therapeutic setting.
Now, after a hiatus of almost 50 years, there is renewed global interest in the scientific investigation of psychedelics. The attention was spurred in part by several exploratory studies of DMT in humans conducted in the 1990s by Rick Strassman, MD, and colleagues at the University of New Mexico, Albuquerque.
Around the same time, Franz X. Vollenweider, MD, and colleagues at the University of Zürich began researching psilocybin and its effects on human behavior. However, it was a 2006 study of psilocybin by a team of researchers at Johns Hopkins University, Baltimore, that is widely cited as a catalyst for the current renaissance in psychedelic research.
To provide a broad-based, international perspective on these agents, including their current legal status and indications, treatment regimens, safety, efficacy, and future considerations, this news organization interviewed nine expert researchers from around the globe.
Global legal status
In most, if not all, countries, it is still illegal to prescribe psychedelics in other than a research setting.
They can be used in research, but only with approval from the Food and Drug Administration under licensure from the Drug Enforcement Administration.
France lists all synthetic hallucinogens and hallucinogenic mushrooms as narcotic. As a result, possession, use, transportation, and collection are subject to criminal sanctions.
In France, NMDA antagonists such as ketamine and nitrous oxide are regarded as psychedelic molecules and can be used off label for various conditions or as part of research protocols authorized by the French public health code.
Although psychedelics are illegal under Mexican law, they are commonly used in indigenous communities as part of traditional rituals.
“The line between traditional consumption and psychedelic tourism is very thin,” José J. Mendoza Velásquez, MD, professor in the department of mental health, National Autonomous University of Mexico, Mexico City, said in an interview.
Psychedelics also are illegal in the United Kingdom, although government agencies have recently allowed research groups to investigate them. Psychedelics cannot be prescribed in Germany, Spain, or Italy. However, investigators in these countries can request permission from regulatory agencies to conduct research.
Brazil allows psychedelic substances to be researched, particularly ayahuasca, which has long traditional and religious roots in the country.
However, as in other countries, none of the classic psychedelics is regulated for therapeutic use in Brazil. It is widely expected that the Brazilian government will approve MDMA sometime in 2024 for use in the treatment of PTSD.
Potential indications
Psychedelics are currently under investigation as potential treatments for major depression, treatment-resistant depression, PTSD, pain management, and anorexia, among other conditions.
In France, Florian Ferreri, MD, PhD, at Hospital Saint-Antoine, Paris, is researching ketamine for treatment of patients with suicidal crisis/ideation and treatment-resistant depression.
In the United Kingdom, David Nutt, FMedSci, Edmond J. Safra Professor of Neuropsychopharmacology at Imperial College London, and his team have conducted studies of the use of psychedelics in conjunction with psychological support for patients with treatment-resistant depression, and they are currently exploring their use in the treatment of anorexia and various pain syndromes.
In Germany, Gerhard Gründer, MD, professor of psychiatry at the Central Institute of Mental Health, in Mannheim, noted that a study of psilocybin for treatment-resistant depression will launch sometime in 2021. In Italy, current research is focusing on MDMA and ketamine in the laboratory environment and in animal models for treating depression and drug abuse.
Researcher Helen Dolengevich-Segal, MD, a psychiatrist at Hospital Universitario del Henares, Madrid, noted that although research on esketamine for the treatment of severe depressive disorder with suicidal thoughts is underway, there is very limited published research from that country into the use of classic psychedelics for various psychiatric disorders, given their current illegal status.
Mexico’s Dr. Velásquez noted that although he is prohibited from prescribing psychedelics, he does have patients who take the drugs to augment medical treatment. For instance, he said, his patients frequently use psilocybin to help with severe depression, pain, and insomnia.
Environment is key
Most researchers agree that for psychedelics to be safe and effective, patient education and administration in a controlled environment by experienced clinicians are key to successful treatment.
Roland R. Griffiths, PhD, director of the Center for Psychedelic and Consciousness Research at Johns Hopkins, said that ongoing U.S. psilocybin research – primarily in major depressive disorder and psychological distress associated with life-threatening illness, drug addiction, anorexia nervosa, obsessive-compulsive disorder, and headache – generally includes one or two treatment sessions, each of which lasts 6-8 hours.
Such sessions typically involve oral administration of a moderately high dose of a psychedelic under what he characterizes as “psychologically supported conditions.”
For Dr. Griffiths, there are serious potential risks associated with the use of psilocybin and other psychedelics outside such environments.
“When taken in uncontrolled conditions, classic psychedelics can produce confusion and disorientation resulting in behavior dangerous to the participant and others, including life-threatening risk,” he said.
Dr. Gründer agreed.
“At the moment, I cannot imagine that you would go to the pharmacy with a prescription for psilocybin and get yourself a pill and then take it in a quiet little room,” he said. Dr. Dolengevich-Segal and Dr. Velásquez echoed these sentiments, noting the optimal location for administration is one that is quiet and secure and where patients feel safe.
Luís Fernando Tófoli, MD, PhD, professor of medical psychology and psychiatry at the University of Campinas, and Eduardo Schenberg, PhD, founder and CEO of Instituto Phaneros in São Paulo, Brazil, said more research is needed to determine the optimal therapeutic environment for individual agents.
“Most studies have a low number of participants (around 20 or 30), especially in neuroimaging, with high unblinding rates,” Dr. Schenberg said. “Therefore, novel methodological approaches are also necessary, as these substances do not easily fit into the traditional pharmacology epistemic model.”
Risks, abuse potential
The abuse potential of psychedelics is an ongoing concern for the public, researchers, and regulators, but the consensus among nearly all of these experts is that when administered by medical professionals in controlled settings, these drugs are associated with extremely low risk.
It is recreational use that presents an abuse concern, said Dr. Ferreri, but with the low doses used in psychiatry, the risk is “very limited or even nonexistent.”
Dr. Nutt said the abuse potential of psychedelics is so low that they can be used to treat addiction.
“Functionally, psychedelics are antiaddictive,” Dr. Nutt said. “The fact is, if you take them repeatedly, you develop tolerance, and the effect disappears. You can’t overcome it. But everyone believes they’re addictive because they’re scheduled drugs.”
Dr. Velásquez is something of an outlier. He believes the abuse potential with psychedelics is poorly understood and that some patients may develop tolerance, which is a potential gateway to dependence.
“Such is the case with LSD,” he said, “where this substance also favors tolerance to other psychedelic drugs such as psilocybin.”
Dosing also seems to play a key role in mitigating potential abuse, said Luca Pani, MD, professor of pharmacology and psychiatry at the University of Modena, Italy. Dr. Pani explained that with low doses and microdoses of psychedelics, the potential for abuse is eliminated.
Dr. Nutt, Dr. Pani, and Dr. Ferreri also noted the importance of medical supervision. For instance, said Dr. Ferreri, when administering ketamine, his team closely monitors both mental and physical parameters – heart rate and blood pressure, in particular – because the drug can have hypertensive effects.
Dr. Schenberg noted that ibogaine, a naturally occurring psychedelic frequently used by traditional communities in Africa in rituals and for healing purposes, could cause potentially fatal arrhythmias, so it’s critical that the treatment is administered in a hospital setting that has a cardiac unit.
Dr. Pani said there is a need for more research, especially regarding the molecular mechanisms behind the behavioral effects of low-dose psychedelic therapy and the potential risks of multiple treatments with the drugs.
“Although extensive toxicology has been conducted on a single active dose of psilocybin, which has been proven to be safe, further research is required to understand better the possible health risks, especially in relation to cardiac and lung tissue,” he said.
Psychologically challenging
The experts note that given the relative lack of experience with psychedelic therapy, preparing patients for potential adverse effects is paramount. This is particularly relevant in the research setting and highlights the need for adequate patient screening and aftercare.
Dr. Gründer and Dr. Dolengevich-Segal emphasized the importance of having qualified personnel available in the event that patients experience adverse psychological events during treatment.
For Dr. Gründer, the potential for psilocybin to cause patients to lose control, experience psychotic symptoms, or become paranoid warrants considerable preparation by treating physicians.
Patients occasionally experience fear and anxiety during treatment, though it’s usually short-lived, said Dr. Griffiths. Nevertheless, these experiences may open the door to greater insight. “A number of people report that these psychologically challenging states are a valuable part of the overall experience,” he said.
The situation is similar in Spain, where Dr. Dolengevich-Segal noted that typical treatment regimens have a strong focus on the patient’s experience as a therapeutic tool. As in the United Kingdom and the United States, her team guides patients to what they call a “peak experience,” which allows them to gain a better understanding of the trauma underlying their mental health problems.
Dr. Nutt said that in the United Kingdom, they haven’t seen adverse reactions in patients receiving psychedelic therapy, although sedatives such as benzodiazepines could be used to manage them. He added that at his center, two therapists are present at every treatment session, and all personnel are “trained medics or psychologists.”
Patient education
Preparing and educating patients about the therapy are critical, said Dr. Gründer, especially given the intense response psychedelic treatment often invokes.
Echoing Dr. Gründer, Dr. Tófoli said explaining the nature of psychedelic treatment to potential patients helps ease anxiety.
Dr. Griffiths noted that in the United States, study participants are not only educated about the potential effects of psychedelic agents but also undergo several hours of psychological preparation in advance of their first treatment session and are provided with psychological support after treatment.
There is also a strong emphasis on patient preparation and education in the United Kingdom, where patients meet with therapists before and after treatment. During these posttreatment debriefings, clinicians use the patients’ experience with psychedelics to help them gain insight into the underlying cause of their depression.
Dr. Schenberg noted that at his institution in São Paulo, there are online courses to teach clinicians about psychedelic therapy for psychiatric disorders. Next year, he added, a new training program in MDMA-assisted psychotherapy will begin.
Working out treatment protocols
Treatment protocols for psychedelics vary by agent and indication from country to country. For instance, Dr. Pani noted that current psychedelic research in Italy predominantly focuses more on microdosing, which involves administering 1% of the pharmacologically active dose to a maximum of 100 mcg, in contrast to low dosing or full dosing.
Therapeutic regimens in Brazil, said Dr. Schenberg, also differ by agent but share common elements. For instance, psychedelics are always administered in a research setting, and sessions include concomitant psychotherapy.
In Germany, investigators are working to determine optimal treatment regimen for psilocybin for resistant depression in a randomized three-arm study planned for 2021.
For Mexico’s Dr. Velásquez, treatment regimens are complex and varied. Either way, he said, patients always require long-term follow-up.
With ketamine therapy, Dr. Ferreri said his team administers the drug in 45- to 60-minute intravenous infusion sessions in a hospital room without light or sound stimulation. Regardless of the drug’s immediate effect, he said, the protocol is repeated within a 6-month period.
The question of the duration of treatment effect is important. Dr. Griffiths said research suggests that the positive effects of psilocybin are long lasting and that most individuals report positive changes in mood, attitude, and behavior that endure for months or even years after the session.
