User login
Anticoagulation not routinely needed after TAVR: ADAPT-TAVR
In patients undergoing transcatheter aortic valve replacement (TAVR), the incidence of leaflet thrombosis was numerically lower in those treated with the anticoagulant edoxaban for 6 months after the procedure than in those who received dual antiplatelet therapy, although the difference was not statistically significant, in the ADAPT-TAVR study.
There was no difference in new cerebral thromboembolism or neurologic/neurocognitive function between the two groups in the study.
Also, there was no significant relation between subclinical leaflet thrombosis and increased risk for cerebral thromboembolism and neurologic dysfunction.
The ADAPT-TAVR trial was presented April 4 at the American College of Cardiology (ACC) 2022 Scientific Session by Duk-Woo Park, MD, Asan Medical Center, Seoul, South Korea. It was simultaneously published online in Circulation.
“The key messages from this study are that subclinical leaflet thrombosis has not been proven to affect clinical outcomes for patients undergoing valve replacement and that in patients in whom leaflet thrombosis causes no symptoms or complications, its presence should not dictate the type of antithrombotic therapy that patients receive following the implantation of an artificial heart valve,” Dr. Park said.
“These findings do not support the routine use of computed tomography scans to detect subclinical leaflet thrombosis,” he added.
Commenting on the study at an ACC press conference, Megan Coylewright, MD, director of the Structural Heart Program at Erlanger Health System, Chattanooga, Tennessee, said: “Oftentimes when studies are negative, we’re disappointed. In this case, I think we are pleased that the study is negative because it suggests we do not have to expose our TAVR patients to anticoagulation for benefit.”
Dr. Coylewright explained that the ADAPT-TAVR study was asking whether clots form on the valve, as defined by CT.
“We are worried about that for two reasons: could that clot cause a stroke, and could that clot cause the valve to break down over time. This study looked at the first issue. And it found that there was some clot build up on the valve, but that it wasn’t significantly different between the anticoagulant and dual antiplatelet groups. And there was no correlation with embolic events, she noted.
“It shows how fast our field moves. In the U.S. now, we are using aspirin alone at 81 mg for patients who do not have an indication for oral anticoagulation after TAVR. We are moving away from dual antiplatelet therapy because the bleeding risk is so bad,” Dr. Coylewright said.
In his presentation, Dr. Park explained that it is believed that oral anticoagulants are more effective than antiplatelet therapy at reducing subclinical leaflet thrombosis, but it is not known whether there is a causal association between subclinical leaflet thrombosis and cerebral embolism, or whether oral anticoagulation can reduce cerebral embolism related to subclinical leaflet thrombosis.
The ADAPT-TAVR was conducted to look at these issues. The open-label randomized trial was conducted in five centers in Hong Kong, South Korea, and Taiwan.
For the study, 229 patients who had undergone successful TAVR and did not have an indication for anticoagulation were randomized to edoxaban 60 mg once daily, edoxaban 30 mg once daily for patients needing a reduced dose, or dual antiplatelet therapy for 6 months.
The primary endpoint was an incidence of leaflet thrombosis on four-dimensional CT at 6 months.
Results showed a strong trend toward a lower incidence of leaflet thrombosis in the edoxaban groups than in the dual antiplatelet group (9.8% vs. 18.4%; P = .076).
There was a nonsignificant difference in the percentage of patients with new cerebral lesions identified on brain MRI between the edoxaban and dual antiplatelet groups (25.0% vs. 20.2%).
The percentage of patients with worsening of neurologic and neurocognitive function was not different among the groups.
The incidence of any or major bleeding events was not different between two therapies.
There was also no significant association of the presence or extent of leaflet thrombosis with new cerebral lesions or change of neurologic or neurocognitive function.
Dr. Park noted that the trial had several limitations, including an open-label design, use of surrogate imaging outcomes for the primary outcome, and the relatively short follow-up period, so the study was underpowered to detect any meaningful differences in clinical efficacy and safety outcomes. The results should thus be considered hypothesis-generating, highlighting the need for further research, he added.
The long-term effect of leaflet thrombosis or different antithrombotic strategies on bioprosthetic valve durability is still unknown, Dr. Park said.
He also pointed out that the findings cannot be directly extrapolated to patients with an established indication for oral anticoagulant therapy.
The ADAPT-TAVR trial was an investigator-initiated trial and was funded by the CardioVascular Research Foundation (Seoul, Korea) and Daiichi Sankyo Korea.
A version of this article first appeared on Medscape.com.
In patients undergoing transcatheter aortic valve replacement (TAVR), the incidence of leaflet thrombosis was numerically lower in those treated with the anticoagulant edoxaban for 6 months after the procedure than in those who received dual antiplatelet therapy, although the difference was not statistically significant, in the ADAPT-TAVR study.
There was no difference in new cerebral thromboembolism or neurologic/neurocognitive function between the two groups in the study.
Also, there was no significant relation between subclinical leaflet thrombosis and increased risk for cerebral thromboembolism and neurologic dysfunction.
The ADAPT-TAVR trial was presented April 4 at the American College of Cardiology (ACC) 2022 Scientific Session by Duk-Woo Park, MD, Asan Medical Center, Seoul, South Korea. It was simultaneously published online in Circulation.
“The key messages from this study are that subclinical leaflet thrombosis has not been proven to affect clinical outcomes for patients undergoing valve replacement and that in patients in whom leaflet thrombosis causes no symptoms or complications, its presence should not dictate the type of antithrombotic therapy that patients receive following the implantation of an artificial heart valve,” Dr. Park said.
“These findings do not support the routine use of computed tomography scans to detect subclinical leaflet thrombosis,” he added.
Commenting on the study at an ACC press conference, Megan Coylewright, MD, director of the Structural Heart Program at Erlanger Health System, Chattanooga, Tennessee, said: “Oftentimes when studies are negative, we’re disappointed. In this case, I think we are pleased that the study is negative because it suggests we do not have to expose our TAVR patients to anticoagulation for benefit.”
Dr. Coylewright explained that the ADAPT-TAVR study was asking whether clots form on the valve, as defined by CT.
“We are worried about that for two reasons: could that clot cause a stroke, and could that clot cause the valve to break down over time. This study looked at the first issue. And it found that there was some clot build up on the valve, but that it wasn’t significantly different between the anticoagulant and dual antiplatelet groups. And there was no correlation with embolic events, she noted.
“It shows how fast our field moves. In the U.S. now, we are using aspirin alone at 81 mg for patients who do not have an indication for oral anticoagulation after TAVR. We are moving away from dual antiplatelet therapy because the bleeding risk is so bad,” Dr. Coylewright said.
In his presentation, Dr. Park explained that it is believed that oral anticoagulants are more effective than antiplatelet therapy at reducing subclinical leaflet thrombosis, but it is not known whether there is a causal association between subclinical leaflet thrombosis and cerebral embolism, or whether oral anticoagulation can reduce cerebral embolism related to subclinical leaflet thrombosis.
The ADAPT-TAVR was conducted to look at these issues. The open-label randomized trial was conducted in five centers in Hong Kong, South Korea, and Taiwan.
For the study, 229 patients who had undergone successful TAVR and did not have an indication for anticoagulation were randomized to edoxaban 60 mg once daily, edoxaban 30 mg once daily for patients needing a reduced dose, or dual antiplatelet therapy for 6 months.
The primary endpoint was an incidence of leaflet thrombosis on four-dimensional CT at 6 months.
Results showed a strong trend toward a lower incidence of leaflet thrombosis in the edoxaban groups than in the dual antiplatelet group (9.8% vs. 18.4%; P = .076).
There was a nonsignificant difference in the percentage of patients with new cerebral lesions identified on brain MRI between the edoxaban and dual antiplatelet groups (25.0% vs. 20.2%).
The percentage of patients with worsening of neurologic and neurocognitive function was not different among the groups.
The incidence of any or major bleeding events was not different between two therapies.
There was also no significant association of the presence or extent of leaflet thrombosis with new cerebral lesions or change of neurologic or neurocognitive function.
Dr. Park noted that the trial had several limitations, including an open-label design, use of surrogate imaging outcomes for the primary outcome, and the relatively short follow-up period, so the study was underpowered to detect any meaningful differences in clinical efficacy and safety outcomes. The results should thus be considered hypothesis-generating, highlighting the need for further research, he added.
The long-term effect of leaflet thrombosis or different antithrombotic strategies on bioprosthetic valve durability is still unknown, Dr. Park said.
He also pointed out that the findings cannot be directly extrapolated to patients with an established indication for oral anticoagulant therapy.
The ADAPT-TAVR trial was an investigator-initiated trial and was funded by the CardioVascular Research Foundation (Seoul, Korea) and Daiichi Sankyo Korea.
A version of this article first appeared on Medscape.com.
In patients undergoing transcatheter aortic valve replacement (TAVR), the incidence of leaflet thrombosis was numerically lower in those treated with the anticoagulant edoxaban for 6 months after the procedure than in those who received dual antiplatelet therapy, although the difference was not statistically significant, in the ADAPT-TAVR study.
There was no difference in new cerebral thromboembolism or neurologic/neurocognitive function between the two groups in the study.
Also, there was no significant relation between subclinical leaflet thrombosis and increased risk for cerebral thromboembolism and neurologic dysfunction.
The ADAPT-TAVR trial was presented April 4 at the American College of Cardiology (ACC) 2022 Scientific Session by Duk-Woo Park, MD, Asan Medical Center, Seoul, South Korea. It was simultaneously published online in Circulation.
“The key messages from this study are that subclinical leaflet thrombosis has not been proven to affect clinical outcomes for patients undergoing valve replacement and that in patients in whom leaflet thrombosis causes no symptoms or complications, its presence should not dictate the type of antithrombotic therapy that patients receive following the implantation of an artificial heart valve,” Dr. Park said.
“These findings do not support the routine use of computed tomography scans to detect subclinical leaflet thrombosis,” he added.
Commenting on the study at an ACC press conference, Megan Coylewright, MD, director of the Structural Heart Program at Erlanger Health System, Chattanooga, Tennessee, said: “Oftentimes when studies are negative, we’re disappointed. In this case, I think we are pleased that the study is negative because it suggests we do not have to expose our TAVR patients to anticoagulation for benefit.”
Dr. Coylewright explained that the ADAPT-TAVR study was asking whether clots form on the valve, as defined by CT.
“We are worried about that for two reasons: could that clot cause a stroke, and could that clot cause the valve to break down over time. This study looked at the first issue. And it found that there was some clot build up on the valve, but that it wasn’t significantly different between the anticoagulant and dual antiplatelet groups. And there was no correlation with embolic events, she noted.
“It shows how fast our field moves. In the U.S. now, we are using aspirin alone at 81 mg for patients who do not have an indication for oral anticoagulation after TAVR. We are moving away from dual antiplatelet therapy because the bleeding risk is so bad,” Dr. Coylewright said.
In his presentation, Dr. Park explained that it is believed that oral anticoagulants are more effective than antiplatelet therapy at reducing subclinical leaflet thrombosis, but it is not known whether there is a causal association between subclinical leaflet thrombosis and cerebral embolism, or whether oral anticoagulation can reduce cerebral embolism related to subclinical leaflet thrombosis.
The ADAPT-TAVR was conducted to look at these issues. The open-label randomized trial was conducted in five centers in Hong Kong, South Korea, and Taiwan.
For the study, 229 patients who had undergone successful TAVR and did not have an indication for anticoagulation were randomized to edoxaban 60 mg once daily, edoxaban 30 mg once daily for patients needing a reduced dose, or dual antiplatelet therapy for 6 months.
The primary endpoint was an incidence of leaflet thrombosis on four-dimensional CT at 6 months.
Results showed a strong trend toward a lower incidence of leaflet thrombosis in the edoxaban groups than in the dual antiplatelet group (9.8% vs. 18.4%; P = .076).
There was a nonsignificant difference in the percentage of patients with new cerebral lesions identified on brain MRI between the edoxaban and dual antiplatelet groups (25.0% vs. 20.2%).
The percentage of patients with worsening of neurologic and neurocognitive function was not different among the groups.
The incidence of any or major bleeding events was not different between two therapies.
There was also no significant association of the presence or extent of leaflet thrombosis with new cerebral lesions or change of neurologic or neurocognitive function.
Dr. Park noted that the trial had several limitations, including an open-label design, use of surrogate imaging outcomes for the primary outcome, and the relatively short follow-up period, so the study was underpowered to detect any meaningful differences in clinical efficacy and safety outcomes. The results should thus be considered hypothesis-generating, highlighting the need for further research, he added.
The long-term effect of leaflet thrombosis or different antithrombotic strategies on bioprosthetic valve durability is still unknown, Dr. Park said.
He also pointed out that the findings cannot be directly extrapolated to patients with an established indication for oral anticoagulant therapy.
The ADAPT-TAVR trial was an investigator-initiated trial and was funded by the CardioVascular Research Foundation (Seoul, Korea) and Daiichi Sankyo Korea.
A version of this article first appeared on Medscape.com.
FDA approves leadless, single-chamber pacemaker system
The Food and Drug Administration has granted approval to Abbott’s Aveir leadless, single-chamber pacemaker system for patients with bradycardia.
In a press release, Abbott said the device has a unique mapping capability that allows interventionists implanting the device to measure electrical signals within the heart to determine the correct placement before final implantation. Aveir is implanted directly into the right ventricle via a catheter.
The company also said Aveir has a battery life that’s up to twice as long as other commercially available leadless pacemakers when following International Association for Standardization (ISO) standard settings. And the device can be retrieved if necessary, the press release said.
“Leadless pacemakers address known complications associated with traditional pacemakers,” Rahul Doshi, MD, director of electrophysiology at Honor Health in Scottsdale, Ariz., said in the press release. “In addition, the Aveir leadless pacemaker brings unique innovations we’ve been seeking, such as the ability to ensure electrical performance before we commit to placement.”
Investigators of the LEADLESS II phase 2 study reported last year on what they called “key design improvements” of the Aveir device compared to the first leadless pacemaker, the discontinued Nanostim. They included a 12% longer battery life, a shorter and wider form factor, a modified docking button that allows for retrievability, a modified delivery system, and an application-specific integrated circuit chip that can support a dual-chamber pacing system in the future.
The study reported that 96% of the 200 enrolled patients met the primary safety endpoint of no serious device-related adverse events at 6 weeks after implantation. A similar percentage achieved therapeutic pacing and sensing amplitude.
The study also reported that interventionists accurately positioned Aveir the first time or with a single repositioning in 96% of cases.
The Food and Drug Administration has granted approval to Abbott’s Aveir leadless, single-chamber pacemaker system for patients with bradycardia.
In a press release, Abbott said the device has a unique mapping capability that allows interventionists implanting the device to measure electrical signals within the heart to determine the correct placement before final implantation. Aveir is implanted directly into the right ventricle via a catheter.
The company also said Aveir has a battery life that’s up to twice as long as other commercially available leadless pacemakers when following International Association for Standardization (ISO) standard settings. And the device can be retrieved if necessary, the press release said.
“Leadless pacemakers address known complications associated with traditional pacemakers,” Rahul Doshi, MD, director of electrophysiology at Honor Health in Scottsdale, Ariz., said in the press release. “In addition, the Aveir leadless pacemaker brings unique innovations we’ve been seeking, such as the ability to ensure electrical performance before we commit to placement.”
Investigators of the LEADLESS II phase 2 study reported last year on what they called “key design improvements” of the Aveir device compared to the first leadless pacemaker, the discontinued Nanostim. They included a 12% longer battery life, a shorter and wider form factor, a modified docking button that allows for retrievability, a modified delivery system, and an application-specific integrated circuit chip that can support a dual-chamber pacing system in the future.
The study reported that 96% of the 200 enrolled patients met the primary safety endpoint of no serious device-related adverse events at 6 weeks after implantation. A similar percentage achieved therapeutic pacing and sensing amplitude.
The study also reported that interventionists accurately positioned Aveir the first time or with a single repositioning in 96% of cases.
The Food and Drug Administration has granted approval to Abbott’s Aveir leadless, single-chamber pacemaker system for patients with bradycardia.
In a press release, Abbott said the device has a unique mapping capability that allows interventionists implanting the device to measure electrical signals within the heart to determine the correct placement before final implantation. Aveir is implanted directly into the right ventricle via a catheter.
The company also said Aveir has a battery life that’s up to twice as long as other commercially available leadless pacemakers when following International Association for Standardization (ISO) standard settings. And the device can be retrieved if necessary, the press release said.
“Leadless pacemakers address known complications associated with traditional pacemakers,” Rahul Doshi, MD, director of electrophysiology at Honor Health in Scottsdale, Ariz., said in the press release. “In addition, the Aveir leadless pacemaker brings unique innovations we’ve been seeking, such as the ability to ensure electrical performance before we commit to placement.”
Investigators of the LEADLESS II phase 2 study reported last year on what they called “key design improvements” of the Aveir device compared to the first leadless pacemaker, the discontinued Nanostim. They included a 12% longer battery life, a shorter and wider form factor, a modified docking button that allows for retrievability, a modified delivery system, and an application-specific integrated circuit chip that can support a dual-chamber pacing system in the future.
The study reported that 96% of the 200 enrolled patients met the primary safety endpoint of no serious device-related adverse events at 6 weeks after implantation. A similar percentage achieved therapeutic pacing and sensing amplitude.
The study also reported that interventionists accurately positioned Aveir the first time or with a single repositioning in 96% of cases.
New HF guidelines feature ‘quad’ therapy, tweaked terminology
The new heart failure (HF) guidelines released by three North American societies had a lot of catching up to do given the significant, even paradigm-shifting, additions to available treatment options in the last few years.
The landscape now includes both new and repurposed drug therapies that benefit almost without regard to ejection fraction (EF), and evidence-based urgency to engage patients early on with at least four core medication classes, so-called quadruple therapy.
The guideline document offers a roadmap for navigating those key issues and many others and uses some creative tactics. They include the introduction of generalist-friendly labels for the traditional but obscurely named four stages of HF severity that, it is hoped, will have wider reach and expand the use of effective therapies.
It introduces additional disease-staging terminology that characterizes the syndrome as a continuum:
- “At risk for HF” for stage A, applied to asymptomatic patients with risk factors such as diabetes or hypertension but no known cardiac changes.
- “Pre-HF” for stage B, which adds cardiac structural changes or elevated natriuretic peptides, still in the absence of symptoms.
- “Symptomatic HF” for stage C, that is, structural disease with current or previous symptoms.
- “Advanced HF” for stage D, characterized by severe debilitating symptoms or repeated hospitalizations even with guideline-directed medical therapy (GDMT).
The new terms should be “easier for primary care physicians as well as nonspecialists” to remember and use effectively “and easier to translate to the patients,” compared with the solely alphabetical staging labels appearing in the guidelines for more than 15 years, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, said in an interview.
An emphasis on “at risk for HF” and “pre-HF” in the new document may help efforts to expand primary prevention of HF and management of preclinical HF. The guideline, Dr. Bozkurt said, includes specific treatment recommendations for those early stages.
The document also updates and sometimes introduces “recommendations for advanced heart failure, acute heart failure, and comorbidities – specifically for atrial fibrillation, iron deficiency, sleep apnea, coronary artery disease, and valvular heart disease,” Dr. Bozkurt observed, as well as for cardiomyopathy and HF related to pregnancy and cancer chemotherapy. “So, it’s a very comprehensive guideline.”
Dr. Bozkurt is vice chair of the guideline writing committee and helped introduce the guideline at the annual scientific sessions of the American College of Cardiology. The document, developed by the ACC, the American Heart Association, and the Heart Failure Society of America, was published April 1, 2022, in the societies’ flagship journals, Journal of the American College of Cardiology, Circulation, and the Journal of Cardiac Failure, respectively. It replaces the 2013 guideline from the ACC and AHA and the ACC/AHA/HFSA–focused update from 2017.
“We really need to treat early, and then we need to treat appropriately,” Douglas L. Mann, MD, Washington University in St. Louis, said in an interview. Dr. Mann, who was not involved in development of the new guideline, said he is “enthusiastic” about the new staging terminology.
“I think it makes it easier to convey the message that these people do need medicines, will benefit from medicines, and in some cases heart failure can be preventable,” he said. “I’m in favor of anything that simplifies it and makes it more readily interpretable by busy doctors who aren’t specialists.”
With the new staging terminology and in other ways, the guideline seems to appreciate cardiomyopathy as a journey from preclinical to advanced symptomatic stages – the preclinical “at-risk” stage tightening focus on primary prevention – and updated thinking on classification of HF by EF.
For example, there is new consideration of “HF with improved ejection fraction” (HFimpEF), which suggests the patient may be evolving from HF with reduced EF (HFrEF) to HF with EF that is preserved or mildly reduced, or vice versa.
With HFimpEF, which identifies patients previously with an EF of 40% or lower that improves to beyond 40% at follow-up testing, patients should continue on the medications they had been previously taking for HFrEF, Dr. Bozkurt said.
Patients at risk for HF, in stage A by the older terminology, are characterized by one or more significant HF risk factors, such as hypertension, diabetes, or coronary disease, as they have been in prior guidelines. But the new document, Dr. Bozkurt observed, adds genetic cardiomyopathies and exposure to cardiotoxic agents to the list.
Perhaps surprisingly, the guideline also includes elevated natriuretic peptides as an indicator of “at risk for HF,” with implications for screening. The evidence suggests that, “for patients who are at risk for heart failure, natriuretic peptide-based screening, followed by team-based care, can prevent development of left ventricular dysfunction in heart failure,” Dr. Bozkurt said.
Persons at risk for HF realistically encompass a huge swath of the population given the world prevalence of high blood pressure, obesity, and diabetes. Management of stage A, therefore, focuses on established tenets of primary cardiovascular prevention, such as weight and BP control, exercise, and healthy dietary choices.
They may well be eligible for treatment with sodium-glucose transporter 2 (SGLT2) inhibitors, which have been “game changers,” Dr. Mann said. “Now you can give them to diabetics and it’s going to prevent heart failure and [cardiovascular] events. We didn’t have a drug like that before, so I think that places a lot of emphasis on aggressive treatment of diabetes.”
For patients with symptomatic HF, the document touts multidisciplinary care and early initiation of drugs from each of four drug classes. Such quadruple therapy includes an SGLT2 inhibitor along with a beta-blocker, a mineralocorticoid receptor antagonist (MRA), and a renin-angiotensin system (RAS) inhibitor: the “core foundational therapies” for patients with HFrEF, Dr. Bozkurt observed.
Of note, she said, the angiotensin receptor–neprilysin inhibitor sacubitril/valsartan (Entresto, Novartis) is the preferred RAS inhibitor. But “if the ARNI cannot be used, then use ACE inhibitors.” If the patient is intolerant of ACE inhibitors because of cough or angioedema, then the choice should be an angiotensin-receptor blocker.
