Commentary

New Guidelines of Care for the Management of Nonmelanoma Skin Cancer
In January 2018, the American Academy of Dermatology (AAD) released its first guidelines of care for the management of nonmelanoma skin cancer (...
From the Dermatology Department, University of Connecticut Health Center, Farmington.
The authors report no conflict of interest.
Correspondence: Jane M. Grant-Kels, MD, University of Connecticut Dermatology Department, 21 South Rd, Farmington, CT 06032 (grant@uchc.edu).

Management of nonmelanoma skin cancer (NMSC) in elderly patients carries a risk for morbidity; these patients frequently struggle to care for their biopsy sites and experience biopsy- and surgery-related complications. To minimize this treatment-related morbidity, we designed a knifeless treatment approach that employs reflectance confocal microscopy (RCM) in lieu of skin biopsy to establish the diagnosis of NMSC, then uses either intralesional or topical chemotherapy or immunotherapy (as appropriate, depending on depth of invasion) to cure the NMSC. By using this approach, the patient is spared surgery-related difficulties.
Management of nonmelanoma skin cancer (NMSC) in elderly patients can cause morbidity because these patients frequently struggle to care for their biopsy sites and experience biopsy- and surgery-related complications. To minimize this treatment-related morbidity, we designed a knifeless treatment approach that employs reflectance confocal microscopy (RCM) in lieu of skin biopsy to establish the diagnosis of NMSC, then uses either intralesional or topical chemotherapy or immunotherapy (as appropriate, depending on depth of invasion) to cure the NMSC. With this approach, the patient is spared both biopsy- and surgery-related difficulties, though both intralesional and topical chemotherapy are accompanied by their own risks for adverse effects.
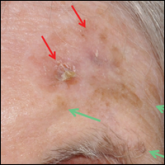
Elderly patients, diabetic patients, and patients with lesions suspicious for NMSC on areas prone to poor wound healing or to notable treatment-related morbidity (eg, lower legs, genitals, the face of younger patients) are offered skin biopsy or RCM; the latter is performed during the appointment by an RCM-trained medical assistant. Patients who elect to undergo RCM and who have a diagnosis of superficial basal cell carcinoma (BCC) or squamous cell carcinoma (SCC) in situ are then treated with topical imiquimod or 5-fluorouracil. Patients with an invasive subtype of either BCC, SCC, or keratoacanthoma receive intralesional 5-fluorouracil injected at a concentration of 50 mg/cc at weekly intervals until the lesion blanches, with ongoing follow-up until the lesion is observed to have resolved under dermoscopic inspection.
When resolution is uncertain, RCM is repeated to assess for tumor clearance. Repeat RCM is performed at least 4 weeks after termination of treatment to avoid misinterpretation caused by treatment-related tissue inflammation. Patients who are not cured using this management approach are offered appropriate surgical management.
Reflectance confocal microscopy has emerged as an effective modality for confirming the diagnosis of NMSC with high sensitivity and specificity.1,2 Emergence of this technology presents an opportunity for improving the way the NMSC is managed because RCM allows dermatologists to confirm the diagnosis of BCC and SCC by interpretation of RCM mosaics rather than by histopathologic examination of biopsied tissue. Our knifeless approach to skin cancer management is especially beneficial when biopsy and dermatologic surgery are likely to confer notable morbidity, such as managing NMSC on the face of a young adult, in the frail elderly population, or in diabetic patients, and when treating sites on the lower extremity prone to poor wound healing.

In January 2018, the American Academy of Dermatology (AAD) released its first guidelines of care for the management of nonmelanoma skin cancer (...

Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma and is a diagnostic challenge in its early stages. It often can be...