User login
OSA Endotypes and Phenotypes: Toward Personalized OSA Care
Obstructive sleep apnea (OSA) contributes a major health burden to society due to its high prevalence and substantial neurocognitive and cardiovascular consequences. Estimates suggest that at least 10% of adults in North America are afflicted with OSA, making it probably the most common respiratory disease in the developed world (Peppard et al. Am J Epidemiol. 2013;177[9]:1006). Nasal CPAP is a highly efficacious therapy that has been shown to improve neurocognitive and cardiovascular outcomes. However, CPAP is not always well tolerated. Alternative therapies, such as oral appliances and upper airway surgery, have highly variable efficacy, and evidence of important clinical benefits are uncertain. Therefore, efforts are ongoing to determine optimal alternative strategies for therapy.
In order to treat any condition optimally, one needs to be able to predict who is at highest risk of developing the condition, then to assess the consequences if left untreated, and finally to be able to predict response to various treatment options. Currently, the OSA field is still in its early stages of our understanding. Clinically, we are often faced with patients who have varying presentations and manifestations, but, for reasons that are unclear. For instance, two individuals with the same body mass index may have very different clinical manifestations, one with severe OSA and one without any OSA. Similarly, two individuals with an apnea hypopnea index of 40 events per hour (ie, severe OSA) may have very different symptoms attributable to OSA, eg, one could be asymptomatic and the other could be debilitated from sleepiness. We and others have been making efforts to determine why these phenomenon occur. At present, the techniques to define mechanisms underlying OSA are labor-intensive, requiring one or two overnight experiments to gather meaningful data. Although we are gathering new insights based on these techniques, efforts are ongoing to simplify these approaches and to make assessment of pathophysiologic characteristics more accessible to the clinician (Orr et al. Am J Respir Crit Care Med. 2017 Nov 30. doi: 10.1164/rccm.201707-1357LE. [Epub ahead of print]).
We ultimately believe that a thorough analysis of a sleep recording combined with demographic data and other readily available clinical data (perhaps plasma biomarkers) may yield sufficient information for us to know why OSA is occurring and what interventions might be helpful for an individual patient. Currently, our use of the polysomnogram to derive only an apnea hypopnea index does not take full advantage of the available data. An apnea hypopnea index can be readily obtained from home sleep testing and does not truly provide much insight into why a given individual has OSA, what symptoms are attributable to OSA, and what interventions might be considered for the afflicted individual. By analogy, if the only useful data derived from an ECG were a heart rate, the test would rapidly become obsolete. Along these lines, if the only role for the sleep clinician was to prescribe CPAP to everyone with an AHI greater than 5/h, there would be little need or interest in specialized training. In contrast, we suggest that rich insights regarding pathophysiology and mechanisms should be gathered and may influence clinical management of patients afflicted with OSA. Thus, we encourage more thorough analyses of available data to maximize information gleaned and, ultimately, to optimize clinical outcomes.
Recent studies suggest that sleep apnea occurs for varying reasons, a concept that is now thought to be clinically important (Jordan et al. Lancet. 2014;383[9918]:736). We draw a crucial distinction between endotypes (mechanisms underlying disease) and phenotypes (clinical expression of disease). Important endotypes include compromised upper airway anatomy, dysfunction in pharyngeal dilator muscles, unstable ventilatory control (high loop gain), and low arousal threshold (wake up easily), among others. Important phenotypes of sleep apnea are emerging and still evolving to include minimally symptomatic OSA, OSA with daytime sleepiness, and OSA with major cardiometabolic risk, among others. Several important concepts have emerged regarding different OSA endotypes and phenotypes:
1 The mechanism underlying OSA may predict potential response to therapeutic interventions. For instance, the endotype of OSA with unstable ventilatory control (high loop gain) may respond to agents such as oxygen and acetazolamide, which serve to stabilize control of breathing. In patients with anatomical compromise at the level of the velopharynx, uvulopalatopharyngoplasty may be an effective intervention. For patients with multiple pathophysiologic abnormalities, combination therapy may be required to alleviate OSA (Edwards et al. Sleep. 2016;9[11]:1973).
2 Given that OSA has many underlying etiologies, efforts are underway to determine whether individuals with different risk factors for OSA develop their disease based on varying mechanisms. As an example, people with posttraumatic stress disorder (PTSD) may be at increased risk of OSA perhaps on the basis of a low threshold for arousal (Orr et al. JCSM. 2017, 13[1]: 57-63). Another example would be patients with neuromuscular disease who may be at risk of OSA primarily based on impaired pharyngeal dilator muscle function.
3 A new concept is emerging whereby endotypes of OSA may actually predict differing OSA phenotypes. In theory, loop gain-driven OSA may have different consequences from OSA driven by compromise of pharyngeal anatomy. To this point, data suggest that OSA in the elderly may not have as many consequences as OSA in younger people matched on severity of illness. OSA in the elderly has lower loop gain than OSA in younger people and is associated with less negative intrathoracic pressure at the time of arousal as compared with younger individuals with OSA (Kobayashi et al. Chest. 2010; 137[6]:1310). As such, the endotype of OSA in the elderly may explain why the clinical consequences are fewer than in the younger OSA counterparts.
4 The mechanism underlying OSA may be important in determining response to clinical interventions, such as nasal CPAP. Patients with a low arousal threshold may be prone to insomnia when placed on CPAP and could theoretically be poorly tolerant of therapy based on disrupted sleep architecture. Such patients may benefit from non-myorelaxant hypnotic therapy to consolidate sleep and improve CPAP adherence. In addition, patients with high loop gain (unstable ventilatory control) may be prone to develop central apneas when placed on CPAP therapy (Stanchina et al. Ann Am Thorac Soc. 2015;12[9]:1351). These patients may benefit from newer technologies, eg, auto or adaptive servo ventilation - ASV. High loop gain has also been shown to predict failure of upper airway surgery as a treatment for OSA by several groups (Li et al. JCSM. 2017;13[9]:1029). Such patients should, perhaps, undergo nonsurgical therapies for OSA.
We emphasize that some of the points being made are somewhat speculative and, thus, encourage further basic and clinical research to test our assumptions. Robust, multicenter clinical trials assessing hard outcomes will ultimately be required to change the current standard of care. Nonetheless, we believe that a more thorough understanding of OSA pathogenesis can help guide clinical care today and will be critical to the optimal treatment of afflicted individuals tomorrow.
Dr. Owens is Assistant Clinical Professor of Medicine; Dr. Deacon is a Post-Doctoral Research Scholar; and Dr. Malhotra is Kenneth M. Moser Professor of Medicine and Chief, Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego.
Obstructive sleep apnea (OSA) contributes a major health burden to society due to its high prevalence and substantial neurocognitive and cardiovascular consequences. Estimates suggest that at least 10% of adults in North America are afflicted with OSA, making it probably the most common respiratory disease in the developed world (Peppard et al. Am J Epidemiol. 2013;177[9]:1006). Nasal CPAP is a highly efficacious therapy that has been shown to improve neurocognitive and cardiovascular outcomes. However, CPAP is not always well tolerated. Alternative therapies, such as oral appliances and upper airway surgery, have highly variable efficacy, and evidence of important clinical benefits are uncertain. Therefore, efforts are ongoing to determine optimal alternative strategies for therapy.
In order to treat any condition optimally, one needs to be able to predict who is at highest risk of developing the condition, then to assess the consequences if left untreated, and finally to be able to predict response to various treatment options. Currently, the OSA field is still in its early stages of our understanding. Clinically, we are often faced with patients who have varying presentations and manifestations, but, for reasons that are unclear. For instance, two individuals with the same body mass index may have very different clinical manifestations, one with severe OSA and one without any OSA. Similarly, two individuals with an apnea hypopnea index of 40 events per hour (ie, severe OSA) may have very different symptoms attributable to OSA, eg, one could be asymptomatic and the other could be debilitated from sleepiness. We and others have been making efforts to determine why these phenomenon occur. At present, the techniques to define mechanisms underlying OSA are labor-intensive, requiring one or two overnight experiments to gather meaningful data. Although we are gathering new insights based on these techniques, efforts are ongoing to simplify these approaches and to make assessment of pathophysiologic characteristics more accessible to the clinician (Orr et al. Am J Respir Crit Care Med. 2017 Nov 30. doi: 10.1164/rccm.201707-1357LE. [Epub ahead of print]).
We ultimately believe that a thorough analysis of a sleep recording combined with demographic data and other readily available clinical data (perhaps plasma biomarkers) may yield sufficient information for us to know why OSA is occurring and what interventions might be helpful for an individual patient. Currently, our use of the polysomnogram to derive only an apnea hypopnea index does not take full advantage of the available data. An apnea hypopnea index can be readily obtained from home sleep testing and does not truly provide much insight into why a given individual has OSA, what symptoms are attributable to OSA, and what interventions might be considered for the afflicted individual. By analogy, if the only useful data derived from an ECG were a heart rate, the test would rapidly become obsolete. Along these lines, if the only role for the sleep clinician was to prescribe CPAP to everyone with an AHI greater than 5/h, there would be little need or interest in specialized training. In contrast, we suggest that rich insights regarding pathophysiology and mechanisms should be gathered and may influence clinical management of patients afflicted with OSA. Thus, we encourage more thorough analyses of available data to maximize information gleaned and, ultimately, to optimize clinical outcomes.
Recent studies suggest that sleep apnea occurs for varying reasons, a concept that is now thought to be clinically important (Jordan et al. Lancet. 2014;383[9918]:736). We draw a crucial distinction between endotypes (mechanisms underlying disease) and phenotypes (clinical expression of disease). Important endotypes include compromised upper airway anatomy, dysfunction in pharyngeal dilator muscles, unstable ventilatory control (high loop gain), and low arousal threshold (wake up easily), among others. Important phenotypes of sleep apnea are emerging and still evolving to include minimally symptomatic OSA, OSA with daytime sleepiness, and OSA with major cardiometabolic risk, among others. Several important concepts have emerged regarding different OSA endotypes and phenotypes:
1 The mechanism underlying OSA may predict potential response to therapeutic interventions. For instance, the endotype of OSA with unstable ventilatory control (high loop gain) may respond to agents such as oxygen and acetazolamide, which serve to stabilize control of breathing. In patients with anatomical compromise at the level of the velopharynx, uvulopalatopharyngoplasty may be an effective intervention. For patients with multiple pathophysiologic abnormalities, combination therapy may be required to alleviate OSA (Edwards et al. Sleep. 2016;9[11]:1973).
2 Given that OSA has many underlying etiologies, efforts are underway to determine whether individuals with different risk factors for OSA develop their disease based on varying mechanisms. As an example, people with posttraumatic stress disorder (PTSD) may be at increased risk of OSA perhaps on the basis of a low threshold for arousal (Orr et al. JCSM. 2017, 13[1]: 57-63). Another example would be patients with neuromuscular disease who may be at risk of OSA primarily based on impaired pharyngeal dilator muscle function.
3 A new concept is emerging whereby endotypes of OSA may actually predict differing OSA phenotypes. In theory, loop gain-driven OSA may have different consequences from OSA driven by compromise of pharyngeal anatomy. To this point, data suggest that OSA in the elderly may not have as many consequences as OSA in younger people matched on severity of illness. OSA in the elderly has lower loop gain than OSA in younger people and is associated with less negative intrathoracic pressure at the time of arousal as compared with younger individuals with OSA (Kobayashi et al. Chest. 2010; 137[6]:1310). As such, the endotype of OSA in the elderly may explain why the clinical consequences are fewer than in the younger OSA counterparts.
4 The mechanism underlying OSA may be important in determining response to clinical interventions, such as nasal CPAP. Patients with a low arousal threshold may be prone to insomnia when placed on CPAP and could theoretically be poorly tolerant of therapy based on disrupted sleep architecture. Such patients may benefit from non-myorelaxant hypnotic therapy to consolidate sleep and improve CPAP adherence. In addition, patients with high loop gain (unstable ventilatory control) may be prone to develop central apneas when placed on CPAP therapy (Stanchina et al. Ann Am Thorac Soc. 2015;12[9]:1351). These patients may benefit from newer technologies, eg, auto or adaptive servo ventilation - ASV. High loop gain has also been shown to predict failure of upper airway surgery as a treatment for OSA by several groups (Li et al. JCSM. 2017;13[9]:1029). Such patients should, perhaps, undergo nonsurgical therapies for OSA.
We emphasize that some of the points being made are somewhat speculative and, thus, encourage further basic and clinical research to test our assumptions. Robust, multicenter clinical trials assessing hard outcomes will ultimately be required to change the current standard of care. Nonetheless, we believe that a more thorough understanding of OSA pathogenesis can help guide clinical care today and will be critical to the optimal treatment of afflicted individuals tomorrow.
Dr. Owens is Assistant Clinical Professor of Medicine; Dr. Deacon is a Post-Doctoral Research Scholar; and Dr. Malhotra is Kenneth M. Moser Professor of Medicine and Chief, Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego.
Obstructive sleep apnea (OSA) contributes a major health burden to society due to its high prevalence and substantial neurocognitive and cardiovascular consequences. Estimates suggest that at least 10% of adults in North America are afflicted with OSA, making it probably the most common respiratory disease in the developed world (Peppard et al. Am J Epidemiol. 2013;177[9]:1006). Nasal CPAP is a highly efficacious therapy that has been shown to improve neurocognitive and cardiovascular outcomes. However, CPAP is not always well tolerated. Alternative therapies, such as oral appliances and upper airway surgery, have highly variable efficacy, and evidence of important clinical benefits are uncertain. Therefore, efforts are ongoing to determine optimal alternative strategies for therapy.
In order to treat any condition optimally, one needs to be able to predict who is at highest risk of developing the condition, then to assess the consequences if left untreated, and finally to be able to predict response to various treatment options. Currently, the OSA field is still in its early stages of our understanding. Clinically, we are often faced with patients who have varying presentations and manifestations, but, for reasons that are unclear. For instance, two individuals with the same body mass index may have very different clinical manifestations, one with severe OSA and one without any OSA. Similarly, two individuals with an apnea hypopnea index of 40 events per hour (ie, severe OSA) may have very different symptoms attributable to OSA, eg, one could be asymptomatic and the other could be debilitated from sleepiness. We and others have been making efforts to determine why these phenomenon occur. At present, the techniques to define mechanisms underlying OSA are labor-intensive, requiring one or two overnight experiments to gather meaningful data. Although we are gathering new insights based on these techniques, efforts are ongoing to simplify these approaches and to make assessment of pathophysiologic characteristics more accessible to the clinician (Orr et al. Am J Respir Crit Care Med. 2017 Nov 30. doi: 10.1164/rccm.201707-1357LE. [Epub ahead of print]).
We ultimately believe that a thorough analysis of a sleep recording combined with demographic data and other readily available clinical data (perhaps plasma biomarkers) may yield sufficient information for us to know why OSA is occurring and what interventions might be helpful for an individual patient. Currently, our use of the polysomnogram to derive only an apnea hypopnea index does not take full advantage of the available data. An apnea hypopnea index can be readily obtained from home sleep testing and does not truly provide much insight into why a given individual has OSA, what symptoms are attributable to OSA, and what interventions might be considered for the afflicted individual. By analogy, if the only useful data derived from an ECG were a heart rate, the test would rapidly become obsolete. Along these lines, if the only role for the sleep clinician was to prescribe CPAP to everyone with an AHI greater than 5/h, there would be little need or interest in specialized training. In contrast, we suggest that rich insights regarding pathophysiology and mechanisms should be gathered and may influence clinical management of patients afflicted with OSA. Thus, we encourage more thorough analyses of available data to maximize information gleaned and, ultimately, to optimize clinical outcomes.
Recent studies suggest that sleep apnea occurs for varying reasons, a concept that is now thought to be clinically important (Jordan et al. Lancet. 2014;383[9918]:736). We draw a crucial distinction between endotypes (mechanisms underlying disease) and phenotypes (clinical expression of disease). Important endotypes include compromised upper airway anatomy, dysfunction in pharyngeal dilator muscles, unstable ventilatory control (high loop gain), and low arousal threshold (wake up easily), among others. Important phenotypes of sleep apnea are emerging and still evolving to include minimally symptomatic OSA, OSA with daytime sleepiness, and OSA with major cardiometabolic risk, among others. Several important concepts have emerged regarding different OSA endotypes and phenotypes:
1 The mechanism underlying OSA may predict potential response to therapeutic interventions. For instance, the endotype of OSA with unstable ventilatory control (high loop gain) may respond to agents such as oxygen and acetazolamide, which serve to stabilize control of breathing. In patients with anatomical compromise at the level of the velopharynx, uvulopalatopharyngoplasty may be an effective intervention. For patients with multiple pathophysiologic abnormalities, combination therapy may be required to alleviate OSA (Edwards et al. Sleep. 2016;9[11]:1973).
2 Given that OSA has many underlying etiologies, efforts are underway to determine whether individuals with different risk factors for OSA develop their disease based on varying mechanisms. As an example, people with posttraumatic stress disorder (PTSD) may be at increased risk of OSA perhaps on the basis of a low threshold for arousal (Orr et al. JCSM. 2017, 13[1]: 57-63). Another example would be patients with neuromuscular disease who may be at risk of OSA primarily based on impaired pharyngeal dilator muscle function.
3 A new concept is emerging whereby endotypes of OSA may actually predict differing OSA phenotypes. In theory, loop gain-driven OSA may have different consequences from OSA driven by compromise of pharyngeal anatomy. To this point, data suggest that OSA in the elderly may not have as many consequences as OSA in younger people matched on severity of illness. OSA in the elderly has lower loop gain than OSA in younger people and is associated with less negative intrathoracic pressure at the time of arousal as compared with younger individuals with OSA (Kobayashi et al. Chest. 2010; 137[6]:1310). As such, the endotype of OSA in the elderly may explain why the clinical consequences are fewer than in the younger OSA counterparts.
4 The mechanism underlying OSA may be important in determining response to clinical interventions, such as nasal CPAP. Patients with a low arousal threshold may be prone to insomnia when placed on CPAP and could theoretically be poorly tolerant of therapy based on disrupted sleep architecture. Such patients may benefit from non-myorelaxant hypnotic therapy to consolidate sleep and improve CPAP adherence. In addition, patients with high loop gain (unstable ventilatory control) may be prone to develop central apneas when placed on CPAP therapy (Stanchina et al. Ann Am Thorac Soc. 2015;12[9]:1351). These patients may benefit from newer technologies, eg, auto or adaptive servo ventilation - ASV. High loop gain has also been shown to predict failure of upper airway surgery as a treatment for OSA by several groups (Li et al. JCSM. 2017;13[9]:1029). Such patients should, perhaps, undergo nonsurgical therapies for OSA.
We emphasize that some of the points being made are somewhat speculative and, thus, encourage further basic and clinical research to test our assumptions. Robust, multicenter clinical trials assessing hard outcomes will ultimately be required to change the current standard of care. Nonetheless, we believe that a more thorough understanding of OSA pathogenesis can help guide clinical care today and will be critical to the optimal treatment of afflicted individuals tomorrow.
Dr. Owens is Assistant Clinical Professor of Medicine; Dr. Deacon is a Post-Doctoral Research Scholar; and Dr. Malhotra is Kenneth M. Moser Professor of Medicine and Chief, Division of Pulmonary, Critical Care and Sleep Medicine, University of California San Diego.
Sneak Peek: Journal of Hospital Medicine – Oct. 2017
BACKGROUND: Hospitalized patients frequently report poor sleep, partly due to the inpatient environment. In-hospital sound and light levels are not well described on non–intensive care unit (non-ICU) wards. Although non-ICU wards may have lower average and peak noise levels, sound level changes (SLCs), which are important in disrupting sleep, may still be a substantial problem.
OBJECTIVE: To compare ambient sound and light levels, including SLCs, in ICU and non-ICU environments.
DESIGN: Observational study.
SETTING: Tertiary-care hospital.
MEASUREMENTS: Sound measurements of 0.5 Hz were analyzed to provide average hourly sound levels, sound peaks, and SLCs greater than or equal to 17.5 decibels (dB). For light data, measurements taken at 2-minute intervals provided average and maximum light levels.
