User login
Suspect an eating disorder? Suggest CBT
Refer patients with eating disorder not otherwise specified (NOS) for cognitive behavioral therapy. CBT, which has proven to be the most useful behavioral treatment for bulimia,1 has now been shown to be effective for patients in the NOS category.2
Strength of recommendation
B: 1 high-quality, randomized controlled trial (RCT).
Fairburn CG, Cooper Z, Doll HA, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311-319.
ILLUSTRATIVE CASE
A 23-year-old patient with a body mass index (BMI) of 18 tells you she’s fat and she’s afraid of gaining weight. Further questioning reveals that your patient binges on cookies and potato chips about once a week, then compensates for overeating by taking laxatives or exercising excessively—a practice she’s been following since she started college several years ago. The eating disorder she describes does not meet the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) for bulimia or anorexia nervosa, although it has elements of both. Rather, it fits the diagnostic criteria for eating disorder NOS. You’re aware that CBT is the first-line behavioral treatment for bulimia, and wonder whether it would be helpful for your patient.
Eating disorders often go undetected and untreated in primary care practices,3 as many patients don’t volunteer information about their weight or behaviors related to food, and physicians often fail to ask. Overall, as few as 10% of those with eating disorders receive any form of treatment.1
Would you recognize this loosely defined disorder?
In the United States, the lifetime prevalence of eating disorders is 0.6% for anorexia nervosa (0.3% for men and 0.9% for women), 1.0% for bulimia (0.5% for men and 1.5% for women), and 2.8% for binge-eating disorder (2.0% for men, 3.5% for women).4 Eating disorder NOS, which encompasses subthreshold cases of anorexia or bulimia, patients with elements of both anorexia and bulimia, and patients with binge-eating disorder, accounts for 50% to 80% of eating disorder diagnoses in outpatient settings. Yet there have been few studies of the treatment of these patients.2,5,6
A review of DSM-IV criteria
The diagnostic criteria for anorexia nervosa include a refusal to maintain a weight of at least 85% of normal body weight (or having a BMI ≤17.5), intense fear of gaining weight, disturbance in the way one’s body shape is experienced, and amenorrhea in females who are post-menarche.
Criteria for bulimia include recurrent episodes of binge eating (consuming a large amount of food with a sense of lack of control over eating) and recurrent inappropriate compensatory behaviors to prevent weight gain (self-induced vomiting, excessive exercise, fasting, laxatives, diuretics, or enemas) at least twice weekly for 3 months; and self-evaluation that is unduly influenced by body shape and weight.7 Most patients with eating disorder NOS have clinical features of both anorexia and bulimia.6
APA guidelines are silent on NOS
CBT has consistently proven to be the most useful behavioral treatment for patients with bulimia.1 Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine—the only medication with Food and Drug Administration approval for the treatment of an eating disorder8 —are about as effective as CBT, and the combination of CBT and an SSRI is superior to either treatment alone.9 CBT has also been found to be somewhat effective in treating binge-eating disorder.10
Anorexia nervosa, the most deadly eating disorder (the mortality rate is 6.6%11 ) and the most difficult to treat, is the exception. Several studies have assessed CBT for treating anorexia, but it has not been found to be very effective.10,12,13
The 2006 American Psychiatric Association practice guidelines for the treatment of patients with eating disorders feature recommendations for anorexia, bulimia, and binge-eating disorder, but do not address eating disorder NOS.10 The National Institute for Clinical Excellence (NICE) in the United Kingdom issued guidelines for the treatment of eating disorders in 2004. In response to the lack of evidence for treating eating disorder NOS, NICE recommended basing treatment on the form of eating disorder that most closely resembles the patient’s presentation.14 Fairburn et al addressed the lack of evidence for treatment of eating disorder NOS with the study summarized here.
STUDY SUMMARY: Both broad and focused CBT delivered results
Conducted at 2 eating disorder centers in the United Kingdom, this RCT included 154 patients, 18 to 65 years of age, who met DSM-IV criteria for either bulimia or eating disorder NOS. Exclusion criteria included prior treatment with CBT or other evidence-based treatment for the same eating disorder, and a BMI ≤17.5.
Most of the patients were female (95.5%) and white (90.3%), with a median age of 26 years and a median duration of eating disorder of 8.6 years. Sixty-two percent of the patients had a diagnosis of eating disorder NOS, and 38% were diagnosed with bulimia. Half of the patients had another current psychiatric diagnosis—a major depressive disorder, an anxiety disorder, or substance abuse.
The patients were randomized into 4 groups: Two received immediate treatment, and the other 2, referred to as waiting list controls, waited 8 weeks before beginning treatment. Treatment consisted of 1 of 2 forms of CBT-E, an enhanced form of CBT used to treat adult outpatients with eating disorders. Patients either received CBT-Ef, a focused form of CBT that exclusively targets eating disorder psychopathology, or CBT-Eb, a broader form of therapy that also addresses other problems that are common in patients with eating disorders, such as perfectionism and low self-esteem.
Both types of CBT-E featured a 90-minute preparatory session, 20 50-minute sessions, and 1 review session 20 weeks after completion of treatment. In the first 4 sessions, CBT-Ef and CBT-Eb were identical—addressing the eating disorder exclusively. CBT-Ef continued to focus on the eating disorder for the rest of the sessions, while subsequent CBT-Eb sessions also dealt with mood intolerance, interpersonal difficulties, and related issues. Five therapists—4 psychologists and 1 nurse-therapist—conducted the treatments.
Patients were weaned from ongoing psychiatric therapy during the study, but those who were on antidepressant therapy (n=76) were able to continue it. Patients were assessed before treatment, at the end of the waiting period for those in the control groups, after 8 weeks of treatment, at the end of treatment, and 20, 40, and 60 weeks after completion of treatment. (Twenty-two percent of the enrollees did not complete treatment.)
Primary outcomes were based on the Eating Disorder Examination (EDE), administered by assessors who were not involved in the treatment and were blinded to the patients’ group assignment. Change in severity of eating disorder features was measured by the global EDE score (0-6) and attaining a global EDE score <1.74 (<1 standard deviation above the community mean).
No treatment vs CBT. The waiting period left little doubt of the short-term efficacy of CBT: After 8 weeks, there was significant improvement in eating disorder behaviors and overall severity in both the CBT-Ef and CBT-Eb groups (EDE scores fell from 4.15 at baseline to 3.26 and from 4.04 to 2.89, respectively). In the same time period, scores for the waiting list control groups remained flat (from 4.08 at baseline to 3.99).
At the end of treatment and at the 60-week follow-up, patients in both forms of CBT-E showed significant improvement across all measures, with no significant difference between treatments. By the end of treatment, 66.4% of those who completed all of the CBT sessions had global EDE scores <1.74 (considered clinically significant).
Subgroup analysis offers opportunity for fine-tuning
When analyzed separately, the patients with bulimia and those with eating disorder NOS did equally well at the end of treatment: 52.7% of those with bulimia and 53.3% of those with eating disorder NOS had global EDE scores <1.74. At the 60-week follow-up, the patients with bulimia maintained their improvement slightly more: 61.4% had global EDE scores <1.74, compared with 45.7% of the patients with eating disorder NOS.
The researchers also compared the outcomes of patients with the most complex additional psychopathology with those of patients with less complex problems. Greater complexity was defined as moderate ratings in at least 2 of the following domains: mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties.
Broad focus more effective for high complexity. Overall, those in the more complex subgroup did not respond as well; 48% had global EDE scores <1.74, vs 60% of those in the less complex group. However, those in the more complex subgroup did better with the broad form of CBT (at 60-week follow up, 60% had scores <1.74 with CBT-Eb, compared with 40% in the CBT-Ef treatment arm), while the less complex subgroup did better with the more tightly focused CBT-Ef. 2
WHAT’S NEW: Evidence supports CBT for NOS diagnosis
The most recent (2004) Cochrane review of “psychotherapy for bulimia nervosa and binging” included 40 RCTs of patients with bulimia, binge-eating disorder, and eating disorder NOS with recurrent binge-eating episodes (included in 7 studies). While the review confirmed that CBT is effective for bulimia and “similar syndromes,” it identified a need for larger and higher quality trials of CBT, particularly in patients with eating disorder NOS.1 The study reviewed in this PURL—the first large, high-quality trial to include a number of patients with eating disorder NOS—provides strong evidence that CBT is effective for this group of patients.2
CAVEATS: Limited wait time leaves unanswered questions
One limitation of this study is the lack of a control group beyond the 8-week waiting period. Prior studies of CBT for bulimia that delayed therapy for those in the control groups for a longer duration have consistently shown that patients receiving CBT did significantly better than those in the control group.9 While a “no treatment” group would have made the results more robust in this case, it would not have been ethical to withhold treatment for the entire length of the study.
It is noteworthy, too, that this study only included patients with a BMI >17.5. Patients with a diagnosis of anorexia nervosa, who by definition have a lower BMI, will need other treatments, including hospitalization in some cases.
CHALLENGES TO IMPLEMENTATION: Identifying patients and therapists
The primary challenge is to determine which of your patients have eating disorders. When discussing diet, adding a simple question such as, “Are you happy with your current weight?” can help you identify those who meet the criteria for an eating disorder or are at high risk.3
Identifying local mental health providers who are trained to provide CBT for patients with eating disorders is another concern. Insurance coverage for this intensive treatment may also be a limiting factor in some cases.
Many studies support the use of fluoxetine for patients with bulimia, and combined treatment with SSRIs and CBT has been shown to be superior to either treatment alone.8,10,14 Consider starting the patient on an antidepressant while she (or he) awaits the start of CBT.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURLs) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Hay PJ, Bacaltchuk J, Stefano S. Psychotherapy for bulimia nervosa and binging. Cochrane Database Syst Rev. 2004;(3):CD000562.
2. Fairburn CG, Cooper Z, Doll HA, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311-319.
3. Pritts SD, Susman J. Diagnosis of eating disorders in primary care. Am Fam Physician. 2003;67:297-304.
4. Hudson JI, Hiripi E, Pope HG Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348-358.
5. Button EJ, Benson E, Nollett C, et al. Don’t forget EDNOS (eating disorder not otherwise specified): patterns of service use in an eating disorders service. Psychiatr Bull. 2005;29:134-136.
6. Fairburn CG, Cooper Z, Bohn K, et al. The severity and status of eating disorder NOS: implications for DSM-V. Behav Res Ther. 2007;45:1705-1715.
7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. rev. Washington, DC: American Psychiatric Association; 2000:583-595,787.
8. Berkman ND, Bulik CM, Brownley KA, et al. Management of eating disorders. Evidence Report/Technology Assessment No.135. AHRQ Publication No. 06-E010. Rockville, MD: Agency for Healthcare Research and Quality; April 2006.
9. Shapiro JR, Berkman ND, Brownley KA, et al. Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:321-336.
10. American Psychiatric Association Practice Guideline. Treatment of patients with eating disorders. 3rd ed Available at: http://www.psychiatryonline.com/pracGuide/pracGuideTopic_12.aspx. Accessed April 9, 2009.
11. Eckert ED, Halmi KA, Marchi P, et al. Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychol Med. 1995;25:143-156.
12. Hay PJ, Bacaltchuk J, Byrnes RT, et al. Individual psychotherapy in the outpatient treatment of adults with anorexia nervosa. Cochrane Database Syst Rev. 2009;(1):CD003909.
13. Morris J, Twaddle S. Anorexia Nervosa. BMJ. 2007;334:894-898.
14. National Collaborating Centre for Mental Health. Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. Clinical guideline 9. Available at: http://www.nice.org.uk/guidance/CG9/niceguidance/pdf/English. Accessed June 28, 2007.
Refer patients with eating disorder not otherwise specified (NOS) for cognitive behavioral therapy. CBT, which has proven to be the most useful behavioral treatment for bulimia,1 has now been shown to be effective for patients in the NOS category.2
Strength of recommendation
B: 1 high-quality, randomized controlled trial (RCT).
Fairburn CG, Cooper Z, Doll HA, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311-319.
ILLUSTRATIVE CASE
A 23-year-old patient with a body mass index (BMI) of 18 tells you she’s fat and she’s afraid of gaining weight. Further questioning reveals that your patient binges on cookies and potato chips about once a week, then compensates for overeating by taking laxatives or exercising excessively—a practice she’s been following since she started college several years ago. The eating disorder she describes does not meet the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) for bulimia or anorexia nervosa, although it has elements of both. Rather, it fits the diagnostic criteria for eating disorder NOS. You’re aware that CBT is the first-line behavioral treatment for bulimia, and wonder whether it would be helpful for your patient.
Eating disorders often go undetected and untreated in primary care practices,3 as many patients don’t volunteer information about their weight or behaviors related to food, and physicians often fail to ask. Overall, as few as 10% of those with eating disorders receive any form of treatment.1
Would you recognize this loosely defined disorder?
In the United States, the lifetime prevalence of eating disorders is 0.6% for anorexia nervosa (0.3% for men and 0.9% for women), 1.0% for bulimia (0.5% for men and 1.5% for women), and 2.8% for binge-eating disorder (2.0% for men, 3.5% for women).4 Eating disorder NOS, which encompasses subthreshold cases of anorexia or bulimia, patients with elements of both anorexia and bulimia, and patients with binge-eating disorder, accounts for 50% to 80% of eating disorder diagnoses in outpatient settings. Yet there have been few studies of the treatment of these patients.2,5,6
A review of DSM-IV criteria
The diagnostic criteria for anorexia nervosa include a refusal to maintain a weight of at least 85% of normal body weight (or having a BMI ≤17.5), intense fear of gaining weight, disturbance in the way one’s body shape is experienced, and amenorrhea in females who are post-menarche.
Criteria for bulimia include recurrent episodes of binge eating (consuming a large amount of food with a sense of lack of control over eating) and recurrent inappropriate compensatory behaviors to prevent weight gain (self-induced vomiting, excessive exercise, fasting, laxatives, diuretics, or enemas) at least twice weekly for 3 months; and self-evaluation that is unduly influenced by body shape and weight.7 Most patients with eating disorder NOS have clinical features of both anorexia and bulimia.6
APA guidelines are silent on NOS
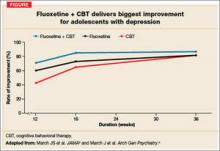
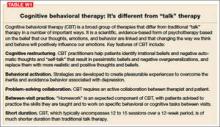
CBT has consistently proven to be the most useful behavioral treatment for patients with bulimia.1 Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine—the only medication with Food and Drug Administration approval for the treatment of an eating disorder8 —are about as effective as CBT, and the combination of CBT and an SSRI is superior to either treatment alone.9 CBT has also been found to be somewhat effective in treating binge-eating disorder.10
Anorexia nervosa, the most deadly eating disorder (the mortality rate is 6.6%11 ) and the most difficult to treat, is the exception. Several studies have assessed CBT for treating anorexia, but it has not been found to be very effective.10,12,13
The 2006 American Psychiatric Association practice guidelines for the treatment of patients with eating disorders feature recommendations for anorexia, bulimia, and binge-eating disorder, but do not address eating disorder NOS.10 The National Institute for Clinical Excellence (NICE) in the United Kingdom issued guidelines for the treatment of eating disorders in 2004. In response to the lack of evidence for treating eating disorder NOS, NICE recommended basing treatment on the form of eating disorder that most closely resembles the patient’s presentation.14 Fairburn et al addressed the lack of evidence for treatment of eating disorder NOS with the study summarized here.
STUDY SUMMARY: Both broad and focused CBT delivered results
Conducted at 2 eating disorder centers in the United Kingdom, this RCT included 154 patients, 18 to 65 years of age, who met DSM-IV criteria for either bulimia or eating disorder NOS. Exclusion criteria included prior treatment with CBT or other evidence-based treatment for the same eating disorder, and a BMI ≤17.5.
Most of the patients were female (95.5%) and white (90.3%), with a median age of 26 years and a median duration of eating disorder of 8.6 years. Sixty-two percent of the patients had a diagnosis of eating disorder NOS, and 38% were diagnosed with bulimia. Half of the patients had another current psychiatric diagnosis—a major depressive disorder, an anxiety disorder, or substance abuse.
The patients were randomized into 4 groups: Two received immediate treatment, and the other 2, referred to as waiting list controls, waited 8 weeks before beginning treatment. Treatment consisted of 1 of 2 forms of CBT-E, an enhanced form of CBT used to treat adult outpatients with eating disorders. Patients either received CBT-Ef, a focused form of CBT that exclusively targets eating disorder psychopathology, or CBT-Eb, a broader form of therapy that also addresses other problems that are common in patients with eating disorders, such as perfectionism and low self-esteem.
Both types of CBT-E featured a 90-minute preparatory session, 20 50-minute sessions, and 1 review session 20 weeks after completion of treatment. In the first 4 sessions, CBT-Ef and CBT-Eb were identical—addressing the eating disorder exclusively. CBT-Ef continued to focus on the eating disorder for the rest of the sessions, while subsequent CBT-Eb sessions also dealt with mood intolerance, interpersonal difficulties, and related issues. Five therapists—4 psychologists and 1 nurse-therapist—conducted the treatments.
Patients were weaned from ongoing psychiatric therapy during the study, but those who were on antidepressant therapy (n=76) were able to continue it. Patients were assessed before treatment, at the end of the waiting period for those in the control groups, after 8 weeks of treatment, at the end of treatment, and 20, 40, and 60 weeks after completion of treatment. (Twenty-two percent of the enrollees did not complete treatment.)
Primary outcomes were based on the Eating Disorder Examination (EDE), administered by assessors who were not involved in the treatment and were blinded to the patients’ group assignment. Change in severity of eating disorder features was measured by the global EDE score (0-6) and attaining a global EDE score <1.74 (<1 standard deviation above the community mean).
No treatment vs CBT. The waiting period left little doubt of the short-term efficacy of CBT: After 8 weeks, there was significant improvement in eating disorder behaviors and overall severity in both the CBT-Ef and CBT-Eb groups (EDE scores fell from 4.15 at baseline to 3.26 and from 4.04 to 2.89, respectively). In the same time period, scores for the waiting list control groups remained flat (from 4.08 at baseline to 3.99).
At the end of treatment and at the 60-week follow-up, patients in both forms of CBT-E showed significant improvement across all measures, with no significant difference between treatments. By the end of treatment, 66.4% of those who completed all of the CBT sessions had global EDE scores <1.74 (considered clinically significant).
Subgroup analysis offers opportunity for fine-tuning
When analyzed separately, the patients with bulimia and those with eating disorder NOS did equally well at the end of treatment: 52.7% of those with bulimia and 53.3% of those with eating disorder NOS had global EDE scores <1.74. At the 60-week follow-up, the patients with bulimia maintained their improvement slightly more: 61.4% had global EDE scores <1.74, compared with 45.7% of the patients with eating disorder NOS.
The researchers also compared the outcomes of patients with the most complex additional psychopathology with those of patients with less complex problems. Greater complexity was defined as moderate ratings in at least 2 of the following domains: mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties.
Broad focus more effective for high complexity. Overall, those in the more complex subgroup did not respond as well; 48% had global EDE scores <1.74, vs 60% of those in the less complex group. However, those in the more complex subgroup did better with the broad form of CBT (at 60-week follow up, 60% had scores <1.74 with CBT-Eb, compared with 40% in the CBT-Ef treatment arm), while the less complex subgroup did better with the more tightly focused CBT-Ef. 2
WHAT’S NEW: Evidence supports CBT for NOS diagnosis
The most recent (2004) Cochrane review of “psychotherapy for bulimia nervosa and binging” included 40 RCTs of patients with bulimia, binge-eating disorder, and eating disorder NOS with recurrent binge-eating episodes (included in 7 studies). While the review confirmed that CBT is effective for bulimia and “similar syndromes,” it identified a need for larger and higher quality trials of CBT, particularly in patients with eating disorder NOS.1 The study reviewed in this PURL—the first large, high-quality trial to include a number of patients with eating disorder NOS—provides strong evidence that CBT is effective for this group of patients.2
CAVEATS: Limited wait time leaves unanswered questions
One limitation of this study is the lack of a control group beyond the 8-week waiting period. Prior studies of CBT for bulimia that delayed therapy for those in the control groups for a longer duration have consistently shown that patients receiving CBT did significantly better than those in the control group.9 While a “no treatment” group would have made the results more robust in this case, it would not have been ethical to withhold treatment for the entire length of the study.
It is noteworthy, too, that this study only included patients with a BMI >17.5. Patients with a diagnosis of anorexia nervosa, who by definition have a lower BMI, will need other treatments, including hospitalization in some cases.
CHALLENGES TO IMPLEMENTATION: Identifying patients and therapists
The primary challenge is to determine which of your patients have eating disorders. When discussing diet, adding a simple question such as, “Are you happy with your current weight?” can help you identify those who meet the criteria for an eating disorder or are at high risk.3
Identifying local mental health providers who are trained to provide CBT for patients with eating disorders is another concern. Insurance coverage for this intensive treatment may also be a limiting factor in some cases.
Many studies support the use of fluoxetine for patients with bulimia, and combined treatment with SSRIs and CBT has been shown to be superior to either treatment alone.8,10,14 Consider starting the patient on an antidepressant while she (or he) awaits the start of CBT.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURLs) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Refer patients with eating disorder not otherwise specified (NOS) for cognitive behavioral therapy. CBT, which has proven to be the most useful behavioral treatment for bulimia,1 has now been shown to be effective for patients in the NOS category.2
Strength of recommendation
B: 1 high-quality, randomized controlled trial (RCT).
Fairburn CG, Cooper Z, Doll HA, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311-319.
ILLUSTRATIVE CASE
A 23-year-old patient with a body mass index (BMI) of 18 tells you she’s fat and she’s afraid of gaining weight. Further questioning reveals that your patient binges on cookies and potato chips about once a week, then compensates for overeating by taking laxatives or exercising excessively—a practice she’s been following since she started college several years ago. The eating disorder she describes does not meet the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) for bulimia or anorexia nervosa, although it has elements of both. Rather, it fits the diagnostic criteria for eating disorder NOS. You’re aware that CBT is the first-line behavioral treatment for bulimia, and wonder whether it would be helpful for your patient.
Eating disorders often go undetected and untreated in primary care practices,3 as many patients don’t volunteer information about their weight or behaviors related to food, and physicians often fail to ask. Overall, as few as 10% of those with eating disorders receive any form of treatment.1
Would you recognize this loosely defined disorder?
In the United States, the lifetime prevalence of eating disorders is 0.6% for anorexia nervosa (0.3% for men and 0.9% for women), 1.0% for bulimia (0.5% for men and 1.5% for women), and 2.8% for binge-eating disorder (2.0% for men, 3.5% for women).4 Eating disorder NOS, which encompasses subthreshold cases of anorexia or bulimia, patients with elements of both anorexia and bulimia, and patients with binge-eating disorder, accounts for 50% to 80% of eating disorder diagnoses in outpatient settings. Yet there have been few studies of the treatment of these patients.2,5,6
A review of DSM-IV criteria
The diagnostic criteria for anorexia nervosa include a refusal to maintain a weight of at least 85% of normal body weight (or having a BMI ≤17.5), intense fear of gaining weight, disturbance in the way one’s body shape is experienced, and amenorrhea in females who are post-menarche.
Criteria for bulimia include recurrent episodes of binge eating (consuming a large amount of food with a sense of lack of control over eating) and recurrent inappropriate compensatory behaviors to prevent weight gain (self-induced vomiting, excessive exercise, fasting, laxatives, diuretics, or enemas) at least twice weekly for 3 months; and self-evaluation that is unduly influenced by body shape and weight.7 Most patients with eating disorder NOS have clinical features of both anorexia and bulimia.6
APA guidelines are silent on NOS
CBT has consistently proven to be the most useful behavioral treatment for patients with bulimia.1 Selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine—the only medication with Food and Drug Administration approval for the treatment of an eating disorder8 —are about as effective as CBT, and the combination of CBT and an SSRI is superior to either treatment alone.9 CBT has also been found to be somewhat effective in treating binge-eating disorder.10
Anorexia nervosa, the most deadly eating disorder (the mortality rate is 6.6%11 ) and the most difficult to treat, is the exception. Several studies have assessed CBT for treating anorexia, but it has not been found to be very effective.10,12,13
The 2006 American Psychiatric Association practice guidelines for the treatment of patients with eating disorders feature recommendations for anorexia, bulimia, and binge-eating disorder, but do not address eating disorder NOS.10 The National Institute for Clinical Excellence (NICE) in the United Kingdom issued guidelines for the treatment of eating disorders in 2004. In response to the lack of evidence for treating eating disorder NOS, NICE recommended basing treatment on the form of eating disorder that most closely resembles the patient’s presentation.14 Fairburn et al addressed the lack of evidence for treatment of eating disorder NOS with the study summarized here.
STUDY SUMMARY: Both broad and focused CBT delivered results
Conducted at 2 eating disorder centers in the United Kingdom, this RCT included 154 patients, 18 to 65 years of age, who met DSM-IV criteria for either bulimia or eating disorder NOS. Exclusion criteria included prior treatment with CBT or other evidence-based treatment for the same eating disorder, and a BMI ≤17.5.
Most of the patients were female (95.5%) and white (90.3%), with a median age of 26 years and a median duration of eating disorder of 8.6 years. Sixty-two percent of the patients had a diagnosis of eating disorder NOS, and 38% were diagnosed with bulimia. Half of the patients had another current psychiatric diagnosis—a major depressive disorder, an anxiety disorder, or substance abuse.
The patients were randomized into 4 groups: Two received immediate treatment, and the other 2, referred to as waiting list controls, waited 8 weeks before beginning treatment. Treatment consisted of 1 of 2 forms of CBT-E, an enhanced form of CBT used to treat adult outpatients with eating disorders. Patients either received CBT-Ef, a focused form of CBT that exclusively targets eating disorder psychopathology, or CBT-Eb, a broader form of therapy that also addresses other problems that are common in patients with eating disorders, such as perfectionism and low self-esteem.
Both types of CBT-E featured a 90-minute preparatory session, 20 50-minute sessions, and 1 review session 20 weeks after completion of treatment. In the first 4 sessions, CBT-Ef and CBT-Eb were identical—addressing the eating disorder exclusively. CBT-Ef continued to focus on the eating disorder for the rest of the sessions, while subsequent CBT-Eb sessions also dealt with mood intolerance, interpersonal difficulties, and related issues. Five therapists—4 psychologists and 1 nurse-therapist—conducted the treatments.
Patients were weaned from ongoing psychiatric therapy during the study, but those who were on antidepressant therapy (n=76) were able to continue it. Patients were assessed before treatment, at the end of the waiting period for those in the control groups, after 8 weeks of treatment, at the end of treatment, and 20, 40, and 60 weeks after completion of treatment. (Twenty-two percent of the enrollees did not complete treatment.)
Primary outcomes were based on the Eating Disorder Examination (EDE), administered by assessors who were not involved in the treatment and were blinded to the patients’ group assignment. Change in severity of eating disorder features was measured by the global EDE score (0-6) and attaining a global EDE score <1.74 (<1 standard deviation above the community mean).
No treatment vs CBT. The waiting period left little doubt of the short-term efficacy of CBT: After 8 weeks, there was significant improvement in eating disorder behaviors and overall severity in both the CBT-Ef and CBT-Eb groups (EDE scores fell from 4.15 at baseline to 3.26 and from 4.04 to 2.89, respectively). In the same time period, scores for the waiting list control groups remained flat (from 4.08 at baseline to 3.99).
At the end of treatment and at the 60-week follow-up, patients in both forms of CBT-E showed significant improvement across all measures, with no significant difference between treatments. By the end of treatment, 66.4% of those who completed all of the CBT sessions had global EDE scores <1.74 (considered clinically significant).
Subgroup analysis offers opportunity for fine-tuning
When analyzed separately, the patients with bulimia and those with eating disorder NOS did equally well at the end of treatment: 52.7% of those with bulimia and 53.3% of those with eating disorder NOS had global EDE scores <1.74. At the 60-week follow-up, the patients with bulimia maintained their improvement slightly more: 61.4% had global EDE scores <1.74, compared with 45.7% of the patients with eating disorder NOS.
The researchers also compared the outcomes of patients with the most complex additional psychopathology with those of patients with less complex problems. Greater complexity was defined as moderate ratings in at least 2 of the following domains: mood intolerance, clinical perfectionism, low self-esteem, and interpersonal difficulties.
Broad focus more effective for high complexity. Overall, those in the more complex subgroup did not respond as well; 48% had global EDE scores <1.74, vs 60% of those in the less complex group. However, those in the more complex subgroup did better with the broad form of CBT (at 60-week follow up, 60% had scores <1.74 with CBT-Eb, compared with 40% in the CBT-Ef treatment arm), while the less complex subgroup did better with the more tightly focused CBT-Ef. 2
WHAT’S NEW: Evidence supports CBT for NOS diagnosis
The most recent (2004) Cochrane review of “psychotherapy for bulimia nervosa and binging” included 40 RCTs of patients with bulimia, binge-eating disorder, and eating disorder NOS with recurrent binge-eating episodes (included in 7 studies). While the review confirmed that CBT is effective for bulimia and “similar syndromes,” it identified a need for larger and higher quality trials of CBT, particularly in patients with eating disorder NOS.1 The study reviewed in this PURL—the first large, high-quality trial to include a number of patients with eating disorder NOS—provides strong evidence that CBT is effective for this group of patients.2
CAVEATS: Limited wait time leaves unanswered questions
One limitation of this study is the lack of a control group beyond the 8-week waiting period. Prior studies of CBT for bulimia that delayed therapy for those in the control groups for a longer duration have consistently shown that patients receiving CBT did significantly better than those in the control group.9 While a “no treatment” group would have made the results more robust in this case, it would not have been ethical to withhold treatment for the entire length of the study.
It is noteworthy, too, that this study only included patients with a BMI >17.5. Patients with a diagnosis of anorexia nervosa, who by definition have a lower BMI, will need other treatments, including hospitalization in some cases.
CHALLENGES TO IMPLEMENTATION: Identifying patients and therapists
The primary challenge is to determine which of your patients have eating disorders. When discussing diet, adding a simple question such as, “Are you happy with your current weight?” can help you identify those who meet the criteria for an eating disorder or are at high risk.3
Identifying local mental health providers who are trained to provide CBT for patients with eating disorders is another concern. Insurance coverage for this intensive treatment may also be a limiting factor in some cases.
Many studies support the use of fluoxetine for patients with bulimia, and combined treatment with SSRIs and CBT has been shown to be superior to either treatment alone.8,10,14 Consider starting the patient on an antidepressant while she (or he) awaits the start of CBT.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURLs) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Hay PJ, Bacaltchuk J, Stefano S. Psychotherapy for bulimia nervosa and binging. Cochrane Database Syst Rev. 2004;(3):CD000562.
2. Fairburn CG, Cooper Z, Doll HA, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311-319.
3. Pritts SD, Susman J. Diagnosis of eating disorders in primary care. Am Fam Physician. 2003;67:297-304.
4. Hudson JI, Hiripi E, Pope HG Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348-358.
5. Button EJ, Benson E, Nollett C, et al. Don’t forget EDNOS (eating disorder not otherwise specified): patterns of service use in an eating disorders service. Psychiatr Bull. 2005;29:134-136.
6. Fairburn CG, Cooper Z, Bohn K, et al. The severity and status of eating disorder NOS: implications for DSM-V. Behav Res Ther. 2007;45:1705-1715.
7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. rev. Washington, DC: American Psychiatric Association; 2000:583-595,787.
8. Berkman ND, Bulik CM, Brownley KA, et al. Management of eating disorders. Evidence Report/Technology Assessment No.135. AHRQ Publication No. 06-E010. Rockville, MD: Agency for Healthcare Research and Quality; April 2006.
9. Shapiro JR, Berkman ND, Brownley KA, et al. Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:321-336.
10. American Psychiatric Association Practice Guideline. Treatment of patients with eating disorders. 3rd ed Available at: http://www.psychiatryonline.com/pracGuide/pracGuideTopic_12.aspx. Accessed April 9, 2009.
11. Eckert ED, Halmi KA, Marchi P, et al. Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychol Med. 1995;25:143-156.
12. Hay PJ, Bacaltchuk J, Byrnes RT, et al. Individual psychotherapy in the outpatient treatment of adults with anorexia nervosa. Cochrane Database Syst Rev. 2009;(1):CD003909.
13. Morris J, Twaddle S. Anorexia Nervosa. BMJ. 2007;334:894-898.
14. National Collaborating Centre for Mental Health. Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. Clinical guideline 9. Available at: http://www.nice.org.uk/guidance/CG9/niceguidance/pdf/English. Accessed June 28, 2007.
1. Hay PJ, Bacaltchuk J, Stefano S. Psychotherapy for bulimia nervosa and binging. Cochrane Database Syst Rev. 2004;(3):CD000562.
