User login
Should routine colon cancer screening start at 45, not 50?
SAN FRANCISCO – For years, 50 years old has been the age at which screening for colorectal cancer (CRC) began in the United States, but recently, one group lowered the starting age to 45 years.
This move by the American Cancer Society in 2018 was made in reaction to reports of an increase in the incidence of CRC in younger adults.
However, other groups have stayed with the benchmark 50 years. This includes the U.S. Preventive Services Task Force and the National Comprehensive Cancer Network.
Should the age be lowered in view of the mounting reports of an increase in CRC in younger adults? Experts argued both for and against the move here at the 2020 Gastrointestinal Cancers Symposium.
“We’re having this debate because the health of more than 20 million Americans is in the balance,” commented David Weinberg, MD, MSc, chairman of the department of medicine at Fox Chase Cancer Center in Philadelphia. “This is not just an academic discussion.” If the screening age shifts to 5 years earlier, the impact nationally would be about 30,000 colorectal cancers and 11,000 deaths averted.
“It will take about 11 million additional colonoscopies ... and the overall bill would be $10 billion. That’s not a small number, but if the country has the resources and we want to do this, I would say we can,” argued Uri Ladabaum, MD, director of the gastrointestinal cancer prevention program and the clinical chief of the division of gastroenterology and hepatology at Stanford (Calif.) University.
Lower the age
Dr. Ladabaum argued in favor of lowering the age to 45 years to start screening. “In life, 60 may be the new 40, but for colorectal cancer screening, 45 is definitely the new 50,” he said. Anticipating arguments against such a move, he focused on several points.
First, the magnitude of the problem is certainly not small, he noted, pointing to a 2017 study showing that colorectal cancer rates have increased by 1%-2.4% annually since the mid-1980s in persons aged 20-39 years and by 0.5%-1.3% since the mid-1990s in adults aged 40-54 years (J Natl Cancer Inst. 2017;109:djw322). Rectal cancer incidence has been increasing even more rapidly, at a rate of about 3.2% annually during 1974-2013 in adults aged 20-29 years.
Overall, people who were born around 1990 and later have double the risk of colon cancer (incidence rate ratio, 2.40) and quadruple the risk of rectal cancer (IRR, 4.32) as compared with those born circa 1950.
“Thus, 45- to 49-year-olds are beginning to look like yesterday’s 50- to 54-year-olds used to be,” said Dr. Ladabaum.
One issue that has been raised is lead-time bias, with the burning question: Are the cancers found in adults in their 40s simply the same ones that would have eventually been detected in their 50s? Dr. Ladabaum argued that they are not, referencing a 2019 study showing that among persons aged 40 through 49 years, the disease was diagnosed at later stages (JAMA. 2019;321:1933-4).
For those aged 40- 49 years, there was a significant increase in incidence during 1995-2015. The proportion of distant cancers increased significantly (from 21.7% to 26.6%; P less than .001), and the authors of the study had noted that this increase of 4.9% could not be explained by a decrease in unstaged cases. “In the early ’90s and mid-’90s, we began to see an increase in all stages,” Dr. Ladabaum noted. “And the most important thing here is the distant cancers over time. They’ve gone up.” If the only explanation was lead time bias in people aged 40- 49 years, then a person screened and diagnosed with cancer at age 48 would have earlier-stage disease than if it had been found at age 51. “So is this all lead-time bias?” he said. “I think the answer is no.”
Next, Dr. Ladabaum tackled the issue of whether benefit/risk ratio of CRC screening is different among younger vs. older adults. This is difficult to tease out, he suggested, as the data are sparse and there were no controlled studies to date to address that. One study from Taiwan, which looked at the outcomes of fecal immunochemical testing (FIT), showed that in different age groups, the hazard ratio for detecting cancer in those with positive results is higher in younger people vs. older ones (J Clin Gastroenterol. 2016 Oct;50[9]:761-8).
“Indirect evidence shows that if we do a FIT test and it’s positive, it probably means something,” he said. “But is there something magical that at age 50 and older – that it becomes a screenable disease, and through age 49 it’s not screenable? I would say no. Biology is not like this.”
Finally, is it cost effective to start earlier? In a modeling projection published last summer by Dr. Ladabaum and colleagues, starting at 45 years would avert about four colorectal cancers and two colorectal cancer deaths per 1,000 people, and the cohort would gain approximately 14 quality-adjusted life years (Gastroenterology. 2019;157:137-48).
“The incremental cost per quality-adjusted life year gained is highly acceptable,” said Dr. Ladabaum. “This is well within the range of what’s considered cost-effective in the United States – under $35,000 for colonoscopy, and under $8,000 for fecal immunochemical tests.”
Therefore, the answer is yes, it is cost effective, he concluded.
Not so fast ...
Arguing the case against a lowering of the starting age, Dr. Weinberg agreed with Dr. Ladabaum that colon cancer risk for younger people is rising.
That risk has increased from 5.9/100,000 to 7.2/100,000, which is a relative increase of 22%, he noted.
“That is what newspapers will want to put on their headlines to sensationalize it – that the risk of colon cancer for young people is up by over 20%,” said Dr. Weinberg. “But that represents an absolute risk of just 1.3 more people/100,000. Put in some context, 99.9% of people in their 40s will not develop colon cancer.”
This observation was not to “make light of the remainder,” he emphasized, but “the overwhelming majority are not going to get this disease at this age,” he noted.
“It’s also not entirely clear that starting screening at 45 is the right answer,” he added.
“Taken to a somewhat ridiculous extreme,” he continued, “why not start at 40? You’ll catch more people that way, but no one is advocating that.”
A better understanding of the factors contributing to the increased CRC incidence seen in younger adults is very important, he argued, and he suggested that some of it may occur because of screening, along with factors such as obesity, diabetes, and childhood exposures.
Modeling has been done to calculate the risk and benefit of early screening, but while useful for decision making, models are “usually wrong and sit near the bottom of the evidence hierarchy.”
“Models help inform decisions, but they don’t define the standard of care,” Dr. Weinberg said. “No one would vaccinate a population based on a model.”
Dr. Weinberg also emphasized that the new recommendation from the American Cancer Society to start screening at age 45 years is qualified. This means that while “clear evidence of benefit exists,” so does uncertainty about whether “the benefits really outweigh the harms.”
The current evidence for reducing the screening age is not yet clear, he believes, and he questioned the premise that age should be the only criteria for cancer stratification.
Dr. Weinberg cited one study that looked at early-onset colon cancer (ages 18-49 years) and compared it with two groups: patients diagnosed at 50 years and older and matched controls (Clin Gastroenterol Hepatol. 2019;S1542-3565[19]31108-5). Besides age, the study authors identified several nonmodifiable risk factors that were associated with early-onset disease, including sex, race, history of inflammatory bowel disease (IBD), and family history of colorectal cancer.
“Being male was a risk factor and having a family history increased your risk by three times,” said Dr. Weinberg. “And I would note that this study had removed people, at least as best one can, who were known to have syndromic risks of early-onset colon cancer (such as familial adenomatous polyposis.”
Earlier screening (by age 40 years) should already be taking place in people with such syndromes, he commented, as well as those with a known family history and IBD. “Those recommendations were there before the ACS, and we don’t necessarily need another one,” he added.
To make things a little more confusing, a second recent study, using National Cancer Data Base data from 2004 to 2015, identified another set of factors associated with colon cancer in younger adults (Cancer. 2019 Nov 1;125:3828-35). This study showed diagnosis younger than 50 years rose only in non-Hispanic white men, in Hispanic and non-Hispanic white women, and in those living in urban vs. rural areas.
“But it gets more interesting,” Dr. Weinberg pointed out. “Risk increased over time for people in the highest zip code income quartile and those with private insurance, and risk was lower for people with Medicaid and no insurance at all,” he noted. “Well, that smacks of access to me,” he commented.
Another issue is the possibility of lead-time bias. During 1975-2015, incidence rose over time, according to Surveillance, Epidemiology, and End Results data (J Natl Cancer Inst. 2017 Aug;109:djw322). Screening of persons younger than age 49 years also more than doubled, from a low level in 2000 of about 6% to more than 15% by 2010. As screening increases, the incidence increases, Dr. Weinberg pointed out. “But mortality doesn’t change. And despite what Dr. Ladabaum said a moment ago about lead-time bias, that is textbook lead-time bias in any epidemiology study.”
Finally, it is essential to carefully weigh the benefit against the risk, Dr. Weinberg said.
A core principle of population screening is to create more future health benefits than harms, and if the screening age is lowered, several million additional colonoscopies will be performed.
Colonoscopy reduces the colorectal cancer mortality risk by about 75%, and the incidence of the disease is 7.2/100,000 in the younger age group. But colonoscopy-specific mortality – just having the test – is associated with a death rate of 7/100,000,” Dr. Weinberg pointed out. “Let’s not forget that there is a risk associated with this procedure.” (Gastrointest Endosc. 2011 Oct;74:745-52).
Dr. Weinberg emphasized that everyone wants to reduce the burden of cancer, and models are helpful for that purpose. “They’re obviously thought provoking, but they’re not adequate to drive change without additional evidence of clinical and cost-effectiveness,” he said. “These are important questions that need better data.”
He added that without changing the current screening protocol, “we could certainly emphasize more than ever the impact of family history and IBD on colon cancer risk and colon cancer prevention.”
“And certainly, there’s plenty of evidence that patients with a known family history of colon cancer are not getting screened at the right age or with the right frequency,” Dr. Weinberg concluded. “We can do better. All of us can do better.”
Dr. Weinberg has disclosed relationships with Fujifilm and Exact Sciences. Dr. Ladabaum has disclosed relationships with Lean Medical, Universal Dx, Clinical Genomics, Medtronic, Modus GI, and Quorum Consulting.
This article first appeared on Medscape.com.
SAN FRANCISCO – For years, 50 years old has been the age at which screening for colorectal cancer (CRC) began in the United States, but recently, one group lowered the starting age to 45 years.
This move by the American Cancer Society in 2018 was made in reaction to reports of an increase in the incidence of CRC in younger adults.
However, other groups have stayed with the benchmark 50 years. This includes the U.S. Preventive Services Task Force and the National Comprehensive Cancer Network.
Should the age be lowered in view of the mounting reports of an increase in CRC in younger adults? Experts argued both for and against the move here at the 2020 Gastrointestinal Cancers Symposium.
“We’re having this debate because the health of more than 20 million Americans is in the balance,” commented David Weinberg, MD, MSc, chairman of the department of medicine at Fox Chase Cancer Center in Philadelphia. “This is not just an academic discussion.” If the screening age shifts to 5 years earlier, the impact nationally would be about 30,000 colorectal cancers and 11,000 deaths averted.
“It will take about 11 million additional colonoscopies ... and the overall bill would be $10 billion. That’s not a small number, but if the country has the resources and we want to do this, I would say we can,” argued Uri Ladabaum, MD, director of the gastrointestinal cancer prevention program and the clinical chief of the division of gastroenterology and hepatology at Stanford (Calif.) University.
Lower the age
Dr. Ladabaum argued in favor of lowering the age to 45 years to start screening. “In life, 60 may be the new 40, but for colorectal cancer screening, 45 is definitely the new 50,” he said. Anticipating arguments against such a move, he focused on several points.
First, the magnitude of the problem is certainly not small, he noted, pointing to a 2017 study showing that colorectal cancer rates have increased by 1%-2.4% annually since the mid-1980s in persons aged 20-39 years and by 0.5%-1.3% since the mid-1990s in adults aged 40-54 years (J Natl Cancer Inst. 2017;109:djw322). Rectal cancer incidence has been increasing even more rapidly, at a rate of about 3.2% annually during 1974-2013 in adults aged 20-29 years.
Overall, people who were born around 1990 and later have double the risk of colon cancer (incidence rate ratio, 2.40) and quadruple the risk of rectal cancer (IRR, 4.32) as compared with those born circa 1950.
“Thus, 45- to 49-year-olds are beginning to look like yesterday’s 50- to 54-year-olds used to be,” said Dr. Ladabaum.
One issue that has been raised is lead-time bias, with the burning question: Are the cancers found in adults in their 40s simply the same ones that would have eventually been detected in their 50s? Dr. Ladabaum argued that they are not, referencing a 2019 study showing that among persons aged 40 through 49 years, the disease was diagnosed at later stages (JAMA. 2019;321:1933-4).
For those aged 40- 49 years, there was a significant increase in incidence during 1995-2015. The proportion of distant cancers increased significantly (from 21.7% to 26.6%; P less than .001), and the authors of the study had noted that this increase of 4.9% could not be explained by a decrease in unstaged cases. “In the early ’90s and mid-’90s, we began to see an increase in all stages,” Dr. Ladabaum noted. “And the most important thing here is the distant cancers over time. They’ve gone up.” If the only explanation was lead time bias in people aged 40- 49 years, then a person screened and diagnosed with cancer at age 48 would have earlier-stage disease than if it had been found at age 51. “So is this all lead-time bias?” he said. “I think the answer is no.”
Next, Dr. Ladabaum tackled the issue of whether benefit/risk ratio of CRC screening is different among younger vs. older adults. This is difficult to tease out, he suggested, as the data are sparse and there were no controlled studies to date to address that. One study from Taiwan, which looked at the outcomes of fecal immunochemical testing (FIT), showed that in different age groups, the hazard ratio for detecting cancer in those with positive results is higher in younger people vs. older ones (J Clin Gastroenterol. 2016 Oct;50[9]:761-8).
“Indirect evidence shows that if we do a FIT test and it’s positive, it probably means something,” he said. “But is there something magical that at age 50 and older – that it becomes a screenable disease, and through age 49 it’s not screenable? I would say no. Biology is not like this.”
Finally, is it cost effective to start earlier? In a modeling projection published last summer by Dr. Ladabaum and colleagues, starting at 45 years would avert about four colorectal cancers and two colorectal cancer deaths per 1,000 people, and the cohort would gain approximately 14 quality-adjusted life years (Gastroenterology. 2019;157:137-48).
“The incremental cost per quality-adjusted life year gained is highly acceptable,” said Dr. Ladabaum. “This is well within the range of what’s considered cost-effective in the United States – under $35,000 for colonoscopy, and under $8,000 for fecal immunochemical tests.”
Therefore, the answer is yes, it is cost effective, he concluded.
Not so fast ...
Arguing the case against a lowering of the starting age, Dr. Weinberg agreed with Dr. Ladabaum that colon cancer risk for younger people is rising.
That risk has increased from 5.9/100,000 to 7.2/100,000, which is a relative increase of 22%, he noted.
“That is what newspapers will want to put on their headlines to sensationalize it – that the risk of colon cancer for young people is up by over 20%,” said Dr. Weinberg. “But that represents an absolute risk of just 1.3 more people/100,000. Put in some context, 99.9% of people in their 40s will not develop colon cancer.”
This observation was not to “make light of the remainder,” he emphasized, but “the overwhelming majority are not going to get this disease at this age,” he noted.
“It’s also not entirely clear that starting screening at 45 is the right answer,” he added.
“Taken to a somewhat ridiculous extreme,” he continued, “why not start at 40? You’ll catch more people that way, but no one is advocating that.”
A better understanding of the factors contributing to the increased CRC incidence seen in younger adults is very important, he argued, and he suggested that some of it may occur because of screening, along with factors such as obesity, diabetes, and childhood exposures.
Modeling has been done to calculate the risk and benefit of early screening, but while useful for decision making, models are “usually wrong and sit near the bottom of the evidence hierarchy.”
“Models help inform decisions, but they don’t define the standard of care,” Dr. Weinberg said. “No one would vaccinate a population based on a model.”
Dr. Weinberg also emphasized that the new recommendation from the American Cancer Society to start screening at age 45 years is qualified. This means that while “clear evidence of benefit exists,” so does uncertainty about whether “the benefits really outweigh the harms.”
The current evidence for reducing the screening age is not yet clear, he believes, and he questioned the premise that age should be the only criteria for cancer stratification.
Dr. Weinberg cited one study that looked at early-onset colon cancer (ages 18-49 years) and compared it with two groups: patients diagnosed at 50 years and older and matched controls (Clin Gastroenterol Hepatol. 2019;S1542-3565[19]31108-5). Besides age, the study authors identified several nonmodifiable risk factors that were associated with early-onset disease, including sex, race, history of inflammatory bowel disease (IBD), and family history of colorectal cancer.
“Being male was a risk factor and having a family history increased your risk by three times,” said Dr. Weinberg. “And I would note that this study had removed people, at least as best one can, who were known to have syndromic risks of early-onset colon cancer (such as familial adenomatous polyposis.”
Earlier screening (by age 40 years) should already be taking place in people with such syndromes, he commented, as well as those with a known family history and IBD. “Those recommendations were there before the ACS, and we don’t necessarily need another one,” he added.
To make things a little more confusing, a second recent study, using National Cancer Data Base data from 2004 to 2015, identified another set of factors associated with colon cancer in younger adults (Cancer. 2019 Nov 1;125:3828-35). This study showed diagnosis younger than 50 years rose only in non-Hispanic white men, in Hispanic and non-Hispanic white women, and in those living in urban vs. rural areas.
“But it gets more interesting,” Dr. Weinberg pointed out. “Risk increased over time for people in the highest zip code income quartile and those with private insurance, and risk was lower for people with Medicaid and no insurance at all,” he noted. “Well, that smacks of access to me,” he commented.
Another issue is the possibility of lead-time bias. During 1975-2015, incidence rose over time, according to Surveillance, Epidemiology, and End Results data (J Natl Cancer Inst. 2017 Aug;109:djw322). Screening of persons younger than age 49 years also more than doubled, from a low level in 2000 of about 6% to more than 15% by 2010. As screening increases, the incidence increases, Dr. Weinberg pointed out. “But mortality doesn’t change. And despite what Dr. Ladabaum said a moment ago about lead-time bias, that is textbook lead-time bias in any epidemiology study.”
