User login
European Academy of Dermatology & Venereology (EADV): Annual Congress
Is PASI 90 becoming the new PASI 75?
ISTANBUL – With the majority of psoriasis patients now achieving PASI 90 responses in randomized trials of the latest-generation biologic agents, a push is on to replace PASI 75 with PASI 90 as the new goal defining treatment success. But some dermatologists have misgivings about raising the bar.
"More and more, editorialists are promoting the idea of silencing psoriasis in all patients. This is a tricky and challenging goal," Dr. Hervé Bachelez said at the annual congress of the European Academy of Dermatology and Venereology.
"You’ve probably noticed that PASI 90 and even PASI 100 are becoming important as secondary endpoints in virtually all clinical trials. It’s good, it’s legitimate, and the PASI 90 probably better reflects the wishes of the patient and the physician than the PASI 75. But we have to wait and see what the caveats of this are. You can say, ‘Let’s push the response rate up to PASI 100 in all patients,’ but the danger is that if you cross a line, you may be unable to precisely regulate the level of immunosuppression in some patients. Basically you can expect some safety issues in real life that you would not see in clinical trials," cautioned Dr. Bachelez, professor of dermatology and head of the inflammatory skin diseases unit at Saint Louis University Hospital, Paris.
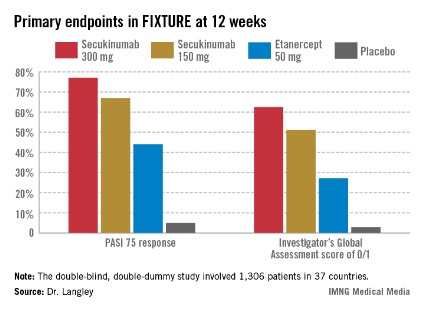
Not so many years ago the notion of PASI 90 responses in high double figures seemed a pipedream, he observed. For example, the week-12 PASI 90 rate in published randomized trials of methotrexate was only 9%, while for the first-generation tumor necrosis factor inhibitor etanercept, the rates were 19%-23%. In contrast, among the highlights of this year’s EADV congress were the presentation of results from clinical trials of two investigational interleukin-17 inhibitors: In the pivotal Phase III FIXTURE trial, secukinumab-treated patients had a PASI 90 response rate of 72% at week 16, while the week-16 PASI 90 rate in the Phase II OLE trial was 87% in patients on brodalimab, and even out to week 96, it was 78%.
Underscoring Dr. Bachelez’ concern that the randomized trial experience likely underestimates the true extent of safety hazards posed by potent therapies in daily clinical practice was a report by a consortium of 13 Spanish dermatology departments responsible for the BIOBADADERM registry. The Spanish registry is focused on safety and includes only psoriasis patients on systemic therapy, whether biologics or classic drugs. Among the first 1,042 enrollees receiving systemic therapy, fully 30% would not have been eligible for participation in randomized controlled trials for various reasons, including age greater than 70 years, having chronic kidney or liver disease, a history of hepatitis B or C, HIV infection, or cancer, or having psoriasis of a type other than chronic plaque disease.
The disturbing finding was that during 2,179 person-years of prospective follow-up, the large group of patients ineligible for randomized trials had a 2.7-fold increased risk of serious adverse events compared with patients on systemic therapy who were eligible for study participation.
The number needed to harm was calculated as follows: For every 40 patients treated with systemic therapy for 2.1 years despite not being eligible for randomized trials, one additional serious adverse event can be expected compared with similar treatment in randomized trial-eligible patients, according to the investigators (Arch. Dermatol. 2012;148:463-70). And that’s without pushing the envelope by trying to aim for a PASI 90 response, Dr. Bachelez noted.
A contrary view regarding PASI 90 as an emerging standard of treatment excellence was put forth elsewhere at the meeting by Dr. Peter van de Kerkhof, professor and head of the department of dermatology at Radboud University in Nijmegen, the Netherlands.
He cited multiple studies demonstrating that substantial PASI reductions may not translate into tangible improvements in patients’ quality of life. For example, among psoriasis patients who achieved a PASI 75 response in one European study, 65% still had a Dermatology Life Quality Index (DLQI) score of 2 or more (Eur. J. Dermatol. 2010;20:62-7).
"This implies that there is something more to be wished for by patients, even when PASI 75 is reached," according to Dr. van de Kerkhof.
Moreover, in another trial, even among patients with a PASI score of 0 at week 24, only 70% had an optimal DLQI of 0, not 100% as most dermatologists might expect (Br. J. Dermatol. 2006;154:1161-8).
A recent survey of 2,151 European psoriasis patients and their dermatologists highlighted a substantial degree of dissatisfaction with current therapies. Patients on biologics had higher rates of improvement from severe to moderate or mild disease than did those on any other forms of psoriasis therapy, yet 41% of patients on biologics were dissatisfied with their treatment (J. Dermatolog. Treat. 2013;24:193-8).
"I think it’s extremely important that we continue to innovate treatment possibilities for psoriasis in order to improve outcomes for our patients," Dr. van de Kerkhof said.
What patients really want, surveys suggest, are treatments that render them clear or nearly clear, and do so quickly. In one survey, patients rated as the most important characteristic about a therapy the rapidity with which it could achieve a moderate 50% improvement in symptoms. They rated that as higher in importance to them than the therapy’s long-term risks (Arch. Dermatol. 2007;143:1175-9), Dr. van de Kerkhof noted.
Patients also place a high priority on improvement of a broad array of symptoms that aren’t captured by either the PASI or the DLQI, Dr. Bruce E. Strober noted in a separate presentation. These include itching, plaque-related pain, altered skin appearance, flaking, and bleeding.
For this reason, he and a group of his coworkers have created and are now validating a new tool for the assessment of patient-related outcomes in psoriasis called the Psoriasis Symptom Diary (Value Health 2013;16:1014-22). The 16-item tool takes less than 5 minutes for a patient to fill out and is designed to replace the DLQI both in clinical trials and everyday practice. The goal is to be able to walk into the examination room, take a quick look at the Psoriasis Symptom Diary, and know from that how a patient is currently doing even before asking for the patient to disrobe.
"Let’s face it: Outside of skin cancer, when we’re doing dermatology, we’re in the quality of life business. That means we’re asking patients how they’re doing at every visit for psoriasis, atopic dermatitis, or severe acne. The DLQI does that, but it’s not psoriasis specific," said Dr. Strober, vice chair and director of the clinical trials unit in the department of dermatology at the University of Connecticut, Farmington.
As for the PASI, he doesn’t use it except in structured clinical trials. It’s too time consuming and has a high rate of inter- and intrarater variability.
"In the United States, dermatologists never do PASI scores in their clinics. The PASI score has numerous drawbacks that make it impractical in a regular practice setting," Dr. Strober said. "In my own practice, I routinely do a 5-point Physician’s Global Assessment along with an estimate of involved body surface area. I think that gives you a good picture of the objective level of psoriasis severity."
Dr. Bachelez, Dr. van de Kerkhof, and Dr. Strober each reported receiving research grants from and serving on advisory boards for 9-14 pharmaceutical companies engaged in developing new treatments for psoriasis.
ISTANBUL – With the majority of psoriasis patients now achieving PASI 90 responses in randomized trials of the latest-generation biologic agents, a push is on to replace PASI 75 with PASI 90 as the new goal defining treatment success. But some dermatologists have misgivings about raising the bar.
"More and more, editorialists are promoting the idea of silencing psoriasis in all patients. This is a tricky and challenging goal," Dr. Hervé Bachelez said at the annual congress of the European Academy of Dermatology and Venereology.
"You’ve probably noticed that PASI 90 and even PASI 100 are becoming important as secondary endpoints in virtually all clinical trials. It’s good, it’s legitimate, and the PASI 90 probably better reflects the wishes of the patient and the physician than the PASI 75. But we have to wait and see what the caveats of this are. You can say, ‘Let’s push the response rate up to PASI 100 in all patients,’ but the danger is that if you cross a line, you may be unable to precisely regulate the level of immunosuppression in some patients. Basically you can expect some safety issues in real life that you would not see in clinical trials," cautioned Dr. Bachelez, professor of dermatology and head of the inflammatory skin diseases unit at Saint Louis University Hospital, Paris.
Not so many years ago the notion of PASI 90 responses in high double figures seemed a pipedream, he observed. For example, the week-12 PASI 90 rate in published randomized trials of methotrexate was only 9%, while for the first-generation tumor necrosis factor inhibitor etanercept, the rates were 19%-23%. In contrast, among the highlights of this year’s EADV congress were the presentation of results from clinical trials of two investigational interleukin-17 inhibitors: In the pivotal Phase III FIXTURE trial, secukinumab-treated patients had a PASI 90 response rate of 72% at week 16, while the week-16 PASI 90 rate in the Phase II OLE trial was 87% in patients on brodalimab, and even out to week 96, it was 78%.
Underscoring Dr. Bachelez’ concern that the randomized trial experience likely underestimates the true extent of safety hazards posed by potent therapies in daily clinical practice was a report by a consortium of 13 Spanish dermatology departments responsible for the BIOBADADERM registry. The Spanish registry is focused on safety and includes only psoriasis patients on systemic therapy, whether biologics or classic drugs. Among the first 1,042 enrollees receiving systemic therapy, fully 30% would not have been eligible for participation in randomized controlled trials for various reasons, including age greater than 70 years, having chronic kidney or liver disease, a history of hepatitis B or C, HIV infection, or cancer, or having psoriasis of a type other than chronic plaque disease.
The disturbing finding was that during 2,179 person-years of prospective follow-up, the large group of patients ineligible for randomized trials had a 2.7-fold increased risk of serious adverse events compared with patients on systemic therapy who were eligible for study participation.
The number needed to harm was calculated as follows: For every 40 patients treated with systemic therapy for 2.1 years despite not being eligible for randomized trials, one additional serious adverse event can be expected compared with similar treatment in randomized trial-eligible patients, according to the investigators (Arch. Dermatol. 2012;148:463-70). And that’s without pushing the envelope by trying to aim for a PASI 90 response, Dr. Bachelez noted.
A contrary view regarding PASI 90 as an emerging standard of treatment excellence was put forth elsewhere at the meeting by Dr. Peter van de Kerkhof, professor and head of the department of dermatology at Radboud University in Nijmegen, the Netherlands.
He cited multiple studies demonstrating that substantial PASI reductions may not translate into tangible improvements in patients’ quality of life. For example, among psoriasis patients who achieved a PASI 75 response in one European study, 65% still had a Dermatology Life Quality Index (DLQI) score of 2 or more (Eur. J. Dermatol. 2010;20:62-7).
"This implies that there is something more to be wished for by patients, even when PASI 75 is reached," according to Dr. van de Kerkhof.
Moreover, in another trial, even among patients with a PASI score of 0 at week 24, only 70% had an optimal DLQI of 0, not 100% as most dermatologists might expect (Br. J. Dermatol. 2006;154:1161-8).
A recent survey of 2,151 European psoriasis patients and their dermatologists highlighted a substantial degree of dissatisfaction with current therapies. Patients on biologics had higher rates of improvement from severe to moderate or mild disease than did those on any other forms of psoriasis therapy, yet 41% of patients on biologics were dissatisfied with their treatment (J. Dermatolog. Treat. 2013;24:193-8).
"I think it’s extremely important that we continue to innovate treatment possibilities for psoriasis in order to improve outcomes for our patients," Dr. van de Kerkhof said.
What patients really want, surveys suggest, are treatments that render them clear or nearly clear, and do so quickly. In one survey, patients rated as the most important characteristic about a therapy the rapidity with which it could achieve a moderate 50% improvement in symptoms. They rated that as higher in importance to them than the therapy’s long-term risks (Arch. Dermatol. 2007;143:1175-9), Dr. van de Kerkhof noted.
Patients also place a high priority on improvement of a broad array of symptoms that aren’t captured by either the PASI or the DLQI, Dr. Bruce E. Strober noted in a separate presentation. These include itching, plaque-related pain, altered skin appearance, flaking, and bleeding.
For this reason, he and a group of his coworkers have created and are now validating a new tool for the assessment of patient-related outcomes in psoriasis called the Psoriasis Symptom Diary (Value Health 2013;16:1014-22). The 16-item tool takes less than 5 minutes for a patient to fill out and is designed to replace the DLQI both in clinical trials and everyday practice. The goal is to be able to walk into the examination room, take a quick look at the Psoriasis Symptom Diary, and know from that how a patient is currently doing even before asking for the patient to disrobe.
"Let’s face it: Outside of skin cancer, when we’re doing dermatology, we’re in the quality of life business. That means we’re asking patients how they’re doing at every visit for psoriasis, atopic dermatitis, or severe acne. The DLQI does that, but it’s not psoriasis specific," said Dr. Strober, vice chair and director of the clinical trials unit in the department of dermatology at the University of Connecticut, Farmington.
As for the PASI, he doesn’t use it except in structured clinical trials. It’s too time consuming and has a high rate of inter- and intrarater variability.
"In the United States, dermatologists never do PASI scores in their clinics. The PASI score has numerous drawbacks that make it impractical in a regular practice setting," Dr. Strober said. "In my own practice, I routinely do a 5-point Physician’s Global Assessment along with an estimate of involved body surface area. I think that gives you a good picture of the objective level of psoriasis severity."
Dr. Bachelez, Dr. van de Kerkhof, and Dr. Strober each reported receiving research grants from and serving on advisory boards for 9-14 pharmaceutical companies engaged in developing new treatments for psoriasis.
ISTANBUL – With the majority of psoriasis patients now achieving PASI 90 responses in randomized trials of the latest-generation biologic agents, a push is on to replace PASI 75 with PASI 90 as the new goal defining treatment success. But some dermatologists have misgivings about raising the bar.
"More and more, editorialists are promoting the idea of silencing psoriasis in all patients. This is a tricky and challenging goal," Dr. Hervé Bachelez said at the annual congress of the European Academy of Dermatology and Venereology.
"You’ve probably noticed that PASI 90 and even PASI 100 are becoming important as secondary endpoints in virtually all clinical trials. It’s good, it’s legitimate, and the PASI 90 probably better reflects the wishes of the patient and the physician than the PASI 75. But we have to wait and see what the caveats of this are. You can say, ‘Let’s push the response rate up to PASI 100 in all patients,’ but the danger is that if you cross a line, you may be unable to precisely regulate the level of immunosuppression in some patients. Basically you can expect some safety issues in real life that you would not see in clinical trials," cautioned Dr. Bachelez, professor of dermatology and head of the inflammatory skin diseases unit at Saint Louis University Hospital, Paris.
Not so many years ago the notion of PASI 90 responses in high double figures seemed a pipedream, he observed. For example, the week-12 PASI 90 rate in published randomized trials of methotrexate was only 9%, while for the first-generation tumor necrosis factor inhibitor etanercept, the rates were 19%-23%. In contrast, among the highlights of this year’s EADV congress were the presentation of results from clinical trials of two investigational interleukin-17 inhibitors: In the pivotal Phase III FIXTURE trial, secukinumab-treated patients had a PASI 90 response rate of 72% at week 16, while the week-16 PASI 90 rate in the Phase II OLE trial was 87% in patients on brodalimab, and even out to week 96, it was 78%.
Underscoring Dr. Bachelez’ concern that the randomized trial experience likely underestimates the true extent of safety hazards posed by potent therapies in daily clinical practice was a report by a consortium of 13 Spanish dermatology departments responsible for the BIOBADADERM registry. The Spanish registry is focused on safety and includes only psoriasis patients on systemic therapy, whether biologics or classic drugs. Among the first 1,042 enrollees receiving systemic therapy, fully 30% would not have been eligible for participation in randomized controlled trials for various reasons, including age greater than 70 years, having chronic kidney or liver disease, a history of hepatitis B or C, HIV infection, or cancer, or having psoriasis of a type other than chronic plaque disease.
The disturbing finding was that during 2,179 person-years of prospective follow-up, the large group of patients ineligible for randomized trials had a 2.7-fold increased risk of serious adverse events compared with patients on systemic therapy who were eligible for study participation.
The number needed to harm was calculated as follows: For every 40 patients treated with systemic therapy for 2.1 years despite not being eligible for randomized trials, one additional serious adverse event can be expected compared with similar treatment in randomized trial-eligible patients, according to the investigators (Arch. Dermatol. 2012;148:463-70). And that’s without pushing the envelope by trying to aim for a PASI 90 response, Dr. Bachelez noted.
A contrary view regarding PASI 90 as an emerging standard of treatment excellence was put forth elsewhere at the meeting by Dr. Peter van de Kerkhof, professor and head of the department of dermatology at Radboud University in Nijmegen, the Netherlands.
He cited multiple studies demonstrating that substantial PASI reductions may not translate into tangible improvements in patients’ quality of life. For example, among psoriasis patients who achieved a PASI 75 response in one European study, 65% still had a Dermatology Life Quality Index (DLQI) score of 2 or more (Eur. J. Dermatol. 2010;20:62-7).
