User login
Formerly Skin & Allergy News
ass lick
assault rifle
balls
ballsac
black jack
bleach
Boko Haram
bondage
causas
cheap
child abuse
cocaine
compulsive behaviors
cost of miracles
cunt
Daech
display network stats
drug paraphernalia
explosion
fart
fda and death
fda AND warn
fda AND warning
fda AND warns
feom
fuck
gambling
gfc
gun
human trafficking
humira AND expensive
illegal
ISIL
ISIS
Islamic caliphate
Islamic state
madvocate
masturbation
mixed martial arts
MMA
molestation
national rifle association
NRA
nsfw
nuccitelli
pedophile
pedophilia
poker
porn
porn
pornography
psychedelic drug
recreational drug
sex slave rings
shit
slot machine
snort
substance abuse
terrorism
terrorist
texarkana
Texas hold 'em
UFC
section[contains(@class, 'nav-hidden')]
section[contains(@class, 'nav-hidden active')]
The leading independent newspaper covering dermatology news and commentary.
Analysis supports link between psoriasis and obstructive sleep apnea
TOPLINE:
Patients with psoriasis had a 1.77-fold increased risk of having obstructive sleep apnea, in a study comparing patients with psoriasis with controls.
METHODOLOGY:
- Prior studies have established a link between psoriasis and obstructive sleep apnea (OSA), but some have suggested that confounders may drive the association.
- Using a case-control design, researchers analyzed data from 156,707 participants in the National Institutes of Health’s : 5140 with psoriasis and 151,567 controls.
- They used Pearson’s x 2 test to compare the prevalence of OSA among cases and controls, logistic regression to calculate odds ratios (ORs) in multivariable analysis, and two-sided t-tests to evaluate the significance between continuous variables.
TAKEAWAY:
- Compared with controls, patients with psoriasis were older (a mean of 62.4 vs 57.3 years, respectively), more likely to be White (86.1% vs 70.6%), reported higher annual household incomes (59.9% vs 52.6%), and were more likely to smoke (48.2% vs 43.4%).
- The rate of OSA was significantly higher among patients with psoriasis compared with controls (29.3% vs 17.1%; P < .001).
- On unadjusted multivariable logistic regression controlling for age, gender, and race, psoriasis was significantly associated with OSA (OR, 1.77, 95% CI, 1.66 - 1.89; P < .001).
- Psoriasis was also significantly associated with OSA in the adjusted model controlling for age, gender, race, BMI, and smoking status (OR, 1.66, 95% CI, 1.55 - 1.77; P < .001) and in the adjusted model controlling for age, gender, race, BMI, smoking status, type 2 diabetes, congestive heart failure, hypertension, history of myocardial infarction, angina, and peripheral artery disease (OR, 1.45, 95% CI, 1.35 - 1.55; P <.001).
IN PRACTICE:
“This study further substantiates the association between psoriasis and OSA, reinforcing the importance of evaluation for OSA when clinically appropriate given that both psoriasis and OSA contribute to adverse health outcomes,” the authors conclude.
SOURCE:
Corresponding author Jeffrey M. Cohen, MD, of the Department of Dermatology at Yale University, New Haven, Connecticut, led the research. The study was published online in the Journal of the American Academy of Dermatology.
LIMITATIONS:
Study limitations included the use of electronic health record data, a potential lack of generalizability to the US population, and reliance on survey data for certain variables such as income and smoking status.
DISCLOSURES:
The All of Us Research Program is supported by the National Institutes of Health. Cohen disclosed that he serves on a data safety and monitoring board for Advarra.
A version of this article appeared on Medscape.com.
TOPLINE:
Patients with psoriasis had a 1.77-fold increased risk of having obstructive sleep apnea, in a study comparing patients with psoriasis with controls.
METHODOLOGY:
- Prior studies have established a link between psoriasis and obstructive sleep apnea (OSA), but some have suggested that confounders may drive the association.
- Using a case-control design, researchers analyzed data from 156,707 participants in the National Institutes of Health’s : 5140 with psoriasis and 151,567 controls.
- They used Pearson’s x 2 test to compare the prevalence of OSA among cases and controls, logistic regression to calculate odds ratios (ORs) in multivariable analysis, and two-sided t-tests to evaluate the significance between continuous variables.
TAKEAWAY:
- Compared with controls, patients with psoriasis were older (a mean of 62.4 vs 57.3 years, respectively), more likely to be White (86.1% vs 70.6%), reported higher annual household incomes (59.9% vs 52.6%), and were more likely to smoke (48.2% vs 43.4%).
- The rate of OSA was significantly higher among patients with psoriasis compared with controls (29.3% vs 17.1%; P < .001).
- On unadjusted multivariable logistic regression controlling for age, gender, and race, psoriasis was significantly associated with OSA (OR, 1.77, 95% CI, 1.66 - 1.89; P < .001).
- Psoriasis was also significantly associated with OSA in the adjusted model controlling for age, gender, race, BMI, and smoking status (OR, 1.66, 95% CI, 1.55 - 1.77; P < .001) and in the adjusted model controlling for age, gender, race, BMI, smoking status, type 2 diabetes, congestive heart failure, hypertension, history of myocardial infarction, angina, and peripheral artery disease (OR, 1.45, 95% CI, 1.35 - 1.55; P <.001).
IN PRACTICE:
“This study further substantiates the association between psoriasis and OSA, reinforcing the importance of evaluation for OSA when clinically appropriate given that both psoriasis and OSA contribute to adverse health outcomes,” the authors conclude.
SOURCE:
Corresponding author Jeffrey M. Cohen, MD, of the Department of Dermatology at Yale University, New Haven, Connecticut, led the research. The study was published online in the Journal of the American Academy of Dermatology.
LIMITATIONS:
Study limitations included the use of electronic health record data, a potential lack of generalizability to the US population, and reliance on survey data for certain variables such as income and smoking status.
DISCLOSURES:
The All of Us Research Program is supported by the National Institutes of Health. Cohen disclosed that he serves on a data safety and monitoring board for Advarra.
A version of this article appeared on Medscape.com.
TOPLINE:
Patients with psoriasis had a 1.77-fold increased risk of having obstructive sleep apnea, in a study comparing patients with psoriasis with controls.
METHODOLOGY:
- Prior studies have established a link between psoriasis and obstructive sleep apnea (OSA), but some have suggested that confounders may drive the association.
- Using a case-control design, researchers analyzed data from 156,707 participants in the National Institutes of Health’s : 5140 with psoriasis and 151,567 controls.
- They used Pearson’s x 2 test to compare the prevalence of OSA among cases and controls, logistic regression to calculate odds ratios (ORs) in multivariable analysis, and two-sided t-tests to evaluate the significance between continuous variables.
TAKEAWAY:
- Compared with controls, patients with psoriasis were older (a mean of 62.4 vs 57.3 years, respectively), more likely to be White (86.1% vs 70.6%), reported higher annual household incomes (59.9% vs 52.6%), and were more likely to smoke (48.2% vs 43.4%).
- The rate of OSA was significantly higher among patients with psoriasis compared with controls (29.3% vs 17.1%; P < .001).
- On unadjusted multivariable logistic regression controlling for age, gender, and race, psoriasis was significantly associated with OSA (OR, 1.77, 95% CI, 1.66 - 1.89; P < .001).
- Psoriasis was also significantly associated with OSA in the adjusted model controlling for age, gender, race, BMI, and smoking status (OR, 1.66, 95% CI, 1.55 - 1.77; P < .001) and in the adjusted model controlling for age, gender, race, BMI, smoking status, type 2 diabetes, congestive heart failure, hypertension, history of myocardial infarction, angina, and peripheral artery disease (OR, 1.45, 95% CI, 1.35 - 1.55; P <.001).
IN PRACTICE:
“This study further substantiates the association between psoriasis and OSA, reinforcing the importance of evaluation for OSA when clinically appropriate given that both psoriasis and OSA contribute to adverse health outcomes,” the authors conclude.
SOURCE:
Corresponding author Jeffrey M. Cohen, MD, of the Department of Dermatology at Yale University, New Haven, Connecticut, led the research. The study was published online in the Journal of the American Academy of Dermatology.
LIMITATIONS:
Study limitations included the use of electronic health record data, a potential lack of generalizability to the US population, and reliance on survey data for certain variables such as income and smoking status.
DISCLOSURES:
The All of Us Research Program is supported by the National Institutes of Health. Cohen disclosed that he serves on a data safety and monitoring board for Advarra.
A version of this article appeared on Medscape.com.
What’s new in acne treatment?
NEW YORK — New treatments for acne, including the recent FDA approval of a topical gel that combines an antibiotic, a retinoid, and an antimicrobial agent, and reports on the safe use of lasers in people with darker skin types, were presented at the annual Mount Sinai Winter Symposium – Advances in Medical and Surgical Dermatology.
“Patients want clear skin and many don’t care how they get there. I see patients who have been on minocycline [a broad-spectrum antibiotic] for 2 years; this is really not the best way to treat our patients,” said Joshua Zeichner, MD, associate professor of dermatology at the Icahn School of Medicine at Mount Sinai Hospital, New York, who reviewed the current state of acne treatments at the meeting.
Patients often do not care about the risk of developing antibiotic resistance, he noted, citing a survey (funded by Almirall and presented at a previous conference), which found that less than 10% of adult patients or caregivers of patients being treated for acne were moderately or extremely worried about antibiotics compared with more than 65% of the clinicians. But despite their concerns, nearly 60% of clinicians surveyed reported prescribing broad-spectrum antibiotics “most” or “all of the time,” he said.
Dr. Zeichner said that patients’ short-term wishes overriding dermatologists’ own concerns can lead to antibiotic resistance, with a negative impact on patients’ microbiomes. He encouraged prescribers to incorporate sarecycline and other narrow spectrum antibiotics into their practice as part of antibiotic stewardship. These drugs have less of an impact on the gut microbiome than broad spectrum antibiotics, while targeting the patient’s acne.
Dr. Zeichner noted that “acne is more than a 12-week disease,” but manufacturers of acne treatments can only market information based on what is in the product labeling, which usually includes 12-week results. Yet, for many acne treatments, “as you continue treating over time, you’re seeing much better improvements,” he said.
As an example, he referred to data from an unpublished phase 4 Galderma study. Patients aged 17-35 years with acne and scarring who were treated with trifarotene cream demonstrated about a 52% rate of success in acne clearance as measured by the Investigator Global Assessment (IGA) at 24 weeks, up from 31.4% at 12 weeks, highlighting the need to consider long-term data, which is helpful for patients to know, he said.
Dr. Zeichner noted that many patients and their caregivers are enthusiastic about the idea of treatment that does not involve pharmaceuticals and that these options, while not “silver bullets,” are available and advancing.
These include light-based devices. He referred to a 7-week, open label efficacy and safety study of a photo-pneumatic device with broadband light (Strata Skin Sciences). This device uses thermal heat to target and destroy Cutibacterium acnes and reduce sebum production and has a vacuum feature that removes occlusive material from the pilosebaceous unit, which he said “leads directly to a reduction in acne lesions.”
Of note is the fact that the device’ filters out visible wavelength light, which minimizes absorption by melanin in the epidermis that can damage darker skin, making the treatment safe for most skin types. In the study of patients with mild to moderate facial acne, aged 12-40 years, treatment resulted in significant reductions in mean inflammatory and noninflammatory lesion counts, and mean IGA score at day 49 compared with baseline.
Similarly, Dr. Zeichner presented a 2022 study demonstrating the use of higher spectrum lasers (a 1726-nm [nanometer] laser) to shrink sebaceous glands and reduce sebum production to treat acne. In addition, lasers that operate at such a high frequency do not cause hyperpigmentation in individuals with darker skin types, he said.
Dr. Zeichner disclosed that he is an advisor, consultant, or speaker for AbbVie, Allergan, Arcutis, Beiersdorf, Dermavant, Galderma, Kenvue, L’Oreal, Ortho, Pfizer, Regeneron, UCB, and Sun.
A version of this article first appeared on Medscape.com.
NEW YORK — New treatments for acne, including the recent FDA approval of a topical gel that combines an antibiotic, a retinoid, and an antimicrobial agent, and reports on the safe use of lasers in people with darker skin types, were presented at the annual Mount Sinai Winter Symposium – Advances in Medical and Surgical Dermatology.
“Patients want clear skin and many don’t care how they get there. I see patients who have been on minocycline [a broad-spectrum antibiotic] for 2 years; this is really not the best way to treat our patients,” said Joshua Zeichner, MD, associate professor of dermatology at the Icahn School of Medicine at Mount Sinai Hospital, New York, who reviewed the current state of acne treatments at the meeting.
Patients often do not care about the risk of developing antibiotic resistance, he noted, citing a survey (funded by Almirall and presented at a previous conference), which found that less than 10% of adult patients or caregivers of patients being treated for acne were moderately or extremely worried about antibiotics compared with more than 65% of the clinicians. But despite their concerns, nearly 60% of clinicians surveyed reported prescribing broad-spectrum antibiotics “most” or “all of the time,” he said.
Dr. Zeichner said that patients’ short-term wishes overriding dermatologists’ own concerns can lead to antibiotic resistance, with a negative impact on patients’ microbiomes. He encouraged prescribers to incorporate sarecycline and other narrow spectrum antibiotics into their practice as part of antibiotic stewardship. These drugs have less of an impact on the gut microbiome than broad spectrum antibiotics, while targeting the patient’s acne.
Dr. Zeichner noted that “acne is more than a 12-week disease,” but manufacturers of acne treatments can only market information based on what is in the product labeling, which usually includes 12-week results. Yet, for many acne treatments, “as you continue treating over time, you’re seeing much better improvements,” he said.
As an example, he referred to data from an unpublished phase 4 Galderma study. Patients aged 17-35 years with acne and scarring who were treated with trifarotene cream demonstrated about a 52% rate of success in acne clearance as measured by the Investigator Global Assessment (IGA) at 24 weeks, up from 31.4% at 12 weeks, highlighting the need to consider long-term data, which is helpful for patients to know, he said.
Dr. Zeichner noted that many patients and their caregivers are enthusiastic about the idea of treatment that does not involve pharmaceuticals and that these options, while not “silver bullets,” are available and advancing.
These include light-based devices. He referred to a 7-week, open label efficacy and safety study of a photo-pneumatic device with broadband light (Strata Skin Sciences). This device uses thermal heat to target and destroy Cutibacterium acnes and reduce sebum production and has a vacuum feature that removes occlusive material from the pilosebaceous unit, which he said “leads directly to a reduction in acne lesions.”
