User login
Intragestational injection of methotrexate
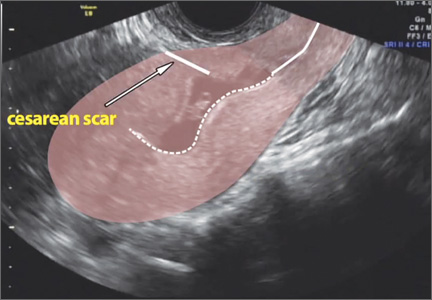
The presentation of a cesarean scar ectopic pregnancy can at times be daunting, especially without familiarity regarding its management. Women with cesarean scar ectopic pregnancy most often have no symptoms, although vaginal bleeding and abdominal pain can present. Upon visual diagnosis with transabdominal or transvaginal ultrasound, the preferred treatment method is direct injection of methotrexate into the gestational sac within the cesarean scar.
In this video, my colleagues review the indications and contraindications for direct injection of methotrexate as well as alternative treatment methods for this type of nonviable pregnancy that is increasing in frequency (given the US cesarean delivery rate). Demonstrated is the technique for methotrexate injection in the case of a 34-year-old woman (G6P0232) with ultrasound and beta−human chorionic gonadotropin confirmation of cesarean scar ectopic pregnancy.
We hope this video serves as a useful reference in your practice.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The presentation of a cesarean scar ectopic pregnancy can at times be daunting, especially without familiarity regarding its management. Women with cesarean scar ectopic pregnancy most often have no symptoms, although vaginal bleeding and abdominal pain can present. Upon visual diagnosis with transabdominal or transvaginal ultrasound, the preferred treatment method is direct injection of methotrexate into the gestational sac within the cesarean scar.
In this video, my colleagues review the indications and contraindications for direct injection of methotrexate as well as alternative treatment methods for this type of nonviable pregnancy that is increasing in frequency (given the US cesarean delivery rate). Demonstrated is the technique for methotrexate injection in the case of a 34-year-old woman (G6P0232) with ultrasound and beta−human chorionic gonadotropin confirmation of cesarean scar ectopic pregnancy.
We hope this video serves as a useful reference in your practice.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The presentation of a cesarean scar ectopic pregnancy can at times be daunting, especially without familiarity regarding its management. Women with cesarean scar ectopic pregnancy most often have no symptoms, although vaginal bleeding and abdominal pain can present. Upon visual diagnosis with transabdominal or transvaginal ultrasound, the preferred treatment method is direct injection of methotrexate into the gestational sac within the cesarean scar.
In this video, my colleagues review the indications and contraindications for direct injection of methotrexate as well as alternative treatment methods for this type of nonviable pregnancy that is increasing in frequency (given the US cesarean delivery rate). Demonstrated is the technique for methotrexate injection in the case of a 34-year-old woman (G6P0232) with ultrasound and beta−human chorionic gonadotropin confirmation of cesarean scar ectopic pregnancy.
We hope this video serves as a useful reference in your practice.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Laparoscopic management of interstitial ectopic pregnancy
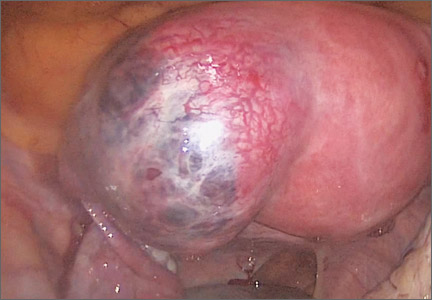
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Interstitial ectopic pregnancies, commonly reported as “cornual” ectopic pregnancies, are rare, accounting for only 2% to 3% of all tubal ectopic pregnancies. They can be managed medically with methotrexate or surgically via laparotomy or laparoscopy. Many variations of laparoscopic techniques have been described in the literature but no standardized surgical management has been established.
In this video, we begin by reviewing interstitial ectopic pregnancy and surgical approaches to treatment, with a focus on key surgical techniques and steps for successful laparoscopic management.
We then present the case of a 40-year-old woman (G3P1011) at 7 weeks 2 days gestation with a 5-cm left interstitial ectopic pregnancy who underwent a laparoscopic cornual resection.
We hope this video can serve as a quick reference in your practice for the surgical management of interstitial ectopic pregnancies.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Surgical removal of malpositioned IUDs
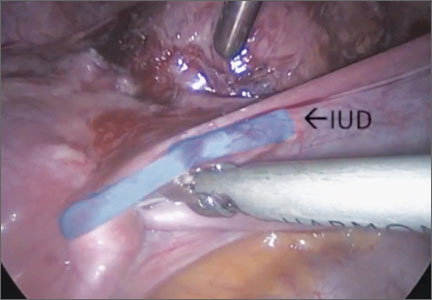
Today’s intrauterine devices (IUDs) represent an excellent form of long-acting reversible contraception. Depending on the type of IUD, many also are used to help alleviate such gynecologic symptoms as abnormal uterine bleeding. Approximately 10% of IUD insertions are complicated by malpositioning, which can include embedding, translocation, or perforation. Malpositioned IUDs are often amenable to office removal but, occasionally, hysteroscopy or laparoscopy is necessary.
In this video, we begin by reviewing techniques for complicated office IUD removal. Then we present 4 cases of malpositioned IUDs that required surgical intervention; hysteroscopic, laparoscopic, or combined techniques were used in each case. This video highlights how preoperative imaging often is not sufficient to determine the necessary surgical approach. Therefore, patients should be counseled on the potential need for hysteroscopy or laparoscopy to surgically remove a malpositioned IUD.
Although risk factors for malpositioned IUDs are not well studied in the literature, understanding proper placement and identification of complications at the time of IUD placement are essential to malpositioning prevention.
My colleagues and I hope you enjoy this video.
—Dr. Arnold Advincula

