User login
VIDEO: Blood pressure and LDL lowering in elderly do not slow cognitive decline
NEW ORLEANS – Blood pressure and cholesterol lowering in elderly patients with moderate vascular risk did not prevent cognitive decline in HOPE-3, the large randomized Heart Outcomes and Prevention Evaluation-3 trial, Jackie Bosch, PhD, reported at the American Heart Association scientific sessions.
Disappointing, but the study also brought some welcome glass-half-full good news: Although treatment did not slow cognitive decline, it didn’t worsen it, either, as some had feared. That means the clinically meaningful reduction in cardiovascular events conferred with blood pressure and cholesterol lowering previously reported in HOPE-3 does not come at the cost of an increased risk of dementia.
Rosuvastatin had no adverse effect on cognitive function in HOPE-3. This is an important finding, given the black box warning for statins mandated by the Food and Drug Administration, which was based only on observational postmarketing surveillance data,” observed Dr. Bosch of the Population Health Research Institute at McMaster University in Hamilton, Ont.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bosch reported on the 1,626 subjects who were at least 70 years old at baseline – their mean age was 75 – and who completed a battery of cognitive and functional status tests and questionnaires at baseline.
The primary outcome in the HOPE-3 cognition substudy was decline over time in processing speed as measured on the Digit Symbol Substitution Test. There was an equal decline, regardless of whether patients were on blood pressure lowering, rosuvastatin, both, or double placebo.
Nor did statin- or blood pressure–lowering therapy have any impact on the secondary endpoints of decline in executive function as assessed by the modified Montreal Cognitive Assessment or the change in psychomotor speed as reflected in the Trail Making Test part B.
Moreover, treatment had no effect on age-related decline in overall functional status. During a mean of 5.6 years of follow-up, 22% of participants developed a new functional impairment regardless of whether they were on blood pressure– and/or cholesterol-lowering medication or double placebo.
Intriguingly, however, subgroup analyses provided a glimmer of hope. Patients who were in the top tertile for blood pressure at baseline, with a systolic blood pressure of 133 mm Hg or more, as well as the top tertile for LDL cholesterol, with an LDL of at least 112 mg/dL, showed significantly less decline in cognitive function over time if they were on rosuvastatin and blood pressure lowering than with double placebo. This higher-risk group showed a mean loss of only 4.65 points on the Digit Symbol Substitution Test, compared with an 11.8-point drop for those on double placebo. This is a post-hoc analysis, however, and the efficacy signal must be viewed as hypothesis generating, Dr. Bosch stressed.
Discussant Philip B. Gorelick, MD, MPH, said that he didn’t find the negative HOPE-3 cognition results surprising. After all, he coauthored a recent AHA/American Stroke Association Scientific Statement on the impact of hypertension on cognitive function that scrutinized 10 clinical hypertension trials and concluded that only two of them – SYST-EUR (Systolic Hypertension in Europe) and PROGRESS (Peridopril Protection Against Recurrent Stroke Study) – showed any indication that treating hypertension reduced cognitive decline (Hypertension. 2016. doi: 10.1161/HYP.0000000000000053).
Plus, a 2016 Cochrane Collaboration review of the published evidence concluded that, in older people at vascular risk, statins do not prevent cognitive decline or dementia after 3.5-5 years of treatment (Cochrane Database Syst Rev. 2016 Jan 4;[1]:CD003160).
“The horse may be out of the barn for many of our patients when we start intervening later in life. That’s not to say it can’t work, but the Alzheimer’s changes and disease process are beginning 20 or 30 years earlier, so we’ve got to intervene earlier,” said Dr. Gorelick, professor of translational science and molecular medicine at the Michigan State University College of Human Medicine, Grand Rapids.
Dr. Bosch concurred. “We know that, in epidemiologic studies, midlife hypertension is strongly associated with later cognitive impairment. We’ve missed the boat on the 70-year-olds,” she said. “We need to start treatment earlier and probably for longer.”
Dr. Bosch reported having no financial conflicts regarding the HOPE-3 study, which was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. Dr. Gorelick reported serving as a consultant to Novartis regarding blood pressure lowering and maintenance of cognition.
NEW ORLEANS – Blood pressure and cholesterol lowering in elderly patients with moderate vascular risk did not prevent cognitive decline in HOPE-3, the large randomized Heart Outcomes and Prevention Evaluation-3 trial, Jackie Bosch, PhD, reported at the American Heart Association scientific sessions.
Disappointing, but the study also brought some welcome glass-half-full good news: Although treatment did not slow cognitive decline, it didn’t worsen it, either, as some had feared. That means the clinically meaningful reduction in cardiovascular events conferred with blood pressure and cholesterol lowering previously reported in HOPE-3 does not come at the cost of an increased risk of dementia.
Rosuvastatin had no adverse effect on cognitive function in HOPE-3. This is an important finding, given the black box warning for statins mandated by the Food and Drug Administration, which was based only on observational postmarketing surveillance data,” observed Dr. Bosch of the Population Health Research Institute at McMaster University in Hamilton, Ont.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bosch reported on the 1,626 subjects who were at least 70 years old at baseline – their mean age was 75 – and who completed a battery of cognitive and functional status tests and questionnaires at baseline.
The primary outcome in the HOPE-3 cognition substudy was decline over time in processing speed as measured on the Digit Symbol Substitution Test. There was an equal decline, regardless of whether patients were on blood pressure lowering, rosuvastatin, both, or double placebo.
Nor did statin- or blood pressure–lowering therapy have any impact on the secondary endpoints of decline in executive function as assessed by the modified Montreal Cognitive Assessment or the change in psychomotor speed as reflected in the Trail Making Test part B.
Moreover, treatment had no effect on age-related decline in overall functional status. During a mean of 5.6 years of follow-up, 22% of participants developed a new functional impairment regardless of whether they were on blood pressure– and/or cholesterol-lowering medication or double placebo.
Intriguingly, however, subgroup analyses provided a glimmer of hope. Patients who were in the top tertile for blood pressure at baseline, with a systolic blood pressure of 133 mm Hg or more, as well as the top tertile for LDL cholesterol, with an LDL of at least 112 mg/dL, showed significantly less decline in cognitive function over time if they were on rosuvastatin and blood pressure lowering than with double placebo. This higher-risk group showed a mean loss of only 4.65 points on the Digit Symbol Substitution Test, compared with an 11.8-point drop for those on double placebo. This is a post-hoc analysis, however, and the efficacy signal must be viewed as hypothesis generating, Dr. Bosch stressed.
Discussant Philip B. Gorelick, MD, MPH, said that he didn’t find the negative HOPE-3 cognition results surprising. After all, he coauthored a recent AHA/American Stroke Association Scientific Statement on the impact of hypertension on cognitive function that scrutinized 10 clinical hypertension trials and concluded that only two of them – SYST-EUR (Systolic Hypertension in Europe) and PROGRESS (Peridopril Protection Against Recurrent Stroke Study) – showed any indication that treating hypertension reduced cognitive decline (Hypertension. 2016. doi: 10.1161/HYP.0000000000000053).
Plus, a 2016 Cochrane Collaboration review of the published evidence concluded that, in older people at vascular risk, statins do not prevent cognitive decline or dementia after 3.5-5 years of treatment (Cochrane Database Syst Rev. 2016 Jan 4;[1]:CD003160).
“The horse may be out of the barn for many of our patients when we start intervening later in life. That’s not to say it can’t work, but the Alzheimer’s changes and disease process are beginning 20 or 30 years earlier, so we’ve got to intervene earlier,” said Dr. Gorelick, professor of translational science and molecular medicine at the Michigan State University College of Human Medicine, Grand Rapids.
Dr. Bosch concurred. “We know that, in epidemiologic studies, midlife hypertension is strongly associated with later cognitive impairment. We’ve missed the boat on the 70-year-olds,” she said. “We need to start treatment earlier and probably for longer.”
Dr. Bosch reported having no financial conflicts regarding the HOPE-3 study, which was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. Dr. Gorelick reported serving as a consultant to Novartis regarding blood pressure lowering and maintenance of cognition.
NEW ORLEANS – Blood pressure and cholesterol lowering in elderly patients with moderate vascular risk did not prevent cognitive decline in HOPE-3, the large randomized Heart Outcomes and Prevention Evaluation-3 trial, Jackie Bosch, PhD, reported at the American Heart Association scientific sessions.
Disappointing, but the study also brought some welcome glass-half-full good news: Although treatment did not slow cognitive decline, it didn’t worsen it, either, as some had feared. That means the clinically meaningful reduction in cardiovascular events conferred with blood pressure and cholesterol lowering previously reported in HOPE-3 does not come at the cost of an increased risk of dementia.
Rosuvastatin had no adverse effect on cognitive function in HOPE-3. This is an important finding, given the black box warning for statins mandated by the Food and Drug Administration, which was based only on observational postmarketing surveillance data,” observed Dr. Bosch of the Population Health Research Institute at McMaster University in Hamilton, Ont.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Bosch reported on the 1,626 subjects who were at least 70 years old at baseline – their mean age was 75 – and who completed a battery of cognitive and functional status tests and questionnaires at baseline.
The primary outcome in the HOPE-3 cognition substudy was decline over time in processing speed as measured on the Digit Symbol Substitution Test. There was an equal decline, regardless of whether patients were on blood pressure lowering, rosuvastatin, both, or double placebo.
Nor did statin- or blood pressure–lowering therapy have any impact on the secondary endpoints of decline in executive function as assessed by the modified Montreal Cognitive Assessment or the change in psychomotor speed as reflected in the Trail Making Test part B.
Moreover, treatment had no effect on age-related decline in overall functional status. During a mean of 5.6 years of follow-up, 22% of participants developed a new functional impairment regardless of whether they were on blood pressure– and/or cholesterol-lowering medication or double placebo.
Intriguingly, however, subgroup analyses provided a glimmer of hope. Patients who were in the top tertile for blood pressure at baseline, with a systolic blood pressure of 133 mm Hg or more, as well as the top tertile for LDL cholesterol, with an LDL of at least 112 mg/dL, showed significantly less decline in cognitive function over time if they were on rosuvastatin and blood pressure lowering than with double placebo. This higher-risk group showed a mean loss of only 4.65 points on the Digit Symbol Substitution Test, compared with an 11.8-point drop for those on double placebo. This is a post-hoc analysis, however, and the efficacy signal must be viewed as hypothesis generating, Dr. Bosch stressed.
Discussant Philip B. Gorelick, MD, MPH, said that he didn’t find the negative HOPE-3 cognition results surprising. After all, he coauthored a recent AHA/American Stroke Association Scientific Statement on the impact of hypertension on cognitive function that scrutinized 10 clinical hypertension trials and concluded that only two of them – SYST-EUR (Systolic Hypertension in Europe) and PROGRESS (Peridopril Protection Against Recurrent Stroke Study) – showed any indication that treating hypertension reduced cognitive decline (Hypertension. 2016. doi: 10.1161/HYP.0000000000000053).
Plus, a 2016 Cochrane Collaboration review of the published evidence concluded that, in older people at vascular risk, statins do not prevent cognitive decline or dementia after 3.5-5 years of treatment (Cochrane Database Syst Rev. 2016 Jan 4;[1]:CD003160).
“The horse may be out of the barn for many of our patients when we start intervening later in life. That’s not to say it can’t work, but the Alzheimer’s changes and disease process are beginning 20 or 30 years earlier, so we’ve got to intervene earlier,” said Dr. Gorelick, professor of translational science and molecular medicine at the Michigan State University College of Human Medicine, Grand Rapids.
Dr. Bosch concurred. “We know that, in epidemiologic studies, midlife hypertension is strongly associated with later cognitive impairment. We’ve missed the boat on the 70-year-olds,” she said. “We need to start treatment earlier and probably for longer.”
Dr. Bosch reported having no financial conflicts regarding the HOPE-3 study, which was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. Dr. Gorelick reported serving as a consultant to Novartis regarding blood pressure lowering and maintenance of cognition.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: Nearly 6 years of blood pressure lowering and statin therapy in elderly patients with moderate vascular risk did not prevent cognitive decline relative to placebo, but the treatment did not worsen it, either.
Data source: This analysis of cognitive and functional outcomes in the randomized multicenter HOPE-3 trial included 1,626 participants who were at least 70 years old at baseline, when they were randomized to blood pressure lowering or placebo and rosuvastatin or placebo and followed for a mean of 5.6 years.
Disclosures: The HOPE-3 study was funded by unrestricted grants from the Canadian Institutes of Health Research and AstraZeneca. The presenter reported having no financial conflicts of interest.
VIDEO: PRECISION exonerates celecoxib: cardiovascular risk is no worse than that of nonselective NSAIDs
NEW ORLEANS – The cardiovascular safety profile of the nonsteroidal anti-inflammatory drug (NSAID) celecoxib, a selective inhibitor of COX-2, is no worse than those of the nonselective NSAIDs naproxen and ibuprofen, according to a trial reported at the American Heart Association scientific sessions.
The trial, known as PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen Or Naproxen) was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that 2%-3% of patients experienced a cardiovascular event (cardiovascular death, myocardial infarction, or stroke) during a follow-up approaching 3 years, regardless of which drug they were assigned to take, with the slight differences falling within predefined margins for noninferiority of celecoxib, investigators reported in a session and related press conference.
Additionally, celecoxib yielded a lower rate of gastrointestinal events when compared with each of the other drugs and a lower rate of renal events when compared with ibuprofen.
“After the withdrawal of rofecoxib, everybody thought they knew the answer, that COX-2 inhibitors had an unfavorable cardiovascular profile,” commented first author Steven E. Nissen, MD, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “We didn’t find that. And this is the type of study that once again teaches us that if we jump to conclusions about this based on mechanistic considerations, we often make very bad decisions.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Efforts are under way to disseminate the PRECISION findings to rheumatologists and other groups who do much of the NSAID prescribing.
“Any time you have something that has findings like the findings we have, it takes some time to trickle down to the prescribers. It’s going to be our job to communicate both the value and the important limitations of the trial so that people can make informed decisions about which of these drugs to use and in whom,” Dr. Nissen said.