Finally, it is essential to carefully weigh the benefit against the risk, Dr. Weinberg said.
A core principle of population screening is to create more future health benefits than harms, and if the screening age is lowered, several million additional colonoscopies will be performed.
Colonoscopy reduces the colorectal cancer mortality risk by about 75%, and the incidence of the disease is 7.2/100,000 in the younger age group. But colonoscopy-specific mortality – just having the test – is associated with a death rate of 7/100,000,” Dr. Weinberg pointed out. “Let’s not forget that there is a risk associated with this procedure.” (Gastrointest Endosc. 2011 Oct;74:745-52).
Dr. Weinberg emphasized that everyone wants to reduce the burden of cancer, and models are helpful for that purpose. “They’re obviously thought provoking, but they’re not adequate to drive change without additional evidence of clinical and cost-effectiveness,” he said. “These are important questions that need better data.”
He added that without changing the current screening protocol, “we could certainly emphasize more than ever the impact of family history and IBD on colon cancer risk and colon cancer prevention.”
“And certainly, there’s plenty of evidence that patients with a known family history of colon cancer are not getting screened at the right age or with the right frequency,” Dr. Weinberg concluded. “We can do better. All of us can do better.”
Dr. Weinberg has disclosed relationships with Fujifilm and Exact Sciences. Dr. Ladabaum has disclosed relationships with Lean Medical, Universal Dx, Clinical Genomics, Medtronic, Modus GI, and Quorum Consulting.
This article first appeared on Medscape.com.
SAN FRANCISCO – For years, 50 years old has been the age at which screening for colorectal cancer (CRC) began in the United States, but recently, one group lowered the starting age to 45 years.
This move by the American Cancer Society in 2018 was made in reaction to reports of an increase in the incidence of CRC in younger adults.
However, other groups have stayed with the benchmark 50 years. This includes the U.S. Preventive Services Task Force and the National Comprehensive Cancer Network.
Should the age be lowered in view of the mounting reports of an increase in CRC in younger adults? Experts argued both for and against the move here at the 2020 Gastrointestinal Cancers Symposium.
“We’re having this debate because the health of more than 20 million Americans is in the balance,” commented David Weinberg, MD, MSc, chairman of the department of medicine at Fox Chase Cancer Center in Philadelphia. “This is not just an academic discussion.” If the screening age shifts to 5 years earlier, the impact nationally would be about 30,000 colorectal cancers and 11,000 deaths averted.
“It will take about 11 million additional colonoscopies ... and the overall bill would be $10 billion. That’s not a small number, but if the country has the resources and we want to do this, I would say we can,” argued Uri Ladabaum, MD, director of the gastrointestinal cancer prevention program and the clinical chief of the division of gastroenterology and hepatology at Stanford (Calif.) University.
Lower the age
Dr. Ladabaum argued in favor of lowering the age to 45 years to start screening. “In life, 60 may be the new 40, but for colorectal cancer screening, 45 is definitely the new 50,” he said. Anticipating arguments against such a move, he focused on several points.
First, the magnitude of the problem is certainly not small, he noted, pointing to a 2017 study showing that colorectal cancer rates have increased by 1%-2.4% annually since the mid-1980s in persons aged 20-39 years and by 0.5%-1.3% since the mid-1990s in adults aged 40-54 years (J Natl Cancer Inst. 2017;109:djw322). Rectal cancer incidence has been increasing even more rapidly, at a rate of about 3.2% annually during 1974-2013 in adults aged 20-29 years.
Overall, people who were born around 1990 and later have double the risk of colon cancer (incidence rate ratio, 2.40) and quadruple the risk of rectal cancer (IRR, 4.32) as compared with those born circa 1950.
“Thus, 45- to 49-year-olds are beginning to look like yesterday’s 50- to 54-year-olds used to be,” said Dr. Ladabaum.
One issue that has been raised is lead-time bias, with the burning question: Are the cancers found in adults in their 40s simply the same ones that would have eventually been detected in their 50s? Dr. Ladabaum argued that they are not, referencing a 2019 study showing that among persons aged 40 through 49 years, the disease was diagnosed at later stages (JAMA. 2019;321:1933-4).
For those aged 40- 49 years, there was a significant increase in incidence during 1995-2015. The proportion of distant cancers increased significantly (from 21.7% to 26.6%; P less than .001), and the authors of the study had noted that this increase of 4.9% could not be explained by a decrease in unstaged cases. “In the early ’90s and mid-’90s, we began to see an increase in all stages,” Dr. Ladabaum noted. “And the most important thing here is the distant cancers over time. They’ve gone up.” If the only explanation was lead time bias in people aged 40- 49 years, then a person screened and diagnosed with cancer at age 48 would have earlier-stage disease than if it had been found at age 51. “So is this all lead-time bias?” he said. “I think the answer is no.”
Next, Dr. Ladabaum tackled the issue of whether benefit/risk ratio of CRC screening is different among younger vs. older adults. This is difficult to tease out, he suggested, as the data are sparse and there were no controlled studies to date to address that. One study from Taiwan, which looked at the outcomes of fecal immunochemical testing (FIT), showed that in different age groups, the hazard ratio for detecting cancer in those with positive results is higher in younger people vs. older ones (J Clin Gastroenterol. 2016 Oct;50[9]:761-8).
“Indirect evidence shows that if we do a FIT test and it’s positive, it probably means something,” he said. “But is there something magical that at age 50 and older – that it becomes a screenable disease, and through age 49 it’s not screenable? I would say no. Biology is not like this.”
Finally, is it cost effective to start earlier? In a modeling projection published last summer by Dr. Ladabaum and colleagues, starting at 45 years would avert about four colorectal cancers and two colorectal cancer deaths per 1,000 people, and the cohort would gain approximately 14 quality-adjusted life years (Gastroenterology. 2019;157:137-48).
“The incremental cost per quality-adjusted life year gained is highly acceptable,” said Dr. Ladabaum. “This is well within the range of what’s considered cost-effective in the United States – under $35,000 for colonoscopy, and under $8,000 for fecal immunochemical tests.”
Therefore, the answer is yes, it is cost effective, he concluded.
Not so fast ...
Arguing the case against a lowering of the starting age, Dr. Weinberg agreed with Dr. Ladabaum that colon cancer risk for younger people is rising.
That risk has increased from 5.9/100,000 to 7.2/100,000, which is a relative increase of 22%, he noted.
“That is what newspapers will want to put on their headlines to sensationalize it – that the risk of colon cancer for young people is up by over 20%,” said Dr. Weinberg. “But that represents an absolute risk of just 1.3 more people/100,000. Put in some context, 99.9% of people in their 40s will not develop colon cancer.”
This observation was not to “make light of the remainder,” he emphasized, but “the overwhelming majority are not going to get this disease at this age,” he noted.
“It’s also not entirely clear that starting screening at 45 is the right answer,” he added.
“Taken to a somewhat ridiculous extreme,” he continued, “why not start at 40? You’ll catch more people that way, but no one is advocating that.”
A better understanding of the factors contributing to the increased CRC incidence seen in younger adults is very important, he argued, and he suggested that some of it may occur because of screening, along with factors such as obesity, diabetes, and childhood exposures.
Modeling has been done to calculate the risk and benefit of early screening, but while useful for decision making, models are “usually wrong and sit near the bottom of the evidence hierarchy.”
“Models help inform decisions, but they don’t define the standard of care,” Dr. Weinberg said. “No one would vaccinate a population based on a model.”
Dr. Weinberg also emphasized that the new recommendation from the American Cancer Society to start screening at age 45 years is qualified. This means that while “clear evidence of benefit exists,” so does uncertainty about whether “the benefits really outweigh the harms.”
The current evidence for reducing the screening age is not yet clear, he believes, and he questioned the premise that age should be the only criteria for cancer stratification.
Dr. Weinberg cited one study that looked at early-onset colon cancer (ages 18-49 years) and compared it with two groups: patients diagnosed at 50 years and older and matched controls (Clin Gastroenterol Hepatol. 2019;S1542-3565[19]31108-5). Besides age, the study authors identified several nonmodifiable risk factors that were associated with early-onset disease, including sex, race, history of inflammatory bowel disease (IBD), and family history of colorectal cancer.
“Being male was a risk factor and having a family history increased your risk by three times,” said Dr. Weinberg. “And I would note that this study had removed people, at least as best one can, who were known to have syndromic risks of early-onset colon cancer (such as familial adenomatous polyposis.”
Earlier screening (by age 40 years) should already be taking place in people with such syndromes, he commented, as well as those with a known family history and IBD. “Those recommendations were there before the ACS, and we don’t necessarily need another one,” he added.
To make things a little more confusing, a second recent study, using National Cancer Data Base data from 2004 to 2015, identified another set of factors associated with colon cancer in younger adults (Cancer. 2019 Nov 1;125:3828-35). This study showed diagnosis younger than 50 years rose only in non-Hispanic white men, in Hispanic and non-Hispanic white women, and in those living in urban vs. rural areas.
“But it gets more interesting,” Dr. Weinberg pointed out. “Risk increased over time for people in the highest zip code income quartile and those with private insurance, and risk was lower for people with Medicaid and no insurance at all,” he noted. “Well, that smacks of access to me,” he commented.
Another issue is the possibility of lead-time bias. During 1975-2015, incidence rose over time, according to Surveillance, Epidemiology, and End Results data (J Natl Cancer Inst. 2017 Aug;109:djw322). Screening of persons younger than age 49 years also more than doubled, from a low level in 2000 of about 6% to more than 15% by 2010. As screening increases, the incidence increases, Dr. Weinberg pointed out. “But mortality doesn’t change. And despite what Dr. Ladabaum said a moment ago about lead-time bias, that is textbook lead-time bias in any epidemiology study.”
Finally, it is essential to carefully weigh the benefit against the risk, Dr. Weinberg said.
A core principle of population screening is to create more future health benefits than harms, and if the screening age is lowered, several million additional colonoscopies will be performed.
Colonoscopy reduces the colorectal cancer mortality risk by about 75%, and the incidence of the disease is 7.2/100,000 in the younger age group. But colonoscopy-specific mortality – just having the test – is associated with a death rate of 7/100,000,” Dr. Weinberg pointed out. “Let’s not forget that there is a risk associated with this procedure.” (Gastrointest Endosc. 2011 Oct;74:745-52).
Dr. Weinberg emphasized that everyone wants to reduce the burden of cancer, and models are helpful for that purpose. “They’re obviously thought provoking, but they’re not adequate to drive change without additional evidence of clinical and cost-effectiveness,” he said. “These are important questions that need better data.”
He added that without changing the current screening protocol, “we could certainly emphasize more than ever the impact of family history and IBD on colon cancer risk and colon cancer prevention.”
“And certainly, there’s plenty of evidence that patients with a known family history of colon cancer are not getting screened at the right age or with the right frequency,” Dr. Weinberg concluded. “We can do better. All of us can do better.”
Dr. Weinberg has disclosed relationships with Fujifilm and Exact Sciences. Dr. Ladabaum has disclosed relationships with Lean Medical, Universal Dx, Clinical Genomics, Medtronic, Modus GI, and Quorum Consulting.
This article first appeared on Medscape.com.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Multiomics blood test outperforms others for CRC
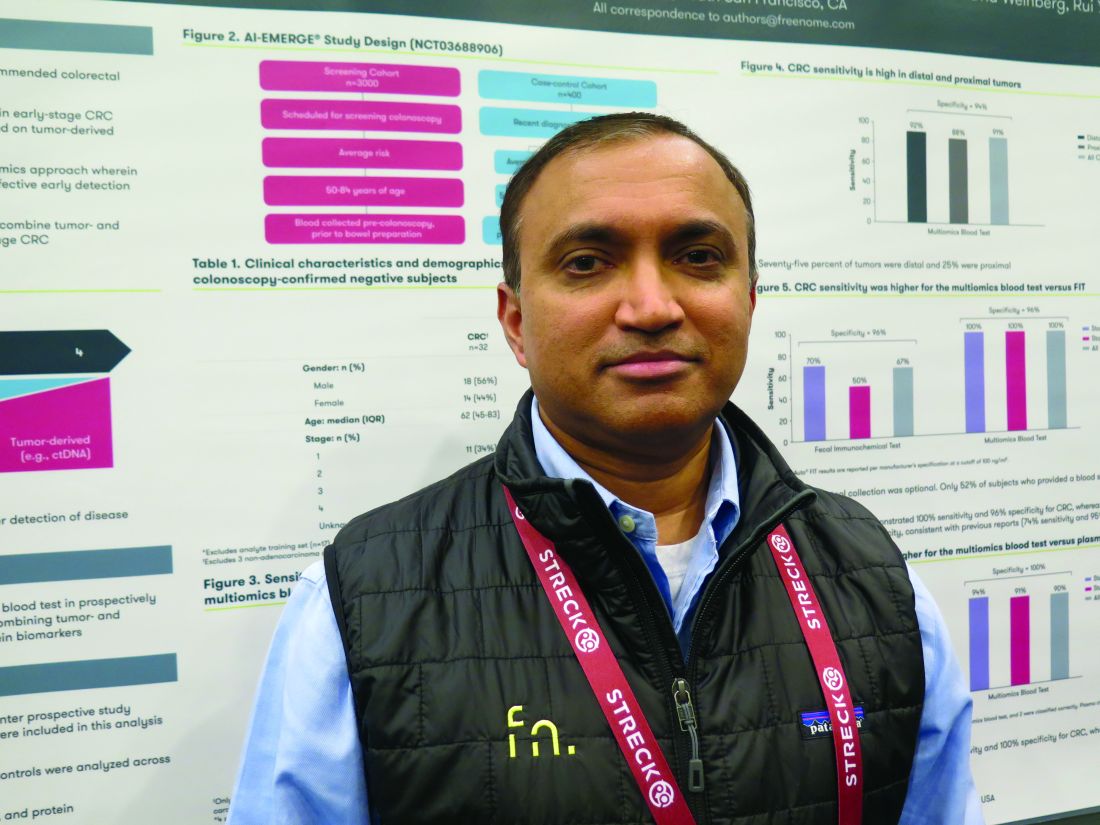
SAN FRANCISCO – A blood-based test that integrates data from multiple molecular “omes,” such as the genome and proteome, performs well at spotting early-stage colorectal cancer (CRC), the AI-EMERGE study suggests.
Moreover, the test netted better sensitivity than a fecal immunochemical test (FIT), a circulating tumor DNA (ctDNA) test, and a carcinoembryonic antigen (CEA) test.
Findings were reported in a poster session at the 2020 GI Cancers Symposium, which is cosponsored by the American Gastroenterological Association, American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology.
“Today, about a third of age-appropriate adults are not up to date with [CRC] screening,” lead study investigator Girish Putcha, MD, PhD, chief medical officer of Freenome in San Francisco, noted at the symposium. “A noninvasive blood-based screening test having high sensitivity and specificity for [CRC] generally, but especially for early-stage disease, could help improve adherence and ultimately reduce mortality.”
Dr. Putcha and colleagues evaluated a blood-based multiomics test in 32 patients with CRC of all stages and 539 colonoscopy-confirmed negative control subjects.
The test uses a multiomics platform to pick up both tumor-derived signal and non–tumor-derived signal from the body’s immune response and other sources. The test uses machine learning, and entails whole-genome sequencing, bisulfite sequencing (for assessment of DNA methylation), and protein quantification methods.
At 94% specificity, the test had a 94% sensitivity for spotting stage I and II CRC, 91% sensitivity for stage III and IV CRC, and 91% sensitivity for CRC of any stage. By location, sensitivity was 92% for distal tumors and 88% for proximal tumors.
The multiomics test outperformed a ctDNA test, a CEA test, and a FIT. At a specificity of 96% for both tests, the multiomics test yielded a higher sensitivity than a commercially available FIT stool test (OC-Auto FIT, Polymedco) for stage I and II disease (100% vs. 70%), stage III and IV disease (100% vs. 50%), and any-stage disease (100% vs. 67%).
When set at 100% specificity, the multiomics test outperformed a commercially available plasma ctDNA test (Avenio, Roche) set at 75% specificity. The multiomics test yielded a higher sensitivity for stage I and II disease (94% vs. 38%), stage III and IV disease (91% vs. 55%), and any-stage disease (90% vs. 47%).
At a specificity of 94% for both tests, the multiomics test yielded a higher sensitivity than plasma CEA level for stage I and II disease (94% vs. 18%), stage III and IV disease (91% vs. 45%), and any-stage disease (91% vs. 31%).
“Although there were many exciting aspects to this study, the test’s ability to detect cancers without loss of sensitivity for early-stage cancers was striking to me,” said Michael J. Hall, MD, of Fox Chase Cancer Center in Philadelphia, who was not involved in the study. “The loss of sensitivity in early tumors has been a limitation of other tests – FOBT [fecal occult blood test], FIT – so if this is replicable, this is exciting.”
Although the study was small for a CRC screening assessment, “the preliminary results presented in the poster were certainly compelling enough to support more research,” Dr. Hall said.
Dr. Putcha said that the test will be validated in a prospective, multicenter trial of roughly 10,000 participants at average risk, expected to open later this year. Further research will also help assess the test’s performance among patients with inflammatory bowel disease, for whom false-positive results with some screening tests have been problematic.
The study was sponsored by Freenome. Dr. Putcha is employed by Freenome and has a relationship with Palmetto GBA. Dr. Hall disclosed relationships with Ambry Genetics, AstraZeneca, Caris Life Sciences, Foundation Medicine, Invitae, and Myriad Genetics, and he shares a patent with institutional colleagues for a novel method to investigate hereditary CRC genes.
SOURCE: Putcha G et al. 2020 GI Cancers Symposium, Abstract 66.
Visit the AGA GI Patient Center for education to share with your patients about currently available CRC screenings at https://www.gastro.org/
SAN FRANCISCO – A blood-based test that integrates data from multiple molecular “omes,” such as the genome and proteome, performs well at spotting early-stage colorectal cancer (CRC), the AI-EMERGE study suggests.
