User login
Prediction: LVADs will rule end-stage heart failure
SNOWMASS, COLO. – Multifaceted progress in mechanical circulatory support as long-term therapy in end-stage heart failure is happening at a brisk pace, Y. Joseph C. Woo, MD, reported at the Annual Cardiovascular Conference at Snowmass.
declared Dr. Woo, professor and chair of the department of cardiothoracic surgery at Stanford (Calif.) University.
That’s quite a prediction, especially considering the source: Stanford is where the late Dr. Norman Shumway – widely considered “the father of heart transplantation” – performed the first adult heart transplant in the United States in 1968.
Dr. Woo was coauthor of an American Heart Association policy statement on the future of cardiovascular disease in the United States, which forecast a 25% increase in heart failure between 2010 and 2030 (Circulation. 2011 Mar 1;123[8]:933-44). There is simply no way that heart transplantation can begin to meet the projected growing need for effective therapy in patients with end-stage disease.
Here’s what Dr. Woo sees as the future of MCS:
Minimally invasive implantation
At Stanford, LVAD implantations are now routinely done off-pump on a beating heart.
“We clamp only when there is a sound reason, like the presence of left ventricular thrombus, where you run the risk of embolization without the cross clamp,” the surgeon said.
Concomitant valvular surgery
At Stanford and other centers of excellence, surgeons perform additional procedures as warranted while they implant an LVAD, including atrial fibrillation ablation, revascularization of the right heart coronaries, patent foramen ovale closure, and repair of the tricuspid, pulmonic, or aortic valves.
Enhanced right ventricular management
Survival is greatly impaired if a patient with an LVAD later requires the addition of a right ventricular assist device. This realization has led to the development of multiple preoperative risk scoring systems by the Stanford group (Ann Thorac Surg. 2013 Sep;96[3]:857-63) and others, including investigators at the Deutsche Herzzentrum Berlin, the world’s busiest heart transplant center. The purpose is to identify upfront those patients who are likely to later develop right heart failure so they can receive biventricular MCS from the start.
Adjunctive biologic therapies
Intramyocardial injection of 25 million allogeneic mesenchymal precursor cells during LVAD implantation appeared to be safe and showed a promising efficacy signal in a 30-patient, multicenter, double-blind, placebo-controlled, National Institutes of Health–sponsored proof of concept study in which Dr. Woo was a coinvestigator (Circulation. 2014 Jun 3;129[22]:2287-96).
The goal of this research effort is to provide a cell therapy assist to the LVAD as a bridge to recovery of left ventricular function such that the device might eventually no longer be needed, he explained.
These cells are immune privileged. They can be transplanted into recipients without need for immunosuppressive therapy or HLA matching, basically as an off the shelf product. Rather than transforming into cardiomyocytes, it appears that the mechanism by which the donor cells enhance cardiac performance in heart failure is via secretion of a shower of growth and angiogenic factors.
Based upon the encouraging results of the initial study, a 90-patient, phase II, double-blind clinical trial is underway. In order to better evaluate efficacy, this time the patients will receive 150 million mesenchymal precursor cells rather than 25 million.
New technologies
The developmental pipeline is chock full of MCS devices. The trend is to go smaller and simpler. HeartWare is developing a miniaturized version of its approved continuous flow centrifugal force LVAD. The ReliantHeart aVAD, an intraventricular device less than 2.5 cm in diameter, is approved in Europe and under study in the U.S. The Thoratec HeartMate III is a smaller version of the HeartMate II, which is FDA-approved as destination therapy. And the Circulite Synergy micropump, designed to provide partial circulatory support to patients who don’t require a full-force LVAD, is the size of a AA battery.
Dr. Woo reported having no financial conflicts.
bjancin@frontlinemedcom.com
SNOWMASS, COLO. – Multifaceted progress in mechanical circulatory support as long-term therapy in end-stage heart failure is happening at a brisk pace, Y. Joseph C. Woo, MD, reported at the Annual Cardiovascular Conference at Snowmass.
declared Dr. Woo, professor and chair of the department of cardiothoracic surgery at Stanford (Calif.) University.
That’s quite a prediction, especially considering the source: Stanford is where the late Dr. Norman Shumway – widely considered “the father of heart transplantation” – performed the first adult heart transplant in the United States in 1968.
Dr. Woo was coauthor of an American Heart Association policy statement on the future of cardiovascular disease in the United States, which forecast a 25% increase in heart failure between 2010 and 2030 (Circulation. 2011 Mar 1;123[8]:933-44). There is simply no way that heart transplantation can begin to meet the projected growing need for effective therapy in patients with end-stage disease.
Here’s what Dr. Woo sees as the future of MCS:
Minimally invasive implantation
At Stanford, LVAD implantations are now routinely done off-pump on a beating heart.
“We clamp only when there is a sound reason, like the presence of left ventricular thrombus, where you run the risk of embolization without the cross clamp,” the surgeon said.
Concomitant valvular surgery
At Stanford and other centers of excellence, surgeons perform additional procedures as warranted while they implant an LVAD, including atrial fibrillation ablation, revascularization of the right heart coronaries, patent foramen ovale closure, and repair of the tricuspid, pulmonic, or aortic valves.
Enhanced right ventricular management
Survival is greatly impaired if a patient with an LVAD later requires the addition of a right ventricular assist device. This realization has led to the development of multiple preoperative risk scoring systems by the Stanford group (Ann Thorac Surg. 2013 Sep;96[3]:857-63) and others, including investigators at the Deutsche Herzzentrum Berlin, the world’s busiest heart transplant center. The purpose is to identify upfront those patients who are likely to later develop right heart failure so they can receive biventricular MCS from the start.
Adjunctive biologic therapies
Intramyocardial injection of 25 million allogeneic mesenchymal precursor cells during LVAD implantation appeared to be safe and showed a promising efficacy signal in a 30-patient, multicenter, double-blind, placebo-controlled, National Institutes of Health–sponsored proof of concept study in which Dr. Woo was a coinvestigator (Circulation. 2014 Jun 3;129[22]:2287-96).
The goal of this research effort is to provide a cell therapy assist to the LVAD as a bridge to recovery of left ventricular function such that the device might eventually no longer be needed, he explained.
These cells are immune privileged. They can be transplanted into recipients without need for immunosuppressive therapy or HLA matching, basically as an off the shelf product. Rather than transforming into cardiomyocytes, it appears that the mechanism by which the donor cells enhance cardiac performance in heart failure is via secretion of a shower of growth and angiogenic factors.
Based upon the encouraging results of the initial study, a 90-patient, phase II, double-blind clinical trial is underway. In order to better evaluate efficacy, this time the patients will receive 150 million mesenchymal precursor cells rather than 25 million.
New technologies
The developmental pipeline is chock full of MCS devices. The trend is to go smaller and simpler. HeartWare is developing a miniaturized version of its approved continuous flow centrifugal force LVAD. The ReliantHeart aVAD, an intraventricular device less than 2.5 cm in diameter, is approved in Europe and under study in the U.S. The Thoratec HeartMate III is a smaller version of the HeartMate II, which is FDA-approved as destination therapy. And the Circulite Synergy micropump, designed to provide partial circulatory support to patients who don’t require a full-force LVAD, is the size of a AA battery.
Dr. Woo reported having no financial conflicts.
bjancin@frontlinemedcom.com
SNOWMASS, COLO. – Multifaceted progress in mechanical circulatory support as long-term therapy in end-stage heart failure is happening at a brisk pace, Y. Joseph C. Woo, MD, reported at the Annual Cardiovascular Conference at Snowmass.
declared Dr. Woo, professor and chair of the department of cardiothoracic surgery at Stanford (Calif.) University.
That’s quite a prediction, especially considering the source: Stanford is where the late Dr. Norman Shumway – widely considered “the father of heart transplantation” – performed the first adult heart transplant in the United States in 1968.
Dr. Woo was coauthor of an American Heart Association policy statement on the future of cardiovascular disease in the United States, which forecast a 25% increase in heart failure between 2010 and 2030 (Circulation. 2011 Mar 1;123[8]:933-44). There is simply no way that heart transplantation can begin to meet the projected growing need for effective therapy in patients with end-stage disease.
Here’s what Dr. Woo sees as the future of MCS:
Minimally invasive implantation
At Stanford, LVAD implantations are now routinely done off-pump on a beating heart.
“We clamp only when there is a sound reason, like the presence of left ventricular thrombus, where you run the risk of embolization without the cross clamp,” the surgeon said.
Concomitant valvular surgery
At Stanford and other centers of excellence, surgeons perform additional procedures as warranted while they implant an LVAD, including atrial fibrillation ablation, revascularization of the right heart coronaries, patent foramen ovale closure, and repair of the tricuspid, pulmonic, or aortic valves.
Enhanced right ventricular management
Survival is greatly impaired if a patient with an LVAD later requires the addition of a right ventricular assist device. This realization has led to the development of multiple preoperative risk scoring systems by the Stanford group (Ann Thorac Surg. 2013 Sep;96[3]:857-63) and others, including investigators at the Deutsche Herzzentrum Berlin, the world’s busiest heart transplant center. The purpose is to identify upfront those patients who are likely to later develop right heart failure so they can receive biventricular MCS from the start.
Adjunctive biologic therapies
Intramyocardial injection of 25 million allogeneic mesenchymal precursor cells during LVAD implantation appeared to be safe and showed a promising efficacy signal in a 30-patient, multicenter, double-blind, placebo-controlled, National Institutes of Health–sponsored proof of concept study in which Dr. Woo was a coinvestigator (Circulation. 2014 Jun 3;129[22]:2287-96).
The goal of this research effort is to provide a cell therapy assist to the LVAD as a bridge to recovery of left ventricular function such that the device might eventually no longer be needed, he explained.
These cells are immune privileged. They can be transplanted into recipients without need for immunosuppressive therapy or HLA matching, basically as an off the shelf product. Rather than transforming into cardiomyocytes, it appears that the mechanism by which the donor cells enhance cardiac performance in heart failure is via secretion of a shower of growth and angiogenic factors.
Based upon the encouraging results of the initial study, a 90-patient, phase II, double-blind clinical trial is underway. In order to better evaluate efficacy, this time the patients will receive 150 million mesenchymal precursor cells rather than 25 million.
New technologies
The developmental pipeline is chock full of MCS devices. The trend is to go smaller and simpler. HeartWare is developing a miniaturized version of its approved continuous flow centrifugal force LVAD. The ReliantHeart aVAD, an intraventricular device less than 2.5 cm in diameter, is approved in Europe and under study in the U.S. The Thoratec HeartMate III is a smaller version of the HeartMate II, which is FDA-approved as destination therapy. And the Circulite Synergy micropump, designed to provide partial circulatory support to patients who don’t require a full-force LVAD, is the size of a AA battery.
Dr. Woo reported having no financial conflicts.
bjancin@frontlinemedcom.com
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Prolonged dual-antiplatelet therapy after PCI challenged
WASHINGTON – Guidelines were recently modified to permit shorter duration of dual-antiplatelet therapy (DAPT) after percutaneous coronary intervention, but a series of ongoing trials are evaluating whether DAPT can be abandoned altogether in many if not most percutaneous coronary intervention (PCI) patients, according to a review of this major potential change in direction presented at CRT 2017 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
“The 1-year duration of dual-antiplatelet therapy post PCI with a drug eluting stent is based on anecdotal historical data,” asserted Patrick W. Serruys, MD, PhD, professor of cardiology, Imperial College, London. Citing several sets of data consistent with the conclusion that single agents provide adequate protection against thrombus formation but reduced risk of bleeding relative to DAPT, he suggested that it is now critical to challenge the old standard.
It has long been understood that greater protection against thrombus formation with more aggressive antiplatelet therapy is purchased with a higher risk of bleeding, but there appears to be a fundamental change in orientation. Several new pieces of evidence, including data showing that shorter duration of DAPT is as good as longer duration, has placed this trade-off in doubt at least over the longer term.
To some degree, the current standard was based on the premise that thrombotic events are more important than bleeding events, according to Usman Baber, MD, assistant professor of cardiology, Icahn School of Medicine at Mount Sinai, New York. He said, “That thought process really dominated thinking for many years, but this is completely unsupported by the data.” Instead, he noted that hazard ratios after thrombotic and bleeding events are almost identical, but the risk of death after bleeding is more persistent, while risk of ischemic events typically diminishes after an initial peak.
There is no shortage of studies that have attempted to determine the ideal combination and duration of antiplatelet therapies after PCI, but the heterogeneity of study design has prohibited definitive conclusions. In particular, Dr. Serruys suggested that there is no level 1 evidence confirming the value of adding aspirin, which he emphasized has a relatively nonspecific effect, over that of P2Y12 inhibitor alone.
In the design phase of the GLOBAL LEADERS trial, Dr. Serruys recounted, he first argued for a design in which aspirin was eliminated altogether and then for a protocol with only a single week of aspirin, but was met with strong objections each time. In the end, the experimental protocol calls for 1 month of aspirin plus ticagrelor before patients are continued on ticagrelor alone. This is being compared with the current standard, which is aspirin plus ticagrelor or clopidogrel for 12 months followed by another 12 months of aspirin alone.
GLOBAL LEADERS is an all-comers trial in which patients are randomized before PCI. All patients at the 131 participating centers in 18 countries are receiving the same stent (BioMatrix Flex). The primary endpoint is all-cause mortality, and enrollment is completed. The results are expected in November of this year.
There are numerous other studies addressing the same question. Like GLOBAL LEADERS, the TWILIGHT trial is also investigator-initiated and is near the halfway mark for a 9,000-patient enrollment. In this study, patients are being randomized to aspirin plus ticagrelor or ticagrelor alone after they have achieved a successful placement of a drug-eluting stent. This trial, however, is restricted to those with diabetes, chronic kidney disease, or other high-risk features. The primary endpoint is major bleeding. Completion is expected in 2019.
The SMART-CHOICE trial is enrolling roughly 5,000 PCI patients receiving a drug-eluting stent. Patients are being randomized to a P2Y12 antagonist monotherapy plus aspirin or the P2Y12 antagonist alone. The primary endpoint is a composite of major adverse cardiovascular events as well as major bleeding events.