Of note is the fact that the device’ filters out visible wavelength light, which minimizes absorption by melanin in the epidermis that can damage darker skin, making the treatment safe for most skin types. In the study of patients with mild to moderate facial acne, aged 12-40 years, treatment resulted in significant reductions in mean inflammatory and noninflammatory lesion counts, and mean IGA score at day 49 compared with baseline.
Similarly, Dr. Zeichner presented a 2022 study demonstrating the use of higher spectrum lasers (a 1726-nm [nanometer] laser) to shrink sebaceous glands and reduce sebum production to treat acne. In addition, lasers that operate at such a high frequency do not cause hyperpigmentation in individuals with darker skin types, he said.
Dr. Zeichner disclosed that he is an advisor, consultant, or speaker for AbbVie, Allergan, Arcutis, Beiersdorf, Dermavant, Galderma, Kenvue, L’Oreal, Ortho, Pfizer, Regeneron, UCB, and Sun.
A version of this article first appeared on Medscape.com.
NEW YORK — New treatments for acne, including the recent FDA approval of a topical gel that combines an antibiotic, a retinoid, and an antimicrobial agent, and reports on the safe use of lasers in people with darker skin types, were presented at the annual Mount Sinai Winter Symposium – Advances in Medical and Surgical Dermatology.
“Patients want clear skin and many don’t care how they get there. I see patients who have been on minocycline [a broad-spectrum antibiotic] for 2 years; this is really not the best way to treat our patients,” said Joshua Zeichner, MD, associate professor of dermatology at the Icahn School of Medicine at Mount Sinai Hospital, New York, who reviewed the current state of acne treatments at the meeting.
Patients often do not care about the risk of developing antibiotic resistance, he noted, citing a survey (funded by Almirall and presented at a previous conference), which found that less than 10% of adult patients or caregivers of patients being treated for acne were moderately or extremely worried about antibiotics compared with more than 65% of the clinicians. But despite their concerns, nearly 60% of clinicians surveyed reported prescribing broad-spectrum antibiotics “most” or “all of the time,” he said.
Dr. Zeichner said that patients’ short-term wishes overriding dermatologists’ own concerns can lead to antibiotic resistance, with a negative impact on patients’ microbiomes. He encouraged prescribers to incorporate sarecycline and other narrow spectrum antibiotics into their practice as part of antibiotic stewardship. These drugs have less of an impact on the gut microbiome than broad spectrum antibiotics, while targeting the patient’s acne.
Dr. Zeichner noted that “acne is more than a 12-week disease,” but manufacturers of acne treatments can only market information based on what is in the product labeling, which usually includes 12-week results. Yet, for many acne treatments, “as you continue treating over time, you’re seeing much better improvements,” he said.
As an example, he referred to data from an unpublished phase 4 Galderma study. Patients aged 17-35 years with acne and scarring who were treated with trifarotene cream demonstrated about a 52% rate of success in acne clearance as measured by the Investigator Global Assessment (IGA) at 24 weeks, up from 31.4% at 12 weeks, highlighting the need to consider long-term data, which is helpful for patients to know, he said.
Dr. Zeichner noted that many patients and their caregivers are enthusiastic about the idea of treatment that does not involve pharmaceuticals and that these options, while not “silver bullets,” are available and advancing.
These include light-based devices. He referred to a 7-week, open label efficacy and safety study of a photo-pneumatic device with broadband light (Strata Skin Sciences). This device uses thermal heat to target and destroy Cutibacterium acnes and reduce sebum production and has a vacuum feature that removes occlusive material from the pilosebaceous unit, which he said “leads directly to a reduction in acne lesions.”
Of note is the fact that the device’ filters out visible wavelength light, which minimizes absorption by melanin in the epidermis that can damage darker skin, making the treatment safe for most skin types. In the study of patients with mild to moderate facial acne, aged 12-40 years, treatment resulted in significant reductions in mean inflammatory and noninflammatory lesion counts, and mean IGA score at day 49 compared with baseline.
Similarly, Dr. Zeichner presented a 2022 study demonstrating the use of higher spectrum lasers (a 1726-nm [nanometer] laser) to shrink sebaceous glands and reduce sebum production to treat acne. In addition, lasers that operate at such a high frequency do not cause hyperpigmentation in individuals with darker skin types, he said.
Dr. Zeichner disclosed that he is an advisor, consultant, or speaker for AbbVie, Allergan, Arcutis, Beiersdorf, Dermavant, Galderma, Kenvue, L’Oreal, Ortho, Pfizer, Regeneron, UCB, and Sun.
A version of this article first appeared on Medscape.com.
Eight wealth tips just for doctors
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
The average physician makes $352,000, and some earn well into the $500,000s. So, doctors don’t have to worry about money, right?
You know the answer to that.
One thing all physicians have in common about money, says James M. Dahle, MD, FACEP, founder of The White Coat Investor, is that they don’t receive any training in business, personal finance, or investing throughout their schooling or careers unless they seek it out. This leaves many unprepared to make the best investing and money-saving decisions, while others get too frustrated about their lack of knowledge to even dip their toe into the investing pool.
Exhibit A: Four out of 10 physicians have a net worth below $1 million, according to the Medscape Physician Wealth & Debt Report 2023. Elizabeth Chiang, MD, PhD, an oculoplastic surgeon and a physician money coach at Grow Your Wealthy Mindset, notes that many of those doctors are over age 65, “which means they essentially can’t retire.”
And that’s just one pain point.
Physicians have money concerns specific to their profession and background. Luckily, some fellow doctors also serve as financial and wealth advisors just for other doctors.
Blind Spot #1
The early lean years skew doctors’ money outlook. “We have an extended training period, which commonly consists of taking on a large amount of debt, followed by 3 to 8 years of being paid a modest salary, and then finally a large boost in income,” explains Dr. Chiang. This can lay a shaky foundation for the earning years to come, and as a result, a lot of doctors just don’t think about money in healthy ways. Once their incomes increase, physicians may be surprised, for example, that making a multiple six-figure salary means paying six figures in taxes.
The Fix
Treat financial health like physical health. That means money cannot be a taboo subject. “The misguided mindset is that we didn’t become physicians to make money, we did it to help people,” explains Jordan Frey, MD, creator of the blog, The Prudent Plastic Surgeon.
Dr. Frey acknowledges that the desire to help is certainly true. But the result is a false idea that “to think about our personal finances makes us a worse doctor.”
Blind Spot #2
Because doctors know a lot about one thing (medicine), they might assume they know a lot about everything (such as investing). “Totally different fields with a different language and different way to think about it,” Dahle explains. This overconfidence could lead to some negligent or risky financial decisions.
The Fix
Educate yourself. There are several books on personal finance and investing written by physicians for physicians. Dr. Chiang recommends The Physician Philosopher’s Guide to Personal Finance, by James Turner, MD; Financial Freedom Rx, by Chirag Shah, MD, and Jayanth Sridhar, MD; and The Physician’s Guide to Finance, by Nicholas Christian and Amanda Christian, MD. There are also podcasts, blogs, and courses to help educate doctors on finance, such as the Fire Your Financial Advisor course by The White Coat Investor.
Blind Spot #3
Undersaving. Retirement saving is one thing, but 24% of doctors say they don’t even put money away in a taxable savings account, according to the Wealth & Debt Report.
Cobin Soelberg, MD, JD, a board-certified anesthesiologist and founder and principal advisor with Greeley Wealth Management, is the treasurer of his anesthesiology group. “I get to see every month how much people are saving, and even on an anesthesiologist salary, where everyone’s making about $400,000 a year, a lot of people are not saving anything, which is crazy.”
Undersaving can be both a time issue and a mindset one.
Time: Doctors often start investing in their retirement accounts later than the average professional, says Dr. Chiang. “A lot of physicians will max out their 401k or 403b,” she explains. “But if you’re putting in $20,000 a year and only starting when you’re in your early 30s, that’s not enough to get you to retirement.”
Mindset: Doctors also see people of all ages who are sick, dying, and injured. “They all know someone who worked hard and saved and then dropped dead at 55,” explains Dr. Dahle. This, he says, can lead to a bit of a “you only live once” attitude that prioritizes spending over saving.
The Fix
Shoot for 20%. If you can’t save 20% of your gross now, strive to get to that point. Think of it as telling a patient they have to change their behavior or trouble will come - not if, but when. “Develop a written investing plan and then stick with it through thick and thin,” says Dr. Dahle. “Once you have a reasonable plan, all you have to do is fund it adequately by saving 20% of your gross income, and a doctor will easily retire as a multimillionaire.”
Blind Spot #4
Bad investment strategies. Thirty-six percent of doctors experience their largest financial losses from lousy investments, according to the Wealth & Debt Report. Meanwhile, 17% of PCPs and 12% of specialists say they haven’t made any investments at all. That’s a terrible mix of doing the wrong thing and doing a worse thing.
The Fix
Don’t overthink investing, but don’t underthink it either. “As high-income earners, doctors just don’t need to take this high level of risk to reach their financial goals,” Dr. Frey says. A good investment plan doesn’t require you to time the stock market or predict individual stock winners. Consider what Vanguard founder Jack Bogle once said about investing: “Be bored by the process but elated by the outcome.”
Dr. Frey suggests going super-simple: index funds. Ignore investing strategies with actively managed mutual funds or individual stocks, as well as risky alternative investments such as cryptocurrency and angel investments. Everyone assumes doctors have money to burn, and they will push sketchy investment ideas at them. Avoid.
Blind Spot #5
Not taking debt seriously enough. The average medical student debt is $250,000 and can exceed $500,000, says Dr. Soelberg. Many doctors spend the first 10 to 20 years of their careers paying this off. Today’s graduates are paying more than 7% on their loans.
And it’s not just student debt: 39% of physicians carry five or more credit cards, and 34% have mortgages larger than $300,000 (with half of those are more than than $500K), per the Wealth & Debt Report.
The Fix
Treat debt like cancer. It’s a lethal enemy you can’t get rid of right away, but a steady, aggressive, long-term attack will have the best results. Dr. Soelberg suggests allocating the most you can afford per month, whether that’s $1000 or $5000, toward debt. Raise the amount as your income grows. Do the same with your 401k or retirement plan. Whatever is left, you can spend. Five to 10 years later, you will realize, “Wow. I’m debt free.”
Blind Spot #6
Not putting in the work to improve your situation. Seventy-one percent of doctors admit they haven’t done anything to reduce major expenses, according to the Wealth & Debt Report. Are you leaving major money on the table?
The Fix
Audit yourself in major areas like housing and taxes. While the average professional may need to put 10% to 20% down on a home, physicians can qualify for physician mortgage loans and can often put down 3% or less, says Dr. Chiang. If you can afford the higher mortgage payment, excess savings earmarked for a larger down payment can be put toward debt or invested.
Another trick, if you’re able, is to seek an area that is less in demand at a higher salary. “Physicians in places like New York City or San Francisco tend to make less than physicians in the Midwest or the South,” Dr. Chiang explains. A colleague of hers moved to rural Pennsylvania, where he made a high salary and had a low cost of living for 3½ years, paid off his student debt, and then relocated to an area where he wanted to live long term.
As for taxes, become familiar with tax law. Research things like, “What is considered a business expense for doctors?” says Brett Mollard, MD, a diagnostic radiologist who provides financial advice to younger physicians. “What will your estimated total tax burden be at the end of the year? Will you need to make extra payments to prevent owing a large sum of money from underpaying or to avoid tax penalties?”
Blind Spot #7
Living like a rock star on a doctor’s income. Getting caught up in trying to live the same lifestyle as your colleagues is a classic bear trap. “Sitting in the doctor’s lounge, it’s so crazy,” Dr. Soelberg says. He describes conversations like, “‘Where did you go on your trip?’ ‘What new toys are you buying?’” There’s pressure to live up to an image of what a doctor’s life is supposed to look like before you’ve sorted the basic things like paying off debt.
The Fix
Live like a resident even if you haven’t been one for years, at least until you’re in a better financial position. “You’re already used to living a life of lower means, and you’re an expert when it comes to delaying gratification,” says Dr. Mollard. “Do it a little longer.” Live frugally and spend only on things that bring you joy. “A lot of physicians are trying to be really rich in all areas of their life instead of the ones that actually matter to them,” Dr. Soelberg says. Identify what’s important to you and only splurge on that.
Blind Spot #8
Never asking for help. The right financial planner can provide expert help. Emphasis on right. “Doctors can be very trusting of other professionals, even when they should not be,” says Dr. Dahle. He notes that in financial services, many people masquerade as knowledgeable advisors who are really just salespeople. While legitimate financial advisors strive to make their clients money, they are also ultimately out to line their pockets and love to work with physician salaries. Thus, doctors can end up working with financial planners that don’t specifically understand their situations or end up taking too much from their clients.
The Fix
Find a planner who specializes in, or at least understands, physicians. Ask them how they make money, says Dr. Chiang. If someone hesitates to tell you about their fee structure or if it sounds like a lot, shop around and ask colleagues for recommendations.
“Ultimately, the path to wealth is to create and grow the margin between what you make and what you spend,” says Dr. Frey. Throw some investing into the mix and physicians can set themselves up on a path for a stress-free financial life.
A version of this article appeared on Medscape.com.