RESULTS: The ICU rooms were louder than non-ICU wards; hourly averages ranged from 56.1 plus or minus 1.3 dB to 60.3 plus or minus 1.7 dB in the ICU, 47.3 plus or minus 3.7 dB to 55.1 plus or minus 3.7 dB on the telemetry floor, and 44.6 plus or minus 2.1 dB to 53.7 plus or minus 3.6 dB on the general ward. However, SLCs greater than or equal to 17.5 dB were not statistically different (ICU, 203.9 plus or minus 28.8 times; non-ICU, 270.9 plus or minus 39.5; P = 0.11). In both ICU and non-ICU wards, average daytime light levels were less than 250 lux, and peak light levels occurred in the afternoon and early evening.
CONCLUSIONS: While quieter, non-ICU wards have as many SLCs as ICUs do, which has implications for quality improvement measurements. Efforts to further reduce average noise levels might be counterproductive. Light levels in the hospital (ICU and non-ICU) may not be optimal for maintenance of a normal circadian rhythm for most people.
Read the entire article in the Journal of Hospital Medicine.
Also in JHM this month
Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters
AUTHORS: Rachel Weiss, MD, Eric Vittinghoff, PhD, MPH, Margaret C. Fang, MD, MPH, Jenica E. W. Cimino, Kristen Adams Chasteen, MD, Robert M. Arnold, MD, Andrew D. Auerbach, MD, Wendy G. Anderson, MD, MS
A concise tool for measuring care coordination from the provider’s perspective in the hospital setting
AUTHORS: Christine M. Weston, PhD, and Sehyo Yune, MD, Eric B. Bass, MD, MPH, Scott A. Berkowitz, MD, MBA, Daniel J. Brotman, MD, Amy Deutschendorf, MS, RN, ACNS-BC, Eric E. Howell, MD, Melissa B. Richardson, MBA Carol Sylvester, RN, MS, Albert W. Wu, MD, MPH
Post–intensive care unit psychiatric comorbidity and quality of life
AUTHORS: Sophia Wang, MD, and Chris Mosher, MD, Anthony J. Perkins, MS, Sujuan Gao, PhD, Sue Lasiter, RN, PhD, Sikandar Khan, MD, Malaz Boustani, MD, MPH, Babar Khan, MD, MS
An opportunity to improve Medicare’s planned readmissions measure
AUTHORS: Chad Ellimoottil, MD, MS, Roger K. Khouri Jr., MD, Apoorv Dhir, BA, Hechuan Hou, MS, David C. Miller, MD, MPH, James M. Dupree, MD, MPH
Against medical advice discharges
AUTHORS: David Alfandre, MD, MSPH, Jay Brenner, MD, Eberechukwu Onukwugha, MS, PhD
BACKGROUND: Hospitalized patients frequently report poor sleep, partly due to the inpatient environment. In-hospital sound and light levels are not well described on non–intensive care unit (non-ICU) wards. Although non-ICU wards may have lower average and peak noise levels, sound level changes (SLCs), which are important in disrupting sleep, may still be a substantial problem.
OBJECTIVE: To compare ambient sound and light levels, including SLCs, in ICU and non-ICU environments.
DESIGN: Observational study.
SETTING: Tertiary-care hospital.
MEASUREMENTS: Sound measurements of 0.5 Hz were analyzed to provide average hourly sound levels, sound peaks, and SLCs greater than or equal to 17.5 decibels (dB). For light data, measurements taken at 2-minute intervals provided average and maximum light levels.
RESULTS: The ICU rooms were louder than non-ICU wards; hourly averages ranged from 56.1 plus or minus 1.3 dB to 60.3 plus or minus 1.7 dB in the ICU, 47.3 plus or minus 3.7 dB to 55.1 plus or minus 3.7 dB on the telemetry floor, and 44.6 plus or minus 2.1 dB to 53.7 plus or minus 3.6 dB on the general ward. However, SLCs greater than or equal to 17.5 dB were not statistically different (ICU, 203.9 plus or minus 28.8 times; non-ICU, 270.9 plus or minus 39.5; P = 0.11). In both ICU and non-ICU wards, average daytime light levels were less than 250 lux, and peak light levels occurred in the afternoon and early evening.
CONCLUSIONS: While quieter, non-ICU wards have as many SLCs as ICUs do, which has implications for quality improvement measurements. Efforts to further reduce average noise levels might be counterproductive. Light levels in the hospital (ICU and non-ICU) may not be optimal for maintenance of a normal circadian rhythm for most people.
Read the entire article in the Journal of Hospital Medicine.
Also in JHM this month
Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters
AUTHORS: Rachel Weiss, MD, Eric Vittinghoff, PhD, MPH, Margaret C. Fang, MD, MPH, Jenica E. W. Cimino, Kristen Adams Chasteen, MD, Robert M. Arnold, MD, Andrew D. Auerbach, MD, Wendy G. Anderson, MD, MS
A concise tool for measuring care coordination from the provider’s perspective in the hospital setting
AUTHORS: Christine M. Weston, PhD, and Sehyo Yune, MD, Eric B. Bass, MD, MPH, Scott A. Berkowitz, MD, MBA, Daniel J. Brotman, MD, Amy Deutschendorf, MS, RN, ACNS-BC, Eric E. Howell, MD, Melissa B. Richardson, MBA Carol Sylvester, RN, MS, Albert W. Wu, MD, MPH
Post–intensive care unit psychiatric comorbidity and quality of life
AUTHORS: Sophia Wang, MD, and Chris Mosher, MD, Anthony J. Perkins, MS, Sujuan Gao, PhD, Sue Lasiter, RN, PhD, Sikandar Khan, MD, Malaz Boustani, MD, MPH, Babar Khan, MD, MS
An opportunity to improve Medicare’s planned readmissions measure
AUTHORS: Chad Ellimoottil, MD, MS, Roger K. Khouri Jr., MD, Apoorv Dhir, BA, Hechuan Hou, MS, David C. Miller, MD, MPH, James M. Dupree, MD, MPH
Against medical advice discharges
AUTHORS: David Alfandre, MD, MSPH, Jay Brenner, MD, Eberechukwu Onukwugha, MS, PhD
BACKGROUND: Hospitalized patients frequently report poor sleep, partly due to the inpatient environment. In-hospital sound and light levels are not well described on non–intensive care unit (non-ICU) wards. Although non-ICU wards may have lower average and peak noise levels, sound level changes (SLCs), which are important in disrupting sleep, may still be a substantial problem.
OBJECTIVE: To compare ambient sound and light levels, including SLCs, in ICU and non-ICU environments.
DESIGN: Observational study.
SETTING: Tertiary-care hospital.
MEASUREMENTS: Sound measurements of 0.5 Hz were analyzed to provide average hourly sound levels, sound peaks, and SLCs greater than or equal to 17.5 decibels (dB). For light data, measurements taken at 2-minute intervals provided average and maximum light levels.
RESULTS: The ICU rooms were louder than non-ICU wards; hourly averages ranged from 56.1 plus or minus 1.3 dB to 60.3 plus or minus 1.7 dB in the ICU, 47.3 plus or minus 3.7 dB to 55.1 plus or minus 3.7 dB on the telemetry floor, and 44.6 plus or minus 2.1 dB to 53.7 plus or minus 3.6 dB on the general ward. However, SLCs greater than or equal to 17.5 dB were not statistically different (ICU, 203.9 plus or minus 28.8 times; non-ICU, 270.9 plus or minus 39.5; P = 0.11). In both ICU and non-ICU wards, average daytime light levels were less than 250 lux, and peak light levels occurred in the afternoon and early evening.
CONCLUSIONS: While quieter, non-ICU wards have as many SLCs as ICUs do, which has implications for quality improvement measurements. Efforts to further reduce average noise levels might be counterproductive. Light levels in the hospital (ICU and non-ICU) may not be optimal for maintenance of a normal circadian rhythm for most people.
Read the entire article in the Journal of Hospital Medicine.
Also in JHM this month
Associations of physician empathy with patient anxiety and ratings of communication in hospital admission encounters
AUTHORS: Rachel Weiss, MD, Eric Vittinghoff, PhD, MPH, Margaret C. Fang, MD, MPH, Jenica E. W. Cimino, Kristen Adams Chasteen, MD, Robert M. Arnold, MD, Andrew D. Auerbach, MD, Wendy G. Anderson, MD, MS
A concise tool for measuring care coordination from the provider’s perspective in the hospital setting
AUTHORS: Christine M. Weston, PhD, and Sehyo Yune, MD, Eric B. Bass, MD, MPH, Scott A. Berkowitz, MD, MBA, Daniel J. Brotman, MD, Amy Deutschendorf, MS, RN, ACNS-BC, Eric E. Howell, MD, Melissa B. Richardson, MBA Carol Sylvester, RN, MS, Albert W. Wu, MD, MPH
Post–intensive care unit psychiatric comorbidity and quality of life
AUTHORS: Sophia Wang, MD, and Chris Mosher, MD, Anthony J. Perkins, MS, Sujuan Gao, PhD, Sue Lasiter, RN, PhD, Sikandar Khan, MD, Malaz Boustani, MD, MPH, Babar Khan, MD, MS
An opportunity to improve Medicare’s planned readmissions measure
AUTHORS: Chad Ellimoottil, MD, MS, Roger K. Khouri Jr., MD, Apoorv Dhir, BA, Hechuan Hou, MS, David C. Miller, MD, MPH, James M. Dupree, MD, MPH
Against medical advice discharges
AUTHORS: David Alfandre, MD, MSPH, Jay Brenner, MD, Eberechukwu Onukwugha, MS, PhD
Sound and Light Levels Are Similarly Disruptive in ICU and non-ICU Wards
The hospital environment fails to promote adequate sleep for acutely or critically ill patients. Intensive care units (ICUs) have received the most scrutiny, because critically ill patients suffer from severely fragmented sleep as well as a lack of deeper, more restorative sleep.1-4 ICU survivors frequently cite sleep deprivation, contributed to by ambient noise, as a major stressor while receiving care.5,6 Importantly, efforts to modify the ICU environment to promote sleep have been associated with reductions in delirium.7,8 However, sleep deprivation and delirium in the hospital are not limited to ICU patients.
Sleep in the non-ICU setting is also notoriously poor, with 50%-80% of patients reporting sleep as “unsound” or otherwise subjectively poor.9-11 Additionally, patients frequently ask for and/or receive pharmacological sleeping aids12 despite little evidence of efficacy13 and increasing evidence of harm.14 Here too, efforts to improve sleep seems to attenuate risk of delirium,15 which remains a substantial problem on general wards, with incidence reported as high as 20%-30%. The reasons for poor sleep in the hospital are multifactorial, but data suggest that the inpatient environment, including noise and light levels, which are measurable and modifiable entities, contribute significantly to the problem.16
The World Health Organization (WHO) recommends that nighttime baseline noise levels do not exceed 30 decibels (dB) and that nighttime noise peaks (ie, loud noises) do not exceed 40 dB17; most studies suggest that ICU and general ward rooms are above this range on average.10,18 Others have also demonstrated an association between loud noises and patients’ subjective perception of poor sleep.10,19 However, when considering clinically important noise, peak and average noise levels may not be the key factor in causing arousals from sleep. Buxton and colleagues20 found that noise quality affects arousal probability; for example, electronic alarms and conversational noise are more likely to cause awakenings compared with the opening or closing of doors and ice machines. Importantly, peak and average noise levels may also matter less for sleep than do sound level changes (SLCs), which are defined as the difference between background/baseline noise and peak noise. Using healthy subjects exposed to simulated ICU noise, Stanchina et al.21 found that SLCs >17.5 dB were more likely to cause polysomnographic arousals from sleep regardless of peak noise level. This sound pressure change of approximately 20 dB would be perceived as 4 times louder, or, as an example, would be the difference between normal conversation between 2 people (~40 dB) that is then interrupted by the start of a vacuum cleaner (~60 dB). To our knowledge, no other studies have closely examined SLCs in different hospital environments.
Ambient light also likely affects sleep quality in the hospital. The circadian rhythm system, which controls the human sleep–wake cycle as well as multiple other physiologic functions, depends on ambient light as the primary external factor for regulating the internal clock.22,23 Insufficient and inappropriately timed light exposure can desynchronize the biological clock, thereby negatively affecting sleep quality.24,25 Conversely, patients exposed to early-morning bright light may sleep better while in the hospital.16 In addition to sleep patterns, ambient light affects other aspects of patient care; for example, lower light levels in the hospital have recently been associated with higher levels of fatigue and mood disturbance.26A growing body of data has investigated the ambient environment in the ICU, but fewer studies have focused on sound and light analysis in other inpatient areas such as the general ward and telemetry floors. We examined sound and light levels in the ICU and non-ICU environment, hypothesizing that average sound levels would be higher in the ICU than on non-ICU floors but that the number of SLCs >17.5 dB would be similar. Additionally, we expected that average light levels would be higher in the ICU than on non-ICU floors.
METHODS
This was an observational study of the sound and light environment in the inpatient setting. Per our Institutional Review Board, no consent was required. Battery-operated sound-level (SDL600, Extech Instruments, Nashua, NH) and light-level (SDL400, Extech Instruments, Nashua, NH) meters were placed in 24 patient rooms in our tertiary-care adult hospital in La Jolla, CA. Recordings were obtained in randomly selected, single-patient occupied rooms that were from 3 different hospital units and included 8 general ward rooms, 8 telemetry floor rooms, and 8 ICU rooms. We recorded for approximately 24-72 hours. Depending on the geographic layout of the room, meters were placed as close to the head of the patient’s bed as possible and were generally not placed farther than 2 meters away from the patient’s head of bed; all rooms contained a window.
Sound Measurements
Sound meters measured ambient noise in dB every 2 seconds and were set for A-weighted frequency measurements. We averaged individual data points to obtain hourly averages for ICU and non-ICU rooms. For hourly sound averages, we further separated the data to compare the general ward telemetry floors (both non-ICU), the latter of which has more patient monitoring and a lower nurse-to-patient ratio compared with the general ward floor.
Data from ICU versus non-ICU rooms were analyzed for the number of sound peaks throughout the 24-hour day and for sound peak over the nighttime, defined as the number of times sound levels exceeded 65 dB, 70 dB, or 80 dB, which were averaged over 24 hours and over the nighttime (10 PM to 6 AM). We also calculated the number of average SLCs ≥17.5 dB observed over 24 hours and over the nighttime.
Light Measurements
Light meters measured luminescence in lux at a frequency of 120 seconds. We averaged individual data points to obtain hourly averages for ICU and non-ICU rooms. In addition to hourly averages, light-level data were analyzed for maximum levels throughout the day and night.
Statistical Analysis
Hourly sound-level averages between the 3 floors were evaluated using a 1-way analysis of variance (ANOVA); sound averages from the general ward and telemetry floor were also compared at each hour using a Student t test. Light-level data, sound-level peak data, as well as SLC data were also evaluated using a Student t test.
RESULTS
Sound Measurements
Examples of the raw data distribution for individual sound recordings in an ICU and non-ICU room are shown in Figure 1A and 1B. Sound-level analysis with specific average values and significance levels between ICU and non-ICU rooms (with non-ICU rooms further divided between telemetry and general ward floors for purposes of hourly averages) are shown in Table 1. The average hourly values in all 3 locations were always above the 30-35 dB level (nighttime and daytime, respectively) recommended by the WHO (Figure 1C). A 1-way ANOVA analysis revealed significant differences between the 3 floors at all time points except for 10 AM. An analysis of the means at each time point between the telemetry floor and the general ward floor showed that the telemetry floor had significantly higher sound averages compared with the general ward floor at 10 PM, 11 PM, and 12 AM. Sound levels dropped during the nighttime on both non-ICU wards but remained fairly constant throughout the day and night in the ICU.
Importantly, despite average and peak sound levels showing that the ICU environment is louder overall, there were an equivalent number of SLCs ≥ 17.5 dB in the ICU and on non-ICU floors. The number of SLCs ≥ 17.5 dB is not statistically different when comparing ICU and non-ICU rooms either averaged over 24 hours or averaged over the nighttime (Figure 1E).
Light Measurements
Examples of light levels over a 24-hour period in an ICU and non-ICU room are shown in Figure 2A and 2B, respectively. Maximum average light levels (reported here as average value ± standard deviation to demonstrate variability within the data) in the ICU were 169.7 ± 127.1 lux and occurred at 1 PM, while maximum average light levels in the non-ICU rooms were 213.5 ± 341.6 lux and occurred at 5 PM (Figure 2C). Average light levels in the morning hours remained low and ranged from 15.9 ± 12.7 lux to 38.9 ± 43.4 lux in the ICU and from 22.3 ± 17.5 lux to 100.7 ± 92.0 lux on the non-ICU floors. The maximum measured level from any of the recordings was 2530 lux and occurred in a general ward room in the 5 PM hour. Overall, light averages remained low, but this particular room had light levels that were significantly higher than the others. A t test analysis of the hourly averages revealed only 1 time point of significant difference between the 2 floors; at 7 AM, the general ward floor had a higher lux level of 49.9 ± 27.5 versus 19.2 ± 10.7 in the ICU (P = 0.038). Otherwise, there were no differences between light levels in ICU rooms versus non-ICU rooms. Evaluation of the data revealed a substantial amount of variability in light levels throughout the daytime hours. Light levels during the nighttime remained low and were not significantly different between the 2 groups.
DISCUSSION
To our knowledge, this is the first study to directly compare the ICU and non-ICU environment for its potential impact on sleep and circadian alignment. Our study adds to the literature with several novel findings. First, average sound levels on non-ICU wards are lower than in the ICU. Second, although quieter on average, SLCs >17.5 dB occurred an equivalent number of times for both the ICU and non-ICU wards. Third, average daytime light levels in both the ICU and non-ICU environment are low. Lastly, peak light levels for both ICU and non-ICU wards occur later in the day instead of in the morning. All of the above have potential impact for optimizing the ward environment to better aid in sleep for patients.
Sound-Level Findings
Data on sound levels for non-ICU floors are limited but mostly consistent with our finding
Average and peak sound levels contribute to the ambient noise experienced by patients but may not be the source of sleep disruptions. Using polysomnography in healthy subjects exposed to recordings of ICU noise, Stanchina et al.21 showed that SLCs from baseline and not peak sound levels determined whether a subject was aroused from sleep by sound. Accordingly, they also found that increasing baseline sound levels by using white noise reduced the number of arousals that subjects experienced. To our knowledge, other studies have not quantified and compared SLCs in the ICU and non-ICU environments. Our data show that patients on non-ICU floors experience at least the same number of SLCs, and thereby the same potential for arousals from sleep, when compared with ICU patients. The higher baseline level of noise in the ICU likely explains the relatively lower number of SLCs when compared with the non-ICU floors. Although decreasing overall noise to promote sleep in the hospital seems like the obvious solution, the treatment for noise pollution in the hospital may actually be more background noise, not less.
Recent studies support the clinical implications of our findings. First, decreasing overall noise levels is difficult to accomplish.29 Second, recent studies utilized white noise in different hospital settings with some success in improving patients’ subjective sleep quality, although more studies using objective data measurements are needed to further understand the impact of white noise on sleep in hospitalized patients.30,31 Third, efforts at reducing interruptions—which likely will decrease the number of SLCs—such as clustering nursing care or reducing intermittent alarms may be more beneficial in improving sleep than efforts at decreasing average sound levels. For example, Bartick et al. reduced the number of patient interruptions at night by eliminating routine vital signs and clustering medication administration. Although they included other interventions as well, we note that this approach likely reduced SLCs and was associated with a reduction in the use of sedative medications.32 Ultimately, our data show that a focus on reducing SLCs will be one necessary component of a multipronged solution to improving inpatient sleep.33
Light-Level Findings
Because of its effect on circadian rhythms, the daily light-dark cycle has a powerful impact on human physiology and behavior, which includes sleep.34 Little is understood about how light affects sleep and other circadian-related functions in general ward patients, as it is not commonly measured. Our findings suggest that patients admitted to the hospital are exposed to light levels and patterns that may not optimally promote wake and sleep. Encouragingly, we did not find excessive average light levels during the nighttime in either ICU or non-ICU environment of our hospital, although others have described intrusive nighttime light in the hospital setting.35,36 Even short bursts of low or moderate light during the nighttime can cause circadian phase delay,37 and efforts to maintain darkness in patient rooms at night should continue.