Moreover, the test netted better sensitivity than a fecal immunochemical test (FIT), a circulating tumor DNA (ctDNA) test, and a carcinoembryonic antigen (CEA) test.
Findings were reported in a poster session at the 2020 GI Cancers Symposium, which is cosponsored by the American Gastroenterological Association, American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology.
“Today, about a third of age-appropriate adults are not up to date with [CRC] screening,” lead study investigator Girish Putcha, MD, PhD, chief medical officer of Freenome in San Francisco, noted at the symposium. “A noninvasive blood-based screening test having high sensitivity and specificity for [CRC] generally, but especially for early-stage disease, could help improve adherence and ultimately reduce mortality.”
Dr. Putcha and colleagues evaluated a blood-based multiomics test in 32 patients with CRC of all stages and 539 colonoscopy-confirmed negative control subjects.
The test uses a multiomics platform to pick up both tumor-derived signal and non–tumor-derived signal from the body’s immune response and other sources. The test uses machine learning, and entails whole-genome sequencing, bisulfite sequencing (for assessment of DNA methylation), and protein quantification methods.
At 94% specificity, the test had a 94% sensitivity for spotting stage I and II CRC, 91% sensitivity for stage III and IV CRC, and 91% sensitivity for CRC of any stage. By location, sensitivity was 92% for distal tumors and 88% for proximal tumors.
The multiomics test outperformed a ctDNA test, a CEA test, and a FIT. At a specificity of 96% for both tests, the multiomics test yielded a higher sensitivity than a commercially available FIT stool test (OC-Auto FIT, Polymedco) for stage I and II disease (100% vs. 70%), stage III and IV disease (100% vs. 50%), and any-stage disease (100% vs. 67%).
When set at 100% specificity, the multiomics test outperformed a commercially available plasma ctDNA test (Avenio, Roche) set at 75% specificity. The multiomics test yielded a higher sensitivity for stage I and II disease (94% vs. 38%), stage III and IV disease (91% vs. 55%), and any-stage disease (90% vs. 47%).
At a specificity of 94% for both tests, the multiomics test yielded a higher sensitivity than plasma CEA level for stage I and II disease (94% vs. 18%), stage III and IV disease (91% vs. 45%), and any-stage disease (91% vs. 31%).
“Although there were many exciting aspects to this study, the test’s ability to detect cancers without loss of sensitivity for early-stage cancers was striking to me,” said Michael J. Hall, MD, of Fox Chase Cancer Center in Philadelphia, who was not involved in the study. “The loss of sensitivity in early tumors has been a limitation of other tests – FOBT [fecal occult blood test], FIT – so if this is replicable, this is exciting.”
Although the study was small for a CRC screening assessment, “the preliminary results presented in the poster were certainly compelling enough to support more research,” Dr. Hall said.
Dr. Putcha said that the test will be validated in a prospective, multicenter trial of roughly 10,000 participants at average risk, expected to open later this year. Further research will also help assess the test’s performance among patients with inflammatory bowel disease, for whom false-positive results with some screening tests have been problematic.
The study was sponsored by Freenome. Dr. Putcha is employed by Freenome and has a relationship with Palmetto GBA. Dr. Hall disclosed relationships with Ambry Genetics, AstraZeneca, Caris Life Sciences, Foundation Medicine, Invitae, and Myriad Genetics, and he shares a patent with institutional colleagues for a novel method to investigate hereditary CRC genes.
SOURCE: Putcha G et al. 2020 GI Cancers Symposium, Abstract 66.
Visit the AGA GI Patient Center for education to share with your patients about currently available CRC screenings at https://www.gastro.org/
SAN FRANCISCO – A blood-based test that integrates data from multiple molecular “omes,” such as the genome and proteome, performs well at spotting early-stage colorectal cancer (CRC), the AI-EMERGE study suggests.
Moreover, the test netted better sensitivity than a fecal immunochemical test (FIT), a circulating tumor DNA (ctDNA) test, and a carcinoembryonic antigen (CEA) test.
Findings were reported in a poster session at the 2020 GI Cancers Symposium, which is cosponsored by the American Gastroenterological Association, American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology.
“Today, about a third of age-appropriate adults are not up to date with [CRC] screening,” lead study investigator Girish Putcha, MD, PhD, chief medical officer of Freenome in San Francisco, noted at the symposium. “A noninvasive blood-based screening test having high sensitivity and specificity for [CRC] generally, but especially for early-stage disease, could help improve adherence and ultimately reduce mortality.”
Dr. Putcha and colleagues evaluated a blood-based multiomics test in 32 patients with CRC of all stages and 539 colonoscopy-confirmed negative control subjects.
The test uses a multiomics platform to pick up both tumor-derived signal and non–tumor-derived signal from the body’s immune response and other sources. The test uses machine learning, and entails whole-genome sequencing, bisulfite sequencing (for assessment of DNA methylation), and protein quantification methods.
At 94% specificity, the test had a 94% sensitivity for spotting stage I and II CRC, 91% sensitivity for stage III and IV CRC, and 91% sensitivity for CRC of any stage. By location, sensitivity was 92% for distal tumors and 88% for proximal tumors.
The multiomics test outperformed a ctDNA test, a CEA test, and a FIT. At a specificity of 96% for both tests, the multiomics test yielded a higher sensitivity than a commercially available FIT stool test (OC-Auto FIT, Polymedco) for stage I and II disease (100% vs. 70%), stage III and IV disease (100% vs. 50%), and any-stage disease (100% vs. 67%).
When set at 100% specificity, the multiomics test outperformed a commercially available plasma ctDNA test (Avenio, Roche) set at 75% specificity. The multiomics test yielded a higher sensitivity for stage I and II disease (94% vs. 38%), stage III and IV disease (91% vs. 55%), and any-stage disease (90% vs. 47%).
At a specificity of 94% for both tests, the multiomics test yielded a higher sensitivity than plasma CEA level for stage I and II disease (94% vs. 18%), stage III and IV disease (91% vs. 45%), and any-stage disease (91% vs. 31%).
“Although there were many exciting aspects to this study, the test’s ability to detect cancers without loss of sensitivity for early-stage cancers was striking to me,” said Michael J. Hall, MD, of Fox Chase Cancer Center in Philadelphia, who was not involved in the study. “The loss of sensitivity in early tumors has been a limitation of other tests – FOBT [fecal occult blood test], FIT – so if this is replicable, this is exciting.”
Although the study was small for a CRC screening assessment, “the preliminary results presented in the poster were certainly compelling enough to support more research,” Dr. Hall said.
Dr. Putcha said that the test will be validated in a prospective, multicenter trial of roughly 10,000 participants at average risk, expected to open later this year. Further research will also help assess the test’s performance among patients with inflammatory bowel disease, for whom false-positive results with some screening tests have been problematic.
The study was sponsored by Freenome. Dr. Putcha is employed by Freenome and has a relationship with Palmetto GBA. Dr. Hall disclosed relationships with Ambry Genetics, AstraZeneca, Caris Life Sciences, Foundation Medicine, Invitae, and Myriad Genetics, and he shares a patent with institutional colleagues for a novel method to investigate hereditary CRC genes.
SOURCE: Putcha G et al. 2020 GI Cancers Symposium, Abstract 66.
Visit the AGA GI Patient Center for education to share with your patients about currently available CRC screenings at https://www.gastro.org/
Multiomics blood test outperforms other tests for colorectal cancer screening
SAN FRANCISCO – A blood-based test that integrates data from multiple molecular “omes,” such as the genome and proteome, performs well at spotting early-stage colorectal cancer, the AI-EMERGE study suggests.
Moreover, the test netted better sensitivity than a fecal immunochemical test (FIT), a circulating tumor DNA (ctDNA) test, and a carcinoembryonic antigen (CEA) test.
These findings were reported in a poster session at the 2020 GI Cancers Symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology.
“Today, about a third of age-appropriate adults are not up to date with colorectal cancer screening,” lead study investigator Girish Putcha, MD, PhD, chief medical officer of Freenome in San Francisco, noted at the symposium. “A noninvasive blood-based screening test having high sensitivity and specificity for colorectal cancer generally, but especially for early-stage disease, could help improve adherence and ultimately reduce mortality.”
Dr. Putcha and colleagues evaluated a blood-based multiomics test in 32 patients with colorectal cancer of all stages and 539 colonoscopy-confirmed negative control subjects.
The test uses a multiomics platform to pick up both tumor-derived signal and non–tumor-derived signal from the body’s immune response and other sources. The test uses machine learning, and entails whole-genome sequencing, bisulfite sequencing (for assessment of DNA methylation), and protein quantification methods.
At 94% specificity, the test had a 94% sensitivity for spotting stage I and II colorectal cancer, 91% sensitivity for stage III and IV colorectal cancer, and 91% sensitivity for colorectal cancer of any stage. By location, sensitivity was 92% for distal tumors and 88% for proximal tumors.
The multiomics test outperformed a ctDNA test, a CEA test, and a FIT. At a specificity of 96% for both tests, the multiomics test yielded a higher sensitivity than a commercially available FIT stool test (OC-Auto FIT, Polymedco) for stage I and II disease (100% vs. 70%), stage III and IV disease (100% vs. 50%), and any-stage disease (100% vs. 67%).
When set at 100% specificity, the multiomics test outperformed a commercially available plasma ctDNA test (Avenio, Roche) set at 75% specificity. The multiomics test yielded a higher sensitivity for stage I and II disease (94% vs. 38%), stage III and IV disease (91% vs. 55%), and any-stage disease (90% vs. 47%).
At a specificity of 94% for both tests, the multiomics test yielded a higher sensitivity than plasma CEA level for stage I and II disease (94% vs. 18%), stage III and IV disease (91% vs. 45%), and any-stage disease (91% vs. 31%).
“Although there were many exciting aspects to this study, the test’s ability to detect cancers without loss of sensitivity for early-stage cancers was striking to me,” said Michael J. Hall, MD, of Fox Chase Cancer Center in Philadelphia, who was not involved in this study. “The loss of sensitivity in early tumors has been a limitation of other tests – FOBT [fecal occult blood test], FIT – so if this is replicable, this is exciting.”
Dr. Hall added that the need for only a blood sample would be a plus in screening healthy people. “When we consider the discomfort and inconvenience of colonoscopy, mammogram, and prostate cancer screening, and how they lead to reduced uptake of screening, the attractiveness of a noninvasive blood-based screening only increases further,” he elaborated.
Although the study was small for a colorectal cancer screening assessment, “the preliminary results presented in the poster were certainly compelling enough to support more research,” Dr. Hall said.
Dr. Putcha said that the test will be validated in a prospective, multicenter trial of roughly 10,000 participants at average risk, expected to open later this year. Further research will also help assess the test’s performance among patients with inflammatory bowel disease, for whom false-positive results with some available screening tests have been problematic.
The current study was sponsored by Freenome. Dr. Putcha is employed by Freenome and has a relationship with Palmetto GBA. Dr. Hall disclosed relationships with Ambry Genetics, AstraZeneca, Caris Life Sciences, Foundation Medicine, Invitae, and Myriad Genetics, and he shares a patent with institutional colleagues for a novel method to investigate hereditary colorectal cancer genes.
*This story was updated on Feb. 4, 2020.
SOURCE: Putcha G et al. 2020 GI Cancers Symposium, Abstract 66.
SAN FRANCISCO – A blood-based test that integrates data from multiple molecular “omes,” such as the genome and proteome, performs well at spotting early-stage colorectal cancer, the AI-EMERGE study suggests.
Moreover, the test netted better sensitivity than a fecal immunochemical test (FIT), a circulating tumor DNA (ctDNA) test, and a carcinoembryonic antigen (CEA) test.
These findings were reported in a poster session at the 2020 GI Cancers Symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology.
“Today, about a third of age-appropriate adults are not up to date with colorectal cancer screening,” lead study investigator Girish Putcha, MD, PhD, chief medical officer of Freenome in San Francisco, noted at the symposium. “A noninvasive blood-based screening test having high sensitivity and specificity for colorectal cancer generally, but especially for early-stage disease, could help improve adherence and ultimately reduce mortality.”
Dr. Putcha and colleagues evaluated a blood-based multiomics test in 32 patients with colorectal cancer of all stages and 539 colonoscopy-confirmed negative control subjects.
The test uses a multiomics platform to pick up both tumor-derived signal and non–tumor-derived signal from the body’s immune response and other sources. The test uses machine learning, and entails whole-genome sequencing, bisulfite sequencing (for assessment of DNA methylation), and protein quantification methods.
At 94% specificity, the test had a 94% sensitivity for spotting stage I and II colorectal cancer, 91% sensitivity for stage III and IV colorectal cancer, and 91% sensitivity for colorectal cancer of any stage. By location, sensitivity was 92% for distal tumors and 88% for proximal tumors.
The multiomics test outperformed a ctDNA test, a CEA test, and a FIT. At a specificity of 96% for both tests, the multiomics test yielded a higher sensitivity than a commercially available FIT stool test (OC-Auto FIT, Polymedco) for stage I and II disease (100% vs. 70%), stage III and IV disease (100% vs. 50%), and any-stage disease (100% vs. 67%).
When set at 100% specificity, the multiomics test outperformed a commercially available plasma ctDNA test (Avenio, Roche) set at 75% specificity. The multiomics test yielded a higher sensitivity for stage I and II disease (94% vs. 38%), stage III and IV disease (91% vs. 55%), and any-stage disease (90% vs. 47%).
At a specificity of 94% for both tests, the multiomics test yielded a higher sensitivity than plasma CEA level for stage I and II disease (94% vs. 18%), stage III and IV disease (91% vs. 45%), and any-stage disease (91% vs. 31%).
“Although there were many exciting aspects to this study, the test’s ability to detect cancers without loss of sensitivity for early-stage cancers was striking to me,” said Michael J. Hall, MD, of Fox Chase Cancer Center in Philadelphia, who was not involved in this study. “The loss of sensitivity in early tumors has been a limitation of other tests – FOBT [fecal occult blood test], FIT – so if this is replicable, this is exciting.”
Dr. Hall added that the need for only a blood sample would be a plus in screening healthy people. “When we consider the discomfort and inconvenience of colonoscopy, mammogram, and prostate cancer screening, and how they lead to reduced uptake of screening, the attractiveness of a noninvasive blood-based screening only increases further,” he elaborated.
Although the study was small for a colorectal cancer screening assessment, “the preliminary results presented in the poster were certainly compelling enough to support more research,” Dr. Hall said.
Dr. Putcha said that the test will be validated in a prospective, multicenter trial of roughly 10,000 participants at average risk, expected to open later this year. Further research will also help assess the test’s performance among patients with inflammatory bowel disease, for whom false-positive results with some available screening tests have been problematic.
The current study was sponsored by Freenome. Dr. Putcha is employed by Freenome and has a relationship with Palmetto GBA. Dr. Hall disclosed relationships with Ambry Genetics, AstraZeneca, Caris Life Sciences, Foundation Medicine, Invitae, and Myriad Genetics, and he shares a patent with institutional colleagues for a novel method to investigate hereditary colorectal cancer genes.
*This story was updated on Feb. 4, 2020.
SOURCE: Putcha G et al. 2020 GI Cancers Symposium, Abstract 66.
SAN FRANCISCO – A blood-based test that integrates data from multiple molecular “omes,” such as the genome and proteome, performs well at spotting early-stage colorectal cancer, the AI-EMERGE study suggests.
Moreover, the test netted better sensitivity than a fecal immunochemical test (FIT), a circulating tumor DNA (ctDNA) test, and a carcinoembryonic antigen (CEA) test.
These findings were reported in a poster session at the 2020 GI Cancers Symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology.
“Today, about a third of age-appropriate adults are not up to date with colorectal cancer screening,” lead study investigator Girish Putcha, MD, PhD, chief medical officer of Freenome in San Francisco, noted at the symposium. “A noninvasive blood-based screening test having high sensitivity and specificity for colorectal cancer generally, but especially for early-stage disease, could help improve adherence and ultimately reduce mortality.”
Dr. Putcha and colleagues evaluated a blood-based multiomics test in 32 patients with colorectal cancer of all stages and 539 colonoscopy-confirmed negative control subjects.
The test uses a multiomics platform to pick up both tumor-derived signal and non–tumor-derived signal from the body’s immune response and other sources. The test uses machine learning, and entails whole-genome sequencing, bisulfite sequencing (for assessment of DNA methylation), and protein quantification methods.
At 94% specificity, the test had a 94% sensitivity for spotting stage I and II colorectal cancer, 91% sensitivity for stage III and IV colorectal cancer, and 91% sensitivity for colorectal cancer of any stage. By location, sensitivity was 92% for distal tumors and 88% for proximal tumors.
The multiomics test outperformed a ctDNA test, a CEA test, and a FIT. At a specificity of 96% for both tests, the multiomics test yielded a higher sensitivity than a commercially available FIT stool test (OC-Auto FIT, Polymedco) for stage I and II disease (100% vs. 70%), stage III and IV disease (100% vs. 50%), and any-stage disease (100% vs. 67%).
When set at 100% specificity, the multiomics test outperformed a commercially available plasma ctDNA test (Avenio, Roche) set at 75% specificity. The multiomics test yielded a higher sensitivity for stage I and II disease (94% vs. 38%), stage III and IV disease (91% vs. 55%), and any-stage disease (90% vs. 47%).
At a specificity of 94% for both tests, the multiomics test yielded a higher sensitivity than plasma CEA level for stage I and II disease (94% vs. 18%), stage III and IV disease (91% vs. 45%), and any-stage disease (91% vs. 31%).