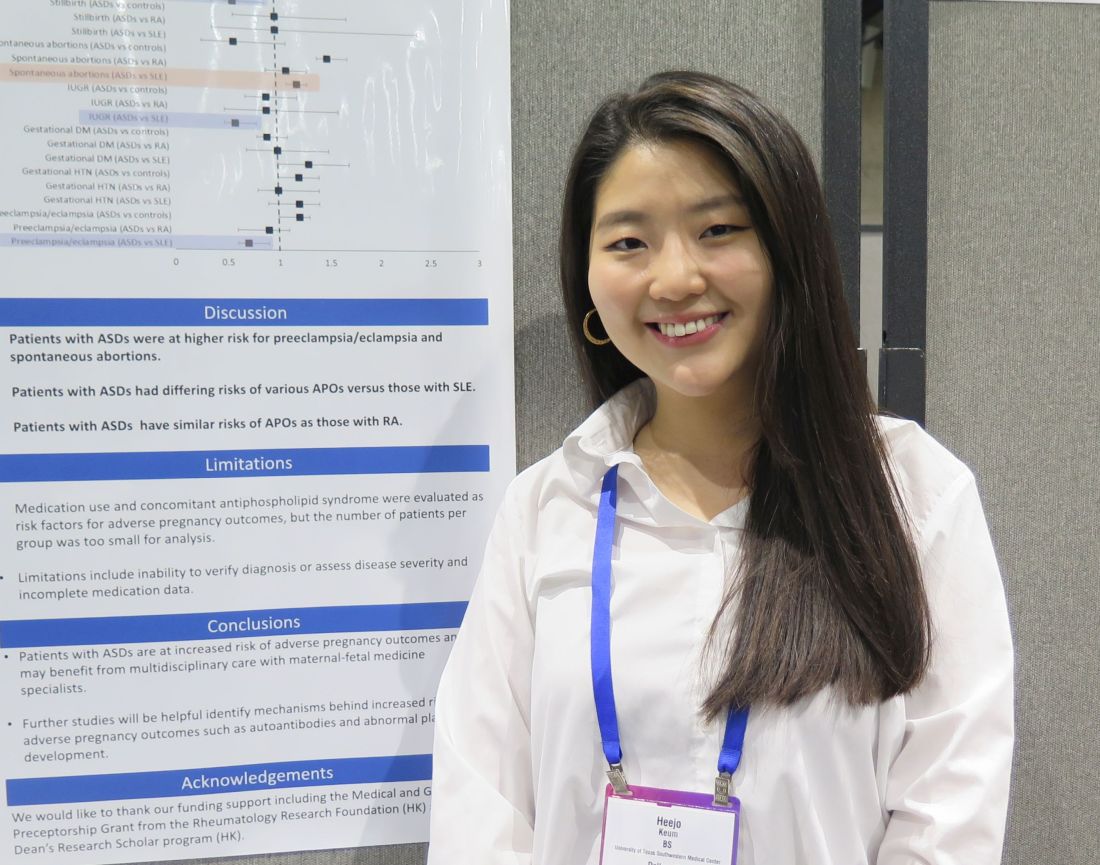
Autoimmune Skin Diseases Linked To Risk Of Adverse Pregnancy Outcomes
SAN DIEGO — , results from a large case-control study suggest.
Patients with systemic autoimmune conditions are known to have an increased risk for adverse pregnancy outcomes, “but we weren’t sure if that was the case for patients with autoimmune skin conditions,” presenting study author Heejo Keum, a fourth-year medical student at the University of Texas Southwestern Medical Center, Dallas, said in an interview during a poster session at the American College of Rheumatology (ACR) 2023 annual meeting. “There are case reports or nationwide population-based studies on patients with alopecia areata and vitiligo, but those were outside of the US, so we wanted to see if these outcomes could be studied in a larger population-based study in the US.”
Drawing from the TriNetX US Collaborative Network, a database of electronic medical records of 94 million patients in the United States, the researchers identified pregnant patients aged 15-44 years between January 1, 2016, and December 31, 2021. Cases were defined as patients diagnosed with at least one autoimmune skin disease (ASD) prior to the end of pregnancy, including alopecia areata, bullous pemphigoid, cicatricial pemphigoid, dermatitis herpetiformis, cutaneous lupus erythematosus, epidermolysis bullosa acquisita, morphea, pemphigus foliaceus, pemphigus vulgaris, vitiligo, and amyopathic DM. There were two control groups: healthy controls (those without ASDs, systemic lupus erythematosus or rheumatoid arthritis) and disease controls (those with SLE or RA). The researchers used ICD-10 codes to identify pregnancy endpoints, including live births, spontaneous abortion, and stillbirth. Patients with a history of hidradenitis suppurative were excluded from the analysis, as were those with common autoimmune disease such as Hashimoto’s thyroiditis, Grave’s disease, and type 1 diabetes.
The primary outcomes were adverse pregnancy outcomes defined as spontaneous abortion, gestational hypertension, preeclampsia/eclampsia, gestational diabetes, intrauterine growth restriction (IUGR), preterm premature rupture of membranes (PPROM), and preterm birth. The researchers used 1:1 propensity scoring to match patients with ASDs to controls by age, race, ethnicity, comorbidities, obesity, and substance use, and used odds ratio (OR) analysis with a 95% confidence interval (CI) to calculate each outcome.
Ms. Keum reported results from 3,654 women with ASDs, 3,654 healthy controls, 2,147 women with SLE, and 889 women with RA.
The three most common ASDs were vitiligo (30%), alopecia areata (30%), and cutaneous lupus erythematosus (27%). Compared with healthy controls, patients with ASDs were more likely to have spontaneous abortions (OR=1.5 [1.4-1.7], P<.001), and preeclampsia/eclampsia (OR=1.2 [1.0-1.3], P=.04). Compared with women with SLE, women with ASDs were less likely to have preeclampsia/eclampsia (OR=0.7 [0.6-0.9, P=.001); preterm birth (OR= 0.5 [0.4-0.7], P<.001); PPROM (OR=0.6 [0.4-0.9], P=.004), or an infant with IUGR (OR=0.6 [0.5-0.8], P<.001), but they were more likely to have a spontaneous abortion (OR=1.2 [1.1-1.3], P=.003). Overall, patients with ASDs had similar risks for adverse pregnancy outcomes as patients with RA.
“We found that patients with cutaneous lupus and vitiligo had higher rates of spontaneous abortion, which is interesting because we didn’t expect that,” Ms. Keum told this news organization. “Studies have shown that vitiligo patients might have an increased risk of pregnancy loss, so I think it’s important to have that discussion with those patients. It might benefit them to talk to a maternal-fetal medicine specialist. As for next steps, we want to look at how medication use and disease flare or disease severity play a role in APOs.”
In their poster, the researchers acknowledged limitations of the study, including the inability to verify diagnoses or assess disease severity. Also, while medication use and concomitant antiphospholipid syndrome were evaluated as risk factors for advanced pregnancy outcomes, the number of patients per group was too small for analysis.
Karl Saardi, MD, director of the inpatient dermatology service at George Washington University Hospital, Washington, who was asked to comment on the study, said that in his view, the choice of disease states included in the analysis “is a bit arbitrary.” He added that “it would have been more helpful to compare controls versus discoid lupus versus systemic lupus or controls versus amyopathic dermatomyositis versus dermatomyositis with myopathy.”
The study received funding support from the Rheumatology Research Foundation and the UT Southwestern Dean’s Research Scholar program. Neither Ms. Keum nor Dr. Saardi reported having relevant disclosures.
SAN DIEGO — , results from a large case-control study suggest.
Patients with systemic autoimmune conditions are known to have an increased risk for adverse pregnancy outcomes, “but we weren’t sure if that was the case for patients with autoimmune skin conditions,” presenting study author Heejo Keum, a fourth-year medical student at the University of Texas Southwestern Medical Center, Dallas, said in an interview during a poster session at the American College of Rheumatology (ACR) 2023 annual meeting. “There are case reports or nationwide population-based studies on patients with alopecia areata and vitiligo, but those were outside of the US, so we wanted to see if these outcomes could be studied in a larger population-based study in the US.”
Drawing from the TriNetX US Collaborative Network, a database of electronic medical records of 94 million patients in the United States, the researchers identified pregnant patients aged 15-44 years between January 1, 2016, and December 31, 2021. Cases were defined as patients diagnosed with at least one autoimmune skin disease (ASD) prior to the end of pregnancy, including alopecia areata, bullous pemphigoid, cicatricial pemphigoid, dermatitis herpetiformis, cutaneous lupus erythematosus, epidermolysis bullosa acquisita, morphea, pemphigus foliaceus, pemphigus vulgaris, vitiligo, and amyopathic DM. There were two control groups: healthy controls (those without ASDs, systemic lupus erythematosus or rheumatoid arthritis) and disease controls (those with SLE or RA). The researchers used ICD-10 codes to identify pregnancy endpoints, including live births, spontaneous abortion, and stillbirth. Patients with a history of hidradenitis suppurative were excluded from the analysis, as were those with common autoimmune disease such as Hashimoto’s thyroiditis, Grave’s disease, and type 1 diabetes.
The primary outcomes were adverse pregnancy outcomes defined as spontaneous abortion, gestational hypertension, preeclampsia/eclampsia, gestational diabetes, intrauterine growth restriction (IUGR), preterm premature rupture of membranes (PPROM), and preterm birth. The researchers used 1:1 propensity scoring to match patients with ASDs to controls by age, race, ethnicity, comorbidities, obesity, and substance use, and used odds ratio (OR) analysis with a 95% confidence interval (CI) to calculate each outcome.
Ms. Keum reported results from 3,654 women with ASDs, 3,654 healthy controls, 2,147 women with SLE, and 889 women with RA.
The three most common ASDs were vitiligo (30%), alopecia areata (30%), and cutaneous lupus erythematosus (27%). Compared with healthy controls, patients with ASDs were more likely to have spontaneous abortions (OR=1.5 [1.4-1.7], P<.001), and preeclampsia/eclampsia (OR=1.2 [1.0-1.3], P=.04). Compared with women with SLE, women with ASDs were less likely to have preeclampsia/eclampsia (OR=0.7 [0.6-0.9, P=.001); preterm birth (OR= 0.5 [0.4-0.7], P<.001); PPROM (OR=0.6 [0.4-0.9], P=.004), or an infant with IUGR (OR=0.6 [0.5-0.8], P<.001), but they were more likely to have a spontaneous abortion (OR=1.2 [1.1-1.3], P=.003). Overall, patients with ASDs had similar risks for adverse pregnancy outcomes as patients with RA.
“We found that patients with cutaneous lupus and vitiligo had higher rates of spontaneous abortion, which is interesting because we didn’t expect that,” Ms. Keum told this news organization. “Studies have shown that vitiligo patients might have an increased risk of pregnancy loss, so I think it’s important to have that discussion with those patients. It might benefit them to talk to a maternal-fetal medicine specialist. As for next steps, we want to look at how medication use and disease flare or disease severity play a role in APOs.”
In their poster, the researchers acknowledged limitations of the study, including the inability to verify diagnoses or assess disease severity. Also, while medication use and concomitant antiphospholipid syndrome were evaluated as risk factors for advanced pregnancy outcomes, the number of patients per group was too small for analysis.
Karl Saardi, MD, director of the inpatient dermatology service at George Washington University Hospital, Washington, who was asked to comment on the study, said that in his view, the choice of disease states included in the analysis “is a bit arbitrary.” He added that “it would have been more helpful to compare controls versus discoid lupus versus systemic lupus or controls versus amyopathic dermatomyositis versus dermatomyositis with myopathy.”
The study received funding support from the Rheumatology Research Foundation and the UT Southwestern Dean’s Research Scholar program. Neither Ms. Keum nor Dr. Saardi reported having relevant disclosures.
SAN DIEGO — , results from a large case-control study suggest.
Patients with systemic autoimmune conditions are known to have an increased risk for adverse pregnancy outcomes, “but we weren’t sure if that was the case for patients with autoimmune skin conditions,” presenting study author Heejo Keum, a fourth-year medical student at the University of Texas Southwestern Medical Center, Dallas, said in an interview during a poster session at the American College of Rheumatology (ACR) 2023 annual meeting. “There are case reports or nationwide population-based studies on patients with alopecia areata and vitiligo, but those were outside of the US, so we wanted to see if these outcomes could be studied in a larger population-based study in the US.”
Drawing from the TriNetX US Collaborative Network, a database of electronic medical records of 94 million patients in the United States, the researchers identified pregnant patients aged 15-44 years between January 1, 2016, and December 31, 2021. Cases were defined as patients diagnosed with at least one autoimmune skin disease (ASD) prior to the end of pregnancy, including alopecia areata, bullous pemphigoid, cicatricial pemphigoid, dermatitis herpetiformis, cutaneous lupus erythematosus, epidermolysis bullosa acquisita, morphea, pemphigus foliaceus, pemphigus vulgaris, vitiligo, and amyopathic DM. There were two control groups: healthy controls (those without ASDs, systemic lupus erythematosus or rheumatoid arthritis) and disease controls (those with SLE or RA). The researchers used ICD-10 codes to identify pregnancy endpoints, including live births, spontaneous abortion, and stillbirth. Patients with a history of hidradenitis suppurative were excluded from the analysis, as were those with common autoimmune disease such as Hashimoto’s thyroiditis, Grave’s disease, and type 1 diabetes.
The primary outcomes were adverse pregnancy outcomes defined as spontaneous abortion, gestational hypertension, preeclampsia/eclampsia, gestational diabetes, intrauterine growth restriction (IUGR), preterm premature rupture of membranes (PPROM), and preterm birth. The researchers used 1:1 propensity scoring to match patients with ASDs to controls by age, race, ethnicity, comorbidities, obesity, and substance use, and used odds ratio (OR) analysis with a 95% confidence interval (CI) to calculate each outcome.
Ms. Keum reported results from 3,654 women with ASDs, 3,654 healthy controls, 2,147 women with SLE, and 889 women with RA.
The three most common ASDs were vitiligo (30%), alopecia areata (30%), and cutaneous lupus erythematosus (27%). Compared with healthy controls, patients with ASDs were more likely to have spontaneous abortions (OR=1.5 [1.4-1.7], P<.001), and preeclampsia/eclampsia (OR=1.2 [1.0-1.3], P=.04). Compared with women with SLE, women with ASDs were less likely to have preeclampsia/eclampsia (OR=0.7 [0.6-0.9, P=.001); preterm birth (OR= 0.5 [0.4-0.7], P<.001); PPROM (OR=0.6 [0.4-0.9], P=.004), or an infant with IUGR (OR=0.6 [0.5-0.8], P<.001), but they were more likely to have a spontaneous abortion (OR=1.2 [1.1-1.3], P=.003). Overall, patients with ASDs had similar risks for adverse pregnancy outcomes as patients with RA.
“We found that patients with cutaneous lupus and vitiligo had higher rates of spontaneous abortion, which is interesting because we didn’t expect that,” Ms. Keum told this news organization. “Studies have shown that vitiligo patients might have an increased risk of pregnancy loss, so I think it’s important to have that discussion with those patients. It might benefit them to talk to a maternal-fetal medicine specialist. As for next steps, we want to look at how medication use and disease flare or disease severity play a role in APOs.”
In their poster, the researchers acknowledged limitations of the study, including the inability to verify diagnoses or assess disease severity. Also, while medication use and concomitant antiphospholipid syndrome were evaluated as risk factors for advanced pregnancy outcomes, the number of patients per group was too small for analysis.
Karl Saardi, MD, director of the inpatient dermatology service at George Washington University Hospital, Washington, who was asked to comment on the study, said that in his view, the choice of disease states included in the analysis “is a bit arbitrary.” He added that “it would have been more helpful to compare controls versus discoid lupus versus systemic lupus or controls versus amyopathic dermatomyositis versus dermatomyositis with myopathy.”