Our measurements show that average daytime light levels did not exceed 250 lux, which corresponds to low, office-level lighting, while the brightest average light levels occurred in the afternoon for both environments. These levels are consistent with other reports26,35,36 as is the light-level variability noted throughout the day (which is not unexpected given room positioning, patient preference, curtains, etc). The level and amount of daytime light needed to maintain circadian rhythms in humans is still unknown.38 Brighter light is generally more effective at influencing the circadian pacemaker in a dose-dependent manner.39 Although entrainment (synchronization of the body’s biological rhythm with environmental cues such as ambient light) of the human circadian rhythm has been shown with low light levels (eg, <100 lux), these studies included healthy volunteers in a carefully controlled, constant, routine environment.23 How these data apply to acutely ill subjects in the hospital environment is not clear. We note that low to moderate levels of light (50-1000 lux) are less effective for entrainment of the circadian rhythm in older people (age >65 years, the majority of our admissions) compared with younger people. Thus, older, hospitalized patients may require greater light levels for regulation of the sleep-wake cycle.40 These data are important when designing interventions to improve light for and maintain circadian rhythms in hospitalized patients. For example, Simons et al. found that dynamic light-application therapy, which achieved a maximum average lux level of <800 lux, did not reduce rates of delirium in critically ill patients (mean age ~65). One interpretation of these results, though there are many others, is that the light levels achieved were not high enough to influence circadian timing in hospitalized, mostly elderly patients. The physiological impact of light on the circadian rhythm in hospitalized patients still remains to be measured.
LIMITATIONS
Our study does have a few limitations. We did not assess sound quality, which is another determinant of arousal potential.20 Also, a shorter measurement interval might be useful in determining sharper sound increases. It may also be important to consider A- versus C-weighted measurements of sound levels, as A-weighted measurements usually reflect higher-frequency sound while C-weighted measurements usually reflect low-frequency noise18; we obtained only A-weighted measurements in our study. However, A-weighted measurements are generally considered more reflective of what the human ear considers noise and are used more standardly than C-weighted measurements.
Regarding light measurements, we recorded from rooms facing different cardinal directions and during different times of the year, which likely contributed to some of the variability in the daytime light levels on both floors. Additionally, light levels were not measured directly at the patient’s eye level. However, given that overhead fluorescent lighting was the primary source of lighting, it is doubtful that we substantially underestimated optic-nerve light levels. In the future, it may also be important to measure the different wavelengths of lights, as blue light may have a greater impact on sleep than other wavelengths.41 Although our findings align with others’, we note that this was a single-center study, which could limit the generalizability of our findings given inter-hospital variations in patient volume, interior layout and structure, and geographic location.
CONCLUSIONS
Overall, our study suggests that the light and sound environment for sleep in the inpatient setting, including both the ICU and non-ICU wards, has multiple areas for improvement. Our data also suggest specific directions for future clinical efforts at improvement. For example, efforts to decrease average sound levels may worsen sleep fragmentation. Similarly, more light during the day may be more helpful than further attempts to limit light during the night.
Disclosure
This research was funded in part by a NIH/NCATS flagship Clinical and Translational Science Award Grant (5KL2TR001112). None of the authors report any conflict of interest, financial or otherwise, in the preparation of this article.
1. Freedman NS, Gazendam J, Levan L, Pack AI, Schwab RJ. Abnormal sleep/wake
cycles and the effect of environmental noise on sleep disruption in the intensive
care unit. Am J Respir Crit Care Med. 2001;163(2):451-457. PubMed
2. Watson PL, Pandharipande P, Gehlbach BK, et al. Atypical sleep in ventilated
patients: empirical electroencephalography findings and the path toward revised ICU sleep scoring criteria. Crit Care Med. 2013;41(8):1958-1967. PubMed
3. Gehlbach BK, Chapotot F, Leproult R, et al. Temporal disorganization of circadian rhythmicity and sleep-wake regulation in mechanically ventilated patients receiving continuous intravenous sedation. Sleep. 2012;35(8):1105-1114. PubMed
4. Elliott R, McKinley S, Cistulli P, Fien M. Characterisation of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care. 2013;17(2):R46. PubMed
5. Novaes MA, Aronovich A, Ferraz MB, Knobel E. Stressors in ICU: patients’ evaluation. Intensive Care Med. 1997;23(12):1282-1285. PubMed
6. Tembo AC, Parker V, Higgins I. The experience of sleep deprivation in intensive care patients: findings from a larger hermeneutic phenomenological study. Intensive Crit Care Nurs. 2013;29(6):310-316. PubMed
7. Kamdar BB, Yang J, King LM, et al. Developing, implementing, and evaluating a multifaceted quality improvement intervention to promote sleep in an ICU. Am J Med Qual. 2014;29(6):546-554. PubMed
8. Patel J, Baldwin J, Bunting P, Laha S. The effect of a multicomponent multidisciplinary bundle of interventions on sleep and delirium in medical and surgical intensive care patients. Anaesthesia. 2014;69(6):540-549. PubMed
9. Manian FA, Manian CJ. Sleep quality in adult hospitalized patients with infection: an observational study. Am J Med Sci. 2015;349(1):56-60. PubMed
10. Park MJ, Yoo JH, Cho BW, Kim KT, Jeong WC, Ha M. Noise in hospital rooms and sleep disturbance in hospitalized medical patients. Environ Health Toxicol. 2014;29:e2014006. PubMed
11. Dobing S, Frolova N, McAlister F, Ringrose J. Sleep quality and factors influencing self-reported sleep duration and quality in the general internal medicine inpatient population. PLoS One. 2016;11(6):e0156735. PubMed
12. Gillis CM, Poyant JO, Degrado JR, Ye L, Anger KE, Owens RL. Inpatient pharmacological
sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652-657. PubMed
13. Krenk L, Jennum P, Kehlet H. Postoperative sleep disturbances after zolpidem treatment in fast-track hip and knee replacement. J Clin Sleep Med. 2014;10(3):321-326. PubMed
14. Kolla BP, Lovely JK, Mansukhani MP, Morgenthaler TI. Zolpidem is independently
associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1-6. PubMed
15. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. PubMed
16. Bano M, Chiaromanni F, Corrias M, et al. The influence of environmental factors on sleep quality in hospitalized medical patients. Front Neurol. 2014;5:267. PubMed
17. Berglund BLTSD. Guidelines for Community Noise. World Health Organization. 1999.
18. Knauert M, Jeon S, Murphy TE, Yaggi HK, Pisani MA, Redeker NS. Comparing average levels and peak occurrence of overnight sound in the medical intensive care unit on A-weighted and C-weighted decibel scales. J Crit Care. 2016;36:1-7. PubMed
19. Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172(1):68-70. PubMed
20. Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. PubMed
21. Stanchina ML, Abu-Hijleh M, Chaudhry BK, Carlisle CC, Millman RP. The influence of white noise on sleep in subjects exposed to ICU noise. Sleep Med. 2005;6(5):423-428. PubMed
22. Czeisler CA, Allan JS, Strogatz SH, et al. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science. 1986;233(4764):667-671. PubMed
23. Duffy JF, Czeisler CA. Effect of light on human circadian physiology. Sleep Med Clin. 2009;4(2):165-177. PubMed
24. Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210(4475):1267-1269. PubMed
25. Zeitzer JM, Dijk DJ, Kronauer R, Brown E, Czeisler C. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J Physiol. 2000;526:695-702. PubMed
26. Bernhofer EI, Higgins PA, Daly BJ, Burant CJ, Hornick TR. Hospital lighting and its association with sleep, mood and pain in medical inpatients. J Adv Nurs. 2014;70(5):1164-1173. PubMed
27. Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care. 2013;17(5):R187. PubMed
28. Gillis S. Pharmacologic treatment of depression during pregnancy. J Midwifery Womens Health. 2000;45(4):357-359. PubMed
29. Tainter CR, Levine AR, Quraishi SA, et al. Noise levels in surgical ICUs are consistently above recommended standards. Crit Care Med. 2016;44(1):147-152. PubMed
30. Farrehi PM, Clore KR, Scott JR, Vanini G, Clauw DJ. Efficacy of Sleep Tool Education During Hospitalization: A Randomized Controlled Trial. Am J Med. 2016;129(12):1329.e9-1329.e17. PubMed
31. Farokhnezhad Afshar P, Bahramnezhad F, Asgari P, Shiri M. Effect of white noise on sleep in patients admitted to a coronary care. J Caring Sci. 2016;5(2):103-109. PubMed
32. Bartick MC, Thai X, Schmidt T, Altaye A, Solet JM. Decrease in as-needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5(3):E20-E24. PubMed
33. Tamrat R, Huynh-Le MP, Goyal M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: a systematic review. J Gen Intern Med. 2014;29(5):788-795. PubMed
34. Dijk DJ, Archer SN. Light, sleep, and circadian rhythms: together again. PLoS Biol. 2009;7(6):e1000145. PubMed
35. Verceles AC, Liu X, Terrin ML, et al. Ambient light levels and critical care outcomes. J Crit Care. 2013;28(1):110.e1-110.e8. PubMed
36. Hu RF, Hegadoren KM, Wang XY, Jiang XY. An investigation of light and sound levels on intensive care units in China. Aust Crit Care. 2016;29(2):62-67. PubMed
37. Zeitzer JM, Ruby NF, Fisicaro RA, Heller HC. Response of the human circadian system to millisecond flashes of light. PLoS One. 2011;6(7):e22078. PubMed
38. Duffy JF, Wright KP, Jr. Entrainment of the human circadian system by light. J Biol Rhythms. 2005;20(4):326-338. PubMed
39. Wright KP Jr, Gronfier C, Duffy JF, Czeisler CA. Intrinsic period and light intensity determine the phase relationship between melatonin and sleep in humans. J Biol Rhythms. 2005;20(2):168-177. PubMed
40. Duffy JF, Zeitzer JM, Czeisler CA. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol Aging. 2007;28(5):799-807. PubMed
41. Figueiro MG, Plitnick BA, Lok A, et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging. 2014;9:1527-1537. PubMed
The hospital environment fails to promote adequate sleep for acutely or critically ill patients. Intensive care units (ICUs) have received the most scrutiny, because critically ill patients suffer from severely fragmented sleep as well as a lack of deeper, more restorative sleep.1-4 ICU survivors frequently cite sleep deprivation, contributed to by ambient noise, as a major stressor while receiving care.5,6 Importantly, efforts to modify the ICU environment to promote sleep have been associated with reductions in delirium.7,8 However, sleep deprivation and delirium in the hospital are not limited to ICU patients.
Sleep in the non-ICU setting is also notoriously poor, with 50%-80% of patients reporting sleep as “unsound” or otherwise subjectively poor.9-11 Additionally, patients frequently ask for and/or receive pharmacological sleeping aids12 despite little evidence of efficacy13 and increasing evidence of harm.14 Here too, efforts to improve sleep seems to attenuate risk of delirium,15 which remains a substantial problem on general wards, with incidence reported as high as 20%-30%. The reasons for poor sleep in the hospital are multifactorial, but data suggest that the inpatient environment, including noise and light levels, which are measurable and modifiable entities, contribute significantly to the problem.16
The World Health Organization (WHO) recommends that nighttime baseline noise levels do not exceed 30 decibels (dB) and that nighttime noise peaks (ie, loud noises) do not exceed 40 dB17; most studies suggest that ICU and general ward rooms are above this range on average.10,18 Others have also demonstrated an association between loud noises and patients’ subjective perception of poor sleep.10,19 However, when considering clinically important noise, peak and average noise levels may not be the key factor in causing arousals from sleep. Buxton and colleagues20 found that noise quality affects arousal probability; for example, electronic alarms and conversational noise are more likely to cause awakenings compared with the opening or closing of doors and ice machines. Importantly, peak and average noise levels may also matter less for sleep than do sound level changes (SLCs), which are defined as the difference between background/baseline noise and peak noise. Using healthy subjects exposed to simulated ICU noise, Stanchina et al.21 found that SLCs >17.5 dB were more likely to cause polysomnographic arousals from sleep regardless of peak noise level. This sound pressure change of approximately 20 dB would be perceived as 4 times louder, or, as an example, would be the difference between normal conversation between 2 people (~40 dB) that is then interrupted by the start of a vacuum cleaner (~60 dB). To our knowledge, no other studies have closely examined SLCs in different hospital environments.
Ambient light also likely affects sleep quality in the hospital. The circadian rhythm system, which controls the human sleep–wake cycle as well as multiple other physiologic functions, depends on ambient light as the primary external factor for regulating the internal clock.22,23 Insufficient and inappropriately timed light exposure can desynchronize the biological clock, thereby negatively affecting sleep quality.24,25 Conversely, patients exposed to early-morning bright light may sleep better while in the hospital.16 In addition to sleep patterns, ambient light affects other aspects of patient care; for example, lower light levels in the hospital have recently been associated with higher levels of fatigue and mood disturbance.26A growing body of data has investigated the ambient environment in the ICU, but fewer studies have focused on sound and light analysis in other inpatient areas such as the general ward and telemetry floors. We examined sound and light levels in the ICU and non-ICU environment, hypothesizing that average sound levels would be higher in the ICU than on non-ICU floors but that the number of SLCs >17.5 dB would be similar. Additionally, we expected that average light levels would be higher in the ICU than on non-ICU floors.
METHODS
This was an observational study of the sound and light environment in the inpatient setting. Per our Institutional Review Board, no consent was required. Battery-operated sound-level (SDL600, Extech Instruments, Nashua, NH) and light-level (SDL400, Extech Instruments, Nashua, NH) meters were placed in 24 patient rooms in our tertiary-care adult hospital in La Jolla, CA. Recordings were obtained in randomly selected, single-patient occupied rooms that were from 3 different hospital units and included 8 general ward rooms, 8 telemetry floor rooms, and 8 ICU rooms. We recorded for approximately 24-72 hours. Depending on the geographic layout of the room, meters were placed as close to the head of the patient’s bed as possible and were generally not placed farther than 2 meters away from the patient’s head of bed; all rooms contained a window.
Sound Measurements
Sound meters measured ambient noise in dB every 2 seconds and were set for A-weighted frequency measurements. We averaged individual data points to obtain hourly averages for ICU and non-ICU rooms. For hourly sound averages, we further separated the data to compare the general ward telemetry floors (both non-ICU), the latter of which has more patient monitoring and a lower nurse-to-patient ratio compared with the general ward floor.
Data from ICU versus non-ICU rooms were analyzed for the number of sound peaks throughout the 24-hour day and for sound peak over the nighttime, defined as the number of times sound levels exceeded 65 dB, 70 dB, or 80 dB, which were averaged over 24 hours and over the nighttime (10 PM to 6 AM). We also calculated the number of average SLCs ≥17.5 dB observed over 24 hours and over the nighttime.
Light Measurements
Light meters measured luminescence in lux at a frequency of 120 seconds. We averaged individual data points to obtain hourly averages for ICU and non-ICU rooms. In addition to hourly averages, light-level data were analyzed for maximum levels throughout the day and night.
Statistical Analysis
Hourly sound-level averages between the 3 floors were evaluated using a 1-way analysis of variance (ANOVA); sound averages from the general ward and telemetry floor were also compared at each hour using a Student t test. Light-level data, sound-level peak data, as well as SLC data were also evaluated using a Student t test.
RESULTS
Sound Measurements
Examples of the raw data distribution for individual sound recordings in an ICU and non-ICU room are shown in Figure 1A and 1B. Sound-level analysis with specific average values and significance levels between ICU and non-ICU rooms (with non-ICU rooms further divided between telemetry and general ward floors for purposes of hourly averages) are shown in Table 1. The average hourly values in all 3 locations were always above the 30-35 dB level (nighttime and daytime, respectively) recommended by the WHO (Figure 1C). A 1-way ANOVA analysis revealed significant differences between the 3 floors at all time points except for 10 AM. An analysis of the means at each time point between the telemetry floor and the general ward floor showed that the telemetry floor had significantly higher sound averages compared with the general ward floor at 10 PM, 11 PM, and 12 AM. Sound levels dropped during the nighttime on both non-ICU wards but remained fairly constant throughout the day and night in the ICU.
Importantly, despite average and peak sound levels showing that the ICU environment is louder overall, there were an equivalent number of SLCs ≥ 17.5 dB in the ICU and on non-ICU floors. The number of SLCs ≥ 17.5 dB is not statistically different when comparing ICU and non-ICU rooms either averaged over 24 hours or averaged over the nighttime (Figure 1E).
Light Measurements
Examples of light levels over a 24-hour period in an ICU and non-ICU room are shown in Figure 2A and 2B, respectively. Maximum average light levels (reported here as average value ± standard deviation to demonstrate variability within the data) in the ICU were 169.7 ± 127.1 lux and occurred at 1 PM, while maximum average light levels in the non-ICU rooms were 213.5 ± 341.6 lux and occurred at 5 PM (Figure 2C). Average light levels in the morning hours remained low and ranged from 15.9 ± 12.7 lux to 38.9 ± 43.4 lux in the ICU and from 22.3 ± 17.5 lux to 100.7 ± 92.0 lux on the non-ICU floors. The maximum measured level from any of the recordings was 2530 lux and occurred in a general ward room in the 5 PM hour. Overall, light averages remained low, but this particular room had light levels that were significantly higher than the others. A t test analysis of the hourly averages revealed only 1 time point of significant difference between the 2 floors; at 7 AM, the general ward floor had a higher lux level of 49.9 ± 27.5 versus 19.2 ± 10.7 in the ICU (P = 0.038). Otherwise, there were no differences between light levels in ICU rooms versus non-ICU rooms. Evaluation of the data revealed a substantial amount of variability in light levels throughout the daytime hours. Light levels during the nighttime remained low and were not significantly different between the 2 groups.
DISCUSSION
To our knowledge, this is the first study to directly compare the ICU and non-ICU environment for its potential impact on sleep and circadian alignment. Our study adds to the literature with several novel findings. First, average sound levels on non-ICU wards are lower than in the ICU. Second, although quieter on average, SLCs >17.5 dB occurred an equivalent number of times for both the ICU and non-ICU wards. Third, average daytime light levels in both the ICU and non-ICU environment are low. Lastly, peak light levels for both ICU and non-ICU wards occur later in the day instead of in the morning. All of the above have potential impact for optimizing the ward environment to better aid in sleep for patients.
Sound-Level Findings
Data on sound levels for non-ICU floors are limited but mostly consistent with our finding
Average and peak sound levels contribute to the ambient noise experienced by patients but may not be the source of sleep disruptions. Using polysomnography in healthy subjects exposed to recordings of ICU noise, Stanchina et al.21 showed that SLCs from baseline and not peak sound levels determined whether a subject was aroused from sleep by sound. Accordingly, they also found that increasing baseline sound levels by using white noise reduced the number of arousals that subjects experienced. To our knowledge, other studies have not quantified and compared SLCs in the ICU and non-ICU environments. Our data show that patients on non-ICU floors experience at least the same number of SLCs, and thereby the same potential for arousals from sleep, when compared with ICU patients. The higher baseline level of noise in the ICU likely explains the relatively lower number of SLCs when compared with the non-ICU floors. Although decreasing overall noise to promote sleep in the hospital seems like the obvious solution, the treatment for noise pollution in the hospital may actually be more background noise, not less.
Recent studies support the clinical implications of our findings. First, decreasing overall noise levels is difficult to accomplish.29 Second, recent studies utilized white noise in different hospital settings with some success in improving patients’ subjective sleep quality, although more studies using objective data measurements are needed to further understand the impact of white noise on sleep in hospitalized patients.30,31 Third, efforts at reducing interruptions—which likely will decrease the number of SLCs—such as clustering nursing care or reducing intermittent alarms may be more beneficial in improving sleep than efforts at decreasing average sound levels. For example, Bartick et al. reduced the number of patient interruptions at night by eliminating routine vital signs and clustering medication administration. Although they included other interventions as well, we note that this approach likely reduced SLCs and was associated with a reduction in the use of sedative medications.32 Ultimately, our data show that a focus on reducing SLCs will be one necessary component of a multipronged solution to improving inpatient sleep.33
Light-Level Findings
Because of its effect on circadian rhythms, the daily light-dark cycle has a powerful impact on human physiology and behavior, which includes sleep.34 Little is understood about how light affects sleep and other circadian-related functions in general ward patients, as it is not commonly measured. Our findings suggest that patients admitted to the hospital are exposed to light levels and patterns that may not optimally promote wake and sleep. Encouragingly, we did not find excessive average light levels during the nighttime in either ICU or non-ICU environment of our hospital, although others have described intrusive nighttime light in the hospital setting.35,36 Even short bursts of low or moderate light during the nighttime can cause circadian phase delay,37 and efforts to maintain darkness in patient rooms at night should continue.
