User login
RUC Predicted to Slash AK Reimbursement
WAIKOLOA, HAWAII – Look for a major cut in reimbursement for the treatment of actinic keratoses when the matter comes up for review by the American Medical Association Relative Value Scale Update Committee in January, according to Dr. Brett M. Coldiron.
"It’s going to be bad, bad. The best-case scenario our team has worked out is a 25% cut," Dr. Coldiron said at the Hawaii Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
It’s entirely possible that the committee will instead recommend closer to a 50% slash in its report to the Center for Medicare and Medicaid Services, added Dr. Coldiron, who has represented dermatology on the Relative Value Scale Update Committee (RUC) or served in an advisory capacity for the past 19 years.
"That first AK relative value rating was based on numbing [the AK], curetting it twice, electrodesiccation, and [the rating estimated] 47 minutes of nursing time. It’s an extraordinary rating ... [times have changed], and now it’s finally up for review," explained Dr. Coldiron, president of the American College of Mohs Surgery and a 2013 member of the board of directors for the American Academy of Dermatology.
Dermatologists perform 86% of all AK treatments in the United States. And the number of procedures in which they bill Medicare for treating 15 or more AKs jumped by 185% from 1995 to 2006, to nearly 734,000 procedures per year.
Meanwhile, the number of Mohs surgery procedures billed to Medicare has increased by a whopping 400%, skin biopsies by dermatologists have increased by 82%, destructions by 68%, and excisions by 22%.
"Those are extraordinary increases, and you have to realize that they’re underestimates because they don’t include billing under Medicare private plans, which take up about 20% of Medicare dollars," he said.
All the Mohs surgery–related codes will come up for RUC review in April 2013. Dr. Coldiron anticipates reimbursement to be cut by about 20%.
He provided the audience with a colorful behind-the-scenes account of the RUC review process.
"The RUC is the Super Bowl of AMA committees, where everybody sits around a table and tries to strip money away from another specialty," he explained. "The RUC is 26 sharks in a tank with nothing to eat but each other. And we’re a small specialty with a ‘Bite Me’ sign on us. We’re less than 1% of all physicians. We have a seat on RUC because we were there from the beginning. But we have many specialty-specific codes which they can target, and we have rapidly increasing utilization."
What’s it like to stand up for dermatology at a RUC review before adversaries representing 25 other medical specialties? "I present the codes and they shoot questions; they just pound on you, sometimes for days. It’s very uncomfortable. They try to figure out what a code is really worth. It’s not much fun at all," said Dr. Coldiron, a dermatologist at the University of Cincinnati.
This intense battle is fueled by jealousy on the part of other specialties, he said. "Dermatology has done better than anybody else in RUC during the past 20 years. Our share of the Medicare pie has gone from about 2% to 3% of the whole Medicare pool, and they’re all aware of this."
He suspects many of his fellow dermatologists will respond to the coming cut in payment for AK therapy by saying, "Well, I used to bill for 10 AKs when I did 15, now I’m going to bill for all 15 of them." That’s a bad idea, in his view. If utilization suddenly shoots up, reimbursement will simply get cut again. And sharp increases in utilization will attract unwanted attention from the Recovery Audit Contractors (RACs). On a contingency basis, Medicare pays RACS 9%-13% of the money recovered through RAC audits for inappropriate billing.
The anticipated cuts in reimbursement for codes covering AK therapy, Mohs surgery, and medical pathology represent a particularly serious threat to academic dermatology, since most departments derive a substantial portion of their funding from those clinical services. Moreover, academic dermatologists have already been hit harder than others by the loss of consultation codes in the Medicare fee schedule, which translates to an estimated $7,000 per year in lost income for most.
The RUC cuts in reimbursement for AK treatment and Mohs surgery will hurt. But they are by no means the biggest threat facing dermatology, in Dr. Coldiron’s view. That distinction belongs to the Independent Payment Advisory Panel (IPAP) empowered by the Patient Protection and Affordable Care Act. The panel’s job will be to identify overused, overpaid, or useless services and cut Medicare payment rates for providers of those services. Their decisions cannot be reversed except by a two-thirds majority of Congress.
"This is serious for us and all small specialties because anything could happen. Why cover Mohs surgery at all? After all, it’s not covered in Great Britain or France, and they’ve got pretty good health care. Why cover acne – isn’t that cosmetic? Why pay pathologists for seborrheic keratoses? There are all kinds of possibilities here that we need to be prepared for," he cautioned.
He predicted that dermatology and other small specialties will get hit first and hardest by health care cost containment efforts. The RUC doesn’t like dermatology. Nor do Medicare officials and some key members of Congress. Neither does the Medicare Payment Advisory Commission (MedPAC), an independent federal body created to help Congress address complicated health policy issues.
"MedPAC likes primary care. They’re getting a bad attitude after 19 years of no increase for primary care. They want all procedure-oriented specialists to be paid the same as the cognitives," Dr. Coldiron said.
He added that fundamental misconceptions regarding dermatology abound. "They think that what dermatologists do is not important, that it’s cosmetic. And that our increase in Relative Value Units is due to waste, abuse, and minor procedure codes that pay too much. If dermatology disappeared there would be few tears shed," according to Dr. Coldiron.
These critics focus on the fact that dermatology, having reinvented itself as a skin surgical specialty, has become the most procedurally oriented of all specialties. Indeed, in the Medicare database, 73% of dermatologists’ income comes from procedures; ophthalmology is a distant second at 56%.
Dermatology’s critics are unwilling to recognize that the main reason for the big jump in dermatologic procedures during the last 2 decades is the ongoing skin cancer epidemic, Dr. Coldiron continued. He was a coinvestigator in a major study that documented a 75% jump in the age-adjusted rate of skin cancer procedures in the Medicare fee-for-service population between 1992 and 2006 (Arch. Dermatol. 2010;146:283-7).
By 2008, the estimated annual incidence of nonmelanoma skin cancer in the United States stood at nearly 3.7 million cases, far higher than previously recognized (Semin. Cutan. Med. Surg. 2011;30:3-5). Today the incidence is close to 4 million cases per year, he added.
"That’s the result of a lot of baby boomers lying out in the sun. The problem is that the government doesn’t want to pay for it. They would rather pretend it doesn’t exist," Dr. Coldiron concluded.
He reported having no financial conflicts. SDEF and this news organization are owned by Elsevier.
WAIKOLOA, HAWAII – Look for a major cut in reimbursement for the treatment of actinic keratoses when the matter comes up for review by the American Medical Association Relative Value Scale Update Committee in January, according to Dr. Brett M. Coldiron.
"It’s going to be bad, bad. The best-case scenario our team has worked out is a 25% cut," Dr. Coldiron said at the Hawaii Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
It’s entirely possible that the committee will instead recommend closer to a 50% slash in its report to the Center for Medicare and Medicaid Services, added Dr. Coldiron, who has represented dermatology on the Relative Value Scale Update Committee (RUC) or served in an advisory capacity for the past 19 years.
"That first AK relative value rating was based on numbing [the AK], curetting it twice, electrodesiccation, and [the rating estimated] 47 minutes of nursing time. It’s an extraordinary rating ... [times have changed], and now it’s finally up for review," explained Dr. Coldiron, president of the American College of Mohs Surgery and a 2013 member of the board of directors for the American Academy of Dermatology.
Dermatologists perform 86% of all AK treatments in the United States. And the number of procedures in which they bill Medicare for treating 15 or more AKs jumped by 185% from 1995 to 2006, to nearly 734,000 procedures per year.
Meanwhile, the number of Mohs surgery procedures billed to Medicare has increased by a whopping 400%, skin biopsies by dermatologists have increased by 82%, destructions by 68%, and excisions by 22%.
"Those are extraordinary increases, and you have to realize that they’re underestimates because they don’t include billing under Medicare private plans, which take up about 20% of Medicare dollars," he said.
All the Mohs surgery–related codes will come up for RUC review in April 2013. Dr. Coldiron anticipates reimbursement to be cut by about 20%.
He provided the audience with a colorful behind-the-scenes account of the RUC review process.
"The RUC is the Super Bowl of AMA committees, where everybody sits around a table and tries to strip money away from another specialty," he explained. "The RUC is 26 sharks in a tank with nothing to eat but each other. And we’re a small specialty with a ‘Bite Me’ sign on us. We’re less than 1% of all physicians. We have a seat on RUC because we were there from the beginning. But we have many specialty-specific codes which they can target, and we have rapidly increasing utilization."
What’s it like to stand up for dermatology at a RUC review before adversaries representing 25 other medical specialties? "I present the codes and they shoot questions; they just pound on you, sometimes for days. It’s very uncomfortable. They try to figure out what a code is really worth. It’s not much fun at all," said Dr. Coldiron, a dermatologist at the University of Cincinnati.
This intense battle is fueled by jealousy on the part of other specialties, he said. "Dermatology has done better than anybody else in RUC during the past 20 years. Our share of the Medicare pie has gone from about 2% to 3% of the whole Medicare pool, and they’re all aware of this."
He suspects many of his fellow dermatologists will respond to the coming cut in payment for AK therapy by saying, "Well, I used to bill for 10 AKs when I did 15, now I’m going to bill for all 15 of them." That’s a bad idea, in his view. If utilization suddenly shoots up, reimbursement will simply get cut again. And sharp increases in utilization will attract unwanted attention from the Recovery Audit Contractors (RACs). On a contingency basis, Medicare pays RACS 9%-13% of the money recovered through RAC audits for inappropriate billing.
The anticipated cuts in reimbursement for codes covering AK therapy, Mohs surgery, and medical pathology represent a particularly serious threat to academic dermatology, since most departments derive a substantial portion of their funding from those clinical services. Moreover, academic dermatologists have already been hit harder than others by the loss of consultation codes in the Medicare fee schedule, which translates to an estimated $7,000 per year in lost income for most.
The RUC cuts in reimbursement for AK treatment and Mohs surgery will hurt. But they are by no means the biggest threat facing dermatology, in Dr. Coldiron’s view. That distinction belongs to the Independent Payment Advisory Panel (IPAP) empowered by the Patient Protection and Affordable Care Act. The panel’s job will be to identify overused, overpaid, or useless services and cut Medicare payment rates for providers of those services. Their decisions cannot be reversed except by a two-thirds majority of Congress.
"This is serious for us and all small specialties because anything could happen. Why cover Mohs surgery at all? After all, it’s not covered in Great Britain or France, and they’ve got pretty good health care. Why cover acne – isn’t that cosmetic? Why pay pathologists for seborrheic keratoses? There are all kinds of possibilities here that we need to be prepared for," he cautioned.
He predicted that dermatology and other small specialties will get hit first and hardest by health care cost containment efforts. The RUC doesn’t like dermatology. Nor do Medicare officials and some key members of Congress. Neither does the Medicare Payment Advisory Commission (MedPAC), an independent federal body created to help Congress address complicated health policy issues.
"MedPAC likes primary care. They’re getting a bad attitude after 19 years of no increase for primary care. They want all procedure-oriented specialists to be paid the same as the cognitives," Dr. Coldiron said.
He added that fundamental misconceptions regarding dermatology abound. "They think that what dermatologists do is not important, that it’s cosmetic. And that our increase in Relative Value Units is due to waste, abuse, and minor procedure codes that pay too much. If dermatology disappeared there would be few tears shed," according to Dr. Coldiron.
These critics focus on the fact that dermatology, having reinvented itself as a skin surgical specialty, has become the most procedurally oriented of all specialties. Indeed, in the Medicare database, 73% of dermatologists’ income comes from procedures; ophthalmology is a distant second at 56%.
Dermatology’s critics are unwilling to recognize that the main reason for the big jump in dermatologic procedures during the last 2 decades is the ongoing skin cancer epidemic, Dr. Coldiron continued. He was a coinvestigator in a major study that documented a 75% jump in the age-adjusted rate of skin cancer procedures in the Medicare fee-for-service population between 1992 and 2006 (Arch. Dermatol. 2010;146:283-7).
By 2008, the estimated annual incidence of nonmelanoma skin cancer in the United States stood at nearly 3.7 million cases, far higher than previously recognized (Semin. Cutan. Med. Surg. 2011;30:3-5). Today the incidence is close to 4 million cases per year, he added.
"That’s the result of a lot of baby boomers lying out in the sun. The problem is that the government doesn’t want to pay for it. They would rather pretend it doesn’t exist," Dr. Coldiron concluded.
He reported having no financial conflicts. SDEF and this news organization are owned by Elsevier.
WAIKOLOA, HAWAII – Look for a major cut in reimbursement for the treatment of actinic keratoses when the matter comes up for review by the American Medical Association Relative Value Scale Update Committee in January, according to Dr. Brett M. Coldiron.
"It’s going to be bad, bad. The best-case scenario our team has worked out is a 25% cut," Dr. Coldiron said at the Hawaii Dermatology Seminar, sponsored by Skin Disease Education Foundation (SDEF).
It’s entirely possible that the committee will instead recommend closer to a 50% slash in its report to the Center for Medicare and Medicaid Services, added Dr. Coldiron, who has represented dermatology on the Relative Value Scale Update Committee (RUC) or served in an advisory capacity for the past 19 years.
"That first AK relative value rating was based on numbing [the AK], curetting it twice, electrodesiccation, and [the rating estimated] 47 minutes of nursing time. It’s an extraordinary rating ... [times have changed], and now it’s finally up for review," explained Dr. Coldiron, president of the American College of Mohs Surgery and a 2013 member of the board of directors for the American Academy of Dermatology.
Dermatologists perform 86% of all AK treatments in the United States. And the number of procedures in which they bill Medicare for treating 15 or more AKs jumped by 185% from 1995 to 2006, to nearly 734,000 procedures per year.
Meanwhile, the number of Mohs surgery procedures billed to Medicare has increased by a whopping 400%, skin biopsies by dermatologists have increased by 82%, destructions by 68%, and excisions by 22%.
"Those are extraordinary increases, and you have to realize that they’re underestimates because they don’t include billing under Medicare private plans, which take up about 20% of Medicare dollars," he said.
All the Mohs surgery–related codes will come up for RUC review in April 2013. Dr. Coldiron anticipates reimbursement to be cut by about 20%.
He provided the audience with a colorful behind-the-scenes account of the RUC review process.
"The RUC is the Super Bowl of AMA committees, where everybody sits around a table and tries to strip money away from another specialty," he explained. "The RUC is 26 sharks in a tank with nothing to eat but each other. And we’re a small specialty with a ‘Bite Me’ sign on us. We’re less than 1% of all physicians. We have a seat on RUC because we were there from the beginning. But we have many specialty-specific codes which they can target, and we have rapidly increasing utilization."