"This implies that there is something more to be wished for by patients, even when PASI 75 is reached," according to Dr. van de Kerkhof.
Moreover, in another trial, even among patients with a PASI score of 0 at week 24, only 70% had an optimal DLQI of 0, not 100% as most dermatologists might expect (Br. J. Dermatol. 2006;154:1161-8).
A recent survey of 2,151 European psoriasis patients and their dermatologists highlighted a substantial degree of dissatisfaction with current therapies. Patients on biologics had higher rates of improvement from severe to moderate or mild disease than did those on any other forms of psoriasis therapy, yet 41% of patients on biologics were dissatisfied with their treatment (J. Dermatolog. Treat. 2013;24:193-8).
"I think it’s extremely important that we continue to innovate treatment possibilities for psoriasis in order to improve outcomes for our patients," Dr. van de Kerkhof said.
What patients really want, surveys suggest, are treatments that render them clear or nearly clear, and do so quickly. In one survey, patients rated as the most important characteristic about a therapy the rapidity with which it could achieve a moderate 50% improvement in symptoms. They rated that as higher in importance to them than the therapy’s long-term risks (Arch. Dermatol. 2007;143:1175-9), Dr. van de Kerkhof noted.
Patients also place a high priority on improvement of a broad array of symptoms that aren’t captured by either the PASI or the DLQI, Dr. Bruce E. Strober noted in a separate presentation. These include itching, plaque-related pain, altered skin appearance, flaking, and bleeding.
For this reason, he and a group of his coworkers have created and are now validating a new tool for the assessment of patient-related outcomes in psoriasis called the Psoriasis Symptom Diary (Value Health 2013;16:1014-22). The 16-item tool takes less than 5 minutes for a patient to fill out and is designed to replace the DLQI both in clinical trials and everyday practice. The goal is to be able to walk into the examination room, take a quick look at the Psoriasis Symptom Diary, and know from that how a patient is currently doing even before asking for the patient to disrobe.
"Let’s face it: Outside of skin cancer, when we’re doing dermatology, we’re in the quality of life business. That means we’re asking patients how they’re doing at every visit for psoriasis, atopic dermatitis, or severe acne. The DLQI does that, but it’s not psoriasis specific," said Dr. Strober, vice chair and director of the clinical trials unit in the department of dermatology at the University of Connecticut, Farmington.
As for the PASI, he doesn’t use it except in structured clinical trials. It’s too time consuming and has a high rate of inter- and intrarater variability.
"In the United States, dermatologists never do PASI scores in their clinics. The PASI score has numerous drawbacks that make it impractical in a regular practice setting," Dr. Strober said. "In my own practice, I routinely do a 5-point Physician’s Global Assessment along with an estimate of involved body surface area. I think that gives you a good picture of the objective level of psoriasis severity."
Dr. Bachelez, Dr. van de Kerkhof, and Dr. Strober each reported receiving research grants from and serving on advisory boards for 9-14 pharmaceutical companies engaged in developing new treatments for psoriasis.
EXPERT ANALYSIS FROM THE eadv CONGRESS
Lower serum IgE level tied to better treatment response in atopic dermatitis
ISTANBUL – Baseline total serum immunoglobulin E shows promise as a biomarker predictive of long-term treatment outcomes in atopic dermatitis patients.
In a retrospective study involving 175 Finnish patients with atopic dermatitis followed for a mean of 4.2 years, total clearance was achieved in 54% of patients with a baseline total serum IgE below 1,000 IU/mL, 38% of those with a baseline value of 1,000-10,000 IU/mL, and in a mere 8.3% with a baseline total serum IgE in excess of 10,000 IU/mL, Dr. Ville Kiiski reported at the annual congress of the European Academy of Dermatology and Venereology.
Similarly, treatment response, a lower bar as an endpoint in that it was defined as a lasting reduction in atopic dermatitis severity but not necessarily total clearance, occurred in 93% of those with a baseline total serum IgE below 1,000 IU/mL, compared with 64% of patients with a baseline of 1,000-10,000 IU/mL and 13% with a baseline level greater than 10,000 IU/mL, added Dr. Kiiski of Helsinki University.
Of note, this was largely an adult patient population, with a mean age of 32 years, although the range was 3-78 years. And these patients had atopic dermatitis of sufficient severity that it brought them to a specialized outpatient atopic dermatitis clinic at the Helsinki Skin and Allergy Hospital, where their baseline total serum IgE was measured.
Maintenance therapy during more than 4 years of follow-up was topical tacrolimus (Protopic) in 122 patients and topical corticosteroids and tacrolimus in 53.
Treatment had only a modest effect on total serum IgE levels over time. The median value was 1,472 IU/mL at baseline and 1,114 IU/mL more than 4 years later.
This retrospective study was free of commercial sponsorship, and Dr. Kiiski reported having no financial conflicts of interest.
ISTANBUL – Baseline total serum immunoglobulin E shows promise as a biomarker predictive of long-term treatment outcomes in atopic dermatitis patients.
In a retrospective study involving 175 Finnish patients with atopic dermatitis followed for a mean of 4.2 years, total clearance was achieved in 54% of patients with a baseline total serum IgE below 1,000 IU/mL, 38% of those with a baseline value of 1,000-10,000 IU/mL, and in a mere 8.3% with a baseline total serum IgE in excess of 10,000 IU/mL, Dr. Ville Kiiski reported at the annual congress of the European Academy of Dermatology and Venereology.
Similarly, treatment response, a lower bar as an endpoint in that it was defined as a lasting reduction in atopic dermatitis severity but not necessarily total clearance, occurred in 93% of those with a baseline total serum IgE below 1,000 IU/mL, compared with 64% of patients with a baseline of 1,000-10,000 IU/mL and 13% with a baseline level greater than 10,000 IU/mL, added Dr. Kiiski of Helsinki University.
Of note, this was largely an adult patient population, with a mean age of 32 years, although the range was 3-78 years. And these patients had atopic dermatitis of sufficient severity that it brought them to a specialized outpatient atopic dermatitis clinic at the Helsinki Skin and Allergy Hospital, where their baseline total serum IgE was measured.
Maintenance therapy during more than 4 years of follow-up was topical tacrolimus (Protopic) in 122 patients and topical corticosteroids and tacrolimus in 53.
Treatment had only a modest effect on total serum IgE levels over time. The median value was 1,472 IU/mL at baseline and 1,114 IU/mL more than 4 years later.
This retrospective study was free of commercial sponsorship, and Dr. Kiiski reported having no financial conflicts of interest.
ISTANBUL – Baseline total serum immunoglobulin E shows promise as a biomarker predictive of long-term treatment outcomes in atopic dermatitis patients.
In a retrospective study involving 175 Finnish patients with atopic dermatitis followed for a mean of 4.2 years, total clearance was achieved in 54% of patients with a baseline total serum IgE below 1,000 IU/mL, 38% of those with a baseline value of 1,000-10,000 IU/mL, and in a mere 8.3% with a baseline total serum IgE in excess of 10,000 IU/mL, Dr. Ville Kiiski reported at the annual congress of the European Academy of Dermatology and Venereology.
Similarly, treatment response, a lower bar as an endpoint in that it was defined as a lasting reduction in atopic dermatitis severity but not necessarily total clearance, occurred in 93% of those with a baseline total serum IgE below 1,000 IU/mL, compared with 64% of patients with a baseline of 1,000-10,000 IU/mL and 13% with a baseline level greater than 10,000 IU/mL, added Dr. Kiiski of Helsinki University.
Of note, this was largely an adult patient population, with a mean age of 32 years, although the range was 3-78 years. And these patients had atopic dermatitis of sufficient severity that it brought them to a specialized outpatient atopic dermatitis clinic at the Helsinki Skin and Allergy Hospital, where their baseline total serum IgE was measured.
Maintenance therapy during more than 4 years of follow-up was topical tacrolimus (Protopic) in 122 patients and topical corticosteroids and tacrolimus in 53.
Treatment had only a modest effect on total serum IgE levels over time. The median value was 1,472 IU/mL at baseline and 1,114 IU/mL more than 4 years later.
This retrospective study was free of commercial sponsorship, and Dr. Kiiski reported having no financial conflicts of interest.
AT THE EADV CONGRESS
Major finding: A reduction in atopic dermatitis severity during 4.2 years of topical therapy occurred in 93% of patients with a baseline total serum IgE level below 1,000 IU/mL, compared with 64% of those with a baseline IgE of 1,000-10,000 IU/mL, and just 13% of patients with a baseline value greater than 10,000 IU/mL.
Data source: This was a retrospective study involving 175 patients with atopic dermatitis followed for a mean of 4.2 years of treatment.
Disclosures: This retrospective study was free of commercial sponsorship, and Dr. Kiiski reported having no financial conflicts of interest.
Azelaic acid 15% gel tames women’s acne
ISTANBUL, TURKEY – Azelaic acid 15% gel constitutes an effective and well-tolerated treatment option for women with adult acne, according to the findings of an investigator-blinded, 9-month, randomized clinical trial.
The results showed azelaic acid 15% gel was similar in effectiveness to adapalene 0.1% gel, a widely prescribed treatment for this common condition, Dr. Anja Thielitz reported at the annual congress of the European Academy of Dermatology and Venereology.
However, azelaic acid 15% gel had a clear advantage in terms of tolerability. Median scores for skin redness, dryness, and scaling were significantly lower in the azelaic acid–treated group, added Dr. Thielitz of Otto von Guericke University in Magdeburg, Germany.
The single-center study involved 55 women aged 18-45 years, all with mild to moderate adult acne. They were randomized to one of three study arms: azelaic acid 15% gel twice daily for 9 months; adapalene 0.1% gel once daily, or 3 months of twice-daily azelaic acid 15% gel followed by 6 months of observation with no treatment.
Inflammatory and noninflammatory acne lesion counts, microcomedones, acne grading scale scores, and Dermatology Life Quality Index scores improved similarly in all three groups after 3 months. For example, median total lesion counts decreased from approximately 50 to 20, and median scores on the Leeds revised acne grading system dropped from 4 to roughly 2.5. Similar degrees of additional improvement were seen during months 4-9 in the two groups who remained on active treatment.
In contrast, some backsliding – although less than Dr. Thielitz had anticipated occurred during the untreated observation period among patients who halted the azelaic acid 15% gel after 3 months. By month 9, their total lesion count was 31% greater than the group that stayed on the topical therapy for the full 9 months.
Of note, azelaic acid 15% gel is technically an off-label therapy for adult female acne. The medication’s approved indication is in treating mild to moderate rosacea.
Dr. Thielitz reported having no financial conflicts in this investigator-initiated randomized trial.
ISTANBUL, TURKEY – Azelaic acid 15% gel constitutes an effective and well-tolerated treatment option for women with adult acne, according to the findings of an investigator-blinded, 9-month, randomized clinical trial.
The results showed azelaic acid 15% gel was similar in effectiveness to adapalene 0.1% gel, a widely prescribed treatment for this common condition, Dr. Anja Thielitz reported at the annual congress of the European Academy of Dermatology and Venereology.
However, azelaic acid 15% gel had a clear advantage in terms of tolerability. Median scores for skin redness, dryness, and scaling were significantly lower in the azelaic acid–treated group, added Dr. Thielitz of Otto von Guericke University in Magdeburg, Germany.
The single-center study involved 55 women aged 18-45 years, all with mild to moderate adult acne. They were randomized to one of three study arms: azelaic acid 15% gel twice daily for 9 months; adapalene 0.1% gel once daily, or 3 months of twice-daily azelaic acid 15% gel followed by 6 months of observation with no treatment.
Inflammatory and noninflammatory acne lesion counts, microcomedones, acne grading scale scores, and Dermatology Life Quality Index scores improved similarly in all three groups after 3 months. For example, median total lesion counts decreased from approximately 50 to 20, and median scores on the Leeds revised acne grading system dropped from 4 to roughly 2.5. Similar degrees of additional improvement were seen during months 4-9 in the two groups who remained on active treatment.
In contrast, some backsliding – although less than Dr. Thielitz had anticipated occurred during the untreated observation period among patients who halted the azelaic acid 15% gel after 3 months. By month 9, their total lesion count was 31% greater than the group that stayed on the topical therapy for the full 9 months.
Of note, azelaic acid 15% gel is technically an off-label therapy for adult female acne. The medication’s approved indication is in treating mild to moderate rosacea.
Dr. Thielitz reported having no financial conflicts in this investigator-initiated randomized trial.
ISTANBUL, TURKEY – Azelaic acid 15% gel constitutes an effective and well-tolerated treatment option for women with adult acne, according to the findings of an investigator-blinded, 9-month, randomized clinical trial.
The results showed azelaic acid 15% gel was similar in effectiveness to adapalene 0.1% gel, a widely prescribed treatment for this common condition, Dr. Anja Thielitz reported at the annual congress of the European Academy of Dermatology and Venereology.
However, azelaic acid 15% gel had a clear advantage in terms of tolerability. Median scores for skin redness, dryness, and scaling were significantly lower in the azelaic acid–treated group, added Dr. Thielitz of Otto von Guericke University in Magdeburg, Germany.
The single-center study involved 55 women aged 18-45 years, all with mild to moderate adult acne. They were randomized to one of three study arms: azelaic acid 15% gel twice daily for 9 months; adapalene 0.1% gel once daily, or 3 months of twice-daily azelaic acid 15% gel followed by 6 months of observation with no treatment.
Inflammatory and noninflammatory acne lesion counts, microcomedones, acne grading scale scores, and Dermatology Life Quality Index scores improved similarly in all three groups after 3 months. For example, median total lesion counts decreased from approximately 50 to 20, and median scores on the Leeds revised acne grading system dropped from 4 to roughly 2.5. Similar degrees of additional improvement were seen during months 4-9 in the two groups who remained on active treatment.
In contrast, some backsliding – although less than Dr. Thielitz had anticipated occurred during the untreated observation period among patients who halted the azelaic acid 15% gel after 3 months. By month 9, their total lesion count was 31% greater than the group that stayed on the topical therapy for the full 9 months.
Of note, azelaic acid 15% gel is technically an off-label therapy for adult female acne. The medication’s approved indication is in treating mild to moderate rosacea.
Dr. Thielitz reported having no financial conflicts in this investigator-initiated randomized trial.
AT THE EADV CONGRESS
Major finding: Azelaic acid 15% gel and adapalene 0.1% gel displayed comparable efficacy in treating women with adult acne, with median scores on the Leeds Revised Acne Grading Scale dropping from 4 to roughly 2.5 at 3 months and 2 at 9 months.
Data source: An investigator-blinded, randomized, 9-month study of 55 women with mild to moderate acne.
Disclosures: The presenter reported having no financial conflicts regarding this single-center, investigator-initiated study.
Hidradenitis Suppurativa Linked to Metabolic Syndrome
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ISTANBUL, TURKEY – Patients with hidradenitis suppurativa have a sharply increased prevalence of the metabolic syndrome, according to the first case-control study to examine the relationship.
Metabolic syndrome is known to be associated with increased cardiovascular risk, which may be particularly high in patients with hidradenitis suppurativa (HS), a dermatologic disease with an estimated prevalence of 1%-4%, because they develop metabolic syndrome at a much younger age than do individuals without the dermatologic disease, Dr. Wolfram Sterry said at the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights from a single-center, case-control study that comprised 80 patients with HS with a mean 12-year disease duration and 100 age- and gender-matched controls. Patients’ mean age was 40 years (PLoS One 2012 [doi:10.1371/journal.pone.0031810]).
The prevalence of metabolic syndrome was 40% in the HS group and 13% in controls, for an adjusted 4.5-fold increased likelihood, reported Dr. Sterry, professor and chairman of the department of dermatology at Charité University Hospital, Berlin.
Of the five metabolic derangements used in defining the metabolic syndrome, four were significantly more prevalent in subjects with HS. They were 5.9-fold more likely than were matched controls to have central obesity, 4.1-fold more likely to have hyperglycemia, 4.6-fold more likely to have low HDL cholesterol, and 2.2-fold more likely to be hypertriglyceridemic. Hypertension was present in 48% of HS patients and 35% of controls, a difference that did not achieve statistical significance.
Of note, HS patients with metabolic syndrome had more pronounced metabolic abnormalities than did controls with metabolic syndrome. While the definition of metabolic syndrome requires the presence of at least three of five metabolic alterations, half of all HS patients with metabolic syndrome met four or more of the criteria, compared with 39% of controls.
Moreover, metabolic syndrome occurred at a much younger age in subjects with HS than is typical in the general population or than was seen in controls. Indeed, 40% of HS patients under age 35 had metabolic syndrome, compared with none of the matched controls. Thus, the odds ratio for metabolic syndrome in HS patients aged 34 years or less was increased more than 20-fold compared with controls, while in the 35- to 44-year-old age group it was increased 6.2-fold, and in HS patients aged 45 and older it was 2-fold higher.