A cautionary view
“The investigators addressed an extremely important question, which is what is the cardiovascular safety of agents that we administer for a general medical condition over the long term,” commented invited discussant Elliott M. Antman, MD, a senior physician at Brigham and Women’s Hospital and associate dean for Clinical and Translational Research at Harvard Medical School in Boston. “We don’t see a lot of trials like that, but we do need this information.”
“This is not a comparison of drugs; this is a comparison of drug regimens because the investigators were able to increase the dose to control the subjects’ pain,” Dr. Antman elaborated. “And they were able to increase the dose of naproxen and ibuprofen comparatively more than they could for celecoxib,” which was capped at 200 mg per day at most study sites.
Furthermore, only about one-fifth of the patients studied had known heart disease. “We know that the more likely a person is to have atherosclerosis, the more likely they are to experience harm from COX-2 inhibition,” he said. “So given the profile of the patients in this trial, it’s unlikely that we would have been able to detect that signal of harm from COX-2 inhibition, particularly at this dose.”
Dr. Antman also had concerns about the impact on concomitant aspirin therapy (the benefit of which can be affected by nonselective NSAIDs) and about possible differences in the reasons for dropouts that may have biased findings toward celecoxib. “I believe we need more information in order to more completely interpret this trial,” he summarized.
For now, he advised physicians to follow guidance put forth by the American Heart Association: Avoid NSAIDs in patients with known heart disease, and if one must use them, try to use the lowest-risk drug in the lowest dose needed for the shortest period of time.
In the future, “we should actually break out of the mold of assigning everybody in the trial a common phenotype and reporting the average result, but instead take a precision medicine approach, where we look at the polymorphisms in the COX enzyme, look at the polymorphisms in the ability to metabolize these drugs, and actually see if we can be more precise,” Dr. Antman maintained. “Finally, there is an urgent clinical need for the development of novel analgesics and other therapeutics to avoid the cardiovascular risk from all NSAIDs.”
Trial details
Patients were eligible for PRECISION, a Pfizer-funded trial, if they had osteoarthritis or rheumatoid arthritis and were at increased cardiovascular risk.
In all, 24,081 patients from 926 centers globally were randomly assigned to double-blind treatment with celecoxib, naproxen, or ibuprofen, all of which are now available as generics in the United States.
“Patients were randomized to the FDA-approved doses of these drugs, and they could have their dose increased if they had unrelieved pain up to the maximum allowed by regulatory authorities in the local jurisdictions where the study was done,” Dr. Nissen noted, pointing out that studies initially generating some concern about celecoxib used a supratherapeutic dose of 800 mg daily.
As COX-2 inhibitors are less likely than nonselective NSAIDs to cause ulcers, which might affect compliance and outcomes, all patients additionally received esomeprazole for gastroprotection “to try to level the playing field,” he explained.
The mean treatment duration was 20.3 months, and the mean follow-up duration was 34.1 months, according to data reported at the meeting and simultaneously published (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593). On average, the daily dose of drug received was 209 mg for celecoxib, 852 mg for naproxen, and 2,045 mg for ibuprofen.
In intention-to-treat analyses, the rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% in the celecoxib group, 2.5% in the naproxen group, and 2.7% in the ibuprofen group. The hazard ratio was 0.93 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.85 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Differences were more marked in the on-treatment population. Here, the rate of the primary outcome was 1.7% in the celecoxib group, 1.8% in the naproxen group, and 1.9% in the ibuprofen group. The HR was 0.90 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.81 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Secondary outcomes, which tested for superiority, showed that the rate of major adverse cardiovascular events was 15% higher in the ibuprofen group as compared with the celecoxib group in the intent-to-treat population. The difference translated to a near-significant reduction in risk with the latter (HR, 0.87; P = .06) that appeared greater in the on-treatment population.
However, Dr. Nissen cautioned that he could not state that celecoxib was superior. “Secondary and tertiary endpoints in a clinical trial are hypothesis generating, and they are not considered definitive evidence,” he commented. At the same time, “the FDA is going to have to deal with that because what do they do with labeling? What do they do with over-the-counter access to these various drugs?”
The rate of all-cause mortality was 25% higher with naproxen than with celecoxib (HR, 0.80; P = .052).
The rate of gastrointestinal events was 54% higher with ibuprofen (HR, 0.65; P = .002) and 41% higher with naproxen (HR, 0.71; P = .01) as compared with celecoxib. And the rate of renal events was 64% higher with ibuprofen than with celecoxib (HR, 0.61; P = .004).
In a post hoc analysis of global safety, the rate of serious cardiovascular, gastrointestinal, and renal events was 28% higher with ibuprofen (HR, 0.78; P less than .001) and 15% higher with naproxen (HR, 0.87; P = .03) than with celecoxib.
Of note, the findings for the primary endpoint were similar regardless of whether patients were taking low-dose aspirin or not. “There was no interaction with aspirin use,” Dr. Nissen stated. “This was not about the interference of ibuprofen or naproxen with aspirin use.”
Analyses of pain relief using a visual analogue scale showed no clinically meaningful differences, suggesting that the drug doses used were equally analgesic, he said. Stopping of study drug because of lack of efficacy was slightly more common in the celecoxib group.
“We didn’t study the low-dose, intermittent use of these drugs that most of the public engages in, and it’s really important that we crisply communicate that to the public because somebody who takes occasionally ibuprofen or naproxen for a headache should not look at these comparative data in a way that should necessarily influence their behavior. We just don’t know the answer,” cautioned Dr. Nissen, who disclosed that he received grant support from Pfizer during the conduct of the trial.
But the findings are relevant for individuals who take over-the-counter NSAIDs at doses exceeding the label, a phenomenon known as dose creep. “We need to reemphasize to the public that the labeled over-the-counter dose is what you should take. You shouldn’t double up or triple up on the drugs because the issue of high-dose therapy, which is what we studied, suggests that there are really potentially important gastrointestinal, renal, and cardiovascular risks,” he said.
NEW ORLEANS – The cardiovascular safety profile of the nonsteroidal anti-inflammatory drug (NSAID) celecoxib, a selective inhibitor of COX-2, is no worse than those of the nonselective NSAIDs naproxen and ibuprofen, according to a trial reported at the American Heart Association scientific sessions.
The trial, known as PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen Or Naproxen) was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that 2%-3% of patients experienced a cardiovascular event (cardiovascular death, myocardial infarction, or stroke) during a follow-up approaching 3 years, regardless of which drug they were assigned to take, with the slight differences falling within predefined margins for noninferiority of celecoxib, investigators reported in a session and related press conference.
Additionally, celecoxib yielded a lower rate of gastrointestinal events when compared with each of the other drugs and a lower rate of renal events when compared with ibuprofen.
“After the withdrawal of rofecoxib, everybody thought they knew the answer, that COX-2 inhibitors had an unfavorable cardiovascular profile,” commented first author Steven E. Nissen, MD, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “We didn’t find that. And this is the type of study that once again teaches us that if we jump to conclusions about this based on mechanistic considerations, we often make very bad decisions.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Efforts are under way to disseminate the PRECISION findings to rheumatologists and other groups who do much of the NSAID prescribing.
“Any time you have something that has findings like the findings we have, it takes some time to trickle down to the prescribers. It’s going to be our job to communicate both the value and the important limitations of the trial so that people can make informed decisions about which of these drugs to use and in whom,” Dr. Nissen said.
A cautionary view
“The investigators addressed an extremely important question, which is what is the cardiovascular safety of agents that we administer for a general medical condition over the long term,” commented invited discussant Elliott M. Antman, MD, a senior physician at Brigham and Women’s Hospital and associate dean for Clinical and Translational Research at Harvard Medical School in Boston. “We don’t see a lot of trials like that, but we do need this information.”
“This is not a comparison of drugs; this is a comparison of drug regimens because the investigators were able to increase the dose to control the subjects’ pain,” Dr. Antman elaborated. “And they were able to increase the dose of naproxen and ibuprofen comparatively more than they could for celecoxib,” which was capped at 200 mg per day at most study sites.
Furthermore, only about one-fifth of the patients studied had known heart disease. “We know that the more likely a person is to have atherosclerosis, the more likely they are to experience harm from COX-2 inhibition,” he said. “So given the profile of the patients in this trial, it’s unlikely that we would have been able to detect that signal of harm from COX-2 inhibition, particularly at this dose.”
Dr. Antman also had concerns about the impact on concomitant aspirin therapy (the benefit of which can be affected by nonselective NSAIDs) and about possible differences in the reasons for dropouts that may have biased findings toward celecoxib. “I believe we need more information in order to more completely interpret this trial,” he summarized.
For now, he advised physicians to follow guidance put forth by the American Heart Association: Avoid NSAIDs in patients with known heart disease, and if one must use them, try to use the lowest-risk drug in the lowest dose needed for the shortest period of time.
In the future, “we should actually break out of the mold of assigning everybody in the trial a common phenotype and reporting the average result, but instead take a precision medicine approach, where we look at the polymorphisms in the COX enzyme, look at the polymorphisms in the ability to metabolize these drugs, and actually see if we can be more precise,” Dr. Antman maintained. “Finally, there is an urgent clinical need for the development of novel analgesics and other therapeutics to avoid the cardiovascular risk from all NSAIDs.”
Trial details
Patients were eligible for PRECISION, a Pfizer-funded trial, if they had osteoarthritis or rheumatoid arthritis and were at increased cardiovascular risk.
In all, 24,081 patients from 926 centers globally were randomly assigned to double-blind treatment with celecoxib, naproxen, or ibuprofen, all of which are now available as generics in the United States.
“Patients were randomized to the FDA-approved doses of these drugs, and they could have their dose increased if they had unrelieved pain up to the maximum allowed by regulatory authorities in the local jurisdictions where the study was done,” Dr. Nissen noted, pointing out that studies initially generating some concern about celecoxib used a supratherapeutic dose of 800 mg daily.
As COX-2 inhibitors are less likely than nonselective NSAIDs to cause ulcers, which might affect compliance and outcomes, all patients additionally received esomeprazole for gastroprotection “to try to level the playing field,” he explained.
The mean treatment duration was 20.3 months, and the mean follow-up duration was 34.1 months, according to data reported at the meeting and simultaneously published (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593). On average, the daily dose of drug received was 209 mg for celecoxib, 852 mg for naproxen, and 2,045 mg for ibuprofen.
In intention-to-treat analyses, the rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% in the celecoxib group, 2.5% in the naproxen group, and 2.7% in the ibuprofen group. The hazard ratio was 0.93 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.85 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Differences were more marked in the on-treatment population. Here, the rate of the primary outcome was 1.7% in the celecoxib group, 1.8% in the naproxen group, and 1.9% in the ibuprofen group. The HR was 0.90 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.81 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Secondary outcomes, which tested for superiority, showed that the rate of major adverse cardiovascular events was 15% higher in the ibuprofen group as compared with the celecoxib group in the intent-to-treat population. The difference translated to a near-significant reduction in risk with the latter (HR, 0.87; P = .06) that appeared greater in the on-treatment population.
However, Dr. Nissen cautioned that he could not state that celecoxib was superior. “Secondary and tertiary endpoints in a clinical trial are hypothesis generating, and they are not considered definitive evidence,” he commented. At the same time, “the FDA is going to have to deal with that because what do they do with labeling? What do they do with over-the-counter access to these various drugs?”
The rate of all-cause mortality was 25% higher with naproxen than with celecoxib (HR, 0.80; P = .052).
The rate of gastrointestinal events was 54% higher with ibuprofen (HR, 0.65; P = .002) and 41% higher with naproxen (HR, 0.71; P = .01) as compared with celecoxib. And the rate of renal events was 64% higher with ibuprofen than with celecoxib (HR, 0.61; P = .004).
In a post hoc analysis of global safety, the rate of serious cardiovascular, gastrointestinal, and renal events was 28% higher with ibuprofen (HR, 0.78; P less than .001) and 15% higher with naproxen (HR, 0.87; P = .03) than with celecoxib.
Of note, the findings for the primary endpoint were similar regardless of whether patients were taking low-dose aspirin or not. “There was no interaction with aspirin use,” Dr. Nissen stated. “This was not about the interference of ibuprofen or naproxen with aspirin use.”
Analyses of pain relief using a visual analogue scale showed no clinically meaningful differences, suggesting that the drug doses used were equally analgesic, he said. Stopping of study drug because of lack of efficacy was slightly more common in the celecoxib group.
“We didn’t study the low-dose, intermittent use of these drugs that most of the public engages in, and it’s really important that we crisply communicate that to the public because somebody who takes occasionally ibuprofen or naproxen for a headache should not look at these comparative data in a way that should necessarily influence their behavior. We just don’t know the answer,” cautioned Dr. Nissen, who disclosed that he received grant support from Pfizer during the conduct of the trial.
But the findings are relevant for individuals who take over-the-counter NSAIDs at doses exceeding the label, a phenomenon known as dose creep. “We need to reemphasize to the public that the labeled over-the-counter dose is what you should take. You shouldn’t double up or triple up on the drugs because the issue of high-dose therapy, which is what we studied, suggests that there are really potentially important gastrointestinal, renal, and cardiovascular risks,” he said.
NEW ORLEANS – The cardiovascular safety profile of the nonsteroidal anti-inflammatory drug (NSAID) celecoxib, a selective inhibitor of COX-2, is no worse than those of the nonselective NSAIDs naproxen and ibuprofen, according to a trial reported at the American Heart Association scientific sessions.
The trial, known as PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen Or Naproxen) was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that 2%-3% of patients experienced a cardiovascular event (cardiovascular death, myocardial infarction, or stroke) during a follow-up approaching 3 years, regardless of which drug they were assigned to take, with the slight differences falling within predefined margins for noninferiority of celecoxib, investigators reported in a session and related press conference.
Additionally, celecoxib yielded a lower rate of gastrointestinal events when compared with each of the other drugs and a lower rate of renal events when compared with ibuprofen.
“After the withdrawal of rofecoxib, everybody thought they knew the answer, that COX-2 inhibitors had an unfavorable cardiovascular profile,” commented first author Steven E. Nissen, MD, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “We didn’t find that. And this is the type of study that once again teaches us that if we jump to conclusions about this based on mechanistic considerations, we often make very bad decisions.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Efforts are under way to disseminate the PRECISION findings to rheumatologists and other groups who do much of the NSAID prescribing.