What’s it like to stand up for dermatology at a RUC review before adversaries representing 25 other medical specialties? "I present the codes and they shoot questions; they just pound on you, sometimes for days. It’s very uncomfortable. They try to figure out what a code is really worth. It’s not much fun at all," said Dr. Coldiron, a dermatologist at the University of Cincinnati.
This intense battle is fueled by jealousy on the part of other specialties, he said. "Dermatology has done better than anybody else in RUC during the past 20 years. Our share of the Medicare pie has gone from about 2% to 3% of the whole Medicare pool, and they’re all aware of this."
He suspects many of his fellow dermatologists will respond to the coming cut in payment for AK therapy by saying, "Well, I used to bill for 10 AKs when I did 15, now I’m going to bill for all 15 of them." That’s a bad idea, in his view. If utilization suddenly shoots up, reimbursement will simply get cut again. And sharp increases in utilization will attract unwanted attention from the Recovery Audit Contractors (RACs). On a contingency basis, Medicare pays RACS 9%-13% of the money recovered through RAC audits for inappropriate billing.
The anticipated cuts in reimbursement for codes covering AK therapy, Mohs surgery, and medical pathology represent a particularly serious threat to academic dermatology, since most departments derive a substantial portion of their funding from those clinical services. Moreover, academic dermatologists have already been hit harder than others by the loss of consultation codes in the Medicare fee schedule, which translates to an estimated $7,000 per year in lost income for most.
The RUC cuts in reimbursement for AK treatment and Mohs surgery will hurt. But they are by no means the biggest threat facing dermatology, in Dr. Coldiron’s view. That distinction belongs to the Independent Payment Advisory Panel (IPAP) empowered by the Patient Protection and Affordable Care Act. The panel’s job will be to identify overused, overpaid, or useless services and cut Medicare payment rates for providers of those services. Their decisions cannot be reversed except by a two-thirds majority of Congress.
"This is serious for us and all small specialties because anything could happen. Why cover Mohs surgery at all? After all, it’s not covered in Great Britain or France, and they’ve got pretty good health care. Why cover acne – isn’t that cosmetic? Why pay pathologists for seborrheic keratoses? There are all kinds of possibilities here that we need to be prepared for," he cautioned.
He predicted that dermatology and other small specialties will get hit first and hardest by health care cost containment efforts. The RUC doesn’t like dermatology. Nor do Medicare officials and some key members of Congress. Neither does the Medicare Payment Advisory Commission (MedPAC), an independent federal body created to help Congress address complicated health policy issues.
"MedPAC likes primary care. They’re getting a bad attitude after 19 years of no increase for primary care. They want all procedure-oriented specialists to be paid the same as the cognitives," Dr. Coldiron said.
He added that fundamental misconceptions regarding dermatology abound. "They think that what dermatologists do is not important, that it’s cosmetic. And that our increase in Relative Value Units is due to waste, abuse, and minor procedure codes that pay too much. If dermatology disappeared there would be few tears shed," according to Dr. Coldiron.
These critics focus on the fact that dermatology, having reinvented itself as a skin surgical specialty, has become the most procedurally oriented of all specialties. Indeed, in the Medicare database, 73% of dermatologists’ income comes from procedures; ophthalmology is a distant second at 56%.
Dermatology’s critics are unwilling to recognize that the main reason for the big jump in dermatologic procedures during the last 2 decades is the ongoing skin cancer epidemic, Dr. Coldiron continued. He was a coinvestigator in a major study that documented a 75% jump in the age-adjusted rate of skin cancer procedures in the Medicare fee-for-service population between 1992 and 2006 (Arch. Dermatol. 2010;146:283-7).
By 2008, the estimated annual incidence of nonmelanoma skin cancer in the United States stood at nearly 3.7 million cases, far higher than previously recognized (Semin. Cutan. Med. Surg. 2011;30:3-5). Today the incidence is close to 4 million cases per year, he added.
"That’s the result of a lot of baby boomers lying out in the sun. The problem is that the government doesn’t want to pay for it. They would rather pretend it doesn’t exist," Dr. Coldiron concluded.
He reported having no financial conflicts. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
Economic Forecast: Rough Road Ahead for Dermatologists
WAIKOLOA, HAWAII – Dr. Brett M. Coldiron is a sort of latter-day Paul Revere, travelling far and wide to spread the alarm to his fellow dermatologists – not of Redcoats a’coming, but of the need to prepare for looming economic hard times.
"I wasn’t invited to speak at your meeting, so I invited myself," he declared by way of introduction at the Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF), as he launched into an analysis of dermatology’s near-term financial future.
"I’m here to present your 5-year economic plan – what you can expect. I think you can plan your next 5 years based on these predictions. It’s not pretty; and it’s not kind," cautioned Dr. Coldiron, whose expertise regarding health care policy and reform has been forged through long-term involvement representing dermatology on the American Medical Association’s Relative Value Scale Update, Health Care Finance, and Government Health Care Policy committees.
His core message to his colleagues boiled down to this: "Don’t build palaces. It’s time to hunker down."
Dermatology is a heavily procedurally oriented, small specialty – less then 1% of all physicians – which has experienced dramatic growth in procedure volume over the past couple decades. As such, it is a high-priority target for congressional cost-cutting efforts. In the first 4 months of next year, Dr. Coldiron said he expects reimbursement for codes pertaining to actinic keratosis treatment to be cut by 25%-50%, along with a roughly 20% reduction in payment for Mohs surgery. And that’s just the beginning.
Dermatology and other small specialties will bear the brunt of any cost-savings attempts by Congress. Dermatology has powerful enemies in Congress, the Centers for Medicare and Medicaid Services, and the American Medical Association, who view dermatologists as overpaid, wasteful abusers of the system, explained Dr. Coldiron, who is president of the American College of Mohs Surgery and a 2013 member of the American Academy of Dermatology’s board of directors.
Among his predictions for the next 5 years:
• Hospitals and pharmacies, if squeezed too hard, will simply close. Insurers will move into other lines of business coverage. Pharmaceutical companies will reduce their research and development budgets. Thus, reducing physician income will be one of the few politically acceptable health care cost-cutting avenues available.
• There will be more bundling of minor procedures into evaluation and management fees.
• The government will attempt to force all physicians to accept Medicaid. "They’ll probably try to tie it to your acceptance of Medicare. Or maybe they’ll say, ‘We paid for 4 years of postgraduate education; now you owe us 4 years of taking Medicaid,’ " he said.
• The use of physician assistants and nurse practitioners will grow in dermatology. This will result in increased utilization and more intense billing audits along with reimbursement cuts aimed at cancelling out the economic impact of greater utilization.
• Cosmetic procedures and reconstructive surgery will remain safe havens. "They may try to pass a cosmetic procedure tax, but I think the fact that you have another source of income is very important," noted Dr. Coldiron, a dermatologist at the University of Cincinnati.
He recommended that dermatologists temper their income projections for the coming half-decade: "Don’t promise big salaries to new associates, only a percentage of income collected."
Also, read the fine print before jumping on board one of the accountable care organizations that are springing up. "This is government-driven managed care with capitation. What they’re going to do is extract from the specialists and give back to primary care. It’s kind of a loser’s game," he said.
Beyond the next 5 years, however, the outlook for dermatology is bright, Dr. Coldiron stressed.
"Be strong. We are not greedy specialists; we are a frontline specialty fighting an epidemic of skin cancer. We are needed by our patients and by the health care system. The pendulum will eventually swing back our way," he concluded.
Dr. Coldiron reported having no relevant financial conflicts. SDEF and this news organization are owned by Elsevier.
WAIKOLOA, HAWAII – Dr. Brett M. Coldiron is a sort of latter-day Paul Revere, travelling far and wide to spread the alarm to his fellow dermatologists – not of Redcoats a’coming, but of the need to prepare for looming economic hard times.
"I wasn’t invited to speak at your meeting, so I invited myself," he declared by way of introduction at the Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF), as he launched into an analysis of dermatology’s near-term financial future.
"I’m here to present your 5-year economic plan – what you can expect. I think you can plan your next 5 years based on these predictions. It’s not pretty; and it’s not kind," cautioned Dr. Coldiron, whose expertise regarding health care policy and reform has been forged through long-term involvement representing dermatology on the American Medical Association’s Relative Value Scale Update, Health Care Finance, and Government Health Care Policy committees.
His core message to his colleagues boiled down to this: "Don’t build palaces. It’s time to hunker down."
Dermatology is a heavily procedurally oriented, small specialty – less then 1% of all physicians – which has experienced dramatic growth in procedure volume over the past couple decades. As such, it is a high-priority target for congressional cost-cutting efforts. In the first 4 months of next year, Dr. Coldiron said he expects reimbursement for codes pertaining to actinic keratosis treatment to be cut by 25%-50%, along with a roughly 20% reduction in payment for Mohs surgery. And that’s just the beginning.
Dermatology and other small specialties will bear the brunt of any cost-savings attempts by Congress. Dermatology has powerful enemies in Congress, the Centers for Medicare and Medicaid Services, and the American Medical Association, who view dermatologists as overpaid, wasteful abusers of the system, explained Dr. Coldiron, who is president of the American College of Mohs Surgery and a 2013 member of the American Academy of Dermatology’s board of directors.
Among his predictions for the next 5 years:
• Hospitals and pharmacies, if squeezed too hard, will simply close. Insurers will move into other lines of business coverage. Pharmaceutical companies will reduce their research and development budgets. Thus, reducing physician income will be one of the few politically acceptable health care cost-cutting avenues available.
• There will be more bundling of minor procedures into evaluation and management fees.
• The government will attempt to force all physicians to accept Medicaid. "They’ll probably try to tie it to your acceptance of Medicare. Or maybe they’ll say, ‘We paid for 4 years of postgraduate education; now you owe us 4 years of taking Medicaid,’ " he said.
• The use of physician assistants and nurse practitioners will grow in dermatology. This will result in increased utilization and more intense billing audits along with reimbursement cuts aimed at cancelling out the economic impact of greater utilization.
• Cosmetic procedures and reconstructive surgery will remain safe havens. "They may try to pass a cosmetic procedure tax, but I think the fact that you have another source of income is very important," noted Dr. Coldiron, a dermatologist at the University of Cincinnati.
He recommended that dermatologists temper their income projections for the coming half-decade: "Don’t promise big salaries to new associates, only a percentage of income collected."
Also, read the fine print before jumping on board one of the accountable care organizations that are springing up. "This is government-driven managed care with capitation. What they’re going to do is extract from the specialists and give back to primary care. It’s kind of a loser’s game," he said.
Beyond the next 5 years, however, the outlook for dermatology is bright, Dr. Coldiron stressed.
"Be strong. We are not greedy specialists; we are a frontline specialty fighting an epidemic of skin cancer. We are needed by our patients and by the health care system. The pendulum will eventually swing back our way," he concluded.
Dr. Coldiron reported having no relevant financial conflicts. SDEF and this news organization are owned by Elsevier.
WAIKOLOA, HAWAII – Dr. Brett M. Coldiron is a sort of latter-day Paul Revere, travelling far and wide to spread the alarm to his fellow dermatologists – not of Redcoats a’coming, but of the need to prepare for looming economic hard times.
"I wasn’t invited to speak at your meeting, so I invited myself," he declared by way of introduction at the Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF), as he launched into an analysis of dermatology’s near-term financial future.
"I’m here to present your 5-year economic plan – what you can expect. I think you can plan your next 5 years based on these predictions. It’s not pretty; and it’s not kind," cautioned Dr. Coldiron, whose expertise regarding health care policy and reform has been forged through long-term involvement representing dermatology on the American Medical Association’s Relative Value Scale Update, Health Care Finance, and Government Health Care Policy committees.
His core message to his colleagues boiled down to this: "Don’t build palaces. It’s time to hunker down."
Dermatology is a heavily procedurally oriented, small specialty – less then 1% of all physicians – which has experienced dramatic growth in procedure volume over the past couple decades. As such, it is a high-priority target for congressional cost-cutting efforts. In the first 4 months of next year, Dr. Coldiron said he expects reimbursement for codes pertaining to actinic keratosis treatment to be cut by 25%-50%, along with a roughly 20% reduction in payment for Mohs surgery. And that’s just the beginning.
Dermatology and other small specialties will bear the brunt of any cost-savings attempts by Congress. Dermatology has powerful enemies in Congress, the Centers for Medicare and Medicaid Services, and the American Medical Association, who view dermatologists as overpaid, wasteful abusers of the system, explained Dr. Coldiron, who is president of the American College of Mohs Surgery and a 2013 member of the American Academy of Dermatology’s board of directors.
Among his predictions for the next 5 years:
• Hospitals and pharmacies, if squeezed too hard, will simply close. Insurers will move into other lines of business coverage. Pharmaceutical companies will reduce their research and development budgets. Thus, reducing physician income will be one of the few politically acceptable health care cost-cutting avenues available.
• There will be more bundling of minor procedures into evaluation and management fees.
• The government will attempt to force all physicians to accept Medicaid. "They’ll probably try to tie it to your acceptance of Medicare. Or maybe they’ll say, ‘We paid for 4 years of postgraduate education; now you owe us 4 years of taking Medicaid,’ " he said.
• The use of physician assistants and nurse practitioners will grow in dermatology. This will result in increased utilization and more intense billing audits along with reimbursement cuts aimed at cancelling out the economic impact of greater utilization.
• Cosmetic procedures and reconstructive surgery will remain safe havens. "They may try to pass a cosmetic procedure tax, but I think the fact that you have another source of income is very important," noted Dr. Coldiron, a dermatologist at the University of Cincinnati.
He recommended that dermatologists temper their income projections for the coming half-decade: "Don’t promise big salaries to new associates, only a percentage of income collected."
Also, read the fine print before jumping on board one of the accountable care organizations that are springing up. "This is government-driven managed care with capitation. What they’re going to do is extract from the specialists and give back to primary care. It’s kind of a loser’s game," he said.
Beyond the next 5 years, however, the outlook for dermatology is bright, Dr. Coldiron stressed.
"Be strong. We are not greedy specialists; we are a frontline specialty fighting an epidemic of skin cancer. We are needed by our patients and by the health care system. The pendulum will eventually swing back our way," he concluded.