After the STOP DAPT trial showed that 3 months of DAPT after PCI was as safe as prolonged DAPT in patients receiving a everolimus-eluting chromium-cobalt stent (Cardiovasc Interv Ther. 2016;31:196-209), the same group of Japanese investigators conceived the STOP-DAPT2 trial. In this trial, 3,000 patients are being randomized a standard DAPT or clopidogrel monotherapy beginning 1 month after PCI. The primary outcome is similar to that of SMART-CHOICE.
In yet another trial cited by Dr. Serruys, patients will receive DAPT only if the PCI outcome is considered suboptimal. For those judged to have a good result, patients will receive ticagrelor alone. Outcomes at the end of 1 year will be monitored.
The movement toward antiplatelet monotherapy is driven by recognition that “the need to mitigate the risk of bleeding is an important as the need to mitigate thrombosis,” Dr. Baber explained. Like Dr. Serruys, he believes it is important to challenge the standard.
“By testing single, specific, and potent antiplatelet therapy and getting rid of the old and nonspecific platelet drug called acetylsalicylic acid, we may be able to simplify risk management after PCI,” agreed Dr. Serruys. If, as expected, the GLOBAL LEADERS and other monotherapy antiplatelet trials meet their endpoints, it will mean a major evolution in postprocedural risk management.
Dr. Serruys reported no financial relationships to disclose.
WASHINGTON – Guidelines were recently modified to permit shorter duration of dual-antiplatelet therapy (DAPT) after percutaneous coronary intervention, but a series of ongoing trials are evaluating whether DAPT can be abandoned altogether in many if not most percutaneous coronary intervention (PCI) patients, according to a review of this major potential change in direction presented at CRT 2017 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
“The 1-year duration of dual-antiplatelet therapy post PCI with a drug eluting stent is based on anecdotal historical data,” asserted Patrick W. Serruys, MD, PhD, professor of cardiology, Imperial College, London. Citing several sets of data consistent with the conclusion that single agents provide adequate protection against thrombus formation but reduced risk of bleeding relative to DAPT, he suggested that it is now critical to challenge the old standard.
It has long been understood that greater protection against thrombus formation with more aggressive antiplatelet therapy is purchased with a higher risk of bleeding, but there appears to be a fundamental change in orientation. Several new pieces of evidence, including data showing that shorter duration of DAPT is as good as longer duration, has placed this trade-off in doubt at least over the longer term.
To some degree, the current standard was based on the premise that thrombotic events are more important than bleeding events, according to Usman Baber, MD, assistant professor of cardiology, Icahn School of Medicine at Mount Sinai, New York. He said, “That thought process really dominated thinking for many years, but this is completely unsupported by the data.” Instead, he noted that hazard ratios after thrombotic and bleeding events are almost identical, but the risk of death after bleeding is more persistent, while risk of ischemic events typically diminishes after an initial peak.
There is no shortage of studies that have attempted to determine the ideal combination and duration of antiplatelet therapies after PCI, but the heterogeneity of study design has prohibited definitive conclusions. In particular, Dr. Serruys suggested that there is no level 1 evidence confirming the value of adding aspirin, which he emphasized has a relatively nonspecific effect, over that of P2Y12 inhibitor alone.
In the design phase of the GLOBAL LEADERS trial, Dr. Serruys recounted, he first argued for a design in which aspirin was eliminated altogether and then for a protocol with only a single week of aspirin, but was met with strong objections each time. In the end, the experimental protocol calls for 1 month of aspirin plus ticagrelor before patients are continued on ticagrelor alone. This is being compared with the current standard, which is aspirin plus ticagrelor or clopidogrel for 12 months followed by another 12 months of aspirin alone.
GLOBAL LEADERS is an all-comers trial in which patients are randomized before PCI. All patients at the 131 participating centers in 18 countries are receiving the same stent (BioMatrix Flex). The primary endpoint is all-cause mortality, and enrollment is completed. The results are expected in November of this year.
There are numerous other studies addressing the same question. Like GLOBAL LEADERS, the TWILIGHT trial is also investigator-initiated and is near the halfway mark for a 9,000-patient enrollment. In this study, patients are being randomized to aspirin plus ticagrelor or ticagrelor alone after they have achieved a successful placement of a drug-eluting stent. This trial, however, is restricted to those with diabetes, chronic kidney disease, or other high-risk features. The primary endpoint is major bleeding. Completion is expected in 2019.
The SMART-CHOICE trial is enrolling roughly 5,000 PCI patients receiving a drug-eluting stent. Patients are being randomized to a P2Y12 antagonist monotherapy plus aspirin or the P2Y12 antagonist alone. The primary endpoint is a composite of major adverse cardiovascular events as well as major bleeding events.
After the STOP DAPT trial showed that 3 months of DAPT after PCI was as safe as prolonged DAPT in patients receiving a everolimus-eluting chromium-cobalt stent (Cardiovasc Interv Ther. 2016;31:196-209), the same group of Japanese investigators conceived the STOP-DAPT2 trial. In this trial, 3,000 patients are being randomized a standard DAPT or clopidogrel monotherapy beginning 1 month after PCI. The primary outcome is similar to that of SMART-CHOICE.
In yet another trial cited by Dr. Serruys, patients will receive DAPT only if the PCI outcome is considered suboptimal. For those judged to have a good result, patients will receive ticagrelor alone. Outcomes at the end of 1 year will be monitored.
The movement toward antiplatelet monotherapy is driven by recognition that “the need to mitigate the risk of bleeding is an important as the need to mitigate thrombosis,” Dr. Baber explained. Like Dr. Serruys, he believes it is important to challenge the standard.
“By testing single, specific, and potent antiplatelet therapy and getting rid of the old and nonspecific platelet drug called acetylsalicylic acid, we may be able to simplify risk management after PCI,” agreed Dr. Serruys. If, as expected, the GLOBAL LEADERS and other monotherapy antiplatelet trials meet their endpoints, it will mean a major evolution in postprocedural risk management.
Dr. Serruys reported no financial relationships to disclose.
WASHINGTON – Guidelines were recently modified to permit shorter duration of dual-antiplatelet therapy (DAPT) after percutaneous coronary intervention, but a series of ongoing trials are evaluating whether DAPT can be abandoned altogether in many if not most percutaneous coronary intervention (PCI) patients, according to a review of this major potential change in direction presented at CRT 2017 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
“The 1-year duration of dual-antiplatelet therapy post PCI with a drug eluting stent is based on anecdotal historical data,” asserted Patrick W. Serruys, MD, PhD, professor of cardiology, Imperial College, London. Citing several sets of data consistent with the conclusion that single agents provide adequate protection against thrombus formation but reduced risk of bleeding relative to DAPT, he suggested that it is now critical to challenge the old standard.
It has long been understood that greater protection against thrombus formation with more aggressive antiplatelet therapy is purchased with a higher risk of bleeding, but there appears to be a fundamental change in orientation. Several new pieces of evidence, including data showing that shorter duration of DAPT is as good as longer duration, has placed this trade-off in doubt at least over the longer term.
To some degree, the current standard was based on the premise that thrombotic events are more important than bleeding events, according to Usman Baber, MD, assistant professor of cardiology, Icahn School of Medicine at Mount Sinai, New York. He said, “That thought process really dominated thinking for many years, but this is completely unsupported by the data.” Instead, he noted that hazard ratios after thrombotic and bleeding events are almost identical, but the risk of death after bleeding is more persistent, while risk of ischemic events typically diminishes after an initial peak.
There is no shortage of studies that have attempted to determine the ideal combination and duration of antiplatelet therapies after PCI, but the heterogeneity of study design has prohibited definitive conclusions. In particular, Dr. Serruys suggested that there is no level 1 evidence confirming the value of adding aspirin, which he emphasized has a relatively nonspecific effect, over that of P2Y12 inhibitor alone.
In the design phase of the GLOBAL LEADERS trial, Dr. Serruys recounted, he first argued for a design in which aspirin was eliminated altogether and then for a protocol with only a single week of aspirin, but was met with strong objections each time. In the end, the experimental protocol calls for 1 month of aspirin plus ticagrelor before patients are continued on ticagrelor alone. This is being compared with the current standard, which is aspirin plus ticagrelor or clopidogrel for 12 months followed by another 12 months of aspirin alone.
GLOBAL LEADERS is an all-comers trial in which patients are randomized before PCI. All patients at the 131 participating centers in 18 countries are receiving the same stent (BioMatrix Flex). The primary endpoint is all-cause mortality, and enrollment is completed. The results are expected in November of this year.
There are numerous other studies addressing the same question. Like GLOBAL LEADERS, the TWILIGHT trial is also investigator-initiated and is near the halfway mark for a 9,000-patient enrollment. In this study, patients are being randomized to aspirin plus ticagrelor or ticagrelor alone after they have achieved a successful placement of a drug-eluting stent. This trial, however, is restricted to those with diabetes, chronic kidney disease, or other high-risk features. The primary endpoint is major bleeding. Completion is expected in 2019.
The SMART-CHOICE trial is enrolling roughly 5,000 PCI patients receiving a drug-eluting stent. Patients are being randomized to a P2Y12 antagonist monotherapy plus aspirin or the P2Y12 antagonist alone. The primary endpoint is a composite of major adverse cardiovascular events as well as major bleeding events.
After the STOP DAPT trial showed that 3 months of DAPT after PCI was as safe as prolonged DAPT in patients receiving a everolimus-eluting chromium-cobalt stent (Cardiovasc Interv Ther. 2016;31:196-209), the same group of Japanese investigators conceived the STOP-DAPT2 trial. In this trial, 3,000 patients are being randomized a standard DAPT or clopidogrel monotherapy beginning 1 month after PCI. The primary outcome is similar to that of SMART-CHOICE.
In yet another trial cited by Dr. Serruys, patients will receive DAPT only if the PCI outcome is considered suboptimal. For those judged to have a good result, patients will receive ticagrelor alone. Outcomes at the end of 1 year will be monitored.
The movement toward antiplatelet monotherapy is driven by recognition that “the need to mitigate the risk of bleeding is an important as the need to mitigate thrombosis,” Dr. Baber explained. Like Dr. Serruys, he believes it is important to challenge the standard.
“By testing single, specific, and potent antiplatelet therapy and getting rid of the old and nonspecific platelet drug called acetylsalicylic acid, we may be able to simplify risk management after PCI,” agreed Dr. Serruys. If, as expected, the GLOBAL LEADERS and other monotherapy antiplatelet trials meet their endpoints, it will mean a major evolution in postprocedural risk management.
Dr. Serruys reported no financial relationships to disclose.
EXPERT ANALYSIS FROM CRT 2017
Robotic PCI success rates higher with radial access
WASHINGTON – The clinical and technical success rates are higher among patients undergoing robotic percutaneous coronary interventions through radial than femoral access, according to registry data presented at CRT 2017 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
Although both the clinical and technical success rates were high with either type of access, the advantage for radial over femoral access was significant for each, reported Ali Pourdjabbar, MD, an interventional cardiologist completing his fellowship at the University of California, San Diego. However, as this was not a randomized trial, he placed emphasis on the message that robotic percutaneous coronary intervention (PCI) is safe and effective when performed through either access point.
Clinical success, defined as less than 30% residual occlusion with TIMI3 flow and no major adverse cardiovascular events, such as myocardial infarction, cardiovascular death, or revascularization, was achieved in 99.4% of the 310 patients treated through radial access and 94.7% of the 191 patients treated through femoral access (P = .002). Technical success, defined as PCI performed without any manual assistance, was achieved in 92.4% of procedures performed through radial access and 86.7% of those performed through femoral access (P = .03).
There were no significant differences in the two groups for contrast use or fluoroscopy time, but the time to completing PCI was shorter with the radial approach (57 vs. 66 minutes; P less than .04).
However, the groups did differ in baseline characteristics, according to Dr. Pourdjabbar. Patients undergoing robotic PCI through a radial approach were younger, less likely to have diabetes, and less likely to have received a prior PCI. Most importantly, they were less likely to have complex lesions. Patients treated with radial access had higher average body mass indexes.
“It is important to recognize that this was a nonrandomized, retrospective analysis,” Dr. Pourdjabbar emphasized. He noted that one reason for this analysis was to confirm that efficacy and safety was just as good with radial access, which although an approved robotic approach, was supported with fewer data at the time that the device became available.
However, it is notable that 60% of the robotic procedures were done with the radial approach, which is approximately double the proportion currently performed in the United States when done manually, according to data presented by Dr. Pourdjabbar. He noted that radial access has been more commonly used outside of the United States, but rates have also started climbing in this country, rising from less than 5% of cases in 2005 to nearly one third of cases in the most recent analysis. It is unclear why robotic procedures are performed more frequently through radial access, but Dr. Pourdjabbar speculated that centers innovating with robots might also be in the vanguard of the movement toward radial PCI.
Of reasons to consider robots, Dr. Pourdjabbar suggested that the safety advantages for the interventionalist are particularly compelling. Citing a variety of data associating cath lab radiation exposure to health risks for physicians and staff, Dr. Pourdjabbar explained that the operator performs robotic PCI from a shielded cockpit that completely eliminates exposure to radiation. A next generation robotic device, called the CorPath GRX System, is expected to further reduce opportunities for radiation exposure by allowing the operator to disengage the guide catheter in cases when this had to be done manually with the first generation CorPath 200 system.
Asked about the learning curve of PCI robotics, Dr. Pourdjabbar said that the principles appear to be grasped quickly by interventionalists, but he acknowledged that his experience as a training fellow has been limited. However, Rajesh V. Swaminathan, MD, an interventionalist affiliated with Duke University, Durham, N.C., who has experience with robotic PCI, reported that although the tactile sense of the guide wire is lost in robotic PCI, the procedure has typically proceeded more quickly in his hands once access is achieved.
“The greatest learning curve may with the staff that has to get used to not having the interventionalist at the table,” observed Dr. Swaminathan, who was a moderator of the session in which these data were presented.
WASHINGTON – The clinical and technical success rates are higher among patients undergoing robotic percutaneous coronary interventions through radial than femoral access, according to registry data presented at CRT 2017 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
Although both the clinical and technical success rates were high with either type of access, the advantage for radial over femoral access was significant for each, reported Ali Pourdjabbar, MD, an interventional cardiologist completing his fellowship at the University of California, San Diego. However, as this was not a randomized trial, he placed emphasis on the message that robotic percutaneous coronary intervention (PCI) is safe and effective when performed through either access point.
