User login
Children with noncomplex chronic diseases use one-third of annual Medicaid pediatric spending
, accounting for a third of Medicaid pediatric expenditures, according to a retrospective, cross-sectional analysis.
Generalizing to the 35 million children on Medicaid nationally, the NC-CD population accounts for $35 billion in annual Medicaid spending (Pediatrics. 2017. doi: 10.1542/peds.2017-0492).
“An improved understanding of children with NC-CDs and their associated health care expenditures is needed to improve health care delivery for this population and may provide opportunities for health policy interventions to reduce costs of care,” they said.
The per member per year (PMPY) expenditures for children with NC-CDs was significantly less than that of children with complex chronic disease (C-CDs), but the annual aggregate expenditure for the NC-CD group represents a substantial cost because of the high prevalence of these conditions. The annual expenditures for the entire group was $7,226,354,620 over the study period, or $3,037 PMPY. The total PMPY expenditure for children with NC-CDs ($2,801) was significantly greater than children without chronic disease ($1,151) and lower than children with C-CDs ($12,569).
Children with NC-CDs accounted for 36% of the study population and 33% of the annualized aggregate expenditure. Children without chronic disease accounted for 53% of the study population and 20% of annualized aggregate expenditure. Children with C-CDs accounted for 11% of the study population and 47% of the annualized aggregate expenditure.
, accounting for a third of Medicaid pediatric expenditures, according to a retrospective, cross-sectional analysis.
Generalizing to the 35 million children on Medicaid nationally, the NC-CD population accounts for $35 billion in annual Medicaid spending (Pediatrics. 2017. doi: 10.1542/peds.2017-0492).
“An improved understanding of children with NC-CDs and their associated health care expenditures is needed to improve health care delivery for this population and may provide opportunities for health policy interventions to reduce costs of care,” they said.
The per member per year (PMPY) expenditures for children with NC-CDs was significantly less than that of children with complex chronic disease (C-CDs), but the annual aggregate expenditure for the NC-CD group represents a substantial cost because of the high prevalence of these conditions. The annual expenditures for the entire group was $7,226,354,620 over the study period, or $3,037 PMPY. The total PMPY expenditure for children with NC-CDs ($2,801) was significantly greater than children without chronic disease ($1,151) and lower than children with C-CDs ($12,569).
Children with NC-CDs accounted for 36% of the study population and 33% of the annualized aggregate expenditure. Children without chronic disease accounted for 53% of the study population and 20% of annualized aggregate expenditure. Children with C-CDs accounted for 11% of the study population and 47% of the annualized aggregate expenditure.
, accounting for a third of Medicaid pediatric expenditures, according to a retrospective, cross-sectional analysis.
Generalizing to the 35 million children on Medicaid nationally, the NC-CD population accounts for $35 billion in annual Medicaid spending (Pediatrics. 2017. doi: 10.1542/peds.2017-0492).
“An improved understanding of children with NC-CDs and their associated health care expenditures is needed to improve health care delivery for this population and may provide opportunities for health policy interventions to reduce costs of care,” they said.
The per member per year (PMPY) expenditures for children with NC-CDs was significantly less than that of children with complex chronic disease (C-CDs), but the annual aggregate expenditure for the NC-CD group represents a substantial cost because of the high prevalence of these conditions. The annual expenditures for the entire group was $7,226,354,620 over the study period, or $3,037 PMPY. The total PMPY expenditure for children with NC-CDs ($2,801) was significantly greater than children without chronic disease ($1,151) and lower than children with C-CDs ($12,569).
Children with NC-CDs accounted for 36% of the study population and 33% of the annualized aggregate expenditure. Children without chronic disease accounted for 53% of the study population and 20% of annualized aggregate expenditure. Children with C-CDs accounted for 11% of the study population and 47% of the annualized aggregate expenditure.
FROM PEDIATRICS
Maternal protection against measles steadily declines prior to vaccination
, and for coxsackievirus (CoxA16), for which there currently is no vaccine.
EV71 and CoxA16 are enteroviruses that are common agents of hand-foot-and-mouth disease. Some patients infected with EV71 or CoxA16 develop neurological and systemic complications that can kill them. An EV71 vaccine, which is initially administered at 6 months, has been licensed in China since December 2015.
In a longitudinally designed study conducted by Chuanxi Fu and Jichuan Shen of Guangzhou (China) Center for Disease Control and Prevention, and their associates, sera was collected from 717 infants ages 0, 3, and 6 months, and examined for levels of measles IgG antibodies, and neutralizing antibodies for EV71 and CoxA16. Measles IgG antibody concentration from 717, 233, and 75 sera were assessed in infants of 0 month, 3 months, and 6 months, and 225, 217, and 72 sera were assessed for EV71 and CoxA16 at these time periods.
This study provides evidence of the rapid declining of measles antibodies in infants prior to vaccination under the Expanded Program on Immunization schedule in China, and confirms the rapid decrease of measles antibody levels suggested by prior cross-sectional studies in China. “Further modifications of vaccination strategies for measles, earlier vaccination for EV71 infection, and development and provision of a CoxA16 vaccine should be investigated and considered in the future,” concluded the researchers.
, and for coxsackievirus (CoxA16), for which there currently is no vaccine.
EV71 and CoxA16 are enteroviruses that are common agents of hand-foot-and-mouth disease. Some patients infected with EV71 or CoxA16 develop neurological and systemic complications that can kill them. An EV71 vaccine, which is initially administered at 6 months, has been licensed in China since December 2015.
In a longitudinally designed study conducted by Chuanxi Fu and Jichuan Shen of Guangzhou (China) Center for Disease Control and Prevention, and their associates, sera was collected from 717 infants ages 0, 3, and 6 months, and examined for levels of measles IgG antibodies, and neutralizing antibodies for EV71 and CoxA16. Measles IgG antibody concentration from 717, 233, and 75 sera were assessed in infants of 0 month, 3 months, and 6 months, and 225, 217, and 72 sera were assessed for EV71 and CoxA16 at these time periods.
This study provides evidence of the rapid declining of measles antibodies in infants prior to vaccination under the Expanded Program on Immunization schedule in China, and confirms the rapid decrease of measles antibody levels suggested by prior cross-sectional studies in China. “Further modifications of vaccination strategies for measles, earlier vaccination for EV71 infection, and development and provision of a CoxA16 vaccine should be investigated and considered in the future,” concluded the researchers.
, and for coxsackievirus (CoxA16), for which there currently is no vaccine.
EV71 and CoxA16 are enteroviruses that are common agents of hand-foot-and-mouth disease. Some patients infected with EV71 or CoxA16 develop neurological and systemic complications that can kill them. An EV71 vaccine, which is initially administered at 6 months, has been licensed in China since December 2015.
In a longitudinally designed study conducted by Chuanxi Fu and Jichuan Shen of Guangzhou (China) Center for Disease Control and Prevention, and their associates, sera was collected from 717 infants ages 0, 3, and 6 months, and examined for levels of measles IgG antibodies, and neutralizing antibodies for EV71 and CoxA16. Measles IgG antibody concentration from 717, 233, and 75 sera were assessed in infants of 0 month, 3 months, and 6 months, and 225, 217, and 72 sera were assessed for EV71 and CoxA16 at these time periods.
This study provides evidence of the rapid declining of measles antibodies in infants prior to vaccination under the Expanded Program on Immunization schedule in China, and confirms the rapid decrease of measles antibody levels suggested by prior cross-sectional studies in China. “Further modifications of vaccination strategies for measles, earlier vaccination for EV71 infection, and development and provision of a CoxA16 vaccine should be investigated and considered in the future,” concluded the researchers.