“Any time you have something that has findings like the findings we have, it takes some time to trickle down to the prescribers. It’s going to be our job to communicate both the value and the important limitations of the trial so that people can make informed decisions about which of these drugs to use and in whom,” Dr. Nissen said.
A cautionary view
“The investigators addressed an extremely important question, which is what is the cardiovascular safety of agents that we administer for a general medical condition over the long term,” commented invited discussant Elliott M. Antman, MD, a senior physician at Brigham and Women’s Hospital and associate dean for Clinical and Translational Research at Harvard Medical School in Boston. “We don’t see a lot of trials like that, but we do need this information.”
“This is not a comparison of drugs; this is a comparison of drug regimens because the investigators were able to increase the dose to control the subjects’ pain,” Dr. Antman elaborated. “And they were able to increase the dose of naproxen and ibuprofen comparatively more than they could for celecoxib,” which was capped at 200 mg per day at most study sites.
Furthermore, only about one-fifth of the patients studied had known heart disease. “We know that the more likely a person is to have atherosclerosis, the more likely they are to experience harm from COX-2 inhibition,” he said. “So given the profile of the patients in this trial, it’s unlikely that we would have been able to detect that signal of harm from COX-2 inhibition, particularly at this dose.”
Dr. Antman also had concerns about the impact on concomitant aspirin therapy (the benefit of which can be affected by nonselective NSAIDs) and about possible differences in the reasons for dropouts that may have biased findings toward celecoxib. “I believe we need more information in order to more completely interpret this trial,” he summarized.
For now, he advised physicians to follow guidance put forth by the American Heart Association: Avoid NSAIDs in patients with known heart disease, and if one must use them, try to use the lowest-risk drug in the lowest dose needed for the shortest period of time.
In the future, “we should actually break out of the mold of assigning everybody in the trial a common phenotype and reporting the average result, but instead take a precision medicine approach, where we look at the polymorphisms in the COX enzyme, look at the polymorphisms in the ability to metabolize these drugs, and actually see if we can be more precise,” Dr. Antman maintained. “Finally, there is an urgent clinical need for the development of novel analgesics and other therapeutics to avoid the cardiovascular risk from all NSAIDs.”
Trial details
Patients were eligible for PRECISION, a Pfizer-funded trial, if they had osteoarthritis or rheumatoid arthritis and were at increased cardiovascular risk.
In all, 24,081 patients from 926 centers globally were randomly assigned to double-blind treatment with celecoxib, naproxen, or ibuprofen, all of which are now available as generics in the United States.
“Patients were randomized to the FDA-approved doses of these drugs, and they could have their dose increased if they had unrelieved pain up to the maximum allowed by regulatory authorities in the local jurisdictions where the study was done,” Dr. Nissen noted, pointing out that studies initially generating some concern about celecoxib used a supratherapeutic dose of 800 mg daily.
As COX-2 inhibitors are less likely than nonselective NSAIDs to cause ulcers, which might affect compliance and outcomes, all patients additionally received esomeprazole for gastroprotection “to try to level the playing field,” he explained.
The mean treatment duration was 20.3 months, and the mean follow-up duration was 34.1 months, according to data reported at the meeting and simultaneously published (N Engl J Med. 2016 Nov 13. doi: 10.1056/NEJMoa1611593). On average, the daily dose of drug received was 209 mg for celecoxib, 852 mg for naproxen, and 2,045 mg for ibuprofen.
In intention-to-treat analyses, the rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% in the celecoxib group, 2.5% in the naproxen group, and 2.7% in the ibuprofen group. The hazard ratio was 0.93 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.85 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Differences were more marked in the on-treatment population. Here, the rate of the primary outcome was 1.7% in the celecoxib group, 1.8% in the naproxen group, and 1.9% in the ibuprofen group. The HR was 0.90 for celecoxib versus naproxen (P less than .001 for noninferiority) and 0.81 for celecoxib versus ibuprofen (P less than .001 for noninferiority).
Secondary outcomes, which tested for superiority, showed that the rate of major adverse cardiovascular events was 15% higher in the ibuprofen group as compared with the celecoxib group in the intent-to-treat population. The difference translated to a near-significant reduction in risk with the latter (HR, 0.87; P = .06) that appeared greater in the on-treatment population.
However, Dr. Nissen cautioned that he could not state that celecoxib was superior. “Secondary and tertiary endpoints in a clinical trial are hypothesis generating, and they are not considered definitive evidence,” he commented. At the same time, “the FDA is going to have to deal with that because what do they do with labeling? What do they do with over-the-counter access to these various drugs?”
The rate of all-cause mortality was 25% higher with naproxen than with celecoxib (HR, 0.80; P = .052).
The rate of gastrointestinal events was 54% higher with ibuprofen (HR, 0.65; P = .002) and 41% higher with naproxen (HR, 0.71; P = .01) as compared with celecoxib. And the rate of renal events was 64% higher with ibuprofen than with celecoxib (HR, 0.61; P = .004).
In a post hoc analysis of global safety, the rate of serious cardiovascular, gastrointestinal, and renal events was 28% higher with ibuprofen (HR, 0.78; P less than .001) and 15% higher with naproxen (HR, 0.87; P = .03) than with celecoxib.
Of note, the findings for the primary endpoint were similar regardless of whether patients were taking low-dose aspirin or not. “There was no interaction with aspirin use,” Dr. Nissen stated. “This was not about the interference of ibuprofen or naproxen with aspirin use.”
Analyses of pain relief using a visual analogue scale showed no clinically meaningful differences, suggesting that the drug doses used were equally analgesic, he said. Stopping of study drug because of lack of efficacy was slightly more common in the celecoxib group.
“We didn’t study the low-dose, intermittent use of these drugs that most of the public engages in, and it’s really important that we crisply communicate that to the public because somebody who takes occasionally ibuprofen or naproxen for a headache should not look at these comparative data in a way that should necessarily influence their behavior. We just don’t know the answer,” cautioned Dr. Nissen, who disclosed that he received grant support from Pfizer during the conduct of the trial.
But the findings are relevant for individuals who take over-the-counter NSAIDs at doses exceeding the label, a phenomenon known as dose creep. “We need to reemphasize to the public that the labeled over-the-counter dose is what you should take. You shouldn’t double up or triple up on the drugs because the issue of high-dose therapy, which is what we studied, suggests that there are really potentially important gastrointestinal, renal, and cardiovascular risks,” he said.
AT THE AHA SCIENTIFIC SESSIONS
Key clinical point:
Major finding: The rate of the primary composite outcome of cardiovascular death (including hemorrhagic death), nonfatal myocardial infarction, or nonfatal stroke was 2.3% with celecoxib, 2.5% with naproxen, and 2.7% with ibuprofen (P less than .001 for noninferiority).
Data source: A randomized, controlled trial among 24,081 patients who required NSAIDs for painful arthritis and were at increased cardiovascular risk (PRECISION trial).
Disclosures: Dr. Nissen disclosed that he received grant support from Pfizer during the conduct of the trial. The trial was funded by Pfizer.
VIDEO: PCI outcomes lag in women, minorities
WASHINGTON – The relatively low number of women and minority-group patients enrolled into cardiovascular disease clinical trials may skew the results, based on a comparison of outcomes following coronary stenting in an analysis of more than 4,000 patients.
During 12 months following coronary-disease treatment with percutaneous coronary intervention (PCI), women of diverse racial and ethnic backgrounds had a statistically significant 60% relative increase in death and myocardial infarctions, compared with white men, after adjustment for known baseline variables, Wayne B. Batchelor, MD, reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Minority patients, a mix of women and men, had a 90% relative rise in death and MIs, and a 60% higher rate of MIs after adjustment, both statistically significant differences.
Dr. Batchelor and his associates have not yet analyzed what factors are behind these worse outcomes in women and minority patients. But he suspects social and economic factors may provide at least some explanation, including income, education, language fluency, exercise habits, and access to health care.
“I think the trends we saw are real; the question is what accounts for the differences,” said Dr. Batchelor, an interventional cardiologist in Tallahassee, Fla. Regardless of the causes, he believes that the outcome differences have important immediate messages.
“We need to ensure better representation of women and minorities in clinical trials,” he said in an interview. “We don’t collect enough data from women and minorities. Historically, they have been underrepresented in trials.”
Another lesson is the importance of putting women and minority patients with cardiovascular disease on guideline-directed treatment, including dual antiplatelet therapy, lipid-lowering drugs, and antihypertensive drugs. The results show potential opportunity to further improve outcomes in women and minority patients, Dr. Batchelor said at the meeting, sponsored by the Cardiovascular Research Foundation.
The PLATINUM Diversity trial enrolled 1,501 women and men from minority groups with coronary disease who required PCI at one of 52 U.S. sites. For his analysis, Dr. Batchelor combined the 12-month outcomes of these patients with 12-month data from 2,687 unselected patients enrolled in the PROMUS Element Plus post-marketing approval study, a group of mostly white men.
The PLATINUM Diversity trial was sponsored by Boston Scientific. Dr. Batchelor has received research support from and has been a speaker for and consultant to Boston Scientific. He also has been a speaker for and consultant to Abbott Vascular and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com On Twitter @mitchelzoler
WASHINGTON – The relatively low number of women and minority-group patients enrolled into cardiovascular disease clinical trials may skew the results, based on a comparison of outcomes following coronary stenting in an analysis of more than 4,000 patients.
During 12 months following coronary-disease treatment with percutaneous coronary intervention (PCI), women of diverse racial and ethnic backgrounds had a statistically significant 60% relative increase in death and myocardial infarctions, compared with white men, after adjustment for known baseline variables, Wayne B. Batchelor, MD, reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Minority patients, a mix of women and men, had a 90% relative rise in death and MIs, and a 60% higher rate of MIs after adjustment, both statistically significant differences.
Dr. Batchelor and his associates have not yet analyzed what factors are behind these worse outcomes in women and minority patients. But he suspects social and economic factors may provide at least some explanation, including income, education, language fluency, exercise habits, and access to health care.
“I think the trends we saw are real; the question is what accounts for the differences,” said Dr. Batchelor, an interventional cardiologist in Tallahassee, Fla. Regardless of the causes, he believes that the outcome differences have important immediate messages.
“We need to ensure better representation of women and minorities in clinical trials,” he said in an interview. “We don’t collect enough data from women and minorities. Historically, they have been underrepresented in trials.”
Another lesson is the importance of putting women and minority patients with cardiovascular disease on guideline-directed treatment, including dual antiplatelet therapy, lipid-lowering drugs, and antihypertensive drugs. The results show potential opportunity to further improve outcomes in women and minority patients, Dr. Batchelor said at the meeting, sponsored by the Cardiovascular Research Foundation.
The PLATINUM Diversity trial enrolled 1,501 women and men from minority groups with coronary disease who required PCI at one of 52 U.S. sites. For his analysis, Dr. Batchelor combined the 12-month outcomes of these patients with 12-month data from 2,687 unselected patients enrolled in the PROMUS Element Plus post-marketing approval study, a group of mostly white men.
The PLATINUM Diversity trial was sponsored by Boston Scientific. Dr. Batchelor has received research support from and has been a speaker for and consultant to Boston Scientific. He also has been a speaker for and consultant to Abbott Vascular and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com On Twitter @mitchelzoler
WASHINGTON – The relatively low number of women and minority-group patients enrolled into cardiovascular disease clinical trials may skew the results, based on a comparison of outcomes following coronary stenting in an analysis of more than 4,000 patients.
During 12 months following coronary-disease treatment with percutaneous coronary intervention (PCI), women of diverse racial and ethnic backgrounds had a statistically significant 60% relative increase in death and myocardial infarctions, compared with white men, after adjustment for known baseline variables, Wayne B. Batchelor, MD, reported at the Transcatheter Cardiovascular Therapeutics annual meeting.
Minority patients, a mix of women and men, had a 90% relative rise in death and MIs, and a 60% higher rate of MIs after adjustment, both statistically significant differences.
Dr. Batchelor and his associates have not yet analyzed what factors are behind these worse outcomes in women and minority patients. But he suspects social and economic factors may provide at least some explanation, including income, education, language fluency, exercise habits, and access to health care.
“I think the trends we saw are real; the question is what accounts for the differences,” said Dr. Batchelor, an interventional cardiologist in Tallahassee, Fla. Regardless of the causes, he believes that the outcome differences have important immediate messages.
“We need to ensure better representation of women and minorities in clinical trials,” he said in an interview. “We don’t collect enough data from women and minorities. Historically, they have been underrepresented in trials.”
Another lesson is the importance of putting women and minority patients with cardiovascular disease on guideline-directed treatment, including dual antiplatelet therapy, lipid-lowering drugs, and antihypertensive drugs. The results show potential opportunity to further improve outcomes in women and minority patients, Dr. Batchelor said at the meeting, sponsored by the Cardiovascular Research Foundation.
The PLATINUM Diversity trial enrolled 1,501 women and men from minority groups with coronary disease who required PCI at one of 52 U.S. sites. For his analysis, Dr. Batchelor combined the 12-month outcomes of these patients with 12-month data from 2,687 unselected patients enrolled in the PROMUS Element Plus post-marketing approval study, a group of mostly white men.
The PLATINUM Diversity trial was sponsored by Boston Scientific. Dr. Batchelor has received research support from and has been a speaker for and consultant to Boston Scientific. He also has been a speaker for and consultant to Abbott Vascular and Medtronic.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
mzoler@frontlinemedcom.com On Twitter @mitchelzoler
Key clinical point:
Major finding: One year after percutaneous coronary intervention, death or myocardial infarction was 60% higher in women and 90% higher in minorities, compared with white men.
Data source: PLATINUM Diversity, a multicenter, single-arm study with 1,501 patients, and the PROMUS Element Plus U.S. postmarketing approval study with 2,683 patients.
Disclosures: The PLATINUM Diversity trial was sponsored by Boston Scientific. Dr. Batchelor has received research support from and has been a speaker for and consultant to Boston Scientific. He also has been a speaker for and consultant to Abbott Vascular and Medtronic.