The study received funding support from the Rheumatology Research Foundation and the UT Southwestern Dean’s Research Scholar program. Neither Ms. Keum nor Dr. Saardi reported having relevant disclosures.
FROM ACR 2023
Rx for resilience: Five prescriptions for physician burnout
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Physician burnout persists even as the height of the COVID-19 crisis fades farther into the rear-view mirror. The causes for the sadness, stress, and frustration among doctors vary, but the effects are universal and often debilitating: exhaustion, emotional detachment, lethargy, feeling useless, and lacking purpose.
When surveyed, physicians pointed to many systemic solutions for burnout in Medscape’s Physician Burnout & Depression Report 2023, such as a need for greater compensation, more manageable workloads and schedules, and more support staff. But for many doctors, these fixes may be years if not decades away. Equally important are strategies for relieving burnout symptoms now, especially as we head into a busy holiday season.
Because not every stress-relief practice works for everyone, it’s crucial to try various methods until you find something that makes a difference for you, said Christine Gibson, MD, a family physician and trauma therapist in Calgary, Alta., and author of The Modern Trauma Toolkit.
“Every person should have a toolkit of the things that bring them out of the psychological and physical distress that dysregulates their nervous system,” said Dr. Gibson.
Once you learn the personal ways to alleviate your specific brand of burnout, you can start working on systemic changes that might help the culture of medicine overall.
Symptoms speak louder than words
It seems obvious, but if you aren’t aware that what you’re feeling is burnout, you probably aren’t going to find effective steps to relieve it. Jessi Gold, MD, assistant professor and director of wellness, engagement, and outreach in the department of psychiatry, Washington University in St. Louis, is a psychiatrist who treats health care professionals, including frontline workers during the height of the pandemic. But even as a burnout expert, she admits that she misses the signs in herself.
“I was fighting constant fatigue, falling asleep the minute I got home from work every day, but I thought a B12 shot would solve all my problems. I didn’t realize I was having symptoms of burnout until my own therapist told me,” said Dr. Gold. “As doctors, we spend so much time focusing on other people that we don’t necessarily notice very much in ourselves – usually once it starts to impact our job.”
Practices like meditation and mindfulness can help you delve into your feelings and emotions and notice how you’re doing. But you may also need to ask spouses, partners, and friends and family – or better yet, a mental health professional – if they notice that you seem burnt out.
Practice ‘in the moment’ relief
Sometimes, walking away at the moment of stress helps like when stepping away from a heated argument. “Step out of a frustrating staff meeting to go to the bathroom and splash your face,” said Eran Magan, PhD, a psychologist at the University of Pennsylvania, Philadelphia, and founder and CEO of the suicide prevention system EarlyAlert.me. “Tell a patient you need to check something in the next room, so you have time to take a breath.”
Dr. Magan recommended finding techniques that help lower acute stress while it’s actually happening. First, find a way to escape or excuse yourself from the event, and when possible, stop situations that are actively upsetting or triggering in their tracks.
Next, recharge by doing something that helps you feel better, like looking at a cute video of your child or grandchild or closing your eyes and taking a deep breath. You can also try to “catch” good feelings from someone else, said Dr. Magan. Ask someone about a trip, vacation, holiday, or pleasant event. “Ask a colleague about something that makes [them] happy,” he said. “Happiness can be infectious too.”
Burnout is also in the body
“Body psychotherapy” or somatic therapy is a treatment that focuses on how emotions appear within your body. Dr. Gibson said it’s a valuable tool for addressing trauma and a mainstay in many a medical career; it’s useful to help physicians learn to “befriend” their nervous system.
Somatic therapy exercises involve things like body scanning, scanning for physical sensations; conscious breathing, connecting to each inhale and exhale; grounding your weight by releasing tension through your feet, doing a total body stretch; or releasing shoulder and neck tension by consciously relaxing each of these muscle groups.
“We spend our whole day in sympathetic tone; our amygdala’s are firing, telling us that we’re in danger,” said Dr. Gibson. “We actually have to practice getting into and spending time in our parasympathetic nervous system to restore the balance in our autonomic nervous system.”
Somatic therapy includes a wide array of exercises that help reconnect you to your body through calming or activation. The movements release tension, ground you, and restore balance.
Bite-sized tools for well-being
Because of the prevalence of physician burnout, there’s been a groundswell of researchers and organizations who have turned their focus toward improving the well-being in the health care workforce.
One such effort comes from the Duke Center for the Advancement of Well-being Science, which “camouflages” well-being tools as continuing education credits to make them accessible for busy, stressed, and overworked physicians.
“They’re called bite-sized tools for well-being, and they have actual evidence behind them,” said Dr. Gold. For example, she said, one tools is a text program called Three Good Things that encourages physicians to send a text listing three positive things that happened during the day. The exercise lasts 15 days, and texters have access to others’ answers as well. After 3 months, participants’ baseline depression, gratitude, and life satisfaction had all “significantly improved.”
“It feels almost ridiculous that that could work, but it does,” said Dr. Gold. “I’ve had patients push back and say: ‘Well, isn’t that toxic positivity?’ But really what it is is dialectics. It’s not saying there’s only positive; it’s just making you realize there is more than just the negative.”
These and other short interventions focus on concepts such as joy, humor, awe, engagement, and self-kindness to build resilience and help physicians recover from burnout symptoms.
Cognitive restructuring could work
Cognitive restructuring is a therapeutic process of learning new ways of interpreting and responding to people and situations. It helps you change the “filter” through which you interact with your environment. Dr. Gibson said it’s a tool to use with care after other modes of therapy that help you understand your patterns and how they developed because of how you view and understand the world.
“The message of [cognitive-behavioral therapy] or cognitive restructuring is there’s something wrong with the way you’re thinking, and we need to change it or fix it, but in a traumatic system [like health care], you’re thinking has been an adaptive process related to the harm in the environment you’re in,” said Dr. Gibson.
“So, if you [jump straight to cognitive restructuring before other types of therapy], then we just gaslight ourselves into believing that there’s something wrong with us, that we haven’t adapted sufficiently to an environment that’s actually harmful.”
Strive for a few systemic changes
Systemic changes can be small ones within your own sphere. For example, Dr. Magan said, work toward making little tweaks to the flow of your day that will increase calm and reduce frustration.
“Make a ‘bug list,’ little, regular demands that drain your energy, and discuss them with your colleagues and supervisors to see if they can be improved,” he said. Examples include everyday frustrations like having unsolicited visitors popping into your office, scheduling complex patients too late in the day, or having a computer freeze whenever you access patient charts.
Though not always financially feasible, affecting real change and finding relief from all these insidious bugs can improve your mental health and burnout symptoms.
“Physicians tend to work extremely hard in order to keep holding together a system that is often not inherently sustainable, like the fascia of a body under tremendous strain,” said Dr. Magan. “Sometimes the brave thing to do is to refuse to continue being the lynchpin and let things break, so the system will have to start improving itself, rather than demanding more and more of the people in it.”
A version of this article first appeared on Medscape.com.
Isotretinoin users do not have higher suicide risk: meta-analysis
.
Instead, those who are treated with the drug for severe acne may have a lower risk of suicide attempts 2-4 years after treatment, wrote the authors, led by Nicole Kye Wen Tan, MBBS, of Yong Loo Lin School of Medicine at the National University of Singapore. The results were published online in JAMA Dermatology.
The analysis showed that the 1-year absolute risk from between two and eight studies of suicide attempts, suicidal ideation, completed suicides, and self-harm were each less than 0.5%. For comparison, the absolute risk of depression was 3.83% (95% confidence interval [CI], 2.45-5.93; I2 [measuring heterogeneity] = 77%) in 11 studies.
Less likely to attempt suicide
Isotretinoin users were less likely than were nonusers to attempt suicide at 2 years (relative risk [RR], 0.92; 95% CI, 0.84-1.00; I2 = 0%); 3 years (RR, 0.86; 95% CI, 0.77-0.95; I2 = 0%); and 4 years (RR, 0.85; 95% CI, 0.72-1.00; I2 = 23%) following treatment.
Additionally, isotretinoin was not linked with the risk of “all psychiatric disorders” (RR, 1.08; 95% CI, 0.99-1.19; I2 = 0%).
Among the study limitations, the authors noted that because of the widespread claims that isotretinoin can affect mental health, it is plausible that patients at high risk of psychiatric illness were less likely to be treated with isotretinoin in the first place, which could have resulted in underestimating psychiatric risks in the observational studies.
“Two things can be true”
John S. Barbieri, MD, MBA, assistant professor at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at the Brigham and Women’s Hospital in Boston, who was not involved with this research, said the study helps confirm what he and many others have long thought.
The results of the meta-analysis show that “two things can be true, which often gets lost with isotretinoin,” he said. At a population level, isotretinoin improves mental health but on the individual level, it may cause rare side effects that harm mental health, he added.
In making decisions on the use of isotretinoin, he continued, “we should feel reassured that the likely outcome is improved mental health compared to other alternatives that we have, but at the same time we should be vigilant about monitoring a patient’s mental health while they are being treated with isotretinoin.”
He said that this topic draws extreme views on social media, with people who want the drug off the market and those who discount concerns altogether.
“I think the real answer is a little more in the middle,” he said. “We still have to be thoughtful when we use it.”
Because outcomes such as suicide in patients on isotretinoin are not common, Dr. Barbieri said, smaller studies individually have lacked precision on effect. The size of this meta-analysis helps add confidence in the results, he said.
In addition, this study can help clinicians point to numbers when they talk with their patients about benefits and risks, he said.
What a meta-analysis might miss
In an accompanying editorial, Parker Magin, PhD, of the School of Medicine and Public Health, University of Newcastle, Callaghan, New South Wales, Australia, and Shaun Prentice, PhD, of the School of Psychology, Faculty of Health and Medical Sciences at the University of Adelaide, South Australia, wrote that though the work by Tan et al. is “broadly reassuring,” they have concerns about the patients a meta-analysis might miss.
They wrote that other studies have shown evidence both of biological plausibility that isotretinoin may be linked with psychiatric effects and that it may cause these side effects. “One could conclude that it is plausible that isotretinoin has markedly adverse, idiosyncratic psychiatric effects in a small minority of individual patients,” they wrote. “It is also plausible that these presumably rare occurrences are not detectable in studies where the majority of patients experience no adverse psychiatric outcomes or even positive outcomes.”
Far from the “final word”
Dr. Magin and Dr. Prentice pointed out that while the study adds to the literature on his topic, the relationship between acne, psychiatric conditions, and isotretinoin is complex and thus these findings “are far from the final word.”
Randomized, controlled trials have limited use in this area and observational studies are always susceptible to bias, they noted. “Clinicians, though, can take some degree of further reassurance from this extension of the literature around the psychiatric sequelae of isotretinoin,” they wrote.
Senior author Hazel Oon, MD, of the National Skin Centre, Singapore, disclosed ties with AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly, Galderma, Janssen, LEO Pharma, Novartis, and Pfizer. No other author disclosures were reported. Dr. Barbieri is an associate editor at JAMA Dermatology and is cochair of the American Academy of Dermatology Acne Guidelines Work Group.
.
Instead, those who are treated with the drug for severe acne may have a lower risk of suicide attempts 2-4 years after treatment, wrote the authors, led by Nicole Kye Wen Tan, MBBS, of Yong Loo Lin School of Medicine at the National University of Singapore. The results were published online in JAMA Dermatology.
The analysis showed that the 1-year absolute risk from between two and eight studies of suicide attempts, suicidal ideation, completed suicides, and self-harm were each less than 0.5%. For comparison, the absolute risk of depression was 3.83% (95% confidence interval [CI], 2.45-5.93; I2 [measuring heterogeneity] = 77%) in 11 studies.
Less likely to attempt suicide
Isotretinoin users were less likely than were nonusers to attempt suicide at 2 years (relative risk [RR], 0.92; 95% CI, 0.84-1.00; I2 = 0%); 3 years (RR, 0.86; 95% CI, 0.77-0.95; I2 = 0%); and 4 years (RR, 0.85; 95% CI, 0.72-1.00; I2 = 23%) following treatment.
Additionally, isotretinoin was not linked with the risk of “all psychiatric disorders” (RR, 1.08; 95% CI, 0.99-1.19; I2 = 0%).
Among the study limitations, the authors noted that because of the widespread claims that isotretinoin can affect mental health, it is plausible that patients at high risk of psychiatric illness were less likely to be treated with isotretinoin in the first place, which could have resulted in underestimating psychiatric risks in the observational studies.
“Two things can be true”
John S. Barbieri, MD, MBA, assistant professor at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at the Brigham and Women’s Hospital in Boston, who was not involved with this research, said the study helps confirm what he and many others have long thought.
The results of the meta-analysis show that “two things can be true, which often gets lost with isotretinoin,” he said. At a population level, isotretinoin improves mental health but on the individual level, it may cause rare side effects that harm mental health, he added.
In making decisions on the use of isotretinoin, he continued, “we should feel reassured that the likely outcome is improved mental health compared to other alternatives that we have, but at the same time we should be vigilant about monitoring a patient’s mental health while they are being treated with isotretinoin.”
He said that this topic draws extreme views on social media, with people who want the drug off the market and those who discount concerns altogether.
“I think the real answer is a little more in the middle,” he said. “We still have to be thoughtful when we use it.”
Because outcomes such as suicide in patients on isotretinoin are not common, Dr. Barbieri said, smaller studies individually have lacked precision on effect. The size of this meta-analysis helps add confidence in the results, he said.
In addition, this study can help clinicians point to numbers when they talk with their patients about benefits and risks, he said.
What a meta-analysis might miss
In an accompanying editorial, Parker Magin, PhD, of the School of Medicine and Public Health, University of Newcastle, Callaghan, New South Wales, Australia, and Shaun Prentice, PhD, of the School of Psychology, Faculty of Health and Medical Sciences at the University of Adelaide, South Australia, wrote that though the work by Tan et al. is “broadly reassuring,” they have concerns about the patients a meta-analysis might miss.
They wrote that other studies have shown evidence both of biological plausibility that isotretinoin may be linked with psychiatric effects and that it may cause these side effects. “One could conclude that it is plausible that isotretinoin has markedly adverse, idiosyncratic psychiatric effects in a small minority of individual patients,” they wrote. “It is also plausible that these presumably rare occurrences are not detectable in studies where the majority of patients experience no adverse psychiatric outcomes or even positive outcomes.”