2. Fairburn CG, Cooper Z, Doll HA, et al. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. Am J Psychiatry. 2009;166:311-319.
3. Pritts SD, Susman J. Diagnosis of eating disorders in primary care. Am Fam Physician. 2003;67:297-304.
4. Hudson JI, Hiripi E, Pope HG Jr, et al. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61:348-358.
5. Button EJ, Benson E, Nollett C, et al. Don’t forget EDNOS (eating disorder not otherwise specified): patterns of service use in an eating disorders service. Psychiatr Bull. 2005;29:134-136.
6. Fairburn CG, Cooper Z, Bohn K, et al. The severity and status of eating disorder NOS: implications for DSM-V. Behav Res Ther. 2007;45:1705-1715.
7. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. rev. Washington, DC: American Psychiatric Association; 2000:583-595,787.
8. Berkman ND, Bulik CM, Brownley KA, et al. Management of eating disorders. Evidence Report/Technology Assessment No.135. AHRQ Publication No. 06-E010. Rockville, MD: Agency for Healthcare Research and Quality; April 2006.
9. Shapiro JR, Berkman ND, Brownley KA, et al. Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40:321-336.
10. American Psychiatric Association Practice Guideline. Treatment of patients with eating disorders. 3rd ed Available at: http://www.psychiatryonline.com/pracGuide/pracGuideTopic_12.aspx. Accessed April 9, 2009.
11. Eckert ED, Halmi KA, Marchi P, et al. Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychol Med. 1995;25:143-156.
12. Hay PJ, Bacaltchuk J, Byrnes RT, et al. Individual psychotherapy in the outpatient treatment of adults with anorexia nervosa. Cochrane Database Syst Rev. 2009;(1):CD003909.
13. Morris J, Twaddle S. Anorexia Nervosa. BMJ. 2007;334:894-898.
14. National Collaborating Centre for Mental Health. Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. Clinical guideline 9. Available at: http://www.nice.org.uk/guidance/CG9/niceguidance/pdf/English. Accessed June 28, 2007.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
When to suggest this OC alternative
Recommend continuous or extended use of the transvaginal contraceptive ring to women who want fewer days of menstrual bleeding and have trouble remembering to, or prefer not to, take a daily pill. If breakthrough bleeding is troublesome, suggest a 4-day ring-free interval.1
Strength of recommendation
B: Based on a single randomized controlled trial (RCT) with <80% follow up.
Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring: a randomized controlled trial. Obstet Gynecol. 2008;112:563-571.
ILLUSTRATIVE CASE
Case 1: A healthy 25-year-old woman comes to see you because she’s worried about getting pregnant. She’s been on an extended-cycle oral contraceptive (OC) for several months and is happy to have her period only once every 3 months, but she frequently forgets to take her pill.
What can you offer that will give her the benefits of an extended-cycle OC, without the risk of pregnancy she incurs each time she misses a pill?
Case 2: You started a healthy 18-year-old on the transvaginal ring 6 months ago. After counseling, she opted for continuous cycling, so she inserts a new ring right after she removes the old one, on the same date each month. Although she likes the ring, she’s disturbed by a recent increase in breakthrough bleeding. What can you recommend to decrease the bleeding?
Clinicians have long known that the traditional 21/7 OC cycle is not necessary for safety or efficacy. More recently, many women have been happy to learn that there is no physiologic reason to have a monthly period when they’re using combination hormonal contraception. They’re also happy to discover that fewer periods often mean fewer premenstrual mood swings, episodes of painful cramping, and instances of other troublesome symptoms.
The transvaginal ring is often overlooked
The US Food and Drug Administration (FDA) has approved 2 combination OCs for extended-cycle use and 1 for continuous use. But any monophasic OC can be used off-label for extended or continuous cycling to decrease bleeding frequency. So, too, can the transvaginal contraceptive ring (NuvaRing), an infrequently used contraceptive. (According to 1 study, just 5.7% of US women using contraception used either the ring or the patch.2 ) The ring has been studied for extended use,3 but does not have FDA approval for longer-term regimens.
NuvaRing is a flexible, transparent device that contains the progestin etonogestrel and ethinyl estradiol. The manufacturer recommends a 21/7 cycle, inserting the ring in the vagina and leaving it in place for 3 weeks, removing it for 1 week, and then inserting a new ring.4 The ring is well suited to women who have no contraindications to hormonal contraception but have difficulty remembering to take a pill every day—or simply prefer the convenience of less frequent dosing.
While the ring has been found to be effective and tolerable when used without a hormone-free interval—28-, 49-, 91- and 364-day dosing has been studied—breakthrough bleeding or spotting is a frequent side effect of extended-cycle hormonal contraception. In 1 study, 43% of women on a 49-day ring cycle experienced breakthrough bleeding, compared with 16% of those on a 28-day cycle.3
High satisfaction, low risk
Nonetheless, women who use the transvaginal ring often report high satisfaction. One study found that 61% of women were very satisfied with this method of contraception, compared with 34% of triphasic OC users (P<.003).5 The risk of pregnancy (1-2 pregnancies per 100 women-years of use, according to the manufacturer4 ) and the risk of venous thromboembolism (10-30 in 100,000 vs 4-11 in 100,000 nonpregnant women who are not using hormonal contraception) are comparable to that of women using OCs.6,7 The risk of other severe side effects associated with the vaginal ring is comparable to that of OCs, as well.
STUDY SUMMARY: An effective option that women used post-trial
This RCT recruited women between the ages of 18 and 45 years who had been using combination hormonal contraceptives—OCs, the transdermal patch, or the transvaginal ring. All had been on a 21/7 cycle for at least 2 months. Exclusion criteria included a body mass index ≥38 kg/m2, smoking >10 cigarettes per day, use of other estrogen- or phytoestrogen-containing products, and the presence of ovarian cysts >2.5 cm or endometrial thickness >8 mm. Women who wanted to get pregnant within a year were also excluded.
The study began with a baseline phase during which participants completed one 21/7 cycle with the ring for those using the ring prior to the study or two 21/7 cycles for those using the pill or patch prior to the study. Daily flow was assessed during this initial phase, using a scale of 0 to 4, with 4 being the heaviest. Women who completed this phase and wanted to continue using the ring (N=74) were then randomized into 2 groups (n=37) for the 6-month extended phase.
Group 1 was assigned to use the contraceptive ring with no hormone-free days. Participants were instructed to replace the rings monthly, on the same calendar day of the month. Group 2 also used the ring on a continuous basis with monthly replacement, but those who experienced breakthrough bleeding for more than 5 days were permitted to remove the ring for 4 days. Women in both groups kept a daily diary of ring usage, degree of menstrual flow, and symptomatology, including pelvic pain, headaches, and mood.
Most subjects were white (76%), nonsmokers (84%), and unmarried (68% in Group 1 and 57% in Group 2), with an average age of 28 to 29 years. Eight patients (22%) in Group 1 withdrew from the study prior to completing the 6-month extended phase, 4 of them because of side effects. Only 1 woman withdrew from Group 2, because of plans for pregnancy. No one became pregnant while using the ring.
Hormone-free interval reduced bleeding. In Group 1, the average daily flow score was slightly reduced with continuous use (from 0.33 during the 21/7 baseline phase to 0.21 in the 6-month extended phase), but researchers reported no significant difference in flow-free days. On average, 85% of the days were flow-free in the 21/7 phase, vs 89% in the extended phase.
In Group 2, flow-free days increased, from 83% in the baseline phase to 95% in the extended phase, and average flow scores fell from 0.38 to 0.17.
Overall, the 65 participants who completed 6 months of continuous ring use had fewer bleeding days per month—1.8 days, on average, vs 3.3 days during the initial 21/7 phase, but more days of spotting per month (2.5 vs 1.8 days). There was no difference between Groups 1 and 2 in pelvic pain, headache, or mood scores, and no significant difference in headache or mood scores between the baseline and continuous phases of the trial. Pelvic pain scores were lower during the extended phase, however—0.18 vs 0.32 on a scale of 0 to 10.
A high continuation rate. After the 6-month extended phase, 57 of the 65 remaining participants chose to continue using the ring for contraception, on a continuous dosing basis—a continuation rate of 88%. But more than half of the women who chose to stick with the ring (57%) decided not to take advantage of the 4-day hormone-free interval to manage breakthrough bleeding or spotting, regardless of original group assignment.
WHAT’S NEW?: The ring moves further mainstream
Continuous or extended use of the transvaginal ring may be a new idea for many patients—and physicians. But the idea may catch on in light of this study’s findings. Given the high rate of unwanted pregnancy in the United States, many women may benefit from a contraceptive that is as safe and effective as an OC but doesn’t involve a daily pill.
CAVEATS: Side effects, off-label concerns
In 2005, Oddsson et al found that women who used the ring reported more vaginitis and more leukorrhea than women who used OCs; conversely, they reported less nausea and less acne. Other side effects that are common to hormonal contraceptives, such as headache and weight gain, occurred at similar rates among women using the ring and OCs.6
However, the high proportion of patients who elected to keep using the ring at the end of the study by Sulak et al suggests that its side effects are acceptable.1 As with all contraception, however, patient preference is a key consideration. The study population was highly motivated, particularly since women who had difficulty with this means of contraception dropped out after the baseline phase of the trial.
Off-label use. Pharmacokinetic research involving the contraceptive ring has shown that hormone levels required to protect against pregnancy persist for at least 35 days after it is placed in the vagina.8 The manufacturer has data only to confirm contraceptive efficacy for up to 28 days and therefore does not recommend use beyond 4 weeks.4
This study highlights another off-label issue: Women in Group 2, who were allowed to remove the ring for 4 day-intervals to decrease breakthrough bleeding, were instructed to reinsert the same ring after 4 days and keep it in place until the next scheduled replacement date. But the manufacturer does not recommend reinsertion of a ring that has been out of the body for more than 3 hours. In my practice (KR), women are generally unwilling to store and replace a ring, preferring to place a new one after removal for more than a few hours.
Should she try continuous use?
Changing the ring on the same date each month may boost adherence for some women. Funding. The research was funded by an unrestricted educational grant from Organon, Inc, the manufacturer of NuvaRing, which included salary support for 5 of the 6 authors. The published study gives no additional information about the involvement of the pharmaceutical company.
Contraindications, drug interactions. As with other combined hormonal contraceptives, women who have a history of venous thromboembolism, headaches with focal neurological symptoms, severe hypertension, breast or endometrial cancer, or liver disease, and smokers older than 35 years should not use the contraceptive ring.4 In addition, women need to be aware that a number of medications—griseofulvin, rifampin, phenytoin, carbamazepine, and herbal products containing St. John’s Wort, among others—may reduce the effectiveness of the contraceptive ring.4
CHALLENGES TO IMPLEMENTATION: Going off-label isn’t for everyone
When it comes to choosing a contraceptive method, patient preference is paramount. Some women may not be comfortable inserting or removing the ring and should be counseled on other forms of contraception. Women who prefer to bleed every month should not use extended cycling. Similarly, some physicians may not be comfortable recommending an off-label use of the ring.
Those who are comfortable making the recommendation should be prepared to educate patients about this method of contraception and to discuss the benefits of extended or continuous use of the ring. For some women, the memory-triggering mechanism of changing the ring on the same date each month may boost adherence. For others, replacing the ring every 28 days may be acceptable—again, depending on patient preference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURLs) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring: a randomized controlled trial. Obstet Gynecol. 2008;112:563-571.
2. Frost JJ, Singh S, Finer LB. US women’s one-year contraceptive use patterns, 2004. Perspect Sex Reprod Health. 2007;39:48-55.
3. Miller L, Verhoeven C, Hout J. Extended regimens of the contraceptive vaginal ring: a randomized trial. Obstet Gynecol. 2005;106:473-482.
4. NuvaRing (etonogestrel/ethinyl estradiol vaginal ring) [prescribing information]. Roseland, NJ: Organon USA Inc; June 2008. Available at: http://www.spfiles.com/pinuvaring.pdf. Accessed March 10, 2009.
5. Schafer JE, Osborne LM, Davis AR, et al. Acceptability and satisfaction using Quick Start with the contraceptive vaginal ring versus an oral contraceptive. Contraception. 2006;73:488-492.
6. Oddsson K, Leifels-Fischer B, de Melo NR, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1-year randomized trial. Contraception. 2005;71:176-182.
7. Wilks JF. Hormonal birth control and pregnancy: a comparative analysis of thromboembolic risk. Ann Pharmacother. 2003;37:912-916.
8. Timmer C, Mulders T. Pharmacokinetics of etonogestrel and ethinylestradiol released from a combined contraceptive vaginal ring. Clin Pharmacokinet. 2000;39:233-242.
Recommend continuous or extended use of the transvaginal contraceptive ring to women who want fewer days of menstrual bleeding and have trouble remembering to, or prefer not to, take a daily pill. If breakthrough bleeding is troublesome, suggest a 4-day ring-free interval.1
Strength of recommendation
B: Based on a single randomized controlled trial (RCT) with <80% follow up.
Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring: a randomized controlled trial. Obstet Gynecol. 2008;112:563-571.
ILLUSTRATIVE CASE
Case 1: A healthy 25-year-old woman comes to see you because she’s worried about getting pregnant. She’s been on an extended-cycle oral contraceptive (OC) for several months and is happy to have her period only once every 3 months, but she frequently forgets to take her pill.
What can you offer that will give her the benefits of an extended-cycle OC, without the risk of pregnancy she incurs each time she misses a pill?
Case 2: You started a healthy 18-year-old on the transvaginal ring 6 months ago. After counseling, she opted for continuous cycling, so she inserts a new ring right after she removes the old one, on the same date each month. Although she likes the ring, she’s disturbed by a recent increase in breakthrough bleeding. What can you recommend to decrease the bleeding?
Clinicians have long known that the traditional 21/7 OC cycle is not necessary for safety or efficacy. More recently, many women have been happy to learn that there is no physiologic reason to have a monthly period when they’re using combination hormonal contraception. They’re also happy to discover that fewer periods often mean fewer premenstrual mood swings, episodes of painful cramping, and instances of other troublesome symptoms.
The transvaginal ring is often overlooked
The US Food and Drug Administration (FDA) has approved 2 combination OCs for extended-cycle use and 1 for continuous use. But any monophasic OC can be used off-label for extended or continuous cycling to decrease bleeding frequency. So, too, can the transvaginal contraceptive ring (NuvaRing), an infrequently used contraceptive. (According to 1 study, just 5.7% of US women using contraception used either the ring or the patch.2 ) The ring has been studied for extended use,3 but does not have FDA approval for longer-term regimens.
NuvaRing is a flexible, transparent device that contains the progestin etonogestrel and ethinyl estradiol. The manufacturer recommends a 21/7 cycle, inserting the ring in the vagina and leaving it in place for 3 weeks, removing it for 1 week, and then inserting a new ring.4 The ring is well suited to women who have no contraindications to hormonal contraception but have difficulty remembering to take a pill every day—or simply prefer the convenience of less frequent dosing.
While the ring has been found to be effective and tolerable when used without a hormone-free interval—28-, 49-, 91- and 364-day dosing has been studied—breakthrough bleeding or spotting is a frequent side effect of extended-cycle hormonal contraception. In 1 study, 43% of women on a 49-day ring cycle experienced breakthrough bleeding, compared with 16% of those on a 28-day cycle.3
High satisfaction, low risk
Nonetheless, women who use the transvaginal ring often report high satisfaction. One study found that 61% of women were very satisfied with this method of contraception, compared with 34% of triphasic OC users (P<.003).5 The risk of pregnancy (1-2 pregnancies per 100 women-years of use, according to the manufacturer4 ) and the risk of venous thromboembolism (10-30 in 100,000 vs 4-11 in 100,000 nonpregnant women who are not using hormonal contraception) are comparable to that of women using OCs.6,7 The risk of other severe side effects associated with the vaginal ring is comparable to that of OCs, as well.
STUDY SUMMARY: An effective option that women used post-trial
This RCT recruited women between the ages of 18 and 45 years who had been using combination hormonal contraceptives—OCs, the transdermal patch, or the transvaginal ring. All had been on a 21/7 cycle for at least 2 months. Exclusion criteria included a body mass index ≥38 kg/m2, smoking >10 cigarettes per day, use of other estrogen- or phytoestrogen-containing products, and the presence of ovarian cysts >2.5 cm or endometrial thickness >8 mm. Women who wanted to get pregnant within a year were also excluded.
The study began with a baseline phase during which participants completed one 21/7 cycle with the ring for those using the ring prior to the study or two 21/7 cycles for those using the pill or patch prior to the study. Daily flow was assessed during this initial phase, using a scale of 0 to 4, with 4 being the heaviest. Women who completed this phase and wanted to continue using the ring (N=74) were then randomized into 2 groups (n=37) for the 6-month extended phase.
Group 1 was assigned to use the contraceptive ring with no hormone-free days. Participants were instructed to replace the rings monthly, on the same calendar day of the month. Group 2 also used the ring on a continuous basis with monthly replacement, but those who experienced breakthrough bleeding for more than 5 days were permitted to remove the ring for 4 days. Women in both groups kept a daily diary of ring usage, degree of menstrual flow, and symptomatology, including pelvic pain, headaches, and mood.
Most subjects were white (76%), nonsmokers (84%), and unmarried (68% in Group 1 and 57% in Group 2), with an average age of 28 to 29 years. Eight patients (22%) in Group 1 withdrew from the study prior to completing the 6-month extended phase, 4 of them because of side effects. Only 1 woman withdrew from Group 2, because of plans for pregnancy. No one became pregnant while using the ring.
Hormone-free interval reduced bleeding. In Group 1, the average daily flow score was slightly reduced with continuous use (from 0.33 during the 21/7 baseline phase to 0.21 in the 6-month extended phase), but researchers reported no significant difference in flow-free days. On average, 85% of the days were flow-free in the 21/7 phase, vs 89% in the extended phase.
In Group 2, flow-free days increased, from 83% in the baseline phase to 95% in the extended phase, and average flow scores fell from 0.38 to 0.17.
Overall, the 65 participants who completed 6 months of continuous ring use had fewer bleeding days per month—1.8 days, on average, vs 3.3 days during the initial 21/7 phase, but more days of spotting per month (2.5 vs 1.8 days). There was no difference between Groups 1 and 2 in pelvic pain, headache, or mood scores, and no significant difference in headache or mood scores between the baseline and continuous phases of the trial. Pelvic pain scores were lower during the extended phase, however—0.18 vs 0.32 on a scale of 0 to 10.
A high continuation rate. After the 6-month extended phase, 57 of the 65 remaining participants chose to continue using the ring for contraception, on a continuous dosing basis—a continuation rate of 88%. But more than half of the women who chose to stick with the ring (57%) decided not to take advantage of the 4-day hormone-free interval to manage breakthrough bleeding or spotting, regardless of original group assignment.
WHAT’S NEW?: The ring moves further mainstream
Continuous or extended use of the transvaginal ring may be a new idea for many patients—and physicians. But the idea may catch on in light of this study’s findings. Given the high rate of unwanted pregnancy in the United States, many women may benefit from a contraceptive that is as safe and effective as an OC but doesn’t involve a daily pill.
CAVEATS: Side effects, off-label concerns
In 2005, Oddsson et al found that women who used the ring reported more vaginitis and more leukorrhea than women who used OCs; conversely, they reported less nausea and less acne. Other side effects that are common to hormonal contraceptives, such as headache and weight gain, occurred at similar rates among women using the ring and OCs.6
However, the high proportion of patients who elected to keep using the ring at the end of the study by Sulak et al suggests that its side effects are acceptable.1 As with all contraception, however, patient preference is a key consideration. The study population was highly motivated, particularly since women who had difficulty with this means of contraception dropped out after the baseline phase of the trial.
Off-label use. Pharmacokinetic research involving the contraceptive ring has shown that hormone levels required to protect against pregnancy persist for at least 35 days after it is placed in the vagina.8 The manufacturer has data only to confirm contraceptive efficacy for up to 28 days and therefore does not recommend use beyond 4 weeks.4
This study highlights another off-label issue: Women in Group 2, who were allowed to remove the ring for 4 day-intervals to decrease breakthrough bleeding, were instructed to reinsert the same ring after 4 days and keep it in place until the next scheduled replacement date. But the manufacturer does not recommend reinsertion of a ring that has been out of the body for more than 3 hours. In my practice (KR), women are generally unwilling to store and replace a ring, preferring to place a new one after removal for more than a few hours.
Should she try continuous use?
Changing the ring on the same date each month may boost adherence for some women. Funding. The research was funded by an unrestricted educational grant from Organon, Inc, the manufacturer of NuvaRing, which included salary support for 5 of the 6 authors. The published study gives no additional information about the involvement of the pharmaceutical company.
Contraindications, drug interactions. As with other combined hormonal contraceptives, women who have a history of venous thromboembolism, headaches with focal neurological symptoms, severe hypertension, breast or endometrial cancer, or liver disease, and smokers older than 35 years should not use the contraceptive ring.4 In addition, women need to be aware that a number of medications—griseofulvin, rifampin, phenytoin, carbamazepine, and herbal products containing St. John’s Wort, among others—may reduce the effectiveness of the contraceptive ring.4
CHALLENGES TO IMPLEMENTATION: Going off-label isn’t for everyone
When it comes to choosing a contraceptive method, patient preference is paramount. Some women may not be comfortable inserting or removing the ring and should be counseled on other forms of contraception. Women who prefer to bleed every month should not use extended cycling. Similarly, some physicians may not be comfortable recommending an off-label use of the ring.
Those who are comfortable making the recommendation should be prepared to educate patients about this method of contraception and to discuss the benefits of extended or continuous use of the ring. For some women, the memory-triggering mechanism of changing the ring on the same date each month may boost adherence. For others, replacing the ring every 28 days may be acceptable—again, depending on patient preference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURLs) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Recommend continuous or extended use of the transvaginal contraceptive ring to women who want fewer days of menstrual bleeding and have trouble remembering to, or prefer not to, take a daily pill. If breakthrough bleeding is troublesome, suggest a 4-day ring-free interval.1
Strength of recommendation
B: Based on a single randomized controlled trial (RCT) with <80% follow up.
Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring: a randomized controlled trial. Obstet Gynecol. 2008;112:563-571.
ILLUSTRATIVE CASE
Case 1: A healthy 25-year-old woman comes to see you because she’s worried about getting pregnant. She’s been on an extended-cycle oral contraceptive (OC) for several months and is happy to have her period only once every 3 months, but she frequently forgets to take her pill.
What can you offer that will give her the benefits of an extended-cycle OC, without the risk of pregnancy she incurs each time she misses a pill?
Case 2: You started a healthy 18-year-old on the transvaginal ring 6 months ago. After counseling, she opted for continuous cycling, so she inserts a new ring right after she removes the old one, on the same date each month. Although she likes the ring, she’s disturbed by a recent increase in breakthrough bleeding. What can you recommend to decrease the bleeding?
Clinicians have long known that the traditional 21/7 OC cycle is not necessary for safety or efficacy. More recently, many women have been happy to learn that there is no physiologic reason to have a monthly period when they’re using combination hormonal contraception. They’re also happy to discover that fewer periods often mean fewer premenstrual mood swings, episodes of painful cramping, and instances of other troublesome symptoms.
The transvaginal ring is often overlooked
The US Food and Drug Administration (FDA) has approved 2 combination OCs for extended-cycle use and 1 for continuous use. But any monophasic OC can be used off-label for extended or continuous cycling to decrease bleeding frequency. So, too, can the transvaginal contraceptive ring (NuvaRing), an infrequently used contraceptive. (According to 1 study, just 5.7% of US women using contraception used either the ring or the patch.2 ) The ring has been studied for extended use,3 but does not have FDA approval for longer-term regimens.
NuvaRing is a flexible, transparent device that contains the progestin etonogestrel and ethinyl estradiol. The manufacturer recommends a 21/7 cycle, inserting the ring in the vagina and leaving it in place for 3 weeks, removing it for 1 week, and then inserting a new ring.4 The ring is well suited to women who have no contraindications to hormonal contraception but have difficulty remembering to take a pill every day—or simply prefer the convenience of less frequent dosing.
While the ring has been found to be effective and tolerable when used without a hormone-free interval—28-, 49-, 91- and 364-day dosing has been studied—breakthrough bleeding or spotting is a frequent side effect of extended-cycle hormonal contraception. In 1 study, 43% of women on a 49-day ring cycle experienced breakthrough bleeding, compared with 16% of those on a 28-day cycle.3
High satisfaction, low risk
Nonetheless, women who use the transvaginal ring often report high satisfaction. One study found that 61% of women were very satisfied with this method of contraception, compared with 34% of triphasic OC users (P<.003).5 The risk of pregnancy (1-2 pregnancies per 100 women-years of use, according to the manufacturer4 ) and the risk of venous thromboembolism (10-30 in 100,000 vs 4-11 in 100,000 nonpregnant women who are not using hormonal contraception) are comparable to that of women using OCs.6,7 The risk of other severe side effects associated with the vaginal ring is comparable to that of OCs, as well.
STUDY SUMMARY: An effective option that women used post-trial
This RCT recruited women between the ages of 18 and 45 years who had been using combination hormonal contraceptives—OCs, the transdermal patch, or the transvaginal ring. All had been on a 21/7 cycle for at least 2 months. Exclusion criteria included a body mass index ≥38 kg/m2, smoking >10 cigarettes per day, use of other estrogen- or phytoestrogen-containing products, and the presence of ovarian cysts >2.5 cm or endometrial thickness >8 mm. Women who wanted to get pregnant within a year were also excluded.
The study began with a baseline phase during which participants completed one 21/7 cycle with the ring for those using the ring prior to the study or two 21/7 cycles for those using the pill or patch prior to the study. Daily flow was assessed during this initial phase, using a scale of 0 to 4, with 4 being the heaviest. Women who completed this phase and wanted to continue using the ring (N=74) were then randomized into 2 groups (n=37) for the 6-month extended phase.
Group 1 was assigned to use the contraceptive ring with no hormone-free days. Participants were instructed to replace the rings monthly, on the same calendar day of the month. Group 2 also used the ring on a continuous basis with monthly replacement, but those who experienced breakthrough bleeding for more than 5 days were permitted to remove the ring for 4 days. Women in both groups kept a daily diary of ring usage, degree of menstrual flow, and symptomatology, including pelvic pain, headaches, and mood.
Most subjects were white (76%), nonsmokers (84%), and unmarried (68% in Group 1 and 57% in Group 2), with an average age of 28 to 29 years. Eight patients (22%) in Group 1 withdrew from the study prior to completing the 6-month extended phase, 4 of them because of side effects. Only 1 woman withdrew from Group 2, because of plans for pregnancy. No one became pregnant while using the ring.
Hormone-free interval reduced bleeding. In Group 1, the average daily flow score was slightly reduced with continuous use (from 0.33 during the 21/7 baseline phase to 0.21 in the 6-month extended phase), but researchers reported no significant difference in flow-free days. On average, 85% of the days were flow-free in the 21/7 phase, vs 89% in the extended phase.
In Group 2, flow-free days increased, from 83% in the baseline phase to 95% in the extended phase, and average flow scores fell from 0.38 to 0.17.
Overall, the 65 participants who completed 6 months of continuous ring use had fewer bleeding days per month—1.8 days, on average, vs 3.3 days during the initial 21/7 phase, but more days of spotting per month (2.5 vs 1.8 days). There was no difference between Groups 1 and 2 in pelvic pain, headache, or mood scores, and no significant difference in headache or mood scores between the baseline and continuous phases of the trial. Pelvic pain scores were lower during the extended phase, however—0.18 vs 0.32 on a scale of 0 to 10.
A high continuation rate. After the 6-month extended phase, 57 of the 65 remaining participants chose to continue using the ring for contraception, on a continuous dosing basis—a continuation rate of 88%. But more than half of the women who chose to stick with the ring (57%) decided not to take advantage of the 4-day hormone-free interval to manage breakthrough bleeding or spotting, regardless of original group assignment.
WHAT’S NEW?: The ring moves further mainstream
Continuous or extended use of the transvaginal ring may be a new idea for many patients—and physicians. But the idea may catch on in light of this study’s findings. Given the high rate of unwanted pregnancy in the United States, many women may benefit from a contraceptive that is as safe and effective as an OC but doesn’t involve a daily pill.
CAVEATS: Side effects, off-label concerns
In 2005, Oddsson et al found that women who used the ring reported more vaginitis and more leukorrhea than women who used OCs; conversely, they reported less nausea and less acne. Other side effects that are common to hormonal contraceptives, such as headache and weight gain, occurred at similar rates among women using the ring and OCs.6
However, the high proportion of patients who elected to keep using the ring at the end of the study by Sulak et al suggests that its side effects are acceptable.1 As with all contraception, however, patient preference is a key consideration. The study population was highly motivated, particularly since women who had difficulty with this means of contraception dropped out after the baseline phase of the trial.
Off-label use. Pharmacokinetic research involving the contraceptive ring has shown that hormone levels required to protect against pregnancy persist for at least 35 days after it is placed in the vagina.8 The manufacturer has data only to confirm contraceptive efficacy for up to 28 days and therefore does not recommend use beyond 4 weeks.4
This study highlights another off-label issue: Women in Group 2, who were allowed to remove the ring for 4 day-intervals to decrease breakthrough bleeding, were instructed to reinsert the same ring after 4 days and keep it in place until the next scheduled replacement date. But the manufacturer does not recommend reinsertion of a ring that has been out of the body for more than 3 hours. In my practice (KR), women are generally unwilling to store and replace a ring, preferring to place a new one after removal for more than a few hours.
Should she try continuous use?
Changing the ring on the same date each month may boost adherence for some women. Funding. The research was funded by an unrestricted educational grant from Organon, Inc, the manufacturer of NuvaRing, which included salary support for 5 of the 6 authors. The published study gives no additional information about the involvement of the pharmaceutical company.
Contraindications, drug interactions. As with other combined hormonal contraceptives, women who have a history of venous thromboembolism, headaches with focal neurological symptoms, severe hypertension, breast or endometrial cancer, or liver disease, and smokers older than 35 years should not use the contraceptive ring.4 In addition, women need to be aware that a number of medications—griseofulvin, rifampin, phenytoin, carbamazepine, and herbal products containing St. John’s Wort, among others—may reduce the effectiveness of the contraceptive ring.4
CHALLENGES TO IMPLEMENTATION: Going off-label isn’t for everyone
When it comes to choosing a contraceptive method, patient preference is paramount. Some women may not be comfortable inserting or removing the ring and should be counseled on other forms of contraception. Women who prefer to bleed every month should not use extended cycling. Similarly, some physicians may not be comfortable recommending an off-label use of the ring.
Those who are comfortable making the recommendation should be prepared to educate patients about this method of contraception and to discuss the benefits of extended or continuous use of the ring. For some women, the memory-triggering mechanism of changing the ring on the same date each month may boost adherence. For others, replacing the ring every 28 days may be acceptable—again, depending on patient preference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURLs) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring: a randomized controlled trial. Obstet Gynecol. 2008;112:563-571.
2. Frost JJ, Singh S, Finer LB. US women’s one-year contraceptive use patterns, 2004. Perspect Sex Reprod Health. 2007;39:48-55.
3. Miller L, Verhoeven C, Hout J. Extended regimens of the contraceptive vaginal ring: a randomized trial. Obstet Gynecol. 2005;106:473-482.
4. NuvaRing (etonogestrel/ethinyl estradiol vaginal ring) [prescribing information]. Roseland, NJ: Organon USA Inc; June 2008. Available at: http://www.spfiles.com/pinuvaring.pdf. Accessed March 10, 2009.
5. Schafer JE, Osborne LM, Davis AR, et al. Acceptability and satisfaction using Quick Start with the contraceptive vaginal ring versus an oral contraceptive. Contraception. 2006;73:488-492.
6. Oddsson K, Leifels-Fischer B, de Melo NR, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1-year randomized trial. Contraception. 2005;71:176-182.
7. Wilks JF. Hormonal birth control and pregnancy: a comparative analysis of thromboembolic risk. Ann Pharmacother. 2003;37:912-916.
8. Timmer C, Mulders T. Pharmacokinetics of etonogestrel and ethinylestradiol released from a combined contraceptive vaginal ring. Clin Pharmacokinet. 2000;39:233-242.
1. Sulak PJ, Smith V, Coffee A, et al. Frequency and management of breakthrough bleeding with continuous use of the transvaginal contraceptive ring: a randomized controlled trial. Obstet Gynecol. 2008;112:563-571.
2. Frost JJ, Singh S, Finer LB. US women’s one-year contraceptive use patterns, 2004. Perspect Sex Reprod Health. 2007;39:48-55.
3. Miller L, Verhoeven C, Hout J. Extended regimens of the contraceptive vaginal ring: a randomized trial. Obstet Gynecol. 2005;106:473-482.