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Today’s intrauterine devices (IUDs) represent an excellent form of long-acting reversible contraception. Depending on the type of IUD, many also are used to help alleviate such gynecologic symptoms as abnormal uterine bleeding. Approximately 10% of IUD insertions are complicated by malpositioning, which can include embedding, translocation, or perforation. Malpositioned IUDs are often amenable to office removal but, occasionally, hysteroscopy or laparoscopy is necessary.
In this video, we begin by reviewing techniques for complicated office IUD removal. Then we present 4 cases of malpositioned IUDs that required surgical intervention; hysteroscopic, laparoscopic, or combined techniques were used in each case. This video highlights how preoperative imaging often is not sufficient to determine the necessary surgical approach. Therefore, patients should be counseled on the potential need for hysteroscopy or laparoscopy to surgically remove a malpositioned IUD.
Although risk factors for malpositioned IUDs are not well studied in the literature, understanding proper placement and identification of complications at the time of IUD placement are essential to malpositioning prevention.
My colleagues and I hope you enjoy this video.
—Dr. Arnold Advincula

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Today’s intrauterine devices (IUDs) represent an excellent form of long-acting reversible contraception. Depending on the type of IUD, many also are used to help alleviate such gynecologic symptoms as abnormal uterine bleeding. Approximately 10% of IUD insertions are complicated by malpositioning, which can include embedding, translocation, or perforation. Malpositioned IUDs are often amenable to office removal but, occasionally, hysteroscopy or laparoscopy is necessary.
In this video, we begin by reviewing techniques for complicated office IUD removal. Then we present 4 cases of malpositioned IUDs that required surgical intervention; hysteroscopic, laparoscopic, or combined techniques were used in each case. This video highlights how preoperative imaging often is not sufficient to determine the necessary surgical approach. Therefore, patients should be counseled on the potential need for hysteroscopy or laparoscopy to surgically remove a malpositioned IUD.
Although risk factors for malpositioned IUDs are not well studied in the literature, understanding proper placement and identification of complications at the time of IUD placement are essential to malpositioning prevention.
My colleagues and I hope you enjoy this video.
—Dr. Arnold Advincula

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
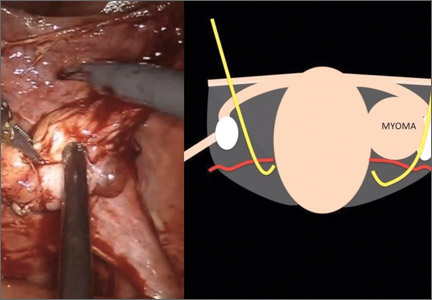
Surgical management of broad ligament fibroids
Although broad ligament fibroids are rare, their surgical management includes nuances of anatomical awareness, traction and counter-traction techniques, and proper hemostasis.
This month’s surgical video presents the case of a 40-year-old woman who presented to the emergency department with sudden-onset abdominal pain. She had a history of menorrhagia and dysmenorrhea and had undergone uterine artery embolization.
The objectives of this technique video are to provide:
- an overview of the background, clinical presentation, and imaging related to broad ligament fibroids
- pertinent anatomical landmarks
- a clinical case of robot-assisted laparoscopic myomectomy, demonstrating surgical technique
- key points for successful and safe surgical management.
I hope you find this video to be a useful tool for your practice and that you share it, and the other technique videos on my Video Channel, with your colleagues.