Far from the “final word”
Dr. Magin and Dr. Prentice pointed out that while the study adds to the literature on his topic, the relationship between acne, psychiatric conditions, and isotretinoin is complex and thus these findings “are far from the final word.”
Randomized, controlled trials have limited use in this area and observational studies are always susceptible to bias, they noted. “Clinicians, though, can take some degree of further reassurance from this extension of the literature around the psychiatric sequelae of isotretinoin,” they wrote.
Senior author Hazel Oon, MD, of the National Skin Centre, Singapore, disclosed ties with AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly, Galderma, Janssen, LEO Pharma, Novartis, and Pfizer. No other author disclosures were reported. Dr. Barbieri is an associate editor at JAMA Dermatology and is cochair of the American Academy of Dermatology Acne Guidelines Work Group.
.
Instead, those who are treated with the drug for severe acne may have a lower risk of suicide attempts 2-4 years after treatment, wrote the authors, led by Nicole Kye Wen Tan, MBBS, of Yong Loo Lin School of Medicine at the National University of Singapore. The results were published online in JAMA Dermatology.
The analysis showed that the 1-year absolute risk from between two and eight studies of suicide attempts, suicidal ideation, completed suicides, and self-harm were each less than 0.5%. For comparison, the absolute risk of depression was 3.83% (95% confidence interval [CI], 2.45-5.93; I2 [measuring heterogeneity] = 77%) in 11 studies.
Less likely to attempt suicide
Isotretinoin users were less likely than were nonusers to attempt suicide at 2 years (relative risk [RR], 0.92; 95% CI, 0.84-1.00; I2 = 0%); 3 years (RR, 0.86; 95% CI, 0.77-0.95; I2 = 0%); and 4 years (RR, 0.85; 95% CI, 0.72-1.00; I2 = 23%) following treatment.
Additionally, isotretinoin was not linked with the risk of “all psychiatric disorders” (RR, 1.08; 95% CI, 0.99-1.19; I2 = 0%).
Among the study limitations, the authors noted that because of the widespread claims that isotretinoin can affect mental health, it is plausible that patients at high risk of psychiatric illness were less likely to be treated with isotretinoin in the first place, which could have resulted in underestimating psychiatric risks in the observational studies.
“Two things can be true”
John S. Barbieri, MD, MBA, assistant professor at Harvard Medical School and director of the Advanced Acne Therapeutics Clinic at the Brigham and Women’s Hospital in Boston, who was not involved with this research, said the study helps confirm what he and many others have long thought.
The results of the meta-analysis show that “two things can be true, which often gets lost with isotretinoin,” he said. At a population level, isotretinoin improves mental health but on the individual level, it may cause rare side effects that harm mental health, he added.
In making decisions on the use of isotretinoin, he continued, “we should feel reassured that the likely outcome is improved mental health compared to other alternatives that we have, but at the same time we should be vigilant about monitoring a patient’s mental health while they are being treated with isotretinoin.”
He said that this topic draws extreme views on social media, with people who want the drug off the market and those who discount concerns altogether.
“I think the real answer is a little more in the middle,” he said. “We still have to be thoughtful when we use it.”
Because outcomes such as suicide in patients on isotretinoin are not common, Dr. Barbieri said, smaller studies individually have lacked precision on effect. The size of this meta-analysis helps add confidence in the results, he said.
In addition, this study can help clinicians point to numbers when they talk with their patients about benefits and risks, he said.
What a meta-analysis might miss
In an accompanying editorial, Parker Magin, PhD, of the School of Medicine and Public Health, University of Newcastle, Callaghan, New South Wales, Australia, and Shaun Prentice, PhD, of the School of Psychology, Faculty of Health and Medical Sciences at the University of Adelaide, South Australia, wrote that though the work by Tan et al. is “broadly reassuring,” they have concerns about the patients a meta-analysis might miss.
They wrote that other studies have shown evidence both of biological plausibility that isotretinoin may be linked with psychiatric effects and that it may cause these side effects. “One could conclude that it is plausible that isotretinoin has markedly adverse, idiosyncratic psychiatric effects in a small minority of individual patients,” they wrote. “It is also plausible that these presumably rare occurrences are not detectable in studies where the majority of patients experience no adverse psychiatric outcomes or even positive outcomes.”
Far from the “final word”
Dr. Magin and Dr. Prentice pointed out that while the study adds to the literature on his topic, the relationship between acne, psychiatric conditions, and isotretinoin is complex and thus these findings “are far from the final word.”
Randomized, controlled trials have limited use in this area and observational studies are always susceptible to bias, they noted. “Clinicians, though, can take some degree of further reassurance from this extension of the literature around the psychiatric sequelae of isotretinoin,” they wrote.
Senior author Hazel Oon, MD, of the National Skin Centre, Singapore, disclosed ties with AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly, Galderma, Janssen, LEO Pharma, Novartis, and Pfizer. No other author disclosures were reported. Dr. Barbieri is an associate editor at JAMA Dermatology and is cochair of the American Academy of Dermatology Acne Guidelines Work Group.
FROM JAMA DERMATOLOGY
Dietary supplements may play a role in managing vitiligo
, Ammar Ahmed, MD, associate professor of dermatology at Dell Medical School at the University of Texas, Austin, said at the annual Integrative Dermatology Symposium.
Data on the use of dietary supplements for vitiligo are scarce and of limited quality, but existing studies and current understanding of the pathogenesis of vitiligo have convinced Dr. Ahmed to recommend oral Ginkgo biloba, vitamin C, vitamin E, and alpha-lipoic acid – as well as vitamin D if levels are insufficient – for patients receiving phototherapy, and outside of phototherapy when patients express interest, he said.
Melanocyte stress and subsequent autoimmune destruction appear to be “key pathways at play in vitiligo,” with melanocytes exhibiting increased susceptibility to physiologic stress, including a reduced capacity to manage exposure to reactive oxygen species. “It’s more theory than proven science, but if oxidative damage is one of the key factors [affecting] melanocytes, can we ... reverse the damage to those melanocytes with antioxidants?” he said. “I don’t know, but there’s certainly some emerging evidence that we may.”
There are no human data on the effectiveness of an antioxidant-rich diet for vitiligo, but given its theoretical basis of efficacy, it “seems reasonable to recommend,” said Dr. Ahmed. “When my patients ask me, I tell them to eat a colorful diet – with a lot of colorful fruits and vegetables.” In addition, he said, “we know that individuals with vitiligo, just as patients with psoriasis and other inflammatory disorders, appear to have a higher risk for insulin resistance and metabolic syndrome, even after accounting for confounders,” making a healthy diet all the more important.
Two case reports have described improvement with a gluten-free diet, but “that’s it,” he said. “My take is, unless stronger evidence exists, let your patients enjoy their bread.” No other specific diet has been shown to cause, exacerbate, or improve vitiligo, he noted.
Dr. Ahmed offered his views on the literature on this topic, highlighting studies that have caught his eye on antioxidants and other supplements in patients with vitiligo:
Vitamins C and E, and alpha-lipoic acid: In a randomized controlled trial of 35 patients with nonsegmental vitiligo conducted at the San Gallicano Dermatological Institute in Rome, those who received an antioxidant cocktail (alpha-lipoic acid, 100 mg; vitamin C, 100 mg; vitamin E, 40 mg; and polyunsaturated fatty acids) for 2 months before and during narrow-band ultraviolet-B (NB-UVB) therapy had significantly more repigmentation than that of patients who received NB-UVB alone. Forty-seven percent of those in the antioxidant group obtained greater than 75% repigmentation at 6 months vs. 18% in the control arm.
“This is a pretty high-quality trial. They even did in-vitro analysis showing that the antioxidant group had decreased measures of oxidative stress in the melanocytes,” Dr. Ahmed said. A handout he provided to patients receiving UVB therapy includes recommendations for vitamin C, vitamin E, and alpha-lipoic acid supplementation.
Another controlled prospective study of 130 patients with vitiligo, also conducted in Italy, utilized a different antioxidant cocktail in a tablet – Phyllanthus emblica (known as Indian gooseberry), vitamin E, and carotenoids – taken three times a day, in conjunction with standard topical therapy and phototherapy. At 6 months, a significantly higher number of patients receiving the cocktail had mild repigmentation and were less likely to have no repigmentation compared with patients who did not receive the antioxidants. “Nobody did really great, but the cocktail group did a little better,” he said. “So there’s promise.”
Vitamin D: In-vitro studies show that vitamin D may protect melanocytes against oxidative stress, and two small controlled trials showed improvement in vitiligo with vitamin D supplementation (1,500-5,000 IU daily) and no NB-UVB therapy. However, a recent, higher-quality 6-month trial that evaluated 5,000 IU/day of vitamin D in patients with generalized vitiligo showed no advantage over NB-UVB therapy alone. “I tell patients, if you’re insufficient, take vitamin D (supplements) to get your levels up,” Dr. Ahmed sad. “But if you’re already sufficient, I’m not confident there will be a significant benefit.”
Ginkgo biloba: A small double-blind controlled trial randomized 47 patients with limited and slow-spreading vitiligo to receive Ginkgo biloba extract 40 mg three times a day or placebo. At 6 months, 10 patients who received the extract had greater than 75% repigmentation compared with 2 patients in the placebo group. Patients receiving Ginkgo biloba, which has immunomodulatory and antioxidant properties, were also significantly more likely to have disease stabilization.
“I tend to recommend it to patients not doing phototherapy, as well as those receiving phototherapy, especially since the study showed benefit as a monotherapy,” Dr. Ahmed said in an interview after the meeting.
Phenylalanine: Various oral and/or topical formulations of this amino acid and precursor to tyrosine/melanin have been shown to have repigmentation effects when combined with UVA phototherapy or sunlight, but the studies are of limited quality and the oral dosages studied (50 mg/kg per day to 100 mg/kg per day) appear to be a bit high, Dr. Ahmed said at the meeting. “It can add up in cost, and I worry a little about side effects, so I don’t recommend it as much.”
Polypodium leucotomos (PL): This plant extract, from a fern native to Central America and parts of South America, is familiar as a photoprotective supplement, he said, and a few randomized controlled trials show that it may improve repigmentation outcomes, especially on the hands and neck, when combined with NB-UVB in patients with vitiligo.
One of these trials, published in 2021, showed greater than 50% repigmentation at 6 months in 48% of patients with generalized vitiligo who received oral PL (480 mg twice a day) and NB-UVB, versus 22% in patients receiving NB-UVB alone. PL may be “reasonable to consider, though it can get a little pricey,” he said.
Other supplements: Nigella sativa seed oil (black seed oil) and the Ayurvedic herb Picrorhiza kurroa (also known as kutki), have shown some promise and merit further study in vitiligo, Dr. Ahmed said. Data on vitamin B12 and folate are mixed, and there is no evidence of a helpful role of zinc for vitiligo, he noted at the meeting.
Overall, there is a “paucity of large, high-quality trials for [complementary] therapies for vitiligo,” Dr. Ahmed said. “We need big randomized controlled trials ... and we need stratification. The problem is a lot of these studies don’t stratify: Is the patient active or inactive, for instance? Do they have poliosis or not?” Also missing in many studies are data on safety and adverse events. “Is that because of an excellent safety profile or lack of scientific rigor? I don’t know.”
Future approaches to vitiligo management will likely integrate alternative/nutritional modalities with conventional medical treatments, newer targeted therapies, and surgery when necessary, he said. In the case of surgery, he referred to the June 2023 Food and Drug Administration approval of the RECELL Autologous Cell Harvesting Device for repigmentation of stable depigmented vitiligo lesions, an office-based grafting procedure.
The topical Janus kinase (JAK) inhibitor ruxolitinib (Opzelura) approved in 2022 for nonsegmental vitiligo, he said, produced “good, not great” results in two pivotal phase 3 trials . At 24 weeks, about 30% of patients on the treatment achieved at least a 75% improvement in the facial Vitiligo Area Scoring Index (F-VASI75), compared with about 10% of patients in the placebo groups.
Asked to comment on antioxidant pathways and the potential of complementary therapies for vitiligo, Jason Hawkes, MD, a dermatologist in Rocklin, Calif., who also spoke at the IDS meeting, said that oxidative stress is among the processes that may contribute to melanocyte degeneration seen in vitiligo.
The immunopathogenesis of vitiligo is “multilayered and complex,” he said. “While the T lymphocyte plays a central role in this disease, there are other genetic and biologic processes [including oxidative stress] that also contribute to the destruction of melanocytes.”
Reducing oxidative stress in the body and skin via supplements such as vitamin E, coenzyme Q10, and alpha-lipoic acid “may represent complementary treatments used for the treatment of vitiligo,” said Dr. Hawkes. And as more is learned about the pathogenic role of oxidative stress and its impact on diseases of pigmentation, “therapeutic targeting of the antioxidation-related signaling pathways in the skin may represent a novel treatment for vitiligo or other related conditions.”
Dr. Hawkes disclosed ties with AbbVie, Arcutis, Bristol-Myers Squibb, Boehringer Ingelheim, Janssen, LEO, Lilly, Novartis, Pfizer, Regeneron, Sanofi, Sun Pharma, and UCB. Dr. Hawkes disclosed serving as an investigator and advisory board member for Avita and an investigator for Pfizer.
, Ammar Ahmed, MD, associate professor of dermatology at Dell Medical School at the University of Texas, Austin, said at the annual Integrative Dermatology Symposium.
Data on the use of dietary supplements for vitiligo are scarce and of limited quality, but existing studies and current understanding of the pathogenesis of vitiligo have convinced Dr. Ahmed to recommend oral Ginkgo biloba, vitamin C, vitamin E, and alpha-lipoic acid – as well as vitamin D if levels are insufficient – for patients receiving phototherapy, and outside of phototherapy when patients express interest, he said.
Melanocyte stress and subsequent autoimmune destruction appear to be “key pathways at play in vitiligo,” with melanocytes exhibiting increased susceptibility to physiologic stress, including a reduced capacity to manage exposure to reactive oxygen species. “It’s more theory than proven science, but if oxidative damage is one of the key factors [affecting] melanocytes, can we ... reverse the damage to those melanocytes with antioxidants?” he said. “I don’t know, but there’s certainly some emerging evidence that we may.”
There are no human data on the effectiveness of an antioxidant-rich diet for vitiligo, but given its theoretical basis of efficacy, it “seems reasonable to recommend,” said Dr. Ahmed. “When my patients ask me, I tell them to eat a colorful diet – with a lot of colorful fruits and vegetables.” In addition, he said, “we know that individuals with vitiligo, just as patients with psoriasis and other inflammatory disorders, appear to have a higher risk for insulin resistance and metabolic syndrome, even after accounting for confounders,” making a healthy diet all the more important.