“Although there were many exciting aspects to this study, the test’s ability to detect cancers without loss of sensitivity for early-stage cancers was striking to me,” said Michael J. Hall, MD, of Fox Chase Cancer Center in Philadelphia, who was not involved in this study. “The loss of sensitivity in early tumors has been a limitation of other tests – FOBT [fecal occult blood test], FIT – so if this is replicable, this is exciting.”
Dr. Hall added that the need for only a blood sample would be a plus in screening healthy people. “When we consider the discomfort and inconvenience of colonoscopy, mammogram, and prostate cancer screening, and how they lead to reduced uptake of screening, the attractiveness of a noninvasive blood-based screening only increases further,” he elaborated.
Although the study was small for a colorectal cancer screening assessment, “the preliminary results presented in the poster were certainly compelling enough to support more research,” Dr. Hall said.
Dr. Putcha said that the test will be validated in a prospective, multicenter trial of roughly 10,000 participants at average risk, expected to open later this year. Further research will also help assess the test’s performance among patients with inflammatory bowel disease, for whom false-positive results with some available screening tests have been problematic.
The current study was sponsored by Freenome. Dr. Putcha is employed by Freenome and has a relationship with Palmetto GBA. Dr. Hall disclosed relationships with Ambry Genetics, AstraZeneca, Caris Life Sciences, Foundation Medicine, Invitae, and Myriad Genetics, and he shares a patent with institutional colleagues for a novel method to investigate hereditary colorectal cancer genes.
*This story was updated on Feb. 4, 2020.
SOURCE: Putcha G et al. 2020 GI Cancers Symposium, Abstract 66.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Avelumab maintenance in gastric cancer is down but maybe not out
SAN FRANCISCO – Maintenance therapy with avelumab does not prolong survival in patients with advanced gastric cancer relative to continued chemotherapy, results of the JAVELIN Gastric 100 trial suggest.
However, it may not be end of the line for avelumab in this setting, as the checkpoint inhibitor may benefit certain subgroups of patients, according to Markus H. Moehler, MD, PhD, of the Johannes Gutenberg-University Clinic in Mainz, Germany, who presented results from the trial at the symposium.
In the phase 3 trial, investigators enrolled 805 patients with untreated locally advanced or metastatic HER2-negative gastric or gastroesophageal junction cancer. All patients received first-line chemotherapy.
The 499 patients (62%) who did not experience progression were randomized to receive the anti– programmed death-ligand 1 (PD-L1) antibody avelumab (n = 249) or continued chemotherapy (n = 250). There were 6 patients in the avelumab arm and 12 in the chemotherapy arm who did not receive maintenance treatment, and 7 patients in the chemotherapy arm received best supportive care as maintenance.
Efficacy and safety
The minimum follow-up was 18 months. The median overall survival in the entire population was about the same for both treatment groups, 10.4 months with avelumab and 10.9 months with chemotherapy (P = .1779).
Findings were similar among the 12.3% of patients whose tumors were PD-L1 positive as defined by staining of at least 1% of tumor cells. The median overall survival in this group was 16.2 months with avelumab and 17.7 months with chemotherapy (P = .6352).
On exploratory analysis, results with avelumab were more favorable among the 64.3% of patients whose tumors were PD-L1 positive as defined by a combined positive score (CPS) of 1 or greater. The median overall survival in this group was 14.9 months with avelumab and 11.6 months with chemotherapy.
In subgroup analyses by other characteristics, avelumab appeared to have the edge among patients free of metastases at baseline. In this group, the median overall survival was 16.3 months with avelumab, compared with 10.7 months with chemotherapy (hazard ratio for death, 0.52).
Among all patients, the pattern comparing avelumab with chemotherapy was similar for median progression-free survival (3.2 months vs. 4.4 months) and objective response rate (13.3% vs. 14.4%). The median duration of response was not reached.
“JAVELIN Gastric 100 did not meet its primary objective of demonstrating superior overall survival with avelumab maintenance versus chemotherapy or best supportive care in gastric cancer, either in all randomized patients or in the PD-L1–positive population,” Dr. Moehler said. “However, avelumab maintenance showed clear clinical activity. Further studies are needed to identify patients who can derive benefit from checkpoint inhibitor therapy across the continuum of care with gastric and gastroesophageal junction cancer.”
The avelumab and chemotherapy groups had similar rates of any grade 3 or higher adverse events (54.3% vs. 53.8%), but the avelumab group had a lower rate of treatment-related grade 3 or higher adverse events (12.8% vs. 32.8%).
A ‘yin-yang’ pattern of survival
“Monotherapy checkpoint blockade with anti–programmed death-1 (PD-1) and anti–PD-L1 inhibitors has had relatively unimpressive results in gastroesophageal adenocarcinoma as a whole,” said invited discussant Daniel V. T. Catenacci, MD, of University of Chicago Medicine.
He added that the JAVELIN Gastric 100 survival analysis was noteworthy for the presence of a “yin-yang” pattern, whereby the avelumab curve during follow-up was lower than the chemotherapy curve initially but came out on top eventually.
The 12-month overall survival rate was 43.6% with avelumab and 45.3% with chemotherapy. The 24-month overall survival rates were 22.1% and 15.5%, respectively.
This type of pattern is seen in many similar gastroesophageal adenocarcinoma trials of checkpoint inhibitor monotherapy, even among patients selected for higher CPS, Dr. Catenacci noted.
“This tells us that standard chemotherapy is better in a large subgroup of patients and worse in a separate subgroup: those with MSI-high [microsatellite instability–high], and then MSS [microsatellite stable] with even higher PD-L1 scores like CPS greater than 50, low burden of disease (few metastatic sites), preserved performance status, EBV [Epstein-Barr virus] positivity, Asians within global studies compared with non-Asians, and other unknown factors,” Dr. Catenacci explained.
He commended the design of the JAVELIN Gastric 100 trial, whereby the 38% of patients having rapidly progressive disease were excluded, as this subset is known to fare poorly on checkpoint inhibitor monotherapy.
“This could be potentially a great way to select for those patients most likely to benefit,” Dr. Catenacci said. “Unfortunately, even despite that large fallout, the yin-yang curve was still observed in the intention-to-treat population (unselected by any biomarker). This tells us that, even among the most stable and best prognostic patients, checkpoint blockade is still inferior to standard chemotherapy in a large subgroup of patients.”
However, among patients with a CPS of at least 1, the overall survival curve was consistently higher with avelumab.
“So perhaps by excluding patients with rapid disease progression (about 40% of patients) and then those that are CPS 0 (about 33% more of the total), you can then safely switch to monotherapy checkpoint blockade to first do no harm, and also to do better than standard chemotherapy,” Dr. Catenacci proposed.
“However, we have to be careful, as this was an unplanned retrospective analysis and so should be confirmed prospectively. We might also argue that a higher CPS cut off of greater than or equal to 10 could enrich for the benefit observed. Future ongoing phase 3 studies may help to further increase our understanding of where and where not to implement checkpoint monotherapy or combination therapy with standard chemotherapy.”
The JAVELIN Gastric 100 trial was sponsored by EMD Serono and Merck KGaA, which market avelumab in collaboration with Pfizer. Dr. Moehler disclosed relationships with these companies and many others. Dr. Catenacci disclosed relationships with Merck and other companies.
The 2020 GI Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
SOURCE: Moehler MH et al. 2020 GI Cancers Symposium, Abstract 278.
SAN FRANCISCO – Maintenance therapy with avelumab does not prolong survival in patients with advanced gastric cancer relative to continued chemotherapy, results of the JAVELIN Gastric 100 trial suggest.
However, it may not be end of the line for avelumab in this setting, as the checkpoint inhibitor may benefit certain subgroups of patients, according to Markus H. Moehler, MD, PhD, of the Johannes Gutenberg-University Clinic in Mainz, Germany, who presented results from the trial at the symposium.
In the phase 3 trial, investigators enrolled 805 patients with untreated locally advanced or metastatic HER2-negative gastric or gastroesophageal junction cancer. All patients received first-line chemotherapy.
The 499 patients (62%) who did not experience progression were randomized to receive the anti– programmed death-ligand 1 (PD-L1) antibody avelumab (n = 249) or continued chemotherapy (n = 250). There were 6 patients in the avelumab arm and 12 in the chemotherapy arm who did not receive maintenance treatment, and 7 patients in the chemotherapy arm received best supportive care as maintenance.
Efficacy and safety
The minimum follow-up was 18 months. The median overall survival in the entire population was about the same for both treatment groups, 10.4 months with avelumab and 10.9 months with chemotherapy (P = .1779).
Findings were similar among the 12.3% of patients whose tumors were PD-L1 positive as defined by staining of at least 1% of tumor cells. The median overall survival in this group was 16.2 months with avelumab and 17.7 months with chemotherapy (P = .6352).
On exploratory analysis, results with avelumab were more favorable among the 64.3% of patients whose tumors were PD-L1 positive as defined by a combined positive score (CPS) of 1 or greater. The median overall survival in this group was 14.9 months with avelumab and 11.6 months with chemotherapy.
In subgroup analyses by other characteristics, avelumab appeared to have the edge among patients free of metastases at baseline. In this group, the median overall survival was 16.3 months with avelumab, compared with 10.7 months with chemotherapy (hazard ratio for death, 0.52).
Among all patients, the pattern comparing avelumab with chemotherapy was similar for median progression-free survival (3.2 months vs. 4.4 months) and objective response rate (13.3% vs. 14.4%). The median duration of response was not reached.
“JAVELIN Gastric 100 did not meet its primary objective of demonstrating superior overall survival with avelumab maintenance versus chemotherapy or best supportive care in gastric cancer, either in all randomized patients or in the PD-L1–positive population,” Dr. Moehler said. “However, avelumab maintenance showed clear clinical activity. Further studies are needed to identify patients who can derive benefit from checkpoint inhibitor therapy across the continuum of care with gastric and gastroesophageal junction cancer.”
The avelumab and chemotherapy groups had similar rates of any grade 3 or higher adverse events (54.3% vs. 53.8%), but the avelumab group had a lower rate of treatment-related grade 3 or higher adverse events (12.8% vs. 32.8%).
A ‘yin-yang’ pattern of survival
“Monotherapy checkpoint blockade with anti–programmed death-1 (PD-1) and anti–PD-L1 inhibitors has had relatively unimpressive results in gastroesophageal adenocarcinoma as a whole,” said invited discussant Daniel V. T. Catenacci, MD, of University of Chicago Medicine.
He added that the JAVELIN Gastric 100 survival analysis was noteworthy for the presence of a “yin-yang” pattern, whereby the avelumab curve during follow-up was lower than the chemotherapy curve initially but came out on top eventually.
The 12-month overall survival rate was 43.6% with avelumab and 45.3% with chemotherapy. The 24-month overall survival rates were 22.1% and 15.5%, respectively.
This type of pattern is seen in many similar gastroesophageal adenocarcinoma trials of checkpoint inhibitor monotherapy, even among patients selected for higher CPS, Dr. Catenacci noted.
“This tells us that standard chemotherapy is better in a large subgroup of patients and worse in a separate subgroup: those with MSI-high [microsatellite instability–high], and then MSS [microsatellite stable] with even higher PD-L1 scores like CPS greater than 50, low burden of disease (few metastatic sites), preserved performance status, EBV [Epstein-Barr virus] positivity, Asians within global studies compared with non-Asians, and other unknown factors,” Dr. Catenacci explained.
He commended the design of the JAVELIN Gastric 100 trial, whereby the 38% of patients having rapidly progressive disease were excluded, as this subset is known to fare poorly on checkpoint inhibitor monotherapy.
“This could be potentially a great way to select for those patients most likely to benefit,” Dr. Catenacci said. “Unfortunately, even despite that large fallout, the yin-yang curve was still observed in the intention-to-treat population (unselected by any biomarker). This tells us that, even among the most stable and best prognostic patients, checkpoint blockade is still inferior to standard chemotherapy in a large subgroup of patients.”
However, among patients with a CPS of at least 1, the overall survival curve was consistently higher with avelumab.
“So perhaps by excluding patients with rapid disease progression (about 40% of patients) and then those that are CPS 0 (about 33% more of the total), you can then safely switch to monotherapy checkpoint blockade to first do no harm, and also to do better than standard chemotherapy,” Dr. Catenacci proposed.
“However, we have to be careful, as this was an unplanned retrospective analysis and so should be confirmed prospectively. We might also argue that a higher CPS cut off of greater than or equal to 10 could enrich for the benefit observed. Future ongoing phase 3 studies may help to further increase our understanding of where and where not to implement checkpoint monotherapy or combination therapy with standard chemotherapy.”
The JAVELIN Gastric 100 trial was sponsored by EMD Serono and Merck KGaA, which market avelumab in collaboration with Pfizer. Dr. Moehler disclosed relationships with these companies and many others. Dr. Catenacci disclosed relationships with Merck and other companies.
The 2020 GI Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
SOURCE: Moehler MH et al. 2020 GI Cancers Symposium, Abstract 278.
SAN FRANCISCO – Maintenance therapy with avelumab does not prolong survival in patients with advanced gastric cancer relative to continued chemotherapy, results of the JAVELIN Gastric 100 trial suggest.
However, it may not be end of the line for avelumab in this setting, as the checkpoint inhibitor may benefit certain subgroups of patients, according to Markus H. Moehler, MD, PhD, of the Johannes Gutenberg-University Clinic in Mainz, Germany, who presented results from the trial at the symposium.
In the phase 3 trial, investigators enrolled 805 patients with untreated locally advanced or metastatic HER2-negative gastric or gastroesophageal junction cancer. All patients received first-line chemotherapy.
The 499 patients (62%) who did not experience progression were randomized to receive the anti– programmed death-ligand 1 (PD-L1) antibody avelumab (n = 249) or continued chemotherapy (n = 250). There were 6 patients in the avelumab arm and 12 in the chemotherapy arm who did not receive maintenance treatment, and 7 patients in the chemotherapy arm received best supportive care as maintenance.
Efficacy and safety
The minimum follow-up was 18 months. The median overall survival in the entire population was about the same for both treatment groups, 10.4 months with avelumab and 10.9 months with chemotherapy (P = .1779).
Findings were similar among the 12.3% of patients whose tumors were PD-L1 positive as defined by staining of at least 1% of tumor cells. The median overall survival in this group was 16.2 months with avelumab and 17.7 months with chemotherapy (P = .6352).
On exploratory analysis, results with avelumab were more favorable among the 64.3% of patients whose tumors were PD-L1 positive as defined by a combined positive score (CPS) of 1 or greater. The median overall survival in this group was 14.9 months with avelumab and 11.6 months with chemotherapy.
In subgroup analyses by other characteristics, avelumab appeared to have the edge among patients free of metastases at baseline. In this group, the median overall survival was 16.3 months with avelumab, compared with 10.7 months with chemotherapy (hazard ratio for death, 0.52).
Among all patients, the pattern comparing avelumab with chemotherapy was similar for median progression-free survival (3.2 months vs. 4.4 months) and objective response rate (13.3% vs. 14.4%). The median duration of response was not reached.
“JAVELIN Gastric 100 did not meet its primary objective of demonstrating superior overall survival with avelumab maintenance versus chemotherapy or best supportive care in gastric cancer, either in all randomized patients or in the PD-L1–positive population,” Dr. Moehler said. “However, avelumab maintenance showed clear clinical activity. Further studies are needed to identify patients who can derive benefit from checkpoint inhibitor therapy across the continuum of care with gastric and gastroesophageal junction cancer.”
The avelumab and chemotherapy groups had similar rates of any grade 3 or higher adverse events (54.3% vs. 53.8%), but the avelumab group had a lower rate of treatment-related grade 3 or higher adverse events (12.8% vs. 32.8%).
A ‘yin-yang’ pattern of survival
“Monotherapy checkpoint blockade with anti–programmed death-1 (PD-1) and anti–PD-L1 inhibitors has had relatively unimpressive results in gastroesophageal adenocarcinoma as a whole,” said invited discussant Daniel V. T. Catenacci, MD, of University of Chicago Medicine.
He added that the JAVELIN Gastric 100 survival analysis was noteworthy for the presence of a “yin-yang” pattern, whereby the avelumab curve during follow-up was lower than the chemotherapy curve initially but came out on top eventually.
The 12-month overall survival rate was 43.6% with avelumab and 45.3% with chemotherapy. The 24-month overall survival rates were 22.1% and 15.5%, respectively.
This type of pattern is seen in many similar gastroesophageal adenocarcinoma trials of checkpoint inhibitor monotherapy, even among patients selected for higher CPS, Dr. Catenacci noted.
“This tells us that standard chemotherapy is better in a large subgroup of patients and worse in a separate subgroup: those with MSI-high [microsatellite instability–high], and then MSS [microsatellite stable] with even higher PD-L1 scores like CPS greater than 50, low burden of disease (few metastatic sites), preserved performance status, EBV [Epstein-Barr virus] positivity, Asians within global studies compared with non-Asians, and other unknown factors,” Dr. Catenacci explained.
He commended the design of the JAVELIN Gastric 100 trial, whereby the 38% of patients having rapidly progressive disease were excluded, as this subset is known to fare poorly on checkpoint inhibitor monotherapy.
“This could be potentially a great way to select for those patients most likely to benefit,” Dr. Catenacci said. “Unfortunately, even despite that large fallout, the yin-yang curve was still observed in the intention-to-treat population (unselected by any biomarker). This tells us that, even among the most stable and best prognostic patients, checkpoint blockade is still inferior to standard chemotherapy in a large subgroup of patients.”
However, among patients with a CPS of at least 1, the overall survival curve was consistently higher with avelumab.
“So perhaps by excluding patients with rapid disease progression (about 40% of patients) and then those that are CPS 0 (about 33% more of the total), you can then safely switch to monotherapy checkpoint blockade to first do no harm, and also to do better than standard chemotherapy,” Dr. Catenacci proposed.