“We have very effective therapies offering survival and morbidity benefits as well as improvements in quality of life and reverse remodeling,” Dr. Bozkurt observed. “The most important message is that optimization of therapies, including all of these medication classes, saves lives.”
The guideline also includes, for the first time, a series of “value statements” on cost-effectiveness of different therapies that assign a “high-value” rating to MRAs, hydralazine, and isosorbide dinitrate in otherwise optimally treated self-identified African Americans, and device therapy in appropriately selected patients. The statements hold SGLT2 inhibitors in chronic symptomatic HF and cardiac transplantation in advanced GDMT-resistant HF to be of “intermediate” value.
The value statements, Dr. Bozkurt noted, “are included throughout the document when there is evidence; when there is a high-quality cost-effectiveness study published.”
Dr. Bozkurt disclosed receiving honoraria or consulting fees from Amgen, AstraZeneca, Baxter International, Bristol-Myers Squibb, Sanofi-Aventis, scPharmaceuticals, and Vifor Pharma; serving on a data safety monitoring board for LivaNova USA; and holding other relationships with Abbott Laboratories and Relypsa. Dr. Mann disclosed receiving honoraria or consulting fees from MyoKardia, Novartis, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
The new heart failure (HF) guidelines released by three North American societies had a lot of catching up to do given the significant, even paradigm-shifting, additions to available treatment options in the last few years.
The landscape now includes both new and repurposed drug therapies that benefit almost without regard to ejection fraction (EF), and evidence-based urgency to engage patients early on with at least four core medication classes, so-called quadruple therapy.
The guideline document offers a roadmap for navigating those key issues and many others and uses some creative tactics. They include the introduction of generalist-friendly labels for the traditional but obscurely named four stages of HF severity that, it is hoped, will have wider reach and expand the use of effective therapies.
It introduces additional disease-staging terminology that characterizes the syndrome as a continuum:
- “At risk for HF” for stage A, applied to asymptomatic patients with risk factors such as diabetes or hypertension but no known cardiac changes.
- “Pre-HF” for stage B, which adds cardiac structural changes or elevated natriuretic peptides, still in the absence of symptoms.
- “Symptomatic HF” for stage C, that is, structural disease with current or previous symptoms.
- “Advanced HF” for stage D, characterized by severe debilitating symptoms or repeated hospitalizations even with guideline-directed medical therapy (GDMT).
The new terms should be “easier for primary care physicians as well as nonspecialists” to remember and use effectively “and easier to translate to the patients,” compared with the solely alphabetical staging labels appearing in the guidelines for more than 15 years, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, said in an interview.
An emphasis on “at risk for HF” and “pre-HF” in the new document may help efforts to expand primary prevention of HF and management of preclinical HF. The guideline, Dr. Bozkurt said, includes specific treatment recommendations for those early stages.
The document also updates and sometimes introduces “recommendations for advanced heart failure, acute heart failure, and comorbidities – specifically for atrial fibrillation, iron deficiency, sleep apnea, coronary artery disease, and valvular heart disease,” Dr. Bozkurt observed, as well as for cardiomyopathy and HF related to pregnancy and cancer chemotherapy. “So, it’s a very comprehensive guideline.”
Dr. Bozkurt is vice chair of the guideline writing committee and helped introduce the guideline at the annual scientific sessions of the American College of Cardiology. The document, developed by the ACC, the American Heart Association, and the Heart Failure Society of America, was published April 1, 2022, in the societies’ flagship journals, Journal of the American College of Cardiology, Circulation, and the Journal of Cardiac Failure, respectively. It replaces the 2013 guideline from the ACC and AHA and the ACC/AHA/HFSA–focused update from 2017.
“We really need to treat early, and then we need to treat appropriately,” Douglas L. Mann, MD, Washington University in St. Louis, said in an interview. Dr. Mann, who was not involved in development of the new guideline, said he is “enthusiastic” about the new staging terminology.
“I think it makes it easier to convey the message that these people do need medicines, will benefit from medicines, and in some cases heart failure can be preventable,” he said. “I’m in favor of anything that simplifies it and makes it more readily interpretable by busy doctors who aren’t specialists.”
With the new staging terminology and in other ways, the guideline seems to appreciate cardiomyopathy as a journey from preclinical to advanced symptomatic stages – the preclinical “at-risk” stage tightening focus on primary prevention – and updated thinking on classification of HF by EF.
For example, there is new consideration of “HF with improved ejection fraction” (HFimpEF), which suggests the patient may be evolving from HF with reduced EF (HFrEF) to HF with EF that is preserved or mildly reduced, or vice versa.
With HFimpEF, which identifies patients previously with an EF of 40% or lower that improves to beyond 40% at follow-up testing, patients should continue on the medications they had been previously taking for HFrEF, Dr. Bozkurt said.
Patients at risk for HF, in stage A by the older terminology, are characterized by one or more significant HF risk factors, such as hypertension, diabetes, or coronary disease, as they have been in prior guidelines. But the new document, Dr. Bozkurt observed, adds genetic cardiomyopathies and exposure to cardiotoxic agents to the list.
Perhaps surprisingly, the guideline also includes elevated natriuretic peptides as an indicator of “at risk for HF,” with implications for screening. The evidence suggests that, “for patients who are at risk for heart failure, natriuretic peptide-based screening, followed by team-based care, can prevent development of left ventricular dysfunction in heart failure,” Dr. Bozkurt said.
Persons at risk for HF realistically encompass a huge swath of the population given the world prevalence of high blood pressure, obesity, and diabetes. Management of stage A, therefore, focuses on established tenets of primary cardiovascular prevention, such as weight and BP control, exercise, and healthy dietary choices.
They may well be eligible for treatment with sodium-glucose transporter 2 (SGLT2) inhibitors, which have been “game changers,” Dr. Mann said. “Now you can give them to diabetics and it’s going to prevent heart failure and [cardiovascular] events. We didn’t have a drug like that before, so I think that places a lot of emphasis on aggressive treatment of diabetes.”
For patients with symptomatic HF, the document touts multidisciplinary care and early initiation of drugs from each of four drug classes. Such quadruple therapy includes an SGLT2 inhibitor along with a beta-blocker, a mineralocorticoid receptor antagonist (MRA), and a renin-angiotensin system (RAS) inhibitor: the “core foundational therapies” for patients with HFrEF, Dr. Bozkurt observed.
Of note, she said, the angiotensin receptor–neprilysin inhibitor sacubitril/valsartan (Entresto, Novartis) is the preferred RAS inhibitor. But “if the ARNI cannot be used, then use ACE inhibitors.” If the patient is intolerant of ACE inhibitors because of cough or angioedema, then the choice should be an angiotensin-receptor blocker.
“We have very effective therapies offering survival and morbidity benefits as well as improvements in quality of life and reverse remodeling,” Dr. Bozkurt observed. “The most important message is that optimization of therapies, including all of these medication classes, saves lives.”
The guideline also includes, for the first time, a series of “value statements” on cost-effectiveness of different therapies that assign a “high-value” rating to MRAs, hydralazine, and isosorbide dinitrate in otherwise optimally treated self-identified African Americans, and device therapy in appropriately selected patients. The statements hold SGLT2 inhibitors in chronic symptomatic HF and cardiac transplantation in advanced GDMT-resistant HF to be of “intermediate” value.
The value statements, Dr. Bozkurt noted, “are included throughout the document when there is evidence; when there is a high-quality cost-effectiveness study published.”
Dr. Bozkurt disclosed receiving honoraria or consulting fees from Amgen, AstraZeneca, Baxter International, Bristol-Myers Squibb, Sanofi-Aventis, scPharmaceuticals, and Vifor Pharma; serving on a data safety monitoring board for LivaNova USA; and holding other relationships with Abbott Laboratories and Relypsa. Dr. Mann disclosed receiving honoraria or consulting fees from MyoKardia, Novartis, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
The new heart failure (HF) guidelines released by three North American societies had a lot of catching up to do given the significant, even paradigm-shifting, additions to available treatment options in the last few years.
The landscape now includes both new and repurposed drug therapies that benefit almost without regard to ejection fraction (EF), and evidence-based urgency to engage patients early on with at least four core medication classes, so-called quadruple therapy.
The guideline document offers a roadmap for navigating those key issues and many others and uses some creative tactics. They include the introduction of generalist-friendly labels for the traditional but obscurely named four stages of HF severity that, it is hoped, will have wider reach and expand the use of effective therapies.
It introduces additional disease-staging terminology that characterizes the syndrome as a continuum:
- “At risk for HF” for stage A, applied to asymptomatic patients with risk factors such as diabetes or hypertension but no known cardiac changes.
- “Pre-HF” for stage B, which adds cardiac structural changes or elevated natriuretic peptides, still in the absence of symptoms.
- “Symptomatic HF” for stage C, that is, structural disease with current or previous symptoms.
- “Advanced HF” for stage D, characterized by severe debilitating symptoms or repeated hospitalizations even with guideline-directed medical therapy (GDMT).
The new terms should be “easier for primary care physicians as well as nonspecialists” to remember and use effectively “and easier to translate to the patients,” compared with the solely alphabetical staging labels appearing in the guidelines for more than 15 years, Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, said in an interview.
An emphasis on “at risk for HF” and “pre-HF” in the new document may help efforts to expand primary prevention of HF and management of preclinical HF. The guideline, Dr. Bozkurt said, includes specific treatment recommendations for those early stages.
The document also updates and sometimes introduces “recommendations for advanced heart failure, acute heart failure, and comorbidities – specifically for atrial fibrillation, iron deficiency, sleep apnea, coronary artery disease, and valvular heart disease,” Dr. Bozkurt observed, as well as for cardiomyopathy and HF related to pregnancy and cancer chemotherapy. “So, it’s a very comprehensive guideline.”
Dr. Bozkurt is vice chair of the guideline writing committee and helped introduce the guideline at the annual scientific sessions of the American College of Cardiology. The document, developed by the ACC, the American Heart Association, and the Heart Failure Society of America, was published April 1, 2022, in the societies’ flagship journals, Journal of the American College of Cardiology, Circulation, and the Journal of Cardiac Failure, respectively. It replaces the 2013 guideline from the ACC and AHA and the ACC/AHA/HFSA–focused update from 2017.
“We really need to treat early, and then we need to treat appropriately,” Douglas L. Mann, MD, Washington University in St. Louis, said in an interview. Dr. Mann, who was not involved in development of the new guideline, said he is “enthusiastic” about the new staging terminology.
“I think it makes it easier to convey the message that these people do need medicines, will benefit from medicines, and in some cases heart failure can be preventable,” he said. “I’m in favor of anything that simplifies it and makes it more readily interpretable by busy doctors who aren’t specialists.”
With the new staging terminology and in other ways, the guideline seems to appreciate cardiomyopathy as a journey from preclinical to advanced symptomatic stages – the preclinical “at-risk” stage tightening focus on primary prevention – and updated thinking on classification of HF by EF.
For example, there is new consideration of “HF with improved ejection fraction” (HFimpEF), which suggests the patient may be evolving from HF with reduced EF (HFrEF) to HF with EF that is preserved or mildly reduced, or vice versa.
With HFimpEF, which identifies patients previously with an EF of 40% or lower that improves to beyond 40% at follow-up testing, patients should continue on the medications they had been previously taking for HFrEF, Dr. Bozkurt said.
Patients at risk for HF, in stage A by the older terminology, are characterized by one or more significant HF risk factors, such as hypertension, diabetes, or coronary disease, as they have been in prior guidelines. But the new document, Dr. Bozkurt observed, adds genetic cardiomyopathies and exposure to cardiotoxic agents to the list.
Perhaps surprisingly, the guideline also includes elevated natriuretic peptides as an indicator of “at risk for HF,” with implications for screening. The evidence suggests that, “for patients who are at risk for heart failure, natriuretic peptide-based screening, followed by team-based care, can prevent development of left ventricular dysfunction in heart failure,” Dr. Bozkurt said.
Persons at risk for HF realistically encompass a huge swath of the population given the world prevalence of high blood pressure, obesity, and diabetes. Management of stage A, therefore, focuses on established tenets of primary cardiovascular prevention, such as weight and BP control, exercise, and healthy dietary choices.
They may well be eligible for treatment with sodium-glucose transporter 2 (SGLT2) inhibitors, which have been “game changers,” Dr. Mann said. “Now you can give them to diabetics and it’s going to prevent heart failure and [cardiovascular] events. We didn’t have a drug like that before, so I think that places a lot of emphasis on aggressive treatment of diabetes.”
For patients with symptomatic HF, the document touts multidisciplinary care and early initiation of drugs from each of four drug classes. Such quadruple therapy includes an SGLT2 inhibitor along with a beta-blocker, a mineralocorticoid receptor antagonist (MRA), and a renin-angiotensin system (RAS) inhibitor: the “core foundational therapies” for patients with HFrEF, Dr. Bozkurt observed.
Of note, she said, the angiotensin receptor–neprilysin inhibitor sacubitril/valsartan (Entresto, Novartis) is the preferred RAS inhibitor. But “if the ARNI cannot be used, then use ACE inhibitors.” If the patient is intolerant of ACE inhibitors because of cough or angioedema, then the choice should be an angiotensin-receptor blocker.
“We have very effective therapies offering survival and morbidity benefits as well as improvements in quality of life and reverse remodeling,” Dr. Bozkurt observed. “The most important message is that optimization of therapies, including all of these medication classes, saves lives.”
The guideline also includes, for the first time, a series of “value statements” on cost-effectiveness of different therapies that assign a “high-value” rating to MRAs, hydralazine, and isosorbide dinitrate in otherwise optimally treated self-identified African Americans, and device therapy in appropriately selected patients. The statements hold SGLT2 inhibitors in chronic symptomatic HF and cardiac transplantation in advanced GDMT-resistant HF to be of “intermediate” value.
The value statements, Dr. Bozkurt noted, “are included throughout the document when there is evidence; when there is a high-quality cost-effectiveness study published.”
Dr. Bozkurt disclosed receiving honoraria or consulting fees from Amgen, AstraZeneca, Baxter International, Bristol-Myers Squibb, Sanofi-Aventis, scPharmaceuticals, and Vifor Pharma; serving on a data safety monitoring board for LivaNova USA; and holding other relationships with Abbott Laboratories and Relypsa. Dr. Mann disclosed receiving honoraria or consulting fees from MyoKardia, Novartis, and Novo Nordisk.
A version of this article first appeared on Medscape.com.
FROM ACC 2022
Mavacamten controlled hypertrophic cardiomyopathy for over 1 year
WASHINGTON – Treatment of patients with symptomatic obstructive hypertrophic cardiomyopathy who remained on treatment with the investigational agent mavacamten for a median of 62 weeks continued to show the same level of safe response to the drug as seen after the first 30 weeks on treatment in the pivotal trial for this agent.
The new findings from longer-term treatment bode well for mavacamten. That’s because if the drug is used in routine practice to avoid the need for surgery or an invasive intervention to reduce blockage of a patient’s left ventricular outflow tract, the duration of mavacamten treatment will likely need to continue for many years and even for decades, said Florian Rader, MD, who presented the results at the annual scientific sessions of the American College of Cardiology.
“In practice, mavacamten will probably be used for many, many years, especially as it replaces septal-reduction therapy, so we need long-term data,” noted Dr. Rader during a press briefing on his report. “I’m very happy with the long-term data” in the follow-up study.
The Food and Drug Administration is currently considering whether to approve mavacamten for routine marketing to treat patients with symptomatic obstructive hypertrophic cardiomyopathy (oHCM), with a decision expected by the end of April 2022.
The study Dr. Rader reported followed 231 patients with symptomatic oHCM who had completed the 30-week pivotal trial of mavacamten, EXPLORER-HCM, and opted to continue on open-label extended treatment with mavacamten, either continuing the treatment they started during the trial or crossing over to receive mavacamten after receiving placebo during the trial.
The major findings from EXPLORER-LTE (long-term extension) were that continued treatment for a median of about 62 weeks maintained the safety and efficacy findings seen at the end of the blinded, randomized, initial 30-week phase, said Dr. Rader, codirector of the Clinic for Hypertrophic Cardiomyopathy and Aortopathies at Cedars-Sinai Medical Center in Los Angeles.
‘Almost revolutionary’
Mavacamten represents “an almost revolutionary change” for treating oHCM, commented Maya E. Guglin, MD, professor of clinical medicine and an advanced heart failure physician at Indiana University, Indianapolis. “Until now, there was no good medical treatment for symptomatic oHCM. This will change the landscape, and without question it will change guidelines for treating oHCM,” said Dr. Guglin during the press briefing.
“All of us who care for patients with oHCM have looked forward to having a disease-specific therapy. It is encouraging to see that the safety and efficacy remained high with long-term follow-up,” commented Kyle W. Klarich, MD, a professor and cardiologist who specializes in treating patients with HCM at the Mayo Clinic in Rochester, Minn.
Mavacamten is a direct myosin inhibitor that reduces the excess number of myosin-actin cross bridges that form in patients with oHCM, and thereby directly targets the pathophysiology that underlies the disorder, explained Dr. Rader.
The patients on mavacamten included in the long-term extension reported by Dr. Rader averaged 60 years of age, and 61% were men. They averaged a 35.6–mm Hg drop in their resting left ventricular outflow tract (LVOT) gradient after 48 weeks on treatment, and a 32.8–mm Hg reduction after 84 weeks. When the investigators measured their LVOT gradient during a valsalva maneuver, their reductions from baseline averaged 45.3 mm Hg after 48 weeks and 46.4 mm Hg after 84 weeks.
Resting left ventricular ejection fraction also fell, by an average of 7.0 percentage points from baseline after 48 weeks, and by an average of 9.0 percentage points after 84 weeks. After 48 weeks on treatment, 68% of patients had at least a one-class improvement from baseline in their New York Heart Association functional class.
The safety results showed that most treatment-related adverse events were mild or moderate, and about 2% of patients had a serious drug-related adverse event. Ten of the 231 patients discontinued mavacamten because of a treated-related adverse event.
EXPLORER-HCM and EXPLORER-LTE were sponsored by MyoKardia, the company that is developing mavacamten and which is now owned by Bristol-Myers Squibb. Dr. Rader has been a consultant to MyoKardia as well as to Medtronic and ReCor. Dr. Guglin and Dr. Klarich had no disclosures.
WASHINGTON – Treatment of patients with symptomatic obstructive hypertrophic cardiomyopathy who remained on treatment with the investigational agent mavacamten for a median of 62 weeks continued to show the same level of safe response to the drug as seen after the first 30 weeks on treatment in the pivotal trial for this agent.
The new findings from longer-term treatment bode well for mavacamten. That’s because if the drug is used in routine practice to avoid the need for surgery or an invasive intervention to reduce blockage of a patient’s left ventricular outflow tract, the duration of mavacamten treatment will likely need to continue for many years and even for decades, said Florian Rader, MD, who presented the results at the annual scientific sessions of the American College of Cardiology.
“In practice, mavacamten will probably be used for many, many years, especially as it replaces septal-reduction therapy, so we need long-term data,” noted Dr. Rader during a press briefing on his report. “I’m very happy with the long-term data” in the follow-up study.
The Food and Drug Administration is currently considering whether to approve mavacamten for routine marketing to treat patients with symptomatic obstructive hypertrophic cardiomyopathy (oHCM), with a decision expected by the end of April 2022.
The study Dr. Rader reported followed 231 patients with symptomatic oHCM who had completed the 30-week pivotal trial of mavacamten, EXPLORER-HCM, and opted to continue on open-label extended treatment with mavacamten, either continuing the treatment they started during the trial or crossing over to receive mavacamten after receiving placebo during the trial.
The major findings from EXPLORER-LTE (long-term extension) were that continued treatment for a median of about 62 weeks maintained the safety and efficacy findings seen at the end of the blinded, randomized, initial 30-week phase, said Dr. Rader, codirector of the Clinic for Hypertrophic Cardiomyopathy and Aortopathies at Cedars-Sinai Medical Center in Los Angeles.
‘Almost revolutionary’
Mavacamten represents “an almost revolutionary change” for treating oHCM, commented Maya E. Guglin, MD, professor of clinical medicine and an advanced heart failure physician at Indiana University, Indianapolis. “Until now, there was no good medical treatment for symptomatic oHCM. This will change the landscape, and without question it will change guidelines for treating oHCM,” said Dr. Guglin during the press briefing.
“All of us who care for patients with oHCM have looked forward to having a disease-specific therapy. It is encouraging to see that the safety and efficacy remained high with long-term follow-up,” commented Kyle W. Klarich, MD, a professor and cardiologist who specializes in treating patients with HCM at the Mayo Clinic in Rochester, Minn.
Mavacamten is a direct myosin inhibitor that reduces the excess number of myosin-actin cross bridges that form in patients with oHCM, and thereby directly targets the pathophysiology that underlies the disorder, explained Dr. Rader.
The patients on mavacamten included in the long-term extension reported by Dr. Rader averaged 60 years of age, and 61% were men. They averaged a 35.6–mm Hg drop in their resting left ventricular outflow tract (LVOT) gradient after 48 weeks on treatment, and a 32.8–mm Hg reduction after 84 weeks. When the investigators measured their LVOT gradient during a valsalva maneuver, their reductions from baseline averaged 45.3 mm Hg after 48 weeks and 46.4 mm Hg after 84 weeks.
Resting left ventricular ejection fraction also fell, by an average of 7.0 percentage points from baseline after 48 weeks, and by an average of 9.0 percentage points after 84 weeks. After 48 weeks on treatment, 68% of patients had at least a one-class improvement from baseline in their New York Heart Association functional class.
The safety results showed that most treatment-related adverse events were mild or moderate, and about 2% of patients had a serious drug-related adverse event. Ten of the 231 patients discontinued mavacamten because of a treated-related adverse event.
EXPLORER-HCM and EXPLORER-LTE were sponsored by MyoKardia, the company that is developing mavacamten and which is now owned by Bristol-Myers Squibb. Dr. Rader has been a consultant to MyoKardia as well as to Medtronic and ReCor. Dr. Guglin and Dr. Klarich had no disclosures.
WASHINGTON – Treatment of patients with symptomatic obstructive hypertrophic cardiomyopathy who remained on treatment with the investigational agent mavacamten for a median of 62 weeks continued to show the same level of safe response to the drug as seen after the first 30 weeks on treatment in the pivotal trial for this agent.