4. NuvaRing (etonogestrel/ethinyl estradiol vaginal ring) [prescribing information]. Roseland, NJ: Organon USA Inc; June 2008. Available at: http://www.spfiles.com/pinuvaring.pdf. Accessed March 10, 2009.
5. Schafer JE, Osborne LM, Davis AR, et al. Acceptability and satisfaction using Quick Start with the contraceptive vaginal ring versus an oral contraceptive. Contraception. 2006;73:488-492.
6. Oddsson K, Leifels-Fischer B, de Melo NR, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1-year randomized trial. Contraception. 2005;71:176-182.
7. Wilks JF. Hormonal birth control and pregnancy: a comparative analysis of thromboembolic risk. Ann Pharmacother. 2003;37:912-916.
8. Timmer C, Mulders T. Pharmacokinetics of etonogestrel and ethinylestradiol released from a combined contraceptive vaginal ring. Clin Pharmacokinet. 2000;39:233-242.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
Arthroscopic surgery for knee osteoarthritis? Just say no
ILLUSTRATIVE CASE
A 52-year-old man comes to your office complaining of ongoing knee pain—pain that he knows is related to his osteoarthritis (OA). The patient does not want a total knee replacement, and it’s unlikely that his arthritis is extensive enough to warrant it. You wonder whether he’s a potential candidate for arthroscopic knee surgery and if the lavage and articular cartilage debridement the procedure entails would alleviate his symptoms.
Knee pain related to OA is a common complaint in the office setting, and primary care physicians use many medical and physical interventions to manage the symptoms. If these fall short in patients with more advanced disease, however, physicians often recommend an orthopedic surgery consult to consider surgical management.
Lavage and debridement: The (questionable) effects
Arthroscopic knee surgery involves lavage (to remove particulate material, such as cartilage fragments) and debridement (to smooth the articular surfaces). Theoretically, this widely used surgery reduces synovitis and improves joint motion, resulting in a decrease in pain and an improvement in function. But what does the latest research tell us?
A randomized controlled trial (RCT) by Moseley et al in 2002 found arthroscopic knee surgery to be of no benefit for moderate to severe OA.2 Because this finding was so contrary to current practice, the authors’ conclusion was not widely accepted. Arthroscopic surgery continued to be used for moderately severe knee arthritis.3 Indeed, the 2008 guidelines from the American Academy of Orthopaedic Surgeons (AAOS) state that “arthroscopic partial meniscectomy or loose body removal is an option in patients with symptomatic OA of the knee who also have primary signs and symptoms of a torn meniscus and/or a loose body.”4
However, these guidelines do not include the evidence from the study by Kirkley et al1 detailed below.
STUDY SUMMARY: New RCT echoes earlier conclusion
Kirkley et al conducted a nonblinded RCT of 188 patients with moderate to severe OA of the knee; those with large meniscal tears, malalignment, previous arthroscopic surgery, or severe bicompartmental arthritis were excluded.
The control group received optimal medical and physical therapy, consisting of 1 hour of physical therapy a week, twice-daily exercises, and stepwise use of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and intraarticular hyaluronic acid injections. The intervention group had arthroscopic surgery (debridement of articular cartilage and menisci, excision of osteophytes, and removal of loose bodies), and received medical and physical therapy.
The primary outcome measure was the validated Western Ontario and McMaster Universities Arthritis Index (WOMAC) score. (The range is 0 to 2400, with higher scores indicating more severe symptoms.)
After 2 years, the researchers found minimal difference in the WOMAC scores of the control group (897±583) and the surgery group (874±624); the absolute difference was –23±605 (95% confidence interval, –208 to 161; P=.22). There was no difference in the secondary outcomes of quality of life, pain, and function. Nor did surgery provide any benefit to the subgroup of patients with mechanical symptoms.1
These findings echoed those of Moseley et al’s 2002 single-blinded RCT, in which researchers assigned 180 patients to arthroscopic surgery or sham surgery, and found surgery to be of no benefit.2 That study was criticized because of its methodology; the researchers used an outcome measure that was not validated and failed to exclude patients with more advanced disease and malalignment, who might be expected to have a poor response to surgery. The 2008 study by Kirkley et al had no such methodological flaws and, in retrospect, it appears that these perceived flaws did not account for the negative findings of the 2002 study.
WHAT’S NEW?: No room for doubt
Evidence from the new RCT confirms the findings of the 2002 trial. It clearly shows that arthroscopic surgery for knee OA is not beneficial, even in patients with mechanical symptoms. Kirkley’s study avoided the criticism of the earlier study by using a validated outcome measure, excluding patients with malalignment, and performing a subgroup analysis of patients with mechanical symptoms. We now have 2 studies that show no benefit from arthroscopic knee surgery in patients with OA, whether or not they have mechanical problems.
So what can you do for patients with moderate to severe knee pain from osteoarthritis? Offer them medical and physical therapy (TABLE) and the assurance that there is nothing to be gained from arthroscopic surgery.
TABLE
How to treat knee OA without surgery
|
CAVEATS: Large meniscal tears: An exception to the rule
These findings do not necessarily apply to patients with evidence of large meniscal tears. This subset of knee OA patients may benefit from surgical management.
CHALLENGES TO IMPLEMENTATION: What to say to patients seeking a referral
Patients may have read about arthroscopic knee surgery or know someone who underwent the procedure and come to you asking for a referral to an orthopedic surgeon. In such a case, we suggest a straightforward approach.
Discuss arthroscopic surgery’s proven lack of benefit and offer equally effective conservative therapies. For patients who may be eligible for a total knee replacement, a referral to an orthopedic surgeon for evaluation is appropriate.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097-1107.
2. Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
3. Hawker G, Guan J, Judge A, et al. Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am. 2008;90:2337-2345.
4. American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (non-arthroplasty): full guideline. December 6, 2008. Available at: http://www.aaos.org/Research/guidelines/GuidelineOAKnee.asp. Accessed February 16, 2009.
5. Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2005;(1):CD002946.-
6. Michel BA, Stucki G, Frey D, et al. Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Arthritis Rheum. 2005;52:779-786.
7. Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006;354:795-808.
8. Arroll B, Goodyear-Smith F. Corticosteroid injections for osteoarthritis of the knee: meta-analysis. BMJ. 2004;328:869-870.
9. Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol. 2001;28:156-164.
10. Berman BM, Lao L, Langenberg P, et al. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141:901-910.
ILLUSTRATIVE CASE
A 52-year-old man comes to your office complaining of ongoing knee pain—pain that he knows is related to his osteoarthritis (OA). The patient does not want a total knee replacement, and it’s unlikely that his arthritis is extensive enough to warrant it. You wonder whether he’s a potential candidate for arthroscopic knee surgery and if the lavage and articular cartilage debridement the procedure entails would alleviate his symptoms.
Knee pain related to OA is a common complaint in the office setting, and primary care physicians use many medical and physical interventions to manage the symptoms. If these fall short in patients with more advanced disease, however, physicians often recommend an orthopedic surgery consult to consider surgical management.
Lavage and debridement: The (questionable) effects
Arthroscopic knee surgery involves lavage (to remove particulate material, such as cartilage fragments) and debridement (to smooth the articular surfaces). Theoretically, this widely used surgery reduces synovitis and improves joint motion, resulting in a decrease in pain and an improvement in function. But what does the latest research tell us?
A randomized controlled trial (RCT) by Moseley et al in 2002 found arthroscopic knee surgery to be of no benefit for moderate to severe OA.2 Because this finding was so contrary to current practice, the authors’ conclusion was not widely accepted. Arthroscopic surgery continued to be used for moderately severe knee arthritis.3 Indeed, the 2008 guidelines from the American Academy of Orthopaedic Surgeons (AAOS) state that “arthroscopic partial meniscectomy or loose body removal is an option in patients with symptomatic OA of the knee who also have primary signs and symptoms of a torn meniscus and/or a loose body.”4
However, these guidelines do not include the evidence from the study by Kirkley et al1 detailed below.
STUDY SUMMARY: New RCT echoes earlier conclusion
Kirkley et al conducted a nonblinded RCT of 188 patients with moderate to severe OA of the knee; those with large meniscal tears, malalignment, previous arthroscopic surgery, or severe bicompartmental arthritis were excluded.
The control group received optimal medical and physical therapy, consisting of 1 hour of physical therapy a week, twice-daily exercises, and stepwise use of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and intraarticular hyaluronic acid injections. The intervention group had arthroscopic surgery (debridement of articular cartilage and menisci, excision of osteophytes, and removal of loose bodies), and received medical and physical therapy.
The primary outcome measure was the validated Western Ontario and McMaster Universities Arthritis Index (WOMAC) score. (The range is 0 to 2400, with higher scores indicating more severe symptoms.)
After 2 years, the researchers found minimal difference in the WOMAC scores of the control group (897±583) and the surgery group (874±624); the absolute difference was –23±605 (95% confidence interval, –208 to 161; P=.22). There was no difference in the secondary outcomes of quality of life, pain, and function. Nor did surgery provide any benefit to the subgroup of patients with mechanical symptoms.1
These findings echoed those of Moseley et al’s 2002 single-blinded RCT, in which researchers assigned 180 patients to arthroscopic surgery or sham surgery, and found surgery to be of no benefit.2 That study was criticized because of its methodology; the researchers used an outcome measure that was not validated and failed to exclude patients with more advanced disease and malalignment, who might be expected to have a poor response to surgery. The 2008 study by Kirkley et al had no such methodological flaws and, in retrospect, it appears that these perceived flaws did not account for the negative findings of the 2002 study.
WHAT’S NEW?: No room for doubt
Evidence from the new RCT confirms the findings of the 2002 trial. It clearly shows that arthroscopic surgery for knee OA is not beneficial, even in patients with mechanical symptoms. Kirkley’s study avoided the criticism of the earlier study by using a validated outcome measure, excluding patients with malalignment, and performing a subgroup analysis of patients with mechanical symptoms. We now have 2 studies that show no benefit from arthroscopic knee surgery in patients with OA, whether or not they have mechanical problems.
So what can you do for patients with moderate to severe knee pain from osteoarthritis? Offer them medical and physical therapy (TABLE) and the assurance that there is nothing to be gained from arthroscopic surgery.
TABLE
How to treat knee OA without surgery
|
CAVEATS: Large meniscal tears: An exception to the rule
These findings do not necessarily apply to patients with evidence of large meniscal tears. This subset of knee OA patients may benefit from surgical management.
CHALLENGES TO IMPLEMENTATION: What to say to patients seeking a referral
Patients may have read about arthroscopic knee surgery or know someone who underwent the procedure and come to you asking for a referral to an orthopedic surgeon. In such a case, we suggest a straightforward approach.
Discuss arthroscopic surgery’s proven lack of benefit and offer equally effective conservative therapies. For patients who may be eligible for a total knee replacement, a referral to an orthopedic surgeon for evaluation is appropriate.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
ILLUSTRATIVE CASE
A 52-year-old man comes to your office complaining of ongoing knee pain—pain that he knows is related to his osteoarthritis (OA). The patient does not want a total knee replacement, and it’s unlikely that his arthritis is extensive enough to warrant it. You wonder whether he’s a potential candidate for arthroscopic knee surgery and if the lavage and articular cartilage debridement the procedure entails would alleviate his symptoms.
Knee pain related to OA is a common complaint in the office setting, and primary care physicians use many medical and physical interventions to manage the symptoms. If these fall short in patients with more advanced disease, however, physicians often recommend an orthopedic surgery consult to consider surgical management.
Lavage and debridement: The (questionable) effects
Arthroscopic knee surgery involves lavage (to remove particulate material, such as cartilage fragments) and debridement (to smooth the articular surfaces). Theoretically, this widely used surgery reduces synovitis and improves joint motion, resulting in a decrease in pain and an improvement in function. But what does the latest research tell us?
A randomized controlled trial (RCT) by Moseley et al in 2002 found arthroscopic knee surgery to be of no benefit for moderate to severe OA.2 Because this finding was so contrary to current practice, the authors’ conclusion was not widely accepted. Arthroscopic surgery continued to be used for moderately severe knee arthritis.3 Indeed, the 2008 guidelines from the American Academy of Orthopaedic Surgeons (AAOS) state that “arthroscopic partial meniscectomy or loose body removal is an option in patients with symptomatic OA of the knee who also have primary signs and symptoms of a torn meniscus and/or a loose body.”4
However, these guidelines do not include the evidence from the study by Kirkley et al1 detailed below.
STUDY SUMMARY: New RCT echoes earlier conclusion
Kirkley et al conducted a nonblinded RCT of 188 patients with moderate to severe OA of the knee; those with large meniscal tears, malalignment, previous arthroscopic surgery, or severe bicompartmental arthritis were excluded.
The control group received optimal medical and physical therapy, consisting of 1 hour of physical therapy a week, twice-daily exercises, and stepwise use of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and intraarticular hyaluronic acid injections. The intervention group had arthroscopic surgery (debridement of articular cartilage and menisci, excision of osteophytes, and removal of loose bodies), and received medical and physical therapy.
The primary outcome measure was the validated Western Ontario and McMaster Universities Arthritis Index (WOMAC) score. (The range is 0 to 2400, with higher scores indicating more severe symptoms.)
After 2 years, the researchers found minimal difference in the WOMAC scores of the control group (897±583) and the surgery group (874±624); the absolute difference was –23±605 (95% confidence interval, –208 to 161; P=.22). There was no difference in the secondary outcomes of quality of life, pain, and function. Nor did surgery provide any benefit to the subgroup of patients with mechanical symptoms.1
These findings echoed those of Moseley et al’s 2002 single-blinded RCT, in which researchers assigned 180 patients to arthroscopic surgery or sham surgery, and found surgery to be of no benefit.2 That study was criticized because of its methodology; the researchers used an outcome measure that was not validated and failed to exclude patients with more advanced disease and malalignment, who might be expected to have a poor response to surgery. The 2008 study by Kirkley et al had no such methodological flaws and, in retrospect, it appears that these perceived flaws did not account for the negative findings of the 2002 study.
WHAT’S NEW?: No room for doubt
Evidence from the new RCT confirms the findings of the 2002 trial. It clearly shows that arthroscopic surgery for knee OA is not beneficial, even in patients with mechanical symptoms. Kirkley’s study avoided the criticism of the earlier study by using a validated outcome measure, excluding patients with malalignment, and performing a subgroup analysis of patients with mechanical symptoms. We now have 2 studies that show no benefit from arthroscopic knee surgery in patients with OA, whether or not they have mechanical problems.
So what can you do for patients with moderate to severe knee pain from osteoarthritis? Offer them medical and physical therapy (TABLE) and the assurance that there is nothing to be gained from arthroscopic surgery.
TABLE
How to treat knee OA without surgery
|
CAVEATS: Large meniscal tears: An exception to the rule
These findings do not necessarily apply to patients with evidence of large meniscal tears. This subset of knee OA patients may benefit from surgical management.
CHALLENGES TO IMPLEMENTATION: What to say to patients seeking a referral
Patients may have read about arthroscopic knee surgery or know someone who underwent the procedure and come to you asking for a referral to an orthopedic surgeon. In such a case, we suggest a straightforward approach.
Discuss arthroscopic surgery’s proven lack of benefit and offer equally effective conservative therapies. For patients who may be eligible for a total knee replacement, a referral to an orthopedic surgeon for evaluation is appropriate.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097-1107.
2. Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
3. Hawker G, Guan J, Judge A, et al. Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am. 2008;90:2337-2345.
4. American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (non-arthroplasty): full guideline. December 6, 2008. Available at: http://www.aaos.org/Research/guidelines/GuidelineOAKnee.asp. Accessed February 16, 2009.
5. Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2005;(1):CD002946.-
6. Michel BA, Stucki G, Frey D, et al. Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Arthritis Rheum. 2005;52:779-786.
7. Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006;354:795-808.
8. Arroll B, Goodyear-Smith F. Corticosteroid injections for osteoarthritis of the knee: meta-analysis. BMJ. 2004;328:869-870.
9. Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol. 2001;28:156-164.
10. Berman BM, Lao L, Langenberg P, et al. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141:901-910.
1. Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097-1107.
2. Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
3. Hawker G, Guan J, Judge A, et al. Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am. 2008;90:2337-2345.
4. American Academy of Orthopaedic Surgeons. Treatment of osteoarthritis of the knee (non-arthroplasty): full guideline. December 6, 2008. Available at: http://www.aaos.org/Research/guidelines/GuidelineOAKnee.asp. Accessed February 16, 2009.
5. Towheed TE, Maxwell L, Anastassiades TP, et al. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev. 2005;(1):CD002946.-
6. Michel BA, Stucki G, Frey D, et al. Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Arthritis Rheum. 2005;52:779-786.
7. Clegg DO, Reda DJ, Harris CL, et al. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. N Engl J Med. 2006;354:795-808.
8. Arroll B, Goodyear-Smith F. Corticosteroid injections for osteoarthritis of the knee: meta-analysis. BMJ. 2004;328:869-870.
9. Fransen M, Crosbie J, Edmonds J. Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. J Rheumatol. 2001;28:156-164.
10. Berman BM, Lao L, Langenberg P, et al. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004;141:901-910.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
This antiemetic may help kids skip that trip to the hospital
Give oral ondansetron to children with acute gastroenteritis and moderate dehydration who are unable to tolerate oral rehydration to reduce the vomiting and avoid the need for intravenous (IV) hydration or hospitalization.1
Strength of recommendation
A: Meta-analysis of 6 high-quality studies
DeCamp LS, Byerley JS, Doshi N, et al. Use of antiemetic agents in acute gastroenteritis, a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2008;162:858-865.
ILLUSTRATIVE CASE
Sarah, a 2-year-old who has been vomiting and had diarrhea for the past 2 days, is brought to your office by her parents. They tell you she’s unable to tolerate oral fluids, and vomited twice after being given small amounts of juice and soup earlier in the day. Sarah has decreased urine output, but she is not febrile and has no blood in her stools. On examination, you find mild tachycardia, dry mucous membranes, delayed capillary refill, and normal mental status.
You try giving Sarah an oral electrolyte solution, but she vomits immediately. Her parents are reluctant to take her to the emergency department for intravenous (IV) hydration, and ask if you can provide a safe and effective alternative.
Each year in the United States, pediatric gastroenteritis and dehydration are responsible for approximately 1.5 million outpatient visits2 and 150,000 to 170,000 hospital admissions.3 Oral hydration, recommended by pediatric practice guidelines2,4 and the World Health Organization,5 is safe and generally effective. But, as in Sarah’s case, emesis frequently interferes, leading to hospital admission for IV hydration.
An antiemetic with fewer adverse effects
Older antiemetic medications, such as promethazine, prochlorperazine, and metoclopramide, can cause sedation and extrapyramidal reactions. Ondansetron, a selective 5-hydroxytryptamine (5-HT3) receptor antagonist that has been used to control postoperative and chemotherapy-associated nausea and vomiting in children and adults, does not cause either problem. In recent studies of ondansetron’s effectiveness in treating children with gastroenteritis, increased diarrhea, lasting up to 48 hours after administration, was the only adverse event.1
Two earlier systematic reviews—a meta-analysis by Szajewska et al6 and a Cochrane review7—found clinical benefits of ondansetron for vomiting associated with acute gastroenteritis. But both concluded that the evidence was insufficient to recommend routine use of this drug. The meta-analysis that we review below included additional studies, and the researchers reached a different conclusion.
STUDY SUMMARY: Antiemetic decreases vomiting, hospitalization
DeCamp et al conducted a systematic review and meta-analysis of 11 prospective controlled trials that evaluated antiemetic use in children with vomiting from acute gastroenteritis.1 Six of the 11 trials focused on ondansetron;8-13 these 6 were the most recently published and of the highest quality. (The researchers found the remaining 5 trials to be of low methodological quality, with small sample sizes and inconsistent results, and concluded that the antiemetics they assessed should not be used for outpatients with gastroenteritis.) Their meta-analysis of these 6 trials is the focus of this PURL.
The ondansetron studies included a total of 745 children with vomiting and a clinical diagnosis of gastroenteritis. In 5 of the trials, patients received only 1 dose of ondansetron;8-10,12,13 in the sixth, families received additional doses of ondansetron to use at home.11 In 3 trials, patients were given oral ondansetron—a tablet placed on the tongue that dissolves in minutes. The remaining 3 used an IV formulation.8,10,13 Five trials were conducted in emergency departments (EDs),9-13 and 1 in an inpatient setting.8
Big reductions. Children who received ondansetron had significantly less vomiting (16.9% vs 37.8%) and IV fluid administration (13.9% vs 33.9%), and fewer hospital admissions (7.5% vs 14.6%) compared with patients who were given a placebo (TABLE). Diarrhea, the only adverse event to be systematically evaluated, was assessed in all but 1 of the trials.8-12 In 3 of the 5 that reported on this side effect, patients who received ondansetron had an increase in diarrhea for up to 48 hours.8,11,12
TABLE
Ondansetron reduces vomiting, hospitalization, and IV fluid use
| TOTAL NUMBER OF PATIENTS (N=745) | ONDANSETRON | PLACEBO | RR (95% CI) | NNT (95% CI) |
|---|---|---|---|---|
| Continued vomiting (n=659) | 16.9% | 37.8% | 0.45 (0.33-0.62) | 5 (4-7) |
| IV fluid administration (n=489) | 13.9% | 33.9% | 0.41 (0.28-0.62) | 5 (4-8) |
| Hospital admission (n=662) | 7.5% | 14.6% | 0.52 (0.27-0.95) | 14 (9-44) |
| CI, confidence interval; IV, intravenous; NNT, number needed to treat; RR, relative risk. | ||||
| Source: DeCamp LS, et al. Arch Pediatr Adolesc Med.1 | ||||
WHAT’S NEW: Support for a strategy increasingly used in EDs
Physicians are just beginning to adopt the use of ondansetron as a strategy for avoiding IV hydration and hospitalization for children with vomiting associated with minor gastrointestinal illness. As an adjunct to our report on this meta-analysis, we analyzed the use of the antiemetic in children between the ages of 1 and 10 years in emergency visits reported to the National Ambulatory Medical Care Survey database from 2002 to 2006. Among an estimate of more than 3 million pediatric visits to EDs for acute gastroenteritis in each of these years, in 2002 only 0.53% were treated with ondansetron. By 2006, that percentage had risen to 6.43%.
A similar analysis of both ED and outpatient visits to academic medical centers and teaching hospitals from 2005 through 2008 (estimated using data through October 2008), derived from the University Health System Consortium Clinical Database, showed a similar trend. In 2005, only 0.5% of children presenting to EDs and 0.5% of those seeking outpatient care for acute gastritis received ondansetron. By 2008, the numbers had grown to an estimated 3.43% and 3.60%, respectively.
Given the positive results of the DeCamp study and the fact that oral ondansetron is now available in a generic formulation, we expect the use of this antiemetic to increase in both outpatient and emergency settings. We think quite a few IV lines and hospitalizations could be avoided with the use of this antiemetic, not to mention the symptomatic relief for children.
CAVEATS: Studies didn’t look at milder cases, primary care
None of the studies of oral ondansetron for acute gastroenteritis involved outpatient settings, and all 6 of the trials featured children who were moderately ill. It has not yet been determined whether the benefits seen in the ED will apply to an ambulatory population in which many potential candidates for ondansetron have milder gastroenteritis. Nor is it clear whether oral ondansetron would complement oral rehydration in primary care practices. More detailed evaluation of the reduction of vomiting at home over the course of the illness would help to answer these questions.
Nonetheless, ondansetron appears to be safe. Increased diarrhea, the only documented side effect, resolved after 48 hours, and did not appear to result in higher health care utilization.
Don’t prescribe over the phone. It is important to note that all the ondansetron trials included an evaluation of each patient to consider other etiologies, such as central nervous system disorders or toxic exposures, prior to treatment. Physicians are cautioned not to prescribe antiemetics over the telephone—or without first ruling out more serious illnesses in which vomiting is part of the presentation.
Studies were funded by pharma. The primary studies of ondansetron were funded by GlaxoSmithKline, the pharmaceutical company that manufactures the drug under the trade name Zofran. The authors of the meta-analysis reviewed the Clinical Trials Registry and the reference lists of the articles and contacted other experts to find any unreported trials, but found no evidence of negative publication bias. Therefore, we have confidence in these findings. Ideally, additional studies will be conducted without drug company support, in an outpatient setting, to clarify the use of ondansetron as an adjunct to oral rehydration.
CHALLENGES TO IMPLEMENTATION: No major barriers
Cost should not be a barrier to the use of oral ondansetron. The generic formulation sells for $10 to $20 per tablet, and is covered by most health insurers. However, treatment of children with acute gastroenteritis and moderate dehydration in the office setting would likely require a period of observation for tolerance of oral rehydration before and after administration of ondansetron. This may be impractical in some busy clinics.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
The authors wish to acknowledge Sofia Medvedev, PhD, of the University HealthSystem Consortium in Oak Brook, Ill, for analysis of the National Ambulatory Medical Care Survey data and the UHC Clinical Database.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. DeCamp LS, Byerley JS, Doshi N, et al. Use of antiemetic agents in acute gastroenteritis, a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2008;162:858-865.
2. King CK, Glass R, Bresee JS, et al. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep. 2003;52(RR-16):1-16.
3. Malek MA, Curns AT, Holman RC, et al. Diarrhea- and rotavirus-associated hospitalizations among children less than 5 years of age: United States, 1997 and 2000. Pediatrics. 2006;117:1887-1892.
4. Practice parameter: the management of acute gastroenteritis in young children. American Academy of Pediatrics, Provisional Committee on Quality Improvement, Subcommittee on Acute Gastroenteritis. Pediatrics. 1996;97:424-435.
5. World Health Organization. Clinical management of acute diarrhoea. WHO/Unicef joint statement. Available at http://www.who.int/child_adolescent_health/documents/who_fch_cah_04_7/en/index.html. Accessed January 15, 2009.
6. Szajewska H, Gieruszczak-Bialek D, Dylag M. Meta-analysis: ondansetron for vomiting in acute gastroenteritis in children. Aliment Pharmacol Ther. 2007;25:393-400.
7. Alhashimi D, Alhashimi H, Fedorowicz Z. Antiemetics for reducing vomiting related to acute gastroenteritis in children and adolescents. Cochrane Database Syst Rev. 2006;(4):CD005506.-
8. Cubeddu LX, Trujillo LM, Talmaciu I, et al. Antiemetic activity of ondansetron in acute gastroenteritis. Aliment Pharmacol Ther. 1997;11:185-191.
9. Roslund G, Hepps TS, McQuillen KK. The role of oral ondansetron in children with vomiting as a result of acute gastritis/gastroenteritis who have failed oral rehydration therapy: a randomized controlled trial. Ann Emerg Med. 2008;52:22-29.
10. Reeves JJ, Shannon MW, Fleisher GR. Ondansetron decreases vomiting associated with acute gastroenteritis; a randomized, controlled trial. Pediatrics. 2002;109:e62.-Available at: http://pediatrics.aappublications.org/cgi/reprint/109/4/e62. Accessed January 12, 2009.
11. Ramsook C, Sahagun-Carreon I, Kozinetz CA, et al. A randomized clinical trial comparing oral ondansetron with placebo in children with vomiting from acute gastroenteritis. Ann Emerg Med. 2002;39:397-403.
12. Freedman SB, Adler M, Seshadri R, et al. Oral ondansetron for gastroenteritis in a pediatric emergency department. N Engl J Med. 2006;354:1698-1705.
13. Stork CM, Brown KM, Reilly TH, et al. Emergency department treatment of viral gastritis using intravenous ondansetron or dexamethasone in children. Acad Emerg Med. 2006;13:1027-1033.
Give oral ondansetron to children with acute gastroenteritis and moderate dehydration who are unable to tolerate oral rehydration to reduce the vomiting and avoid the need for intravenous (IV) hydration or hospitalization.1
Strength of recommendation
A: Meta-analysis of 6 high-quality studies
DeCamp LS, Byerley JS, Doshi N, et al. Use of antiemetic agents in acute gastroenteritis, a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2008;162:858-865.
ILLUSTRATIVE CASE
Sarah, a 2-year-old who has been vomiting and had diarrhea for the past 2 days, is brought to your office by her parents. They tell you she’s unable to tolerate oral fluids, and vomited twice after being given small amounts of juice and soup earlier in the day. Sarah has decreased urine output, but she is not febrile and has no blood in her stools. On examination, you find mild tachycardia, dry mucous membranes, delayed capillary refill, and normal mental status.
You try giving Sarah an oral electrolyte solution, but she vomits immediately. Her parents are reluctant to take her to the emergency department for intravenous (IV) hydration, and ask if you can provide a safe and effective alternative.
Each year in the United States, pediatric gastroenteritis and dehydration are responsible for approximately 1.5 million outpatient visits2 and 150,000 to 170,000 hospital admissions.3 Oral hydration, recommended by pediatric practice guidelines2,4 and the World Health Organization,5 is safe and generally effective. But, as in Sarah’s case, emesis frequently interferes, leading to hospital admission for IV hydration.
An antiemetic with fewer adverse effects
Older antiemetic medications, such as promethazine, prochlorperazine, and metoclopramide, can cause sedation and extrapyramidal reactions. Ondansetron, a selective 5-hydroxytryptamine (5-HT3) receptor antagonist that has been used to control postoperative and chemotherapy-associated nausea and vomiting in children and adults, does not cause either problem. In recent studies of ondansetron’s effectiveness in treating children with gastroenteritis, increased diarrhea, lasting up to 48 hours after administration, was the only adverse event.1
Two earlier systematic reviews—a meta-analysis by Szajewska et al6 and a Cochrane review7—found clinical benefits of ondansetron for vomiting associated with acute gastroenteritis. But both concluded that the evidence was insufficient to recommend routine use of this drug. The meta-analysis that we review below included additional studies, and the researchers reached a different conclusion.
STUDY SUMMARY: Antiemetic decreases vomiting, hospitalization
DeCamp et al conducted a systematic review and meta-analysis of 11 prospective controlled trials that evaluated antiemetic use in children with vomiting from acute gastroenteritis.1 Six of the 11 trials focused on ondansetron;8-13 these 6 were the most recently published and of the highest quality. (The researchers found the remaining 5 trials to be of low methodological quality, with small sample sizes and inconsistent results, and concluded that the antiemetics they assessed should not be used for outpatients with gastroenteritis.) Their meta-analysis of these 6 trials is the focus of this PURL.
The ondansetron studies included a total of 745 children with vomiting and a clinical diagnosis of gastroenteritis. In 5 of the trials, patients received only 1 dose of ondansetron;8-10,12,13 in the sixth, families received additional doses of ondansetron to use at home.11 In 3 trials, patients were given oral ondansetron—a tablet placed on the tongue that dissolves in minutes. The remaining 3 used an IV formulation.8,10,13 Five trials were conducted in emergency departments (EDs),9-13 and 1 in an inpatient setting.8
Big reductions. Children who received ondansetron had significantly less vomiting (16.9% vs 37.8%) and IV fluid administration (13.9% vs 33.9%), and fewer hospital admissions (7.5% vs 14.6%) compared with patients who were given a placebo (TABLE). Diarrhea, the only adverse event to be systematically evaluated, was assessed in all but 1 of the trials.8-12 In 3 of the 5 that reported on this side effect, patients who received ondansetron had an increase in diarrhea for up to 48 hours.8,11,12
TABLE
Ondansetron reduces vomiting, hospitalization, and IV fluid use
| TOTAL NUMBER OF PATIENTS (N=745) | ONDANSETRON | PLACEBO | RR (95% CI) | NNT (95% CI) |
|---|---|---|---|---|
| Continued vomiting (n=659) | 16.9% | 37.8% | 0.45 (0.33-0.62) | 5 (4-7) |
| IV fluid administration (n=489) | 13.9% | 33.9% | 0.41 (0.28-0.62) | 5 (4-8) |
| Hospital admission (n=662) | 7.5% | 14.6% | 0.52 (0.27-0.95) | 14 (9-44) |
| CI, confidence interval; IV, intravenous; NNT, number needed to treat; RR, relative risk. | ||||
| Source: DeCamp LS, et al. Arch Pediatr Adolesc Med.1 | ||||
WHAT’S NEW: Support for a strategy increasingly used in EDs
Physicians are just beginning to adopt the use of ondansetron as a strategy for avoiding IV hydration and hospitalization for children with vomiting associated with minor gastrointestinal illness. As an adjunct to our report on this meta-analysis, we analyzed the use of the antiemetic in children between the ages of 1 and 10 years in emergency visits reported to the National Ambulatory Medical Care Survey database from 2002 to 2006. Among an estimate of more than 3 million pediatric visits to EDs for acute gastroenteritis in each of these years, in 2002 only 0.53% were treated with ondansetron. By 2006, that percentage had risen to 6.43%.
A similar analysis of both ED and outpatient visits to academic medical centers and teaching hospitals from 2005 through 2008 (estimated using data through October 2008), derived from the University Health System Consortium Clinical Database, showed a similar trend. In 2005, only 0.5% of children presenting to EDs and 0.5% of those seeking outpatient care for acute gastritis received ondansetron. By 2008, the numbers had grown to an estimated 3.43% and 3.60%, respectively.