Although broad ligament fibroids are rare, their surgical management includes nuances of anatomical awareness, traction and counter-traction techniques, and proper hemostasis.
This month’s surgical video presents the case of a 40-year-old woman who presented to the emergency department with sudden-onset abdominal pain. She had a history of menorrhagia and dysmenorrhea and had undergone uterine artery embolization.
The objectives of this technique video are to provide:
- an overview of the background, clinical presentation, and imaging related to broad ligament fibroids
- pertinent anatomical landmarks
- a clinical case of robot-assisted laparoscopic myomectomy, demonstrating surgical technique
- key points for successful and safe surgical management.
I hope you find this video to be a useful tool for your practice and that you share it, and the other technique videos on my Video Channel, with your colleagues.

Although broad ligament fibroids are rare, their surgical management includes nuances of anatomical awareness, traction and counter-traction techniques, and proper hemostasis.
This month’s surgical video presents the case of a 40-year-old woman who presented to the emergency department with sudden-onset abdominal pain. She had a history of menorrhagia and dysmenorrhea and had undergone uterine artery embolization.
The objectives of this technique video are to provide:
- an overview of the background, clinical presentation, and imaging related to broad ligament fibroids
- pertinent anatomical landmarks
- a clinical case of robot-assisted laparoscopic myomectomy, demonstrating surgical technique
- key points for successful and safe surgical management.
I hope you find this video to be a useful tool for your practice and that you share it, and the other technique videos on my Video Channel, with your colleagues.

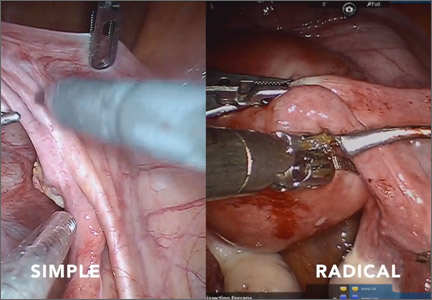
Simple versus radical hysterectomy
Hysterectomy is one of the fundamental surgical procedures in gynecology. Understanding the nuances of both the anatomy and the surgical dissection techniques of this procedure is especially important when approaching complex cases in either benign or oncologic settings.
This month’s surgical video contribution is by my gynecologic oncology colleagues, who highlight the key differences between the simple and radical hysterectomy. They emphasize key surgical principles for the benefit of both benign and oncologic surgeons.
The objectives of this video are to:
- compare the surgical techniques of a simple versus radical hysterectomy
- review the relevant anatomy as it relates to the varying types of hysterectomy
- provide an educational review of the different types of hysterectomy.
This video does an excellent job of achieving its objectives. I hope you share it with your colleagues and residents.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Hysterectomy is one of the fundamental surgical procedures in gynecology. Understanding the nuances of both the anatomy and the surgical dissection techniques of this procedure is especially important when approaching complex cases in either benign or oncologic settings.
This month’s surgical video contribution is by my gynecologic oncology colleagues, who highlight the key differences between the simple and radical hysterectomy. They emphasize key surgical principles for the benefit of both benign and oncologic surgeons.
The objectives of this video are to:
- compare the surgical techniques of a simple versus radical hysterectomy
- review the relevant anatomy as it relates to the varying types of hysterectomy
- provide an educational review of the different types of hysterectomy.
This video does an excellent job of achieving its objectives. I hope you share it with your colleagues and residents.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Hysterectomy is one of the fundamental surgical procedures in gynecology. Understanding the nuances of both the anatomy and the surgical dissection techniques of this procedure is especially important when approaching complex cases in either benign or oncologic settings.
This month’s surgical video contribution is by my gynecologic oncology colleagues, who highlight the key differences between the simple and radical hysterectomy. They emphasize key surgical principles for the benefit of both benign and oncologic surgeons.
The objectives of this video are to:
- compare the surgical techniques of a simple versus radical hysterectomy
- review the relevant anatomy as it relates to the varying types of hysterectomy
- provide an educational review of the different types of hysterectomy.
This video does an excellent job of achieving its objectives. I hope you share it with your colleagues and residents.

Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
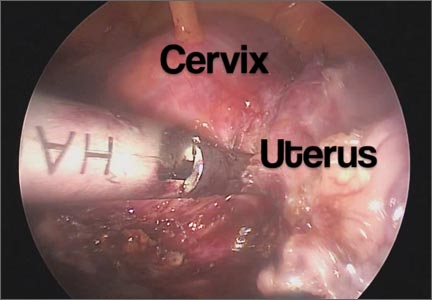
Mastering the uterine manipulator: Basics and beyond
An essential but often overlooked component of a successful minimally invasive gynecologic procedure is uterine manipulation. Regardless of whether conservative or extirpative surgery is being performed, the ability to optimally position the uterus within the pelvis is critical to safe and efficient surgical dissection. The addition of a colpotomizer cup to any uterine manipulator further enhances the ability to perform a conventional or robot-assisted laparoscopic hysterectomy.
The following video, produced by my third-year resident, Katherine Palmerola, MD, and my second-year fellow, Mireille Truong, MD, aims to provide a quick reference for gynecologists to use to help teach their surgical assistants the fundamentals of assembly and use of a uterine manipulator. This video also can be used as a resource for educating residents and medical students on the essentials of uterine manipulation.
The objectives of this video are to:
- outline the required instruments and steps for assembling a uterine manipulator and colpotomizer cup
- demonstrate the technical nuances of proper uterine manipulation intraoperatively
- highlight important clinical applications of uterine manipulation during pelvic surgery.
I hope this video proves to be a valuable resource for your practice.
– Dr. Arnold Advincula

Watch for these video topics coming soon:
• Tips and tricks to understanding retroperitoneal anatomy
• Simple versus radical hysterectomy: Anatomical nuances.
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
An essential but often overlooked component of a successful minimally invasive gynecologic procedure is uterine manipulation. Regardless of whether conservative or extirpative surgery is being performed, the ability to optimally position the uterus within the pelvis is critical to safe and efficient surgical dissection. The addition of a colpotomizer cup to any uterine manipulator further enhances the ability to perform a conventional or robot-assisted laparoscopic hysterectomy.
The following video, produced by my third-year resident, Katherine Palmerola, MD, and my second-year fellow, Mireille Truong, MD, aims to provide a quick reference for gynecologists to use to help teach their surgical assistants the fundamentals of assembly and use of a uterine manipulator. This video also can be used as a resource for educating residents and medical students on the essentials of uterine manipulation.
The objectives of this video are to:
- outline the required instruments and steps for assembling a uterine manipulator and colpotomizer cup
- demonstrate the technical nuances of proper uterine manipulation intraoperatively
- highlight important clinical applications of uterine manipulation during pelvic surgery.
I hope this video proves to be a valuable resource for your practice.
– Dr. Arnold Advincula

Watch for these video topics coming soon:
• Tips and tricks to understanding retroperitoneal anatomy
• Simple versus radical hysterectomy: Anatomical nuances.
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
An essential but often overlooked component of a successful minimally invasive gynecologic procedure is uterine manipulation. Regardless of whether conservative or extirpative surgery is being performed, the ability to optimally position the uterus within the pelvis is critical to safe and efficient surgical dissection. The addition of a colpotomizer cup to any uterine manipulator further enhances the ability to perform a conventional or robot-assisted laparoscopic hysterectomy.
The following video, produced by my third-year resident, Katherine Palmerola, MD, and my second-year fellow, Mireille Truong, MD, aims to provide a quick reference for gynecologists to use to help teach their surgical assistants the fundamentals of assembly and use of a uterine manipulator. This video also can be used as a resource for educating residents and medical students on the essentials of uterine manipulation.
The objectives of this video are to:
- outline the required instruments and steps for assembling a uterine manipulator and colpotomizer cup
- demonstrate the technical nuances of proper uterine manipulation intraoperatively
- highlight important clinical applications of uterine manipulation during pelvic surgery.
I hope this video proves to be a valuable resource for your practice.
– Dr. Arnold Advincula