Dr. Coldiron reported having no relevant financial conflicts. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE HAWAII DERMATOLOGY SEMINAR SPONSORED BY SKIN DISEASE EDUCATION FOUNDATION
Study Results Support Ingenol Mebutate's AK Effectiveness
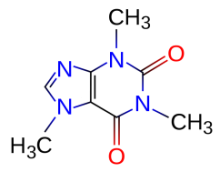
Topical ingenol mebutate gel effectively treated actinic keratoses when applied to the face, scalp, trunk, or extremities for 2-3 days, according to a report in the March 15 issue of the New England Journal of Medicine.
Compared with existing therapies for actinic keratoses, the chief advantage of ingenol mebutate gel is the short exposure time, reported Dr. Mark Lebwohl, professor and chairman of the department of dermatology at Mount Sinai School of Medicine, New York, and his associates. This allows for relatively rapid resolution of local reactions, and it will likely improve adherence to treatment, which in turn should improve the therapy’s effectiveness, they noted.
"Many patients find it difficult to adhere to the currently available regimens of topical treatment that last for periods of 1-4 months, which may result in ‘real-world’ effectiveness lower than that achieved in supervised and patient-compensated clinical trials," Dr. Lebwohl and his colleagues wrote.
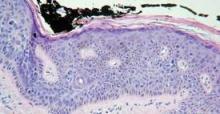
The researchers evaluated the safety and effectiveness of ingenol mebutate gel compared with a placebo in a manufacturer-sponsored, randomized, double-blind trial of 1,005 patients treated at four medical centers. The majority of the patients had Fitzpatrick type I or II skin, and their mean age was 65 years.
Approximately half of the study patients had a history of skin cancer, and 75% had already had their keratosis treated with cryotherapy, imiquimod, or topical fluorouracil.
In each patient, a 25-cm contiguous field containing at least four to eight clinically typical and discrete actinic keratoses was selected for treatment. The study patients were divided into two groups according to the location of the treated area: on the head (face or scalp), and on the body (trunk or extremities).
Those with facial or scalp lesions were randomly assigned to self-apply either 0.015% active gel (277 patients) or placebo gel (270 patients) to the area once daily for 3 consecutive days. Those with trunk or extremity lesions were randomly assigned to self-apply 0.05% active gel (226 patients) or placebo gel (232 patients) to the area once daily for 2 consecutive days.
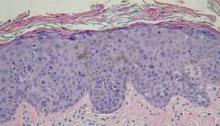
The primary end point was complete clearance of all clinically visible actinic keratoses in the treatment area on day 57.
Among patients with facial or scalp lesions, 42.2% of those who used active gel reached this end point, compared with only 3.7% of those who used placebo gel. Among patients with trunk or extremity lesions, 34.1% who used active gel reached this end point, compared with only 4.7% of those who used placebo gel.
In addition, patients with face or scalp lesions that were treated with ingenol mebutate showed a median reduction of 83% in the number of actinic keratoses, compared with a 0% reduction with placebo gel. "We calculated that the number of patients who needed to be treated with ingenol mebutate to obtain complete clearance in one patient was 2.6," the investigators reported (N. Engl. J. Med. 2012;366:1010-19).
Patients with trunk or extremity lesions treated with ingenol mebutate showed a median reduction of 75% in the number of actinic keratoses, compared with a 0% reduction with placebo gel. "We calculated that the number of patients who would need to be treated with ingenol mebutate to obtain complete clearance in one patient was 3.4," the researchers noted.
A secondary end point was partial (75% or more) clearance in the number of clinically visible actinic keratoses in the treatment area on day 57.
Among patients with facial or scalp lesions, 63.9% of those who used active gel reached this end point, compared with only 7.4% of those who used placebo gel. Among patients with trunk or extremity lesions, 49.1% of those who used active gel reached this end point, compared with only 6.9% of those who used placebo gel.
Patients who used ingenol mebutate showed minimal scarring or change in pigmentation. Local reactions such as erythema, crusting, swelling, vesiculation, or pustulation were common, but were mild to moderate in intensity; they peaked within a few days of treatment and resolved rapidly afterward, with no sequelae. One patient developed eye pain, burning, and periorbital edema related to ingenol mebutate and dropped out of the study, Dr. Lebwohl and his associates noted.
"Future studies are needed to assess the risks and benefits of treating larger areas of skin, using multiple treatments in the same area, and using combination therapies," they added.
This study was funded by LEO Pharma, maker of ingenol mebutate. Dr. Lebwohl reported ties to LEO Pharma, Graceway, PharmaDerm, and Peplin LTD.
Topical ingenol mebutate gel effectively treated actinic keratoses when applied to the face, scalp, trunk, or extremities for 2-3 days, according to a report in the March 15 issue of the New England Journal of Medicine.
Compared with existing therapies for actinic keratoses, the chief advantage of ingenol mebutate gel is the short exposure time, reported Dr. Mark Lebwohl, professor and chairman of the department of dermatology at Mount Sinai School of Medicine, New York, and his associates. This allows for relatively rapid resolution of local reactions, and it will likely improve adherence to treatment, which in turn should improve the therapy’s effectiveness, they noted.
"Many patients find it difficult to adhere to the currently available regimens of topical treatment that last for periods of 1-4 months, which may result in ‘real-world’ effectiveness lower than that achieved in supervised and patient-compensated clinical trials," Dr. Lebwohl and his colleagues wrote.
The researchers evaluated the safety and effectiveness of ingenol mebutate gel compared with a placebo in a manufacturer-sponsored, randomized, double-blind trial of 1,005 patients treated at four medical centers. The majority of the patients had Fitzpatrick type I or II skin, and their mean age was 65 years.
Approximately half of the study patients had a history of skin cancer, and 75% had already had their keratosis treated with cryotherapy, imiquimod, or topical fluorouracil.
In each patient, a 25-cm contiguous field containing at least four to eight clinically typical and discrete actinic keratoses was selected for treatment. The study patients were divided into two groups according to the location of the treated area: on the head (face or scalp), and on the body (trunk or extremities).
Those with facial or scalp lesions were randomly assigned to self-apply either 0.015% active gel (277 patients) or placebo gel (270 patients) to the area once daily for 3 consecutive days. Those with trunk or extremity lesions were randomly assigned to self-apply 0.05% active gel (226 patients) or placebo gel (232 patients) to the area once daily for 2 consecutive days.
The primary end point was complete clearance of all clinically visible actinic keratoses in the treatment area on day 57.
Among patients with facial or scalp lesions, 42.2% of those who used active gel reached this end point, compared with only 3.7% of those who used placebo gel. Among patients with trunk or extremity lesions, 34.1% who used active gel reached this end point, compared with only 4.7% of those who used placebo gel.
In addition, patients with face or scalp lesions that were treated with ingenol mebutate showed a median reduction of 83% in the number of actinic keratoses, compared with a 0% reduction with placebo gel. "We calculated that the number of patients who needed to be treated with ingenol mebutate to obtain complete clearance in one patient was 2.6," the investigators reported (N. Engl. J. Med. 2012;366:1010-19).
Patients with trunk or extremity lesions treated with ingenol mebutate showed a median reduction of 75% in the number of actinic keratoses, compared with a 0% reduction with placebo gel. "We calculated that the number of patients who would need to be treated with ingenol mebutate to obtain complete clearance in one patient was 3.4," the researchers noted.
A secondary end point was partial (75% or more) clearance in the number of clinically visible actinic keratoses in the treatment area on day 57.
Among patients with facial or scalp lesions, 63.9% of those who used active gel reached this end point, compared with only 7.4% of those who used placebo gel. Among patients with trunk or extremity lesions, 49.1% of those who used active gel reached this end point, compared with only 6.9% of those who used placebo gel.
Patients who used ingenol mebutate showed minimal scarring or change in pigmentation. Local reactions such as erythema, crusting, swelling, vesiculation, or pustulation were common, but were mild to moderate in intensity; they peaked within a few days of treatment and resolved rapidly afterward, with no sequelae. One patient developed eye pain, burning, and periorbital edema related to ingenol mebutate and dropped out of the study, Dr. Lebwohl and his associates noted.
"Future studies are needed to assess the risks and benefits of treating larger areas of skin, using multiple treatments in the same area, and using combination therapies," they added.
This study was funded by LEO Pharma, maker of ingenol mebutate. Dr. Lebwohl reported ties to LEO Pharma, Graceway, PharmaDerm, and Peplin LTD.
Topical ingenol mebutate gel effectively treated actinic keratoses when applied to the face, scalp, trunk, or extremities for 2-3 days, according to a report in the March 15 issue of the New England Journal of Medicine.
Compared with existing therapies for actinic keratoses, the chief advantage of ingenol mebutate gel is the short exposure time, reported Dr. Mark Lebwohl, professor and chairman of the department of dermatology at Mount Sinai School of Medicine, New York, and his associates. This allows for relatively rapid resolution of local reactions, and it will likely improve adherence to treatment, which in turn should improve the therapy’s effectiveness, they noted.
"Many patients find it difficult to adhere to the currently available regimens of topical treatment that last for periods of 1-4 months, which may result in ‘real-world’ effectiveness lower than that achieved in supervised and patient-compensated clinical trials," Dr. Lebwohl and his colleagues wrote.
The researchers evaluated the safety and effectiveness of ingenol mebutate gel compared with a placebo in a manufacturer-sponsored, randomized, double-blind trial of 1,005 patients treated at four medical centers. The majority of the patients had Fitzpatrick type I or II skin, and their mean age was 65 years.
Approximately half of the study patients had a history of skin cancer, and 75% had already had their keratosis treated with cryotherapy, imiquimod, or topical fluorouracil.
In each patient, a 25-cm contiguous field containing at least four to eight clinically typical and discrete actinic keratoses was selected for treatment. The study patients were divided into two groups according to the location of the treated area: on the head (face or scalp), and on the body (trunk or extremities).
Those with facial or scalp lesions were randomly assigned to self-apply either 0.015% active gel (277 patients) or placebo gel (270 patients) to the area once daily for 3 consecutive days. Those with trunk or extremity lesions were randomly assigned to self-apply 0.05% active gel (226 patients) or placebo gel (232 patients) to the area once daily for 2 consecutive days.
The primary end point was complete clearance of all clinically visible actinic keratoses in the treatment area on day 57.
Among patients with facial or scalp lesions, 42.2% of those who used active gel reached this end point, compared with only 3.7% of those who used placebo gel. Among patients with trunk or extremity lesions, 34.1% who used active gel reached this end point, compared with only 4.7% of those who used placebo gel.
In addition, patients with face or scalp lesions that were treated with ingenol mebutate showed a median reduction of 83% in the number of actinic keratoses, compared with a 0% reduction with placebo gel. "We calculated that the number of patients who needed to be treated with ingenol mebutate to obtain complete clearance in one patient was 2.6," the investigators reported (N. Engl. J. Med. 2012;366:1010-19).
Patients with trunk or extremity lesions treated with ingenol mebutate showed a median reduction of 75% in the number of actinic keratoses, compared with a 0% reduction with placebo gel. "We calculated that the number of patients who would need to be treated with ingenol mebutate to obtain complete clearance in one patient was 3.4," the researchers noted.
A secondary end point was partial (75% or more) clearance in the number of clinically visible actinic keratoses in the treatment area on day 57.
Among patients with facial or scalp lesions, 63.9% of those who used active gel reached this end point, compared with only 7.4% of those who used placebo gel. Among patients with trunk or extremity lesions, 49.1% of those who used active gel reached this end point, compared with only 6.9% of those who used placebo gel.
Patients who used ingenol mebutate showed minimal scarring or change in pigmentation. Local reactions such as erythema, crusting, swelling, vesiculation, or pustulation were common, but were mild to moderate in intensity; they peaked within a few days of treatment and resolved rapidly afterward, with no sequelae. One patient developed eye pain, burning, and periorbital edema related to ingenol mebutate and dropped out of the study, Dr. Lebwohl and his associates noted.
"Future studies are needed to assess the risks and benefits of treating larger areas of skin, using multiple treatments in the same area, and using combination therapies," they added.
This study was funded by LEO Pharma, maker of ingenol mebutate. Dr. Lebwohl reported ties to LEO Pharma, Graceway, PharmaDerm, and Peplin LTD.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: In patients with facial or scalp lesions, 42.2% who used ingenol mebutate gel achieved complete clearance at 2 months, compared with only 3.7% of those who used placebo gel; in patients with trunk or extremity lesions, 34.1% who used active gel achieved complete clearance, compared with only 4.7% of those who used placebo gel.
Data Source: Data are from a manufacturer-sponsored, randomized, double-blind trial of 1,005 patients treated at four medical centers.
Disclosures: This study was funded by LEO Pharma, maker of ingenol mebutate. Dr. Lebwohl reported ties to LEO Pharma, Graceway, PharmaDerm, and Peplin LTD.
Numbing Agents Cause More Pain in PDT
WAIKOLOA, HAWAII – Using EMLA or lidocaine cream in conjunction with topical 5-aminolevulinic acid photodynamic therapy may boost uptake of the photosensitizer, but the clinical outcomes can be unpredictable, according to Dr. E. Victor Ross.
"Our worst scenarios have been when we’ve used EMLA on the skin. We’ve stopped using EMLA or lidocaine cream on the skin in ALA-PDT because of the very pronounced, enhanced photodynamic effects. You get great long-term results, but such a bad short-term result that lots of people didn’t want to go through it," said Dr. Ross of Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Using a topical numbing agent seemed to be an attractive option because patients often complain that photodynamic therapy (PDT) is painful. Plus, there seemed to be an added benefit: The anesthetic cream increased aminolevulanic acid (ALA) uptake by the skin, such that ALA incubation times before application of the light source could be greatly compressed. But clinical outcomes were too unpredictable, he said at the seminar sponsored by Skin Disease Education Foundation (SDEF). After several patients had unintended florid full photopeels involving 1½ weeks of downtime, it was time to abandon the practice.
When ALA-PDT first appeared about 10 years ago, the indication was for the treatment of actinic keratoses (AKs). Today this approved indication remains the No. 1 reason Dr. Ross utilizes the therapy, he said. But PDT’s role has expanded off label to include cosmetic procedures and the treatment of warts, nonmelanoma skin cancer, nevus sebaceous, as well as acne, which he considers "one of the great opportunities for PDT." In addition, in Asia, dermatologists are now refining the use of PDT with hematoporphyrin derivatives for the treatment of port wine stains and other vascular lesions.