Given the positive results of the DeCamp study and the fact that oral ondansetron is now available in a generic formulation, we expect the use of this antiemetic to increase in both outpatient and emergency settings. We think quite a few IV lines and hospitalizations could be avoided with the use of this antiemetic, not to mention the symptomatic relief for children.
CAVEATS: Studies didn’t look at milder cases, primary care
None of the studies of oral ondansetron for acute gastroenteritis involved outpatient settings, and all 6 of the trials featured children who were moderately ill. It has not yet been determined whether the benefits seen in the ED will apply to an ambulatory population in which many potential candidates for ondansetron have milder gastroenteritis. Nor is it clear whether oral ondansetron would complement oral rehydration in primary care practices. More detailed evaluation of the reduction of vomiting at home over the course of the illness would help to answer these questions.
Nonetheless, ondansetron appears to be safe. Increased diarrhea, the only documented side effect, resolved after 48 hours, and did not appear to result in higher health care utilization.
Don’t prescribe over the phone. It is important to note that all the ondansetron trials included an evaluation of each patient to consider other etiologies, such as central nervous system disorders or toxic exposures, prior to treatment. Physicians are cautioned not to prescribe antiemetics over the telephone—or without first ruling out more serious illnesses in which vomiting is part of the presentation.
Studies were funded by pharma. The primary studies of ondansetron were funded by GlaxoSmithKline, the pharmaceutical company that manufactures the drug under the trade name Zofran. The authors of the meta-analysis reviewed the Clinical Trials Registry and the reference lists of the articles and contacted other experts to find any unreported trials, but found no evidence of negative publication bias. Therefore, we have confidence in these findings. Ideally, additional studies will be conducted without drug company support, in an outpatient setting, to clarify the use of ondansetron as an adjunct to oral rehydration.
CHALLENGES TO IMPLEMENTATION: No major barriers
Cost should not be a barrier to the use of oral ondansetron. The generic formulation sells for $10 to $20 per tablet, and is covered by most health insurers. However, treatment of children with acute gastroenteritis and moderate dehydration in the office setting would likely require a period of observation for tolerance of oral rehydration before and after administration of ondansetron. This may be impractical in some busy clinics.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
The authors wish to acknowledge Sofia Medvedev, PhD, of the University HealthSystem Consortium in Oak Brook, Ill, for analysis of the National Ambulatory Medical Care Survey data and the UHC Clinical Database.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Give oral ondansetron to children with acute gastroenteritis and moderate dehydration who are unable to tolerate oral rehydration to reduce the vomiting and avoid the need for intravenous (IV) hydration or hospitalization.1
Strength of recommendation
A: Meta-analysis of 6 high-quality studies
DeCamp LS, Byerley JS, Doshi N, et al. Use of antiemetic agents in acute gastroenteritis, a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2008;162:858-865.
ILLUSTRATIVE CASE
Sarah, a 2-year-old who has been vomiting and had diarrhea for the past 2 days, is brought to your office by her parents. They tell you she’s unable to tolerate oral fluids, and vomited twice after being given small amounts of juice and soup earlier in the day. Sarah has decreased urine output, but she is not febrile and has no blood in her stools. On examination, you find mild tachycardia, dry mucous membranes, delayed capillary refill, and normal mental status.
You try giving Sarah an oral electrolyte solution, but she vomits immediately. Her parents are reluctant to take her to the emergency department for intravenous (IV) hydration, and ask if you can provide a safe and effective alternative.
Each year in the United States, pediatric gastroenteritis and dehydration are responsible for approximately 1.5 million outpatient visits2 and 150,000 to 170,000 hospital admissions.3 Oral hydration, recommended by pediatric practice guidelines2,4 and the World Health Organization,5 is safe and generally effective. But, as in Sarah’s case, emesis frequently interferes, leading to hospital admission for IV hydration.
An antiemetic with fewer adverse effects
Older antiemetic medications, such as promethazine, prochlorperazine, and metoclopramide, can cause sedation and extrapyramidal reactions. Ondansetron, a selective 5-hydroxytryptamine (5-HT3) receptor antagonist that has been used to control postoperative and chemotherapy-associated nausea and vomiting in children and adults, does not cause either problem. In recent studies of ondansetron’s effectiveness in treating children with gastroenteritis, increased diarrhea, lasting up to 48 hours after administration, was the only adverse event.1
Two earlier systematic reviews—a meta-analysis by Szajewska et al6 and a Cochrane review7—found clinical benefits of ondansetron for vomiting associated with acute gastroenteritis. But both concluded that the evidence was insufficient to recommend routine use of this drug. The meta-analysis that we review below included additional studies, and the researchers reached a different conclusion.
STUDY SUMMARY: Antiemetic decreases vomiting, hospitalization
DeCamp et al conducted a systematic review and meta-analysis of 11 prospective controlled trials that evaluated antiemetic use in children with vomiting from acute gastroenteritis.1 Six of the 11 trials focused on ondansetron;8-13 these 6 were the most recently published and of the highest quality. (The researchers found the remaining 5 trials to be of low methodological quality, with small sample sizes and inconsistent results, and concluded that the antiemetics they assessed should not be used for outpatients with gastroenteritis.) Their meta-analysis of these 6 trials is the focus of this PURL.
The ondansetron studies included a total of 745 children with vomiting and a clinical diagnosis of gastroenteritis. In 5 of the trials, patients received only 1 dose of ondansetron;8-10,12,13 in the sixth, families received additional doses of ondansetron to use at home.11 In 3 trials, patients were given oral ondansetron—a tablet placed on the tongue that dissolves in minutes. The remaining 3 used an IV formulation.8,10,13 Five trials were conducted in emergency departments (EDs),9-13 and 1 in an inpatient setting.8
Big reductions. Children who received ondansetron had significantly less vomiting (16.9% vs 37.8%) and IV fluid administration (13.9% vs 33.9%), and fewer hospital admissions (7.5% vs 14.6%) compared with patients who were given a placebo (TABLE). Diarrhea, the only adverse event to be systematically evaluated, was assessed in all but 1 of the trials.8-12 In 3 of the 5 that reported on this side effect, patients who received ondansetron had an increase in diarrhea for up to 48 hours.8,11,12
TABLE
Ondansetron reduces vomiting, hospitalization, and IV fluid use
| TOTAL NUMBER OF PATIENTS (N=745) | ONDANSETRON | PLACEBO | RR (95% CI) | NNT (95% CI) |
|---|---|---|---|---|
| Continued vomiting (n=659) | 16.9% | 37.8% | 0.45 (0.33-0.62) | 5 (4-7) |
| IV fluid administration (n=489) | 13.9% | 33.9% | 0.41 (0.28-0.62) | 5 (4-8) |
| Hospital admission (n=662) | 7.5% | 14.6% | 0.52 (0.27-0.95) | 14 (9-44) |
| CI, confidence interval; IV, intravenous; NNT, number needed to treat; RR, relative risk. | ||||
| Source: DeCamp LS, et al. Arch Pediatr Adolesc Med.1 | ||||
WHAT’S NEW: Support for a strategy increasingly used in EDs
Physicians are just beginning to adopt the use of ondansetron as a strategy for avoiding IV hydration and hospitalization for children with vomiting associated with minor gastrointestinal illness. As an adjunct to our report on this meta-analysis, we analyzed the use of the antiemetic in children between the ages of 1 and 10 years in emergency visits reported to the National Ambulatory Medical Care Survey database from 2002 to 2006. Among an estimate of more than 3 million pediatric visits to EDs for acute gastroenteritis in each of these years, in 2002 only 0.53% were treated with ondansetron. By 2006, that percentage had risen to 6.43%.
A similar analysis of both ED and outpatient visits to academic medical centers and teaching hospitals from 2005 through 2008 (estimated using data through October 2008), derived from the University Health System Consortium Clinical Database, showed a similar trend. In 2005, only 0.5% of children presenting to EDs and 0.5% of those seeking outpatient care for acute gastritis received ondansetron. By 2008, the numbers had grown to an estimated 3.43% and 3.60%, respectively.
Given the positive results of the DeCamp study and the fact that oral ondansetron is now available in a generic formulation, we expect the use of this antiemetic to increase in both outpatient and emergency settings. We think quite a few IV lines and hospitalizations could be avoided with the use of this antiemetic, not to mention the symptomatic relief for children.
CAVEATS: Studies didn’t look at milder cases, primary care
None of the studies of oral ondansetron for acute gastroenteritis involved outpatient settings, and all 6 of the trials featured children who were moderately ill. It has not yet been determined whether the benefits seen in the ED will apply to an ambulatory population in which many potential candidates for ondansetron have milder gastroenteritis. Nor is it clear whether oral ondansetron would complement oral rehydration in primary care practices. More detailed evaluation of the reduction of vomiting at home over the course of the illness would help to answer these questions.
Nonetheless, ondansetron appears to be safe. Increased diarrhea, the only documented side effect, resolved after 48 hours, and did not appear to result in higher health care utilization.
Don’t prescribe over the phone. It is important to note that all the ondansetron trials included an evaluation of each patient to consider other etiologies, such as central nervous system disorders or toxic exposures, prior to treatment. Physicians are cautioned not to prescribe antiemetics over the telephone—or without first ruling out more serious illnesses in which vomiting is part of the presentation.
Studies were funded by pharma. The primary studies of ondansetron were funded by GlaxoSmithKline, the pharmaceutical company that manufactures the drug under the trade name Zofran. The authors of the meta-analysis reviewed the Clinical Trials Registry and the reference lists of the articles and contacted other experts to find any unreported trials, but found no evidence of negative publication bias. Therefore, we have confidence in these findings. Ideally, additional studies will be conducted without drug company support, in an outpatient setting, to clarify the use of ondansetron as an adjunct to oral rehydration.
CHALLENGES TO IMPLEMENTATION: No major barriers
Cost should not be a barrier to the use of oral ondansetron. The generic formulation sells for $10 to $20 per tablet, and is covered by most health insurers. However, treatment of children with acute gastroenteritis and moderate dehydration in the office setting would likely require a period of observation for tolerance of oral rehydration before and after administration of ondansetron. This may be impractical in some busy clinics.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
The authors wish to acknowledge Sofia Medvedev, PhD, of the University HealthSystem Consortium in Oak Brook, Ill, for analysis of the National Ambulatory Medical Care Survey data and the UHC Clinical Database.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. DeCamp LS, Byerley JS, Doshi N, et al. Use of antiemetic agents in acute gastroenteritis, a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2008;162:858-865.
2. King CK, Glass R, Bresee JS, et al. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep. 2003;52(RR-16):1-16.
3. Malek MA, Curns AT, Holman RC, et al. Diarrhea- and rotavirus-associated hospitalizations among children less than 5 years of age: United States, 1997 and 2000. Pediatrics. 2006;117:1887-1892.
4. Practice parameter: the management of acute gastroenteritis in young children. American Academy of Pediatrics, Provisional Committee on Quality Improvement, Subcommittee on Acute Gastroenteritis. Pediatrics. 1996;97:424-435.
5. World Health Organization. Clinical management of acute diarrhoea. WHO/Unicef joint statement. Available at http://www.who.int/child_adolescent_health/documents/who_fch_cah_04_7/en/index.html. Accessed January 15, 2009.
6. Szajewska H, Gieruszczak-Bialek D, Dylag M. Meta-analysis: ondansetron for vomiting in acute gastroenteritis in children. Aliment Pharmacol Ther. 2007;25:393-400.
7. Alhashimi D, Alhashimi H, Fedorowicz Z. Antiemetics for reducing vomiting related to acute gastroenteritis in children and adolescents. Cochrane Database Syst Rev. 2006;(4):CD005506.-
8. Cubeddu LX, Trujillo LM, Talmaciu I, et al. Antiemetic activity of ondansetron in acute gastroenteritis. Aliment Pharmacol Ther. 1997;11:185-191.
9. Roslund G, Hepps TS, McQuillen KK. The role of oral ondansetron in children with vomiting as a result of acute gastritis/gastroenteritis who have failed oral rehydration therapy: a randomized controlled trial. Ann Emerg Med. 2008;52:22-29.
10. Reeves JJ, Shannon MW, Fleisher GR. Ondansetron decreases vomiting associated with acute gastroenteritis; a randomized, controlled trial. Pediatrics. 2002;109:e62.-Available at: http://pediatrics.aappublications.org/cgi/reprint/109/4/e62. Accessed January 12, 2009.
11. Ramsook C, Sahagun-Carreon I, Kozinetz CA, et al. A randomized clinical trial comparing oral ondansetron with placebo in children with vomiting from acute gastroenteritis. Ann Emerg Med. 2002;39:397-403.
12. Freedman SB, Adler M, Seshadri R, et al. Oral ondansetron for gastroenteritis in a pediatric emergency department. N Engl J Med. 2006;354:1698-1705.
13. Stork CM, Brown KM, Reilly TH, et al. Emergency department treatment of viral gastritis using intravenous ondansetron or dexamethasone in children. Acad Emerg Med. 2006;13:1027-1033.
1. DeCamp LS, Byerley JS, Doshi N, et al. Use of antiemetic agents in acute gastroenteritis, a systematic review and meta-analysis. Arch Pediatr Adolesc Med. 2008;162:858-865.
2. King CK, Glass R, Bresee JS, et al. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm Rep. 2003;52(RR-16):1-16.
3. Malek MA, Curns AT, Holman RC, et al. Diarrhea- and rotavirus-associated hospitalizations among children less than 5 years of age: United States, 1997 and 2000. Pediatrics. 2006;117:1887-1892.
4. Practice parameter: the management of acute gastroenteritis in young children. American Academy of Pediatrics, Provisional Committee on Quality Improvement, Subcommittee on Acute Gastroenteritis. Pediatrics. 1996;97:424-435.
5. World Health Organization. Clinical management of acute diarrhoea. WHO/Unicef joint statement. Available at http://www.who.int/child_adolescent_health/documents/who_fch_cah_04_7/en/index.html. Accessed January 15, 2009.
6. Szajewska H, Gieruszczak-Bialek D, Dylag M. Meta-analysis: ondansetron for vomiting in acute gastroenteritis in children. Aliment Pharmacol Ther. 2007;25:393-400.
7. Alhashimi D, Alhashimi H, Fedorowicz Z. Antiemetics for reducing vomiting related to acute gastroenteritis in children and adolescents. Cochrane Database Syst Rev. 2006;(4):CD005506.-
8. Cubeddu LX, Trujillo LM, Talmaciu I, et al. Antiemetic activity of ondansetron in acute gastroenteritis. Aliment Pharmacol Ther. 1997;11:185-191.
9. Roslund G, Hepps TS, McQuillen KK. The role of oral ondansetron in children with vomiting as a result of acute gastritis/gastroenteritis who have failed oral rehydration therapy: a randomized controlled trial. Ann Emerg Med. 2008;52:22-29.
10. Reeves JJ, Shannon MW, Fleisher GR. Ondansetron decreases vomiting associated with acute gastroenteritis; a randomized, controlled trial. Pediatrics. 2002;109:e62.-Available at: http://pediatrics.aappublications.org/cgi/reprint/109/4/e62. Accessed January 12, 2009.
11. Ramsook C, Sahagun-Carreon I, Kozinetz CA, et al. A randomized clinical trial comparing oral ondansetron with placebo in children with vomiting from acute gastroenteritis. Ann Emerg Med. 2002;39:397-403.
12. Freedman SB, Adler M, Seshadri R, et al. Oral ondansetron for gastroenteritis in a pediatric emergency department. N Engl J Med. 2006;354:1698-1705.
13. Stork CM, Brown KM, Reilly TH, et al. Emergency department treatment of viral gastritis using intravenous ondansetron or dexamethasone in children. Acad Emerg Med. 2006;13:1027-1033.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
Let them eat nuts—this snack is safe for diverticulosis patients
ILLUSTRATIVE CASE
John M, a 50-year-old patient, recently had a routine colonoscopy and was diagnosed with diverticulosis. Concerned because a friend has had multiple bouts of diverticulitis and a partial colectomy, John schedules an appointment to discuss management of diverticulosis. His friend has told John he’ll have to follow a strict diet and avoid nuts, corn, and popcorn altogether. Anxious to avoid the complications his friend has experienced, John turns to you for dietary advice. Would you know what dietary advice is best?
Diverticulosis affects one-third of the US population by age 60; by the age of 85, two-thirds are affected.2,3 This common digestive disorder has been associated with a diet high in refined carbohydrates, and is less prevalent among people who follow a vegetarian diet.4-6 Up to 35% of patients with diverticulosis develop complications, including diverticulitis and diverticular bleeding, that frequently require hospitalization and invasive procedures.7,8
Nuts or no nuts? In search of evidence
Biological mechanisms responsible for the development of diverticular complications are poorly understood.1,4 But luminal trauma has been suggested as a contributory factor and nuts, corn, popcorn, and seeds have long been viewed as likely culprits.8 Thus, physicians have historically advised patients with diverticular disease to avoid these foods.8-12
That recommendation, however, had little evidence to support it. Until the study by Strate et al that we report on here, no studies had assessed the consumption of nuts, corn, popcorn, or seeds as a risk factor for diverticulitis or diverticular complications.1,13 Conversely, there was a growing body of evidence that a diet rich in nuts may provide protection against many common disorders, including coronary heart disease, diabetes, colon and prostate cancers, and gall bladder disease.14-19 The research by Strate et al settles the matter, but it also provides an interesting twist.
STUDY SUMMARY: Nuts and popcorn linked to lower risk
The Strate trial is part of the Health Professionals Follow-up Study, a prospective cohort study that followed male health professionals in the United States from 1986 to 2004.20 A counterpart to the all-female Nurses’ Health Study, this long-running study allowed investigators to evaluate the relationship between nutritional factors and the incidence of serious illnesses such as cancer, heart disease, and other vascular diseases. The study population was comprised of 47,228 men between the ages of 40 and 75 years who completed periodic self-administered medical and dietary questionnaires.
At baseline, all the men were free of diverticulosis or related complications, as well as cancer and inflammatory bowel disease. During the 18 years of follow-up, 801 incident cases of diverticulitis and 383 cases of diverticular bleeding occurred. After analyzing the data, the researchers reported that, not only was the consumption of nuts and/or popcorn not associated with an increased risk of diverticulitis, it had a protective effect. The hazard ratios for men with the highest intake of nuts and/or popcorn (at least twice a week) compared with men with the lowest intake (less than once a month) were 0.80 (95% confidence interval [CI], 0.63-1.01) for nuts and 0.72 (95% CI, 0.56-0.92) for popcorn. The researchers found no association, positive or negative, between corn consumption and diverticulitis, nor between nut, corn, or popcorn consumption and diverticular bleeding or the development of uncomplicated diverticulosis.1
FIGURE
Colonoscopy reveals diverticular disease
This colonoscopic image shows the presence of a diverticulum.
WHAT’S NEW?: A long-standing belief gets debunked
This study—the first to examine the relationship between a diet rich in nuts, corn, or popcorn and diverticular disease—showed that these foods did not increase the risk of developing diverticulosis, diverticulitis, or diverticular bleeding. Moreover, it found an association between a diet rich in nuts or popcorn and a decreased risk of diverticulitis. Although we can’t characterize this as a cause-and-effect relationship based on this study, the evidence convinces us that, at the least, nuts, corn, and popcorn do not increase the risk of diverticular disease. We think we can confidently tell patients to enjoy these foods.
CAVEATS: Protective effect of nuts is tough to explain
As with all cohort studies, there is a possibility of unmeasured confounding variables which, in this case, could account for the protective effect of nuts and popcorn suggested by the decreased risk of diverticulitis. Although this was a large and carefully conducted prospective cohort study involving health professionals, we are not aware of any proven pathophysiologic mechanism by which nuts, corn, and popcorn may either increase or decrease the risk of diverticular disease or its complications.
A randomized controlled trial addressing this dietary issue is unlikely—and probably unnecessary. This study provides the strongest evidence on this topic by far. We think many patients have been unnecessarily deprived of these foods.
The study did not enroll young patients or women. However, diverticulosis is rare before the age of 40.2,9 And, because no clear sex difference has been observed in diverticular disease, we see no reason why this evidence should not apply equally to female patients.2,13
Also of note: This study did not assess total seed intake, per se. Rather, it assessed the consumption of strawberries and blueberries, the source of the seeds. The researchers found no association between strawberries and blueberries and diverticular complications, and we see no reason to tell patients to avoid them.
CHALLENGES TO IMPLEMENTATION: There are no obstacles to implementation
Dietary advice is an integral part of primary care practice. We see no challenges to implementing this practice changer, which should come as welcome news to patients at risk of diverticular disease or its complications.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
2. Hughes LE. Postmortem survey of diverticular disease of the colon. II. The muscular abnormality of the sigmoid colon. Gut. 1969;10:344-351.
3. Bogardus ST, Jr. What do we know about diverticular disease? A brief overview. J Clin Gastroenterol. 2006;40(suppl 3):S108-S111.
4. Floch MH, Bina I. The natural history of diverticulitis: fact and theory. J Clin Gastroenterol. 2004;38(5 suppl):S2-S7.
5. Nair P, Mayberry JF. Vegetarianism, dietary fibre and gastro-intestinal disease. Dig Dis. 1994;12:177-185.
6. Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. Br Med J. 1971;2:450-454.
7. McGuire HH, Jr. Bleeding colonic diverticula. A reappraisal of natural history and management. Ann Surg. 1994;220:653-656.
8. Horner JL. Natural history of diverticulosis of the colon. Am J Dig Dis. 1958;3:343-350.
9. Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057-2066.
10. Schechter S, Mulvey J, Eisenstat TE. Management of uncomplicated acute diverticulitis: results of a survey. Dis Colon Rectum. 1999;42:470-475.
11. National Digestive Diseases Information Clearing-house. Diverticulosis and diverticulitis. Bethesda, Md: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health; July 2008. NIH publication 08-1163. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/diverticulosis/. Accessed December 17, 2008.
12. Gearhart SL. Diverticular disease and common anorectal disorders. In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008:chap 291.
13. Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
14. Hu FB, Stampfer MJ, Manson JE, et al. Frequent nut consumption and risk of coronary heart disease in women: prospective cohort study. BMJ. 1998;317:1341-1345.
15. Blomhoff R, Carlsen MH, Andersen LF, et al. Health benefits of nuts: potential role of antioxidants. Br J Nutr. 2006;96(suppl 2):S52-S60.
16. Jenab M, Ferrari P, Slimani N, et al. Association of nut and seed intake with colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol Biomarkers Prev. 2004;13:1595-1603.
17. Jiang R, Manson JE, Stampfer MJ, et al. Nut and peanut butter consumption and risk of type 2 diabetes in women. JAMA. 2002;288:2554-2560.
18. Tsai CJ, Leitzmann MF, Hu FB, et al. Frequent nut consumption and decreased risk of cholecystectomy in women. Am J Clin Nutr. 2004;80:76-81.
19. Albert CM, Gaziano JM, Willett WC, et al. Nut consumption and decreased risk of sudden cardiac death in the Physicians’ Health Study. Arch Intern Med. 2002;162:1382-1387.
20. Harvard School of Public Health. Health professionals follow-up study. Available at: http://www.hsph.harvard.edu/hpfs/. Accessed December 17, 2008.
ILLUSTRATIVE CASE
John M, a 50-year-old patient, recently had a routine colonoscopy and was diagnosed with diverticulosis. Concerned because a friend has had multiple bouts of diverticulitis and a partial colectomy, John schedules an appointment to discuss management of diverticulosis. His friend has told John he’ll have to follow a strict diet and avoid nuts, corn, and popcorn altogether. Anxious to avoid the complications his friend has experienced, John turns to you for dietary advice. Would you know what dietary advice is best?
Diverticulosis affects one-third of the US population by age 60; by the age of 85, two-thirds are affected.2,3 This common digestive disorder has been associated with a diet high in refined carbohydrates, and is less prevalent among people who follow a vegetarian diet.4-6 Up to 35% of patients with diverticulosis develop complications, including diverticulitis and diverticular bleeding, that frequently require hospitalization and invasive procedures.7,8
Nuts or no nuts? In search of evidence
Biological mechanisms responsible for the development of diverticular complications are poorly understood.1,4 But luminal trauma has been suggested as a contributory factor and nuts, corn, popcorn, and seeds have long been viewed as likely culprits.8 Thus, physicians have historically advised patients with diverticular disease to avoid these foods.8-12
That recommendation, however, had little evidence to support it. Until the study by Strate et al that we report on here, no studies had assessed the consumption of nuts, corn, popcorn, or seeds as a risk factor for diverticulitis or diverticular complications.1,13 Conversely, there was a growing body of evidence that a diet rich in nuts may provide protection against many common disorders, including coronary heart disease, diabetes, colon and prostate cancers, and gall bladder disease.14-19 The research by Strate et al settles the matter, but it also provides an interesting twist.
STUDY SUMMARY: Nuts and popcorn linked to lower risk
The Strate trial is part of the Health Professionals Follow-up Study, a prospective cohort study that followed male health professionals in the United States from 1986 to 2004.20 A counterpart to the all-female Nurses’ Health Study, this long-running study allowed investigators to evaluate the relationship between nutritional factors and the incidence of serious illnesses such as cancer, heart disease, and other vascular diseases. The study population was comprised of 47,228 men between the ages of 40 and 75 years who completed periodic self-administered medical and dietary questionnaires.
At baseline, all the men were free of diverticulosis or related complications, as well as cancer and inflammatory bowel disease. During the 18 years of follow-up, 801 incident cases of diverticulitis and 383 cases of diverticular bleeding occurred. After analyzing the data, the researchers reported that, not only was the consumption of nuts and/or popcorn not associated with an increased risk of diverticulitis, it had a protective effect. The hazard ratios for men with the highest intake of nuts and/or popcorn (at least twice a week) compared with men with the lowest intake (less than once a month) were 0.80 (95% confidence interval [CI], 0.63-1.01) for nuts and 0.72 (95% CI, 0.56-0.92) for popcorn. The researchers found no association, positive or negative, between corn consumption and diverticulitis, nor between nut, corn, or popcorn consumption and diverticular bleeding or the development of uncomplicated diverticulosis.1
FIGURE
Colonoscopy reveals diverticular disease
This colonoscopic image shows the presence of a diverticulum.
WHAT’S NEW?: A long-standing belief gets debunked
This study—the first to examine the relationship between a diet rich in nuts, corn, or popcorn and diverticular disease—showed that these foods did not increase the risk of developing diverticulosis, diverticulitis, or diverticular bleeding. Moreover, it found an association between a diet rich in nuts or popcorn and a decreased risk of diverticulitis. Although we can’t characterize this as a cause-and-effect relationship based on this study, the evidence convinces us that, at the least, nuts, corn, and popcorn do not increase the risk of diverticular disease. We think we can confidently tell patients to enjoy these foods.
CAVEATS: Protective effect of nuts is tough to explain
As with all cohort studies, there is a possibility of unmeasured confounding variables which, in this case, could account for the protective effect of nuts and popcorn suggested by the decreased risk of diverticulitis. Although this was a large and carefully conducted prospective cohort study involving health professionals, we are not aware of any proven pathophysiologic mechanism by which nuts, corn, and popcorn may either increase or decrease the risk of diverticular disease or its complications.
A randomized controlled trial addressing this dietary issue is unlikely—and probably unnecessary. This study provides the strongest evidence on this topic by far. We think many patients have been unnecessarily deprived of these foods.
The study did not enroll young patients or women. However, diverticulosis is rare before the age of 40.2,9 And, because no clear sex difference has been observed in diverticular disease, we see no reason why this evidence should not apply equally to female patients.2,13
Also of note: This study did not assess total seed intake, per se. Rather, it assessed the consumption of strawberries and blueberries, the source of the seeds. The researchers found no association between strawberries and blueberries and diverticular complications, and we see no reason to tell patients to avoid them.
CHALLENGES TO IMPLEMENTATION: There are no obstacles to implementation
Dietary advice is an integral part of primary care practice. We see no challenges to implementing this practice changer, which should come as welcome news to patients at risk of diverticular disease or its complications.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
ILLUSTRATIVE CASE
John M, a 50-year-old patient, recently had a routine colonoscopy and was diagnosed with diverticulosis. Concerned because a friend has had multiple bouts of diverticulitis and a partial colectomy, John schedules an appointment to discuss management of diverticulosis. His friend has told John he’ll have to follow a strict diet and avoid nuts, corn, and popcorn altogether. Anxious to avoid the complications his friend has experienced, John turns to you for dietary advice. Would you know what dietary advice is best?
Diverticulosis affects one-third of the US population by age 60; by the age of 85, two-thirds are affected.2,3 This common digestive disorder has been associated with a diet high in refined carbohydrates, and is less prevalent among people who follow a vegetarian diet.4-6 Up to 35% of patients with diverticulosis develop complications, including diverticulitis and diverticular bleeding, that frequently require hospitalization and invasive procedures.7,8
Nuts or no nuts? In search of evidence
Biological mechanisms responsible for the development of diverticular complications are poorly understood.1,4 But luminal trauma has been suggested as a contributory factor and nuts, corn, popcorn, and seeds have long been viewed as likely culprits.8 Thus, physicians have historically advised patients with diverticular disease to avoid these foods.8-12
That recommendation, however, had little evidence to support it. Until the study by Strate et al that we report on here, no studies had assessed the consumption of nuts, corn, popcorn, or seeds as a risk factor for diverticulitis or diverticular complications.1,13 Conversely, there was a growing body of evidence that a diet rich in nuts may provide protection against many common disorders, including coronary heart disease, diabetes, colon and prostate cancers, and gall bladder disease.14-19 The research by Strate et al settles the matter, but it also provides an interesting twist.
STUDY SUMMARY: Nuts and popcorn linked to lower risk
The Strate trial is part of the Health Professionals Follow-up Study, a prospective cohort study that followed male health professionals in the United States from 1986 to 2004.20 A counterpart to the all-female Nurses’ Health Study, this long-running study allowed investigators to evaluate the relationship between nutritional factors and the incidence of serious illnesses such as cancer, heart disease, and other vascular diseases. The study population was comprised of 47,228 men between the ages of 40 and 75 years who completed periodic self-administered medical and dietary questionnaires.
At baseline, all the men were free of diverticulosis or related complications, as well as cancer and inflammatory bowel disease. During the 18 years of follow-up, 801 incident cases of diverticulitis and 383 cases of diverticular bleeding occurred. After analyzing the data, the researchers reported that, not only was the consumption of nuts and/or popcorn not associated with an increased risk of diverticulitis, it had a protective effect. The hazard ratios for men with the highest intake of nuts and/or popcorn (at least twice a week) compared with men with the lowest intake (less than once a month) were 0.80 (95% confidence interval [CI], 0.63-1.01) for nuts and 0.72 (95% CI, 0.56-0.92) for popcorn. The researchers found no association, positive or negative, between corn consumption and diverticulitis, nor between nut, corn, or popcorn consumption and diverticular bleeding or the development of uncomplicated diverticulosis.1
FIGURE
Colonoscopy reveals diverticular disease
This colonoscopic image shows the presence of a diverticulum.
WHAT’S NEW?: A long-standing belief gets debunked
This study—the first to examine the relationship between a diet rich in nuts, corn, or popcorn and diverticular disease—showed that these foods did not increase the risk of developing diverticulosis, diverticulitis, or diverticular bleeding. Moreover, it found an association between a diet rich in nuts or popcorn and a decreased risk of diverticulitis. Although we can’t characterize this as a cause-and-effect relationship based on this study, the evidence convinces us that, at the least, nuts, corn, and popcorn do not increase the risk of diverticular disease. We think we can confidently tell patients to enjoy these foods.
CAVEATS: Protective effect of nuts is tough to explain
As with all cohort studies, there is a possibility of unmeasured confounding variables which, in this case, could account for the protective effect of nuts and popcorn suggested by the decreased risk of diverticulitis. Although this was a large and carefully conducted prospective cohort study involving health professionals, we are not aware of any proven pathophysiologic mechanism by which nuts, corn, and popcorn may either increase or decrease the risk of diverticular disease or its complications.
A randomized controlled trial addressing this dietary issue is unlikely—and probably unnecessary. This study provides the strongest evidence on this topic by far. We think many patients have been unnecessarily deprived of these foods.
The study did not enroll young patients or women. However, diverticulosis is rare before the age of 40.2,9 And, because no clear sex difference has been observed in diverticular disease, we see no reason why this evidence should not apply equally to female patients.2,13
Also of note: This study did not assess total seed intake, per se. Rather, it assessed the consumption of strawberries and blueberries, the source of the seeds. The researchers found no association between strawberries and blueberries and diverticular complications, and we see no reason to tell patients to avoid them.