Clinical success, defined as less than 30% residual occlusion with TIMI3 flow and no major adverse cardiovascular events, such as myocardial infarction, cardiovascular death, or revascularization, was achieved in 99.4% of the 310 patients treated through radial access and 94.7% of the 191 patients treated through femoral access (P = .002). Technical success, defined as PCI performed without any manual assistance, was achieved in 92.4% of procedures performed through radial access and 86.7% of those performed through femoral access (P = .03).
There were no significant differences in the two groups for contrast use or fluoroscopy time, but the time to completing PCI was shorter with the radial approach (57 vs. 66 minutes; P less than .04).
However, the groups did differ in baseline characteristics, according to Dr. Pourdjabbar. Patients undergoing robotic PCI through a radial approach were younger, less likely to have diabetes, and less likely to have received a prior PCI. Most importantly, they were less likely to have complex lesions. Patients treated with radial access had higher average body mass indexes.
“It is important to recognize that this was a nonrandomized, retrospective analysis,” Dr. Pourdjabbar emphasized. He noted that one reason for this analysis was to confirm that efficacy and safety was just as good with radial access, which although an approved robotic approach, was supported with fewer data at the time that the device became available.
However, it is notable that 60% of the robotic procedures were done with the radial approach, which is approximately double the proportion currently performed in the United States when done manually, according to data presented by Dr. Pourdjabbar. He noted that radial access has been more commonly used outside of the United States, but rates have also started climbing in this country, rising from less than 5% of cases in 2005 to nearly one third of cases in the most recent analysis. It is unclear why robotic procedures are performed more frequently through radial access, but Dr. Pourdjabbar speculated that centers innovating with robots might also be in the vanguard of the movement toward radial PCI.
Of reasons to consider robots, Dr. Pourdjabbar suggested that the safety advantages for the interventionalist are particularly compelling. Citing a variety of data associating cath lab radiation exposure to health risks for physicians and staff, Dr. Pourdjabbar explained that the operator performs robotic PCI from a shielded cockpit that completely eliminates exposure to radiation. A next generation robotic device, called the CorPath GRX System, is expected to further reduce opportunities for radiation exposure by allowing the operator to disengage the guide catheter in cases when this had to be done manually with the first generation CorPath 200 system.
Asked about the learning curve of PCI robotics, Dr. Pourdjabbar said that the principles appear to be grasped quickly by interventionalists, but he acknowledged that his experience as a training fellow has been limited. However, Rajesh V. Swaminathan, MD, an interventionalist affiliated with Duke University, Durham, N.C., who has experience with robotic PCI, reported that although the tactile sense of the guide wire is lost in robotic PCI, the procedure has typically proceeded more quickly in his hands once access is achieved.
“The greatest learning curve may with the staff that has to get used to not having the interventionalist at the table,” observed Dr. Swaminathan, who was a moderator of the session in which these data were presented.
WASHINGTON – The clinical and technical success rates are higher among patients undergoing robotic percutaneous coronary interventions through radial than femoral access, according to registry data presented at CRT 2017 sponsored by the Cardiovascular Research Institute at Washington Hospital Center.
Although both the clinical and technical success rates were high with either type of access, the advantage for radial over femoral access was significant for each, reported Ali Pourdjabbar, MD, an interventional cardiologist completing his fellowship at the University of California, San Diego. However, as this was not a randomized trial, he placed emphasis on the message that robotic percutaneous coronary intervention (PCI) is safe and effective when performed through either access point.
Clinical success, defined as less than 30% residual occlusion with TIMI3 flow and no major adverse cardiovascular events, such as myocardial infarction, cardiovascular death, or revascularization, was achieved in 99.4% of the 310 patients treated through radial access and 94.7% of the 191 patients treated through femoral access (P = .002). Technical success, defined as PCI performed without any manual assistance, was achieved in 92.4% of procedures performed through radial access and 86.7% of those performed through femoral access (P = .03).
There were no significant differences in the two groups for contrast use or fluoroscopy time, but the time to completing PCI was shorter with the radial approach (57 vs. 66 minutes; P less than .04).
However, the groups did differ in baseline characteristics, according to Dr. Pourdjabbar. Patients undergoing robotic PCI through a radial approach were younger, less likely to have diabetes, and less likely to have received a prior PCI. Most importantly, they were less likely to have complex lesions. Patients treated with radial access had higher average body mass indexes.
“It is important to recognize that this was a nonrandomized, retrospective analysis,” Dr. Pourdjabbar emphasized. He noted that one reason for this analysis was to confirm that efficacy and safety was just as good with radial access, which although an approved robotic approach, was supported with fewer data at the time that the device became available.
However, it is notable that 60% of the robotic procedures were done with the radial approach, which is approximately double the proportion currently performed in the United States when done manually, according to data presented by Dr. Pourdjabbar. He noted that radial access has been more commonly used outside of the United States, but rates have also started climbing in this country, rising from less than 5% of cases in 2005 to nearly one third of cases in the most recent analysis. It is unclear why robotic procedures are performed more frequently through radial access, but Dr. Pourdjabbar speculated that centers innovating with robots might also be in the vanguard of the movement toward radial PCI.
Of reasons to consider robots, Dr. Pourdjabbar suggested that the safety advantages for the interventionalist are particularly compelling. Citing a variety of data associating cath lab radiation exposure to health risks for physicians and staff, Dr. Pourdjabbar explained that the operator performs robotic PCI from a shielded cockpit that completely eliminates exposure to radiation. A next generation robotic device, called the CorPath GRX System, is expected to further reduce opportunities for radiation exposure by allowing the operator to disengage the guide catheter in cases when this had to be done manually with the first generation CorPath 200 system.
Asked about the learning curve of PCI robotics, Dr. Pourdjabbar said that the principles appear to be grasped quickly by interventionalists, but he acknowledged that his experience as a training fellow has been limited. However, Rajesh V. Swaminathan, MD, an interventionalist affiliated with Duke University, Durham, N.C., who has experience with robotic PCI, reported that although the tactile sense of the guide wire is lost in robotic PCI, the procedure has typically proceeded more quickly in his hands once access is achieved.
“The greatest learning curve may with the staff that has to get used to not having the interventionalist at the table,” observed Dr. Swaminathan, who was a moderator of the session in which these data were presented.
AT CRT 2017
Key clinical point: Registry data shows higher success rate for radial versus femoral access in robotic percutaneous coronary interventions.
Major finding: In robotic PCI, the clinical success rate was 99.4% with radial access and 94.7% (P = .002) with femoral access.
Data source: A nonrandomized, retrospective analysis.
Disclosures: Dr. Pourdjabbar reported no financial relationships to disclose.
Consider ultraslow thrombolysis for mechanical valve thrombosis
SNOWMASS, COLO. – Ultraslow infusion of a very-low-dose thrombolytic agent for treatment of mechanical prosthetic valve thrombosis appears to be as effective as surgery – the former first-line therapy – and sports a far lower stroke risk, Rick A. Nishimura, MD, said at the Annual Cardiovascular Conference at Snowmass.
“I’m not saying you have to use this, but I think it’s reasonable to consider it, especially if the patient is at high risk for surgery and low risk for thrombolysis,” according to Dr. Nishimura, professor of cardiovascular diseases and hypertension at the Mayo Clinic in Rochester, Minn.
He added that he and his Mayo colleagues have begun using the novel therapy and are favorably impressed with the resultant complete normalization of valve gradients and low complication rate.
Dr. Nishimura was cochair of the writing committee for the current American College of Cardiology/American Heart Association guidelines for management of valvular heart disease (Circulation. 2014 Jun 10;129[23]:e521-643). Those guidelines state that emergency surgery is the treatment of choice for thrombosis of a left-sided mechanical heart valve. That strong recommendation was based on a dozen nonrandomized studies reported prior to 2013 which showed a 95% success rate with surgery compared with 75% with conventional large-bolus thrombolytic therapy, a high 10%-12% mortality with either form of therapy, and a stroke risk of 12%-14% with thrombolytic therapy, substantially higher than for surgery.
Since release of the ACC/AHA guidelines, however, there’s been an important new development: Three groups outside of the United States have pioneered ultraslow thrombolytic therapy for mechanical prosthetic valve thrombosis. The supporting evidence comes from cohort studies, with no randomized trials done to date. But the collective reported experience from these three research teams shows a 90%-95% success rate – comparable to surgery – along with stroke and mortality rates in the low single digits.
The Turkish group waits until the patient’s international normalized ratio (INR) is below 2.5, then administers 25 mg of tissue plasminogen activator guided by transesophageal echocardiography (TEE) over 25 hours.
“We traditionally give 90 mg over 1 hour, so this is very, very slow therapy,” Dr. Nishimura observed.
After the 24-hour infusion, TEE is repeated. If imaging shows the clot is not resolved, another 25 mg of tissue plasminogen activator is given over 24 hours. This process is repeated for up to 8 days as needed (Am Heart J. 2015 Aug;170[2]:409-18).
Dr. Nishimura advised reserving ultraslow thrombolytic therapy for patients who are hemodynamically stable; this treatment takes a while to work, so patients in severe heart failure should be sent straight away to surgery. The novel therapy is best suited for patients with recent-onset mechanical valve thrombosis, a low INR, TEE evidence that the clot isn’t huge, and/or when surgical expertise isn’t readily available.
Before you can treat a prosthetic mechanical valve thrombosis, however, you have to make the diagnosis. Here’s what Dr. Nishimura recommends: First, suspect the condition on the basis of clinical symptoms of heart failure and dull, muffled S1 and S2 sounds on auscultation, especially in a patient who presents with a low INR.
Next, prove that obstruction is present via Doppler echocardiographic evidence of an abnormal gradient across the mechanical valve.
Finally, determine if the mechanical valve shows abnormal disc motion with sticking leaflets. TEE is excellent for visualizing a mechanical mitral valve but isn’t helpful if it’s a mechanical aortic valve.
“Old-fashioned fluoroscopy is the best approach for looking at leaflet motion in the atrial valve and mitral valve. We’ve got 3-D cine now that provides beautiful images, but if you can get the same information with a quick fluoroscopy, go with the fluoroscopy,” the cardiologist suggested.
He reported having no financial conflicts of interest.
SNOWMASS, COLO. – Ultraslow infusion of a very-low-dose thrombolytic agent for treatment of mechanical prosthetic valve thrombosis appears to be as effective as surgery – the former first-line therapy – and sports a far lower stroke risk, Rick A. Nishimura, MD, said at the Annual Cardiovascular Conference at Snowmass.
“I’m not saying you have to use this, but I think it’s reasonable to consider it, especially if the patient is at high risk for surgery and low risk for thrombolysis,” according to Dr. Nishimura, professor of cardiovascular diseases and hypertension at the Mayo Clinic in Rochester, Minn.
He added that he and his Mayo colleagues have begun using the novel therapy and are favorably impressed with the resultant complete normalization of valve gradients and low complication rate.
Dr. Nishimura was cochair of the writing committee for the current American College of Cardiology/American Heart Association guidelines for management of valvular heart disease (Circulation. 2014 Jun 10;129[23]:e521-643). Those guidelines state that emergency surgery is the treatment of choice for thrombosis of a left-sided mechanical heart valve. That strong recommendation was based on a dozen nonrandomized studies reported prior to 2013 which showed a 95% success rate with surgery compared with 75% with conventional large-bolus thrombolytic therapy, a high 10%-12% mortality with either form of therapy, and a stroke risk of 12%-14% with thrombolytic therapy, substantially higher than for surgery.
Since release of the ACC/AHA guidelines, however, there’s been an important new development: Three groups outside of the United States have pioneered ultraslow thrombolytic therapy for mechanical prosthetic valve thrombosis. The supporting evidence comes from cohort studies, with no randomized trials done to date. But the collective reported experience from these three research teams shows a 90%-95% success rate – comparable to surgery – along with stroke and mortality rates in the low single digits.
The Turkish group waits until the patient’s international normalized ratio (INR) is below 2.5, then administers 25 mg of tissue plasminogen activator guided by transesophageal echocardiography (TEE) over 25 hours.
“We traditionally give 90 mg over 1 hour, so this is very, very slow therapy,” Dr. Nishimura observed.
After the 24-hour infusion, TEE is repeated. If imaging shows the clot is not resolved, another 25 mg of tissue plasminogen activator is given over 24 hours. This process is repeated for up to 8 days as needed (Am Heart J. 2015 Aug;170[2]:409-18).
Dr. Nishimura advised reserving ultraslow thrombolytic therapy for patients who are hemodynamically stable; this treatment takes a while to work, so patients in severe heart failure should be sent straight away to surgery. The novel therapy is best suited for patients with recent-onset mechanical valve thrombosis, a low INR, TEE evidence that the clot isn’t huge, and/or when surgical expertise isn’t readily available.
Before you can treat a prosthetic mechanical valve thrombosis, however, you have to make the diagnosis. Here’s what Dr. Nishimura recommends: First, suspect the condition on the basis of clinical symptoms of heart failure and dull, muffled S1 and S2 sounds on auscultation, especially in a patient who presents with a low INR.
Next, prove that obstruction is present via Doppler echocardiographic evidence of an abnormal gradient across the mechanical valve.
Finally, determine if the mechanical valve shows abnormal disc motion with sticking leaflets. TEE is excellent for visualizing a mechanical mitral valve but isn’t helpful if it’s a mechanical aortic valve.
“Old-fashioned fluoroscopy is the best approach for looking at leaflet motion in the atrial valve and mitral valve. We’ve got 3-D cine now that provides beautiful images, but if you can get the same information with a quick fluoroscopy, go with the fluoroscopy,” the cardiologist suggested.
He reported having no financial conflicts of interest.
SNOWMASS, COLO. – Ultraslow infusion of a very-low-dose thrombolytic agent for treatment of mechanical prosthetic valve thrombosis appears to be as effective as surgery – the former first-line therapy – and sports a far lower stroke risk, Rick A. Nishimura, MD, said at the Annual Cardiovascular Conference at Snowmass.
“I’m not saying you have to use this, but I think it’s reasonable to consider it, especially if the patient is at high risk for surgery and low risk for thrombolysis,” according to Dr. Nishimura, professor of cardiovascular diseases and hypertension at the Mayo Clinic in Rochester, Minn.