“Our research has shown that the benefits of these experiences can last as long as 14 months, often longer, and that many participants characterize their psilocybin experience as among the most profound and personally meaningful experiences of their lives,” said Dr. Griffiths.
Dr. Nutt agreed, noting that a single intense “trip” can improve mood for weeks, months, or even years. Nevertheless, he said, in his experience, approximately three-quarters of patients treated with psychedelics for major depression relapse within 3-9 months.
“Most get better,” he said, “but the majority of depression comes back over a period of months.”
Given the current illegal status of the drugs, he said it’s nearly impossible to provide patients with regular, subsequent treatment with psychedelics over time.
“My suspicion is that you might well have to dose four or five times over a couple of years to get people to escape from very severe depression,” said Dr. Nutt. “The longer they’ve been depressed, the harder it is for them to make a full recovery, because it’s more entrenched in the brain.”
All experts agree that exciting times are ahead for psychedelics as therapeutics for a wide range of psychiatric disorders.
“We can look forward to continued growth and expansion of this research,” said Dr. Griffiths, “including the refinement of protocols for a variety of therapeutic indications and to the development of a variety of new classic psychedelic compounds.”
A version of this article first appeared on Medscape.com.
Buprenorphine for OUD may also mitigate risk with concomitant benzo, Z-drug use
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Buprenorphine for the treatment of opioid-use disorder (OUD) may also mitigate the risk associated with concomitant benzodiazepine and Z-drug use, which is frequent in this patient population, new research suggests.
A case-crossover study of more than 20,000 participants with OUD showed that drug treatment days in which benzodiazepines and Z-drugs were taken were associated with an 88% increase in nonfatal overdose; buprenorphine appeared to reduce this risk by almost 40%.
“One of our two primary findings is that patients with opioid use disorder can still benefit substantially from buprenorphine treatment, even if they have benzodiazepines on board,” lead author Kevin Xu, MD, a resident at the Washington University, St. Louis, told this news organization.
The other key finding was that “not all benzodiazepines are equal” and that some are associated with higher risk than others, Dr. Xu added.
“If anything, patients who are on buprenorphine and benzodiazepines do not necessarily need to be abruptly tapered off their benzodiazepines. Our data actually demonstrate that there are safe avenues for them,” he added.
The findings were published online March 3 in the American Journal of Psychiatry.
Cloudy relationship
Buprenorphine is commonly used to treat patients with OUD because of its ability to decrease all-cause mortality. However,
In addition, recent research shows that benzodiazepine/Z-drug use is associated with a variety of potential adverse effects, including respiratory depression, overdose, and addiction risk.
The relationship between benzodiazepine use and buprenorphine treatment outcomes is poorly characterized in individuals with OUD. Although some studies suggest benzodiazepines may enhance retention in buprenorphine maintenance treatment, others suggest a link to increased adverse events, including all-cause mortality, drug-related poisonings, and accidental injury–related emergency department visits.
In addition, there has been little research on the potential adverse effects associated with use of selective benzodiazepine receptor modulators in patients with OUD. These so-called Z-drugs include zolpidem, zaleplon, and eszopiclone.
Nevertheless, previous research in the general population shows that these medications have a range of adverse effects similar to those of benzodiazepines, with comparable dose-response effects on all-cause mortality.
“The challenge for any clinician is that many patients who are addicted to opioids are also polysubstance users,” said Dr. Xu. “There are so many hopeful articles regarding the benefits of buprenorphine treatment in opioid use disorder patients, but it seems like the individuals with polysubstance use are largely ignored in the setting of the opioid epidemic.”
“And this is really the back story that got me inspired to study this particular topic,” he added.
Improve, nullify, or reverse?
Given these questions, the researchers set out to quantify the odds of nonfatal drug-related poisoning, including overdoses, associated with benzodiazepine or Z-drug use by patients with OUD who were also taking buprenorphine.
“While the drug-related poisoning variable encompasses opioid overdoses, we used a broad definition per CDC guidelines to also include other types of drug overdoses – including poisoning events involving stimulants, overdoses involving sedatives, and overdoses involving psychotropic prescription drugs” that are commonly used by patients with OUD, said Dr. Xu.
They also wanted to determine whether the use of benzodiazepines or Z-drugs would improve, nullify, or reverse the protective effect of buprenorphine. The researchers also evaluated whether different sedative and hypnotic subtypes of these drugs were associated with different poisoning risks.
The researchers analyzed pharmaceutical claims data from 304,676 individuals (aged 12-64 years) in the IBM MarketScan Commercial and Multi-State Medicaid Databases. All had received buprenorphine treatment for OUD between Jan. 1, 2006, and Dec. 31, 2016.
Buprenorphine use was converted to a daily milligram dose and was classified as either greater than 12 mg or less than or equal to 12 mg, because previous research suggests there may be differences in treatment retention associated with this dose. Given the case-control nature of the investigation, patients who did not experience a drug-related poisoning were excluded from the analysis.
The study’s primary unit of observation was person-days, which were those days during which patients were enrolled in a health insurance plan. Participants were evaluated for 1 year before their first drug-related poisoning and 1 year after their first such poisoning. The primary outcome was nonfatal drug-related poisonings, including overdoses. The primary exposure was determined on the basis of benzodiazepine or Z-drug prescriptions.
The daily dose of benzodiazepines or Z-drugs was standardized as a function of diazepam-equivalent milligrams. Doses were classified as either high dose (diazepam-equivalent mg dose >30 mg) or low dose (≤30 mg). The drugs were also distinguished on the basis of their pharmacologic properties, such as whether they were short-acting or long-acting.
37% risk reduction
Of the original cohort of 304,676 patients with OUD, the study’s final analytic sample included 23,036 patients (mean age, 30 years; 51% men), representing 14,213,075 person-days of insurance coverage. Of these, 2,210,927 person-days (15.6%) entailed claims for buprenorphine (mean daily dose, 15.4 mg; SD, 7.31 mg).
A total of 474,181 person-days included claims for benzodiazepines or Z-drugs with concurrent buprenorphine treatment. The mean daily dose of any benzodiazepine or Z-drug was 23.4 diazepam-milligram equivalents. The mean daily dose of short-acting benzodiazepines, long-acting benzodiazepines, and Z-drugs was 25.3, 31.3, and 4.9 diazepam-milligram equivalents, respectively.
Buprenorphine treatment days were associated with a 37% lower chance of drug-related poisoning (95% confidence interval, 0.60-0.66) in comparison with nontreatment days. On the other hand, the odds of poisoning increased by 81% on days on which patients were treated with Z-drugs or benzodiazepines (95% CI, 1.73-1.91).
Interestingly, individual analyses showed that benzodiazepine and Z-drug treatment days were associated with increased odds of poisoning events (odds ratio, 1.29; 95% CI, 1.19-1.39). Odds of poisoning events on benzodiazepine-only treatment days, on the other hand, were markedly lower (OR, 1.88; 95% CI, 1.78-1.98).
Subgroup analyses revealed that both short-acting and long-acting benzodiazepine treatment days were associated with comparably elevated odds of drug-related poisoning (OR, 1.86 and 1.68, respectively). High-dose benzodiazepine treatment days were associated with higher increased odds of a poisoning event (122%) in comparison with low-dose treatment days (78%).
High-dose, but not low-dose, benzodiazepine or Z-drug treatment was linked to increased poisonings when the drug was taken concurrently with buprenorphine (OR, 1.64; 95% CI, 1.39-1.93). However, the risk was still lower than the risk associated with taking the agents without concurrent treatment with buprenorphine (low-dose OR, 1.69; high-dose OR, 2.23).
‘Not all benzodiazepines are bad’
Dr. Xu noted that the findings have potentially important implications for clinical practice, beginning with the dose-dependent relationship between benzodiazepine/Z-drug use and drug-related poisonings among individuals with OUD. This indicates that lowering doses or shortening treatment duration may reduce risk, he said.
Similarly, the lower risk associated with long-acting benzodiazepines relative to short-acting beonzodiazepines – as well as the substantially lower risk associated with Z-drugs, compared with either short- or long-acting benzodiazepines – suggests that switching from benzodiazepines to long-acting agents or Z-drugs may lower the risk for overdose, he added.
“Clinicians are often challenged by patients with opioid use disorder who are also on benzodiazepines or Z-drugs. There’s an inclination to say no to them, because they’re too high risk to start buprenorphine maintenance, or abruptly taper the benzodiazepines, which can be very destabilizing,” he noted.
“Our data show that people on benzodiazepines can absolutely receive buprenorphine and still get some benefit,” Dr. Xu said. “In addition, not all benzodiazepines are bad for these individuals. There are safer formulations and safer doses, too.”
However, he added, he would not initiate benzodiazepine treatment if he didn’t have to, especially long-term treatment.
“One of the messages from our data is that this clearly contributes to higher overdose risk. But we often inherit patients who already have benzodiazepines on board, so we need to figure out what to do. That is the question that nobody had really clearly addressed prior to this study,” Dr. Xu concluded.
Vigilance needed
Commenting on the findings for this news organization, Jerrold F. Rosenbaum, MD, Stanley Cobb Professor of Psychiatry, Harvard Medical School, Boston, urged caution when combining benzodiazepines with opioids.
“There are situations where you need to be circumspect about the use of benzodiazepines, and that’s clearly when people are being prescribed them in combination with other drugs that could be either sedating or respiratory depressant,” said Dr. Rosenbaum, who was not involved with the research.
“This paper reminds us that physicians need to be particularly vigilant about situations where patients might be combining the two agents,” he added.
Dr. Rosenbaum noted that patients who are using more medication than prescribed are at risk “for not appreciating the synergy” between the two treatments in terms of adverse events such as respiratory depression.
In addition, “if they’re intending to do themselves harm, the lethality of an overdose will be certainly far more than the benzodiazepines or opiates alone,” he said.
Another potential challenge for clinicians are situations in which patients are taking benzodiazepines for preexisting conditions that also require opiates. “Then you have to use special vigilance and try to use lowest doses to reduce the total burden of medication to minimize the potential risk,” said Dr. Rosenbaum.
The study was funded by the National Institutes of Health. Dr. Xu has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FIT unfit for inpatient, emergency settings
Most fecal immunochemical tests (FIT) in the hospital setting or the ED are performed for inappropriate indications, according to new data.
“This is the largest study that focuses exclusively on the use of FIT in the ED, inpatient wards, and in the ICU, and it shows significant misuse,” said investigator Umer Bhatti, MD, from Indiana University, Indianapolis.
The only “validated indication” for FIT is to screen for colorectal cancer. However, “99.5% of the FIT tests done in our study were for inappropriate indications,” he reported at the annual meeting of the American College of Gastroenterology, where the study was honored with an ACG Presidential Poster Award.
And the inappropriate use of FIT in these settings had no positive effect on clinical decision-making, he added.
For their study, Dr. Bhatti and colleagues looked at all instances of FIT use in their hospital’s electronic medical records from November 2017 to October 2019 to assess how often FIT was being used, the indications for which it was being used, and the impact of its use on clinical care.