FROM VACCINE
Children with HIV benefit from double dose of PCV13 vaccine
, while children with kidney or lung disease may need only one dose, reported Sabelle Jallow, PhD, of the University of the Witwatersrand, Johannesburg, South Africa, and associates.
An open-label study was conducted at Chris Hani Baragwanath Academic Hospital (CHBAH) in Soweto, South Africa, to determine the immunogenicity of one and two doses of PCV13 in vaccine-naive children with HIV infection, kidney disease, or lung disease. Of the 112 children in the study, there were 50 HIV-infected children, 8 children with kidney disease, 9 with lung disease, and 45 HIV-uninfected control children with no chronic illness. The average age at enrollment was 62 months, 53% of participants were female, and 96% were of black African descent. At-risk children were given two doses of PCV13, 2 months apart, while control children received only one PCV13 dose (Vaccine. 2017. doi: 10.1016/j.vaccine.2017.06.081).
“In future studies, a larger spectrum of comorbidities should be included to determine the most cost-effective vaccination regimens particularly in low income countries,” the researchers noted.
, while children with kidney or lung disease may need only one dose, reported Sabelle Jallow, PhD, of the University of the Witwatersrand, Johannesburg, South Africa, and associates.
An open-label study was conducted at Chris Hani Baragwanath Academic Hospital (CHBAH) in Soweto, South Africa, to determine the immunogenicity of one and two doses of PCV13 in vaccine-naive children with HIV infection, kidney disease, or lung disease. Of the 112 children in the study, there were 50 HIV-infected children, 8 children with kidney disease, 9 with lung disease, and 45 HIV-uninfected control children with no chronic illness. The average age at enrollment was 62 months, 53% of participants were female, and 96% were of black African descent. At-risk children were given two doses of PCV13, 2 months apart, while control children received only one PCV13 dose (Vaccine. 2017. doi: 10.1016/j.vaccine.2017.06.081).
“In future studies, a larger spectrum of comorbidities should be included to determine the most cost-effective vaccination regimens particularly in low income countries,” the researchers noted.
, while children with kidney or lung disease may need only one dose, reported Sabelle Jallow, PhD, of the University of the Witwatersrand, Johannesburg, South Africa, and associates.
An open-label study was conducted at Chris Hani Baragwanath Academic Hospital (CHBAH) in Soweto, South Africa, to determine the immunogenicity of one and two doses of PCV13 in vaccine-naive children with HIV infection, kidney disease, or lung disease. Of the 112 children in the study, there were 50 HIV-infected children, 8 children with kidney disease, 9 with lung disease, and 45 HIV-uninfected control children with no chronic illness. The average age at enrollment was 62 months, 53% of participants were female, and 96% were of black African descent. At-risk children were given two doses of PCV13, 2 months apart, while control children received only one PCV13 dose (Vaccine. 2017. doi: 10.1016/j.vaccine.2017.06.081).
“In future studies, a larger spectrum of comorbidities should be included to determine the most cost-effective vaccination regimens particularly in low income countries,” the researchers noted.
FROM VACCINE
Study indicates parent-reported penicillin allergy in question
, according to David Vyles, DO, and his associates at the Medical College of Wisconsin, Milwaukee.
Because there is no process to safely and rapidly diagnose true penicillin allergy in a critical care setting, pediatric providers are reluctant to prescribe penicillin to children with a reported allergy. In this study, a three-tier penicillin testing process was used to evaluate the accuracy of a parent-reported penicillin allergy questionnaire in identifying children likely to be at low risk for penicillin allergy in an ED setting.
“Our results in the current study highlight that the high percentage of patients reporting a penicillin allergy to medical providers are likely inconsistent with true allergy,” concluded Dr. Vyles and his associates.
Read more at Pediatrics (2017. doi: 10.1542/peds.2017-0471).
, according to David Vyles, DO, and his associates at the Medical College of Wisconsin, Milwaukee.
Because there is no process to safely and rapidly diagnose true penicillin allergy in a critical care setting, pediatric providers are reluctant to prescribe penicillin to children with a reported allergy. In this study, a three-tier penicillin testing process was used to evaluate the accuracy of a parent-reported penicillin allergy questionnaire in identifying children likely to be at low risk for penicillin allergy in an ED setting.
“Our results in the current study highlight that the high percentage of patients reporting a penicillin allergy to medical providers are likely inconsistent with true allergy,” concluded Dr. Vyles and his associates.
Read more at Pediatrics (2017. doi: 10.1542/peds.2017-0471).
, according to David Vyles, DO, and his associates at the Medical College of Wisconsin, Milwaukee.
Because there is no process to safely and rapidly diagnose true penicillin allergy in a critical care setting, pediatric providers are reluctant to prescribe penicillin to children with a reported allergy. In this study, a three-tier penicillin testing process was used to evaluate the accuracy of a parent-reported penicillin allergy questionnaire in identifying children likely to be at low risk for penicillin allergy in an ED setting.
“Our results in the current study highlight that the high percentage of patients reporting a penicillin allergy to medical providers are likely inconsistent with true allergy,” concluded Dr. Vyles and his associates.
Read more at Pediatrics (2017. doi: 10.1542/peds.2017-0471).
FROM PEDIATRICS
Daily probiotics have no effect on infections causing child care absences
Results of a double-blind, placebo-controlled study do not support use of probiotics to prevent upper respiratory and gastrointestinal infections in children aged 8-14 months at enrollment, as the probiotics did not reduce infection-related child care absences.
In the study of 290 Danish infants randomly allocated to receive a placebo or a combination of Bifidobacterium animalis subsp lactis (BB-12) and Lactobacillus rhamnosus (LGG) in a dose of 109 colony-forming units of each daily for a 6-month intervention period, there were no differences in absences from child care between the two groups (1.14 days; 95% confidence interval, −0.55 to 2.82), reported Rikke Pilmann Laursen, MSc, and her associates at the University of Copenhagen (Pediatrics. 2017. doi: 10.1542/peds.2017-0735).
Infants were a mean 10 months old at baseline, and 47% were still breastfeeding. The mean age at breastfeeding discontinuation was 12 months.
In terms of the number of children with one or more episodes of an upper respiratory tract infection, the LGG and BB-12 vs. placebo odds ratio was 1.22 (95% CI, 0.74-2.00; P = .43). The number of children with one or more episodes of diarrhea in the LGG and BB-12 vs. placebo odds ratio was 1.42 (95% CI, 0.88-2.32; P = .15).
The effect of probiotics in preventing infections in preschool-aged children has been explored in several studies and recent reviews, suggesting an effect specifically on upper respiratory tract and GI infections in small children. This study diverges in that it examined the effect of a combination of probiotics on absences from child care related to those infections in infants aged 8-14 months at the time of enrollment, whereas previous studies focused on children older than 1 year.
This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
Any intervention that can prevent child care–associated illnesses can have economic and educational implications, as well as public health ones. However, in the Laursen et al. study, almost 47% of the infants enrolled were breastfed, as opposed to previous studies in which the children participating generally were over 1 year old.
Given the positive effects of breastfeeding in preventing infections and the high percentage of infants who were breastfed in this study, it may be harder to distinguish the effects of the probiotic supplement in the Laursen et al. study. Indirectly, this study suggests additional information on the relative value of a probiotic intervention, compared with breastfeeding and diet, is warranted, and perhaps there is another reason to encourage breastfeeding as long as possible.