Two case reports have described improvement with a gluten-free diet, but “that’s it,” he said. “My take is, unless stronger evidence exists, let your patients enjoy their bread.” No other specific diet has been shown to cause, exacerbate, or improve vitiligo, he noted.
Dr. Ahmed offered his views on the literature on this topic, highlighting studies that have caught his eye on antioxidants and other supplements in patients with vitiligo:
Vitamins C and E, and alpha-lipoic acid: In a randomized controlled trial of 35 patients with nonsegmental vitiligo conducted at the San Gallicano Dermatological Institute in Rome, those who received an antioxidant cocktail (alpha-lipoic acid, 100 mg; vitamin C, 100 mg; vitamin E, 40 mg; and polyunsaturated fatty acids) for 2 months before and during narrow-band ultraviolet-B (NB-UVB) therapy had significantly more repigmentation than that of patients who received NB-UVB alone. Forty-seven percent of those in the antioxidant group obtained greater than 75% repigmentation at 6 months vs. 18% in the control arm.
“This is a pretty high-quality trial. They even did in-vitro analysis showing that the antioxidant group had decreased measures of oxidative stress in the melanocytes,” Dr. Ahmed said. A handout he provided to patients receiving UVB therapy includes recommendations for vitamin C, vitamin E, and alpha-lipoic acid supplementation.
Another controlled prospective study of 130 patients with vitiligo, also conducted in Italy, utilized a different antioxidant cocktail in a tablet – Phyllanthus emblica (known as Indian gooseberry), vitamin E, and carotenoids – taken three times a day, in conjunction with standard topical therapy and phototherapy. At 6 months, a significantly higher number of patients receiving the cocktail had mild repigmentation and were less likely to have no repigmentation compared with patients who did not receive the antioxidants. “Nobody did really great, but the cocktail group did a little better,” he said. “So there’s promise.”
Vitamin D: In-vitro studies show that vitamin D may protect melanocytes against oxidative stress, and two small controlled trials showed improvement in vitiligo with vitamin D supplementation (1,500-5,000 IU daily) and no NB-UVB therapy. However, a recent, higher-quality 6-month trial that evaluated 5,000 IU/day of vitamin D in patients with generalized vitiligo showed no advantage over NB-UVB therapy alone. “I tell patients, if you’re insufficient, take vitamin D (supplements) to get your levels up,” Dr. Ahmed sad. “But if you’re already sufficient, I’m not confident there will be a significant benefit.”
Ginkgo biloba: A small double-blind controlled trial randomized 47 patients with limited and slow-spreading vitiligo to receive Ginkgo biloba extract 40 mg three times a day or placebo. At 6 months, 10 patients who received the extract had greater than 75% repigmentation compared with 2 patients in the placebo group. Patients receiving Ginkgo biloba, which has immunomodulatory and antioxidant properties, were also significantly more likely to have disease stabilization.
“I tend to recommend it to patients not doing phototherapy, as well as those receiving phototherapy, especially since the study showed benefit as a monotherapy,” Dr. Ahmed said in an interview after the meeting.
Phenylalanine: Various oral and/or topical formulations of this amino acid and precursor to tyrosine/melanin have been shown to have repigmentation effects when combined with UVA phototherapy or sunlight, but the studies are of limited quality and the oral dosages studied (50 mg/kg per day to 100 mg/kg per day) appear to be a bit high, Dr. Ahmed said at the meeting. “It can add up in cost, and I worry a little about side effects, so I don’t recommend it as much.”
Polypodium leucotomos (PL): This plant extract, from a fern native to Central America and parts of South America, is familiar as a photoprotective supplement, he said, and a few randomized controlled trials show that it may improve repigmentation outcomes, especially on the hands and neck, when combined with NB-UVB in patients with vitiligo.
One of these trials, published in 2021, showed greater than 50% repigmentation at 6 months in 48% of patients with generalized vitiligo who received oral PL (480 mg twice a day) and NB-UVB, versus 22% in patients receiving NB-UVB alone. PL may be “reasonable to consider, though it can get a little pricey,” he said.
Other supplements: Nigella sativa seed oil (black seed oil) and the Ayurvedic herb Picrorhiza kurroa (also known as kutki), have shown some promise and merit further study in vitiligo, Dr. Ahmed said. Data on vitamin B12 and folate are mixed, and there is no evidence of a helpful role of zinc for vitiligo, he noted at the meeting.
Overall, there is a “paucity of large, high-quality trials for [complementary] therapies for vitiligo,” Dr. Ahmed said. “We need big randomized controlled trials ... and we need stratification. The problem is a lot of these studies don’t stratify: Is the patient active or inactive, for instance? Do they have poliosis or not?” Also missing in many studies are data on safety and adverse events. “Is that because of an excellent safety profile or lack of scientific rigor? I don’t know.”
Future approaches to vitiligo management will likely integrate alternative/nutritional modalities with conventional medical treatments, newer targeted therapies, and surgery when necessary, he said. In the case of surgery, he referred to the June 2023 Food and Drug Administration approval of the RECELL Autologous Cell Harvesting Device for repigmentation of stable depigmented vitiligo lesions, an office-based grafting procedure.
The topical Janus kinase (JAK) inhibitor ruxolitinib (Opzelura) approved in 2022 for nonsegmental vitiligo, he said, produced “good, not great” results in two pivotal phase 3 trials . At 24 weeks, about 30% of patients on the treatment achieved at least a 75% improvement in the facial Vitiligo Area Scoring Index (F-VASI75), compared with about 10% of patients in the placebo groups.
Asked to comment on antioxidant pathways and the potential of complementary therapies for vitiligo, Jason Hawkes, MD, a dermatologist in Rocklin, Calif., who also spoke at the IDS meeting, said that oxidative stress is among the processes that may contribute to melanocyte degeneration seen in vitiligo.
The immunopathogenesis of vitiligo is “multilayered and complex,” he said. “While the T lymphocyte plays a central role in this disease, there are other genetic and biologic processes [including oxidative stress] that also contribute to the destruction of melanocytes.”
Reducing oxidative stress in the body and skin via supplements such as vitamin E, coenzyme Q10, and alpha-lipoic acid “may represent complementary treatments used for the treatment of vitiligo,” said Dr. Hawkes. And as more is learned about the pathogenic role of oxidative stress and its impact on diseases of pigmentation, “therapeutic targeting of the antioxidation-related signaling pathways in the skin may represent a novel treatment for vitiligo or other related conditions.”
Dr. Hawkes disclosed ties with AbbVie, Arcutis, Bristol-Myers Squibb, Boehringer Ingelheim, Janssen, LEO, Lilly, Novartis, Pfizer, Regeneron, Sanofi, Sun Pharma, and UCB. Dr. Hawkes disclosed serving as an investigator and advisory board member for Avita and an investigator for Pfizer.
, Ammar Ahmed, MD, associate professor of dermatology at Dell Medical School at the University of Texas, Austin, said at the annual Integrative Dermatology Symposium.
Data on the use of dietary supplements for vitiligo are scarce and of limited quality, but existing studies and current understanding of the pathogenesis of vitiligo have convinced Dr. Ahmed to recommend oral Ginkgo biloba, vitamin C, vitamin E, and alpha-lipoic acid – as well as vitamin D if levels are insufficient – for patients receiving phototherapy, and outside of phototherapy when patients express interest, he said.
Melanocyte stress and subsequent autoimmune destruction appear to be “key pathways at play in vitiligo,” with melanocytes exhibiting increased susceptibility to physiologic stress, including a reduced capacity to manage exposure to reactive oxygen species. “It’s more theory than proven science, but if oxidative damage is one of the key factors [affecting] melanocytes, can we ... reverse the damage to those melanocytes with antioxidants?” he said. “I don’t know, but there’s certainly some emerging evidence that we may.”
There are no human data on the effectiveness of an antioxidant-rich diet for vitiligo, but given its theoretical basis of efficacy, it “seems reasonable to recommend,” said Dr. Ahmed. “When my patients ask me, I tell them to eat a colorful diet – with a lot of colorful fruits and vegetables.” In addition, he said, “we know that individuals with vitiligo, just as patients with psoriasis and other inflammatory disorders, appear to have a higher risk for insulin resistance and metabolic syndrome, even after accounting for confounders,” making a healthy diet all the more important.
Two case reports have described improvement with a gluten-free diet, but “that’s it,” he said. “My take is, unless stronger evidence exists, let your patients enjoy their bread.” No other specific diet has been shown to cause, exacerbate, or improve vitiligo, he noted.
Dr. Ahmed offered his views on the literature on this topic, highlighting studies that have caught his eye on antioxidants and other supplements in patients with vitiligo:
Vitamins C and E, and alpha-lipoic acid: In a randomized controlled trial of 35 patients with nonsegmental vitiligo conducted at the San Gallicano Dermatological Institute in Rome, those who received an antioxidant cocktail (alpha-lipoic acid, 100 mg; vitamin C, 100 mg; vitamin E, 40 mg; and polyunsaturated fatty acids) for 2 months before and during narrow-band ultraviolet-B (NB-UVB) therapy had significantly more repigmentation than that of patients who received NB-UVB alone. Forty-seven percent of those in the antioxidant group obtained greater than 75% repigmentation at 6 months vs. 18% in the control arm.
“This is a pretty high-quality trial. They even did in-vitro analysis showing that the antioxidant group had decreased measures of oxidative stress in the melanocytes,” Dr. Ahmed said. A handout he provided to patients receiving UVB therapy includes recommendations for vitamin C, vitamin E, and alpha-lipoic acid supplementation.
Another controlled prospective study of 130 patients with vitiligo, also conducted in Italy, utilized a different antioxidant cocktail in a tablet – Phyllanthus emblica (known as Indian gooseberry), vitamin E, and carotenoids – taken three times a day, in conjunction with standard topical therapy and phototherapy. At 6 months, a significantly higher number of patients receiving the cocktail had mild repigmentation and were less likely to have no repigmentation compared with patients who did not receive the antioxidants. “Nobody did really great, but the cocktail group did a little better,” he said. “So there’s promise.”
Vitamin D: In-vitro studies show that vitamin D may protect melanocytes against oxidative stress, and two small controlled trials showed improvement in vitiligo with vitamin D supplementation (1,500-5,000 IU daily) and no NB-UVB therapy. However, a recent, higher-quality 6-month trial that evaluated 5,000 IU/day of vitamin D in patients with generalized vitiligo showed no advantage over NB-UVB therapy alone. “I tell patients, if you’re insufficient, take vitamin D (supplements) to get your levels up,” Dr. Ahmed sad. “But if you’re already sufficient, I’m not confident there will be a significant benefit.”
Ginkgo biloba: A small double-blind controlled trial randomized 47 patients with limited and slow-spreading vitiligo to receive Ginkgo biloba extract 40 mg three times a day or placebo. At 6 months, 10 patients who received the extract had greater than 75% repigmentation compared with 2 patients in the placebo group. Patients receiving Ginkgo biloba, which has immunomodulatory and antioxidant properties, were also significantly more likely to have disease stabilization.
“I tend to recommend it to patients not doing phototherapy, as well as those receiving phototherapy, especially since the study showed benefit as a monotherapy,” Dr. Ahmed said in an interview after the meeting.
Phenylalanine: Various oral and/or topical formulations of this amino acid and precursor to tyrosine/melanin have been shown to have repigmentation effects when combined with UVA phototherapy or sunlight, but the studies are of limited quality and the oral dosages studied (50 mg/kg per day to 100 mg/kg per day) appear to be a bit high, Dr. Ahmed said at the meeting. “It can add up in cost, and I worry a little about side effects, so I don’t recommend it as much.”
Polypodium leucotomos (PL): This plant extract, from a fern native to Central America and parts of South America, is familiar as a photoprotective supplement, he said, and a few randomized controlled trials show that it may improve repigmentation outcomes, especially on the hands and neck, when combined with NB-UVB in patients with vitiligo.
One of these trials, published in 2021, showed greater than 50% repigmentation at 6 months in 48% of patients with generalized vitiligo who received oral PL (480 mg twice a day) and NB-UVB, versus 22% in patients receiving NB-UVB alone. PL may be “reasonable to consider, though it can get a little pricey,” he said.
Other supplements: Nigella sativa seed oil (black seed oil) and the Ayurvedic herb Picrorhiza kurroa (also known as kutki), have shown some promise and merit further study in vitiligo, Dr. Ahmed said. Data on vitamin B12 and folate are mixed, and there is no evidence of a helpful role of zinc for vitiligo, he noted at the meeting.
Overall, there is a “paucity of large, high-quality trials for [complementary] therapies for vitiligo,” Dr. Ahmed said. “We need big randomized controlled trials ... and we need stratification. The problem is a lot of these studies don’t stratify: Is the patient active or inactive, for instance? Do they have poliosis or not?” Also missing in many studies are data on safety and adverse events. “Is that because of an excellent safety profile or lack of scientific rigor? I don’t know.”
Future approaches to vitiligo management will likely integrate alternative/nutritional modalities with conventional medical treatments, newer targeted therapies, and surgery when necessary, he said. In the case of surgery, he referred to the June 2023 Food and Drug Administration approval of the RECELL Autologous Cell Harvesting Device for repigmentation of stable depigmented vitiligo lesions, an office-based grafting procedure.
The topical Janus kinase (JAK) inhibitor ruxolitinib (Opzelura) approved in 2022 for nonsegmental vitiligo, he said, produced “good, not great” results in two pivotal phase 3 trials . At 24 weeks, about 30% of patients on the treatment achieved at least a 75% improvement in the facial Vitiligo Area Scoring Index (F-VASI75), compared with about 10% of patients in the placebo groups.
Asked to comment on antioxidant pathways and the potential of complementary therapies for vitiligo, Jason Hawkes, MD, a dermatologist in Rocklin, Calif., who also spoke at the IDS meeting, said that oxidative stress is among the processes that may contribute to melanocyte degeneration seen in vitiligo.
The immunopathogenesis of vitiligo is “multilayered and complex,” he said. “While the T lymphocyte plays a central role in this disease, there are other genetic and biologic processes [including oxidative stress] that also contribute to the destruction of melanocytes.”