Cardiorespiratory fitness improves survival after depression
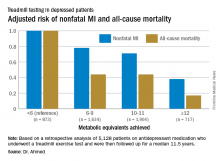
ROME – Cardiorespiratory fitness provided strong and graded protection against all-cause mortality and nonfatal MI in a study of more than 5,000 patients treated for depression, Amjad M. Ahmed, MD, reported at the annual congress of the European Society of Cardiology.
“These results highlight the importance of assessing fitness to identify risk as well as promoting an active lifestyle in patients with depression,” said Dr. Ahmed of Abdulaziz University for Health Sciences in Riyadh, Saudi Arabia.
This analysis focused on the 5,128 subjects who were on antidepressant medication at the time of their treadmill test. Their baseline cardiorespiratory fitness, as estimated by achieved peak metabolic equivalents (METs) on the treadmill, varied inversely with their risks of acute MI and all-cause mortality in the years to come. However, the less fit a patient was, the greater the burden of traditional cardiovascular risk factors. For example, the prevalence of hypertension was 86% in patients who achieved fewer than 6 METs, 75% in those who achieved 6-9 METs, 62% in depressed patients who reached 10-11 METs, and 51% in those who achieved 12 METs or more.
For this reason, Dr. Ahmed and coinvestigators performed a Cox multivariate regression analysis adjusted extensively for potential confounders, including age, sex, race, cardiovascular risk factors, known coronary artery disease, the use of cardiovascular medications, and the reason for the referral for stress testing.
When an achieved MET below 6 was used as the reference standard, for every 1 MET above 6 that patients achieved, their adjusted risk of all-cause mortality decreased by 18%, and the risk of nonfatal MI fell by 8%.
Session cochair Martin Halle, MD, pointed out what he viewed as a major limitation of the study.
“You didn’t follow their physical fitness over time, so you can’t say that increasing their METs would bring a better prognosis,” said Dr. Halle, professor and chairman of the department of preventive and rehabilitative sports medicine at the Technical University of Munich.
Dr. Ahmed reported having no financial conflicts of interest related to the Henry Ford FIT Project.
ROME – Cardiorespiratory fitness provided strong and graded protection against all-cause mortality and nonfatal MI in a study of more than 5,000 patients treated for depression, Amjad M. Ahmed, MD, reported at the annual congress of the European Society of Cardiology.
“These results highlight the importance of assessing fitness to identify risk as well as promoting an active lifestyle in patients with depression,” said Dr. Ahmed of Abdulaziz University for Health Sciences in Riyadh, Saudi Arabia.
This analysis focused on the 5,128 subjects who were on antidepressant medication at the time of their treadmill test. Their baseline cardiorespiratory fitness, as estimated by achieved peak metabolic equivalents (METs) on the treadmill, varied inversely with their risks of acute MI and all-cause mortality in the years to come. However, the less fit a patient was, the greater the burden of traditional cardiovascular risk factors. For example, the prevalence of hypertension was 86% in patients who achieved fewer than 6 METs, 75% in those who achieved 6-9 METs, 62% in depressed patients who reached 10-11 METs, and 51% in those who achieved 12 METs or more.
For this reason, Dr. Ahmed and coinvestigators performed a Cox multivariate regression analysis adjusted extensively for potential confounders, including age, sex, race, cardiovascular risk factors, known coronary artery disease, the use of cardiovascular medications, and the reason for the referral for stress testing.
When an achieved MET below 6 was used as the reference standard, for every 1 MET above 6 that patients achieved, their adjusted risk of all-cause mortality decreased by 18%, and the risk of nonfatal MI fell by 8%.
Session cochair Martin Halle, MD, pointed out what he viewed as a major limitation of the study.
“You didn’t follow their physical fitness over time, so you can’t say that increasing their METs would bring a better prognosis,” said Dr. Halle, professor and chairman of the department of preventive and rehabilitative sports medicine at the Technical University of Munich.
Dr. Ahmed reported having no financial conflicts of interest related to the Henry Ford FIT Project.
ROME – Cardiorespiratory fitness provided strong and graded protection against all-cause mortality and nonfatal MI in a study of more than 5,000 patients treated for depression, Amjad M. Ahmed, MD, reported at the annual congress of the European Society of Cardiology.
“These results highlight the importance of assessing fitness to identify risk as well as promoting an active lifestyle in patients with depression,” said Dr. Ahmed of Abdulaziz University for Health Sciences in Riyadh, Saudi Arabia.
This analysis focused on the 5,128 subjects who were on antidepressant medication at the time of their treadmill test. Their baseline cardiorespiratory fitness, as estimated by achieved peak metabolic equivalents (METs) on the treadmill, varied inversely with their risks of acute MI and all-cause mortality in the years to come. However, the less fit a patient was, the greater the burden of traditional cardiovascular risk factors. For example, the prevalence of hypertension was 86% in patients who achieved fewer than 6 METs, 75% in those who achieved 6-9 METs, 62% in depressed patients who reached 10-11 METs, and 51% in those who achieved 12 METs or more.
For this reason, Dr. Ahmed and coinvestigators performed a Cox multivariate regression analysis adjusted extensively for potential confounders, including age, sex, race, cardiovascular risk factors, known coronary artery disease, the use of cardiovascular medications, and the reason for the referral for stress testing.
When an achieved MET below 6 was used as the reference standard, for every 1 MET above 6 that patients achieved, their adjusted risk of all-cause mortality decreased by 18%, and the risk of nonfatal MI fell by 8%.
Session cochair Martin Halle, MD, pointed out what he viewed as a major limitation of the study.
“You didn’t follow their physical fitness over time, so you can’t say that increasing their METs would bring a better prognosis,” said Dr. Halle, professor and chairman of the department of preventive and rehabilitative sports medicine at the Technical University of Munich.
Dr. Ahmed reported having no financial conflicts of interest related to the Henry Ford FIT Project.
AT THE ESC CONGRESS 2016
Key clinical point:
Major finding: For every 1-MET increase a patient on antidepressant medication achieved above 6 METs during a Bruce protocol treadmill exercise test, the risk of all-cause mortality during the subsequent 11.5 years decreased by an adjusted 18%.
Data source: A retrospective analysis of 5,128 patients on antidepressant medication who underwent a treadmill exercise test as part of the Henry Ford Exercise Testing Project and were then followed up for a median of 11.5 years.
Disclosures: The study presenter reported having no relevant financial conflicts.
Most infective endocarditis calls for early surgery
CHICAGO - Turning to surgery earlier in infective endocarditis may hold the key to a cure for some patients. Upcoming guidelines for surgical treatment of infective endocarditis lend evidence-based support to early surgical intervention in this high-mortality condition.
“Infective endocarditis is the most severe and potentially devastating complication for heart valve disease,” said Joseph Coselli, MD, in a presentation that reviewed current trends in incidence of infective endocarditis (IE) and laid out a rationale and strategy for early surgical intervention in some patients.
“Untreated infective endocarditis is universally fatal,” said Dr. Coselli. Even with current treatments, however, overall mortality for infective endocarditis is 20%-25%, he said.
Speaking at the joint AATS-ACC Heart Valve Summit, Dr. Coselli, chief of the division of cardiothoracic surgery at Baylor College of Medicine, Houston, reviewed the key points in the upcoming guideline and the evidence that backs up the guidelines.
Dr. Coselli served on the writing committee for the 2016 AATS consensus guidelines for the surgical treatment of infective endocarditis; the guidelines are currently in press.
The guidelines propose that “at the time of surgery, the patient should be on an effective antimicrobial regimen to which the causative agent is sensitive,” he said. This is a level I recommendation, as is the recommendation that the surgeon should understand the pathology as well as possible before the procedure. Usually, say the guidelines, this is obtained by means of a transesophageal echocardiogram (TEE), assigning level I status to this recommendation as well.
According to the guidelines, patients with IE who may be surgical candidates during their hospitalization, regardless of whether their antimicrobial course is complete, include those who present with valve dysfunction that results in symptoms of heart failure. Surgery should also be considered in patients with left-sided IE with S. aureus, fungi, or other highly resistant organisms as the causative pathogen. If heart block, an aortic or annular abscess, or destructive penetrating lesions are present, surgery is also indicated. Finally, the guidelines recommend considering surgery if patients have persistent bacteremia or fevers at 5 to 7 days after initiation of appropriate antimicrobial therapy. All of these are class I indications in the upcoming guidelines, he said.
The patient who has relapsing infection, defined by the guidelines as recurrent bacteremia “after a complete course of appropriate antibiotics and subsequently negative blood culture,” who has no other identifiable source of infection, may also be a candidate.
Given the dearth of randomized trials in the area, no recommendation for intervention is backed by a level of evidence greater than B, said Dr. Coselli. And knowledge gaps persist in many areas, such as the appropriate timing of surgery in IE when there are neurological complications. Also, he said, “embolism risk needs to be better understood.” Imaging improvements would help guide decision-making, as would better data about contemporary rates of IE relapse and recurrence, said Dr. Coselli.
Though these surgeries should be done at centers that can field a complete team, and by experience valve surgeons, early intervention may be a key to success: “Operate before a devastating complication occurs,” said Dr. Coselli. “Understand what you see; don’t be afraid of radical debridement, and master alternative options to reconstruction” depending on the heart’s appearance in the OR, he said.
Surgeons can run into trouble in IE cases if they wait too long. “A patient who’s already had an embolic stroke may be too sick,” said Dr. Coselli. Insensitive organisms and ineffective antimicrobial therapy set the patient up for recurrent IE or treatment failure as well.
Having guidance for surgical intervention is important because cardiologists and surgeons will be seeing more infective endocarditis patients as heroin and other illicit intravenous drug use continues to rise, said Dr. Coselli. IE in intravenous drug users now accounts for up to 30% of all patients who seek treatment for IE, he said, citing a study that tracked characteristics of endocarditis patients undergoing surgery at a single institution from 2002-2014 (J Thorac Cardiovasc Surg. 2016 Sep;152:832-41). Incidence in intravenous drug users can range to 2,000 cases per 100,000 patient-years, he said.
The study, conducted by Joon Bum Kim, MD, PhD, and his colleagues at Massachusetts General and Brigham and Women’s hospitals, both in Boston, followed 436 patients with IE, 78 of whom were intravenous drug users (IVDUs) at the time of diagnosis. Overall, the IVDUs were younger (mean age, 36 plus or minus 10 years) when compared with the non-IVDU group (mean age, 58 plus or minus 14 years; P less than 0.001). The non-IVDU cohort were also significantly more likely to have hypertension and diabetes, but less likely to smoke. However, IVDUs were more likely to have embolic events, and to have right-sided valve involvement.
Though early mortality was better in the IVDU group post-surgically, late complications, including reinfection and reoperation, were significantly more likely to occur in the IVDUs, with reinfection more than four times as frequent in IVDUs (aggregate valve-related complications, 41% in IVDUs vs. 10% in non-IVDUs; P = 0.001).
Despite the additional morbidity seen in IVDU-associated endocarditis, the 10-year survival rate was virtually identical between the two groups.
For many IE patients, said Dr. Coselli, “the arguments against surgery have lost strength.” Active systemic infections are treatable, sicker patients can be operated on earlier, and surgeons will gain experience with this sometimes technically challenging surgery, he said. Finally, Dr. Coselli said, even though the best available data support early surgical intervention in select IE patients, “final cure of IE is always the result of antimicrobial treatment and the patient’s own defense.”
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO - Turning to surgery earlier in infective endocarditis may hold the key to a cure for some patients. Upcoming guidelines for surgical treatment of infective endocarditis lend evidence-based support to early surgical intervention in this high-mortality condition.
“Infective endocarditis is the most severe and potentially devastating complication for heart valve disease,” said Joseph Coselli, MD, in a presentation that reviewed current trends in incidence of infective endocarditis (IE) and laid out a rationale and strategy for early surgical intervention in some patients.
“Untreated infective endocarditis is universally fatal,” said Dr. Coselli. Even with current treatments, however, overall mortality for infective endocarditis is 20%-25%, he said.
Speaking at the joint AATS-ACC Heart Valve Summit, Dr. Coselli, chief of the division of cardiothoracic surgery at Baylor College of Medicine, Houston, reviewed the key points in the upcoming guideline and the evidence that backs up the guidelines.
Dr. Coselli served on the writing committee for the 2016 AATS consensus guidelines for the surgical treatment of infective endocarditis; the guidelines are currently in press.
The guidelines propose that “at the time of surgery, the patient should be on an effective antimicrobial regimen to which the causative agent is sensitive,” he said. This is a level I recommendation, as is the recommendation that the surgeon should understand the pathology as well as possible before the procedure. Usually, say the guidelines, this is obtained by means of a transesophageal echocardiogram (TEE), assigning level I status to this recommendation as well.
According to the guidelines, patients with IE who may be surgical candidates during their hospitalization, regardless of whether their antimicrobial course is complete, include those who present with valve dysfunction that results in symptoms of heart failure. Surgery should also be considered in patients with left-sided IE with S. aureus, fungi, or other highly resistant organisms as the causative pathogen. If heart block, an aortic or annular abscess, or destructive penetrating lesions are present, surgery is also indicated. Finally, the guidelines recommend considering surgery if patients have persistent bacteremia or fevers at 5 to 7 days after initiation of appropriate antimicrobial therapy. All of these are class I indications in the upcoming guidelines, he said.
The patient who has relapsing infection, defined by the guidelines as recurrent bacteremia “after a complete course of appropriate antibiotics and subsequently negative blood culture,” who has no other identifiable source of infection, may also be a candidate.
Given the dearth of randomized trials in the area, no recommendation for intervention is backed by a level of evidence greater than B, said Dr. Coselli. And knowledge gaps persist in many areas, such as the appropriate timing of surgery in IE when there are neurological complications. Also, he said, “embolism risk needs to be better understood.” Imaging improvements would help guide decision-making, as would better data about contemporary rates of IE relapse and recurrence, said Dr. Coselli.