Michael D. Cabana, MD, MPH, is a professor of pediatrics, epidemiology and biostatistics and a member of the faculty at the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco. Daniel J. Merenstein, MD, is an associate professor of family medicine at Georgetown University, Washington. Pharmavite, Bayer, and Sanofi have provided Georgetown University with consulting funding. Both physicians, who commented in an editorial accompanying the article by Laursen et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1729), disclosed no financial relationships relevant to this article. Dr. Merenstein has been an expert witness for Proctor & Gamble while Dr. Cabana has served as a consultant for BioGaia, Nestle, Mead Johnson, and Wyeth.
Any intervention that can prevent child care–associated illnesses can have economic and educational implications, as well as public health ones. However, in the Laursen et al. study, almost 47% of the infants enrolled were breastfed, as opposed to previous studies in which the children participating generally were over 1 year old.
Given the positive effects of breastfeeding in preventing infections and the high percentage of infants who were breastfed in this study, it may be harder to distinguish the effects of the probiotic supplement in the Laursen et al. study. Indirectly, this study suggests additional information on the relative value of a probiotic intervention, compared with breastfeeding and diet, is warranted, and perhaps there is another reason to encourage breastfeeding as long as possible.
Michael D. Cabana, MD, MPH, is a professor of pediatrics, epidemiology and biostatistics and a member of the faculty at the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco. Daniel J. Merenstein, MD, is an associate professor of family medicine at Georgetown University, Washington. Pharmavite, Bayer, and Sanofi have provided Georgetown University with consulting funding. Both physicians, who commented in an editorial accompanying the article by Laursen et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1729), disclosed no financial relationships relevant to this article. Dr. Merenstein has been an expert witness for Proctor & Gamble while Dr. Cabana has served as a consultant for BioGaia, Nestle, Mead Johnson, and Wyeth.
Any intervention that can prevent child care–associated illnesses can have economic and educational implications, as well as public health ones. However, in the Laursen et al. study, almost 47% of the infants enrolled were breastfed, as opposed to previous studies in which the children participating generally were over 1 year old.
Given the positive effects of breastfeeding in preventing infections and the high percentage of infants who were breastfed in this study, it may be harder to distinguish the effects of the probiotic supplement in the Laursen et al. study. Indirectly, this study suggests additional information on the relative value of a probiotic intervention, compared with breastfeeding and diet, is warranted, and perhaps there is another reason to encourage breastfeeding as long as possible.
Michael D. Cabana, MD, MPH, is a professor of pediatrics, epidemiology and biostatistics and a member of the faculty at the Philip R. Lee Institute for Health Policy Studies at the University of California, San Francisco. Daniel J. Merenstein, MD, is an associate professor of family medicine at Georgetown University, Washington. Pharmavite, Bayer, and Sanofi have provided Georgetown University with consulting funding. Both physicians, who commented in an editorial accompanying the article by Laursen et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1729), disclosed no financial relationships relevant to this article. Dr. Merenstein has been an expert witness for Proctor & Gamble while Dr. Cabana has served as a consultant for BioGaia, Nestle, Mead Johnson, and Wyeth.
Results of a double-blind, placebo-controlled study do not support use of probiotics to prevent upper respiratory and gastrointestinal infections in children aged 8-14 months at enrollment, as the probiotics did not reduce infection-related child care absences.
In the study of 290 Danish infants randomly allocated to receive a placebo or a combination of Bifidobacterium animalis subsp lactis (BB-12) and Lactobacillus rhamnosus (LGG) in a dose of 109 colony-forming units of each daily for a 6-month intervention period, there were no differences in absences from child care between the two groups (1.14 days; 95% confidence interval, −0.55 to 2.82), reported Rikke Pilmann Laursen, MSc, and her associates at the University of Copenhagen (Pediatrics. 2017. doi: 10.1542/peds.2017-0735).
Infants were a mean 10 months old at baseline, and 47% were still breastfeeding. The mean age at breastfeeding discontinuation was 12 months.
In terms of the number of children with one or more episodes of an upper respiratory tract infection, the LGG and BB-12 vs. placebo odds ratio was 1.22 (95% CI, 0.74-2.00; P = .43). The number of children with one or more episodes of diarrhea in the LGG and BB-12 vs. placebo odds ratio was 1.42 (95% CI, 0.88-2.32; P = .15).
The effect of probiotics in preventing infections in preschool-aged children has been explored in several studies and recent reviews, suggesting an effect specifically on upper respiratory tract and GI infections in small children. This study diverges in that it examined the effect of a combination of probiotics on absences from child care related to those infections in infants aged 8-14 months at the time of enrollment, whereas previous studies focused on children older than 1 year.
This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
Results of a double-blind, placebo-controlled study do not support use of probiotics to prevent upper respiratory and gastrointestinal infections in children aged 8-14 months at enrollment, as the probiotics did not reduce infection-related child care absences.
In the study of 290 Danish infants randomly allocated to receive a placebo or a combination of Bifidobacterium animalis subsp lactis (BB-12) and Lactobacillus rhamnosus (LGG) in a dose of 109 colony-forming units of each daily for a 6-month intervention period, there were no differences in absences from child care between the two groups (1.14 days; 95% confidence interval, −0.55 to 2.82), reported Rikke Pilmann Laursen, MSc, and her associates at the University of Copenhagen (Pediatrics. 2017. doi: 10.1542/peds.2017-0735).
Infants were a mean 10 months old at baseline, and 47% were still breastfeeding. The mean age at breastfeeding discontinuation was 12 months.
In terms of the number of children with one or more episodes of an upper respiratory tract infection, the LGG and BB-12 vs. placebo odds ratio was 1.22 (95% CI, 0.74-2.00; P = .43). The number of children with one or more episodes of diarrhea in the LGG and BB-12 vs. placebo odds ratio was 1.42 (95% CI, 0.88-2.32; P = .15).
The effect of probiotics in preventing infections in preschool-aged children has been explored in several studies and recent reviews, suggesting an effect specifically on upper respiratory tract and GI infections in small children. This study diverges in that it examined the effect of a combination of probiotics on absences from child care related to those infections in infants aged 8-14 months at the time of enrollment, whereas previous studies focused on children older than 1 year.
This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: Intention-to-treat analysis showed no difference between the probiotics and placebo study groups.
Data source: A randomized, double-blind, placebo-controlled study of 290 infants aged 8-14 months at enrollment.
Disclosures: This study was funded by Innovation Fund Denmark, the University of Copenhagen, and Chr Hansen A/S. Dr. Kim Fleischer Michaelsen and Dr. Christian Mølgaard received a grant from Chr Hansen for the current study. None of the other investigators had any relevant financial disclosures.
Clearer instructions linked to fewer medication dosing errors
In nine pediatric dosing trials, more than 80% of parents made more than one medication dosing error, according to a study by H. Shonna Yin, MD, and associates. Misunderstandings about how to accurately choose the right dosing tools as well as confusion related to units of measure contribute to most errors. Matching dosing tools more closely with prescribed dose volumes, as well as using pictograms, can greatly reduce the number of pediatric medication errors, the researchers noted.
The study shows that 83.5% of parents made at least one dosing error (overdosing was present in 12.1% of errors), and 29.3% of parents made at least one large error in administering their children’s medicine. Parents who received text-only instructions or milliliter/teaspoon labels made more large errors. The biggest influence on errors resulted from providing tools more closely matched to the recommended dose measurements.
The researchers conducted a randomized controlled experiment in three pediatric clinics. Each site’s institutional review board approved the study. An average of 491 parents of children older than 8 years were randomly assigned to one of four groups, and given labels and dosing tools that varied in label instruction format and units. Each parent measured nine doses of liquid medicine in a random order, using three different tools.