“However, we have to be careful, as this was an unplanned retrospective analysis and so should be confirmed prospectively. We might also argue that a higher CPS cut off of greater than or equal to 10 could enrich for the benefit observed. Future ongoing phase 3 studies may help to further increase our understanding of where and where not to implement checkpoint monotherapy or combination therapy with standard chemotherapy.”
The JAVELIN Gastric 100 trial was sponsored by EMD Serono and Merck KGaA, which market avelumab in collaboration with Pfizer. Dr. Moehler disclosed relationships with these companies and many others. Dr. Catenacci disclosed relationships with Merck and other companies.
The 2020 GI Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
SOURCE: Moehler MH et al. 2020 GI Cancers Symposium, Abstract 278.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Dual immunotherapy goes the distance in MSI-H colorectal cancer
SAN FRANCISCO – First-line dual immune checkpoint inhibitor therapy for microsatellite instability–high/DNA mismatch repair–deficient (MSI-H/dMMR) metastatic colorectal cancer has impressive durability, an update of the multicohort CheckMate 142 trial shows.
“We all know that MSI-H colorectal cancer patients have a poor prognosis,” said lead investigator Heinz-Josef Lenz, MD, codirector of the Colorectal Center and section head of the GI oncology program at the University of Southern California Norris Comprehensive Cancer Center, Los Angeles. First-line chemotherapy in this population yields median overall survival on the order of 20-22 months.
The cohort of 45 patients treated on the phase 2 trial received the programmed death–1 inhibitor nivolumab (Opdivo) every 2 weeks, plus a low dose of the CTLA4 inhibitor ipilimumab (Yervoy) every 6 weeks as first-line therapy for MSI-H metastatic colorectal cancer. (Nivolumab, with or without ipilimumab, has received Food and Drug Administration accelerated approval as second-line therapy based on data from other cohorts in the trial.)
Previously reported initial results, at a median follow-up of 13.8 months, showed that the investigator-assessed objective response rate was 60% (ESMO 2018, Abstract LBA18_PR). As of the update, now at a median follow-up of 19.9 months, that rate was 64%, according to data reported at the 2020 GI Cancers Symposium.
“Nivolumab and ipilimumab demonstrates clinically meaningful durable benefits and may present an option for first-line treatment for MSI-H metastatic colorectal cancer patients,” Dr. Lenz summarized.
“The incredible complete response rates and overall response rates seen are never seen with chemotherapy, and it’s very well tolerated, so if I have a choice, I would start with nivolumab-ipilimumab in first-line MSI-H,” he added. “The [National Comprehensive Cancer Network] guidelines recommend that you can start in first line with this combination if patients are not candidates for chemotherapy. So they leave this door open, that you have an opportunity to use immunotherapy in this patient population.”
Choosing single or dual immunotherapy
Given the so-called financial toxicity of dual nivolumab and ipilimumab therapy and lack of a randomized comparison against single-agent nivolumab, a session attendee said, can clinicians simply use the latter?
“Very importantly, in this clinical trial, ipilimumab was given every 6 weeks. As you know, the 2-week regimens are significantly more toxic,” Dr. Lenz noted. The combination using this low dose has safety similar to that seen with nivolumab alone. And in cross-trial comparisons, at least, “the combination seems to be a little bit more active, so I always choose both,” he said, adding that the financial aspects are beyond his purview.
However, session cochair Joseph J.Y. Sung, MD, PhD, MBBS, the Mok Hing Yiu Professor of Medicine in the department of medicine and therapeutics at the Chinese University of Hong Kong, had a different view.
“I think there is still room for a randomized study to prove the combination’s superiority against single immunotherapy,” he said in an interview. “If I’m treating an MSI patient, I would stick to single immunotherapy until I see more evidence that this combination has a substantial improvement in the outcome that is worth the money.”
Study details
The patients studied were unselected for baseline tumor expression of programmed death–ligand 1, with 27% having expression of 1% or greater and 58% having expression below that threshold.
As of the data cutoff for the update, 47% of patients were still on treatment, Dr. Lenz reported at the symposium, sponsored by the American Gastroenterological Association, American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology. The most common reason for stopping treatment was disease progression.
The investigator-assessed objective response rate, the primary endpoint, consisted of complete responses in 9% of patients and partial responses in 56%. (The rate as assessed by blinded independent central reviewers was 58%, consisting of complete responses in 18% and partial responses in 40%.)
“The high response rate was consistent among all evaluated subgroups,” Dr. Lenz noted, with no differences detected by presence or absence of Lynch syndrome and/or specific microsatellite-related mutations.
Median time to response was 2.6 months, and median duration of response was not reached. Median progression-free and overall survival were also not reached, but 15-month rates were 75% and 84%, respectively.
The rate of grade 3-4 treatment-related adverse events was 20%, and the rate of grade 3-4 serious treatment-related adverse events was 11%. Only 4% of patients discontinued treatment because of such events.
Ongoing trials may take immunotherapy even further in this patient population, according to Dr. Lenz. “We are all waiting for the treatments with the immunotherapy in combination with chemo and bevacizumab in first line. Will that change the efficacy and toxicity?” he elaborated. “You can imagine, in the MSI-H patients with the immunotherapy alone, we haven’t reached median progression-free and overall survival, so it may take a long time to get this data.”
Dr. Lenz reported receiving honoraria from Bayer, Boehringer Ingelheim, Merck Serono, and Roche; consulting or advising with Bayer, Merck Serono, Pfizer, and Roche; receiving travel expenses from Bayer, Merck Serono, and Roche. The trial was funded by Bristol-Myers Squibb. Dr. Sung reported that he had no relevant conflicts of interest.
SOURCE: Lenz H-J et al. 2020 GI Cancers Symposium, Abstract 11.
SAN FRANCISCO – First-line dual immune checkpoint inhibitor therapy for microsatellite instability–high/DNA mismatch repair–deficient (MSI-H/dMMR) metastatic colorectal cancer has impressive durability, an update of the multicohort CheckMate 142 trial shows.
“We all know that MSI-H colorectal cancer patients have a poor prognosis,” said lead investigator Heinz-Josef Lenz, MD, codirector of the Colorectal Center and section head of the GI oncology program at the University of Southern California Norris Comprehensive Cancer Center, Los Angeles. First-line chemotherapy in this population yields median overall survival on the order of 20-22 months.
The cohort of 45 patients treated on the phase 2 trial received the programmed death–1 inhibitor nivolumab (Opdivo) every 2 weeks, plus a low dose of the CTLA4 inhibitor ipilimumab (Yervoy) every 6 weeks as first-line therapy for MSI-H metastatic colorectal cancer. (Nivolumab, with or without ipilimumab, has received Food and Drug Administration accelerated approval as second-line therapy based on data from other cohorts in the trial.)
Previously reported initial results, at a median follow-up of 13.8 months, showed that the investigator-assessed objective response rate was 60% (ESMO 2018, Abstract LBA18_PR). As of the update, now at a median follow-up of 19.9 months, that rate was 64%, according to data reported at the 2020 GI Cancers Symposium.
“Nivolumab and ipilimumab demonstrates clinically meaningful durable benefits and may present an option for first-line treatment for MSI-H metastatic colorectal cancer patients,” Dr. Lenz summarized.
“The incredible complete response rates and overall response rates seen are never seen with chemotherapy, and it’s very well tolerated, so if I have a choice, I would start with nivolumab-ipilimumab in first-line MSI-H,” he added. “The [National Comprehensive Cancer Network] guidelines recommend that you can start in first line with this combination if patients are not candidates for chemotherapy. So they leave this door open, that you have an opportunity to use immunotherapy in this patient population.”
Choosing single or dual immunotherapy
Given the so-called financial toxicity of dual nivolumab and ipilimumab therapy and lack of a randomized comparison against single-agent nivolumab, a session attendee said, can clinicians simply use the latter?
“Very importantly, in this clinical trial, ipilimumab was given every 6 weeks. As you know, the 2-week regimens are significantly more toxic,” Dr. Lenz noted. The combination using this low dose has safety similar to that seen with nivolumab alone. And in cross-trial comparisons, at least, “the combination seems to be a little bit more active, so I always choose both,” he said, adding that the financial aspects are beyond his purview.
However, session cochair Joseph J.Y. Sung, MD, PhD, MBBS, the Mok Hing Yiu Professor of Medicine in the department of medicine and therapeutics at the Chinese University of Hong Kong, had a different view.
“I think there is still room for a randomized study to prove the combination’s superiority against single immunotherapy,” he said in an interview. “If I’m treating an MSI patient, I would stick to single immunotherapy until I see more evidence that this combination has a substantial improvement in the outcome that is worth the money.”
Study details
The patients studied were unselected for baseline tumor expression of programmed death–ligand 1, with 27% having expression of 1% or greater and 58% having expression below that threshold.
As of the data cutoff for the update, 47% of patients were still on treatment, Dr. Lenz reported at the symposium, sponsored by the American Gastroenterological Association, American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology. The most common reason for stopping treatment was disease progression.
The investigator-assessed objective response rate, the primary endpoint, consisted of complete responses in 9% of patients and partial responses in 56%. (The rate as assessed by blinded independent central reviewers was 58%, consisting of complete responses in 18% and partial responses in 40%.)
“The high response rate was consistent among all evaluated subgroups,” Dr. Lenz noted, with no differences detected by presence or absence of Lynch syndrome and/or specific microsatellite-related mutations.
Median time to response was 2.6 months, and median duration of response was not reached. Median progression-free and overall survival were also not reached, but 15-month rates were 75% and 84%, respectively.
The rate of grade 3-4 treatment-related adverse events was 20%, and the rate of grade 3-4 serious treatment-related adverse events was 11%. Only 4% of patients discontinued treatment because of such events.
Ongoing trials may take immunotherapy even further in this patient population, according to Dr. Lenz. “We are all waiting for the treatments with the immunotherapy in combination with chemo and bevacizumab in first line. Will that change the efficacy and toxicity?” he elaborated. “You can imagine, in the MSI-H patients with the immunotherapy alone, we haven’t reached median progression-free and overall survival, so it may take a long time to get this data.”
Dr. Lenz reported receiving honoraria from Bayer, Boehringer Ingelheim, Merck Serono, and Roche; consulting or advising with Bayer, Merck Serono, Pfizer, and Roche; receiving travel expenses from Bayer, Merck Serono, and Roche. The trial was funded by Bristol-Myers Squibb. Dr. Sung reported that he had no relevant conflicts of interest.
SOURCE: Lenz H-J et al. 2020 GI Cancers Symposium, Abstract 11.
SAN FRANCISCO – First-line dual immune checkpoint inhibitor therapy for microsatellite instability–high/DNA mismatch repair–deficient (MSI-H/dMMR) metastatic colorectal cancer has impressive durability, an update of the multicohort CheckMate 142 trial shows.
“We all know that MSI-H colorectal cancer patients have a poor prognosis,” said lead investigator Heinz-Josef Lenz, MD, codirector of the Colorectal Center and section head of the GI oncology program at the University of Southern California Norris Comprehensive Cancer Center, Los Angeles. First-line chemotherapy in this population yields median overall survival on the order of 20-22 months.
The cohort of 45 patients treated on the phase 2 trial received the programmed death–1 inhibitor nivolumab (Opdivo) every 2 weeks, plus a low dose of the CTLA4 inhibitor ipilimumab (Yervoy) every 6 weeks as first-line therapy for MSI-H metastatic colorectal cancer. (Nivolumab, with or without ipilimumab, has received Food and Drug Administration accelerated approval as second-line therapy based on data from other cohorts in the trial.)
Previously reported initial results, at a median follow-up of 13.8 months, showed that the investigator-assessed objective response rate was 60% (ESMO 2018, Abstract LBA18_PR). As of the update, now at a median follow-up of 19.9 months, that rate was 64%, according to data reported at the 2020 GI Cancers Symposium.
“Nivolumab and ipilimumab demonstrates clinically meaningful durable benefits and may present an option for first-line treatment for MSI-H metastatic colorectal cancer patients,” Dr. Lenz summarized.
“The incredible complete response rates and overall response rates seen are never seen with chemotherapy, and it’s very well tolerated, so if I have a choice, I would start with nivolumab-ipilimumab in first-line MSI-H,” he added. “The [National Comprehensive Cancer Network] guidelines recommend that you can start in first line with this combination if patients are not candidates for chemotherapy. So they leave this door open, that you have an opportunity to use immunotherapy in this patient population.”
Choosing single or dual immunotherapy
Given the so-called financial toxicity of dual nivolumab and ipilimumab therapy and lack of a randomized comparison against single-agent nivolumab, a session attendee said, can clinicians simply use the latter?
“Very importantly, in this clinical trial, ipilimumab was given every 6 weeks. As you know, the 2-week regimens are significantly more toxic,” Dr. Lenz noted. The combination using this low dose has safety similar to that seen with nivolumab alone. And in cross-trial comparisons, at least, “the combination seems to be a little bit more active, so I always choose both,” he said, adding that the financial aspects are beyond his purview.
However, session cochair Joseph J.Y. Sung, MD, PhD, MBBS, the Mok Hing Yiu Professor of Medicine in the department of medicine and therapeutics at the Chinese University of Hong Kong, had a different view.
“I think there is still room for a randomized study to prove the combination’s superiority against single immunotherapy,” he said in an interview. “If I’m treating an MSI patient, I would stick to single immunotherapy until I see more evidence that this combination has a substantial improvement in the outcome that is worth the money.”
Study details
The patients studied were unselected for baseline tumor expression of programmed death–ligand 1, with 27% having expression of 1% or greater and 58% having expression below that threshold.
As of the data cutoff for the update, 47% of patients were still on treatment, Dr. Lenz reported at the symposium, sponsored by the American Gastroenterological Association, American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology. The most common reason for stopping treatment was disease progression.
The investigator-assessed objective response rate, the primary endpoint, consisted of complete responses in 9% of patients and partial responses in 56%. (The rate as assessed by blinded independent central reviewers was 58%, consisting of complete responses in 18% and partial responses in 40%.)
“The high response rate was consistent among all evaluated subgroups,” Dr. Lenz noted, with no differences detected by presence or absence of Lynch syndrome and/or specific microsatellite-related mutations.
Median time to response was 2.6 months, and median duration of response was not reached. Median progression-free and overall survival were also not reached, but 15-month rates were 75% and 84%, respectively.
The rate of grade 3-4 treatment-related adverse events was 20%, and the rate of grade 3-4 serious treatment-related adverse events was 11%. Only 4% of patients discontinued treatment because of such events.
Ongoing trials may take immunotherapy even further in this patient population, according to Dr. Lenz. “We are all waiting for the treatments with the immunotherapy in combination with chemo and bevacizumab in first line. Will that change the efficacy and toxicity?” he elaborated. “You can imagine, in the MSI-H patients with the immunotherapy alone, we haven’t reached median progression-free and overall survival, so it may take a long time to get this data.”
Dr. Lenz reported receiving honoraria from Bayer, Boehringer Ingelheim, Merck Serono, and Roche; consulting or advising with Bayer, Merck Serono, Pfizer, and Roche; receiving travel expenses from Bayer, Merck Serono, and Roche. The trial was funded by Bristol-Myers Squibb. Dr. Sung reported that he had no relevant conflicts of interest.
SOURCE: Lenz H-J et al. 2020 GI Cancers Symposium, Abstract 11.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Resecting primary tumors fails to boost survival in metastatic CRC
SAN FRANCISCO – The common practice of resecting asymptomatic primary tumors in patients with unresectable metastases of colorectal cancer does not improve survival but does increase morbidity, and it should therefore be discontinued, according to the phase 3 iPACS trial.
About 80% of patients with stage IV colorectal cancer at diagnosis have metastases that cannot be resected. “For asymptomatic patients, there is no consensus regarding resection of the primary tumor. There have been no randomized controlled trials comparing upfront chemotherapy with primary tumor resection,” said lead investigator Yukihide Kanemitsu, MD, department of colorectal surgery, National Cancer Center Hospital, Tokyo.
He and coinvestigators with the Japan Clinical Oncology Group enrolled in the randomized controlled trial 160 patients with untreated stage IV colorectal cancer who did not have any symptoms from their primary and had up to three unresectable sites of metastases (liver, lungs, distant lymph nodes, and/or peritoneum).
The trial was stopped early for futility, Dr. Kanemitsu reported at the 2020 GI Cancers Symposium. Median overall survival was slightly more than 2 years regardless of whether patients immediately received chemotherapy or underwent primary tumor resection before receiving chemotherapy.
However, 4% of the patients who underwent resection died in the postoperative period from complications. And the resection group had more frequent and more severe chemotherapy-related morbidity, with a higher rate of grade 3 and 4 adverse events (49% vs. 36%).
“Chemotherapy remains the standard therapy for asymptomatic unresectable stage IV colorectal cancer patients,” Dr. Kanemitsu concluded. “Primary tumor resection is not recommended for these patients.”
RCTs should remain the gold standard
“As someone who has built my career on health services research over the last decade working with real-world data, I have become alarmed in recent years at what appears to be a conversation in our community about leaving the randomized controlled trial behind and just using real-world evidence,” said invited discussant Christopher M. Booth, MD, professor, departments of oncology and medicine, Queen’s University, Kingston, Ont., and Canada Research Chair in Population Cancer Care. “Fundamentally, I think this is a really bad idea. The randomized controlled trial should remain the gold standard for efficacy of new cancer therapies.”
The high level of use of primary tumor resection has largely been driven by a meta-analysis that found a dramatic reduction in risk of death with this surgery (Ann Surg Oncol. 2014;21:3900-8), he noted. However, a subsequent retrospective cohort study showed that the apparent benefit disappeared with application of rigorous statistical methods that compensated for biases in the data (Cancer. 2017;123:1124-33).
“I completely support the conclusions presented today,” Dr. Booth asserted, citing the lack of efficacy and greater morbidity and postoperative mortality of primary tumor resection in iPACS, along with the totality of research evidence. “While we can learn a lot from real-world data, it cannot replace randomized controlled trials. In our patients with an asymptomatic primary tumor in the context of incurable colorectal cancer, I believe there is no longer a role for primary tumor resection.”