Many U.S. dermatologists have incorporated PDT into their practices, with ALA being more widely used as a photosensitizer than methyl aminolevulinate (MAL). Yet PDT is a therapy that hasn’t been fully optimized; it is still fraught with side effects and suboptimal results, he said. Moreover, some fundamental issues regarding PDT remain unanswered: For example, the optimal duration of photosensitizer incubation time for various indications is still controversial.
Dr. Ross said he opts for what he considers a middle-of-the-road approach, with ALA application times of about 90-120 minutes, which he views as having an optimal balance between side effects and effectiveness. Even so, he noted that among the 8-10 patients per week he treats with ALA-PDT on average, 1 or 2 experience mild side effects.
"I don’t think we’re quite ‘there’ yet with PDT, although we’re getting closer. There are still so many tricks involved in making it work without side effects. We’ve still got some work to do," he said.
In addition to advising his colleagues to stay away from topical anesthetic creams, he offered additional tips for the use of ALA-PDT. Among them:
• Sending acne into long-term remission via PDT remains the Holy Grail, he said. The objective is to enhance the fluorescence of protoporphyrin 9 at the sebaceous gland while sparing the epidermis.
Some investigators are using low-intensity blue light at the skin surface while the photosensitizer is incubating in order to bleach it out of the epidermis, or, alternatively, warming and cooling the skin.
The best results Dr. Ross said he has seen have come through an arduous regimen involving three 3-hour-long ALA applications scheduled a month apart. There’s a delayed effect, with significant improvement coming at 3-6 months.
"It’s a tough, tough therapy to get through. There are lots of pustules and papules, and the acne invariably gets worse before it gets better. This doesn’t play into the hands of the typical teenager, who wants to get better right away," Dr. Ross said.
• A creamy solution of ALA will create more protoporphyrin 9 than an aqueous solution will.
• A red light source should be considered for deeper structures, such as basal cell carcinomas or sebaceous glands, and blue light for treating more superficial skin lesions. Although continuous blue light is 40 times more potent per photon than red light in exciting protoporphyrin 9, it doesn’t penetrate as deeply.
• Performing low-density fractional CO2 ablative laser therapy prior to application of the photosensitizing agent is "an exciting advance" in PDT, he said.
The innovation was developed by an international team led by investigators at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, who published a split-face randomized study involving 15 patients with a total of 212 facial AKs. At the 3-month follow-up, the complete response rate of grade II-III lesions treated with MAL-PDT preceded by fractional ablative laser therapy was 87.5%, vs. 58.8% with conventional MAL-PDT. The complete response rate of grade I AKs was 100% with fractional laser/MAL-PDT, vs. 79% for MAL-PDT alone.
The fractional laser–pretreated areas also displayed significantly greater improvement in photoaging and fewer new AKs at follow-up: 3, compared with 11. But these superior outcomes came at a price: higher pain scores during illumination and significantly worse erythema and crusting post treatment (Br. J. Dermatol. 2012 Feb. 20 [doi:10.1111/j.1365-2133.2012.10893.x]).
Fractional CO2 laser pretreatment enhances conversion of the photosensitizing agent to protoporphyrin 9, Dr. Ross explained. He compared the tiny holes in the skin created by the fractional laser to the process of aerating a lawn. The holes create conduits for the photosensitizer to bypass the stratum corneum, which is the major obstacle to uptake of ALA or MAL. Once the photosensitizer skips past the stratum corneum, it quickly spreads laterally throughout the epidermis.
However, Dr. Ross offered a note of caution regarding this novel approach. He said that he performed the therapy recently and found that 30 minutes of ALA incubation was too much.
"If you do these procedures, I would say go very light and just leave the ALA for less than 30 minutes to start, because the response you’re going to get when using a fractional laser beforehand is profound. It’s a huge difference," he said.
Dr. Ross reported that he serves as a consultant to and receives research support from Palomar. He also disclosed receiving research support from Candela, Cutera, Lumenis, Sciton, and Ulthera.
SDEF and this news organization are owned by Elsevier.
WAIKOLOA, HAWAII – Using EMLA or lidocaine cream in conjunction with topical 5-aminolevulinic acid photodynamic therapy may boost uptake of the photosensitizer, but the clinical outcomes can be unpredictable, according to Dr. E. Victor Ross.
"Our worst scenarios have been when we’ve used EMLA on the skin. We’ve stopped using EMLA or lidocaine cream on the skin in ALA-PDT because of the very pronounced, enhanced photodynamic effects. You get great long-term results, but such a bad short-term result that lots of people didn’t want to go through it," said Dr. Ross of Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Using a topical numbing agent seemed to be an attractive option because patients often complain that photodynamic therapy (PDT) is painful. Plus, there seemed to be an added benefit: The anesthetic cream increased aminolevulanic acid (ALA) uptake by the skin, such that ALA incubation times before application of the light source could be greatly compressed. But clinical outcomes were too unpredictable, he said at the seminar sponsored by Skin Disease Education Foundation (SDEF). After several patients had unintended florid full photopeels involving 1½ weeks of downtime, it was time to abandon the practice.
When ALA-PDT first appeared about 10 years ago, the indication was for the treatment of actinic keratoses (AKs). Today this approved indication remains the No. 1 reason Dr. Ross utilizes the therapy, he said. But PDT’s role has expanded off label to include cosmetic procedures and the treatment of warts, nonmelanoma skin cancer, nevus sebaceous, as well as acne, which he considers "one of the great opportunities for PDT." In addition, in Asia, dermatologists are now refining the use of PDT with hematoporphyrin derivatives for the treatment of port wine stains and other vascular lesions.
Many U.S. dermatologists have incorporated PDT into their practices, with ALA being more widely used as a photosensitizer than methyl aminolevulinate (MAL). Yet PDT is a therapy that hasn’t been fully optimized; it is still fraught with side effects and suboptimal results, he said. Moreover, some fundamental issues regarding PDT remain unanswered: For example, the optimal duration of photosensitizer incubation time for various indications is still controversial.
Dr. Ross said he opts for what he considers a middle-of-the-road approach, with ALA application times of about 90-120 minutes, which he views as having an optimal balance between side effects and effectiveness. Even so, he noted that among the 8-10 patients per week he treats with ALA-PDT on average, 1 or 2 experience mild side effects.
"I don’t think we’re quite ‘there’ yet with PDT, although we’re getting closer. There are still so many tricks involved in making it work without side effects. We’ve still got some work to do," he said.
In addition to advising his colleagues to stay away from topical anesthetic creams, he offered additional tips for the use of ALA-PDT. Among them:
• Sending acne into long-term remission via PDT remains the Holy Grail, he said. The objective is to enhance the fluorescence of protoporphyrin 9 at the sebaceous gland while sparing the epidermis.
Some investigators are using low-intensity blue light at the skin surface while the photosensitizer is incubating in order to bleach it out of the epidermis, or, alternatively, warming and cooling the skin.
The best results Dr. Ross said he has seen have come through an arduous regimen involving three 3-hour-long ALA applications scheduled a month apart. There’s a delayed effect, with significant improvement coming at 3-6 months.
"It’s a tough, tough therapy to get through. There are lots of pustules and papules, and the acne invariably gets worse before it gets better. This doesn’t play into the hands of the typical teenager, who wants to get better right away," Dr. Ross said.
• A creamy solution of ALA will create more protoporphyrin 9 than an aqueous solution will.
• A red light source should be considered for deeper structures, such as basal cell carcinomas or sebaceous glands, and blue light for treating more superficial skin lesions. Although continuous blue light is 40 times more potent per photon than red light in exciting protoporphyrin 9, it doesn’t penetrate as deeply.
• Performing low-density fractional CO2 ablative laser therapy prior to application of the photosensitizing agent is "an exciting advance" in PDT, he said.
The innovation was developed by an international team led by investigators at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, who published a split-face randomized study involving 15 patients with a total of 212 facial AKs. At the 3-month follow-up, the complete response rate of grade II-III lesions treated with MAL-PDT preceded by fractional ablative laser therapy was 87.5%, vs. 58.8% with conventional MAL-PDT. The complete response rate of grade I AKs was 100% with fractional laser/MAL-PDT, vs. 79% for MAL-PDT alone.
The fractional laser–pretreated areas also displayed significantly greater improvement in photoaging and fewer new AKs at follow-up: 3, compared with 11. But these superior outcomes came at a price: higher pain scores during illumination and significantly worse erythema and crusting post treatment (Br. J. Dermatol. 2012 Feb. 20 [doi:10.1111/j.1365-2133.2012.10893.x]).
Fractional CO2 laser pretreatment enhances conversion of the photosensitizing agent to protoporphyrin 9, Dr. Ross explained. He compared the tiny holes in the skin created by the fractional laser to the process of aerating a lawn. The holes create conduits for the photosensitizer to bypass the stratum corneum, which is the major obstacle to uptake of ALA or MAL. Once the photosensitizer skips past the stratum corneum, it quickly spreads laterally throughout the epidermis.
However, Dr. Ross offered a note of caution regarding this novel approach. He said that he performed the therapy recently and found that 30 minutes of ALA incubation was too much.
"If you do these procedures, I would say go very light and just leave the ALA for less than 30 minutes to start, because the response you’re going to get when using a fractional laser beforehand is profound. It’s a huge difference," he said.
Dr. Ross reported that he serves as a consultant to and receives research support from Palomar. He also disclosed receiving research support from Candela, Cutera, Lumenis, Sciton, and Ulthera.
SDEF and this news organization are owned by Elsevier.
WAIKOLOA, HAWAII – Using EMLA or lidocaine cream in conjunction with topical 5-aminolevulinic acid photodynamic therapy may boost uptake of the photosensitizer, but the clinical outcomes can be unpredictable, according to Dr. E. Victor Ross.
"Our worst scenarios have been when we’ve used EMLA on the skin. We’ve stopped using EMLA or lidocaine cream on the skin in ALA-PDT because of the very pronounced, enhanced photodynamic effects. You get great long-term results, but such a bad short-term result that lots of people didn’t want to go through it," said Dr. Ross of Scripps Clinic Laser and Cosmetic Dermatology Center in Carmel Valley, Calif.
Using a topical numbing agent seemed to be an attractive option because patients often complain that photodynamic therapy (PDT) is painful. Plus, there seemed to be an added benefit: The anesthetic cream increased aminolevulanic acid (ALA) uptake by the skin, such that ALA incubation times before application of the light source could be greatly compressed. But clinical outcomes were too unpredictable, he said at the seminar sponsored by Skin Disease Education Foundation (SDEF). After several patients had unintended florid full photopeels involving 1½ weeks of downtime, it was time to abandon the practice.
When ALA-PDT first appeared about 10 years ago, the indication was for the treatment of actinic keratoses (AKs). Today this approved indication remains the No. 1 reason Dr. Ross utilizes the therapy, he said. But PDT’s role has expanded off label to include cosmetic procedures and the treatment of warts, nonmelanoma skin cancer, nevus sebaceous, as well as acne, which he considers "one of the great opportunities for PDT." In addition, in Asia, dermatologists are now refining the use of PDT with hematoporphyrin derivatives for the treatment of port wine stains and other vascular lesions.
Many U.S. dermatologists have incorporated PDT into their practices, with ALA being more widely used as a photosensitizer than methyl aminolevulinate (MAL). Yet PDT is a therapy that hasn’t been fully optimized; it is still fraught with side effects and suboptimal results, he said. Moreover, some fundamental issues regarding PDT remain unanswered: For example, the optimal duration of photosensitizer incubation time for various indications is still controversial.
Dr. Ross said he opts for what he considers a middle-of-the-road approach, with ALA application times of about 90-120 minutes, which he views as having an optimal balance between side effects and effectiveness. Even so, he noted that among the 8-10 patients per week he treats with ALA-PDT on average, 1 or 2 experience mild side effects.
"I don’t think we’re quite ‘there’ yet with PDT, although we’re getting closer. There are still so many tricks involved in making it work without side effects. We’ve still got some work to do," he said.
In addition to advising his colleagues to stay away from topical anesthetic creams, he offered additional tips for the use of ALA-PDT. Among them:
• Sending acne into long-term remission via PDT remains the Holy Grail, he said. The objective is to enhance the fluorescence of protoporphyrin 9 at the sebaceous gland while sparing the epidermis.
Some investigators are using low-intensity blue light at the skin surface while the photosensitizer is incubating in order to bleach it out of the epidermis, or, alternatively, warming and cooling the skin.
The best results Dr. Ross said he has seen have come through an arduous regimen involving three 3-hour-long ALA applications scheduled a month apart. There’s a delayed effect, with significant improvement coming at 3-6 months.
"It’s a tough, tough therapy to get through. There are lots of pustules and papules, and the acne invariably gets worse before it gets better. This doesn’t play into the hands of the typical teenager, who wants to get better right away," Dr. Ross said.
• A creamy solution of ALA will create more protoporphyrin 9 than an aqueous solution will.
• A red light source should be considered for deeper structures, such as basal cell carcinomas or sebaceous glands, and blue light for treating more superficial skin lesions. Although continuous blue light is 40 times more potent per photon than red light in exciting protoporphyrin 9, it doesn’t penetrate as deeply.
• Performing low-density fractional CO2 ablative laser therapy prior to application of the photosensitizing agent is "an exciting advance" in PDT, he said.
The innovation was developed by an international team led by investigators at the Wellman Center for Photomedicine at Massachusetts General Hospital, Boston, who published a split-face randomized study involving 15 patients with a total of 212 facial AKs. At the 3-month follow-up, the complete response rate of grade II-III lesions treated with MAL-PDT preceded by fractional ablative laser therapy was 87.5%, vs. 58.8% with conventional MAL-PDT. The complete response rate of grade I AKs was 100% with fractional laser/MAL-PDT, vs. 79% for MAL-PDT alone.
The fractional laser–pretreated areas also displayed significantly greater improvement in photoaging and fewer new AKs at follow-up: 3, compared with 11. But these superior outcomes came at a price: higher pain scores during illumination and significantly worse erythema and crusting post treatment (Br. J. Dermatol. 2012 Feb. 20 [doi:10.1111/j.1365-2133.2012.10893.x]).
Fractional CO2 laser pretreatment enhances conversion of the photosensitizing agent to protoporphyrin 9, Dr. Ross explained. He compared the tiny holes in the skin created by the fractional laser to the process of aerating a lawn. The holes create conduits for the photosensitizer to bypass the stratum corneum, which is the major obstacle to uptake of ALA or MAL. Once the photosensitizer skips past the stratum corneum, it quickly spreads laterally throughout the epidermis.