Parents in group 1 received text and pictogram dosing instructions with milliliter-only labels and tools. They had decreased odds of making a dosing error compared with parents who received milliliter/teaspoon labels and tools without pictographic instructions in groups 2 and 4, and had lower odds of making large dosing errors compared with group 3, whose participants received text-only instructions (Pediatrics. 2017 June 27. doi: 10.1542/peds.2016-3237).
“Our findings support the use of a specific algorithm to help health care providers and pharmacists determine which dosing tool is most optimal to provide to parents,” said Dr. Yin. “We found that pictograms were associated with statistically significant reductions in large overdosing errors, with a trend for reduction in any error.”
No financial disclosures or conflicts of interest were reported.
In nine pediatric dosing trials, more than 80% of parents made more than one medication dosing error, according to a study by H. Shonna Yin, MD, and associates. Misunderstandings about how to accurately choose the right dosing tools as well as confusion related to units of measure contribute to most errors. Matching dosing tools more closely with prescribed dose volumes, as well as using pictograms, can greatly reduce the number of pediatric medication errors, the researchers noted.
The study shows that 83.5% of parents made at least one dosing error (overdosing was present in 12.1% of errors), and 29.3% of parents made at least one large error in administering their children’s medicine. Parents who received text-only instructions or milliliter/teaspoon labels made more large errors. The biggest influence on errors resulted from providing tools more closely matched to the recommended dose measurements.
The researchers conducted a randomized controlled experiment in three pediatric clinics. Each site’s institutional review board approved the study. An average of 491 parents of children older than 8 years were randomly assigned to one of four groups, and given labels and dosing tools that varied in label instruction format and units. Each parent measured nine doses of liquid medicine in a random order, using three different tools.
Parents in group 1 received text and pictogram dosing instructions with milliliter-only labels and tools. They had decreased odds of making a dosing error compared with parents who received milliliter/teaspoon labels and tools without pictographic instructions in groups 2 and 4, and had lower odds of making large dosing errors compared with group 3, whose participants received text-only instructions (Pediatrics. 2017 June 27. doi: 10.1542/peds.2016-3237).
“Our findings support the use of a specific algorithm to help health care providers and pharmacists determine which dosing tool is most optimal to provide to parents,” said Dr. Yin. “We found that pictograms were associated with statistically significant reductions in large overdosing errors, with a trend for reduction in any error.”
No financial disclosures or conflicts of interest were reported.
In nine pediatric dosing trials, more than 80% of parents made more than one medication dosing error, according to a study by H. Shonna Yin, MD, and associates. Misunderstandings about how to accurately choose the right dosing tools as well as confusion related to units of measure contribute to most errors. Matching dosing tools more closely with prescribed dose volumes, as well as using pictograms, can greatly reduce the number of pediatric medication errors, the researchers noted.
The study shows that 83.5% of parents made at least one dosing error (overdosing was present in 12.1% of errors), and 29.3% of parents made at least one large error in administering their children’s medicine. Parents who received text-only instructions or milliliter/teaspoon labels made more large errors. The biggest influence on errors resulted from providing tools more closely matched to the recommended dose measurements.
The researchers conducted a randomized controlled experiment in three pediatric clinics. Each site’s institutional review board approved the study. An average of 491 parents of children older than 8 years were randomly assigned to one of four groups, and given labels and dosing tools that varied in label instruction format and units. Each parent measured nine doses of liquid medicine in a random order, using three different tools.
Parents in group 1 received text and pictogram dosing instructions with milliliter-only labels and tools. They had decreased odds of making a dosing error compared with parents who received milliliter/teaspoon labels and tools without pictographic instructions in groups 2 and 4, and had lower odds of making large dosing errors compared with group 3, whose participants received text-only instructions (Pediatrics. 2017 June 27. doi: 10.1542/peds.2016-3237).
“Our findings support the use of a specific algorithm to help health care providers and pharmacists determine which dosing tool is most optimal to provide to parents,” said Dr. Yin. “We found that pictograms were associated with statistically significant reductions in large overdosing errors, with a trend for reduction in any error.”
No financial disclosures or conflicts of interest were reported.
FROM PEDIATRICS
Key clinical point:
Major finding: In nine dosing trials, 83.5% of parents made more than one medication dosing error, mainly overdosing.
Data source: A randomized controlled study. Recruitment took place in pediatric outpatient clinics in New York, California, and Georgia. Each site’s institutional review board approved the study.
Disclosures: The National Institutes of Health/National Institute of Child Health and Human Development funded the study. The authors declared no conflict of interest.
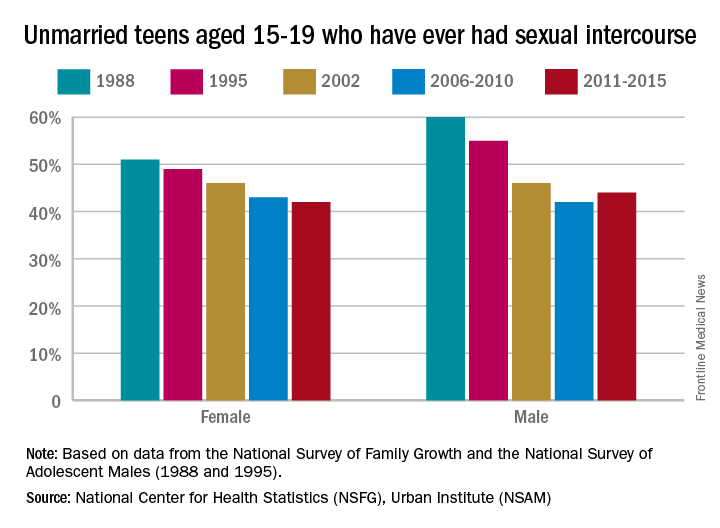
Less sex, more contraception use in teens in last decade
, according to a report by Joyce C. Abma, PhD, and Gladys M. Martinez, PhD, of the Division of Vital Statistics at the National Center for Health Statistics, Hyattsville, Md.
The percentage of female teens who had ever had sexual intercourse declined from 51% in 1988 to 42% in 2011-2015. For male teens, the percentage who were sexually experienced declined from 60% in 1988 to 44% in 2011-2015.
Male teens’ condom use during their first sexual experiences increased from 71% in 2002 to 77% in 2011-2015. This plateau in male contraception is in part the result of various types of contraception for women being developed and widely distributed in the course of these years, such as intrauterine devices.
The report features the most recent data from the National Survey of Family Growth (NSFG), resulting in 4 years of interviews spanning 2011 through 2015 and including 2,047 female teens and 2,087 male teens aged 15-19 years (National Health Statistics Reports; no 104. Hyattsville, MD: National Center for Health Statistics. 2017). Data also was abstracted from the 1988 and 1995 National Surveys of Adolescent Males, a national panel survey of male teens.
NSFG is currently the only source of ongoing data on the topics of sexual activity and contraceptive use for the total U.S. population of teenagers, paralleling the teen population whose pregnancy and birth rates are captured by birth certificates as part of the statistics of the National Center for Health Statistics. “Using data from the 2011-2015 NSFG and earlier NSFG surveys, this report provides an update of information on U.S. teenagers’ sexual activity and contraceptive use, thus helping to improve understanding of their risk of pregnancy,” said Dr. Abma and her associates. “This report … provides insights into the ways in which those determinants are changing with time, how they differ by sociodemographic groups, and what circumstances are most associated with them. The information can be used to monitor and understand trends in teen sexual behavior and contraception use.”
The 2011-2015 National Survey of Family Growth was conducted by the National Center for Health Statistics with the support and assistance of a number of other organizations and individuals. Interviewing and other tasks were carried out by the University of Michigan’s Survey Research Center and the Institute for Social Research under a contract with NCHS.