Watch for these video topics coming soon:
• Tips and tricks to understanding retroperitoneal anatomy
• Simple versus radical hysterectomy: Anatomical nuances.
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The Extracorporeal C-Incision Tissue Extraction (ExCITE) technique
As a result of recent concerns regarding the use of power morcellation, clinicians have been faced with the need to develop alternative techniques for contained tissue extraction during minimally invasive gynecologic procedures such as myomectomy and hysterectomy.
The following video represents a refined and reproducible approach that incorporates a containment bag (Anchor Medical) and a self-retaining retractor (Applied Medical) in order to meet the following objectives:
- tissue extraction without the need for power morcellation
- specimen containment to avoid intraperitoneal spillage
- ability to continue to offer minimally invasive surgical options to patients through a safe and standardized approach to tissue extraction.
The example case is real-time, contained, intact removal of an 8-cm, 130-g fibroid.

I hope you enjoy the featured opening session on best tissue extraction standards at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver and stop by to visit me at the OBG Management booth.
— Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
As a result of recent concerns regarding the use of power morcellation, clinicians have been faced with the need to develop alternative techniques for contained tissue extraction during minimally invasive gynecologic procedures such as myomectomy and hysterectomy.
The following video represents a refined and reproducible approach that incorporates a containment bag (Anchor Medical) and a self-retaining retractor (Applied Medical) in order to meet the following objectives:
- tissue extraction without the need for power morcellation
- specimen containment to avoid intraperitoneal spillage
- ability to continue to offer minimally invasive surgical options to patients through a safe and standardized approach to tissue extraction.
The example case is real-time, contained, intact removal of an 8-cm, 130-g fibroid.

I hope you enjoy the featured opening session on best tissue extraction standards at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver and stop by to visit me at the OBG Management booth.
— Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
As a result of recent concerns regarding the use of power morcellation, clinicians have been faced with the need to develop alternative techniques for contained tissue extraction during minimally invasive gynecologic procedures such as myomectomy and hysterectomy.
The following video represents a refined and reproducible approach that incorporates a containment bag (Anchor Medical) and a self-retaining retractor (Applied Medical) in order to meet the following objectives:
- tissue extraction without the need for power morcellation
- specimen containment to avoid intraperitoneal spillage
- ability to continue to offer minimally invasive surgical options to patients through a safe and standardized approach to tissue extraction.
The example case is real-time, contained, intact removal of an 8-cm, 130-g fibroid.

I hope you enjoy the featured opening session on best tissue extraction standards at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver and stop by to visit me at the OBG Management booth.
— Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
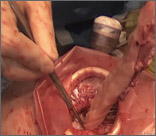
Total laparoscopic versus laparoscopic supracervical hysterectomy
It gives me great pleasure to introduce this month’s surgical video. The following feature presentation was produced by my third-year fellow, Mireille Truong, MD, and my third-year resident, Sarah Horvath, MD. The focus of this surgical video is to compare and contrast total laparoscopic hysterectomy (TLH) with laparoscopic supracervical hysterectomy (LSH). The indication for the TLH case was refractory dysmenorrhea and for the LSH case was as part of a concomitant sacrocervicopexy. The particular methods for specimen removal demonstrated include through the colpotomy for TLH and cold knife manual morcellation within a bag using an Alexis retractor for LSH.
The objectives of this surgical video are to:
- Highlight the clinical advantages and disadvantages between cervical removal or retention at the time of a minimally invasive laparoscopic hysterectomy
- Demonstrate the surgical nuances between TLH and LSH
- Provide a potential resource for patient counseling as well as medical student and resident education.
I encourage you to share this video as an educational resource with your colleagues, residents, students, and patients alike.

I hope to see you at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver, November 17–21, 2014. Visit www.aagl.org/globalcongress for more information.
— Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
It gives me great pleasure to introduce this month’s surgical video. The following feature presentation was produced by my third-year fellow, Mireille Truong, MD, and my third-year resident, Sarah Horvath, MD. The focus of this surgical video is to compare and contrast total laparoscopic hysterectomy (TLH) with laparoscopic supracervical hysterectomy (LSH). The indication for the TLH case was refractory dysmenorrhea and for the LSH case was as part of a concomitant sacrocervicopexy. The particular methods for specimen removal demonstrated include through the colpotomy for TLH and cold knife manual morcellation within a bag using an Alexis retractor for LSH.
The objectives of this surgical video are to:
- Highlight the clinical advantages and disadvantages between cervical removal or retention at the time of a minimally invasive laparoscopic hysterectomy
- Demonstrate the surgical nuances between TLH and LSH
- Provide a potential resource for patient counseling as well as medical student and resident education.
I encourage you to share this video as an educational resource with your colleagues, residents, students, and patients alike.