Our measurements show that average daytime light levels did not exceed 250 lux, which corresponds to low, office-level lighting, while the brightest average light levels occurred in the afternoon for both environments. These levels are consistent with other reports26,35,36 as is the light-level variability noted throughout the day (which is not unexpected given room positioning, patient preference, curtains, etc). The level and amount of daytime light needed to maintain circadian rhythms in humans is still unknown.38 Brighter light is generally more effective at influencing the circadian pacemaker in a dose-dependent manner.39 Although entrainment (synchronization of the body’s biological rhythm with environmental cues such as ambient light) of the human circadian rhythm has been shown with low light levels (eg, <100 lux), these studies included healthy volunteers in a carefully controlled, constant, routine environment.23 How these data apply to acutely ill subjects in the hospital environment is not clear. We note that low to moderate levels of light (50-1000 lux) are less effective for entrainment of the circadian rhythm in older people (age >65 years, the majority of our admissions) compared with younger people. Thus, older, hospitalized patients may require greater light levels for regulation of the sleep-wake cycle.40 These data are important when designing interventions to improve light for and maintain circadian rhythms in hospitalized patients. For example, Simons et al. found that dynamic light-application therapy, which achieved a maximum average lux level of <800 lux, did not reduce rates of delirium in critically ill patients (mean age ~65). One interpretation of these results, though there are many others, is that the light levels achieved were not high enough to influence circadian timing in hospitalized, mostly elderly patients. The physiological impact of light on the circadian rhythm in hospitalized patients still remains to be measured.
LIMITATIONS
Our study does have a few limitations. We did not assess sound quality, which is another determinant of arousal potential.20 Also, a shorter measurement interval might be useful in determining sharper sound increases. It may also be important to consider A- versus C-weighted measurements of sound levels, as A-weighted measurements usually reflect higher-frequency sound while C-weighted measurements usually reflect low-frequency noise18; we obtained only A-weighted measurements in our study. However, A-weighted measurements are generally considered more reflective of what the human ear considers noise and are used more standardly than C-weighted measurements.
Regarding light measurements, we recorded from rooms facing different cardinal directions and during different times of the year, which likely contributed to some of the variability in the daytime light levels on both floors. Additionally, light levels were not measured directly at the patient’s eye level. However, given that overhead fluorescent lighting was the primary source of lighting, it is doubtful that we substantially underestimated optic-nerve light levels. In the future, it may also be important to measure the different wavelengths of lights, as blue light may have a greater impact on sleep than other wavelengths.41 Although our findings align with others’, we note that this was a single-center study, which could limit the generalizability of our findings given inter-hospital variations in patient volume, interior layout and structure, and geographic location.
CONCLUSIONS
Overall, our study suggests that the light and sound environment for sleep in the inpatient setting, including both the ICU and non-ICU wards, has multiple areas for improvement. Our data also suggest specific directions for future clinical efforts at improvement. For example, efforts to decrease average sound levels may worsen sleep fragmentation. Similarly, more light during the day may be more helpful than further attempts to limit light during the night.
Disclosure
This research was funded in part by a NIH/NCATS flagship Clinical and Translational Science Award Grant (5KL2TR001112). None of the authors report any conflict of interest, financial or otherwise, in the preparation of this article.
The hospital environment fails to promote adequate sleep for acutely or critically ill patients. Intensive care units (ICUs) have received the most scrutiny, because critically ill patients suffer from severely fragmented sleep as well as a lack of deeper, more restorative sleep.1-4 ICU survivors frequently cite sleep deprivation, contributed to by ambient noise, as a major stressor while receiving care.5,6 Importantly, efforts to modify the ICU environment to promote sleep have been associated with reductions in delirium.7,8 However, sleep deprivation and delirium in the hospital are not limited to ICU patients.
Sleep in the non-ICU setting is also notoriously poor, with 50%-80% of patients reporting sleep as “unsound” or otherwise subjectively poor.9-11 Additionally, patients frequently ask for and/or receive pharmacological sleeping aids12 despite little evidence of efficacy13 and increasing evidence of harm.14 Here too, efforts to improve sleep seems to attenuate risk of delirium,15 which remains a substantial problem on general wards, with incidence reported as high as 20%-30%. The reasons for poor sleep in the hospital are multifactorial, but data suggest that the inpatient environment, including noise and light levels, which are measurable and modifiable entities, contribute significantly to the problem.16
The World Health Organization (WHO) recommends that nighttime baseline noise levels do not exceed 30 decibels (dB) and that nighttime noise peaks (ie, loud noises) do not exceed 40 dB17; most studies suggest that ICU and general ward rooms are above this range on average.10,18 Others have also demonstrated an association between loud noises and patients’ subjective perception of poor sleep.10,19 However, when considering clinically important noise, peak and average noise levels may not be the key factor in causing arousals from sleep. Buxton and colleagues20 found that noise quality affects arousal probability; for example, electronic alarms and conversational noise are more likely to cause awakenings compared with the opening or closing of doors and ice machines. Importantly, peak and average noise levels may also matter less for sleep than do sound level changes (SLCs), which are defined as the difference between background/baseline noise and peak noise. Using healthy subjects exposed to simulated ICU noise, Stanchina et al.21 found that SLCs >17.5 dB were more likely to cause polysomnographic arousals from sleep regardless of peak noise level. This sound pressure change of approximately 20 dB would be perceived as 4 times louder, or, as an example, would be the difference between normal conversation between 2 people (~40 dB) that is then interrupted by the start of a vacuum cleaner (~60 dB). To our knowledge, no other studies have closely examined SLCs in different hospital environments.
Ambient light also likely affects sleep quality in the hospital. The circadian rhythm system, which controls the human sleep–wake cycle as well as multiple other physiologic functions, depends on ambient light as the primary external factor for regulating the internal clock.22,23 Insufficient and inappropriately timed light exposure can desynchronize the biological clock, thereby negatively affecting sleep quality.24,25 Conversely, patients exposed to early-morning bright light may sleep better while in the hospital.16 In addition to sleep patterns, ambient light affects other aspects of patient care; for example, lower light levels in the hospital have recently been associated with higher levels of fatigue and mood disturbance.26A growing body of data has investigated the ambient environment in the ICU, but fewer studies have focused on sound and light analysis in other inpatient areas such as the general ward and telemetry floors. We examined sound and light levels in the ICU and non-ICU environment, hypothesizing that average sound levels would be higher in the ICU than on non-ICU floors but that the number of SLCs >17.5 dB would be similar. Additionally, we expected that average light levels would be higher in the ICU than on non-ICU floors.
METHODS
This was an observational study of the sound and light environment in the inpatient setting. Per our Institutional Review Board, no consent was required. Battery-operated sound-level (SDL600, Extech Instruments, Nashua, NH) and light-level (SDL400, Extech Instruments, Nashua, NH) meters were placed in 24 patient rooms in our tertiary-care adult hospital in La Jolla, CA. Recordings were obtained in randomly selected, single-patient occupied rooms that were from 3 different hospital units and included 8 general ward rooms, 8 telemetry floor rooms, and 8 ICU rooms. We recorded for approximately 24-72 hours. Depending on the geographic layout of the room, meters were placed as close to the head of the patient’s bed as possible and were generally not placed farther than 2 meters away from the patient’s head of bed; all rooms contained a window.
Sound Measurements
Sound meters measured ambient noise in dB every 2 seconds and were set for A-weighted frequency measurements. We averaged individual data points to obtain hourly averages for ICU and non-ICU rooms. For hourly sound averages, we further separated the data to compare the general ward telemetry floors (both non-ICU), the latter of which has more patient monitoring and a lower nurse-to-patient ratio compared with the general ward floor.
Data from ICU versus non-ICU rooms were analyzed for the number of sound peaks throughout the 24-hour day and for sound peak over the nighttime, defined as the number of times sound levels exceeded 65 dB, 70 dB, or 80 dB, which were averaged over 24 hours and over the nighttime (10 PM to 6 AM). We also calculated the number of average SLCs ≥17.5 dB observed over 24 hours and over the nighttime.
Light Measurements
Light meters measured luminescence in lux at a frequency of 120 seconds. We averaged individual data points to obtain hourly averages for ICU and non-ICU rooms. In addition to hourly averages, light-level data were analyzed for maximum levels throughout the day and night.
Statistical Analysis
Hourly sound-level averages between the 3 floors were evaluated using a 1-way analysis of variance (ANOVA); sound averages from the general ward and telemetry floor were also compared at each hour using a Student t test. Light-level data, sound-level peak data, as well as SLC data were also evaluated using a Student t test.
RESULTS
Sound Measurements
Examples of the raw data distribution for individual sound recordings in an ICU and non-ICU room are shown in Figure 1A and 1B. Sound-level analysis with specific average values and significance levels between ICU and non-ICU rooms (with non-ICU rooms further divided between telemetry and general ward floors for purposes of hourly averages) are shown in Table 1. The average hourly values in all 3 locations were always above the 30-35 dB level (nighttime and daytime, respectively) recommended by the WHO (Figure 1C). A 1-way ANOVA analysis revealed significant differences between the 3 floors at all time points except for 10 AM. An analysis of the means at each time point between the telemetry floor and the general ward floor showed that the telemetry floor had significantly higher sound averages compared with the general ward floor at 10 PM, 11 PM, and 12 AM. Sound levels dropped during the nighttime on both non-ICU wards but remained fairly constant throughout the day and night in the ICU.
Importantly, despite average and peak sound levels showing that the ICU environment is louder overall, there were an equivalent number of SLCs ≥ 17.5 dB in the ICU and on non-ICU floors. The number of SLCs ≥ 17.5 dB is not statistically different when comparing ICU and non-ICU rooms either averaged over 24 hours or averaged over the nighttime (Figure 1E).
Light Measurements
Examples of light levels over a 24-hour period in an ICU and non-ICU room are shown in Figure 2A and 2B, respectively. Maximum average light levels (reported here as average value ± standard deviation to demonstrate variability within the data) in the ICU were 169.7 ± 127.1 lux and occurred at 1 PM, while maximum average light levels in the non-ICU rooms were 213.5 ± 341.6 lux and occurred at 5 PM (Figure 2C). Average light levels in the morning hours remained low and ranged from 15.9 ± 12.7 lux to 38.9 ± 43.4 lux in the ICU and from 22.3 ± 17.5 lux to 100.7 ± 92.0 lux on the non-ICU floors. The maximum measured level from any of the recordings was 2530 lux and occurred in a general ward room in the 5 PM hour. Overall, light averages remained low, but this particular room had light levels that were significantly higher than the others. A t test analysis of the hourly averages revealed only 1 time point of significant difference between the 2 floors; at 7 AM, the general ward floor had a higher lux level of 49.9 ± 27.5 versus 19.2 ± 10.7 in the ICU (P = 0.038). Otherwise, there were no differences between light levels in ICU rooms versus non-ICU rooms. Evaluation of the data revealed a substantial amount of variability in light levels throughout the daytime hours. Light levels during the nighttime remained low and were not significantly different between the 2 groups.
DISCUSSION
To our knowledge, this is the first study to directly compare the ICU and non-ICU environment for its potential impact on sleep and circadian alignment. Our study adds to the literature with several novel findings. First, average sound levels on non-ICU wards are lower than in the ICU. Second, although quieter on average, SLCs >17.5 dB occurred an equivalent number of times for both the ICU and non-ICU wards. Third, average daytime light levels in both the ICU and non-ICU environment are low. Lastly, peak light levels for both ICU and non-ICU wards occur later in the day instead of in the morning. All of the above have potential impact for optimizing the ward environment to better aid in sleep for patients.
Sound-Level Findings
Data on sound levels for non-ICU floors are limited but mostly consistent with our finding
Average and peak sound levels contribute to the ambient noise experienced by patients but may not be the source of sleep disruptions. Using polysomnography in healthy subjects exposed to recordings of ICU noise, Stanchina et al.21 showed that SLCs from baseline and not peak sound levels determined whether a subject was aroused from sleep by sound. Accordingly, they also found that increasing baseline sound levels by using white noise reduced the number of arousals that subjects experienced. To our knowledge, other studies have not quantified and compared SLCs in the ICU and non-ICU environments. Our data show that patients on non-ICU floors experience at least the same number of SLCs, and thereby the same potential for arousals from sleep, when compared with ICU patients. The higher baseline level of noise in the ICU likely explains the relatively lower number of SLCs when compared with the non-ICU floors. Although decreasing overall noise to promote sleep in the hospital seems like the obvious solution, the treatment for noise pollution in the hospital may actually be more background noise, not less.
Recent studies support the clinical implications of our findings. First, decreasing overall noise levels is difficult to accomplish.29 Second, recent studies utilized white noise in different hospital settings with some success in improving patients’ subjective sleep quality, although more studies using objective data measurements are needed to further understand the impact of white noise on sleep in hospitalized patients.30,31 Third, efforts at reducing interruptions—which likely will decrease the number of SLCs—such as clustering nursing care or reducing intermittent alarms may be more beneficial in improving sleep than efforts at decreasing average sound levels. For example, Bartick et al. reduced the number of patient interruptions at night by eliminating routine vital signs and clustering medication administration. Although they included other interventions as well, we note that this approach likely reduced SLCs and was associated with a reduction in the use of sedative medications.32 Ultimately, our data show that a focus on reducing SLCs will be one necessary component of a multipronged solution to improving inpatient sleep.33
Light-Level Findings
Because of its effect on circadian rhythms, the daily light-dark cycle has a powerful impact on human physiology and behavior, which includes sleep.34 Little is understood about how light affects sleep and other circadian-related functions in general ward patients, as it is not commonly measured. Our findings suggest that patients admitted to the hospital are exposed to light levels and patterns that may not optimally promote wake and sleep. Encouragingly, we did not find excessive average light levels during the nighttime in either ICU or non-ICU environment of our hospital, although others have described intrusive nighttime light in the hospital setting.35,36 Even short bursts of low or moderate light during the nighttime can cause circadian phase delay,37 and efforts to maintain darkness in patient rooms at night should continue.
Our measurements show that average daytime light levels did not exceed 250 lux, which corresponds to low, office-level lighting, while the brightest average light levels occurred in the afternoon for both environments. These levels are consistent with other reports26,35,36 as is the light-level variability noted throughout the day (which is not unexpected given room positioning, patient preference, curtains, etc). The level and amount of daytime light needed to maintain circadian rhythms in humans is still unknown.38 Brighter light is generally more effective at influencing the circadian pacemaker in a dose-dependent manner.39 Although entrainment (synchronization of the body’s biological rhythm with environmental cues such as ambient light) of the human circadian rhythm has been shown with low light levels (eg, <100 lux), these studies included healthy volunteers in a carefully controlled, constant, routine environment.23 How these data apply to acutely ill subjects in the hospital environment is not clear. We note that low to moderate levels of light (50-1000 lux) are less effective for entrainment of the circadian rhythm in older people (age >65 years, the majority of our admissions) compared with younger people. Thus, older, hospitalized patients may require greater light levels for regulation of the sleep-wake cycle.40 These data are important when designing interventions to improve light for and maintain circadian rhythms in hospitalized patients. For example, Simons et al. found that dynamic light-application therapy, which achieved a maximum average lux level of <800 lux, did not reduce rates of delirium in critically ill patients (mean age ~65). One interpretation of these results, though there are many others, is that the light levels achieved were not high enough to influence circadian timing in hospitalized, mostly elderly patients. The physiological impact of light on the circadian rhythm in hospitalized patients still remains to be measured.
LIMITATIONS
Our study does have a few limitations. We did not assess sound quality, which is another determinant of arousal potential.20 Also, a shorter measurement interval might be useful in determining sharper sound increases. It may also be important to consider A- versus C-weighted measurements of sound levels, as A-weighted measurements usually reflect higher-frequency sound while C-weighted measurements usually reflect low-frequency noise18; we obtained only A-weighted measurements in our study. However, A-weighted measurements are generally considered more reflective of what the human ear considers noise and are used more standardly than C-weighted measurements.
Regarding light measurements, we recorded from rooms facing different cardinal directions and during different times of the year, which likely contributed to some of the variability in the daytime light levels on both floors. Additionally, light levels were not measured directly at the patient’s eye level. However, given that overhead fluorescent lighting was the primary source of lighting, it is doubtful that we substantially underestimated optic-nerve light levels. In the future, it may also be important to measure the different wavelengths of lights, as blue light may have a greater impact on sleep than other wavelengths.41 Although our findings align with others’, we note that this was a single-center study, which could limit the generalizability of our findings given inter-hospital variations in patient volume, interior layout and structure, and geographic location.
CONCLUSIONS
Overall, our study suggests that the light and sound environment for sleep in the inpatient setting, including both the ICU and non-ICU wards, has multiple areas for improvement. Our data also suggest specific directions for future clinical efforts at improvement. For example, efforts to decrease average sound levels may worsen sleep fragmentation. Similarly, more light during the day may be more helpful than further attempts to limit light during the night.
Disclosure
This research was funded in part by a NIH/NCATS flagship Clinical and Translational Science Award Grant (5KL2TR001112). None of the authors report any conflict of interest, financial or otherwise, in the preparation of this article.