They identified 550 patients, 48% of whom were women, who underwent at least one FIT test. Mean age of the study cohort was 54 years. Only three of the tests, or 0.5%, were performed to screen for colorectal cancer (95% confidence interval, 0.09%-1.52%).
Among the indications documented for FIT were anemia in 242 (44.0%) patients, suspected GI bleeding in 225 (40.9%), abdominal pain in 31 (5.6%), and change in bowel habits in 19 (3.5%).
The tests were performed most often in the ED (45.3%) and on the hospital floor (42.2%), but were also performed in the ICU (10.5%) and burn unit (2.0%).
Overall, 297 of the tests, or 54%, were negative, and 253, or 46%, were positive.
“GI consults were obtained in 46.2% of the FIT-positive group, compared with 13.1% of the FIT-negative patients” (odds ratio, 5.93; 95% CI, 3.88-9.04, P < .0001), Dr. Bhatti reported.
Among FIT-positive patients, those with overt bleeding were more likely to receive a GI consultation than those without (OR, 3.3; 95% CI, 1.9-5.5; P < .0001).
Of the 117 FIT-positive patients who underwent a GI consultation, upper endoscopy was a more common outcome than colonoscopy (51.3% vs. 23.1%; P < .0001). Of the 34 patients who underwent colonoscopy or sigmoidoscopy, one was diagnosed with colorectal cancer and one with advanced adenoma.
Overt GI bleeding was a better predictor of a GI consultation than a positive FIT result. In fact, use of FIT for patients with overt GI bleeding indicates a poor understanding of the test’s utility, the investigators reported.
“For patients with overt GI bleeding, having a positive FIT made no difference on how often a bleeding source was identified on endoscopy, suggesting that FIT should not be used to guide decisions about endoscopy or hospitalization,” Dr. Bhatti said.
In light of these findings, the team urges their peers to consider measures to reduce FIT tests for unnecessary indications.
“We feel that FIT is unfit for use in the inpatient and emergency settings, and measures should be taken to curb its use,” Dr. Bhatti concluded. “We presented our data to our hospital leadership and a decision was made to remove the FIT as an orderable test from the EMR.”
These results are “striking,” said Jennifer Christie, MD, from the University, Atlanta.
“We should be educating our ER providers and inpatient providers about the proper use of FIT,” she said in an interview. “Another option – and this has been done in many settings with the fecal occult blood test – is just take FIT off the units or out of the ER, so providers won’t be tempted to use it as an assessment of these patients. Because often times, as this study showed, it doesn’t really impact outcomes.”
In fact, unnecessary FI testing could put patients at risk for unnecessary procedures. “We also know that calling for an inpatient or ER consult from a gastroenterologist may increase both length of stay and costs,” she added.
Dr. Bhatti and Dr. Christie disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Most fecal immunochemical tests (FIT) in the hospital setting or the ED are performed for inappropriate indications, according to new data.
“This is the largest study that focuses exclusively on the use of FIT in the ED, inpatient wards, and in the ICU, and it shows significant misuse,” said investigator Umer Bhatti, MD, from Indiana University, Indianapolis.
The only “validated indication” for FIT is to screen for colorectal cancer. However, “99.5% of the FIT tests done in our study were for inappropriate indications,” he reported at the annual meeting of the American College of Gastroenterology, where the study was honored with an ACG Presidential Poster Award.
And the inappropriate use of FIT in these settings had no positive effect on clinical decision-making, he added.
For their study, Dr. Bhatti and colleagues looked at all instances of FIT use in their hospital’s electronic medical records from November 2017 to October 2019 to assess how often FIT was being used, the indications for which it was being used, and the impact of its use on clinical care.
They identified 550 patients, 48% of whom were women, who underwent at least one FIT test. Mean age of the study cohort was 54 years. Only three of the tests, or 0.5%, were performed to screen for colorectal cancer (95% confidence interval, 0.09%-1.52%).
Among the indications documented for FIT were anemia in 242 (44.0%) patients, suspected GI bleeding in 225 (40.9%), abdominal pain in 31 (5.6%), and change in bowel habits in 19 (3.5%).
The tests were performed most often in the ED (45.3%) and on the hospital floor (42.2%), but were also performed in the ICU (10.5%) and burn unit (2.0%).
Overall, 297 of the tests, or 54%, were negative, and 253, or 46%, were positive.
“GI consults were obtained in 46.2% of the FIT-positive group, compared with 13.1% of the FIT-negative patients” (odds ratio, 5.93; 95% CI, 3.88-9.04, P < .0001), Dr. Bhatti reported.
Among FIT-positive patients, those with overt bleeding were more likely to receive a GI consultation than those without (OR, 3.3; 95% CI, 1.9-5.5; P < .0001).
Of the 117 FIT-positive patients who underwent a GI consultation, upper endoscopy was a more common outcome than colonoscopy (51.3% vs. 23.1%; P < .0001). Of the 34 patients who underwent colonoscopy or sigmoidoscopy, one was diagnosed with colorectal cancer and one with advanced adenoma.
Overt GI bleeding was a better predictor of a GI consultation than a positive FIT result. In fact, use of FIT for patients with overt GI bleeding indicates a poor understanding of the test’s utility, the investigators reported.
“For patients with overt GI bleeding, having a positive FIT made no difference on how often a bleeding source was identified on endoscopy, suggesting that FIT should not be used to guide decisions about endoscopy or hospitalization,” Dr. Bhatti said.
In light of these findings, the team urges their peers to consider measures to reduce FIT tests for unnecessary indications.
“We feel that FIT is unfit for use in the inpatient and emergency settings, and measures should be taken to curb its use,” Dr. Bhatti concluded. “We presented our data to our hospital leadership and a decision was made to remove the FIT as an orderable test from the EMR.”
These results are “striking,” said Jennifer Christie, MD, from the University, Atlanta.
“We should be educating our ER providers and inpatient providers about the proper use of FIT,” she said in an interview. “Another option – and this has been done in many settings with the fecal occult blood test – is just take FIT off the units or out of the ER, so providers won’t be tempted to use it as an assessment of these patients. Because often times, as this study showed, it doesn’t really impact outcomes.”
In fact, unnecessary FI testing could put patients at risk for unnecessary procedures. “We also know that calling for an inpatient or ER consult from a gastroenterologist may increase both length of stay and costs,” she added.
Dr. Bhatti and Dr. Christie disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Most fecal immunochemical tests (FIT) in the hospital setting or the ED are performed for inappropriate indications, according to new data.
“This is the largest study that focuses exclusively on the use of FIT in the ED, inpatient wards, and in the ICU, and it shows significant misuse,” said investigator Umer Bhatti, MD, from Indiana University, Indianapolis.
The only “validated indication” for FIT is to screen for colorectal cancer. However, “99.5% of the FIT tests done in our study were for inappropriate indications,” he reported at the annual meeting of the American College of Gastroenterology, where the study was honored with an ACG Presidential Poster Award.
And the inappropriate use of FIT in these settings had no positive effect on clinical decision-making, he added.
For their study, Dr. Bhatti and colleagues looked at all instances of FIT use in their hospital’s electronic medical records from November 2017 to October 2019 to assess how often FIT was being used, the indications for which it was being used, and the impact of its use on clinical care.
They identified 550 patients, 48% of whom were women, who underwent at least one FIT test. Mean age of the study cohort was 54 years. Only three of the tests, or 0.5%, were performed to screen for colorectal cancer (95% confidence interval, 0.09%-1.52%).
Among the indications documented for FIT were anemia in 242 (44.0%) patients, suspected GI bleeding in 225 (40.9%), abdominal pain in 31 (5.6%), and change in bowel habits in 19 (3.5%).
The tests were performed most often in the ED (45.3%) and on the hospital floor (42.2%), but were also performed in the ICU (10.5%) and burn unit (2.0%).
Overall, 297 of the tests, or 54%, were negative, and 253, or 46%, were positive.
“GI consults were obtained in 46.2% of the FIT-positive group, compared with 13.1% of the FIT-negative patients” (odds ratio, 5.93; 95% CI, 3.88-9.04, P < .0001), Dr. Bhatti reported.
Among FIT-positive patients, those with overt bleeding were more likely to receive a GI consultation than those without (OR, 3.3; 95% CI, 1.9-5.5; P < .0001).
Of the 117 FIT-positive patients who underwent a GI consultation, upper endoscopy was a more common outcome than colonoscopy (51.3% vs. 23.1%; P < .0001). Of the 34 patients who underwent colonoscopy or sigmoidoscopy, one was diagnosed with colorectal cancer and one with advanced adenoma.
Overt GI bleeding was a better predictor of a GI consultation than a positive FIT result. In fact, use of FIT for patients with overt GI bleeding indicates a poor understanding of the test’s utility, the investigators reported.
“For patients with overt GI bleeding, having a positive FIT made no difference on how often a bleeding source was identified on endoscopy, suggesting that FIT should not be used to guide decisions about endoscopy or hospitalization,” Dr. Bhatti said.
In light of these findings, the team urges their peers to consider measures to reduce FIT tests for unnecessary indications.
“We feel that FIT is unfit for use in the inpatient and emergency settings, and measures should be taken to curb its use,” Dr. Bhatti concluded. “We presented our data to our hospital leadership and a decision was made to remove the FIT as an orderable test from the EMR.”
These results are “striking,” said Jennifer Christie, MD, from the University, Atlanta.
“We should be educating our ER providers and inpatient providers about the proper use of FIT,” she said in an interview. “Another option – and this has been done in many settings with the fecal occult blood test – is just take FIT off the units or out of the ER, so providers won’t be tempted to use it as an assessment of these patients. Because often times, as this study showed, it doesn’t really impact outcomes.”
In fact, unnecessary FI testing could put patients at risk for unnecessary procedures. “We also know that calling for an inpatient or ER consult from a gastroenterologist may increase both length of stay and costs,” she added.
Dr. Bhatti and Dr. Christie disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Probiotic blend may help patients with GI symptoms
A novel five-strain probiotic blend could provide relief for patients with functional GI disorders, a new study shows.
The combination “improved patient’s functional GI symptoms and displayed a favorable safety profile,” said lead study investigator Lucinda A. Harris, MD, MS, from the Mayo Clinic School of Medicine in Scottsdale, Ariz.
“Results of this study are promising, and additional studies would support the novel probiotic blend’s efficacy, safety, and durability of effect,” said Dr. Harris during her presentation at the virtual American College of Gastroenterology 2020 Annual Scientific Meeting.
Treatment with probiotics, such as Bifidobacterium lactis strains Bl-04, Bi-07, and HN019 and Lactobacillus strains L. acidophilus NCFM and L. paracasei Lpc-37 – administered alone or in multistrain blends – has been shown to improve diarrhea, abdominal pain, bloating, and constipation symptoms in patients with GI disturbances, she reported.
“Multiple pathophysiologic processes may cause functional GI symptoms, including altered gut microbiota,” she said. “The administration of probiotics can impact intestinal microbial balance, thereby contributing to improvement in functional GI symptoms.”