An increased prevalence of metabolic syndrome also has been documented in patients with psoriasis. But the prevalence of metabolic syndrome appears to be higher in HS patients and the metabolic disorder occurs at an earlier age than in psoriasis.
There was no correlation between duration or severity of HS and the prevalence of metabolic syndrome, according to Dr. Sterry. That’s an important message for physicians who see patients with the skin disease because it means such patients should be evaluated for metabolic syndrome early on, even if they have only moderate skin disease. After all, the elements of the metabolic syndrome are modifiable cardiovascular risk factors.
The lack of correlation between HS severity or duration and metabolic syndrome prevalence also has implications for the mechanism underlying the increased risk of metabolic syndrome in HS. When Dr. Sterry and coworkers compared the levels of metabolic syndrome parameters in the 42 patients with prior surgical treatment of their HS to the 38 patients who had not undergone surgery, they found no significant differences even though the surgical patients presumably had less inflammatory load. This led them to speculate that chronic inflammation may not be the major driver of the metabolic abnormalities in HS patients.
"It must be that a genetic predisposition for metabolic syndrome then induces the development of acne inversa [hidradenitis suppurativa] in predisposed individuals," Dr. Sterry said.
The proposed mechanism involves metabolic syndrome–induced poor blood circulation in the intertriginous axillary, perianal, and inguinal skin where HS most often occurs, with resultant increased interleukin-10 production by CD4-positive T cells. Interleukin-10, in turn, inhibits keratinocyte production of interleukins-20 and -22, which induce antimicrobial proteins in the skin. This would set the stage for HS, which is characterized by bacterial persistence in obstructed hair follicles, nodules, and fistulating sinuses.
Of course, this is speculation, Dr. Sterry was quick to acknowledge.
"Acne inversa is also known as hidradenitis suppurativa, apocrine acne, pyoderma fistulans significa ... If a disease has that many names, that’s always a sign that we don’t know too much about it," the dermatologist observed.
In a separate study presented at the EADV, investigators found that the most common comorbid conditions in a cohort of 154 patients with HS enrolled in a clinical trial of adalimumab (Humira) therapy were depression as defined by a score of 10 or more on the Patient Health Questionnaire–9, which had a prevalence of 42%; severe obesity marked by a body mass index of at least 40 kg/m2, present in 28% of patients; and uncontrolled hypertension, which was present in 27%. However, the investigators did not look at metabolic syndrome.
Dr. Sterry reported having no financial conflicts regarding this unfunded case-control study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ISTANBUL, TURKEY – Patients with hidradenitis suppurativa have a sharply increased prevalence of the metabolic syndrome, according to the first case-control study to examine the relationship.
Metabolic syndrome is known to be associated with increased cardiovascular risk, which may be particularly high in patients with hidradenitis suppurativa (HS), a dermatologic disease with an estimated prevalence of 1%-4%, because they develop metabolic syndrome at a much younger age than do individuals without the dermatologic disease, Dr. Wolfram Sterry said at the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights from a single-center, case-control study that comprised 80 patients with HS with a mean 12-year disease duration and 100 age- and gender-matched controls. Patients’ mean age was 40 years (PLoS One 2012 [doi:10.1371/journal.pone.0031810]).
The prevalence of metabolic syndrome was 40% in the HS group and 13% in controls, for an adjusted 4.5-fold increased likelihood, reported Dr. Sterry, professor and chairman of the department of dermatology at Charité University Hospital, Berlin.
Of the five metabolic derangements used in defining the metabolic syndrome, four were significantly more prevalent in subjects with HS. They were 5.9-fold more likely than were matched controls to have central obesity, 4.1-fold more likely to have hyperglycemia, 4.6-fold more likely to have low HDL cholesterol, and 2.2-fold more likely to be hypertriglyceridemic. Hypertension was present in 48% of HS patients and 35% of controls, a difference that did not achieve statistical significance.
Of note, HS patients with metabolic syndrome had more pronounced metabolic abnormalities than did controls with metabolic syndrome. While the definition of metabolic syndrome requires the presence of at least three of five metabolic alterations, half of all HS patients with metabolic syndrome met four or more of the criteria, compared with 39% of controls.
Moreover, metabolic syndrome occurred at a much younger age in subjects with HS than is typical in the general population or than was seen in controls. Indeed, 40% of HS patients under age 35 had metabolic syndrome, compared with none of the matched controls. Thus, the odds ratio for metabolic syndrome in HS patients aged 34 years or less was increased more than 20-fold compared with controls, while in the 35- to 44-year-old age group it was increased 6.2-fold, and in HS patients aged 45 and older it was 2-fold higher.
An increased prevalence of metabolic syndrome also has been documented in patients with psoriasis. But the prevalence of metabolic syndrome appears to be higher in HS patients and the metabolic disorder occurs at an earlier age than in psoriasis.
There was no correlation between duration or severity of HS and the prevalence of metabolic syndrome, according to Dr. Sterry. That’s an important message for physicians who see patients with the skin disease because it means such patients should be evaluated for metabolic syndrome early on, even if they have only moderate skin disease. After all, the elements of the metabolic syndrome are modifiable cardiovascular risk factors.
The lack of correlation between HS severity or duration and metabolic syndrome prevalence also has implications for the mechanism underlying the increased risk of metabolic syndrome in HS. When Dr. Sterry and coworkers compared the levels of metabolic syndrome parameters in the 42 patients with prior surgical treatment of their HS to the 38 patients who had not undergone surgery, they found no significant differences even though the surgical patients presumably had less inflammatory load. This led them to speculate that chronic inflammation may not be the major driver of the metabolic abnormalities in HS patients.
"It must be that a genetic predisposition for metabolic syndrome then induces the development of acne inversa [hidradenitis suppurativa] in predisposed individuals," Dr. Sterry said.
The proposed mechanism involves metabolic syndrome–induced poor blood circulation in the intertriginous axillary, perianal, and inguinal skin where HS most often occurs, with resultant increased interleukin-10 production by CD4-positive T cells. Interleukin-10, in turn, inhibits keratinocyte production of interleukins-20 and -22, which induce antimicrobial proteins in the skin. This would set the stage for HS, which is characterized by bacterial persistence in obstructed hair follicles, nodules, and fistulating sinuses.
Of course, this is speculation, Dr. Sterry was quick to acknowledge.
"Acne inversa is also known as hidradenitis suppurativa, apocrine acne, pyoderma fistulans significa ... If a disease has that many names, that’s always a sign that we don’t know too much about it," the dermatologist observed.
In a separate study presented at the EADV, investigators found that the most common comorbid conditions in a cohort of 154 patients with HS enrolled in a clinical trial of adalimumab (Humira) therapy were depression as defined by a score of 10 or more on the Patient Health Questionnaire–9, which had a prevalence of 42%; severe obesity marked by a body mass index of at least 40 kg/m2, present in 28% of patients; and uncontrolled hypertension, which was present in 27%. However, the investigators did not look at metabolic syndrome.
Dr. Sterry reported having no financial conflicts regarding this unfunded case-control study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
Earn 0.25 hours AMA PRA Category 1 credit: Read this article, and click the link at the end to take the post-test.
ISTANBUL, TURKEY – Patients with hidradenitis suppurativa have a sharply increased prevalence of the metabolic syndrome, according to the first case-control study to examine the relationship.
Metabolic syndrome is known to be associated with increased cardiovascular risk, which may be particularly high in patients with hidradenitis suppurativa (HS), a dermatologic disease with an estimated prevalence of 1%-4%, because they develop metabolic syndrome at a much younger age than do individuals without the dermatologic disease, Dr. Wolfram Sterry said at the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights from a single-center, case-control study that comprised 80 patients with HS with a mean 12-year disease duration and 100 age- and gender-matched controls. Patients’ mean age was 40 years (PLoS One 2012 [doi:10.1371/journal.pone.0031810]).
The prevalence of metabolic syndrome was 40% in the HS group and 13% in controls, for an adjusted 4.5-fold increased likelihood, reported Dr. Sterry, professor and chairman of the department of dermatology at Charité University Hospital, Berlin.
Of the five metabolic derangements used in defining the metabolic syndrome, four were significantly more prevalent in subjects with HS. They were 5.9-fold more likely than were matched controls to have central obesity, 4.1-fold more likely to have hyperglycemia, 4.6-fold more likely to have low HDL cholesterol, and 2.2-fold more likely to be hypertriglyceridemic. Hypertension was present in 48% of HS patients and 35% of controls, a difference that did not achieve statistical significance.
Of note, HS patients with metabolic syndrome had more pronounced metabolic abnormalities than did controls with metabolic syndrome. While the definition of metabolic syndrome requires the presence of at least three of five metabolic alterations, half of all HS patients with metabolic syndrome met four or more of the criteria, compared with 39% of controls.
Moreover, metabolic syndrome occurred at a much younger age in subjects with HS than is typical in the general population or than was seen in controls. Indeed, 40% of HS patients under age 35 had metabolic syndrome, compared with none of the matched controls. Thus, the odds ratio for metabolic syndrome in HS patients aged 34 years or less was increased more than 20-fold compared with controls, while in the 35- to 44-year-old age group it was increased 6.2-fold, and in HS patients aged 45 and older it was 2-fold higher.
An increased prevalence of metabolic syndrome also has been documented in patients with psoriasis. But the prevalence of metabolic syndrome appears to be higher in HS patients and the metabolic disorder occurs at an earlier age than in psoriasis.
There was no correlation between duration or severity of HS and the prevalence of metabolic syndrome, according to Dr. Sterry. That’s an important message for physicians who see patients with the skin disease because it means such patients should be evaluated for metabolic syndrome early on, even if they have only moderate skin disease. After all, the elements of the metabolic syndrome are modifiable cardiovascular risk factors.
The lack of correlation between HS severity or duration and metabolic syndrome prevalence also has implications for the mechanism underlying the increased risk of metabolic syndrome in HS. When Dr. Sterry and coworkers compared the levels of metabolic syndrome parameters in the 42 patients with prior surgical treatment of their HS to the 38 patients who had not undergone surgery, they found no significant differences even though the surgical patients presumably had less inflammatory load. This led them to speculate that chronic inflammation may not be the major driver of the metabolic abnormalities in HS patients.
"It must be that a genetic predisposition for metabolic syndrome then induces the development of acne inversa [hidradenitis suppurativa] in predisposed individuals," Dr. Sterry said.
The proposed mechanism involves metabolic syndrome–induced poor blood circulation in the intertriginous axillary, perianal, and inguinal skin where HS most often occurs, with resultant increased interleukin-10 production by CD4-positive T cells. Interleukin-10, in turn, inhibits keratinocyte production of interleukins-20 and -22, which induce antimicrobial proteins in the skin. This would set the stage for HS, which is characterized by bacterial persistence in obstructed hair follicles, nodules, and fistulating sinuses.
Of course, this is speculation, Dr. Sterry was quick to acknowledge.
"Acne inversa is also known as hidradenitis suppurativa, apocrine acne, pyoderma fistulans significa ... If a disease has that many names, that’s always a sign that we don’t know too much about it," the dermatologist observed.
In a separate study presented at the EADV, investigators found that the most common comorbid conditions in a cohort of 154 patients with HS enrolled in a clinical trial of adalimumab (Humira) therapy were depression as defined by a score of 10 or more on the Patient Health Questionnaire–9, which had a prevalence of 42%; severe obesity marked by a body mass index of at least 40 kg/m2, present in 28% of patients; and uncontrolled hypertension, which was present in 27%. However, the investigators did not look at metabolic syndrome.
Dr. Sterry reported having no financial conflicts regarding this unfunded case-control study.
To earn 0.25 hours AMA PRA Category 1 credit after reading this article, take the post-test here.
AT THE EADV CONGRESS
Hidradenitis suppurativa linked to metabolic syndrome
ISTANBUL, TURKEY – Patients with hidradenitis suppurativa have a sharply increased prevalence of the metabolic syndrome, according to the first case-control study to examine the relationship.
Metabolic syndrome is known to be associated with increased cardiovascular risk, which may be particularly high in patients with hidradenitis suppurativa (HS), a dermatologic disease with an estimated prevalence of 1%-4%, because they develop metabolic syndrome at a much younger age than do individuals without the dermatologic disease, Dr. Wolfram Sterry said at the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights from a single-center, case-control study that comprised 80 patients with HS with a mean 12-year disease duration and 100 age- and gender-matched controls. Patients’ mean age was 40 years (PLoS One 2012 [doi:10.1371/journal.pone.0031810]).
The prevalence of metabolic syndrome was 40% in the HS group and 13% in controls, for an adjusted 4.5-fold increased likelihood, reported Dr. Sterry, professor and chairman of the department of dermatology at Charité University Hospital, Berlin.
Of the five metabolic derangements used in defining the metabolic syndrome, four were significantly more prevalent in subjects with HS. They were 5.9-fold more likely than were matched controls to have central obesity, 4.1-fold more likely to have hyperglycemia, 4.6-fold more likely to have low HDL cholesterol, and 2.2-fold more likely to be hypertriglyceridemic. Hypertension was present in 48% of HS patients and 35% of controls, a difference that did not achieve statistical significance.
Of note, HS patients with metabolic syndrome had more pronounced metabolic abnormalities than did controls with metabolic syndrome. While the definition of metabolic syndrome requires the presence of at least three of five metabolic alterations, half of all HS patients with metabolic syndrome met four or more of the criteria, compared with 39% of controls.
Moreover, metabolic syndrome occurred at a much younger age in subjects with HS than is typical in the general population or than was seen in controls. Indeed, 40% of HS patients under age 35 had metabolic syndrome, compared with none of the matched controls. Thus, the odds ratio for metabolic syndrome in HS patients aged 34 years or less was increased more than 20-fold compared with controls, while in the 35- to 44-year-old age group it was increased 6.2-fold, and in HS patients aged 45 and older it was 2-fold higher.
An increased prevalence of metabolic syndrome also has been documented in patients with psoriasis. But the prevalence of metabolic syndrome appears to be higher in HS patients and the metabolic disorder occurs at an earlier age than in psoriasis.
There was no correlation between duration or severity of HS and the prevalence of metabolic syndrome, according to Dr. Sterry. That’s an important message for physicians who see patients with the skin disease because it means such patients should be evaluated for metabolic syndrome early on, even if they have only moderate skin disease. After all, the elements of the metabolic syndrome are modifiable cardiovascular risk factors.
The lack of correlation between HS severity or duration and metabolic syndrome prevalence also has implications for the mechanism underlying the increased risk of metabolic syndrome in HS. When Dr. Sterry and coworkers compared the levels of metabolic syndrome parameters in the 42 patients with prior surgical treatment of their HS to the 38 patients who had not undergone surgery, they found no significant differences even though the surgical patients presumably had less inflammatory load. This led them to speculate that chronic inflammation may not be the major driver of the metabolic abnormalities in HS patients.
"It must be that a genetic predisposition for metabolic syndrome then induces the development of acne inversa [hidradenitis suppurativa] in predisposed individuals," Dr. Sterry said.
The proposed mechanism involves metabolic syndrome–induced poor blood circulation in the intertriginous axillary, perianal, and inguinal skin where HS most often occurs, with resultant increased interleukin-10 production by CD4-positive T cells. Interleukin-10, in turn, inhibits keratinocyte production of interleukins-20 and -22, which induce antimicrobial proteins in the skin. This would set the stage for HS, which is characterized by bacterial persistence in obstructed hair follicles, nodules, and fistulating sinuses.
Of course, this is speculation, Dr. Sterry was quick to acknowledge.
"Acne inversa is also known as hidradenitis suppurativa, apocrine acne, pyoderma fistulans significa ... If a disease has that many names, that’s always a sign that we don’t know too much about it," the dermatologist observed.
In a separate study presented at the EADV, investigators found that the most common comorbid conditions in a cohort of 154 patients with HS enrolled in a clinical trial of adalimumab (Humira) therapy were depression as defined by a score of 10 or more on the Patient Health Questionnaire–9, which had a prevalence of 42%; severe obesity marked by a body mass index of at least 40 kg/m2, present in 28% of patients; and uncontrolled hypertension, which was present in 27%. However, the investigators did not look at metabolic syndrome.
Dr. Sterry reported having no financial conflicts regarding this unfunded case-control study.
ISTANBUL, TURKEY – Patients with hidradenitis suppurativa have a sharply increased prevalence of the metabolic syndrome, according to the first case-control study to examine the relationship.
Metabolic syndrome is known to be associated with increased cardiovascular risk, which may be particularly high in patients with hidradenitis suppurativa (HS), a dermatologic disease with an estimated prevalence of 1%-4%, because they develop metabolic syndrome at a much younger age than do individuals without the dermatologic disease, Dr. Wolfram Sterry said at the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights from a single-center, case-control study that comprised 80 patients with HS with a mean 12-year disease duration and 100 age- and gender-matched controls. Patients’ mean age was 40 years (PLoS One 2012 [doi:10.1371/journal.pone.0031810]).