Though these surgeries should be done at centers that can field a complete team, and by experience valve surgeons, early intervention may be a key to success: “Operate before a devastating complication occurs,” said Dr. Coselli. “Understand what you see; don’t be afraid of radical debridement, and master alternative options to reconstruction” depending on the heart’s appearance in the OR, he said.
Surgeons can run into trouble in IE cases if they wait too long. “A patient who’s already had an embolic stroke may be too sick,” said Dr. Coselli. Insensitive organisms and ineffective antimicrobial therapy set the patient up for recurrent IE or treatment failure as well.
Having guidance for surgical intervention is important because cardiologists and surgeons will be seeing more infective endocarditis patients as heroin and other illicit intravenous drug use continues to rise, said Dr. Coselli. IE in intravenous drug users now accounts for up to 30% of all patients who seek treatment for IE, he said, citing a study that tracked characteristics of endocarditis patients undergoing surgery at a single institution from 2002-2014 (J Thorac Cardiovasc Surg. 2016 Sep;152:832-41). Incidence in intravenous drug users can range to 2,000 cases per 100,000 patient-years, he said.
The study, conducted by Joon Bum Kim, MD, PhD, and his colleagues at Massachusetts General and Brigham and Women’s hospitals, both in Boston, followed 436 patients with IE, 78 of whom were intravenous drug users (IVDUs) at the time of diagnosis. Overall, the IVDUs were younger (mean age, 36 plus or minus 10 years) when compared with the non-IVDU group (mean age, 58 plus or minus 14 years; P less than 0.001). The non-IVDU cohort were also significantly more likely to have hypertension and diabetes, but less likely to smoke. However, IVDUs were more likely to have embolic events, and to have right-sided valve involvement.
Though early mortality was better in the IVDU group post-surgically, late complications, including reinfection and reoperation, were significantly more likely to occur in the IVDUs, with reinfection more than four times as frequent in IVDUs (aggregate valve-related complications, 41% in IVDUs vs. 10% in non-IVDUs; P = 0.001).
Despite the additional morbidity seen in IVDU-associated endocarditis, the 10-year survival rate was virtually identical between the two groups.
For many IE patients, said Dr. Coselli, “the arguments against surgery have lost strength.” Active systemic infections are treatable, sicker patients can be operated on earlier, and surgeons will gain experience with this sometimes technically challenging surgery, he said. Finally, Dr. Coselli said, even though the best available data support early surgical intervention in select IE patients, “final cure of IE is always the result of antimicrobial treatment and the patient’s own defense.”
koakes@frontlinemedcom.com
On Twitter @karioakes
CHICAGO - Turning to surgery earlier in infective endocarditis may hold the key to a cure for some patients. Upcoming guidelines for surgical treatment of infective endocarditis lend evidence-based support to early surgical intervention in this high-mortality condition.
“Infective endocarditis is the most severe and potentially devastating complication for heart valve disease,” said Joseph Coselli, MD, in a presentation that reviewed current trends in incidence of infective endocarditis (IE) and laid out a rationale and strategy for early surgical intervention in some patients.
“Untreated infective endocarditis is universally fatal,” said Dr. Coselli. Even with current treatments, however, overall mortality for infective endocarditis is 20%-25%, he said.
Speaking at the joint AATS-ACC Heart Valve Summit, Dr. Coselli, chief of the division of cardiothoracic surgery at Baylor College of Medicine, Houston, reviewed the key points in the upcoming guideline and the evidence that backs up the guidelines.
Dr. Coselli served on the writing committee for the 2016 AATS consensus guidelines for the surgical treatment of infective endocarditis; the guidelines are currently in press.
The guidelines propose that “at the time of surgery, the patient should be on an effective antimicrobial regimen to which the causative agent is sensitive,” he said. This is a level I recommendation, as is the recommendation that the surgeon should understand the pathology as well as possible before the procedure. Usually, say the guidelines, this is obtained by means of a transesophageal echocardiogram (TEE), assigning level I status to this recommendation as well.
According to the guidelines, patients with IE who may be surgical candidates during their hospitalization, regardless of whether their antimicrobial course is complete, include those who present with valve dysfunction that results in symptoms of heart failure. Surgery should also be considered in patients with left-sided IE with S. aureus, fungi, or other highly resistant organisms as the causative pathogen. If heart block, an aortic or annular abscess, or destructive penetrating lesions are present, surgery is also indicated. Finally, the guidelines recommend considering surgery if patients have persistent bacteremia or fevers at 5 to 7 days after initiation of appropriate antimicrobial therapy. All of these are class I indications in the upcoming guidelines, he said.
The patient who has relapsing infection, defined by the guidelines as recurrent bacteremia “after a complete course of appropriate antibiotics and subsequently negative blood culture,” who has no other identifiable source of infection, may also be a candidate.
Given the dearth of randomized trials in the area, no recommendation for intervention is backed by a level of evidence greater than B, said Dr. Coselli. And knowledge gaps persist in many areas, such as the appropriate timing of surgery in IE when there are neurological complications. Also, he said, “embolism risk needs to be better understood.” Imaging improvements would help guide decision-making, as would better data about contemporary rates of IE relapse and recurrence, said Dr. Coselli.
Though these surgeries should be done at centers that can field a complete team, and by experience valve surgeons, early intervention may be a key to success: “Operate before a devastating complication occurs,” said Dr. Coselli. “Understand what you see; don’t be afraid of radical debridement, and master alternative options to reconstruction” depending on the heart’s appearance in the OR, he said.
Surgeons can run into trouble in IE cases if they wait too long. “A patient who’s already had an embolic stroke may be too sick,” said Dr. Coselli. Insensitive organisms and ineffective antimicrobial therapy set the patient up for recurrent IE or treatment failure as well.
Having guidance for surgical intervention is important because cardiologists and surgeons will be seeing more infective endocarditis patients as heroin and other illicit intravenous drug use continues to rise, said Dr. Coselli. IE in intravenous drug users now accounts for up to 30% of all patients who seek treatment for IE, he said, citing a study that tracked characteristics of endocarditis patients undergoing surgery at a single institution from 2002-2014 (J Thorac Cardiovasc Surg. 2016 Sep;152:832-41). Incidence in intravenous drug users can range to 2,000 cases per 100,000 patient-years, he said.
The study, conducted by Joon Bum Kim, MD, PhD, and his colleagues at Massachusetts General and Brigham and Women’s hospitals, both in Boston, followed 436 patients with IE, 78 of whom were intravenous drug users (IVDUs) at the time of diagnosis. Overall, the IVDUs were younger (mean age, 36 plus or minus 10 years) when compared with the non-IVDU group (mean age, 58 plus or minus 14 years; P less than 0.001). The non-IVDU cohort were also significantly more likely to have hypertension and diabetes, but less likely to smoke. However, IVDUs were more likely to have embolic events, and to have right-sided valve involvement.
Though early mortality was better in the IVDU group post-surgically, late complications, including reinfection and reoperation, were significantly more likely to occur in the IVDUs, with reinfection more than four times as frequent in IVDUs (aggregate valve-related complications, 41% in IVDUs vs. 10% in non-IVDUs; P = 0.001).
Despite the additional morbidity seen in IVDU-associated endocarditis, the 10-year survival rate was virtually identical between the two groups.
For many IE patients, said Dr. Coselli, “the arguments against surgery have lost strength.” Active systemic infections are treatable, sicker patients can be operated on earlier, and surgeons will gain experience with this sometimes technically challenging surgery, he said. Finally, Dr. Coselli said, even though the best available data support early surgical intervention in select IE patients, “final cure of IE is always the result of antimicrobial treatment and the patient’s own defense.”
koakes@frontlinemedcom.com
On Twitter @karioakes
EXPERT ANALYSIS FROM THE HEART VALVE SUMMIT 2016
Cancer type, age at time of diagnosis implicated in risk of CVD-related deaths
Survivorship data derived from a U.K. cancer registry make it possible to more closely pinpoint the risk of cardiovascular disease in patients treated for cancer as adolescents and young adults.
Researchers report that 6% of the 2,016 deaths occurring in 200,945 cancer survivors diagnosed between the ages of 15 and 39 years were directly related to cardiovascular disease. A multivariable Poisson regression analysis of data from the Teenage and Young Adult Cancer Survivor Study also showed that survivors who were diagnosed between the ages of 15 and 19 years had 4.2 times the risk (95% confidence interval, 3.4-5.2) of death from cardiovascular disease, compared with their peers in the general population. But for survivors who were aged 35-39 years when diagnosed, that risk decreased to 1.2 times (95% CI, 1.1-1.3) that of their general population peers (P less than .0001). The standardized mortality ratios and absolute excess risks for ischemic heart disease, valvular heart disease, and cardiomyopathy were similar (Circulation. 2016;134:1521-33).
The findings should help clinicians craft more effective after-cancer care, according to Mike Hawkins, DPhil. “It helps them focus the most intensive follow-up care on those most at risk,” Dr. Hawkins, an epidemiology professor and director of the Centre for Childhood Cancer Survivor Studies at the University of Birmingham (England), said in a statement. “It is important for survivors because it empowers them by providing them with their long-term chances of a specific side effect of cancer treatment.”
The most significant relationship between cardiovascular disease and cancer occurred in those diagnosed with Hodgkin lymphoma, and at an earlier age. Overall, Hodgkin lymphoma survivors had a 3.8 times higher risk of cardiovascular disease–related death than their peers not diagnosed with any cancer. In those diagnosed at age 15-19 years, 6.9% had died from cardiovascular disease by age 55 years, compared with 2% of those who’d been diagnosed at age 35-39 years. Among these two age groups in the general population, fewer than 1% typically die from cardiovascular disease–related deaths. In Hodgkin lymphoma survivors aged 60 years or older, 27.5% of excess deaths were from cardiovascular disease.
Although not stratified by treatment, the study includes risk estimates for other cancers diagnosed in the teen and young adult years, stratified by the age at diagnosis, something the authors of the study noted is “a considerable advance on previous knowledge.”
Survivors of all age groups in the cohort diagnosed with a variety of cancers experienced a greater risk of death from heart disease, compared with their peers in the general population.
Survivorship data derived from a U.K. cancer registry make it possible to more closely pinpoint the risk of cardiovascular disease in patients treated for cancer as adolescents and young adults.
Researchers report that 6% of the 2,016 deaths occurring in 200,945 cancer survivors diagnosed between the ages of 15 and 39 years were directly related to cardiovascular disease. A multivariable Poisson regression analysis of data from the Teenage and Young Adult Cancer Survivor Study also showed that survivors who were diagnosed between the ages of 15 and 19 years had 4.2 times the risk (95% confidence interval, 3.4-5.2) of death from cardiovascular disease, compared with their peers in the general population. But for survivors who were aged 35-39 years when diagnosed, that risk decreased to 1.2 times (95% CI, 1.1-1.3) that of their general population peers (P less than .0001). The standardized mortality ratios and absolute excess risks for ischemic heart disease, valvular heart disease, and cardiomyopathy were similar (Circulation. 2016;134:1521-33).
The findings should help clinicians craft more effective after-cancer care, according to Mike Hawkins, DPhil. “It helps them focus the most intensive follow-up care on those most at risk,” Dr. Hawkins, an epidemiology professor and director of the Centre for Childhood Cancer Survivor Studies at the University of Birmingham (England), said in a statement. “It is important for survivors because it empowers them by providing them with their long-term chances of a specific side effect of cancer treatment.”
The most significant relationship between cardiovascular disease and cancer occurred in those diagnosed with Hodgkin lymphoma, and at an earlier age. Overall, Hodgkin lymphoma survivors had a 3.8 times higher risk of cardiovascular disease–related death than their peers not diagnosed with any cancer. In those diagnosed at age 15-19 years, 6.9% had died from cardiovascular disease by age 55 years, compared with 2% of those who’d been diagnosed at age 35-39 years. Among these two age groups in the general population, fewer than 1% typically die from cardiovascular disease–related deaths. In Hodgkin lymphoma survivors aged 60 years or older, 27.5% of excess deaths were from cardiovascular disease.
Although not stratified by treatment, the study includes risk estimates for other cancers diagnosed in the teen and young adult years, stratified by the age at diagnosis, something the authors of the study noted is “a considerable advance on previous knowledge.”
Survivors of all age groups in the cohort diagnosed with a variety of cancers experienced a greater risk of death from heart disease, compared with their peers in the general population.
Survivorship data derived from a U.K. cancer registry make it possible to more closely pinpoint the risk of cardiovascular disease in patients treated for cancer as adolescents and young adults.
Researchers report that 6% of the 2,016 deaths occurring in 200,945 cancer survivors diagnosed between the ages of 15 and 39 years were directly related to cardiovascular disease. A multivariable Poisson regression analysis of data from the Teenage and Young Adult Cancer Survivor Study also showed that survivors who were diagnosed between the ages of 15 and 19 years had 4.2 times the risk (95% confidence interval, 3.4-5.2) of death from cardiovascular disease, compared with their peers in the general population. But for survivors who were aged 35-39 years when diagnosed, that risk decreased to 1.2 times (95% CI, 1.1-1.3) that of their general population peers (P less than .0001). The standardized mortality ratios and absolute excess risks for ischemic heart disease, valvular heart disease, and cardiomyopathy were similar (Circulation. 2016;134:1521-33).
The findings should help clinicians craft more effective after-cancer care, according to Mike Hawkins, DPhil. “It helps them focus the most intensive follow-up care on those most at risk,” Dr. Hawkins, an epidemiology professor and director of the Centre for Childhood Cancer Survivor Studies at the University of Birmingham (England), said in a statement. “It is important for survivors because it empowers them by providing them with their long-term chances of a specific side effect of cancer treatment.”
The most significant relationship between cardiovascular disease and cancer occurred in those diagnosed with Hodgkin lymphoma, and at an earlier age. Overall, Hodgkin lymphoma survivors had a 3.8 times higher risk of cardiovascular disease–related death than their peers not diagnosed with any cancer. In those diagnosed at age 15-19 years, 6.9% had died from cardiovascular disease by age 55 years, compared with 2% of those who’d been diagnosed at age 35-39 years. Among these two age groups in the general population, fewer than 1% typically die from cardiovascular disease–related deaths. In Hodgkin lymphoma survivors aged 60 years or older, 27.5% of excess deaths were from cardiovascular disease.