1. Freedman NS, Gazendam J, Levan L, Pack AI, Schwab RJ. Abnormal sleep/wake
cycles and the effect of environmental noise on sleep disruption in the intensive
care unit. Am J Respir Crit Care Med. 2001;163(2):451-457. PubMed
2. Watson PL, Pandharipande P, Gehlbach BK, et al. Atypical sleep in ventilated
patients: empirical electroencephalography findings and the path toward revised ICU sleep scoring criteria. Crit Care Med. 2013;41(8):1958-1967. PubMed
3. Gehlbach BK, Chapotot F, Leproult R, et al. Temporal disorganization of circadian rhythmicity and sleep-wake regulation in mechanically ventilated patients receiving continuous intravenous sedation. Sleep. 2012;35(8):1105-1114. PubMed
4. Elliott R, McKinley S, Cistulli P, Fien M. Characterisation of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care. 2013;17(2):R46. PubMed
5. Novaes MA, Aronovich A, Ferraz MB, Knobel E. Stressors in ICU: patients’ evaluation. Intensive Care Med. 1997;23(12):1282-1285. PubMed
6. Tembo AC, Parker V, Higgins I. The experience of sleep deprivation in intensive care patients: findings from a larger hermeneutic phenomenological study. Intensive Crit Care Nurs. 2013;29(6):310-316. PubMed
7. Kamdar BB, Yang J, King LM, et al. Developing, implementing, and evaluating a multifaceted quality improvement intervention to promote sleep in an ICU. Am J Med Qual. 2014;29(6):546-554. PubMed
8. Patel J, Baldwin J, Bunting P, Laha S. The effect of a multicomponent multidisciplinary bundle of interventions on sleep and delirium in medical and surgical intensive care patients. Anaesthesia. 2014;69(6):540-549. PubMed
9. Manian FA, Manian CJ. Sleep quality in adult hospitalized patients with infection: an observational study. Am J Med Sci. 2015;349(1):56-60. PubMed
10. Park MJ, Yoo JH, Cho BW, Kim KT, Jeong WC, Ha M. Noise in hospital rooms and sleep disturbance in hospitalized medical patients. Environ Health Toxicol. 2014;29:e2014006. PubMed
11. Dobing S, Frolova N, McAlister F, Ringrose J. Sleep quality and factors influencing self-reported sleep duration and quality in the general internal medicine inpatient population. PLoS One. 2016;11(6):e0156735. PubMed
12. Gillis CM, Poyant JO, Degrado JR, Ye L, Anger KE, Owens RL. Inpatient pharmacological
sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652-657. PubMed
13. Krenk L, Jennum P, Kehlet H. Postoperative sleep disturbances after zolpidem treatment in fast-track hip and knee replacement. J Clin Sleep Med. 2014;10(3):321-326. PubMed
14. Kolla BP, Lovely JK, Mansukhani MP, Morgenthaler TI. Zolpidem is independently
associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1-6. PubMed
15. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. PubMed
16. Bano M, Chiaromanni F, Corrias M, et al. The influence of environmental factors on sleep quality in hospitalized medical patients. Front Neurol. 2014;5:267. PubMed
17. Berglund BLTSD. Guidelines for Community Noise. World Health Organization. 1999.
18. Knauert M, Jeon S, Murphy TE, Yaggi HK, Pisani MA, Redeker NS. Comparing average levels and peak occurrence of overnight sound in the medical intensive care unit on A-weighted and C-weighted decibel scales. J Crit Care. 2016;36:1-7. PubMed
19. Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172(1):68-70. PubMed
20. Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. PubMed
21. Stanchina ML, Abu-Hijleh M, Chaudhry BK, Carlisle CC, Millman RP. The influence of white noise on sleep in subjects exposed to ICU noise. Sleep Med. 2005;6(5):423-428. PubMed
22. Czeisler CA, Allan JS, Strogatz SH, et al. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science. 1986;233(4764):667-671. PubMed
23. Duffy JF, Czeisler CA. Effect of light on human circadian physiology. Sleep Med Clin. 2009;4(2):165-177. PubMed
24. Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210(4475):1267-1269. PubMed
25. Zeitzer JM, Dijk DJ, Kronauer R, Brown E, Czeisler C. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J Physiol. 2000;526:695-702. PubMed
26. Bernhofer EI, Higgins PA, Daly BJ, Burant CJ, Hornick TR. Hospital lighting and its association with sleep, mood and pain in medical inpatients. J Adv Nurs. 2014;70(5):1164-1173. PubMed
27. Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care. 2013;17(5):R187. PubMed
28. Gillis S. Pharmacologic treatment of depression during pregnancy. J Midwifery Womens Health. 2000;45(4):357-359. PubMed
29. Tainter CR, Levine AR, Quraishi SA, et al. Noise levels in surgical ICUs are consistently above recommended standards. Crit Care Med. 2016;44(1):147-152. PubMed
30. Farrehi PM, Clore KR, Scott JR, Vanini G, Clauw DJ. Efficacy of Sleep Tool Education During Hospitalization: A Randomized Controlled Trial. Am J Med. 2016;129(12):1329.e9-1329.e17. PubMed
31. Farokhnezhad Afshar P, Bahramnezhad F, Asgari P, Shiri M. Effect of white noise on sleep in patients admitted to a coronary care. J Caring Sci. 2016;5(2):103-109. PubMed
32. Bartick MC, Thai X, Schmidt T, Altaye A, Solet JM. Decrease in as-needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5(3):E20-E24. PubMed
33. Tamrat R, Huynh-Le MP, Goyal M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: a systematic review. J Gen Intern Med. 2014;29(5):788-795. PubMed
34. Dijk DJ, Archer SN. Light, sleep, and circadian rhythms: together again. PLoS Biol. 2009;7(6):e1000145. PubMed
35. Verceles AC, Liu X, Terrin ML, et al. Ambient light levels and critical care outcomes. J Crit Care. 2013;28(1):110.e1-110.e8. PubMed
36. Hu RF, Hegadoren KM, Wang XY, Jiang XY. An investigation of light and sound levels on intensive care units in China. Aust Crit Care. 2016;29(2):62-67. PubMed
37. Zeitzer JM, Ruby NF, Fisicaro RA, Heller HC. Response of the human circadian system to millisecond flashes of light. PLoS One. 2011;6(7):e22078. PubMed
38. Duffy JF, Wright KP, Jr. Entrainment of the human circadian system by light. J Biol Rhythms. 2005;20(4):326-338. PubMed
39. Wright KP Jr, Gronfier C, Duffy JF, Czeisler CA. Intrinsic period and light intensity determine the phase relationship between melatonin and sleep in humans. J Biol Rhythms. 2005;20(2):168-177. PubMed
40. Duffy JF, Zeitzer JM, Czeisler CA. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol Aging. 2007;28(5):799-807. PubMed
41. Figueiro MG, Plitnick BA, Lok A, et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging. 2014;9:1527-1537. PubMed
1. Freedman NS, Gazendam J, Levan L, Pack AI, Schwab RJ. Abnormal sleep/wake
cycles and the effect of environmental noise on sleep disruption in the intensive
care unit. Am J Respir Crit Care Med. 2001;163(2):451-457. PubMed
2. Watson PL, Pandharipande P, Gehlbach BK, et al. Atypical sleep in ventilated
patients: empirical electroencephalography findings and the path toward revised ICU sleep scoring criteria. Crit Care Med. 2013;41(8):1958-1967. PubMed
3. Gehlbach BK, Chapotot F, Leproult R, et al. Temporal disorganization of circadian rhythmicity and sleep-wake regulation in mechanically ventilated patients receiving continuous intravenous sedation. Sleep. 2012;35(8):1105-1114. PubMed
4. Elliott R, McKinley S, Cistulli P, Fien M. Characterisation of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care. 2013;17(2):R46. PubMed
5. Novaes MA, Aronovich A, Ferraz MB, Knobel E. Stressors in ICU: patients’ evaluation. Intensive Care Med. 1997;23(12):1282-1285. PubMed
6. Tembo AC, Parker V, Higgins I. The experience of sleep deprivation in intensive care patients: findings from a larger hermeneutic phenomenological study. Intensive Crit Care Nurs. 2013;29(6):310-316. PubMed
7. Kamdar BB, Yang J, King LM, et al. Developing, implementing, and evaluating a multifaceted quality improvement intervention to promote sleep in an ICU. Am J Med Qual. 2014;29(6):546-554. PubMed
8. Patel J, Baldwin J, Bunting P, Laha S. The effect of a multicomponent multidisciplinary bundle of interventions on sleep and delirium in medical and surgical intensive care patients. Anaesthesia. 2014;69(6):540-549. PubMed
9. Manian FA, Manian CJ. Sleep quality in adult hospitalized patients with infection: an observational study. Am J Med Sci. 2015;349(1):56-60. PubMed
10. Park MJ, Yoo JH, Cho BW, Kim KT, Jeong WC, Ha M. Noise in hospital rooms and sleep disturbance in hospitalized medical patients. Environ Health Toxicol. 2014;29:e2014006. PubMed
11. Dobing S, Frolova N, McAlister F, Ringrose J. Sleep quality and factors influencing self-reported sleep duration and quality in the general internal medicine inpatient population. PLoS One. 2016;11(6):e0156735. PubMed
12. Gillis CM, Poyant JO, Degrado JR, Ye L, Anger KE, Owens RL. Inpatient pharmacological
sleep aid utilization is common at a tertiary medical center. J Hosp Med. 2014;9(10):652-657. PubMed
13. Krenk L, Jennum P, Kehlet H. Postoperative sleep disturbances after zolpidem treatment in fast-track hip and knee replacement. J Clin Sleep Med. 2014;10(3):321-326. PubMed
14. Kolla BP, Lovely JK, Mansukhani MP, Morgenthaler TI. Zolpidem is independently
associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1-6. PubMed
15. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. PubMed
16. Bano M, Chiaromanni F, Corrias M, et al. The influence of environmental factors on sleep quality in hospitalized medical patients. Front Neurol. 2014;5:267. PubMed
17. Berglund BLTSD. Guidelines for Community Noise. World Health Organization. 1999.
18. Knauert M, Jeon S, Murphy TE, Yaggi HK, Pisani MA, Redeker NS. Comparing average levels and peak occurrence of overnight sound in the medical intensive care unit on A-weighted and C-weighted decibel scales. J Crit Care. 2016;36:1-7. PubMed
19. Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: far from a quiet night. Arch Intern Med. 2012;172(1):68-70. PubMed
20. Buxton OM, Ellenbogen JM, Wang W, et al. Sleep disruption due to hospital noises: a prospective evaluation. Ann Intern Med. 2012;157(3):170-179. PubMed
21. Stanchina ML, Abu-Hijleh M, Chaudhry BK, Carlisle CC, Millman RP. The influence of white noise on sleep in subjects exposed to ICU noise. Sleep Med. 2005;6(5):423-428. PubMed
22. Czeisler CA, Allan JS, Strogatz SH, et al. Bright light resets the human circadian pacemaker independent of the timing of the sleep-wake cycle. Science. 1986;233(4764):667-671. PubMed
23. Duffy JF, Czeisler CA. Effect of light on human circadian physiology. Sleep Med Clin. 2009;4(2):165-177. PubMed
24. Lewy AJ, Wehr TA, Goodwin FK, Newsome DA, Markey SP. Light suppresses melatonin secretion in humans. Science. 1980;210(4475):1267-1269. PubMed
25. Zeitzer JM, Dijk DJ, Kronauer R, Brown E, Czeisler C. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J Physiol. 2000;526:695-702. PubMed
26. Bernhofer EI, Higgins PA, Daly BJ, Burant CJ, Hornick TR. Hospital lighting and its association with sleep, mood and pain in medical inpatients. J Adv Nurs. 2014;70(5):1164-1173. PubMed
27. Darbyshire JL, Young JD. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care. 2013;17(5):R187. PubMed
28. Gillis S. Pharmacologic treatment of depression during pregnancy. J Midwifery Womens Health. 2000;45(4):357-359. PubMed
29. Tainter CR, Levine AR, Quraishi SA, et al. Noise levels in surgical ICUs are consistently above recommended standards. Crit Care Med. 2016;44(1):147-152. PubMed
30. Farrehi PM, Clore KR, Scott JR, Vanini G, Clauw DJ. Efficacy of Sleep Tool Education During Hospitalization: A Randomized Controlled Trial. Am J Med. 2016;129(12):1329.e9-1329.e17. PubMed
31. Farokhnezhad Afshar P, Bahramnezhad F, Asgari P, Shiri M. Effect of white noise on sleep in patients admitted to a coronary care. J Caring Sci. 2016;5(2):103-109. PubMed
32. Bartick MC, Thai X, Schmidt T, Altaye A, Solet JM. Decrease in as-needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5(3):E20-E24. PubMed
33. Tamrat R, Huynh-Le MP, Goyal M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: a systematic review. J Gen Intern Med. 2014;29(5):788-795. PubMed
34. Dijk DJ, Archer SN. Light, sleep, and circadian rhythms: together again. PLoS Biol. 2009;7(6):e1000145. PubMed
35. Verceles AC, Liu X, Terrin ML, et al. Ambient light levels and critical care outcomes. J Crit Care. 2013;28(1):110.e1-110.e8. PubMed
36. Hu RF, Hegadoren KM, Wang XY, Jiang XY. An investigation of light and sound levels on intensive care units in China. Aust Crit Care. 2016;29(2):62-67. PubMed
37. Zeitzer JM, Ruby NF, Fisicaro RA, Heller HC. Response of the human circadian system to millisecond flashes of light. PLoS One. 2011;6(7):e22078. PubMed
38. Duffy JF, Wright KP, Jr. Entrainment of the human circadian system by light. J Biol Rhythms. 2005;20(4):326-338. PubMed
39. Wright KP Jr, Gronfier C, Duffy JF, Czeisler CA. Intrinsic period and light intensity determine the phase relationship between melatonin and sleep in humans. J Biol Rhythms. 2005;20(2):168-177. PubMed
40. Duffy JF, Zeitzer JM, Czeisler CA. Decreased sensitivity to phase-delaying effects of moderate intensity light in older subjects. Neurobiol Aging. 2007;28(5):799-807. PubMed
41. Figueiro MG, Plitnick BA, Lok A, et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin Interv Aging. 2014;9:1527-1537. PubMed
© 2017 Society of Hospital Medicine
Inpatient Sleep Aid Utilization
Sleep is known to be poor among hospitalized patients for many reasons.[1] Patients may have pain, dyspnea, or other discomforts that prevent sleep. Diagnostic and therapeutic procedures, including medication administration and routine nursing care, may take place during normal sleep times. Environmental factors such as noise and light frequently remain at daytime levels during normal sleep times.[2] In response, patients frequently request pharmacological sleep aids. Unfortunately, the use of sleep medications has been linked to clinically relevant and detrimental outcomes such as delirium and falls, particularly in the elderly. For example, in the landmark study by Inouye et al., a multicomponent intervention was used to successfully reduce delirium in older (>70 years) hospitalized patients.[3] One of the successful components was nonpharmacological sleep promotion, which reduced the use of pharmacological sleep aids from 46% to 35% of patients. Most recently, Kolla and colleagues found zolpidem tartrate use to be a risk factor (odds ratio 4.37) for inpatient falls, a known risk factor for morbidity and increased healthcare costs.[4]
The scope of recent pharmacological sleep aid use in the inpatient setting is not well described. Frighetto and colleagues described the pattern of in‐hospital drug use more than 12 years ago, before the concerns above were described, with 29% of patients receiving a medication for sleep, mostly benzodiazepines.[5] In 2008, Bartick and colleagues also found a very high rate of sleep aid use (42% of patients), but additionally described in 2010 an intervention to minimize sleep disruption that successfully reduced sleep aid use by 38%.[6] Both concerns over side effects and sleep promotion efforts might have reduced the current rate of medication use. Therefore, we sought to evaluate the prescription and administration of pharmacological sleep aids in general medical and surgical inpatients at our institution. Using our electronic medical records, including preadmission and discharge medication records, we assessed new and continued usage of medications for sleep complaints following hospital admission.
METHODS
Patients and Design
Records were reviewed for all adult patient (18 years or older) admissions to 1 of 4 units (2 general medicine and 2 general surgical units) from January 1, 2013 to February 28, 2013. These units do not have specific policies to promote sleep, such as nocturnal noise and light reduction or clustering of care. Brigham and Women's Hospital (BWH) is a 793‐bed university‐affiliated teaching hospital. Approval for this retrospective chart review study was obtained from the Partners Healthcare Institutional Review Board.
BWH uses an in‐house electronic health record system, which gathers information from a wider healthcare system (Partners Healthcare). Medications, problem lists, and allergies are available from within‐system providers and prior encounters. Admitting physicians are also required to document a preadmission medication list. A computerized physician order entry (CPOE) system is used for all medication orders. Although standardized admission order sets are used, none of these sets contains a pharmacological sleep aid. There is decision support for geriatric patients (age >65 years) that may recommend reduced starting doses for some medications.[7]
Medications Monitored for Treatment of Sleep Complaints
Using our electronic medication ordering and administration system, each patient admission was reviewed for any medication that might be used for treatment of sleep complaints. The list of sleep medications was based on those commonly used for the outpatient treatment of insomnia, as well as others included based on the authors' experience as clinical inpatient pharmacists.[8, 9, 10] Admissions were reviewed for the following medications: first generation antihistamines (diphenhydramine, hydroxyzine), tricyclic antidepressants (amitriptyline, nortriptyline, desipramine), serotonin‐norepinephrine reuptake inhibitor antidepressants (mirtazapine, trazodone, nefazodone), melatonin agonists (ramelteon), nonbenzodiazepine hypnotics (zolpidem tartrate, eszopiclone), benzodiazepines (oxazepam, temazepam, lorazepam, triazolam, diazepam), typical antipsychotics (haloperidol, fluphenazine, thioridazine, chlorpromazine), and atypical antipsychotics (quetiapine fumarate, ziprasidone, olanzapine, risperidone, aripiprazole). Melatonin, which is not regulated by the US Food and Drug Administration (FDA), cannot be prescribed using our CPOE system.
Determination of Medication Administration for Treatment of Sleep Complaints
The charts of patients receiving 1 or more of these monitored medications were then reviewed by the authors to determine if the medication was indeed prescribed for insomnia/sleep. Chart documents reviewed were the patient's problem list from outpatient provider notes; admission note, including past medical history and home medications; the preadmission medication list; and the inpatient daily progress note. The medication was considered to be used for sleep complaints (as opposed to another indication) when any of the additional following inclusion criteria were met: the medication was part of the patient's home medication regimen for insomnia, the medication order indicated that the medication was for insomnia/difficulty sleeping, or the medication was administered without a specific indication between the hours of 6 pm and 6 am. The medication was not considered to be used primarily as a sleep aid if any of the following were present (exclusion criteria): utilization for an as needed reason including anxiety, agitation, itching, nausea, muscle spasm; utilization for a documented disorder including depression, anxiety, schizophrenia, bipolar disorder, alcohol withdrawal, or epilepsy; intramuscular administration of olanzapine or ziprasidone; or topical administration of diphenhydramine.
Medication Administration Characteristics
For each medication that was administered for difficulty sleeping, the following data were documented: dose in milligrams, route of administration, time of administration, administration timing directions (eg, times 1 [x1], as needed [PRN], or standing), an increase or decrease in dose during hospital stay, documentation of the medication in discharge notes or discharge medications, and documentation of development of an allergy or adverse reaction due to the medication. Changes in dose were recorded. If a patient received more than 1 study medication, each individual medication and dose was evaluated for inclusion in the study analysis. Other data collected included the total number of days of exposure to each sleep aid during admission, the date of initiation, the total number of days of exposure to more than 1 sleep aid during admission, and the location of initiation of each individual sleep aid (eg, intensive care unit, medical floor). Appropriate time of administration was defined as sleep aid administration between 9 pm and 12 am.
RESULTS
Patients
During the 59‐day study period, there were 642 patients admitted to the study units. Two hundred seventy‐six patients received 1 of the monitored medications; however, 106 patients received the medication for an indication other than insomnia/difficulty sleeping. In 2 patients, incomplete records prevented ascertainment of the motivation for using the monitored medication. Thus, 168 patients (26.2%) were determined to have received a medication for sleep complaints and were included in the study analysis (Figure 1). Table 1 lists the characteristics of the 168 patients, of whom 10 had a prior documented sleep disorder such as insomnia (6 patients), restless leg syndrome (1 patient), and obstructive sleep apnea (3 patients). The rate of sleep medication use was lower, though not drastically so, in patients 65 years of age compared to those <65 years of age.