The prevalence of metabolic syndrome was 40% in the HS group and 13% in controls, for an adjusted 4.5-fold increased likelihood, reported Dr. Sterry, professor and chairman of the department of dermatology at Charité University Hospital, Berlin.
Of the five metabolic derangements used in defining the metabolic syndrome, four were significantly more prevalent in subjects with HS. They were 5.9-fold more likely than were matched controls to have central obesity, 4.1-fold more likely to have hyperglycemia, 4.6-fold more likely to have low HDL cholesterol, and 2.2-fold more likely to be hypertriglyceridemic. Hypertension was present in 48% of HS patients and 35% of controls, a difference that did not achieve statistical significance.
Of note, HS patients with metabolic syndrome had more pronounced metabolic abnormalities than did controls with metabolic syndrome. While the definition of metabolic syndrome requires the presence of at least three of five metabolic alterations, half of all HS patients with metabolic syndrome met four or more of the criteria, compared with 39% of controls.
Moreover, metabolic syndrome occurred at a much younger age in subjects with HS than is typical in the general population or than was seen in controls. Indeed, 40% of HS patients under age 35 had metabolic syndrome, compared with none of the matched controls. Thus, the odds ratio for metabolic syndrome in HS patients aged 34 years or less was increased more than 20-fold compared with controls, while in the 35- to 44-year-old age group it was increased 6.2-fold, and in HS patients aged 45 and older it was 2-fold higher.
An increased prevalence of metabolic syndrome also has been documented in patients with psoriasis. But the prevalence of metabolic syndrome appears to be higher in HS patients and the metabolic disorder occurs at an earlier age than in psoriasis.
There was no correlation between duration or severity of HS and the prevalence of metabolic syndrome, according to Dr. Sterry. That’s an important message for physicians who see patients with the skin disease because it means such patients should be evaluated for metabolic syndrome early on, even if they have only moderate skin disease. After all, the elements of the metabolic syndrome are modifiable cardiovascular risk factors.
The lack of correlation between HS severity or duration and metabolic syndrome prevalence also has implications for the mechanism underlying the increased risk of metabolic syndrome in HS. When Dr. Sterry and coworkers compared the levels of metabolic syndrome parameters in the 42 patients with prior surgical treatment of their HS to the 38 patients who had not undergone surgery, they found no significant differences even though the surgical patients presumably had less inflammatory load. This led them to speculate that chronic inflammation may not be the major driver of the metabolic abnormalities in HS patients.
"It must be that a genetic predisposition for metabolic syndrome then induces the development of acne inversa [hidradenitis suppurativa] in predisposed individuals," Dr. Sterry said.
The proposed mechanism involves metabolic syndrome–induced poor blood circulation in the intertriginous axillary, perianal, and inguinal skin where HS most often occurs, with resultant increased interleukin-10 production by CD4-positive T cells. Interleukin-10, in turn, inhibits keratinocyte production of interleukins-20 and -22, which induce antimicrobial proteins in the skin. This would set the stage for HS, which is characterized by bacterial persistence in obstructed hair follicles, nodules, and fistulating sinuses.
Of course, this is speculation, Dr. Sterry was quick to acknowledge.
"Acne inversa is also known as hidradenitis suppurativa, apocrine acne, pyoderma fistulans significa ... If a disease has that many names, that’s always a sign that we don’t know too much about it," the dermatologist observed.
In a separate study presented at the EADV, investigators found that the most common comorbid conditions in a cohort of 154 patients with HS enrolled in a clinical trial of adalimumab (Humira) therapy were depression as defined by a score of 10 or more on the Patient Health Questionnaire–9, which had a prevalence of 42%; severe obesity marked by a body mass index of at least 40 kg/m2, present in 28% of patients; and uncontrolled hypertension, which was present in 27%. However, the investigators did not look at metabolic syndrome.
Dr. Sterry reported having no financial conflicts regarding this unfunded case-control study.
ISTANBUL, TURKEY – Patients with hidradenitis suppurativa have a sharply increased prevalence of the metabolic syndrome, according to the first case-control study to examine the relationship.
Metabolic syndrome is known to be associated with increased cardiovascular risk, which may be particularly high in patients with hidradenitis suppurativa (HS), a dermatologic disease with an estimated prevalence of 1%-4%, because they develop metabolic syndrome at a much younger age than do individuals without the dermatologic disease, Dr. Wolfram Sterry said at the annual congress of the European Academy of Dermatology and Venereology.
He presented highlights from a single-center, case-control study that comprised 80 patients with HS with a mean 12-year disease duration and 100 age- and gender-matched controls. Patients’ mean age was 40 years (PLoS One 2012 [doi:10.1371/journal.pone.0031810]).
The prevalence of metabolic syndrome was 40% in the HS group and 13% in controls, for an adjusted 4.5-fold increased likelihood, reported Dr. Sterry, professor and chairman of the department of dermatology at Charité University Hospital, Berlin.
Of the five metabolic derangements used in defining the metabolic syndrome, four were significantly more prevalent in subjects with HS. They were 5.9-fold more likely than were matched controls to have central obesity, 4.1-fold more likely to have hyperglycemia, 4.6-fold more likely to have low HDL cholesterol, and 2.2-fold more likely to be hypertriglyceridemic. Hypertension was present in 48% of HS patients and 35% of controls, a difference that did not achieve statistical significance.
Of note, HS patients with metabolic syndrome had more pronounced metabolic abnormalities than did controls with metabolic syndrome. While the definition of metabolic syndrome requires the presence of at least three of five metabolic alterations, half of all HS patients with metabolic syndrome met four or more of the criteria, compared with 39% of controls.
Moreover, metabolic syndrome occurred at a much younger age in subjects with HS than is typical in the general population or than was seen in controls. Indeed, 40% of HS patients under age 35 had metabolic syndrome, compared with none of the matched controls. Thus, the odds ratio for metabolic syndrome in HS patients aged 34 years or less was increased more than 20-fold compared with controls, while in the 35- to 44-year-old age group it was increased 6.2-fold, and in HS patients aged 45 and older it was 2-fold higher.
An increased prevalence of metabolic syndrome also has been documented in patients with psoriasis. But the prevalence of metabolic syndrome appears to be higher in HS patients and the metabolic disorder occurs at an earlier age than in psoriasis.
There was no correlation between duration or severity of HS and the prevalence of metabolic syndrome, according to Dr. Sterry. That’s an important message for physicians who see patients with the skin disease because it means such patients should be evaluated for metabolic syndrome early on, even if they have only moderate skin disease. After all, the elements of the metabolic syndrome are modifiable cardiovascular risk factors.
The lack of correlation between HS severity or duration and metabolic syndrome prevalence also has implications for the mechanism underlying the increased risk of metabolic syndrome in HS. When Dr. Sterry and coworkers compared the levels of metabolic syndrome parameters in the 42 patients with prior surgical treatment of their HS to the 38 patients who had not undergone surgery, they found no significant differences even though the surgical patients presumably had less inflammatory load. This led them to speculate that chronic inflammation may not be the major driver of the metabolic abnormalities in HS patients.
"It must be that a genetic predisposition for metabolic syndrome then induces the development of acne inversa [hidradenitis suppurativa] in predisposed individuals," Dr. Sterry said.
The proposed mechanism involves metabolic syndrome–induced poor blood circulation in the intertriginous axillary, perianal, and inguinal skin where HS most often occurs, with resultant increased interleukin-10 production by CD4-positive T cells. Interleukin-10, in turn, inhibits keratinocyte production of interleukins-20 and -22, which induce antimicrobial proteins in the skin. This would set the stage for HS, which is characterized by bacterial persistence in obstructed hair follicles, nodules, and fistulating sinuses.
Of course, this is speculation, Dr. Sterry was quick to acknowledge.
"Acne inversa is also known as hidradenitis suppurativa, apocrine acne, pyoderma fistulans significa ... If a disease has that many names, that’s always a sign that we don’t know too much about it," the dermatologist observed.
In a separate study presented at the EADV, investigators found that the most common comorbid conditions in a cohort of 154 patients with HS enrolled in a clinical trial of adalimumab (Humira) therapy were depression as defined by a score of 10 or more on the Patient Health Questionnaire–9, which had a prevalence of 42%; severe obesity marked by a body mass index of at least 40 kg/m2, present in 28% of patients; and uncontrolled hypertension, which was present in 27%. However, the investigators did not look at metabolic syndrome.
Dr. Sterry reported having no financial conflicts regarding this unfunded case-control study.
AT THE EADV CONGRESS
Major finding: The prevalence of metabolic syndrome was 40% in a cohort of patients with hidradenitis suppurativa compared with 13% in matched controls.
Data source: A case-control study involving 80 patients with hidradenitis suppurativa and 100 age- and gender-matched controls.
Disclosures: Dr. Sterry, the presenter of this unfunded investigation, reported having no financial conflicts of interest.
Fixed maintenance secukinumab beats as-needed dosing
ISTANBUL – Psoriasis patients who initially achieve a high-level response to secukinumab are significantly more likely to retain it over the long haul if they follow a fixed maintenance therapy schedule of once-monthly subcutaneous dosing rather than dosing as needed in the event of the start of relapse, according to the phase III SCULPTURE trial.
Secukinumab is an investigational fully human IgG1 monoclonal antibody targeting interleukin-17A, a key player in psoriasis, because it generates downstream proinflammatory cytokines and stimulates keratinocyte growth. Earlier studies indicated the investigational biologic had unprecedented clinical efficacy and rapidity of response. These observations gave rise to the hypothesis in SCULPTURE that maintenance dosing as needed upon relapse would prove noninferior to conventional fixed once-monthly maintenance therapy.
If the study hypothesis proved valid, it would mean less exposure to potential medication side effects, lower drug costs, and greater patient convenience. However, the hypothesis wasn’t borne out in the 966-patient, double-blind, randomized SCULPTURE (Study Comparing Retreatment Upon Start of Relapse), Dr. Ulrich Mrowietz reported at the annual congress of the European Academy of Dermatology and Venereology.
SCULPTURE participants had moderate-to-severe chronic plaque psoriasis despite prior systemic therapies, including biologic agents in many cases. They were randomized double blind to induction therapy involving five once-weekly subcutaneous injections of secukinumab at either 150 or 300 mg. At week 8, 843 participants with a Psoriasis Area and Severity Index (PASI) 75 response were re-randomized to maintenance therapy at the same dose, to be delivered either once monthly or as needed for relapse. The definition of relapse in this study required two elements: loss of PASI 75 response, and at least a 20% fall from the maximum PASI improvement, compared with baseline.
At week 52, 78.2% of patients randomized to 300 mg of secukinumab on a fixed once-monthly schedule still maintained a PASI 75 response. This was a significantly better outcome than the 67.7% PASI 75 rate in patients assigned to secukinumab 300 mg as needed, the 62.1% rate in those on secukinumab 150 mg once monthly, and the 52% PASI 75 rate in patients on secukinumab 150 mg as needed, reported Dr. Mrowietz of the University Medical Center Schleswig-Holstein, Kiel (Germany).
He found a bright spot in the negative results: While patients assigned to as-needed maintenance therapy achieved roughly an absolute 10% lower PASI 75 rate at 1 year, those in the secukinumab 150-mg group did so with only 46% the number of doses received by patients in the fixed monthly therapy group, while those in the retreatment-as-needed with secukinumab 300-mg group got only 39% of the number of doses, compared with patients on fixed monthly therapy.
"Fixed monthly dosing is the best maintenance regimen. But, in selected patients, there may be an opportunity with secukinumab to deviate from the usual fixed dosing regimen in favor of an as-needed approach," he said.
This tradeoff of an absolute 10% reduction in efficacy in return for a dosing regimen that entails less than half as much medication over the course of a year could prove of interest to payers, he noted.
The key, according to Dr. Mrowietz, will be to try to identify criteria helpful in selecting patients with an increased likelihood of a high-level response to the retreat-as-needed management strategy. The phase III trial was completed so recently that those necessary subanalyses have yet to be done.
However, Dr. Kristian Reich, another investigator involved in the secukinumab clinical trials program, drew a different message from SCULPTURE. He observed that these newer biologic agents are so effective that the bar has been raised with regard to patient expectations. Many patients won’t be satisfied with a PASI 75 response once a PASI 90 is achievable. And with fixed monthly maintenance secukinumab, it often is.
Indeed, the week-52 PASI 90 rate in SCULPTURE was a highly robust 59.7% in patients on fixed monthly secukinumab 300 mg and 45.8% for fixed monthly low-dose therapy, compared with the unimpressive 13.8% and 11.2% PASI 90 rates with high- and low-dose as-needed therapy.
"My take from this is that the best way to use this drug for continuous disease control is to give the drug every 4 weeks. What this study tells us is for those patients where you have to stop, where you have to use on-and-off therapy because they go away for 2 months to Africa, or they have a major operation, or for other reasons, these data are reassuring that we can use the drug safely on an intermittent basis," said Dr. Reich of Georg-August University in Göttingen, Germany.
Prior to SCULPTURE, he and other investigators were concerned that intermittent secukinumab therapy might promote the development of harmful antidrug antibodies. But antidrug antibodies arose in only three patients on fixed monthly maintenance therapy and two patients on as-needed therapy, and had no impact upon clinical efficacy or safety, he noted.
Another phase III trial presented in Istanbul was ERASURE (Efficacy and Safety of Subcutaneous Secukinumab for Moderate to Severe Chronic Plaque-Type Psoriasis for Up to 1 Year). Dr. Boni E. Elewski reported on 738 patients with moderate-to-severe chronic plaque psoriasis who were randomized double blind to secukinumab at 150 mg or 300 mg, or to placebo. Participants averaged a PASI score of 22 at baseline, along with 33% body surface area involvement. Psoriatic arthritis was present in 23% of subjects.
The co-primary endpoints in ERASURE were the week 12 PASI 75 response rates and Investigator’s Global Assessment scores of 0/1, indicative of clear or almost clear on a modified 5-point scale. The week-12 PASI 75 rates were 81.6% in the secukinumab 300 mg group, 71.6% with secukinumab 150 mg, and 4.5% with placebo. The week-12 IGA 0/1 rates were 65.3%, 51.2%, and 2.4%, said Dr. Elewski of the University of Alabama, Birmingham.
Among the other notable findings in ERASURE were the 69.8% PASI 90 and 41.6% PASI 100 responses at week 16 in the group assigned to secukinumab 300 mg, the fact that only one patient, on secukinumab 150 mg, developed transient antidrug antibodies, and the complete absence of cardiovascular events during 52 weeks on secukinumab, observed Dr. Elewski, professor of dermatology at the University of Alabama, Birmingham.
Dr. Mrowietz, Dr. Reich, and Dr. Elewski reported having received research grants from and serving as consultants to Novartis, which sponsored the secukinumab clinical trials program. The dermatologists serve in similar capacities with other pharmaceutical companies developing new medications for psoriasis.
ISTANBUL – Psoriasis patients who initially achieve a high-level response to secukinumab are significantly more likely to retain it over the long haul if they follow a fixed maintenance therapy schedule of once-monthly subcutaneous dosing rather than dosing as needed in the event of the start of relapse, according to the phase III SCULPTURE trial.
Secukinumab is an investigational fully human IgG1 monoclonal antibody targeting interleukin-17A, a key player in psoriasis, because it generates downstream proinflammatory cytokines and stimulates keratinocyte growth. Earlier studies indicated the investigational biologic had unprecedented clinical efficacy and rapidity of response. These observations gave rise to the hypothesis in SCULPTURE that maintenance dosing as needed upon relapse would prove noninferior to conventional fixed once-monthly maintenance therapy.
If the study hypothesis proved valid, it would mean less exposure to potential medication side effects, lower drug costs, and greater patient convenience. However, the hypothesis wasn’t borne out in the 966-patient, double-blind, randomized SCULPTURE (Study Comparing Retreatment Upon Start of Relapse), Dr. Ulrich Mrowietz reported at the annual congress of the European Academy of Dermatology and Venereology.
SCULPTURE participants had moderate-to-severe chronic plaque psoriasis despite prior systemic therapies, including biologic agents in many cases. They were randomized double blind to induction therapy involving five once-weekly subcutaneous injections of secukinumab at either 150 or 300 mg. At week 8, 843 participants with a Psoriasis Area and Severity Index (PASI) 75 response were re-randomized to maintenance therapy at the same dose, to be delivered either once monthly or as needed for relapse. The definition of relapse in this study required two elements: loss of PASI 75 response, and at least a 20% fall from the maximum PASI improvement, compared with baseline.
At week 52, 78.2% of patients randomized to 300 mg of secukinumab on a fixed once-monthly schedule still maintained a PASI 75 response. This was a significantly better outcome than the 67.7% PASI 75 rate in patients assigned to secukinumab 300 mg as needed, the 62.1% rate in those on secukinumab 150 mg once monthly, and the 52% PASI 75 rate in patients on secukinumab 150 mg as needed, reported Dr. Mrowietz of the University Medical Center Schleswig-Holstein, Kiel (Germany).