Reducing oxidative stress in the body and skin via supplements such as vitamin E, coenzyme Q10, and alpha-lipoic acid “may represent complementary treatments used for the treatment of vitiligo,” said Dr. Hawkes. And as more is learned about the pathogenic role of oxidative stress and its impact on diseases of pigmentation, “therapeutic targeting of the antioxidation-related signaling pathways in the skin may represent a novel treatment for vitiligo or other related conditions.”
Dr. Hawkes disclosed ties with AbbVie, Arcutis, Bristol-Myers Squibb, Boehringer Ingelheim, Janssen, LEO, Lilly, Novartis, Pfizer, Regeneron, Sanofi, Sun Pharma, and UCB. Dr. Hawkes disclosed serving as an investigator and advisory board member for Avita and an investigator for Pfizer.
FROM IDS 2023
FDA warns of potentially lethal reaction to seizure meds
that can be life threatening if not detected and treated promptly, the Food and Drug Administration warns in an alert.
Known as drug reaction with eosinophilia and systemic symptoms (DRESS), it may start as a rash but can quickly progress and cause injury to internal organs, the need for hospitalization, and death, the FDA notes.
A search of the FDA Adverse Event Reporting System (FAERS) and the medical literature through March 2023 identified 32 serious cases of DRESS worldwide that were associated with levetiracetam.
Three cases occurred in the United States, and 29 occurred abroad. In all 32 cases, the patients were hospitalized and received medical treatment; in 2 cases, the patients died.
The median time to onset of DRESS in the levetiracetam cases was 24 days; times ranged from 7 to 170 days. The reported signs and symptoms included skin rash (n = 22), fever (n = 20), eosinophilia (n = 17), lymph node swelling (n = 9), and atypical lymphocytes (n = 4).
Twenty-two levetiracetam-associated cases of DRESS involved injury to one or more organs, including the liver, lungs, kidneys, and gallbladder.
In 25 of the 29 cases for which information on treatment discontinuation was available, DRESS symptoms resolved when levetiracetam was discontinued.
As for clobazam, a search of FAERS and the medical literature through July 2023 identified 10 serious cases of DRESS worldwide – 1 in the United States and 9 abroad. All 10 patients were hospitalized and received medical treatment. No deaths were reported.
The median time to onset of clobazam-associated DRESS was 21.5 days (range, 7-103 days). The reported signs and symptoms included skin rash (n = 10), fever (n = 8), eosinophilia (n = 7), facial swelling (n = 7), leukocytosis (n = 4), lymph node swelling (n = 4), and leukopenia/thrombocytopenia (n = 1).
In nine cases, there was injury to one or more organs, including the liver, kidneys, and gastrointestinal tract.
DRESS symptoms resolved in all 10 cases when treatment with clobazam was stopped. DRESS and other serious skin reactions reported with clobazam, a benzodiazepine, have not generally been associated with other benzodiazepines, the FDA notes.
Label updates
As a result of these cases, warnings about the risk of DRESS will be added to the prescribing information and patient medication guides for these medicines, the FDA announced.
“Health care professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA said.
They noted that diagnosis is often difficult because early signs and symptoms, such as fever and swollen lymph nodes, may be present without evidence of a rash.
DRESS may develop 2-8 weeks after starting levetiracetam or clobazam. Symptoms and intensity can vary widely.
DRESS can also be confused with other serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
The FDA says patients should be advised of the signs and symptoms of DRESS and be told to stop taking the medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam.
Adverse reactions with these medications should be reported to the FDA’s MedWatch program.
A version of this article appeared on Medscape.com.
that can be life threatening if not detected and treated promptly, the Food and Drug Administration warns in an alert.
Known as drug reaction with eosinophilia and systemic symptoms (DRESS), it may start as a rash but can quickly progress and cause injury to internal organs, the need for hospitalization, and death, the FDA notes.
A search of the FDA Adverse Event Reporting System (FAERS) and the medical literature through March 2023 identified 32 serious cases of DRESS worldwide that were associated with levetiracetam.
Three cases occurred in the United States, and 29 occurred abroad. In all 32 cases, the patients were hospitalized and received medical treatment; in 2 cases, the patients died.
The median time to onset of DRESS in the levetiracetam cases was 24 days; times ranged from 7 to 170 days. The reported signs and symptoms included skin rash (n = 22), fever (n = 20), eosinophilia (n = 17), lymph node swelling (n = 9), and atypical lymphocytes (n = 4).
Twenty-two levetiracetam-associated cases of DRESS involved injury to one or more organs, including the liver, lungs, kidneys, and gallbladder.
In 25 of the 29 cases for which information on treatment discontinuation was available, DRESS symptoms resolved when levetiracetam was discontinued.
As for clobazam, a search of FAERS and the medical literature through July 2023 identified 10 serious cases of DRESS worldwide – 1 in the United States and 9 abroad. All 10 patients were hospitalized and received medical treatment. No deaths were reported.
The median time to onset of clobazam-associated DRESS was 21.5 days (range, 7-103 days). The reported signs and symptoms included skin rash (n = 10), fever (n = 8), eosinophilia (n = 7), facial swelling (n = 7), leukocytosis (n = 4), lymph node swelling (n = 4), and leukopenia/thrombocytopenia (n = 1).
In nine cases, there was injury to one or more organs, including the liver, kidneys, and gastrointestinal tract.
DRESS symptoms resolved in all 10 cases when treatment with clobazam was stopped. DRESS and other serious skin reactions reported with clobazam, a benzodiazepine, have not generally been associated with other benzodiazepines, the FDA notes.
Label updates
As a result of these cases, warnings about the risk of DRESS will be added to the prescribing information and patient medication guides for these medicines, the FDA announced.
“Health care professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA said.
They noted that diagnosis is often difficult because early signs and symptoms, such as fever and swollen lymph nodes, may be present without evidence of a rash.
DRESS may develop 2-8 weeks after starting levetiracetam or clobazam. Symptoms and intensity can vary widely.
DRESS can also be confused with other serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
The FDA says patients should be advised of the signs and symptoms of DRESS and be told to stop taking the medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam.
Adverse reactions with these medications should be reported to the FDA’s MedWatch program.
A version of this article appeared on Medscape.com.
that can be life threatening if not detected and treated promptly, the Food and Drug Administration warns in an alert.
Known as drug reaction with eosinophilia and systemic symptoms (DRESS), it may start as a rash but can quickly progress and cause injury to internal organs, the need for hospitalization, and death, the FDA notes.
A search of the FDA Adverse Event Reporting System (FAERS) and the medical literature through March 2023 identified 32 serious cases of DRESS worldwide that were associated with levetiracetam.
Three cases occurred in the United States, and 29 occurred abroad. In all 32 cases, the patients were hospitalized and received medical treatment; in 2 cases, the patients died.
The median time to onset of DRESS in the levetiracetam cases was 24 days; times ranged from 7 to 170 days. The reported signs and symptoms included skin rash (n = 22), fever (n = 20), eosinophilia (n = 17), lymph node swelling (n = 9), and atypical lymphocytes (n = 4).
Twenty-two levetiracetam-associated cases of DRESS involved injury to one or more organs, including the liver, lungs, kidneys, and gallbladder.
In 25 of the 29 cases for which information on treatment discontinuation was available, DRESS symptoms resolved when levetiracetam was discontinued.
As for clobazam, a search of FAERS and the medical literature through July 2023 identified 10 serious cases of DRESS worldwide – 1 in the United States and 9 abroad. All 10 patients were hospitalized and received medical treatment. No deaths were reported.
The median time to onset of clobazam-associated DRESS was 21.5 days (range, 7-103 days). The reported signs and symptoms included skin rash (n = 10), fever (n = 8), eosinophilia (n = 7), facial swelling (n = 7), leukocytosis (n = 4), lymph node swelling (n = 4), and leukopenia/thrombocytopenia (n = 1).
In nine cases, there was injury to one or more organs, including the liver, kidneys, and gastrointestinal tract.
DRESS symptoms resolved in all 10 cases when treatment with clobazam was stopped. DRESS and other serious skin reactions reported with clobazam, a benzodiazepine, have not generally been associated with other benzodiazepines, the FDA notes.
Label updates
As a result of these cases, warnings about the risk of DRESS will be added to the prescribing information and patient medication guides for these medicines, the FDA announced.
“Health care professionals should be aware that prompt recognition and early treatment is important for improving DRESS outcomes and decreasing mortality,” the FDA said.
They noted that diagnosis is often difficult because early signs and symptoms, such as fever and swollen lymph nodes, may be present without evidence of a rash.
DRESS may develop 2-8 weeks after starting levetiracetam or clobazam. Symptoms and intensity can vary widely.
DRESS can also be confused with other serious skin reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
The FDA says patients should be advised of the signs and symptoms of DRESS and be told to stop taking the medicine and seek immediate medical attention if DRESS is suspected during treatment with levetiracetam or clobazam.
Adverse reactions with these medications should be reported to the FDA’s MedWatch program.
A version of this article appeared on Medscape.com.
New consensus guide on rare drug hypersensitivity reaction
TOPLINE:
).
METHODOLOGY:
Data on the evaluation, assessment, and treatment of the rare but potentially life-threatening drug hypersensitivity reaction are lacking.
To support clinicians in diagnosing and managing DRESS, a steering committee conducted a literature review to examine current research, identify evidence, and develop consensus statements. They invited experts from 21 countries across four continents to participate in a Delphi consensus process.
An international panel of 54 experts (including 45 dermatologists) initially assessed 100 statements related to baseline workup, severity of the condition, and treatment. Two more statements were added in the second round.
After revisions and the second round, the group reached consensus for 93 statements overall.
TAKEAWAY:
The statements generating the most disagreement involved diagnosis. The group ultimately supported the value of measuring the viral load of Epstein-Barr virus, cytomegalovirus, and human herpesvirus 6 in all patients with suspected DRESS. The group also agreed on screening for hepatitis A, B, and C in cases of liver involvement and screening for hepatitis B and C before starting systemic therapy.
The group agreed with previous severity criteria that differentiate between mild, moderate, and severe DRESS based on the extent of liver, kidney, and blood involvement and the damage of other organs.
Consensus on treatment was reached for all 12 relevant statements in the first Delphi round. Recommendations included the use of corticosteroids and immediate discontinuation of the drugs causing the reaction.
IN PRACTICE:
“This Delphi exercise aimed to provide a common ground of consensus,” the authors noted. However, “each of the addressed categories needs more in-depth follow-up studies to improve the clinical management of patients.”
SOURCE:
The DRESS Delphi consensus group conducted its exercise under the leadership of Marie-Charlotte Brüggen, MD, of the University Hospital of Zürich. The consensus was published online in the JAMA Dermatology.
LIMITATIONS:
Published evidence was limited because of the low prevalence of DRESS. The consensus statements should therefore be considered with caution and in the context of a clinician’s expertise and available resources. Research gaps also persist in how DRESS may vary with region and ethnicity. The severity thresholds need validation in a revised multicenter statement.
DISCLOSURES:
The consensus review received no outside funding. Dr. Brüggen disclosed relationships with the Swiss National Science Foundation, Christine Kühne – Center for Allergy Research and Education, FreeNovation, LEO Foundation, Olga Mayenfisch Foundation, University of Zürich, LEO Pharma, Pierre Fabre Eczema Foundation, Eli Lilly, AbbVie, GSK, and AstraZeneca. Coauthors disclosed relationships with multiple pharmaceutical companies, foundations, and medical publishing companies.
A version of this article appeared on Medscape.com.
TOPLINE:
).
METHODOLOGY:
Data on the evaluation, assessment, and treatment of the rare but potentially life-threatening drug hypersensitivity reaction are lacking.
To support clinicians in diagnosing and managing DRESS, a steering committee conducted a literature review to examine current research, identify evidence, and develop consensus statements. They invited experts from 21 countries across four continents to participate in a Delphi consensus process.
An international panel of 54 experts (including 45 dermatologists) initially assessed 100 statements related to baseline workup, severity of the condition, and treatment. Two more statements were added in the second round.
After revisions and the second round, the group reached consensus for 93 statements overall.
TAKEAWAY:
The statements generating the most disagreement involved diagnosis. The group ultimately supported the value of measuring the viral load of Epstein-Barr virus, cytomegalovirus, and human herpesvirus 6 in all patients with suspected DRESS. The group also agreed on screening for hepatitis A, B, and C in cases of liver involvement and screening for hepatitis B and C before starting systemic therapy.
The group agreed with previous severity criteria that differentiate between mild, moderate, and severe DRESS based on the extent of liver, kidney, and blood involvement and the damage of other organs.
Consensus on treatment was reached for all 12 relevant statements in the first Delphi round. Recommendations included the use of corticosteroids and immediate discontinuation of the drugs causing the reaction.
IN PRACTICE:
“This Delphi exercise aimed to provide a common ground of consensus,” the authors noted. However, “each of the addressed categories needs more in-depth follow-up studies to improve the clinical management of patients.”
SOURCE:
The DRESS Delphi consensus group conducted its exercise under the leadership of Marie-Charlotte Brüggen, MD, of the University Hospital of Zürich. The consensus was published online in the JAMA Dermatology.
LIMITATIONS:
Published evidence was limited because of the low prevalence of DRESS. The consensus statements should therefore be considered with caution and in the context of a clinician’s expertise and available resources. Research gaps also persist in how DRESS may vary with region and ethnicity. The severity thresholds need validation in a revised multicenter statement.
DISCLOSURES:
The consensus review received no outside funding. Dr. Brüggen disclosed relationships with the Swiss National Science Foundation, Christine Kühne – Center for Allergy Research and Education, FreeNovation, LEO Foundation, Olga Mayenfisch Foundation, University of Zürich, LEO Pharma, Pierre Fabre Eczema Foundation, Eli Lilly, AbbVie, GSK, and AstraZeneca. Coauthors disclosed relationships with multiple pharmaceutical companies, foundations, and medical publishing companies.
A version of this article appeared on Medscape.com.
TOPLINE:
).
METHODOLOGY:
Data on the evaluation, assessment, and treatment of the rare but potentially life-threatening drug hypersensitivity reaction are lacking.
To support clinicians in diagnosing and managing DRESS, a steering committee conducted a literature review to examine current research, identify evidence, and develop consensus statements. They invited experts from 21 countries across four continents to participate in a Delphi consensus process.
An international panel of 54 experts (including 45 dermatologists) initially assessed 100 statements related to baseline workup, severity of the condition, and treatment. Two more statements were added in the second round.
After revisions and the second round, the group reached consensus for 93 statements overall.