He added that he and his Mayo colleagues have begun using the novel therapy and are favorably impressed with the resultant complete normalization of valve gradients and low complication rate.
Dr. Nishimura was cochair of the writing committee for the current American College of Cardiology/American Heart Association guidelines for management of valvular heart disease (Circulation. 2014 Jun 10;129[23]:e521-643). Those guidelines state that emergency surgery is the treatment of choice for thrombosis of a left-sided mechanical heart valve. That strong recommendation was based on a dozen nonrandomized studies reported prior to 2013 which showed a 95% success rate with surgery compared with 75% with conventional large-bolus thrombolytic therapy, a high 10%-12% mortality with either form of therapy, and a stroke risk of 12%-14% with thrombolytic therapy, substantially higher than for surgery.
Since release of the ACC/AHA guidelines, however, there’s been an important new development: Three groups outside of the United States have pioneered ultraslow thrombolytic therapy for mechanical prosthetic valve thrombosis. The supporting evidence comes from cohort studies, with no randomized trials done to date. But the collective reported experience from these three research teams shows a 90%-95% success rate – comparable to surgery – along with stroke and mortality rates in the low single digits.
The Turkish group waits until the patient’s international normalized ratio (INR) is below 2.5, then administers 25 mg of tissue plasminogen activator guided by transesophageal echocardiography (TEE) over 25 hours.
“We traditionally give 90 mg over 1 hour, so this is very, very slow therapy,” Dr. Nishimura observed.
After the 24-hour infusion, TEE is repeated. If imaging shows the clot is not resolved, another 25 mg of tissue plasminogen activator is given over 24 hours. This process is repeated for up to 8 days as needed (Am Heart J. 2015 Aug;170[2]:409-18).
Dr. Nishimura advised reserving ultraslow thrombolytic therapy for patients who are hemodynamically stable; this treatment takes a while to work, so patients in severe heart failure should be sent straight away to surgery. The novel therapy is best suited for patients with recent-onset mechanical valve thrombosis, a low INR, TEE evidence that the clot isn’t huge, and/or when surgical expertise isn’t readily available.
Before you can treat a prosthetic mechanical valve thrombosis, however, you have to make the diagnosis. Here’s what Dr. Nishimura recommends: First, suspect the condition on the basis of clinical symptoms of heart failure and dull, muffled S1 and S2 sounds on auscultation, especially in a patient who presents with a low INR.
Next, prove that obstruction is present via Doppler echocardiographic evidence of an abnormal gradient across the mechanical valve.
Finally, determine if the mechanical valve shows abnormal disc motion with sticking leaflets. TEE is excellent for visualizing a mechanical mitral valve but isn’t helpful if it’s a mechanical aortic valve.
“Old-fashioned fluoroscopy is the best approach for looking at leaflet motion in the atrial valve and mitral valve. We’ve got 3-D cine now that provides beautiful images, but if you can get the same information with a quick fluoroscopy, go with the fluoroscopy,” the cardiologist suggested.
He reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Will genome editing advance animal-to-human transplantation?
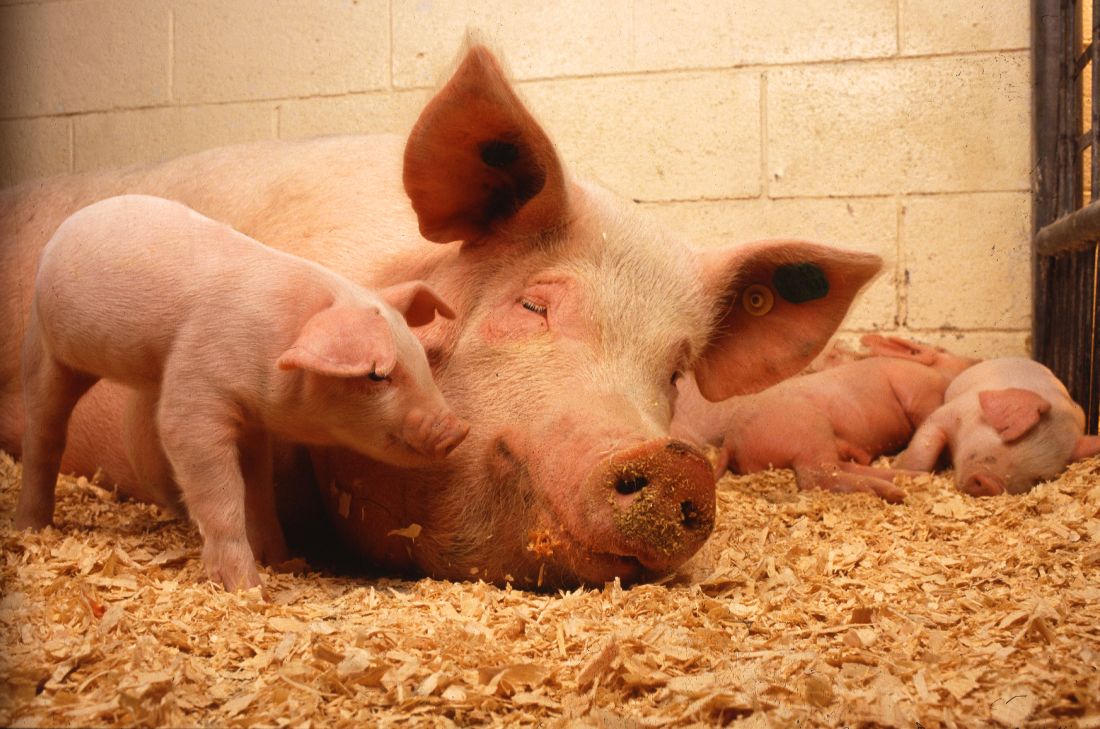
Advances in gene editing are pushing the possibility of raising pigs for organs that may be transplanted into humans with immunosuppression regimens comparable to those now used in human-to-human transplants, coauthors James Butler, MD, and A. Joseph Tector, MD, PhD, stated in an expert opinion in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:488-92).
Developments in genome editing could bring new approaches to management of cardiopulmonary diseases, Dr. Butler and Dr. Tector noted. “Recently, cardiac-specific and lung-specific applications have been described, which will allow for the rapid creation of new models of heart and lung disease,” they said. Specifically, they noted gene targeting might eventually offer a way to treat challenging genetic problems “like the heterogeneous nature of nonsquamous cell lung cancer.”
Dr. Butler is with the department of surgery at Indiana University, Indianapolis, and Dr. Tector is with the department of surgery at the University of Alabama at Birmingham.
CRISPR technology has been used in developing multiple gene knockout pigs and neutralizing three separate porcine genes that encode human xenoantigens in a single reaction, leading to efficient methods for creating pigs with multiple genetic modifications.
According to the website of the Broad Institute of MIT and Harvard, Cambridge, Mass., where researchers perfected the system to work in eukaryotes, CRISPR works by using short RNA sequences designed by researchers to guide the system to matching sequences of DNA. When the target DNA is found, Cas9 – one of the enzymes produced by the CRISPR system – binds to the DNA and cuts it, shutting the targeted gene off.
“By facilitating high-throughput model creation, CRISPR has elucidated which modifications are necessary and which are not; despite the ability to alter many loci concurrently, recent evidence has implicated three porcine genes that are responsible for the majority of human-antiporcine humoral immunity,” Dr. Butler and Dr. Tector wrote.
Those genes are the Gal[alpha]1-3 epitope (Gal-alpha), CMAH and B4GaINT2 genes. “Each of these three genes is expressed in pigs but has been evolutionarily silenced in humans,” the coauthors added.
While CRISPR genome editing has yet to reach its full potential, researchers and clinicians should pay attention, according to Dr. Butler and Dr. Tector.
More recent modifications of CRISPR technology have shown promise in not just knocking out or turning off specific genes, but rather guiding directed replacement of genes with researcher-designed substitutes. This can enable permanent transformation of functional genes with altered behavior, according to the Broad Institute website.
Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler has no relevant financial relationships to disclose.
CRISPR and CRISPR-associated proteins have emerged as effective genome editing techniques that may lead to cardiac and lung models and possibly xenotransplantation, Ari A. Mennander, MD, PhD, of the Tampere (Finland) University Heart Hospital, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:492).
The concept Dr. Butler and Dr. Tector discuss involves not using antibodies to ameliorate porcine antibodies that cause rejection in humans, but rather reengineering the genetic composition of pigs to eliminate those antibodies. “According to the wildest of dreams, these genes affecting porcine glycan expression may be silenced, and the human–antiporcine humoral immunity is controlled down to the level comparable with human allograft rejection,” Dr. Mennander said.
However, such a breakthrough carries with it consequences, Dr. Mennander said. “Should one worry about the induction of zoonosis, as well as the ethical aspects of transplanting the patient a whole organ of a pig? Would even a successful xenotransplant program seriously compete with artificial hearts or allografts?” Embracing the method too early would open its advocates to ridicule, he said.
“We are to applaud the researchers for ever-lasting and exemplary enthusiasm for a futuristic new surgical solution; the future may lie as much in current clinical solutions as in innovative discoveries based on persistent scientific experiments,” Dr. Mennander said.
Dr. Mennander had no relevant financial relationships to disclose.
CRISPR and CRISPR-associated proteins have emerged as effective genome editing techniques that may lead to cardiac and lung models and possibly xenotransplantation, Ari A. Mennander, MD, PhD, of the Tampere (Finland) University Heart Hospital, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:492).
The concept Dr. Butler and Dr. Tector discuss involves not using antibodies to ameliorate porcine antibodies that cause rejection in humans, but rather reengineering the genetic composition of pigs to eliminate those antibodies. “According to the wildest of dreams, these genes affecting porcine glycan expression may be silenced, and the human–antiporcine humoral immunity is controlled down to the level comparable with human allograft rejection,” Dr. Mennander said.
However, such a breakthrough carries with it consequences, Dr. Mennander said. “Should one worry about the induction of zoonosis, as well as the ethical aspects of transplanting the patient a whole organ of a pig? Would even a successful xenotransplant program seriously compete with artificial hearts or allografts?” Embracing the method too early would open its advocates to ridicule, he said.
“We are to applaud the researchers for ever-lasting and exemplary enthusiasm for a futuristic new surgical solution; the future may lie as much in current clinical solutions as in innovative discoveries based on persistent scientific experiments,” Dr. Mennander said.
Dr. Mennander had no relevant financial relationships to disclose.
CRISPR and CRISPR-associated proteins have emerged as effective genome editing techniques that may lead to cardiac and lung models and possibly xenotransplantation, Ari A. Mennander, MD, PhD, of the Tampere (Finland) University Heart Hospital, said in his invited commentary (J Thorac Cardiovasc Surg. 2017;153:492).
The concept Dr. Butler and Dr. Tector discuss involves not using antibodies to ameliorate porcine antibodies that cause rejection in humans, but rather reengineering the genetic composition of pigs to eliminate those antibodies. “According to the wildest of dreams, these genes affecting porcine glycan expression may be silenced, and the human–antiporcine humoral immunity is controlled down to the level comparable with human allograft rejection,” Dr. Mennander said.
However, such a breakthrough carries with it consequences, Dr. Mennander said. “Should one worry about the induction of zoonosis, as well as the ethical aspects of transplanting the patient a whole organ of a pig? Would even a successful xenotransplant program seriously compete with artificial hearts or allografts?” Embracing the method too early would open its advocates to ridicule, he said.
“We are to applaud the researchers for ever-lasting and exemplary enthusiasm for a futuristic new surgical solution; the future may lie as much in current clinical solutions as in innovative discoveries based on persistent scientific experiments,” Dr. Mennander said.
Dr. Mennander had no relevant financial relationships to disclose.
Advances in gene editing are pushing the possibility of raising pigs for organs that may be transplanted into humans with immunosuppression regimens comparable to those now used in human-to-human transplants, coauthors James Butler, MD, and A. Joseph Tector, MD, PhD, stated in an expert opinion in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:488-92).
Developments in genome editing could bring new approaches to management of cardiopulmonary diseases, Dr. Butler and Dr. Tector noted. “Recently, cardiac-specific and lung-specific applications have been described, which will allow for the rapid creation of new models of heart and lung disease,” they said. Specifically, they noted gene targeting might eventually offer a way to treat challenging genetic problems “like the heterogeneous nature of nonsquamous cell lung cancer.”
Dr. Butler is with the department of surgery at Indiana University, Indianapolis, and Dr. Tector is with the department of surgery at the University of Alabama at Birmingham.
CRISPR technology has been used in developing multiple gene knockout pigs and neutralizing three separate porcine genes that encode human xenoantigens in a single reaction, leading to efficient methods for creating pigs with multiple genetic modifications.
According to the website of the Broad Institute of MIT and Harvard, Cambridge, Mass., where researchers perfected the system to work in eukaryotes, CRISPR works by using short RNA sequences designed by researchers to guide the system to matching sequences of DNA. When the target DNA is found, Cas9 – one of the enzymes produced by the CRISPR system – binds to the DNA and cuts it, shutting the targeted gene off.
“By facilitating high-throughput model creation, CRISPR has elucidated which modifications are necessary and which are not; despite the ability to alter many loci concurrently, recent evidence has implicated three porcine genes that are responsible for the majority of human-antiporcine humoral immunity,” Dr. Butler and Dr. Tector wrote.
Those genes are the Gal[alpha]1-3 epitope (Gal-alpha), CMAH and B4GaINT2 genes. “Each of these three genes is expressed in pigs but has been evolutionarily silenced in humans,” the coauthors added.
While CRISPR genome editing has yet to reach its full potential, researchers and clinicians should pay attention, according to Dr. Butler and Dr. Tector.
More recent modifications of CRISPR technology have shown promise in not just knocking out or turning off specific genes, but rather guiding directed replacement of genes with researcher-designed substitutes. This can enable permanent transformation of functional genes with altered behavior, according to the Broad Institute website.
Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler has no relevant financial relationships to disclose.
Advances in gene editing are pushing the possibility of raising pigs for organs that may be transplanted into humans with immunosuppression regimens comparable to those now used in human-to-human transplants, coauthors James Butler, MD, and A. Joseph Tector, MD, PhD, stated in an expert opinion in the February issue of the Journal of Thoracic and Cardiovascular Surgery (2017;153:488-92).
