User login
Chest Pain and Vomiting with Prior Heart Attack
ANSWER
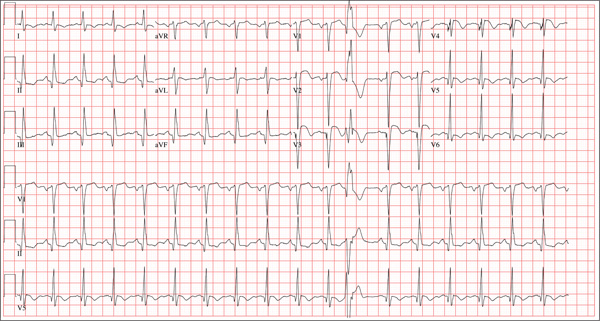
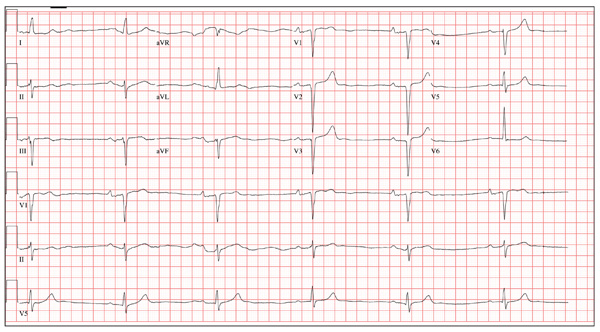
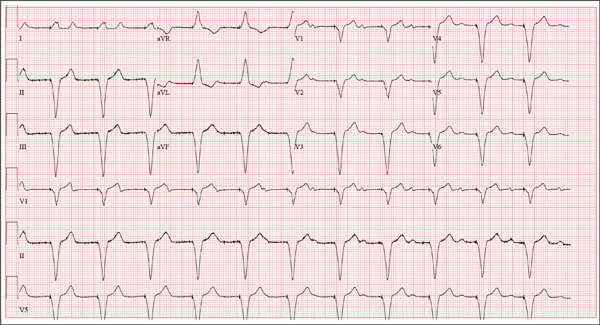
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
ANSWER
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
ANSWER
The correct interpretation includes sinus tachycardia with occasional premature ventricular complexes (PVCs), left atrial enlargement, evidence of a previous inferior MI, and an acute anterior MI. Sinus tachycardia is evidenced by a rate ≥ 100 beats/min and the presence of a P wave for every QRS complex with a constant PR interval. A single PVC is evident (12th beat of the rhythm strips V1, II, and V5).
Left atrial enlargement is evidenced by a large P wave in lead II and a biphasic P wave with the terminal portion larger than the initial portion in lead V1. An old inferior MI is evidenced by the presence of Q waves in leads II, III, and aVF.
An evolving anterior MI is diagnosed by the presence of poor R-wave progression with ST-segment elevations and T-wave inversion in leads V2, V3, and V4. This was subsequently confirmed by clinically significant elevations of serum troponin levels and by cardiac catheterization, which revealed occlusion of the left anterior descending artery distal to the internal mammary artery anastomosis.
Three hours ago, this 69-year-old man started to experience substernal chest pain, nausea, and vomiting. He had stopped for lunch after spending the morning raking leaves; his chest pain began while he was at the drive-through window at a local fast food restaurant. By the time he got home, he was nauseous and had an episode of emesis. The pain is described as a “dull, heavy ache” with radiation to the left neck and arm. The patient states he is diaphoretic, but attributes it to the labor associated with his yardwork. He recalls that his first heart attack started in a similar way and fears he is having another. Following the emesis, his nausea stopped, and he rested in his recliner, hoping his symptoms would resolve. Unfortunately, the chest pain worsened, and he drove himself to the clinic rather than calling 911. (He didn’t want to go to the ED or get billed for the ambulance ride.) Review of his medical history reveals coronary artery disease, evidenced by an inferior MI in 2008. This was treated with coronary artery bypass surgery with reversed saphenous vein grafts placed to the first and second obtuse marginal branches of the circumflex coronary artery, reversed saphenous vein graft to the posterior descending artery, and an internal mammary artery graft placed to the proximal left anterior descending artery. His history is also remarkable for hyperlipidemia, hypertension, and obesity. He is a retired postal worker who has lived alone since his wife died three years ago. He drinks a six-pack of beer daily and continues to smoke one to two packs of cigarettes per day, depending on his activities. His family history includes coronary artery disease, hypertension, diabetes, and stroke. His current medications include aspirin, atorvastatin, clopidogrel, furosemide, isosorbide dinitrate, metoprolol, nicotine patch, potassium chloride, and valsartan. He is intolerant of ACE inhibitors, due to the resulting chronic, dry cough. The review of systems reveals that he has had headaches over the past week and that he recently recovered from the flu. He has had no changes in bowel or bladder function, shortness of breath, or recent weight loss or gain. Vital signs include a blood pressure of 168/100 mm Hg; pulse, 110 beats/min; respiratory rate, 18 breaths/min-1; O2 saturation, 98% on room air; and temperature, 37.2°C. His weight is 108 kg, and his height is 170 cm. Physical findings show that the lungs are clear to auscultation; his rhythm is regular with no murmurs, rubs, or gallops; and the point of maximum impulse is not displaced. The neck veins are flat, and there is no peripheral edema. A well-healed median sternotomy scar is evident, as are bilateral lower extremity saphenous vein harvest scars. The abdomen is soft and nontender, and peripheral pulses are strong and equal bilaterally. There are no neurologic abnormalities noted. Laboratory samples and an ECG are obtained. The following findings are noted on the ECG: a ventricular rate of 108 beats/min; PR interval, 140 ms; QRS duration, 116 ms; QT/QTc interval, 372/498 ms; P axis, 70°; R axis, 75°; and T axis, 167°. What is your interpretation of this ECG?
Thumb: Scaling with Pitted Nail Plate
ANSWER
The most likely diagnosis is psoriasis (choice “d”), which can manifest with localized involvement (see discussion below).
Fungal infection (choice “a”) is unlikely, given the negative results of the KOH prep and total lack of response to treatment for that diagnosis.
Eczema (choice “b”) does not manifest as such thick, adherent scale. If any nail changes were involved, they would likely consist of transverse nail ridges.
A variant of squamous cell carcinoma (SCC; choice “c”)—caused by human papillomavirus (HPV), for example—can produce somewhat similar changes in the skin. But it would be unlikely to lead to nail changes, and it would not be intermittent, as this rash was in apparent response to OTC cream.
DISCUSSION
A punch biopsy is sometimes required to confirm the diagnosis of psoriasis, but this combination of skin and nail changes is quite suggestive of that entity. In this case, the confirmation was made by a different route: The rheumatologist judged that the patient’s arthritis was psoriatic in nature. The arthritis was treated with methotrexate, which soon cleared the skin disease without any help from dermatology.