| Patients | Value |
|---|---|
| |
| Age, y | 57.919.8a |
| Age 65 years | 70 (41.7) |
| Age 64 years | 98 (58.3) |
| Female, n (%) | 97 (57.7) |
| Ethnicity, n (%) | |
| Caucasian | 114 (67.9) |
| Black | 18 (10.7) |
| Hispanic | 13 (7.7) |
| Other | 23 (13.7) |
| Admitted to floor from: | |
| Emergency department | 95 (56.5) |
| Operating room | 30 (17.9) |
| Transferred from outside hospital | 35 (20.8) |
| Intensive care unit | 8 (4.8) |
| Admission service, n (%) | |
| Medical | 109 (64.9) |
| Surgical | 59 (35.1) |
| Hospital length of stay | 10.516.0a |
| Known sleep disorder | |
| Insomnia | 6 (3.6) |
| Restless leg syndrome | 1 (0.6) |
| Obstructive sleep apnea | 3(1.8) |
Medications Used for Treatment of Sleep Complaints
Of the 25 monitored medications, 13 were administered to patients for sleep during the study period. The most commonly administered medications (percent of patients, median dose, absolute dose range) were trazodone (30.4%, 50 mg, 12.5450 mg), lorazepam (24.4%, 0.5 mg, 0.25 mg2 mg), and zolpidem tartrate (17.9%, 10 mg, 2.5 mg10 mg) (Table 2). As only a few of these medications (diphenhydramine, ramelteon, temazepam, triazolam, zolpidem) have a formal FDA indication for insomnia, most patients (72%) were treated using an off‐label medication. Although the types of medication used did not vary substantially between young and old patients, the median doses and ranges were lower in the elderly. Admitting service did not substantially influence the medication or dose chosen for sleep complaints (data not shown).
| Medication | All Patients, N=168, n (%) | Patients <65 Years Old, n=98, n (%) | Patients >65 Years Old, n=70, n (%) |
|---|---|---|---|
| |||
| Trazodoneb | 51 (30.4) | 29 (29.6) | 22 (31.4) |
| Median dose | 50 | 50 | 25 |
| Dose range | 12.5450 | 25450 | 12.5200 |
| Lorazepamc | 41 (24.4) | 24 (24.5) | 17 (24.3) |
| Median dose | 0.5 | 1 | 0.25 |
| Dose range | 0.252 | 0.252 | 0.251 |
| Zolpidem tartratec | 30 (17.9) | 20 (20.4) | 10 (14.3) |
| Median dose | 10 | 10 | 5 |
| Dose range | 2.510 | 2.510 | 2.510 |
| Quetiapine fumarate | 21 (12.5) | 9 (9.2) | 12 (17.1) |
| Median dose | 50 | 50 | 25 |
| Dose range | 12.5300 | 12.5300 | 12.5100 |
| Haloperidol | 18 (10.7) | 7 (7.1) | 11 (15.7) |
| Median dose | 1 | 5 | 1 |
| Dose range | 0.2510 | 0.510 | 0.251 |
| Diphenhydraminec | 16 (9.5) | 12 (12.2) | 4 (5.7) |
| Median dose | 25 | 25 | 12.5 |
| Dose range | 12.550 | 12.550 | 12.525 |
| Mirtazapine | 7 (4.2) | 3 (3.1) | 4 (5.7) |
| Median dose | 15 | 30 | 7.5 |
| Dose range | 7.545 | 7.530 | 7.545 |
| Olanzapine | 5 (3.6) | 3 (3.1) | 2 (2.9) |
| Median dose | 5 | 5 | 2.5 |
| Dose range | 2.512.5 | 512.5 | 2.52.5 |
| Amitriptyline | 5 (3.0) | 4 (4.1) | 1 (1.4) |
| Median dose | 25 | 25 | 25 |
| Dose range | 25100 | 25100 | |
| Diazepam | 5 (3.0) | 3 (3.1) | 2 (2.9) |
| Median dose | 5 | 5 | 10 |
| Dose range | 510 | ||
| Oxazepam | 2 (1.2) | 0 | 2 (2.9) |
| Median dose | 10 | 10 | |
| Dose range | 1010 | 1010 | |
| Temazepamc | 1 (0.6) | 0 | 1 (1.4) |
| Median dose | 15 | 15 | |
| Dose range | |||
| Hydroxyzine | 1 (0.6) | 1 (1.0) | 0 |
| Median dose | 50 | 50 | |
| Dose range | |||
Initiation, Duration, and Changes to Medications for Treatment of Sleep Complaints
None of the medication orders were part of a standardized order set. The sleep medication for the majority of patients (n=108, 64.3%) was initiated during their time on the study units (general inpatient hospital wards). Most patients (n=90, 53.6%) were ordered for a sleep aid within 48 hours of admission to the hospital. The patients who received medication for sleep had a median length of stay of 6 (interquartile range [IQR], 311) days on the study units, and received medication for a median of 2 (IQR, 15) days (Table 3). One hundred twenty patients (71.4%) were continued on a sleep aid until discharge. Essentially the same percentage of patients experienced an increase (14.9%) or decrease (14.9%) in the dose of their sleep aid during admission. Although most patients received 1 medication for sleep throughout their admission, almost one‐quarter of the patients were given 2 or more medications for sleep during their admission to the floor, sometimes including multiple medications on the same night.
| Variable | Patients, N=168 |
|---|---|
| |
| Total sleep aids each patient received during hospital length of stay, n (%) | |
| 1 sleep aid | 132 (78.6) |
| 2 sleep aids | 28 (16.7) |
| 3 sleep aids | 6 (3.6) |
| 4 sleep aids | 2 (1.2) |
| Patients who received multiple sleep aids for 1 or more days during hospital length of stay, n (%) | 20 (11.9) |
| Length of stay on study units, d | 6 [310.75]a |
| Length of sleep aid therapy on study units, d | 2 [15]a |
Of patients not known to be previously on sleep aid therapy, 40 (34.4%) of them were discharged home on a sleep aid.
Medication Administration Characteristics
Sleep medications were prescribed most frequently as standing orders (63.7%), rather than x1 (17.7%) or PRN (18.6%). Although the majority of sleep medications were administered between the hours of 9 pm and 12 am, more than 35% of doses were given outside of this range (Figure 2).
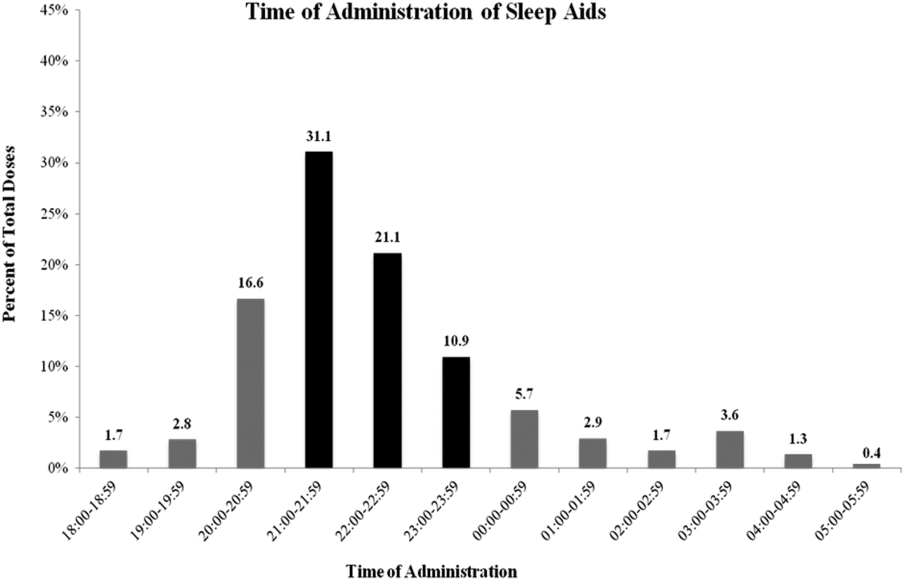
DISCUSSION
Our results confirm the continued frequent use of pharmacological sleep aids in the hospital setting, even in the elderly, despite recent concerns regarding the use of certain sleep medications. Additional, novel findings of our study are: (1) medications used for sleep complaints in the hospital are frequently those without a formal indication for sleep, (2) medications for sleep complaints are frequently administered too early or too late at night to be consistent with good sleep hygiene, and (3) many patients never previously on a medication for insomnia are discharged with a prescription for a sleep aid.
Despite recent warnings regarding side effects especially in the elderly, our rate of medication use has only slightly improved from prior reports from more than a decade ago.[3, 5] This high rate of use is likely due to a combination of patient, clinician, and environmental factors. In our sample, the sleep aid orders were not part of an order set; thus, the orders were either the result of patient request or in response to a patient report of poor sleep. Patients and clinicians may perceive medications for sleep as highly effective and safe, despite evidence to the contrary. Another factor is that both patients and clinicians may be unaware of nonpharmacological interventions that might improve sleep. Similarly, hospital environmental factors (noise, light) may be so disruptive as to preclude these interventions or opportunities for adequate sleep. Thus, the continued high use of medication for sleep is due in part to the lack of patient and clinician education and the difficulty in changing the hospital environment and culture, especially with only limited data on the value of sleep during recovery from illness.
Clinicians typically receive little training regarding sleep or its importance. In fact, most clinicians do not assess or communicate about the patient's quality of sleep.[11] Many may not know that there is little evidence of benefit of pharmacological sleep aids in the hospital. For example, a recent report found, in contrast to the authors' hypothesis, no changes in sleep architecture or duration using 10 mg of zolpidem tartrate in postoperative patients.[12] In our study, we found that some patients required an increase in the dose of their medications or were transitioned to a different sleep aid class (suggesting that sleep aids were ineffective). Alternatively, some patients' sleep aids were discontinued during hospital admission, again, likely due to perceived ineffectiveness or perhaps side effects. It is possible that the effectiveness of these medications might be influenced by timing of administration. This too was variable in our study. Proper clinician education around sleep hygiene might prevent early medication administration (which might lead to middle‐of‐the‐night awakenings) or delayed administration (which will delay the sleep phase), as was frequently seen in our cohort.
Despite emerging evidence of the importance of sleep in maintaining adequate immune, cardiovascular, and cognitive function, there are limited data regarding the benefits of sleep during acute illness.[13, 14, 15, 16] In the absence of compelling data, promoting sleep in the hospital has been difficult. The successful interventions used by Inouye and Bartick and their colleagues to minimize sedative hypnotic use included: a bedtime routine (eg, milk or herbal tea, relaxation tapes or music, back massage, toilet at bedtime), unit‐wide noise‐reduction strategies (eg, silent pill crushers, vibrating beepers, quiet hallways, and noise‐monitoring equipment that alerted staff above a certain decibel level), and schedule adjustments to allow sleep (eg, rescheduling of medications, intravenous fluids, and procedures), all of which require substantial clinician care or may not be possible in more acutely ill patients. Although such changes might be costly, sleep promotion and minimization of sleep aids continues to be part of a strategy that reduces delirium, hospital costs, and hospital length of stay.[16] From a patient perspective, many are interested in nondrug alternatives, especially those who have never used medications before, but few are told of them.[17]
Novel findings of our study include the types of medications used for sleep in the hospital. We found that a variety of medications and classes of medications were prescribed by clinicians for sleep complaints during hospitalization. This variability is due to a number of factors including the lack of rigorous data in this area, well‐established guidelines, or clinician education. We speculate that the high rates of use of nonbenzodiazepine and non‐ gamma‐aminobutyric acid (GABA)ergic agents, such as trazodone and quetiapine, reflect concerns about the use of medications such as zolpidem. Conversely, this means patients are increasingly treated with medications without formal FDA labeling for sleep. It does appear at least that the median doses of medication prescribed were lower in those over age 65 years compared to younger patients, although we cannot determine whether this reflects physician awareness or effective decision support used during computerized order entry. The geriatric decision support recommends a reduced dose for some (eg, trazodone, haloperidol) but not all (eg, quetiapine, lorazepam) of the monitored medications.
We found that many patients, even those who were never previously known to have insomnia, were discharged with a prescription for a sleep medication. Our study design is limited in assessing whether this prescription was needed or not, that is, whether or not the patient will have insomnia (sleep difficulty despite adequate opportunity for sleep) after hospital discharge. However, other studies have suggested that acute illness can be a precipitant for insomnia. Some of this literature has focused on patients in the intensive care unit, but it seems reasonable that patients on general medical and surgical wards (not having come through the intensive care units) might also be at risk for insomnia.[18] A study by Zisberg and colleagues in an elderly Israeli cohort found hospitalization (even without intensive care unit stay) to be both a starting point and a stopping point for chronic sleep medication use.[19] Alternatively, patients may not continue to suffer from insomnia after discharge, and thus the prescription for a sleep aid is inappropriate, as it is likely to have no benefit but may carry risk.[20] Regardless of whether hospital‐acquired insomnia persists past discharge, our findings suggest that some patients will start on chronic medication use for insomnia. Importantly, these patients may have limited understanding of the reason for their prescription, medication risks and benefits, and are unlikely to receive guidance on sleep hygiene or referral to a sleep specialist if needed. In our case, the high rate of prescriptions likely reflects the way in which inpatient medications can be added as a discharge medication automatically. This represents an area for improvement at our institution.
Limitations
This retrospective, single‐center study has several limitations. First, although our results are specific to our institution, our use of pharmacological sleep aids is similar to those previously reported in the literature. Our results are consistent in some ways with the changing trends in outpatient management of insomnia, in which trazodone and quetiapine are now frequently used. Second, we rely on the medical record for prior documentation of insomnia and/or use of medications for insomnia. However, our rate of prior diagnosis of insomnia or medication use of 8.3% is consistent with epidemiological studies.[21] Third, in this retrospective study we may have included some medications in our analysis that may have been given for indications other than sleep promotion, such as medications for anxiety or agitation. However, sleep promotion may have been an intended benefit of the medication choice. Fourth, we did not follow patients after discharge to know whether they continued with sleep medication use outside the hospital. Finally, in this retrospective chart review, we focused on utilization metrics, not on efficacy (which we can only infer) or adverse effects, such as altered mental status or falls. Moreover, we did not compare those patients who did and who did not receive any medication for sleep. However, such work will be crucial in future studies.
CONCLUSIONS
Despite increasing evidence of risks such as delirium or falls, pharmacological sleep aid use in hospitalized patients, even the elderly, remains common. A variety of medications are used, with variable administration times, which likely reflects the few rigorous studies or guidelines for the use of pharmacological sleep aids in hospitalized patients. Many patients not known to be on medications for sleep before admission leave the hospital with a sleep aid prescription. Our results suggest the need to better understand the factors that contribute to the high rate of sleep aid use in hospitalized patients. Clinician education regarding sleep, and nonpharmacological strategies to improve sleep in the hospital, are also needed.
Disclosure: Nothing to report.
- , , , . Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473–482.
- . Sleep and the sleep environment of older adults in acute care settings. J Gerontol Nurs. 2008;34(6):15–21.
- , , , et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676.
- , , , . Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1–6.
- , , , , , . An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17.
- , , , , . Decrease in as‐needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5(3):E20–E24.
- , , , , , . Guided prescription of psychotropic medications for geriatric inpatients. Arch Intern Med. 2005;165(7):802–807.
- , , , . National use of prescription medications for insomnia: NHANES 1999–2010. Sleep. 2014;37(2):343–349.
- , . Safety of low doses of quetiapine when used for insomnia. Ann Pharmacother. 2012;46(5):718–722.
- , . Ten‐year trends in the pharmacological treatment of insomnia. Sleep. 1999;22(3):371–375.
- , , , . How do clinicians assess, communicate about, and manage patient sleep in the hospital? J Nurs Adm. 2013;43(6):342–347.
- , , . Postoperative sleep disturbances after zolpidem treatment in fast‐track hip and knee replacement. J Clin Sleep Med. 2014;10(3):321–326.
- , , . Sleep deprivation after septic insult increases mortality independent of age. J Trauma. 2009;66(1):50–54.
- , , , , , . Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. Faseb J. 1996;10(5):643–653.
- , , , et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185–2186.
- , , , et al. Quality improvement and cost savings with multicomponent delirium interventions: replication of the Hospital Elder Life Program in a community hospital. Psychosomatics. 2013;54(3):219–226.
- , , , , . Hospitalized patients' preference in the treatment of insomnia: pharmacological versus non‐pharmacological. Can J Clin Pharmacol. 2003;10(2):89–92.
- , , , et al. Post‐discharge insomnia symptoms are associated with quality of life impairment among survivors of acute lung injury. Sleep Med. 2012;13(8):1106–1109.
- , , , , , . Hospitalization as a turning point for sleep medication use in older adults: prospective cohort study. Drugs Aging. 2012;29(7):565–576.
- , , , et al. Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013;61(7):1128–1134.
- , . Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484.
Sleep is known to be poor among hospitalized patients for many reasons.[1] Patients may have pain, dyspnea, or other discomforts that prevent sleep. Diagnostic and therapeutic procedures, including medication administration and routine nursing care, may take place during normal sleep times. Environmental factors such as noise and light frequently remain at daytime levels during normal sleep times.[2] In response, patients frequently request pharmacological sleep aids. Unfortunately, the use of sleep medications has been linked to clinically relevant and detrimental outcomes such as delirium and falls, particularly in the elderly. For example, in the landmark study by Inouye et al., a multicomponent intervention was used to successfully reduce delirium in older (>70 years) hospitalized patients.[3] One of the successful components was nonpharmacological sleep promotion, which reduced the use of pharmacological sleep aids from 46% to 35% of patients. Most recently, Kolla and colleagues found zolpidem tartrate use to be a risk factor (odds ratio 4.37) for inpatient falls, a known risk factor for morbidity and increased healthcare costs.[4]
The scope of recent pharmacological sleep aid use in the inpatient setting is not well described. Frighetto and colleagues described the pattern of in‐hospital drug use more than 12 years ago, before the concerns above were described, with 29% of patients receiving a medication for sleep, mostly benzodiazepines.[5] In 2008, Bartick and colleagues also found a very high rate of sleep aid use (42% of patients), but additionally described in 2010 an intervention to minimize sleep disruption that successfully reduced sleep aid use by 38%.[6] Both concerns over side effects and sleep promotion efforts might have reduced the current rate of medication use. Therefore, we sought to evaluate the prescription and administration of pharmacological sleep aids in general medical and surgical inpatients at our institution. Using our electronic medical records, including preadmission and discharge medication records, we assessed new and continued usage of medications for sleep complaints following hospital admission.
METHODS
Patients and Design
Records were reviewed for all adult patient (18 years or older) admissions to 1 of 4 units (2 general medicine and 2 general surgical units) from January 1, 2013 to February 28, 2013. These units do not have specific policies to promote sleep, such as nocturnal noise and light reduction or clustering of care. Brigham and Women's Hospital (BWH) is a 793‐bed university‐affiliated teaching hospital. Approval for this retrospective chart review study was obtained from the Partners Healthcare Institutional Review Board.
BWH uses an in‐house electronic health record system, which gathers information from a wider healthcare system (Partners Healthcare). Medications, problem lists, and allergies are available from within‐system providers and prior encounters. Admitting physicians are also required to document a preadmission medication list. A computerized physician order entry (CPOE) system is used for all medication orders. Although standardized admission order sets are used, none of these sets contains a pharmacological sleep aid. There is decision support for geriatric patients (age >65 years) that may recommend reduced starting doses for some medications.[7]
Medications Monitored for Treatment of Sleep Complaints
Using our electronic medication ordering and administration system, each patient admission was reviewed for any medication that might be used for treatment of sleep complaints. The list of sleep medications was based on those commonly used for the outpatient treatment of insomnia, as well as others included based on the authors' experience as clinical inpatient pharmacists.[8, 9, 10] Admissions were reviewed for the following medications: first generation antihistamines (diphenhydramine, hydroxyzine), tricyclic antidepressants (amitriptyline, nortriptyline, desipramine), serotonin‐norepinephrine reuptake inhibitor antidepressants (mirtazapine, trazodone, nefazodone), melatonin agonists (ramelteon), nonbenzodiazepine hypnotics (zolpidem tartrate, eszopiclone), benzodiazepines (oxazepam, temazepam, lorazepam, triazolam, diazepam), typical antipsychotics (haloperidol, fluphenazine, thioridazine, chlorpromazine), and atypical antipsychotics (quetiapine fumarate, ziprasidone, olanzapine, risperidone, aripiprazole). Melatonin, which is not regulated by the US Food and Drug Administration (FDA), cannot be prescribed using our CPOE system.
Determination of Medication Administration for Treatment of Sleep Complaints
The charts of patients receiving 1 or more of these monitored medications were then reviewed by the authors to determine if the medication was indeed prescribed for insomnia/sleep. Chart documents reviewed were the patient's problem list from outpatient provider notes; admission note, including past medical history and home medications; the preadmission medication list; and the inpatient daily progress note. The medication was considered to be used for sleep complaints (as opposed to another indication) when any of the additional following inclusion criteria were met: the medication was part of the patient's home medication regimen for insomnia, the medication order indicated that the medication was for insomnia/difficulty sleeping, or the medication was administered without a specific indication between the hours of 6 pm and 6 am. The medication was not considered to be used primarily as a sleep aid if any of the following were present (exclusion criteria): utilization for an as needed reason including anxiety, agitation, itching, nausea, muscle spasm; utilization for a documented disorder including depression, anxiety, schizophrenia, bipolar disorder, alcohol withdrawal, or epilepsy; intramuscular administration of olanzapine or ziprasidone; or topical administration of diphenhydramine.
Medication Administration Characteristics
For each medication that was administered for difficulty sleeping, the following data were documented: dose in milligrams, route of administration, time of administration, administration timing directions (eg, times 1 [x1], as needed [PRN], or standing), an increase or decrease in dose during hospital stay, documentation of the medication in discharge notes or discharge medications, and documentation of development of an allergy or adverse reaction due to the medication. Changes in dose were recorded. If a patient received more than 1 study medication, each individual medication and dose was evaluated for inclusion in the study analysis. Other data collected included the total number of days of exposure to each sleep aid during admission, the date of initiation, the total number of days of exposure to more than 1 sleep aid during admission, and the location of initiation of each individual sleep aid (eg, intensive care unit, medical floor). Appropriate time of administration was defined as sleep aid administration between 9 pm and 12 am.