I hope to see you at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver, November 17–21, 2014. Visit www.aagl.org/globalcongress for more information.
— Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
It gives me great pleasure to introduce this month’s surgical video. The following feature presentation was produced by my third-year fellow, Mireille Truong, MD, and my third-year resident, Sarah Horvath, MD. The focus of this surgical video is to compare and contrast total laparoscopic hysterectomy (TLH) with laparoscopic supracervical hysterectomy (LSH). The indication for the TLH case was refractory dysmenorrhea and for the LSH case was as part of a concomitant sacrocervicopexy. The particular methods for specimen removal demonstrated include through the colpotomy for TLH and cold knife manual morcellation within a bag using an Alexis retractor for LSH.
The objectives of this surgical video are to:
- Highlight the clinical advantages and disadvantages between cervical removal or retention at the time of a minimally invasive laparoscopic hysterectomy
- Demonstrate the surgical nuances between TLH and LSH
- Provide a potential resource for patient counseling as well as medical student and resident education.
I encourage you to share this video as an educational resource with your colleagues, residents, students, and patients alike.

I hope to see you at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver, November 17–21, 2014. Visit www.aagl.org/globalcongress for more information.
— Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this video! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
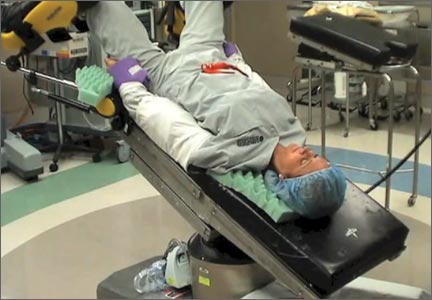
Preventing postoperative neuropathies: Patient positioning for minimally invasive procedures
In this comprehensive educational video we review appropriate patient positioning for laparoscopic and robotic surgery to prevent postoperative neuropathies that can be experienced with gynecologic surgery. We also include a case-based review of injuries specific to the brachial plexus, ulnar nerve, and femoral nerve.
Our technique involves the use of a bed sheet, an egg crate foam mattress pad, and boot-type stirrups. We recommend setting up the operating room table to facilitate tucking of the patient’s arms and to prevent slippage of the patient when she is placed in steep Trendelenburg. For all steps involved, see the video.
Tips for setting up the operating room bed include:
- Use of a single bed sheet placed across the head of a bare table with an egg crate foam mattress pad over the sheet to prevent the need for strapping the patient to the bed or the use of shoulder braces to prevent slippage.
- For low dorsal lithotomy positioning, flex the patient’s hips with a trunk-to-thigh angle of approximately 170°, and never more than 180°.
- For arm tucking, remove the arm boards and excess egg crate foam from the patient’s side and placecushioning over the elbow and the wrist. Keep the patient’s hand pronated when tucking and do not allow the arm to hang over the side of the bed.
- If the patient is obese, support the tucked arm by placing the arm boards beneath the arm parallel to the bed.
Next month we continue our series on surgical techniques with a video on why choosing the proper colpotomy cup is critical for successful minimally invasive hysterectomy.

Will you be joining me at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver this November? Safe patient positioning for minimally invasive surgery and other exciting topics will be discussed. Visit www.aagl.org/globalcongress for more information.
—Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In this comprehensive educational video we review appropriate patient positioning for laparoscopic and robotic surgery to prevent postoperative neuropathies that can be experienced with gynecologic surgery. We also include a case-based review of injuries specific to the brachial plexus, ulnar nerve, and femoral nerve.
Our technique involves the use of a bed sheet, an egg crate foam mattress pad, and boot-type stirrups. We recommend setting up the operating room table to facilitate tucking of the patient’s arms and to prevent slippage of the patient when she is placed in steep Trendelenburg. For all steps involved, see the video.
Tips for setting up the operating room bed include:
- Use of a single bed sheet placed across the head of a bare table with an egg crate foam mattress pad over the sheet to prevent the need for strapping the patient to the bed or the use of shoulder braces to prevent slippage.
- For low dorsal lithotomy positioning, flex the patient’s hips with a trunk-to-thigh angle of approximately 170°, and never more than 180°.
- For arm tucking, remove the arm boards and excess egg crate foam from the patient’s side and placecushioning over the elbow and the wrist. Keep the patient’s hand pronated when tucking and do not allow the arm to hang over the side of the bed.
- If the patient is obese, support the tucked arm by placing the arm boards beneath the arm parallel to the bed.
Next month we continue our series on surgical techniques with a video on why choosing the proper colpotomy cup is critical for successful minimally invasive hysterectomy.