CHALLENGES TO IMPLEMENTATION: There are no obstacles to implementation
Dietary advice is an integral part of primary care practice. We see no challenges to implementing this practice changer, which should come as welcome news to patients at risk of diverticular disease or its complications.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
2. Hughes LE. Postmortem survey of diverticular disease of the colon. II. The muscular abnormality of the sigmoid colon. Gut. 1969;10:344-351.
3. Bogardus ST, Jr. What do we know about diverticular disease? A brief overview. J Clin Gastroenterol. 2006;40(suppl 3):S108-S111.
4. Floch MH, Bina I. The natural history of diverticulitis: fact and theory. J Clin Gastroenterol. 2004;38(5 suppl):S2-S7.
5. Nair P, Mayberry JF. Vegetarianism, dietary fibre and gastro-intestinal disease. Dig Dis. 1994;12:177-185.
6. Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. Br Med J. 1971;2:450-454.
7. McGuire HH, Jr. Bleeding colonic diverticula. A reappraisal of natural history and management. Ann Surg. 1994;220:653-656.
8. Horner JL. Natural history of diverticulosis of the colon. Am J Dig Dis. 1958;3:343-350.
9. Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057-2066.
10. Schechter S, Mulvey J, Eisenstat TE. Management of uncomplicated acute diverticulitis: results of a survey. Dis Colon Rectum. 1999;42:470-475.
11. National Digestive Diseases Information Clearing-house. Diverticulosis and diverticulitis. Bethesda, Md: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health; July 2008. NIH publication 08-1163. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/diverticulosis/. Accessed December 17, 2008.
12. Gearhart SL. Diverticular disease and common anorectal disorders. In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008:chap 291.
13. Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
14. Hu FB, Stampfer MJ, Manson JE, et al. Frequent nut consumption and risk of coronary heart disease in women: prospective cohort study. BMJ. 1998;317:1341-1345.
15. Blomhoff R, Carlsen MH, Andersen LF, et al. Health benefits of nuts: potential role of antioxidants. Br J Nutr. 2006;96(suppl 2):S52-S60.
16. Jenab M, Ferrari P, Slimani N, et al. Association of nut and seed intake with colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol Biomarkers Prev. 2004;13:1595-1603.
17. Jiang R, Manson JE, Stampfer MJ, et al. Nut and peanut butter consumption and risk of type 2 diabetes in women. JAMA. 2002;288:2554-2560.
18. Tsai CJ, Leitzmann MF, Hu FB, et al. Frequent nut consumption and decreased risk of cholecystectomy in women. Am J Clin Nutr. 2004;80:76-81.
19. Albert CM, Gaziano JM, Willett WC, et al. Nut consumption and decreased risk of sudden cardiac death in the Physicians’ Health Study. Arch Intern Med. 2002;162:1382-1387.
20. Harvard School of Public Health. Health professionals follow-up study. Available at: http://www.hsph.harvard.edu/hpfs/. Accessed December 17, 2008.
1. Strate LL, Liu YL, Syngal S, et al. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. 2008;300:907-914.
2. Hughes LE. Postmortem survey of diverticular disease of the colon. II. The muscular abnormality of the sigmoid colon. Gut. 1969;10:344-351.
3. Bogardus ST, Jr. What do we know about diverticular disease? A brief overview. J Clin Gastroenterol. 2006;40(suppl 3):S108-S111.
4. Floch MH, Bina I. The natural history of diverticulitis: fact and theory. J Clin Gastroenterol. 2004;38(5 suppl):S2-S7.
5. Nair P, Mayberry JF. Vegetarianism, dietary fibre and gastro-intestinal disease. Dig Dis. 1994;12:177-185.
6. Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. Br Med J. 1971;2:450-454.
7. McGuire HH, Jr. Bleeding colonic diverticula. A reappraisal of natural history and management. Ann Surg. 1994;220:653-656.
8. Horner JL. Natural history of diverticulosis of the colon. Am J Dig Dis. 1958;3:343-350.
9. Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057-2066.
10. Schechter S, Mulvey J, Eisenstat TE. Management of uncomplicated acute diverticulitis: results of a survey. Dis Colon Rectum. 1999;42:470-475.
11. National Digestive Diseases Information Clearing-house. Diverticulosis and diverticulitis. Bethesda, Md: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health; July 2008. NIH publication 08-1163. Available at: http://digestive.niddk.nih.gov/ddiseases/pubs/diverticulosis/. Accessed December 17, 2008.
12. Gearhart SL. Diverticular disease and common anorectal disorders. In: Fauci AS, Braunwald E, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 17th ed. New York: McGraw-Hill; 2008:chap 291.
13. Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121.
14. Hu FB, Stampfer MJ, Manson JE, et al. Frequent nut consumption and risk of coronary heart disease in women: prospective cohort study. BMJ. 1998;317:1341-1345.
15. Blomhoff R, Carlsen MH, Andersen LF, et al. Health benefits of nuts: potential role of antioxidants. Br J Nutr. 2006;96(suppl 2):S52-S60.
16. Jenab M, Ferrari P, Slimani N, et al. Association of nut and seed intake with colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol Biomarkers Prev. 2004;13:1595-1603.
17. Jiang R, Manson JE, Stampfer MJ, et al. Nut and peanut butter consumption and risk of type 2 diabetes in women. JAMA. 2002;288:2554-2560.
18. Tsai CJ, Leitzmann MF, Hu FB, et al. Frequent nut consumption and decreased risk of cholecystectomy in women. Am J Clin Nutr. 2004;80:76-81.
19. Albert CM, Gaziano JM, Willett WC, et al. Nut consumption and decreased risk of sudden cardiac death in the Physicians’ Health Study. Arch Intern Med. 2002;162:1382-1387.
20. Harvard School of Public Health. Health professionals follow-up study. Available at: http://www.hsph.harvard.edu/hpfs/. Accessed December 17, 2008.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
Saline irrigation spells relief for sinusitis sufferers
ILLUSTRATIVE CASE
A 45-year-old woman presents to your office with an 8-month history of nasal congestion and thick nasal discharge. Her symptoms have waxed and waned, the patient reports. She’s tried decongestants, antibiotics, and nasal steroids, with limited success. The patient has not had a recent respiratory infection, has never had sinus surgery, and does not want to be on long-term medication. You wonder if there’s an alternative treatment you can offer.
Rhinosinusitis is one of the most common conditions seen by primary care physicians in the United States, and its incidence and prevalence are increasing.2,3 While acute rhinosinusitis is usually self-limiting and resolves within a month, some patients develop chronic—and hard to treat—sinonasal symptoms.
No single cause, no definitive treatment
We’ve moved away from the notion that chronic rhinosinusitis is always a manifestation of persistent bacterial infection, and now recognize that there’s an inflammatory, nonbacterial component.4 In any given patient, several mechanisms—acting either simultaneously or independently—may contribute to sinonasal symptoms.3
Chronic sinusitis is treated in a variety of ways, including medications, immunotherapy, and surgery. Despite their limited efficacy, antibiotics and nasal steroids have been the mainstays of treatment.5 Treating underlying allergies, when they exist, may be helpful. But regardless of which treatment patients receive for chronic rhinosinusitis, many remain symptomatic.6
Benefits of saline irrigation extend beyond postop care
Otolaryngologists recommend saline irrigation after sinus surgery to clear secretions, debris, and crusts; reduce the risk of postoperative mucosal adhesions; and expedite mucosal healing.7,8 Saline irrigation is also gaining popularity as an alternative approach to chronic sinusitis symptom relief, and several randomized controlled trials (RCTs) have demonstrated both objective and subjective efficacy of this treatment for sinonasal disease.8-11
In 2007, the Cochrane Collaboration reviewed evidence for the effectiveness of nasal saline irrigation for symptoms of chronic rhinosinusitis. The reviewers concluded that it is well tolerated and beneficial, whether used alone or as an adjunctive treatment.12
Nasal saline sprays are often recommended because they’re thought to be better tolerated than other delivery modes.13 There have, however, been no comparisons of the relative efficacy of different means of saline delivery, until now.
STUDY SUMMARY: Nasal irrigation and spray go head-to-head
This study was a high-quality, prospective RCT comparing nasal spray and nasal irrigation.1 Subjects were recruited from the general population. To be eligible, participants had to be 18 years of age or older and have reported at least one of the following chronic rhinosinusitis symptoms on 4 or more days each week in the preceding 2 weeks:
- nasal stuffiness
- nasal dryness or crusting
- nasal congestion
- thick or discolored nasal discharge.
In addition, the symptoms must have been present on at least 15 of the preceding 30 days. Exclusion criteria included recent sinus surgery, a respiratory infection within the past 2 weeks, and the use of nasal saline within the past month.
Researchers enrolled 127 patients in the study; 63 were randomized to the nasal spray group and 64 to the large-volume, low-pressure irrigation group. Demographic and baseline characteristics of the groups were similar. The average ages of those in the irrigation and spray groups were 45 and 48 years, respectively. Most patients were nonsmokers and had been symptomatic for 7 to 12 months.
Twice-daily treatment. Researchers asked the patients to perform the assigned treatment twice daily for 8 weeks, but the patients were also permitted to continue using their usual medications. Symptom severity and disease-specific quality of life were assessed with the Sino-Nasal Outcome Test (SNOT-20), a 20-item survey that measures physical problems, emotional consequences, and functional limitations of sinusitis.14
The SNOT-20 is a validated, self-administered survey that asks patients to score items such as runny nose, postnasal discharge, need to blow the nose, reduced productivity, and embarrassment, on a 0- to 5-point scale (0=never, 5=always). A SNOT-20 score of 100 indicates the worst possible symptoms.
As a measure of chronicity of symptoms, patients were also asked to estimate how many months they’d had these symptoms during the last year. In addition, they were instructed to keep a diary to document treatment compliance and the use of other medications for sinonasal symptoms.
To measure outcomes, the researchers provided patients with mail-in packets so they could send in their completed SNOT-20 questionnaire and the medication diary completed at 2, 4, and 8 weeks after randomization.
Biggest improvements seen in irrigation group
Severity of symptoms. In each outcome measurement period, the saline irrigation group had lower SNOT-20 scores than the nasal spray group. At 2 weeks, the irrigation group scores were 4.4 points lower than the spray group (P=.02); at 4 weeks, the scores were 8.2 points lower (P<.001), and at 8 weeks the scores were 6.4 points lower (P=.002). Those in the irrigation group also had a significantly greater change from baseline than the patients in the spray group at 4 weeks (16.2 vs 7.4, P=.002) and at 8 weeks (15.0 vs 8.5, P=.04). The difference was marginally significant at 2 weeks (12.2 vs 6.7, P=.05).
Frequency of symptoms. At 8 weeks, 40% of the irrigation group and 61% of the nasal spray group reported nasal or sinus symptoms “often or always.” The absolute risk reduction in symptom frequency with saline irrigations, therefore, was 0.21; 95% confidence interval, 0.02-0.38 (P=.01). The odds of frequent nasal symptoms were 50% lower in the irrigation group compared to the spray group.
WHAT’S NEW: One delivery method is better than another
Prior studies had proven the effectiveness of nasal saline for reduction of rhinosinusitis symptoms. This RCT demonstrated that large-volume, low-pressure nasal irrigation brings greater symptom relief than nasal spray.
The researchers found little difference between the 2 groups in the rate of adverse effects, and reported that nasal irrigation appears to be well accepted once patients become accustomed to it. The fact that the participants were recruited from the general population further suggests that the results will be generalizable to primary care patients.
CAVEATS: High dropout rate in irrigation group
The absence of a control group prevents us from knowing the effect of saline nasal spray or irrigation compared with no treatment. In prior studies, however, nasal saline spray was found to be more effective than placebo in reducing rhinosinusitis symptoms.8,15
It is notable that a significant portion (21%) of the irrigation group abandoned this treatment by 8 weeks; in comparison, just 7% of the nasal spray group discontinued treatment.
This lower rate of adherence makes the beneficial effects of the irrigation group even more impressive. But it also suggests that a significant portion of patients are unlikely to stay with this recommended regimen. For those who try saline irrigation and choose not to continue it or are unwilling even to try it, saline spray is a reasonable alternative.
It should be noted that financial support for this study was provided by NeilMed Pharmaceuticals, a manufacturer of nasal saline solution and irrigation devices. However, the sponsor was not involved in the design or conduct of the study, in data collection or analysis, or in the preparation of the manuscript.
CHALLENGES TO IMPLEMENTATION: Tx may “scare away” some patients
Despite its effectiveness in reducing rhinosinusitis symptoms, performing large-volume, low-pressure nasal saline irrigation is not intuitive—and may sound downright scary to some patients. The need to learn how to perform nasal irrigation effectively, overcome the fear of water in the nasal cavity, and find the time to perform irrigation regularly can be barriers to this treatment.
A little bit of coaching can go a long way
A study by Rabago et al16 found that coached practice and patient education are effective tools in mastery of the technique ( PATIENT HANDOUT ).10,17 The researchers also found that several home strategies—incorporating nasal irrigation into the daily hygiene routine, placing the materials in a convenient location, and using warm water—facilitate regular use.
There is evidence, too, that patients who successfully use large-volume, low-pressure saline irrigation gain more than symptom relief. Rabago et al also found that effective use of this technique was associated with a sense of empowerment, and led to improved self-management skills, as well as a rapid, and long-term, improvement in quality of life.16
Saline nasal irrigation Your step-by-step guide
STEP 1: GATHER THE SUPPLIES
- - Salt (kosher, canning, or pickling salt)
- - Baking soda
- - Nasal irrigation pot (available at most pharmacies)
- - Measuring spoons
- - Container with lid
OR
- - An irrigation kit that includes the device and premixed saline packets
STEP 2: PREPARE THE SOLUTION
- - Put 1 tsp salt and ½ tsp baking soda into the container.
- - Add 1 pint of lukewarm tap water.
- - Mix contents.
- - Fill the nasal pot.
STEP 3: POSITION YOUR HEAD
- - Lean over the sink; rotate your head to one side.
- - Insert the spout of the irrigation device into the uppermost nostril.
- - Breathe through your mouth.
- - Raise the handle of the nasal pot so the solution flows into the upper nostril; in a few moments, the solution will begin to drain from the lower nostril.
- - Continue until the pot is empty, then exhale gently through both nostrils and gently blow your nose.
- - Refill the nasal pot, turn your head to the opposite side, and repeat with the other nostril.
- - Do this twice a day or as directed.
STEP 4: CLEAN AND PUT AWAY THE EQUIPMENT
- - Wash the nasal pot daily with warm water and dish detergent; rinse thoroughly.
- - Store unused saline solution in the sealed container; it can be kept at room temperature and reused for 2 days.
Adapted from: University of Wisconsin Department of Family Medicine.17
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Click here to view PURL METHODOLOGY
1. Pynnonen MA, Mukerji SS, Kim HM, et al. Nasal saline for chronic sinonasal symptoms: a randomized controlled trial. Arch Otolaryngol Head Neck Surg. 2007;133:11115-1120.
2. Gliklich RE, Metson R. Economic implications of chronic sinusitis. Otolaryngol Head Neck Surg. 1998;118(3 Pt 1):344-349.
3. International Rhinosinusitis Advisory Board. Infectious rhinosinusitis in adults classification, etiology and management. Ear Nose Throat J. 1997;76(12 suppl):s5-s22.
4. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):s1-s7.
5. Sharp HJ, Denman D, Puumala S, et al. Treatment of acute and chronic rhinosinusitis in the United States, 1999-2002. Arch Otolaryngol Head Neck Surg. 2007;133:260-265.
6. Subramanian HN, Schechtman KB, Hamilos DL. A retrospective analysis of treatment outcomes and time to relapse after intensive medical treatment for chronic sinusitis. Am J Rhinol. 2002;16:303-312.
7. Druce HM. Adjuncts to medical management of sinusitis. Otolaryngol Head Neck Surg. 1990;103(5 Pt 2):880-883.
8. Tomooka LT, Murphy C, Davidson TM. Clinical study and literature review of nasal irrigation. Laryngoscope. 2000;110:1189-1193.
9. Heatley DG, McConnell KE, Kille TL, et al. Nasal irrigation for the alleviation of sinonasal symptoms. Otolaryngol Head Neck Surg. 2001;125:44-48.
10. Rabago D, Zgierska A, Mundt M, et al. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51:1049-1055.
11. Taccariello M, Parikh A, Darby Y, et al. Nasal douching as a valuable adjunct in the management of chronic rhinosinusitis. Rhinology. 1999;37:29-32.
12. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.-
13. Keojampa BK, Nguyen MH, Ryan MW. Effects of buffered saline solution on nasal mucociliary clearance and nasal airway patency. Otolaryngol Head Neck Surg. 2004;131:679-682.
14. Piccirillo JF, Merritt MG, Jr, Richards ML. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002;126:41-47.
15. Hauptman G, Ryan MW. The effect of saline solutions on nasal patency and mucociliary clearance in rhinosinusitis patients. Otolaryngol Head Neck Surg. 2007;137:815-821.
16. Rabago D, Barrett B, Marchand L, et al. Qualitative aspects of nasal irrigation use by patients with chronic sinus disease in a multimethod study. Ann Fam Med. 2006;4:295-301.
17. University of Wisconsin Department of Family Medicine. Nasal Irrigation Instructions. Available at: http://www.fammed.wisc.edu/files/webfm-uploads/documents/research/nasalirrigationinstructions.pdf. Accessed December 1, 2008.
ILLUSTRATIVE CASE
A 45-year-old woman presents to your office with an 8-month history of nasal congestion and thick nasal discharge. Her symptoms have waxed and waned, the patient reports. She’s tried decongestants, antibiotics, and nasal steroids, with limited success. The patient has not had a recent respiratory infection, has never had sinus surgery, and does not want to be on long-term medication. You wonder if there’s an alternative treatment you can offer.
Rhinosinusitis is one of the most common conditions seen by primary care physicians in the United States, and its incidence and prevalence are increasing.2,3 While acute rhinosinusitis is usually self-limiting and resolves within a month, some patients develop chronic—and hard to treat—sinonasal symptoms.
No single cause, no definitive treatment
We’ve moved away from the notion that chronic rhinosinusitis is always a manifestation of persistent bacterial infection, and now recognize that there’s an inflammatory, nonbacterial component.4 In any given patient, several mechanisms—acting either simultaneously or independently—may contribute to sinonasal symptoms.3
Chronic sinusitis is treated in a variety of ways, including medications, immunotherapy, and surgery. Despite their limited efficacy, antibiotics and nasal steroids have been the mainstays of treatment.5 Treating underlying allergies, when they exist, may be helpful. But regardless of which treatment patients receive for chronic rhinosinusitis, many remain symptomatic.6
Benefits of saline irrigation extend beyond postop care
Otolaryngologists recommend saline irrigation after sinus surgery to clear secretions, debris, and crusts; reduce the risk of postoperative mucosal adhesions; and expedite mucosal healing.7,8 Saline irrigation is also gaining popularity as an alternative approach to chronic sinusitis symptom relief, and several randomized controlled trials (RCTs) have demonstrated both objective and subjective efficacy of this treatment for sinonasal disease.8-11
In 2007, the Cochrane Collaboration reviewed evidence for the effectiveness of nasal saline irrigation for symptoms of chronic rhinosinusitis. The reviewers concluded that it is well tolerated and beneficial, whether used alone or as an adjunctive treatment.12
Nasal saline sprays are often recommended because they’re thought to be better tolerated than other delivery modes.13 There have, however, been no comparisons of the relative efficacy of different means of saline delivery, until now.
STUDY SUMMARY: Nasal irrigation and spray go head-to-head
This study was a high-quality, prospective RCT comparing nasal spray and nasal irrigation.1 Subjects were recruited from the general population. To be eligible, participants had to be 18 years of age or older and have reported at least one of the following chronic rhinosinusitis symptoms on 4 or more days each week in the preceding 2 weeks:
- nasal stuffiness
- nasal dryness or crusting
- nasal congestion
- thick or discolored nasal discharge.
In addition, the symptoms must have been present on at least 15 of the preceding 30 days. Exclusion criteria included recent sinus surgery, a respiratory infection within the past 2 weeks, and the use of nasal saline within the past month.
Researchers enrolled 127 patients in the study; 63 were randomized to the nasal spray group and 64 to the large-volume, low-pressure irrigation group. Demographic and baseline characteristics of the groups were similar. The average ages of those in the irrigation and spray groups were 45 and 48 years, respectively. Most patients were nonsmokers and had been symptomatic for 7 to 12 months.
Twice-daily treatment. Researchers asked the patients to perform the assigned treatment twice daily for 8 weeks, but the patients were also permitted to continue using their usual medications. Symptom severity and disease-specific quality of life were assessed with the Sino-Nasal Outcome Test (SNOT-20), a 20-item survey that measures physical problems, emotional consequences, and functional limitations of sinusitis.14
The SNOT-20 is a validated, self-administered survey that asks patients to score items such as runny nose, postnasal discharge, need to blow the nose, reduced productivity, and embarrassment, on a 0- to 5-point scale (0=never, 5=always). A SNOT-20 score of 100 indicates the worst possible symptoms.
As a measure of chronicity of symptoms, patients were also asked to estimate how many months they’d had these symptoms during the last year. In addition, they were instructed to keep a diary to document treatment compliance and the use of other medications for sinonasal symptoms.
To measure outcomes, the researchers provided patients with mail-in packets so they could send in their completed SNOT-20 questionnaire and the medication diary completed at 2, 4, and 8 weeks after randomization.
Biggest improvements seen in irrigation group
Severity of symptoms. In each outcome measurement period, the saline irrigation group had lower SNOT-20 scores than the nasal spray group. At 2 weeks, the irrigation group scores were 4.4 points lower than the spray group (P=.02); at 4 weeks, the scores were 8.2 points lower (P<.001), and at 8 weeks the scores were 6.4 points lower (P=.002). Those in the irrigation group also had a significantly greater change from baseline than the patients in the spray group at 4 weeks (16.2 vs 7.4, P=.002) and at 8 weeks (15.0 vs 8.5, P=.04). The difference was marginally significant at 2 weeks (12.2 vs 6.7, P=.05).
Frequency of symptoms. At 8 weeks, 40% of the irrigation group and 61% of the nasal spray group reported nasal or sinus symptoms “often or always.” The absolute risk reduction in symptom frequency with saline irrigations, therefore, was 0.21; 95% confidence interval, 0.02-0.38 (P=.01). The odds of frequent nasal symptoms were 50% lower in the irrigation group compared to the spray group.
WHAT’S NEW: One delivery method is better than another
Prior studies had proven the effectiveness of nasal saline for reduction of rhinosinusitis symptoms. This RCT demonstrated that large-volume, low-pressure nasal irrigation brings greater symptom relief than nasal spray.
The researchers found little difference between the 2 groups in the rate of adverse effects, and reported that nasal irrigation appears to be well accepted once patients become accustomed to it. The fact that the participants were recruited from the general population further suggests that the results will be generalizable to primary care patients.
CAVEATS: High dropout rate in irrigation group
The absence of a control group prevents us from knowing the effect of saline nasal spray or irrigation compared with no treatment. In prior studies, however, nasal saline spray was found to be more effective than placebo in reducing rhinosinusitis symptoms.8,15
It is notable that a significant portion (21%) of the irrigation group abandoned this treatment by 8 weeks; in comparison, just 7% of the nasal spray group discontinued treatment.
This lower rate of adherence makes the beneficial effects of the irrigation group even more impressive. But it also suggests that a significant portion of patients are unlikely to stay with this recommended regimen. For those who try saline irrigation and choose not to continue it or are unwilling even to try it, saline spray is a reasonable alternative.
It should be noted that financial support for this study was provided by NeilMed Pharmaceuticals, a manufacturer of nasal saline solution and irrigation devices. However, the sponsor was not involved in the design or conduct of the study, in data collection or analysis, or in the preparation of the manuscript.
CHALLENGES TO IMPLEMENTATION: Tx may “scare away” some patients
Despite its effectiveness in reducing rhinosinusitis symptoms, performing large-volume, low-pressure nasal saline irrigation is not intuitive—and may sound downright scary to some patients. The need to learn how to perform nasal irrigation effectively, overcome the fear of water in the nasal cavity, and find the time to perform irrigation regularly can be barriers to this treatment.
A little bit of coaching can go a long way
A study by Rabago et al16 found that coached practice and patient education are effective tools in mastery of the technique ( PATIENT HANDOUT ).10,17 The researchers also found that several home strategies—incorporating nasal irrigation into the daily hygiene routine, placing the materials in a convenient location, and using warm water—facilitate regular use.
There is evidence, too, that patients who successfully use large-volume, low-pressure saline irrigation gain more than symptom relief. Rabago et al also found that effective use of this technique was associated with a sense of empowerment, and led to improved self-management skills, as well as a rapid, and long-term, improvement in quality of life.16
Saline nasal irrigation Your step-by-step guide
STEP 1: GATHER THE SUPPLIES
- - Salt (kosher, canning, or pickling salt)
- - Baking soda
- - Nasal irrigation pot (available at most pharmacies)
- - Measuring spoons
- - Container with lid
OR
- - An irrigation kit that includes the device and premixed saline packets
STEP 2: PREPARE THE SOLUTION
- - Put 1 tsp salt and ½ tsp baking soda into the container.
- - Add 1 pint of lukewarm tap water.
- - Mix contents.
- - Fill the nasal pot.
STEP 3: POSITION YOUR HEAD
- - Lean over the sink; rotate your head to one side.
- - Insert the spout of the irrigation device into the uppermost nostril.
- - Breathe through your mouth.
- - Raise the handle of the nasal pot so the solution flows into the upper nostril; in a few moments, the solution will begin to drain from the lower nostril.
- - Continue until the pot is empty, then exhale gently through both nostrils and gently blow your nose.
- - Refill the nasal pot, turn your head to the opposite side, and repeat with the other nostril.
- - Do this twice a day or as directed.
STEP 4: CLEAN AND PUT AWAY THE EQUIPMENT
- - Wash the nasal pot daily with warm water and dish detergent; rinse thoroughly.
- - Store unused saline solution in the sealed container; it can be kept at room temperature and reused for 2 days.
Adapted from: University of Wisconsin Department of Family Medicine.17
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Click here to view PURL METHODOLOGY
ILLUSTRATIVE CASE
A 45-year-old woman presents to your office with an 8-month history of nasal congestion and thick nasal discharge. Her symptoms have waxed and waned, the patient reports. She’s tried decongestants, antibiotics, and nasal steroids, with limited success. The patient has not had a recent respiratory infection, has never had sinus surgery, and does not want to be on long-term medication. You wonder if there’s an alternative treatment you can offer.
Rhinosinusitis is one of the most common conditions seen by primary care physicians in the United States, and its incidence and prevalence are increasing.2,3 While acute rhinosinusitis is usually self-limiting and resolves within a month, some patients develop chronic—and hard to treat—sinonasal symptoms.
No single cause, no definitive treatment
We’ve moved away from the notion that chronic rhinosinusitis is always a manifestation of persistent bacterial infection, and now recognize that there’s an inflammatory, nonbacterial component.4 In any given patient, several mechanisms—acting either simultaneously or independently—may contribute to sinonasal symptoms.3
Chronic sinusitis is treated in a variety of ways, including medications, immunotherapy, and surgery. Despite their limited efficacy, antibiotics and nasal steroids have been the mainstays of treatment.5 Treating underlying allergies, when they exist, may be helpful. But regardless of which treatment patients receive for chronic rhinosinusitis, many remain symptomatic.6
Benefits of saline irrigation extend beyond postop care
Otolaryngologists recommend saline irrigation after sinus surgery to clear secretions, debris, and crusts; reduce the risk of postoperative mucosal adhesions; and expedite mucosal healing.7,8 Saline irrigation is also gaining popularity as an alternative approach to chronic sinusitis symptom relief, and several randomized controlled trials (RCTs) have demonstrated both objective and subjective efficacy of this treatment for sinonasal disease.8-11
In 2007, the Cochrane Collaboration reviewed evidence for the effectiveness of nasal saline irrigation for symptoms of chronic rhinosinusitis. The reviewers concluded that it is well tolerated and beneficial, whether used alone or as an adjunctive treatment.12
Nasal saline sprays are often recommended because they’re thought to be better tolerated than other delivery modes.13 There have, however, been no comparisons of the relative efficacy of different means of saline delivery, until now.
STUDY SUMMARY: Nasal irrigation and spray go head-to-head
This study was a high-quality, prospective RCT comparing nasal spray and nasal irrigation.1 Subjects were recruited from the general population. To be eligible, participants had to be 18 years of age or older and have reported at least one of the following chronic rhinosinusitis symptoms on 4 or more days each week in the preceding 2 weeks:
- nasal stuffiness
- nasal dryness or crusting
- nasal congestion
- thick or discolored nasal discharge.
In addition, the symptoms must have been present on at least 15 of the preceding 30 days. Exclusion criteria included recent sinus surgery, a respiratory infection within the past 2 weeks, and the use of nasal saline within the past month.
Researchers enrolled 127 patients in the study; 63 were randomized to the nasal spray group and 64 to the large-volume, low-pressure irrigation group. Demographic and baseline characteristics of the groups were similar. The average ages of those in the irrigation and spray groups were 45 and 48 years, respectively. Most patients were nonsmokers and had been symptomatic for 7 to 12 months.
Twice-daily treatment. Researchers asked the patients to perform the assigned treatment twice daily for 8 weeks, but the patients were also permitted to continue using their usual medications. Symptom severity and disease-specific quality of life were assessed with the Sino-Nasal Outcome Test (SNOT-20), a 20-item survey that measures physical problems, emotional consequences, and functional limitations of sinusitis.14
The SNOT-20 is a validated, self-administered survey that asks patients to score items such as runny nose, postnasal discharge, need to blow the nose, reduced productivity, and embarrassment, on a 0- to 5-point scale (0=never, 5=always). A SNOT-20 score of 100 indicates the worst possible symptoms.
As a measure of chronicity of symptoms, patients were also asked to estimate how many months they’d had these symptoms during the last year. In addition, they were instructed to keep a diary to document treatment compliance and the use of other medications for sinonasal symptoms.
To measure outcomes, the researchers provided patients with mail-in packets so they could send in their completed SNOT-20 questionnaire and the medication diary completed at 2, 4, and 8 weeks after randomization.
Biggest improvements seen in irrigation group
Severity of symptoms. In each outcome measurement period, the saline irrigation group had lower SNOT-20 scores than the nasal spray group. At 2 weeks, the irrigation group scores were 4.4 points lower than the spray group (P=.02); at 4 weeks, the scores were 8.2 points lower (P<.001), and at 8 weeks the scores were 6.4 points lower (P=.002). Those in the irrigation group also had a significantly greater change from baseline than the patients in the spray group at 4 weeks (16.2 vs 7.4, P=.002) and at 8 weeks (15.0 vs 8.5, P=.04). The difference was marginally significant at 2 weeks (12.2 vs 6.7, P=.05).
Frequency of symptoms. At 8 weeks, 40% of the irrigation group and 61% of the nasal spray group reported nasal or sinus symptoms “often or always.” The absolute risk reduction in symptom frequency with saline irrigations, therefore, was 0.21; 95% confidence interval, 0.02-0.38 (P=.01). The odds of frequent nasal symptoms were 50% lower in the irrigation group compared to the spray group.
WHAT’S NEW: One delivery method is better than another
Prior studies had proven the effectiveness of nasal saline for reduction of rhinosinusitis symptoms. This RCT demonstrated that large-volume, low-pressure nasal irrigation brings greater symptom relief than nasal spray.
The researchers found little difference between the 2 groups in the rate of adverse effects, and reported that nasal irrigation appears to be well accepted once patients become accustomed to it. The fact that the participants were recruited from the general population further suggests that the results will be generalizable to primary care patients.
CAVEATS: High dropout rate in irrigation group
The absence of a control group prevents us from knowing the effect of saline nasal spray or irrigation compared with no treatment. In prior studies, however, nasal saline spray was found to be more effective than placebo in reducing rhinosinusitis symptoms.8,15
It is notable that a significant portion (21%) of the irrigation group abandoned this treatment by 8 weeks; in comparison, just 7% of the nasal spray group discontinued treatment.
This lower rate of adherence makes the beneficial effects of the irrigation group even more impressive. But it also suggests that a significant portion of patients are unlikely to stay with this recommended regimen. For those who try saline irrigation and choose not to continue it or are unwilling even to try it, saline spray is a reasonable alternative.
It should be noted that financial support for this study was provided by NeilMed Pharmaceuticals, a manufacturer of nasal saline solution and irrigation devices. However, the sponsor was not involved in the design or conduct of the study, in data collection or analysis, or in the preparation of the manuscript.
CHALLENGES TO IMPLEMENTATION: Tx may “scare away” some patients
Despite its effectiveness in reducing rhinosinusitis symptoms, performing large-volume, low-pressure nasal saline irrigation is not intuitive—and may sound downright scary to some patients. The need to learn how to perform nasal irrigation effectively, overcome the fear of water in the nasal cavity, and find the time to perform irrigation regularly can be barriers to this treatment.