The new findings from longer-term treatment bode well for mavacamten. That’s because if the drug is used in routine practice to avoid the need for surgery or an invasive intervention to reduce blockage of a patient’s left ventricular outflow tract, the duration of mavacamten treatment will likely need to continue for many years and even for decades, said Florian Rader, MD, who presented the results at the annual scientific sessions of the American College of Cardiology.
“In practice, mavacamten will probably be used for many, many years, especially as it replaces septal-reduction therapy, so we need long-term data,” noted Dr. Rader during a press briefing on his report. “I’m very happy with the long-term data” in the follow-up study.
The Food and Drug Administration is currently considering whether to approve mavacamten for routine marketing to treat patients with symptomatic obstructive hypertrophic cardiomyopathy (oHCM), with a decision expected by the end of April 2022.
The study Dr. Rader reported followed 231 patients with symptomatic oHCM who had completed the 30-week pivotal trial of mavacamten, EXPLORER-HCM, and opted to continue on open-label extended treatment with mavacamten, either continuing the treatment they started during the trial or crossing over to receive mavacamten after receiving placebo during the trial.
The major findings from EXPLORER-LTE (long-term extension) were that continued treatment for a median of about 62 weeks maintained the safety and efficacy findings seen at the end of the blinded, randomized, initial 30-week phase, said Dr. Rader, codirector of the Clinic for Hypertrophic Cardiomyopathy and Aortopathies at Cedars-Sinai Medical Center in Los Angeles.
‘Almost revolutionary’
Mavacamten represents “an almost revolutionary change” for treating oHCM, commented Maya E. Guglin, MD, professor of clinical medicine and an advanced heart failure physician at Indiana University, Indianapolis. “Until now, there was no good medical treatment for symptomatic oHCM. This will change the landscape, and without question it will change guidelines for treating oHCM,” said Dr. Guglin during the press briefing.
“All of us who care for patients with oHCM have looked forward to having a disease-specific therapy. It is encouraging to see that the safety and efficacy remained high with long-term follow-up,” commented Kyle W. Klarich, MD, a professor and cardiologist who specializes in treating patients with HCM at the Mayo Clinic in Rochester, Minn.
Mavacamten is a direct myosin inhibitor that reduces the excess number of myosin-actin cross bridges that form in patients with oHCM, and thereby directly targets the pathophysiology that underlies the disorder, explained Dr. Rader.
The patients on mavacamten included in the long-term extension reported by Dr. Rader averaged 60 years of age, and 61% were men. They averaged a 35.6–mm Hg drop in their resting left ventricular outflow tract (LVOT) gradient after 48 weeks on treatment, and a 32.8–mm Hg reduction after 84 weeks. When the investigators measured their LVOT gradient during a valsalva maneuver, their reductions from baseline averaged 45.3 mm Hg after 48 weeks and 46.4 mm Hg after 84 weeks.
Resting left ventricular ejection fraction also fell, by an average of 7.0 percentage points from baseline after 48 weeks, and by an average of 9.0 percentage points after 84 weeks. After 48 weeks on treatment, 68% of patients had at least a one-class improvement from baseline in their New York Heart Association functional class.
The safety results showed that most treatment-related adverse events were mild or moderate, and about 2% of patients had a serious drug-related adverse event. Ten of the 231 patients discontinued mavacamten because of a treated-related adverse event.
EXPLORER-HCM and EXPLORER-LTE were sponsored by MyoKardia, the company that is developing mavacamten and which is now owned by Bristol-Myers Squibb. Dr. Rader has been a consultant to MyoKardia as well as to Medtronic and ReCor. Dr. Guglin and Dr. Klarich had no disclosures.
AT ACC 2022
VALOR-HCM: Novel drug may delay, avert invasive therapy in OHCM
Treatment with a novel myosin-inhibiting agent may improve symptoms and hemodynamics enough in patients with obstructive hypertrophic cardiomyopathy (OHCM) so that they can avoid or at least delay septal reduction therapy (SRT), suggests a randomized trial of modest size and duration.
Of 112 patients with OHCM who were sick enough while receiving standard medications to qualify for SRT, those assigned to take mavacamten (MyoKardia) instead of placebo were far less likely to still be eligible for SRT 16 weeks later.
In other words, their OHCM had improved enough during therapy with mavacamten such that SRT, either surgical septal myectomy or transcatheter alcohol septal ablation, could no longer be recommended per guidelines.
Mavacamten, which lessens myocardial contractility by selective inhibition of cardiac myosin, is the first agent tested in prospective trials to appear as a viable medical option in patients with severe, symptomatic OHCM, observed principal investigator Milind Y. Desai, MD, MBA, of the Cleveland Clinic.
“There’s clearly an unmet need for noninvasive therapies, medical therapies, that work in OHCM,” he said in an interview. Mavacamten “adds to the armamentarium” of OHCM management options and may give patients with symptoms despite conventional medications an alternative to SRT, which is considered definitive but has drawbacks.
The goal of SRT is to alleviate obstruction of the left ventricular outflow tract (LVOT), but surgical SRT requires a sternotomy, with all the risks and recovery time that entails. Catheter-based alcohol septal ablation is a less common alternative for some patients with suitable anatomy, Dr. Desai noted.
But those procedures “are not uniformly available, and even when available, the outcomes are fairly heterogeneous,” he said. “The guidelines recommend that you should go to a center with a mortality rate of less than 1% with these procedures. Centers like that are very few across the world,” and procedural mortality can be much higher at centers with less SRT experience.
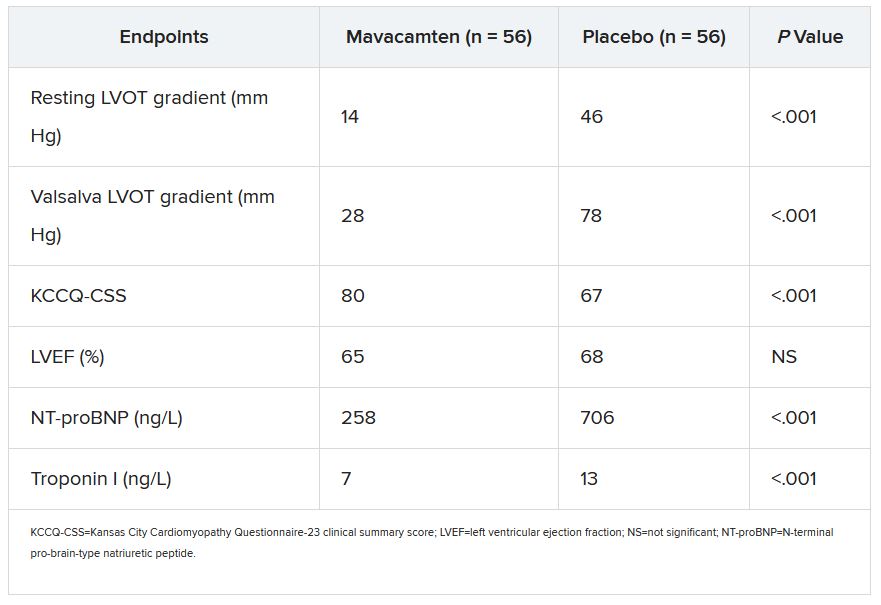
Dr. Desai presented the results of VALOR-HCM at the annual scientific sessions of the American College of Cardiology. Of the 56 patients assigned to mavacamten, 10 (17.9%) decided to undergo SRT by the end of the trial, or otherwise still met guideline-recommended criteria for receiving SRT, the primary endpoint. In comparison, 43 of the 56 patients (76.8%) in the control group (P < .0001) met that endpoint.
More patients receiving mavacamten improved by at least one New York Heart Association (NYHA) functional class during the trial’s 16 weeks: 63% versus 21% for those assigned to placebo. And 27% and 2%, respectively, improved by at least two NYHA classes, Dr. Desai said.
Guidelines recommend that SRT be reserved for patients in NYHA class III or IV heart failure with a resting or provoked LVOT gradient of at least 50 mm Hg.
Of note, Desai said, only two patients in each group elected to undergo SRT during the study. “The primary endpoint was driven by reduction in guideline eligibility for SRT, but 95% of patients in the study chose to continue with medical therapy.”
Speaking as a panelist after Dr. Desai’s presentation, Lynne W. Stevenson, MD, lauded the phase 3 trial’s “brave design,” which featured a highly unusual subjective primary endpoint and framed it as an advantage.
That the trial showed a significant mavacamten effect for that endpoint “answered, in one step, the question of what does this actually mean to the patient – which often takes much longer,” observed Dr. Stevenson, from Vanderbilt University, Nashville, Tenn.
Even so, she added, whether patients still qualified for SRT in the trial at least had to be supported by objective measures of LVOT gradient and NT-proBNP levels.
“My perspective is that of a cardiac surgeon who performs septal myectomies,” said John Cleveland, MD, University of Colorado at Denver, Aurora, who said he was impressed at how few patients receiving mavacamten went on to undergo SRT, while the rest were able to at least defer that decision.
Current recommendations are that patients who go to SRT “should be maximally medically treated and still symptomatic,” Dr. Cleveland observed at a press conference on VALOR-HCM. Should mavacamten be added to the list of agents to use before resorting to invasive therapy? “My answer would be yes,” he said, and patients who remain symptomatic even while receiving the myosin inhibitor and other medications should proceed to SRT.
The trial’s patients had documented OHCM, severe symptoms, and a resting or provoked LVOT gradient of at least 50 mm Hg despite maximally tolerated medications – which could include disopyramide, beta-blockers, and calcium channel blockers. About half the study population was female, and 89% were White. All had been referred for SRT.
Active therapy consisted of mavacamten initiated at 5 mg/day, with up-titrations at 8 and 12 weeks as tolerated, guided by echocardiographic left ventricular ejection fraction and LVOT gradient.
Most secondary endpoints improved significantly in patients receiving the drug, compared with placebo. They included measures of quality of life, symptom status, ventricular function, natriuretic peptides, and troponin I.
The secondary outcomes are consistent with what was observed in the EXPLORER-HCM trial, which in 2020 suggested that mavacamten could improve measures of quality of life, NYHA functional class, LVOT gradient, peak VO2, and other metrics in patients with OHCM.
Dr. Desai said mavacamten was well tolerated. “There were two patients who had a transient drop in ejection fraction to less than 50%, so the drug was temporarily discontinued, but resumed at a lower dose and they were able to complete the study.”
Dr. Stevenson commented on the “pretty quick” up-titration of mavacamten dosages in a study lasting only 4 months, which could have been a concern given the drug’s limited track record and its mechanism of action targeting contractility. “Fortunately, no serious safety signals” were observed.
Dr. Desai emphasized that mavacamten up-titrations were strictly guided by regular echocardiographic monitoring and assessment of LVOT gradients, in addition to clinical responses. And that, he said, is likely how up-titrations should be carried out if mavacamten is approved for OHCM.
VALOR-HCM was supported by MyoKardia. Dr. Desai disclosed receiving honoraria or consulting fees from Caristo Diagnostics, Medtronic, and MyoKardia. Dr. Stevenson disclosed receiving honoraria or consulting fees from Novartis; serving on a data safety monitoring board for Livanova; and other relationships with Abbott Medical, Biotronik, Boston Scientific, Bristol-Myers Squibb, Endotronic, Gore Medical, and Johnson & Johnson. Dr. Cleveland had no disclosures.
A version of this article first appeared on Medscape.com.
Treatment with a novel myosin-inhibiting agent may improve symptoms and hemodynamics enough in patients with obstructive hypertrophic cardiomyopathy (OHCM) so that they can avoid or at least delay septal reduction therapy (SRT), suggests a randomized trial of modest size and duration.
Of 112 patients with OHCM who were sick enough while receiving standard medications to qualify for SRT, those assigned to take mavacamten (MyoKardia) instead of placebo were far less likely to still be eligible for SRT 16 weeks later.
In other words, their OHCM had improved enough during therapy with mavacamten such that SRT, either surgical septal myectomy or transcatheter alcohol septal ablation, could no longer be recommended per guidelines.
Mavacamten, which lessens myocardial contractility by selective inhibition of cardiac myosin, is the first agent tested in prospective trials to appear as a viable medical option in patients with severe, symptomatic OHCM, observed principal investigator Milind Y. Desai, MD, MBA, of the Cleveland Clinic.
“There’s clearly an unmet need for noninvasive therapies, medical therapies, that work in OHCM,” he said in an interview. Mavacamten “adds to the armamentarium” of OHCM management options and may give patients with symptoms despite conventional medications an alternative to SRT, which is considered definitive but has drawbacks.
The goal of SRT is to alleviate obstruction of the left ventricular outflow tract (LVOT), but surgical SRT requires a sternotomy, with all the risks and recovery time that entails. Catheter-based alcohol septal ablation is a less common alternative for some patients with suitable anatomy, Dr. Desai noted.
But those procedures “are not uniformly available, and even when available, the outcomes are fairly heterogeneous,” he said. “The guidelines recommend that you should go to a center with a mortality rate of less than 1% with these procedures. Centers like that are very few across the world,” and procedural mortality can be much higher at centers with less SRT experience.
Dr. Desai presented the results of VALOR-HCM at the annual scientific sessions of the American College of Cardiology. Of the 56 patients assigned to mavacamten, 10 (17.9%) decided to undergo SRT by the end of the trial, or otherwise still met guideline-recommended criteria for receiving SRT, the primary endpoint. In comparison, 43 of the 56 patients (76.8%) in the control group (P < .0001) met that endpoint.
More patients receiving mavacamten improved by at least one New York Heart Association (NYHA) functional class during the trial’s 16 weeks: 63% versus 21% for those assigned to placebo. And 27% and 2%, respectively, improved by at least two NYHA classes, Dr. Desai said.
Guidelines recommend that SRT be reserved for patients in NYHA class III or IV heart failure with a resting or provoked LVOT gradient of at least 50 mm Hg.
Of note, Desai said, only two patients in each group elected to undergo SRT during the study. “The primary endpoint was driven by reduction in guideline eligibility for SRT, but 95% of patients in the study chose to continue with medical therapy.”
Speaking as a panelist after Dr. Desai’s presentation, Lynne W. Stevenson, MD, lauded the phase 3 trial’s “brave design,” which featured a highly unusual subjective primary endpoint and framed it as an advantage.
That the trial showed a significant mavacamten effect for that endpoint “answered, in one step, the question of what does this actually mean to the patient – which often takes much longer,” observed Dr. Stevenson, from Vanderbilt University, Nashville, Tenn.
Even so, she added, whether patients still qualified for SRT in the trial at least had to be supported by objective measures of LVOT gradient and NT-proBNP levels.
“My perspective is that of a cardiac surgeon who performs septal myectomies,” said John Cleveland, MD, University of Colorado at Denver, Aurora, who said he was impressed at how few patients receiving mavacamten went on to undergo SRT, while the rest were able to at least defer that decision.
Current recommendations are that patients who go to SRT “should be maximally medically treated and still symptomatic,” Dr. Cleveland observed at a press conference on VALOR-HCM. Should mavacamten be added to the list of agents to use before resorting to invasive therapy? “My answer would be yes,” he said, and patients who remain symptomatic even while receiving the myosin inhibitor and other medications should proceed to SRT.
The trial’s patients had documented OHCM, severe symptoms, and a resting or provoked LVOT gradient of at least 50 mm Hg despite maximally tolerated medications – which could include disopyramide, beta-blockers, and calcium channel blockers. About half the study population was female, and 89% were White. All had been referred for SRT.
Active therapy consisted of mavacamten initiated at 5 mg/day, with up-titrations at 8 and 12 weeks as tolerated, guided by echocardiographic left ventricular ejection fraction and LVOT gradient.
Most secondary endpoints improved significantly in patients receiving the drug, compared with placebo. They included measures of quality of life, symptom status, ventricular function, natriuretic peptides, and troponin I.
The secondary outcomes are consistent with what was observed in the EXPLORER-HCM trial, which in 2020 suggested that mavacamten could improve measures of quality of life, NYHA functional class, LVOT gradient, peak VO2, and other metrics in patients with OHCM.
Dr. Desai said mavacamten was well tolerated. “There were two patients who had a transient drop in ejection fraction to less than 50%, so the drug was temporarily discontinued, but resumed at a lower dose and they were able to complete the study.”
Dr. Stevenson commented on the “pretty quick” up-titration of mavacamten dosages in a study lasting only 4 months, which could have been a concern given the drug’s limited track record and its mechanism of action targeting contractility. “Fortunately, no serious safety signals” were observed.
Dr. Desai emphasized that mavacamten up-titrations were strictly guided by regular echocardiographic monitoring and assessment of LVOT gradients, in addition to clinical responses. And that, he said, is likely how up-titrations should be carried out if mavacamten is approved for OHCM.
VALOR-HCM was supported by MyoKardia. Dr. Desai disclosed receiving honoraria or consulting fees from Caristo Diagnostics, Medtronic, and MyoKardia. Dr. Stevenson disclosed receiving honoraria or consulting fees from Novartis; serving on a data safety monitoring board for Livanova; and other relationships with Abbott Medical, Biotronik, Boston Scientific, Bristol-Myers Squibb, Endotronic, Gore Medical, and Johnson & Johnson. Dr. Cleveland had no disclosures.
A version of this article first appeared on Medscape.com.
Treatment with a novel myosin-inhibiting agent may improve symptoms and hemodynamics enough in patients with obstructive hypertrophic cardiomyopathy (OHCM) so that they can avoid or at least delay septal reduction therapy (SRT), suggests a randomized trial of modest size and duration.
Of 112 patients with OHCM who were sick enough while receiving standard medications to qualify for SRT, those assigned to take mavacamten (MyoKardia) instead of placebo were far less likely to still be eligible for SRT 16 weeks later.
In other words, their OHCM had improved enough during therapy with mavacamten such that SRT, either surgical septal myectomy or transcatheter alcohol septal ablation, could no longer be recommended per guidelines.
Mavacamten, which lessens myocardial contractility by selective inhibition of cardiac myosin, is the first agent tested in prospective trials to appear as a viable medical option in patients with severe, symptomatic OHCM, observed principal investigator Milind Y. Desai, MD, MBA, of the Cleveland Clinic.
“There’s clearly an unmet need for noninvasive therapies, medical therapies, that work in OHCM,” he said in an interview. Mavacamten “adds to the armamentarium” of OHCM management options and may give patients with symptoms despite conventional medications an alternative to SRT, which is considered definitive but has drawbacks.
The goal of SRT is to alleviate obstruction of the left ventricular outflow tract (LVOT), but surgical SRT requires a sternotomy, with all the risks and recovery time that entails. Catheter-based alcohol septal ablation is a less common alternative for some patients with suitable anatomy, Dr. Desai noted.
But those procedures “are not uniformly available, and even when available, the outcomes are fairly heterogeneous,” he said. “The guidelines recommend that you should go to a center with a mortality rate of less than 1% with these procedures. Centers like that are very few across the world,” and procedural mortality can be much higher at centers with less SRT experience.
Dr. Desai presented the results of VALOR-HCM at the annual scientific sessions of the American College of Cardiology. Of the 56 patients assigned to mavacamten, 10 (17.9%) decided to undergo SRT by the end of the trial, or otherwise still met guideline-recommended criteria for receiving SRT, the primary endpoint. In comparison, 43 of the 56 patients (76.8%) in the control group (P < .0001) met that endpoint.
More patients receiving mavacamten improved by at least one New York Heart Association (NYHA) functional class during the trial’s 16 weeks: 63% versus 21% for those assigned to placebo. And 27% and 2%, respectively, improved by at least two NYHA classes, Dr. Desai said.
Guidelines recommend that SRT be reserved for patients in NYHA class III or IV heart failure with a resting or provoked LVOT gradient of at least 50 mm Hg.
Of note, Desai said, only two patients in each group elected to undergo SRT during the study. “The primary endpoint was driven by reduction in guideline eligibility for SRT, but 95% of patients in the study chose to continue with medical therapy.”
Speaking as a panelist after Dr. Desai’s presentation, Lynne W. Stevenson, MD, lauded the phase 3 trial’s “brave design,” which featured a highly unusual subjective primary endpoint and framed it as an advantage.
That the trial showed a significant mavacamten effect for that endpoint “answered, in one step, the question of what does this actually mean to the patient – which often takes much longer,” observed Dr. Stevenson, from Vanderbilt University, Nashville, Tenn.
Even so, she added, whether patients still qualified for SRT in the trial at least had to be supported by objective measures of LVOT gradient and NT-proBNP levels.
“My perspective is that of a cardiac surgeon who performs septal myectomies,” said John Cleveland, MD, University of Colorado at Denver, Aurora, who said he was impressed at how few patients receiving mavacamten went on to undergo SRT, while the rest were able to at least defer that decision.
Current recommendations are that patients who go to SRT “should be maximally medically treated and still symptomatic,” Dr. Cleveland observed at a press conference on VALOR-HCM. Should mavacamten be added to the list of agents to use before resorting to invasive therapy? “My answer would be yes,” he said, and patients who remain symptomatic even while receiving the myosin inhibitor and other medications should proceed to SRT.
The trial’s patients had documented OHCM, severe symptoms, and a resting or provoked LVOT gradient of at least 50 mm Hg despite maximally tolerated medications – which could include disopyramide, beta-blockers, and calcium channel blockers. About half the study population was female, and 89% were White. All had been referred for SRT.
Active therapy consisted of mavacamten initiated at 5 mg/day, with up-titrations at 8 and 12 weeks as tolerated, guided by echocardiographic left ventricular ejection fraction and LVOT gradient.
Most secondary endpoints improved significantly in patients receiving the drug, compared with placebo. They included measures of quality of life, symptom status, ventricular function, natriuretic peptides, and troponin I.
The secondary outcomes are consistent with what was observed in the EXPLORER-HCM trial, which in 2020 suggested that mavacamten could improve measures of quality of life, NYHA functional class, LVOT gradient, peak VO2, and other metrics in patients with OHCM.
Dr. Desai said mavacamten was well tolerated. “There were two patients who had a transient drop in ejection fraction to less than 50%, so the drug was temporarily discontinued, but resumed at a lower dose and they were able to complete the study.”
Dr. Stevenson commented on the “pretty quick” up-titration of mavacamten dosages in a study lasting only 4 months, which could have been a concern given the drug’s limited track record and its mechanism of action targeting contractility. “Fortunately, no serious safety signals” were observed.
Dr. Desai emphasized that mavacamten up-titrations were strictly guided by regular echocardiographic monitoring and assessment of LVOT gradients, in addition to clinical responses. And that, he said, is likely how up-titrations should be carried out if mavacamten is approved for OHCM.