Although not stratified by treatment, the study includes risk estimates for other cancers diagnosed in the teen and young adult years, stratified by the age at diagnosis, something the authors of the study noted is “a considerable advance on previous knowledge.”
Survivors of all age groups in the cohort diagnosed with a variety of cancers experienced a greater risk of death from heart disease, compared with their peers in the general population.
FROM CIRCULATION
Key clinical point:
Major finding: Cancer survivors who were diagnosed at age 15-19 years had 4.2 times the risk of death from cardiovascular disease than did their peers in the general population.
Data source: A U.K. cancer registry of 200,945 persons between 15 and 39 years at time of diagnosis.
Disclosures: This study was supported by the National Institute for Health Research in the United Kingdom. The authors had no relevant disclosures.
Mitral valve disease often missed in pulmonary hypertension
LOS ANGELES – Dyspnea in pulmonary hypertension is caused by mitral valve disease until proven otherwise, according to Paul Forfia, MD, director of pulmonary hypertension, right heart failure, and pulmonary thromboendarterectomy at Temple University, Philadelphia.
Although mitral valve disease is a well-recognized cause of pulmonary hypertension, its significance is often underestimated in practice.
“Whether the valve is regurgitant or stenotic makes absolutely no difference. When you delay” repair or replacement, “the patient keeps getting sicker,” he said. In time, “everyone is standing around wringing their hands going, ‘Oh my god, what are we going to do? Are you serious? Fix the valve.’ We see this type of patient a couple times a month,” Dr. Forfia said at the American College of Chest Physicians annual meeting.
“I have seen lifesaving mitral valve surgery put off for many years in patients with pulmonary hypertension, when all they needed was to have their valve fixed,” he said.
Whatever the case, pulmonologists who want the valve fixed often end up playing patient ping pong with cardiologists who want the hypertension controlled beforehand, but “if I treat the pulmonary circulation first, all I am going to do is unmask the left heart failure. There will be no functional improvement whatsoever,” Dr. Forfia said.
Surgery is the best solution as long as patients are well enough to recover. “With pulmonary hypertension in the setting of severe mitral valve regurgitation or stenosis, whether the pulmonary hypertension is related to passive left heart congestion or associated with pulmonary arteriopathy, the only sensible option is to correct the underlying valvular abnormality,” he said. The surgery should be done at an institution capable of managing postop pulmonary arteriopathy, if present.
The ping pong solution is to send patients to an expert pulmonology center; the mitral valve problem will be spotted right away.
“There is no pulmonary pressure cutoff that should prohibit surgery” in patients able to recover. “There is no such thing as a pulmonary artery pressure too high to be explained by mitral valve disease. The pulmonary pressure can be as high as it wants to be. You will get nowhere by thinking the pressure is too high to address the valve,” Dr. Forfia said.
Often “you hear, ‘I’m afraid the person is going to die on the table.’ I always say ‘if the patient is not going to die on the table, they are going to die in their living room of progressive heart failure because you [didn’t] fix their valve. I have never had a patient with pulmonary hypertension not separate from cardiopulmonary bypass. It’s a myth,” he said.
When there’s a “question if the dyspnea is coming from the mitral valve, we routinely use exercise right heart catheterization to probe the situation. We have a recumbent bike in the cath lab. You’ll often provoke significant left heart congestion with a low workload. It’s very revealing to the significance of mitral valve disease,” he said.
Aortic valve disease is also missed in pulmonary hypertension. “It’s not [a] similar” problem; “it’s the same” problem, Dr. Forfia said.
Dr. Forfia is a consultant for Bayer, Actelion, and United Therapeutics.
LOS ANGELES – Dyspnea in pulmonary hypertension is caused by mitral valve disease until proven otherwise, according to Paul Forfia, MD, director of pulmonary hypertension, right heart failure, and pulmonary thromboendarterectomy at Temple University, Philadelphia.
Although mitral valve disease is a well-recognized cause of pulmonary hypertension, its significance is often underestimated in practice.
“Whether the valve is regurgitant or stenotic makes absolutely no difference. When you delay” repair or replacement, “the patient keeps getting sicker,” he said. In time, “everyone is standing around wringing their hands going, ‘Oh my god, what are we going to do? Are you serious? Fix the valve.’ We see this type of patient a couple times a month,” Dr. Forfia said at the American College of Chest Physicians annual meeting.
“I have seen lifesaving mitral valve surgery put off for many years in patients with pulmonary hypertension, when all they needed was to have their valve fixed,” he said.
Whatever the case, pulmonologists who want the valve fixed often end up playing patient ping pong with cardiologists who want the hypertension controlled beforehand, but “if I treat the pulmonary circulation first, all I am going to do is unmask the left heart failure. There will be no functional improvement whatsoever,” Dr. Forfia said.
Surgery is the best solution as long as patients are well enough to recover. “With pulmonary hypertension in the setting of severe mitral valve regurgitation or stenosis, whether the pulmonary hypertension is related to passive left heart congestion or associated with pulmonary arteriopathy, the only sensible option is to correct the underlying valvular abnormality,” he said. The surgery should be done at an institution capable of managing postop pulmonary arteriopathy, if present.
The ping pong solution is to send patients to an expert pulmonology center; the mitral valve problem will be spotted right away.
“There is no pulmonary pressure cutoff that should prohibit surgery” in patients able to recover. “There is no such thing as a pulmonary artery pressure too high to be explained by mitral valve disease. The pulmonary pressure can be as high as it wants to be. You will get nowhere by thinking the pressure is too high to address the valve,” Dr. Forfia said.
Often “you hear, ‘I’m afraid the person is going to die on the table.’ I always say ‘if the patient is not going to die on the table, they are going to die in their living room of progressive heart failure because you [didn’t] fix their valve. I have never had a patient with pulmonary hypertension not separate from cardiopulmonary bypass. It’s a myth,” he said.
When there’s a “question if the dyspnea is coming from the mitral valve, we routinely use exercise right heart catheterization to probe the situation. We have a recumbent bike in the cath lab. You’ll often provoke significant left heart congestion with a low workload. It’s very revealing to the significance of mitral valve disease,” he said.
Aortic valve disease is also missed in pulmonary hypertension. “It’s not [a] similar” problem; “it’s the same” problem, Dr. Forfia said.
Dr. Forfia is a consultant for Bayer, Actelion, and United Therapeutics.
LOS ANGELES – Dyspnea in pulmonary hypertension is caused by mitral valve disease until proven otherwise, according to Paul Forfia, MD, director of pulmonary hypertension, right heart failure, and pulmonary thromboendarterectomy at Temple University, Philadelphia.
Although mitral valve disease is a well-recognized cause of pulmonary hypertension, its significance is often underestimated in practice.
“Whether the valve is regurgitant or stenotic makes absolutely no difference. When you delay” repair or replacement, “the patient keeps getting sicker,” he said. In time, “everyone is standing around wringing their hands going, ‘Oh my god, what are we going to do? Are you serious? Fix the valve.’ We see this type of patient a couple times a month,” Dr. Forfia said at the American College of Chest Physicians annual meeting.
“I have seen lifesaving mitral valve surgery put off for many years in patients with pulmonary hypertension, when all they needed was to have their valve fixed,” he said.
Whatever the case, pulmonologists who want the valve fixed often end up playing patient ping pong with cardiologists who want the hypertension controlled beforehand, but “if I treat the pulmonary circulation first, all I am going to do is unmask the left heart failure. There will be no functional improvement whatsoever,” Dr. Forfia said.
Surgery is the best solution as long as patients are well enough to recover. “With pulmonary hypertension in the setting of severe mitral valve regurgitation or stenosis, whether the pulmonary hypertension is related to passive left heart congestion or associated with pulmonary arteriopathy, the only sensible option is to correct the underlying valvular abnormality,” he said. The surgery should be done at an institution capable of managing postop pulmonary arteriopathy, if present.
The ping pong solution is to send patients to an expert pulmonology center; the mitral valve problem will be spotted right away.
“There is no pulmonary pressure cutoff that should prohibit surgery” in patients able to recover. “There is no such thing as a pulmonary artery pressure too high to be explained by mitral valve disease. The pulmonary pressure can be as high as it wants to be. You will get nowhere by thinking the pressure is too high to address the valve,” Dr. Forfia said.
Often “you hear, ‘I’m afraid the person is going to die on the table.’ I always say ‘if the patient is not going to die on the table, they are going to die in their living room of progressive heart failure because you [didn’t] fix their valve. I have never had a patient with pulmonary hypertension not separate from cardiopulmonary bypass. It’s a myth,” he said.
When there’s a “question if the dyspnea is coming from the mitral valve, we routinely use exercise right heart catheterization to probe the situation. We have a recumbent bike in the cath lab. You’ll often provoke significant left heart congestion with a low workload. It’s very revealing to the significance of mitral valve disease,” he said.
Aortic valve disease is also missed in pulmonary hypertension. “It’s not [a] similar” problem; “it’s the same” problem, Dr. Forfia said.
Dr. Forfia is a consultant for Bayer, Actelion, and United Therapeutics.
EXPERT ANALYSIS FROM CHEST 2016
Heart failure targets African Americans
ORLANDO – The disparity in U.S. heart failure incidence continued undiminished during 2002-2013, with African Americans maintaining a steady 2.3-fold increased rate of heart failure, compared with whites, based on national levels of heart failure hospitalizations, a reasonable surrogate for incidence rates, Boback Ziaeian, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
The same period also showed a substantial relative improvement in the heart failure hospitalization rates among U.S. Hispanics, compared with whites, so that, by 2013, the ethnic disparity seen in 2002 between Hispanics and whites largely disappeared, reported Dr. Ziaeian, a cardiologist at the University of California, Los Angeles. The data he analyzed also showed that Asian Americans had the lowest heart failure hospitalization rates of any racial or ethnic group throughout the 11-year period, and that the incidence of heart failure fell more sharply in women than in men during the period, based on the hospitalization numbers.
Age-adjusted heart failure hospitalizations among whites dropped by 30%, and among African Americans by a nearly identical 29%. But this maintained a greater than twofold disparity in rates between the two groups. Among whites, the rate per 100,000 fell from 448 to 315; among African Americans, it dropped from 1,048 to 741. In 2013, the rate of heart failure hospitalizations was 2.4-fold higher in African Americans, compared with whites.
Heart failure hospitalizations fell among Hispanics from 650 per 100,000 to 337 per 100,000 in 2013, a 48% drop that brought the rate among Hispanics to nearly the same as among whites. Asian Americans remained the group with the least heart failure throughout the period, falling from 343 hospitalizations per 100,000 in 2002 to 181 per 100,000 in 2013, a 47% drop.
Among women, the age-adjusted rate per 100,000 fell from 486 to 311, a 36% drop, compared with a decrease from 582 to 431 per 100,000 in men, a 26% reduction. Lower incidence in women may reflect better risk factor control during the study period, compared with men, such as a higher rate of quiting smoking and better treatment compliance, Dr. Ziaeian suggested.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ORLANDO – The disparity in U.S. heart failure incidence continued undiminished during 2002-2013, with African Americans maintaining a steady 2.3-fold increased rate of heart failure, compared with whites, based on national levels of heart failure hospitalizations, a reasonable surrogate for incidence rates, Boback Ziaeian, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
The same period also showed a substantial relative improvement in the heart failure hospitalization rates among U.S. Hispanics, compared with whites, so that, by 2013, the ethnic disparity seen in 2002 between Hispanics and whites largely disappeared, reported Dr. Ziaeian, a cardiologist at the University of California, Los Angeles. The data he analyzed also showed that Asian Americans had the lowest heart failure hospitalization rates of any racial or ethnic group throughout the 11-year period, and that the incidence of heart failure fell more sharply in women than in men during the period, based on the hospitalization numbers.
Age-adjusted heart failure hospitalizations among whites dropped by 30%, and among African Americans by a nearly identical 29%. But this maintained a greater than twofold disparity in rates between the two groups. Among whites, the rate per 100,000 fell from 448 to 315; among African Americans, it dropped from 1,048 to 741. In 2013, the rate of heart failure hospitalizations was 2.4-fold higher in African Americans, compared with whites.
Heart failure hospitalizations fell among Hispanics from 650 per 100,000 to 337 per 100,000 in 2013, a 48% drop that brought the rate among Hispanics to nearly the same as among whites. Asian Americans remained the group with the least heart failure throughout the period, falling from 343 hospitalizations per 100,000 in 2002 to 181 per 100,000 in 2013, a 47% drop.
Among women, the age-adjusted rate per 100,000 fell from 486 to 311, a 36% drop, compared with a decrease from 582 to 431 per 100,000 in men, a 26% reduction. Lower incidence in women may reflect better risk factor control during the study period, compared with men, such as a higher rate of quiting smoking and better treatment compliance, Dr. Ziaeian suggested.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
ORLANDO – The disparity in U.S. heart failure incidence continued undiminished during 2002-2013, with African Americans maintaining a steady 2.3-fold increased rate of heart failure, compared with whites, based on national levels of heart failure hospitalizations, a reasonable surrogate for incidence rates, Boback Ziaeian, MD, reported at the annual scientific meeting of the Heart Failure Society of America.
The same period also showed a substantial relative improvement in the heart failure hospitalization rates among U.S. Hispanics, compared with whites, so that, by 2013, the ethnic disparity seen in 2002 between Hispanics and whites largely disappeared, reported Dr. Ziaeian, a cardiologist at the University of California, Los Angeles. The data he analyzed also showed that Asian Americans had the lowest heart failure hospitalization rates of any racial or ethnic group throughout the 11-year period, and that the incidence of heart failure fell more sharply in women than in men during the period, based on the hospitalization numbers.
Age-adjusted heart failure hospitalizations among whites dropped by 30%, and among African Americans by a nearly identical 29%. But this maintained a greater than twofold disparity in rates between the two groups. Among whites, the rate per 100,000 fell from 448 to 315; among African Americans, it dropped from 1,048 to 741. In 2013, the rate of heart failure hospitalizations was 2.4-fold higher in African Americans, compared with whites.