In their study, Dr. Harris and her colleagues evaluated the safety and efficacy of a five-strain probiotic blend – composed of Bl-04, Bi-07, HN019, NCFM, and Lpc-37 – in people with functional GI disturbances.
In the open-label, multicenter study, all 188 adult participants (mean age, 44.1 years; 72.3% female) demonstrated symptoms of functional GI disturbances. Each received an oral capsule of the probiotic blend once daily for 30 days.
Patients were assessed at multiple time points: screening (days –15 to –1), baseline (day 1), day 14, day 30, and a follow-up visit (day 42). The study’s primary efficacy endpoint was patient-reported improvement in overall GI well-being at day 30. Secondary outcomes included changes in GI symptoms, assessed with the 11-point GI Health Symptom Questionnaire. The incidence of treatment-emergent adverse events was assessed during all patient visits.
By day 30, 85.1% of patients had achieved the primary endpoint and indicated a positive response when asked about their overall GI well-being. All of the improvements reported at day 30 were generally observed at day 14 as well.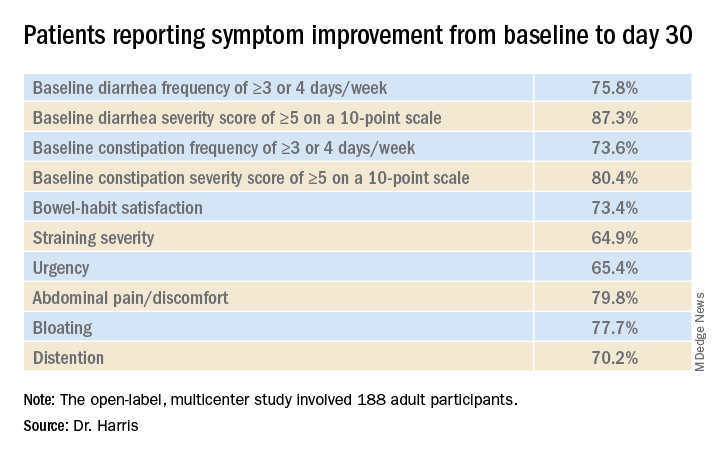
“In addition, we observed a mean decrease in I-FABP [intestinal fatty-acid binding protein] of 32.7% in patients with the highest quartile of baseline I-FABP levels,” Dr. Harris reported.
With respect to tolerability, adverse events were reported by 18.6% of participants and treatment-related adverse events were reported by 8.0%.
“Overall, 35 patients experienced a treatment-emergent adverse event,” she said. “Six patients experienced flatulence and five patients had a cough.” There were no deaths, no serious treatment-emergent adverse events, and no drug-related discontinuations
Placebo effect?
“We know that the biome has a role in modulating a number of physiologic processes, so looking at biomic influence for functional disease makes sense,” said David A. Johnson, MD, from the Eastern Virginia Medical School in Norfolk, who was not involved in the study.
However, one of the limitations of this study is the potential for a marked placebo effect, he said in an interview. “When you do an open-label trial in functional diseases, there’s a high placebo rate response. This effect is less pronounced in longer trials, but shorter trials like this one definitely carry the risk of increased placebo responses.”
“Although promising, a randomized control trial evaluating the microbiome as a response to the treatment intervention would be extremely helpful in defining the true role of effect,” he added.
This study was funded by Bausch Health Americas, Inc. Harris reports financial relationships with Allergan, Ironwood, and Takeda. Johnson has disclosed no relevant financial relationships; he writes the Johnson on Gastroenterology blog on Medscape.
A version of this article originally appeared on Medscape.com.
A novel five-strain probiotic blend could provide relief for patients with functional GI disorders, a new study shows.
The combination “improved patient’s functional GI symptoms and displayed a favorable safety profile,” said lead study investigator Lucinda A. Harris, MD, MS, from the Mayo Clinic School of Medicine in Scottsdale, Ariz.
“Results of this study are promising, and additional studies would support the novel probiotic blend’s efficacy, safety, and durability of effect,” said Dr. Harris during her presentation at the virtual American College of Gastroenterology 2020 Annual Scientific Meeting.
Treatment with probiotics, such as Bifidobacterium lactis strains Bl-04, Bi-07, and HN019 and Lactobacillus strains L. acidophilus NCFM and L. paracasei Lpc-37 – administered alone or in multistrain blends – has been shown to improve diarrhea, abdominal pain, bloating, and constipation symptoms in patients with GI disturbances, she reported.
“Multiple pathophysiologic processes may cause functional GI symptoms, including altered gut microbiota,” she said. “The administration of probiotics can impact intestinal microbial balance, thereby contributing to improvement in functional GI symptoms.”
In their study, Dr. Harris and her colleagues evaluated the safety and efficacy of a five-strain probiotic blend – composed of Bl-04, Bi-07, HN019, NCFM, and Lpc-37 – in people with functional GI disturbances.
In the open-label, multicenter study, all 188 adult participants (mean age, 44.1 years; 72.3% female) demonstrated symptoms of functional GI disturbances. Each received an oral capsule of the probiotic blend once daily for 30 days.
Patients were assessed at multiple time points: screening (days –15 to –1), baseline (day 1), day 14, day 30, and a follow-up visit (day 42). The study’s primary efficacy endpoint was patient-reported improvement in overall GI well-being at day 30. Secondary outcomes included changes in GI symptoms, assessed with the 11-point GI Health Symptom Questionnaire. The incidence of treatment-emergent adverse events was assessed during all patient visits.
By day 30, 85.1% of patients had achieved the primary endpoint and indicated a positive response when asked about their overall GI well-being. All of the improvements reported at day 30 were generally observed at day 14 as well.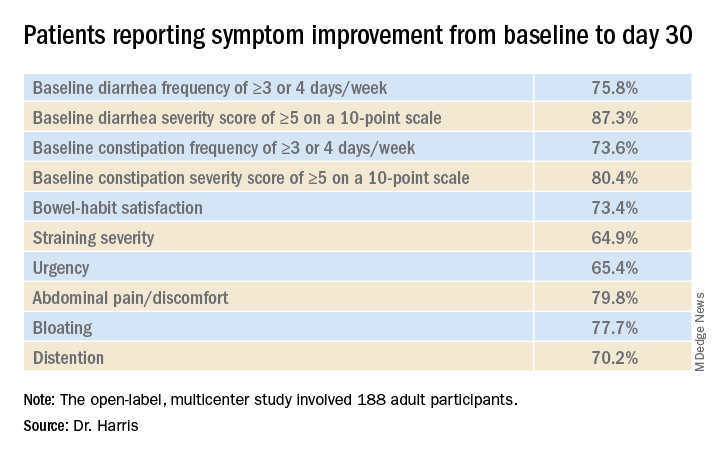
“In addition, we observed a mean decrease in I-FABP [intestinal fatty-acid binding protein] of 32.7% in patients with the highest quartile of baseline I-FABP levels,” Dr. Harris reported.
With respect to tolerability, adverse events were reported by 18.6% of participants and treatment-related adverse events were reported by 8.0%.
“Overall, 35 patients experienced a treatment-emergent adverse event,” she said. “Six patients experienced flatulence and five patients had a cough.” There were no deaths, no serious treatment-emergent adverse events, and no drug-related discontinuations
Placebo effect?
“We know that the biome has a role in modulating a number of physiologic processes, so looking at biomic influence for functional disease makes sense,” said David A. Johnson, MD, from the Eastern Virginia Medical School in Norfolk, who was not involved in the study.
However, one of the limitations of this study is the potential for a marked placebo effect, he said in an interview. “When you do an open-label trial in functional diseases, there’s a high placebo rate response. This effect is less pronounced in longer trials, but shorter trials like this one definitely carry the risk of increased placebo responses.”
“Although promising, a randomized control trial evaluating the microbiome as a response to the treatment intervention would be extremely helpful in defining the true role of effect,” he added.
This study was funded by Bausch Health Americas, Inc. Harris reports financial relationships with Allergan, Ironwood, and Takeda. Johnson has disclosed no relevant financial relationships; he writes the Johnson on Gastroenterology blog on Medscape.
A version of this article originally appeared on Medscape.com.
A novel five-strain probiotic blend could provide relief for patients with functional GI disorders, a new study shows.
The combination “improved patient’s functional GI symptoms and displayed a favorable safety profile,” said lead study investigator Lucinda A. Harris, MD, MS, from the Mayo Clinic School of Medicine in Scottsdale, Ariz.
“Results of this study are promising, and additional studies would support the novel probiotic blend’s efficacy, safety, and durability of effect,” said Dr. Harris during her presentation at the virtual American College of Gastroenterology 2020 Annual Scientific Meeting.
Treatment with probiotics, such as Bifidobacterium lactis strains Bl-04, Bi-07, and HN019 and Lactobacillus strains L. acidophilus NCFM and L. paracasei Lpc-37 – administered alone or in multistrain blends – has been shown to improve diarrhea, abdominal pain, bloating, and constipation symptoms in patients with GI disturbances, she reported.
“Multiple pathophysiologic processes may cause functional GI symptoms, including altered gut microbiota,” she said. “The administration of probiotics can impact intestinal microbial balance, thereby contributing to improvement in functional GI symptoms.”
In their study, Dr. Harris and her colleagues evaluated the safety and efficacy of a five-strain probiotic blend – composed of Bl-04, Bi-07, HN019, NCFM, and Lpc-37 – in people with functional GI disturbances.
In the open-label, multicenter study, all 188 adult participants (mean age, 44.1 years; 72.3% female) demonstrated symptoms of functional GI disturbances. Each received an oral capsule of the probiotic blend once daily for 30 days.
Patients were assessed at multiple time points: screening (days –15 to –1), baseline (day 1), day 14, day 30, and a follow-up visit (day 42). The study’s primary efficacy endpoint was patient-reported improvement in overall GI well-being at day 30. Secondary outcomes included changes in GI symptoms, assessed with the 11-point GI Health Symptom Questionnaire. The incidence of treatment-emergent adverse events was assessed during all patient visits.
By day 30, 85.1% of patients had achieved the primary endpoint and indicated a positive response when asked about their overall GI well-being. All of the improvements reported at day 30 were generally observed at day 14 as well.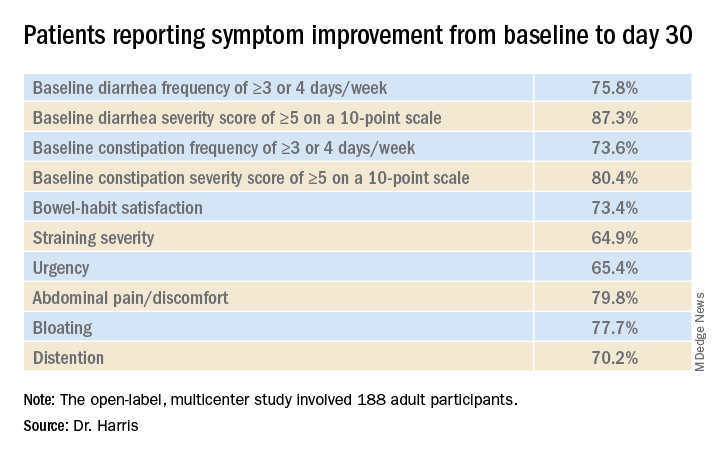
“In addition, we observed a mean decrease in I-FABP [intestinal fatty-acid binding protein] of 32.7% in patients with the highest quartile of baseline I-FABP levels,” Dr. Harris reported.
With respect to tolerability, adverse events were reported by 18.6% of participants and treatment-related adverse events were reported by 8.0%.
“Overall, 35 patients experienced a treatment-emergent adverse event,” she said. “Six patients experienced flatulence and five patients had a cough.” There were no deaths, no serious treatment-emergent adverse events, and no drug-related discontinuations
Placebo effect?
“We know that the biome has a role in modulating a number of physiologic processes, so looking at biomic influence for functional disease makes sense,” said David A. Johnson, MD, from the Eastern Virginia Medical School in Norfolk, who was not involved in the study.
However, one of the limitations of this study is the potential for a marked placebo effect, he said in an interview. “When you do an open-label trial in functional diseases, there’s a high placebo rate response. This effect is less pronounced in longer trials, but shorter trials like this one definitely carry the risk of increased placebo responses.”
“Although promising, a randomized control trial evaluating the microbiome as a response to the treatment intervention would be extremely helpful in defining the true role of effect,” he added.
This study was funded by Bausch Health Americas, Inc. Harris reports financial relationships with Allergan, Ironwood, and Takeda. Johnson has disclosed no relevant financial relationships; he writes the Johnson on Gastroenterology blog on Medscape.
A version of this article originally appeared on Medscape.com.
Tofacitinib retreatment effective for ulcerative colitis
Retreatment with tofacitinib after a period of treatment interruption was well tolerated and effective in patients with ulcerative colitis who had shown a previous response to tofacitinib induction, according to an analysis of data from the OCTAVE extension trial.
“Clinical response was recaptured in most patients by month 2, and about half of patients by month 36, irrespective of prior anti–[tumor necrosis factor] status,” said lead researcher Edward V. Loftus Jr, MD, from the Mayo Medical School, Rochester, Minn.
A temporary suspension of treatment with the oral, small-molecule Janus kinase (JAK) inhibitor might be necessary for a number of reasons, such as if a patient has to undergo surgery, experiences adverse events, or becomes pregnant.
For their study, Dr. Loftus and colleagues set out to assess the safety and efficacy of retreatment after a period of interruption.
“The population we’re interested in are patients who received tofacitinib during induction and placebo during maintenance” in the original OCTAVE trials, said Dr. Loftus. “They then either completed the trial or flared and rolled over to the open-label extension.”
The researchers looked at the 100 patients who had achieved a clinical response after 8 weeks of treatment with tofacitinib 10 mg twice-daily in the OCTAVE Induction 1 and OCTAVE Induction 2 trials and then received placebo in the OCTAVE Sustain trial and experienced treatment failure between week 8 and week 52. These patients went on to receive tofacitinib 10 mg twice daily as part of the ongoing, open-label, long-term extension OCTAVE Open trial.
Treatment failure was defined as an increase of at least 3 points from the baseline total Mayo score achieved in OCTAVE Sustain, plus an increase of at least 1 point in rectal bleeding and endoscopic subscores and an absolute endoscopic subscore of at least 2 points after at least 8 weeks of treatment. Efficacy was evaluated for up to 36 months in the open-label extension; adverse events were assessed throughout the study period.
The median time to treatment failure was 135 days, Dr. Loftus reported during his award-winning presentation at the virtual annual meeting of the American College of Gastroenterology.
On last observation carried forward (LOCF) analysis, or observed data, 85.2% of the patients had recaptured clinical response by month 2. That rate fell to 74.3% when the analysis was modified for nonresponder imputation (NRI).
“The truth lies somewhere in between,” Dr. Loftus said.
Of interest, a clinical response to tofacitinib retreatment at month 2 was achieved by 92.5% (observed data) and 80.4% (NRI-LOCF) of patients who experienced treatment failure after tumor necrosis factor inhibitor therapy.
“Many patients were able to regain response with tofacitinib and then maintain that over time,” said Dr. Loftus.
Study supports retreatment, which is good news for patients
Incidence rates of adverse events were comparable in the retreatment population and in the overall extension cohort. “There are no signals jumping out, saying that safety events were higher or more frequent in this retreatment population, which is reassuring,” Dr. Loftus added.
Findings such as these are to be expected given the mechanism of action and pharmacologic features of tofacitinib, said Gionata Fiorino, MD, from Humanitas University in Milan, who was not involved in the study.
“I think this is important for patients who need to stop therapy for several reasons – pregnancy, adverse events that do not require permanent withdrawal of the drug, or surgical interventions – and experience a flare after drug withdrawal,” he said in an interview.
“There are several other therapeutic options for these patients, but I have experienced many patients who do not respond to other mechanisms of action apart from JAK [inhibitors],” he added. “And, in the case of a patient who has stopped the drug after having achieved remission, this study clearly supports retreatment, which is good news, especially for patients.”
This study was funded by Pfizer. Dr. Loftus reported financial relationships with AbbVie, Allergan, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Eli Lilly, Exact Sciences, Genentech, Gilead, Janssen, Pfizer, Robarts Clinical Trials, Takeda, and UCB. Dr. Fiorino reports financial relationships with MSD, Takeda, AbbVie, Janssen, Pfizer, Celltrion, Sandoz, AlfaSigma, Samsung, Amgen, Roche, and Ferring.
A version of this article originally appeared on Medscape.com.
Retreatment with tofacitinib after a period of treatment interruption was well tolerated and effective in patients with ulcerative colitis who had shown a previous response to tofacitinib induction, according to an analysis of data from the OCTAVE extension trial.
“Clinical response was recaptured in most patients by month 2, and about half of patients by month 36, irrespective of prior anti–[tumor necrosis factor] status,” said lead researcher Edward V. Loftus Jr, MD, from the Mayo Medical School, Rochester, Minn.
A temporary suspension of treatment with the oral, small-molecule Janus kinase (JAK) inhibitor might be necessary for a number of reasons, such as if a patient has to undergo surgery, experiences adverse events, or becomes pregnant.
For their study, Dr. Loftus and colleagues set out to assess the safety and efficacy of retreatment after a period of interruption.
“The population we’re interested in are patients who received tofacitinib during induction and placebo during maintenance” in the original OCTAVE trials, said Dr. Loftus. “They then either completed the trial or flared and rolled over to the open-label extension.”
The researchers looked at the 100 patients who had achieved a clinical response after 8 weeks of treatment with tofacitinib 10 mg twice-daily in the OCTAVE Induction 1 and OCTAVE Induction 2 trials and then received placebo in the OCTAVE Sustain trial and experienced treatment failure between week 8 and week 52. These patients went on to receive tofacitinib 10 mg twice daily as part of the ongoing, open-label, long-term extension OCTAVE Open trial.
Treatment failure was defined as an increase of at least 3 points from the baseline total Mayo score achieved in OCTAVE Sustain, plus an increase of at least 1 point in rectal bleeding and endoscopic subscores and an absolute endoscopic subscore of at least 2 points after at least 8 weeks of treatment. Efficacy was evaluated for up to 36 months in the open-label extension; adverse events were assessed throughout the study period.
The median time to treatment failure was 135 days, Dr. Loftus reported during his award-winning presentation at the virtual annual meeting of the American College of Gastroenterology.
On last observation carried forward (LOCF) analysis, or observed data, 85.2% of the patients had recaptured clinical response by month 2. That rate fell to 74.3% when the analysis was modified for nonresponder imputation (NRI).
“The truth lies somewhere in between,” Dr. Loftus said.
Of interest, a clinical response to tofacitinib retreatment at month 2 was achieved by 92.5% (observed data) and 80.4% (NRI-LOCF) of patients who experienced treatment failure after tumor necrosis factor inhibitor therapy.
“Many patients were able to regain response with tofacitinib and then maintain that over time,” said Dr. Loftus.
Study supports retreatment, which is good news for patients
Incidence rates of adverse events were comparable in the retreatment population and in the overall extension cohort. “There are no signals jumping out, saying that safety events were higher or more frequent in this retreatment population, which is reassuring,” Dr. Loftus added.
Findings such as these are to be expected given the mechanism of action and pharmacologic features of tofacitinib, said Gionata Fiorino, MD, from Humanitas University in Milan, who was not involved in the study.
“I think this is important for patients who need to stop therapy for several reasons – pregnancy, adverse events that do not require permanent withdrawal of the drug, or surgical interventions – and experience a flare after drug withdrawal,” he said in an interview.
“There are several other therapeutic options for these patients, but I have experienced many patients who do not respond to other mechanisms of action apart from JAK [inhibitors],” he added. “And, in the case of a patient who has stopped the drug after having achieved remission, this study clearly supports retreatment, which is good news, especially for patients.”
This study was funded by Pfizer. Dr. Loftus reported financial relationships with AbbVie, Allergan, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Eli Lilly, Exact Sciences, Genentech, Gilead, Janssen, Pfizer, Robarts Clinical Trials, Takeda, and UCB. Dr. Fiorino reports financial relationships with MSD, Takeda, AbbVie, Janssen, Pfizer, Celltrion, Sandoz, AlfaSigma, Samsung, Amgen, Roche, and Ferring.
A version of this article originally appeared on Medscape.com.
Retreatment with tofacitinib after a period of treatment interruption was well tolerated and effective in patients with ulcerative colitis who had shown a previous response to tofacitinib induction, according to an analysis of data from the OCTAVE extension trial.
“Clinical response was recaptured in most patients by month 2, and about half of patients by month 36, irrespective of prior anti–[tumor necrosis factor] status,” said lead researcher Edward V. Loftus Jr, MD, from the Mayo Medical School, Rochester, Minn.
A temporary suspension of treatment with the oral, small-molecule Janus kinase (JAK) inhibitor might be necessary for a number of reasons, such as if a patient has to undergo surgery, experiences adverse events, or becomes pregnant.
For their study, Dr. Loftus and colleagues set out to assess the safety and efficacy of retreatment after a period of interruption.
“The population we’re interested in are patients who received tofacitinib during induction and placebo during maintenance” in the original OCTAVE trials, said Dr. Loftus. “They then either completed the trial or flared and rolled over to the open-label extension.”
The researchers looked at the 100 patients who had achieved a clinical response after 8 weeks of treatment with tofacitinib 10 mg twice-daily in the OCTAVE Induction 1 and OCTAVE Induction 2 trials and then received placebo in the OCTAVE Sustain trial and experienced treatment failure between week 8 and week 52. These patients went on to receive tofacitinib 10 mg twice daily as part of the ongoing, open-label, long-term extension OCTAVE Open trial.