Will you be joining me at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver this November? Safe patient positioning for minimally invasive surgery and other exciting topics will be discussed. Visit www.aagl.org/globalcongress for more information.
—Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
In this comprehensive educational video we review appropriate patient positioning for laparoscopic and robotic surgery to prevent postoperative neuropathies that can be experienced with gynecologic surgery. We also include a case-based review of injuries specific to the brachial plexus, ulnar nerve, and femoral nerve.
Our technique involves the use of a bed sheet, an egg crate foam mattress pad, and boot-type stirrups. We recommend setting up the operating room table to facilitate tucking of the patient’s arms and to prevent slippage of the patient when she is placed in steep Trendelenburg. For all steps involved, see the video.
Tips for setting up the operating room bed include:
- Use of a single bed sheet placed across the head of a bare table with an egg crate foam mattress pad over the sheet to prevent the need for strapping the patient to the bed or the use of shoulder braces to prevent slippage.
- For low dorsal lithotomy positioning, flex the patient’s hips with a trunk-to-thigh angle of approximately 170°, and never more than 180°.
- For arm tucking, remove the arm boards and excess egg crate foam from the patient’s side and placecushioning over the elbow and the wrist. Keep the patient’s hand pronated when tucking and do not allow the arm to hang over the side of the bed.
- If the patient is obese, support the tucked arm by placing the arm boards beneath the arm parallel to the bed.
Next month we continue our series on surgical techniques with a video on why choosing the proper colpotomy cup is critical for successful minimally invasive hysterectomy.