Heart failure hospitalizations fell among Hispanics from 650 per 100,000 to 337 per 100,000 in 2013, a 48% drop that brought the rate among Hispanics to nearly the same as among whites. Asian Americans remained the group with the least heart failure throughout the period, falling from 343 hospitalizations per 100,000 in 2002 to 181 per 100,000 in 2013, a 47% drop.
Among women, the age-adjusted rate per 100,000 fell from 486 to 311, a 36% drop, compared with a decrease from 582 to 431 per 100,000 in men, a 26% reduction. Lower incidence in women may reflect better risk factor control during the study period, compared with men, such as a higher rate of quiting smoking and better treatment compliance, Dr. Ziaeian suggested.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE HFSA ANNUAL SCIENTIFIC MEETING
Key clinical point:
Major finding: In 2013, age-adjusted heart failure hospitalization was 741/100,000 in African Americans and 315/100,000 in whites.
Data source: The National Inpatient Sample and U.S. Census data.
Disclosures: Dr. Ziaeian had no disclosures.
‘Excellent’ real-world experience with LAA closure device
A device that closes the left atrial appendage to prevent stroke in patients with nonvalvular atrial fibrillation showed a 95.6% procedural success rate in a study of real-world experience since it was approved by the FDA in 2015, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
The study was based on data collected by Boston Scientific, the manufacturer of the Watchman device, regarding 3,822 consecutive patients who underwent the implantation during a 14-month period. The “excellent” procedural success rate, together with low short-term complication rates, are especially “remarkable” because 71% of the interventional cardiologists and electrophysiologists who performed these procedures had no experience with the device prior to FDA approval, said Vivek Y. Reddy, MD, of Mount Sinai Medical Center, New York.
For this study, the implantations were done by 382 physicians at 169 U.S. medical centers. A total of 3,653 procedures were successful. The median duration of the implantation was “an acceptable” 50 minutes (range, 10-210 minutes), and an average of 1.38 devices (range, 1-6) were required per patient. In 23% of cases, a “partial recapture” of a device was necessary to reposition it (J Am Coll Cardiol. 2016 Nov. doi: 10.1016/j.jacc.2016.10.010).
The rates of major complications within 1 week – pericardial tamponade (<1%), procedure-related stroke (0.08%), and mortality (0.08%) – were characterized as “favorable.”
The most common complication was pericardial effusion requiring intervention, which developed in 39 patients (1.02%). The effusions were drained percutaneously in most (24) of these patients. Another 11 patients (0.29%) developed mild pericardial effusions requiring only conservative management.
Three strokes, two ischemic and one hemorrhagic, were deemed related to the procedure, though the hemorrhagic bleed may have resulted chiefly from anticoagulation medications. Three deaths were judged to be related to the procedure: All were secondary to pericardial tamponade associated with perforation by the device.
“It is worth comparing [this] cardiac tamponade rate with [that of] another left atrial cardiovascular procedure, catheter ablation of atrial fibrillation,” Dr. Reddy noted.
A worldwide survey of more than 20,000 catheter ablations reported a pericardial tamponade rate of 1.31%, and another study of more than 93,000 ablation procedures performed during a 1-year period reported a rate of 1.52%, he said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Other short-term complications in this study included nine cases of device embolization (0.24%). Six of these required surgical removal of the device, while three were retrieved percutaneously.
No sponsor was cited for this study. Boston Scientific, maker of the Watchman left atrial appendage closure device, collected the data on all implantations of the device in the United States following FDA approval. Dr. Reddy and his associates reported ties to Boston Scientific, Coherex, SentreHeart, Abbott Vascular, and St. Jude Medical.
The results reported by Dr. Reddy and his colleagues are remarkably favorable for the earliest phase of widespread dissemination of this technology, especially in the context of the much higher rates of medication-related adverse events that occur with long-term oral anticoagulation. These findings should reassure us that left atrial appendage device closure has been safely introduced into clinical practice in the United States.
The study design, however, raises some concerns, and clinicians should be aware that complications may have been underreported. The manufacturer’s employees collected the data regarding complications in a somewhat informal manner, so this was not an objective study meeting the rigorous standards of clinical trials or postmarketing registries. These “clinical specialists” only included complications that developed within 1 week of the procedure, which fails to address possible delayed complications such as device-related thrombus. And they also didn’t track some important complications such as vascular events and bleeding events.
Jacqueline Saw, MD, of Vancouver General Hospital, and Matthew J. Price, MD, of Scripps Clinic in La Jolla, Calif., made these remarks in an editorial (J Am Coll Cardiol. 2016 Nov. doi: 10.1016/j.jacc.2016.10.019) accompanying Dr. Reddy’s report. Dr. Saw reported ties to Boston Scientific, AstraZeneca, Abbott Vascular, St. Jude Medical, Servier, Bayer, and Sunovion. Dr. Price reported ties to Boston Scientific, St. Jude Medical, W.L. Gore, Medtronic, AstraZeneca, Abbott Vascular, and Terumo.
The results reported by Dr. Reddy and his colleagues are remarkably favorable for the earliest phase of widespread dissemination of this technology, especially in the context of the much higher rates of medication-related adverse events that occur with long-term oral anticoagulation. These findings should reassure us that left atrial appendage device closure has been safely introduced into clinical practice in the United States.
The study design, however, raises some concerns, and clinicians should be aware that complications may have been underreported. The manufacturer’s employees collected the data regarding complications in a somewhat informal manner, so this was not an objective study meeting the rigorous standards of clinical trials or postmarketing registries. These “clinical specialists” only included complications that developed within 1 week of the procedure, which fails to address possible delayed complications such as device-related thrombus. And they also didn’t track some important complications such as vascular events and bleeding events.
Jacqueline Saw, MD, of Vancouver General Hospital, and Matthew J. Price, MD, of Scripps Clinic in La Jolla, Calif., made these remarks in an editorial (J Am Coll Cardiol. 2016 Nov. doi: 10.1016/j.jacc.2016.10.019) accompanying Dr. Reddy’s report. Dr. Saw reported ties to Boston Scientific, AstraZeneca, Abbott Vascular, St. Jude Medical, Servier, Bayer, and Sunovion. Dr. Price reported ties to Boston Scientific, St. Jude Medical, W.L. Gore, Medtronic, AstraZeneca, Abbott Vascular, and Terumo.
The results reported by Dr. Reddy and his colleagues are remarkably favorable for the earliest phase of widespread dissemination of this technology, especially in the context of the much higher rates of medication-related adverse events that occur with long-term oral anticoagulation. These findings should reassure us that left atrial appendage device closure has been safely introduced into clinical practice in the United States.
The study design, however, raises some concerns, and clinicians should be aware that complications may have been underreported. The manufacturer’s employees collected the data regarding complications in a somewhat informal manner, so this was not an objective study meeting the rigorous standards of clinical trials or postmarketing registries. These “clinical specialists” only included complications that developed within 1 week of the procedure, which fails to address possible delayed complications such as device-related thrombus. And they also didn’t track some important complications such as vascular events and bleeding events.
Jacqueline Saw, MD, of Vancouver General Hospital, and Matthew J. Price, MD, of Scripps Clinic in La Jolla, Calif., made these remarks in an editorial (J Am Coll Cardiol. 2016 Nov. doi: 10.1016/j.jacc.2016.10.019) accompanying Dr. Reddy’s report. Dr. Saw reported ties to Boston Scientific, AstraZeneca, Abbott Vascular, St. Jude Medical, Servier, Bayer, and Sunovion. Dr. Price reported ties to Boston Scientific, St. Jude Medical, W.L. Gore, Medtronic, AstraZeneca, Abbott Vascular, and Terumo.
A device that closes the left atrial appendage to prevent stroke in patients with nonvalvular atrial fibrillation showed a 95.6% procedural success rate in a study of real-world experience since it was approved by the FDA in 2015, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
The study was based on data collected by Boston Scientific, the manufacturer of the Watchman device, regarding 3,822 consecutive patients who underwent the implantation during a 14-month period. The “excellent” procedural success rate, together with low short-term complication rates, are especially “remarkable” because 71% of the interventional cardiologists and electrophysiologists who performed these procedures had no experience with the device prior to FDA approval, said Vivek Y. Reddy, MD, of Mount Sinai Medical Center, New York.
For this study, the implantations were done by 382 physicians at 169 U.S. medical centers. A total of 3,653 procedures were successful. The median duration of the implantation was “an acceptable” 50 minutes (range, 10-210 minutes), and an average of 1.38 devices (range, 1-6) were required per patient. In 23% of cases, a “partial recapture” of a device was necessary to reposition it (J Am Coll Cardiol. 2016 Nov. doi: 10.1016/j.jacc.2016.10.010).
The rates of major complications within 1 week – pericardial tamponade (<1%), procedure-related stroke (0.08%), and mortality (0.08%) – were characterized as “favorable.”
The most common complication was pericardial effusion requiring intervention, which developed in 39 patients (1.02%). The effusions were drained percutaneously in most (24) of these patients. Another 11 patients (0.29%) developed mild pericardial effusions requiring only conservative management.
Three strokes, two ischemic and one hemorrhagic, were deemed related to the procedure, though the hemorrhagic bleed may have resulted chiefly from anticoagulation medications. Three deaths were judged to be related to the procedure: All were secondary to pericardial tamponade associated with perforation by the device.
“It is worth comparing [this] cardiac tamponade rate with [that of] another left atrial cardiovascular procedure, catheter ablation of atrial fibrillation,” Dr. Reddy noted.
A worldwide survey of more than 20,000 catheter ablations reported a pericardial tamponade rate of 1.31%, and another study of more than 93,000 ablation procedures performed during a 1-year period reported a rate of 1.52%, he said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Other short-term complications in this study included nine cases of device embolization (0.24%). Six of these required surgical removal of the device, while three were retrieved percutaneously.
No sponsor was cited for this study. Boston Scientific, maker of the Watchman left atrial appendage closure device, collected the data on all implantations of the device in the United States following FDA approval. Dr. Reddy and his associates reported ties to Boston Scientific, Coherex, SentreHeart, Abbott Vascular, and St. Jude Medical.
A device that closes the left atrial appendage to prevent stroke in patients with nonvalvular atrial fibrillation showed a 95.6% procedural success rate in a study of real-world experience since it was approved by the FDA in 2015, according to a report presented at the Transcatheter Cardiovascular Therapeutics annual meeting and published simultaneously in the Journal of the American College of Cardiology.
The study was based on data collected by Boston Scientific, the manufacturer of the Watchman device, regarding 3,822 consecutive patients who underwent the implantation during a 14-month period. The “excellent” procedural success rate, together with low short-term complication rates, are especially “remarkable” because 71% of the interventional cardiologists and electrophysiologists who performed these procedures had no experience with the device prior to FDA approval, said Vivek Y. Reddy, MD, of Mount Sinai Medical Center, New York.
For this study, the implantations were done by 382 physicians at 169 U.S. medical centers. A total of 3,653 procedures were successful. The median duration of the implantation was “an acceptable” 50 minutes (range, 10-210 minutes), and an average of 1.38 devices (range, 1-6) were required per patient. In 23% of cases, a “partial recapture” of a device was necessary to reposition it (J Am Coll Cardiol. 2016 Nov. doi: 10.1016/j.jacc.2016.10.010).
The rates of major complications within 1 week – pericardial tamponade (<1%), procedure-related stroke (0.08%), and mortality (0.08%) – were characterized as “favorable.”
The most common complication was pericardial effusion requiring intervention, which developed in 39 patients (1.02%). The effusions were drained percutaneously in most (24) of these patients. Another 11 patients (0.29%) developed mild pericardial effusions requiring only conservative management.
Three strokes, two ischemic and one hemorrhagic, were deemed related to the procedure, though the hemorrhagic bleed may have resulted chiefly from anticoagulation medications. Three deaths were judged to be related to the procedure: All were secondary to pericardial tamponade associated with perforation by the device.
“It is worth comparing [this] cardiac tamponade rate with [that of] another left atrial cardiovascular procedure, catheter ablation of atrial fibrillation,” Dr. Reddy noted.
A worldwide survey of more than 20,000 catheter ablations reported a pericardial tamponade rate of 1.31%, and another study of more than 93,000 ablation procedures performed during a 1-year period reported a rate of 1.52%, he said at the meeting, which was sponsored by the Cardiovascular Research Foundation.
Other short-term complications in this study included nine cases of device embolization (0.24%). Six of these required surgical removal of the device, while three were retrieved percutaneously.
No sponsor was cited for this study. Boston Scientific, maker of the Watchman left atrial appendage closure device, collected the data on all implantations of the device in the United States following FDA approval. Dr. Reddy and his associates reported ties to Boston Scientific, Coherex, SentreHeart, Abbott Vascular, and St. Jude Medical.
FROM TCT 2016
Key clinical point: A left atrial appendage closure device to prevent stroke in patients with nonvalvular atrial fibrillation showed a 95.6% procedural success rate.
Major finding: Of 3,822 implantations, 3,653 (95.6%) were successful, and 1-week complication rates were low, with <1% pericardial tamponade, 0.08% procedure-related stroke, and 0.08% mortality.
Data source: An analysis of manufacturer-collected data on all 3,822 consecutive device implantations at 169 medical centers from March 2015 to May 2016.
Disclosures: No sponsor was cited for this study. Boston Scientific, maker of the Watchman left atrial appendage closure device, collected the data on all implantations of the device in the United States following FDA approval. Dr. Reddy and his associates reported ties to Boston Scientific, Coherex, SentreHeart, Abbott Vascular, and St. Jude Medical.
Using CHIMPS for type A dissection in a high-risk patient
Traditional open repair for type A aortic dissection in patients with Marfan syndrome and a previous cardiovascular surgery carries a high risk of morbidity and mortality, but a team of surgeons from China have reported on a hybrid technique that combines open and endovascular approaches to repair type A dissection in a patient with Marfan syndrome.
In the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:1191-3), Hong-wei Zhang, MD, and colleagues from West China Hospital of Sichuan University, explained their technique using chimney and sandwich grafts to repair a type A dissection in the patient late after Bentall surgery. “With great advancements in recent thoracic endovascular aortic repair technology, innovative hybrid operations combining open and endovascular techniques hold promising potential to expand treatment options,” Dr. Zhang and coauthors said.