RESULTS
Patients
During the 59‐day study period, there were 642 patients admitted to the study units. Two hundred seventy‐six patients received 1 of the monitored medications; however, 106 patients received the medication for an indication other than insomnia/difficulty sleeping. In 2 patients, incomplete records prevented ascertainment of the motivation for using the monitored medication. Thus, 168 patients (26.2%) were determined to have received a medication for sleep complaints and were included in the study analysis (Figure 1). Table 1 lists the characteristics of the 168 patients, of whom 10 had a prior documented sleep disorder such as insomnia (6 patients), restless leg syndrome (1 patient), and obstructive sleep apnea (3 patients). The rate of sleep medication use was lower, though not drastically so, in patients 65 years of age compared to those <65 years of age.

| Patients | Value |
|---|---|
| |
| Age, y | 57.919.8a |
| Age 65 years | 70 (41.7) |
| Age 64 years | 98 (58.3) |
| Female, n (%) | 97 (57.7) |
| Ethnicity, n (%) | |
| Caucasian | 114 (67.9) |
| Black | 18 (10.7) |
| Hispanic | 13 (7.7) |
| Other | 23 (13.7) |
| Admitted to floor from: | |
| Emergency department | 95 (56.5) |
| Operating room | 30 (17.9) |
| Transferred from outside hospital | 35 (20.8) |
| Intensive care unit | 8 (4.8) |
| Admission service, n (%) | |
| Medical | 109 (64.9) |
| Surgical | 59 (35.1) |
| Hospital length of stay | 10.516.0a |
| Known sleep disorder | |
| Insomnia | 6 (3.6) |
| Restless leg syndrome | 1 (0.6) |
| Obstructive sleep apnea | 3(1.8) |
Medications Used for Treatment of Sleep Complaints
Of the 25 monitored medications, 13 were administered to patients for sleep during the study period. The most commonly administered medications (percent of patients, median dose, absolute dose range) were trazodone (30.4%, 50 mg, 12.5450 mg), lorazepam (24.4%, 0.5 mg, 0.25 mg2 mg), and zolpidem tartrate (17.9%, 10 mg, 2.5 mg10 mg) (Table 2). As only a few of these medications (diphenhydramine, ramelteon, temazepam, triazolam, zolpidem) have a formal FDA indication for insomnia, most patients (72%) were treated using an off‐label medication. Although the types of medication used did not vary substantially between young and old patients, the median doses and ranges were lower in the elderly. Admitting service did not substantially influence the medication or dose chosen for sleep complaints (data not shown).
| Medication | All Patients, N=168, n (%) | Patients <65 Years Old, n=98, n (%) | Patients >65 Years Old, n=70, n (%) |
|---|---|---|---|
| |||
| Trazodoneb | 51 (30.4) | 29 (29.6) | 22 (31.4) |
| Median dose | 50 | 50 | 25 |
| Dose range | 12.5450 | 25450 | 12.5200 |
| Lorazepamc | 41 (24.4) | 24 (24.5) | 17 (24.3) |
| Median dose | 0.5 | 1 | 0.25 |
| Dose range | 0.252 | 0.252 | 0.251 |
| Zolpidem tartratec | 30 (17.9) | 20 (20.4) | 10 (14.3) |
| Median dose | 10 | 10 | 5 |
| Dose range | 2.510 | 2.510 | 2.510 |
| Quetiapine fumarate | 21 (12.5) | 9 (9.2) | 12 (17.1) |
| Median dose | 50 | 50 | 25 |
| Dose range | 12.5300 | 12.5300 | 12.5100 |
| Haloperidol | 18 (10.7) | 7 (7.1) | 11 (15.7) |
| Median dose | 1 | 5 | 1 |
| Dose range | 0.2510 | 0.510 | 0.251 |
| Diphenhydraminec | 16 (9.5) | 12 (12.2) | 4 (5.7) |
| Median dose | 25 | 25 | 12.5 |
| Dose range | 12.550 | 12.550 | 12.525 |
| Mirtazapine | 7 (4.2) | 3 (3.1) | 4 (5.7) |
| Median dose | 15 | 30 | 7.5 |
| Dose range | 7.545 | 7.530 | 7.545 |
| Olanzapine | 5 (3.6) | 3 (3.1) | 2 (2.9) |
| Median dose | 5 | 5 | 2.5 |
| Dose range | 2.512.5 | 512.5 | 2.52.5 |
| Amitriptyline | 5 (3.0) | 4 (4.1) | 1 (1.4) |
| Median dose | 25 | 25 | 25 |
| Dose range | 25100 | 25100 | |
| Diazepam | 5 (3.0) | 3 (3.1) | 2 (2.9) |
| Median dose | 5 | 5 | 10 |
| Dose range | 510 | ||
| Oxazepam | 2 (1.2) | 0 | 2 (2.9) |
| Median dose | 10 | 10 | |
| Dose range | 1010 | 1010 | |
| Temazepamc | 1 (0.6) | 0 | 1 (1.4) |
| Median dose | 15 | 15 | |
| Dose range | |||
| Hydroxyzine | 1 (0.6) | 1 (1.0) | 0 |
| Median dose | 50 | 50 | |
| Dose range | |||
Initiation, Duration, and Changes to Medications for Treatment of Sleep Complaints
None of the medication orders were part of a standardized order set. The sleep medication for the majority of patients (n=108, 64.3%) was initiated during their time on the study units (general inpatient hospital wards). Most patients (n=90, 53.6%) were ordered for a sleep aid within 48 hours of admission to the hospital. The patients who received medication for sleep had a median length of stay of 6 (interquartile range [IQR], 311) days on the study units, and received medication for a median of 2 (IQR, 15) days (Table 3). One hundred twenty patients (71.4%) were continued on a sleep aid until discharge. Essentially the same percentage of patients experienced an increase (14.9%) or decrease (14.9%) in the dose of their sleep aid during admission. Although most patients received 1 medication for sleep throughout their admission, almost one‐quarter of the patients were given 2 or more medications for sleep during their admission to the floor, sometimes including multiple medications on the same night.
| Variable | Patients, N=168 |
|---|---|
| |
| Total sleep aids each patient received during hospital length of stay, n (%) | |
| 1 sleep aid | 132 (78.6) |
| 2 sleep aids | 28 (16.7) |
| 3 sleep aids | 6 (3.6) |
| 4 sleep aids | 2 (1.2) |
| Patients who received multiple sleep aids for 1 or more days during hospital length of stay, n (%) | 20 (11.9) |
| Length of stay on study units, d | 6 [310.75]a |
| Length of sleep aid therapy on study units, d | 2 [15]a |
Of patients not known to be previously on sleep aid therapy, 40 (34.4%) of them were discharged home on a sleep aid.
Medication Administration Characteristics
Sleep medications were prescribed most frequently as standing orders (63.7%), rather than x1 (17.7%) or PRN (18.6%). Although the majority of sleep medications were administered between the hours of 9 pm and 12 am, more than 35% of doses were given outside of this range (Figure 2).
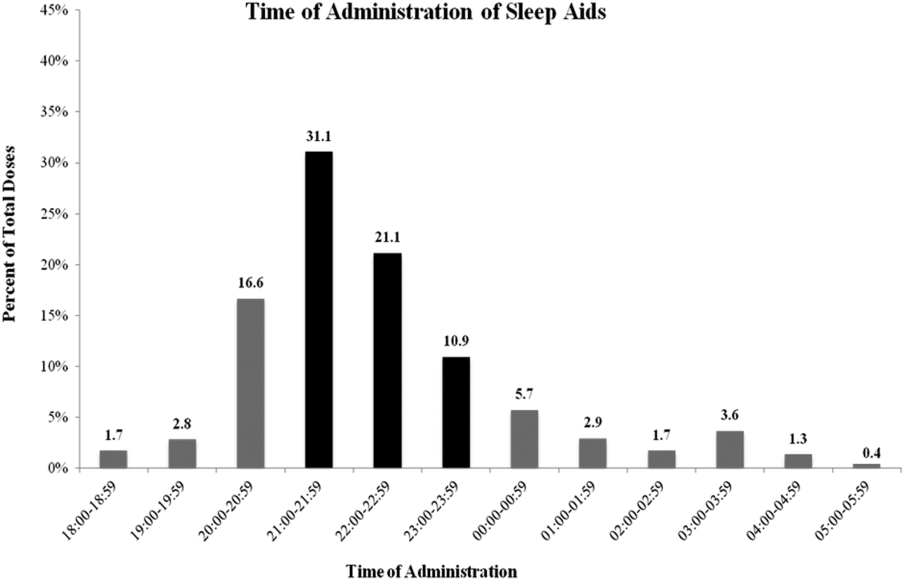
DISCUSSION
Our results confirm the continued frequent use of pharmacological sleep aids in the hospital setting, even in the elderly, despite recent concerns regarding the use of certain sleep medications. Additional, novel findings of our study are: (1) medications used for sleep complaints in the hospital are frequently those without a formal indication for sleep, (2) medications for sleep complaints are frequently administered too early or too late at night to be consistent with good sleep hygiene, and (3) many patients never previously on a medication for insomnia are discharged with a prescription for a sleep aid.
Despite recent warnings regarding side effects especially in the elderly, our rate of medication use has only slightly improved from prior reports from more than a decade ago.[3, 5] This high rate of use is likely due to a combination of patient, clinician, and environmental factors. In our sample, the sleep aid orders were not part of an order set; thus, the orders were either the result of patient request or in response to a patient report of poor sleep. Patients and clinicians may perceive medications for sleep as highly effective and safe, despite evidence to the contrary. Another factor is that both patients and clinicians may be unaware of nonpharmacological interventions that might improve sleep. Similarly, hospital environmental factors (noise, light) may be so disruptive as to preclude these interventions or opportunities for adequate sleep. Thus, the continued high use of medication for sleep is due in part to the lack of patient and clinician education and the difficulty in changing the hospital environment and culture, especially with only limited data on the value of sleep during recovery from illness.
Clinicians typically receive little training regarding sleep or its importance. In fact, most clinicians do not assess or communicate about the patient's quality of sleep.[11] Many may not know that there is little evidence of benefit of pharmacological sleep aids in the hospital. For example, a recent report found, in contrast to the authors' hypothesis, no changes in sleep architecture or duration using 10 mg of zolpidem tartrate in postoperative patients.[12] In our study, we found that some patients required an increase in the dose of their medications or were transitioned to a different sleep aid class (suggesting that sleep aids were ineffective). Alternatively, some patients' sleep aids were discontinued during hospital admission, again, likely due to perceived ineffectiveness or perhaps side effects. It is possible that the effectiveness of these medications might be influenced by timing of administration. This too was variable in our study. Proper clinician education around sleep hygiene might prevent early medication administration (which might lead to middle‐of‐the‐night awakenings) or delayed administration (which will delay the sleep phase), as was frequently seen in our cohort.
Despite emerging evidence of the importance of sleep in maintaining adequate immune, cardiovascular, and cognitive function, there are limited data regarding the benefits of sleep during acute illness.[13, 14, 15, 16] In the absence of compelling data, promoting sleep in the hospital has been difficult. The successful interventions used by Inouye and Bartick and their colleagues to minimize sedative hypnotic use included: a bedtime routine (eg, milk or herbal tea, relaxation tapes or music, back massage, toilet at bedtime), unit‐wide noise‐reduction strategies (eg, silent pill crushers, vibrating beepers, quiet hallways, and noise‐monitoring equipment that alerted staff above a certain decibel level), and schedule adjustments to allow sleep (eg, rescheduling of medications, intravenous fluids, and procedures), all of which require substantial clinician care or may not be possible in more acutely ill patients. Although such changes might be costly, sleep promotion and minimization of sleep aids continues to be part of a strategy that reduces delirium, hospital costs, and hospital length of stay.[16] From a patient perspective, many are interested in nondrug alternatives, especially those who have never used medications before, but few are told of them.[17]
Novel findings of our study include the types of medications used for sleep in the hospital. We found that a variety of medications and classes of medications were prescribed by clinicians for sleep complaints during hospitalization. This variability is due to a number of factors including the lack of rigorous data in this area, well‐established guidelines, or clinician education. We speculate that the high rates of use of nonbenzodiazepine and non‐ gamma‐aminobutyric acid (GABA)ergic agents, such as trazodone and quetiapine, reflect concerns about the use of medications such as zolpidem. Conversely, this means patients are increasingly treated with medications without formal FDA labeling for sleep. It does appear at least that the median doses of medication prescribed were lower in those over age 65 years compared to younger patients, although we cannot determine whether this reflects physician awareness or effective decision support used during computerized order entry. The geriatric decision support recommends a reduced dose for some (eg, trazodone, haloperidol) but not all (eg, quetiapine, lorazepam) of the monitored medications.
We found that many patients, even those who were never previously known to have insomnia, were discharged with a prescription for a sleep medication. Our study design is limited in assessing whether this prescription was needed or not, that is, whether or not the patient will have insomnia (sleep difficulty despite adequate opportunity for sleep) after hospital discharge. However, other studies have suggested that acute illness can be a precipitant for insomnia. Some of this literature has focused on patients in the intensive care unit, but it seems reasonable that patients on general medical and surgical wards (not having come through the intensive care units) might also be at risk for insomnia.[18] A study by Zisberg and colleagues in an elderly Israeli cohort found hospitalization (even without intensive care unit stay) to be both a starting point and a stopping point for chronic sleep medication use.[19] Alternatively, patients may not continue to suffer from insomnia after discharge, and thus the prescription for a sleep aid is inappropriate, as it is likely to have no benefit but may carry risk.[20] Regardless of whether hospital‐acquired insomnia persists past discharge, our findings suggest that some patients will start on chronic medication use for insomnia. Importantly, these patients may have limited understanding of the reason for their prescription, medication risks and benefits, and are unlikely to receive guidance on sleep hygiene or referral to a sleep specialist if needed. In our case, the high rate of prescriptions likely reflects the way in which inpatient medications can be added as a discharge medication automatically. This represents an area for improvement at our institution.
Limitations
This retrospective, single‐center study has several limitations. First, although our results are specific to our institution, our use of pharmacological sleep aids is similar to those previously reported in the literature. Our results are consistent in some ways with the changing trends in outpatient management of insomnia, in which trazodone and quetiapine are now frequently used. Second, we rely on the medical record for prior documentation of insomnia and/or use of medications for insomnia. However, our rate of prior diagnosis of insomnia or medication use of 8.3% is consistent with epidemiological studies.[21] Third, in this retrospective study we may have included some medications in our analysis that may have been given for indications other than sleep promotion, such as medications for anxiety or agitation. However, sleep promotion may have been an intended benefit of the medication choice. Fourth, we did not follow patients after discharge to know whether they continued with sleep medication use outside the hospital. Finally, in this retrospective chart review, we focused on utilization metrics, not on efficacy (which we can only infer) or adverse effects, such as altered mental status or falls. Moreover, we did not compare those patients who did and who did not receive any medication for sleep. However, such work will be crucial in future studies.
CONCLUSIONS
Despite increasing evidence of risks such as delirium or falls, pharmacological sleep aid use in hospitalized patients, even the elderly, remains common. A variety of medications are used, with variable administration times, which likely reflects the few rigorous studies or guidelines for the use of pharmacological sleep aids in hospitalized patients. Many patients not known to be on medications for sleep before admission leave the hospital with a sleep aid prescription. Our results suggest the need to better understand the factors that contribute to the high rate of sleep aid use in hospitalized patients. Clinician education regarding sleep, and nonpharmacological strategies to improve sleep in the hospital, are also needed.
Disclosure: Nothing to report.
Sleep is known to be poor among hospitalized patients for many reasons.[1] Patients may have pain, dyspnea, or other discomforts that prevent sleep. Diagnostic and therapeutic procedures, including medication administration and routine nursing care, may take place during normal sleep times. Environmental factors such as noise and light frequently remain at daytime levels during normal sleep times.[2] In response, patients frequently request pharmacological sleep aids. Unfortunately, the use of sleep medications has been linked to clinically relevant and detrimental outcomes such as delirium and falls, particularly in the elderly. For example, in the landmark study by Inouye et al., a multicomponent intervention was used to successfully reduce delirium in older (>70 years) hospitalized patients.[3] One of the successful components was nonpharmacological sleep promotion, which reduced the use of pharmacological sleep aids from 46% to 35% of patients. Most recently, Kolla and colleagues found zolpidem tartrate use to be a risk factor (odds ratio 4.37) for inpatient falls, a known risk factor for morbidity and increased healthcare costs.[4]
The scope of recent pharmacological sleep aid use in the inpatient setting is not well described. Frighetto and colleagues described the pattern of in‐hospital drug use more than 12 years ago, before the concerns above were described, with 29% of patients receiving a medication for sleep, mostly benzodiazepines.[5] In 2008, Bartick and colleagues also found a very high rate of sleep aid use (42% of patients), but additionally described in 2010 an intervention to minimize sleep disruption that successfully reduced sleep aid use by 38%.[6] Both concerns over side effects and sleep promotion efforts might have reduced the current rate of medication use. Therefore, we sought to evaluate the prescription and administration of pharmacological sleep aids in general medical and surgical inpatients at our institution. Using our electronic medical records, including preadmission and discharge medication records, we assessed new and continued usage of medications for sleep complaints following hospital admission.
METHODS
Patients and Design
Records were reviewed for all adult patient (18 years or older) admissions to 1 of 4 units (2 general medicine and 2 general surgical units) from January 1, 2013 to February 28, 2013. These units do not have specific policies to promote sleep, such as nocturnal noise and light reduction or clustering of care. Brigham and Women's Hospital (BWH) is a 793‐bed university‐affiliated teaching hospital. Approval for this retrospective chart review study was obtained from the Partners Healthcare Institutional Review Board.
BWH uses an in‐house electronic health record system, which gathers information from a wider healthcare system (Partners Healthcare). Medications, problem lists, and allergies are available from within‐system providers and prior encounters. Admitting physicians are also required to document a preadmission medication list. A computerized physician order entry (CPOE) system is used for all medication orders. Although standardized admission order sets are used, none of these sets contains a pharmacological sleep aid. There is decision support for geriatric patients (age >65 years) that may recommend reduced starting doses for some medications.[7]
Medications Monitored for Treatment of Sleep Complaints
Using our electronic medication ordering and administration system, each patient admission was reviewed for any medication that might be used for treatment of sleep complaints. The list of sleep medications was based on those commonly used for the outpatient treatment of insomnia, as well as others included based on the authors' experience as clinical inpatient pharmacists.[8, 9, 10] Admissions were reviewed for the following medications: first generation antihistamines (diphenhydramine, hydroxyzine), tricyclic antidepressants (amitriptyline, nortriptyline, desipramine), serotonin‐norepinephrine reuptake inhibitor antidepressants (mirtazapine, trazodone, nefazodone), melatonin agonists (ramelteon), nonbenzodiazepine hypnotics (zolpidem tartrate, eszopiclone), benzodiazepines (oxazepam, temazepam, lorazepam, triazolam, diazepam), typical antipsychotics (haloperidol, fluphenazine, thioridazine, chlorpromazine), and atypical antipsychotics (quetiapine fumarate, ziprasidone, olanzapine, risperidone, aripiprazole). Melatonin, which is not regulated by the US Food and Drug Administration (FDA), cannot be prescribed using our CPOE system.
Determination of Medication Administration for Treatment of Sleep Complaints
The charts of patients receiving 1 or more of these monitored medications were then reviewed by the authors to determine if the medication was indeed prescribed for insomnia/sleep. Chart documents reviewed were the patient's problem list from outpatient provider notes; admission note, including past medical history and home medications; the preadmission medication list; and the inpatient daily progress note. The medication was considered to be used for sleep complaints (as opposed to another indication) when any of the additional following inclusion criteria were met: the medication was part of the patient's home medication regimen for insomnia, the medication order indicated that the medication was for insomnia/difficulty sleeping, or the medication was administered without a specific indication between the hours of 6 pm and 6 am. The medication was not considered to be used primarily as a sleep aid if any of the following were present (exclusion criteria): utilization for an as needed reason including anxiety, agitation, itching, nausea, muscle spasm; utilization for a documented disorder including depression, anxiety, schizophrenia, bipolar disorder, alcohol withdrawal, or epilepsy; intramuscular administration of olanzapine or ziprasidone; or topical administration of diphenhydramine.