Developments in genome editing could bring new approaches to management of cardiopulmonary diseases, Dr. Butler and Dr. Tector noted. “Recently, cardiac-specific and lung-specific applications have been described, which will allow for the rapid creation of new models of heart and lung disease,” they said. Specifically, they noted gene targeting might eventually offer a way to treat challenging genetic problems “like the heterogeneous nature of nonsquamous cell lung cancer.”
Dr. Butler is with the department of surgery at Indiana University, Indianapolis, and Dr. Tector is with the department of surgery at the University of Alabama at Birmingham.
CRISPR technology has been used in developing multiple gene knockout pigs and neutralizing three separate porcine genes that encode human xenoantigens in a single reaction, leading to efficient methods for creating pigs with multiple genetic modifications.
According to the website of the Broad Institute of MIT and Harvard, Cambridge, Mass., where researchers perfected the system to work in eukaryotes, CRISPR works by using short RNA sequences designed by researchers to guide the system to matching sequences of DNA. When the target DNA is found, Cas9 – one of the enzymes produced by the CRISPR system – binds to the DNA and cuts it, shutting the targeted gene off.
“By facilitating high-throughput model creation, CRISPR has elucidated which modifications are necessary and which are not; despite the ability to alter many loci concurrently, recent evidence has implicated three porcine genes that are responsible for the majority of human-antiporcine humoral immunity,” Dr. Butler and Dr. Tector wrote.
Those genes are the Gal[alpha]1-3 epitope (Gal-alpha), CMAH and B4GaINT2 genes. “Each of these three genes is expressed in pigs but has been evolutionarily silenced in humans,” the coauthors added.
While CRISPR genome editing has yet to reach its full potential, researchers and clinicians should pay attention, according to Dr. Butler and Dr. Tector.
More recent modifications of CRISPR technology have shown promise in not just knocking out or turning off specific genes, but rather guiding directed replacement of genes with researcher-designed substitutes. This can enable permanent transformation of functional genes with altered behavior, according to the Broad Institute website.
Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler has no relevant financial relationships to disclose.
Key clinical point: CRISPR/Cas9 genome editing is advancing the creation of animal models for xenotransplantation into humans.
Major finding: Genome editing tools are moving xenotransplantation models quickly toward potential treatments for cardiopulmonary disease.
Data source: Expert opinion with literature review.
Disclosures: Dr. Tector disclosed he has received funding from United Therapeutics and founded Xenobridge with patents for xenotransplantation. Dr. Butler reported having no relevant financial disclosures.
Use of bilateral internal mammary arteries in CABG stagnates
HOUSTON – Over the past 5 years there has been no growth in bilateral internal mammary artery use among Medicare beneficiaries, and the frequency of bilateral internal mammary artery use during coronary artery bypass grafting remained low, according to a large observational analysis.
“Despite a growing evidence base supporting bilateral internal mammary artery use with regard to long-term survival and freedom from repeat revascularization, rates of bilateral internal mammary artery [BIMA] use remain low, with no evidence of growth,” Alexander Iribarne, MD, said during an interview at the annual meeting of the Society of Thoracic Surgeons. “Therefore, there is significant opportunity for adoption of bilateral internal mammary artery grafting in the United States.”
The most recent report of CABG trends in the United States published from the STS database showed that in 2009, fewer than 5% of patients who underwent CABG received a BIMA (J Thorac Cardiovasc Surg. 2012 Feb;143[2]:273-81). In an effort to characterize the adoption rate and regional variation of BIMA use in the United States, Dr. Iribarne, director of cardiac surgical research in the section of cardiac surgery at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his associates examined records from nearly 150 million Medicare beneficiaries from 2009-2014. “This work is unique in that we not only looked at trends in rates of usage but also how this varied by geographic location,” he said.
“I was surprised to find that despite the growing literature supporting BIMA use, there was no growth in rates of usage over the 5-year study period, with rates remaining low,” Dr. Iribarne said. “I was also surprised to see that there was significant regional variation in use that appeared to correlate, in part, with overall CABG volume, although the moderate correlation coefficient indicates that additional factors beyond CABG volume are involved.”
A key limitation of the study, he said, was that its patients were aged 65 and older. Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
HOUSTON – Over the past 5 years there has been no growth in bilateral internal mammary artery use among Medicare beneficiaries, and the frequency of bilateral internal mammary artery use during coronary artery bypass grafting remained low, according to a large observational analysis.
“Despite a growing evidence base supporting bilateral internal mammary artery use with regard to long-term survival and freedom from repeat revascularization, rates of bilateral internal mammary artery [BIMA] use remain low, with no evidence of growth,” Alexander Iribarne, MD, said during an interview at the annual meeting of the Society of Thoracic Surgeons. “Therefore, there is significant opportunity for adoption of bilateral internal mammary artery grafting in the United States.”
The most recent report of CABG trends in the United States published from the STS database showed that in 2009, fewer than 5% of patients who underwent CABG received a BIMA (J Thorac Cardiovasc Surg. 2012 Feb;143[2]:273-81). In an effort to characterize the adoption rate and regional variation of BIMA use in the United States, Dr. Iribarne, director of cardiac surgical research in the section of cardiac surgery at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his associates examined records from nearly 150 million Medicare beneficiaries from 2009-2014. “This work is unique in that we not only looked at trends in rates of usage but also how this varied by geographic location,” he said.
“I was surprised to find that despite the growing literature supporting BIMA use, there was no growth in rates of usage over the 5-year study period, with rates remaining low,” Dr. Iribarne said. “I was also surprised to see that there was significant regional variation in use that appeared to correlate, in part, with overall CABG volume, although the moderate correlation coefficient indicates that additional factors beyond CABG volume are involved.”
A key limitation of the study, he said, was that its patients were aged 65 and older. Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
HOUSTON – Over the past 5 years there has been no growth in bilateral internal mammary artery use among Medicare beneficiaries, and the frequency of bilateral internal mammary artery use during coronary artery bypass grafting remained low, according to a large observational analysis.
“Despite a growing evidence base supporting bilateral internal mammary artery use with regard to long-term survival and freedom from repeat revascularization, rates of bilateral internal mammary artery [BIMA] use remain low, with no evidence of growth,” Alexander Iribarne, MD, said during an interview at the annual meeting of the Society of Thoracic Surgeons. “Therefore, there is significant opportunity for adoption of bilateral internal mammary artery grafting in the United States.”
The most recent report of CABG trends in the United States published from the STS database showed that in 2009, fewer than 5% of patients who underwent CABG received a BIMA (J Thorac Cardiovasc Surg. 2012 Feb;143[2]:273-81). In an effort to characterize the adoption rate and regional variation of BIMA use in the United States, Dr. Iribarne, director of cardiac surgical research in the section of cardiac surgery at Dartmouth-Hitchcock Medical Center, Lebanon, N.H., and his associates examined records from nearly 150 million Medicare beneficiaries from 2009-2014. “This work is unique in that we not only looked at trends in rates of usage but also how this varied by geographic location,” he said.
“I was surprised to find that despite the growing literature supporting BIMA use, there was no growth in rates of usage over the 5-year study period, with rates remaining low,” Dr. Iribarne said. “I was also surprised to see that there was significant regional variation in use that appeared to correlate, in part, with overall CABG volume, although the moderate correlation coefficient indicates that additional factors beyond CABG volume are involved.”
A key limitation of the study, he said, was that its patients were aged 65 and older. Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
AT THE STS ANNUAL MEETING
Key clinical point:
Major finding: The absolute national rate of BIMA use fell from 0.216 claims per 1,000 beneficiaries in 2009 to 0.143 in 2014 (P less than .001).
Data source: An analysis of medical records from nearly 150 million Medicare beneficiaries during 2009-2014.
Disclosures: Dr. Iribarne disclosed that he receives grant funding from the American Association for Thoracic Surgery Graham Foundation and the Dartmouth SYNERGY Clinical and Translational Science Institute.
Esophageal retractor found handy tool in AF ablation
ORLANDO – A relatively simple mechanical tool to move the esophagus away from the energy delivered during ablation of atrial fibrillation (AF) does what it is supposed to do, according to data from a multicenter observational study presented at the AF Symposium 2017.
When esophageal temperature during the ablation procedure was monitored in 101 consecutive cases, no recording exceeded 38° C, according to Valay Parikh, MD, a clinical cardiac electrophysiology fellow working under Dhanunjaya Lakkireddy, MD, at the Kansas University Medical Center, Kansas City.
The tool is a stylet constructed from a nickel-titanium (nitinol) alloy. Malleable at room temperature, the stylet is inserted into an 18 Fr orogastric (OG) tube. Firmer at body temperature, the stylet within the OG tube is maneuvered to displace the esophagus away from the adjacent left atrium when radiofrequency ablation (RFA) is being administered.
The tool, marketed under the brand name EsoSure, was first made available almost 2 years ago, but the recently completed multicenter observational study was conducted to provide a more systematic evaluation of its safety and efficacy in routine use. In this study, 101 consecutive patients scheduled for RFA for AF had their esophagus displaced by the stylet during the procedure. The temperature of the esophagus as well as any adverse events involving the upper gastrointestinal tract were evaluated during the procedure. Patients were then followed for at least 6 months.
“The principal finding of our study is that mechanical displacement of the esophagus with the help of the EsoSure device is safe and provides sufficient room to deliver the intended energy at the site of ablation without any rise in temperature over 38° C,” Dr. Parikh reported.
The mean age of the 101 patients who participated in this study was 65 years. About half were female. The mean body mass index (BMI) was 32 kg/m2. The mean CHA2DS2-VASc score was 2.4. Barium x-rays were used to confirm esophageal displacement.
After the procedure, patients were discharged on a proton pump inhibitor and sucralfate, which inhibits pepsin activity and protects against ulceration. Follow-up endoscopy was performed only when medically indicated, but all patients were evaluated over the course of follow-up for odynophagia, dysphagia, hematemesis, dyspepsia, and other GI symptoms.
Pulmonary vein isolation (PVI) was achieved successfully in all cases. Although there was a rapid temperature rise at the site of ablation over the course of RFA, the esophagus was adequately displaced from the source of energy, as confirmed with the absence of significant temperature rises in this tissue. The mean esophageal displacement was 2.53 cm.
The only complication in this series, occurring in 7% of patients, was dysphagia. All cases of dysphagia developed immediately or soon after the procedure. All were mild, and all resolved within several days. There were no late GI complications observed, although Dr. Parikh acknowledged that no follow-up endoscopy was performed to rule out any esophageal injury.
In contrast, without the deviation permitted by the esophageal retractor, the rapid rise in temperature “could have precluded PVI,” Dr. Parikh maintained. He said that the retractor permitted the esophagus to be cleared from potential injury, as indicated by the lack of a temperature rise in esophageal tissue, in 100% of the cases. He noted that the tool is now in routine use at his center.
According to Dr. Lakkireddy, this tool is already in routine use at several centers across the country. The goal of this study was to provide an objective documentation of the ability of the device to enable successful posterior wall isolation during PVI without esophageal injury.
“It helped us get to the endpoint without a problem 100% of the time,” Dr. Lakkireddy reported.
Dr. Parikh has no industry relationships relevant to this study.
ORLANDO – A relatively simple mechanical tool to move the esophagus away from the energy delivered during ablation of atrial fibrillation (AF) does what it is supposed to do, according to data from a multicenter observational study presented at the AF Symposium 2017.
When esophageal temperature during the ablation procedure was monitored in 101 consecutive cases, no recording exceeded 38° C, according to Valay Parikh, MD, a clinical cardiac electrophysiology fellow working under Dhanunjaya Lakkireddy, MD, at the Kansas University Medical Center, Kansas City.
The tool is a stylet constructed from a nickel-titanium (nitinol) alloy. Malleable at room temperature, the stylet is inserted into an 18 Fr orogastric (OG) tube. Firmer at body temperature, the stylet within the OG tube is maneuvered to displace the esophagus away from the adjacent left atrium when radiofrequency ablation (RFA) is being administered.
The tool, marketed under the brand name EsoSure, was first made available almost 2 years ago, but the recently completed multicenter observational study was conducted to provide a more systematic evaluation of its safety and efficacy in routine use. In this study, 101 consecutive patients scheduled for RFA for AF had their esophagus displaced by the stylet during the procedure. The temperature of the esophagus as well as any adverse events involving the upper gastrointestinal tract were evaluated during the procedure. Patients were then followed for at least 6 months.
“The principal finding of our study is that mechanical displacement of the esophagus with the help of the EsoSure device is safe and provides sufficient room to deliver the intended energy at the site of ablation without any rise in temperature over 38° C,” Dr. Parikh reported.
The mean age of the 101 patients who participated in this study was 65 years. About half were female. The mean body mass index (BMI) was 32 kg/m2. The mean CHA2DS2-VASc score was 2.4. Barium x-rays were used to confirm esophageal displacement.
After the procedure, patients were discharged on a proton pump inhibitor and sucralfate, which inhibits pepsin activity and protects against ulceration. Follow-up endoscopy was performed only when medically indicated, but all patients were evaluated over the course of follow-up for odynophagia, dysphagia, hematemesis, dyspepsia, and other GI symptoms.
Pulmonary vein isolation (PVI) was achieved successfully in all cases. Although there was a rapid temperature rise at the site of ablation over the course of RFA, the esophagus was adequately displaced from the source of energy, as confirmed with the absence of significant temperature rises in this tissue. The mean esophageal displacement was 2.53 cm.
The only complication in this series, occurring in 7% of patients, was dysphagia. All cases of dysphagia developed immediately or soon after the procedure. All were mild, and all resolved within several days. There were no late GI complications observed, although Dr. Parikh acknowledged that no follow-up endoscopy was performed to rule out any esophageal injury.
In contrast, without the deviation permitted by the esophageal retractor, the rapid rise in temperature “could have precluded PVI,” Dr. Parikh maintained. He said that the retractor permitted the esophagus to be cleared from potential injury, as indicated by the lack of a temperature rise in esophageal tissue, in 100% of the cases. He noted that the tool is now in routine use at his center.
According to Dr. Lakkireddy, this tool is already in routine use at several centers across the country. The goal of this study was to provide an objective documentation of the ability of the device to enable successful posterior wall isolation during PVI without esophageal injury.