Study details
In the iPACS trial, patients in the primary tumor resection group underwent open or laparoscopic colectomy/high anterior resection with a D1-D3 lymph node dissection. Concurrent resection of involved organs was not permitted, except for the mesentery, small intestine, greater omentum, and ovary.
In the resection group, the time between surgery and start of chemotherapy was 8 to 56 days, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
With a median follow-up of 22.0 months, median overall survival was 25.9 months with primary tumor resection followed by chemotherapy and 26.7 months with chemotherapy alone (hazard ratio for death, 1.10; P = .69). Findings were similar in subgroup analyses. Median progression-free survival was 10.4 and 12.1 months, respectively (hazard ratio for progression or death, 1.08).
Patients in the primary tumor resection group had higher rates of chemotherapy-related grade 3 and 4 paresthesia (5% vs. 1%), hypertension (17% vs. 8%), diarrhea (5% vs. 1%), and neuropathy (14% vs. 9%), Dr. Kanemitsu reported.
In terms of secondary surgeries, the R0 (curative) resection rate was 3% in the primary tumor resection group and 5% in the chemotherapy group. Thirteen percent of patients in the chemotherapy group underwent palliative surgery for symptoms caused by their primary tumor.
Dr. Kanemitsu disclosed that he receives honoraria from Chugai Pharma, Covidien, Ethicon, and Intuitive Surgical, and that he has a consulting or advisory role with Covidien. The study was funded by a Health and Labor Sciences Research Grant for Clinical Cancer Research. Dr. Booth disclosed that he has no conflicts of interest.
SOURCE: Kanemitsu Y et al. 2020 GI Cancers Symposium. Abstract 7.
SAN FRANCISCO – The common practice of resecting asymptomatic primary tumors in patients with unresectable metastases of colorectal cancer does not improve survival but does increase morbidity, and it should therefore be discontinued, according to the phase 3 iPACS trial.
About 80% of patients with stage IV colorectal cancer at diagnosis have metastases that cannot be resected. “For asymptomatic patients, there is no consensus regarding resection of the primary tumor. There have been no randomized controlled trials comparing upfront chemotherapy with primary tumor resection,” said lead investigator Yukihide Kanemitsu, MD, department of colorectal surgery, National Cancer Center Hospital, Tokyo.
He and coinvestigators with the Japan Clinical Oncology Group enrolled in the randomized controlled trial 160 patients with untreated stage IV colorectal cancer who did not have any symptoms from their primary and had up to three unresectable sites of metastases (liver, lungs, distant lymph nodes, and/or peritoneum).
The trial was stopped early for futility, Dr. Kanemitsu reported at the 2020 GI Cancers Symposium. Median overall survival was slightly more than 2 years regardless of whether patients immediately received chemotherapy or underwent primary tumor resection before receiving chemotherapy.
However, 4% of the patients who underwent resection died in the postoperative period from complications. And the resection group had more frequent and more severe chemotherapy-related morbidity, with a higher rate of grade 3 and 4 adverse events (49% vs. 36%).
“Chemotherapy remains the standard therapy for asymptomatic unresectable stage IV colorectal cancer patients,” Dr. Kanemitsu concluded. “Primary tumor resection is not recommended for these patients.”
RCTs should remain the gold standard
“As someone who has built my career on health services research over the last decade working with real-world data, I have become alarmed in recent years at what appears to be a conversation in our community about leaving the randomized controlled trial behind and just using real-world evidence,” said invited discussant Christopher M. Booth, MD, professor, departments of oncology and medicine, Queen’s University, Kingston, Ont., and Canada Research Chair in Population Cancer Care. “Fundamentally, I think this is a really bad idea. The randomized controlled trial should remain the gold standard for efficacy of new cancer therapies.”
The high level of use of primary tumor resection has largely been driven by a meta-analysis that found a dramatic reduction in risk of death with this surgery (Ann Surg Oncol. 2014;21:3900-8), he noted. However, a subsequent retrospective cohort study showed that the apparent benefit disappeared with application of rigorous statistical methods that compensated for biases in the data (Cancer. 2017;123:1124-33).
“I completely support the conclusions presented today,” Dr. Booth asserted, citing the lack of efficacy and greater morbidity and postoperative mortality of primary tumor resection in iPACS, along with the totality of research evidence. “While we can learn a lot from real-world data, it cannot replace randomized controlled trials. In our patients with an asymptomatic primary tumor in the context of incurable colorectal cancer, I believe there is no longer a role for primary tumor resection.”
Study details
In the iPACS trial, patients in the primary tumor resection group underwent open or laparoscopic colectomy/high anterior resection with a D1-D3 lymph node dissection. Concurrent resection of involved organs was not permitted, except for the mesentery, small intestine, greater omentum, and ovary.
In the resection group, the time between surgery and start of chemotherapy was 8 to 56 days, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
With a median follow-up of 22.0 months, median overall survival was 25.9 months with primary tumor resection followed by chemotherapy and 26.7 months with chemotherapy alone (hazard ratio for death, 1.10; P = .69). Findings were similar in subgroup analyses. Median progression-free survival was 10.4 and 12.1 months, respectively (hazard ratio for progression or death, 1.08).
Patients in the primary tumor resection group had higher rates of chemotherapy-related grade 3 and 4 paresthesia (5% vs. 1%), hypertension (17% vs. 8%), diarrhea (5% vs. 1%), and neuropathy (14% vs. 9%), Dr. Kanemitsu reported.
In terms of secondary surgeries, the R0 (curative) resection rate was 3% in the primary tumor resection group and 5% in the chemotherapy group. Thirteen percent of patients in the chemotherapy group underwent palliative surgery for symptoms caused by their primary tumor.
Dr. Kanemitsu disclosed that he receives honoraria from Chugai Pharma, Covidien, Ethicon, and Intuitive Surgical, and that he has a consulting or advisory role with Covidien. The study was funded by a Health and Labor Sciences Research Grant for Clinical Cancer Research. Dr. Booth disclosed that he has no conflicts of interest.
SOURCE: Kanemitsu Y et al. 2020 GI Cancers Symposium. Abstract 7.
SAN FRANCISCO – The common practice of resecting asymptomatic primary tumors in patients with unresectable metastases of colorectal cancer does not improve survival but does increase morbidity, and it should therefore be discontinued, according to the phase 3 iPACS trial.
About 80% of patients with stage IV colorectal cancer at diagnosis have metastases that cannot be resected. “For asymptomatic patients, there is no consensus regarding resection of the primary tumor. There have been no randomized controlled trials comparing upfront chemotherapy with primary tumor resection,” said lead investigator Yukihide Kanemitsu, MD, department of colorectal surgery, National Cancer Center Hospital, Tokyo.
He and coinvestigators with the Japan Clinical Oncology Group enrolled in the randomized controlled trial 160 patients with untreated stage IV colorectal cancer who did not have any symptoms from their primary and had up to three unresectable sites of metastases (liver, lungs, distant lymph nodes, and/or peritoneum).
The trial was stopped early for futility, Dr. Kanemitsu reported at the 2020 GI Cancers Symposium. Median overall survival was slightly more than 2 years regardless of whether patients immediately received chemotherapy or underwent primary tumor resection before receiving chemotherapy.
However, 4% of the patients who underwent resection died in the postoperative period from complications. And the resection group had more frequent and more severe chemotherapy-related morbidity, with a higher rate of grade 3 and 4 adverse events (49% vs. 36%).
“Chemotherapy remains the standard therapy for asymptomatic unresectable stage IV colorectal cancer patients,” Dr. Kanemitsu concluded. “Primary tumor resection is not recommended for these patients.”
RCTs should remain the gold standard
“As someone who has built my career on health services research over the last decade working with real-world data, I have become alarmed in recent years at what appears to be a conversation in our community about leaving the randomized controlled trial behind and just using real-world evidence,” said invited discussant Christopher M. Booth, MD, professor, departments of oncology and medicine, Queen’s University, Kingston, Ont., and Canada Research Chair in Population Cancer Care. “Fundamentally, I think this is a really bad idea. The randomized controlled trial should remain the gold standard for efficacy of new cancer therapies.”
The high level of use of primary tumor resection has largely been driven by a meta-analysis that found a dramatic reduction in risk of death with this surgery (Ann Surg Oncol. 2014;21:3900-8), he noted. However, a subsequent retrospective cohort study showed that the apparent benefit disappeared with application of rigorous statistical methods that compensated for biases in the data (Cancer. 2017;123:1124-33).
“I completely support the conclusions presented today,” Dr. Booth asserted, citing the lack of efficacy and greater morbidity and postoperative mortality of primary tumor resection in iPACS, along with the totality of research evidence. “While we can learn a lot from real-world data, it cannot replace randomized controlled trials. In our patients with an asymptomatic primary tumor in the context of incurable colorectal cancer, I believe there is no longer a role for primary tumor resection.”
Study details
In the iPACS trial, patients in the primary tumor resection group underwent open or laparoscopic colectomy/high anterior resection with a D1-D3 lymph node dissection. Concurrent resection of involved organs was not permitted, except for the mesentery, small intestine, greater omentum, and ovary.
In the resection group, the time between surgery and start of chemotherapy was 8 to 56 days, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
With a median follow-up of 22.0 months, median overall survival was 25.9 months with primary tumor resection followed by chemotherapy and 26.7 months with chemotherapy alone (hazard ratio for death, 1.10; P = .69). Findings were similar in subgroup analyses. Median progression-free survival was 10.4 and 12.1 months, respectively (hazard ratio for progression or death, 1.08).
Patients in the primary tumor resection group had higher rates of chemotherapy-related grade 3 and 4 paresthesia (5% vs. 1%), hypertension (17% vs. 8%), diarrhea (5% vs. 1%), and neuropathy (14% vs. 9%), Dr. Kanemitsu reported.
In terms of secondary surgeries, the R0 (curative) resection rate was 3% in the primary tumor resection group and 5% in the chemotherapy group. Thirteen percent of patients in the chemotherapy group underwent palliative surgery for symptoms caused by their primary tumor.
Dr. Kanemitsu disclosed that he receives honoraria from Chugai Pharma, Covidien, Ethicon, and Intuitive Surgical, and that he has a consulting or advisory role with Covidien. The study was funded by a Health and Labor Sciences Research Grant for Clinical Cancer Research. Dr. Booth disclosed that he has no conflicts of interest.
SOURCE: Kanemitsu Y et al. 2020 GI Cancers Symposium. Abstract 7.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Cisplatin-gemcitabine is highly active in BRCA/PALB2+ pancreatic cancer
SAN FRANCISCO – The combination of cisplatin and gemcitabine is highly efficacious as first-line therapy for advanced pancreatic cancer in patients with a germline BRCA1/2 or PALB2 mutation, with no additional benefit seen from concurrent veliparib, a phase 2 randomized controlled trial finds.
Up to 9% of pancreatic ductal adenocarcinomas occur in individuals with one of these germline mutations, which render cells more sensitive to platinum agents and PARP inhibitors because of ineffective DNA repair.
In the trial, nearly two-thirds of patients had a response to cisplatin-gemcitabine alone, according to results reported at the 2020 GI Cancers Symposium and simultaneously published (J Clin Oncol. 2020 Jan 24. doi: 10.1200/JCO.19.02931). Although almost three-quarters had a response when the investigational PARP 1/2 inhibitor veliparib was added, the difference was not statistically significant and toxicity was greater.
“Both arms were very active and substantially exceeded the prespecified thresholds,” said lead investigator Eileen Mary O’Reilly, MD, section head of Hepatopancreaticobilary & Neuroendocrine Cancers at Memorial Sloan Kettering Cancer Center in New York.
“The doublet is our recommendation for moving forward, and we believe these data define a reference regimen for germline BRCA-mutated or PALB2-mutated pancreas cancer,” she stated, noting that the PARP inhibitor olaparib (Lynparza) conferred benefit when used as maintenance therapy in the POLO trial. “I think the strategy that at the current time is best supported by the totality of the data is platinum-based therapy upfront and then sequential use of the PARP inhibitor as a maintenance approach.”
The trial was designed in 2012, before efficacy of the FOLFIRINOX regimen was well established, so an obvious question is which chemotherapy to use, Dr. O’Reilly acknowledged.
“I would say these are the only prospective randomized data we have with platinum-based therapy in germline-mutated pancreas cancer. So it comes with a high level of evidence,” she maintained. “Nonetheless, I think FOLFIRINOX is also an option. The options are good, and it probably will depend on the patient in front of you because there certainly are some lack of toxicity advantages, for the most part, to cisplatin and gemcitabine. This was a well-tolerated regimen.”
Implications for practice
“I wouldn’t say this is a negative study. It’s negative with respect to the veliparib question, but otherwise, it’s a very exciting study,” Richard L. Schilsky, MD, chief medical officer and executive vice president of ASCO, said in an interview. “Seeing response rates of 60% and 70% in patients with metastatic pancreatic cancer is kind of unprecedented, and that’s quite remarkable.”
The reason for the lack of additional benefit from veliparib is unclear, he said. But it may be related to the specific PARP inhibitor or to the smaller sample size or very high response rate seen with chemotherapy alone, which possibly precluded detection of a significant difference.
When choosing between chemotherapy regimens, evidence favors the doublet, according to Dr. Schilsky. “FOLFIRINOX doesn’t have a 70% response rate; it may be 35%. If it was my family member, I would say, get gemcitabine-platinum if you have a BRCA mutation.”
“I think the real take-home message, quite honestly, for most oncologists is that patients with pancreatic cancer should be tested for germline BRCA mutations,” he recommended. “It can not only help inform the therapy choice, but of course, some of these cancers are going to run in families because these are germline mutations and they are going to reveal families that have a high risk of not only pancreatic cancer, but breast, ovarian, and all the other BRCA-associated cancers.”
Study details
The trial was conducted among 52 patients with untreated locally advanced or metastatic pancreatic ductal adenocarcinoma. Fully 94% had a BRCA mutation, while the rest had a PALB2 mutation, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
The response rate – the trial’s primary endpoint – was 65.2% with cisplatin-gemcitabine alone and 74.1% with cisplatin-gemcitabine plus veliparib (P = .55), with both arms far exceeding not only the 10% prespecified as “acceptable,” but also the 30% prespecified as “promising.” The respective disease control rates were 78.3% and 100% (P = .02).
Median progression-free survival was 9.7 months with chemotherapy alone and 10.1 months with chemotherapy plus the PARP inhibitor (P = .73). “If you reference an unselected population, that would be about 5 to 7 months,” Dr. O’Reilly noted. Median overall survival was 16.4 months and 15.5 months, respectively (P = .6). For the entire trial cohort, the 2-year overall survival rate was 30.6% and the 3-year overall survival rate was 17.8%.
“The combination came at the expense of hematologic toxicity,” Dr. O’Reilly said, with patients given veliparib having higher rates of grade 3 or 4 neutropenia (48% vs. 30%), thrombocytopenia (55% vs. 9%), and anemia (52% vs. 35%).
In an exploratory analysis among all patients receiving 4 or more months of chemotherapy and then continuing on or starting a PARP inhibitor as their next therapy, without disease progression, median overall survival was 23.4 months, very similar to what was seen in the POLO trial, she noted.
Dr. O’Reilly disclosed that she has ties with Vesselon, Polaris, and CytomX, and that her institution receives grant/research support from Celgene, Sanofi, Genentech-Roche, AstraZeneca, BMS, Silenseed, MabVax, Halozyme, and Acta Biologica. The trial was funded by the Lustgarten Foundation, the David M. Rubenstein Center for Pancreatic Cancer Research, the Reiss Family Foundation, the National Cancer Institute’s Cancer Therapy Evaluation Program, and NCI grants. Dr. Schilsky disclosed that he has no conflicts of interest.
SOURCE: O’Reilly EM et al. 2020 GI Cancers Symposium. Abstract 639.
SAN FRANCISCO – The combination of cisplatin and gemcitabine is highly efficacious as first-line therapy for advanced pancreatic cancer in patients with a germline BRCA1/2 or PALB2 mutation, with no additional benefit seen from concurrent veliparib, a phase 2 randomized controlled trial finds.
Up to 9% of pancreatic ductal adenocarcinomas occur in individuals with one of these germline mutations, which render cells more sensitive to platinum agents and PARP inhibitors because of ineffective DNA repair.
In the trial, nearly two-thirds of patients had a response to cisplatin-gemcitabine alone, according to results reported at the 2020 GI Cancers Symposium and simultaneously published (J Clin Oncol. 2020 Jan 24. doi: 10.1200/JCO.19.02931). Although almost three-quarters had a response when the investigational PARP 1/2 inhibitor veliparib was added, the difference was not statistically significant and toxicity was greater.
“Both arms were very active and substantially exceeded the prespecified thresholds,” said lead investigator Eileen Mary O’Reilly, MD, section head of Hepatopancreaticobilary & Neuroendocrine Cancers at Memorial Sloan Kettering Cancer Center in New York.
“The doublet is our recommendation for moving forward, and we believe these data define a reference regimen for germline BRCA-mutated or PALB2-mutated pancreas cancer,” she stated, noting that the PARP inhibitor olaparib (Lynparza) conferred benefit when used as maintenance therapy in the POLO trial. “I think the strategy that at the current time is best supported by the totality of the data is platinum-based therapy upfront and then sequential use of the PARP inhibitor as a maintenance approach.”
The trial was designed in 2012, before efficacy of the FOLFIRINOX regimen was well established, so an obvious question is which chemotherapy to use, Dr. O’Reilly acknowledged.
“I would say these are the only prospective randomized data we have with platinum-based therapy in germline-mutated pancreas cancer. So it comes with a high level of evidence,” she maintained. “Nonetheless, I think FOLFIRINOX is also an option. The options are good, and it probably will depend on the patient in front of you because there certainly are some lack of toxicity advantages, for the most part, to cisplatin and gemcitabine. This was a well-tolerated regimen.”