He found a bright spot in the negative results: While patients assigned to as-needed maintenance therapy achieved roughly an absolute 10% lower PASI 75 rate at 1 year, those in the secukinumab 150-mg group did so with only 46% the number of doses received by patients in the fixed monthly therapy group, while those in the retreatment-as-needed with secukinumab 300-mg group got only 39% of the number of doses, compared with patients on fixed monthly therapy.
"Fixed monthly dosing is the best maintenance regimen. But, in selected patients, there may be an opportunity with secukinumab to deviate from the usual fixed dosing regimen in favor of an as-needed approach," he said.
This tradeoff of an absolute 10% reduction in efficacy in return for a dosing regimen that entails less than half as much medication over the course of a year could prove of interest to payers, he noted.
The key, according to Dr. Mrowietz, will be to try to identify criteria helpful in selecting patients with an increased likelihood of a high-level response to the retreat-as-needed management strategy. The phase III trial was completed so recently that those necessary subanalyses have yet to be done.
However, Dr. Kristian Reich, another investigator involved in the secukinumab clinical trials program, drew a different message from SCULPTURE. He observed that these newer biologic agents are so effective that the bar has been raised with regard to patient expectations. Many patients won’t be satisfied with a PASI 75 response once a PASI 90 is achievable. And with fixed monthly maintenance secukinumab, it often is.
Indeed, the week-52 PASI 90 rate in SCULPTURE was a highly robust 59.7% in patients on fixed monthly secukinumab 300 mg and 45.8% for fixed monthly low-dose therapy, compared with the unimpressive 13.8% and 11.2% PASI 90 rates with high- and low-dose as-needed therapy.
"My take from this is that the best way to use this drug for continuous disease control is to give the drug every 4 weeks. What this study tells us is for those patients where you have to stop, where you have to use on-and-off therapy because they go away for 2 months to Africa, or they have a major operation, or for other reasons, these data are reassuring that we can use the drug safely on an intermittent basis," said Dr. Reich of Georg-August University in Göttingen, Germany.
Prior to SCULPTURE, he and other investigators were concerned that intermittent secukinumab therapy might promote the development of harmful antidrug antibodies. But antidrug antibodies arose in only three patients on fixed monthly maintenance therapy and two patients on as-needed therapy, and had no impact upon clinical efficacy or safety, he noted.
Another phase III trial presented in Istanbul was ERASURE (Efficacy and Safety of Subcutaneous Secukinumab for Moderate to Severe Chronic Plaque-Type Psoriasis for Up to 1 Year). Dr. Boni E. Elewski reported on 738 patients with moderate-to-severe chronic plaque psoriasis who were randomized double blind to secukinumab at 150 mg or 300 mg, or to placebo. Participants averaged a PASI score of 22 at baseline, along with 33% body surface area involvement. Psoriatic arthritis was present in 23% of subjects.
The co-primary endpoints in ERASURE were the week 12 PASI 75 response rates and Investigator’s Global Assessment scores of 0/1, indicative of clear or almost clear on a modified 5-point scale. The week-12 PASI 75 rates were 81.6% in the secukinumab 300 mg group, 71.6% with secukinumab 150 mg, and 4.5% with placebo. The week-12 IGA 0/1 rates were 65.3%, 51.2%, and 2.4%, said Dr. Elewski of the University of Alabama, Birmingham.
Among the other notable findings in ERASURE were the 69.8% PASI 90 and 41.6% PASI 100 responses at week 16 in the group assigned to secukinumab 300 mg, the fact that only one patient, on secukinumab 150 mg, developed transient antidrug antibodies, and the complete absence of cardiovascular events during 52 weeks on secukinumab, observed Dr. Elewski, professor of dermatology at the University of Alabama, Birmingham.
Dr. Mrowietz, Dr. Reich, and Dr. Elewski reported having received research grants from and serving as consultants to Novartis, which sponsored the secukinumab clinical trials program. The dermatologists serve in similar capacities with other pharmaceutical companies developing new medications for psoriasis.
ISTANBUL – Psoriasis patients who initially achieve a high-level response to secukinumab are significantly more likely to retain it over the long haul if they follow a fixed maintenance therapy schedule of once-monthly subcutaneous dosing rather than dosing as needed in the event of the start of relapse, according to the phase III SCULPTURE trial.
Secukinumab is an investigational fully human IgG1 monoclonal antibody targeting interleukin-17A, a key player in psoriasis, because it generates downstream proinflammatory cytokines and stimulates keratinocyte growth. Earlier studies indicated the investigational biologic had unprecedented clinical efficacy and rapidity of response. These observations gave rise to the hypothesis in SCULPTURE that maintenance dosing as needed upon relapse would prove noninferior to conventional fixed once-monthly maintenance therapy.
If the study hypothesis proved valid, it would mean less exposure to potential medication side effects, lower drug costs, and greater patient convenience. However, the hypothesis wasn’t borne out in the 966-patient, double-blind, randomized SCULPTURE (Study Comparing Retreatment Upon Start of Relapse), Dr. Ulrich Mrowietz reported at the annual congress of the European Academy of Dermatology and Venereology.
SCULPTURE participants had moderate-to-severe chronic plaque psoriasis despite prior systemic therapies, including biologic agents in many cases. They were randomized double blind to induction therapy involving five once-weekly subcutaneous injections of secukinumab at either 150 or 300 mg. At week 8, 843 participants with a Psoriasis Area and Severity Index (PASI) 75 response were re-randomized to maintenance therapy at the same dose, to be delivered either once monthly or as needed for relapse. The definition of relapse in this study required two elements: loss of PASI 75 response, and at least a 20% fall from the maximum PASI improvement, compared with baseline.
At week 52, 78.2% of patients randomized to 300 mg of secukinumab on a fixed once-monthly schedule still maintained a PASI 75 response. This was a significantly better outcome than the 67.7% PASI 75 rate in patients assigned to secukinumab 300 mg as needed, the 62.1% rate in those on secukinumab 150 mg once monthly, and the 52% PASI 75 rate in patients on secukinumab 150 mg as needed, reported Dr. Mrowietz of the University Medical Center Schleswig-Holstein, Kiel (Germany).
He found a bright spot in the negative results: While patients assigned to as-needed maintenance therapy achieved roughly an absolute 10% lower PASI 75 rate at 1 year, those in the secukinumab 150-mg group did so with only 46% the number of doses received by patients in the fixed monthly therapy group, while those in the retreatment-as-needed with secukinumab 300-mg group got only 39% of the number of doses, compared with patients on fixed monthly therapy.
"Fixed monthly dosing is the best maintenance regimen. But, in selected patients, there may be an opportunity with secukinumab to deviate from the usual fixed dosing regimen in favor of an as-needed approach," he said.
This tradeoff of an absolute 10% reduction in efficacy in return for a dosing regimen that entails less than half as much medication over the course of a year could prove of interest to payers, he noted.
The key, according to Dr. Mrowietz, will be to try to identify criteria helpful in selecting patients with an increased likelihood of a high-level response to the retreat-as-needed management strategy. The phase III trial was completed so recently that those necessary subanalyses have yet to be done.
However, Dr. Kristian Reich, another investigator involved in the secukinumab clinical trials program, drew a different message from SCULPTURE. He observed that these newer biologic agents are so effective that the bar has been raised with regard to patient expectations. Many patients won’t be satisfied with a PASI 75 response once a PASI 90 is achievable. And with fixed monthly maintenance secukinumab, it often is.
Indeed, the week-52 PASI 90 rate in SCULPTURE was a highly robust 59.7% in patients on fixed monthly secukinumab 300 mg and 45.8% for fixed monthly low-dose therapy, compared with the unimpressive 13.8% and 11.2% PASI 90 rates with high- and low-dose as-needed therapy.
"My take from this is that the best way to use this drug for continuous disease control is to give the drug every 4 weeks. What this study tells us is for those patients where you have to stop, where you have to use on-and-off therapy because they go away for 2 months to Africa, or they have a major operation, or for other reasons, these data are reassuring that we can use the drug safely on an intermittent basis," said Dr. Reich of Georg-August University in Göttingen, Germany.
Prior to SCULPTURE, he and other investigators were concerned that intermittent secukinumab therapy might promote the development of harmful antidrug antibodies. But antidrug antibodies arose in only three patients on fixed monthly maintenance therapy and two patients on as-needed therapy, and had no impact upon clinical efficacy or safety, he noted.
Another phase III trial presented in Istanbul was ERASURE (Efficacy and Safety of Subcutaneous Secukinumab for Moderate to Severe Chronic Plaque-Type Psoriasis for Up to 1 Year). Dr. Boni E. Elewski reported on 738 patients with moderate-to-severe chronic plaque psoriasis who were randomized double blind to secukinumab at 150 mg or 300 mg, or to placebo. Participants averaged a PASI score of 22 at baseline, along with 33% body surface area involvement. Psoriatic arthritis was present in 23% of subjects.
The co-primary endpoints in ERASURE were the week 12 PASI 75 response rates and Investigator’s Global Assessment scores of 0/1, indicative of clear or almost clear on a modified 5-point scale. The week-12 PASI 75 rates were 81.6% in the secukinumab 300 mg group, 71.6% with secukinumab 150 mg, and 4.5% with placebo. The week-12 IGA 0/1 rates were 65.3%, 51.2%, and 2.4%, said Dr. Elewski of the University of Alabama, Birmingham.
Among the other notable findings in ERASURE were the 69.8% PASI 90 and 41.6% PASI 100 responses at week 16 in the group assigned to secukinumab 300 mg, the fact that only one patient, on secukinumab 150 mg, developed transient antidrug antibodies, and the complete absence of cardiovascular events during 52 weeks on secukinumab, observed Dr. Elewski, professor of dermatology at the University of Alabama, Birmingham.
Dr. Mrowietz, Dr. Reich, and Dr. Elewski reported having received research grants from and serving as consultants to Novartis, which sponsored the secukinumab clinical trials program. The dermatologists serve in similar capacities with other pharmaceutical companies developing new medications for psoriasis.
AT THE EADV CONGRESS
Major finding: Among psoriasis patients who achieved a PASI 75 response to 5 weeks of induction therapy with subcutaneous secukinumab, 59.7% who were placed on a maintenance regimen of 300 mg every 4 weeks had a PASI 90 response at week 52, compared with 13.8% whose maintenance program involved taking 300 mg on an as-needed basis at the start of relapse.
Data source: The SCULPTURE study was a prospective, double-blind, 52-week, phase III clinical trial including 843 patients.
Disclosures: The study was sponsored by Novartis. Speakers reported having received research grants from and serving as consultants to the company.
Vismodegib prolongs positive response in advanced skin cancer
ISTANBUL – Vismodegib-treated patients with locally advanced basal cell carcinoma showed triple the median response duration after 24 months’ follow-up beyond the primary analysis of the drug, Dr. Luc Dirix reported at the annual congress of the European Academy of Dermatology and Venereology.
Vismodegib, the first-in-class oral medication for treatment of advanced BCC, showed a greatly improved duration of response and no new safety signals in updated results from the ERIVANCE BCC trial, which earlier had earned the drug marketing approval from the Food and Drug Administration and European Medicines Agency.
After 24 months beyond what was included in the primary analysis of ERIVANCE BCC (N. Engl. J. Med. 2012;366:2171-9), the median duration of response by investigator assessment in patients with locally advanced BCC increased from 7.6 to 26.2 months, and increased from 7.6 to 12.9 months in those with metastatic BCC.
"The main new fact is that the median duration of response has increased importantly. That’s a very impressive improvement in disease control, especially in patients with locally advanced disease. It’s a major change from what you’ll find in the New England Journal of Medicine publication," observed Dr. Dirix of Sint-AugustinusHospital, Antwerp, Belgium.
Dr. Dirix reported that, with the additional 24 months of follow-up in the ERIVANCE BCC study, median progression-free survival now stands at 9.3 months in the group with metastatic BCC and 12.9 months in those with locally advanced disease. The objective response rate, which was 43% in patients with locally advanced BCC and 30% in those with metastatic disease in the primary analysis, hasn’t changed significantly with the additional follow-up, he said.
The median overall survival was 33 months. Twelve of the original 33 patients in the cohort with metastatic BCC have died of progressive disease, as have 4 of 63 with locally advanced BCC.
The ERIVANCE BCC trial is an open-label, phase II study in which participants were placed on vismodegib at 150 mg once daily until the occurrence of disease progression, intolerable toxicity, or patient request to withdraw. At the latest follow-up, only 13% of the original study population remained on the drug, Dr. Dirix said. Half of the patients with metastatic BCC who discontinued the drug did so because of disease progression, but only 16% of those with locally advanced BCC stopped treatment. Instead, side effects were the main reason locally advanced BCC patients discontinued therapy.
"The additional 24 months of follow-up didn’t result in any new safety signal, but there are numerous side effects, especially muscle spasms, alopecia, dysgeusia, and others, mostly mild or moderate," said Dr. Dirix.
An estimated 1.6 million new cases of BCC were diagnosed in the United States in 2006, making it the most common form of cancer in the country. Most BCCs are readily treated. However, some cases can progress to locally advanced or metastatic BCC, a disfiguring and potentially life-threatening condition that is not treatable surgically or via radiation therapy, and for which no effective therapy existed before. Vismodegib (Erivedge) provides an oral drug option that works as an inhibitor of the hedgehog pathway, which plays a key role in the pathogenesis of most BCCs.
With vismodegib intended as lifelong treatment in patients with advanced BCC, and considerable research interest in exploring the drug in other forms of BCC, reliable safety data are needed. Also at the EADV Congress, Dr. Rainer Kunstfeld presented new safety information in an interim analysis from an ongoing study known as STEVIE (Safety Events in Vismodegib), the largest study of the hedgehog pathway inhibitor. His report included the first 300 of a planned 1,200 patients with advanced BCC to be placed on vismodegib.
The data underscore the point that advanced BCC is primarily a disease of the elderly. The mean age of the 278 patients with locally advanced BCC is 70 years, and 65 years in the 22 with metastatic BCC. The median treatment duration as of the data cutoff for this analysis was 5.8 months.
Forty-five percent of patients in the locally advanced BCC group have discontinued treatment, as have 32% of those with metastatic disease, Dr. Kunstfeld said. The reasons differed for the two groups. Discontinuation due to disease progression or death was more than twice as common in patients with metastatic BCC. Patients with locally advanced disease were much more likely to halt treatment because of adverse events.
Ninety-three percent of STEVIE participants experienced at least one adverse event. Roughly two-thirds of these side effects were mild or moderate – that is, grade 1 or 2 – while the remainder were grade 3. The incidence of the most common adverse events were muscle spasms in 59% of participants, alopecia in 49%, distorted sense of taste in 41%, loss of the sense of taste in 26%, asthenia in 23%, and weight loss in 16%. These data were consistent with the safety profile seen in the ERIVANCE BCC study, observed Dr. Kunstfeld, a dermatologist at the Medical University of Vienna.
Of the 251 patients with tumor assessments available to date, more than 95% showed some degree of therapeutic benefit. A complete response was documented in 17.5% of patients, a partial response in 39.8%, and 39% had stable disease. Fewer than 3% have experienced disease progression during this early follow-up period.
The ERIVANCE BCC and STEVIE studies are funded by Genentech. Dr. Dirix and Dr. Kunstfeld reported having no financial conflicts of interest.
ISTANBUL – Vismodegib-treated patients with locally advanced basal cell carcinoma showed triple the median response duration after 24 months’ follow-up beyond the primary analysis of the drug, Dr. Luc Dirix reported at the annual congress of the European Academy of Dermatology and Venereology.
Vismodegib, the first-in-class oral medication for treatment of advanced BCC, showed a greatly improved duration of response and no new safety signals in updated results from the ERIVANCE BCC trial, which earlier had earned the drug marketing approval from the Food and Drug Administration and European Medicines Agency.
After 24 months beyond what was included in the primary analysis of ERIVANCE BCC (N. Engl. J. Med. 2012;366:2171-9), the median duration of response by investigator assessment in patients with locally advanced BCC increased from 7.6 to 26.2 months, and increased from 7.6 to 12.9 months in those with metastatic BCC.
"The main new fact is that the median duration of response has increased importantly. That’s a very impressive improvement in disease control, especially in patients with locally advanced disease. It’s a major change from what you’ll find in the New England Journal of Medicine publication," observed Dr. Dirix of Sint-AugustinusHospital, Antwerp, Belgium.
Dr. Dirix reported that, with the additional 24 months of follow-up in the ERIVANCE BCC study, median progression-free survival now stands at 9.3 months in the group with metastatic BCC and 12.9 months in those with locally advanced disease. The objective response rate, which was 43% in patients with locally advanced BCC and 30% in those with metastatic disease in the primary analysis, hasn’t changed significantly with the additional follow-up, he said.
The median overall survival was 33 months. Twelve of the original 33 patients in the cohort with metastatic BCC have died of progressive disease, as have 4 of 63 with locally advanced BCC.