VALOR-HCM was supported by MyoKardia. Dr. Desai disclosed receiving honoraria or consulting fees from Caristo Diagnostics, Medtronic, and MyoKardia. Dr. Stevenson disclosed receiving honoraria or consulting fees from Novartis; serving on a data safety monitoring board for Livanova; and other relationships with Abbott Medical, Biotronik, Boston Scientific, Bristol-Myers Squibb, Endotronic, Gore Medical, and Johnson & Johnson. Dr. Cleveland had no disclosures.
A version of this article first appeared on Medscape.com.
FROM ACC 2022
SCORED: Sotagliflozin shows robust MACE benefit
WASHINGTON – Results from new analyses further fleshed out the potent effect by the investigational SGLT1&2 inhibitor sotagliflozin on major cardiovascular adverse events in patients with type 2 diabetes, chronic kidney disease, and at high risk for cardiovascular disease in the SCORED trial that randomized more than 10,000 patients.
In prespecified, secondary analyses of the SCORED results, treatment with sotagliflozin during a median of 16 months was linked to a significant 21% risk reduction relative to placebo for the combined incidence of total major adverse cardiovascular events (MACE), which included cardiovascular death, first and recurrent episodes of nonfatal MI, and nonfatal stroke among the 5,144 randomized patients who entered the trial with a history of cardiovascular disease (CVD), Deepak L. Bhatt, MD, said at the annual scientific sessions of the American College of Cardiology.
Among the 5,440 patients in the study who did not have a history of CVD (although they did have at least one major risk factor or at least two minor risk factors), treatment with sotagliflozin was linked to a significant 26% relative risk reduction in total MACE events.
Part of these overall MACE benefits resulted from similar improvements from sotagliflozin treatment on the individual outcomes of total nonfatal MI and total nonfatal strokes. Treatment with sotagliflozin cut these MIs by a significant 31% in patients with a history of CVD relative to patients who received placebo, and by a relative 34% in those without a CVD event in their history, a difference compared with placebo that fell short of significance, said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of interventional cardiovascular programs at Brigham and Women’s Health, both in Boston.
Treatment with sotagliflozin also cut total nonfatal strokes by 31% relative to placebo in patients with a history of CVD, and by a relative 38% in those without a CVD history. Both differences fell short of significance.
An early MACE benefit and a stroke benefit
“This stroke benefit has not been clearly seen” with any agent from the closely related sodium-glucose cotransport-2 (SGLT2) inhibitor class, and “the MACE benefit appeared very early,” within 3 months from the start of sotagliflozin treatment, “which may be because of the SGLT1 inhibition,” Dr. Bhatt said during his report.
The SGLT1 receptor is the primary mechanism cells in the gut use to absorb glucose and galactose in the human gastrointestinal tract, Dr. Bhatt explained, while the SGLT2 receptor appears on kidney cells and is the major player in the reabsorption of filtered glucose. The SGLT2 inhibitor class includes the agents canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), while sotagliflozin inhibits both SGLT1 and SGLT2.
Main results from SCORED appeared in a report first released in late 2020, and showed that for the study’s primary endpoint treatment with sotagliflozin linked with a significant 26% relative risk reduction for the composite of cardiovascular deaths, hospitalizations for heart failure, and urgent visits for heart failure (N Engl J Med. 2021 Jan 14;384[2]:129-39). Patient follow-up in SCORED was not as long as originally planned when the study stopped early due to a loss of funding from a sponsor that was triggered by the COVID-19 pandemic.
MACE results ‘heterogeneous’ from SGLT2 inhibitors
Sotagliflozin and agents from the SGLT2 inhibitor class “have been consistent” in their benefits for reducing cardiovascular death and hospitalization for heart failure, but for MACE, the results from the SGLT2 inhibitors “have been more heterogeneous,” and the effect of sotagliflozin on MACE “were different in SCORED,” commented Michelle L. O’Donoghue, MD, MPH, a cardiologist at Brigham and Women’s Hospital in Boston who was not involved with this work.
“The results suggest a benefit [from sotagliflozin] on atherosclerotic events, which could be a potential advantage” compared with the SGLT2 inhibitors, “but the heterogeneity of this effect” among these agents means that more confirmatory data are needed for sotagliflozin, Dr. O’Donoghue said in an interview.
“There is a lot of enthusiasm for the concept” of combined inhibition of the SGLT1 and 2 receptors, and if more evidence for unique benefits of this effect accumulate “it may lead to increased enthusiasm for sotagliflozin,” she said. “A lot will also depend on pricing decisions” for sotagliflozin, if it receives U.S. marketing approval from the Food and Drug Administration. Decisions about which agent from the SGLT2 inhibitor class to prescribe “are often being made based on price right now,” Dr. O’Donoghue said.
Lexicon Pharmaceuticals, the company developing sotagliflozin, has announced plans to resubmit its new drug application for sotagliflozin to the FDA later in 2022, with the agency’s approval decision likely occurring late in 2022 or sometime during 2023. In February, the company withdrew its December 2021 application to correct a “technical issue” it had found.
An additional analysis reported by Dr. Bhatt used combined data from SCORED as well as several additional randomized trials of sotagliflozin involving a total of more than 20,000 patients that showed a significant 21% reduction in the incidence of MACE compared with placebo.
During his talk, Dr. Bhatt said that sotagliflozin was potentially superior to the agents that inhibit only SGLT2. In an interview, he based this tentative assessment on at least four attributes of sotagliflozin that have emerged from trial results:
- The drug’s ability to significantly reduce MACE and to have this effect apparent within a few months of treatment onset;
- The significantly reduced rate of stroke with sotagliflozin (when patients are not subdivided into those with or without a history of CVD) that has not yet been seen with any SGLT2 inhibitor;
- The ability of sotagliflozin to reduce hemoglobin A1c levels in patients with type 2 diabetes even when their estimated glomerular filtration rate is less than 30 mL/min per 1.73 m2, an effect not seen with SGLT2 inhibitors and possibly explained by sotagliflozin having an effect on gut absorption of glucose in addition to its SGLT2 inhibitory effect in the kidney;
- And the proven ability of sotagliflozin to be safe and effective when initiated in patients hospitalized for heart failure, a property that so far has only also been shown for the SGLT2 inhibitor empagliflozin in the EMPULSE trial (Nature Med. 2022 Mar;28: 568-74).
SCORED was sponsored by Sanofi and Lexicon Pharmaceuticals, the companies originally developing sotagliflozin, although with the withdrawal of Sanofi’s support, further development is now sponsored entirely by Lexicon. Dr. Bhatt received research funding from Sanofi and Lexicon that was paid to Brigham and Women’s Health, and he has been an advisor to numerous companies. Dr. O’Donoghue has been a consultant to Amgen, Janssen, and Novartis, and has received research funding from Amgen, AZ MedImmune, Intarcia, Janssen, Merck, and Novartis.
WASHINGTON – Results from new analyses further fleshed out the potent effect by the investigational SGLT1&2 inhibitor sotagliflozin on major cardiovascular adverse events in patients with type 2 diabetes, chronic kidney disease, and at high risk for cardiovascular disease in the SCORED trial that randomized more than 10,000 patients.
In prespecified, secondary analyses of the SCORED results, treatment with sotagliflozin during a median of 16 months was linked to a significant 21% risk reduction relative to placebo for the combined incidence of total major adverse cardiovascular events (MACE), which included cardiovascular death, first and recurrent episodes of nonfatal MI, and nonfatal stroke among the 5,144 randomized patients who entered the trial with a history of cardiovascular disease (CVD), Deepak L. Bhatt, MD, said at the annual scientific sessions of the American College of Cardiology.
Among the 5,440 patients in the study who did not have a history of CVD (although they did have at least one major risk factor or at least two minor risk factors), treatment with sotagliflozin was linked to a significant 26% relative risk reduction in total MACE events.
Part of these overall MACE benefits resulted from similar improvements from sotagliflozin treatment on the individual outcomes of total nonfatal MI and total nonfatal strokes. Treatment with sotagliflozin cut these MIs by a significant 31% in patients with a history of CVD relative to patients who received placebo, and by a relative 34% in those without a CVD event in their history, a difference compared with placebo that fell short of significance, said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of interventional cardiovascular programs at Brigham and Women’s Health, both in Boston.
Treatment with sotagliflozin also cut total nonfatal strokes by 31% relative to placebo in patients with a history of CVD, and by a relative 38% in those without a CVD history. Both differences fell short of significance.
An early MACE benefit and a stroke benefit
“This stroke benefit has not been clearly seen” with any agent from the closely related sodium-glucose cotransport-2 (SGLT2) inhibitor class, and “the MACE benefit appeared very early,” within 3 months from the start of sotagliflozin treatment, “which may be because of the SGLT1 inhibition,” Dr. Bhatt said during his report.
The SGLT1 receptor is the primary mechanism cells in the gut use to absorb glucose and galactose in the human gastrointestinal tract, Dr. Bhatt explained, while the SGLT2 receptor appears on kidney cells and is the major player in the reabsorption of filtered glucose. The SGLT2 inhibitor class includes the agents canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), while sotagliflozin inhibits both SGLT1 and SGLT2.
Main results from SCORED appeared in a report first released in late 2020, and showed that for the study’s primary endpoint treatment with sotagliflozin linked with a significant 26% relative risk reduction for the composite of cardiovascular deaths, hospitalizations for heart failure, and urgent visits for heart failure (N Engl J Med. 2021 Jan 14;384[2]:129-39). Patient follow-up in SCORED was not as long as originally planned when the study stopped early due to a loss of funding from a sponsor that was triggered by the COVID-19 pandemic.
MACE results ‘heterogeneous’ from SGLT2 inhibitors
Sotagliflozin and agents from the SGLT2 inhibitor class “have been consistent” in their benefits for reducing cardiovascular death and hospitalization for heart failure, but for MACE, the results from the SGLT2 inhibitors “have been more heterogeneous,” and the effect of sotagliflozin on MACE “were different in SCORED,” commented Michelle L. O’Donoghue, MD, MPH, a cardiologist at Brigham and Women’s Hospital in Boston who was not involved with this work.
“The results suggest a benefit [from sotagliflozin] on atherosclerotic events, which could be a potential advantage” compared with the SGLT2 inhibitors, “but the heterogeneity of this effect” among these agents means that more confirmatory data are needed for sotagliflozin, Dr. O’Donoghue said in an interview.
“There is a lot of enthusiasm for the concept” of combined inhibition of the SGLT1 and 2 receptors, and if more evidence for unique benefits of this effect accumulate “it may lead to increased enthusiasm for sotagliflozin,” she said. “A lot will also depend on pricing decisions” for sotagliflozin, if it receives U.S. marketing approval from the Food and Drug Administration. Decisions about which agent from the SGLT2 inhibitor class to prescribe “are often being made based on price right now,” Dr. O’Donoghue said.
Lexicon Pharmaceuticals, the company developing sotagliflozin, has announced plans to resubmit its new drug application for sotagliflozin to the FDA later in 2022, with the agency’s approval decision likely occurring late in 2022 or sometime during 2023. In February, the company withdrew its December 2021 application to correct a “technical issue” it had found.
An additional analysis reported by Dr. Bhatt used combined data from SCORED as well as several additional randomized trials of sotagliflozin involving a total of more than 20,000 patients that showed a significant 21% reduction in the incidence of MACE compared with placebo.
During his talk, Dr. Bhatt said that sotagliflozin was potentially superior to the agents that inhibit only SGLT2. In an interview, he based this tentative assessment on at least four attributes of sotagliflozin that have emerged from trial results:
- The drug’s ability to significantly reduce MACE and to have this effect apparent within a few months of treatment onset;
- The significantly reduced rate of stroke with sotagliflozin (when patients are not subdivided into those with or without a history of CVD) that has not yet been seen with any SGLT2 inhibitor;
- The ability of sotagliflozin to reduce hemoglobin A1c levels in patients with type 2 diabetes even when their estimated glomerular filtration rate is less than 30 mL/min per 1.73 m2, an effect not seen with SGLT2 inhibitors and possibly explained by sotagliflozin having an effect on gut absorption of glucose in addition to its SGLT2 inhibitory effect in the kidney;
- And the proven ability of sotagliflozin to be safe and effective when initiated in patients hospitalized for heart failure, a property that so far has only also been shown for the SGLT2 inhibitor empagliflozin in the EMPULSE trial (Nature Med. 2022 Mar;28: 568-74).
SCORED was sponsored by Sanofi and Lexicon Pharmaceuticals, the companies originally developing sotagliflozin, although with the withdrawal of Sanofi’s support, further development is now sponsored entirely by Lexicon. Dr. Bhatt received research funding from Sanofi and Lexicon that was paid to Brigham and Women’s Health, and he has been an advisor to numerous companies. Dr. O’Donoghue has been a consultant to Amgen, Janssen, and Novartis, and has received research funding from Amgen, AZ MedImmune, Intarcia, Janssen, Merck, and Novartis.
WASHINGTON – Results from new analyses further fleshed out the potent effect by the investigational SGLT1&2 inhibitor sotagliflozin on major cardiovascular adverse events in patients with type 2 diabetes, chronic kidney disease, and at high risk for cardiovascular disease in the SCORED trial that randomized more than 10,000 patients.
In prespecified, secondary analyses of the SCORED results, treatment with sotagliflozin during a median of 16 months was linked to a significant 21% risk reduction relative to placebo for the combined incidence of total major adverse cardiovascular events (MACE), which included cardiovascular death, first and recurrent episodes of nonfatal MI, and nonfatal stroke among the 5,144 randomized patients who entered the trial with a history of cardiovascular disease (CVD), Deepak L. Bhatt, MD, said at the annual scientific sessions of the American College of Cardiology.
Among the 5,440 patients in the study who did not have a history of CVD (although they did have at least one major risk factor or at least two minor risk factors), treatment with sotagliflozin was linked to a significant 26% relative risk reduction in total MACE events.
Part of these overall MACE benefits resulted from similar improvements from sotagliflozin treatment on the individual outcomes of total nonfatal MI and total nonfatal strokes. Treatment with sotagliflozin cut these MIs by a significant 31% in patients with a history of CVD relative to patients who received placebo, and by a relative 34% in those without a CVD event in their history, a difference compared with placebo that fell short of significance, said Dr. Bhatt, professor of medicine at Harvard Medical School and executive director of interventional cardiovascular programs at Brigham and Women’s Health, both in Boston.
Treatment with sotagliflozin also cut total nonfatal strokes by 31% relative to placebo in patients with a history of CVD, and by a relative 38% in those without a CVD history. Both differences fell short of significance.
An early MACE benefit and a stroke benefit
“This stroke benefit has not been clearly seen” with any agent from the closely related sodium-glucose cotransport-2 (SGLT2) inhibitor class, and “the MACE benefit appeared very early,” within 3 months from the start of sotagliflozin treatment, “which may be because of the SGLT1 inhibition,” Dr. Bhatt said during his report.
The SGLT1 receptor is the primary mechanism cells in the gut use to absorb glucose and galactose in the human gastrointestinal tract, Dr. Bhatt explained, while the SGLT2 receptor appears on kidney cells and is the major player in the reabsorption of filtered glucose. The SGLT2 inhibitor class includes the agents canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance), while sotagliflozin inhibits both SGLT1 and SGLT2.
Main results from SCORED appeared in a report first released in late 2020, and showed that for the study’s primary endpoint treatment with sotagliflozin linked with a significant 26% relative risk reduction for the composite of cardiovascular deaths, hospitalizations for heart failure, and urgent visits for heart failure (N Engl J Med. 2021 Jan 14;384[2]:129-39). Patient follow-up in SCORED was not as long as originally planned when the study stopped early due to a loss of funding from a sponsor that was triggered by the COVID-19 pandemic.
MACE results ‘heterogeneous’ from SGLT2 inhibitors
Sotagliflozin and agents from the SGLT2 inhibitor class “have been consistent” in their benefits for reducing cardiovascular death and hospitalization for heart failure, but for MACE, the results from the SGLT2 inhibitors “have been more heterogeneous,” and the effect of sotagliflozin on MACE “were different in SCORED,” commented Michelle L. O’Donoghue, MD, MPH, a cardiologist at Brigham and Women’s Hospital in Boston who was not involved with this work.
“The results suggest a benefit [from sotagliflozin] on atherosclerotic events, which could be a potential advantage” compared with the SGLT2 inhibitors, “but the heterogeneity of this effect” among these agents means that more confirmatory data are needed for sotagliflozin, Dr. O’Donoghue said in an interview.
“There is a lot of enthusiasm for the concept” of combined inhibition of the SGLT1 and 2 receptors, and if more evidence for unique benefits of this effect accumulate “it may lead to increased enthusiasm for sotagliflozin,” she said. “A lot will also depend on pricing decisions” for sotagliflozin, if it receives U.S. marketing approval from the Food and Drug Administration. Decisions about which agent from the SGLT2 inhibitor class to prescribe “are often being made based on price right now,” Dr. O’Donoghue said.
Lexicon Pharmaceuticals, the company developing sotagliflozin, has announced plans to resubmit its new drug application for sotagliflozin to the FDA later in 2022, with the agency’s approval decision likely occurring late in 2022 or sometime during 2023. In February, the company withdrew its December 2021 application to correct a “technical issue” it had found.
An additional analysis reported by Dr. Bhatt used combined data from SCORED as well as several additional randomized trials of sotagliflozin involving a total of more than 20,000 patients that showed a significant 21% reduction in the incidence of MACE compared with placebo.
During his talk, Dr. Bhatt said that sotagliflozin was potentially superior to the agents that inhibit only SGLT2. In an interview, he based this tentative assessment on at least four attributes of sotagliflozin that have emerged from trial results:
- The drug’s ability to significantly reduce MACE and to have this effect apparent within a few months of treatment onset;
- The significantly reduced rate of stroke with sotagliflozin (when patients are not subdivided into those with or without a history of CVD) that has not yet been seen with any SGLT2 inhibitor;
- The ability of sotagliflozin to reduce hemoglobin A1c levels in patients with type 2 diabetes even when their estimated glomerular filtration rate is less than 30 mL/min per 1.73 m2, an effect not seen with SGLT2 inhibitors and possibly explained by sotagliflozin having an effect on gut absorption of glucose in addition to its SGLT2 inhibitory effect in the kidney;
- And the proven ability of sotagliflozin to be safe and effective when initiated in patients hospitalized for heart failure, a property that so far has only also been shown for the SGLT2 inhibitor empagliflozin in the EMPULSE trial (Nature Med. 2022 Mar;28: 568-74).
SCORED was sponsored by Sanofi and Lexicon Pharmaceuticals, the companies originally developing sotagliflozin, although with the withdrawal of Sanofi’s support, further development is now sponsored entirely by Lexicon. Dr. Bhatt received research funding from Sanofi and Lexicon that was paid to Brigham and Women’s Health, and he has been an advisor to numerous companies. Dr. O’Donoghue has been a consultant to Amgen, Janssen, and Novartis, and has received research funding from Amgen, AZ MedImmune, Intarcia, Janssen, Merck, and Novartis.
AT ACC 2022
Low-sodium diet did not cut clinical events in heart failure trial
A low-sodium diet was not associated with a reduction in future clinical events in a new study in ambulatory patients with heart failure. But there was a moderate benefit on quality of life and New York Heart Association (NYHA) functional class.
The results of the SODIUM-HF trial were presented April 2 at the annual scientific sessions of the American College of Cardiology, conducted virtually and in person in Washington. They were also simultaneously published online in the Lancet.
The study found that a strategy to reduce dietary sodium intake to less than 1,500 mg daily was not more effective than usual care in reducing the primary endpoint of risk for hospitalization or emergency department visits due to cardiovascular causes or all-cause death at 12 months.
“This is the largest and longest trial to look at the question of reducing dietary sodium in heart failure patients,” lead author Justin Ezekowitz, MBBCh, from the Canadian VIGOUR Center at the University of Alberta, Edmonton, Canada, told this news organization.
But he pointed out that there were fewer events than expected in the study, which was stopped early because of a combination of futility and practical difficulties caused by the COVID pandemic, so it could have been underpowered. Dr. Ezekowitz also suggested that a greater reduction in sodium than achieved in this study or a longer follow-up may be required to show an effect on clinical events.
“We hope others will do additional studies of sodium as well as other dietary recommendations as part of a comprehensive diet for heart failure patients,” he commented.
Dr. Ezekowitz said that the study results did not allow blanket recommendations to be made on reducing sodium intake in heart failure.
But he added: “I don’t think we should write off sodium reduction in this population. I think we can tell patients that reducing dietary sodium may potentially improve symptoms and quality of life, and I will continue to recommend reducing sodium as part of an overall healthy diet. We don’t want to throw the baby out with the bathwater.”
Dr. Ezekowitz noted that heart failure is associated with neurohormonal activation and abnormalities in autonomic control that lead to sodium and water retention; thus, dietary restriction of sodium has been historically endorsed as a mechanism to prevent fluid overload and subsequent clinical outcomes; however, clinical trials so far have shown mixed results.
“The guidelines used to strongly recommend a reduction in sodium intake in heart failure patients, but this advice has backed off in recent years because of the lack of data. Most heart failure guidelines now do not make any recommendations on dietary sodium,” he said.
SODIUM-HF was a pragmatic, multinational, open-label, randomized trial conducted in six countries (Australia, Canada, Chile, Colombia, Mexico, and New Zealand), which included 809 patients (median age, 67 years) with chronic heart failure (NYHA functional class II–III) who were receiving optimally tolerated guideline-directed medical treatment. They were randomly assigned to usual care according to local guidelines or a low-sodium diet of less than 100 mmol (<1,500 mg/day). Patients with a baseline sodium intake of less than 1,500 mg/day were excluded.
In the intervention group, patients were asked to follow low-sodium menus developed by dietitians localized to each region. They also received behavioral counseling by trained dietitians or physicians or nurses.
Dietary sodium intake was assessed by using a 3-day food record (including 1 weekend day) at baseline, 6 months, and 12 months in both groups and, for the intervention group, also at 3 and 9 months to monitor and support dietary adherence.
Dr. Ezekowitz explained that although the best method for measuring sodium levels would normally be a 24-hour urine sodium, this would be impractical in a large clinical trial. In addition, he pointed out that urinary sodium is not an accurate measure of actual sodium levels in patients taking diuretics, so it is not a good measure to use in a heart failure population.
“The food record method of assessing sodium levels has been well validated; I think we measured it as accurately as we could have done,” he added.
Results showed that between baseline and 12 months, the median sodium intake decreased from 2,286 mg/day to 1,658 mg/day in the low-sodium group and from 2,119 mg/day to 2,073 mg/day in the usual care group. The median difference between groups was 415 mg/day at 12 months.
By 12 months, events comprising the primary outcome (hospitalization or emergency department visits due to cardiovascular causes or all-cause death) had occurred in 15% of patients in the low-sodium diet group and 17% of those in the usual care group (hazard ratio [HR], 0.89 [95% CI, 0.63 - 1.26]; P = .53).