Treatment failure was defined as an increase of at least 3 points from the baseline total Mayo score achieved in OCTAVE Sustain, plus an increase of at least 1 point in rectal bleeding and endoscopic subscores and an absolute endoscopic subscore of at least 2 points after at least 8 weeks of treatment. Efficacy was evaluated for up to 36 months in the open-label extension; adverse events were assessed throughout the study period.
The median time to treatment failure was 135 days, Dr. Loftus reported during his award-winning presentation at the virtual annual meeting of the American College of Gastroenterology.
On last observation carried forward (LOCF) analysis, or observed data, 85.2% of the patients had recaptured clinical response by month 2. That rate fell to 74.3% when the analysis was modified for nonresponder imputation (NRI).
“The truth lies somewhere in between,” Dr. Loftus said.
Of interest, a clinical response to tofacitinib retreatment at month 2 was achieved by 92.5% (observed data) and 80.4% (NRI-LOCF) of patients who experienced treatment failure after tumor necrosis factor inhibitor therapy.
“Many patients were able to regain response with tofacitinib and then maintain that over time,” said Dr. Loftus.
Study supports retreatment, which is good news for patients
Incidence rates of adverse events were comparable in the retreatment population and in the overall extension cohort. “There are no signals jumping out, saying that safety events were higher or more frequent in this retreatment population, which is reassuring,” Dr. Loftus added.
Findings such as these are to be expected given the mechanism of action and pharmacologic features of tofacitinib, said Gionata Fiorino, MD, from Humanitas University in Milan, who was not involved in the study.
“I think this is important for patients who need to stop therapy for several reasons – pregnancy, adverse events that do not require permanent withdrawal of the drug, or surgical interventions – and experience a flare after drug withdrawal,” he said in an interview.
“There are several other therapeutic options for these patients, but I have experienced many patients who do not respond to other mechanisms of action apart from JAK [inhibitors],” he added. “And, in the case of a patient who has stopped the drug after having achieved remission, this study clearly supports retreatment, which is good news, especially for patients.”
This study was funded by Pfizer. Dr. Loftus reported financial relationships with AbbVie, Allergan, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Eli Lilly, Exact Sciences, Genentech, Gilead, Janssen, Pfizer, Robarts Clinical Trials, Takeda, and UCB. Dr. Fiorino reports financial relationships with MSD, Takeda, AbbVie, Janssen, Pfizer, Celltrion, Sandoz, AlfaSigma, Samsung, Amgen, Roche, and Ferring.
A version of this article originally appeared on Medscape.com.
Cannabis may improve liver function in patients with obesity
Cannabis use is associated with a decrease in the prevalence of steatohepatitis and a slowing of its progression in patients with obesity, results from a retrospective cohort study show.
This suggests “that the anti-inflammatory effects of cannabis may be leading to reduced prevalence of steatohepatitis in cannabis users,” said Ikechukwu Achebe, MD, from the John H. Stroger, Jr. Hospital of Cook County in Chicago.
Liver injuries such as nonalcoholic steatohepatitis are characterized by hepatocellular injury and inflammation, which combine to contribute to an increase in the risk for liver failure, cirrhosis, and hepatocellular carcinoma.
“This is where cannabis comes in,” said Dr. Achebe, who presented the study results at the virtual annual meeting of the American College of Gastroenterology. “It is the most commonly used psychoactive substance worldwide and has been shown to reduce hepatic myofibroblast and stellate cell injury. Studies using mouse models have demonstrated reduced liver fibrosis and cirrhosis as a consequence of cannabis exposure.”
Given this possible connection, Dr. Achebe and colleagues set out to determine whether cannabis use affects the prevalence and progression of nonalcoholic fatty liver disease (NAFLD) in obese patients.
To do so, they analyzed the discharge records of 879,952 obese adults in the 2016 Healthcare Cost and Utilization Project National Inpatient Sample. The primary outcome was the prevalence of the four presentations of NAFLD: steatosis, steatohepatitis, cirrhosis, and hepatocellular carcinoma.
The researchers compared disease stages in cannabis users and nonusers. In the study cohort of 14,236 patients, 1.6% used cannabis. Steatohepatitis was less common among cannabis users than among nonusers (0.4% vs. 0.7%; P < .001), as was cirrhosis (1.1% vs. 1.5%; P < .001).
After propensity matching, the association between cannabis use and lower rates of steatohepatitis remained significant (0.4% vs. 0.5%; P = .035), but the association between cannabis use and the prevalence of nonalcoholic fatty liver, cirrhosis, and hepatocellular carcinoma did not.
These results might be partly explained by the protective effect of cannabis on hepatocytes regulated by the endocannabinoid system, the researchers concluded.
More studies are needed to explore this relation, said Dr. Achebe.
The challenge of self-reported use
The study is “incredibly interesting,” said Nancy S. Reau, MD, from Rush Medical College, Chicago. However, the association between cannabis and nonalcoholic fatty liver needs to be further investigated before clinicians can counsel their patients to use the agent to prevent progression.
It is difficult in a study such as this to tease out other lifestyle factors that might be linked to cannabis use, she explained. For example, “is it possible that the cannabis users exercise more, drink more coffee, or eat differently?”
And “self-reported use is challenging,” Dr. Reau said in an interview. “This cannot differentiate someone who occasionally uses from someone who is a heavy daily user. There must be some minimum level of exposure needed for it to have protective effects, if they exist.”
This study was honored at the meeting as an ACG Newsworthy Abstract and an ACG Outstanding Poster Presenter.
Dr. Achebe disclosed no relevant financial relationships. Dr. Reau reported receiving research support from Genfit and having a consultant relationship with Intercept Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
Cannabis use is associated with a decrease in the prevalence of steatohepatitis and a slowing of its progression in patients with obesity, results from a retrospective cohort study show.
This suggests “that the anti-inflammatory effects of cannabis may be leading to reduced prevalence of steatohepatitis in cannabis users,” said Ikechukwu Achebe, MD, from the John H. Stroger, Jr. Hospital of Cook County in Chicago.
Liver injuries such as nonalcoholic steatohepatitis are characterized by hepatocellular injury and inflammation, which combine to contribute to an increase in the risk for liver failure, cirrhosis, and hepatocellular carcinoma.
“This is where cannabis comes in,” said Dr. Achebe, who presented the study results at the virtual annual meeting of the American College of Gastroenterology. “It is the most commonly used psychoactive substance worldwide and has been shown to reduce hepatic myofibroblast and stellate cell injury. Studies using mouse models have demonstrated reduced liver fibrosis and cirrhosis as a consequence of cannabis exposure.”
Given this possible connection, Dr. Achebe and colleagues set out to determine whether cannabis use affects the prevalence and progression of nonalcoholic fatty liver disease (NAFLD) in obese patients.
To do so, they analyzed the discharge records of 879,952 obese adults in the 2016 Healthcare Cost and Utilization Project National Inpatient Sample. The primary outcome was the prevalence of the four presentations of NAFLD: steatosis, steatohepatitis, cirrhosis, and hepatocellular carcinoma.
The researchers compared disease stages in cannabis users and nonusers. In the study cohort of 14,236 patients, 1.6% used cannabis. Steatohepatitis was less common among cannabis users than among nonusers (0.4% vs. 0.7%; P < .001), as was cirrhosis (1.1% vs. 1.5%; P < .001).
After propensity matching, the association between cannabis use and lower rates of steatohepatitis remained significant (0.4% vs. 0.5%; P = .035), but the association between cannabis use and the prevalence of nonalcoholic fatty liver, cirrhosis, and hepatocellular carcinoma did not.
These results might be partly explained by the protective effect of cannabis on hepatocytes regulated by the endocannabinoid system, the researchers concluded.
More studies are needed to explore this relation, said Dr. Achebe.
The challenge of self-reported use
The study is “incredibly interesting,” said Nancy S. Reau, MD, from Rush Medical College, Chicago. However, the association between cannabis and nonalcoholic fatty liver needs to be further investigated before clinicians can counsel their patients to use the agent to prevent progression.
It is difficult in a study such as this to tease out other lifestyle factors that might be linked to cannabis use, she explained. For example, “is it possible that the cannabis users exercise more, drink more coffee, or eat differently?”
And “self-reported use is challenging,” Dr. Reau said in an interview. “This cannot differentiate someone who occasionally uses from someone who is a heavy daily user. There must be some minimum level of exposure needed for it to have protective effects, if they exist.”
This study was honored at the meeting as an ACG Newsworthy Abstract and an ACG Outstanding Poster Presenter.
Dr. Achebe disclosed no relevant financial relationships. Dr. Reau reported receiving research support from Genfit and having a consultant relationship with Intercept Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
Cannabis use is associated with a decrease in the prevalence of steatohepatitis and a slowing of its progression in patients with obesity, results from a retrospective cohort study show.
This suggests “that the anti-inflammatory effects of cannabis may be leading to reduced prevalence of steatohepatitis in cannabis users,” said Ikechukwu Achebe, MD, from the John H. Stroger, Jr. Hospital of Cook County in Chicago.
Liver injuries such as nonalcoholic steatohepatitis are characterized by hepatocellular injury and inflammation, which combine to contribute to an increase in the risk for liver failure, cirrhosis, and hepatocellular carcinoma.
“This is where cannabis comes in,” said Dr. Achebe, who presented the study results at the virtual annual meeting of the American College of Gastroenterology. “It is the most commonly used psychoactive substance worldwide and has been shown to reduce hepatic myofibroblast and stellate cell injury. Studies using mouse models have demonstrated reduced liver fibrosis and cirrhosis as a consequence of cannabis exposure.”
Given this possible connection, Dr. Achebe and colleagues set out to determine whether cannabis use affects the prevalence and progression of nonalcoholic fatty liver disease (NAFLD) in obese patients.
To do so, they analyzed the discharge records of 879,952 obese adults in the 2016 Healthcare Cost and Utilization Project National Inpatient Sample. The primary outcome was the prevalence of the four presentations of NAFLD: steatosis, steatohepatitis, cirrhosis, and hepatocellular carcinoma.
The researchers compared disease stages in cannabis users and nonusers. In the study cohort of 14,236 patients, 1.6% used cannabis. Steatohepatitis was less common among cannabis users than among nonusers (0.4% vs. 0.7%; P < .001), as was cirrhosis (1.1% vs. 1.5%; P < .001).
After propensity matching, the association between cannabis use and lower rates of steatohepatitis remained significant (0.4% vs. 0.5%; P = .035), but the association between cannabis use and the prevalence of nonalcoholic fatty liver, cirrhosis, and hepatocellular carcinoma did not.
These results might be partly explained by the protective effect of cannabis on hepatocytes regulated by the endocannabinoid system, the researchers concluded.
More studies are needed to explore this relation, said Dr. Achebe.
The challenge of self-reported use
The study is “incredibly interesting,” said Nancy S. Reau, MD, from Rush Medical College, Chicago. However, the association between cannabis and nonalcoholic fatty liver needs to be further investigated before clinicians can counsel their patients to use the agent to prevent progression.
It is difficult in a study such as this to tease out other lifestyle factors that might be linked to cannabis use, she explained. For example, “is it possible that the cannabis users exercise more, drink more coffee, or eat differently?”