“It helped us get to the endpoint without a problem 100% of the time,” Dr. Lakkireddy reported.
Dr. Parikh has no industry relationships relevant to this study.
ORLANDO – A relatively simple mechanical tool to move the esophagus away from the energy delivered during ablation of atrial fibrillation (AF) does what it is supposed to do, according to data from a multicenter observational study presented at the AF Symposium 2017.
When esophageal temperature during the ablation procedure was monitored in 101 consecutive cases, no recording exceeded 38° C, according to Valay Parikh, MD, a clinical cardiac electrophysiology fellow working under Dhanunjaya Lakkireddy, MD, at the Kansas University Medical Center, Kansas City.
The tool is a stylet constructed from a nickel-titanium (nitinol) alloy. Malleable at room temperature, the stylet is inserted into an 18 Fr orogastric (OG) tube. Firmer at body temperature, the stylet within the OG tube is maneuvered to displace the esophagus away from the adjacent left atrium when radiofrequency ablation (RFA) is being administered.
The tool, marketed under the brand name EsoSure, was first made available almost 2 years ago, but the recently completed multicenter observational study was conducted to provide a more systematic evaluation of its safety and efficacy in routine use. In this study, 101 consecutive patients scheduled for RFA for AF had their esophagus displaced by the stylet during the procedure. The temperature of the esophagus as well as any adverse events involving the upper gastrointestinal tract were evaluated during the procedure. Patients were then followed for at least 6 months.
“The principal finding of our study is that mechanical displacement of the esophagus with the help of the EsoSure device is safe and provides sufficient room to deliver the intended energy at the site of ablation without any rise in temperature over 38° C,” Dr. Parikh reported.
The mean age of the 101 patients who participated in this study was 65 years. About half were female. The mean body mass index (BMI) was 32 kg/m2. The mean CHA2DS2-VASc score was 2.4. Barium x-rays were used to confirm esophageal displacement.
After the procedure, patients were discharged on a proton pump inhibitor and sucralfate, which inhibits pepsin activity and protects against ulceration. Follow-up endoscopy was performed only when medically indicated, but all patients were evaluated over the course of follow-up for odynophagia, dysphagia, hematemesis, dyspepsia, and other GI symptoms.
Pulmonary vein isolation (PVI) was achieved successfully in all cases. Although there was a rapid temperature rise at the site of ablation over the course of RFA, the esophagus was adequately displaced from the source of energy, as confirmed with the absence of significant temperature rises in this tissue. The mean esophageal displacement was 2.53 cm.
The only complication in this series, occurring in 7% of patients, was dysphagia. All cases of dysphagia developed immediately or soon after the procedure. All were mild, and all resolved within several days. There were no late GI complications observed, although Dr. Parikh acknowledged that no follow-up endoscopy was performed to rule out any esophageal injury.
In contrast, without the deviation permitted by the esophageal retractor, the rapid rise in temperature “could have precluded PVI,” Dr. Parikh maintained. He said that the retractor permitted the esophagus to be cleared from potential injury, as indicated by the lack of a temperature rise in esophageal tissue, in 100% of the cases. He noted that the tool is now in routine use at his center.
According to Dr. Lakkireddy, this tool is already in routine use at several centers across the country. The goal of this study was to provide an objective documentation of the ability of the device to enable successful posterior wall isolation during PVI without esophageal injury.
“It helped us get to the endpoint without a problem 100% of the time,” Dr. Lakkireddy reported.
Dr. Parikh has no industry relationships relevant to this study.
AT THE INTERNATIONAL AF SYMPOSIUM
Key clinical point: The efficacy of a tool to move the esophagus out of the way when performing ablation for atrial fibrillation is supported by a multicenter study.
Major finding: In 101 consecutive cases at four centers, all ablations were completed successfully with no esophageal temperature rise.
Data source: Prospective observational study.
Disclosures: Dr. Parikh has no industry relationships relevant to this study.
Moderate stenosis in coronary arteries grows severe over time
HOUSTON – Most nongrafted, moderately stenosed coronary arteries progress to severe stenosis or occlusion in the long term, results from a large, long-term study have shown.
“Not uncommonly, patients referred for coronary surgery have one or more coronary arteries with only moderate stenosis,” Joseph F. Sabik III, MD, said at the annual meeting of the Society of Thoracic Surgeons.
“There is controversy as to whether arteries with only moderate stenosis should be grafted during coronary surgery, and if it should be grafted, with what conduit?” For example, the Fractional Flow Reserve-Guided PCI versus Medical Therapy in Stable Coronary Disease study, known as FAME, suggests not intervening on moderate stenosis, since stenting non–ischemia-producing lesions led to worse outcomes (N Engl J Med. 2012 Sep 13;367:991-1001). However, Dr. Sabik, who chairs the department of surgery at University Hospitals Cleveland Medical Center, and his associates recently reported that grafting moderately stenosed coronary arteries during surgical revascularization is not harmful and can be beneficial by improving survival if an internal thoracic artery graft is used (J. Thoracic Cardiovasc Surg. 2016 Mar;151[3]:806-11).
In an effort to determine how grafting moderately stenosed coronary arteries influences native-vessel disease progression, and whether grafting may be protective from late ischemia, Dr. Sabik and his associates evaluated the medical records of 55,567 patients who underwent primary isolated coronary artery bypass graft (CABG) surgery at the Cleveland Clinic from 1972 to 2011. Of the 55,567 patients, 1,902 had a single coronary artery with angiographically moderate stenosis (defined as a narrowing of 50%-69%) and results of at least one postoperative angiogram available. Of these moderately stenosed coronary arteries (MSCAs), 488 were not grafted, 385 were internal thoracic artery (ITA)–grafted, and 1,028 were saphenous vein (SV)–grafted. At follow-up angiograms, information about disease progression was available for 488 nongrafted, 371 ITA-grafted, and 957 SV-grafted MSCAs, and patency information was available for 376 ITA and 1,016 SV grafts to these MSCAs. Grafts were considered patent if they were not occluded. Severe occlusion was defined as a narrowing of more than 70%.
The researchers found that at 1, 5, 10, and 15 years, native-vessel disease progressed from moderate to severe stenosis/occlusion in 32%, 52%, 66%, and 72% of nongrafted MSCAs, respectively; in 55%, 73%, 84%, and 87% of ITA-grafted MSCAs, and in 67%, 82%, 90%, and 92% of SV-grafted MSCAs. After Dr. Sabik and his associates adjusted for patient characteristics, disease progression in MSCAs was significantly higher with ITA and SV grafting, compared with nongrafting (odds ratios, 3.6 and 9.9, respectively). At 1, 5, 10, and 15 years, occlusion in grafts to MSCAs was 8%, 9%, 11%, and 15%, respectively, for ITA grafts and 13%, 32%, 46%, and 56% for SV grafts. At these same time points, protection from myocardial ischemia in ITA-grafted vs. nongrafted MSCAs was 29%, 47%, 59%, and 61%.
“Our opinion is you that shouldn’t ignore moderate lesions,” Dr. Sabik, surgeon-in-chief and vice president for surgical operations for the University Hospitals system, said in an interview at the meeting. “Although it may not help that patient over the next short period of time, over their lifespan it will. What works for intervention doesn’t necessarily mean it’s right for bypass surgery. If you have a vessel that’s only moderately stenosed you should at least consider grafting it, because moderate lesions progress over time. Bypassing it helps people live longer when you use an internal thoracic artery graft, because they are likely to remain patent. You always have to individualize the therapy, but the key is to use your grafts in the best way possible.”
Dr. Sabik disclosed that he has received research grants from Medtronic, Abbott Vascular, and Edwards Lifesciences.
HOUSTON – Most nongrafted, moderately stenosed coronary arteries progress to severe stenosis or occlusion in the long term, results from a large, long-term study have shown.
“Not uncommonly, patients referred for coronary surgery have one or more coronary arteries with only moderate stenosis,” Joseph F. Sabik III, MD, said at the annual meeting of the Society of Thoracic Surgeons.
“There is controversy as to whether arteries with only moderate stenosis should be grafted during coronary surgery, and if it should be grafted, with what conduit?” For example, the Fractional Flow Reserve-Guided PCI versus Medical Therapy in Stable Coronary Disease study, known as FAME, suggests not intervening on moderate stenosis, since stenting non–ischemia-producing lesions led to worse outcomes (N Engl J Med. 2012 Sep 13;367:991-1001). However, Dr. Sabik, who chairs the department of surgery at University Hospitals Cleveland Medical Center, and his associates recently reported that grafting moderately stenosed coronary arteries during surgical revascularization is not harmful and can be beneficial by improving survival if an internal thoracic artery graft is used (J. Thoracic Cardiovasc Surg. 2016 Mar;151[3]:806-11).
In an effort to determine how grafting moderately stenosed coronary arteries influences native-vessel disease progression, and whether grafting may be protective from late ischemia, Dr. Sabik and his associates evaluated the medical records of 55,567 patients who underwent primary isolated coronary artery bypass graft (CABG) surgery at the Cleveland Clinic from 1972 to 2011. Of the 55,567 patients, 1,902 had a single coronary artery with angiographically moderate stenosis (defined as a narrowing of 50%-69%) and results of at least one postoperative angiogram available. Of these moderately stenosed coronary arteries (MSCAs), 488 were not grafted, 385 were internal thoracic artery (ITA)–grafted, and 1,028 were saphenous vein (SV)–grafted. At follow-up angiograms, information about disease progression was available for 488 nongrafted, 371 ITA-grafted, and 957 SV-grafted MSCAs, and patency information was available for 376 ITA and 1,016 SV grafts to these MSCAs. Grafts were considered patent if they were not occluded. Severe occlusion was defined as a narrowing of more than 70%.
The researchers found that at 1, 5, 10, and 15 years, native-vessel disease progressed from moderate to severe stenosis/occlusion in 32%, 52%, 66%, and 72% of nongrafted MSCAs, respectively; in 55%, 73%, 84%, and 87% of ITA-grafted MSCAs, and in 67%, 82%, 90%, and 92% of SV-grafted MSCAs. After Dr. Sabik and his associates adjusted for patient characteristics, disease progression in MSCAs was significantly higher with ITA and SV grafting, compared with nongrafting (odds ratios, 3.6 and 9.9, respectively). At 1, 5, 10, and 15 years, occlusion in grafts to MSCAs was 8%, 9%, 11%, and 15%, respectively, for ITA grafts and 13%, 32%, 46%, and 56% for SV grafts. At these same time points, protection from myocardial ischemia in ITA-grafted vs. nongrafted MSCAs was 29%, 47%, 59%, and 61%.
“Our opinion is you that shouldn’t ignore moderate lesions,” Dr. Sabik, surgeon-in-chief and vice president for surgical operations for the University Hospitals system, said in an interview at the meeting. “Although it may not help that patient over the next short period of time, over their lifespan it will. What works for intervention doesn’t necessarily mean it’s right for bypass surgery. If you have a vessel that’s only moderately stenosed you should at least consider grafting it, because moderate lesions progress over time. Bypassing it helps people live longer when you use an internal thoracic artery graft, because they are likely to remain patent. You always have to individualize the therapy, but the key is to use your grafts in the best way possible.”
Dr. Sabik disclosed that he has received research grants from Medtronic, Abbott Vascular, and Edwards Lifesciences.
HOUSTON – Most nongrafted, moderately stenosed coronary arteries progress to severe stenosis or occlusion in the long term, results from a large, long-term study have shown.
“Not uncommonly, patients referred for coronary surgery have one or more coronary arteries with only moderate stenosis,” Joseph F. Sabik III, MD, said at the annual meeting of the Society of Thoracic Surgeons.
“There is controversy as to whether arteries with only moderate stenosis should be grafted during coronary surgery, and if it should be grafted, with what conduit?” For example, the Fractional Flow Reserve-Guided PCI versus Medical Therapy in Stable Coronary Disease study, known as FAME, suggests not intervening on moderate stenosis, since stenting non–ischemia-producing lesions led to worse outcomes (N Engl J Med. 2012 Sep 13;367:991-1001). However, Dr. Sabik, who chairs the department of surgery at University Hospitals Cleveland Medical Center, and his associates recently reported that grafting moderately stenosed coronary arteries during surgical revascularization is not harmful and can be beneficial by improving survival if an internal thoracic artery graft is used (J. Thoracic Cardiovasc Surg. 2016 Mar;151[3]:806-11).
In an effort to determine how grafting moderately stenosed coronary arteries influences native-vessel disease progression, and whether grafting may be protective from late ischemia, Dr. Sabik and his associates evaluated the medical records of 55,567 patients who underwent primary isolated coronary artery bypass graft (CABG) surgery at the Cleveland Clinic from 1972 to 2011. Of the 55,567 patients, 1,902 had a single coronary artery with angiographically moderate stenosis (defined as a narrowing of 50%-69%) and results of at least one postoperative angiogram available. Of these moderately stenosed coronary arteries (MSCAs), 488 were not grafted, 385 were internal thoracic artery (ITA)–grafted, and 1,028 were saphenous vein (SV)–grafted. At follow-up angiograms, information about disease progression was available for 488 nongrafted, 371 ITA-grafted, and 957 SV-grafted MSCAs, and patency information was available for 376 ITA and 1,016 SV grafts to these MSCAs. Grafts were considered patent if they were not occluded. Severe occlusion was defined as a narrowing of more than 70%.
The researchers found that at 1, 5, 10, and 15 years, native-vessel disease progressed from moderate to severe stenosis/occlusion in 32%, 52%, 66%, and 72% of nongrafted MSCAs, respectively; in 55%, 73%, 84%, and 87% of ITA-grafted MSCAs, and in 67%, 82%, 90%, and 92% of SV-grafted MSCAs. After Dr. Sabik and his associates adjusted for patient characteristics, disease progression in MSCAs was significantly higher with ITA and SV grafting, compared with nongrafting (odds ratios, 3.6 and 9.9, respectively). At 1, 5, 10, and 15 years, occlusion in grafts to MSCAs was 8%, 9%, 11%, and 15%, respectively, for ITA grafts and 13%, 32%, 46%, and 56% for SV grafts. At these same time points, protection from myocardial ischemia in ITA-grafted vs. nongrafted MSCAs was 29%, 47%, 59%, and 61%.