However, Dr. Ross offered a note of caution regarding this novel approach. He said that he performed the therapy recently and found that 30 minutes of ALA incubation was too much.
"If you do these procedures, I would say go very light and just leave the ALA for less than 30 minutes to start, because the response you’re going to get when using a fractional laser beforehand is profound. It’s a huge difference," he said.
Dr. Ross reported that he serves as a consultant to and receives research support from Palomar. He also disclosed receiving research support from Candela, Cutera, Lumenis, Sciton, and Ulthera.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
'Early, Proactive' Management of Chemo Toxicites Improves QOL
Skin conditions in cancer patients can lead to a decreased quality of life because of the psychosocial impact, financial burden, poor health, and disruption of anticancer treatments, said Dr. Mario E. Lacouture at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF).
Clinical trials are underway to address management, cost, and quality of life, but in the meantime, "an early and proactive approach toward toxicities is advisable," he said.
Dr. Lacouture, a dermatologist at Memorial Sloan-Kettering Cancer Center in New York, discussed common cancer-associated dermatology at the seminar.
• Rashes. A RAF inhibitor–induced rash can occur within 1-2 weeks of starting treatment, Dr. Lacouture noted. This rash is associated with sensations of burning or itching in photo-exposed areas. In most cases, the rash can be managed with topical steroids and oral GABA agonists. Vemurafenib use also has been associated with rashes, as well as with photosensitivity, itching, and alopecia, he said.
In addition, mTOR inhibitor–induced rashes involving erythematous pruritic papules and ulcerlike lesions have been observed in patients on everolimus and temsirolimus.
• Skin cancers. Data from several studies suggest that the incidence of squamous cell carcinomas in patients on RAF inhibitors is 7%, and the incidence of actinic keratoses in these patients is 4%, according to Dr. Lacouture. These conditions usually develop after approximately 6 months of treatment. They can be managed by surgery or destruction; and there have been no reports of metastases.
• Hand-foot syndrome. Hand-Foot Syndrome (HFSR) is a common side effect in cancer patients that usually occurs within 45 days of starting treatment, said Dr. Lacouture. HFSR is often associated with the use of sorafenib, sunitinib, and pazopanib, and the histology of these patients shows epidermal necrosis, he noted. Patients who develop HFSR may need to temporarily reduce their medications. Additional management of HFSR includes avoiding excess pressure on the affected areas and keeping them cool and moist to reduce patient discomfort.
• Hair and nail changes. Changes in hair can occur in patients being treated with epidermal growth factor receptor inhibitors (EGFRIs), including a slower hair growth rate and alopecia, Dr. Lacouture said. Changes in hair texture such as increased brittleness and hair curling also have been observed, he said. Other hair-related adverse events can include hirsutism on the face and eyelash trichomegaly. In addition, paronychia has been observed in patients on EGFRIs for more than 6 months.
• Radiation dermatitis. Approximately 50% of cancer patients develop radiation dermatitis, including 87% of breast cancer patients, reported Dr. Lacouture. However, the treatment of radiation dermatitis remains challenging, he said. In several studies, patients who used a nonsteroidal topical, including aloe vera and trolamine, showed no significant improvement in radiation dermatitis, compared with controls. However, studies are ongoing, and significant improvements in radiation dermatitis in breast cancer patients have been seen with topical corticosteroids including mometasone, beclomethasone, and betamethasone.
Dr. Lacouture disclosed financial relationships with multiple companies including Amgen, Bristol-Myers Squibb, Genentech, GlaxoSmithKline, Merck, and Roche. SDEF and this news organization are owned by Elsevier.
Skin conditions in cancer patients can lead to a decreased quality of life because of the psychosocial impact, financial burden, poor health, and disruption of anticancer treatments, said Dr. Mario E. Lacouture at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF).
Clinical trials are underway to address management, cost, and quality of life, but in the meantime, "an early and proactive approach toward toxicities is advisable," he said.
Dr. Lacouture, a dermatologist at Memorial Sloan-Kettering Cancer Center in New York, discussed common cancer-associated dermatology at the seminar.
• Rashes. A RAF inhibitor–induced rash can occur within 1-2 weeks of starting treatment, Dr. Lacouture noted. This rash is associated with sensations of burning or itching in photo-exposed areas. In most cases, the rash can be managed with topical steroids and oral GABA agonists. Vemurafenib use also has been associated with rashes, as well as with photosensitivity, itching, and alopecia, he said.
In addition, mTOR inhibitor–induced rashes involving erythematous pruritic papules and ulcerlike lesions have been observed in patients on everolimus and temsirolimus.
• Skin cancers. Data from several studies suggest that the incidence of squamous cell carcinomas in patients on RAF inhibitors is 7%, and the incidence of actinic keratoses in these patients is 4%, according to Dr. Lacouture. These conditions usually develop after approximately 6 months of treatment. They can be managed by surgery or destruction; and there have been no reports of metastases.
• Hand-foot syndrome. Hand-Foot Syndrome (HFSR) is a common side effect in cancer patients that usually occurs within 45 days of starting treatment, said Dr. Lacouture. HFSR is often associated with the use of sorafenib, sunitinib, and pazopanib, and the histology of these patients shows epidermal necrosis, he noted. Patients who develop HFSR may need to temporarily reduce their medications. Additional management of HFSR includes avoiding excess pressure on the affected areas and keeping them cool and moist to reduce patient discomfort.
• Hair and nail changes. Changes in hair can occur in patients being treated with epidermal growth factor receptor inhibitors (EGFRIs), including a slower hair growth rate and alopecia, Dr. Lacouture said. Changes in hair texture such as increased brittleness and hair curling also have been observed, he said. Other hair-related adverse events can include hirsutism on the face and eyelash trichomegaly. In addition, paronychia has been observed in patients on EGFRIs for more than 6 months.
• Radiation dermatitis. Approximately 50% of cancer patients develop radiation dermatitis, including 87% of breast cancer patients, reported Dr. Lacouture. However, the treatment of radiation dermatitis remains challenging, he said. In several studies, patients who used a nonsteroidal topical, including aloe vera and trolamine, showed no significant improvement in radiation dermatitis, compared with controls. However, studies are ongoing, and significant improvements in radiation dermatitis in breast cancer patients have been seen with topical corticosteroids including mometasone, beclomethasone, and betamethasone.
Dr. Lacouture disclosed financial relationships with multiple companies including Amgen, Bristol-Myers Squibb, Genentech, GlaxoSmithKline, Merck, and Roche. SDEF and this news organization are owned by Elsevier.
Skin conditions in cancer patients can lead to a decreased quality of life because of the psychosocial impact, financial burden, poor health, and disruption of anticancer treatments, said Dr. Mario E. Lacouture at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF).
Clinical trials are underway to address management, cost, and quality of life, but in the meantime, "an early and proactive approach toward toxicities is advisable," he said.
Dr. Lacouture, a dermatologist at Memorial Sloan-Kettering Cancer Center in New York, discussed common cancer-associated dermatology at the seminar.
• Rashes. A RAF inhibitor–induced rash can occur within 1-2 weeks of starting treatment, Dr. Lacouture noted. This rash is associated with sensations of burning or itching in photo-exposed areas. In most cases, the rash can be managed with topical steroids and oral GABA agonists. Vemurafenib use also has been associated with rashes, as well as with photosensitivity, itching, and alopecia, he said.
In addition, mTOR inhibitor–induced rashes involving erythematous pruritic papules and ulcerlike lesions have been observed in patients on everolimus and temsirolimus.
• Skin cancers. Data from several studies suggest that the incidence of squamous cell carcinomas in patients on RAF inhibitors is 7%, and the incidence of actinic keratoses in these patients is 4%, according to Dr. Lacouture. These conditions usually develop after approximately 6 months of treatment. They can be managed by surgery or destruction; and there have been no reports of metastases.
• Hand-foot syndrome. Hand-Foot Syndrome (HFSR) is a common side effect in cancer patients that usually occurs within 45 days of starting treatment, said Dr. Lacouture. HFSR is often associated with the use of sorafenib, sunitinib, and pazopanib, and the histology of these patients shows epidermal necrosis, he noted. Patients who develop HFSR may need to temporarily reduce their medications. Additional management of HFSR includes avoiding excess pressure on the affected areas and keeping them cool and moist to reduce patient discomfort.
• Hair and nail changes. Changes in hair can occur in patients being treated with epidermal growth factor receptor inhibitors (EGFRIs), including a slower hair growth rate and alopecia, Dr. Lacouture said. Changes in hair texture such as increased brittleness and hair curling also have been observed, he said. Other hair-related adverse events can include hirsutism on the face and eyelash trichomegaly. In addition, paronychia has been observed in patients on EGFRIs for more than 6 months.
• Radiation dermatitis. Approximately 50% of cancer patients develop radiation dermatitis, including 87% of breast cancer patients, reported Dr. Lacouture. However, the treatment of radiation dermatitis remains challenging, he said. In several studies, patients who used a nonsteroidal topical, including aloe vera and trolamine, showed no significant improvement in radiation dermatitis, compared with controls. However, studies are ongoing, and significant improvements in radiation dermatitis in breast cancer patients have been seen with topical corticosteroids including mometasone, beclomethasone, and betamethasone.
Dr. Lacouture disclosed financial relationships with multiple companies including Amgen, Bristol-Myers Squibb, Genentech, GlaxoSmithKline, Merck, and Roche. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
Identifying AK Variants Is Key to Management
The ability to distinguish between the two key variants of actinic keratosis is key to effective management, according to Dr. Theodore Rosen.
Pigmented actinic keratosis (AK) that spreads typically occurs in patients older than age 60 years and affects more women than men. The lesions are larger than 1.5 cm and have a history of lateral spread. "The lesions are flat, with a smooth, scaly surface, and they occur on sun-exposed skin, mostly the face, and near other manifestations of photodamage," noted Dr. Rosen at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF).
Differential diagnosis includes solar lentigo, lentigo maligna, lentigo maligna melanoma, seborrheic keratosis, and pigmented squamous cell carcinoma in situ. "The presence of dots, globules, and asymmetry on dermatoscopy can help you distinguish spreading pigmented AKs from other lesions," said Dr. Rosen, professor of dermatology at Baylor College of Medicine, Houston.
The other main variant, proliferating AK, also tends to affect patients older than age 60 but it occurs more commonly in men than in women. This variant is greater than 1.5 cm in size with a history of rapid lateral spread, and it is marked by a confluent scaly surface with some palpability. Affected areas include sun-exposed skin, mostly the face, and areas near other manifestations of photodamage. "This variant is resistant to usual topical therapy, and the differential diagnosis may include eczema, psoriasis, squamous cell carcinoma in situ, and superficial basal cell carcinoma," said Dr. Rosen, who is also chief of the dermatology clinic at the Houston-based Michael E. DeBakey VA Medical Center. Histology reveals fingerlike invasive projections into the dermis of atypical squamous cells.
The appearance of multiple AKs in a cosmetic unit indicates that the clinician should consider the entire photodamaged area to be diseased. This concept, known as field-directed therapy, "not only addresses apparent clinical lesions, but also reveals and may treat subclinical lesions," he said. "Field therapy may also offer the advantage of reversing basic cellular aberrations leading to transition into invasive cutaneous malignancy."
Another trend in the treatment of AKs is the development of new imiquimod formulations. Results from two placebo-controlled studies of daily application of 2.5% and 3.75% imiquimod creams to the face and balding scalp for two 3-week cycles revealed that both formulations were more effective than placebo and had an acceptable safety profile (J. Am. Acad. Dermatol. 2010;62:573-81). The final evaluation occurred 8 weeks after the final treatment, said Dr. Rosen, who was one of the study investigators. Results from this and other studies led to Food and Drug Administration approval of imiquimod 2.5% (Zyclara) for AKs on July 19, 2011, but the formulation is not yet commercially available.
In a more recent analysis, investigators assessed complete clearance rates in AK patients from four phase III trials of imiquimod who were followed for 1 year (J. Drugs Dermatol. 2011;10:165-70). For imiquimod 3.75% and 2.5% cream, respectively, complete clearance was sustained for 1 year in 40.5% and 33.3% of patients from the 2-week cycle studies, and in 47.9% and 43.2% of patients from the 3-week cycle studies.
Combination therapies for AKs have become increasingly popular. Treatments include cryosurgery followed by diclofenac, 5-fluorouracil followed by cryosurgery, cryosurgery followed by imiquimod 5% or 3.75%, photodynamic therapy (PTD) followed by imiquimod 5%, and tazarotene followed by PDT. "For all studies where field therapy is combined with lesion-directed therapy or with another field therapy, the combination proved superior to monotherapy," Dr. Rosen said.
He went on to note that there is considerable user variation – such as time, the distance the device is held from the skin, and the type of unit used – in the delivery of cryosurgery to treat AKs. The variation "may have more to do with skin temperature than any other variable," said Dr. Rosen. In one study, investigators used an infrared detector in a liquid nitrogen container to deliver cryotherapy to a temperature of –5° C in 36 patients with 180 thin AKs (Dermatol. Surg. 2010;36:1956-61). The clearance rates were 67% at 1 week and 100% at 6 weeks.
Treatment of AKs with radiation is another area of study. In one recent trial, 12 patients with refractory AK and 4 patients with AKs near a nonmelanoma skin cancer underwent external beam radiation therapy five times a week for 4-6 weeks. The total dose of radiation ranged from 4 to 60 Gy (J. Clin. Aesthet. Dermatol. 2011;4:47-50). Of the 16 patients, 13 had complete resolution of AKs, 1 noted a prompt recurrence, and 90% said they were "very satisfied" with the treatment results.
Treating AKs with methyl aminolevulinate photodynamic therapy (MAL-PDT) is also being investigated. In a multicenter study conducted in Scandinavia, 120 patients with 1,572 AKs underwent MAL-PDT followed by immediate exposure to the sun for 1.5-2.5 hours (Br. J. Dermatol. 2011;164:1083-90). At 3 months, 75%-77% of the lesions had cleared. This approach "has an advantage for the health care provider in that no equipment is needed," Dr. Rosen said. "The advantage for the patient is that the therapy is nearly pain free."
Dr. Rosen disclosed that he is a consultant and a member of the speakers bureau for Medicis, which makes imiquimod. He is also a consultant for LEO Pharma.
SDEF and this news organization are owned by Elsevier.
The ability to distinguish between the two key variants of actinic keratosis is key to effective management, according to Dr. Theodore Rosen.
Pigmented actinic keratosis (AK) that spreads typically occurs in patients older than age 60 years and affects more women than men. The lesions are larger than 1.5 cm and have a history of lateral spread. "The lesions are flat, with a smooth, scaly surface, and they occur on sun-exposed skin, mostly the face, and near other manifestations of photodamage," noted Dr. Rosen at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF).
Differential diagnosis includes solar lentigo, lentigo maligna, lentigo maligna melanoma, seborrheic keratosis, and pigmented squamous cell carcinoma in situ. "The presence of dots, globules, and asymmetry on dermatoscopy can help you distinguish spreading pigmented AKs from other lesions," said Dr. Rosen, professor of dermatology at Baylor College of Medicine, Houston.
The other main variant, proliferating AK, also tends to affect patients older than age 60 but it occurs more commonly in men than in women. This variant is greater than 1.5 cm in size with a history of rapid lateral spread, and it is marked by a confluent scaly surface with some palpability. Affected areas include sun-exposed skin, mostly the face, and areas near other manifestations of photodamage. "This variant is resistant to usual topical therapy, and the differential diagnosis may include eczema, psoriasis, squamous cell carcinoma in situ, and superficial basal cell carcinoma," said Dr. Rosen, who is also chief of the dermatology clinic at the Houston-based Michael E. DeBakey VA Medical Center. Histology reveals fingerlike invasive projections into the dermis of atypical squamous cells.
The appearance of multiple AKs in a cosmetic unit indicates that the clinician should consider the entire photodamaged area to be diseased. This concept, known as field-directed therapy, "not only addresses apparent clinical lesions, but also reveals and may treat subclinical lesions," he said. "Field therapy may also offer the advantage of reversing basic cellular aberrations leading to transition into invasive cutaneous malignancy."
Another trend in the treatment of AKs is the development of new imiquimod formulations. Results from two placebo-controlled studies of daily application of 2.5% and 3.75% imiquimod creams to the face and balding scalp for two 3-week cycles revealed that both formulations were more effective than placebo and had an acceptable safety profile (J. Am. Acad. Dermatol. 2010;62:573-81). The final evaluation occurred 8 weeks after the final treatment, said Dr. Rosen, who was one of the study investigators. Results from this and other studies led to Food and Drug Administration approval of imiquimod 2.5% (Zyclara) for AKs on July 19, 2011, but the formulation is not yet commercially available.
In a more recent analysis, investigators assessed complete clearance rates in AK patients from four phase III trials of imiquimod who were followed for 1 year (J. Drugs Dermatol. 2011;10:165-70). For imiquimod 3.75% and 2.5% cream, respectively, complete clearance was sustained for 1 year in 40.5% and 33.3% of patients from the 2-week cycle studies, and in 47.9% and 43.2% of patients from the 3-week cycle studies.
Combination therapies for AKs have become increasingly popular. Treatments include cryosurgery followed by diclofenac, 5-fluorouracil followed by cryosurgery, cryosurgery followed by imiquimod 5% or 3.75%, photodynamic therapy (PTD) followed by imiquimod 5%, and tazarotene followed by PDT. "For all studies where field therapy is combined with lesion-directed therapy or with another field therapy, the combination proved superior to monotherapy," Dr. Rosen said.
He went on to note that there is considerable user variation – such as time, the distance the device is held from the skin, and the type of unit used – in the delivery of cryosurgery to treat AKs. The variation "may have more to do with skin temperature than any other variable," said Dr. Rosen. In one study, investigators used an infrared detector in a liquid nitrogen container to deliver cryotherapy to a temperature of –5° C in 36 patients with 180 thin AKs (Dermatol. Surg. 2010;36:1956-61). The clearance rates were 67% at 1 week and 100% at 6 weeks.
Treatment of AKs with radiation is another area of study. In one recent trial, 12 patients with refractory AK and 4 patients with AKs near a nonmelanoma skin cancer underwent external beam radiation therapy five times a week for 4-6 weeks. The total dose of radiation ranged from 4 to 60 Gy (J. Clin. Aesthet. Dermatol. 2011;4:47-50). Of the 16 patients, 13 had complete resolution of AKs, 1 noted a prompt recurrence, and 90% said they were "very satisfied" with the treatment results.
Treating AKs with methyl aminolevulinate photodynamic therapy (MAL-PDT) is also being investigated. In a multicenter study conducted in Scandinavia, 120 patients with 1,572 AKs underwent MAL-PDT followed by immediate exposure to the sun for 1.5-2.5 hours (Br. J. Dermatol. 2011;164:1083-90). At 3 months, 75%-77% of the lesions had cleared. This approach "has an advantage for the health care provider in that no equipment is needed," Dr. Rosen said. "The advantage for the patient is that the therapy is nearly pain free."
Dr. Rosen disclosed that he is a consultant and a member of the speakers bureau for Medicis, which makes imiquimod. He is also a consultant for LEO Pharma.
SDEF and this news organization are owned by Elsevier.
The ability to distinguish between the two key variants of actinic keratosis is key to effective management, according to Dr. Theodore Rosen.
Pigmented actinic keratosis (AK) that spreads typically occurs in patients older than age 60 years and affects more women than men. The lesions are larger than 1.5 cm and have a history of lateral spread. "The lesions are flat, with a smooth, scaly surface, and they occur on sun-exposed skin, mostly the face, and near other manifestations of photodamage," noted Dr. Rosen at the annual Hawaii Dermatology Seminar sponsored by Skin Disease Education Foundation (SDEF).
Differential diagnosis includes solar lentigo, lentigo maligna, lentigo maligna melanoma, seborrheic keratosis, and pigmented squamous cell carcinoma in situ. "The presence of dots, globules, and asymmetry on dermatoscopy can help you distinguish spreading pigmented AKs from other lesions," said Dr. Rosen, professor of dermatology at Baylor College of Medicine, Houston.
The other main variant, proliferating AK, also tends to affect patients older than age 60 but it occurs more commonly in men than in women. This variant is greater than 1.5 cm in size with a history of rapid lateral spread, and it is marked by a confluent scaly surface with some palpability. Affected areas include sun-exposed skin, mostly the face, and areas near other manifestations of photodamage. "This variant is resistant to usual topical therapy, and the differential diagnosis may include eczema, psoriasis, squamous cell carcinoma in situ, and superficial basal cell carcinoma," said Dr. Rosen, who is also chief of the dermatology clinic at the Houston-based Michael E. DeBakey VA Medical Center. Histology reveals fingerlike invasive projections into the dermis of atypical squamous cells.
The appearance of multiple AKs in a cosmetic unit indicates that the clinician should consider the entire photodamaged area to be diseased. This concept, known as field-directed therapy, "not only addresses apparent clinical lesions, but also reveals and may treat subclinical lesions," he said. "Field therapy may also offer the advantage of reversing basic cellular aberrations leading to transition into invasive cutaneous malignancy."
Another trend in the treatment of AKs is the development of new imiquimod formulations. Results from two placebo-controlled studies of daily application of 2.5% and 3.75% imiquimod creams to the face and balding scalp for two 3-week cycles revealed that both formulations were more effective than placebo and had an acceptable safety profile (J. Am. Acad. Dermatol. 2010;62:573-81). The final evaluation occurred 8 weeks after the final treatment, said Dr. Rosen, who was one of the study investigators. Results from this and other studies led to Food and Drug Administration approval of imiquimod 2.5% (Zyclara) for AKs on July 19, 2011, but the formulation is not yet commercially available.
In a more recent analysis, investigators assessed complete clearance rates in AK patients from four phase III trials of imiquimod who were followed for 1 year (J. Drugs Dermatol. 2011;10:165-70). For imiquimod 3.75% and 2.5% cream, respectively, complete clearance was sustained for 1 year in 40.5% and 33.3% of patients from the 2-week cycle studies, and in 47.9% and 43.2% of patients from the 3-week cycle studies.
Combination therapies for AKs have become increasingly popular. Treatments include cryosurgery followed by diclofenac, 5-fluorouracil followed by cryosurgery, cryosurgery followed by imiquimod 5% or 3.75%, photodynamic therapy (PTD) followed by imiquimod 5%, and tazarotene followed by PDT. "For all studies where field therapy is combined with lesion-directed therapy or with another field therapy, the combination proved superior to monotherapy," Dr. Rosen said.
He went on to note that there is considerable user variation – such as time, the distance the device is held from the skin, and the type of unit used – in the delivery of cryosurgery to treat AKs. The variation "may have more to do with skin temperature than any other variable," said Dr. Rosen. In one study, investigators used an infrared detector in a liquid nitrogen container to deliver cryotherapy to a temperature of –5° C in 36 patients with 180 thin AKs (Dermatol. Surg. 2010;36:1956-61). The clearance rates were 67% at 1 week and 100% at 6 weeks.
Treatment of AKs with radiation is another area of study. In one recent trial, 12 patients with refractory AK and 4 patients with AKs near a nonmelanoma skin cancer underwent external beam radiation therapy five times a week for 4-6 weeks. The total dose of radiation ranged from 4 to 60 Gy (J. Clin. Aesthet. Dermatol. 2011;4:47-50). Of the 16 patients, 13 had complete resolution of AKs, 1 noted a prompt recurrence, and 90% said they were "very satisfied" with the treatment results.
Treating AKs with methyl aminolevulinate photodynamic therapy (MAL-PDT) is also being investigated. In a multicenter study conducted in Scandinavia, 120 patients with 1,572 AKs underwent MAL-PDT followed by immediate exposure to the sun for 1.5-2.5 hours (Br. J. Dermatol. 2011;164:1083-90). At 3 months, 75%-77% of the lesions had cleared. This approach "has an advantage for the health care provider in that no equipment is needed," Dr. Rosen said. "The advantage for the patient is that the therapy is nearly pain free."
Dr. Rosen disclosed that he is a consultant and a member of the speakers bureau for Medicis, which makes imiquimod. He is also a consultant for LEO Pharma.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM THE SDEF HAWAII DERMATOLOGY SEMINAR
Picato Gel Approved to Treat Actinic Keratoses
The Food and Drug Administration approved two strengths of ingenol mebutate gel for the treatment of actinic keratoses Jan. 23.
The 0.015% formulation of ingenol mebutate gel (Picato) was approved for the treatment of lesions on the face and scalp once daily for 3 consecutive days; the 0.05% gel was cleared for once-daily treatment of the trunk and extremities for 3 consecutive days. The gel may be applied to the affected area, up to one contiguous skin area of about 25 cm2.
Ingenol mebutate is taken from the milky sap of a plant called radium weed – or Euphorbia peplus – which has been used traditionally as a treatment for skin conditions. It is thought that the treatment induces cell death, but the mechanism of action isn’t fully understood.
Approval was supported by four double-blind, vehicle (placebo)-controlled trials of about 1,000 patients, two of which were done in the trunk and extremities and the other two in the neck and scalp.
In the trunk and extremity studies, ingenol mebutate gel had a complete clearance rate (100% of lesions gone) of 28% and 42%, compared with 5% for the vehicle control in both studies. Partial clearance rates (at least 75% of lesions cleared) were 44% and 55%, vs. 7% for the vehicle control in both studies.
In the face and scalp studies, the complete clearance rates were 37% and 47%, vs. 2% and 5% for controls. Partial clearance rates came in at 60% and 68%, vs. 7% and 8% for vehicle controls.
The most common adverse events were local skin reactions, application site pain, and application site pruritus.
Manufacturer LEO Pharmaceuticals is planning to launch in the United States at the end of the first quarter or the beginning of the second quarter, President and CEO John Koconis said in an interview.
"The Pink Sheet" and this news organization are owned by Elsevier.
The Food and Drug Administration approved two strengths of ingenol mebutate gel for the treatment of actinic keratoses Jan. 23.
The 0.015% formulation of ingenol mebutate gel (Picato) was approved for the treatment of lesions on the face and scalp once daily for 3 consecutive days; the 0.05% gel was cleared for once-daily treatment of the trunk and extremities for 3 consecutive days. The gel may be applied to the affected area, up to one contiguous skin area of about 25 cm2.
Ingenol mebutate is taken from the milky sap of a plant called radium weed – or Euphorbia peplus – which has been used traditionally as a treatment for skin conditions. It is thought that the treatment induces cell death, but the mechanism of action isn’t fully understood.
Approval was supported by four double-blind, vehicle (placebo)-controlled trials of about 1,000 patients, two of which were done in the trunk and extremities and the other two in the neck and scalp.
In the trunk and extremity studies, ingenol mebutate gel had a complete clearance rate (100% of lesions gone) of 28% and 42%, compared with 5% for the vehicle control in both studies. Partial clearance rates (at least 75% of lesions cleared) were 44% and 55%, vs. 7% for the vehicle control in both studies.
In the face and scalp studies, the complete clearance rates were 37% and 47%, vs. 2% and 5% for controls. Partial clearance rates came in at 60% and 68%, vs. 7% and 8% for vehicle controls.
The most common adverse events were local skin reactions, application site pain, and application site pruritus.
Manufacturer LEO Pharmaceuticals is planning to launch in the United States at the end of the first quarter or the beginning of the second quarter, President and CEO John Koconis said in an interview.
"The Pink Sheet" and this news organization are owned by Elsevier.
The Food and Drug Administration approved two strengths of ingenol mebutate gel for the treatment of actinic keratoses Jan. 23.
The 0.015% formulation of ingenol mebutate gel (Picato) was approved for the treatment of lesions on the face and scalp once daily for 3 consecutive days; the 0.05% gel was cleared for once-daily treatment of the trunk and extremities for 3 consecutive days. The gel may be applied to the affected area, up to one contiguous skin area of about 25 cm2.
Ingenol mebutate is taken from the milky sap of a plant called radium weed – or Euphorbia peplus – which has been used traditionally as a treatment for skin conditions. It is thought that the treatment induces cell death, but the mechanism of action isn’t fully understood.
Approval was supported by four double-blind, vehicle (placebo)-controlled trials of about 1,000 patients, two of which were done in the trunk and extremities and the other two in the neck and scalp.
In the trunk and extremity studies, ingenol mebutate gel had a complete clearance rate (100% of lesions gone) of 28% and 42%, compared with 5% for the vehicle control in both studies. Partial clearance rates (at least 75% of lesions cleared) were 44% and 55%, vs. 7% for the vehicle control in both studies.
In the face and scalp studies, the complete clearance rates were 37% and 47%, vs. 2% and 5% for controls. Partial clearance rates came in at 60% and 68%, vs. 7% and 8% for vehicle controls.
The most common adverse events were local skin reactions, application site pain, and application site pruritus.
Manufacturer LEO Pharmaceuticals is planning to launch in the United States at the end of the first quarter or the beginning of the second quarter, President and CEO John Koconis said in an interview.
"The Pink Sheet" and this news organization are owned by Elsevier.
Blog: An Early Look at Caffeine for Cancer Prevention
The Mole: What prompted you to conduct this study?
Dr. Lizzul: Skin cancer of the nonmelanoma type (i.e., squamous cell and basal cell carcinoma) is the most common skin cancer and is most often a result of sunlight exposure. Ultraviolet B light is believed to be mostly responsible for these cancers. Many squamous cell skin cancers are curable if detected early. However, many people still suffer from these cancers and some also die from them. Actinic keratoses are precancerous skin tumors that mainly result from long-term sun exposure in susceptible persons. They have the potential to progress to squamous cell carcinoma. Finding effective methods of preventing UV-induced cancers and precancerous lesions would have a major impact on the total amount of human cancer.
The Mole: Could you briefly explain your hypothesis?
Dr. Conney: In studying the effect of tea on UVB carcinogenesisis in an animal model, we found that caffeine was the major active constituent, and that pure caffeine inhibited carcinogenesis in this animal model. Topical caffeine was also active. Topical caffeine inhibited carcinogenesis in mice pretreated with UVB with a high risk of skin cancer in the absence of further UVB. Mechanistic studies showed that caffeine enhanced apoptosis (programmed cell death) in UVB-treated epidermis and in tumors. We hypothesize that topical caffeine will inhibit proliferation and stimulate apoptosis in the actinic keratoses.
Dr. Lizzul: The hypothesis to be tested in this study is that treatment of actinic keratoses with caffeine for 2 weeks will enhance apoptosis and inhibit the growth of these skin lesions in humans. The purpose of this study is to determine the effects of topical applications of caffeine on apoptosis (programmed cell death), proliferation, and the ATR/Chk1 pathway in actinic keratoses in human skin in vivo.
Our collaborators at Rutgers University found that treatment of UVB-pretreated high-risk mice with caffeine topically once a day, 5 days a week for 18 weeks inhibited the formation of keratoacanthomas and squamous cell carcinomas, decreased the size of the tumors, and enhanced apoptosis in the tumor. In an additional study, they found that treatment of high-risk mice topically with caffeine once a day for 3 or 14 days enhanced apoptosis in focal hyperplastic areas of the epidermis but not in diffuse hyperplastic areas.
We anticipate that most keratoses will have evidence of DNA damage and a p53 mutation and that treatment of the keratoses with caffeine for two weeks will stimulate apoptosis substantially and have a smaller inhibitory effect on proliferation. If our hypothesis that topical applications of caffeine to keratoses enhances apoptosis, this regimen may be helpful in decreasing the numbers of keratoses and inhibiting the formation of squamous cell carcinomas.
The Mole: Could you briefly explain the study protocol?
Dr. Lizzul: This is an investigator-initiated, randomized, double-blind, placebo-controlled trial of topical caffeine 6% vs. placebo for actinic keratosis.
The study visits will take place over four or five nonconsecutive days. A skin biopsy is conducted at study onset, then subjects will initiate treatment with topical caffeine or placebo at the study site.
They will be treating their lesions with either topical caffeine or placebo, three times daily for two weeks. Two weeks after the initiation of treatment, another skin biopsy is performed. A portion of the biopsy from the lesion will undergo diagnostic histopathology and the other portion will be evaluated for markers of proliferation and apoptosis. Saliva will also be collected from each subject before and after study cream treatment to detect salivary caffeine level by HPLC. Salivary caffeine levels will be used as an indicator of systemic absorption.
The Mole: Although this is a preliminary study, can you speculate on the eventual clinical implications of your research?
Dr. Lizzul: This study, if successful, will be a prelude to additional studies to determine whether topical applications of caffeine will inhibit the formation or cause regression of these lesions in high-risk individuals.
The Mole: What are the next steps for research on this topic?
Dr. Lizzul: In addition, a goal of this study is to develop additional information regarding possible health benefits of commonly used natural products, specifically caffeine, in the prevention and possible treatment of actinic keratoses, which may eventually progress to squamous cell carcinomas.
Moreover, once this phase I study in complete, and the data are analyzed, we would move on to a larger phase II study, with increased number of patients, a longer time period of treatment and follow up, and dose ranging exploration to identify an optimal time period and concentration of topical caffeine that would be used to treat actinic keratosis and/or skin cancers, such as squamous cell carcinoma (SCC), or even basal cell carcinoma (BCC).
Finally, it is important to recognize our co-investigator and chair of the department of dermatology at Tufts, Dr. Alice B. Gottlieb, as well dermatology resident Andrew Wang, and Tufts medical student Ari Goldminz, for their work.
—Heidi Splete (on Twitter @hsplete)
The Mole: What prompted you to conduct this study?
Dr. Lizzul: Skin cancer of the nonmelanoma type (i.e., squamous cell and basal cell carcinoma) is the most common skin cancer and is most often a result of sunlight exposure. Ultraviolet B light is believed to be mostly responsible for these cancers. Many squamous cell skin cancers are curable if detected early. However, many people still suffer from these cancers and some also die from them. Actinic keratoses are precancerous skin tumors that mainly result from long-term sun exposure in susceptible persons. They have the potential to progress to squamous cell carcinoma. Finding effective methods of preventing UV-induced cancers and precancerous lesions would have a major impact on the total amount of human cancer.
The Mole: Could you briefly explain your hypothesis?
Dr. Conney: In studying the effect of tea on UVB carcinogenesisis in an animal model, we found that caffeine was the major active constituent, and that pure caffeine inhibited carcinogenesis in this animal model. Topical caffeine was also active. Topical caffeine inhibited carcinogenesis in mice pretreated with UVB with a high risk of skin cancer in the absence of further UVB. Mechanistic studies showed that caffeine enhanced apoptosis (programmed cell death) in UVB-treated epidermis and in tumors. We hypothesize that topical caffeine will inhibit proliferation and stimulate apoptosis in the actinic keratoses.
Dr. Lizzul: The hypothesis to be tested in this study is that treatment of actinic keratoses with caffeine for 2 weeks will enhance apoptosis and inhibit the growth of these skin lesions in humans. The purpose of this study is to determine the effects of topical applications of caffeine on apoptosis (programmed cell death), proliferation, and the ATR/Chk1 pathway in actinic keratoses in human skin in vivo.
Our collaborators at Rutgers University found that treatment of UVB-pretreated high-risk mice with caffeine topically once a day, 5 days a week for 18 weeks inhibited the formation of keratoacanthomas and squamous cell carcinomas, decreased the size of the tumors, and enhanced apoptosis in the tumor. In an additional study, they found that treatment of high-risk mice topically with caffeine once a day for 3 or 14 days enhanced apoptosis in focal hyperplastic areas of the epidermis but not in diffuse hyperplastic areas.
We anticipate that most keratoses will have evidence of DNA damage and a p53 mutation and that treatment of the keratoses with caffeine for two weeks will stimulate apoptosis substantially and have a smaller inhibitory effect on proliferation. If our hypothesis that topical applications of caffeine to keratoses enhances apoptosis, this regimen may be helpful in decreasing the numbers of keratoses and inhibiting the formation of squamous cell carcinomas.
The Mole: Could you briefly explain the study protocol?
Dr. Lizzul: This is an investigator-initiated, randomized, double-blind, placebo-controlled trial of topical caffeine 6% vs. placebo for actinic keratosis.
The study visits will take place over four or five nonconsecutive days. A skin biopsy is conducted at study onset, then subjects will initiate treatment with topical caffeine or placebo at the study site.
They will be treating their lesions with either topical caffeine or placebo, three times daily for two weeks. Two weeks after the initiation of treatment, another skin biopsy is performed. A portion of the biopsy from the lesion will undergo diagnostic histopathology and the other portion will be evaluated for markers of proliferation and apoptosis. Saliva will also be collected from each subject before and after study cream treatment to detect salivary caffeine level by HPLC. Salivary caffeine levels will be used as an indicator of systemic absorption.
The Mole: Although this is a preliminary study, can you speculate on the eventual clinical implications of your research?
Dr. Lizzul: This study, if successful, will be a prelude to additional studies to determine whether topical applications of caffeine will inhibit the formation or cause regression of these lesions in high-risk individuals.
The Mole: What are the next steps for research on this topic?
Dr. Lizzul: In addition, a goal of this study is to develop additional information regarding possible health benefits of commonly used natural products, specifically caffeine, in the prevention and possible treatment of actinic keratoses, which may eventually progress to squamous cell carcinomas.
Moreover, once this phase I study in complete, and the data are analyzed, we would move on to a larger phase II study, with increased number of patients, a longer time period of treatment and follow up, and dose ranging exploration to identify an optimal time period and concentration of topical caffeine that would be used to treat actinic keratosis and/or skin cancers, such as squamous cell carcinoma (SCC), or even basal cell carcinoma (BCC).
Finally, it is important to recognize our co-investigator and chair of the department of dermatology at Tufts, Dr. Alice B. Gottlieb, as well dermatology resident Andrew Wang, and Tufts medical student Ari Goldminz, for their work.
—Heidi Splete (on Twitter @hsplete)
The Mole: What prompted you to conduct this study?
Dr. Lizzul: Skin cancer of the nonmelanoma type (i.e., squamous cell and basal cell carcinoma) is the most common skin cancer and is most often a result of sunlight exposure. Ultraviolet B light is believed to be mostly responsible for these cancers. Many squamous cell skin cancers are curable if detected early. However, many people still suffer from these cancers and some also die from them. Actinic keratoses are precancerous skin tumors that mainly result from long-term sun exposure in susceptible persons. They have the potential to progress to squamous cell carcinoma. Finding effective methods of preventing UV-induced cancers and precancerous lesions would have a major impact on the total amount of human cancer.
The Mole: Could you briefly explain your hypothesis?
Dr. Conney: In studying the effect of tea on UVB carcinogenesisis in an animal model, we found that caffeine was the major active constituent, and that pure caffeine inhibited carcinogenesis in this animal model. Topical caffeine was also active. Topical caffeine inhibited carcinogenesis in mice pretreated with UVB with a high risk of skin cancer in the absence of further UVB. Mechanistic studies showed that caffeine enhanced apoptosis (programmed cell death) in UVB-treated epidermis and in tumors. We hypothesize that topical caffeine will inhibit proliferation and stimulate apoptosis in the actinic keratoses.
Dr. Lizzul: The hypothesis to be tested in this study is that treatment of actinic keratoses with caffeine for 2 weeks will enhance apoptosis and inhibit the growth of these skin lesions in humans. The purpose of this study is to determine the effects of topical applications of caffeine on apoptosis (programmed cell death), proliferation, and the ATR/Chk1 pathway in actinic keratoses in human skin in vivo.
Our collaborators at Rutgers University found that treatment of UVB-pretreated high-risk mice with caffeine topically once a day, 5 days a week for 18 weeks inhibited the formation of keratoacanthomas and squamous cell carcinomas, decreased the size of the tumors, and enhanced apoptosis in the tumor. In an additional study, they found that treatment of high-risk mice topically with caffeine once a day for 3 or 14 days enhanced apoptosis in focal hyperplastic areas of the epidermis but not in diffuse hyperplastic areas.
We anticipate that most keratoses will have evidence of DNA damage and a p53 mutation and that treatment of the keratoses with caffeine for two weeks will stimulate apoptosis substantially and have a smaller inhibitory effect on proliferation. If our hypothesis that topical applications of caffeine to keratoses enhances apoptosis, this regimen may be helpful in decreasing the numbers of keratoses and inhibiting the formation of squamous cell carcinomas.
The Mole: Could you briefly explain the study protocol?
Dr. Lizzul: This is an investigator-initiated, randomized, double-blind, placebo-controlled trial of topical caffeine 6% vs. placebo for actinic keratosis.
The study visits will take place over four or five nonconsecutive days. A skin biopsy is conducted at study onset, then subjects will initiate treatment with topical caffeine or placebo at the study site.
They will be treating their lesions with either topical caffeine or placebo, three times daily for two weeks. Two weeks after the initiation of treatment, another skin biopsy is performed. A portion of the biopsy from the lesion will undergo diagnostic histopathology and the other portion will be evaluated for markers of proliferation and apoptosis. Saliva will also be collected from each subject before and after study cream treatment to detect salivary caffeine level by HPLC. Salivary caffeine levels will be used as an indicator of systemic absorption.
The Mole: Although this is a preliminary study, can you speculate on the eventual clinical implications of your research?
Dr. Lizzul: This study, if successful, will be a prelude to additional studies to determine whether topical applications of caffeine will inhibit the formation or cause regression of these lesions in high-risk individuals.
The Mole: What are the next steps for research on this topic?
Dr. Lizzul: In addition, a goal of this study is to develop additional information regarding possible health benefits of commonly used natural products, specifically caffeine, in the prevention and possible treatment of actinic keratoses, which may eventually progress to squamous cell carcinomas.
Moreover, once this phase I study in complete, and the data are analyzed, we would move on to a larger phase II study, with increased number of patients, a longer time period of treatment and follow up, and dose ranging exploration to identify an optimal time period and concentration of topical caffeine that would be used to treat actinic keratosis and/or skin cancers, such as squamous cell carcinoma (SCC), or even basal cell carcinoma (BCC).
Finally, it is important to recognize our co-investigator and chair of the department of dermatology at Tufts, Dr. Alice B. Gottlieb, as well dermatology resident Andrew Wang, and Tufts medical student Ari Goldminz, for their work.
—Heidi Splete (on Twitter @hsplete)
Lines Blur Between Dysplasia, Carcinoma in Situ
SAN DIEGO – It’s not getting any easier to make the histological distinction between carcinoma in situ and simple dysplasia in a sun-damaged epidermis, but it may be getting less critical to get it right, noted Dr. John B. Campbell.
During his presentation at a meeting sponsored by the American Society for Mohs Surgery, Dr. Campbell, a Mohs pathologist in private practice in San Diego, showed slides depicting disorderly cells that typify dysplasia extending high up into the epidermis along the edges of specimens containing in situ carcinoma. "There are a lot of things that go along with dysplastic changes," he said. "The nuclei become larger; they stain darker; they have less cytoplasm so that the N/C [nuclear to cytoplasmic] ratio increases."
"At some place along the edges of the specimen you’re going to have to draw a line between in situ carcinoma and simple dysplasia. There are gradations that are somewhat subjective."
Pathologists commonly envision a line midway through the epidermis. If the dark and disorganized cells reach that point, they call it "moderate dysplasia." If they’re clumped in the lower third of the epidermis, it merits a call of "mild dysplasia," and if they extend to near the surface, it’s "severe."
"Dysplastic changes that are wall-to-wall, top-to-bottom are carcinoma in situ," he said. "You’ll need to develop criteria on your own."
In the meantime, the pressure to make the right call may be easing.
"What I’ve seen happening in the last few years is that we’re becoming less and less sensitive about dysplasia at the edges of in situ carcinomas because we can treat them so easily topically," said Dr. Campbell. Beyond watchful waiting or freezing, such regions can now be well managed with topical therapies such as Aldara (imiquimod) or Efudex (fluorouracil).
"Once we’ve cleared the unequivocal carcinoma in situ, people are letting a significant amount of dysplasia remain and then treating it in follow-up.
"There’s really no downside to [conservative or topical management] as long as the patient is reliable," he said.
Taking a careful look at the site during follow-up visits will easily reveal any cell changes that might prompt a fresh biopsy. One finding of note in such cases is the proclivity of dysplastic cells to take a downward course along appendage structures such as eccrine ducts and follicles in the epithelium. "They can go down quite deep ... maybe 2 mm deep to the surface," he said.
In his practice, Dr. Campbell and his colleagues characterize such findings as "advanced actinic keratoses," and note the presence of dysplastic cells along appendage structures.
Dr. Campbell reported no relevant disclosures.
SAN DIEGO – It’s not getting any easier to make the histological distinction between carcinoma in situ and simple dysplasia in a sun-damaged epidermis, but it may be getting less critical to get it right, noted Dr. John B. Campbell.
During his presentation at a meeting sponsored by the American Society for Mohs Surgery, Dr. Campbell, a Mohs pathologist in private practice in San Diego, showed slides depicting disorderly cells that typify dysplasia extending high up into the epidermis along the edges of specimens containing in situ carcinoma. "There are a lot of things that go along with dysplastic changes," he said. "The nuclei become larger; they stain darker; they have less cytoplasm so that the N/C [nuclear to cytoplasmic] ratio increases."
"At some place along the edges of the specimen you’re going to have to draw a line between in situ carcinoma and simple dysplasia. There are gradations that are somewhat subjective."
Pathologists commonly envision a line midway through the epidermis. If the dark and disorganized cells reach that point, they call it "moderate dysplasia." If they’re clumped in the lower third of the epidermis, it merits a call of "mild dysplasia," and if they extend to near the surface, it’s "severe."
"Dysplastic changes that are wall-to-wall, top-to-bottom are carcinoma in situ," he said. "You’ll need to develop criteria on your own."
In the meantime, the pressure to make the right call may be easing.
"What I’ve seen happening in the last few years is that we’re becoming less and less sensitive about dysplasia at the edges of in situ carcinomas because we can treat them so easily topically," said Dr. Campbell. Beyond watchful waiting or freezing, such regions can now be well managed with topical therapies such as Aldara (imiquimod) or Efudex (fluorouracil).
"Once we’ve cleared the unequivocal carcinoma in situ, people are letting a significant amount of dysplasia remain and then treating it in follow-up.
"There’s really no downside to [conservative or topical management] as long as the patient is reliable," he said.
Taking a careful look at the site during follow-up visits will easily reveal any cell changes that might prompt a fresh biopsy. One finding of note in such cases is the proclivity of dysplastic cells to take a downward course along appendage structures such as eccrine ducts and follicles in the epithelium. "They can go down quite deep ... maybe 2 mm deep to the surface," he said.
In his practice, Dr. Campbell and his colleagues characterize such findings as "advanced actinic keratoses," and note the presence of dysplastic cells along appendage structures.
Dr. Campbell reported no relevant disclosures.
SAN DIEGO – It’s not getting any easier to make the histological distinction between carcinoma in situ and simple dysplasia in a sun-damaged epidermis, but it may be getting less critical to get it right, noted Dr. John B. Campbell.
During his presentation at a meeting sponsored by the American Society for Mohs Surgery, Dr. Campbell, a Mohs pathologist in private practice in San Diego, showed slides depicting disorderly cells that typify dysplasia extending high up into the epidermis along the edges of specimens containing in situ carcinoma. "There are a lot of things that go along with dysplastic changes," he said. "The nuclei become larger; they stain darker; they have less cytoplasm so that the N/C [nuclear to cytoplasmic] ratio increases."
"At some place along the edges of the specimen you’re going to have to draw a line between in situ carcinoma and simple dysplasia. There are gradations that are somewhat subjective."
Pathologists commonly envision a line midway through the epidermis. If the dark and disorganized cells reach that point, they call it "moderate dysplasia." If they’re clumped in the lower third of the epidermis, it merits a call of "mild dysplasia," and if they extend to near the surface, it’s "severe."
"Dysplastic changes that are wall-to-wall, top-to-bottom are carcinoma in situ," he said. "You’ll need to develop criteria on your own."
In the meantime, the pressure to make the right call may be easing.
"What I’ve seen happening in the last few years is that we’re becoming less and less sensitive about dysplasia at the edges of in situ carcinomas because we can treat them so easily topically," said Dr. Campbell. Beyond watchful waiting or freezing, such regions can now be well managed with topical therapies such as Aldara (imiquimod) or Efudex (fluorouracil).
"Once we’ve cleared the unequivocal carcinoma in situ, people are letting a significant amount of dysplasia remain and then treating it in follow-up.
"There’s really no downside to [conservative or topical management] as long as the patient is reliable," he said.
Taking a careful look at the site during follow-up visits will easily reveal any cell changes that might prompt a fresh biopsy. One finding of note in such cases is the proclivity of dysplastic cells to take a downward course along appendage structures such as eccrine ducts and follicles in the epithelium. "They can go down quite deep ... maybe 2 mm deep to the surface," he said.
In his practice, Dr. Campbell and his colleagues characterize such findings as "advanced actinic keratoses," and note the presence of dysplastic cells along appendage structures.
Dr. Campbell reported no relevant disclosures.
EXPERT ANALYSIS FROM A MEETING SPONSORED BY THE AMERICAN SOCIETY FOR MOHS SURGERY
Expert: Risk of AK Progression to SCC Hard to Predict
NAPA, CALIF. – Because actinic keratoses are the most common lesions with premalignant potential in the skin, knowing how to predict their malignancy can be life saving, according to Dr. Miriam S. Bettencourt.
Most AKs do not progress to squamous cell carcinoma (SCC), but most invasive SCCs have evidence of preexisting AK, she said. Of the AKs that progress, 10% will metastasize, giving patients a 5-year survival rate, Dr. Bettencourt of the University of Nevada, Las Vegas.
"Major risk factors for AK malignancy include induration and inflammation, a diameter of over 1 cm, rapid enlargement, bleeding, erythema, and ulceration. Minor risk factors include pigmentation changes, palpability, pain, pruritus, and hyperkeratosis.
Hyperkeratotic AKs greater than 1 cm on the hands, wrists, or forearms have a 50% or greater risk for malignancy, she noted.
Other risk factors include age at diagnosis, human papillomavirus status, skin type, sunburns during childhood, proximity to the Equator, amount of outdoor activity, and a history of skin cancer.
Organ-transplant recipients have a 250-fold greater risk for developing AKs, and a 100-fold risk for SCC; 40% of organ-transplant patients with an AK will show progression to SCC, compared with 10% of the average population, she said.
However, the wide range of rates for the risk of AK progression to SCC found in the literature highlights the difficulty of putting risk into perspective, she noted.
In one study, of 169 patients with AKs, 65% developed an SCC from an AK; 97% of the patients had a contiguous AK near the site of the SCC (Dermatol. Surg. 1995;21:184). But a review of 875 studies of AKs found a much lower rate; 11 studies were identified that predicted the risk of malignancy. The review found the rate to be 0.025% to 10% per lesion, per year (Eur. J. Dermatol. 2006;16:335-9).
In another study, 10% of AKs were found to transform into SCC in 2 years (Dermatol. Surg. 2007;33:1099-101).
A more recent report suggests that AKs also may progress to basal cell carcinomas (BCCs), she reported. In a study of 7,784 lesions on the face and ears of 169 patients, 65% of SCCs and 36% of BCCs arose in lesions that were previously diagnosed as AKs (Cancer 2009;115:2523-30). The study also found the risk of progression of AK to SCC to be 0.6% at year 1 and 2.6% at year 4.
It is important to remember that risk applies to each individual AK and that the fate of any one AK is impossible to predict, said Dr. Bettencourt. "Although the risk [of progression] is small, since most [patients] have multiple AKs, the risk of transformation is much greater than the risk of any individual lesion."
She recommended treating all AKs because some may be difficult to distinguish from SCC and lentigo maligna.
Dr. Bettencourt reported being on the speakers bureaus of PharmaDerm and Graceway, and conducting clinical trials for 3M Pharmaceuticals.
NAPA, CALIF. – Because actinic keratoses are the most common lesions with premalignant potential in the skin, knowing how to predict their malignancy can be life saving, according to Dr. Miriam S. Bettencourt.
Most AKs do not progress to squamous cell carcinoma (SCC), but most invasive SCCs have evidence of preexisting AK, she said. Of the AKs that progress, 10% will metastasize, giving patients a 5-year survival rate, Dr. Bettencourt of the University of Nevada, Las Vegas.
"Major risk factors for AK malignancy include induration and inflammation, a diameter of over 1 cm, rapid enlargement, bleeding, erythema, and ulceration. Minor risk factors include pigmentation changes, palpability, pain, pruritus, and hyperkeratosis.
Hyperkeratotic AKs greater than 1 cm on the hands, wrists, or forearms have a 50% or greater risk for malignancy, she noted.
Other risk factors include age at diagnosis, human papillomavirus status, skin type, sunburns during childhood, proximity to the Equator, amount of outdoor activity, and a history of skin cancer.
Organ-transplant recipients have a 250-fold greater risk for developing AKs, and a 100-fold risk for SCC; 40% of organ-transplant patients with an AK will show progression to SCC, compared with 10% of the average population, she said.
However, the wide range of rates for the risk of AK progression to SCC found in the literature highlights the difficulty of putting risk into perspective, she noted.
In one study, of 169 patients with AKs, 65% developed an SCC from an AK; 97% of the patients had a contiguous AK near the site of the SCC (Dermatol. Surg. 1995;21:184). But a review of 875 studies of AKs found a much lower rate; 11 studies were identified that predicted the risk of malignancy. The review found the rate to be 0.025% to 10% per lesion, per year (Eur. J. Dermatol. 2006;16:335-9).
In another study, 10% of AKs were found to transform into SCC in 2 years (Dermatol. Surg. 2007;33:1099-101).
A more recent report suggests that AKs also may progress to basal cell carcinomas (BCCs), she reported. In a study of 7,784 lesions on the face and ears of 169 patients, 65% of SCCs and 36% of BCCs arose in lesions that were previously diagnosed as AKs (Cancer 2009;115:2523-30). The study also found the risk of progression of AK to SCC to be 0.6% at year 1 and 2.6% at year 4.
It is important to remember that risk applies to each individual AK and that the fate of any one AK is impossible to predict, said Dr. Bettencourt. "Although the risk [of progression] is small, since most [patients] have multiple AKs, the risk of transformation is much greater than the risk of any individual lesion."
She recommended treating all AKs because some may be difficult to distinguish from SCC and lentigo maligna.
Dr. Bettencourt reported being on the speakers bureaus of PharmaDerm and Graceway, and conducting clinical trials for 3M Pharmaceuticals.
NAPA, CALIF. – Because actinic keratoses are the most common lesions with premalignant potential in the skin, knowing how to predict their malignancy can be life saving, according to Dr. Miriam S. Bettencourt.
Most AKs do not progress to squamous cell carcinoma (SCC), but most invasive SCCs have evidence of preexisting AK, she said. Of the AKs that progress, 10% will metastasize, giving patients a 5-year survival rate, Dr. Bettencourt of the University of Nevada, Las Vegas.
"Major risk factors for AK malignancy include induration and inflammation, a diameter of over 1 cm, rapid enlargement, bleeding, erythema, and ulceration. Minor risk factors include pigmentation changes, palpability, pain, pruritus, and hyperkeratosis.
Hyperkeratotic AKs greater than 1 cm on the hands, wrists, or forearms have a 50% or greater risk for malignancy, she noted.
Other risk factors include age at diagnosis, human papillomavirus status, skin type, sunburns during childhood, proximity to the Equator, amount of outdoor activity, and a history of skin cancer.
Organ-transplant recipients have a 250-fold greater risk for developing AKs, and a 100-fold risk for SCC; 40% of organ-transplant patients with an AK will show progression to SCC, compared with 10% of the average population, she said.
However, the wide range of rates for the risk of AK progression to SCC found in the literature highlights the difficulty of putting risk into perspective, she noted.
In one study, of 169 patients with AKs, 65% developed an SCC from an AK; 97% of the patients had a contiguous AK near the site of the SCC (Dermatol. Surg. 1995;21:184). But a review of 875 studies of AKs found a much lower rate; 11 studies were identified that predicted the risk of malignancy. The review found the rate to be 0.025% to 10% per lesion, per year (Eur. J. Dermatol. 2006;16:335-9).
In another study, 10% of AKs were found to transform into SCC in 2 years (Dermatol. Surg. 2007;33:1099-101).
A more recent report suggests that AKs also may progress to basal cell carcinomas (BCCs), she reported. In a study of 7,784 lesions on the face and ears of 169 patients, 65% of SCCs and 36% of BCCs arose in lesions that were previously diagnosed as AKs (Cancer 2009;115:2523-30). The study also found the risk of progression of AK to SCC to be 0.6% at year 1 and 2.6% at year 4.
It is important to remember that risk applies to each individual AK and that the fate of any one AK is impossible to predict, said Dr. Bettencourt. "Although the risk [of progression] is small, since most [patients] have multiple AKs, the risk of transformation is much greater than the risk of any individual lesion."
She recommended treating all AKs because some may be difficult to distinguish from SCC and lentigo maligna.
Dr. Bettencourt reported being on the speakers bureaus of PharmaDerm and Graceway, and conducting clinical trials for 3M Pharmaceuticals.
EXPERT ANALYSIS FROM THE COASTAL DERMATOLOGY SYMPOSISUM