And “self-reported use is challenging,” Dr. Reau said in an interview. “This cannot differentiate someone who occasionally uses from someone who is a heavy daily user. There must be some minimum level of exposure needed for it to have protective effects, if they exist.”
This study was honored at the meeting as an ACG Newsworthy Abstract and an ACG Outstanding Poster Presenter.
Dr. Achebe disclosed no relevant financial relationships. Dr. Reau reported receiving research support from Genfit and having a consultant relationship with Intercept Pharmaceuticals.
A version of this article originally appeared on Medscape.com.
FROM ACG 2020
Biomarker in the eye may flag neurodegeneration risk
, opening the door to a potential new method of predicting neurodegenerative disease, new research suggests.
In a study of 77 patients undergoing eye surgery for various conditions, more than 70% had more than 20 pg/mL of NfL in their vitreous humor. Higher levels of NfL were associated with higher levels of other biomarkers known to be associated with Alzheimer’s disease, including amyloid-beta and tau proteins.
“The study had three primary findings,” said lead author Manju L. Subramanian, MD, associate professor of ophthalmology at Boston University.
First, the investigators were able to detect levels of NfL in eye fluid; and second, those levels were not in any way correlated to the patient’s clinical eye condition, Dr. Subramanian said. “The third finding was that we were able to correlate those neurofilament light levels with other markers that have been known to be associated with conditions such as Alzheimer’s disease,” she noted.
For Dr. Subramanian, these findings add to the hypothesis that the eye is an extension of the brain. “This is further evidence that the eye might potentially be a proxy for neurodegenerative diseases,” she said. “So finding neurofilament light chain in the eye demonstrates that the eye is not an isolated organ, and things that happen in the body can affect the eye and vice versa.”
The findings were published online Sept. 17 in Alzheimer’s Research & Therapy.
Verge of clinical applicability?
Early diagnosis of neurodegenerative diseases remains a challenge, the investigators noted. As such, there is a palpable need for reliable biomarkers that can help with early diagnosis, prognostic assessment, and measurable response to treatment for Alzheimer’s disease and other neurologic disorders
Recent research has identified NfL as a potential screening tool and some researchers believe it to be on the verge of clinical applicability. In addition, increased levels of the biomarker have been observed in both the cerebrospinal fluid (CSF) and blood of individuals with neurodegeneration and neurological diseases, including Alzheimer’s disease. In previous studies, for example, elevated levels of NfL in CSF and blood have been shown to reliably distinguish between patients with Alzheimer’s disease and healthy volunteers.
Because certain eye diseases have been associated with Alzheimer’s disease in epidemiological studies, they may share common risk factors and pathological mechanisms at the molecular level, the researchers noted. In an earlier study, the current investigators found that cognitive function among patients with eye disease was significantly associated with amyloid-beta and total tau protein levels in the vitreous humor.
Given these connections, the researchers hypothesized that NfL could be identified in the vitreous humor and may be associated with other relevant biomarkers of neuronal origin. “Neurofilament light chain is detectable in the cerebrospinal fluid, but it’s never been tested for detection in the eye,” Dr. Subramanian noted.
In total, vitreous humor samples were collected from 77 unique participants (mean age, 56.2 years; 63% men) as part of the single-center, prospective, cross-sectional cohort study. The researchers aspirated 0.5 to 1.0 ml of undiluted vitreous fluid during vitrectomy, while whole blood was drawn for APOE genotyping.
Immunoassay was used to quantitatively measure for NfL, amyloid-beta, total tau, phosphorylated tau 181 (p-tau181), inflammatory cytokines, chemokines, and vascular proteins in the vitreous humor. The trial’s primary outcome measures were the detection of NfL levels in the vitreous humor, as well as its associations with other proteins.
Significant correlations
Results showed that 55 of the 77 participants (71.4%) had at least 20 pg/ml of NfL protein present in the vitreous humor. The median level was 68.65 pg/ml. Statistically significant associations were found between NfL levels in the vitreous humor and Abeta40, Abeta42, and total tau; higher NfL levels were associated with higher levels of all three biomarkers. On the other hand, NfL levels were not positively associated with increased vitreous levels of p-tau181.
Vitreous NfL concentration was significantly associated with inflammatory cytokines, including interleukin-15, interleukin-16, and monocyte chemoattractant protein-1, as well as vascular proteins such as vascular endothelial growth factor receptor-1, VEGF-C, vascular cell adhesion molecule-1, Tie-2, and intracellular adhesion molecular-1.
Despite these findings, NfL in the vitreous humor was not associated with patients’ clinical ophthalmic conditions or systemic diseases such as hypertension, diabetes, and hyperlipidemia. Similarly, NfL was not significantly associated with APOE genotype E2 and E4, the alleles most commonly associated with Alzheimer’s disease.
Finally, no statistically significant associations were found between NfL and Mini-Mental State Examination (MMSE) scores.
A “first step”
Most research currently examining the role of the eye in neurodegenerative disease is focused on retinal biomarkers imaged by optical coherence tomography, the investigators noted. Although promising, data obtained this way have yielded conflicting results.
Similarly, while the diagnostic potential of the core CSF biomarkers for AD (Abeta40, Abeta42, p-tau, and total tau) is well established, the practical utility of testing CSF for neurodegenerative diseases is limited, wrote the researchers.
As such, an additional biomarker source such as NfL–which is quantifiable and protein-based within eye fluid – has the potential to play an important role in predicting neurodegenerative disease in the clinical setting, they added.
“The holy grail of neurodegenerative-disease diagnosis is early diagnosis. Because if you can implement treatment early, you can slow down and potentially halt the progression of these diseases,” Dr. Subramanian said.
“This study is the first step toward determining if the eye could play a potential role in early diagnosis of conditions such as Alzheimer’s disease,” she added.
That said, Dr. Subramanian was quick to recognize the findings’ preliminary nature and that they do not offer reliable evidence that vitreous NfL levels definitively represent neurodegeneration. As such, the investigators called for more research to validate the association between this type of biomarker with other established biomarkers of neurodegeneration, such as those found in CSF fluid or on MRI and PET scans.
“At this point, we can’t look at eye fluid and say that people have neurodegenerative diseases,” she noted. “The other thing to consider is that vitreous humor is at the back of the eye, so it’s actually a fairly invasive procedure.
“I think the next step is to look at other types of eye fluids such as the aqueous fluid in the front of the eye, or even tear secretions, potentially,” Dr. Subramanian said.
Other study limitations include the lack of an association between NfL levels and MMSE scores and that none of the study participants were actually diagnosed with Alzheimer’s disease. Validation studies are needed to compare vitreous levels of NfL in patients with mild cognitive impairment/AD to normal controls, the investigators noted.
Fascinating but impractical?
Commenting on the findings, Sharon Fekrat, MD, professor of ophthalmology, Duke University, Durham, N.C., agreed that there’s potential importance of the eye in diagnosing neurodegeneration. However, she suggested that vitreous humor may not be the most expedient medium to use.
“I commend the authors for this fascinating work. But practically speaking, if we ultimately want to use intraocular fluid to diagnose Alzheimer’s and perhaps other neurodegeneration, I think aqueous humor might be more practical than the vitreous humor,” said Dr. Fekrat, who was not involved with the research. “What might be even better is to have a device that can be held against the eyeball that measures the levels of various substances inside the eyeball without having to enter the eye,” added Justin Ma, a Duke University medical student working under Dr. Fekrat’s guidance. “It could be similar technology to what’s currently used to measure blood glucose levels,” Mr. Ma added.
The study was supported in part by the National Institute of Aging. Dr. Subramanian, Dr. Fekrat, and Mr. Ma have disclosed no relevant financial relationships. Disclosures for other study authors are listed in the original article.
A version of this article originally appeared on Medscape.com.
, opening the door to a potential new method of predicting neurodegenerative disease, new research suggests.
In a study of 77 patients undergoing eye surgery for various conditions, more than 70% had more than 20 pg/mL of NfL in their vitreous humor. Higher levels of NfL were associated with higher levels of other biomarkers known to be associated with Alzheimer’s disease, including amyloid-beta and tau proteins.
“The study had three primary findings,” said lead author Manju L. Subramanian, MD, associate professor of ophthalmology at Boston University.
First, the investigators were able to detect levels of NfL in eye fluid; and second, those levels were not in any way correlated to the patient’s clinical eye condition, Dr. Subramanian said. “The third finding was that we were able to correlate those neurofilament light levels with other markers that have been known to be associated with conditions such as Alzheimer’s disease,” she noted.
For Dr. Subramanian, these findings add to the hypothesis that the eye is an extension of the brain. “This is further evidence that the eye might potentially be a proxy for neurodegenerative diseases,” she said. “So finding neurofilament light chain in the eye demonstrates that the eye is not an isolated organ, and things that happen in the body can affect the eye and vice versa.”
The findings were published online Sept. 17 in Alzheimer’s Research & Therapy.
Verge of clinical applicability?
Early diagnosis of neurodegenerative diseases remains a challenge, the investigators noted. As such, there is a palpable need for reliable biomarkers that can help with early diagnosis, prognostic assessment, and measurable response to treatment for Alzheimer’s disease and other neurologic disorders
Recent research has identified NfL as a potential screening tool and some researchers believe it to be on the verge of clinical applicability. In addition, increased levels of the biomarker have been observed in both the cerebrospinal fluid (CSF) and blood of individuals with neurodegeneration and neurological diseases, including Alzheimer’s disease. In previous studies, for example, elevated levels of NfL in CSF and blood have been shown to reliably distinguish between patients with Alzheimer’s disease and healthy volunteers.
Because certain eye diseases have been associated with Alzheimer’s disease in epidemiological studies, they may share common risk factors and pathological mechanisms at the molecular level, the researchers noted. In an earlier study, the current investigators found that cognitive function among patients with eye disease was significantly associated with amyloid-beta and total tau protein levels in the vitreous humor.
Given these connections, the researchers hypothesized that NfL could be identified in the vitreous humor and may be associated with other relevant biomarkers of neuronal origin. “Neurofilament light chain is detectable in the cerebrospinal fluid, but it’s never been tested for detection in the eye,” Dr. Subramanian noted.
In total, vitreous humor samples were collected from 77 unique participants (mean age, 56.2 years; 63% men) as part of the single-center, prospective, cross-sectional cohort study. The researchers aspirated 0.5 to 1.0 ml of undiluted vitreous fluid during vitrectomy, while whole blood was drawn for APOE genotyping.
Immunoassay was used to quantitatively measure for NfL, amyloid-beta, total tau, phosphorylated tau 181 (p-tau181), inflammatory cytokines, chemokines, and vascular proteins in the vitreous humor. The trial’s primary outcome measures were the detection of NfL levels in the vitreous humor, as well as its associations with other proteins.
Significant correlations
Results showed that 55 of the 77 participants (71.4%) had at least 20 pg/ml of NfL protein present in the vitreous humor. The median level was 68.65 pg/ml. Statistically significant associations were found between NfL levels in the vitreous humor and Abeta40, Abeta42, and total tau; higher NfL levels were associated with higher levels of all three biomarkers. On the other hand, NfL levels were not positively associated with increased vitreous levels of p-tau181.