This case serves to reinforce the possible mind-body role of stress in the genesis of this disease; however, at least 30% of the time, there is a positive family history. It also demonstrates the seemingly contradictory fact that the severity of the psoriasis doesn’t always correlate with the presence or absence of psoriatic arthritis.
Adding to the difficulty of making the diagnosis of psoriasis is the localized distribution of the scales, since it can usually be corroborated by finding lesions in their usual haunts—such as the extensor surfaces of arms, legs, on the trunk, or in the scalp. Cases such as this one force the provider to carefully consider the differential, which includes fungal infection. But the dermatophytes that cause ordinary fungal infections have to come from predictable sources (eg, children, pets, or farm animals), all missing from this patient’s history.
Had the rash been “fixed” (unchanging), the diagnosis of SCC would have to be considered more carefully. Superficial SCC is called Bowen’s disease, which, in cases such as this, is usually caused by HPV, not by the more typical overexposure to UV light. Though superficial, Bowen’s disease can become focally invasive and can even metastasize.
Had this patient not been treated with methotrexate, we would probably have used topical class 1 corticosteroid creams, which would have had a good chance to improve his skin but not his nail. The patient was also counseled regarding the role of stress and increased alcohol intake in the worsening of his disease. His prognosis for skin and joint disease is decent, though he will probably experience recurrences.
ANSWER
The most likely diagnosis is psoriasis (choice “d”), which can manifest with localized involvement (see discussion below).
Fungal infection (choice “a”) is unlikely, given the negative results of the KOH prep and total lack of response to treatment for that diagnosis.
Eczema (choice “b”) does not manifest as such thick, adherent scale. If any nail changes were involved, they would likely consist of transverse nail ridges.
A variant of squamous cell carcinoma (SCC; choice “c”)—caused by human papillomavirus (HPV), for example—can produce somewhat similar changes in the skin. But it would be unlikely to lead to nail changes, and it would not be intermittent, as this rash was in apparent response to OTC cream.
DISCUSSION
A punch biopsy is sometimes required to confirm the diagnosis of psoriasis, but this combination of skin and nail changes is quite suggestive of that entity. In this case, the confirmation was made by a different route: The rheumatologist judged that the patient’s arthritis was psoriatic in nature. The arthritis was treated with methotrexate, which soon cleared the skin disease without any help from dermatology.
This case serves to reinforce the possible mind-body role of stress in the genesis of this disease; however, at least 30% of the time, there is a positive family history. It also demonstrates the seemingly contradictory fact that the severity of the psoriasis doesn’t always correlate with the presence or absence of psoriatic arthritis.
Adding to the difficulty of making the diagnosis of psoriasis is the localized distribution of the scales, since it can usually be corroborated by finding lesions in their usual haunts—such as the extensor surfaces of arms, legs, on the trunk, or in the scalp. Cases such as this one force the provider to carefully consider the differential, which includes fungal infection. But the dermatophytes that cause ordinary fungal infections have to come from predictable sources (eg, children, pets, or farm animals), all missing from this patient’s history.
Had the rash been “fixed” (unchanging), the diagnosis of SCC would have to be considered more carefully. Superficial SCC is called Bowen’s disease, which, in cases such as this, is usually caused by HPV, not by the more typical overexposure to UV light. Though superficial, Bowen’s disease can become focally invasive and can even metastasize.
Had this patient not been treated with methotrexate, we would probably have used topical class 1 corticosteroid creams, which would have had a good chance to improve his skin but not his nail. The patient was also counseled regarding the role of stress and increased alcohol intake in the worsening of his disease. His prognosis for skin and joint disease is decent, though he will probably experience recurrences.
ANSWER
The most likely diagnosis is psoriasis (choice “d”), which can manifest with localized involvement (see discussion below).
Fungal infection (choice “a”) is unlikely, given the negative results of the KOH prep and total lack of response to treatment for that diagnosis.
Eczema (choice “b”) does not manifest as such thick, adherent scale. If any nail changes were involved, they would likely consist of transverse nail ridges.
A variant of squamous cell carcinoma (SCC; choice “c”)—caused by human papillomavirus (HPV), for example—can produce somewhat similar changes in the skin. But it would be unlikely to lead to nail changes, and it would not be intermittent, as this rash was in apparent response to OTC cream.
DISCUSSION
A punch biopsy is sometimes required to confirm the diagnosis of psoriasis, but this combination of skin and nail changes is quite suggestive of that entity. In this case, the confirmation was made by a different route: The rheumatologist judged that the patient’s arthritis was psoriatic in nature. The arthritis was treated with methotrexate, which soon cleared the skin disease without any help from dermatology.
This case serves to reinforce the possible mind-body role of stress in the genesis of this disease; however, at least 30% of the time, there is a positive family history. It also demonstrates the seemingly contradictory fact that the severity of the psoriasis doesn’t always correlate with the presence or absence of psoriatic arthritis.
Adding to the difficulty of making the diagnosis of psoriasis is the localized distribution of the scales, since it can usually be corroborated by finding lesions in their usual haunts—such as the extensor surfaces of arms, legs, on the trunk, or in the scalp. Cases such as this one force the provider to carefully consider the differential, which includes fungal infection. But the dermatophytes that cause ordinary fungal infections have to come from predictable sources (eg, children, pets, or farm animals), all missing from this patient’s history.
Had the rash been “fixed” (unchanging), the diagnosis of SCC would have to be considered more carefully. Superficial SCC is called Bowen’s disease, which, in cases such as this, is usually caused by HPV, not by the more typical overexposure to UV light. Though superficial, Bowen’s disease can become focally invasive and can even metastasize.
Had this patient not been treated with methotrexate, we would probably have used topical class 1 corticosteroid creams, which would have had a good chance to improve his skin but not his nail. The patient was also counseled regarding the role of stress and increased alcohol intake in the worsening of his disease. His prognosis for skin and joint disease is decent, though he will probably experience recurrences.

About a year ago, this 40-year-old man developed scaling on the distal one-third of his thumbnail. After an ini-tial apparent response to OTC hydrocortisone 1% cream, the condition began to worsen, spreading to more of the thumb. The patient’s primary care provider diagnosed fungal infection and prescribed a combination clotrima-zole/betamethasone cream, which had no effect. A subsequent four-month course of terbinafine (250 mg/d) also yielded no improvement. The patient then requested referral to dermatology. The patient considers himself “quite healthy,” aside from having moderately severe arthritis, for which he takes nabumetone (750 mg bid). His arthritis recently worsened, and he is scheduled to see a rheumatologist in two months. He admits to being under a great deal of stress shortly before his skin condition developed. As a result, he in-creased his alcohol intake for a few months, but he quit drinking altogether soon afterward. He denies any family history of skin disease and has no children or contact with animals. On examination, most of his thumb is covered by thick adherent white scales on a pinkish base. The margins are sharply defined. A KOH prep is performed, but no fungal elements are seen. The adjacent thumbnail has focal areas of pitting in the nail plate, as well as yellowish discoloration on the dis-tal edge. No such changes are seen on his other nails, and examination of his elbows, knees, trunk, and scalp fails to reveal any significant abnormalities.