Medication Administration Characteristics
For each medication that was administered for difficulty sleeping, the following data were documented: dose in milligrams, route of administration, time of administration, administration timing directions (eg, times 1 [x1], as needed [PRN], or standing), an increase or decrease in dose during hospital stay, documentation of the medication in discharge notes or discharge medications, and documentation of development of an allergy or adverse reaction due to the medication. Changes in dose were recorded. If a patient received more than 1 study medication, each individual medication and dose was evaluated for inclusion in the study analysis. Other data collected included the total number of days of exposure to each sleep aid during admission, the date of initiation, the total number of days of exposure to more than 1 sleep aid during admission, and the location of initiation of each individual sleep aid (eg, intensive care unit, medical floor). Appropriate time of administration was defined as sleep aid administration between 9 pm and 12 am.
RESULTS
Patients
During the 59‐day study period, there were 642 patients admitted to the study units. Two hundred seventy‐six patients received 1 of the monitored medications; however, 106 patients received the medication for an indication other than insomnia/difficulty sleeping. In 2 patients, incomplete records prevented ascertainment of the motivation for using the monitored medication. Thus, 168 patients (26.2%) were determined to have received a medication for sleep complaints and were included in the study analysis (Figure 1). Table 1 lists the characteristics of the 168 patients, of whom 10 had a prior documented sleep disorder such as insomnia (6 patients), restless leg syndrome (1 patient), and obstructive sleep apnea (3 patients). The rate of sleep medication use was lower, though not drastically so, in patients 65 years of age compared to those <65 years of age.

| Patients | Value |
|---|---|
| |
| Age, y | 57.919.8a |
| Age 65 years | 70 (41.7) |
| Age 64 years | 98 (58.3) |
| Female, n (%) | 97 (57.7) |
| Ethnicity, n (%) | |
| Caucasian | 114 (67.9) |
| Black | 18 (10.7) |
| Hispanic | 13 (7.7) |
| Other | 23 (13.7) |
| Admitted to floor from: | |
| Emergency department | 95 (56.5) |
| Operating room | 30 (17.9) |
| Transferred from outside hospital | 35 (20.8) |
| Intensive care unit | 8 (4.8) |
| Admission service, n (%) | |
| Medical | 109 (64.9) |
| Surgical | 59 (35.1) |
| Hospital length of stay | 10.516.0a |
| Known sleep disorder | |
| Insomnia | 6 (3.6) |
| Restless leg syndrome | 1 (0.6) |
| Obstructive sleep apnea | 3(1.8) |
Medications Used for Treatment of Sleep Complaints
Of the 25 monitored medications, 13 were administered to patients for sleep during the study period. The most commonly administered medications (percent of patients, median dose, absolute dose range) were trazodone (30.4%, 50 mg, 12.5450 mg), lorazepam (24.4%, 0.5 mg, 0.25 mg2 mg), and zolpidem tartrate (17.9%, 10 mg, 2.5 mg10 mg) (Table 2). As only a few of these medications (diphenhydramine, ramelteon, temazepam, triazolam, zolpidem) have a formal FDA indication for insomnia, most patients (72%) were treated using an off‐label medication. Although the types of medication used did not vary substantially between young and old patients, the median doses and ranges were lower in the elderly. Admitting service did not substantially influence the medication or dose chosen for sleep complaints (data not shown).
| Medication | All Patients, N=168, n (%) | Patients <65 Years Old, n=98, n (%) | Patients >65 Years Old, n=70, n (%) |
|---|---|---|---|
| |||
| Trazodoneb | 51 (30.4) | 29 (29.6) | 22 (31.4) |
| Median dose | 50 | 50 | 25 |
| Dose range | 12.5450 | 25450 | 12.5200 |
| Lorazepamc | 41 (24.4) | 24 (24.5) | 17 (24.3) |
| Median dose | 0.5 | 1 | 0.25 |
| Dose range | 0.252 | 0.252 | 0.251 |
| Zolpidem tartratec | 30 (17.9) | 20 (20.4) | 10 (14.3) |
| Median dose | 10 | 10 | 5 |
| Dose range | 2.510 | 2.510 | 2.510 |
| Quetiapine fumarate | 21 (12.5) | 9 (9.2) | 12 (17.1) |
| Median dose | 50 | 50 | 25 |
| Dose range | 12.5300 | 12.5300 | 12.5100 |
| Haloperidol | 18 (10.7) | 7 (7.1) | 11 (15.7) |
| Median dose | 1 | 5 | 1 |
| Dose range | 0.2510 | 0.510 | 0.251 |
| Diphenhydraminec | 16 (9.5) | 12 (12.2) | 4 (5.7) |
| Median dose | 25 | 25 | 12.5 |
| Dose range | 12.550 | 12.550 | 12.525 |
| Mirtazapine | 7 (4.2) | 3 (3.1) | 4 (5.7) |
| Median dose | 15 | 30 | 7.5 |
| Dose range | 7.545 | 7.530 | 7.545 |
| Olanzapine | 5 (3.6) | 3 (3.1) | 2 (2.9) |
| Median dose | 5 | 5 | 2.5 |
| Dose range | 2.512.5 | 512.5 | 2.52.5 |
| Amitriptyline | 5 (3.0) | 4 (4.1) | 1 (1.4) |
| Median dose | 25 | 25 | 25 |
| Dose range | 25100 | 25100 | |
| Diazepam | 5 (3.0) | 3 (3.1) | 2 (2.9) |
| Median dose | 5 | 5 | 10 |
| Dose range | 510 | ||
| Oxazepam | 2 (1.2) | 0 | 2 (2.9) |
| Median dose | 10 | 10 | |
| Dose range | 1010 | 1010 | |
| Temazepamc | 1 (0.6) | 0 | 1 (1.4) |
| Median dose | 15 | 15 | |
| Dose range | |||
| Hydroxyzine | 1 (0.6) | 1 (1.0) | 0 |
| Median dose | 50 | 50 | |
| Dose range | |||
Initiation, Duration, and Changes to Medications for Treatment of Sleep Complaints
None of the medication orders were part of a standardized order set. The sleep medication for the majority of patients (n=108, 64.3%) was initiated during their time on the study units (general inpatient hospital wards). Most patients (n=90, 53.6%) were ordered for a sleep aid within 48 hours of admission to the hospital. The patients who received medication for sleep had a median length of stay of 6 (interquartile range [IQR], 311) days on the study units, and received medication for a median of 2 (IQR, 15) days (Table 3). One hundred twenty patients (71.4%) were continued on a sleep aid until discharge. Essentially the same percentage of patients experienced an increase (14.9%) or decrease (14.9%) in the dose of their sleep aid during admission. Although most patients received 1 medication for sleep throughout their admission, almost one‐quarter of the patients were given 2 or more medications for sleep during their admission to the floor, sometimes including multiple medications on the same night.
| Variable | Patients, N=168 |
|---|---|
| |
| Total sleep aids each patient received during hospital length of stay, n (%) | |
| 1 sleep aid | 132 (78.6) |
| 2 sleep aids | 28 (16.7) |
| 3 sleep aids | 6 (3.6) |
| 4 sleep aids | 2 (1.2) |
| Patients who received multiple sleep aids for 1 or more days during hospital length of stay, n (%) | 20 (11.9) |
| Length of stay on study units, d | 6 [310.75]a |
| Length of sleep aid therapy on study units, d | 2 [15]a |
Of patients not known to be previously on sleep aid therapy, 40 (34.4%) of them were discharged home on a sleep aid.
Medication Administration Characteristics
Sleep medications were prescribed most frequently as standing orders (63.7%), rather than x1 (17.7%) or PRN (18.6%). Although the majority of sleep medications were administered between the hours of 9 pm and 12 am, more than 35% of doses were given outside of this range (Figure 2).
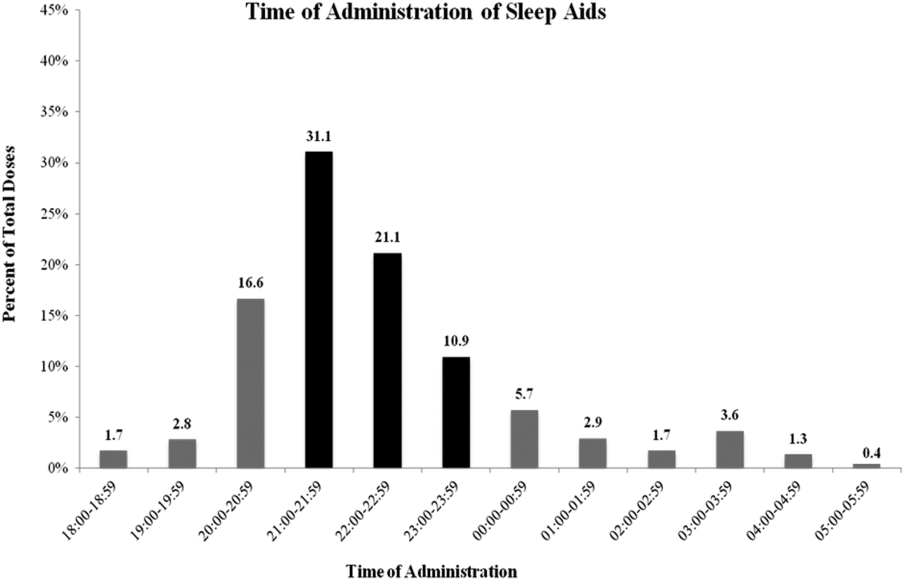
DISCUSSION
Our results confirm the continued frequent use of pharmacological sleep aids in the hospital setting, even in the elderly, despite recent concerns regarding the use of certain sleep medications. Additional, novel findings of our study are: (1) medications used for sleep complaints in the hospital are frequently those without a formal indication for sleep, (2) medications for sleep complaints are frequently administered too early or too late at night to be consistent with good sleep hygiene, and (3) many patients never previously on a medication for insomnia are discharged with a prescription for a sleep aid.
Despite recent warnings regarding side effects especially in the elderly, our rate of medication use has only slightly improved from prior reports from more than a decade ago.[3, 5] This high rate of use is likely due to a combination of patient, clinician, and environmental factors. In our sample, the sleep aid orders were not part of an order set; thus, the orders were either the result of patient request or in response to a patient report of poor sleep. Patients and clinicians may perceive medications for sleep as highly effective and safe, despite evidence to the contrary. Another factor is that both patients and clinicians may be unaware of nonpharmacological interventions that might improve sleep. Similarly, hospital environmental factors (noise, light) may be so disruptive as to preclude these interventions or opportunities for adequate sleep. Thus, the continued high use of medication for sleep is due in part to the lack of patient and clinician education and the difficulty in changing the hospital environment and culture, especially with only limited data on the value of sleep during recovery from illness.
Clinicians typically receive little training regarding sleep or its importance. In fact, most clinicians do not assess or communicate about the patient's quality of sleep.[11] Many may not know that there is little evidence of benefit of pharmacological sleep aids in the hospital. For example, a recent report found, in contrast to the authors' hypothesis, no changes in sleep architecture or duration using 10 mg of zolpidem tartrate in postoperative patients.[12] In our study, we found that some patients required an increase in the dose of their medications or were transitioned to a different sleep aid class (suggesting that sleep aids were ineffective). Alternatively, some patients' sleep aids were discontinued during hospital admission, again, likely due to perceived ineffectiveness or perhaps side effects. It is possible that the effectiveness of these medications might be influenced by timing of administration. This too was variable in our study. Proper clinician education around sleep hygiene might prevent early medication administration (which might lead to middle‐of‐the‐night awakenings) or delayed administration (which will delay the sleep phase), as was frequently seen in our cohort.
Despite emerging evidence of the importance of sleep in maintaining adequate immune, cardiovascular, and cognitive function, there are limited data regarding the benefits of sleep during acute illness.[13, 14, 15, 16] In the absence of compelling data, promoting sleep in the hospital has been difficult. The successful interventions used by Inouye and Bartick and their colleagues to minimize sedative hypnotic use included: a bedtime routine (eg, milk or herbal tea, relaxation tapes or music, back massage, toilet at bedtime), unit‐wide noise‐reduction strategies (eg, silent pill crushers, vibrating beepers, quiet hallways, and noise‐monitoring equipment that alerted staff above a certain decibel level), and schedule adjustments to allow sleep (eg, rescheduling of medications, intravenous fluids, and procedures), all of which require substantial clinician care or may not be possible in more acutely ill patients. Although such changes might be costly, sleep promotion and minimization of sleep aids continues to be part of a strategy that reduces delirium, hospital costs, and hospital length of stay.[16] From a patient perspective, many are interested in nondrug alternatives, especially those who have never used medications before, but few are told of them.[17]
Novel findings of our study include the types of medications used for sleep in the hospital. We found that a variety of medications and classes of medications were prescribed by clinicians for sleep complaints during hospitalization. This variability is due to a number of factors including the lack of rigorous data in this area, well‐established guidelines, or clinician education. We speculate that the high rates of use of nonbenzodiazepine and non‐ gamma‐aminobutyric acid (GABA)ergic agents, such as trazodone and quetiapine, reflect concerns about the use of medications such as zolpidem. Conversely, this means patients are increasingly treated with medications without formal FDA labeling for sleep. It does appear at least that the median doses of medication prescribed were lower in those over age 65 years compared to younger patients, although we cannot determine whether this reflects physician awareness or effective decision support used during computerized order entry. The geriatric decision support recommends a reduced dose for some (eg, trazodone, haloperidol) but not all (eg, quetiapine, lorazepam) of the monitored medications.
We found that many patients, even those who were never previously known to have insomnia, were discharged with a prescription for a sleep medication. Our study design is limited in assessing whether this prescription was needed or not, that is, whether or not the patient will have insomnia (sleep difficulty despite adequate opportunity for sleep) after hospital discharge. However, other studies have suggested that acute illness can be a precipitant for insomnia. Some of this literature has focused on patients in the intensive care unit, but it seems reasonable that patients on general medical and surgical wards (not having come through the intensive care units) might also be at risk for insomnia.[18] A study by Zisberg and colleagues in an elderly Israeli cohort found hospitalization (even without intensive care unit stay) to be both a starting point and a stopping point for chronic sleep medication use.[19] Alternatively, patients may not continue to suffer from insomnia after discharge, and thus the prescription for a sleep aid is inappropriate, as it is likely to have no benefit but may carry risk.[20] Regardless of whether hospital‐acquired insomnia persists past discharge, our findings suggest that some patients will start on chronic medication use for insomnia. Importantly, these patients may have limited understanding of the reason for their prescription, medication risks and benefits, and are unlikely to receive guidance on sleep hygiene or referral to a sleep specialist if needed. In our case, the high rate of prescriptions likely reflects the way in which inpatient medications can be added as a discharge medication automatically. This represents an area for improvement at our institution.
Limitations
This retrospective, single‐center study has several limitations. First, although our results are specific to our institution, our use of pharmacological sleep aids is similar to those previously reported in the literature. Our results are consistent in some ways with the changing trends in outpatient management of insomnia, in which trazodone and quetiapine are now frequently used. Second, we rely on the medical record for prior documentation of insomnia and/or use of medications for insomnia. However, our rate of prior diagnosis of insomnia or medication use of 8.3% is consistent with epidemiological studies.[21] Third, in this retrospective study we may have included some medications in our analysis that may have been given for indications other than sleep promotion, such as medications for anxiety or agitation. However, sleep promotion may have been an intended benefit of the medication choice. Fourth, we did not follow patients after discharge to know whether they continued with sleep medication use outside the hospital. Finally, in this retrospective chart review, we focused on utilization metrics, not on efficacy (which we can only infer) or adverse effects, such as altered mental status or falls. Moreover, we did not compare those patients who did and who did not receive any medication for sleep. However, such work will be crucial in future studies.
CONCLUSIONS
Despite increasing evidence of risks such as delirium or falls, pharmacological sleep aid use in hospitalized patients, even the elderly, remains common. A variety of medications are used, with variable administration times, which likely reflects the few rigorous studies or guidelines for the use of pharmacological sleep aids in hospitalized patients. Many patients not known to be on medications for sleep before admission leave the hospital with a sleep aid prescription. Our results suggest the need to better understand the factors that contribute to the high rate of sleep aid use in hospitalized patients. Clinician education regarding sleep, and nonpharmacological strategies to improve sleep in the hospital, are also needed.
Disclosure: Nothing to report.
- , , , . Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473–482.
- . Sleep and the sleep environment of older adults in acute care settings. J Gerontol Nurs. 2008;34(6):15–21.
- , , , et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676.
- , , , . Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1–6.
- , , , , , . An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17.
- , , , , . Decrease in as‐needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5(3):E20–E24.
- , , , , , . Guided prescription of psychotropic medications for geriatric inpatients. Arch Intern Med. 2005;165(7):802–807.
- , , , . National use of prescription medications for insomnia: NHANES 1999–2010. Sleep. 2014;37(2):343–349.
- , . Safety of low doses of quetiapine when used for insomnia. Ann Pharmacother. 2012;46(5):718–722.
- , . Ten‐year trends in the pharmacological treatment of insomnia. Sleep. 1999;22(3):371–375.
- , , , . How do clinicians assess, communicate about, and manage patient sleep in the hospital? J Nurs Adm. 2013;43(6):342–347.
- , , . Postoperative sleep disturbances after zolpidem treatment in fast‐track hip and knee replacement. J Clin Sleep Med. 2014;10(3):321–326.
- , , . Sleep deprivation after septic insult increases mortality independent of age. J Trauma. 2009;66(1):50–54.
- , , , , , . Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. Faseb J. 1996;10(5):643–653.
- , , , et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185–2186.
- , , , et al. Quality improvement and cost savings with multicomponent delirium interventions: replication of the Hospital Elder Life Program in a community hospital. Psychosomatics. 2013;54(3):219–226.
- , , , , . Hospitalized patients' preference in the treatment of insomnia: pharmacological versus non‐pharmacological. Can J Clin Pharmacol. 2003;10(2):89–92.
- , , , et al. Post‐discharge insomnia symptoms are associated with quality of life impairment among survivors of acute lung injury. Sleep Med. 2012;13(8):1106–1109.
- , , , , , . Hospitalization as a turning point for sleep medication use in older adults: prospective cohort study. Drugs Aging. 2012;29(7):565–576.
- , , , et al. Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013;61(7):1128–1134.
- , . Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484.
- , , , . Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med. 2008;3(6):473–482.
- . Sleep and the sleep environment of older adults in acute care settings. J Gerontol Nurs. 2008;34(6):15–21.
- , , , et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669–676.
- , , , . Zolpidem is independently associated with increased risk of inpatient falls. J Hosp Med. 2013;8(1):1–6.
- , , , , , . An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;2:17.
- , , , , . Decrease in as‐needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5(3):E20–E24.
- , , , , , . Guided prescription of psychotropic medications for geriatric inpatients. Arch Intern Med. 2005;165(7):802–807.
- , , , . National use of prescription medications for insomnia: NHANES 1999–2010. Sleep. 2014;37(2):343–349.
- , . Safety of low doses of quetiapine when used for insomnia. Ann Pharmacother. 2012;46(5):718–722.
- , . Ten‐year trends in the pharmacological treatment of insomnia. Sleep. 1999;22(3):371–375.
- , , , . How do clinicians assess, communicate about, and manage patient sleep in the hospital? J Nurs Adm. 2013;43(6):342–347.
- , , . Postoperative sleep disturbances after zolpidem treatment in fast‐track hip and knee replacement. J Clin Sleep Med. 2014;10(3):321–326.
- , , . Sleep deprivation after septic insult increases mortality independent of age. J Trauma. 2009;66(1):50–54.
- , , , , , . Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. Faseb J. 1996;10(5):643–653.
- , , , et al. Objective sleep duration and quality in hospitalized older adults: associations with blood pressure and mood. J Am Geriatr Soc. 2011;59(11):2185–2186.
- , , , et al. Quality improvement and cost savings with multicomponent delirium interventions: replication of the Hospital Elder Life Program in a community hospital. Psychosomatics. 2013;54(3):219–226.
- , , , , . Hospitalized patients' preference in the treatment of insomnia: pharmacological versus non‐pharmacological. Can J Clin Pharmacol. 2003;10(2):89–92.
- , , , et al. Post‐discharge insomnia symptoms are associated with quality of life impairment among survivors of acute lung injury. Sleep Med. 2012;13(8):1106–1109.
- , , , , , . Hospitalization as a turning point for sleep medication use in older adults: prospective cohort study. Drugs Aging. 2012;29(7):565–576.
- , , , et al. Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013;61(7):1128–1134.
- , . Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479–1484.
© 2014 Society of Hospital Medicine