A little bit of coaching can go a long way
A study by Rabago et al16 found that coached practice and patient education are effective tools in mastery of the technique ( PATIENT HANDOUT ).10,17 The researchers also found that several home strategies—incorporating nasal irrigation into the daily hygiene routine, placing the materials in a convenient location, and using warm water—facilitate regular use.
There is evidence, too, that patients who successfully use large-volume, low-pressure saline irrigation gain more than symptom relief. Rabago et al also found that effective use of this technique was associated with a sense of empowerment, and led to improved self-management skills, as well as a rapid, and long-term, improvement in quality of life.16
Saline nasal irrigation Your step-by-step guide
STEP 1: GATHER THE SUPPLIES
- - Salt (kosher, canning, or pickling salt)
- - Baking soda
- - Nasal irrigation pot (available at most pharmacies)
- - Measuring spoons
- - Container with lid
OR
- - An irrigation kit that includes the device and premixed saline packets
STEP 2: PREPARE THE SOLUTION
- - Put 1 tsp salt and ½ tsp baking soda into the container.
- - Add 1 pint of lukewarm tap water.
- - Mix contents.
- - Fill the nasal pot.
STEP 3: POSITION YOUR HEAD
- - Lean over the sink; rotate your head to one side.
- - Insert the spout of the irrigation device into the uppermost nostril.
- - Breathe through your mouth.
- - Raise the handle of the nasal pot so the solution flows into the upper nostril; in a few moments, the solution will begin to drain from the lower nostril.
- - Continue until the pot is empty, then exhale gently through both nostrils and gently blow your nose.
- - Refill the nasal pot, turn your head to the opposite side, and repeat with the other nostril.
- - Do this twice a day or as directed.
STEP 4: CLEAN AND PUT AWAY THE EQUIPMENT
- - Wash the nasal pot daily with warm water and dish detergent; rinse thoroughly.
- - Store unused saline solution in the sealed container; it can be kept at room temperature and reused for 2 days.
Adapted from: University of Wisconsin Department of Family Medicine.17
Acknowledgement
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Click here to view PURL METHODOLOGY
1. Pynnonen MA, Mukerji SS, Kim HM, et al. Nasal saline for chronic sinonasal symptoms: a randomized controlled trial. Arch Otolaryngol Head Neck Surg. 2007;133:11115-1120.
2. Gliklich RE, Metson R. Economic implications of chronic sinusitis. Otolaryngol Head Neck Surg. 1998;118(3 Pt 1):344-349.
3. International Rhinosinusitis Advisory Board. Infectious rhinosinusitis in adults classification, etiology and management. Ear Nose Throat J. 1997;76(12 suppl):s5-s22.
4. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):s1-s7.
5. Sharp HJ, Denman D, Puumala S, et al. Treatment of acute and chronic rhinosinusitis in the United States, 1999-2002. Arch Otolaryngol Head Neck Surg. 2007;133:260-265.
6. Subramanian HN, Schechtman KB, Hamilos DL. A retrospective analysis of treatment outcomes and time to relapse after intensive medical treatment for chronic sinusitis. Am J Rhinol. 2002;16:303-312.
7. Druce HM. Adjuncts to medical management of sinusitis. Otolaryngol Head Neck Surg. 1990;103(5 Pt 2):880-883.
8. Tomooka LT, Murphy C, Davidson TM. Clinical study and literature review of nasal irrigation. Laryngoscope. 2000;110:1189-1193.
9. Heatley DG, McConnell KE, Kille TL, et al. Nasal irrigation for the alleviation of sinonasal symptoms. Otolaryngol Head Neck Surg. 2001;125:44-48.
10. Rabago D, Zgierska A, Mundt M, et al. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51:1049-1055.
11. Taccariello M, Parikh A, Darby Y, et al. Nasal douching as a valuable adjunct in the management of chronic rhinosinusitis. Rhinology. 1999;37:29-32.
12. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.-
13. Keojampa BK, Nguyen MH, Ryan MW. Effects of buffered saline solution on nasal mucociliary clearance and nasal airway patency. Otolaryngol Head Neck Surg. 2004;131:679-682.
14. Piccirillo JF, Merritt MG, Jr, Richards ML. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002;126:41-47.
15. Hauptman G, Ryan MW. The effect of saline solutions on nasal patency and mucociliary clearance in rhinosinusitis patients. Otolaryngol Head Neck Surg. 2007;137:815-821.
16. Rabago D, Barrett B, Marchand L, et al. Qualitative aspects of nasal irrigation use by patients with chronic sinus disease in a multimethod study. Ann Fam Med. 2006;4:295-301.
17. University of Wisconsin Department of Family Medicine. Nasal Irrigation Instructions. Available at: http://www.fammed.wisc.edu/files/webfm-uploads/documents/research/nasalirrigationinstructions.pdf. Accessed December 1, 2008.
1. Pynnonen MA, Mukerji SS, Kim HM, et al. Nasal saline for chronic sinonasal symptoms: a randomized controlled trial. Arch Otolaryngol Head Neck Surg. 2007;133:11115-1120.
2. Gliklich RE, Metson R. Economic implications of chronic sinusitis. Otolaryngol Head Neck Surg. 1998;118(3 Pt 1):344-349.
3. International Rhinosinusitis Advisory Board. Infectious rhinosinusitis in adults classification, etiology and management. Ear Nose Throat J. 1997;76(12 suppl):s5-s22.
4. Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):s1-s7.
5. Sharp HJ, Denman D, Puumala S, et al. Treatment of acute and chronic rhinosinusitis in the United States, 1999-2002. Arch Otolaryngol Head Neck Surg. 2007;133:260-265.
6. Subramanian HN, Schechtman KB, Hamilos DL. A retrospective analysis of treatment outcomes and time to relapse after intensive medical treatment for chronic sinusitis. Am J Rhinol. 2002;16:303-312.
7. Druce HM. Adjuncts to medical management of sinusitis. Otolaryngol Head Neck Surg. 1990;103(5 Pt 2):880-883.
8. Tomooka LT, Murphy C, Davidson TM. Clinical study and literature review of nasal irrigation. Laryngoscope. 2000;110:1189-1193.
9. Heatley DG, McConnell KE, Kille TL, et al. Nasal irrigation for the alleviation of sinonasal symptoms. Otolaryngol Head Neck Surg. 2001;125:44-48.
10. Rabago D, Zgierska A, Mundt M, et al. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: a randomized controlled trial. J Fam Pract. 2002;51:1049-1055.
11. Taccariello M, Parikh A, Darby Y, et al. Nasal douching as a valuable adjunct in the management of chronic rhinosinusitis. Rhinology. 1999;37:29-32.
12. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.-
13. Keojampa BK, Nguyen MH, Ryan MW. Effects of buffered saline solution on nasal mucociliary clearance and nasal airway patency. Otolaryngol Head Neck Surg. 2004;131:679-682.
14. Piccirillo JF, Merritt MG, Jr, Richards ML. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002;126:41-47.
15. Hauptman G, Ryan MW. The effect of saline solutions on nasal patency and mucociliary clearance in rhinosinusitis patients. Otolaryngol Head Neck Surg. 2007;137:815-821.
16. Rabago D, Barrett B, Marchand L, et al. Qualitative aspects of nasal irrigation use by patients with chronic sinus disease in a multimethod study. Ann Fam Med. 2006;4:295-301.
17. University of Wisconsin Department of Family Medicine. Nasal Irrigation Instructions. Available at: http://www.fammed.wisc.edu/files/webfm-uploads/documents/research/nasalirrigationinstructions.pdf. Accessed December 1, 2008.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
ACE inhibitors and ARBs: One or the other—not both—for high-risk patients
Avoid prescribing an angiotensin-converting enzyme (ACE) inhibitor and an angiotensin receptor blocker (ARB) for patients at high risk of vascular events or renal dysfunction. The combination does not reduce poor outcomes, and leads to more adverse drug-related events than an ACE inhibitor or ARB alone.1
Strength of recommendation
B: 1 large, high-quality randomized controlled trial (RCT).
The ONTARGET investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559.
ILLUSTRATIVE CASE
A 56-year-old patient with well-controlled type 2 diabetes and hypertension comes to see you for routine follow up. His blood pressure is controlled with lisinopril 40 mg/d. But his albumin-to-creatinine ratio is 75 mg/g, and your records reveal that his albuminuria is getting progressively worse.
You’re aware of the potential benefits of a dual angiotensin blockade, and are considering adding an angiotensin receptor blocker (ARB) to your patient’s medication regimen. You wonder whether the combination of an angiotensin-converting enzyme (ACE) inhibitor and an ARB will slow the decline of renal function. You also wonder whether the combination will reduce your patient’s cardiovascular risk.
ACE inhibitors are known to reduce cardiovascular morbidity and mortality, as well as proteinuria in patients with vascular disease or diabetes, whether or not they have heart failure.2 But few studies have compared the effects of ACE inhibitors and ARBs in high-risk patients without heart failure. Nor has there been a definitive study of the effects of an ACE inhibitor–ARB combination on proteinuria and cardiovascular risk.
Are 2 drugs better than 1?
In a recent meta-analysis, researchers reported that combination therapy had a beneficial effect on proteinuria.3 But that observation was based on a small number of patients (N=309 from 10 studies), short follow up, and a lack of data on key clinical end points such as decline of the glomerular filtration rate (GFR) and the onset of dialysis.
Other evidence comes from a study of 199 patients with diabetes and microalbuminuria, in which the ACE inhibitor-ARB combination reduced proteinuria more than either agent alone.4 And in a study of 336 patients with nondiabetic nephropathy, the 2-drug combination slowed the decline in renal function more than monotherapy.5
Small studies raise hopes. These preliminary findings, along with the theoretical benefits of dual angiotensin blockade, suggested that the benefits of taking both agents together could be significant. A large, well-done randomized controlled trial (RCT) was needed to determine the following: (1) whether an ARB is as effective as an ACE inhibitor in reducing morbidity and mortality in high-risk patients who don’t have heart failure, and (2) whether the ACE inhibitor–ARB combination is better than monotherapy for patients at high risk.
The ONTARGET study:
- established that telmisartan, an ARB, is not inferior to ramipril, an ACE inhibitor, in reducing cardiovascular and renal events in high-risk patients without heart failure.
- found that either drug alone is more effective than combination therapy for this patient population.
- cast fresh doubt on the assumption that proteinuria is an accurate surrogate marker for progressive renal dysfunction.
STUDY SUMMARY: Vascular outcomes same for ACE inhibitors, ARBs
The ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET), a multi-year study of thousands of patients, addressed both of those questions. The researchers compared the effects of both telmisartan (Micardis, an ARB) alone and a telmisartan + ramipril (Altace, an ACE inhibitor) combination with the effects of the ACE inhibitor alone in patients ≥55 years of age with established atherosclerotic vascular disease or diabetes with end-organ damage.1 Exclusion criteria included major renal artery stenosis, uncorrected volume or sodium depletion, a serum creatinine concentration of ≥3 mg/dL, and uncontrolled hypertension (>160 mm Hg systolic or >100 mm Hg diastolic).
After a 3-week run-in period to eliminate those who were unable to tolerate either medication or were nonadherent, a total of 25,620 patients remained. They were randomly assigned to take ramipril 10 mg/d, telmisartan 80 mg/d, or both the ACE inhibitor and the ARB. The researchers followed the patients for a median of 56 months.
The primary composite outcome was death from cardiovascular causes, myocardial infarction, stroke, or hospitalization for heart failure;1 the main renal outcome was a composite of first dialysis, doubling of serum creatinine, or death.6
The percentage of patients with the primary outcome was the same in all 3 groups (~16.5%). This finding was somewhat surprising because the blood pressure of patients in the combination therapy group was 2 to 3 mm Hg lower overall (both systolic and diastolic) than the blood pressure of patients on monotherapy—a difference that in other studies has been associated with an estimated 4% to 5% reduction in risk.1,2 Patients in the combination group had more hypotensive symptoms compared with those in the ramipril group (4.8% vs 1.7%, number needed to harm [NNH]=32, P<.001).
Renal dysfunction was highest in dual therapy group
Patients in the combination therapy group had higher rates of renal dysfunction than either the ramipril group (13.5% vs 10.2%, NNH=30, P<.001) or the telmisartan group (10.6%), despite a decrease in proteinuria among those on dual therapy. Patients taking the 2-drug combination also had higher rates of hyperkalemia.
While telmisartan proved to be equal to ramipril in reducing vascular events in high-risk patients, patients taking the ACE inhibitor experienced more cough (NNH=32, P<.001) and angioedema (NNH=500, P=.01). In both monotherapy groups, the rates of adverse drug reactions were probably lower than what we typically see in clinical practice because after the run-in period, only patients who were better able to tolerate both medications remained.
WHAT’S NEW: Combination causes renal impairment
This study established that telmisartan, an ARB, is not inferior to ramipril, an ACE inhibitor, in reducing cardiovascular and renal events in patients without heart failure. In addition, as the largest RCT to explore the effects of a dual blockade of the renin-angiotensin system with an ACE inhibitor and an ARB, it casts fresh doubt on the assumption that proteinuria is an accurate surrogate marker for progressive renal dysfunction. The reduction in proteinuria seen in patients in the combination therapy group came at a cost of increased renal impairment.
CAVEATS: Findings do not apply to heart failure patients
More than 11% of potential subjects were excluded from this study during the run-in period. This suggests that physicians in practice are likely to find a significant number of patients who are unable to tolerate (or fail to adhere to) monotherapy with ACE inhibitors or ARBs.
At baseline, only a small subgroup—13%—had overt diabetic nephropathy, the hallmark for a substantial continuous decline of GFR. However, 38% of the study group had diabetes, and almost 30% of these diabetes patients had microalbuminuria. Subgroup analysis found results consistent with the overall group, and the large sample size reduces the likelihood that these findings were due to low power. The overall rate of dialysis and doubling of serum creatinine was low, but still statistically significant, due to the large size of this study.
In determining treatment for high-risk patients with vascular disease or diabetes, it is important to keep the study population in mind. Studies of patients with poorly controlled congestive heart failure (CHF) have shown potential benefits from an ACE inhibitor–ARB combination.7 The ONTARGET trial specifically excluded individuals with CHF, and its findings—and recommendations to avoid combination therapy—should not be applied to heart failure patients.
CHALLENGES TO IMPLEMENTATION: Best microalbuminuria Tx remains elusive
Although albuminuria has been considered an early sign of the onset of diabetic nephropathy, the ONTARGET study demonstrated that combination therapy may cause further reduction in albuminuria but still adversely affect renal function. Thus, this study raises important questions about the best treatment for patients with diabetes who have microalbuminuria and are already on either an ACE inhibitor or an ARB. We wonder, too, whether we should continue to test for microalbuminuria in patients who are taking one of these agents, given the lack of guidance regarding further treatment.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Click here to view PURL METHODOLOGY
1. The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559.
2. Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145-153.
3. Jennings DL, Kalus JS, Coleman CI, et al. Combination therapy with an ACE inhibitor and an angiotensin receptor blocker for diabetic nephropathy: a meta-analysis. Diabet Med. 2007;24:486-493.
4. Mogensen CE, Neldam S, Tikkanen I, et al. Randomised controlled trial of dual blockade of renin-angiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ. 2000;321:1440-1444.
5. Nakao N, Yoshimura A, Morita H, et al. Combination treatment of angiotensin-II receptor blocker and angiotensin-converting-enzyme inhibitor in non-diabetic renal disease (COOPERATE): a randomised controlled trial. Lancet. 2003;361:117-124.
6. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372:547-553.
7. Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667-1675.
Avoid prescribing an angiotensin-converting enzyme (ACE) inhibitor and an angiotensin receptor blocker (ARB) for patients at high risk of vascular events or renal dysfunction. The combination does not reduce poor outcomes, and leads to more adverse drug-related events than an ACE inhibitor or ARB alone.1
Strength of recommendation
B: 1 large, high-quality randomized controlled trial (RCT).
The ONTARGET investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559.
ILLUSTRATIVE CASE
A 56-year-old patient with well-controlled type 2 diabetes and hypertension comes to see you for routine follow up. His blood pressure is controlled with lisinopril 40 mg/d. But his albumin-to-creatinine ratio is 75 mg/g, and your records reveal that his albuminuria is getting progressively worse.
You’re aware of the potential benefits of a dual angiotensin blockade, and are considering adding an angiotensin receptor blocker (ARB) to your patient’s medication regimen. You wonder whether the combination of an angiotensin-converting enzyme (ACE) inhibitor and an ARB will slow the decline of renal function. You also wonder whether the combination will reduce your patient’s cardiovascular risk.
ACE inhibitors are known to reduce cardiovascular morbidity and mortality, as well as proteinuria in patients with vascular disease or diabetes, whether or not they have heart failure.2 But few studies have compared the effects of ACE inhibitors and ARBs in high-risk patients without heart failure. Nor has there been a definitive study of the effects of an ACE inhibitor–ARB combination on proteinuria and cardiovascular risk.
Are 2 drugs better than 1?
In a recent meta-analysis, researchers reported that combination therapy had a beneficial effect on proteinuria.3 But that observation was based on a small number of patients (N=309 from 10 studies), short follow up, and a lack of data on key clinical end points such as decline of the glomerular filtration rate (GFR) and the onset of dialysis.
Other evidence comes from a study of 199 patients with diabetes and microalbuminuria, in which the ACE inhibitor-ARB combination reduced proteinuria more than either agent alone.4 And in a study of 336 patients with nondiabetic nephropathy, the 2-drug combination slowed the decline in renal function more than monotherapy.5
Small studies raise hopes. These preliminary findings, along with the theoretical benefits of dual angiotensin blockade, suggested that the benefits of taking both agents together could be significant. A large, well-done randomized controlled trial (RCT) was needed to determine the following: (1) whether an ARB is as effective as an ACE inhibitor in reducing morbidity and mortality in high-risk patients who don’t have heart failure, and (2) whether the ACE inhibitor–ARB combination is better than monotherapy for patients at high risk.
The ONTARGET study:
- established that telmisartan, an ARB, is not inferior to ramipril, an ACE inhibitor, in reducing cardiovascular and renal events in high-risk patients without heart failure.
- found that either drug alone is more effective than combination therapy for this patient population.
- cast fresh doubt on the assumption that proteinuria is an accurate surrogate marker for progressive renal dysfunction.
STUDY SUMMARY: Vascular outcomes same for ACE inhibitors, ARBs
The ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET), a multi-year study of thousands of patients, addressed both of those questions. The researchers compared the effects of both telmisartan (Micardis, an ARB) alone and a telmisartan + ramipril (Altace, an ACE inhibitor) combination with the effects of the ACE inhibitor alone in patients ≥55 years of age with established atherosclerotic vascular disease or diabetes with end-organ damage.1 Exclusion criteria included major renal artery stenosis, uncorrected volume or sodium depletion, a serum creatinine concentration of ≥3 mg/dL, and uncontrolled hypertension (>160 mm Hg systolic or >100 mm Hg diastolic).
After a 3-week run-in period to eliminate those who were unable to tolerate either medication or were nonadherent, a total of 25,620 patients remained. They were randomly assigned to take ramipril 10 mg/d, telmisartan 80 mg/d, or both the ACE inhibitor and the ARB. The researchers followed the patients for a median of 56 months.
The primary composite outcome was death from cardiovascular causes, myocardial infarction, stroke, or hospitalization for heart failure;1 the main renal outcome was a composite of first dialysis, doubling of serum creatinine, or death.6
The percentage of patients with the primary outcome was the same in all 3 groups (~16.5%). This finding was somewhat surprising because the blood pressure of patients in the combination therapy group was 2 to 3 mm Hg lower overall (both systolic and diastolic) than the blood pressure of patients on monotherapy—a difference that in other studies has been associated with an estimated 4% to 5% reduction in risk.1,2 Patients in the combination group had more hypotensive symptoms compared with those in the ramipril group (4.8% vs 1.7%, number needed to harm [NNH]=32, P<.001).
Renal dysfunction was highest in dual therapy group
Patients in the combination therapy group had higher rates of renal dysfunction than either the ramipril group (13.5% vs 10.2%, NNH=30, P<.001) or the telmisartan group (10.6%), despite a decrease in proteinuria among those on dual therapy. Patients taking the 2-drug combination also had higher rates of hyperkalemia.
While telmisartan proved to be equal to ramipril in reducing vascular events in high-risk patients, patients taking the ACE inhibitor experienced more cough (NNH=32, P<.001) and angioedema (NNH=500, P=.01). In both monotherapy groups, the rates of adverse drug reactions were probably lower than what we typically see in clinical practice because after the run-in period, only patients who were better able to tolerate both medications remained.
WHAT’S NEW: Combination causes renal impairment
This study established that telmisartan, an ARB, is not inferior to ramipril, an ACE inhibitor, in reducing cardiovascular and renal events in patients without heart failure. In addition, as the largest RCT to explore the effects of a dual blockade of the renin-angiotensin system with an ACE inhibitor and an ARB, it casts fresh doubt on the assumption that proteinuria is an accurate surrogate marker for progressive renal dysfunction. The reduction in proteinuria seen in patients in the combination therapy group came at a cost of increased renal impairment.
CAVEATS: Findings do not apply to heart failure patients
More than 11% of potential subjects were excluded from this study during the run-in period. This suggests that physicians in practice are likely to find a significant number of patients who are unable to tolerate (or fail to adhere to) monotherapy with ACE inhibitors or ARBs.
At baseline, only a small subgroup—13%—had overt diabetic nephropathy, the hallmark for a substantial continuous decline of GFR. However, 38% of the study group had diabetes, and almost 30% of these diabetes patients had microalbuminuria. Subgroup analysis found results consistent with the overall group, and the large sample size reduces the likelihood that these findings were due to low power. The overall rate of dialysis and doubling of serum creatinine was low, but still statistically significant, due to the large size of this study.
In determining treatment for high-risk patients with vascular disease or diabetes, it is important to keep the study population in mind. Studies of patients with poorly controlled congestive heart failure (CHF) have shown potential benefits from an ACE inhibitor–ARB combination.7 The ONTARGET trial specifically excluded individuals with CHF, and its findings—and recommendations to avoid combination therapy—should not be applied to heart failure patients.
CHALLENGES TO IMPLEMENTATION: Best microalbuminuria Tx remains elusive
Although albuminuria has been considered an early sign of the onset of diabetic nephropathy, the ONTARGET study demonstrated that combination therapy may cause further reduction in albuminuria but still adversely affect renal function. Thus, this study raises important questions about the best treatment for patients with diabetes who have microalbuminuria and are already on either an ACE inhibitor or an ARB. We wonder, too, whether we should continue to test for microalbuminuria in patients who are taking one of these agents, given the lack of guidance regarding further treatment.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Click here to view PURL METHODOLOGY
Avoid prescribing an angiotensin-converting enzyme (ACE) inhibitor and an angiotensin receptor blocker (ARB) for patients at high risk of vascular events or renal dysfunction. The combination does not reduce poor outcomes, and leads to more adverse drug-related events than an ACE inhibitor or ARB alone.1
Strength of recommendation
B: 1 large, high-quality randomized controlled trial (RCT).
The ONTARGET investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559.
ILLUSTRATIVE CASE
A 56-year-old patient with well-controlled type 2 diabetes and hypertension comes to see you for routine follow up. His blood pressure is controlled with lisinopril 40 mg/d. But his albumin-to-creatinine ratio is 75 mg/g, and your records reveal that his albuminuria is getting progressively worse.
You’re aware of the potential benefits of a dual angiotensin blockade, and are considering adding an angiotensin receptor blocker (ARB) to your patient’s medication regimen. You wonder whether the combination of an angiotensin-converting enzyme (ACE) inhibitor and an ARB will slow the decline of renal function. You also wonder whether the combination will reduce your patient’s cardiovascular risk.
ACE inhibitors are known to reduce cardiovascular morbidity and mortality, as well as proteinuria in patients with vascular disease or diabetes, whether or not they have heart failure.2 But few studies have compared the effects of ACE inhibitors and ARBs in high-risk patients without heart failure. Nor has there been a definitive study of the effects of an ACE inhibitor–ARB combination on proteinuria and cardiovascular risk.
Are 2 drugs better than 1?
In a recent meta-analysis, researchers reported that combination therapy had a beneficial effect on proteinuria.3 But that observation was based on a small number of patients (N=309 from 10 studies), short follow up, and a lack of data on key clinical end points such as decline of the glomerular filtration rate (GFR) and the onset of dialysis.
Other evidence comes from a study of 199 patients with diabetes and microalbuminuria, in which the ACE inhibitor-ARB combination reduced proteinuria more than either agent alone.4 And in a study of 336 patients with nondiabetic nephropathy, the 2-drug combination slowed the decline in renal function more than monotherapy.5
Small studies raise hopes. These preliminary findings, along with the theoretical benefits of dual angiotensin blockade, suggested that the benefits of taking both agents together could be significant. A large, well-done randomized controlled trial (RCT) was needed to determine the following: (1) whether an ARB is as effective as an ACE inhibitor in reducing morbidity and mortality in high-risk patients who don’t have heart failure, and (2) whether the ACE inhibitor–ARB combination is better than monotherapy for patients at high risk.
The ONTARGET study:
- established that telmisartan, an ARB, is not inferior to ramipril, an ACE inhibitor, in reducing cardiovascular and renal events in high-risk patients without heart failure.
- found that either drug alone is more effective than combination therapy for this patient population.
- cast fresh doubt on the assumption that proteinuria is an accurate surrogate marker for progressive renal dysfunction.
STUDY SUMMARY: Vascular outcomes same for ACE inhibitors, ARBs
The ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET), a multi-year study of thousands of patients, addressed both of those questions. The researchers compared the effects of both telmisartan (Micardis, an ARB) alone and a telmisartan + ramipril (Altace, an ACE inhibitor) combination with the effects of the ACE inhibitor alone in patients ≥55 years of age with established atherosclerotic vascular disease or diabetes with end-organ damage.1 Exclusion criteria included major renal artery stenosis, uncorrected volume or sodium depletion, a serum creatinine concentration of ≥3 mg/dL, and uncontrolled hypertension (>160 mm Hg systolic or >100 mm Hg diastolic).
After a 3-week run-in period to eliminate those who were unable to tolerate either medication or were nonadherent, a total of 25,620 patients remained. They were randomly assigned to take ramipril 10 mg/d, telmisartan 80 mg/d, or both the ACE inhibitor and the ARB. The researchers followed the patients for a median of 56 months.
The primary composite outcome was death from cardiovascular causes, myocardial infarction, stroke, or hospitalization for heart failure;1 the main renal outcome was a composite of first dialysis, doubling of serum creatinine, or death.6
The percentage of patients with the primary outcome was the same in all 3 groups (~16.5%). This finding was somewhat surprising because the blood pressure of patients in the combination therapy group was 2 to 3 mm Hg lower overall (both systolic and diastolic) than the blood pressure of patients on monotherapy—a difference that in other studies has been associated with an estimated 4% to 5% reduction in risk.1,2 Patients in the combination group had more hypotensive symptoms compared with those in the ramipril group (4.8% vs 1.7%, number needed to harm [NNH]=32, P<.001).
Renal dysfunction was highest in dual therapy group
Patients in the combination therapy group had higher rates of renal dysfunction than either the ramipril group (13.5% vs 10.2%, NNH=30, P<.001) or the telmisartan group (10.6%), despite a decrease in proteinuria among those on dual therapy. Patients taking the 2-drug combination also had higher rates of hyperkalemia.
While telmisartan proved to be equal to ramipril in reducing vascular events in high-risk patients, patients taking the ACE inhibitor experienced more cough (NNH=32, P<.001) and angioedema (NNH=500, P=.01). In both monotherapy groups, the rates of adverse drug reactions were probably lower than what we typically see in clinical practice because after the run-in period, only patients who were better able to tolerate both medications remained.
WHAT’S NEW: Combination causes renal impairment
This study established that telmisartan, an ARB, is not inferior to ramipril, an ACE inhibitor, in reducing cardiovascular and renal events in patients without heart failure. In addition, as the largest RCT to explore the effects of a dual blockade of the renin-angiotensin system with an ACE inhibitor and an ARB, it casts fresh doubt on the assumption that proteinuria is an accurate surrogate marker for progressive renal dysfunction. The reduction in proteinuria seen in patients in the combination therapy group came at a cost of increased renal impairment.
CAVEATS: Findings do not apply to heart failure patients
More than 11% of potential subjects were excluded from this study during the run-in period. This suggests that physicians in practice are likely to find a significant number of patients who are unable to tolerate (or fail to adhere to) monotherapy with ACE inhibitors or ARBs.
At baseline, only a small subgroup—13%—had overt diabetic nephropathy, the hallmark for a substantial continuous decline of GFR. However, 38% of the study group had diabetes, and almost 30% of these diabetes patients had microalbuminuria. Subgroup analysis found results consistent with the overall group, and the large sample size reduces the likelihood that these findings were due to low power. The overall rate of dialysis and doubling of serum creatinine was low, but still statistically significant, due to the large size of this study.
In determining treatment for high-risk patients with vascular disease or diabetes, it is important to keep the study population in mind. Studies of patients with poorly controlled congestive heart failure (CHF) have shown potential benefits from an ACE inhibitor–ARB combination.7 The ONTARGET trial specifically excluded individuals with CHF, and its findings—and recommendations to avoid combination therapy—should not be applied to heart failure patients.
CHALLENGES TO IMPLEMENTATION: Best microalbuminuria Tx remains elusive
Although albuminuria has been considered an early sign of the onset of diabetic nephropathy, the ONTARGET study demonstrated that combination therapy may cause further reduction in albuminuria but still adversely affect renal function. Thus, this study raises important questions about the best treatment for patients with diabetes who have microalbuminuria and are already on either an ACE inhibitor or an ARB. We wonder, too, whether we should continue to test for microalbuminuria in patients who are taking one of these agents, given the lack of guidance regarding further treatment.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
PURLs methodology
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Click here to view PURL METHODOLOGY
1. The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559.
2. Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145-153.
3. Jennings DL, Kalus JS, Coleman CI, et al. Combination therapy with an ACE inhibitor and an angiotensin receptor blocker for diabetic nephropathy: a meta-analysis. Diabet Med. 2007;24:486-493.
4. Mogensen CE, Neldam S, Tikkanen I, et al. Randomised controlled trial of dual blockade of renin-angiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ. 2000;321:1440-1444.
5. Nakao N, Yoshimura A, Morita H, et al. Combination treatment of angiotensin-II receptor blocker and angiotensin-converting-enzyme inhibitor in non-diabetic renal disease (COOPERATE): a randomised controlled trial. Lancet. 2003;361:117-124.
6. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372:547-553.
7. Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667-1675.
1. The ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559.
2. Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000;342:145-153.
3. Jennings DL, Kalus JS, Coleman CI, et al. Combination therapy with an ACE inhibitor and an angiotensin receptor blocker for diabetic nephropathy: a meta-analysis. Diabet Med. 2007;24:486-493.
4. Mogensen CE, Neldam S, Tikkanen I, et al. Randomised controlled trial of dual blockade of renin-angiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ. 2000;321:1440-1444.
5. Nakao N, Yoshimura A, Morita H, et al. Combination treatment of angiotensin-II receptor blocker and angiotensin-converting-enzyme inhibitor in non-diabetic renal disease (COOPERATE): a randomised controlled trial. Lancet. 2003;361:117-124.
6. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008;372:547-553.
7. Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667-1675.
Copyright © 2009 The Family Physicians Inquiries Network.
All rights reserved.
Antidepressants causing sexual problems? Give her Viagra
Tell women for whom you prescribe selective and nonselective serotonin reuptake inhibitors (SRIs) to let you know if they develop sexual dysfunction. Offer sildenafil (50 mg with the option to increase to 100 mg) to premenopausal women on stable, effective doses of SRIs who experience this common—and treatable—side effect.1
Strength of recommendation
B: One high-quality RCT that confirms smaller, open-label studies
Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300:395-404.
ILLUSTRATIVE CASE
A 34-year-old woman comes to your office and asks to be taken off the paroxetine you prescribed for her 4 months ago. The medication is working well; her depression has been in remission for at least 12 weeks. But she no longer enjoys sex. She used to have a healthy libido and satisfying arousal and orgasm, but since starting the antidepressant, her sexual interest and pleasure have been low.
Although she’s afraid of sinking back into a depression without the medication, she’s willing to take the risk. If she were your patient, what alternatives would you suggest?
Sexual dysfunction affects an estimated 30% to 50% of patients on selective and nonselective SRIs, and some studies report rates as high as 70% to 80%.2 Many patients stop taking these antidepressants prematurely, often because of sexual side effects.3,4
Phosphodiesterase type 5 (PDE-5) inhibitors are well established as an effective treatment for erectile dysfunction,5 and randomized controlled trials (RCTs) have shown sildenafil to be effective in treating male SRI-induced sexual impairment.6,7 For women, there has been no parallel evidence-based treatment.