Knee Pain After Falling Off Ladder
ANSWER
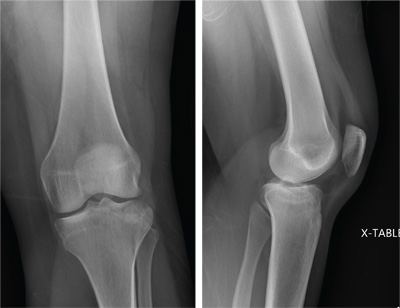
The radiograph shows a lucency within the lateral tibial plateau and tibial metaphysis, consistent with a fracture. It is mildly depressed and slightly comminuted.
Fluid collection is also evident on the lateral view, likely reflecting a lipohemarthrosis. The patient was placed in a knee immobilizer and made non–weight-bearing. She was instructed to follow up with an orthopedist when she returned home (as she was visiting from out of town).
ANSWER
The radiograph shows a lucency within the lateral tibial plateau and tibial metaphysis, consistent with a fracture. It is mildly depressed and slightly comminuted.
Fluid collection is also evident on the lateral view, likely reflecting a lipohemarthrosis. The patient was placed in a knee immobilizer and made non–weight-bearing. She was instructed to follow up with an orthopedist when she returned home (as she was visiting from out of town).
ANSWER
The radiograph shows a lucency within the lateral tibial plateau and tibial metaphysis, consistent with a fracture. It is mildly depressed and slightly comminuted.
Fluid collection is also evident on the lateral view, likely reflecting a lipohemarthrosis. The patient was placed in a knee immobilizer and made non–weight-bearing. She was instructed to follow up with an orthopedist when she returned home (as she was visiting from out of town).
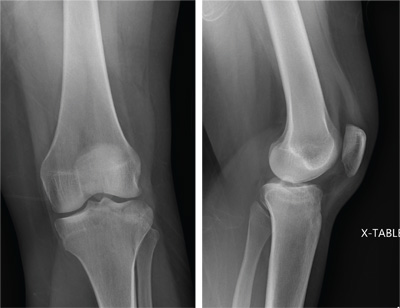
A 25-year-old woman presents for evaluation of left knee pain secondary to a fall. She states she was descending a ladder when she missed a step while still several feet above the ground. She landed on her left foot, awkwardly twisting her leg. She now has swelling and pain in her knee and difficulty bearing weight on that leg. Her medical history is unremarkable. Examination reveals a moderate amount of swelling that limits her ability to flex her left knee. She has diffuse tenderness throughout the knee. Because of the swelling and the patient’s severe discomfort, instability tests are not performed. She has good distal pulses and sensation. Radiographs of the knee are obtained. What is your impression?
The Flu, or a Problem with His Pacemaker?
ANSWER
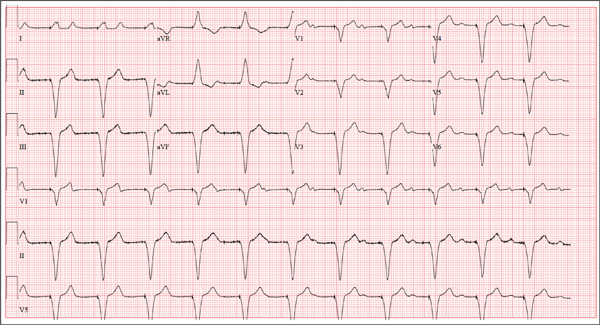
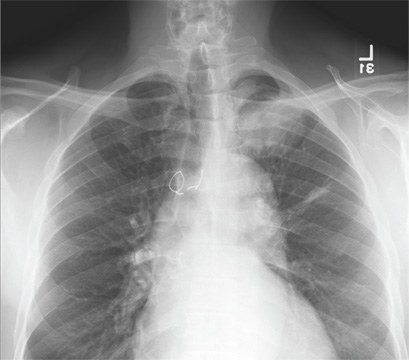
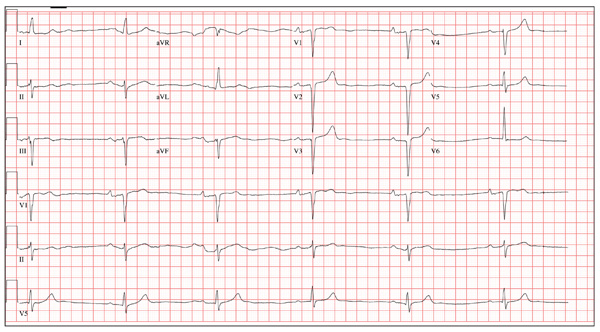
This ECG is remarkable for ventricular pacing at a rate of 70 beats/min, with an underlying sinus rhythm at the same rate as the pacemaker but dissociated from ventricular pacing. Ventricular pacing is evidenced by the presence of a pacing spike before each QRS complex, and the fact that each QRS complex in all leads is wide (200 ms) and does not demonstrate variability within an ECG lead. The T waves are similar in each lead as well. A left-axis deviation of –83° is attributable to pacing from the right ventricle.
What is interesting to note is that P waves are visible and are at a rate very close to that of the ventricular paced beats; however, they show no association with the pacing spike or the QRS complexes. This is most evident in lead V1 and the rhythm strip of lead I, which shows the P waves marching through the QRS and T-wave complexes without being associated with any ventricular conduction. This is an unusual situation in which the sinus rate and the paced ventricular rate are very similar.
Interrogation of the pacemaker generator revealed that the programming had been inadvertently changed from DDDR at a rate of 60 beats/min to VVI at a rate of 70 beats/min. After the device was reprogrammed to its original settings, the patient’s symptoms resolved.
ANSWER
This ECG is remarkable for ventricular pacing at a rate of 70 beats/min, with an underlying sinus rhythm at the same rate as the pacemaker but dissociated from ventricular pacing. Ventricular pacing is evidenced by the presence of a pacing spike before each QRS complex, and the fact that each QRS complex in all leads is wide (200 ms) and does not demonstrate variability within an ECG lead. The T waves are similar in each lead as well. A left-axis deviation of –83° is attributable to pacing from the right ventricle.
What is interesting to note is that P waves are visible and are at a rate very close to that of the ventricular paced beats; however, they show no association with the pacing spike or the QRS complexes. This is most evident in lead V1 and the rhythm strip of lead I, which shows the P waves marching through the QRS and T-wave complexes without being associated with any ventricular conduction. This is an unusual situation in which the sinus rate and the paced ventricular rate are very similar.
Interrogation of the pacemaker generator revealed that the programming had been inadvertently changed from DDDR at a rate of 60 beats/min to VVI at a rate of 70 beats/min. After the device was reprogrammed to its original settings, the patient’s symptoms resolved.
ANSWER
This ECG is remarkable for ventricular pacing at a rate of 70 beats/min, with an underlying sinus rhythm at the same rate as the pacemaker but dissociated from ventricular pacing. Ventricular pacing is evidenced by the presence of a pacing spike before each QRS complex, and the fact that each QRS complex in all leads is wide (200 ms) and does not demonstrate variability within an ECG lead. The T waves are similar in each lead as well. A left-axis deviation of –83° is attributable to pacing from the right ventricle.
What is interesting to note is that P waves are visible and are at a rate very close to that of the ventricular paced beats; however, they show no association with the pacing spike or the QRS complexes. This is most evident in lead V1 and the rhythm strip of lead I, which shows the P waves marching through the QRS and T-wave complexes without being associated with any ventricular conduction. This is an unusual situation in which the sinus rate and the paced ventricular rate are very similar.
Interrogation of the pacemaker generator revealed that the programming had been inadvertently changed from DDDR at a rate of 60 beats/min to VVI at a rate of 70 beats/min. After the device was reprogrammed to its original settings, the patient’s symptoms resolved.
A 75-year-old man presents to your office with complaints of shortness of breath. He states he has had “the flu” for the past week, but it doesn’t seem to be getting any better. His shortness of breath has persisted without change, and he is concerned he may be developing pneumonia. He denies having a productive cough, fevers, chills, or night sweats. Medical history is remarkable for GERD, hyperlipidemia, hypertension, and complete heart block with implantation of a dual-chamber permanent pacemaker in 2010. He has had several surgeries, including a right inguinal hernia repair and an appendectomy. Family history is positive for breast cancer, colon cancer, and stroke. There is no family history of cardiac or pulmonary disease. Social history reveals a retired accountant who lives at home with his wife. He has an occasional brandy in the evening and has never smoked. His current medications include metoprolol, rosu¬\vastatin, and omeprazole. He has no known drug allergies. The review of systems is unremarkable, with the exception of the shortness of breath. The patient is concerned, however, that since his pacemaker was interrogated one week ago, he hasn’t “felt the same.” Physical examination reveals a blood pressure of 130/70 mm Hg; pulse, 70 beats/min; respiratory rate, 16 breaths/min-1; temperature, 36.6°C; and O2 saturation, 97% on room air. The patient’s weight is 105 kg. The cardiovascular exam reveals a regular rate of 70 beats/min, and a grade II/VI early systolic murmur best heard at the left upper sternal border and without radiation. There are no rubs, gallops, or bruits. The pulmonary exam reveals scattered crackles in the right lower chest, which clear with coughing. There are no rhonchi or bronchial breath sounds. All other exams yield normal results. The patient provides a copy of an interrogation report from one year ago, which states his pacemaker is programmed DDDR at a rate of 60 beats/min, with an upper tracking and sensing rate of 130 beats/min, a paced AV delay of 150 ms, and a sensed AV delay of 120 ms. Given the patient’s concern about his most recent interrogation, you call an experienced practitioner to determine whether the patient’s device is functioning appropriately. While waiting, you obtain an ECG, which reveals the following: a ventricular rate of 70 beats/min; PR interval, not measurable; QRS duration, 200 ms; QT/QTc interval, 500/540 ms; no P axis; R axis, –83°; and T axis, 71°. What is your interpretation, and is there any concern regarding his pacemaker function?
All of Her Friends Say She Has Ringworm
ANSWER
The correct answer is pityriasis rosea (PR; choice “d”), which is commonly seen in patients ages 10 to 35 and is about twice as likely to occur in women as in men.
Lichen planus (LP; choice “a”) can mimic PR but lacks the peculiar centripetal scale and oval shape. Furthermore, it does not present with a herald patch.
Guttate psoriasis (choice “b”) could easily be confused for PR. However, it displays heavier white uniform scales with a salmon-pink base, tends to have a distinctly round configuration, and does not involve the appearance of a herald patch.
Secondary syphilis (choice “c”) can usually be ruled out by the sexual history, but also by the lack of a herald patch and the absence of centripetal scaling. Highly variable in appearance, the lesions of secondary syphilis are often seen on the palms.
DISCUSSION
PR was first described in 1860 by Camille Gibert, who used the term pityriasis to describe the fine scale seen with this condition, and chose the term rosea to denote the rosy or pink color.
For a variety of reasons, PR is assumed to be a viral exanthema since, as with many such eruptions, its incidence clusters in the fall and spring, it occurs in close contacts and families, and it is commonly seen in immunocompromised patients. In addition, acquiring the condition appears to confer lifelong immunity.
However, the jury is still out with regard to the exact virus responsible for the disease. Human herpesviruses 6 and 7 are the strongest candidates in terms of antibody production, but no herpesviral particles have been detected in tissue samples.
The so-called herald patch appears initially, in a majority of cases, as a salmon-pink patch that can become as large as 5 to 10 cm, on the trunk or arms. The smaller oval lesions begin to appear within a week or two, averaging 1 to 2 cm in diameter; most display the characteristic “centripetal” scaling, clearly sparing the lesions’ periphery and serving as an essentially pathognomic finding.
On darker-skinned patients, the lesions (including the herald patch) will tend to be brown to black. The examiner must then look for the other characteristic aspects of PR, including the oval (as opposed to round) shape, the long axes of which will often parallel the skin tension lines on the back to produce what is termed the “Christmas tree pattern.” In the author’s experience, the most consistent diagnostic finding is the centripetal scaling seen in at least a few lesions.
Since secondary syphilis is a major item in the differential, obtaining a careful sexual history is essential. If this is uncertain, or if the lesions are not a good fit for PR, obtaining a punch biopsy and serum rapid plasma reagin is necessary. The biopsy in secondary syphilis will show an infiltrate largely composed of plasma cells.
TREATMENT
Once the diagnosis of PR is made, patient education is essential. Affected patients should be reassured about the benign and self-limiting nature of the problem, but also about the likelihood that the condition will persist for up to nine weeks. Darker-skinned patients need to understand that the hyperpigmentation will last for months after the condition has resolved.
Relief of the itching experienced by 75% of PR patients can be achieved with topical steroids (eg, triamcinolone 0.1% cream) and oral antihistamines at bedtime (eg, hydroxyzine 25 to 50 mg) and/or during the daytime (cetirizine 10 mg/d), plus the liberal use of soothing OTC lotions (eg, those containing camphor and menthol). Systemic steroids appear to prolong the condition and are not terribly helpful in controlling the symptoms. In severe cases, phototherapy (narrow-band UVB) can be useful in controlling the itching.
ANSWER
The correct answer is pityriasis rosea (PR; choice “d”), which is commonly seen in patients ages 10 to 35 and is about twice as likely to occur in women as in men.
Lichen planus (LP; choice “a”) can mimic PR but lacks the peculiar centripetal scale and oval shape. Furthermore, it does not present with a herald patch.
Guttate psoriasis (choice “b”) could easily be confused for PR. However, it displays heavier white uniform scales with a salmon-pink base, tends to have a distinctly round configuration, and does not involve the appearance of a herald patch.
Secondary syphilis (choice “c”) can usually be ruled out by the sexual history, but also by the lack of a herald patch and the absence of centripetal scaling. Highly variable in appearance, the lesions of secondary syphilis are often seen on the palms.
DISCUSSION
PR was first described in 1860 by Camille Gibert, who used the term pityriasis to describe the fine scale seen with this condition, and chose the term rosea to denote the rosy or pink color.
For a variety of reasons, PR is assumed to be a viral exanthema since, as with many such eruptions, its incidence clusters in the fall and spring, it occurs in close contacts and families, and it is commonly seen in immunocompromised patients. In addition, acquiring the condition appears to confer lifelong immunity.
However, the jury is still out with regard to the exact virus responsible for the disease. Human herpesviruses 6 and 7 are the strongest candidates in terms of antibody production, but no herpesviral particles have been detected in tissue samples.
The so-called herald patch appears initially, in a majority of cases, as a salmon-pink patch that can become as large as 5 to 10 cm, on the trunk or arms. The smaller oval lesions begin to appear within a week or two, averaging 1 to 2 cm in diameter; most display the characteristic “centripetal” scaling, clearly sparing the lesions’ periphery and serving as an essentially pathognomic finding.
On darker-skinned patients, the lesions (including the herald patch) will tend to be brown to black. The examiner must then look for the other characteristic aspects of PR, including the oval (as opposed to round) shape, the long axes of which will often parallel the skin tension lines on the back to produce what is termed the “Christmas tree pattern.” In the author’s experience, the most consistent diagnostic finding is the centripetal scaling seen in at least a few lesions.
Since secondary syphilis is a major item in the differential, obtaining a careful sexual history is essential. If this is uncertain, or if the lesions are not a good fit for PR, obtaining a punch biopsy and serum rapid plasma reagin is necessary. The biopsy in secondary syphilis will show an infiltrate largely composed of plasma cells.
TREATMENT
Once the diagnosis of PR is made, patient education is essential. Affected patients should be reassured about the benign and self-limiting nature of the problem, but also about the likelihood that the condition will persist for up to nine weeks. Darker-skinned patients need to understand that the hyperpigmentation will last for months after the condition has resolved.
Relief of the itching experienced by 75% of PR patients can be achieved with topical steroids (eg, triamcinolone 0.1% cream) and oral antihistamines at bedtime (eg, hydroxyzine 25 to 50 mg) and/or during the daytime (cetirizine 10 mg/d), plus the liberal use of soothing OTC lotions (eg, those containing camphor and menthol). Systemic steroids appear to prolong the condition and are not terribly helpful in controlling the symptoms. In severe cases, phototherapy (narrow-band UVB) can be useful in controlling the itching.
ANSWER
The correct answer is pityriasis rosea (PR; choice “d”), which is commonly seen in patients ages 10 to 35 and is about twice as likely to occur in women as in men.
Lichen planus (LP; choice “a”) can mimic PR but lacks the peculiar centripetal scale and oval shape. Furthermore, it does not present with a herald patch.
Guttate psoriasis (choice “b”) could easily be confused for PR. However, it displays heavier white uniform scales with a salmon-pink base, tends to have a distinctly round configuration, and does not involve the appearance of a herald patch.
Secondary syphilis (choice “c”) can usually be ruled out by the sexual history, but also by the lack of a herald patch and the absence of centripetal scaling. Highly variable in appearance, the lesions of secondary syphilis are often seen on the palms.
DISCUSSION
PR was first described in 1860 by Camille Gibert, who used the term pityriasis to describe the fine scale seen with this condition, and chose the term rosea to denote the rosy or pink color.
For a variety of reasons, PR is assumed to be a viral exanthema since, as with many such eruptions, its incidence clusters in the fall and spring, it occurs in close contacts and families, and it is commonly seen in immunocompromised patients. In addition, acquiring the condition appears to confer lifelong immunity.
However, the jury is still out with regard to the exact virus responsible for the disease. Human herpesviruses 6 and 7 are the strongest candidates in terms of antibody production, but no herpesviral particles have been detected in tissue samples.
The so-called herald patch appears initially, in a majority of cases, as a salmon-pink patch that can become as large as 5 to 10 cm, on the trunk or arms. The smaller oval lesions begin to appear within a week or two, averaging 1 to 2 cm in diameter; most display the characteristic “centripetal” scaling, clearly sparing the lesions’ periphery and serving as an essentially pathognomic finding.
On darker-skinned patients, the lesions (including the herald patch) will tend to be brown to black. The examiner must then look for the other characteristic aspects of PR, including the oval (as opposed to round) shape, the long axes of which will often parallel the skin tension lines on the back to produce what is termed the “Christmas tree pattern.” In the author’s experience, the most consistent diagnostic finding is the centripetal scaling seen in at least a few lesions.
Since secondary syphilis is a major item in the differential, obtaining a careful sexual history is essential. If this is uncertain, or if the lesions are not a good fit for PR, obtaining a punch biopsy and serum rapid plasma reagin is necessary. The biopsy in secondary syphilis will show an infiltrate largely composed of plasma cells.
TREATMENT
Once the diagnosis of PR is made, patient education is essential. Affected patients should be reassured about the benign and self-limiting nature of the problem, but also about the likelihood that the condition will persist for up to nine weeks. Darker-skinned patients need to understand that the hyperpigmentation will last for months after the condition has resolved.
Relief of the itching experienced by 75% of PR patients can be achieved with topical steroids (eg, triamcinolone 0.1% cream) and oral antihistamines at bedtime (eg, hydroxyzine 25 to 50 mg) and/or during the daytime (cetirizine 10 mg/d), plus the liberal use of soothing OTC lotions (eg, those containing camphor and menthol). Systemic steroids appear to prolong the condition and are not terribly helpful in controlling the symptoms. In severe cases, phototherapy (narrow-band UVB) can be useful in controlling the itching.

Three weeks ago, a 25-year-old woman noticed an asymp¬tomatic lesion of unknown origin on her chest. Since then, smaller versions have appeared in “crops” on her trunk, arms, and lower neck. Friends were unanimous in their opinion that she had “ringworm,” so she consulted her pharmacist, who recommended clotrimazole cream. Despite her use of it, however, the lesions continue to increase in number. Her original lesion has become less red and scaly, though. The patient has felt fine from the outset and maintains that she is “quite healthy” in other respects. Employed as an IT technician, she denies any exposure to children, pets, or sexually transmitted diseases. The patient, who is African-American, has type V skin. Her original lesion—located on her left inframammary chest—is dark brown, macular, oval to round, and measures about 3.8 cm. On her trunk, arms, and lower neck, 15 to 20 oval, papulosquamous lesions are seen; these are widely scattered, all hyperpigmented (brown), and average 1.5 cm in diameter. Several of these smaller lesions have scaly centers that spare the peripheral margins. The long axes of her oval back lesions are parallel with natural lines of cleavage in the skin.
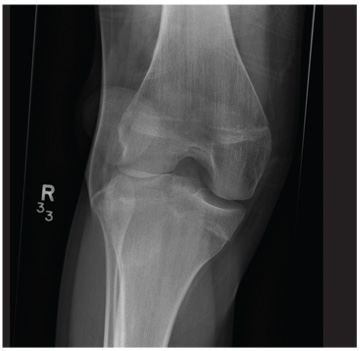
Chest Wall and Knee Pain Following Motor Vehicle Collision
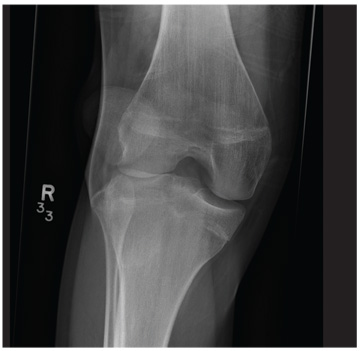
A 20-year-old man presents following a motor vehicle collision in which the car he was driving was broadsided by another vehicle. His air bag deployed, and the patient is now complaining of right-sided chest wall pain and right knee pain. His medical history is unremarkable. In a primary survey, the patient appears stable, with normal vital signs. Inspection of his right knee shows some deformity of the joint, with mild swelling and moderate tenderness. The patient is unable to perform flexion with his right knee. Good distal pulses are present, and sensation is intact. Radiograph of the right knee is obtained. What is your impression?
Man Waits Until Follow-up to Reveal Chest Pain
ANSWER
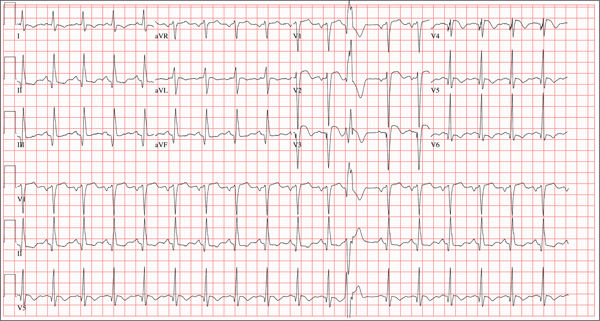
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
ANSWER
The correct interpretation includes marked sinus bradycardia with a first-degree atrioventricular (AV) block, left anterior fascicular block, and evidence of an anteroseptal MI. Marked sinus bradycardia is evidenced by a heart rate significantly less than 60 beats/min (in this case, almost half the rate). A first-degree AV block is apparent by the presence of a PR interval > 200 ms. The presence of a left anterior fascicular block (or left anterior hemiblock) includes a left-axis deviation between –45° and –90°, small Q waves with tall R waves in leads I and aVL, small R waves with deep S waves in leads II, III, and aVF, and a normal or slightly prolonged QRS duration. Finally, an anteroseptal MI is evident from the presence of deep S waves in leads V1 to V3.
The patient was directly admitted to the cardiology service for definitive workup and treatment.
A 64-year-old man presents for follow-up to an appointment one month ago in which he reported a history of acute-onset shortness of breath, fatigue, and exercise intolerance. His health prior to that visit was described as “normal”; he had not seen a clinician since having his tonsils out at age 14. At the previous visit, a complete history documented that the patient is a rancher and farmer who makes his living from his crops and animals. He has never been married and lives out in the country. He has a history of several broken bones that he set himself, with no resultant sequelae. Aside from routine colds and flu, he has not been ill. He stopped smoking 10 years ago when it “got to be too expensive,” and he drinks one shot of whiskey at bedtime each night. He denies any drug allergies; he was taking no medications when he presented for that visit. A physical examination during that appointment revealed the presence of an irregularly irregular rhythm with a ventricular rate of 120 beats/min, a grade II/VI decrescendo diastolic murmur best heard at the right upper sternal border, a grade II/VI mid-systolic murmur best heard at the apex, a large point of maximum impulse (PMI) palpable at the anterior axillary line, and 3+ pitting edema to the level of the knees in both lower extremities. Subsequent workup, including an ECG, echocardiogram, chest x-ray, complete blood count, and chemistry panel, was performed—much to the patient’s displeasure. Pertinent results included a diagnosis of atrial fibrillation, a bicuspid aortic valve, aortic insufficiency, and mitral regurgitation. He was prescribed metoprolol and warfarin and referred to a cardiologist. During the current visit, you learn that he did not continue to take his warfarin, because his shortness of breath went away the day after the previous appointment. He states he doesn’t always remember to take his metoprolol, but when he does, he’ll often take enough to “catch up on” his dosage. He did not follow up with a cardiologist as scheduled. Additionally, he reveals that he experienced chest pain two weeks ago, which he describes as a “sharp, sticking” pain in his left chest. He did not come in because he thought he’d wait until this appointment to discuss it. He remembers being “all sweaty” when he had his chest pain, but adds that it hasn’t happened again. His review of symptoms is remarkable for fatigue since his chest pain. Physical exam reveals cardiac changes. His rhythm is now regular, but at a rate of 40 beats/min. His murmurs are unchanged from the previous visit. Another ECG is obtained, which reveals the following: a ventricular rate of 35 beats/min; PR interval, 258 ms; QRS duration, 116 ms; QT/QTc interval, 532/406 ms; P axis, 74°; R axis, –47°; and T axis, 45°. What is your interpretation of this ECG?
Why This Child Hates to Put On Socks
ANSWER
The correct answer is juvenile plantar dermatosis (JPD; choice “b”). It is a condition related to having thin, dry, hyperreactive skin exposed to friction, wetting and drying, and constant exposure to the nonpermeable surfaces of shoes.
Pitted keratolysis (choice “a”) is a condition caused by sweating and increased warmth. The plantar keratin is broken down with the help of bacteria that overgrow in affected areas; this eventuates in focal loss of keratin in arcuate patterns. It is quite unlikely to occur prior to puberty.
Tinea pedis (choice “c”) is dermatophytosis, or fungal infection of the foot. It is also unusual prior to puberty, unlikely to present in the manner seen in this case, and likely to have responded at least partially to antifungal creams.
Psoriasis (choice “d”) seldom presents with fissuring, would not be confined to weight-bearing surfaces, and would probably have involved other areas, such as the scalp, elbows, knees, or nails.
DISCUSSION
JPD, also known as juvenile plantar dermatitis, is found almost exclusively on the weight-bearing surfaces of the feet of children ages 4 to 8—mostly boys, for whom this represents a manifestation of the atopic diathesis. Seen mostly in the summer, it is thought to be triggered by friction, wetting and drying, and shoe selection (ie, plastic rather than leather soles).
Affected children not only have dry, sensitive skin; their skin is actually thin and fragile as well. Plastic or other synthetic shoe surfaces worn in the summertime are thought to contribute to the friction, heat, and sweating necessary to produce these changes.
As in this case, JPD is often mistaken for tinea pedis but has nothing to do with infection of any kind. Tinea pedis is uncommon in children this young, and it would present in completely different ways, such as between the toes (especially the fourth and fifth) or with blisters on the instep.
Psoriasis, though not unknown in this age-group, does not resemble JPD clinically at all. When suspected, the diagnosis of psoriasis can be corroborated by finding it elsewhere (eg, through a positive family history or biopsy).
Pitted keratolyis is common enough, but is seen in older teens and men whose feet are prone to sweat a great deal. The choice of shoes and occupation are often crucial factors in its development. The clinical hallmark is arcuate whitish maceration on weight-bearing surfaces, which are often malodorous as well.
TREATMENT
The first treatment for JPD is education of parents and patients, reassuring them about the relatively benign nature of the problem. Moisturizing frequently with petrolatum-based moisturizers is necessary for prevention, but changing the type of shoes worn is the most effective step to take; it is also the most difficult, since children this age favor cheap, plastic flip-flops or shoes in the summer.
For the fissures, spraying on a flexible spray bandage can be helpful in protecting them and allowing them to heal. With significant inflammation, the use of mild steroid ointments, such as hydrocortisone 2.5%, can help. But by far, the best relief comes with the change in season and the choice of shoe (leather-soled).
ANSWER
The correct answer is juvenile plantar dermatosis (JPD; choice “b”). It is a condition related to having thin, dry, hyperreactive skin exposed to friction, wetting and drying, and constant exposure to the nonpermeable surfaces of shoes.
Pitted keratolysis (choice “a”) is a condition caused by sweating and increased warmth. The plantar keratin is broken down with the help of bacteria that overgrow in affected areas; this eventuates in focal loss of keratin in arcuate patterns. It is quite unlikely to occur prior to puberty.
Tinea pedis (choice “c”) is dermatophytosis, or fungal infection of the foot. It is also unusual prior to puberty, unlikely to present in the manner seen in this case, and likely to have responded at least partially to antifungal creams.
Psoriasis (choice “d”) seldom presents with fissuring, would not be confined to weight-bearing surfaces, and would probably have involved other areas, such as the scalp, elbows, knees, or nails.
DISCUSSION
JPD, also known as juvenile plantar dermatitis, is found almost exclusively on the weight-bearing surfaces of the feet of children ages 4 to 8—mostly boys, for whom this represents a manifestation of the atopic diathesis. Seen mostly in the summer, it is thought to be triggered by friction, wetting and drying, and shoe selection (ie, plastic rather than leather soles).
Affected children not only have dry, sensitive skin; their skin is actually thin and fragile as well. Plastic or other synthetic shoe surfaces worn in the summertime are thought to contribute to the friction, heat, and sweating necessary to produce these changes.
As in this case, JPD is often mistaken for tinea pedis but has nothing to do with infection of any kind. Tinea pedis is uncommon in children this young, and it would present in completely different ways, such as between the toes (especially the fourth and fifth) or with blisters on the instep.
Psoriasis, though not unknown in this age-group, does not resemble JPD clinically at all. When suspected, the diagnosis of psoriasis can be corroborated by finding it elsewhere (eg, through a positive family history or biopsy).
Pitted keratolyis is common enough, but is seen in older teens and men whose feet are prone to sweat a great deal. The choice of shoes and occupation are often crucial factors in its development. The clinical hallmark is arcuate whitish maceration on weight-bearing surfaces, which are often malodorous as well.
TREATMENT
The first treatment for JPD is education of parents and patients, reassuring them about the relatively benign nature of the problem. Moisturizing frequently with petrolatum-based moisturizers is necessary for prevention, but changing the type of shoes worn is the most effective step to take; it is also the most difficult, since children this age favor cheap, plastic flip-flops or shoes in the summer.
For the fissures, spraying on a flexible spray bandage can be helpful in protecting them and allowing them to heal. With significant inflammation, the use of mild steroid ointments, such as hydrocortisone 2.5%, can help. But by far, the best relief comes with the change in season and the choice of shoe (leather-soled).
ANSWER
The correct answer is juvenile plantar dermatosis (JPD; choice “b”). It is a condition related to having thin, dry, hyperreactive skin exposed to friction, wetting and drying, and constant exposure to the nonpermeable surfaces of shoes.
Pitted keratolysis (choice “a”) is a condition caused by sweating and increased warmth. The plantar keratin is broken down with the help of bacteria that overgrow in affected areas; this eventuates in focal loss of keratin in arcuate patterns. It is quite unlikely to occur prior to puberty.
Tinea pedis (choice “c”) is dermatophytosis, or fungal infection of the foot. It is also unusual prior to puberty, unlikely to present in the manner seen in this case, and likely to have responded at least partially to antifungal creams.
Psoriasis (choice “d”) seldom presents with fissuring, would not be confined to weight-bearing surfaces, and would probably have involved other areas, such as the scalp, elbows, knees, or nails.
DISCUSSION
JPD, also known as juvenile plantar dermatitis, is found almost exclusively on the weight-bearing surfaces of the feet of children ages 4 to 8—mostly boys, for whom this represents a manifestation of the atopic diathesis. Seen mostly in the summer, it is thought to be triggered by friction, wetting and drying, and shoe selection (ie, plastic rather than leather soles).
Affected children not only have dry, sensitive skin; their skin is actually thin and fragile as well. Plastic or other synthetic shoe surfaces worn in the summertime are thought to contribute to the friction, heat, and sweating necessary to produce these changes.
As in this case, JPD is often mistaken for tinea pedis but has nothing to do with infection of any kind. Tinea pedis is uncommon in children this young, and it would present in completely different ways, such as between the toes (especially the fourth and fifth) or with blisters on the instep.
Psoriasis, though not unknown in this age-group, does not resemble JPD clinically at all. When suspected, the diagnosis of psoriasis can be corroborated by finding it elsewhere (eg, through a positive family history or biopsy).
Pitted keratolyis is common enough, but is seen in older teens and men whose feet are prone to sweat a great deal. The choice of shoes and occupation are often crucial factors in its development. The clinical hallmark is arcuate whitish maceration on weight-bearing surfaces, which are often malodorous as well.
TREATMENT
The first treatment for JPD is education of parents and patients, reassuring them about the relatively benign nature of the problem. Moisturizing frequently with petrolatum-based moisturizers is necessary for prevention, but changing the type of shoes worn is the most effective step to take; it is also the most difficult, since children this age favor cheap, plastic flip-flops or shoes in the summer.
For the fissures, spraying on a flexible spray bandage can be helpful in protecting them and allowing them to heal. With significant inflammation, the use of mild steroid ointments, such as hydrocortisone 2.5%, can help. But by far, the best relief comes with the change in season and the choice of shoe (leather-soled).

The distraught mother of an 8-year-old boy brings him urgently to dermatology for evaluation of a condition that has affected his feet for the past two summers. Convinced he has “caught” athlete’s foot, she tried several OTC antifungal creams and sprays, with no good effect. The patient denies symptoms except occasional stinging. In his view, the biggest problem is that the bottoms of his feet are so rough that he hates to put on socks. Additional history taking reveals that the child is markedly atopic, with seasonal allergies, asthma, dry, sensitive skin, and eczema. As an infant, his diaper rashes were so severe that he was hospitalized twice. On inspection, the weight-bearing surfaces of both feet are fissured and shiny, with modest inflammation evident. The plantar aspects of both big toes are especially affected. Though these areas are rough and dry, there is no edema, increased warmth, or tenderness on palpation. His skin elsewhere, though dry, is free of obvious lesions.
Underlying Factors Influence Insulin's Effect
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Q: Help! How do you proceed if, after you’ve continually increased a patient’s insulin dose, his/her blood glucose levels do not improve?
This is a common scenario in diabetes management. Here are nine things to consider when a patient’s situation just doesn’t make sense clinically:
1. Noncompliance with the prescribed dose. This is the most common scenario. Ask the patient, “How many injections do you miss in a typical week?” Assure that he or she is actually taking the currently prescribed amount of insulin before you further increase the dose.
2. Inaccurate insulin dosing. This problem can be due to impaired vision, poor technique, dexterity issues, or dementia. Ask the patient to demonstrate for you how he/she draws up and takes the insulin at home. You might just be surprised at what you see, even in patients who have been giving themselves insulin for years. Consider prescribing an insulin pen or having a family member or significant other dose the insulin if the patient is no longer reliable to accurately dose it for him- or herself.
3. “Bad insulin.” What this actually means is loss of potency. This can be caused by improper storage, exposure to heat or cold, or use of an insulin delivery device (ie, vial or pen) past the 28- to 45-day period recommended, depending on the type of insulin. Replace the vial or pen and re-assess for improvement in diabetes control.
4. Lipohypertrophy of injection sites due to overuse. Palpate and visually inspect injection sites to look for firm or hypertrophied tissue. Advise the patient to avoid these areas for future injection, as absorption from these sites can be poor and unpredictable.
5. Dietary issues. The patient may be increasing his/her food intake along with the increased insulin doses. One clue that should raise suspicion for this occurrence is rapidly increasing body weight. Consider referring the patient to a dietitian for nutrition counseling.
6. New medication. Sometimes a new treatment is added to a patient’s regimen by another provider, and the medication might have an adverse effect on blood glucose control. Common examples include steroids (typically a cortisone injection) or methylprednisolone dose-packs taken during an asthma flare.
7. Occult infection. Urinary tract infections, pneumonia, and the like can impact blood glucose control. Consider ordering a urinalysis and complete blood count if infection seems a likely cause.
8. Major life stressors. Inquire as to what is happening in the patient’s life that might impact his/her body’s response to insulin. They might be in the middle of a divorce or other family crisis or experiencing severe stress at work.
9. Technique and equipment issues. Inaccurate glucose monitoring technique or use of expired strips can lead to “false high” readings. Also, patients with a continuous glucose monitor may record false high results when they are taking acetaminophen. If this is the case, increasing the insulin dose will often result in hypoglycemia.
It may be helpful to keep this clinical checklist handy and add to it any other issues that you come across when the clinical picture doesn’t make sense. You may also want to consider referral to a diabetes educator; patients will often confide what is really going on to an educator in a longer visit, rather than in the typically shorter visits with their health care provider.
SUGGESTED READING
Sadler C, Einhorn D. Tailoring insulin regimens for type 2 diabetes mellitus. JAAPA. 1998;11(4):55-71.
Is Chest Pain Related to Prior Fracture?
ANSWER
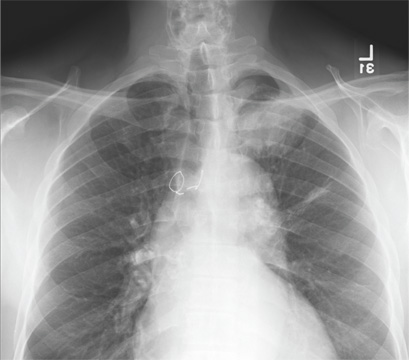
The radiograph demonstrates evidence of previous surgery on the sternum. There also is evidence of scarring or discoid atelectasis along the left mid lung.
Of note, though, is a soft tissue mass (about 5 to 6 cm) within the left pulmonary apex. This lesion could represent a rounded infiltrate, an atypical infection such as a mycetoma, or possibly a pulmonary neoplasm.
Since the patient was stable, he was placed on antibiotics with instructions to follow up with his primary care provider for further work-up on the mass. The patient did follow up; the lesion persisted and subsequent biopsy confirmed carcinoma.
ANSWER
The radiograph demonstrates evidence of previous surgery on the sternum. There also is evidence of scarring or discoid atelectasis along the left mid lung.
Of note, though, is a soft tissue mass (about 5 to 6 cm) within the left pulmonary apex. This lesion could represent a rounded infiltrate, an atypical infection such as a mycetoma, or possibly a pulmonary neoplasm.
Since the patient was stable, he was placed on antibiotics with instructions to follow up with his primary care provider for further work-up on the mass. The patient did follow up; the lesion persisted and subsequent biopsy confirmed carcinoma.
ANSWER
The radiograph demonstrates evidence of previous surgery on the sternum. There also is evidence of scarring or discoid atelectasis along the left mid lung.
Of note, though, is a soft tissue mass (about 5 to 6 cm) within the left pulmonary apex. This lesion could represent a rounded infiltrate, an atypical infection such as a mycetoma, or possibly a pulmonary neoplasm.
Since the patient was stable, he was placed on antibiotics with instructions to follow up with his primary care provider for further work-up on the mass. The patient did follow up; the lesion persisted and subsequent biopsy confirmed carcinoma.
A 61-year-old man presents to your urgent care center for evaluation of “chest pain” he has been experiencing for almost four weeks. He denies any injury or trauma. He describes the pain as “sharp” and “stabbing” and says occasionally it is associated with breathing, localized primarily to the left side. There is no radiation of the pain. He denies fever, nausea, weight loss, night sweats, and hemoptysis. He has smoked a half-pack of cigarettes daily for more than 40 years. His medical history is otherwise unremarkable, except that he was told he had “high blood pressure” and he had his sternum repaired several years ago, following fracture in an accident. Vital signs are as follows: temperature, 36.4°C; blood pressure, 174/100 mm Hg; ventricular rate, 88 beats/min; respiratory rate, 20 breaths/min; and O2 saturation, 100% on room air. He appears to be in no obvious distress. Lung sounds are normal, as is the rest of the physical examination. You obtain a chest radiograph. What is your impression?