They reported on a 33-year-old male with Marfan syndrome (MFS) who had elective aortic root and mechanical valve replacement 10 years earlier. Three days of persistent chest and back pain caused the patient to go to the emergency department, where computed tomography angiography (CTA) confirmed a type A aortic dissection from the distal ascending aorta to the iliac arteries and involving the proximal innominate artery and left common carotid artery (LCCA).
Because the patient refused another open surgery, Dr. Zhang and colleagues executed their hybrid approach, the first step of which was to create an LCCA-left axillar artery bypass with a 6-mm Gore-Tex graft (W.L. Gore & Associates). After they led the graft through the costoclavicular passage, they introduced the first (distal) thoracic stent (Valiant Captivia, Medtronic) from the right femoral artery and deployed it at the proximal descending aorta. They then inserted the second (proximal) thoracic stent graft into the previous ascending synthetic graft.
Next, they delivered the chimney grafts, two Fluency Plus covered stents (Bard Peripheral Vascular), from the right brachial and innominate artery into the ascending graft. Then they delivered two more Fluency grafts from the LCCA into the endolumen of the first (distal) thoracic stent graft.
After they deployed the second (proximal) thoracic stent graft, they deployed the precisely positioned stent grafts from the innominate artery and the LCCA, sandwiching the covered stents for the LCCA between the two thoracic stent grafts. They then occluded the left subclavian artery with a 10-mm double-disk vascular occlude.
Upon angiography at completion, Dr. Zhang and coauthors found an endoleak from the overlap zones between the two thoracic stent grafts.
However, the patient’s postoperative course was uneventful, and CTA 5 days after surgery showed complete sealing of the primary entry tear with patent chimney and sandwich grafts. The patient remained symptom-free at 30 days, when CTA again confirmed patency of the supra-arch grafts.
Dr. Zhang and coauthors acknowledge that carotid-to-carotid bypass could have been an alternative in order to use fewer stent grafts and to reduce the risk of endoleaks in this case, but they opted for this approach because of the dissection of the proximal innominate artery and LCCA and their concern of the long-term patency of a carotid-to-carotid bypass. “To our knowledge, this is the first reported case of a hybrid treatment for new-onset, type A aortic dissection in patients with MFS with a previous Bentall procedure,” Dr. Zhang and coauthors said. “Although further staged repairs are required in our case, this endovascular technique could be an effective and life-saving treatment option for the high-risk repeated surgical patients with MFS.”
Dr. Zhang and coauthors had no financial relationships to disclose.
In their invited commentary, Lars Svensson, MD, PhD, Matthew Eagleton, MD, and Eric Roselli, MD, of the Cleveland Clinic, said the approach Dr. Zhang and colleagues reported on is one of the “novel” endovascular CHIMPS methods for aortic arch repair – CHIMPS meaning chimneys, periscopes, snorkels, and sandwiches (J Thorac Cardiovasc Surg. 2016;152:958-9). But they noted that one of the ongoing challenges with these types of parallel grafts is the gutter leaks that occur between the sandwich grafts.
The commentators noted that CHIMPS procedures are easier alternatives to using spiral branch graft stents for the thoracoabdominal aorta or direct-connecting branch stems from an aortic stent in the arch, but they added, “An important caveat is that the blood supply maintenance and long-term durability may not be adequate.”
The patient Dr. Zhang and colleagues reported on “is young and will need a durable operation,” Dr. Svensson, Dr. Eagleton, and Dr. Roselli said. “Unfortunately, in our experience over time we have observed that these CHIMPS procedures tend to break down and leak into the arch, including the arch actually rupturing,” they said. These patients will need “intensive” monitoring. What’s more, patients with Marfan syndrome are prone to aneurysm formation “and are not good candidates for stenting,” the commentators said.
“Nevertheless, further engineering iterations of CHIMPS may address the problem with gutter leaks and become an alternative to the elephant trunk procedure for those patients who are at particularly high risk,” the commentators said.
Dr. Svensson disclosed he holds a patent with potential royalties for an aortic valve and aortic root stent graft with connecting branch grafts to the coronary ostia. Dr. Roselli is a consultant and investigator for Bolton, Gore, and Medtronic. Dr. Eagleton has no relationships to disclose.
In their invited commentary, Lars Svensson, MD, PhD, Matthew Eagleton, MD, and Eric Roselli, MD, of the Cleveland Clinic, said the approach Dr. Zhang and colleagues reported on is one of the “novel” endovascular CHIMPS methods for aortic arch repair – CHIMPS meaning chimneys, periscopes, snorkels, and sandwiches (J Thorac Cardiovasc Surg. 2016;152:958-9). But they noted that one of the ongoing challenges with these types of parallel grafts is the gutter leaks that occur between the sandwich grafts.
The commentators noted that CHIMPS procedures are easier alternatives to using spiral branch graft stents for the thoracoabdominal aorta or direct-connecting branch stems from an aortic stent in the arch, but they added, “An important caveat is that the blood supply maintenance and long-term durability may not be adequate.”
The patient Dr. Zhang and colleagues reported on “is young and will need a durable operation,” Dr. Svensson, Dr. Eagleton, and Dr. Roselli said. “Unfortunately, in our experience over time we have observed that these CHIMPS procedures tend to break down and leak into the arch, including the arch actually rupturing,” they said. These patients will need “intensive” monitoring. What’s more, patients with Marfan syndrome are prone to aneurysm formation “and are not good candidates for stenting,” the commentators said.
“Nevertheless, further engineering iterations of CHIMPS may address the problem with gutter leaks and become an alternative to the elephant trunk procedure for those patients who are at particularly high risk,” the commentators said.
Dr. Svensson disclosed he holds a patent with potential royalties for an aortic valve and aortic root stent graft with connecting branch grafts to the coronary ostia. Dr. Roselli is a consultant and investigator for Bolton, Gore, and Medtronic. Dr. Eagleton has no relationships to disclose.
In their invited commentary, Lars Svensson, MD, PhD, Matthew Eagleton, MD, and Eric Roselli, MD, of the Cleveland Clinic, said the approach Dr. Zhang and colleagues reported on is one of the “novel” endovascular CHIMPS methods for aortic arch repair – CHIMPS meaning chimneys, periscopes, snorkels, and sandwiches (J Thorac Cardiovasc Surg. 2016;152:958-9). But they noted that one of the ongoing challenges with these types of parallel grafts is the gutter leaks that occur between the sandwich grafts.
The commentators noted that CHIMPS procedures are easier alternatives to using spiral branch graft stents for the thoracoabdominal aorta or direct-connecting branch stems from an aortic stent in the arch, but they added, “An important caveat is that the blood supply maintenance and long-term durability may not be adequate.”
The patient Dr. Zhang and colleagues reported on “is young and will need a durable operation,” Dr. Svensson, Dr. Eagleton, and Dr. Roselli said. “Unfortunately, in our experience over time we have observed that these CHIMPS procedures tend to break down and leak into the arch, including the arch actually rupturing,” they said. These patients will need “intensive” monitoring. What’s more, patients with Marfan syndrome are prone to aneurysm formation “and are not good candidates for stenting,” the commentators said.
“Nevertheless, further engineering iterations of CHIMPS may address the problem with gutter leaks and become an alternative to the elephant trunk procedure for those patients who are at particularly high risk,” the commentators said.
Dr. Svensson disclosed he holds a patent with potential royalties for an aortic valve and aortic root stent graft with connecting branch grafts to the coronary ostia. Dr. Roselli is a consultant and investigator for Bolton, Gore, and Medtronic. Dr. Eagleton has no relationships to disclose.
Traditional open repair for type A aortic dissection in patients with Marfan syndrome and a previous cardiovascular surgery carries a high risk of morbidity and mortality, but a team of surgeons from China have reported on a hybrid technique that combines open and endovascular approaches to repair type A dissection in a patient with Marfan syndrome.
In the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:1191-3), Hong-wei Zhang, MD, and colleagues from West China Hospital of Sichuan University, explained their technique using chimney and sandwich grafts to repair a type A dissection in the patient late after Bentall surgery. “With great advancements in recent thoracic endovascular aortic repair technology, innovative hybrid operations combining open and endovascular techniques hold promising potential to expand treatment options,” Dr. Zhang and coauthors said.
They reported on a 33-year-old male with Marfan syndrome (MFS) who had elective aortic root and mechanical valve replacement 10 years earlier. Three days of persistent chest and back pain caused the patient to go to the emergency department, where computed tomography angiography (CTA) confirmed a type A aortic dissection from the distal ascending aorta to the iliac arteries and involving the proximal innominate artery and left common carotid artery (LCCA).
Because the patient refused another open surgery, Dr. Zhang and colleagues executed their hybrid approach, the first step of which was to create an LCCA-left axillar artery bypass with a 6-mm Gore-Tex graft (W.L. Gore & Associates). After they led the graft through the costoclavicular passage, they introduced the first (distal) thoracic stent (Valiant Captivia, Medtronic) from the right femoral artery and deployed it at the proximal descending aorta. They then inserted the second (proximal) thoracic stent graft into the previous ascending synthetic graft.
Next, they delivered the chimney grafts, two Fluency Plus covered stents (Bard Peripheral Vascular), from the right brachial and innominate artery into the ascending graft. Then they delivered two more Fluency grafts from the LCCA into the endolumen of the first (distal) thoracic stent graft.
After they deployed the second (proximal) thoracic stent graft, they deployed the precisely positioned stent grafts from the innominate artery and the LCCA, sandwiching the covered stents for the LCCA between the two thoracic stent grafts. They then occluded the left subclavian artery with a 10-mm double-disk vascular occlude.
Upon angiography at completion, Dr. Zhang and coauthors found an endoleak from the overlap zones between the two thoracic stent grafts.
However, the patient’s postoperative course was uneventful, and CTA 5 days after surgery showed complete sealing of the primary entry tear with patent chimney and sandwich grafts. The patient remained symptom-free at 30 days, when CTA again confirmed patency of the supra-arch grafts.
Dr. Zhang and coauthors acknowledge that carotid-to-carotid bypass could have been an alternative in order to use fewer stent grafts and to reduce the risk of endoleaks in this case, but they opted for this approach because of the dissection of the proximal innominate artery and LCCA and their concern of the long-term patency of a carotid-to-carotid bypass. “To our knowledge, this is the first reported case of a hybrid treatment for new-onset, type A aortic dissection in patients with MFS with a previous Bentall procedure,” Dr. Zhang and coauthors said. “Although further staged repairs are required in our case, this endovascular technique could be an effective and life-saving treatment option for the high-risk repeated surgical patients with MFS.”
Dr. Zhang and coauthors had no financial relationships to disclose.
Traditional open repair for type A aortic dissection in patients with Marfan syndrome and a previous cardiovascular surgery carries a high risk of morbidity and mortality, but a team of surgeons from China have reported on a hybrid technique that combines open and endovascular approaches to repair type A dissection in a patient with Marfan syndrome.
In the October issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:1191-3), Hong-wei Zhang, MD, and colleagues from West China Hospital of Sichuan University, explained their technique using chimney and sandwich grafts to repair a type A dissection in the patient late after Bentall surgery. “With great advancements in recent thoracic endovascular aortic repair technology, innovative hybrid operations combining open and endovascular techniques hold promising potential to expand treatment options,” Dr. Zhang and coauthors said.
They reported on a 33-year-old male with Marfan syndrome (MFS) who had elective aortic root and mechanical valve replacement 10 years earlier. Three days of persistent chest and back pain caused the patient to go to the emergency department, where computed tomography angiography (CTA) confirmed a type A aortic dissection from the distal ascending aorta to the iliac arteries and involving the proximal innominate artery and left common carotid artery (LCCA).
Because the patient refused another open surgery, Dr. Zhang and colleagues executed their hybrid approach, the first step of which was to create an LCCA-left axillar artery bypass with a 6-mm Gore-Tex graft (W.L. Gore & Associates). After they led the graft through the costoclavicular passage, they introduced the first (distal) thoracic stent (Valiant Captivia, Medtronic) from the right femoral artery and deployed it at the proximal descending aorta. They then inserted the second (proximal) thoracic stent graft into the previous ascending synthetic graft.
Next, they delivered the chimney grafts, two Fluency Plus covered stents (Bard Peripheral Vascular), from the right brachial and innominate artery into the ascending graft. Then they delivered two more Fluency grafts from the LCCA into the endolumen of the first (distal) thoracic stent graft.
After they deployed the second (proximal) thoracic stent graft, they deployed the precisely positioned stent grafts from the innominate artery and the LCCA, sandwiching the covered stents for the LCCA between the two thoracic stent grafts. They then occluded the left subclavian artery with a 10-mm double-disk vascular occlude.
Upon angiography at completion, Dr. Zhang and coauthors found an endoleak from the overlap zones between the two thoracic stent grafts.
However, the patient’s postoperative course was uneventful, and CTA 5 days after surgery showed complete sealing of the primary entry tear with patent chimney and sandwich grafts. The patient remained symptom-free at 30 days, when CTA again confirmed patency of the supra-arch grafts.
Dr. Zhang and coauthors acknowledge that carotid-to-carotid bypass could have been an alternative in order to use fewer stent grafts and to reduce the risk of endoleaks in this case, but they opted for this approach because of the dissection of the proximal innominate artery and LCCA and their concern of the long-term patency of a carotid-to-carotid bypass. “To our knowledge, this is the first reported case of a hybrid treatment for new-onset, type A aortic dissection in patients with MFS with a previous Bentall procedure,” Dr. Zhang and coauthors said. “Although further staged repairs are required in our case, this endovascular technique could be an effective and life-saving treatment option for the high-risk repeated surgical patients with MFS.”
Dr. Zhang and coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Chimney and sandwich grafts facilitate hybrid repair of type A aortic dissection for a Marfan syndrome patient after Bentall surgery.
Major finding: A 33-year-old male with Marfan syndrome and a history of cardiac surgery was asymptomatic 30 days after hybrid repair for type A aortic dissection.
Data source: Case report of single patient at an academic medical center.
Disclosures: Dr. Zhang and coauthors reported having no financial disclosures.