“Our opinion is you that shouldn’t ignore moderate lesions,” Dr. Sabik, surgeon-in-chief and vice president for surgical operations for the University Hospitals system, said in an interview at the meeting. “Although it may not help that patient over the next short period of time, over their lifespan it will. What works for intervention doesn’t necessarily mean it’s right for bypass surgery. If you have a vessel that’s only moderately stenosed you should at least consider grafting it, because moderate lesions progress over time. Bypassing it helps people live longer when you use an internal thoracic artery graft, because they are likely to remain patent. You always have to individualize the therapy, but the key is to use your grafts in the best way possible.”
Dr. Sabik disclosed that he has received research grants from Medtronic, Abbott Vascular, and Edwards Lifesciences.
AT THE STS ANNUAL MEETING
Key clinical point:
Major finding: At 15 years, native-vessel disease progressed from moderate to severe stenosis/occlusion in 72% of nongrafted coronary arteries, in 87% of internal thoracic artery–grafted arteries, and in 92% of saphenous vein–grafted moderately stenosed coronary arteries.
Data source: An analysis of medical records from 55,567 patients who underwent primary isolated CABG at the Cleveland Clinic from 1972 to 2011.
Disclosures: Dr. Sabik disclosed that he has received research grants from Medtronic, Abbott Vascular, and Edwards Lifesciences.
Trials refine device therapy options for heart failure
SNOWMASS, COLO. – The indication for primary prophylactic implantable cardioverter-defibrillator therapy in patients with nonischemic heart failure is likely to be downgraded in the next iteration of the ACC/AHA heart failure guidelines as a consequence of the negative results of the DANISH trial, William T. Abraham, MD, predicted at the Annual Cardiovascular Conference at Snowmass.
In addition to outlining where the guideline recommendations for implantable cardioverter-defibrillator (ICD) therapy stand today, and how they’re likely to change in response to the DANISH findings, he highlighted the latest patient selection criteria for cardiac resynchronization therapy (CRT), which have grown considerably more complicated over time.
“Following the success of neurohormonal inhibitors and antagonists, our only other breakthroughs for the management of heart failure have been CRT and ICDs,” he noted.
The two device therapies are complementary, and indeed are often employed in combination.
“CRT makes patients feel better and saves lives, while ICDs prolong survival without an effect on improving heart failure per se,” the cardiologist explained.
To put the quality of life benefits of CRT into perspective, studies show that the device therapy results in a placebo-subtracted improvement on the Minnesota Living With Heart Failure Questionnaire of 9-10 points.
“This is a large and clinically meaningful improvement in quality of life. Our best drugs for heart failure – beta blockers and ACE inhibitors – improve this same measure by 4 or 5 points,” Dr. Abraham said.
Current American College of Cardiology/American Heart Association heart failure guidelines give a class I, level of evidence: A, recommendation for prophylactic ICD therapy in patients with an left ventricular ejection fraction (LVEF) of 35% or less and New York Heart Association functional class II or III symptoms despite optimal medical therapy, regardless of whether their heart failure is attributable to ischemic heart disease or nonischemic dilated cardiomyopathy.
The DANISH trial investigators looked at the evidence base for primary prevention ICDs in nonischemic heart failure and concluded it needed shoring up. The recommendation relied mainly on subgroup analyses of larger landmark trials done about 15 years ago, before major improvements in medical therapy had occurred. These reservations were the impetus for the DANISH trial, in which more than 1,100 patients with symptomatic systolic heart failure were randomized to an ICD or usual care.
The primary outcome in the DANISH trial – all-cause mortality – occurred in 21.6% of patients in the ICD group and 23.4% of controls during a median follow-up of 68 months, a nonsignificant difference (N Engl J Med. 2016 Sep 29;375[13]:1221-30).
Turning to the CRT guidelines, Dr. Abraham noted that the simple, broad, class I recommendation for this form of device therapy in patients with cardiac dyssynchrony as defined by a QRS duration greater than 120 msec contained in the 2005 ACC/AHA heart failure guidelines has been whittled down over time as new evidence has unfolded. The only class I recommendation in the current guidelines is in patients with an LVEF of 35% or less, sinus rhythm, left bundle branch block with a QRS duration of 150 msec or longer, and NYHA class II, III, or ambulatory IV symptoms while on guideline-directed medical therapy (Circulation. 2012 Oct 1;126:1784-800). “That’s the money group right there. That’s the group for whom we have the greatest confidence of producing the greatest benefit with the application of cardiac resynchronization therapy,” he explained.
Studies examining the use of CRT in heart failure patients with a non–left bundle branch morphology and a QRS duration of less than 150 msec have yielded negative findings. So have attempts to utilize echocardiographic evidence of mechanical dyssynchrony rather than ECG measurement of QRS duration to guide patient selection for CRT.
“In our practice, any patient with a left bundle branch block gets a CRT device. Our confidence in its efficacy is greater in patients with a QRS of at least 150 msec, but the studies demonstrate clear benefit for patients with left bundle branch block and a QRS of 120-149 msec as well,” according to the cardiologist.
Studies also show that patients who are dependent upon ventricular pacing benefit from CRT.
“If you have a patient who requires at least 40% or more ventricular pacing and also has reduced ejection fraction heart failure, that patient should have a CRT device rather than a dual chamber ICD or standard right-sided right ventricular pacemaker,” he said.
All of this presupposes that first and foremost the patient is already on optimized guideline-directed medical therapy.
“With optimal medical therapy, some of these patients may improve their left ventricular ejection fraction above 35%, or they may become asymptomatic and no longer have an indication for CRT,” Dr. Abraham added.
The rationale for utilizing CRT in combination with an ICD is a bit shaky, resting on a single older landmark study, the COMPANION trial (N Engl J Med. 2004; 350:2140-50).
“That study wasn’t powered to answer the question of whether CRT-D [a combined CRT/ICD device] is better than CRT. Really, this remains somewhat of an unanswered question. So where are we today? Essentially, if a patient has an indication for CRT and an indication for an ICD, we implant a combined device,” he said.
Dr. Abraham reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – The indication for primary prophylactic implantable cardioverter-defibrillator therapy in patients with nonischemic heart failure is likely to be downgraded in the next iteration of the ACC/AHA heart failure guidelines as a consequence of the negative results of the DANISH trial, William T. Abraham, MD, predicted at the Annual Cardiovascular Conference at Snowmass.
In addition to outlining where the guideline recommendations for implantable cardioverter-defibrillator (ICD) therapy stand today, and how they’re likely to change in response to the DANISH findings, he highlighted the latest patient selection criteria for cardiac resynchronization therapy (CRT), which have grown considerably more complicated over time.
“Following the success of neurohormonal inhibitors and antagonists, our only other breakthroughs for the management of heart failure have been CRT and ICDs,” he noted.
The two device therapies are complementary, and indeed are often employed in combination.
“CRT makes patients feel better and saves lives, while ICDs prolong survival without an effect on improving heart failure per se,” the cardiologist explained.
To put the quality of life benefits of CRT into perspective, studies show that the device therapy results in a placebo-subtracted improvement on the Minnesota Living With Heart Failure Questionnaire of 9-10 points.
“This is a large and clinically meaningful improvement in quality of life. Our best drugs for heart failure – beta blockers and ACE inhibitors – improve this same measure by 4 or 5 points,” Dr. Abraham said.
Current American College of Cardiology/American Heart Association heart failure guidelines give a class I, level of evidence: A, recommendation for prophylactic ICD therapy in patients with an left ventricular ejection fraction (LVEF) of 35% or less and New York Heart Association functional class II or III symptoms despite optimal medical therapy, regardless of whether their heart failure is attributable to ischemic heart disease or nonischemic dilated cardiomyopathy.
The DANISH trial investigators looked at the evidence base for primary prevention ICDs in nonischemic heart failure and concluded it needed shoring up. The recommendation relied mainly on subgroup analyses of larger landmark trials done about 15 years ago, before major improvements in medical therapy had occurred. These reservations were the impetus for the DANISH trial, in which more than 1,100 patients with symptomatic systolic heart failure were randomized to an ICD or usual care.
The primary outcome in the DANISH trial – all-cause mortality – occurred in 21.6% of patients in the ICD group and 23.4% of controls during a median follow-up of 68 months, a nonsignificant difference (N Engl J Med. 2016 Sep 29;375[13]:1221-30).
Turning to the CRT guidelines, Dr. Abraham noted that the simple, broad, class I recommendation for this form of device therapy in patients with cardiac dyssynchrony as defined by a QRS duration greater than 120 msec contained in the 2005 ACC/AHA heart failure guidelines has been whittled down over time as new evidence has unfolded. The only class I recommendation in the current guidelines is in patients with an LVEF of 35% or less, sinus rhythm, left bundle branch block with a QRS duration of 150 msec or longer, and NYHA class II, III, or ambulatory IV symptoms while on guideline-directed medical therapy (Circulation. 2012 Oct 1;126:1784-800). “That’s the money group right there. That’s the group for whom we have the greatest confidence of producing the greatest benefit with the application of cardiac resynchronization therapy,” he explained.
Studies examining the use of CRT in heart failure patients with a non–left bundle branch morphology and a QRS duration of less than 150 msec have yielded negative findings. So have attempts to utilize echocardiographic evidence of mechanical dyssynchrony rather than ECG measurement of QRS duration to guide patient selection for CRT.
“In our practice, any patient with a left bundle branch block gets a CRT device. Our confidence in its efficacy is greater in patients with a QRS of at least 150 msec, but the studies demonstrate clear benefit for patients with left bundle branch block and a QRS of 120-149 msec as well,” according to the cardiologist.
Studies also show that patients who are dependent upon ventricular pacing benefit from CRT.
“If you have a patient who requires at least 40% or more ventricular pacing and also has reduced ejection fraction heart failure, that patient should have a CRT device rather than a dual chamber ICD or standard right-sided right ventricular pacemaker,” he said.
All of this presupposes that first and foremost the patient is already on optimized guideline-directed medical therapy.
“With optimal medical therapy, some of these patients may improve their left ventricular ejection fraction above 35%, or they may become asymptomatic and no longer have an indication for CRT,” Dr. Abraham added.
The rationale for utilizing CRT in combination with an ICD is a bit shaky, resting on a single older landmark study, the COMPANION trial (N Engl J Med. 2004; 350:2140-50).
“That study wasn’t powered to answer the question of whether CRT-D [a combined CRT/ICD device] is better than CRT. Really, this remains somewhat of an unanswered question. So where are we today? Essentially, if a patient has an indication for CRT and an indication for an ICD, we implant a combined device,” he said.
Dr. Abraham reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
SNOWMASS, COLO. – The indication for primary prophylactic implantable cardioverter-defibrillator therapy in patients with nonischemic heart failure is likely to be downgraded in the next iteration of the ACC/AHA heart failure guidelines as a consequence of the negative results of the DANISH trial, William T. Abraham, MD, predicted at the Annual Cardiovascular Conference at Snowmass.
In addition to outlining where the guideline recommendations for implantable cardioverter-defibrillator (ICD) therapy stand today, and how they’re likely to change in response to the DANISH findings, he highlighted the latest patient selection criteria for cardiac resynchronization therapy (CRT), which have grown considerably more complicated over time.
“Following the success of neurohormonal inhibitors and antagonists, our only other breakthroughs for the management of heart failure have been CRT and ICDs,” he noted.
The two device therapies are complementary, and indeed are often employed in combination.
“CRT makes patients feel better and saves lives, while ICDs prolong survival without an effect on improving heart failure per se,” the cardiologist explained.
To put the quality of life benefits of CRT into perspective, studies show that the device therapy results in a placebo-subtracted improvement on the Minnesota Living With Heart Failure Questionnaire of 9-10 points.
“This is a large and clinically meaningful improvement in quality of life. Our best drugs for heart failure – beta blockers and ACE inhibitors – improve this same measure by 4 or 5 points,” Dr. Abraham said.
Current American College of Cardiology/American Heart Association heart failure guidelines give a class I, level of evidence: A, recommendation for prophylactic ICD therapy in patients with an left ventricular ejection fraction (LVEF) of 35% or less and New York Heart Association functional class II or III symptoms despite optimal medical therapy, regardless of whether their heart failure is attributable to ischemic heart disease or nonischemic dilated cardiomyopathy.
The DANISH trial investigators looked at the evidence base for primary prevention ICDs in nonischemic heart failure and concluded it needed shoring up. The recommendation relied mainly on subgroup analyses of larger landmark trials done about 15 years ago, before major improvements in medical therapy had occurred. These reservations were the impetus for the DANISH trial, in which more than 1,100 patients with symptomatic systolic heart failure were randomized to an ICD or usual care.
The primary outcome in the DANISH trial – all-cause mortality – occurred in 21.6% of patients in the ICD group and 23.4% of controls during a median follow-up of 68 months, a nonsignificant difference (N Engl J Med. 2016 Sep 29;375[13]:1221-30).
Turning to the CRT guidelines, Dr. Abraham noted that the simple, broad, class I recommendation for this form of device therapy in patients with cardiac dyssynchrony as defined by a QRS duration greater than 120 msec contained in the 2005 ACC/AHA heart failure guidelines has been whittled down over time as new evidence has unfolded. The only class I recommendation in the current guidelines is in patients with an LVEF of 35% or less, sinus rhythm, left bundle branch block with a QRS duration of 150 msec or longer, and NYHA class II, III, or ambulatory IV symptoms while on guideline-directed medical therapy (Circulation. 2012 Oct 1;126:1784-800). “That’s the money group right there. That’s the group for whom we have the greatest confidence of producing the greatest benefit with the application of cardiac resynchronization therapy,” he explained.
Studies examining the use of CRT in heart failure patients with a non–left bundle branch morphology and a QRS duration of less than 150 msec have yielded negative findings. So have attempts to utilize echocardiographic evidence of mechanical dyssynchrony rather than ECG measurement of QRS duration to guide patient selection for CRT.
“In our practice, any patient with a left bundle branch block gets a CRT device. Our confidence in its efficacy is greater in patients with a QRS of at least 150 msec, but the studies demonstrate clear benefit for patients with left bundle branch block and a QRS of 120-149 msec as well,” according to the cardiologist.
Studies also show that patients who are dependent upon ventricular pacing benefit from CRT.