Limited options, with little support
Typically, women who reported antidepressant-associated sexual disturbances have been offered options for which there was only weak evidence—dose changes or augmentation with another agent, switching to another antidepressant, or taking occasional drug holidays. A 2004 Cochrane review found that there were no RCTs involving dose changes or drug holidays.8 Among studies of the efficacy of switching to a different drug, nefazodone was the only agent whose use was supported by a double-blind RCT.9 Augmentation trials of a wide range of medications and supplements—including amantadine, bupropion, buspirone, granisetron, mirtazapine, olanzapine, ephedrine, ginkgo biloba, and yohimbine—yielded mixed results. Indeed, the research found that some were no better than placebo.
PDE-5 inhibitors for women? Inconclusive studies to date
Female sexual dysfunction is generally divided into 4 domains: disorders of desire, arousal, orgasm, or pain. Decreased desire and delayed or absent orgasm are the most common sexual side effects of SRI antidepressants in women.10 Several studies of PDE-5 inhibitors in this patient population have had positive results,11-15 so there has been good reason to think that they might help this subset of women. However, all the studies were small and nonblinded, and therefore inconclusive—until now.
STUDY SUMMARY: Finally, a well-done RCT provides some answers
Investigators enrolled 98 premenopausal women from 7 US research centers in a double-blind randomized trial. To qualify, participants had to be diagnosed with major depression in remission, be taking a selective or nonselective SRI for >8 weeks, and be on a stable dose for >4 weeks. They also had to meet Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria for substance-induced sexual dysfunction lasting >4 weeks, but have no history of sexual impairment independent of antidepressants. Finally, participants had to engage in some form of regular sexual activity—intercourse, oral sex, and masturbation all qualified—at least twice a month, and be willing to continue efforts to have sex at least once a week during the study. Women with other medical, psychiatric, or sexual problems were excluded, as were those who were pregnant, breastfeeding, or able to become pregnant and not using reliable contraception.
Participants were randomized to receive 50 mg of sildenafil (n=49) or a matching placebo tablet (n=49), which they were instructed to take 1 to 2 hours before sexual activity. The dose could be adjusted to 2 tablets (100 mg sildenafil) based on investigator assessment of the patient’s response to the initial dose. Participants and all study personnel were blinded to group assignment.
The primary outcome was change from baseline to end-point in the Clinical Global Impression Scale, a clinician-rated scale based on review of patient symptoms that was adapted to evaluate sexual function. Secondary outcomes were changes in 3 other sexual function scales, the Hamilton Rating Scale for Depression, and measured hormone levels.
Investigators followed the women for 8 weeks, measuring outcomes at 2, 4, and 8 weeks.
Sildenafil is better than placebo
Using an intention-to-treat analysis with the last measurement (2, 4, or 8 weeks) as the end-point, both the treatment and placebo groups experienced improvement in sexual function. The sildenafil group improved more than the placebo group. On the Clinical Global Impression Scale (1 to 7, with higher scores indicating worse sexual function), sildenafil users went from a mean of 4.8 to 2.8, while placebo users went from a mean of 4.7 to 3.6. The difference in mean change from baseline was 0.8 (95% confidence interval [CI] 0.6-1.0; P=.001). Using a more conservative analysis in which participants who did not return for the 8-week follow-up visit were assumed to have returned to baseline, the difference in mean change from baseline was smaller (0.6, 95% CI, 0.3-0.8; P=0.03) but still statistically significant.
Orgasmic function shows significant improvement
The sexual function scales used as secondary outcomes provided more detail about which types of sexual dysfunction benefited from sildenafil. On all 3 scales, orgasmic function significantly favored sildenafil over placebo. In the domains of desire, arousal, and pain disorders, small to moderate improvements were seen in both groups, with no statistically significant differences. One potential confounder—a difference in the course of participants’ underlying depression— was ruled out because depression scale results remained unchanged from baseline to endpoint in both groups.
Baseline levels of cortisone, estradiol, follicle-stimulating hormone, leuteinizing hormone, progesterone, prolactin, sex hormone-binding globulin, testosterone, thyroid-stimulating hormone, and thyroxine, were normal, with no differences between the sildenafil and placebo groups.
WHAT’S NEW: Women have an evidence-based option
Like their male counterparts, we can now offer women whose depression is effectively treated by SRI antidepressants—and who are motivated to stay sexually active despite medication-associated side effects—an effective pharmacotherapeutic treatment.
CAVEATS: Side effects and study funding are worth noting
Side effects. Significantly more participants in the sildenafil group vs the placebo group experienced the following side effects: headache (43% vs 27%), visual disturbance (14% vs 2%), dyspepsia (12% vs 0%), flushing (24% vs 0%), nasal congestion (37% vs 6%), and palpitations (8% vs 2%). Nausea was the only side effect that was more common in the placebo group, reported by only 2% of those in the intervention group but 16% of those on placebo.
No serious adverse events occurred, however, and the medication appears to have been well tolerated overall, despite relatively high rates of side effects. Participants in the intervention group used an average of 5 doses of sildenafil per 2-week interval, the same number as those in the placebo group.
Small treatment effect. The difference in response between sildenafil and placebo was not large: 0.8 points on a 7-point scale. But this difference is likely a clinically meaningful effect to the women with this problem.
Drug company funding. Pfizer, the maker of Viagra, funded this study through an investigator-initiated grant. Some researchers argue that female sexual dysfunction has been defined, or even invented, by drug companies seeking to create new markets for their products.16 This concern, coupled with the fact that this is the only double-blind randomized trial to show that sildenafil benefits women with antidepressant-associated sexual impairment, raises the question of whether this finding will be replicated in future trials.
We were reassured by the authors’ statement that Pfizer had no role in the study design, implementation, analysis, or manuscript preparation. And we know from clinical practice that women do suffer from SRI-induced sexual side effects, and sometimes stop taking much-needed antidepressants because the medication interferes with their ability to have a satisfying sex life. We believe this study was well done and offers a promising new therapy that deserves consideration. We hope that additional trials will follow and that investigators and journals will not hesitate to publish negative results.
Not for all women with sexual dysfunction
It’s a safe bet that these findings will be used to market sildenafil to women. It is therefore important for physicians and patients to keep in mind that this trial focused on a well-defined subset of women with sexual dysfunction: those on a stable dose of an SRI, with depression in remission, who were otherwise healthy and not pregnant, breastfeeding, or planning pregnancy, and who were motivated to be sexually active. Although this study does support the use of sildenafil for women in this subset, it does not support the use of PDE-5 inhibitors such as sildenafil for all women with sexual difficulties.
CHALLENGES TO IMPLEMENTATION: You have to ask!
Studies have repeatedly found that many women who experience sexual problems do not broach the subject with their doctors.17 So don’t wait for your female patients to bring it up. Sexual side effects are common enough with SRI antidepressants that all prescribers should mention the possibility in advance. Tell patients to let you know if they develop medication-related sexual dysfunction, and reassure them that there are treatments that can help.
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300:395-404.
2. Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F. Incidence of sexual dysfunction associated with antidepressant agents: A prospective multicenter study of 1022 outpatients. Spanish working group for the study of psychotropic-related sexual dysfunction. J Clin Psychiatry. 2001;62 (suppl 3):S10-S21.
3. Mitchell AJ. Depressed patients and treatment adherence. Lancet. 2006;367:2041-2043.
4. Mitchell AJ, Selmes T. Why don’t patients take their medicine? reasons and solutions in psychiatry. Adv Psychiatr Treat. 2007;13:336-346.
5. Fazio L, Brock G. Erectile dysfunction: Management update. CMAJ. 2004;170:1429-1437.
6. Nurnberg HG, Gelenberg A, Hargreave TB, Harrison WM, Siegel RL, Smith MD. Efficacy of sildenafil citrate for the treatment of erectile dysfunction in men taking serotonin reuptake inhibitors. Am J Psychiatry. 2001;158:1926-1928.
7. Nurnberg HG, Hensley PL, Gelenberg AJ, Fava M, Lauriello J, Paine S. Treatment of antidepressant-associated sexual dysfunction with sildenafil: A randomized controlled trial. JAMA. 2003;289:56-64.
8. Rudkin L, Taylor MJ, Hawton K. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst Rev. 2004;18(4):CD003382.
9. Ferguson JM, Shrivastava RK, Stahl SM, et al. Reemergence of sexual dysfunction in patients with major depressive disorder: Double-blind comparison of nefazodone and sertraline. J Clin Psychiatry. 2001;62:24-29.
10. Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008;77:635-642.
11. Nurnberg HG, Hensley PL, Lauriello J, Parker LM, Keith SJ. Sildenafil for women patients with antidepressant-induced sexual dysfunction. Psychiatr Serv. 1999;50:1076-1078.
12. Nurnberg HG, Lauriello J, Hensley PL, Parker LM, Keith SJ. Sildenafil for sexual dysfunction in women taking antidepressants. Am J Psychiatry. 1999;156:1664.
13. Nurnberg HG, Lauriello J, Hensley PL, Parker LM, Keith SJ. Sildenafil for iatrogenic serotonergic antidepressant medication-induced sexual dysfunction in 4 patients. J Clin Psychiatry. 1999;60:33-35.
14. Ashton AK. Vardenafil reversal of female anorgasmia. Am J Psychiatry. 2004;161:2133.
15. Ashton AK, Weinstein W. Tadalafil reversal of sexual dysfunction caused by serotonin enhancing medications in women. J Sex Marital Ther. 2006;32:1-3.
16. Moynihan R. The making of a disease: Female sexual dysfunction. BMJ. 2003 Jan 4;326:45-47.
17. Rosenberg KP, Bleiberg KL, Koscis J, Gross C. A survey of sexual side effects among severely mentally ill patients taking psychotropic medications: Impact on compliance. J Sex Marital Ther. 2003;29:289-296.
Tell women for whom you prescribe selective and nonselective serotonin reuptake inhibitors (SRIs) to let you know if they develop sexual dysfunction. Offer sildenafil (50 mg with the option to increase to 100 mg) to premenopausal women on stable, effective doses of SRIs who experience this common—and treatable—side effect.1
Strength of recommendation
B: One high-quality RCT that confirms smaller, open-label studies
Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300:395-404.
ILLUSTRATIVE CASE
A 34-year-old woman comes to your office and asks to be taken off the paroxetine you prescribed for her 4 months ago. The medication is working well; her depression has been in remission for at least 12 weeks. But she no longer enjoys sex. She used to have a healthy libido and satisfying arousal and orgasm, but since starting the antidepressant, her sexual interest and pleasure have been low.
Although she’s afraid of sinking back into a depression without the medication, she’s willing to take the risk. If she were your patient, what alternatives would you suggest?
Sexual dysfunction affects an estimated 30% to 50% of patients on selective and nonselective SRIs, and some studies report rates as high as 70% to 80%.2 Many patients stop taking these antidepressants prematurely, often because of sexual side effects.3,4
Phosphodiesterase type 5 (PDE-5) inhibitors are well established as an effective treatment for erectile dysfunction,5 and randomized controlled trials (RCTs) have shown sildenafil to be effective in treating male SRI-induced sexual impairment.6,7 For women, there has been no parallel evidence-based treatment.
Limited options, with little support
Typically, women who reported antidepressant-associated sexual disturbances have been offered options for which there was only weak evidence—dose changes or augmentation with another agent, switching to another antidepressant, or taking occasional drug holidays. A 2004 Cochrane review found that there were no RCTs involving dose changes or drug holidays.8 Among studies of the efficacy of switching to a different drug, nefazodone was the only agent whose use was supported by a double-blind RCT.9 Augmentation trials of a wide range of medications and supplements—including amantadine, bupropion, buspirone, granisetron, mirtazapine, olanzapine, ephedrine, ginkgo biloba, and yohimbine—yielded mixed results. Indeed, the research found that some were no better than placebo.
PDE-5 inhibitors for women? Inconclusive studies to date
Female sexual dysfunction is generally divided into 4 domains: disorders of desire, arousal, orgasm, or pain. Decreased desire and delayed or absent orgasm are the most common sexual side effects of SRI antidepressants in women.10 Several studies of PDE-5 inhibitors in this patient population have had positive results,11-15 so there has been good reason to think that they might help this subset of women. However, all the studies were small and nonblinded, and therefore inconclusive—until now.
STUDY SUMMARY: Finally, a well-done RCT provides some answers
Investigators enrolled 98 premenopausal women from 7 US research centers in a double-blind randomized trial. To qualify, participants had to be diagnosed with major depression in remission, be taking a selective or nonselective SRI for >8 weeks, and be on a stable dose for >4 weeks. They also had to meet Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria for substance-induced sexual dysfunction lasting >4 weeks, but have no history of sexual impairment independent of antidepressants. Finally, participants had to engage in some form of regular sexual activity—intercourse, oral sex, and masturbation all qualified—at least twice a month, and be willing to continue efforts to have sex at least once a week during the study. Women with other medical, psychiatric, or sexual problems were excluded, as were those who were pregnant, breastfeeding, or able to become pregnant and not using reliable contraception.
Participants were randomized to receive 50 mg of sildenafil (n=49) or a matching placebo tablet (n=49), which they were instructed to take 1 to 2 hours before sexual activity. The dose could be adjusted to 2 tablets (100 mg sildenafil) based on investigator assessment of the patient’s response to the initial dose. Participants and all study personnel were blinded to group assignment.
The primary outcome was change from baseline to end-point in the Clinical Global Impression Scale, a clinician-rated scale based on review of patient symptoms that was adapted to evaluate sexual function. Secondary outcomes were changes in 3 other sexual function scales, the Hamilton Rating Scale for Depression, and measured hormone levels.
Investigators followed the women for 8 weeks, measuring outcomes at 2, 4, and 8 weeks.
Sildenafil is better than placebo
Using an intention-to-treat analysis with the last measurement (2, 4, or 8 weeks) as the end-point, both the treatment and placebo groups experienced improvement in sexual function. The sildenafil group improved more than the placebo group. On the Clinical Global Impression Scale (1 to 7, with higher scores indicating worse sexual function), sildenafil users went from a mean of 4.8 to 2.8, while placebo users went from a mean of 4.7 to 3.6. The difference in mean change from baseline was 0.8 (95% confidence interval [CI] 0.6-1.0; P=.001). Using a more conservative analysis in which participants who did not return for the 8-week follow-up visit were assumed to have returned to baseline, the difference in mean change from baseline was smaller (0.6, 95% CI, 0.3-0.8; P=0.03) but still statistically significant.
Orgasmic function shows significant improvement
The sexual function scales used as secondary outcomes provided more detail about which types of sexual dysfunction benefited from sildenafil. On all 3 scales, orgasmic function significantly favored sildenafil over placebo. In the domains of desire, arousal, and pain disorders, small to moderate improvements were seen in both groups, with no statistically significant differences. One potential confounder—a difference in the course of participants’ underlying depression— was ruled out because depression scale results remained unchanged from baseline to endpoint in both groups.
Baseline levels of cortisone, estradiol, follicle-stimulating hormone, leuteinizing hormone, progesterone, prolactin, sex hormone-binding globulin, testosterone, thyroid-stimulating hormone, and thyroxine, were normal, with no differences between the sildenafil and placebo groups.
WHAT’S NEW: Women have an evidence-based option
Like their male counterparts, we can now offer women whose depression is effectively treated by SRI antidepressants—and who are motivated to stay sexually active despite medication-associated side effects—an effective pharmacotherapeutic treatment.
CAVEATS: Side effects and study funding are worth noting
Side effects. Significantly more participants in the sildenafil group vs the placebo group experienced the following side effects: headache (43% vs 27%), visual disturbance (14% vs 2%), dyspepsia (12% vs 0%), flushing (24% vs 0%), nasal congestion (37% vs 6%), and palpitations (8% vs 2%). Nausea was the only side effect that was more common in the placebo group, reported by only 2% of those in the intervention group but 16% of those on placebo.
No serious adverse events occurred, however, and the medication appears to have been well tolerated overall, despite relatively high rates of side effects. Participants in the intervention group used an average of 5 doses of sildenafil per 2-week interval, the same number as those in the placebo group.
Small treatment effect. The difference in response between sildenafil and placebo was not large: 0.8 points on a 7-point scale. But this difference is likely a clinically meaningful effect to the women with this problem.
Drug company funding. Pfizer, the maker of Viagra, funded this study through an investigator-initiated grant. Some researchers argue that female sexual dysfunction has been defined, or even invented, by drug companies seeking to create new markets for their products.16 This concern, coupled with the fact that this is the only double-blind randomized trial to show that sildenafil benefits women with antidepressant-associated sexual impairment, raises the question of whether this finding will be replicated in future trials.
We were reassured by the authors’ statement that Pfizer had no role in the study design, implementation, analysis, or manuscript preparation. And we know from clinical practice that women do suffer from SRI-induced sexual side effects, and sometimes stop taking much-needed antidepressants because the medication interferes with their ability to have a satisfying sex life. We believe this study was well done and offers a promising new therapy that deserves consideration. We hope that additional trials will follow and that investigators and journals will not hesitate to publish negative results.
Not for all women with sexual dysfunction
It’s a safe bet that these findings will be used to market sildenafil to women. It is therefore important for physicians and patients to keep in mind that this trial focused on a well-defined subset of women with sexual dysfunction: those on a stable dose of an SRI, with depression in remission, who were otherwise healthy and not pregnant, breastfeeding, or planning pregnancy, and who were motivated to be sexually active. Although this study does support the use of sildenafil for women in this subset, it does not support the use of PDE-5 inhibitors such as sildenafil for all women with sexual difficulties.
CHALLENGES TO IMPLEMENTATION: You have to ask!
Studies have repeatedly found that many women who experience sexual problems do not broach the subject with their doctors.17 So don’t wait for your female patients to bring it up. Sexual side effects are common enough with SRI antidepressants that all prescribers should mention the possibility in advance. Tell patients to let you know if they develop medication-related sexual dysfunction, and reassure them that there are treatments that can help.
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
Tell women for whom you prescribe selective and nonselective serotonin reuptake inhibitors (SRIs) to let you know if they develop sexual dysfunction. Offer sildenafil (50 mg with the option to increase to 100 mg) to premenopausal women on stable, effective doses of SRIs who experience this common—and treatable—side effect.1
Strength of recommendation
B: One high-quality RCT that confirms smaller, open-label studies
Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300:395-404.
ILLUSTRATIVE CASE
A 34-year-old woman comes to your office and asks to be taken off the paroxetine you prescribed for her 4 months ago. The medication is working well; her depression has been in remission for at least 12 weeks. But she no longer enjoys sex. She used to have a healthy libido and satisfying arousal and orgasm, but since starting the antidepressant, her sexual interest and pleasure have been low.
Although she’s afraid of sinking back into a depression without the medication, she’s willing to take the risk. If she were your patient, what alternatives would you suggest?
Sexual dysfunction affects an estimated 30% to 50% of patients on selective and nonselective SRIs, and some studies report rates as high as 70% to 80%.2 Many patients stop taking these antidepressants prematurely, often because of sexual side effects.3,4
Phosphodiesterase type 5 (PDE-5) inhibitors are well established as an effective treatment for erectile dysfunction,5 and randomized controlled trials (RCTs) have shown sildenafil to be effective in treating male SRI-induced sexual impairment.6,7 For women, there has been no parallel evidence-based treatment.
Limited options, with little support
Typically, women who reported antidepressant-associated sexual disturbances have been offered options for which there was only weak evidence—dose changes or augmentation with another agent, switching to another antidepressant, or taking occasional drug holidays. A 2004 Cochrane review found that there were no RCTs involving dose changes or drug holidays.8 Among studies of the efficacy of switching to a different drug, nefazodone was the only agent whose use was supported by a double-blind RCT.9 Augmentation trials of a wide range of medications and supplements—including amantadine, bupropion, buspirone, granisetron, mirtazapine, olanzapine, ephedrine, ginkgo biloba, and yohimbine—yielded mixed results. Indeed, the research found that some were no better than placebo.
PDE-5 inhibitors for women? Inconclusive studies to date
Female sexual dysfunction is generally divided into 4 domains: disorders of desire, arousal, orgasm, or pain. Decreased desire and delayed or absent orgasm are the most common sexual side effects of SRI antidepressants in women.10 Several studies of PDE-5 inhibitors in this patient population have had positive results,11-15 so there has been good reason to think that they might help this subset of women. However, all the studies were small and nonblinded, and therefore inconclusive—until now.
STUDY SUMMARY: Finally, a well-done RCT provides some answers
Investigators enrolled 98 premenopausal women from 7 US research centers in a double-blind randomized trial. To qualify, participants had to be diagnosed with major depression in remission, be taking a selective or nonselective SRI for >8 weeks, and be on a stable dose for >4 weeks. They also had to meet Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria for substance-induced sexual dysfunction lasting >4 weeks, but have no history of sexual impairment independent of antidepressants. Finally, participants had to engage in some form of regular sexual activity—intercourse, oral sex, and masturbation all qualified—at least twice a month, and be willing to continue efforts to have sex at least once a week during the study. Women with other medical, psychiatric, or sexual problems were excluded, as were those who were pregnant, breastfeeding, or able to become pregnant and not using reliable contraception.
Participants were randomized to receive 50 mg of sildenafil (n=49) or a matching placebo tablet (n=49), which they were instructed to take 1 to 2 hours before sexual activity. The dose could be adjusted to 2 tablets (100 mg sildenafil) based on investigator assessment of the patient’s response to the initial dose. Participants and all study personnel were blinded to group assignment.
The primary outcome was change from baseline to end-point in the Clinical Global Impression Scale, a clinician-rated scale based on review of patient symptoms that was adapted to evaluate sexual function. Secondary outcomes were changes in 3 other sexual function scales, the Hamilton Rating Scale for Depression, and measured hormone levels.
Investigators followed the women for 8 weeks, measuring outcomes at 2, 4, and 8 weeks.
Sildenafil is better than placebo
Using an intention-to-treat analysis with the last measurement (2, 4, or 8 weeks) as the end-point, both the treatment and placebo groups experienced improvement in sexual function. The sildenafil group improved more than the placebo group. On the Clinical Global Impression Scale (1 to 7, with higher scores indicating worse sexual function), sildenafil users went from a mean of 4.8 to 2.8, while placebo users went from a mean of 4.7 to 3.6. The difference in mean change from baseline was 0.8 (95% confidence interval [CI] 0.6-1.0; P=.001). Using a more conservative analysis in which participants who did not return for the 8-week follow-up visit were assumed to have returned to baseline, the difference in mean change from baseline was smaller (0.6, 95% CI, 0.3-0.8; P=0.03) but still statistically significant.
Orgasmic function shows significant improvement
The sexual function scales used as secondary outcomes provided more detail about which types of sexual dysfunction benefited from sildenafil. On all 3 scales, orgasmic function significantly favored sildenafil over placebo. In the domains of desire, arousal, and pain disorders, small to moderate improvements were seen in both groups, with no statistically significant differences. One potential confounder—a difference in the course of participants’ underlying depression— was ruled out because depression scale results remained unchanged from baseline to endpoint in both groups.
Baseline levels of cortisone, estradiol, follicle-stimulating hormone, leuteinizing hormone, progesterone, prolactin, sex hormone-binding globulin, testosterone, thyroid-stimulating hormone, and thyroxine, were normal, with no differences between the sildenafil and placebo groups.
WHAT’S NEW: Women have an evidence-based option
Like their male counterparts, we can now offer women whose depression is effectively treated by SRI antidepressants—and who are motivated to stay sexually active despite medication-associated side effects—an effective pharmacotherapeutic treatment.
CAVEATS: Side effects and study funding are worth noting
Side effects. Significantly more participants in the sildenafil group vs the placebo group experienced the following side effects: headache (43% vs 27%), visual disturbance (14% vs 2%), dyspepsia (12% vs 0%), flushing (24% vs 0%), nasal congestion (37% vs 6%), and palpitations (8% vs 2%). Nausea was the only side effect that was more common in the placebo group, reported by only 2% of those in the intervention group but 16% of those on placebo.
No serious adverse events occurred, however, and the medication appears to have been well tolerated overall, despite relatively high rates of side effects. Participants in the intervention group used an average of 5 doses of sildenafil per 2-week interval, the same number as those in the placebo group.
Small treatment effect. The difference in response between sildenafil and placebo was not large: 0.8 points on a 7-point scale. But this difference is likely a clinically meaningful effect to the women with this problem.
Drug company funding. Pfizer, the maker of Viagra, funded this study through an investigator-initiated grant. Some researchers argue that female sexual dysfunction has been defined, or even invented, by drug companies seeking to create new markets for their products.16 This concern, coupled with the fact that this is the only double-blind randomized trial to show that sildenafil benefits women with antidepressant-associated sexual impairment, raises the question of whether this finding will be replicated in future trials.
We were reassured by the authors’ statement that Pfizer had no role in the study design, implementation, analysis, or manuscript preparation. And we know from clinical practice that women do suffer from SRI-induced sexual side effects, and sometimes stop taking much-needed antidepressants because the medication interferes with their ability to have a satisfying sex life. We believe this study was well done and offers a promising new therapy that deserves consideration. We hope that additional trials will follow and that investigators and journals will not hesitate to publish negative results.
Not for all women with sexual dysfunction
It’s a safe bet that these findings will be used to market sildenafil to women. It is therefore important for physicians and patients to keep in mind that this trial focused on a well-defined subset of women with sexual dysfunction: those on a stable dose of an SRI, with depression in remission, who were otherwise healthy and not pregnant, breastfeeding, or planning pregnancy, and who were motivated to be sexually active. Although this study does support the use of sildenafil for women in this subset, it does not support the use of PDE-5 inhibitors such as sildenafil for all women with sexual difficulties.
CHALLENGES TO IMPLEMENTATION: You have to ask!
Studies have repeatedly found that many women who experience sexual problems do not broach the subject with their doctors.17 So don’t wait for your female patients to bring it up. Sexual side effects are common enough with SRI antidepressants that all prescribers should mention the possibility in advance. Tell patients to let you know if they develop medication-related sexual dysfunction, and reassure them that there are treatments that can help.
Acknowledgment
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300:395-404.
2. Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F. Incidence of sexual dysfunction associated with antidepressant agents: A prospective multicenter study of 1022 outpatients. Spanish working group for the study of psychotropic-related sexual dysfunction. J Clin Psychiatry. 2001;62 (suppl 3):S10-S21.
3. Mitchell AJ. Depressed patients and treatment adherence. Lancet. 2006;367:2041-2043.
4. Mitchell AJ, Selmes T. Why don’t patients take their medicine? reasons and solutions in psychiatry. Adv Psychiatr Treat. 2007;13:336-346.
5. Fazio L, Brock G. Erectile dysfunction: Management update. CMAJ. 2004;170:1429-1437.
6. Nurnberg HG, Gelenberg A, Hargreave TB, Harrison WM, Siegel RL, Smith MD. Efficacy of sildenafil citrate for the treatment of erectile dysfunction in men taking serotonin reuptake inhibitors. Am J Psychiatry. 2001;158:1926-1928.
7. Nurnberg HG, Hensley PL, Gelenberg AJ, Fava M, Lauriello J, Paine S. Treatment of antidepressant-associated sexual dysfunction with sildenafil: A randomized controlled trial. JAMA. 2003;289:56-64.
8. Rudkin L, Taylor MJ, Hawton K. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst Rev. 2004;18(4):CD003382.
9. Ferguson JM, Shrivastava RK, Stahl SM, et al. Reemergence of sexual dysfunction in patients with major depressive disorder: Double-blind comparison of nefazodone and sertraline. J Clin Psychiatry. 2001;62:24-29.
10. Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008;77:635-642.
11. Nurnberg HG, Hensley PL, Lauriello J, Parker LM, Keith SJ. Sildenafil for women patients with antidepressant-induced sexual dysfunction. Psychiatr Serv. 1999;50:1076-1078.
12. Nurnberg HG, Lauriello J, Hensley PL, Parker LM, Keith SJ. Sildenafil for sexual dysfunction in women taking antidepressants. Am J Psychiatry. 1999;156:1664.
13. Nurnberg HG, Lauriello J, Hensley PL, Parker LM, Keith SJ. Sildenafil for iatrogenic serotonergic antidepressant medication-induced sexual dysfunction in 4 patients. J Clin Psychiatry. 1999;60:33-35.
14. Ashton AK. Vardenafil reversal of female anorgasmia. Am J Psychiatry. 2004;161:2133.
15. Ashton AK, Weinstein W. Tadalafil reversal of sexual dysfunction caused by serotonin enhancing medications in women. J Sex Marital Ther. 2006;32:1-3.
16. Moynihan R. The making of a disease: Female sexual dysfunction. BMJ. 2003 Jan 4;326:45-47.
17. Rosenberg KP, Bleiberg KL, Koscis J, Gross C. A survey of sexual side effects among severely mentally ill patients taking psychotropic medications: Impact on compliance. J Sex Marital Ther. 2003;29:289-296.
1. Nurnberg HG, Hensley PL, Heiman JR, Croft HA, Debattista C, Paine S. Sildenafil treatment of women with antidepressant-associated sexual dysfunction: a randomized controlled trial. JAMA. 2008;300:395-404.
2. Montejo AL, Llorca G, Izquierdo JA, Rico-Villademoros F. Incidence of sexual dysfunction associated with antidepressant agents: A prospective multicenter study of 1022 outpatients. Spanish working group for the study of psychotropic-related sexual dysfunction. J Clin Psychiatry. 2001;62 (suppl 3):S10-S21.
3. Mitchell AJ. Depressed patients and treatment adherence. Lancet. 2006;367:2041-2043.
4. Mitchell AJ, Selmes T. Why don’t patients take their medicine? reasons and solutions in psychiatry. Adv Psychiatr Treat. 2007;13:336-346.
5. Fazio L, Brock G. Erectile dysfunction: Management update. CMAJ. 2004;170:1429-1437.
6. Nurnberg HG, Gelenberg A, Hargreave TB, Harrison WM, Siegel RL, Smith MD. Efficacy of sildenafil citrate for the treatment of erectile dysfunction in men taking serotonin reuptake inhibitors. Am J Psychiatry. 2001;158:1926-1928.
7. Nurnberg HG, Hensley PL, Gelenberg AJ, Fava M, Lauriello J, Paine S. Treatment of antidepressant-associated sexual dysfunction with sildenafil: A randomized controlled trial. JAMA. 2003;289:56-64.
8. Rudkin L, Taylor MJ, Hawton K. Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database Syst Rev. 2004;18(4):CD003382.
9. Ferguson JM, Shrivastava RK, Stahl SM, et al. Reemergence of sexual dysfunction in patients with major depressive disorder: Double-blind comparison of nefazodone and sertraline. J Clin Psychiatry. 2001;62:24-29.
10. Frank JE, Mistretta P, Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008;77:635-642.
11. Nurnberg HG, Hensley PL, Lauriello J, Parker LM, Keith SJ. Sildenafil for women patients with antidepressant-induced sexual dysfunction. Psychiatr Serv. 1999;50:1076-1078.
12. Nurnberg HG, Lauriello J, Hensley PL, Parker LM, Keith SJ. Sildenafil for sexual dysfunction in women taking antidepressants. Am J Psychiatry. 1999;156:1664.
13. Nurnberg HG, Lauriello J, Hensley PL, Parker LM, Keith SJ. Sildenafil for iatrogenic serotonergic antidepressant medication-induced sexual dysfunction in 4 patients. J Clin Psychiatry. 1999;60:33-35.
14. Ashton AK. Vardenafil reversal of female anorgasmia. Am J Psychiatry. 2004;161:2133.
15. Ashton AK, Weinstein W. Tadalafil reversal of sexual dysfunction caused by serotonin enhancing medications in women. J Sex Marital Ther. 2006;32:1-3.
16. Moynihan R. The making of a disease: Female sexual dysfunction. BMJ. 2003 Jan 4;326:45-47.
17. Rosenberg KP, Bleiberg KL, Koscis J, Gross C. A survey of sexual side effects among severely mentally ill patients taking psychotropic medications: Impact on compliance. J Sex Marital Ther. 2003;29:289-296.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.
Dust mite control measures don’t help asthma patients
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.
Treat depressed teens with medication and psychotherapy
Refer adolescents with moderate to severe depression for cognitive behavioral therapy (CBT) to improve their outcomes.1-3
Strength of recommendation
B: Two well-done randomized controlled trials (RCTs).
Schoeman Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression. The TORDIA randomized controlled trial. JAMA. 2008;299:901-913.
March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents with Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132-1143.
March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807-820.
ILLUSTRATIVE CASE
Jason, a depressed 17-year-old, is brought in by his mother, who’s worried about his mood and lack of motivation. He reports that his mood has “sunk” over the last 2 months. His mother interjects that she suffers from depression herself and that she’s divorced and unable to compensate for the absence of Jason’s father. She also says that her 2 older sons, both of whom Jason is close to, recently moved out of state. Further questioning reveals that Jason has lost interest in school, sports, friends, and his part-time job; he’s pessimistic about the future and feels helpless and stuck. Jason avoids going out and spends hours on the Internet.
You consider prescribing a selective serotonin reuptake inhibitor (SSRI), but you’re concerned about the potential suicide risk—a risk that’s already elevated for teens with major depressive disorder (MDD). Would a referral to a therapist be a safer choice? Is psychotherapy alone sufficient? What type of therapy is best?
Depressive disorders are common among adolescents and young adults, affecting nearly 1 in 4 by age 24.4 Most seek help from primary care physicians, who typically prescribe SSRIs.5 Yet only about one third of depressed teens achieve complete remission with medication alone.1 For the two thirds who continue to have depressive symptoms, the consequences can be severe. Depressive illness is associated with family conflict, smoking and substance abuse, impaired functioning in school and in relationships, and increased risk of suicide—the third leading cause of death in adolescents.6
Drugs, psychotherapy, or both?
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC), published in November 2007, encourage primary care physicians to take a more active role in detecting and managing adolescent depression.7 GLAD-PC and the American Academy of Child and Adolescent Psychiatry recommend that teens with depressive illness receive psychotherapy, either as primary treatment or in conjunction with antidepressants.7,8 Until recently, however, that recommendation lacked definitive evidence to support it.
STUDY SUMMARIES
2 studies explore combination approach
TADS (Treatment for Adolescents with Depression Study)2,3 and TORDIA (Treatment of Resistant Depression in Adolescents)1 are the only 2 randomized trials to address the role of CBT in combination with antidepressants in treating this patient population. Both show a significant benefit when CBT is added to drug therapy.
TADS: Highest improvement rates with fluoxetine and CBT
The TADS team studied 439 adolescents (ages 12 to 17 years) diagnosed with MDD. Patients were evaluated at consent, baseline, and weeks 6, 12, 18, 30, and 36. Those who were already taking antidepressants were excluded, but concurrent therapy for attention-deficit hyperactivity disorder was permitted.
Participants were randomly assigned to 1 of the following 12-week treatment options:
•Fluoxetine (10-40 mg/d)
•CBT
•Fluoxetine (10-40 mg/d) + CBT
•Placebo
CBT consisted of 15 sessions over 12 weeks, each lasting 50 to 60 minutes. In addition to individual sessions, 2 parental sessions and 1 to 3 family sessions were included. Primary outcome measures were the Clinical Global Impressions-Improvement Scale (CGI-I), which is based on a clinician’s overall assessment of the patient’s improvement; and the Children’s Depression Rating Scale-Revised (CDRS-R), which is derived from parent and adolescent interviews.
At 12 weeks, patients receiving fluoxetine and CBT demonstrated the highest rates of improvement: Seventy-one percent (95% confidence interval [CI], 62%-80%) were “much” or “very much” improved, vs 60.6% (95% CI, 51%-70%) of those on fluoxetine alone. In comparison, 43.2% (95% CI, 34%-52%) of patients receiving CBT alone were much or very much improved at the 12-week mark, and only 34.8% (95% CI, 26%-44%) of those on placebo.
At 18 weeks, the medication/CBT combination remained superior to either psychotherapy or fluoxetine alone. By week 30, all 3 intervention groups converged, and at 36 weeks there was virtually no difference in outcomes (FIGURE).
CBT alone has protective effect. While CBT alone was not significantly better than placebo overall, it demonstrated a protective effect with regard to suicidal events (thoughts, threats, or attempts) compared to fluoxetine. Conversely, fluoxetine accelerated the rate of improvement in mood during the first 30 weeks of treatment.
TORDIA: How to help patients after failed treatment
Brent and colleagues studied 334 patients between the ages of 12 and 18 years who were diagnosed with MDD but did not respond to initial SSRI therapy. After a 4-week trial, they were reevaluated and tapered off the medication, then randomly assigned to 1 of the following treatment groups for 12 weeks:
•Switched to a new SSRI
•Switched to venlafaxine (a selective serotonin-norepinephrine reuptake inhibitor)
•Switched to a new SSRI + CBT
•Switched to venlafaxine + CBT
All patients were reevaluated at week 12. Here, too, the CGI-I and CDRS-R were used for key outcome measures.
Adding CBT to a medication regimen was associated with an increased response rate; choice of antidepressant was not. The groups receiving CBT were significantly more likely to show improvement compared to those who were not undergoing CBT (54.8% [95% CI, 47%-62%] vs 40.5% [95% CI, 33%-48%], number needed to treat [NNT]=7).
WHAT'S NEW?
An alternative that speeds recovery
These 2 studies confirm the value of CBT in treating moderate to severe major depression in combination with antidepressant therapy. TADS provides evidence of both a faster recovery trajectory and lower likelihood of suicidal events with combined treatment. While TORDIA does not demonstrate a quicker recovery in terms of depressed mood or a lower rate of suicidal events, it suggests that for adolescents who do not respond to antidepressants, a referral to CBT will be more effective than a switch to a different drug.
CAVEATS
Approach was not tested with mild depression
Most adolescents who report depressive symptoms to primary care physicians either do not meet the full criteria for major depression or fall into the mild major depression range.9-11 Both of these studies enrolled only those with moderate to severe MDD.
There is evidence, however, that such an approach may not be necessary for teens with milder depression. Many earlier studies of psychotherapy alone vs control (wait list or observation) for patients with sub-threshold depressive disorders or mild major depression demonstrated that psychotherapy is effective in treating these less severe depressive states.7,12 GLAD-PC recommends a 4- to 8-week trial of active monitoring for patients with mild MDD before initiating psychotherapy or medication.2
CHALLENGES TO IMPLEMENTATION
Patient perceptions, stigma
There are 3 major barriers to implementation: patient/parent resistance to psychotherapy, limited access to mental health specialists (lack of supply and insurance coverage limitations), and few quality standards for evidence-based psychotherapeutic approaches in community practice settings.13-15 Many adolescents have a negative view of therapy and feel stigmatized by a referral to a psychotherapist. They may also have a well-developed rationale as to why such treatment would not work for them.16
Physicians can help teens overcome these negative perceptions by giving them an opportunity to discuss their concerns—and by clarifying any misconceptions.17 The idea that “brain changes” cause depression has become popular in recent years,18 and may provide some relief to those who are troubled by the notion that they are somehow to blame for their depression.19 Presenting both antidepressant medication and psychotherapy as interventions that “change the way the brain manages mood” may be helpful in alleviating self-blame.
Consider nontraditional approaches
In areas with limited access to mental health specialists, nontraditional approaches may be needed. One such approach is to help patients arrange an initial interview with a psychotherapist, followed by telephone counseling sessions. For patients 18 years or older, MoodGym (http://moodgym.anu.edu.au/welcome) is also an option. This free Internet site incorporates features of standardized CBT and interpersonal therapy, and has demonstrated efficacy in RCTs of adults.20 For those between the ages of 14 and 21, CATCH-IT (http://catchit-public.bsd.uchicago.edu)21 is another Internet option. The site, which can be accessed by physicians and the general public, focuses on building competencies to reduce current and future depressive symptoms.
In addition, recommend self-help books. While there have been no studies of their value to adolescents, the book with the greatest evidence of efficacy in adults is “Feeling Good: The New Mood Therapy,” by David D. Burns.22
For your part... Before making referrals to mental health specialists, ask therapists whether they incorporate, and have been trained in, cognitive behavioral therapy. In addition, you can remain involved by asking the psychotherapist for a written treatment plan and by encouraging adolescents (and their families) to fully adhere to it.
ACKNOWLEDGEMENTS
The Purls Surveillance System is supported in part by Grant Number ul1rr024999 from the National Center For research resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For research resources or the National Institutes of Health.
Benjamin Van Voorhees is supported by a career development award from the National Institutes of Mental Health (NImHK-08mH072918-01A2).
1. Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299:901-913.
2. March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132-1143.
3. March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807-820.
4. Kessler RC, Walters EE. Epidemiology of DSM-IIIR major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7:3-14.
5. Rushton JL, Clark SJ, Freed GL. Pediatrician and family physician prescription of selective serotonin reuptake inhibitors. Pediatrics. 2000;105:E82.
6. Hankin BL. Adolescent depression: description, causes, and interventions. Epilepsy Behav. 2006;8:102-114.
7. Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE . Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120:e1313-e1326.
8. Birmaher B , Brent DA, Benson RS. Summary of the practice parameters for the assessment and treatment of children and adolescents with depressive disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1998;37:1234-1238.
9. Yates P, Kramer T, Garralda E . Depressive symptoms amongst adolescent primary care attenders. Levels and associations. Soc Psychiatry Psychiatr Epidemiol. 2004;39:588-594.
10. Rushton JL, Forcier M , Schectman RM . Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J Am Acad Child Adolesc Psychiatry. 2002;41:199-205.
11. Johnson JG, Harris ES, Spitzer RL , Williams JB. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health. 2002;30:196-204.
12. Compton SN, March JS, Brent D, Albano AM, Weersing R , Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry. 2004;43:930-959.
13. Asarnow JR, Jaycox L H, Anderson M . Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11:477-497, viii.
14. Wisdom JP, Clarke GN, Green CA. What teens want: barriers to seeking care for depression. Adm Policy Ment Health. 2006;33:133-145.
15. Zuckerbrot R A, Cheung AH, Jensen PS, Stein RE , Laraque D. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120:e1299-e1312.
16. Van Voorhees B W, Fogel J, Houston TK, Cooper LA, Wang NY, Ford DE. Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Ann Fam Med. 2005;3:38-46.
17. Clever SL, Ford DE, Rubenstein LV , et al. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006;44:398-405.
18. Lacasse JR. Consumer advertising of psychiatric medications biases the public against nonpharmacological treatment. Ethical Hum Psychol Psychiatry. 2005;7:175-179.
19. Van Voorhees B W, Cooper L A, Rost KM, et al. Primary care patients with depression are less accepting of treatment than those seen by mental health specialists. J Gen Intern Med. 2003;18:991-1000.
20. Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ. 2004;328:265.
21. Anderson L , Lewis G, Araya R, et al. Self-help books for depression: how can practitioners and patients make the right choice? Br J Gen Pract. 2005;55:387-392.
22. Van Voorhees B W, Vanderploegbooth K, Fogel J, et al. Integrative Internet-based depression prevention for adolescents: a randomized clinical trial in primary care for vulnerability and protective factors. J Can Acad Child Adoles Psychiatry. In press.
Refer adolescents with moderate to severe depression for cognitive behavioral therapy (CBT) to improve their outcomes.1-3
Strength of recommendation
B: Two well-done randomized controlled trials (RCTs).
Schoeman Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression. The TORDIA randomized controlled trial. JAMA. 2008;299:901-913.
March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents with Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132-1143.
March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807-820.
ILLUSTRATIVE CASE
Jason, a depressed 17-year-old, is brought in by his mother, who’s worried about his mood and lack of motivation. He reports that his mood has “sunk” over the last 2 months. His mother interjects that she suffers from depression herself and that she’s divorced and unable to compensate for the absence of Jason’s father. She also says that her 2 older sons, both of whom Jason is close to, recently moved out of state. Further questioning reveals that Jason has lost interest in school, sports, friends, and his part-time job; he’s pessimistic about the future and feels helpless and stuck. Jason avoids going out and spends hours on the Internet.
You consider prescribing a selective serotonin reuptake inhibitor (SSRI), but you’re concerned about the potential suicide risk—a risk that’s already elevated for teens with major depressive disorder (MDD). Would a referral to a therapist be a safer choice? Is psychotherapy alone sufficient? What type of therapy is best?
Depressive disorders are common among adolescents and young adults, affecting nearly 1 in 4 by age 24.4 Most seek help from primary care physicians, who typically prescribe SSRIs.5 Yet only about one third of depressed teens achieve complete remission with medication alone.1 For the two thirds who continue to have depressive symptoms, the consequences can be severe. Depressive illness is associated with family conflict, smoking and substance abuse, impaired functioning in school and in relationships, and increased risk of suicide—the third leading cause of death in adolescents.6
Drugs, psychotherapy, or both?
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC), published in November 2007, encourage primary care physicians to take a more active role in detecting and managing adolescent depression.7 GLAD-PC and the American Academy of Child and Adolescent Psychiatry recommend that teens with depressive illness receive psychotherapy, either as primary treatment or in conjunction with antidepressants.7,8 Until recently, however, that recommendation lacked definitive evidence to support it.
STUDY SUMMARIES
2 studies explore combination approach
TADS (Treatment for Adolescents with Depression Study)2,3 and TORDIA (Treatment of Resistant Depression in Adolescents)1 are the only 2 randomized trials to address the role of CBT in combination with antidepressants in treating this patient population. Both show a significant benefit when CBT is added to drug therapy.
TADS: Highest improvement rates with fluoxetine and CBT
The TADS team studied 439 adolescents (ages 12 to 17 years) diagnosed with MDD. Patients were evaluated at consent, baseline, and weeks 6, 12, 18, 30, and 36. Those who were already taking antidepressants were excluded, but concurrent therapy for attention-deficit hyperactivity disorder was permitted.
Participants were randomly assigned to 1 of the following 12-week treatment options:
•Fluoxetine (10-40 mg/d)
•CBT
•Fluoxetine (10-40 mg/d) + CBT
•Placebo
CBT consisted of 15 sessions over 12 weeks, each lasting 50 to 60 minutes. In addition to individual sessions, 2 parental sessions and 1 to 3 family sessions were included. Primary outcome measures were the Clinical Global Impressions-Improvement Scale (CGI-I), which is based on a clinician’s overall assessment of the patient’s improvement; and the Children’s Depression Rating Scale-Revised (CDRS-R), which is derived from parent and adolescent interviews.
At 12 weeks, patients receiving fluoxetine and CBT demonstrated the highest rates of improvement: Seventy-one percent (95% confidence interval [CI], 62%-80%) were “much” or “very much” improved, vs 60.6% (95% CI, 51%-70%) of those on fluoxetine alone. In comparison, 43.2% (95% CI, 34%-52%) of patients receiving CBT alone were much or very much improved at the 12-week mark, and only 34.8% (95% CI, 26%-44%) of those on placebo.
At 18 weeks, the medication/CBT combination remained superior to either psychotherapy or fluoxetine alone. By week 30, all 3 intervention groups converged, and at 36 weeks there was virtually no difference in outcomes (FIGURE).
CBT alone has protective effect. While CBT alone was not significantly better than placebo overall, it demonstrated a protective effect with regard to suicidal events (thoughts, threats, or attempts) compared to fluoxetine. Conversely, fluoxetine accelerated the rate of improvement in mood during the first 30 weeks of treatment.
TORDIA: How to help patients after failed treatment
Brent and colleagues studied 334 patients between the ages of 12 and 18 years who were diagnosed with MDD but did not respond to initial SSRI therapy. After a 4-week trial, they were reevaluated and tapered off the medication, then randomly assigned to 1 of the following treatment groups for 12 weeks:
•Switched to a new SSRI
•Switched to venlafaxine (a selective serotonin-norepinephrine reuptake inhibitor)
•Switched to a new SSRI + CBT
•Switched to venlafaxine + CBT
All patients were reevaluated at week 12. Here, too, the CGI-I and CDRS-R were used for key outcome measures.
Adding CBT to a medication regimen was associated with an increased response rate; choice of antidepressant was not. The groups receiving CBT were significantly more likely to show improvement compared to those who were not undergoing CBT (54.8% [95% CI, 47%-62%] vs 40.5% [95% CI, 33%-48%], number needed to treat [NNT]=7).
WHAT'S NEW?
An alternative that speeds recovery
These 2 studies confirm the value of CBT in treating moderate to severe major depression in combination with antidepressant therapy. TADS provides evidence of both a faster recovery trajectory and lower likelihood of suicidal events with combined treatment. While TORDIA does not demonstrate a quicker recovery in terms of depressed mood or a lower rate of suicidal events, it suggests that for adolescents who do not respond to antidepressants, a referral to CBT will be more effective than a switch to a different drug.
CAVEATS
Approach was not tested with mild depression
Most adolescents who report depressive symptoms to primary care physicians either do not meet the full criteria for major depression or fall into the mild major depression range.9-11 Both of these studies enrolled only those with moderate to severe MDD.
There is evidence, however, that such an approach may not be necessary for teens with milder depression. Many earlier studies of psychotherapy alone vs control (wait list or observation) for patients with sub-threshold depressive disorders or mild major depression demonstrated that psychotherapy is effective in treating these less severe depressive states.7,12 GLAD-PC recommends a 4- to 8-week trial of active monitoring for patients with mild MDD before initiating psychotherapy or medication.2
CHALLENGES TO IMPLEMENTATION
Patient perceptions, stigma
There are 3 major barriers to implementation: patient/parent resistance to psychotherapy, limited access to mental health specialists (lack of supply and insurance coverage limitations), and few quality standards for evidence-based psychotherapeutic approaches in community practice settings.13-15 Many adolescents have a negative view of therapy and feel stigmatized by a referral to a psychotherapist. They may also have a well-developed rationale as to why such treatment would not work for them.16
Physicians can help teens overcome these negative perceptions by giving them an opportunity to discuss their concerns—and by clarifying any misconceptions.17 The idea that “brain changes” cause depression has become popular in recent years,18 and may provide some relief to those who are troubled by the notion that they are somehow to blame for their depression.19 Presenting both antidepressant medication and psychotherapy as interventions that “change the way the brain manages mood” may be helpful in alleviating self-blame.
Consider nontraditional approaches
In areas with limited access to mental health specialists, nontraditional approaches may be needed. One such approach is to help patients arrange an initial interview with a psychotherapist, followed by telephone counseling sessions. For patients 18 years or older, MoodGym (http://moodgym.anu.edu.au/welcome) is also an option. This free Internet site incorporates features of standardized CBT and interpersonal therapy, and has demonstrated efficacy in RCTs of adults.20 For those between the ages of 14 and 21, CATCH-IT (http://catchit-public.bsd.uchicago.edu)21 is another Internet option. The site, which can be accessed by physicians and the general public, focuses on building competencies to reduce current and future depressive symptoms.
In addition, recommend self-help books. While there have been no studies of their value to adolescents, the book with the greatest evidence of efficacy in adults is “Feeling Good: The New Mood Therapy,” by David D. Burns.22
For your part... Before making referrals to mental health specialists, ask therapists whether they incorporate, and have been trained in, cognitive behavioral therapy. In addition, you can remain involved by asking the psychotherapist for a written treatment plan and by encouraging adolescents (and their families) to fully adhere to it.
ACKNOWLEDGEMENTS
The Purls Surveillance System is supported in part by Grant Number ul1rr024999 from the National Center For research resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For research resources or the National Institutes of Health.
Benjamin Van Voorhees is supported by a career development award from the National Institutes of Mental Health (NImHK-08mH072918-01A2).
Refer adolescents with moderate to severe depression for cognitive behavioral therapy (CBT) to improve their outcomes.1-3
Strength of recommendation
B: Two well-done randomized controlled trials (RCTs).
Schoeman Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression. The TORDIA randomized controlled trial. JAMA. 2008;299:901-913.
March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents with Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132-1143.
March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807-820.
ILLUSTRATIVE CASE
Jason, a depressed 17-year-old, is brought in by his mother, who’s worried about his mood and lack of motivation. He reports that his mood has “sunk” over the last 2 months. His mother interjects that she suffers from depression herself and that she’s divorced and unable to compensate for the absence of Jason’s father. She also says that her 2 older sons, both of whom Jason is close to, recently moved out of state. Further questioning reveals that Jason has lost interest in school, sports, friends, and his part-time job; he’s pessimistic about the future and feels helpless and stuck. Jason avoids going out and spends hours on the Internet.
You consider prescribing a selective serotonin reuptake inhibitor (SSRI), but you’re concerned about the potential suicide risk—a risk that’s already elevated for teens with major depressive disorder (MDD). Would a referral to a therapist be a safer choice? Is psychotherapy alone sufficient? What type of therapy is best?
Depressive disorders are common among adolescents and young adults, affecting nearly 1 in 4 by age 24.4 Most seek help from primary care physicians, who typically prescribe SSRIs.5 Yet only about one third of depressed teens achieve complete remission with medication alone.1 For the two thirds who continue to have depressive symptoms, the consequences can be severe. Depressive illness is associated with family conflict, smoking and substance abuse, impaired functioning in school and in relationships, and increased risk of suicide—the third leading cause of death in adolescents.6
Drugs, psychotherapy, or both?
The Guidelines for Adolescent Depression in Primary Care (GLAD-PC), published in November 2007, encourage primary care physicians to take a more active role in detecting and managing adolescent depression.7 GLAD-PC and the American Academy of Child and Adolescent Psychiatry recommend that teens with depressive illness receive psychotherapy, either as primary treatment or in conjunction with antidepressants.7,8 Until recently, however, that recommendation lacked definitive evidence to support it.
STUDY SUMMARIES
2 studies explore combination approach
TADS (Treatment for Adolescents with Depression Study)2,3 and TORDIA (Treatment of Resistant Depression in Adolescents)1 are the only 2 randomized trials to address the role of CBT in combination with antidepressants in treating this patient population. Both show a significant benefit when CBT is added to drug therapy.
TADS: Highest improvement rates with fluoxetine and CBT
The TADS team studied 439 adolescents (ages 12 to 17 years) diagnosed with MDD. Patients were evaluated at consent, baseline, and weeks 6, 12, 18, 30, and 36. Those who were already taking antidepressants were excluded, but concurrent therapy for attention-deficit hyperactivity disorder was permitted.
Participants were randomly assigned to 1 of the following 12-week treatment options:
•Fluoxetine (10-40 mg/d)
•CBT
•Fluoxetine (10-40 mg/d) + CBT
•Placebo
CBT consisted of 15 sessions over 12 weeks, each lasting 50 to 60 minutes. In addition to individual sessions, 2 parental sessions and 1 to 3 family sessions were included. Primary outcome measures were the Clinical Global Impressions-Improvement Scale (CGI-I), which is based on a clinician’s overall assessment of the patient’s improvement; and the Children’s Depression Rating Scale-Revised (CDRS-R), which is derived from parent and adolescent interviews.
At 12 weeks, patients receiving fluoxetine and CBT demonstrated the highest rates of improvement: Seventy-one percent (95% confidence interval [CI], 62%-80%) were “much” or “very much” improved, vs 60.6% (95% CI, 51%-70%) of those on fluoxetine alone. In comparison, 43.2% (95% CI, 34%-52%) of patients receiving CBT alone were much or very much improved at the 12-week mark, and only 34.8% (95% CI, 26%-44%) of those on placebo.
At 18 weeks, the medication/CBT combination remained superior to either psychotherapy or fluoxetine alone. By week 30, all 3 intervention groups converged, and at 36 weeks there was virtually no difference in outcomes (FIGURE).
CBT alone has protective effect. While CBT alone was not significantly better than placebo overall, it demonstrated a protective effect with regard to suicidal events (thoughts, threats, or attempts) compared to fluoxetine. Conversely, fluoxetine accelerated the rate of improvement in mood during the first 30 weeks of treatment.
TORDIA: How to help patients after failed treatment
Brent and colleagues studied 334 patients between the ages of 12 and 18 years who were diagnosed with MDD but did not respond to initial SSRI therapy. After a 4-week trial, they were reevaluated and tapered off the medication, then randomly assigned to 1 of the following treatment groups for 12 weeks:
•Switched to a new SSRI
•Switched to venlafaxine (a selective serotonin-norepinephrine reuptake inhibitor)
•Switched to a new SSRI + CBT
•Switched to venlafaxine + CBT
All patients were reevaluated at week 12. Here, too, the CGI-I and CDRS-R were used for key outcome measures.
Adding CBT to a medication regimen was associated with an increased response rate; choice of antidepressant was not. The groups receiving CBT were significantly more likely to show improvement compared to those who were not undergoing CBT (54.8% [95% CI, 47%-62%] vs 40.5% [95% CI, 33%-48%], number needed to treat [NNT]=7).
WHAT'S NEW?
An alternative that speeds recovery
These 2 studies confirm the value of CBT in treating moderate to severe major depression in combination with antidepressant therapy. TADS provides evidence of both a faster recovery trajectory and lower likelihood of suicidal events with combined treatment. While TORDIA does not demonstrate a quicker recovery in terms of depressed mood or a lower rate of suicidal events, it suggests that for adolescents who do not respond to antidepressants, a referral to CBT will be more effective than a switch to a different drug.
CAVEATS
Approach was not tested with mild depression
Most adolescents who report depressive symptoms to primary care physicians either do not meet the full criteria for major depression or fall into the mild major depression range.9-11 Both of these studies enrolled only those with moderate to severe MDD.
There is evidence, however, that such an approach may not be necessary for teens with milder depression. Many earlier studies of psychotherapy alone vs control (wait list or observation) for patients with sub-threshold depressive disorders or mild major depression demonstrated that psychotherapy is effective in treating these less severe depressive states.7,12 GLAD-PC recommends a 4- to 8-week trial of active monitoring for patients with mild MDD before initiating psychotherapy or medication.2
CHALLENGES TO IMPLEMENTATION
Patient perceptions, stigma
There are 3 major barriers to implementation: patient/parent resistance to psychotherapy, limited access to mental health specialists (lack of supply and insurance coverage limitations), and few quality standards for evidence-based psychotherapeutic approaches in community practice settings.13-15 Many adolescents have a negative view of therapy and feel stigmatized by a referral to a psychotherapist. They may also have a well-developed rationale as to why such treatment would not work for them.16
Physicians can help teens overcome these negative perceptions by giving them an opportunity to discuss their concerns—and by clarifying any misconceptions.17 The idea that “brain changes” cause depression has become popular in recent years,18 and may provide some relief to those who are troubled by the notion that they are somehow to blame for their depression.19 Presenting both antidepressant medication and psychotherapy as interventions that “change the way the brain manages mood” may be helpful in alleviating self-blame.
Consider nontraditional approaches
In areas with limited access to mental health specialists, nontraditional approaches may be needed. One such approach is to help patients arrange an initial interview with a psychotherapist, followed by telephone counseling sessions. For patients 18 years or older, MoodGym (http://moodgym.anu.edu.au/welcome) is also an option. This free Internet site incorporates features of standardized CBT and interpersonal therapy, and has demonstrated efficacy in RCTs of adults.20 For those between the ages of 14 and 21, CATCH-IT (http://catchit-public.bsd.uchicago.edu)21 is another Internet option. The site, which can be accessed by physicians and the general public, focuses on building competencies to reduce current and future depressive symptoms.
In addition, recommend self-help books. While there have been no studies of their value to adolescents, the book with the greatest evidence of efficacy in adults is “Feeling Good: The New Mood Therapy,” by David D. Burns.22
For your part... Before making referrals to mental health specialists, ask therapists whether they incorporate, and have been trained in, cognitive behavioral therapy. In addition, you can remain involved by asking the psychotherapist for a written treatment plan and by encouraging adolescents (and their families) to fully adhere to it.
ACKNOWLEDGEMENTS
The Purls Surveillance System is supported in part by Grant Number ul1rr024999 from the National Center For research resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For research resources or the National Institutes of Health.
Benjamin Van Voorhees is supported by a career development award from the National Institutes of Mental Health (NImHK-08mH072918-01A2).
1. Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299:901-913.
2. March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132-1143.
3. March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807-820.
4. Kessler RC, Walters EE. Epidemiology of DSM-IIIR major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7:3-14.
5. Rushton JL, Clark SJ, Freed GL. Pediatrician and family physician prescription of selective serotonin reuptake inhibitors. Pediatrics. 2000;105:E82.
6. Hankin BL. Adolescent depression: description, causes, and interventions. Epilepsy Behav. 2006;8:102-114.
7. Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE . Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120:e1313-e1326.
8. Birmaher B , Brent DA, Benson RS. Summary of the practice parameters for the assessment and treatment of children and adolescents with depressive disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1998;37:1234-1238.
9. Yates P, Kramer T, Garralda E . Depressive symptoms amongst adolescent primary care attenders. Levels and associations. Soc Psychiatry Psychiatr Epidemiol. 2004;39:588-594.
10. Rushton JL, Forcier M , Schectman RM . Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J Am Acad Child Adolesc Psychiatry. 2002;41:199-205.
11. Johnson JG, Harris ES, Spitzer RL , Williams JB. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health. 2002;30:196-204.
12. Compton SN, March JS, Brent D, Albano AM, Weersing R , Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry. 2004;43:930-959.
13. Asarnow JR, Jaycox L H, Anderson M . Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11:477-497, viii.
14. Wisdom JP, Clarke GN, Green CA. What teens want: barriers to seeking care for depression. Adm Policy Ment Health. 2006;33:133-145.
15. Zuckerbrot R A, Cheung AH, Jensen PS, Stein RE , Laraque D. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120:e1299-e1312.
16. Van Voorhees B W, Fogel J, Houston TK, Cooper LA, Wang NY, Ford DE. Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Ann Fam Med. 2005;3:38-46.
17. Clever SL, Ford DE, Rubenstein LV , et al. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006;44:398-405.
18. Lacasse JR. Consumer advertising of psychiatric medications biases the public against nonpharmacological treatment. Ethical Hum Psychol Psychiatry. 2005;7:175-179.
19. Van Voorhees B W, Cooper L A, Rost KM, et al. Primary care patients with depression are less accepting of treatment than those seen by mental health specialists. J Gen Intern Med. 2003;18:991-1000.
20. Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ. 2004;328:265.
21. Anderson L , Lewis G, Araya R, et al. Self-help books for depression: how can practitioners and patients make the right choice? Br J Gen Pract. 2005;55:387-392.
22. Van Voorhees B W, Vanderploegbooth K, Fogel J, et al. Integrative Internet-based depression prevention for adolescents: a randomized clinical trial in primary care for vulnerability and protective factors. J Can Acad Child Adoles Psychiatry. In press.
1. Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. 2008;299:901-913.
2. March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Arch Gen Psychiatry. 2007;64:1132-1143.
3. March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807-820.
4. Kessler RC, Walters EE. Epidemiology of DSM-IIIR major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7:3-14.
5. Rushton JL, Clark SJ, Freed GL. Pediatrician and family physician prescription of selective serotonin reuptake inhibitors. Pediatrics. 2000;105:E82.
6. Hankin BL. Adolescent depression: description, causes, and interventions. Epilepsy Behav. 2006;8:102-114.
7. Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE . Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120:e1313-e1326.
8. Birmaher B , Brent DA, Benson RS. Summary of the practice parameters for the assessment and treatment of children and adolescents with depressive disorders. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry. 1998;37:1234-1238.
9. Yates P, Kramer T, Garralda E . Depressive symptoms amongst adolescent primary care attenders. Levels and associations. Soc Psychiatry Psychiatr Epidemiol. 2004;39:588-594.
10. Rushton JL, Forcier M , Schectman RM . Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J Am Acad Child Adolesc Psychiatry. 2002;41:199-205.
11. Johnson JG, Harris ES, Spitzer RL , Williams JB. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health. 2002;30:196-204.
12. Compton SN, March JS, Brent D, Albano AM, Weersing R , Curry J. Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry. 2004;43:930-959.
13. Asarnow JR, Jaycox L H, Anderson M . Depression among youth in primary care models for delivering mental health services. Child Adolesc Psychiatr Clin N Am. 2002;11:477-497, viii.
14. Wisdom JP, Clarke GN, Green CA. What teens want: barriers to seeking care for depression. Adm Policy Ment Health. 2006;33:133-145.
15. Zuckerbrot R A, Cheung AH, Jensen PS, Stein RE , Laraque D. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120:e1299-e1312.
16. Van Voorhees B W, Fogel J, Houston TK, Cooper LA, Wang NY, Ford DE. Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Ann Fam Med. 2005;3:38-46.
17. Clever SL, Ford DE, Rubenstein LV , et al. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006;44:398-405.
18. Lacasse JR. Consumer advertising of psychiatric medications biases the public against nonpharmacological treatment. Ethical Hum Psychol Psychiatry. 2005;7:175-179.
19. Van Voorhees B W, Cooper L A, Rost KM, et al. Primary care patients with depression are less accepting of treatment than those seen by mental health specialists. J Gen Intern Med. 2003;18:991-1000.
20. Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ. 2004;328:265.
21. Anderson L , Lewis G, Araya R, et al. Self-help books for depression: how can practitioners and patients make the right choice? Br J Gen Pract. 2005;55:387-392.
22. Van Voorhees B W, Vanderploegbooth K, Fogel J, et al. Integrative Internet-based depression prevention for adolescents: a randomized clinical trial in primary care for vulnerability and protective factors. J Can Acad Child Adoles Psychiatry. In press.
Copyright © 2008 Family Physicians Inquiries Network. All rights reserved.