, according to a report by Joyce C. Abma, PhD, and Gladys M. Martinez, PhD, of the Division of Vital Statistics at the National Center for Health Statistics, Hyattsville, Md.
The percentage of female teens who had ever had sexual intercourse declined from 51% in 1988 to 42% in 2011-2015. For male teens, the percentage who were sexually experienced declined from 60% in 1988 to 44% in 2011-2015.
Male teens’ condom use during their first sexual experiences increased from 71% in 2002 to 77% in 2011-2015. This plateau in male contraception is in part the result of various types of contraception for women being developed and widely distributed in the course of these years, such as intrauterine devices.
The report features the most recent data from the National Survey of Family Growth (NSFG), resulting in 4 years of interviews spanning 2011 through 2015 and including 2,047 female teens and 2,087 male teens aged 15-19 years (National Health Statistics Reports; no 104. Hyattsville, MD: National Center for Health Statistics. 2017). Data also was abstracted from the 1988 and 1995 National Surveys of Adolescent Males, a national panel survey of male teens.
NSFG is currently the only source of ongoing data on the topics of sexual activity and contraceptive use for the total U.S. population of teenagers, paralleling the teen population whose pregnancy and birth rates are captured by birth certificates as part of the statistics of the National Center for Health Statistics. “Using data from the 2011-2015 NSFG and earlier NSFG surveys, this report provides an update of information on U.S. teenagers’ sexual activity and contraceptive use, thus helping to improve understanding of their risk of pregnancy,” said Dr. Abma and her associates. “This report … provides insights into the ways in which those determinants are changing with time, how they differ by sociodemographic groups, and what circumstances are most associated with them. The information can be used to monitor and understand trends in teen sexual behavior and contraception use.”
The 2011-2015 National Survey of Family Growth was conducted by the National Center for Health Statistics with the support and assistance of a number of other organizations and individuals. Interviewing and other tasks were carried out by the University of Michigan’s Survey Research Center and the Institute for Social Research under a contract with NCHS.
, according to a report by Joyce C. Abma, PhD, and Gladys M. Martinez, PhD, of the Division of Vital Statistics at the National Center for Health Statistics, Hyattsville, Md.
The percentage of female teens who had ever had sexual intercourse declined from 51% in 1988 to 42% in 2011-2015. For male teens, the percentage who were sexually experienced declined from 60% in 1988 to 44% in 2011-2015.
Male teens’ condom use during their first sexual experiences increased from 71% in 2002 to 77% in 2011-2015. This plateau in male contraception is in part the result of various types of contraception for women being developed and widely distributed in the course of these years, such as intrauterine devices.
The report features the most recent data from the National Survey of Family Growth (NSFG), resulting in 4 years of interviews spanning 2011 through 2015 and including 2,047 female teens and 2,087 male teens aged 15-19 years (National Health Statistics Reports; no 104. Hyattsville, MD: National Center for Health Statistics. 2017). Data also was abstracted from the 1988 and 1995 National Surveys of Adolescent Males, a national panel survey of male teens.
NSFG is currently the only source of ongoing data on the topics of sexual activity and contraceptive use for the total U.S. population of teenagers, paralleling the teen population whose pregnancy and birth rates are captured by birth certificates as part of the statistics of the National Center for Health Statistics. “Using data from the 2011-2015 NSFG and earlier NSFG surveys, this report provides an update of information on U.S. teenagers’ sexual activity and contraceptive use, thus helping to improve understanding of their risk of pregnancy,” said Dr. Abma and her associates. “This report … provides insights into the ways in which those determinants are changing with time, how they differ by sociodemographic groups, and what circumstances are most associated with them. The information can be used to monitor and understand trends in teen sexual behavior and contraception use.”
The 2011-2015 National Survey of Family Growth was conducted by the National Center for Health Statistics with the support and assistance of a number of other organizations and individuals. Interviewing and other tasks were carried out by the University of Michigan’s Survey Research Center and the Institute for Social Research under a contract with NCHS.
FROM NATIONAL HEALTH STATISTICS REPORTS
Key clinical point: Contraception use has gone up in the last decade
Major finding: Contraception use has increased to 99% in girls and 77% in boys in the last decade.
Data source: This report presents U.S. data on the sexual activity and contraceptive use of males and females aged 15-19 years, using data from the 2011-2015 and earlier National Surveys of Family Growth and the 1988 and 1995 National Surveys of Adolescent Males.
Disclosures: The 2011-2015 National Survey of Family Growth was conducted by the National Center for Health Statistics with the support and assistance of a number of other organizations and individuals. Interviewing and other tasks were carried out by the University of Michigan’s Survey Research Center and the Institute for Social Research under a contract with NCHS.
Child firearm suicide at highest rate in more than a decade
Boys, older children, and minorities are disproportionately affected when it comes to firearm injuries and deaths in U.S. children and adolescents, and child firearm suicide rates are at the highest they have been in more than a decade, new study results revealed.
Around 19 children are either medically treated for a gunshot wound or killed by one every day in the United States. “The majority of these children are boys 13-17 years old, African American in the case of firearm homicide, and white and American Indian in the case of firearm suicide. Pediatric firearm injuries and deaths are an important public health problem in the United States, contributing substantially each year to premature death, illness, and disability of children,” said Katherine A. Fowler, PhD, of the National Center for Injury Prevention and Control, Atlanta, and her associates. “Finding ways to prevent such injuries and ensure that all children have safe, stable, nurturing relationships and environments remains one of our most important priorities” (Pediatrics. 2017;140(1):e20163486).
“From 2012 to 2014, the average annual case fatality rate was 74% for firearm-related self-harm, 14% for firearm-related assaults, and 6% for unintentional firearm injuries,” the investigators reported.
Boys accounted for 82% of all child firearm deaths from 2012 to 2014. In this time period, the annual rate of firearm death for boys was 4.5 times higher than the annual rate for girls (2.8 vs. 0.6 per 100,000). This difference was even more pronounced by age, with the rate for 13- to 17-year-old boys being six times higher than the rate for same-aged girls. Similarly, boys suffer the majority of nonfatal firearm injuries treated in U.S. emergency departments, accounting for 84% of all nonfatal firearm injuries medically treated each year from 2012 to 2014. The average annual rate of nonfatal firearm injuries for boys was five times the rate for girls at 13 vs. 3 per 100,000.
The annual rate of firearm homicide was 10 times higher among 13- to 17-year-olds versus 0- to 12-year-olds (3 vs. 0.3 per 100,000). Unintentional firearm death rates were approximately twice as high when comparing these two groups (0.2 vs. 0.1 per 100,000).
Dr. Fowler and her associates wrote, “Our findings indicate that most children who died of unintentional firearm injuries were shot by another child in their own age range and most often in the context of playing with a gun or showing it to others. More than one-third of the deaths of older children occurred in incidents in which the shooter thought that the gun was unloaded or thought that the safety was engaged.”
“Child firearm suicide rates showed a significant upward trend between 2007 and 2014, increasing 60% from 1.0 to 1.6 (P less than .05) to the highest rate seen over the period examined,” Dr. Fowler and her associates said.
Firearm suicide rates were 11 times higher among 13- to 17-year-olds vs. 10- to 12-year-olds (2 vs. 0.2 per 100,000). Older children also accounted for 88% of all nonfatal firearm injuries treated in an ED. The overall average annual rate of nonfatal firearm injuries for older children was 19 times that of younger children (24 vs. 1 per 100,000).
The annual firearm homicide rate for African American children was nearly 10 times higher than the rate for white children (4 vs. 0.4 per 100,000). However, the annual rate of firearm suicide among white children was nearly four times higher than the rate for African American children (2. vs. 0.6 per 100,000).
Awareness of the availability of firearms during times of crisis is crucial because suicides are often impulsive in young people, Dr. Fowler and her associates said, “with previous findings indicating that many who attempt suicide spend 10 minutes or less deliberating. Safe storage practices (i.e., unloading and locking all firearms and ammunition) can potentially be lifesaving in these instances,” as the results of previous studies in this age group attest.
Firearm deaths are the third leading cause of death overall among children in the United States aged 1-17 years, beating pediatric congenital anomalies, heart disease, influenza/pneumonia, chronic lower respiratory disease, and cerebrovascular causes. Understanding the nature, scale, and impact of firearm violence against children is an important first step, concluded Dr. Fowler and her associates.
Dr. Fowler and her associates said they had no relevant financial disclosures.
Dr. Fowler’s study brings a lot of uncomfortable statistics to light. Subsequently we are left wondering, What can we do about it? With firearm injury mortality rates in children increasing over the past 2 years according to the CDC’s Web-based Injury Statistics Query and Reporting System, it is crucial that we continue to demand the appropriate support for this public health crisis.
Recognizing the prevalence of guns in homes and the potential dangers of easy access to them makes it essential to ask about firearms as part of our injury prevention guidance and offer counseling to parents and children about safe gun storage, gun locks, or support for legislation to protect children from gun violence.
It is important to engage gun owners about gun safety and “point out that parents may underestimate kids’ propensity to handle guns unsafely, even when they’ve been taught,” as well as the “impulsivity, risk-taking, and unpredictability of adolescence. ... We pediatric clinicians tend not to discuss firearm injury prevention much,” but a recent review of the problem offers some excellent guidance that “may help us to do more,” according to Dr. Nelson (Adolesc Med State Art Rev. 2016;27[2]:323-40).
However problematic it may be to confront the problem of firearm injuries in children and adolescents, we cannot ignore the scale of this current epidemic.
Eliot W. Nelson, MD, is a pediatrician at the University of Vermont Children’s Hospital. He reported having no relevant financial disclosures. These remarks are adapted from an editorial accompanying the report by Fowler et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1300).
Dr. Fowler’s study brings a lot of uncomfortable statistics to light. Subsequently we are left wondering, What can we do about it? With firearm injury mortality rates in children increasing over the past 2 years according to the CDC’s Web-based Injury Statistics Query and Reporting System, it is crucial that we continue to demand the appropriate support for this public health crisis.
Recognizing the prevalence of guns in homes and the potential dangers of easy access to them makes it essential to ask about firearms as part of our injury prevention guidance and offer counseling to parents and children about safe gun storage, gun locks, or support for legislation to protect children from gun violence.
It is important to engage gun owners about gun safety and “point out that parents may underestimate kids’ propensity to handle guns unsafely, even when they’ve been taught,” as well as the “impulsivity, risk-taking, and unpredictability of adolescence. ... We pediatric clinicians tend not to discuss firearm injury prevention much,” but a recent review of the problem offers some excellent guidance that “may help us to do more,” according to Dr. Nelson (Adolesc Med State Art Rev. 2016;27[2]:323-40).
However problematic it may be to confront the problem of firearm injuries in children and adolescents, we cannot ignore the scale of this current epidemic.
Eliot W. Nelson, MD, is a pediatrician at the University of Vermont Children’s Hospital. He reported having no relevant financial disclosures. These remarks are adapted from an editorial accompanying the report by Fowler et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1300).
Dr. Fowler’s study brings a lot of uncomfortable statistics to light. Subsequently we are left wondering, What can we do about it? With firearm injury mortality rates in children increasing over the past 2 years according to the CDC’s Web-based Injury Statistics Query and Reporting System, it is crucial that we continue to demand the appropriate support for this public health crisis.
Recognizing the prevalence of guns in homes and the potential dangers of easy access to them makes it essential to ask about firearms as part of our injury prevention guidance and offer counseling to parents and children about safe gun storage, gun locks, or support for legislation to protect children from gun violence.
It is important to engage gun owners about gun safety and “point out that parents may underestimate kids’ propensity to handle guns unsafely, even when they’ve been taught,” as well as the “impulsivity, risk-taking, and unpredictability of adolescence. ... We pediatric clinicians tend not to discuss firearm injury prevention much,” but a recent review of the problem offers some excellent guidance that “may help us to do more,” according to Dr. Nelson (Adolesc Med State Art Rev. 2016;27[2]:323-40).
However problematic it may be to confront the problem of firearm injuries in children and adolescents, we cannot ignore the scale of this current epidemic.
Eliot W. Nelson, MD, is a pediatrician at the University of Vermont Children’s Hospital. He reported having no relevant financial disclosures. These remarks are adapted from an editorial accompanying the report by Fowler et al. (Pediatrics. 2017. doi: 10.1542/peds.2017-1300).
Boys, older children, and minorities are disproportionately affected when it comes to firearm injuries and deaths in U.S. children and adolescents, and child firearm suicide rates are at the highest they have been in more than a decade, new study results revealed.
Around 19 children are either medically treated for a gunshot wound or killed by one every day in the United States. “The majority of these children are boys 13-17 years old, African American in the case of firearm homicide, and white and American Indian in the case of firearm suicide. Pediatric firearm injuries and deaths are an important public health problem in the United States, contributing substantially each year to premature death, illness, and disability of children,” said Katherine A. Fowler, PhD, of the National Center for Injury Prevention and Control, Atlanta, and her associates. “Finding ways to prevent such injuries and ensure that all children have safe, stable, nurturing relationships and environments remains one of our most important priorities” (Pediatrics. 2017;140(1):e20163486).
“From 2012 to 2014, the average annual case fatality rate was 74% for firearm-related self-harm, 14% for firearm-related assaults, and 6% for unintentional firearm injuries,” the investigators reported.
Boys accounted for 82% of all child firearm deaths from 2012 to 2014. In this time period, the annual rate of firearm death for boys was 4.5 times higher than the annual rate for girls (2.8 vs. 0.6 per 100,000). This difference was even more pronounced by age, with the rate for 13- to 17-year-old boys being six times higher than the rate for same-aged girls. Similarly, boys suffer the majority of nonfatal firearm injuries treated in U.S. emergency departments, accounting for 84% of all nonfatal firearm injuries medically treated each year from 2012 to 2014. The average annual rate of nonfatal firearm injuries for boys was five times the rate for girls at 13 vs. 3 per 100,000.
The annual rate of firearm homicide was 10 times higher among 13- to 17-year-olds versus 0- to 12-year-olds (3 vs. 0.3 per 100,000). Unintentional firearm death rates were approximately twice as high when comparing these two groups (0.2 vs. 0.1 per 100,000).
Dr. Fowler and her associates wrote, “Our findings indicate that most children who died of unintentional firearm injuries were shot by another child in their own age range and most often in the context of playing with a gun or showing it to others. More than one-third of the deaths of older children occurred in incidents in which the shooter thought that the gun was unloaded or thought that the safety was engaged.”
“Child firearm suicide rates showed a significant upward trend between 2007 and 2014, increasing 60% from 1.0 to 1.6 (P less than .05) to the highest rate seen over the period examined,” Dr. Fowler and her associates said.
Firearm suicide rates were 11 times higher among 13- to 17-year-olds vs. 10- to 12-year-olds (2 vs. 0.2 per 100,000). Older children also accounted for 88% of all nonfatal firearm injuries treated in an ED. The overall average annual rate of nonfatal firearm injuries for older children was 19 times that of younger children (24 vs. 1 per 100,000).
The annual firearm homicide rate for African American children was nearly 10 times higher than the rate for white children (4 vs. 0.4 per 100,000). However, the annual rate of firearm suicide among white children was nearly four times higher than the rate for African American children (2. vs. 0.6 per 100,000).
Awareness of the availability of firearms during times of crisis is crucial because suicides are often impulsive in young people, Dr. Fowler and her associates said, “with previous findings indicating that many who attempt suicide spend 10 minutes or less deliberating. Safe storage practices (i.e., unloading and locking all firearms and ammunition) can potentially be lifesaving in these instances,” as the results of previous studies in this age group attest.
Firearm deaths are the third leading cause of death overall among children in the United States aged 1-17 years, beating pediatric congenital anomalies, heart disease, influenza/pneumonia, chronic lower respiratory disease, and cerebrovascular causes. Understanding the nature, scale, and impact of firearm violence against children is an important first step, concluded Dr. Fowler and her associates.
Dr. Fowler and her associates said they had no relevant financial disclosures.
Boys, older children, and minorities are disproportionately affected when it comes to firearm injuries and deaths in U.S. children and adolescents, and child firearm suicide rates are at the highest they have been in more than a decade, new study results revealed.
Around 19 children are either medically treated for a gunshot wound or killed by one every day in the United States. “The majority of these children are boys 13-17 years old, African American in the case of firearm homicide, and white and American Indian in the case of firearm suicide. Pediatric firearm injuries and deaths are an important public health problem in the United States, contributing substantially each year to premature death, illness, and disability of children,” said Katherine A. Fowler, PhD, of the National Center for Injury Prevention and Control, Atlanta, and her associates. “Finding ways to prevent such injuries and ensure that all children have safe, stable, nurturing relationships and environments remains one of our most important priorities” (Pediatrics. 2017;140(1):e20163486).
“From 2012 to 2014, the average annual case fatality rate was 74% for firearm-related self-harm, 14% for firearm-related assaults, and 6% for unintentional firearm injuries,” the investigators reported.
Boys accounted for 82% of all child firearm deaths from 2012 to 2014. In this time period, the annual rate of firearm death for boys was 4.5 times higher than the annual rate for girls (2.8 vs. 0.6 per 100,000). This difference was even more pronounced by age, with the rate for 13- to 17-year-old boys being six times higher than the rate for same-aged girls. Similarly, boys suffer the majority of nonfatal firearm injuries treated in U.S. emergency departments, accounting for 84% of all nonfatal firearm injuries medically treated each year from 2012 to 2014. The average annual rate of nonfatal firearm injuries for boys was five times the rate for girls at 13 vs. 3 per 100,000.
The annual rate of firearm homicide was 10 times higher among 13- to 17-year-olds versus 0- to 12-year-olds (3 vs. 0.3 per 100,000). Unintentional firearm death rates were approximately twice as high when comparing these two groups (0.2 vs. 0.1 per 100,000).
Dr. Fowler and her associates wrote, “Our findings indicate that most children who died of unintentional firearm injuries were shot by another child in their own age range and most often in the context of playing with a gun or showing it to others. More than one-third of the deaths of older children occurred in incidents in which the shooter thought that the gun was unloaded or thought that the safety was engaged.”
“Child firearm suicide rates showed a significant upward trend between 2007 and 2014, increasing 60% from 1.0 to 1.6 (P less than .05) to the highest rate seen over the period examined,” Dr. Fowler and her associates said.
Firearm suicide rates were 11 times higher among 13- to 17-year-olds vs. 10- to 12-year-olds (2 vs. 0.2 per 100,000). Older children also accounted for 88% of all nonfatal firearm injuries treated in an ED. The overall average annual rate of nonfatal firearm injuries for older children was 19 times that of younger children (24 vs. 1 per 100,000).
The annual firearm homicide rate for African American children was nearly 10 times higher than the rate for white children (4 vs. 0.4 per 100,000). However, the annual rate of firearm suicide among white children was nearly four times higher than the rate for African American children (2. vs. 0.6 per 100,000).
Awareness of the availability of firearms during times of crisis is crucial because suicides are often impulsive in young people, Dr. Fowler and her associates said, “with previous findings indicating that many who attempt suicide spend 10 minutes or less deliberating. Safe storage practices (i.e., unloading and locking all firearms and ammunition) can potentially be lifesaving in these instances,” as the results of previous studies in this age group attest.
Firearm deaths are the third leading cause of death overall among children in the United States aged 1-17 years, beating pediatric congenital anomalies, heart disease, influenza/pneumonia, chronic lower respiratory disease, and cerebrovascular causes. Understanding the nature, scale, and impact of firearm violence against children is an important first step, concluded Dr. Fowler and her associates.
Dr. Fowler and her associates said they had no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: Firearm suicide rates were 11 times higher among 13- to 17-year-olds versus 10- to 12-year-olds (2 vs. 0.2 per 100,000).
Data source: National 2012-2014 data from CDC’s National Vital Statistics System and the National Electronic Injury Surveillance System.
Disclosures: Dr. Fowler and her associates said they had no relevant financial disclosures.
Patients’ surrogate decision-makers face stress
WASHINGTON – Making health care–related decisions for relatives in the ICU heightens an individual’s risk for psychological stress, a new study showed.
While 90% of patients admitted to the ICU lack decision capacity, only 20%-29% of the U.S. population has written advanced directives. Therefore, most often, family members are called upon to make decisions for ICU patients’ care.
Sean Cohen, MD, of the University of Washington presented the study’s results in a mini symposium at an international conference of the American Thoracic Society in May.
In this cohort study, 265 patients with acute respiratory distress syndrome and 162 of these patients’ family members were surveyed 3 months after each patient’s discharge. Associations between the family members’ roles and psychological symptoms were examined with regression models. These models were adjusted for family characteristics, which included sex, age, education, and legal next-of-kin status. Results showed that the patients’ family members were on average 52 years of age and that 94% were white, 73% were female, and 64% were legal next-of-kin, mostly spouses or children of the patients.
“I think looking more at identification of the decision-making role and attempting to go toward the surrogates’ preferred role actually mitigates some of these psychological symptoms,” concluded Dr. Cohen.
This study was sponsored by the Cambia Palliative Care Center of Excellence at the University of Washington in Seattle. Funding was provided by the National Institutes of Health and the American Lung Association. The authors reported no other disclosures.
WASHINGTON – Making health care–related decisions for relatives in the ICU heightens an individual’s risk for psychological stress, a new study showed.
While 90% of patients admitted to the ICU lack decision capacity, only 20%-29% of the U.S. population has written advanced directives. Therefore, most often, family members are called upon to make decisions for ICU patients’ care.
Sean Cohen, MD, of the University of Washington presented the study’s results in a mini symposium at an international conference of the American Thoracic Society in May.
In this cohort study, 265 patients with acute respiratory distress syndrome and 162 of these patients’ family members were surveyed 3 months after each patient’s discharge. Associations between the family members’ roles and psychological symptoms were examined with regression models. These models were adjusted for family characteristics, which included sex, age, education, and legal next-of-kin status. Results showed that the patients’ family members were on average 52 years of age and that 94% were white, 73% were female, and 64% were legal next-of-kin, mostly spouses or children of the patients.
“I think looking more at identification of the decision-making role and attempting to go toward the surrogates’ preferred role actually mitigates some of these psychological symptoms,” concluded Dr. Cohen.
This study was sponsored by the Cambia Palliative Care Center of Excellence at the University of Washington in Seattle. Funding was provided by the National Institutes of Health and the American Lung Association. The authors reported no other disclosures.
WASHINGTON – Making health care–related decisions for relatives in the ICU heightens an individual’s risk for psychological stress, a new study showed.
While 90% of patients admitted to the ICU lack decision capacity, only 20%-29% of the U.S. population has written advanced directives. Therefore, most often, family members are called upon to make decisions for ICU patients’ care.
Sean Cohen, MD, of the University of Washington presented the study’s results in a mini symposium at an international conference of the American Thoracic Society in May.
In this cohort study, 265 patients with acute respiratory distress syndrome and 162 of these patients’ family members were surveyed 3 months after each patient’s discharge. Associations between the family members’ roles and psychological symptoms were examined with regression models. These models were adjusted for family characteristics, which included sex, age, education, and legal next-of-kin status. Results showed that the patients’ family members were on average 52 years of age and that 94% were white, 73% were female, and 64% were legal next-of-kin, mostly spouses or children of the patients.
“I think looking more at identification of the decision-making role and attempting to go toward the surrogates’ preferred role actually mitigates some of these psychological symptoms,” concluded Dr. Cohen.
This study was sponsored by the Cambia Palliative Care Center of Excellence at the University of Washington in Seattle. Funding was provided by the National Institutes of Health and the American Lung Association. The authors reported no other disclosures.
AT ATS 2017
Key clinical point:
Major finding: Patients’ family members’ active involvement in the health care decision-making process are more likely to experience symptoms of PTSD (OR, 4.43), depression (OR, 1.80), and anxiety (OR, 1.11; P less .05 for all).
Data source: Cohort study of 265 patients with ARDS and 162 family members of the patients.
Disclosures: This study was sponsored by the Cambia Palliative Care Center of Excellence at the University of Washington in Seattle. Funding was provided by the National Institutes of Health and the American Lung Association. The authors reported no other financial disclosures.
ATS conference participants shout for science
WASHINGTON – A group of about 60 individuals in lab coats marched through the rain from buses to Upper Senate Park on the evening of May 23, gathering in front of a raised podium in the park shadowed by the Capitol Building.
The demonstrators were trying to bring attention to recent policies that threaten to undermine research funding, tobacco regulation, affordable health care, clean air, and other advocacy priorities of the American Thoracic Society. The ATS had organized this rally – “Lab Coats for Lungs” – in conjunction with its international conference, which took place in Washington May 19-24.
“We rally today because we share growing anxiety that science in general, and our field in particular, is being dismissed in the halls of power,” ATS Vice President Polly Parsons, MD, announced from the podium.
Other speakers condemned the Trump administration’s proposals to scale down on environmental, health, and safety regulations, as well as proposed cuts to federal funding for scientific research, including an 18% reduction to National Institutes of Health funding.
Some speakers, including Gary Ewart, ATS chief of advocacy and government relations, and the event’s organizer, encouraged the crowd to raise their voices.
“Tell me what democracy looks like,” he yelled several times.
“This is what democracy looked like,” his fellow marchers shouted.
“What brought us the ability to transplant a lung and save a patient’s life who is dying of respiratory failure? What will cause the next breakthrough discovery? When our elected officials are looking for answers to challenging questions, what should they use for their guiding light?”
“Science!” bellowed the demonstrators, following each of Dr. Moss’s inquiries.
Some of the marchers wore pink lab coats rather than white, as a demonstration of women’s rights and gender equality in the field of science and medicine.
“The idea to wear pink coats was a result of discussions that mentioned that women’s rights were an integral part of the campaign for science, health, and clean air,” said ATS member Naftali Kaminski, MD. “Access to health care is critical to women, as is clean air. This why we chose to wear pink instead of white coats.”
Other speakers included Sen. Tom Carper (D-DE), Sen. Ed Markey (D-MA), pulmonary fibrosis patient advocate Teresa Barnes, and past ATS President David Gozal, MD.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – A group of about 60 individuals in lab coats marched through the rain from buses to Upper Senate Park on the evening of May 23, gathering in front of a raised podium in the park shadowed by the Capitol Building.
The demonstrators were trying to bring attention to recent policies that threaten to undermine research funding, tobacco regulation, affordable health care, clean air, and other advocacy priorities of the American Thoracic Society. The ATS had organized this rally – “Lab Coats for Lungs” – in conjunction with its international conference, which took place in Washington May 19-24.
“We rally today because we share growing anxiety that science in general, and our field in particular, is being dismissed in the halls of power,” ATS Vice President Polly Parsons, MD, announced from the podium.
Other speakers condemned the Trump administration’s proposals to scale down on environmental, health, and safety regulations, as well as proposed cuts to federal funding for scientific research, including an 18% reduction to National Institutes of Health funding.
Some speakers, including Gary Ewart, ATS chief of advocacy and government relations, and the event’s organizer, encouraged the crowd to raise their voices.
“Tell me what democracy looks like,” he yelled several times.
“This is what democracy looked like,” his fellow marchers shouted.
“What brought us the ability to transplant a lung and save a patient’s life who is dying of respiratory failure? What will cause the next breakthrough discovery? When our elected officials are looking for answers to challenging questions, what should they use for their guiding light?”
“Science!” bellowed the demonstrators, following each of Dr. Moss’s inquiries.
Some of the marchers wore pink lab coats rather than white, as a demonstration of women’s rights and gender equality in the field of science and medicine.
“The idea to wear pink coats was a result of discussions that mentioned that women’s rights were an integral part of the campaign for science, health, and clean air,” said ATS member Naftali Kaminski, MD. “Access to health care is critical to women, as is clean air. This why we chose to wear pink instead of white coats.”
Other speakers included Sen. Tom Carper (D-DE), Sen. Ed Markey (D-MA), pulmonary fibrosis patient advocate Teresa Barnes, and past ATS President David Gozal, MD.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
WASHINGTON – A group of about 60 individuals in lab coats marched through the rain from buses to Upper Senate Park on the evening of May 23, gathering in front of a raised podium in the park shadowed by the Capitol Building.
The demonstrators were trying to bring attention to recent policies that threaten to undermine research funding, tobacco regulation, affordable health care, clean air, and other advocacy priorities of the American Thoracic Society. The ATS had organized this rally – “Lab Coats for Lungs” – in conjunction with its international conference, which took place in Washington May 19-24.
“We rally today because we share growing anxiety that science in general, and our field in particular, is being dismissed in the halls of power,” ATS Vice President Polly Parsons, MD, announced from the podium.
Other speakers condemned the Trump administration’s proposals to scale down on environmental, health, and safety regulations, as well as proposed cuts to federal funding for scientific research, including an 18% reduction to National Institutes of Health funding.
Some speakers, including Gary Ewart, ATS chief of advocacy and government relations, and the event’s organizer, encouraged the crowd to raise their voices.
“Tell me what democracy looks like,” he yelled several times.
“This is what democracy looked like,” his fellow marchers shouted.
“What brought us the ability to transplant a lung and save a patient’s life who is dying of respiratory failure? What will cause the next breakthrough discovery? When our elected officials are looking for answers to challenging questions, what should they use for their guiding light?”
“Science!” bellowed the demonstrators, following each of Dr. Moss’s inquiries.
Some of the marchers wore pink lab coats rather than white, as a demonstration of women’s rights and gender equality in the field of science and medicine.
“The idea to wear pink coats was a result of discussions that mentioned that women’s rights were an integral part of the campaign for science, health, and clean air,” said ATS member Naftali Kaminski, MD. “Access to health care is critical to women, as is clean air. This why we chose to wear pink instead of white coats.”
Other speakers included Sen. Tom Carper (D-DE), Sen. Ed Markey (D-MA), pulmonary fibrosis patient advocate Teresa Barnes, and past ATS President David Gozal, MD.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ATS 2017