Will you be joining me at the AAGL Global Congress on Minimally Invasive Gynecology in Vancouver this November? Safe patient positioning for minimally invasive surgery and other exciting topics will be discussed. Visit www.aagl.org/globalcongress for more information.
—Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Understanding the spectrum of multiport and single-site robotics for hysterectomy
We present this video with the objective of demonstrating a hysterectomy performed using the robotic single-site approach in juxtaposition with a robotic multiport hysterectomy. In the video, and briefly here, we review the benefits, disadvantages, and challenges of robotic single-site hysterectomy.
The advantages of single-site robotic hysterectomy include:
- possible improved aesthetics for the patient
- allowance for surgeon independence while minimizing the need for a bedside assistant
- automatic reassignment of the robotic arm controls
- circumvention of certain limitations seen in laparoscopic single-site procedures.
The disadvantages of single-site robotic hysterectomy include:
- instrumentation is nonwristed and less robust than that of multiport instrumentation
- decreased degrees of freedom
- longer suturing time
- restricted assistant port use
- decreased applicability to a wide range of procedures as the surgical approach is limited to less complex and smaller pathology.
Related articles:
The robot is broadly accessible less than 10 years after its introduction to gynecologic surgery. Janelle Yates (News for your Practice; December 2013)
The robot is gaining ground in gynecologic surgery. Should you be using it? Arnold P. Advincula MD; Cheryl B. Iglesia MD; Rosanne M. Kho MD; Jamal Mourad, DO; Marie Fidela R. Paraiso, MD; Jason D. Wright, MD (Roundtable; April 2013)
Identify your learning curve for robotic hysterectomy. Joshua L Woelk, MD, MS, and John B. Gebhart, MD, MS (Guest Editorial; April 2013)
In general, each step of the single-port procedure has been found to be equivalent in time to a multiport approach to robotic-assisted hysterectomy—except for the step of vaginal cuff closure. Since the initial experience, aside from overcoming the learning curve of a new surgical approach, various techniques have been modified in order to surmount this challenge, such as closing the vaginal cuff vertically, using a cutting needle versus a tapered needle, addition of a “plus one” wristed multiport robotic arm, or replacing the single-site robotic needle driver with a multiport 5-mm needle driver.
Nevertheless, widespread adoption of single-site robotic gynecologic surgery still requires further technological improvements, and further research and experience is needed to determine its role, benefits, and applications in gynecologic surgery.
--Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
WE WANT TO HEAR FROM YOU!Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
We present this video with the objective of demonstrating a hysterectomy performed using the robotic single-site approach in juxtaposition with a robotic multiport hysterectomy. In the video, and briefly here, we review the benefits, disadvantages, and challenges of robotic single-site hysterectomy.
The advantages of single-site robotic hysterectomy include:
- possible improved aesthetics for the patient
- allowance for surgeon independence while minimizing the need for a bedside assistant
- automatic reassignment of the robotic arm controls
- circumvention of certain limitations seen in laparoscopic single-site procedures.
The disadvantages of single-site robotic hysterectomy include:
- instrumentation is nonwristed and less robust than that of multiport instrumentation
- decreased degrees of freedom
- longer suturing time
- restricted assistant port use
- decreased applicability to a wide range of procedures as the surgical approach is limited to less complex and smaller pathology.
Related articles:
The robot is broadly accessible less than 10 years after its introduction to gynecologic surgery. Janelle Yates (News for your Practice; December 2013)
The robot is gaining ground in gynecologic surgery. Should you be using it? Arnold P. Advincula MD; Cheryl B. Iglesia MD; Rosanne M. Kho MD; Jamal Mourad, DO; Marie Fidela R. Paraiso, MD; Jason D. Wright, MD (Roundtable; April 2013)
Identify your learning curve for robotic hysterectomy. Joshua L Woelk, MD, MS, and John B. Gebhart, MD, MS (Guest Editorial; April 2013)
In general, each step of the single-port procedure has been found to be equivalent in time to a multiport approach to robotic-assisted hysterectomy—except for the step of vaginal cuff closure. Since the initial experience, aside from overcoming the learning curve of a new surgical approach, various techniques have been modified in order to surmount this challenge, such as closing the vaginal cuff vertically, using a cutting needle versus a tapered needle, addition of a “plus one” wristed multiport robotic arm, or replacing the single-site robotic needle driver with a multiport 5-mm needle driver.
Nevertheless, widespread adoption of single-site robotic gynecologic surgery still requires further technological improvements, and further research and experience is needed to determine its role, benefits, and applications in gynecologic surgery.
--Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
WE WANT TO HEAR FROM YOU!Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
We present this video with the objective of demonstrating a hysterectomy performed using the robotic single-site approach in juxtaposition with a robotic multiport hysterectomy. In the video, and briefly here, we review the benefits, disadvantages, and challenges of robotic single-site hysterectomy.
The advantages of single-site robotic hysterectomy include:
- possible improved aesthetics for the patient
- allowance for surgeon independence while minimizing the need for a bedside assistant
- automatic reassignment of the robotic arm controls
- circumvention of certain limitations seen in laparoscopic single-site procedures.
The disadvantages of single-site robotic hysterectomy include:
- instrumentation is nonwristed and less robust than that of multiport instrumentation
- decreased degrees of freedom
- longer suturing time
- restricted assistant port use
- decreased applicability to a wide range of procedures as the surgical approach is limited to less complex and smaller pathology.
Related articles:
The robot is broadly accessible less than 10 years after its introduction to gynecologic surgery. Janelle Yates (News for your Practice; December 2013)
The robot is gaining ground in gynecologic surgery. Should you be using it? Arnold P. Advincula MD; Cheryl B. Iglesia MD; Rosanne M. Kho MD; Jamal Mourad, DO; Marie Fidela R. Paraiso, MD; Jason D. Wright, MD (Roundtable; April 2013)
Identify your learning curve for robotic hysterectomy. Joshua L Woelk, MD, MS, and John B. Gebhart, MD, MS (Guest Editorial; April 2013)
In general, each step of the single-port procedure has been found to be equivalent in time to a multiport approach to robotic-assisted hysterectomy—except for the step of vaginal cuff closure. Since the initial experience, aside from overcoming the learning curve of a new surgical approach, various techniques have been modified in order to surmount this challenge, such as closing the vaginal cuff vertically, using a cutting needle versus a tapered needle, addition of a “plus one” wristed multiport robotic arm, or replacing the single-site robotic needle driver with a multiport 5-mm needle driver.
Nevertheless, widespread adoption of single-site robotic gynecologic surgery still requires further technological improvements, and further research and experience is needed to determine its role, benefits, and applications in gynecologic surgery.
--Dr. Arnold Advincula, AAGL 2014 Scientific Program Chair
WE WANT TO HEAR FROM YOU!Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com