Vitreous NfL concentration was significantly associated with inflammatory cytokines, including interleukin-15, interleukin-16, and monocyte chemoattractant protein-1, as well as vascular proteins such as vascular endothelial growth factor receptor-1, VEGF-C, vascular cell adhesion molecule-1, Tie-2, and intracellular adhesion molecular-1.
Despite these findings, NfL in the vitreous humor was not associated with patients’ clinical ophthalmic conditions or systemic diseases such as hypertension, diabetes, and hyperlipidemia. Similarly, NfL was not significantly associated with APOE genotype E2 and E4, the alleles most commonly associated with Alzheimer’s disease.
Finally, no statistically significant associations were found between NfL and Mini-Mental State Examination (MMSE) scores.
A “first step”
Most research currently examining the role of the eye in neurodegenerative disease is focused on retinal biomarkers imaged by optical coherence tomography, the investigators noted. Although promising, data obtained this way have yielded conflicting results.
Similarly, while the diagnostic potential of the core CSF biomarkers for AD (Abeta40, Abeta42, p-tau, and total tau) is well established, the practical utility of testing CSF for neurodegenerative diseases is limited, wrote the researchers.
As such, an additional biomarker source such as NfL–which is quantifiable and protein-based within eye fluid – has the potential to play an important role in predicting neurodegenerative disease in the clinical setting, they added.
“The holy grail of neurodegenerative-disease diagnosis is early diagnosis. Because if you can implement treatment early, you can slow down and potentially halt the progression of these diseases,” Dr. Subramanian said.
“This study is the first step toward determining if the eye could play a potential role in early diagnosis of conditions such as Alzheimer’s disease,” she added.
That said, Dr. Subramanian was quick to recognize the findings’ preliminary nature and that they do not offer reliable evidence that vitreous NfL levels definitively represent neurodegeneration. As such, the investigators called for more research to validate the association between this type of biomarker with other established biomarkers of neurodegeneration, such as those found in CSF fluid or on MRI and PET scans.
“At this point, we can’t look at eye fluid and say that people have neurodegenerative diseases,” she noted. “The other thing to consider is that vitreous humor is at the back of the eye, so it’s actually a fairly invasive procedure.
“I think the next step is to look at other types of eye fluids such as the aqueous fluid in the front of the eye, or even tear secretions, potentially,” Dr. Subramanian said.
Other study limitations include the lack of an association between NfL levels and MMSE scores and that none of the study participants were actually diagnosed with Alzheimer’s disease. Validation studies are needed to compare vitreous levels of NfL in patients with mild cognitive impairment/AD to normal controls, the investigators noted.
Fascinating but impractical?
Commenting on the findings, Sharon Fekrat, MD, professor of ophthalmology, Duke University, Durham, N.C., agreed that there’s potential importance of the eye in diagnosing neurodegeneration. However, she suggested that vitreous humor may not be the most expedient medium to use.
“I commend the authors for this fascinating work. But practically speaking, if we ultimately want to use intraocular fluid to diagnose Alzheimer’s and perhaps other neurodegeneration, I think aqueous humor might be more practical than the vitreous humor,” said Dr. Fekrat, who was not involved with the research. “What might be even better is to have a device that can be held against the eyeball that measures the levels of various substances inside the eyeball without having to enter the eye,” added Justin Ma, a Duke University medical student working under Dr. Fekrat’s guidance. “It could be similar technology to what’s currently used to measure blood glucose levels,” Mr. Ma added.
The study was supported in part by the National Institute of Aging. Dr. Subramanian, Dr. Fekrat, and Mr. Ma have disclosed no relevant financial relationships. Disclosures for other study authors are listed in the original article.
A version of this article originally appeared on Medscape.com.
, opening the door to a potential new method of predicting neurodegenerative disease, new research suggests.
In a study of 77 patients undergoing eye surgery for various conditions, more than 70% had more than 20 pg/mL of NfL in their vitreous humor. Higher levels of NfL were associated with higher levels of other biomarkers known to be associated with Alzheimer’s disease, including amyloid-beta and tau proteins.
“The study had three primary findings,” said lead author Manju L. Subramanian, MD, associate professor of ophthalmology at Boston University.
First, the investigators were able to detect levels of NfL in eye fluid; and second, those levels were not in any way correlated to the patient’s clinical eye condition, Dr. Subramanian said. “The third finding was that we were able to correlate those neurofilament light levels with other markers that have been known to be associated with conditions such as Alzheimer’s disease,” she noted.
For Dr. Subramanian, these findings add to the hypothesis that the eye is an extension of the brain. “This is further evidence that the eye might potentially be a proxy for neurodegenerative diseases,” she said. “So finding neurofilament light chain in the eye demonstrates that the eye is not an isolated organ, and things that happen in the body can affect the eye and vice versa.”
The findings were published online Sept. 17 in Alzheimer’s Research & Therapy.
Verge of clinical applicability?
Early diagnosis of neurodegenerative diseases remains a challenge, the investigators noted. As such, there is a palpable need for reliable biomarkers that can help with early diagnosis, prognostic assessment, and measurable response to treatment for Alzheimer’s disease and other neurologic disorders
Recent research has identified NfL as a potential screening tool and some researchers believe it to be on the verge of clinical applicability. In addition, increased levels of the biomarker have been observed in both the cerebrospinal fluid (CSF) and blood of individuals with neurodegeneration and neurological diseases, including Alzheimer’s disease. In previous studies, for example, elevated levels of NfL in CSF and blood have been shown to reliably distinguish between patients with Alzheimer’s disease and healthy volunteers.
Because certain eye diseases have been associated with Alzheimer’s disease in epidemiological studies, they may share common risk factors and pathological mechanisms at the molecular level, the researchers noted. In an earlier study, the current investigators found that cognitive function among patients with eye disease was significantly associated with amyloid-beta and total tau protein levels in the vitreous humor.
Given these connections, the researchers hypothesized that NfL could be identified in the vitreous humor and may be associated with other relevant biomarkers of neuronal origin. “Neurofilament light chain is detectable in the cerebrospinal fluid, but it’s never been tested for detection in the eye,” Dr. Subramanian noted.
In total, vitreous humor samples were collected from 77 unique participants (mean age, 56.2 years; 63% men) as part of the single-center, prospective, cross-sectional cohort study. The researchers aspirated 0.5 to 1.0 ml of undiluted vitreous fluid during vitrectomy, while whole blood was drawn for APOE genotyping.
Immunoassay was used to quantitatively measure for NfL, amyloid-beta, total tau, phosphorylated tau 181 (p-tau181), inflammatory cytokines, chemokines, and vascular proteins in the vitreous humor. The trial’s primary outcome measures were the detection of NfL levels in the vitreous humor, as well as its associations with other proteins.
Significant correlations
Results showed that 55 of the 77 participants (71.4%) had at least 20 pg/ml of NfL protein present in the vitreous humor. The median level was 68.65 pg/ml. Statistically significant associations were found between NfL levels in the vitreous humor and Abeta40, Abeta42, and total tau; higher NfL levels were associated with higher levels of all three biomarkers. On the other hand, NfL levels were not positively associated with increased vitreous levels of p-tau181.
Vitreous NfL concentration was significantly associated with inflammatory cytokines, including interleukin-15, interleukin-16, and monocyte chemoattractant protein-1, as well as vascular proteins such as vascular endothelial growth factor receptor-1, VEGF-C, vascular cell adhesion molecule-1, Tie-2, and intracellular adhesion molecular-1.
Despite these findings, NfL in the vitreous humor was not associated with patients’ clinical ophthalmic conditions or systemic diseases such as hypertension, diabetes, and hyperlipidemia. Similarly, NfL was not significantly associated with APOE genotype E2 and E4, the alleles most commonly associated with Alzheimer’s disease.
Finally, no statistically significant associations were found between NfL and Mini-Mental State Examination (MMSE) scores.
A “first step”
Most research currently examining the role of the eye in neurodegenerative disease is focused on retinal biomarkers imaged by optical coherence tomography, the investigators noted. Although promising, data obtained this way have yielded conflicting results.
Similarly, while the diagnostic potential of the core CSF biomarkers for AD (Abeta40, Abeta42, p-tau, and total tau) is well established, the practical utility of testing CSF for neurodegenerative diseases is limited, wrote the researchers.
As such, an additional biomarker source such as NfL–which is quantifiable and protein-based within eye fluid – has the potential to play an important role in predicting neurodegenerative disease in the clinical setting, they added.
“The holy grail of neurodegenerative-disease diagnosis is early diagnosis. Because if you can implement treatment early, you can slow down and potentially halt the progression of these diseases,” Dr. Subramanian said.
“This study is the first step toward determining if the eye could play a potential role in early diagnosis of conditions such as Alzheimer’s disease,” she added.
That said, Dr. Subramanian was quick to recognize the findings’ preliminary nature and that they do not offer reliable evidence that vitreous NfL levels definitively represent neurodegeneration. As such, the investigators called for more research to validate the association between this type of biomarker with other established biomarkers of neurodegeneration, such as those found in CSF fluid or on MRI and PET scans.
“At this point, we can’t look at eye fluid and say that people have neurodegenerative diseases,” she noted. “The other thing to consider is that vitreous humor is at the back of the eye, so it’s actually a fairly invasive procedure.
“I think the next step is to look at other types of eye fluids such as the aqueous fluid in the front of the eye, or even tear secretions, potentially,” Dr. Subramanian said.
Other study limitations include the lack of an association between NfL levels and MMSE scores and that none of the study participants were actually diagnosed with Alzheimer’s disease. Validation studies are needed to compare vitreous levels of NfL in patients with mild cognitive impairment/AD to normal controls, the investigators noted.
Fascinating but impractical?
Commenting on the findings, Sharon Fekrat, MD, professor of ophthalmology, Duke University, Durham, N.C., agreed that there’s potential importance of the eye in diagnosing neurodegeneration. However, she suggested that vitreous humor may not be the most expedient medium to use.
“I commend the authors for this fascinating work. But practically speaking, if we ultimately want to use intraocular fluid to diagnose Alzheimer’s and perhaps other neurodegeneration, I think aqueous humor might be more practical than the vitreous humor,” said Dr. Fekrat, who was not involved with the research. “What might be even better is to have a device that can be held against the eyeball that measures the levels of various substances inside the eyeball without having to enter the eye,” added Justin Ma, a Duke University medical student working under Dr. Fekrat’s guidance. “It could be similar technology to what’s currently used to measure blood glucose levels,” Mr. Ma added.
The study was supported in part by the National Institute of Aging. Dr. Subramanian, Dr. Fekrat, and Mr. Ma have disclosed no relevant financial relationships. Disclosures for other study authors are listed in the original article.
A version of this article originally appeared on Medscape.com.
FROM ALZHEIMER’S RESEARCH & THERAPY