All-cause death occurred in 6% of patients in the low-sodium diet group and 4% of those in the usual care group (HR, 1.38; P = .32). Cardiovascular-related hospitalization occurred in 10% of the low-sodium group and 12% of the usual care group (HR, 0.82; P = .36), and cardiovascular-related emergency department visits occurred in 4% of both groups (HR, 1.21; P = .60).
The absence of treatment effect for the primary outcome was consistent across most prespecified subgroups, including those with higher vs lower baseline sodium intake. But there was a suggestion of a greater reduction in the primary outcome in individuals younger than age 65 years than in those age 65 years and older.
Quality-of-life measures on the Kansas City Cardiomyopathy Questionnaire (KCCQ) suggested a benefit in the low-sodium group, with mean between-group differences in the change from baseline to 12 months of 3.38 points in the overall summary score, 3.29 points in the clinical summary score, and 3.77 points in the physical limitation score (all differences were statistically significant).
There was no significant difference in 6-minute-walk distance at 12 months between the low-sodium diet group and the usual care group.
NYHA functional class at 12 months differed significantly between groups; the low-sodium diet group had a greater likelihood of improving by one NYHA class than the usual care group (odds ratio, 0.59; P = .0061).
No safety events related to the study treatment were reported in either group.
Dr. Ezekowitz said that to investigate whether longer follow-up may show a difference in events, further analyses are planned at 2 years and 5 years.
Questions on food recall and blinding
Commenting on the findings at the late-breaking clinical trials session at the ACC meeting, Biykem Bozkurt, MD, professor of medicine at Baylor College of Medicine, Houston, congratulated Dr. Ezekowitz on conducting this trial.
“We have been chasing the holy grail of sodium reduction in heart failure for a very long time, so I have to commend you and your team for taking on this challenge, especially during the pandemic,” she said.
But Dr. Bozkurt questioned whether the intervention group actually had a meaningful sodium reduction given that this was measured by food recall and this may have been accounted for by under-reporting of certain food intakes.
Dr. Ezekowitz responded that patients acted as their own controls in that calorie intake, fluid intake, and weight were also assessed and did not change. “So I think we did have a meaningful reduction in sodium,” he said.
Dr. Bozkurt also queried whether the improvements in quality of life and functional status were reliable given that this was an unblinded study.
To this point, Dr. Ezekowitz pointed out that the KCCQ quality-of-life measure was a highly validated instrument and that improvements were seen in these measures at 3, 6, and 12 months. “It is not like these were spurious findings, so I think we have to look at this as a real result,” he argued.
Commenting on the study at an ACC press conference, Mary Norine Walsh, MD, director of the heart failure and cardiac transplantation programs at St. Vincent Heart Center in Indianapolis, said the trial had answered two important questions: that sodium reduction in heart failure may not reduce heart failure hospitalization/death but that patients feel better.
“I think we can safely tell patients that if they slip up a bit they may not end up in hospital,” she added.
This study was funded by the Canadian Institutes of Health Research and the University Hospital Foundation (Edmonton, Alberta, Canada) and the Health Research Council of New Zealand. Dr. Ezekowitz reports research grants from American Regent, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb/Pfizer, eko.ai, US2.ai, Merck, Novartis, Otsuka, Sanofi, and Servier and consulting fees from American Regent, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb/Pfizer, Merck, Novartis, Otsuka, Sanofi, and Servier.
A version of this article first appeared on Medscape.com.
A low-sodium diet was not associated with a reduction in future clinical events in a new study in ambulatory patients with heart failure. But there was a moderate benefit on quality of life and New York Heart Association (NYHA) functional class.
The results of the SODIUM-HF trial were presented April 2 at the annual scientific sessions of the American College of Cardiology, conducted virtually and in person in Washington. They were also simultaneously published online in the Lancet.
The study found that a strategy to reduce dietary sodium intake to less than 1,500 mg daily was not more effective than usual care in reducing the primary endpoint of risk for hospitalization or emergency department visits due to cardiovascular causes or all-cause death at 12 months.
“This is the largest and longest trial to look at the question of reducing dietary sodium in heart failure patients,” lead author Justin Ezekowitz, MBBCh, from the Canadian VIGOUR Center at the University of Alberta, Edmonton, Canada, told this news organization.
But he pointed out that there were fewer events than expected in the study, which was stopped early because of a combination of futility and practical difficulties caused by the COVID pandemic, so it could have been underpowered. Dr. Ezekowitz also suggested that a greater reduction in sodium than achieved in this study or a longer follow-up may be required to show an effect on clinical events.
“We hope others will do additional studies of sodium as well as other dietary recommendations as part of a comprehensive diet for heart failure patients,” he commented.
Dr. Ezekowitz said that the study results did not allow blanket recommendations to be made on reducing sodium intake in heart failure.
But he added: “I don’t think we should write off sodium reduction in this population. I think we can tell patients that reducing dietary sodium may potentially improve symptoms and quality of life, and I will continue to recommend reducing sodium as part of an overall healthy diet. We don’t want to throw the baby out with the bathwater.”
Dr. Ezekowitz noted that heart failure is associated with neurohormonal activation and abnormalities in autonomic control that lead to sodium and water retention; thus, dietary restriction of sodium has been historically endorsed as a mechanism to prevent fluid overload and subsequent clinical outcomes; however, clinical trials so far have shown mixed results.
“The guidelines used to strongly recommend a reduction in sodium intake in heart failure patients, but this advice has backed off in recent years because of the lack of data. Most heart failure guidelines now do not make any recommendations on dietary sodium,” he said.
SODIUM-HF was a pragmatic, multinational, open-label, randomized trial conducted in six countries (Australia, Canada, Chile, Colombia, Mexico, and New Zealand), which included 809 patients (median age, 67 years) with chronic heart failure (NYHA functional class II–III) who were receiving optimally tolerated guideline-directed medical treatment. They were randomly assigned to usual care according to local guidelines or a low-sodium diet of less than 100 mmol (<1,500 mg/day). Patients with a baseline sodium intake of less than 1,500 mg/day were excluded.
In the intervention group, patients were asked to follow low-sodium menus developed by dietitians localized to each region. They also received behavioral counseling by trained dietitians or physicians or nurses.
Dietary sodium intake was assessed by using a 3-day food record (including 1 weekend day) at baseline, 6 months, and 12 months in both groups and, for the intervention group, also at 3 and 9 months to monitor and support dietary adherence.
Dr. Ezekowitz explained that although the best method for measuring sodium levels would normally be a 24-hour urine sodium, this would be impractical in a large clinical trial. In addition, he pointed out that urinary sodium is not an accurate measure of actual sodium levels in patients taking diuretics, so it is not a good measure to use in a heart failure population.
“The food record method of assessing sodium levels has been well validated; I think we measured it as accurately as we could have done,” he added.
Results showed that between baseline and 12 months, the median sodium intake decreased from 2,286 mg/day to 1,658 mg/day in the low-sodium group and from 2,119 mg/day to 2,073 mg/day in the usual care group. The median difference between groups was 415 mg/day at 12 months.
By 12 months, events comprising the primary outcome (hospitalization or emergency department visits due to cardiovascular causes or all-cause death) had occurred in 15% of patients in the low-sodium diet group and 17% of those in the usual care group (hazard ratio [HR], 0.89 [95% CI, 0.63 - 1.26]; P = .53).
All-cause death occurred in 6% of patients in the low-sodium diet group and 4% of those in the usual care group (HR, 1.38; P = .32). Cardiovascular-related hospitalization occurred in 10% of the low-sodium group and 12% of the usual care group (HR, 0.82; P = .36), and cardiovascular-related emergency department visits occurred in 4% of both groups (HR, 1.21; P = .60).
The absence of treatment effect for the primary outcome was consistent across most prespecified subgroups, including those with higher vs lower baseline sodium intake. But there was a suggestion of a greater reduction in the primary outcome in individuals younger than age 65 years than in those age 65 years and older.
Quality-of-life measures on the Kansas City Cardiomyopathy Questionnaire (KCCQ) suggested a benefit in the low-sodium group, with mean between-group differences in the change from baseline to 12 months of 3.38 points in the overall summary score, 3.29 points in the clinical summary score, and 3.77 points in the physical limitation score (all differences were statistically significant).
There was no significant difference in 6-minute-walk distance at 12 months between the low-sodium diet group and the usual care group.
NYHA functional class at 12 months differed significantly between groups; the low-sodium diet group had a greater likelihood of improving by one NYHA class than the usual care group (odds ratio, 0.59; P = .0061).
No safety events related to the study treatment were reported in either group.
Dr. Ezekowitz said that to investigate whether longer follow-up may show a difference in events, further analyses are planned at 2 years and 5 years.
Questions on food recall and blinding
Commenting on the findings at the late-breaking clinical trials session at the ACC meeting, Biykem Bozkurt, MD, professor of medicine at Baylor College of Medicine, Houston, congratulated Dr. Ezekowitz on conducting this trial.
“We have been chasing the holy grail of sodium reduction in heart failure for a very long time, so I have to commend you and your team for taking on this challenge, especially during the pandemic,” she said.
But Dr. Bozkurt questioned whether the intervention group actually had a meaningful sodium reduction given that this was measured by food recall and this may have been accounted for by under-reporting of certain food intakes.
Dr. Ezekowitz responded that patients acted as their own controls in that calorie intake, fluid intake, and weight were also assessed and did not change. “So I think we did have a meaningful reduction in sodium,” he said.
Dr. Bozkurt also queried whether the improvements in quality of life and functional status were reliable given that this was an unblinded study.
To this point, Dr. Ezekowitz pointed out that the KCCQ quality-of-life measure was a highly validated instrument and that improvements were seen in these measures at 3, 6, and 12 months. “It is not like these were spurious findings, so I think we have to look at this as a real result,” he argued.
Commenting on the study at an ACC press conference, Mary Norine Walsh, MD, director of the heart failure and cardiac transplantation programs at St. Vincent Heart Center in Indianapolis, said the trial had answered two important questions: that sodium reduction in heart failure may not reduce heart failure hospitalization/death but that patients feel better.
“I think we can safely tell patients that if they slip up a bit they may not end up in hospital,” she added.
This study was funded by the Canadian Institutes of Health Research and the University Hospital Foundation (Edmonton, Alberta, Canada) and the Health Research Council of New Zealand. Dr. Ezekowitz reports research grants from American Regent, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb/Pfizer, eko.ai, US2.ai, Merck, Novartis, Otsuka, Sanofi, and Servier and consulting fees from American Regent, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb/Pfizer, Merck, Novartis, Otsuka, Sanofi, and Servier.
A version of this article first appeared on Medscape.com.
A low-sodium diet was not associated with a reduction in future clinical events in a new study in ambulatory patients with heart failure. But there was a moderate benefit on quality of life and New York Heart Association (NYHA) functional class.
The results of the SODIUM-HF trial were presented April 2 at the annual scientific sessions of the American College of Cardiology, conducted virtually and in person in Washington. They were also simultaneously published online in the Lancet.
The study found that a strategy to reduce dietary sodium intake to less than 1,500 mg daily was not more effective than usual care in reducing the primary endpoint of risk for hospitalization or emergency department visits due to cardiovascular causes or all-cause death at 12 months.
“This is the largest and longest trial to look at the question of reducing dietary sodium in heart failure patients,” lead author Justin Ezekowitz, MBBCh, from the Canadian VIGOUR Center at the University of Alberta, Edmonton, Canada, told this news organization.
But he pointed out that there were fewer events than expected in the study, which was stopped early because of a combination of futility and practical difficulties caused by the COVID pandemic, so it could have been underpowered. Dr. Ezekowitz also suggested that a greater reduction in sodium than achieved in this study or a longer follow-up may be required to show an effect on clinical events.
“We hope others will do additional studies of sodium as well as other dietary recommendations as part of a comprehensive diet for heart failure patients,” he commented.
Dr. Ezekowitz said that the study results did not allow blanket recommendations to be made on reducing sodium intake in heart failure.
But he added: “I don’t think we should write off sodium reduction in this population. I think we can tell patients that reducing dietary sodium may potentially improve symptoms and quality of life, and I will continue to recommend reducing sodium as part of an overall healthy diet. We don’t want to throw the baby out with the bathwater.”
Dr. Ezekowitz noted that heart failure is associated with neurohormonal activation and abnormalities in autonomic control that lead to sodium and water retention; thus, dietary restriction of sodium has been historically endorsed as a mechanism to prevent fluid overload and subsequent clinical outcomes; however, clinical trials so far have shown mixed results.
“The guidelines used to strongly recommend a reduction in sodium intake in heart failure patients, but this advice has backed off in recent years because of the lack of data. Most heart failure guidelines now do not make any recommendations on dietary sodium,” he said.
SODIUM-HF was a pragmatic, multinational, open-label, randomized trial conducted in six countries (Australia, Canada, Chile, Colombia, Mexico, and New Zealand), which included 809 patients (median age, 67 years) with chronic heart failure (NYHA functional class II–III) who were receiving optimally tolerated guideline-directed medical treatment. They were randomly assigned to usual care according to local guidelines or a low-sodium diet of less than 100 mmol (<1,500 mg/day). Patients with a baseline sodium intake of less than 1,500 mg/day were excluded.
In the intervention group, patients were asked to follow low-sodium menus developed by dietitians localized to each region. They also received behavioral counseling by trained dietitians or physicians or nurses.
Dietary sodium intake was assessed by using a 3-day food record (including 1 weekend day) at baseline, 6 months, and 12 months in both groups and, for the intervention group, also at 3 and 9 months to monitor and support dietary adherence.
Dr. Ezekowitz explained that although the best method for measuring sodium levels would normally be a 24-hour urine sodium, this would be impractical in a large clinical trial. In addition, he pointed out that urinary sodium is not an accurate measure of actual sodium levels in patients taking diuretics, so it is not a good measure to use in a heart failure population.
“The food record method of assessing sodium levels has been well validated; I think we measured it as accurately as we could have done,” he added.
Results showed that between baseline and 12 months, the median sodium intake decreased from 2,286 mg/day to 1,658 mg/day in the low-sodium group and from 2,119 mg/day to 2,073 mg/day in the usual care group. The median difference between groups was 415 mg/day at 12 months.
By 12 months, events comprising the primary outcome (hospitalization or emergency department visits due to cardiovascular causes or all-cause death) had occurred in 15% of patients in the low-sodium diet group and 17% of those in the usual care group (hazard ratio [HR], 0.89 [95% CI, 0.63 - 1.26]; P = .53).
All-cause death occurred in 6% of patients in the low-sodium diet group and 4% of those in the usual care group (HR, 1.38; P = .32). Cardiovascular-related hospitalization occurred in 10% of the low-sodium group and 12% of the usual care group (HR, 0.82; P = .36), and cardiovascular-related emergency department visits occurred in 4% of both groups (HR, 1.21; P = .60).
The absence of treatment effect for the primary outcome was consistent across most prespecified subgroups, including those with higher vs lower baseline sodium intake. But there was a suggestion of a greater reduction in the primary outcome in individuals younger than age 65 years than in those age 65 years and older.
Quality-of-life measures on the Kansas City Cardiomyopathy Questionnaire (KCCQ) suggested a benefit in the low-sodium group, with mean between-group differences in the change from baseline to 12 months of 3.38 points in the overall summary score, 3.29 points in the clinical summary score, and 3.77 points in the physical limitation score (all differences were statistically significant).
There was no significant difference in 6-minute-walk distance at 12 months between the low-sodium diet group and the usual care group.
NYHA functional class at 12 months differed significantly between groups; the low-sodium diet group had a greater likelihood of improving by one NYHA class than the usual care group (odds ratio, 0.59; P = .0061).
No safety events related to the study treatment were reported in either group.
Dr. Ezekowitz said that to investigate whether longer follow-up may show a difference in events, further analyses are planned at 2 years and 5 years.
Questions on food recall and blinding
Commenting on the findings at the late-breaking clinical trials session at the ACC meeting, Biykem Bozkurt, MD, professor of medicine at Baylor College of Medicine, Houston, congratulated Dr. Ezekowitz on conducting this trial.
“We have been chasing the holy grail of sodium reduction in heart failure for a very long time, so I have to commend you and your team for taking on this challenge, especially during the pandemic,” she said.
But Dr. Bozkurt questioned whether the intervention group actually had a meaningful sodium reduction given that this was measured by food recall and this may have been accounted for by under-reporting of certain food intakes.
Dr. Ezekowitz responded that patients acted as their own controls in that calorie intake, fluid intake, and weight were also assessed and did not change. “So I think we did have a meaningful reduction in sodium,” he said.
Dr. Bozkurt also queried whether the improvements in quality of life and functional status were reliable given that this was an unblinded study.
To this point, Dr. Ezekowitz pointed out that the KCCQ quality-of-life measure was a highly validated instrument and that improvements were seen in these measures at 3, 6, and 12 months. “It is not like these were spurious findings, so I think we have to look at this as a real result,” he argued.
Commenting on the study at an ACC press conference, Mary Norine Walsh, MD, director of the heart failure and cardiac transplantation programs at St. Vincent Heart Center in Indianapolis, said the trial had answered two important questions: that sodium reduction in heart failure may not reduce heart failure hospitalization/death but that patients feel better.
“I think we can safely tell patients that if they slip up a bit they may not end up in hospital,” she added.
This study was funded by the Canadian Institutes of Health Research and the University Hospital Foundation (Edmonton, Alberta, Canada) and the Health Research Council of New Zealand. Dr. Ezekowitz reports research grants from American Regent, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb/Pfizer, eko.ai, US2.ai, Merck, Novartis, Otsuka, Sanofi, and Servier and consulting fees from American Regent, Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb/Pfizer, Merck, Novartis, Otsuka, Sanofi, and Servier.
A version of this article first appeared on Medscape.com.
FROM ACC 2022
Even light drinking ups CV risk; harm rises along with intake
Even very light alcohol intake is associated with an increased risk for cardiovascular disease, compared with not drinking at all, and the risk increases exponentially as alcohol intake rises, even at moderate levels, a new study shows.
“Our findings suggest that the observed benefit in individuals with light to moderate alcohol intake, which is consistently shown in epidemiological studies, is likely due to other positive lifestyle factors that are common in these individuals who drink lightly,” senior author Krishna Aragam, MD, Massachusetts General Hospital, Boston, told this news organization.
“Our results also showed that while all levels of alcohol were linked to increased risk of cardiovascular disease, the association was not linear. Rather, light alcohol intake was associated with rather modest risk increases, but there were exponential increases in cardiovascular risk with increasing amounts of alcohol consumption,” he said.
As the risk gradient appeared to increase quite sharply even between 1 and 2 drinks per day, Dr. Aragam suggested that what might be regarded as safe levels of drinking may trend downward in the future.
The study was published online March 25 in JAMA Network Open.
The cohort study used data from the UK Biobank, collected between 2006 and 2010 with follow-up until 2016, to assess the relationship between various levels of alcohol consumption and risk for cardiovascular disease.
Data were analyzed from 371,463 participants (mean age, 57 years; 46% men) who consumed an average of 9.2 standard drinks per week. Of these participants, 33% had hypertension and 7.5% had coronary artery disease.
“Use of the UK biobank database gives the advantage of a large, well-phenotyped population with a lot of information on various lifestyle factors that could be potential confounders,” Dr. Aragam noted.
Results showed that well-established J- or U-shaped curves were seen for the association between alcohol consumption and both the prevalence and hazards of hypertension, coronary artery disease, myocardial infarction, stroke, heart failure, and atrial fibrillation.
However, individuals in the light and moderate consumption group had healthier lifestyle behaviors than abstainers, self-reporting better overall health and exhibiting lower rates of smoking, lower body mass index, higher physical activity, and higher vegetable intake.
Adjustment for these lifestyle factors attenuated the cardioprotective associations with modest alcohol intake. For example, in baseline models, moderate intake was associated with significantly lower risk of hypertension and coronary artery disease, but adjustment for just six lifestyle factors rendered these results insignificant.
“Adjustments for yet unmeasured or unknown factors may further attenuate, if not eliminate, the residual, cardioprotective associations observed among light drinkers,” the researchers suggest.
They also conducted genetic analyses to examine the effect of alcohol and cardiovascular disease.
Dr. Aragam explained that previous work has shown good evidence, in individuals who choose to drink, that several relevant genetic variants predict levels of alcohol consumption quite accurately.
“Mendelian randomization using these gene variants allows for stronger inferences about potential causality than do observational studies, as they are less affected by confounding factors,” he noted.
Newer techniques in Mendelian randomization in which data on several gene variants linked to alcohol consumption are combined into a score allow for a greater understanding of the risk linked to different amount of alcohol intake, he added.
In these Mendelian randomization analyses, a 1-standard deviation increase in genetically predicted alcohol consumption was associated with 1.3-fold higher risk of hypertension (P < .001) and 1.4-fold higher risk of coronary artery disease (P = .006).
Further analyses suggested nonlinear associations between alcohol consumption and both hypertension and coronary artery disease; light alcohol intake was associated with minimal increases in cardiovascular risk, whereas heavier consumption was associated with exponential increases in risk of both clinical and subclinical cardiovascular disease.
These results were replicated in a second database of 30,716 individuals from the Mass General Brigham Biobank.
“The findings of this study suggest that the observed cardioprotective effects of light to moderate alcohol intake may be largely mediated by confounding lifestyle factors,” the researchers conclude. “Genetic analyses suggest causal associations between alcohol intake and cardiovascular disease but with unequal and exponential increases in risk at greater levels of intake, which should be accounted for in health recommendations around the habitual consumption of alcohol.”
What is an acceptable level?
“Specifically, our results suggest that consuming as many as 7 drinks per week is associated with relatively modest increases in cardiovascular risk,” they write.
But they point out that there are unequal increases in cardiovascular risk when progressing from 0 to 7 versus 7 to 14 drinks per week in both men and women.
“Although risk thresholds are inherently somewhat subjective, these findings again bring into question whether an average consumption of 2 drinks per day (14 drinks per week) should be designated a low-risk behavior,” they say.
“Furthermore, as several-fold increases in risk were observed for those consuming 21 or more drinks per week, our results emphasize the importance of aggressive efforts to reduce alcohol intake among heavy drinkers,” they add.
Dr. Aragam elaborated: “Our data suggest that reducing alcohol intake will reduce cardiovascular risk in all individuals, but the extent of the relative risk reduction is quite different depending on the current levels of consumption. For the same absolute reduction in alcohol intake, the gains in terms of reduction in cardiovascular risk will be more pronounced in those who drink heavily and will be more modest in those who drink at a light level.”