TAKEAWAY:
The statements generating the most disagreement involved diagnosis. The group ultimately supported the value of measuring the viral load of Epstein-Barr virus, cytomegalovirus, and human herpesvirus 6 in all patients with suspected DRESS. The group also agreed on screening for hepatitis A, B, and C in cases of liver involvement and screening for hepatitis B and C before starting systemic therapy.
The group agreed with previous severity criteria that differentiate between mild, moderate, and severe DRESS based on the extent of liver, kidney, and blood involvement and the damage of other organs.
Consensus on treatment was reached for all 12 relevant statements in the first Delphi round. Recommendations included the use of corticosteroids and immediate discontinuation of the drugs causing the reaction.
IN PRACTICE:
“This Delphi exercise aimed to provide a common ground of consensus,” the authors noted. However, “each of the addressed categories needs more in-depth follow-up studies to improve the clinical management of patients.”
SOURCE:
The DRESS Delphi consensus group conducted its exercise under the leadership of Marie-Charlotte Brüggen, MD, of the University Hospital of Zürich. The consensus was published online in the JAMA Dermatology.
LIMITATIONS:
Published evidence was limited because of the low prevalence of DRESS. The consensus statements should therefore be considered with caution and in the context of a clinician’s expertise and available resources. Research gaps also persist in how DRESS may vary with region and ethnicity. The severity thresholds need validation in a revised multicenter statement.
DISCLOSURES:
The consensus review received no outside funding. Dr. Brüggen disclosed relationships with the Swiss National Science Foundation, Christine Kühne – Center for Allergy Research and Education, FreeNovation, LEO Foundation, Olga Mayenfisch Foundation, University of Zürich, LEO Pharma, Pierre Fabre Eczema Foundation, Eli Lilly, AbbVie, GSK, and AstraZeneca. Coauthors disclosed relationships with multiple pharmaceutical companies, foundations, and medical publishing companies.
A version of this article appeared on Medscape.com.
Laser epilation may reduce pilonidal disease recurrences when added to standard care
according to the results of a randomized trial.
The study, recently published in JAMA Surgery, enrolled 302 patients ages 11-21 with pilonidal disease. Half of the participants were assigned to receive LE (laser hair removal) plus standard treatment (improved hygiene plus mechanical or chemical hair removal), and half were assigned to receive standard care alone.
At 1 year, 10.4% of the patients who had received LE plus standard treatment had experienced a recurrence of pilonidal disease, compared with 33.6% of patients in the standard treatment group (P < .001). Rates were based on the data available on 96 patients in the LE group and 134 patients in the standard care group.
“These results provide further evidence that laser epilation is safe, well-tolerated, and should be available as an initial treatment option or adjunct treatment modality for all eligible patients,” first author Peter C. Minneci, MD, chair of surgery at Nemours Children’s Health, Delaware Valley, Wilmington, Del, said in a press release reporting the results. “There have been few comparative studies that have investigated recurrence rates after LE versus other treatment modalities,” he and his coauthors wrote in the study, noting that the study “was the first, to our knowledge, to compare LE as an adjunct to standard care versus standard care alone and demonstrate a decrease in recurrence rates.”
Pilonidal disease, a common condition, results when cysts form between the buttocks and is most common in adolescents and young adults. It is thought to recur about 33% of the time, with most cases recurring within 1 year of treatment.
In practice, there are large variations in management strategies for pilonidal disease because evidence for an ideal treatment approach is lacking, Dr. Minneci and coauthors wrote. Although lifestyle modifications and nonepilation hair removal strategies have been linked to a reduced need for surgery, compliance with these strategies is low. Additionally, recurrence contributes to “a high degree of psychosocial stress in patients, who often miss school or sports and may avoid social activities,” Dr. Minneci said in the press release. Therefore, some practitioners have begun using LE – which uses selective thermolysis to remove the hair shaft, follicle, and bulb – as an adjunct to standard treatments in the hopes of avoiding surgery.
A few studies have shown LE is effective in reducing pilonidal disease recurrence, but these studies had small sample sizes, according to the authors.
Study methods
The randomized, nonblinded clinical trial was conducted between 2017 and 2022 at Nationwide Children’s Hospital, Columbus, and enrolled patients aged 11-21 years with a history of pilonidal disease, who did not have active disease.
Those in the control group (151 patients) had an in-person clinic visit where they received education and training about hair removal in the gluteal cleft, and were provided with supplies for hair removal (chemical epilation or shaving) for 6 months (standard of care). Those in the LE group (151 patients) received standard of care therapy, and also received one LE treatment every 4-6 weeks for a total of five treatments. They were encouraged to perform hair removal using chemical or mechanical depilation between visits.
At the 1-year follow-up, data were available in 96 patients in the LE group and 134 patients in the standard care group. At that time, the proportion of those who had a recurrence within 1 year was significantly lower in the LE group than in the standard care group (mean difference, –23.2%; 95% CI, –33.2% to –13.1%; P < .001).
In addition, over the course of a year, those in the LE-treated group had significantly higher Child Attitude Toward Illness scores, indicating that they felt more positively about their illness at 6 months than participants in the standard care group. There were no differences between the groups in terms of patient or caregiver disability days, patient- or caregiver-reported health-related quality of life, health care satisfaction, or perceived stigma. In the LE group, no burns were reported, and no inability to tolerate treatment because of pain.
The study had several limitations, including the potential for participation bias, and because of a loss to follow-up, primary and secondary outcomes were missing data points, which was higher in the LE group. Loss to follow-up in the LE arm increased after 6 months, when laser treatments ended, with many of those patients not completing surveys at 9 and 12 months. The hospital’s pilonidal clinic shut down for 3 months during the COVID-19 pandemic, and when the clinic reopened, 15 patients in the LE arm withdrew from the study.
|In the press release, Dr. Minneci said that confirmation of the effectiveness of LE could help justify insurance coverage for pilonidal disease, noting that LE is usually not covered with insurance, and a course of treatment could cost $800-$1,500.
Dr. Minneci and four of the other six coauthors reported receiving grants from Patient-Centered Outcomes Research Institute during the conduct of the study. One author reported receiving grants from the National Institute on Minority Health and Health Disparities outside the submitted work. The research was funded by a grant from the Patient-Centered Outcomes Research Institute.
according to the results of a randomized trial.
The study, recently published in JAMA Surgery, enrolled 302 patients ages 11-21 with pilonidal disease. Half of the participants were assigned to receive LE (laser hair removal) plus standard treatment (improved hygiene plus mechanical or chemical hair removal), and half were assigned to receive standard care alone.
At 1 year, 10.4% of the patients who had received LE plus standard treatment had experienced a recurrence of pilonidal disease, compared with 33.6% of patients in the standard treatment group (P < .001). Rates were based on the data available on 96 patients in the LE group and 134 patients in the standard care group.
“These results provide further evidence that laser epilation is safe, well-tolerated, and should be available as an initial treatment option or adjunct treatment modality for all eligible patients,” first author Peter C. Minneci, MD, chair of surgery at Nemours Children’s Health, Delaware Valley, Wilmington, Del, said in a press release reporting the results. “There have been few comparative studies that have investigated recurrence rates after LE versus other treatment modalities,” he and his coauthors wrote in the study, noting that the study “was the first, to our knowledge, to compare LE as an adjunct to standard care versus standard care alone and demonstrate a decrease in recurrence rates.”
Pilonidal disease, a common condition, results when cysts form between the buttocks and is most common in adolescents and young adults. It is thought to recur about 33% of the time, with most cases recurring within 1 year of treatment.
In practice, there are large variations in management strategies for pilonidal disease because evidence for an ideal treatment approach is lacking, Dr. Minneci and coauthors wrote. Although lifestyle modifications and nonepilation hair removal strategies have been linked to a reduced need for surgery, compliance with these strategies is low. Additionally, recurrence contributes to “a high degree of psychosocial stress in patients, who often miss school or sports and may avoid social activities,” Dr. Minneci said in the press release. Therefore, some practitioners have begun using LE – which uses selective thermolysis to remove the hair shaft, follicle, and bulb – as an adjunct to standard treatments in the hopes of avoiding surgery.
A few studies have shown LE is effective in reducing pilonidal disease recurrence, but these studies had small sample sizes, according to the authors.
Study methods
The randomized, nonblinded clinical trial was conducted between 2017 and 2022 at Nationwide Children’s Hospital, Columbus, and enrolled patients aged 11-21 years with a history of pilonidal disease, who did not have active disease.
Those in the control group (151 patients) had an in-person clinic visit where they received education and training about hair removal in the gluteal cleft, and were provided with supplies for hair removal (chemical epilation or shaving) for 6 months (standard of care). Those in the LE group (151 patients) received standard of care therapy, and also received one LE treatment every 4-6 weeks for a total of five treatments. They were encouraged to perform hair removal using chemical or mechanical depilation between visits.
At the 1-year follow-up, data were available in 96 patients in the LE group and 134 patients in the standard care group. At that time, the proportion of those who had a recurrence within 1 year was significantly lower in the LE group than in the standard care group (mean difference, –23.2%; 95% CI, –33.2% to –13.1%; P < .001).
In addition, over the course of a year, those in the LE-treated group had significantly higher Child Attitude Toward Illness scores, indicating that they felt more positively about their illness at 6 months than participants in the standard care group. There were no differences between the groups in terms of patient or caregiver disability days, patient- or caregiver-reported health-related quality of life, health care satisfaction, or perceived stigma. In the LE group, no burns were reported, and no inability to tolerate treatment because of pain.
The study had several limitations, including the potential for participation bias, and because of a loss to follow-up, primary and secondary outcomes were missing data points, which was higher in the LE group. Loss to follow-up in the LE arm increased after 6 months, when laser treatments ended, with many of those patients not completing surveys at 9 and 12 months. The hospital’s pilonidal clinic shut down for 3 months during the COVID-19 pandemic, and when the clinic reopened, 15 patients in the LE arm withdrew from the study.
|In the press release, Dr. Minneci said that confirmation of the effectiveness of LE could help justify insurance coverage for pilonidal disease, noting that LE is usually not covered with insurance, and a course of treatment could cost $800-$1,500.
Dr. Minneci and four of the other six coauthors reported receiving grants from Patient-Centered Outcomes Research Institute during the conduct of the study. One author reported receiving grants from the National Institute on Minority Health and Health Disparities outside the submitted work. The research was funded by a grant from the Patient-Centered Outcomes Research Institute.
according to the results of a randomized trial.
The study, recently published in JAMA Surgery, enrolled 302 patients ages 11-21 with pilonidal disease. Half of the participants were assigned to receive LE (laser hair removal) plus standard treatment (improved hygiene plus mechanical or chemical hair removal), and half were assigned to receive standard care alone.
At 1 year, 10.4% of the patients who had received LE plus standard treatment had experienced a recurrence of pilonidal disease, compared with 33.6% of patients in the standard treatment group (P < .001). Rates were based on the data available on 96 patients in the LE group and 134 patients in the standard care group.
“These results provide further evidence that laser epilation is safe, well-tolerated, and should be available as an initial treatment option or adjunct treatment modality for all eligible patients,” first author Peter C. Minneci, MD, chair of surgery at Nemours Children’s Health, Delaware Valley, Wilmington, Del, said in a press release reporting the results. “There have been few comparative studies that have investigated recurrence rates after LE versus other treatment modalities,” he and his coauthors wrote in the study, noting that the study “was the first, to our knowledge, to compare LE as an adjunct to standard care versus standard care alone and demonstrate a decrease in recurrence rates.”
Pilonidal disease, a common condition, results when cysts form between the buttocks and is most common in adolescents and young adults. It is thought to recur about 33% of the time, with most cases recurring within 1 year of treatment.
In practice, there are large variations in management strategies for pilonidal disease because evidence for an ideal treatment approach is lacking, Dr. Minneci and coauthors wrote. Although lifestyle modifications and nonepilation hair removal strategies have been linked to a reduced need for surgery, compliance with these strategies is low. Additionally, recurrence contributes to “a high degree of psychosocial stress in patients, who often miss school or sports and may avoid social activities,” Dr. Minneci said in the press release. Therefore, some practitioners have begun using LE – which uses selective thermolysis to remove the hair shaft, follicle, and bulb – as an adjunct to standard treatments in the hopes of avoiding surgery.
A few studies have shown LE is effective in reducing pilonidal disease recurrence, but these studies had small sample sizes, according to the authors.
Study methods
The randomized, nonblinded clinical trial was conducted between 2017 and 2022 at Nationwide Children’s Hospital, Columbus, and enrolled patients aged 11-21 years with a history of pilonidal disease, who did not have active disease.
Those in the control group (151 patients) had an in-person clinic visit where they received education and training about hair removal in the gluteal cleft, and were provided with supplies for hair removal (chemical epilation or shaving) for 6 months (standard of care). Those in the LE group (151 patients) received standard of care therapy, and also received one LE treatment every 4-6 weeks for a total of five treatments. They were encouraged to perform hair removal using chemical or mechanical depilation between visits.
At the 1-year follow-up, data were available in 96 patients in the LE group and 134 patients in the standard care group. At that time, the proportion of those who had a recurrence within 1 year was significantly lower in the LE group than in the standard care group (mean difference, –23.2%; 95% CI, –33.2% to –13.1%; P < .001).
In addition, over the course of a year, those in the LE-treated group had significantly higher Child Attitude Toward Illness scores, indicating that they felt more positively about their illness at 6 months than participants in the standard care group. There were no differences between the groups in terms of patient or caregiver disability days, patient- or caregiver-reported health-related quality of life, health care satisfaction, or perceived stigma. In the LE group, no burns were reported, and no inability to tolerate treatment because of pain.
The study had several limitations, including the potential for participation bias, and because of a loss to follow-up, primary and secondary outcomes were missing data points, which was higher in the LE group. Loss to follow-up in the LE arm increased after 6 months, when laser treatments ended, with many of those patients not completing surveys at 9 and 12 months. The hospital’s pilonidal clinic shut down for 3 months during the COVID-19 pandemic, and when the clinic reopened, 15 patients in the LE arm withdrew from the study.
|In the press release, Dr. Minneci said that confirmation of the effectiveness of LE could help justify insurance coverage for pilonidal disease, noting that LE is usually not covered with insurance, and a course of treatment could cost $800-$1,500.
Dr. Minneci and four of the other six coauthors reported receiving grants from Patient-Centered Outcomes Research Institute during the conduct of the study. One author reported receiving grants from the National Institute on Minority Health and Health Disparities outside the submitted work. The research was funded by a grant from the Patient-Centered Outcomes Research Institute.
FROM JAMA SURGERY