Implications for practice
“I wouldn’t say this is a negative study. It’s negative with respect to the veliparib question, but otherwise, it’s a very exciting study,” Richard L. Schilsky, MD, chief medical officer and executive vice president of ASCO, said in an interview. “Seeing response rates of 60% and 70% in patients with metastatic pancreatic cancer is kind of unprecedented, and that’s quite remarkable.”
The reason for the lack of additional benefit from veliparib is unclear, he said. But it may be related to the specific PARP inhibitor or to the smaller sample size or very high response rate seen with chemotherapy alone, which possibly precluded detection of a significant difference.
When choosing between chemotherapy regimens, evidence favors the doublet, according to Dr. Schilsky. “FOLFIRINOX doesn’t have a 70% response rate; it may be 35%. If it was my family member, I would say, get gemcitabine-platinum if you have a BRCA mutation.”
“I think the real take-home message, quite honestly, for most oncologists is that patients with pancreatic cancer should be tested for germline BRCA mutations,” he recommended. “It can not only help inform the therapy choice, but of course, some of these cancers are going to run in families because these are germline mutations and they are going to reveal families that have a high risk of not only pancreatic cancer, but breast, ovarian, and all the other BRCA-associated cancers.”
Study details
The trial was conducted among 52 patients with untreated locally advanced or metastatic pancreatic ductal adenocarcinoma. Fully 94% had a BRCA mutation, while the rest had a PALB2 mutation, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
The response rate – the trial’s primary endpoint – was 65.2% with cisplatin-gemcitabine alone and 74.1% with cisplatin-gemcitabine plus veliparib (P = .55), with both arms far exceeding not only the 10% prespecified as “acceptable,” but also the 30% prespecified as “promising.” The respective disease control rates were 78.3% and 100% (P = .02).
Median progression-free survival was 9.7 months with chemotherapy alone and 10.1 months with chemotherapy plus the PARP inhibitor (P = .73). “If you reference an unselected population, that would be about 5 to 7 months,” Dr. O’Reilly noted. Median overall survival was 16.4 months and 15.5 months, respectively (P = .6). For the entire trial cohort, the 2-year overall survival rate was 30.6% and the 3-year overall survival rate was 17.8%.
“The combination came at the expense of hematologic toxicity,” Dr. O’Reilly said, with patients given veliparib having higher rates of grade 3 or 4 neutropenia (48% vs. 30%), thrombocytopenia (55% vs. 9%), and anemia (52% vs. 35%).
In an exploratory analysis among all patients receiving 4 or more months of chemotherapy and then continuing on or starting a PARP inhibitor as their next therapy, without disease progression, median overall survival was 23.4 months, very similar to what was seen in the POLO trial, she noted.
Dr. O’Reilly disclosed that she has ties with Vesselon, Polaris, and CytomX, and that her institution receives grant/research support from Celgene, Sanofi, Genentech-Roche, AstraZeneca, BMS, Silenseed, MabVax, Halozyme, and Acta Biologica. The trial was funded by the Lustgarten Foundation, the David M. Rubenstein Center for Pancreatic Cancer Research, the Reiss Family Foundation, the National Cancer Institute’s Cancer Therapy Evaluation Program, and NCI grants. Dr. Schilsky disclosed that he has no conflicts of interest.
SOURCE: O’Reilly EM et al. 2020 GI Cancers Symposium. Abstract 639.
SAN FRANCISCO – The combination of cisplatin and gemcitabine is highly efficacious as first-line therapy for advanced pancreatic cancer in patients with a germline BRCA1/2 or PALB2 mutation, with no additional benefit seen from concurrent veliparib, a phase 2 randomized controlled trial finds.
Up to 9% of pancreatic ductal adenocarcinomas occur in individuals with one of these germline mutations, which render cells more sensitive to platinum agents and PARP inhibitors because of ineffective DNA repair.
In the trial, nearly two-thirds of patients had a response to cisplatin-gemcitabine alone, according to results reported at the 2020 GI Cancers Symposium and simultaneously published (J Clin Oncol. 2020 Jan 24. doi: 10.1200/JCO.19.02931). Although almost three-quarters had a response when the investigational PARP 1/2 inhibitor veliparib was added, the difference was not statistically significant and toxicity was greater.
“Both arms were very active and substantially exceeded the prespecified thresholds,” said lead investigator Eileen Mary O’Reilly, MD, section head of Hepatopancreaticobilary & Neuroendocrine Cancers at Memorial Sloan Kettering Cancer Center in New York.
“The doublet is our recommendation for moving forward, and we believe these data define a reference regimen for germline BRCA-mutated or PALB2-mutated pancreas cancer,” she stated, noting that the PARP inhibitor olaparib (Lynparza) conferred benefit when used as maintenance therapy in the POLO trial. “I think the strategy that at the current time is best supported by the totality of the data is platinum-based therapy upfront and then sequential use of the PARP inhibitor as a maintenance approach.”
The trial was designed in 2012, before efficacy of the FOLFIRINOX regimen was well established, so an obvious question is which chemotherapy to use, Dr. O’Reilly acknowledged.
“I would say these are the only prospective randomized data we have with platinum-based therapy in germline-mutated pancreas cancer. So it comes with a high level of evidence,” she maintained. “Nonetheless, I think FOLFIRINOX is also an option. The options are good, and it probably will depend on the patient in front of you because there certainly are some lack of toxicity advantages, for the most part, to cisplatin and gemcitabine. This was a well-tolerated regimen.”
Implications for practice
“I wouldn’t say this is a negative study. It’s negative with respect to the veliparib question, but otherwise, it’s a very exciting study,” Richard L. Schilsky, MD, chief medical officer and executive vice president of ASCO, said in an interview. “Seeing response rates of 60% and 70% in patients with metastatic pancreatic cancer is kind of unprecedented, and that’s quite remarkable.”
The reason for the lack of additional benefit from veliparib is unclear, he said. But it may be related to the specific PARP inhibitor or to the smaller sample size or very high response rate seen with chemotherapy alone, which possibly precluded detection of a significant difference.
When choosing between chemotherapy regimens, evidence favors the doublet, according to Dr. Schilsky. “FOLFIRINOX doesn’t have a 70% response rate; it may be 35%. If it was my family member, I would say, get gemcitabine-platinum if you have a BRCA mutation.”
“I think the real take-home message, quite honestly, for most oncologists is that patients with pancreatic cancer should be tested for germline BRCA mutations,” he recommended. “It can not only help inform the therapy choice, but of course, some of these cancers are going to run in families because these are germline mutations and they are going to reveal families that have a high risk of not only pancreatic cancer, but breast, ovarian, and all the other BRCA-associated cancers.”
Study details
The trial was conducted among 52 patients with untreated locally advanced or metastatic pancreatic ductal adenocarcinoma. Fully 94% had a BRCA mutation, while the rest had a PALB2 mutation, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
The response rate – the trial’s primary endpoint – was 65.2% with cisplatin-gemcitabine alone and 74.1% with cisplatin-gemcitabine plus veliparib (P = .55), with both arms far exceeding not only the 10% prespecified as “acceptable,” but also the 30% prespecified as “promising.” The respective disease control rates were 78.3% and 100% (P = .02).
Median progression-free survival was 9.7 months with chemotherapy alone and 10.1 months with chemotherapy plus the PARP inhibitor (P = .73). “If you reference an unselected population, that would be about 5 to 7 months,” Dr. O’Reilly noted. Median overall survival was 16.4 months and 15.5 months, respectively (P = .6). For the entire trial cohort, the 2-year overall survival rate was 30.6% and the 3-year overall survival rate was 17.8%.
“The combination came at the expense of hematologic toxicity,” Dr. O’Reilly said, with patients given veliparib having higher rates of grade 3 or 4 neutropenia (48% vs. 30%), thrombocytopenia (55% vs. 9%), and anemia (52% vs. 35%).
In an exploratory analysis among all patients receiving 4 or more months of chemotherapy and then continuing on or starting a PARP inhibitor as their next therapy, without disease progression, median overall survival was 23.4 months, very similar to what was seen in the POLO trial, she noted.
Dr. O’Reilly disclosed that she has ties with Vesselon, Polaris, and CytomX, and that her institution receives grant/research support from Celgene, Sanofi, Genentech-Roche, AstraZeneca, BMS, Silenseed, MabVax, Halozyme, and Acta Biologica. The trial was funded by the Lustgarten Foundation, the David M. Rubenstein Center for Pancreatic Cancer Research, the Reiss Family Foundation, the National Cancer Institute’s Cancer Therapy Evaluation Program, and NCI grants. Dr. Schilsky disclosed that he has no conflicts of interest.
SOURCE: O’Reilly EM et al. 2020 GI Cancers Symposium. Abstract 639.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Sociodemographic disadvantage confers poorer survival in young adults with CRC
SAN FRANCISCO – Young adults with colorectal cancer who live in neighborhoods with higher levels of disadvantage differ on health measures, present with more advanced disease, and have poorer survival. These were among key findings of a retrospective cohort study reported at the 2020 GI Cancers Symposium.
The incidence of colorectal cancer has risen sharply – 51% – since 1994 among individuals aged younger than age 50 years, with the greatest uptick seen among those aged 20-29 years (J Natl Cancer Inst. 2017;109[8]. doi: 10.1093/jnci/djw322).
“Sociodemographic disparities have been linked to inferior survival. However, their impact and association with outcome in young adults is not well described,” said lead investigator Ashley Matusz-Fisher, MD, of the Levine Cancer Institute in Charlotte, N.C.
The investigators analyzed data from the National Cancer Database for the years 2004-2016, identifying 26,768 patients who received a colorectal cancer diagnosis when aged 18-40 years.
Results showed that those living in areas with low income (less than $38,000 annually) and low educational attainment (high school graduation rate less than 79%), and those living in urban or rural areas (versus metropolitan areas) had 24% and 10% higher risks of death, respectively.
Patients in the low-income, low-education group were more than six times as likely to be black and to lack private health insurance, had greater comorbidity, had larger tumors and more nodal involvement at diagnosis, and were less likely to undergo surgery.
Several factors may be at play for the low-income, low-education group, Dr. Matusz-Fisher speculated: limited access to care, lack of awareness of important symptoms, and inability to afford treatment when it is needed. “That could very well be contributing to them presenting at later stages and then maybe not getting the treatment that other people who have insurance would be getting.
“To try to eliminate these disparities, the first step is recognition, which is what we are doing – recognizing there are disparities – and then making people aware of these disparities,” she commented. “More efforts are needed to increase access and remove barriers to care, with the hope of eliminating disparities and achieving health equity.”
Mitigating disparities
Several studies have looked at mitigating sociodemographic-related disparities in colorectal cancer outcomes, according to session cochair John M. Carethers, MD, AGAF, professor and chair of the department of internal medicine at the University of Michigan, Ann Arbor.
A large Delaware initiative tackled the problem via screening (J Clin Oncol. 2013;31:1928-30). “Now this was over 50 – we don’t typically screen under 50 – but over 50, you can essentially eliminate this disparity with navigation services and screening. How do you do that under 50? I’m not quite sure,” he said in an interview, adding that some organizations are recommending lowering the screening age to 45 or even 40 years in light of rising incidence among young adults.
However, accumulating evidence suggests that there may be inherent biological differences that are harder to overcome. “There is a lot of data … showing that polyps happen earlier and they are bigger in certain racial groups, particularly African Americans and American Indians,” Dr. Carethers elaborated. What is driving the biology is unknown, but the microbiome has come under scrutiny.
“So you are a victim of your circumstances,” he summarized. “You are living in a low-income area, you are eating more proinflammatory-type foods, you are getting your polyps earlier, and then you are getting your cancers earlier.”
Study details
Rural, urban, or metropolitan status was ascertained for 25,861 patients in the study, and area income and education were ascertained for 7,743 patients, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Compared with counterparts living in areas with both high annual income (greater than $68,000) and education (greater than 93% high school graduation rate), patients living in areas with both low annual income (less than $38,000) and education ( less than 79% high school graduation rate) were significantly more likely to be black (odds ratio, 6.4), not have private insurance (odds ratio, 6.3), have pathologic T3/T4 stage (OR, 1.4), have positive nodes (OR, 1.2), and have a Charlson-Deyo comorbidity score of 1 or greater (OR, 1.6). They also were less likely to undergo surgery (OR, 0.63) and more likely to be rehospitalized within 30 days (OR, 1.3).
After adjusting for race, insurance status, T/N stage, and comorbidity score, relative to counterparts in the high-income, high-education group, patients in the low-income, low-education group had an increased risk of death (hazard ratio, 1.24; P = .004). And relative to counterparts living in metropolitan areas, patients living in urban or rural areas had an increased risk of death (HR, 1.10; P = .02).
Among patients with stage IV disease, median overall survival was 26.1 months for those from high-income, high-education areas, but 20.7 months for those from low-income, low-education areas (P less than .001).
Dr. Matusz-Fisher did not report any conflicts of interest. The study did not receive any funding.
SOURCE: Matusz-Fisher A et al. 2020 GI Cancers Symposium, Abstract 13.
SAN FRANCISCO – Young adults with colorectal cancer who live in neighborhoods with higher levels of disadvantage differ on health measures, present with more advanced disease, and have poorer survival. These were among key findings of a retrospective cohort study reported at the 2020 GI Cancers Symposium.
The incidence of colorectal cancer has risen sharply – 51% – since 1994 among individuals aged younger than age 50 years, with the greatest uptick seen among those aged 20-29 years (J Natl Cancer Inst. 2017;109[8]. doi: 10.1093/jnci/djw322).
“Sociodemographic disparities have been linked to inferior survival. However, their impact and association with outcome in young adults is not well described,” said lead investigator Ashley Matusz-Fisher, MD, of the Levine Cancer Institute in Charlotte, N.C.
The investigators analyzed data from the National Cancer Database for the years 2004-2016, identifying 26,768 patients who received a colorectal cancer diagnosis when aged 18-40 years.
Results showed that those living in areas with low income (less than $38,000 annually) and low educational attainment (high school graduation rate less than 79%), and those living in urban or rural areas (versus metropolitan areas) had 24% and 10% higher risks of death, respectively.
Patients in the low-income, low-education group were more than six times as likely to be black and to lack private health insurance, had greater comorbidity, had larger tumors and more nodal involvement at diagnosis, and were less likely to undergo surgery.
Several factors may be at play for the low-income, low-education group, Dr. Matusz-Fisher speculated: limited access to care, lack of awareness of important symptoms, and inability to afford treatment when it is needed. “That could very well be contributing to them presenting at later stages and then maybe not getting the treatment that other people who have insurance would be getting.
“To try to eliminate these disparities, the first step is recognition, which is what we are doing – recognizing there are disparities – and then making people aware of these disparities,” she commented. “More efforts are needed to increase access and remove barriers to care, with the hope of eliminating disparities and achieving health equity.”
Mitigating disparities
Several studies have looked at mitigating sociodemographic-related disparities in colorectal cancer outcomes, according to session cochair John M. Carethers, MD, AGAF, professor and chair of the department of internal medicine at the University of Michigan, Ann Arbor.
A large Delaware initiative tackled the problem via screening (J Clin Oncol. 2013;31:1928-30). “Now this was over 50 – we don’t typically screen under 50 – but over 50, you can essentially eliminate this disparity with navigation services and screening. How do you do that under 50? I’m not quite sure,” he said in an interview, adding that some organizations are recommending lowering the screening age to 45 or even 40 years in light of rising incidence among young adults.
However, accumulating evidence suggests that there may be inherent biological differences that are harder to overcome. “There is a lot of data … showing that polyps happen earlier and they are bigger in certain racial groups, particularly African Americans and American Indians,” Dr. Carethers elaborated. What is driving the biology is unknown, but the microbiome has come under scrutiny.
“So you are a victim of your circumstances,” he summarized. “You are living in a low-income area, you are eating more proinflammatory-type foods, you are getting your polyps earlier, and then you are getting your cancers earlier.”
Study details
Rural, urban, or metropolitan status was ascertained for 25,861 patients in the study, and area income and education were ascertained for 7,743 patients, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Compared with counterparts living in areas with both high annual income (greater than $68,000) and education (greater than 93% high school graduation rate), patients living in areas with both low annual income (less than $38,000) and education ( less than 79% high school graduation rate) were significantly more likely to be black (odds ratio, 6.4), not have private insurance (odds ratio, 6.3), have pathologic T3/T4 stage (OR, 1.4), have positive nodes (OR, 1.2), and have a Charlson-Deyo comorbidity score of 1 or greater (OR, 1.6). They also were less likely to undergo surgery (OR, 0.63) and more likely to be rehospitalized within 30 days (OR, 1.3).
After adjusting for race, insurance status, T/N stage, and comorbidity score, relative to counterparts in the high-income, high-education group, patients in the low-income, low-education group had an increased risk of death (hazard ratio, 1.24; P = .004). And relative to counterparts living in metropolitan areas, patients living in urban or rural areas had an increased risk of death (HR, 1.10; P = .02).
Among patients with stage IV disease, median overall survival was 26.1 months for those from high-income, high-education areas, but 20.7 months for those from low-income, low-education areas (P less than .001).
Dr. Matusz-Fisher did not report any conflicts of interest. The study did not receive any funding.
SOURCE: Matusz-Fisher A et al. 2020 GI Cancers Symposium, Abstract 13.
SAN FRANCISCO – Young adults with colorectal cancer who live in neighborhoods with higher levels of disadvantage differ on health measures, present with more advanced disease, and have poorer survival. These were among key findings of a retrospective cohort study reported at the 2020 GI Cancers Symposium.
The incidence of colorectal cancer has risen sharply – 51% – since 1994 among individuals aged younger than age 50 years, with the greatest uptick seen among those aged 20-29 years (J Natl Cancer Inst. 2017;109[8]. doi: 10.1093/jnci/djw322).