The results also suggest that while all levels of alcohol intake increase cardiovascular risk, there are low levels of alcohol consumption that do not carry major elevations in risk, but these are probably lower than those currently recommended, Dr. Aragam pointed out.
“This doesn’t mean that everyone has to give up drinking alcohol completely, just that you shouldn’t consume with the goal of improving cardiovascular health. In fact, our analyses suggest that in an otherwise healthy person, up to 1 drink per day may not pose outsized risks,” he said. “And, even in a less healthy person who might be smoking, eating poorly, and drinking up to 1 drink per day, it may be a higher priority to focus on smoking cessation and diet than cutting back further on alcohol.”
“Beyond that amount, though, the jury is still out. Our models suggested marked increases in risk even between 1 and 2 drinks per day, and of course even greater risk increases beyond that. So, it’s probably worth revisiting what one might consider a ‘safe’ amount within the moderate drinking categories. The conservative move for now might be to advise a limit of 1 drink per day,” he said.
Dr. Aragam is supported by grants from the National Institutes of Health and the American Heart Association. He reports receiving speaking fees from the Novartis Institute for Biomedical Research.
A version of this article first appeared on Medscape.com.
Even very light alcohol intake is associated with an increased risk for cardiovascular disease, compared with not drinking at all, and the risk increases exponentially as alcohol intake rises, even at moderate levels, a new study shows.
“Our findings suggest that the observed benefit in individuals with light to moderate alcohol intake, which is consistently shown in epidemiological studies, is likely due to other positive lifestyle factors that are common in these individuals who drink lightly,” senior author Krishna Aragam, MD, Massachusetts General Hospital, Boston, told this news organization.
“Our results also showed that while all levels of alcohol were linked to increased risk of cardiovascular disease, the association was not linear. Rather, light alcohol intake was associated with rather modest risk increases, but there were exponential increases in cardiovascular risk with increasing amounts of alcohol consumption,” he said.
As the risk gradient appeared to increase quite sharply even between 1 and 2 drinks per day, Dr. Aragam suggested that what might be regarded as safe levels of drinking may trend downward in the future.
The study was published online March 25 in JAMA Network Open.
The cohort study used data from the UK Biobank, collected between 2006 and 2010 with follow-up until 2016, to assess the relationship between various levels of alcohol consumption and risk for cardiovascular disease.
Data were analyzed from 371,463 participants (mean age, 57 years; 46% men) who consumed an average of 9.2 standard drinks per week. Of these participants, 33% had hypertension and 7.5% had coronary artery disease.
“Use of the UK biobank database gives the advantage of a large, well-phenotyped population with a lot of information on various lifestyle factors that could be potential confounders,” Dr. Aragam noted.
Results showed that well-established J- or U-shaped curves were seen for the association between alcohol consumption and both the prevalence and hazards of hypertension, coronary artery disease, myocardial infarction, stroke, heart failure, and atrial fibrillation.
However, individuals in the light and moderate consumption group had healthier lifestyle behaviors than abstainers, self-reporting better overall health and exhibiting lower rates of smoking, lower body mass index, higher physical activity, and higher vegetable intake.
Adjustment for these lifestyle factors attenuated the cardioprotective associations with modest alcohol intake. For example, in baseline models, moderate intake was associated with significantly lower risk of hypertension and coronary artery disease, but adjustment for just six lifestyle factors rendered these results insignificant.
“Adjustments for yet unmeasured or unknown factors may further attenuate, if not eliminate, the residual, cardioprotective associations observed among light drinkers,” the researchers suggest.
They also conducted genetic analyses to examine the effect of alcohol and cardiovascular disease.
Dr. Aragam explained that previous work has shown good evidence, in individuals who choose to drink, that several relevant genetic variants predict levels of alcohol consumption quite accurately.
“Mendelian randomization using these gene variants allows for stronger inferences about potential causality than do observational studies, as they are less affected by confounding factors,” he noted.
Newer techniques in Mendelian randomization in which data on several gene variants linked to alcohol consumption are combined into a score allow for a greater understanding of the risk linked to different amount of alcohol intake, he added.
In these Mendelian randomization analyses, a 1-standard deviation increase in genetically predicted alcohol consumption was associated with 1.3-fold higher risk of hypertension (P < .001) and 1.4-fold higher risk of coronary artery disease (P = .006).
Further analyses suggested nonlinear associations between alcohol consumption and both hypertension and coronary artery disease; light alcohol intake was associated with minimal increases in cardiovascular risk, whereas heavier consumption was associated with exponential increases in risk of both clinical and subclinical cardiovascular disease.
These results were replicated in a second database of 30,716 individuals from the Mass General Brigham Biobank.
“The findings of this study suggest that the observed cardioprotective effects of light to moderate alcohol intake may be largely mediated by confounding lifestyle factors,” the researchers conclude. “Genetic analyses suggest causal associations between alcohol intake and cardiovascular disease but with unequal and exponential increases in risk at greater levels of intake, which should be accounted for in health recommendations around the habitual consumption of alcohol.”
What is an acceptable level?
“Specifically, our results suggest that consuming as many as 7 drinks per week is associated with relatively modest increases in cardiovascular risk,” they write.
But they point out that there are unequal increases in cardiovascular risk when progressing from 0 to 7 versus 7 to 14 drinks per week in both men and women.
“Although risk thresholds are inherently somewhat subjective, these findings again bring into question whether an average consumption of 2 drinks per day (14 drinks per week) should be designated a low-risk behavior,” they say.
“Furthermore, as several-fold increases in risk were observed for those consuming 21 or more drinks per week, our results emphasize the importance of aggressive efforts to reduce alcohol intake among heavy drinkers,” they add.
Dr. Aragam elaborated: “Our data suggest that reducing alcohol intake will reduce cardiovascular risk in all individuals, but the extent of the relative risk reduction is quite different depending on the current levels of consumption. For the same absolute reduction in alcohol intake, the gains in terms of reduction in cardiovascular risk will be more pronounced in those who drink heavily and will be more modest in those who drink at a light level.”
The results also suggest that while all levels of alcohol intake increase cardiovascular risk, there are low levels of alcohol consumption that do not carry major elevations in risk, but these are probably lower than those currently recommended, Dr. Aragam pointed out.
“This doesn’t mean that everyone has to give up drinking alcohol completely, just that you shouldn’t consume with the goal of improving cardiovascular health. In fact, our analyses suggest that in an otherwise healthy person, up to 1 drink per day may not pose outsized risks,” he said. “And, even in a less healthy person who might be smoking, eating poorly, and drinking up to 1 drink per day, it may be a higher priority to focus on smoking cessation and diet than cutting back further on alcohol.”
“Beyond that amount, though, the jury is still out. Our models suggested marked increases in risk even between 1 and 2 drinks per day, and of course even greater risk increases beyond that. So, it’s probably worth revisiting what one might consider a ‘safe’ amount within the moderate drinking categories. The conservative move for now might be to advise a limit of 1 drink per day,” he said.
Dr. Aragam is supported by grants from the National Institutes of Health and the American Heart Association. He reports receiving speaking fees from the Novartis Institute for Biomedical Research.
A version of this article first appeared on Medscape.com.
Even very light alcohol intake is associated with an increased risk for cardiovascular disease, compared with not drinking at all, and the risk increases exponentially as alcohol intake rises, even at moderate levels, a new study shows.
“Our findings suggest that the observed benefit in individuals with light to moderate alcohol intake, which is consistently shown in epidemiological studies, is likely due to other positive lifestyle factors that are common in these individuals who drink lightly,” senior author Krishna Aragam, MD, Massachusetts General Hospital, Boston, told this news organization.
“Our results also showed that while all levels of alcohol were linked to increased risk of cardiovascular disease, the association was not linear. Rather, light alcohol intake was associated with rather modest risk increases, but there were exponential increases in cardiovascular risk with increasing amounts of alcohol consumption,” he said.
As the risk gradient appeared to increase quite sharply even between 1 and 2 drinks per day, Dr. Aragam suggested that what might be regarded as safe levels of drinking may trend downward in the future.
The study was published online March 25 in JAMA Network Open.
The cohort study used data from the UK Biobank, collected between 2006 and 2010 with follow-up until 2016, to assess the relationship between various levels of alcohol consumption and risk for cardiovascular disease.
Data were analyzed from 371,463 participants (mean age, 57 years; 46% men) who consumed an average of 9.2 standard drinks per week. Of these participants, 33% had hypertension and 7.5% had coronary artery disease.
“Use of the UK biobank database gives the advantage of a large, well-phenotyped population with a lot of information on various lifestyle factors that could be potential confounders,” Dr. Aragam noted.
Results showed that well-established J- or U-shaped curves were seen for the association between alcohol consumption and both the prevalence and hazards of hypertension, coronary artery disease, myocardial infarction, stroke, heart failure, and atrial fibrillation.
However, individuals in the light and moderate consumption group had healthier lifestyle behaviors than abstainers, self-reporting better overall health and exhibiting lower rates of smoking, lower body mass index, higher physical activity, and higher vegetable intake.
Adjustment for these lifestyle factors attenuated the cardioprotective associations with modest alcohol intake. For example, in baseline models, moderate intake was associated with significantly lower risk of hypertension and coronary artery disease, but adjustment for just six lifestyle factors rendered these results insignificant.
“Adjustments for yet unmeasured or unknown factors may further attenuate, if not eliminate, the residual, cardioprotective associations observed among light drinkers,” the researchers suggest.
They also conducted genetic analyses to examine the effect of alcohol and cardiovascular disease.
Dr. Aragam explained that previous work has shown good evidence, in individuals who choose to drink, that several relevant genetic variants predict levels of alcohol consumption quite accurately.
“Mendelian randomization using these gene variants allows for stronger inferences about potential causality than do observational studies, as they are less affected by confounding factors,” he noted.
Newer techniques in Mendelian randomization in which data on several gene variants linked to alcohol consumption are combined into a score allow for a greater understanding of the risk linked to different amount of alcohol intake, he added.
In these Mendelian randomization analyses, a 1-standard deviation increase in genetically predicted alcohol consumption was associated with 1.3-fold higher risk of hypertension (P < .001) and 1.4-fold higher risk of coronary artery disease (P = .006).
Further analyses suggested nonlinear associations between alcohol consumption and both hypertension and coronary artery disease; light alcohol intake was associated with minimal increases in cardiovascular risk, whereas heavier consumption was associated with exponential increases in risk of both clinical and subclinical cardiovascular disease.
These results were replicated in a second database of 30,716 individuals from the Mass General Brigham Biobank.
“The findings of this study suggest that the observed cardioprotective effects of light to moderate alcohol intake may be largely mediated by confounding lifestyle factors,” the researchers conclude. “Genetic analyses suggest causal associations between alcohol intake and cardiovascular disease but with unequal and exponential increases in risk at greater levels of intake, which should be accounted for in health recommendations around the habitual consumption of alcohol.”
What is an acceptable level?
“Specifically, our results suggest that consuming as many as 7 drinks per week is associated with relatively modest increases in cardiovascular risk,” they write.
But they point out that there are unequal increases in cardiovascular risk when progressing from 0 to 7 versus 7 to 14 drinks per week in both men and women.
“Although risk thresholds are inherently somewhat subjective, these findings again bring into question whether an average consumption of 2 drinks per day (14 drinks per week) should be designated a low-risk behavior,” they say.
“Furthermore, as several-fold increases in risk were observed for those consuming 21 or more drinks per week, our results emphasize the importance of aggressive efforts to reduce alcohol intake among heavy drinkers,” they add.
Dr. Aragam elaborated: “Our data suggest that reducing alcohol intake will reduce cardiovascular risk in all individuals, but the extent of the relative risk reduction is quite different depending on the current levels of consumption. For the same absolute reduction in alcohol intake, the gains in terms of reduction in cardiovascular risk will be more pronounced in those who drink heavily and will be more modest in those who drink at a light level.”
The results also suggest that while all levels of alcohol intake increase cardiovascular risk, there are low levels of alcohol consumption that do not carry major elevations in risk, but these are probably lower than those currently recommended, Dr. Aragam pointed out.
“This doesn’t mean that everyone has to give up drinking alcohol completely, just that you shouldn’t consume with the goal of improving cardiovascular health. In fact, our analyses suggest that in an otherwise healthy person, up to 1 drink per day may not pose outsized risks,” he said. “And, even in a less healthy person who might be smoking, eating poorly, and drinking up to 1 drink per day, it may be a higher priority to focus on smoking cessation and diet than cutting back further on alcohol.”
“Beyond that amount, though, the jury is still out. Our models suggested marked increases in risk even between 1 and 2 drinks per day, and of course even greater risk increases beyond that. So, it’s probably worth revisiting what one might consider a ‘safe’ amount within the moderate drinking categories. The conservative move for now might be to advise a limit of 1 drink per day,” he said.
Dr. Aragam is supported by grants from the National Institutes of Health and the American Heart Association. He reports receiving speaking fees from the Novartis Institute for Biomedical Research.
A version of this article first appeared on Medscape.com.
Hybrid ACC 2022 resurrects the live scientific session
Regardless of the pandemic’s sometimes mercurial behavior, the cardiology community appears set to reclaim valued traditions perhaps taken for granted in the pre-COVID era.
They include the bustling scientific congress and its myriad educational and networking prospects, along with pleiotropic effects like unplanned reunions with colleagues and catching up face-to-face with old friends.
That seems evident in the growing number of registrants for live attendance at at the annual scientific sessions of the American College of Cardiology, set for this Saturday through Monday in Washington as well as virtually, for a global reach that was unattainable in the pre-COVID era.
Registrations had hit the 11,000 mark and were picking up speed in recent weeks, ACC 2022 cochair Pamela B. Morris, MD, Medical University of South Carolina, Charleston, said at a mid-March presentation to the media.
They had reached about 12,880 and were still climbing a week before the conference, the ACC confirmed to this news organization. By then the professional registration had surpassed 9,900, of whom more than two-thirds reported plans to attend in person.
Dr. Morris said there had been 117 international submissions for what turned out to be 39 coveted spots on the meeting’s Late-Breaking Clinical Trial (LBCT) and Featured Clinical Research agenda spread across eight separate sessions.
On-site participants at the Walter E. Washington Convention Center should head for the Main Tent in Hall D for all LBCT presentations; venues for the Featured Clinical Research sessions are as noted below. Their real-time virtual equivalents will reside on the online platform’s Hot Topics channel. All noted session times are Eastern Daylight Time.
Saturday, April 2, 9:30 a.m.–10:30 a.m. Joint American College of Cardiology/Journal of the American College of Cardiology LBCT (I)
Leading off the conference’s first LBCT session, the randomized VALOR-HCM trial explored whether 16 weeks of mavacamten (MyoKardia) could help patients with severe obstructive hypertrophic cardiomyopathy (HCM) avoid septal reduction therapy, either surgical or by alcohol ablation.
The 22-center VALOR-HCM trial with an estimated enrollment of 100 follows EXPLORER-HCM, which in 2020 suggested the novel myosin-inhibiting agent could improve symptoms, exercise capacity, cardiac remodeling, and quality of life in such patients.
Simply advising people with heart failure (HF) to consume less salt is one thing, but it’s another to show them clinical trial evidence that it might help keep them out of the hospital. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure) study, conducted at 27 sites in six countries, sought to provide that evidence.
The trial randomly assigned 1,000 patients with NYHA class 2-3 HF to consume no more than 1,500 mg/day in sodium or to receive standard advice to limit sodium intake, and followed them for a year for the endpoint of death from any cause, cardiovascular (CV) hospitalization, or CV emergency department visit.
SODIUM-HF “may provide a rigorous evidence base for sodium restriction in patients with heart failure and may truly change our practice and how we recommend dietary modification,” ACC 2022 vice chair Douglas E. Drachman, MD, Massachusetts General Hospital, Boston, said at the media presentation.
In the same session, the CHAP (Chronic Hypertension and Pregnancy) study explored whether blood pressure (BP) control in pregnant women with new or untreated chronic hypertension could help avert preeclampsia, poor fetal outcomes, and other adverse events.
CHAP assigned about 2,400 women to receive either stepwise antihypertensive therapy to a BP goal of 140/90 mm Hg or lower or no such meds unless their BP reached or exceeded 160/105 mm Hg. Stepwise therapy featured either labetalol or extended-release nifedipine to start, the other agent added as necessary.
The LBCT block also includes the POISE-3 (Perioperative Ischemic Evaluation-3) comparison of the hemostatic agent tranexamic acid vs. placebo in nearly 10,000 patients undergoing noncardiac surgery. A separate randomization of the same cohort, to be reported at a Monday LBCT session, compared pre- and perioperative BP-control strategies.
Saturday, April 2, 12:00 p.m.–1:15 p.m. Featured Clinical Research I. Room 143A
This session features a subgroup analysis by age from the REVERSE-IT trial, which had previously showcased the monoclonal antibody bentracimab (PhaseBio Pharmaceuticals) for its ability to reverse the antiplatelet effects of ticagrelor.
REVERSE-IT is accompanied on the schedule by several secondary-endpoint presentations from trials whose primary outcomes have already been presented at meetings or in the journals.
They include the SCORED trial of sotagliflozin in patients with diabetes and chronic kidney disease (CKD); COMPLETE, which explored complete revascularization of multivessel coronary disease at primary stenting; and the FAME-3 comparison of coronary bypass surgery (CABG) vs. percutaneous coronary intervention (PCI) guided by fractional flow reserve (FFR) readings.
The session is to conclude with EDIT-CMD, which was a small, randomized assessment of diltiazem for improving microvascular dysfunction in patients with chronic angina despite nonobstructive coronary disease.
Sunday, April 3, 8:00 a.m.–9:15 a.m. Joint American College of Cardiology/Journal of the American Medical Association LBCT (II)
The SuperWIN (Supermarket Web Intervention) study tested an innovative strategy for community-based promotion of healthy lifestyle choices: point-of-purchase dietary education for grocery shoppers with an online instructional component, and follow-up to determine whether it influenced future food choices.
“Dietary interventions are notoriously difficult for us to implement, let alone to study scientifically,” Dr. Drachman observed. “So we think that there may be opportunity for dietary interventions to be best implemented at grocery stores where people are doing their shopping for food.”
SuperWIN compared supermarket shoppers with at least one CV risk factor who participated in the education intervention to a nonintervention control group for any changes in their DASH scores. The scores reflected consistency with the venerable DASH diet based on participants’ food purchases over 3 months.
In the same session, the MITIGATE trial explored whether daily administration of icosapent ethyl (Vascepa) might cut the risk of upper respiratory infection (especially from SARS-CoV-2 or seasonal influenza virus) in persons 50 or older with a history of clinical coronary, neurovascular, or peripheral vascular disease or revascularization. The trial has an estimated enrollment of 39,600.
Accompanying SuperWIN and MITIGATE are studies of several dyslipidemia drugs, including the discontinued antisense agent vupanorsen (Pfizer), as tested in TRANSLATE-TIMI 70; the PCSK9 inhibitor alirocumab (Praluent), explored for its effects on coronary plaque volume and composition in the PACMAN-AMI trial; and the APOLLO trial, a phase 1 evaluation of SLN360 (Silence Therapeutics), a short interfering ribonucleic acid (siRNA) that suppresses the molecular machinery in the liver that produces lipoprotein(a), or Lp(a).
The 32-patient APOLLO trial’s recently released top-line results suggested that SLN360 at varying dosages reduced Lp(a) levels by about one-half to more than 90%. Although elevated Lp(a) is known to track with CV risk, it remains to be shown whether dropping Lp(a) levels pharmacologically is protective.
Sunday, April 3, 9:45 a.m.–11:00 a.m. Joint American College of Cardiology/New England Journal of Medicine LBCT (III)
The meeting’s all-HF late-breaker session includes the METEORIC-HF trial, which compared the myotropic agent omecamtiv mecarbil (Cytokinetics) against placebo for effects on exercise performance over 20 weeks. The trial entered 276 patients with HF with reduced ejection fraction (HFrEF) and reduced peak VO2.
The GALACTIC-HF trial had previously suggested that the drug improved the risk of HF-related events or CV death in more than 8000 patients with HFrEF, those with the lowest ejection fractions benefiting the most.
This block of trials also features DIAMOND, the latest trial with a gemologic name to look at the potassium sequestrant patiromer (Veltassa) for any protection against hyperkalemia, a familiar side effect of renin-angiotensin-aldosterone inhibitors. DIAMOND tested patiromer in 878 patients with HFrEF who were on beta-blockers and other HF-appropriate medications and had a history of drug-associated hyperkalemia.
Previously, the AMBER trial of patients with CKD or refractory hypertension on spironolactone had suggested the drug might be protective enough against hyperkalemia to allow higher and more consistent dosing of BP-lowering agents.
Also in the session: the randomized IVVE (Influenza Vaccine to Prevent Adverse Vascular Events) trial, with an estimated 5,000 patients with HF in Africa, Asia, and the Middle East; PROMPT-HF, with a projected 1,310 HF patients and billed as a cluster-randomized pragmatic trial of a strategy for improving guideline-directed outpatient medical therapy; and MAVA-LTE, the long-term extension study of an estimated 310 patients who were in the MAVERICK-HCM and EXPLORER-HCM mavacamten trials.
Sunday, April 3, 12:15–1:30 p.m. Featured Clinical Research II. Main Tent, Hall D
The arrhythmia-centric session includes PARTITA, with its estimated 590 patients with primary- or secondary-prevention implantable cardioverter-defibrillators (ICDs). The trial followed them initially for burden of untreated nonsustained ventricular tachycardia (VT) or events treated with anti-tachycardia pacing. Then it randomly assigned those who experienced a first appropriate ICD shock to either immediate VT ablation or standard care. The latter included ablation on next occurrence of arrhythmic storm.
Investigational oral factor XIa inhibitors, viewed by many as potentially safer as anticoagulants than contemporary oral inhibitors of factor Xa, are now on the scene and include milvexian (Bristol-Myers Squibb/Janssen) and, lately, asundexian (BAY 2433334; Bayer). The latter agent was compared to the factor Xa inhibitor apixaban (Eliquis) in 753 patients with AF in the phase 2 PACIFIC-AF trial, which looked at the newer drug’s safety and optimal dosing.
Also on the bill: a long-term follow-up of the mAFA-2 (Mobile AF Application 2) extension study, which explored the value of a smartphone-based atrial fibrillation (AF) screening app for improving risk of AF-related events; a presentation billed as “Residual Leaks Post Left Atrial Appendage Occlusion”; and one that declares “low rates of guideline-directed care” to be “associated with higher mortality” in patients with pacemakers or ICDs.