“If you have a patient who requires at least 40% or more ventricular pacing and also has reduced ejection fraction heart failure, that patient should have a CRT device rather than a dual chamber ICD or standard right-sided right ventricular pacemaker,” he said.
All of this presupposes that first and foremost the patient is already on optimized guideline-directed medical therapy.
“With optimal medical therapy, some of these patients may improve their left ventricular ejection fraction above 35%, or they may become asymptomatic and no longer have an indication for CRT,” Dr. Abraham added.
The rationale for utilizing CRT in combination with an ICD is a bit shaky, resting on a single older landmark study, the COMPANION trial (N Engl J Med. 2004; 350:2140-50).
“That study wasn’t powered to answer the question of whether CRT-D [a combined CRT/ICD device] is better than CRT. Really, this remains somewhat of an unanswered question. So where are we today? Essentially, if a patient has an indication for CRT and an indication for an ICD, we implant a combined device,” he said.
Dr. Abraham reported serving as a consultant to Abbott Vascular, Medtronic, Novartis, and St. Jude Medical.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Heart disease risk soars in young adults with coronary calcium
Younger adults who have any calcium deposited in their coronary arteries, even a small amount, are at increased risk for adverse coronary heart disease (CHD) outcomes and death, finds an analysis of the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
There’s no evidence, however, that treating such patients would make a difference in outcomes, John Jeffrey Carr, MD, reported in JAMA Cardiology on Feb. 8.
In the prospective, community-based, cohort study, 5,115 black and white adults underwent coronary computed tomographic (CT) imaging between the ages of 32 and 46 years, and had a mean follow-up of 12.5 years.
Compared with counterparts not having any coronary artery calcium (CAC), those having at least some had a 5.0-fold increased risk of CHD events and a 1.6-fold increased risk of death (JAMA Cardiol. 2017 Feb 8; doi: 10.1001/jamacardio.2016.5493).
Estimates suggested that identification of individuals at elevated risk for developing CAC could inform a selective CT screening strategy whereby the number of younger adults screened could be reduced by half, and the number needing to be imaged to find one person with CAC could be reduced from 3.5 to 2.2.
“The finding that CAC present by ages 32-46 years is associated with increased risk of premature CHD and death emphasizes the need for reduction of risk factors and primordial prevention beginning in early life,” wrote Dr. Carr, professor radiology at Vanderbilt University in Nashville, Tenn.
“Whether any kind of general screening for CAC is warranted needs further study, although we suggest that a strategy in which all individuals aged 32 to 46 years are screened is not indicated. Rather, a more targeted approach based on measuring risk factors in early adult life to predict individuals at high risk for developing CAC in whom the CT scan would have the greatest value can be considered,” they propose.
Study details
Participants were recruited to CARDIA when aged 18-30 years, and they underwent CAC measurement at 15, 20, and 25 years after recruitment. Incident events were ascertained starting from the time of the year-15 scan.
At that year-15 scan, 10.2% of participants were found to have CAC. The geometric mean Agatston score was 21.6.
In adjusted analyses, participants with any CAC had sharply higher risks of CHD events (hazard ratio, 5.0), as well as cardiovascular disease events (HR, 3.0). The risk of CHD events increased with CAC score, with hazard ratios of 2.6, 5.8, and 9.8 for individuals with scores of 1-19, 20-99, and 100 or more, respectively.
In addition, participants with any CAC had an elevated adjusted risk of all-cause mortality (HR, 1.6). This risk similarly rose with score but was significant for those having a score of 100 or greater only (hazard ratio, 3.7); the large majority of deaths in this group were deemed to be from CHD events.
The model that the investigators developed predicted the probability of CAC by ages 32-56 years based on risk factors assessed 7 years apart, between the ages of 18 and 38 years.
When stratified by this model, 4.2% of study participants falling into the lowest-risk decile had CAC, compared with 67.8% of those falling into the highest-risk decile.
Analyses suggested that if screening were restricted to those participants having an above-median risk score, fully 77.3% of all those with coronary calcium and 95.5% of all those with CHD events would be identified. Moreover, these yields would be obtained while reducing the number of individuals recommended to be screened by 50.0%.
Several challenges will need to be addressed before computed tomographic (CT) screening of younger adults for coronary artery calcium is ready for prime time.
First, such screenings must be efficient, and the investigator’s new model seems to be a step in this direction.
The model should be further validated in other populations as well as across younger populations (i.e., during the first CAC test, when the age of the cohort was aged 32-46 years) to help substantiate whether testing of younger individuals is efficient or if waiting to screen those who are older than 40-45 years may be preferable.
Second, even if coronary calcium is detected in young adults, individuals’ risk may not be sufficiently elevated to justify long-term statin therapy.
Finally, there are no data in this context to show that intervening with statins improves cardiovascular outcomes. The absence of such data, and consequently the fact that treatment is often not started until later in life, is owing to the economic and ethical considerations of performing a trial that would take decades to conduct.
In the meantime, the study’s findings have implications for care in younger adults who are found to have coronary calcium incidentally and underscore the importance of primordial prevention.
Future studies will be needed to refine our approaches to better select appropriate candidates for CAC testing, even more so in younger than in older individuals.
Ron Blankstein, MD, of Harvard University, Boston, and Philip Greenland, MD, of Northwestern University, Chicago, made these comments in an accompanying editorial (JAMA Cardiol. 2017 Feb 8; doi: 10.1001/jamacardio.2016.5552). They reported having no relevant financial disclosures.
Several challenges will need to be addressed before computed tomographic (CT) screening of younger adults for coronary artery calcium is ready for prime time.
First, such screenings must be efficient, and the investigator’s new model seems to be a step in this direction.
The model should be further validated in other populations as well as across younger populations (i.e., during the first CAC test, when the age of the cohort was aged 32-46 years) to help substantiate whether testing of younger individuals is efficient or if waiting to screen those who are older than 40-45 years may be preferable.
Second, even if coronary calcium is detected in young adults, individuals’ risk may not be sufficiently elevated to justify long-term statin therapy.
Finally, there are no data in this context to show that intervening with statins improves cardiovascular outcomes. The absence of such data, and consequently the fact that treatment is often not started until later in life, is owing to the economic and ethical considerations of performing a trial that would take decades to conduct.
In the meantime, the study’s findings have implications for care in younger adults who are found to have coronary calcium incidentally and underscore the importance of primordial prevention.
Future studies will be needed to refine our approaches to better select appropriate candidates for CAC testing, even more so in younger than in older individuals.
Ron Blankstein, MD, of Harvard University, Boston, and Philip Greenland, MD, of Northwestern University, Chicago, made these comments in an accompanying editorial (JAMA Cardiol. 2017 Feb 8; doi: 10.1001/jamacardio.2016.5552). They reported having no relevant financial disclosures.
Several challenges will need to be addressed before computed tomographic (CT) screening of younger adults for coronary artery calcium is ready for prime time.
First, such screenings must be efficient, and the investigator’s new model seems to be a step in this direction.
The model should be further validated in other populations as well as across younger populations (i.e., during the first CAC test, when the age of the cohort was aged 32-46 years) to help substantiate whether testing of younger individuals is efficient or if waiting to screen those who are older than 40-45 years may be preferable.
Second, even if coronary calcium is detected in young adults, individuals’ risk may not be sufficiently elevated to justify long-term statin therapy.
Finally, there are no data in this context to show that intervening with statins improves cardiovascular outcomes. The absence of such data, and consequently the fact that treatment is often not started until later in life, is owing to the economic and ethical considerations of performing a trial that would take decades to conduct.
In the meantime, the study’s findings have implications for care in younger adults who are found to have coronary calcium incidentally and underscore the importance of primordial prevention.
Future studies will be needed to refine our approaches to better select appropriate candidates for CAC testing, even more so in younger than in older individuals.
Ron Blankstein, MD, of Harvard University, Boston, and Philip Greenland, MD, of Northwestern University, Chicago, made these comments in an accompanying editorial (JAMA Cardiol. 2017 Feb 8; doi: 10.1001/jamacardio.2016.5552). They reported having no relevant financial disclosures.
Younger adults who have any calcium deposited in their coronary arteries, even a small amount, are at increased risk for adverse coronary heart disease (CHD) outcomes and death, finds an analysis of the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
There’s no evidence, however, that treating such patients would make a difference in outcomes, John Jeffrey Carr, MD, reported in JAMA Cardiology on Feb. 8.
In the prospective, community-based, cohort study, 5,115 black and white adults underwent coronary computed tomographic (CT) imaging between the ages of 32 and 46 years, and had a mean follow-up of 12.5 years.
Compared with counterparts not having any coronary artery calcium (CAC), those having at least some had a 5.0-fold increased risk of CHD events and a 1.6-fold increased risk of death (JAMA Cardiol. 2017 Feb 8; doi: 10.1001/jamacardio.2016.5493).
Estimates suggested that identification of individuals at elevated risk for developing CAC could inform a selective CT screening strategy whereby the number of younger adults screened could be reduced by half, and the number needing to be imaged to find one person with CAC could be reduced from 3.5 to 2.2.
“The finding that CAC present by ages 32-46 years is associated with increased risk of premature CHD and death emphasizes the need for reduction of risk factors and primordial prevention beginning in early life,” wrote Dr. Carr, professor radiology at Vanderbilt University in Nashville, Tenn.
“Whether any kind of general screening for CAC is warranted needs further study, although we suggest that a strategy in which all individuals aged 32 to 46 years are screened is not indicated. Rather, a more targeted approach based on measuring risk factors in early adult life to predict individuals at high risk for developing CAC in whom the CT scan would have the greatest value can be considered,” they propose.
Study details
Participants were recruited to CARDIA when aged 18-30 years, and they underwent CAC measurement at 15, 20, and 25 years after recruitment. Incident events were ascertained starting from the time of the year-15 scan.
At that year-15 scan, 10.2% of participants were found to have CAC. The geometric mean Agatston score was 21.6.
In adjusted analyses, participants with any CAC had sharply higher risks of CHD events (hazard ratio, 5.0), as well as cardiovascular disease events (HR, 3.0). The risk of CHD events increased with CAC score, with hazard ratios of 2.6, 5.8, and 9.8 for individuals with scores of 1-19, 20-99, and 100 or more, respectively.
In addition, participants with any CAC had an elevated adjusted risk of all-cause mortality (HR, 1.6). This risk similarly rose with score but was significant for those having a score of 100 or greater only (hazard ratio, 3.7); the large majority of deaths in this group were deemed to be from CHD events.
The model that the investigators developed predicted the probability of CAC by ages 32-56 years based on risk factors assessed 7 years apart, between the ages of 18 and 38 years.
When stratified by this model, 4.2% of study participants falling into the lowest-risk decile had CAC, compared with 67.8% of those falling into the highest-risk decile.
Analyses suggested that if screening were restricted to those participants having an above-median risk score, fully 77.3% of all those with coronary calcium and 95.5% of all those with CHD events would be identified. Moreover, these yields would be obtained while reducing the number of individuals recommended to be screened by 50.0%.
Younger adults who have any calcium deposited in their coronary arteries, even a small amount, are at increased risk for adverse coronary heart disease (CHD) outcomes and death, finds an analysis of the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
There’s no evidence, however, that treating such patients would make a difference in outcomes, John Jeffrey Carr, MD, reported in JAMA Cardiology on Feb. 8.
In the prospective, community-based, cohort study, 5,115 black and white adults underwent coronary computed tomographic (CT) imaging between the ages of 32 and 46 years, and had a mean follow-up of 12.5 years.
Compared with counterparts not having any coronary artery calcium (CAC), those having at least some had a 5.0-fold increased risk of CHD events and a 1.6-fold increased risk of death (JAMA Cardiol. 2017 Feb 8; doi: 10.1001/jamacardio.2016.5493).
Estimates suggested that identification of individuals at elevated risk for developing CAC could inform a selective CT screening strategy whereby the number of younger adults screened could be reduced by half, and the number needing to be imaged to find one person with CAC could be reduced from 3.5 to 2.2.
“The finding that CAC present by ages 32-46 years is associated with increased risk of premature CHD and death emphasizes the need for reduction of risk factors and primordial prevention beginning in early life,” wrote Dr. Carr, professor radiology at Vanderbilt University in Nashville, Tenn.
“Whether any kind of general screening for CAC is warranted needs further study, although we suggest that a strategy in which all individuals aged 32 to 46 years are screened is not indicated. Rather, a more targeted approach based on measuring risk factors in early adult life to predict individuals at high risk for developing CAC in whom the CT scan would have the greatest value can be considered,” they propose.
Study details
Participants were recruited to CARDIA when aged 18-30 years, and they underwent CAC measurement at 15, 20, and 25 years after recruitment. Incident events were ascertained starting from the time of the year-15 scan.
At that year-15 scan, 10.2% of participants were found to have CAC. The geometric mean Agatston score was 21.6.
In adjusted analyses, participants with any CAC had sharply higher risks of CHD events (hazard ratio, 5.0), as well as cardiovascular disease events (HR, 3.0). The risk of CHD events increased with CAC score, with hazard ratios of 2.6, 5.8, and 9.8 for individuals with scores of 1-19, 20-99, and 100 or more, respectively.
In addition, participants with any CAC had an elevated adjusted risk of all-cause mortality (HR, 1.6). This risk similarly rose with score but was significant for those having a score of 100 or greater only (hazard ratio, 3.7); the large majority of deaths in this group were deemed to be from CHD events.
The model that the investigators developed predicted the probability of CAC by ages 32-56 years based on risk factors assessed 7 years apart, between the ages of 18 and 38 years.
When stratified by this model, 4.2% of study participants falling into the lowest-risk decile had CAC, compared with 67.8% of those falling into the highest-risk decile.
Analyses suggested that if screening were restricted to those participants having an above-median risk score, fully 77.3% of all those with coronary calcium and 95.5% of all those with CHD events would be identified. Moreover, these yields would be obtained while reducing the number of individuals recommended to be screened by 50.0%.
FROM JAMA CARDIOLOGY
Key clinical point:
Major finding: Individuals having any versus no coronary artery calcium when aged 32-46 years had elevated risks of CHD events (HR, 5.0) and death (HR, 1.6) by the age of 58 years.
Data source: A prospective community-based cohort study of 5,115 black and white adults (CARDIA Study).
Disclosures: Dr. Carr disclosed that he had no relevant conflicts of interest.