The ERIVANCE BCC trial is an open-label, phase II study in which participants were placed on vismodegib at 150 mg once daily until the occurrence of disease progression, intolerable toxicity, or patient request to withdraw. At the latest follow-up, only 13% of the original study population remained on the drug, Dr. Dirix said. Half of the patients with metastatic BCC who discontinued the drug did so because of disease progression, but only 16% of those with locally advanced BCC stopped treatment. Instead, side effects were the main reason locally advanced BCC patients discontinued therapy.
"The additional 24 months of follow-up didn’t result in any new safety signal, but there are numerous side effects, especially muscle spasms, alopecia, dysgeusia, and others, mostly mild or moderate," said Dr. Dirix.
An estimated 1.6 million new cases of BCC were diagnosed in the United States in 2006, making it the most common form of cancer in the country. Most BCCs are readily treated. However, some cases can progress to locally advanced or metastatic BCC, a disfiguring and potentially life-threatening condition that is not treatable surgically or via radiation therapy, and for which no effective therapy existed before. Vismodegib (Erivedge) provides an oral drug option that works as an inhibitor of the hedgehog pathway, which plays a key role in the pathogenesis of most BCCs.
With vismodegib intended as lifelong treatment in patients with advanced BCC, and considerable research interest in exploring the drug in other forms of BCC, reliable safety data are needed. Also at the EADV Congress, Dr. Rainer Kunstfeld presented new safety information in an interim analysis from an ongoing study known as STEVIE (Safety Events in Vismodegib), the largest study of the hedgehog pathway inhibitor. His report included the first 300 of a planned 1,200 patients with advanced BCC to be placed on vismodegib.
The data underscore the point that advanced BCC is primarily a disease of the elderly. The mean age of the 278 patients with locally advanced BCC is 70 years, and 65 years in the 22 with metastatic BCC. The median treatment duration as of the data cutoff for this analysis was 5.8 months.
Forty-five percent of patients in the locally advanced BCC group have discontinued treatment, as have 32% of those with metastatic disease, Dr. Kunstfeld said. The reasons differed for the two groups. Discontinuation due to disease progression or death was more than twice as common in patients with metastatic BCC. Patients with locally advanced disease were much more likely to halt treatment because of adverse events.
Ninety-three percent of STEVIE participants experienced at least one adverse event. Roughly two-thirds of these side effects were mild or moderate – that is, grade 1 or 2 – while the remainder were grade 3. The incidence of the most common adverse events were muscle spasms in 59% of participants, alopecia in 49%, distorted sense of taste in 41%, loss of the sense of taste in 26%, asthenia in 23%, and weight loss in 16%. These data were consistent with the safety profile seen in the ERIVANCE BCC study, observed Dr. Kunstfeld, a dermatologist at the Medical University of Vienna.
Of the 251 patients with tumor assessments available to date, more than 95% showed some degree of therapeutic benefit. A complete response was documented in 17.5% of patients, a partial response in 39.8%, and 39% had stable disease. Fewer than 3% have experienced disease progression during this early follow-up period.
The ERIVANCE BCC and STEVIE studies are funded by Genentech. Dr. Dirix and Dr. Kunstfeld reported having no financial conflicts of interest.
ISTANBUL – Vismodegib-treated patients with locally advanced basal cell carcinoma showed triple the median response duration after 24 months’ follow-up beyond the primary analysis of the drug, Dr. Luc Dirix reported at the annual congress of the European Academy of Dermatology and Venereology.
Vismodegib, the first-in-class oral medication for treatment of advanced BCC, showed a greatly improved duration of response and no new safety signals in updated results from the ERIVANCE BCC trial, which earlier had earned the drug marketing approval from the Food and Drug Administration and European Medicines Agency.
After 24 months beyond what was included in the primary analysis of ERIVANCE BCC (N. Engl. J. Med. 2012;366:2171-9), the median duration of response by investigator assessment in patients with locally advanced BCC increased from 7.6 to 26.2 months, and increased from 7.6 to 12.9 months in those with metastatic BCC.
"The main new fact is that the median duration of response has increased importantly. That’s a very impressive improvement in disease control, especially in patients with locally advanced disease. It’s a major change from what you’ll find in the New England Journal of Medicine publication," observed Dr. Dirix of Sint-AugustinusHospital, Antwerp, Belgium.
Dr. Dirix reported that, with the additional 24 months of follow-up in the ERIVANCE BCC study, median progression-free survival now stands at 9.3 months in the group with metastatic BCC and 12.9 months in those with locally advanced disease. The objective response rate, which was 43% in patients with locally advanced BCC and 30% in those with metastatic disease in the primary analysis, hasn’t changed significantly with the additional follow-up, he said.
The median overall survival was 33 months. Twelve of the original 33 patients in the cohort with metastatic BCC have died of progressive disease, as have 4 of 63 with locally advanced BCC.
The ERIVANCE BCC trial is an open-label, phase II study in which participants were placed on vismodegib at 150 mg once daily until the occurrence of disease progression, intolerable toxicity, or patient request to withdraw. At the latest follow-up, only 13% of the original study population remained on the drug, Dr. Dirix said. Half of the patients with metastatic BCC who discontinued the drug did so because of disease progression, but only 16% of those with locally advanced BCC stopped treatment. Instead, side effects were the main reason locally advanced BCC patients discontinued therapy.
"The additional 24 months of follow-up didn’t result in any new safety signal, but there are numerous side effects, especially muscle spasms, alopecia, dysgeusia, and others, mostly mild or moderate," said Dr. Dirix.
An estimated 1.6 million new cases of BCC were diagnosed in the United States in 2006, making it the most common form of cancer in the country. Most BCCs are readily treated. However, some cases can progress to locally advanced or metastatic BCC, a disfiguring and potentially life-threatening condition that is not treatable surgically or via radiation therapy, and for which no effective therapy existed before. Vismodegib (Erivedge) provides an oral drug option that works as an inhibitor of the hedgehog pathway, which plays a key role in the pathogenesis of most BCCs.
With vismodegib intended as lifelong treatment in patients with advanced BCC, and considerable research interest in exploring the drug in other forms of BCC, reliable safety data are needed. Also at the EADV Congress, Dr. Rainer Kunstfeld presented new safety information in an interim analysis from an ongoing study known as STEVIE (Safety Events in Vismodegib), the largest study of the hedgehog pathway inhibitor. His report included the first 300 of a planned 1,200 patients with advanced BCC to be placed on vismodegib.
The data underscore the point that advanced BCC is primarily a disease of the elderly. The mean age of the 278 patients with locally advanced BCC is 70 years, and 65 years in the 22 with metastatic BCC. The median treatment duration as of the data cutoff for this analysis was 5.8 months.
Forty-five percent of patients in the locally advanced BCC group have discontinued treatment, as have 32% of those with metastatic disease, Dr. Kunstfeld said. The reasons differed for the two groups. Discontinuation due to disease progression or death was more than twice as common in patients with metastatic BCC. Patients with locally advanced disease were much more likely to halt treatment because of adverse events.
Ninety-three percent of STEVIE participants experienced at least one adverse event. Roughly two-thirds of these side effects were mild or moderate – that is, grade 1 or 2 – while the remainder were grade 3. The incidence of the most common adverse events were muscle spasms in 59% of participants, alopecia in 49%, distorted sense of taste in 41%, loss of the sense of taste in 26%, asthenia in 23%, and weight loss in 16%. These data were consistent with the safety profile seen in the ERIVANCE BCC study, observed Dr. Kunstfeld, a dermatologist at the Medical University of Vienna.
Of the 251 patients with tumor assessments available to date, more than 95% showed some degree of therapeutic benefit. A complete response was documented in 17.5% of patients, a partial response in 39.8%, and 39% had stable disease. Fewer than 3% have experienced disease progression during this early follow-up period.
The ERIVANCE BCC and STEVIE studies are funded by Genentech. Dr. Dirix and Dr. Kunstfeld reported having no financial conflicts of interest.
AT THE EADV CONGRESS
Major finding: With an additional 24 months of follow-up of vismodegib-treated patients with advanced basal cell carcinoma beyond previous results from the ERIVANCE study, the median response duration in patients with locally advanced disease climbed from 7.6 to 26.2 months.
Data source: The ERIVANCE BCC study is an open-label trial in which 63 patients with locally advanced BCC and 33 with metastatic BCC were placed on oral vismodegib at 150 mg/day.
Disclosures: The ERIVANCE BCC and STEVIE studies are funded by Genentech. Dr. Dirix and Dr. Kunstfeld reported having no financial conflicts of interest.
Secukinumab soars in phase III psoriasis studies
ISTANBUL, TURKEY – The investigational interleukin-17A inhibitor secukinumab was the talk of Europe’s premier dermatology conference as a result of a series of world-premiere presentations of not one, but three, phase III clinical trials.
The entire secukinumab pivotal phase III program results were presented together at the annual congress of the European Academy of Dermatology and Venereology. Based on these promising results, Novartis plans to file for Food and Drug Administration and European regulatory approval before the end of 2013.
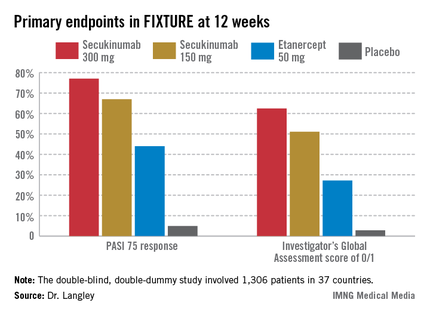
The three randomized, double-blind, multicenter pivotal trials of secukinumab in psoriasis collectively included 3,367 patients with moderate to severe chronic plaque psoriasis. All three studies were strongly positive. Efficacy rates were higher than with current biologics, clinical improvement was remarkably rapid, and the safety profile was reassuring.
"Those of us working in this area of research are really excited by this new data and what it says for the treatment of psoriasis patients," commented Dr. Richard Langley of Dalhousie University, Halifax, N.S.
He presented the centerpiece of this trio of phase III trials, known as the FIXTURE trial. FIXTURE (Full Year Investigative Examination of Secukinumab vs. Etanercept Using 2 Dosing Regimens to Determine Efficacy in Psoriasis) was a 1,306-patient, double-blind, double-dummy trial conducted by 153 investigators in 37 countries. The trial featured a 1-year head-to-head comparison of secukinumab and the widely prescribed tumor necrosis factor (TNF) inhibitor etanercept (Enbrel). The IL-17A inhibitor outperformed etanercept in all of the prespecified primary and secondary outcome measures. Moreover, the two biologics proved equally safe.
"I think it’s interesting in comparing these two molecules that when we look at the data to date, we see comparable safety results. Etanercept is one of the most widely used biologics and has an excellent safety record. That’s reassuring for those of us who are investigating IL-17 signaling," observed Dr. Langley, also the current president of the Canadian Dermatology Association.
FIXTURE participants had a mean baseline Psoriasis Area and Severity Index (PASI) score of 24, an average body mass index of 34 kg/m2, and a mean age in the mid-40s, and were previous inadequate responders to conventional systemic agents and/or biologics. The two co-primary endpoints were 12-week rates of at least a 75% reduction in PASI score, or PASI 75 response, and an Investigator’s Global Assessment (IGA) rating of 0/1, corresponding to clear or nearly clear, on a modified 5-point scale that provides more clinically meaningful information than the older 6-point IGA scale. Patients randomized to the secukinumab 300-mg or 150-mg groups did significantly better on both outcome measures than those assigned to etanercept.
The onset of benefit with secukinumab was swift; a statistically significant improvement compared with etanercept was seen within 2 weeks in terms of IGA scores and within 3 weeks for PASI 75. Secukinumab at 300 mg per subcutaneous injection – the most effective dose across all three pivotal trials – achieved roughly a 50% reduction in PASI scores after 3 weeks, compared with 8 weeks for etanercept, the dermatologist explained.
The PASI 75 response rate at 12 weeks was 77.1% in patients receiving secukinumab at 300 mg, 67% for those receiving secukinumab at 150 mg, 44% for etanercept 50 mg, and 4.9% for placebo.
The highest response rates with secukinumab were seen at week 16 rather than week 12. In the secukinumab 300-mg group, the PASI 75 rate at week 16 was 86.7%, with that high level of response being retained throughout the remainder of the 52-week study. In contrast, the PASI 75 rate at week 16 for etanercept was less than 60%. The IGA 0/1 rate at week 16 was 75.5% in the secukinumab 300-mg group and 60% with secukinumab 150 mg. The peak IGA 0/1 rate in the etanercept arm was only about 45%, and it came much later, at week 26.
Looking at more stringent secondary endpoints, the investigators found that a PASI 90 response was achieved by week 16 in 72.4% of the high-dose secukinumab group, compared with about 30% with etanercept. Twenty-four percent of patients on high-dose secukinumab had a PASI 100 response at week 12, compared with 4% on etanercept. By week 16, 36.8% of the high-dose secukinumab group had a PASI 100 response. At week 52, 65% of the secukinumab 300-mg group maintained a PASI 90 response, compared with 33% of the etanercept group.
The most common adverse event documented in FIXTURE was nasopharyngitis, which occurred in roughly one-third of patients in all four study arms. The serious infection rate was 1%-1.2% in all four study arms. No signals of an increase in malignancies or major adverse cardiovascular events were noted in any of the active treatment groups. Overall, adverse events were similar in both secukinumab arms and comparable to etanercept. Injection-site reactions occurred in 6.1% of the etanercept group and in none of the patients assigned to secukinumab or placebo.
The incidence of treatment-emergent antidrug antibodies in the secukinumab arms was 0.4%, and when it occurred, it had no impact on treatment efficacy or safety. Patients on etanercept weren’t tested for the emergence of antidrug antibodies.
Candida infections occurred in 4.7% of patients on secukinumab 300 mg, 2.3% of those on 150 mg, and 1.2% of the etanercept group. All cases in patients on secukinumab were mild or moderate and easily treated. Candida infections are a side effect of special interest because patients with a genetic defect in the IL-17 pathway can develop chronic mucocutaneous candidiasis. A theoretical concern that pharmacologic inhibition of IL-17 might create a big problem in this regard has not materialized.
The other two phase III secukinumab clinical trials presented in Istanbul – ERASURE and SCULPTURE – showed efficacy and safety results similar to those of FIXTURE. Unlike FIXTURE, neither of those trials featured a head-to-head comparison with another biologic.
These were the first completed phase III studies for any of the three biologics in this novel, highly promising class targeting IL-17 in the treatment of psoriasis and other immune-mediated inflammatory diseases. The other two agents in the pipeline targeting IL-17, brodalumab and ixekizumab, remain in ongoing phase III trials.
Because of the pivotal role IL-17 plays in generating inflammatory cytokines downstream, all three drugs are being studied for additional indications beyond psoriasis. For example, secukinumab, an IgG1 human monoclonal antibody, is in phase III clinical trials for psoriatic arthritis, ankylosing spondylitis, and rheumatoid arthritis, and in phase II for muscular sclerosis and asthma.
One audience member asked Dr. Langley for his thoughts regarding the absence of injection-site reactions in the secukinumab-treated patients. He replied that one obvious factor is that secukinumab injections are given much less frequently: once monthly during maintenance therapy as compared to once weekly with etanercept. In any event, he doesn’t consider injection-site reactions to be clinically relevant.
"Injection-site reactions don’t seem to be a major issue with any of the subcutaneous therapies. It has never in 15 years of using different biologics been an issue that’s made me stop treatment for a patient," he added.
Secukinumab was dosed at baseline, again weekly through week 4, then once monthly from week 8 through the study’s end. Etanercept was dosed at 50 mg twice weekly for 12 weeks, then once weekly in accord with the labeling instructions in most countries. Nonresponders at 12 weeks in the placebo arm were at that point randomized to secukinumab at 300 mg or 150 mg. The statistical analysis in FIXTURE was performed by nonresponder imputation.
"Those who are interested in statistics will know that that’s the most rigorous way that you can look at the data, because anybody who drops out of the study, whether they withdraw consent, have a protocol violation, or have an adverse event, even if they were responding at that time, are considered a failure or nonresponder," Dr. Langley explained.
Asked how he sees secukinumab fitting into patient management, Dr. Langley replied, "Most of us are forced to use conventional therapies and phototherapy to get approval for biologics, but after that I think the safety and efficacy of this drug put it right at the top. I could definitely use this drug as a first-line biologic for patients with plain psoriasis without psoriatic arthritis."
Coinvestigator Dr. Kristian Reich, professor of dermatology at Georg-August University in Göttingen, Germany, said he will probably continue to use TNF inhibitors in psoriasis patients with prominent arthritis, where he believes the TNF inhibitors are particularly beneficial, but he anticipates using secukinumab widely in others.
Dr. Bruce E. Strober, another active clinical trial researcher in psoriasis, said he likes what he sees in the IL-17 inhibitor data.
"I predict as a specialty we’ll become very confident in these drugs 5 years from now. A lot of us will be using them as first line in many patients. That’s my prediction. For now, though, I’m a big fan of TNF inhibition," added Dr. Strober, vice chair of dermatology at the University of Connecticut Medical Center, Farmington.
The secukinumab development program is sponsored by Novartis. Dr. Langley, Dr. Reich, and Dr. Strober disclosed having received research grants from and serving as consultants to Novartis and numerous other companies developing biologic agents for psoriasis.
ISTANBUL, TURKEY – The investigational interleukin-17A inhibitor secukinumab was the talk of Europe’s premier dermatology conference as a result of a series of world-premiere presentations of not one, but three, phase III clinical trials.
The entire secukinumab pivotal phase III program results were presented together at the annual congress of the European Academy of Dermatology and Venereology. Based on these promising results, Novartis plans to file for Food and Drug Administration and European regulatory approval before the end of 2013.
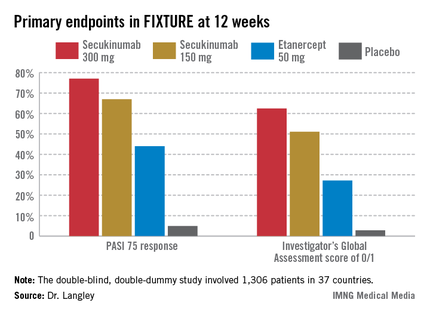
The three randomized, double-blind, multicenter pivotal trials of secukinumab in psoriasis collectively included 3,367 patients with moderate to severe chronic plaque psoriasis. All three studies were strongly positive. Efficacy rates were higher than with current biologics, clinical improvement was remarkably rapid, and the safety profile was reassuring.
"Those of us working in this area of research are really excited by this new data and what it says for the treatment of psoriasis patients," commented Dr. Richard Langley of Dalhousie University, Halifax, N.S.
He presented the centerpiece of this trio of phase III trials, known as the FIXTURE trial. FIXTURE (Full Year Investigative Examination of Secukinumab vs. Etanercept Using 2 Dosing Regimens to Determine Efficacy in Psoriasis) was a 1,306-patient, double-blind, double-dummy trial conducted by 153 investigators in 37 countries. The trial featured a 1-year head-to-head comparison of secukinumab and the widely prescribed tumor necrosis factor (TNF) inhibitor etanercept (Enbrel). The IL-17A inhibitor outperformed etanercept in all of the prespecified primary and secondary outcome measures. Moreover, the two biologics proved equally safe.
"I think it’s interesting in comparing these two molecules that when we look at the data to date, we see comparable safety results. Etanercept is one of the most widely used biologics and has an excellent safety record. That’s reassuring for those of us who are investigating IL-17 signaling," observed Dr. Langley, also the current president of the Canadian Dermatology Association.
FIXTURE participants had a mean baseline Psoriasis Area and Severity Index (PASI) score of 24, an average body mass index of 34 kg/m2, and a mean age in the mid-40s, and were previous inadequate responders to conventional systemic agents and/or biologics. The two co-primary endpoints were 12-week rates of at least a 75% reduction in PASI score, or PASI 75 response, and an Investigator’s Global Assessment (IGA) rating of 0/1, corresponding to clear or nearly clear, on a modified 5-point scale that provides more clinically meaningful information than the older 6-point IGA scale. Patients randomized to the secukinumab 300-mg or 150-mg groups did significantly better on both outcome measures than those assigned to etanercept.
The onset of benefit with secukinumab was swift; a statistically significant improvement compared with etanercept was seen within 2 weeks in terms of IGA scores and within 3 weeks for PASI 75. Secukinumab at 300 mg per subcutaneous injection – the most effective dose across all three pivotal trials – achieved roughly a 50% reduction in PASI scores after 3 weeks, compared with 8 weeks for etanercept, the dermatologist explained.
The PASI 75 response rate at 12 weeks was 77.1% in patients receiving secukinumab at 300 mg, 67% for those receiving secukinumab at 150 mg, 44% for etanercept 50 mg, and 4.9% for placebo.
The highest response rates with secukinumab were seen at week 16 rather than week 12. In the secukinumab 300-mg group, the PASI 75 rate at week 16 was 86.7%, with that high level of response being retained throughout the remainder of the 52-week study. In contrast, the PASI 75 rate at week 16 for etanercept was less than 60%. The IGA 0/1 rate at week 16 was 75.5% in the secukinumab 300-mg group and 60% with secukinumab 150 mg. The peak IGA 0/1 rate in the etanercept arm was only about 45%, and it came much later, at week 26.
Looking at more stringent secondary endpoints, the investigators found that a PASI 90 response was achieved by week 16 in 72.4% of the high-dose secukinumab group, compared with about 30% with etanercept. Twenty-four percent of patients on high-dose secukinumab had a PASI 100 response at week 12, compared with 4% on etanercept. By week 16, 36.8% of the high-dose secukinumab group had a PASI 100 response. At week 52, 65% of the secukinumab 300-mg group maintained a PASI 90 response, compared with 33% of the etanercept group.
The most common adverse event documented in FIXTURE was nasopharyngitis, which occurred in roughly one-third of patients in all four study arms. The serious infection rate was 1%-1.2% in all four study arms. No signals of an increase in malignancies or major adverse cardiovascular events were noted in any of the active treatment groups. Overall, adverse events were similar in both secukinumab arms and comparable to etanercept. Injection-site reactions occurred in 6.1% of the etanercept group and in none of the patients assigned to secukinumab or placebo.
The incidence of treatment-emergent antidrug antibodies in the secukinumab arms was 0.4%, and when it occurred, it had no impact on treatment efficacy or safety. Patients on etanercept weren’t tested for the emergence of antidrug antibodies.
Candida infections occurred in 4.7% of patients on secukinumab 300 mg, 2.3% of those on 150 mg, and 1.2% of the etanercept group. All cases in patients on secukinumab were mild or moderate and easily treated. Candida infections are a side effect of special interest because patients with a genetic defect in the IL-17 pathway can develop chronic mucocutaneous candidiasis. A theoretical concern that pharmacologic inhibition of IL-17 might create a big problem in this regard has not materialized.
The other two phase III secukinumab clinical trials presented in Istanbul – ERASURE and SCULPTURE – showed efficacy and safety results similar to those of FIXTURE. Unlike FIXTURE, neither of those trials featured a head-to-head comparison with another biologic.
These were the first completed phase III studies for any of the three biologics in this novel, highly promising class targeting IL-17 in the treatment of psoriasis and other immune-mediated inflammatory diseases. The other two agents in the pipeline targeting IL-17, brodalumab and ixekizumab, remain in ongoing phase III trials.
Because of the pivotal role IL-17 plays in generating inflammatory cytokines downstream, all three drugs are being studied for additional indications beyond psoriasis. For example, secukinumab, an IgG1 human monoclonal antibody, is in phase III clinical trials for psoriatic arthritis, ankylosing spondylitis, and rheumatoid arthritis, and in phase II for muscular sclerosis and asthma.
One audience member asked Dr. Langley for his thoughts regarding the absence of injection-site reactions in the secukinumab-treated patients. He replied that one obvious factor is that secukinumab injections are given much less frequently: once monthly during maintenance therapy as compared to once weekly with etanercept. In any event, he doesn’t consider injection-site reactions to be clinically relevant.
"Injection-site reactions don’t seem to be a major issue with any of the subcutaneous therapies. It has never in 15 years of using different biologics been an issue that’s made me stop treatment for a patient," he added.
Secukinumab was dosed at baseline, again weekly through week 4, then once monthly from week 8 through the study’s end. Etanercept was dosed at 50 mg twice weekly for 12 weeks, then once weekly in accord with the labeling instructions in most countries. Nonresponders at 12 weeks in the placebo arm were at that point randomized to secukinumab at 300 mg or 150 mg. The statistical analysis in FIXTURE was performed by nonresponder imputation.
"Those who are interested in statistics will know that that’s the most rigorous way that you can look at the data, because anybody who drops out of the study, whether they withdraw consent, have a protocol violation, or have an adverse event, even if they were responding at that time, are considered a failure or nonresponder," Dr. Langley explained.
Asked how he sees secukinumab fitting into patient management, Dr. Langley replied, "Most of us are forced to use conventional therapies and phototherapy to get approval for biologics, but after that I think the safety and efficacy of this drug put it right at the top. I could definitely use this drug as a first-line biologic for patients with plain psoriasis without psoriatic arthritis."
Coinvestigator Dr. Kristian Reich, professor of dermatology at Georg-August University in Göttingen, Germany, said he will probably continue to use TNF inhibitors in psoriasis patients with prominent arthritis, where he believes the TNF inhibitors are particularly beneficial, but he anticipates using secukinumab widely in others.
Dr. Bruce E. Strober, another active clinical trial researcher in psoriasis, said he likes what he sees in the IL-17 inhibitor data.
"I predict as a specialty we’ll become very confident in these drugs 5 years from now. A lot of us will be using them as first line in many patients. That’s my prediction. For now, though, I’m a big fan of TNF inhibition," added Dr. Strober, vice chair of dermatology at the University of Connecticut Medical Center, Farmington.
The secukinumab development program is sponsored by Novartis. Dr. Langley, Dr. Reich, and Dr. Strober disclosed having received research grants from and serving as consultants to Novartis and numerous other companies developing biologic agents for psoriasis.
ISTANBUL, TURKEY – The investigational interleukin-17A inhibitor secukinumab was the talk of Europe’s premier dermatology conference as a result of a series of world-premiere presentations of not one, but three, phase III clinical trials.
The entire secukinumab pivotal phase III program results were presented together at the annual congress of the European Academy of Dermatology and Venereology. Based on these promising results, Novartis plans to file for Food and Drug Administration and European regulatory approval before the end of 2013.
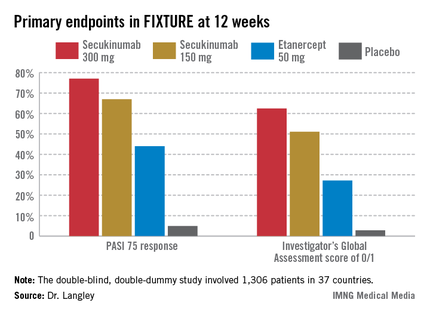
The three randomized, double-blind, multicenter pivotal trials of secukinumab in psoriasis collectively included 3,367 patients with moderate to severe chronic plaque psoriasis. All three studies were strongly positive. Efficacy rates were higher than with current biologics, clinical improvement was remarkably rapid, and the safety profile was reassuring.
"Those of us working in this area of research are really excited by this new data and what it says for the treatment of psoriasis patients," commented Dr. Richard Langley of Dalhousie University, Halifax, N.S.
He presented the centerpiece of this trio of phase III trials, known as the FIXTURE trial. FIXTURE (Full Year Investigative Examination of Secukinumab vs. Etanercept Using 2 Dosing Regimens to Determine Efficacy in Psoriasis) was a 1,306-patient, double-blind, double-dummy trial conducted by 153 investigators in 37 countries. The trial featured a 1-year head-to-head comparison of secukinumab and the widely prescribed tumor necrosis factor (TNF) inhibitor etanercept (Enbrel). The IL-17A inhibitor outperformed etanercept in all of the prespecified primary and secondary outcome measures. Moreover, the two biologics proved equally safe.
"I think it’s interesting in comparing these two molecules that when we look at the data to date, we see comparable safety results. Etanercept is one of the most widely used biologics and has an excellent safety record. That’s reassuring for those of us who are investigating IL-17 signaling," observed Dr. Langley, also the current president of the Canadian Dermatology Association.
FIXTURE participants had a mean baseline Psoriasis Area and Severity Index (PASI) score of 24, an average body mass index of 34 kg/m2, and a mean age in the mid-40s, and were previous inadequate responders to conventional systemic agents and/or biologics. The two co-primary endpoints were 12-week rates of at least a 75% reduction in PASI score, or PASI 75 response, and an Investigator’s Global Assessment (IGA) rating of 0/1, corresponding to clear or nearly clear, on a modified 5-point scale that provides more clinically meaningful information than the older 6-point IGA scale. Patients randomized to the secukinumab 300-mg or 150-mg groups did significantly better on both outcome measures than those assigned to etanercept.
The onset of benefit with secukinumab was swift; a statistically significant improvement compared with etanercept was seen within 2 weeks in terms of IGA scores and within 3 weeks for PASI 75. Secukinumab at 300 mg per subcutaneous injection – the most effective dose across all three pivotal trials – achieved roughly a 50% reduction in PASI scores after 3 weeks, compared with 8 weeks for etanercept, the dermatologist explained.
The PASI 75 response rate at 12 weeks was 77.1% in patients receiving secukinumab at 300 mg, 67% for those receiving secukinumab at 150 mg, 44% for etanercept 50 mg, and 4.9% for placebo.
The highest response rates with secukinumab were seen at week 16 rather than week 12. In the secukinumab 300-mg group, the PASI 75 rate at week 16 was 86.7%, with that high level of response being retained throughout the remainder of the 52-week study. In contrast, the PASI 75 rate at week 16 for etanercept was less than 60%. The IGA 0/1 rate at week 16 was 75.5% in the secukinumab 300-mg group and 60% with secukinumab 150 mg. The peak IGA 0/1 rate in the etanercept arm was only about 45%, and it came much later, at week 26.
Looking at more stringent secondary endpoints, the investigators found that a PASI 90 response was achieved by week 16 in 72.4% of the high-dose secukinumab group, compared with about 30% with etanercept. Twenty-four percent of patients on high-dose secukinumab had a PASI 100 response at week 12, compared with 4% on etanercept. By week 16, 36.8% of the high-dose secukinumab group had a PASI 100 response. At week 52, 65% of the secukinumab 300-mg group maintained a PASI 90 response, compared with 33% of the etanercept group.
The most common adverse event documented in FIXTURE was nasopharyngitis, which occurred in roughly one-third of patients in all four study arms. The serious infection rate was 1%-1.2% in all four study arms. No signals of an increase in malignancies or major adverse cardiovascular events were noted in any of the active treatment groups. Overall, adverse events were similar in both secukinumab arms and comparable to etanercept. Injection-site reactions occurred in 6.1% of the etanercept group and in none of the patients assigned to secukinumab or placebo.
The incidence of treatment-emergent antidrug antibodies in the secukinumab arms was 0.4%, and when it occurred, it had no impact on treatment efficacy or safety. Patients on etanercept weren’t tested for the emergence of antidrug antibodies.
Candida infections occurred in 4.7% of patients on secukinumab 300 mg, 2.3% of those on 150 mg, and 1.2% of the etanercept group. All cases in patients on secukinumab were mild or moderate and easily treated. Candida infections are a side effect of special interest because patients with a genetic defect in the IL-17 pathway can develop chronic mucocutaneous candidiasis. A theoretical concern that pharmacologic inhibition of IL-17 might create a big problem in this regard has not materialized.
The other two phase III secukinumab clinical trials presented in Istanbul – ERASURE and SCULPTURE – showed efficacy and safety results similar to those of FIXTURE. Unlike FIXTURE, neither of those trials featured a head-to-head comparison with another biologic.
These were the first completed phase III studies for any of the three biologics in this novel, highly promising class targeting IL-17 in the treatment of psoriasis and other immune-mediated inflammatory diseases. The other two agents in the pipeline targeting IL-17, brodalumab and ixekizumab, remain in ongoing phase III trials.
Because of the pivotal role IL-17 plays in generating inflammatory cytokines downstream, all three drugs are being studied for additional indications beyond psoriasis. For example, secukinumab, an IgG1 human monoclonal antibody, is in phase III clinical trials for psoriatic arthritis, ankylosing spondylitis, and rheumatoid arthritis, and in phase II for muscular sclerosis and asthma.
One audience member asked Dr. Langley for his thoughts regarding the absence of injection-site reactions in the secukinumab-treated patients. He replied that one obvious factor is that secukinumab injections are given much less frequently: once monthly during maintenance therapy as compared to once weekly with etanercept. In any event, he doesn’t consider injection-site reactions to be clinically relevant.
"Injection-site reactions don’t seem to be a major issue with any of the subcutaneous therapies. It has never in 15 years of using different biologics been an issue that’s made me stop treatment for a patient," he added.
Secukinumab was dosed at baseline, again weekly through week 4, then once monthly from week 8 through the study’s end. Etanercept was dosed at 50 mg twice weekly for 12 weeks, then once weekly in accord with the labeling instructions in most countries. Nonresponders at 12 weeks in the placebo arm were at that point randomized to secukinumab at 300 mg or 150 mg. The statistical analysis in FIXTURE was performed by nonresponder imputation.
"Those who are interested in statistics will know that that’s the most rigorous way that you can look at the data, because anybody who drops out of the study, whether they withdraw consent, have a protocol violation, or have an adverse event, even if they were responding at that time, are considered a failure or nonresponder," Dr. Langley explained.
Asked how he sees secukinumab fitting into patient management, Dr. Langley replied, "Most of us are forced to use conventional therapies and phototherapy to get approval for biologics, but after that I think the safety and efficacy of this drug put it right at the top. I could definitely use this drug as a first-line biologic for patients with plain psoriasis without psoriatic arthritis."
Coinvestigator Dr. Kristian Reich, professor of dermatology at Georg-August University in Göttingen, Germany, said he will probably continue to use TNF inhibitors in psoriasis patients with prominent arthritis, where he believes the TNF inhibitors are particularly beneficial, but he anticipates using secukinumab widely in others.
Dr. Bruce E. Strober, another active clinical trial researcher in psoriasis, said he likes what he sees in the IL-17 inhibitor data.
"I predict as a specialty we’ll become very confident in these drugs 5 years from now. A lot of us will be using them as first line in many patients. That’s my prediction. For now, though, I’m a big fan of TNF inhibition," added Dr. Strober, vice chair of dermatology at the University of Connecticut Medical Center, Farmington.
The secukinumab development program is sponsored by Novartis. Dr. Langley, Dr. Reich, and Dr. Strober disclosed having received research grants from and serving as consultants to Novartis and numerous other companies developing biologic agents for psoriasis.
AT THE EADV CONGRESS
Major finding: The PASI 75 response rate at 12 weeks in patients with moderate to severe chronic plaque psoriasis was 77.1% in those randomized to the investigational interleukin-17A inhibitor secukinumab at 300 mg, 67% for secukinumab at 150 mg, 44% for etanercept 50 mg, and 4.9% for placebo.
Data source: The FIXTURE trial was a randomized, double-blind, double-dummy, year-long, phase III trial involving 1,306 patients with chronic plaque psoriasis not adequately responsive to prior systemic therapies.
Disclosures: The secukinumab development program is sponsored by Novartis. Dr. Langley, Dr. Reich, and Dr. Strober disclosed having received research grants from and serving as consultants to Novartis and numerous other companies developing biologic agents for psoriasis.
Psoriasis linked to nonalcoholic fatty liver disease
ISTANBUL, TURKEY – The prevalence of psoriasis was significantly greater in subjects with nonalcoholic fatty liver disease by a margin of 7% to 4.2%, according to findings from a long-term, population-based cohort study including nearly 4,000 individuals.
This newly identified link between two common diseases – one of which manifests as visible, angry skin lesions; the other silent, insidious, and often unrecognized until its late stages – contains an important message for clinicians, said Dr. Ella van der Voort of Erasmus University in Rotterdam, the Netherlands.
"Physicians should be aware of this increased risk before prescribing for psoriasis patients medications with potential for liver toxicity – and I’m not talking about just psoriasis medications, but also medications in general, like statins," she said at the annual congress of the European Academy of Dermatology and Venereology.
Psoriasis was present in 5.1% of the study group. Most cases were mild, with affected patients having a mean psoriasis area severity index of 2.9 out of a possible 72 and no use of systemic psoriasis therapies. Nevertheless, the prevalence of nonalcoholic fatty liver disease (NAFLD) was 46.2% among the 118 psoriasis patients, compared with 33% in the 2,174 subjects without psoriasis.
NAFLD is now the most common form of chronic liver disease in Western countries. By 2020, when new well-tolerated and highly effective medications for hepatitis C are expected to have made a mark, NAFLD may be the leading reason for liver transplantation in developed countries, Dr. van der Voort observed.
The Rotterdam Study is designed to examine contributors to chronic diseases in the elderly, including cardiovascular, endocrinologic, psychiatric, neurologic, and eye diseases. The first wave of participants enrolled in 1989-93. Dr. van der Voort’s study focused on the third cohort, consisting of 3,932 elderly Rotterdam-area residents enrolled in 2006-2008. The mean age at enrollment was 76 years, and the ongoing routine evaluation of the cohort includes liver ultrasound, lab tests for liver enzyme levels and serologic evidence of hepatitis, and a skin examination.
Dr. van der Voort’s analysis was restricted to the 2,292 third-wave subjects who were not heavy drinkers and didn’t have chronic hepatitis, either of which rules out the diagnosis of NAFLD. The participants were not taking hepatotoxic medications, and there was no uncertainty as to the skin examination findings.
The hallmark of NAFLD is the accumulation of triglycerides in the hepatocytes. The previously well-described risk factors for NAFLD include the metabolic syndrome and its individual components, as well as sedentary lifestyle, smoking, and a poor-quality diet. There is also a genetic component: individuals with a mutation in the phospholipase domain-containing protein 3 (PNPLA3) gene, which codes for an enzyme functioning in hydrolyzation of triglycerides, are predisposed to NAFLD.
The prevalence of metabolic syndrome was 62% in subjects with psoriasis and 52% in those without psoriasis. Individuals with psoriasis also were more likely to be smokers by a margin of 15% to 8%. After adjusting for those variables, as well as alcohol intake, age, gender, liver enzyme levels, and other potential confounders, two strong independent predictors of NAFLD were metabolic syndrome, with an adjusted odds ratio of 3.5, and psoriasis, with an odds ratio of 1.7.
In a multivariate analysis, psoriasis was not only independently associated with a 70% increased likelihood of NAFLD, but psoriasis patients with NAFLD were also 60% more likely to have the more severe forms of NAFLD.
The Rotterdam study is funded chiefly by Dutch scientific research foundations, with secondary pharmaceutical industry support. Dr. van der Voort reported having no financial conflicts of interest.
ISTANBUL, TURKEY – The prevalence of psoriasis was significantly greater in subjects with nonalcoholic fatty liver disease by a margin of 7% to 4.2%, according to findings from a long-term, population-based cohort study including nearly 4,000 individuals.
This newly identified link between two common diseases – one of which manifests as visible, angry skin lesions; the other silent, insidious, and often unrecognized until its late stages – contains an important message for clinicians, said Dr. Ella van der Voort of Erasmus University in Rotterdam, the Netherlands.
"Physicians should be aware of this increased risk before prescribing for psoriasis patients medications with potential for liver toxicity – and I’m not talking about just psoriasis medications, but also medications in general, like statins," she said at the annual congress of the European Academy of Dermatology and Venereology.
Psoriasis was present in 5.1% of the study group. Most cases were mild, with affected patients having a mean psoriasis area severity index of 2.9 out of a possible 72 and no use of systemic psoriasis therapies. Nevertheless, the prevalence of nonalcoholic fatty liver disease (NAFLD) was 46.2% among the 118 psoriasis patients, compared with 33% in the 2,174 subjects without psoriasis.
NAFLD is now the most common form of chronic liver disease in Western countries. By 2020, when new well-tolerated and highly effective medications for hepatitis C are expected to have made a mark, NAFLD may be the leading reason for liver transplantation in developed countries, Dr. van der Voort observed.
The Rotterdam Study is designed to examine contributors to chronic diseases in the elderly, including cardiovascular, endocrinologic, psychiatric, neurologic, and eye diseases. The first wave of participants enrolled in 1989-93. Dr. van der Voort’s study focused on the third cohort, consisting of 3,932 elderly Rotterdam-area residents enrolled in 2006-2008. The mean age at enrollment was 76 years, and the ongoing routine evaluation of the cohort includes liver ultrasound, lab tests for liver enzyme levels and serologic evidence of hepatitis, and a skin examination.
Dr. van der Voort’s analysis was restricted to the 2,292 third-wave subjects who were not heavy drinkers and didn’t have chronic hepatitis, either of which rules out the diagnosis of NAFLD. The participants were not taking hepatotoxic medications, and there was no uncertainty as to the skin examination findings.
The hallmark of NAFLD is the accumulation of triglycerides in the hepatocytes. The previously well-described risk factors for NAFLD include the metabolic syndrome and its individual components, as well as sedentary lifestyle, smoking, and a poor-quality diet. There is also a genetic component: individuals with a mutation in the phospholipase domain-containing protein 3 (PNPLA3) gene, which codes for an enzyme functioning in hydrolyzation of triglycerides, are predisposed to NAFLD.
The prevalence of metabolic syndrome was 62% in subjects with psoriasis and 52% in those without psoriasis. Individuals with psoriasis also were more likely to be smokers by a margin of 15% to 8%. After adjusting for those variables, as well as alcohol intake, age, gender, liver enzyme levels, and other potential confounders, two strong independent predictors of NAFLD were metabolic syndrome, with an adjusted odds ratio of 3.5, and psoriasis, with an odds ratio of 1.7.
In a multivariate analysis, psoriasis was not only independently associated with a 70% increased likelihood of NAFLD, but psoriasis patients with NAFLD were also 60% more likely to have the more severe forms of NAFLD.
The Rotterdam study is funded chiefly by Dutch scientific research foundations, with secondary pharmaceutical industry support. Dr. van der Voort reported having no financial conflicts of interest.
ISTANBUL, TURKEY – The prevalence of psoriasis was significantly greater in subjects with nonalcoholic fatty liver disease by a margin of 7% to 4.2%, according to findings from a long-term, population-based cohort study including nearly 4,000 individuals.
This newly identified link between two common diseases – one of which manifests as visible, angry skin lesions; the other silent, insidious, and often unrecognized until its late stages – contains an important message for clinicians, said Dr. Ella van der Voort of Erasmus University in Rotterdam, the Netherlands.
"Physicians should be aware of this increased risk before prescribing for psoriasis patients medications with potential for liver toxicity – and I’m not talking about just psoriasis medications, but also medications in general, like statins," she said at the annual congress of the European Academy of Dermatology and Venereology.
Psoriasis was present in 5.1% of the study group. Most cases were mild, with affected patients having a mean psoriasis area severity index of 2.9 out of a possible 72 and no use of systemic psoriasis therapies. Nevertheless, the prevalence of nonalcoholic fatty liver disease (NAFLD) was 46.2% among the 118 psoriasis patients, compared with 33% in the 2,174 subjects without psoriasis.
NAFLD is now the most common form of chronic liver disease in Western countries. By 2020, when new well-tolerated and highly effective medications for hepatitis C are expected to have made a mark, NAFLD may be the leading reason for liver transplantation in developed countries, Dr. van der Voort observed.
The Rotterdam Study is designed to examine contributors to chronic diseases in the elderly, including cardiovascular, endocrinologic, psychiatric, neurologic, and eye diseases. The first wave of participants enrolled in 1989-93. Dr. van der Voort’s study focused on the third cohort, consisting of 3,932 elderly Rotterdam-area residents enrolled in 2006-2008. The mean age at enrollment was 76 years, and the ongoing routine evaluation of the cohort includes liver ultrasound, lab tests for liver enzyme levels and serologic evidence of hepatitis, and a skin examination.
Dr. van der Voort’s analysis was restricted to the 2,292 third-wave subjects who were not heavy drinkers and didn’t have chronic hepatitis, either of which rules out the diagnosis of NAFLD. The participants were not taking hepatotoxic medications, and there was no uncertainty as to the skin examination findings.
The hallmark of NAFLD is the accumulation of triglycerides in the hepatocytes. The previously well-described risk factors for NAFLD include the metabolic syndrome and its individual components, as well as sedentary lifestyle, smoking, and a poor-quality diet. There is also a genetic component: individuals with a mutation in the phospholipase domain-containing protein 3 (PNPLA3) gene, which codes for an enzyme functioning in hydrolyzation of triglycerides, are predisposed to NAFLD.
The prevalence of metabolic syndrome was 62% in subjects with psoriasis and 52% in those without psoriasis. Individuals with psoriasis also were more likely to be smokers by a margin of 15% to 8%. After adjusting for those variables, as well as alcohol intake, age, gender, liver enzyme levels, and other potential confounders, two strong independent predictors of NAFLD were metabolic syndrome, with an adjusted odds ratio of 3.5, and psoriasis, with an odds ratio of 1.7.
In a multivariate analysis, psoriasis was not only independently associated with a 70% increased likelihood of NAFLD, but psoriasis patients with NAFLD were also 60% more likely to have the more severe forms of NAFLD.
The Rotterdam study is funded chiefly by Dutch scientific research foundations, with secondary pharmaceutical industry support. Dr. van der Voort reported having no financial conflicts of interest.
AT THE EADV CONGRESS
Major finding: The prevalence of nonalcoholic fatty liver disease in a large cohort of elderly subjects was 46.2% among those with psoriasis and 33% in those without. In a multivariate regression analysis, psoriasis was independently associated with a 70% increased likelihood of the hepatic disease.
Data source: The Rotterdam Study is a long-standing prospective, population-based cohort study. The aim is to determine key factors in the development of a range of chronic diseases common in the elderly.
Disclosures: The Rotterdam Study is funded primarily by Dutch scientific research foundations. The presenter reported having no financial conflicts.
Just over a third of hypertensive kidney patients are at target BP
AMSTERDAM – Eighty percent of Americans with chronic kidney disease have comorbid hypertension, which is controlled in only 36% of cases, according to a large national study.
This is an area of significant unmet medical need in spite of the wide availability of antihypertensive medications, Panagiotis Mavros, Ph.D., said at the annual congress of the European Society of Cardiology.
He presented a cross-sectional study involving 159,306 American adults with stage 1-4 chronic kidney disease (CKD) identified in the GE Centricity electronic medical record database. Fifty-seven percent were in stage 3 and 29% were in stage 2 CKD.
Roughly 43% of this very large group of CKD patients carried the diagnosis of diabetes mellitus. Eighty percent of the CKD population had hypertension, including 10% of the overall study population with previously undiagnosed hypertension. Among the CKD patients with hypertension, 15% were not being treated for it, said Dr. Mavros of Merck in Whitehouse Station, N.J.
Blood pressure was controlled to the target of less than 130/80 mm Hg in 36% of patients with diagnosed hypertension.
Seventy-three percent of treated hypertensive patients with CKD were on combination therapy, typically with three different classes of antihypertensive drugs. Patients on more than three different classes of antihypertensive medications tended to have more advanced CKD. However, the proportion of treated patients with good blood pressure control did not differ according to CKD stage.
This cross-sectional study was funded by Merck. Dr. Mavros is a full-time company employee.
AMSTERDAM – Eighty percent of Americans with chronic kidney disease have comorbid hypertension, which is controlled in only 36% of cases, according to a large national study.
This is an area of significant unmet medical need in spite of the wide availability of antihypertensive medications, Panagiotis Mavros, Ph.D., said at the annual congress of the European Society of Cardiology.
He presented a cross-sectional study involving 159,306 American adults with stage 1-4 chronic kidney disease (CKD) identified in the GE Centricity electronic medical record database. Fifty-seven percent were in stage 3 and 29% were in stage 2 CKD.
Roughly 43% of this very large group of CKD patients carried the diagnosis of diabetes mellitus. Eighty percent of the CKD population had hypertension, including 10% of the overall study population with previously undiagnosed hypertension. Among the CKD patients with hypertension, 15% were not being treated for it, said Dr. Mavros of Merck in Whitehouse Station, N.J.
Blood pressure was controlled to the target of less than 130/80 mm Hg in 36% of patients with diagnosed hypertension.
Seventy-three percent of treated hypertensive patients with CKD were on combination therapy, typically with three different classes of antihypertensive drugs. Patients on more than three different classes of antihypertensive medications tended to have more advanced CKD. However, the proportion of treated patients with good blood pressure control did not differ according to CKD stage.
This cross-sectional study was funded by Merck. Dr. Mavros is a full-time company employee.
AMSTERDAM – Eighty percent of Americans with chronic kidney disease have comorbid hypertension, which is controlled in only 36% of cases, according to a large national study.
This is an area of significant unmet medical need in spite of the wide availability of antihypertensive medications, Panagiotis Mavros, Ph.D., said at the annual congress of the European Society of Cardiology.
He presented a cross-sectional study involving 159,306 American adults with stage 1-4 chronic kidney disease (CKD) identified in the GE Centricity electronic medical record database. Fifty-seven percent were in stage 3 and 29% were in stage 2 CKD.
Roughly 43% of this very large group of CKD patients carried the diagnosis of diabetes mellitus. Eighty percent of the CKD population had hypertension, including 10% of the overall study population with previously undiagnosed hypertension. Among the CKD patients with hypertension, 15% were not being treated for it, said Dr. Mavros of Merck in Whitehouse Station, N.J.
Blood pressure was controlled to the target of less than 130/80 mm Hg in 36% of patients with diagnosed hypertension.
Seventy-three percent of treated hypertensive patients with CKD were on combination therapy, typically with three different classes of antihypertensive drugs. Patients on more than three different classes of antihypertensive medications tended to have more advanced CKD. However, the proportion of treated patients with good blood pressure control did not differ according to CKD stage.
This cross-sectional study was funded by Merck. Dr. Mavros is a full-time company employee.
AT THE ESC CONGRESS 2013
Major finding: Of a large group of patients with chronic kidney disease and comorbid hypertension, 36% were at the blood pressure goal of less than 130/80 mm Hg.
Data source: A cross-sectional study involving more than 159,000 U.S. adults with stage 1-4 chronic kidney disease, 80% of whom had comorbid hypertension.
Disclosures: The study was funded by Merck. The presenter is a full-time employee of the pharmaceutical company.