Monday, April 4, 8:30 a.m.–9:45 a.m. LBCT IV
This session is to open with the PROTECT trial, which sought to determine whether perioperative “aggressive warming” may be cardioprotective in patients with CV risk factors undergoing noncardiac surgery. Its estimated 5,100 patients were randomly assigned to a procedure that achieves normothermia, that is 37° C (98.6° F), vs. standard care in which patients’ core temperature may decline to no further than 35.5° C (95.9° F).
Next on the list are a second POISE-3 comparison of BP-control strategies comparing hypotension avoidance vs. hypertension avoidance in patients undergoing noncardiac surgery; the pivotal CLASP 2 TR trial of patients with symptomatic tricuspid regurgitation on optimal medical therapy with vs. without treatment with the Edwards PASCAL Transcatheter Repair System; and one said to provide “insights from the Corevalve US Pivotal and SURTAVI trials” on 5-year incidence, timing, and predictors of hemodynamic valve deterioration transcatheter and surgical aortic bioprostheses.”
Rounding out the block of presentations: the ADAPT-TAVR comparison of the factor Xa inhibitor edoxaban (Lixiana) to dual-antiplatelet therapy for prevention of leaflet thrombosis after successful transcatheter aortic valve replacement (TAVR). The 235-patient trial was conducted at five centers in South Korea, Hong Kong, and Taiwan.
Monday, April 4, 11:00–12:15 p.m. LBCT V
This session includes the FLAVOUR randomized comparison of PCI guided by either FFR or intravascular ultrasound (IVUS) in 1,700 patients with 40%-70% stenoses. The patients from centers in China and South Korea were followed for death from any cause, MI, or any repeat revascularization at 24 months.
Also scheduled: the 2-year report on 4,000 patients with ST-segment elevation MI (STEMI) in the ACC-sponsored quality improvement program GHATI (Global Heart Attack Treatment Initiative); the GIPS-4 myocardial protection study of an estimated 380 patients with STEMI assigned to receive pre- and post-PCI infusions of sodium thiosulfate or placebo, with infarct size at 4 months as the primary endpoint; and a randomized test of an arrhythmia-monitoring implant for influence on clinical outcomes in 802 patients with a history of MI but no pacemaker or ICD indication, called BIO-GUARD-MI,
Last in the session: the Chocolate Touch Study of peripheral-artery angioplasty using a drug-coated balloon (DCB) with a confectionery name that treats lesions not with theobromine, but the antiproliferative mainstay paclitaxel.
The randomized comparison of the Chocolate Touch DCB (TriReme Medical) and the more established Lutonix DCB (Bard) assigned a projected 585 patients with symptomatic peripheral vascular disease to treatment of superficial femoral or popliteal artery lesions with one of the two paclitaxel-coated balloon catheters.
Monday, April 4, 12:45–2 p.m. Featured Clinical Research III. Room 143A
The final session features five subgroup analyses or other updates from trials that have already reported their primary outcomes. Among them is the SPYRAL HTN-ON MED trial, which helped to revitalize hopes for renal denervation therapy as a catheter-based treatment for drug-resistant hypertension by showing significant effects on both systolic and diastolic blood pressure. The new data follow the trial’s more than 400 patients out to 3 years.
There is also a symptom and quality-of-life analysis from the 530-patient EMPULSE trial of 530 patients with stabilized acute HF assigned in-hospital to start on empagliflozin (Jardiance) or placebo. The trial made a splash last year when it reported a significant improvement in risk for death or HF rehospitalization for its patients put on the SGLT2 inhibitor.
A secondary analysis from CANTOS is also featured; the trial had randomly assigned more than 10,000 patients with recent acute MI and elevated C-reactive protein (CRP) levels to receive or not receive the anti-inflammatory canakinumab (Ilaris). Those assigned to active therapy showed benefits for a range of outcomes, including CV mortality and stroke, but no decreases in cholesterol levels. Billing for the new CANTOS analysis promises insights on the “differential impact of residual inflammatory risk and residual cholesterol risk among atherosclerosis patients with and without chronic kidney disease.”
The session also features “trends and final results” from the NACMI (North American COVID-19 Myocardial Infarction) registry, which had shown excellent primary-PCI results without compromise of door-to-balloon times in patients with confirmed SARS-CoV-2 infection; and a FIDELITY analysis of cardiorenal endpoints by history of CV disease in the study’s more than 13,000 patients with diabetes and CKD assigned to placebo or finerenone (Kerendia), a mineralocorticoid receptor antagonist.
A version of this article first appeared on Medscape.com.
Regardless of the pandemic’s sometimes mercurial behavior, the cardiology community appears set to reclaim valued traditions perhaps taken for granted in the pre-COVID era.
They include the bustling scientific congress and its myriad educational and networking prospects, along with pleiotropic effects like unplanned reunions with colleagues and catching up face-to-face with old friends.
That seems evident in the growing number of registrants for live attendance at at the annual scientific sessions of the American College of Cardiology, set for this Saturday through Monday in Washington as well as virtually, for a global reach that was unattainable in the pre-COVID era.
Registrations had hit the 11,000 mark and were picking up speed in recent weeks, ACC 2022 cochair Pamela B. Morris, MD, Medical University of South Carolina, Charleston, said at a mid-March presentation to the media.
They had reached about 12,880 and were still climbing a week before the conference, the ACC confirmed to this news organization. By then the professional registration had surpassed 9,900, of whom more than two-thirds reported plans to attend in person.
Dr. Morris said there had been 117 international submissions for what turned out to be 39 coveted spots on the meeting’s Late-Breaking Clinical Trial (LBCT) and Featured Clinical Research agenda spread across eight separate sessions.
On-site participants at the Walter E. Washington Convention Center should head for the Main Tent in Hall D for all LBCT presentations; venues for the Featured Clinical Research sessions are as noted below. Their real-time virtual equivalents will reside on the online platform’s Hot Topics channel. All noted session times are Eastern Daylight Time.
Saturday, April 2, 9:30 a.m.–10:30 a.m. Joint American College of Cardiology/Journal of the American College of Cardiology LBCT (I)
Leading off the conference’s first LBCT session, the randomized VALOR-HCM trial explored whether 16 weeks of mavacamten (MyoKardia) could help patients with severe obstructive hypertrophic cardiomyopathy (HCM) avoid septal reduction therapy, either surgical or by alcohol ablation.
The 22-center VALOR-HCM trial with an estimated enrollment of 100 follows EXPLORER-HCM, which in 2020 suggested the novel myosin-inhibiting agent could improve symptoms, exercise capacity, cardiac remodeling, and quality of life in such patients.
Simply advising people with heart failure (HF) to consume less salt is one thing, but it’s another to show them clinical trial evidence that it might help keep them out of the hospital. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure) study, conducted at 27 sites in six countries, sought to provide that evidence.
The trial randomly assigned 1,000 patients with NYHA class 2-3 HF to consume no more than 1,500 mg/day in sodium or to receive standard advice to limit sodium intake, and followed them for a year for the endpoint of death from any cause, cardiovascular (CV) hospitalization, or CV emergency department visit.
SODIUM-HF “may provide a rigorous evidence base for sodium restriction in patients with heart failure and may truly change our practice and how we recommend dietary modification,” ACC 2022 vice chair Douglas E. Drachman, MD, Massachusetts General Hospital, Boston, said at the media presentation.
In the same session, the CHAP (Chronic Hypertension and Pregnancy) study explored whether blood pressure (BP) control in pregnant women with new or untreated chronic hypertension could help avert preeclampsia, poor fetal outcomes, and other adverse events.
CHAP assigned about 2,400 women to receive either stepwise antihypertensive therapy to a BP goal of 140/90 mm Hg or lower or no such meds unless their BP reached or exceeded 160/105 mm Hg. Stepwise therapy featured either labetalol or extended-release nifedipine to start, the other agent added as necessary.
The LBCT block also includes the POISE-3 (Perioperative Ischemic Evaluation-3) comparison of the hemostatic agent tranexamic acid vs. placebo in nearly 10,000 patients undergoing noncardiac surgery. A separate randomization of the same cohort, to be reported at a Monday LBCT session, compared pre- and perioperative BP-control strategies.
Saturday, April 2, 12:00 p.m.–1:15 p.m. Featured Clinical Research I. Room 143A
This session features a subgroup analysis by age from the REVERSE-IT trial, which had previously showcased the monoclonal antibody bentracimab (PhaseBio Pharmaceuticals) for its ability to reverse the antiplatelet effects of ticagrelor.
REVERSE-IT is accompanied on the schedule by several secondary-endpoint presentations from trials whose primary outcomes have already been presented at meetings or in the journals.
They include the SCORED trial of sotagliflozin in patients with diabetes and chronic kidney disease (CKD); COMPLETE, which explored complete revascularization of multivessel coronary disease at primary stenting; and the FAME-3 comparison of coronary bypass surgery (CABG) vs. percutaneous coronary intervention (PCI) guided by fractional flow reserve (FFR) readings.
The session is to conclude with EDIT-CMD, which was a small, randomized assessment of diltiazem for improving microvascular dysfunction in patients with chronic angina despite nonobstructive coronary disease.
Sunday, April 3, 8:00 a.m.–9:15 a.m. Joint American College of Cardiology/Journal of the American Medical Association LBCT (II)
The SuperWIN (Supermarket Web Intervention) study tested an innovative strategy for community-based promotion of healthy lifestyle choices: point-of-purchase dietary education for grocery shoppers with an online instructional component, and follow-up to determine whether it influenced future food choices.
“Dietary interventions are notoriously difficult for us to implement, let alone to study scientifically,” Dr. Drachman observed. “So we think that there may be opportunity for dietary interventions to be best implemented at grocery stores where people are doing their shopping for food.”
SuperWIN compared supermarket shoppers with at least one CV risk factor who participated in the education intervention to a nonintervention control group for any changes in their DASH scores. The scores reflected consistency with the venerable DASH diet based on participants’ food purchases over 3 months.
In the same session, the MITIGATE trial explored whether daily administration of icosapent ethyl (Vascepa) might cut the risk of upper respiratory infection (especially from SARS-CoV-2 or seasonal influenza virus) in persons 50 or older with a history of clinical coronary, neurovascular, or peripheral vascular disease or revascularization. The trial has an estimated enrollment of 39,600.
Accompanying SuperWIN and MITIGATE are studies of several dyslipidemia drugs, including the discontinued antisense agent vupanorsen (Pfizer), as tested in TRANSLATE-TIMI 70; the PCSK9 inhibitor alirocumab (Praluent), explored for its effects on coronary plaque volume and composition in the PACMAN-AMI trial; and the APOLLO trial, a phase 1 evaluation of SLN360 (Silence Therapeutics), a short interfering ribonucleic acid (siRNA) that suppresses the molecular machinery in the liver that produces lipoprotein(a), or Lp(a).
The 32-patient APOLLO trial’s recently released top-line results suggested that SLN360 at varying dosages reduced Lp(a) levels by about one-half to more than 90%. Although elevated Lp(a) is known to track with CV risk, it remains to be shown whether dropping Lp(a) levels pharmacologically is protective.
Sunday, April 3, 9:45 a.m.–11:00 a.m. Joint American College of Cardiology/New England Journal of Medicine LBCT (III)
The meeting’s all-HF late-breaker session includes the METEORIC-HF trial, which compared the myotropic agent omecamtiv mecarbil (Cytokinetics) against placebo for effects on exercise performance over 20 weeks. The trial entered 276 patients with HF with reduced ejection fraction (HFrEF) and reduced peak VO2.
The GALACTIC-HF trial had previously suggested that the drug improved the risk of HF-related events or CV death in more than 8000 patients with HFrEF, those with the lowest ejection fractions benefiting the most.
This block of trials also features DIAMOND, the latest trial with a gemologic name to look at the potassium sequestrant patiromer (Veltassa) for any protection against hyperkalemia, a familiar side effect of renin-angiotensin-aldosterone inhibitors. DIAMOND tested patiromer in 878 patients with HFrEF who were on beta-blockers and other HF-appropriate medications and had a history of drug-associated hyperkalemia.
Previously, the AMBER trial of patients with CKD or refractory hypertension on spironolactone had suggested the drug might be protective enough against hyperkalemia to allow higher and more consistent dosing of BP-lowering agents.
Also in the session: the randomized IVVE (Influenza Vaccine to Prevent Adverse Vascular Events) trial, with an estimated 5,000 patients with HF in Africa, Asia, and the Middle East; PROMPT-HF, with a projected 1,310 HF patients and billed as a cluster-randomized pragmatic trial of a strategy for improving guideline-directed outpatient medical therapy; and MAVA-LTE, the long-term extension study of an estimated 310 patients who were in the MAVERICK-HCM and EXPLORER-HCM mavacamten trials.
Sunday, April 3, 12:15–1:30 p.m. Featured Clinical Research II. Main Tent, Hall D
The arrhythmia-centric session includes PARTITA, with its estimated 590 patients with primary- or secondary-prevention implantable cardioverter-defibrillators (ICDs). The trial followed them initially for burden of untreated nonsustained ventricular tachycardia (VT) or events treated with anti-tachycardia pacing. Then it randomly assigned those who experienced a first appropriate ICD shock to either immediate VT ablation or standard care. The latter included ablation on next occurrence of arrhythmic storm.
Investigational oral factor XIa inhibitors, viewed by many as potentially safer as anticoagulants than contemporary oral inhibitors of factor Xa, are now on the scene and include milvexian (Bristol-Myers Squibb/Janssen) and, lately, asundexian (BAY 2433334; Bayer). The latter agent was compared to the factor Xa inhibitor apixaban (Eliquis) in 753 patients with AF in the phase 2 PACIFIC-AF trial, which looked at the newer drug’s safety and optimal dosing.
Also on the bill: a long-term follow-up of the mAFA-2 (Mobile AF Application 2) extension study, which explored the value of a smartphone-based atrial fibrillation (AF) screening app for improving risk of AF-related events; a presentation billed as “Residual Leaks Post Left Atrial Appendage Occlusion”; and one that declares “low rates of guideline-directed care” to be “associated with higher mortality” in patients with pacemakers or ICDs.
Monday, April 4, 8:30 a.m.–9:45 a.m. LBCT IV
This session is to open with the PROTECT trial, which sought to determine whether perioperative “aggressive warming” may be cardioprotective in patients with CV risk factors undergoing noncardiac surgery. Its estimated 5,100 patients were randomly assigned to a procedure that achieves normothermia, that is 37° C (98.6° F), vs. standard care in which patients’ core temperature may decline to no further than 35.5° C (95.9° F).
Next on the list are a second POISE-3 comparison of BP-control strategies comparing hypotension avoidance vs. hypertension avoidance in patients undergoing noncardiac surgery; the pivotal CLASP 2 TR trial of patients with symptomatic tricuspid regurgitation on optimal medical therapy with vs. without treatment with the Edwards PASCAL Transcatheter Repair System; and one said to provide “insights from the Corevalve US Pivotal and SURTAVI trials” on 5-year incidence, timing, and predictors of hemodynamic valve deterioration transcatheter and surgical aortic bioprostheses.”
Rounding out the block of presentations: the ADAPT-TAVR comparison of the factor Xa inhibitor edoxaban (Lixiana) to dual-antiplatelet therapy for prevention of leaflet thrombosis after successful transcatheter aortic valve replacement (TAVR). The 235-patient trial was conducted at five centers in South Korea, Hong Kong, and Taiwan.
Monday, April 4, 11:00–12:15 p.m. LBCT V
This session includes the FLAVOUR randomized comparison of PCI guided by either FFR or intravascular ultrasound (IVUS) in 1,700 patients with 40%-70% stenoses. The patients from centers in China and South Korea were followed for death from any cause, MI, or any repeat revascularization at 24 months.
Also scheduled: the 2-year report on 4,000 patients with ST-segment elevation MI (STEMI) in the ACC-sponsored quality improvement program GHATI (Global Heart Attack Treatment Initiative); the GIPS-4 myocardial protection study of an estimated 380 patients with STEMI assigned to receive pre- and post-PCI infusions of sodium thiosulfate or placebo, with infarct size at 4 months as the primary endpoint; and a randomized test of an arrhythmia-monitoring implant for influence on clinical outcomes in 802 patients with a history of MI but no pacemaker or ICD indication, called BIO-GUARD-MI,
Last in the session: the Chocolate Touch Study of peripheral-artery angioplasty using a drug-coated balloon (DCB) with a confectionery name that treats lesions not with theobromine, but the antiproliferative mainstay paclitaxel.
The randomized comparison of the Chocolate Touch DCB (TriReme Medical) and the more established Lutonix DCB (Bard) assigned a projected 585 patients with symptomatic peripheral vascular disease to treatment of superficial femoral or popliteal artery lesions with one of the two paclitaxel-coated balloon catheters.
Monday, April 4, 12:45–2 p.m. Featured Clinical Research III. Room 143A
The final session features five subgroup analyses or other updates from trials that have already reported their primary outcomes. Among them is the SPYRAL HTN-ON MED trial, which helped to revitalize hopes for renal denervation therapy as a catheter-based treatment for drug-resistant hypertension by showing significant effects on both systolic and diastolic blood pressure. The new data follow the trial’s more than 400 patients out to 3 years.
There is also a symptom and quality-of-life analysis from the 530-patient EMPULSE trial of 530 patients with stabilized acute HF assigned in-hospital to start on empagliflozin (Jardiance) or placebo. The trial made a splash last year when it reported a significant improvement in risk for death or HF rehospitalization for its patients put on the SGLT2 inhibitor.
A secondary analysis from CANTOS is also featured; the trial had randomly assigned more than 10,000 patients with recent acute MI and elevated C-reactive protein (CRP) levels to receive or not receive the anti-inflammatory canakinumab (Ilaris). Those assigned to active therapy showed benefits for a range of outcomes, including CV mortality and stroke, but no decreases in cholesterol levels. Billing for the new CANTOS analysis promises insights on the “differential impact of residual inflammatory risk and residual cholesterol risk among atherosclerosis patients with and without chronic kidney disease.”
The session also features “trends and final results” from the NACMI (North American COVID-19 Myocardial Infarction) registry, which had shown excellent primary-PCI results without compromise of door-to-balloon times in patients with confirmed SARS-CoV-2 infection; and a FIDELITY analysis of cardiorenal endpoints by history of CV disease in the study’s more than 13,000 patients with diabetes and CKD assigned to placebo or finerenone (Kerendia), a mineralocorticoid receptor antagonist.
A version of this article first appeared on Medscape.com.
Regardless of the pandemic’s sometimes mercurial behavior, the cardiology community appears set to reclaim valued traditions perhaps taken for granted in the pre-COVID era.
They include the bustling scientific congress and its myriad educational and networking prospects, along with pleiotropic effects like unplanned reunions with colleagues and catching up face-to-face with old friends.
That seems evident in the growing number of registrants for live attendance at at the annual scientific sessions of the American College of Cardiology, set for this Saturday through Monday in Washington as well as virtually, for a global reach that was unattainable in the pre-COVID era.
Registrations had hit the 11,000 mark and were picking up speed in recent weeks, ACC 2022 cochair Pamela B. Morris, MD, Medical University of South Carolina, Charleston, said at a mid-March presentation to the media.
They had reached about 12,880 and were still climbing a week before the conference, the ACC confirmed to this news organization. By then the professional registration had surpassed 9,900, of whom more than two-thirds reported plans to attend in person.
Dr. Morris said there had been 117 international submissions for what turned out to be 39 coveted spots on the meeting’s Late-Breaking Clinical Trial (LBCT) and Featured Clinical Research agenda spread across eight separate sessions.
On-site participants at the Walter E. Washington Convention Center should head for the Main Tent in Hall D for all LBCT presentations; venues for the Featured Clinical Research sessions are as noted below. Their real-time virtual equivalents will reside on the online platform’s Hot Topics channel. All noted session times are Eastern Daylight Time.
Saturday, April 2, 9:30 a.m.–10:30 a.m. Joint American College of Cardiology/Journal of the American College of Cardiology LBCT (I)
Leading off the conference’s first LBCT session, the randomized VALOR-HCM trial explored whether 16 weeks of mavacamten (MyoKardia) could help patients with severe obstructive hypertrophic cardiomyopathy (HCM) avoid septal reduction therapy, either surgical or by alcohol ablation.
The 22-center VALOR-HCM trial with an estimated enrollment of 100 follows EXPLORER-HCM, which in 2020 suggested the novel myosin-inhibiting agent could improve symptoms, exercise capacity, cardiac remodeling, and quality of life in such patients.
Simply advising people with heart failure (HF) to consume less salt is one thing, but it’s another to show them clinical trial evidence that it might help keep them out of the hospital. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure) study, conducted at 27 sites in six countries, sought to provide that evidence.
The trial randomly assigned 1,000 patients with NYHA class 2-3 HF to consume no more than 1,500 mg/day in sodium or to receive standard advice to limit sodium intake, and followed them for a year for the endpoint of death from any cause, cardiovascular (CV) hospitalization, or CV emergency department visit.
SODIUM-HF “may provide a rigorous evidence base for sodium restriction in patients with heart failure and may truly change our practice and how we recommend dietary modification,” ACC 2022 vice chair Douglas E. Drachman, MD, Massachusetts General Hospital, Boston, said at the media presentation.
In the same session, the CHAP (Chronic Hypertension and Pregnancy) study explored whether blood pressure (BP) control in pregnant women with new or untreated chronic hypertension could help avert preeclampsia, poor fetal outcomes, and other adverse events.
CHAP assigned about 2,400 women to receive either stepwise antihypertensive therapy to a BP goal of 140/90 mm Hg or lower or no such meds unless their BP reached or exceeded 160/105 mm Hg. Stepwise therapy featured either labetalol or extended-release nifedipine to start, the other agent added as necessary.
The LBCT block also includes the POISE-3 (Perioperative Ischemic Evaluation-3) comparison of the hemostatic agent tranexamic acid vs. placebo in nearly 10,000 patients undergoing noncardiac surgery. A separate randomization of the same cohort, to be reported at a Monday LBCT session, compared pre- and perioperative BP-control strategies.
Saturday, April 2, 12:00 p.m.–1:15 p.m. Featured Clinical Research I. Room 143A
This session features a subgroup analysis by age from the REVERSE-IT trial, which had previously showcased the monoclonal antibody bentracimab (PhaseBio Pharmaceuticals) for its ability to reverse the antiplatelet effects of ticagrelor.
REVERSE-IT is accompanied on the schedule by several secondary-endpoint presentations from trials whose primary outcomes have already been presented at meetings or in the journals.
They include the SCORED trial of sotagliflozin in patients with diabetes and chronic kidney disease (CKD); COMPLETE, which explored complete revascularization of multivessel coronary disease at primary stenting; and the FAME-3 comparison of coronary bypass surgery (CABG) vs. percutaneous coronary intervention (PCI) guided by fractional flow reserve (FFR) readings.