“Sociodemographic disparities have been linked to inferior survival. However, their impact and association with outcome in young adults is not well described,” said lead investigator Ashley Matusz-Fisher, MD, of the Levine Cancer Institute in Charlotte, N.C.
The investigators analyzed data from the National Cancer Database for the years 2004-2016, identifying 26,768 patients who received a colorectal cancer diagnosis when aged 18-40 years.
Results showed that those living in areas with low income (less than $38,000 annually) and low educational attainment (high school graduation rate less than 79%), and those living in urban or rural areas (versus metropolitan areas) had 24% and 10% higher risks of death, respectively.
Patients in the low-income, low-education group were more than six times as likely to be black and to lack private health insurance, had greater comorbidity, had larger tumors and more nodal involvement at diagnosis, and were less likely to undergo surgery.
Several factors may be at play for the low-income, low-education group, Dr. Matusz-Fisher speculated: limited access to care, lack of awareness of important symptoms, and inability to afford treatment when it is needed. “That could very well be contributing to them presenting at later stages and then maybe not getting the treatment that other people who have insurance would be getting.
“To try to eliminate these disparities, the first step is recognition, which is what we are doing – recognizing there are disparities – and then making people aware of these disparities,” she commented. “More efforts are needed to increase access and remove barriers to care, with the hope of eliminating disparities and achieving health equity.”
Mitigating disparities
Several studies have looked at mitigating sociodemographic-related disparities in colorectal cancer outcomes, according to session cochair John M. Carethers, MD, AGAF, professor and chair of the department of internal medicine at the University of Michigan, Ann Arbor.
A large Delaware initiative tackled the problem via screening (J Clin Oncol. 2013;31:1928-30). “Now this was over 50 – we don’t typically screen under 50 – but over 50, you can essentially eliminate this disparity with navigation services and screening. How do you do that under 50? I’m not quite sure,” he said in an interview, adding that some organizations are recommending lowering the screening age to 45 or even 40 years in light of rising incidence among young adults.
However, accumulating evidence suggests that there may be inherent biological differences that are harder to overcome. “There is a lot of data … showing that polyps happen earlier and they are bigger in certain racial groups, particularly African Americans and American Indians,” Dr. Carethers elaborated. What is driving the biology is unknown, but the microbiome has come under scrutiny.
“So you are a victim of your circumstances,” he summarized. “You are living in a low-income area, you are eating more proinflammatory-type foods, you are getting your polyps earlier, and then you are getting your cancers earlier.”
Study details
Rural, urban, or metropolitan status was ascertained for 25,861 patients in the study, and area income and education were ascertained for 7,743 patients, according to data reported at the symposium, sponsored by the American Gastroenterological Association, the American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Compared with counterparts living in areas with both high annual income (greater than $68,000) and education (greater than 93% high school graduation rate), patients living in areas with both low annual income (less than $38,000) and education ( less than 79% high school graduation rate) were significantly more likely to be black (odds ratio, 6.4), not have private insurance (odds ratio, 6.3), have pathologic T3/T4 stage (OR, 1.4), have positive nodes (OR, 1.2), and have a Charlson-Deyo comorbidity score of 1 or greater (OR, 1.6). They also were less likely to undergo surgery (OR, 0.63) and more likely to be rehospitalized within 30 days (OR, 1.3).
After adjusting for race, insurance status, T/N stage, and comorbidity score, relative to counterparts in the high-income, high-education group, patients in the low-income, low-education group had an increased risk of death (hazard ratio, 1.24; P = .004). And relative to counterparts living in metropolitan areas, patients living in urban or rural areas had an increased risk of death (HR, 1.10; P = .02).
Among patients with stage IV disease, median overall survival was 26.1 months for those from high-income, high-education areas, but 20.7 months for those from low-income, low-education areas (P less than .001).
Dr. Matusz-Fisher did not report any conflicts of interest. The study did not receive any funding.
SOURCE: Matusz-Fisher A et al. 2020 GI Cancers Symposium, Abstract 13.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM
Blood test may advance diagnosis of GI cancers
SAN FRANCISCO – A new assay based on methylation patterns in plasma cell-free DNA holds promise for improving detection of diverse gastrointestinal (GI) cancers when they are still curable, findings of the Circulating Cell-free Genome Atlas (CCGA) study suggest.
Among 447 patients with GI cancers of varied types and stages, the multicancer assay had sensitivity exceeding 80% for all stages (exceeding 70% for stages I to III) and specificity exceeding 99%, investigators reported at the 2020 GI Cancers Symposium. In addition, the assay correctly determined the tissue of origin about 90% of the time.
“To pursue early detection at a population scale while minimizing harm and cost, several features are important, including a low false-positive rate, a high detection rate, the ability to localize the site of origin of the malignancy, and limiting overdiagnosis,” noted lead investigator Brian M. Wolpin, MD, MPH, director of the Gastrointestinal Cancer Center and director of the Hale Family Center for Pancreatic Cancer Research at Dana-Farber Cancer Institute in Boston. “This multicancer early detection test evaluating cell-free DNA methylation may be a useful test to detect GI cancers and may guide further evaluation and workup.”
About three-quarters of all cancer patients in the study had symptoms that ultimately led to their diagnosis, Dr. Wolpin acknowledged. But the investigators are conducting two large additional studies among asymptomatic populations to better assess the assay’s screening potential: the STRIVE study, which has enrolled nearly 100,000 women undergoing screening mammography, and the SUMMIT study, which is enrolling 50,000 men and women without a known cancer diagnosis, with enrichment of the sample for smokers.
Clinical potential
“The holy grail, of course, is to try to find any test – a blood test, a urine test, a breath test, a stool test – that will allow us to detect cancer at an earlier and more curable stage, and we have hints now that we are headed in the right direction,” session cochair George A. Fisher Jr., MD, PhD, said in an interview. “I don’t know that this is the technology that will do it, but I think it’s superior to the technology just looking at DNA mutations.”
It is a further merit that the assay also has good accuracy in ascertaining the cancer’s tissue of origin, as that should help streamline the diagnostic workup, he agreed.
The assay is already attractive for patients with suspicious lesions or symptoms, but further research will be needed to assess its performance in detecting asymptomatic cancer, and logistic issues would have to be addressed, according to Dr. Fisher of Stanford (Calif.) University.
“As an outright screening test, I don’t think we are there yet. We would have to identify the populations in whom to use the test and come up with some frequency of how often we use it,” he said. Consideration would need to be given to informed consent, especially as some patients may have a positive assay result but a cancer that can’t be found, generating psychological distress.
And cost will come into play. “The problem is, for most stage I cancers you can screen for, they are still very low in likelihood, so you have to screen a lot of people, which means a lot of expense,” he elaborated.
“It will be interesting in the research world to decide when such a test would become a reasonable standard of care, and how regulators will view that and how insurers will view that in terms of cost-efficacy analysis,” Dr. Fisher concluded.
Study details
The CCGA study has enrolled 15,254 participants with and without cancer at 142 U.S and Canadian sites. Participants provide blood samples (at diagnosis for those with cancer) and are followed up for 5 years.
To develop the assay, the investigators performed targeted methylation sequencing of cell-free DNA from plasma and trained an algorithm to use the methylation patterns to detect more than 20 cancer types and classify them based on the organ of origin.
Dr. Wolpin reported results for a CCGA substudy conducted among 2,185 patients with cancer and 2,131 individuals without cancer. About a fifth of the former group had cancers of the GI tract (colon or rectum in 174 patients, pancreas in 123, esophagus in 71, liver or bile duct in 40, stomach in 25, gallbladder in 14). The population was split into training and validation sets.
The assay had a specificity of 99.8% in the entire training set and 99.3% in the entire validation set, corresponding to false-positives in just 0.2% and 0.7% of the individuals without cancer, according to data reported at the symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
For GI cancers, assay sensitivity for stage I-IV disease was 82% in the training set and 81% in the validation set, and sensitivity for stage I-III disease was 73% and 71%, respectively. By specific nonmetastatic stage, sensitivity was about 50% for stage I disease, 75% for stage II disease, and 85% for stage III disease.
Fully 97% of the GI cancers having detectable cell-free DNA were assigned a tissue of origin by the assay. The predicted tissue of origin had an accuracy of 91% in the training set and 89% in the validation set, with similar values across GI cancer types.
Dr. Wolpin disclosed having a relationship with various pharmaceutical companies, including GRAIL, which funded the study. Dr. Fisher disclosed relationships with numerous pharmaceutical companies and that an immediate family member has stock in Seattle Genetics
SOURCE: Wolpin BM et al. 2020 GI Symposium, Abstract 283.
SAN FRANCISCO – A new assay based on methylation patterns in plasma cell-free DNA holds promise for improving detection of diverse gastrointestinal (GI) cancers when they are still curable, findings of the Circulating Cell-free Genome Atlas (CCGA) study suggest.
Among 447 patients with GI cancers of varied types and stages, the multicancer assay had sensitivity exceeding 80% for all stages (exceeding 70% for stages I to III) and specificity exceeding 99%, investigators reported at the 2020 GI Cancers Symposium. In addition, the assay correctly determined the tissue of origin about 90% of the time.
“To pursue early detection at a population scale while minimizing harm and cost, several features are important, including a low false-positive rate, a high detection rate, the ability to localize the site of origin of the malignancy, and limiting overdiagnosis,” noted lead investigator Brian M. Wolpin, MD, MPH, director of the Gastrointestinal Cancer Center and director of the Hale Family Center for Pancreatic Cancer Research at Dana-Farber Cancer Institute in Boston. “This multicancer early detection test evaluating cell-free DNA methylation may be a useful test to detect GI cancers and may guide further evaluation and workup.”
About three-quarters of all cancer patients in the study had symptoms that ultimately led to their diagnosis, Dr. Wolpin acknowledged. But the investigators are conducting two large additional studies among asymptomatic populations to better assess the assay’s screening potential: the STRIVE study, which has enrolled nearly 100,000 women undergoing screening mammography, and the SUMMIT study, which is enrolling 50,000 men and women without a known cancer diagnosis, with enrichment of the sample for smokers.
Clinical potential
“The holy grail, of course, is to try to find any test – a blood test, a urine test, a breath test, a stool test – that will allow us to detect cancer at an earlier and more curable stage, and we have hints now that we are headed in the right direction,” session cochair George A. Fisher Jr., MD, PhD, said in an interview. “I don’t know that this is the technology that will do it, but I think it’s superior to the technology just looking at DNA mutations.”
It is a further merit that the assay also has good accuracy in ascertaining the cancer’s tissue of origin, as that should help streamline the diagnostic workup, he agreed.
The assay is already attractive for patients with suspicious lesions or symptoms, but further research will be needed to assess its performance in detecting asymptomatic cancer, and logistic issues would have to be addressed, according to Dr. Fisher of Stanford (Calif.) University.
“As an outright screening test, I don’t think we are there yet. We would have to identify the populations in whom to use the test and come up with some frequency of how often we use it,” he said. Consideration would need to be given to informed consent, especially as some patients may have a positive assay result but a cancer that can’t be found, generating psychological distress.
And cost will come into play. “The problem is, for most stage I cancers you can screen for, they are still very low in likelihood, so you have to screen a lot of people, which means a lot of expense,” he elaborated.
“It will be interesting in the research world to decide when such a test would become a reasonable standard of care, and how regulators will view that and how insurers will view that in terms of cost-efficacy analysis,” Dr. Fisher concluded.
Study details
The CCGA study has enrolled 15,254 participants with and without cancer at 142 U.S and Canadian sites. Participants provide blood samples (at diagnosis for those with cancer) and are followed up for 5 years.
To develop the assay, the investigators performed targeted methylation sequencing of cell-free DNA from plasma and trained an algorithm to use the methylation patterns to detect more than 20 cancer types and classify them based on the organ of origin.
Dr. Wolpin reported results for a CCGA substudy conducted among 2,185 patients with cancer and 2,131 individuals without cancer. About a fifth of the former group had cancers of the GI tract (colon or rectum in 174 patients, pancreas in 123, esophagus in 71, liver or bile duct in 40, stomach in 25, gallbladder in 14). The population was split into training and validation sets.
The assay had a specificity of 99.8% in the entire training set and 99.3% in the entire validation set, corresponding to false-positives in just 0.2% and 0.7% of the individuals without cancer, according to data reported at the symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
For GI cancers, assay sensitivity for stage I-IV disease was 82% in the training set and 81% in the validation set, and sensitivity for stage I-III disease was 73% and 71%, respectively. By specific nonmetastatic stage, sensitivity was about 50% for stage I disease, 75% for stage II disease, and 85% for stage III disease.
Fully 97% of the GI cancers having detectable cell-free DNA were assigned a tissue of origin by the assay. The predicted tissue of origin had an accuracy of 91% in the training set and 89% in the validation set, with similar values across GI cancer types.
Dr. Wolpin disclosed having a relationship with various pharmaceutical companies, including GRAIL, which funded the study. Dr. Fisher disclosed relationships with numerous pharmaceutical companies and that an immediate family member has stock in Seattle Genetics
SOURCE: Wolpin BM et al. 2020 GI Symposium, Abstract 283.
SAN FRANCISCO – A new assay based on methylation patterns in plasma cell-free DNA holds promise for improving detection of diverse gastrointestinal (GI) cancers when they are still curable, findings of the Circulating Cell-free Genome Atlas (CCGA) study suggest.
Among 447 patients with GI cancers of varied types and stages, the multicancer assay had sensitivity exceeding 80% for all stages (exceeding 70% for stages I to III) and specificity exceeding 99%, investigators reported at the 2020 GI Cancers Symposium. In addition, the assay correctly determined the tissue of origin about 90% of the time.
“To pursue early detection at a population scale while minimizing harm and cost, several features are important, including a low false-positive rate, a high detection rate, the ability to localize the site of origin of the malignancy, and limiting overdiagnosis,” noted lead investigator Brian M. Wolpin, MD, MPH, director of the Gastrointestinal Cancer Center and director of the Hale Family Center for Pancreatic Cancer Research at Dana-Farber Cancer Institute in Boston. “This multicancer early detection test evaluating cell-free DNA methylation may be a useful test to detect GI cancers and may guide further evaluation and workup.”
About three-quarters of all cancer patients in the study had symptoms that ultimately led to their diagnosis, Dr. Wolpin acknowledged. But the investigators are conducting two large additional studies among asymptomatic populations to better assess the assay’s screening potential: the STRIVE study, which has enrolled nearly 100,000 women undergoing screening mammography, and the SUMMIT study, which is enrolling 50,000 men and women without a known cancer diagnosis, with enrichment of the sample for smokers.
Clinical potential
“The holy grail, of course, is to try to find any test – a blood test, a urine test, a breath test, a stool test – that will allow us to detect cancer at an earlier and more curable stage, and we have hints now that we are headed in the right direction,” session cochair George A. Fisher Jr., MD, PhD, said in an interview. “I don’t know that this is the technology that will do it, but I think it’s superior to the technology just looking at DNA mutations.”
It is a further merit that the assay also has good accuracy in ascertaining the cancer’s tissue of origin, as that should help streamline the diagnostic workup, he agreed.
The assay is already attractive for patients with suspicious lesions or symptoms, but further research will be needed to assess its performance in detecting asymptomatic cancer, and logistic issues would have to be addressed, according to Dr. Fisher of Stanford (Calif.) University.
“As an outright screening test, I don’t think we are there yet. We would have to identify the populations in whom to use the test and come up with some frequency of how often we use it,” he said. Consideration would need to be given to informed consent, especially as some patients may have a positive assay result but a cancer that can’t be found, generating psychological distress.
And cost will come into play. “The problem is, for most stage I cancers you can screen for, they are still very low in likelihood, so you have to screen a lot of people, which means a lot of expense,” he elaborated.
“It will be interesting in the research world to decide when such a test would become a reasonable standard of care, and how regulators will view that and how insurers will view that in terms of cost-efficacy analysis,” Dr. Fisher concluded.
Study details
The CCGA study has enrolled 15,254 participants with and without cancer at 142 U.S and Canadian sites. Participants provide blood samples (at diagnosis for those with cancer) and are followed up for 5 years.
To develop the assay, the investigators performed targeted methylation sequencing of cell-free DNA from plasma and trained an algorithm to use the methylation patterns to detect more than 20 cancer types and classify them based on the organ of origin.
Dr. Wolpin reported results for a CCGA substudy conducted among 2,185 patients with cancer and 2,131 individuals without cancer. About a fifth of the former group had cancers of the GI tract (colon or rectum in 174 patients, pancreas in 123, esophagus in 71, liver or bile duct in 40, stomach in 25, gallbladder in 14). The population was split into training and validation sets.
The assay had a specificity of 99.8% in the entire training set and 99.3% in the entire validation set, corresponding to false-positives in just 0.2% and 0.7% of the individuals without cancer, according to data reported at the symposium, which is sponsored by the American Gastroenterological Association, American Society of Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
For GI cancers, assay sensitivity for stage I-IV disease was 82% in the training set and 81% in the validation set, and sensitivity for stage I-III disease was 73% and 71%, respectively. By specific nonmetastatic stage, sensitivity was about 50% for stage I disease, 75% for stage II disease, and 85% for stage III disease.
Fully 97% of the GI cancers having detectable cell-free DNA were assigned a tissue of origin by the assay. The predicted tissue of origin had an accuracy of 91% in the training set and 89% in the validation set, with similar values across GI cancer types.
Dr. Wolpin disclosed having a relationship with various pharmaceutical companies, including GRAIL, which funded the study. Dr. Fisher disclosed relationships with numerous pharmaceutical companies and that an immediate family member has stock in Seattle Genetics
SOURCE: Wolpin BM et al. 2020 GI Symposium, Abstract 283.
REPORTING FROM THE 2020 GI CANCERS SYMPOSIUM