The session is to conclude with EDIT-CMD, which was a small, randomized assessment of diltiazem for improving microvascular dysfunction in patients with chronic angina despite nonobstructive coronary disease.
Sunday, April 3, 8:00 a.m.–9:15 a.m. Joint American College of Cardiology/Journal of the American Medical Association LBCT (II)
The SuperWIN (Supermarket Web Intervention) study tested an innovative strategy for community-based promotion of healthy lifestyle choices: point-of-purchase dietary education for grocery shoppers with an online instructional component, and follow-up to determine whether it influenced future food choices.
“Dietary interventions are notoriously difficult for us to implement, let alone to study scientifically,” Dr. Drachman observed. “So we think that there may be opportunity for dietary interventions to be best implemented at grocery stores where people are doing their shopping for food.”
SuperWIN compared supermarket shoppers with at least one CV risk factor who participated in the education intervention to a nonintervention control group for any changes in their DASH scores. The scores reflected consistency with the venerable DASH diet based on participants’ food purchases over 3 months.
In the same session, the MITIGATE trial explored whether daily administration of icosapent ethyl (Vascepa) might cut the risk of upper respiratory infection (especially from SARS-CoV-2 or seasonal influenza virus) in persons 50 or older with a history of clinical coronary, neurovascular, or peripheral vascular disease or revascularization. The trial has an estimated enrollment of 39,600.
Accompanying SuperWIN and MITIGATE are studies of several dyslipidemia drugs, including the discontinued antisense agent vupanorsen (Pfizer), as tested in TRANSLATE-TIMI 70; the PCSK9 inhibitor alirocumab (Praluent), explored for its effects on coronary plaque volume and composition in the PACMAN-AMI trial; and the APOLLO trial, a phase 1 evaluation of SLN360 (Silence Therapeutics), a short interfering ribonucleic acid (siRNA) that suppresses the molecular machinery in the liver that produces lipoprotein(a), or Lp(a).
The 32-patient APOLLO trial’s recently released top-line results suggested that SLN360 at varying dosages reduced Lp(a) levels by about one-half to more than 90%. Although elevated Lp(a) is known to track with CV risk, it remains to be shown whether dropping Lp(a) levels pharmacologically is protective.
Sunday, April 3, 9:45 a.m.–11:00 a.m. Joint American College of Cardiology/New England Journal of Medicine LBCT (III)
The meeting’s all-HF late-breaker session includes the METEORIC-HF trial, which compared the myotropic agent omecamtiv mecarbil (Cytokinetics) against placebo for effects on exercise performance over 20 weeks. The trial entered 276 patients with HF with reduced ejection fraction (HFrEF) and reduced peak VO2.
The GALACTIC-HF trial had previously suggested that the drug improved the risk of HF-related events or CV death in more than 8000 patients with HFrEF, those with the lowest ejection fractions benefiting the most.
This block of trials also features DIAMOND, the latest trial with a gemologic name to look at the potassium sequestrant patiromer (Veltassa) for any protection against hyperkalemia, a familiar side effect of renin-angiotensin-aldosterone inhibitors. DIAMOND tested patiromer in 878 patients with HFrEF who were on beta-blockers and other HF-appropriate medications and had a history of drug-associated hyperkalemia.
Previously, the AMBER trial of patients with CKD or refractory hypertension on spironolactone had suggested the drug might be protective enough against hyperkalemia to allow higher and more consistent dosing of BP-lowering agents.
Also in the session: the randomized IVVE (Influenza Vaccine to Prevent Adverse Vascular Events) trial, with an estimated 5,000 patients with HF in Africa, Asia, and the Middle East; PROMPT-HF, with a projected 1,310 HF patients and billed as a cluster-randomized pragmatic trial of a strategy for improving guideline-directed outpatient medical therapy; and MAVA-LTE, the long-term extension study of an estimated 310 patients who were in the MAVERICK-HCM and EXPLORER-HCM mavacamten trials.
Sunday, April 3, 12:15–1:30 p.m. Featured Clinical Research II. Main Tent, Hall D
The arrhythmia-centric session includes PARTITA, with its estimated 590 patients with primary- or secondary-prevention implantable cardioverter-defibrillators (ICDs). The trial followed them initially for burden of untreated nonsustained ventricular tachycardia (VT) or events treated with anti-tachycardia pacing. Then it randomly assigned those who experienced a first appropriate ICD shock to either immediate VT ablation or standard care. The latter included ablation on next occurrence of arrhythmic storm.
Investigational oral factor XIa inhibitors, viewed by many as potentially safer as anticoagulants than contemporary oral inhibitors of factor Xa, are now on the scene and include milvexian (Bristol-Myers Squibb/Janssen) and, lately, asundexian (BAY 2433334; Bayer). The latter agent was compared to the factor Xa inhibitor apixaban (Eliquis) in 753 patients with AF in the phase 2 PACIFIC-AF trial, which looked at the newer drug’s safety and optimal dosing.
Also on the bill: a long-term follow-up of the mAFA-2 (Mobile AF Application 2) extension study, which explored the value of a smartphone-based atrial fibrillation (AF) screening app for improving risk of AF-related events; a presentation billed as “Residual Leaks Post Left Atrial Appendage Occlusion”; and one that declares “low rates of guideline-directed care” to be “associated with higher mortality” in patients with pacemakers or ICDs.
Monday, April 4, 8:30 a.m.–9:45 a.m. LBCT IV
This session is to open with the PROTECT trial, which sought to determine whether perioperative “aggressive warming” may be cardioprotective in patients with CV risk factors undergoing noncardiac surgery. Its estimated 5,100 patients were randomly assigned to a procedure that achieves normothermia, that is 37° C (98.6° F), vs. standard care in which patients’ core temperature may decline to no further than 35.5° C (95.9° F).
Next on the list are a second POISE-3 comparison of BP-control strategies comparing hypotension avoidance vs. hypertension avoidance in patients undergoing noncardiac surgery; the pivotal CLASP 2 TR trial of patients with symptomatic tricuspid regurgitation on optimal medical therapy with vs. without treatment with the Edwards PASCAL Transcatheter Repair System; and one said to provide “insights from the Corevalve US Pivotal and SURTAVI trials” on 5-year incidence, timing, and predictors of hemodynamic valve deterioration transcatheter and surgical aortic bioprostheses.”
Rounding out the block of presentations: the ADAPT-TAVR comparison of the factor Xa inhibitor edoxaban (Lixiana) to dual-antiplatelet therapy for prevention of leaflet thrombosis after successful transcatheter aortic valve replacement (TAVR). The 235-patient trial was conducted at five centers in South Korea, Hong Kong, and Taiwan.
Monday, April 4, 11:00–12:15 p.m. LBCT V
This session includes the FLAVOUR randomized comparison of PCI guided by either FFR or intravascular ultrasound (IVUS) in 1,700 patients with 40%-70% stenoses. The patients from centers in China and South Korea were followed for death from any cause, MI, or any repeat revascularization at 24 months.
Also scheduled: the 2-year report on 4,000 patients with ST-segment elevation MI (STEMI) in the ACC-sponsored quality improvement program GHATI (Global Heart Attack Treatment Initiative); the GIPS-4 myocardial protection study of an estimated 380 patients with STEMI assigned to receive pre- and post-PCI infusions of sodium thiosulfate or placebo, with infarct size at 4 months as the primary endpoint; and a randomized test of an arrhythmia-monitoring implant for influence on clinical outcomes in 802 patients with a history of MI but no pacemaker or ICD indication, called BIO-GUARD-MI,
Last in the session: the Chocolate Touch Study of peripheral-artery angioplasty using a drug-coated balloon (DCB) with a confectionery name that treats lesions not with theobromine, but the antiproliferative mainstay paclitaxel.
The randomized comparison of the Chocolate Touch DCB (TriReme Medical) and the more established Lutonix DCB (Bard) assigned a projected 585 patients with symptomatic peripheral vascular disease to treatment of superficial femoral or popliteal artery lesions with one of the two paclitaxel-coated balloon catheters.
Monday, April 4, 12:45–2 p.m. Featured Clinical Research III. Room 143A
The final session features five subgroup analyses or other updates from trials that have already reported their primary outcomes. Among them is the SPYRAL HTN-ON MED trial, which helped to revitalize hopes for renal denervation therapy as a catheter-based treatment for drug-resistant hypertension by showing significant effects on both systolic and diastolic blood pressure. The new data follow the trial’s more than 400 patients out to 3 years.
There is also a symptom and quality-of-life analysis from the 530-patient EMPULSE trial of 530 patients with stabilized acute HF assigned in-hospital to start on empagliflozin (Jardiance) or placebo. The trial made a splash last year when it reported a significant improvement in risk for death or HF rehospitalization for its patients put on the SGLT2 inhibitor.
A secondary analysis from CANTOS is also featured; the trial had randomly assigned more than 10,000 patients with recent acute MI and elevated C-reactive protein (CRP) levels to receive or not receive the anti-inflammatory canakinumab (Ilaris). Those assigned to active therapy showed benefits for a range of outcomes, including CV mortality and stroke, but no decreases in cholesterol levels. Billing for the new CANTOS analysis promises insights on the “differential impact of residual inflammatory risk and residual cholesterol risk among atherosclerosis patients with and without chronic kidney disease.”
The session also features “trends and final results” from the NACMI (North American COVID-19 Myocardial Infarction) registry, which had shown excellent primary-PCI results without compromise of door-to-balloon times in patients with confirmed SARS-CoV-2 infection; and a FIDELITY analysis of cardiorenal endpoints by history of CV disease in the study’s more than 13,000 patients with diabetes and CKD assigned to placebo or finerenone (Kerendia), a mineralocorticoid receptor antagonist.
A version of this article first appeared on Medscape.com.
Sleep deprivation sends fat to the belly
A controlled study of sleep-deprived young adults has provided the first causal evidence linking the lack of sleep to abdominal obesity and harmful visceral, or “belly” fat. In what the researchers claim is the first-ever study evaluating the relationship between sleep restriction and body fat distribution, they’ve reported the novel finding that the expansion of abdominal adipose tissue, and especially visceral fat, occurred as a function of shortened sleep.
Naima Covassin, PhD, a researcher in cardiovascular medicine at Mayo Clinic in Rochester, Minn., led the randomized, controlled study of 12 healthy, nonobese people randomized to controlled sleep restriction – 2 weeks of 4 hours of sleep a night – or controlled sleep of 9 hours a night, followed by a 3-day recovery period. The study was conducted in the hospital, monitored participants’ caloric intake, and used accelerometry to monitor energy expense. Participants ranged in age from 19 to 39 years.
“What we found was that at the end of 2 weeks these people put on just about a pound, 0.5 kg, of extra weight, which was significant but still very modest,” senior author Virend K. Somers, MD, PhD, said in an interview. “The average person who sleeps 4 hours a night thinks they’re doing OK if they only put on a pound.” Dr. Somers is the Alice Sheets Marriott Professor in Cardiovascular Medicine at Mayo Clinic.
“The problem is,” he said, “that when you do a more specific analysis you find that actually with the 1 pound the significant increase of the fat is in the belly area, particularly inside the belly.”
The study found that the patients on curtailed sleep ate on average an additional 308 calories a day more than their controlled sleep counterparts (95% confidence interval, 59.2-556.8 kcal/day; P = .015), and while that translated into a 0.5-kg weight gain (95% CI, 0.1-0.8 kg; P = .008), it also led to a 7.8-cm2 increase visceral adipose tissue (VAT) (95% CI, 0.3-15.3 cm2; P = .042), representing an increase of around 11%. The study used CT on day 1 and day 18 (1 day after the 3-day recovery period) to evaluate the distribution of abdominal fat.
VAT findings post recovery
After the recovery period, however, the study found that VAT in the sleep-curtailed patients kept rising, yet body weight and subcutaneous fat dropped, and the increase in total abdominal fat flattened. “They slept a lot, they ate fewer calories and their weight came down, but, very importantly, their belly fat went up even further,” Dr. Somers said. On average, it increased another 3.125 cm2 by day 21.
The findings raised a number of questions that need further exploration, Dr. Somers said. “There’s some biochemical message in the body that’s continuing to send fat to the visceral compartment,” he said. “What we don’t know is whether repetitive episodes of inadequate sleep actually accumulate over the years to give people a preponderance of belly fat.”
The study also showed that the traditional parameters used for evaluating cardiovascular risk are not enough, Dr. Somers said. “If we just did body weight, body mass index, and overall body fat percentage, we’d completely miss this,” he said.
Future investigations should focus on two points, he said: identifying the mechanisms that cause VAT accumulation with less sleep, and whether extending sleep can reverse the process.
“The big worry is obviously the heart,” Dr. Somers said. “Remember, these are not sick people. These are young healthy people who are doing the wrong thing with their body fat; they’re sending the fat to the completely wrong place.”
In an invited editorial, endocrinologist Harold Bays, MD, wrote that the study confirmed the need for evaluating sleep disorders as a potential cause of accumulated VAT. Dr. Bays of the University of Louisville (Ky.) is medical director and president of the Louisville Metabolic and Atherosclerosis Research Center.
“The biggest misconception of many clinicians, and some cardiologists, is that obesity is not a disease,” Dr. Bays said in an interview. “Even when some clinicians believe obesity is a disease, they believe its pathogenic potential is limited to visceral fat.” He noted that subcutaneous fat can lead to accumulation of VAT and epicardial fat, as well as fatty infiltration of the liver and other vital organs, resulting in increased epicardial adipose tissue and indirect adverse effects on the heart.
“Thus, even if disruption of sleep does not increase body weight, if disruption of sleep results in fat dysfunction – “sick fat” or adiposopathy – then this may result in increased CVD risk factors and unhealthy body composition, including an increase in visceral fat,” Dr. Bays said.
The study received funding from the National Institutes of Health. Dr. Somers disclosed relationships with Baker Tilly, Jazz Pharmaceuticals, Bayer, Sleep Number and Respicardia. Coauthors had no disclosures. Dr. Bays is medical director of Your Body Goal and chief science officer of the Obesity Medical Association.
A controlled study of sleep-deprived young adults has provided the first causal evidence linking the lack of sleep to abdominal obesity and harmful visceral, or “belly” fat. In what the researchers claim is the first-ever study evaluating the relationship between sleep restriction and body fat distribution, they’ve reported the novel finding that the expansion of abdominal adipose tissue, and especially visceral fat, occurred as a function of shortened sleep.
Naima Covassin, PhD, a researcher in cardiovascular medicine at Mayo Clinic in Rochester, Minn., led the randomized, controlled study of 12 healthy, nonobese people randomized to controlled sleep restriction – 2 weeks of 4 hours of sleep a night – or controlled sleep of 9 hours a night, followed by a 3-day recovery period. The study was conducted in the hospital, monitored participants’ caloric intake, and used accelerometry to monitor energy expense. Participants ranged in age from 19 to 39 years.
“What we found was that at the end of 2 weeks these people put on just about a pound, 0.5 kg, of extra weight, which was significant but still very modest,” senior author Virend K. Somers, MD, PhD, said in an interview. “The average person who sleeps 4 hours a night thinks they’re doing OK if they only put on a pound.” Dr. Somers is the Alice Sheets Marriott Professor in Cardiovascular Medicine at Mayo Clinic.
“The problem is,” he said, “that when you do a more specific analysis you find that actually with the 1 pound the significant increase of the fat is in the belly area, particularly inside the belly.”
The study found that the patients on curtailed sleep ate on average an additional 308 calories a day more than their controlled sleep counterparts (95% confidence interval, 59.2-556.8 kcal/day; P = .015), and while that translated into a 0.5-kg weight gain (95% CI, 0.1-0.8 kg; P = .008), it also led to a 7.8-cm2 increase visceral adipose tissue (VAT) (95% CI, 0.3-15.3 cm2; P = .042), representing an increase of around 11%. The study used CT on day 1 and day 18 (1 day after the 3-day recovery period) to evaluate the distribution of abdominal fat.
VAT findings post recovery
After the recovery period, however, the study found that VAT in the sleep-curtailed patients kept rising, yet body weight and subcutaneous fat dropped, and the increase in total abdominal fat flattened. “They slept a lot, they ate fewer calories and their weight came down, but, very importantly, their belly fat went up even further,” Dr. Somers said. On average, it increased another 3.125 cm2 by day 21.
The findings raised a number of questions that need further exploration, Dr. Somers said. “There’s some biochemical message in the body that’s continuing to send fat to the visceral compartment,” he said. “What we don’t know is whether repetitive episodes of inadequate sleep actually accumulate over the years to give people a preponderance of belly fat.”
The study also showed that the traditional parameters used for evaluating cardiovascular risk are not enough, Dr. Somers said. “If we just did body weight, body mass index, and overall body fat percentage, we’d completely miss this,” he said.
Future investigations should focus on two points, he said: identifying the mechanisms that cause VAT accumulation with less sleep, and whether extending sleep can reverse the process.
“The big worry is obviously the heart,” Dr. Somers said. “Remember, these are not sick people. These are young healthy people who are doing the wrong thing with their body fat; they’re sending the fat to the completely wrong place.”
In an invited editorial, endocrinologist Harold Bays, MD, wrote that the study confirmed the need for evaluating sleep disorders as a potential cause of accumulated VAT. Dr. Bays of the University of Louisville (Ky.) is medical director and president of the Louisville Metabolic and Atherosclerosis Research Center.
“The biggest misconception of many clinicians, and some cardiologists, is that obesity is not a disease,” Dr. Bays said in an interview. “Even when some clinicians believe obesity is a disease, they believe its pathogenic potential is limited to visceral fat.” He noted that subcutaneous fat can lead to accumulation of VAT and epicardial fat, as well as fatty infiltration of the liver and other vital organs, resulting in increased epicardial adipose tissue and indirect adverse effects on the heart.
“Thus, even if disruption of sleep does not increase body weight, if disruption of sleep results in fat dysfunction – “sick fat” or adiposopathy – then this may result in increased CVD risk factors and unhealthy body composition, including an increase in visceral fat,” Dr. Bays said.
The study received funding from the National Institutes of Health. Dr. Somers disclosed relationships with Baker Tilly, Jazz Pharmaceuticals, Bayer, Sleep Number and Respicardia. Coauthors had no disclosures. Dr. Bays is medical director of Your Body Goal and chief science officer of the Obesity Medical Association.
A controlled study of sleep-deprived young adults has provided the first causal evidence linking the lack of sleep to abdominal obesity and harmful visceral, or “belly” fat. In what the researchers claim is the first-ever study evaluating the relationship between sleep restriction and body fat distribution, they’ve reported the novel finding that the expansion of abdominal adipose tissue, and especially visceral fat, occurred as a function of shortened sleep.
Naima Covassin, PhD, a researcher in cardiovascular medicine at Mayo Clinic in Rochester, Minn., led the randomized, controlled study of 12 healthy, nonobese people randomized to controlled sleep restriction – 2 weeks of 4 hours of sleep a night – or controlled sleep of 9 hours a night, followed by a 3-day recovery period. The study was conducted in the hospital, monitored participants’ caloric intake, and used accelerometry to monitor energy expense. Participants ranged in age from 19 to 39 years.
“What we found was that at the end of 2 weeks these people put on just about a pound, 0.5 kg, of extra weight, which was significant but still very modest,” senior author Virend K. Somers, MD, PhD, said in an interview. “The average person who sleeps 4 hours a night thinks they’re doing OK if they only put on a pound.” Dr. Somers is the Alice Sheets Marriott Professor in Cardiovascular Medicine at Mayo Clinic.
“The problem is,” he said, “that when you do a more specific analysis you find that actually with the 1 pound the significant increase of the fat is in the belly area, particularly inside the belly.”
The study found that the patients on curtailed sleep ate on average an additional 308 calories a day more than their controlled sleep counterparts (95% confidence interval, 59.2-556.8 kcal/day; P = .015), and while that translated into a 0.5-kg weight gain (95% CI, 0.1-0.8 kg; P = .008), it also led to a 7.8-cm2 increase visceral adipose tissue (VAT) (95% CI, 0.3-15.3 cm2; P = .042), representing an increase of around 11%. The study used CT on day 1 and day 18 (1 day after the 3-day recovery period) to evaluate the distribution of abdominal fat.
VAT findings post recovery
After the recovery period, however, the study found that VAT in the sleep-curtailed patients kept rising, yet body weight and subcutaneous fat dropped, and the increase in total abdominal fat flattened. “They slept a lot, they ate fewer calories and their weight came down, but, very importantly, their belly fat went up even further,” Dr. Somers said. On average, it increased another 3.125 cm2 by day 21.
The findings raised a number of questions that need further exploration, Dr. Somers said. “There’s some biochemical message in the body that’s continuing to send fat to the visceral compartment,” he said. “What we don’t know is whether repetitive episodes of inadequate sleep actually accumulate over the years to give people a preponderance of belly fat.”
The study also showed that the traditional parameters used for evaluating cardiovascular risk are not enough, Dr. Somers said. “If we just did body weight, body mass index, and overall body fat percentage, we’d completely miss this,” he said.
Future investigations should focus on two points, he said: identifying the mechanisms that cause VAT accumulation with less sleep, and whether extending sleep can reverse the process.
“The big worry is obviously the heart,” Dr. Somers said. “Remember, these are not sick people. These are young healthy people who are doing the wrong thing with their body fat; they’re sending the fat to the completely wrong place.”
In an invited editorial, endocrinologist Harold Bays, MD, wrote that the study confirmed the need for evaluating sleep disorders as a potential cause of accumulated VAT. Dr. Bays of the University of Louisville (Ky.) is medical director and president of the Louisville Metabolic and Atherosclerosis Research Center.
“The biggest misconception of many clinicians, and some cardiologists, is that obesity is not a disease,” Dr. Bays said in an interview. “Even when some clinicians believe obesity is a disease, they believe its pathogenic potential is limited to visceral fat.” He noted that subcutaneous fat can lead to accumulation of VAT and epicardial fat, as well as fatty infiltration of the liver and other vital organs, resulting in increased epicardial adipose tissue and indirect adverse effects on the heart.
“Thus, even if disruption of sleep does not increase body weight, if disruption of sleep results in fat dysfunction – “sick fat” or adiposopathy – then this may result in increased CVD risk factors and unhealthy body composition, including an increase in visceral fat,” Dr. Bays said.
The study received funding from the National Institutes of Health. Dr. Somers disclosed relationships with Baker Tilly, Jazz Pharmaceuticals, Bayer, Sleep Number and Respicardia. Coauthors had no disclosures. Dr. Bays is medical director of Your Body Goal and chief science officer of the Obesity Medical Association.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY