User login
Measures of Success
The headlines are harrowing: corporate layoffs; foreclosures on the rise; 401(k) retirement plans halved; government bailouts adding to the national debt. The worst economic downturn since the Great Depression has generated some unexpected outcomes, yet not all of them are bad for hospitalists. Below, four vignettes highlight HM groups that have achieved success despite—or in some cases because of—these troubled times.
A Better Business Agreement
It has taken nearly two years—and sometimes as many as four meetings a week—but Rajeev Alexander, MD, and his colleagues are nearing the finish line of an evolving business arrangement. The new arrangement has come about due to the economic downturn, which forced Oregon Medical Group (OMG), a multispecialty physician group serving hospitals in the Eugene/Springfield area and the HM group’s employer since 1988, to want to divest themselves of the hospitalist group. Now, after a lengthy negotiation, Dr. Alexander’s group of eight hospitalists is busier than ever.
Through what were essentially multiple quasi-buyouts, divestitures, and mergers, Dr. Alexander’s hospitalist group “spun off” from OMG and affiliated with PeaceHealth, a nonprofit health system serving seven hospitals in Oregon, Washington, and Alaska. The new contract means Dr. Alexander’s group is directly employed by Sacred Heart Hospital, a 541-bed PeaceHealth-owned facility in Eugene.
The new contract included a non-compete clause with OMG, which currently employs five hospitalists, yet Dr. Alexander’s group has maintained its patient volume. Compensation held steady and employee benefits improved. During an independent and slow-moving negotiation, Dr. Alexander’s group has merged with another HM service that originally was employed by PeaceHealth. The two HM groups (technically competitors) now practice in the same hospital and are ironing out the terms of the merger. At the moment, the groups have created a mutually respectful joint governance council.
“We’ve tackled the thorniest of problems,” Dr. Alexander says, “first, creating a combined work schedule to distribute patients and divide the work. Those of us on the governance council figured if we could get the docs to actually work together and share patients and communicate with each other as if they were one group, then the momentum for an actual administrative/contractual merger would feel inevitable.”
Although negotiations are expected to last through the end of the year to finalize such details as compensation, recruiting, and a group mission statement, the medical staff at Sacred Heart considers the merger a “done deal” and has thrown its support behind the effort. “Community outpatient docs have been clamoring for our services, and we have been having to hand out numbers and ask them to wait in line, so to speak,” Dr. Alexander says.
Dr. Alexander says he’s learned some lessons through the extensive negotiation process:
- Stay positive. In any business venture, absolutely nothing is impossible, even dodging a noncompete clause.
- Release your preconceptions. Conspiracy theories might abound, but most hospital administrators have the best of intentions. As highly regulated organizations, hospitals might simply be following their own bylaws and fulfilling responsibilities to stakeholders. Seek out at least one administrator whom you can trust, and with whom you can communicate effectively. A mutual understanding of intentions and objectives makes the process more successful for all concerned.
- Look beyond politics. Your trust and respect for administrators and fellow physicians will go a long way toward overcoming obstacles.
- Stick to your plan. Adhere to your goal of remaining independent, if that is important to you. “Our group resisted being funneled into becoming employed by a very large national hospitalist chain,” Dr. Alexander says, “and I would encourage physicians in other parts of the country to stick to their commitments as well.”
- Trust the negotiation process. Even if all goes well, what you’re shooting for at the beginning might not be exactly what you get after negotiations are over. This does not mean you’ve failed, or that hospital administration tricked you or failed to deliver on promises. It simply means you have created a negotiated settlement; both sides have come to a new appreciation for the other’s requirements and have made necessary and respectful accommodations.
Rural Rewards
Based in Traverse City, Hospitalists of Northwest Michigan (HNM) services four community hospitals and continues to witness solid growth. Since 2000, the group has grown from nine to nearly 40 providers, and from 2005 to 2008, patient encounters doubled. “In these hard economic times, hospitals are inviting us in because we provide value to the hospitals through leadership, increased hospital revenues, and improved recruiting and retention of specialists,” says Troy W. Ahlstrom, MD, president of HNM. “We continue to see healthy growth in patient volume as we align patient care goals with the needs of the hospitals and surrounding communities we serve.”
HNM, which established a service at the regional medical center and then assumed management of HM programs at three other rural hospitals, soon will add a fifth service to its ledger. HNM also began a pediatric program at the regional referral center, and the group is exploring the possibility of providing a network of pediatric care throughout the region.
Having grown up in the region, David Friar, MD, CEO of HNM, not only has a better understanding of the needs of rural hospitals, but also a personal investment in his group’s success. “These are our communities. We don’t view the hospitals as just a place to make a profit, but a place where our neighbors work and our families get their care,” he says.
Drs. Ahlstrom and Friar offer the following advice for achieving success in these economic times:
- Optimize receipts. Concern over compliance audits leads many hospitals to sacrifice group receipts by encouraging undercoding. “We’ve found hospitals do a poor job of negotiating the provider portion of third-party payer contracts and frequently lose provider charges because they focus on the much larger facility fees,” says Dr. Ahlstrom. The group’s receipts increased more than 30% when they began using an outside billing firm and adopted productivity incentives to encourage providers to practice better documentation and charge capture. Improving documentation also supports a hospital’s ability to accurately code its patients, which allows a hospital to bill for a more profitable diagnosis-related group (DRG), and improve its case-mix index. With these changes, Hospitalists of Northwest Michigan has increased provider pay and grown their practice while improving the hospitals’ profitability.
- Encourage frugality. The cost-plus model is popular, but it doesn’t incentivize programs to contain costs. In contrast, the fixed-price model encourages hospitalists to find cheaper ways to provide good care. “Because the money we save goes to us, we’ve all found creative ways to provide quality care for a third less money than similar cost-plus programs,” Dr. Ahlstrom says.
- Align incentives. Hospitals live or die on thin margins, Dr. Ahlstrom says. His group trains its employees to ask: What can I do to make the hospital stronger? “What’s good for the hospital is good for us, so we work with the hospitals, not for the hospitals,” Dr. Friar says.
At its smaller hospitals, HNM incentivized orthopedic admissions so that more surgical cases would stay local. Hospitalists were trained to perform stress tests so the hospital can provide testing on weekends. The group pays hospitalists a bonus for each admission, so when the ED calls, the hospitalists say, “Thanks! I’ll be right there.” The group also increased staffing on weekends.
The end result: It improves the hospital’s bottom line by shortening length of stay, and improving quality of care, patient satisfaction, and group morale.
“When we align the incentives, everybody wins,” says Dr. Friar. “The system has more capacity, the patients get better care, and the hospitalists no longer feel that weekend shifts are a huge burden.”
- Build “system-ness.” Sharing providers between hospitals has helped HNM build a cohesive system of quality care. What began as a way to cover shifts has created an interinstitutional camaraderie that allows for the easier flow of patients, improved communication, and widespread use of best-practice models. Sharing such resources as billing, credentialing, benefits, recruiting, and payroll has helped the group stay competitive, Dr. Ahlstrom says.
Growth in a Down Economy
Jude R. Alexander, MD, president of Inpatient Specialists in Rockville, Md., a bedroom community about 12 miles northwest of Washington, D.C., has continued to grow his group despite the down economy. Hospital admissions in the D.C. area decreased sharply in the second half of 2008, and patient volume rebounded slowly in the first half of 2009.
Inpatient Specialists initially downsized its staff, then it used flex physicians to meet demand as volume increased.
Despite national hospital trends of budget shortfalls, downgraded bond ratings, and increases in uninsured patients, two of Inpatient Specialists’ client hospitals chose to invest in the HM program. Dr. Alexander credits the vote of confidence to his group’s track record of optimal resource utilization, which has inherent cost savings in the millions.
Dr. Alexander also recommends HM groups in tough economic circumstances should:
- Maintain good relationships with partner hospitals;
- Run a lean business;
- Focus on excellent customer service to patients, their families, and their PCPs; and
- Build strong alliances with employed physicians by eliciting and giving constructive feedback.
“Following this basic strategy, Inpatient Specialists has experienced 7% growth in patient volume in the past 12 months,” Dr. Alexander says. “We’ve expanded to 40 full-time equivalent hospitalists, and 40 part-time employees.” Inpatient Specialists has its eye on geographic expansion, as well. The group is targeting services throughout the Capitol region—Maryland, Virginia, and the District of Columbia.
Bankruptcy to Profitability in One Year
In 2007, a few months after the 99-bed Auburn Memorial Hospital in Auburn, N.Y., was forced into bankruptcy, James Leyhane, MD, and his hospitalist group were displeased that they weren’t in control of their own program. Physicians had started leaving the hospital; Dr. Leyhane himself had interviewed at another hospital. “Our CEO approached me to ask what would make it right,” Dr. Leyhane recalls. “I said, ‘We’d need to be employed by the hospital.’ ”
The hospital and the private, six-physician internal-medicine group that employed the program entered bids on the HM group. In March 2008, the HM group became contractually employed by the hospital. Dr. Leyhane was given full control as hospitalist director of Auburn Memorial Hospitalists.
As a result of the new alignment, two major shifts took place. First, the hospital CEO more aggressively recruited subspecialists and surgeons. With the HM group now affiliated with the hospital, recruiting surgeons to Auburn Memorial became much easier. Second, more primary-care physicians (PCPs) began sending their patients to Auburn Memorial.
“We were all shocked at how quickly the administration was able to recruit new subspecialists to the area,” Dr. Leyhane says. “That helped get the profitable procedures back to the hospital.”
The biggest surprise came at the end of 2008. Patient volume had risen 11.5% higher than the hospital’s best-case predictions. “As a result of our emerging from under the umbrella of one physician group, the outlying physicians became less fearful that they might lose their patients to that group,” Dr. Leyhane says. “And in good faith, we still maintain a coverage arrangement with that IM group.”
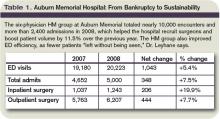
Thus, what was first seen as a bad thing turned into a very good thing for both the hospitalist group and the hospital. Auburn Memorial posted a $3.1 million profit in 2008 (see Table 1).
Dr. Leyhane suggests HM group leaders facing similar financial crunches talk to area subspecialists and find out what it would take to get them affiliated with their institution.
“In our case, a stable hospitalist program was definitely one of their top requests,” Dr. Leyhane says, adding it also would be beneficial to include PCPs in the “what do you want from our hospital?” conversation. TH
Andrea M. Sattinger is a freelance writer based in North Carolina.
Image Source: COLIN ANDERSON/GETTYIMAGES
The headlines are harrowing: corporate layoffs; foreclosures on the rise; 401(k) retirement plans halved; government bailouts adding to the national debt. The worst economic downturn since the Great Depression has generated some unexpected outcomes, yet not all of them are bad for hospitalists. Below, four vignettes highlight HM groups that have achieved success despite—or in some cases because of—these troubled times.
A Better Business Agreement
It has taken nearly two years—and sometimes as many as four meetings a week—but Rajeev Alexander, MD, and his colleagues are nearing the finish line of an evolving business arrangement. The new arrangement has come about due to the economic downturn, which forced Oregon Medical Group (OMG), a multispecialty physician group serving hospitals in the Eugene/Springfield area and the HM group’s employer since 1988, to want to divest themselves of the hospitalist group. Now, after a lengthy negotiation, Dr. Alexander’s group of eight hospitalists is busier than ever.
Through what were essentially multiple quasi-buyouts, divestitures, and mergers, Dr. Alexander’s hospitalist group “spun off” from OMG and affiliated with PeaceHealth, a nonprofit health system serving seven hospitals in Oregon, Washington, and Alaska. The new contract means Dr. Alexander’s group is directly employed by Sacred Heart Hospital, a 541-bed PeaceHealth-owned facility in Eugene.
The new contract included a non-compete clause with OMG, which currently employs five hospitalists, yet Dr. Alexander’s group has maintained its patient volume. Compensation held steady and employee benefits improved. During an independent and slow-moving negotiation, Dr. Alexander’s group has merged with another HM service that originally was employed by PeaceHealth. The two HM groups (technically competitors) now practice in the same hospital and are ironing out the terms of the merger. At the moment, the groups have created a mutually respectful joint governance council.
“We’ve tackled the thorniest of problems,” Dr. Alexander says, “first, creating a combined work schedule to distribute patients and divide the work. Those of us on the governance council figured if we could get the docs to actually work together and share patients and communicate with each other as if they were one group, then the momentum for an actual administrative/contractual merger would feel inevitable.”
Although negotiations are expected to last through the end of the year to finalize such details as compensation, recruiting, and a group mission statement, the medical staff at Sacred Heart considers the merger a “done deal” and has thrown its support behind the effort. “Community outpatient docs have been clamoring for our services, and we have been having to hand out numbers and ask them to wait in line, so to speak,” Dr. Alexander says.
Dr. Alexander says he’s learned some lessons through the extensive negotiation process:
- Stay positive. In any business venture, absolutely nothing is impossible, even dodging a noncompete clause.
- Release your preconceptions. Conspiracy theories might abound, but most hospital administrators have the best of intentions. As highly regulated organizations, hospitals might simply be following their own bylaws and fulfilling responsibilities to stakeholders. Seek out at least one administrator whom you can trust, and with whom you can communicate effectively. A mutual understanding of intentions and objectives makes the process more successful for all concerned.
- Look beyond politics. Your trust and respect for administrators and fellow physicians will go a long way toward overcoming obstacles.
- Stick to your plan. Adhere to your goal of remaining independent, if that is important to you. “Our group resisted being funneled into becoming employed by a very large national hospitalist chain,” Dr. Alexander says, “and I would encourage physicians in other parts of the country to stick to their commitments as well.”
- Trust the negotiation process. Even if all goes well, what you’re shooting for at the beginning might not be exactly what you get after negotiations are over. This does not mean you’ve failed, or that hospital administration tricked you or failed to deliver on promises. It simply means you have created a negotiated settlement; both sides have come to a new appreciation for the other’s requirements and have made necessary and respectful accommodations.
Rural Rewards
Based in Traverse City, Hospitalists of Northwest Michigan (HNM) services four community hospitals and continues to witness solid growth. Since 2000, the group has grown from nine to nearly 40 providers, and from 2005 to 2008, patient encounters doubled. “In these hard economic times, hospitals are inviting us in because we provide value to the hospitals through leadership, increased hospital revenues, and improved recruiting and retention of specialists,” says Troy W. Ahlstrom, MD, president of HNM. “We continue to see healthy growth in patient volume as we align patient care goals with the needs of the hospitals and surrounding communities we serve.”
HNM, which established a service at the regional medical center and then assumed management of HM programs at three other rural hospitals, soon will add a fifth service to its ledger. HNM also began a pediatric program at the regional referral center, and the group is exploring the possibility of providing a network of pediatric care throughout the region.
Having grown up in the region, David Friar, MD, CEO of HNM, not only has a better understanding of the needs of rural hospitals, but also a personal investment in his group’s success. “These are our communities. We don’t view the hospitals as just a place to make a profit, but a place where our neighbors work and our families get their care,” he says.
Drs. Ahlstrom and Friar offer the following advice for achieving success in these economic times:
- Optimize receipts. Concern over compliance audits leads many hospitals to sacrifice group receipts by encouraging undercoding. “We’ve found hospitals do a poor job of negotiating the provider portion of third-party payer contracts and frequently lose provider charges because they focus on the much larger facility fees,” says Dr. Ahlstrom. The group’s receipts increased more than 30% when they began using an outside billing firm and adopted productivity incentives to encourage providers to practice better documentation and charge capture. Improving documentation also supports a hospital’s ability to accurately code its patients, which allows a hospital to bill for a more profitable diagnosis-related group (DRG), and improve its case-mix index. With these changes, Hospitalists of Northwest Michigan has increased provider pay and grown their practice while improving the hospitals’ profitability.
- Encourage frugality. The cost-plus model is popular, but it doesn’t incentivize programs to contain costs. In contrast, the fixed-price model encourages hospitalists to find cheaper ways to provide good care. “Because the money we save goes to us, we’ve all found creative ways to provide quality care for a third less money than similar cost-plus programs,” Dr. Ahlstrom says.
- Align incentives. Hospitals live or die on thin margins, Dr. Ahlstrom says. His group trains its employees to ask: What can I do to make the hospital stronger? “What’s good for the hospital is good for us, so we work with the hospitals, not for the hospitals,” Dr. Friar says.
At its smaller hospitals, HNM incentivized orthopedic admissions so that more surgical cases would stay local. Hospitalists were trained to perform stress tests so the hospital can provide testing on weekends. The group pays hospitalists a bonus for each admission, so when the ED calls, the hospitalists say, “Thanks! I’ll be right there.” The group also increased staffing on weekends.
The end result: It improves the hospital’s bottom line by shortening length of stay, and improving quality of care, patient satisfaction, and group morale.
“When we align the incentives, everybody wins,” says Dr. Friar. “The system has more capacity, the patients get better care, and the hospitalists no longer feel that weekend shifts are a huge burden.”
- Build “system-ness.” Sharing providers between hospitals has helped HNM build a cohesive system of quality care. What began as a way to cover shifts has created an interinstitutional camaraderie that allows for the easier flow of patients, improved communication, and widespread use of best-practice models. Sharing such resources as billing, credentialing, benefits, recruiting, and payroll has helped the group stay competitive, Dr. Ahlstrom says.
Growth in a Down Economy
Jude R. Alexander, MD, president of Inpatient Specialists in Rockville, Md., a bedroom community about 12 miles northwest of Washington, D.C., has continued to grow his group despite the down economy. Hospital admissions in the D.C. area decreased sharply in the second half of 2008, and patient volume rebounded slowly in the first half of 2009.
Inpatient Specialists initially downsized its staff, then it used flex physicians to meet demand as volume increased.
Despite national hospital trends of budget shortfalls, downgraded bond ratings, and increases in uninsured patients, two of Inpatient Specialists’ client hospitals chose to invest in the HM program. Dr. Alexander credits the vote of confidence to his group’s track record of optimal resource utilization, which has inherent cost savings in the millions.
Dr. Alexander also recommends HM groups in tough economic circumstances should:
- Maintain good relationships with partner hospitals;
- Run a lean business;
- Focus on excellent customer service to patients, their families, and their PCPs; and
- Build strong alliances with employed physicians by eliciting and giving constructive feedback.
“Following this basic strategy, Inpatient Specialists has experienced 7% growth in patient volume in the past 12 months,” Dr. Alexander says. “We’ve expanded to 40 full-time equivalent hospitalists, and 40 part-time employees.” Inpatient Specialists has its eye on geographic expansion, as well. The group is targeting services throughout the Capitol region—Maryland, Virginia, and the District of Columbia.
Bankruptcy to Profitability in One Year
In 2007, a few months after the 99-bed Auburn Memorial Hospital in Auburn, N.Y., was forced into bankruptcy, James Leyhane, MD, and his hospitalist group were displeased that they weren’t in control of their own program. Physicians had started leaving the hospital; Dr. Leyhane himself had interviewed at another hospital. “Our CEO approached me to ask what would make it right,” Dr. Leyhane recalls. “I said, ‘We’d need to be employed by the hospital.’ ”
The hospital and the private, six-physician internal-medicine group that employed the program entered bids on the HM group. In March 2008, the HM group became contractually employed by the hospital. Dr. Leyhane was given full control as hospitalist director of Auburn Memorial Hospitalists.
As a result of the new alignment, two major shifts took place. First, the hospital CEO more aggressively recruited subspecialists and surgeons. With the HM group now affiliated with the hospital, recruiting surgeons to Auburn Memorial became much easier. Second, more primary-care physicians (PCPs) began sending their patients to Auburn Memorial.
“We were all shocked at how quickly the administration was able to recruit new subspecialists to the area,” Dr. Leyhane says. “That helped get the profitable procedures back to the hospital.”
The biggest surprise came at the end of 2008. Patient volume had risen 11.5% higher than the hospital’s best-case predictions. “As a result of our emerging from under the umbrella of one physician group, the outlying physicians became less fearful that they might lose their patients to that group,” Dr. Leyhane says. “And in good faith, we still maintain a coverage arrangement with that IM group.”
Thus, what was first seen as a bad thing turned into a very good thing for both the hospitalist group and the hospital. Auburn Memorial posted a $3.1 million profit in 2008 (see Table 1).
Dr. Leyhane suggests HM group leaders facing similar financial crunches talk to area subspecialists and find out what it would take to get them affiliated with their institution.
“In our case, a stable hospitalist program was definitely one of their top requests,” Dr. Leyhane says, adding it also would be beneficial to include PCPs in the “what do you want from our hospital?” conversation. TH
Andrea M. Sattinger is a freelance writer based in North Carolina.
Image Source: COLIN ANDERSON/GETTYIMAGES
The headlines are harrowing: corporate layoffs; foreclosures on the rise; 401(k) retirement plans halved; government bailouts adding to the national debt. The worst economic downturn since the Great Depression has generated some unexpected outcomes, yet not all of them are bad for hospitalists. Below, four vignettes highlight HM groups that have achieved success despite—or in some cases because of—these troubled times.
A Better Business Agreement
It has taken nearly two years—and sometimes as many as four meetings a week—but Rajeev Alexander, MD, and his colleagues are nearing the finish line of an evolving business arrangement. The new arrangement has come about due to the economic downturn, which forced Oregon Medical Group (OMG), a multispecialty physician group serving hospitals in the Eugene/Springfield area and the HM group’s employer since 1988, to want to divest themselves of the hospitalist group. Now, after a lengthy negotiation, Dr. Alexander’s group of eight hospitalists is busier than ever.
Through what were essentially multiple quasi-buyouts, divestitures, and mergers, Dr. Alexander’s hospitalist group “spun off” from OMG and affiliated with PeaceHealth, a nonprofit health system serving seven hospitals in Oregon, Washington, and Alaska. The new contract means Dr. Alexander’s group is directly employed by Sacred Heart Hospital, a 541-bed PeaceHealth-owned facility in Eugene.
The new contract included a non-compete clause with OMG, which currently employs five hospitalists, yet Dr. Alexander’s group has maintained its patient volume. Compensation held steady and employee benefits improved. During an independent and slow-moving negotiation, Dr. Alexander’s group has merged with another HM service that originally was employed by PeaceHealth. The two HM groups (technically competitors) now practice in the same hospital and are ironing out the terms of the merger. At the moment, the groups have created a mutually respectful joint governance council.
“We’ve tackled the thorniest of problems,” Dr. Alexander says, “first, creating a combined work schedule to distribute patients and divide the work. Those of us on the governance council figured if we could get the docs to actually work together and share patients and communicate with each other as if they were one group, then the momentum for an actual administrative/contractual merger would feel inevitable.”
Although negotiations are expected to last through the end of the year to finalize such details as compensation, recruiting, and a group mission statement, the medical staff at Sacred Heart considers the merger a “done deal” and has thrown its support behind the effort. “Community outpatient docs have been clamoring for our services, and we have been having to hand out numbers and ask them to wait in line, so to speak,” Dr. Alexander says.
Dr. Alexander says he’s learned some lessons through the extensive negotiation process:
- Stay positive. In any business venture, absolutely nothing is impossible, even dodging a noncompete clause.
- Release your preconceptions. Conspiracy theories might abound, but most hospital administrators have the best of intentions. As highly regulated organizations, hospitals might simply be following their own bylaws and fulfilling responsibilities to stakeholders. Seek out at least one administrator whom you can trust, and with whom you can communicate effectively. A mutual understanding of intentions and objectives makes the process more successful for all concerned.
- Look beyond politics. Your trust and respect for administrators and fellow physicians will go a long way toward overcoming obstacles.
- Stick to your plan. Adhere to your goal of remaining independent, if that is important to you. “Our group resisted being funneled into becoming employed by a very large national hospitalist chain,” Dr. Alexander says, “and I would encourage physicians in other parts of the country to stick to their commitments as well.”
- Trust the negotiation process. Even if all goes well, what you’re shooting for at the beginning might not be exactly what you get after negotiations are over. This does not mean you’ve failed, or that hospital administration tricked you or failed to deliver on promises. It simply means you have created a negotiated settlement; both sides have come to a new appreciation for the other’s requirements and have made necessary and respectful accommodations.
Rural Rewards
Based in Traverse City, Hospitalists of Northwest Michigan (HNM) services four community hospitals and continues to witness solid growth. Since 2000, the group has grown from nine to nearly 40 providers, and from 2005 to 2008, patient encounters doubled. “In these hard economic times, hospitals are inviting us in because we provide value to the hospitals through leadership, increased hospital revenues, and improved recruiting and retention of specialists,” says Troy W. Ahlstrom, MD, president of HNM. “We continue to see healthy growth in patient volume as we align patient care goals with the needs of the hospitals and surrounding communities we serve.”
HNM, which established a service at the regional medical center and then assumed management of HM programs at three other rural hospitals, soon will add a fifth service to its ledger. HNM also began a pediatric program at the regional referral center, and the group is exploring the possibility of providing a network of pediatric care throughout the region.
Having grown up in the region, David Friar, MD, CEO of HNM, not only has a better understanding of the needs of rural hospitals, but also a personal investment in his group’s success. “These are our communities. We don’t view the hospitals as just a place to make a profit, but a place where our neighbors work and our families get their care,” he says.
Drs. Ahlstrom and Friar offer the following advice for achieving success in these economic times:
- Optimize receipts. Concern over compliance audits leads many hospitals to sacrifice group receipts by encouraging undercoding. “We’ve found hospitals do a poor job of negotiating the provider portion of third-party payer contracts and frequently lose provider charges because they focus on the much larger facility fees,” says Dr. Ahlstrom. The group’s receipts increased more than 30% when they began using an outside billing firm and adopted productivity incentives to encourage providers to practice better documentation and charge capture. Improving documentation also supports a hospital’s ability to accurately code its patients, which allows a hospital to bill for a more profitable diagnosis-related group (DRG), and improve its case-mix index. With these changes, Hospitalists of Northwest Michigan has increased provider pay and grown their practice while improving the hospitals’ profitability.
- Encourage frugality. The cost-plus model is popular, but it doesn’t incentivize programs to contain costs. In contrast, the fixed-price model encourages hospitalists to find cheaper ways to provide good care. “Because the money we save goes to us, we’ve all found creative ways to provide quality care for a third less money than similar cost-plus programs,” Dr. Ahlstrom says.
- Align incentives. Hospitals live or die on thin margins, Dr. Ahlstrom says. His group trains its employees to ask: What can I do to make the hospital stronger? “What’s good for the hospital is good for us, so we work with the hospitals, not for the hospitals,” Dr. Friar says.
At its smaller hospitals, HNM incentivized orthopedic admissions so that more surgical cases would stay local. Hospitalists were trained to perform stress tests so the hospital can provide testing on weekends. The group pays hospitalists a bonus for each admission, so when the ED calls, the hospitalists say, “Thanks! I’ll be right there.” The group also increased staffing on weekends.
The end result: It improves the hospital’s bottom line by shortening length of stay, and improving quality of care, patient satisfaction, and group morale.
“When we align the incentives, everybody wins,” says Dr. Friar. “The system has more capacity, the patients get better care, and the hospitalists no longer feel that weekend shifts are a huge burden.”
- Build “system-ness.” Sharing providers between hospitals has helped HNM build a cohesive system of quality care. What began as a way to cover shifts has created an interinstitutional camaraderie that allows for the easier flow of patients, improved communication, and widespread use of best-practice models. Sharing such resources as billing, credentialing, benefits, recruiting, and payroll has helped the group stay competitive, Dr. Ahlstrom says.
Growth in a Down Economy
Jude R. Alexander, MD, president of Inpatient Specialists in Rockville, Md., a bedroom community about 12 miles northwest of Washington, D.C., has continued to grow his group despite the down economy. Hospital admissions in the D.C. area decreased sharply in the second half of 2008, and patient volume rebounded slowly in the first half of 2009.
Inpatient Specialists initially downsized its staff, then it used flex physicians to meet demand as volume increased.
Despite national hospital trends of budget shortfalls, downgraded bond ratings, and increases in uninsured patients, two of Inpatient Specialists’ client hospitals chose to invest in the HM program. Dr. Alexander credits the vote of confidence to his group’s track record of optimal resource utilization, which has inherent cost savings in the millions.
Dr. Alexander also recommends HM groups in tough economic circumstances should:
- Maintain good relationships with partner hospitals;
- Run a lean business;
- Focus on excellent customer service to patients, their families, and their PCPs; and
- Build strong alliances with employed physicians by eliciting and giving constructive feedback.
“Following this basic strategy, Inpatient Specialists has experienced 7% growth in patient volume in the past 12 months,” Dr. Alexander says. “We’ve expanded to 40 full-time equivalent hospitalists, and 40 part-time employees.” Inpatient Specialists has its eye on geographic expansion, as well. The group is targeting services throughout the Capitol region—Maryland, Virginia, and the District of Columbia.
Bankruptcy to Profitability in One Year
In 2007, a few months after the 99-bed Auburn Memorial Hospital in Auburn, N.Y., was forced into bankruptcy, James Leyhane, MD, and his hospitalist group were displeased that they weren’t in control of their own program. Physicians had started leaving the hospital; Dr. Leyhane himself had interviewed at another hospital. “Our CEO approached me to ask what would make it right,” Dr. Leyhane recalls. “I said, ‘We’d need to be employed by the hospital.’ ”
The hospital and the private, six-physician internal-medicine group that employed the program entered bids on the HM group. In March 2008, the HM group became contractually employed by the hospital. Dr. Leyhane was given full control as hospitalist director of Auburn Memorial Hospitalists.
As a result of the new alignment, two major shifts took place. First, the hospital CEO more aggressively recruited subspecialists and surgeons. With the HM group now affiliated with the hospital, recruiting surgeons to Auburn Memorial became much easier. Second, more primary-care physicians (PCPs) began sending their patients to Auburn Memorial.
“We were all shocked at how quickly the administration was able to recruit new subspecialists to the area,” Dr. Leyhane says. “That helped get the profitable procedures back to the hospital.”
The biggest surprise came at the end of 2008. Patient volume had risen 11.5% higher than the hospital’s best-case predictions. “As a result of our emerging from under the umbrella of one physician group, the outlying physicians became less fearful that they might lose their patients to that group,” Dr. Leyhane says. “And in good faith, we still maintain a coverage arrangement with that IM group.”
Thus, what was first seen as a bad thing turned into a very good thing for both the hospitalist group and the hospital. Auburn Memorial posted a $3.1 million profit in 2008 (see Table 1).
Dr. Leyhane suggests HM group leaders facing similar financial crunches talk to area subspecialists and find out what it would take to get them affiliated with their institution.
“In our case, a stable hospitalist program was definitely one of their top requests,” Dr. Leyhane says, adding it also would be beneficial to include PCPs in the “what do you want from our hospital?” conversation. TH
Andrea M. Sattinger is a freelance writer based in North Carolina.
Image Source: COLIN ANDERSON/GETTYIMAGES
Nice to Meet You
Susan Connelly of Fruitland Park, Fla., is a volunteer at her local community hospital who until recently had never heard of a hospitalist. One day, she entered a hospital room and, as she regularly did with patients she visited, asked if there was anything the man in the bed needed.
“I want to know where my doctor is,” the patient said.
“You mean your doctor hasn’t seen you?” Connelly asked.
“No,” he said. “I’m not even sure he knows I’m here.”
Somewhat incredulous, Connelly retrieved the hospital’s physician handbook and helped the patient look up his physician’s phone number. “I didn’t think too much about it,” she says. But the following week, when she appeared at the hospital to volunteer, a supervisor called her into the office. The supervisor asked Connelly about the incident and gently admonished her for encouraging the patient to call his primary-care physician (PCP), as “a hospitalist is working with him now.”
“A what? I had never even heard the term,” Connelly says. She asked her fellow volunteers, known as patient representatives at her hospital, if they had ever heard of a hospitalist. One had, but only because her husband had been admitted for a hospital stay. Concerned, Connelly wrote letters to the editors of two local newspapers. Both were published (see Figure 2, “Familiar Face Gone Missing,” p. 30).
—Robert Centor, MD, associate dean of medicine, University of Alabama at Birmingham
“If I am admitted to the hospital, my doctor will most likely ‘dump’ me on what is now called a ‘hospitalist,’ ” she wrote. “Information gathered [by the hospitalist] should be forwarded to your doctor; the key word is ‘should.’ Why develop this long-term relationship with a doctor, if when you really need him, he is not there for you and you are dealing with a stranger?”
Why indeed?
It might not happen with every new admission, but patient fears are a reality. The uncertainty of a hospital stay, a new physician, and new medications can take their toll on the human psyche. Patients are upset with their PCP, the hospital, the system; many times it’s the hospitalist who feels the brunt of their anger. Not only do hospitalists have to calm a patient worried about PCP disconnect, but they also have to reassure the patient that they will be attentive to their needs, provide a high quality of care during the hospital stay, and communicate with their PCP about diagnoses, medications, and follow-up care. Hospitalists should weave in some of the documented plusses a hospitalist brings to the table: shorter length of stays, greater patient access and availability, and improved quality of care.
Although some patients might view hospitalists as “strangers,” HM physicians can learn methods to ease patient anxiety and answer tough questions from patients about the role they play in hospital care.
Restore Confidence
Simple conversations can help hospitalists defuse patient dissatisfaction. When a patient asks why their PCP won’t be seeing them in the hospital, it’s best to begin with a reassuring approach. For example, introduce yourself and say you have reviewed the case with their PCP. You can include key information from their medical history and recent hospitalizations, if appropriate.
Robert Centor, MD, a hospitalist and associate dean of medicine at the University of Alabama at Birmingham, suggests a few other key behaviors for initial patient visits. He finds a way to make appropriate physical contact by taking a pulse, checking the heart and lungs, or patting a shoulder to clearly embody the role of the physician in charge.
“And pull up a chair,” he says. “If there is no chair, bring in a chair. But sit down—always.”
Dr. Centor also recommends a transparent approach, “especially in hospital medicine,” he explains. “Be explicit about what you’re thinking, what you’re doing, and why you’re doing it.”1
Transparency can protect you as it informs and comforts patients and their families. For instance, “hospitalized patients are probably hearing from every relative they have and half the friends they have,” Dr. Centor says. “If one of those people is a physician, they may be second-guessing you. You can overcome their wariness by remembering that this is all about bedside manner and the explanations you give them, including discharge instructions.”
Dr. Centor says your bedside manner needs to fit your personality. When you talk to a patient, use language that matches your personality. You can adopt someone else’s introductory script; just make sure to modify it to fit your work environment (see “Strategies to Ease Patient Concerns,” p. 29).
“What Is This?”
Earlier this year, CJ Clarke of Leesburg, Fla., underwent a colonoscopy screening at a local doctor’s office. She had been kept on warfarin (Coumadin) to prevent complications, but after she bled for four days from a puncture sustained during the procedure, she went to the ED. She was admitted, but it wasn’t until the following afternoon that she learned that hospitalists—not her PCP— would be taking care of her.
“This totally unknown guy came in and said he would be filling in for my doctor and communicating with [my PCP],” Clarke says. “It was a weekend, and it turns out the first hospitalist was a substitute hospitalist, so then I got another hospitalist. The first one was subbing for the first hospitalist. I wasn’t exactly mad, but I thought, what is this?”
Clarke thought the first hospitalist was knowledgeable; she took comfort in that. “But the second one was extremely knowledgeable and explained the differences between Coumadin and heparin. He really knew his stuff. He talked to my cardiologist when she came in,” Clarke says. “The only thing that I was sorry about was that my primary didn’t seem to get the information very rapidly.”
Care coordination is a vital step in the discharge process, especially when patients think the flow of information between a hospital and a PCP is immediate and seamless. When Clarke was discharged and she returned home, she scheduled an appointment with her PCP. “When I first called, my [PCP] had not even heard I had been admitted,” Clarke says. But by the time she visited the PCP, “she knew everything. … I think it would have been good if sometime during that five-day hospitalization, she had been told—not afterward. Not that she would have come in, because that is not her policy, but just to know she knew.”
HM’s Role: Extended Education
Many HM groups have designated policies for educating patients and assuaging their fears. Because some PCPs might feel left out of the loop when hospitalists care for their patients, these strategies go beyond patient education.
One of the first steps is to involve PCPs in meaningful ways in their patients’ hospital care. When a patient is particularly angered by his PCP’s absence, invite the PCP to visit, or call the PCP more often and let the patient know you’re doing so. As proposed by Bob Wachter, MD, professor and chief of the division of hospital medicine at the University of California at San Francisco, a former SHM president, and author of the blog “Wachter’s World,” and Steven Pantilat, MD, FHM, professor of clinical medicine in the division of hospital medicine at UCSF, and a former SHM president, “the PCP can endorse the hospitalist model and the individual hospitalist, notice subtle findings that differ from the patient’s baseline, and help clarify patient preferences regarding difficult situations by drawing on their previous relationship with the patient. This visit may also benefit the PCP by providing insights into the patient’s illness, personality, or social support that he or she was unaware of previously.”2,3
Cogent Healthcare uses an outreach program to calm patient fears and connect with PCPs. The Brentwood, Tenn.-based hospitalist company distributes patient education pamphlets to the PCPs with whom they work, and distributes a flier on admission to show patients the photographs and names of their HM team (see “Make Patient Education A Priority,” p. 29).
Hospitalist training in this arena helps prepare physicians for a potentially uncomfortable work environment. “We need to stress in residency training the specific issue of helping make the patient feel comfortable when their own doctor is not seeing them in the hospital,” Dr. Centor says. “Most young hospitalists right out of their residencies have not experienced primary-care practice, and, so far, we don’t know how to get around that.”
Hospitalist groups also should consider broad initiatives to bring hospitalists together with patient representatives and other volunteers who work with patients. If volunteers are ignored in the educational outreach process, it could exacerbate patients’ negative reactions. Teach volunteers what hospitalists are, their benefit to care delivery, and their value in upholding the mission of quality HM. TH
Andrea Sattinger is a freelance writer based in North Carolina.
References
- Centor RM. A hospitalist inpatient system does not improve patient care outcomes. Arch Intern Med. 2008;168(12):1257-1258.
- Lo B. Ethical and policy implications of hospitalist systems. Dis Mon. 2002;48(4):281-290.
- Wachter RM, Pantilat SZ. The “continuity visit” and the hospitalist model of care. Dis Mon. 2002;48(4): 267-272.
Image Source: PETRI ARTTURI ASIKAINEN / GETTY IMAGES
Susan Connelly of Fruitland Park, Fla., is a volunteer at her local community hospital who until recently had never heard of a hospitalist. One day, she entered a hospital room and, as she regularly did with patients she visited, asked if there was anything the man in the bed needed.
“I want to know where my doctor is,” the patient said.
“You mean your doctor hasn’t seen you?” Connelly asked.
“No,” he said. “I’m not even sure he knows I’m here.”
Somewhat incredulous, Connelly retrieved the hospital’s physician handbook and helped the patient look up his physician’s phone number. “I didn’t think too much about it,” she says. But the following week, when she appeared at the hospital to volunteer, a supervisor called her into the office. The supervisor asked Connelly about the incident and gently admonished her for encouraging the patient to call his primary-care physician (PCP), as “a hospitalist is working with him now.”
“A what? I had never even heard the term,” Connelly says. She asked her fellow volunteers, known as patient representatives at her hospital, if they had ever heard of a hospitalist. One had, but only because her husband had been admitted for a hospital stay. Concerned, Connelly wrote letters to the editors of two local newspapers. Both were published (see Figure 2, “Familiar Face Gone Missing,” p. 30).
—Robert Centor, MD, associate dean of medicine, University of Alabama at Birmingham
“If I am admitted to the hospital, my doctor will most likely ‘dump’ me on what is now called a ‘hospitalist,’ ” she wrote. “Information gathered [by the hospitalist] should be forwarded to your doctor; the key word is ‘should.’ Why develop this long-term relationship with a doctor, if when you really need him, he is not there for you and you are dealing with a stranger?”
Why indeed?
It might not happen with every new admission, but patient fears are a reality. The uncertainty of a hospital stay, a new physician, and new medications can take their toll on the human psyche. Patients are upset with their PCP, the hospital, the system; many times it’s the hospitalist who feels the brunt of their anger. Not only do hospitalists have to calm a patient worried about PCP disconnect, but they also have to reassure the patient that they will be attentive to their needs, provide a high quality of care during the hospital stay, and communicate with their PCP about diagnoses, medications, and follow-up care. Hospitalists should weave in some of the documented plusses a hospitalist brings to the table: shorter length of stays, greater patient access and availability, and improved quality of care.
Although some patients might view hospitalists as “strangers,” HM physicians can learn methods to ease patient anxiety and answer tough questions from patients about the role they play in hospital care.
Restore Confidence
Simple conversations can help hospitalists defuse patient dissatisfaction. When a patient asks why their PCP won’t be seeing them in the hospital, it’s best to begin with a reassuring approach. For example, introduce yourself and say you have reviewed the case with their PCP. You can include key information from their medical history and recent hospitalizations, if appropriate.
Robert Centor, MD, a hospitalist and associate dean of medicine at the University of Alabama at Birmingham, suggests a few other key behaviors for initial patient visits. He finds a way to make appropriate physical contact by taking a pulse, checking the heart and lungs, or patting a shoulder to clearly embody the role of the physician in charge.
“And pull up a chair,” he says. “If there is no chair, bring in a chair. But sit down—always.”
Dr. Centor also recommends a transparent approach, “especially in hospital medicine,” he explains. “Be explicit about what you’re thinking, what you’re doing, and why you’re doing it.”1
Transparency can protect you as it informs and comforts patients and their families. For instance, “hospitalized patients are probably hearing from every relative they have and half the friends they have,” Dr. Centor says. “If one of those people is a physician, they may be second-guessing you. You can overcome their wariness by remembering that this is all about bedside manner and the explanations you give them, including discharge instructions.”
Dr. Centor says your bedside manner needs to fit your personality. When you talk to a patient, use language that matches your personality. You can adopt someone else’s introductory script; just make sure to modify it to fit your work environment (see “Strategies to Ease Patient Concerns,” p. 29).
“What Is This?”
Earlier this year, CJ Clarke of Leesburg, Fla., underwent a colonoscopy screening at a local doctor’s office. She had been kept on warfarin (Coumadin) to prevent complications, but after she bled for four days from a puncture sustained during the procedure, she went to the ED. She was admitted, but it wasn’t until the following afternoon that she learned that hospitalists—not her PCP— would be taking care of her.
“This totally unknown guy came in and said he would be filling in for my doctor and communicating with [my PCP],” Clarke says. “It was a weekend, and it turns out the first hospitalist was a substitute hospitalist, so then I got another hospitalist. The first one was subbing for the first hospitalist. I wasn’t exactly mad, but I thought, what is this?”
Clarke thought the first hospitalist was knowledgeable; she took comfort in that. “But the second one was extremely knowledgeable and explained the differences between Coumadin and heparin. He really knew his stuff. He talked to my cardiologist when she came in,” Clarke says. “The only thing that I was sorry about was that my primary didn’t seem to get the information very rapidly.”
Care coordination is a vital step in the discharge process, especially when patients think the flow of information between a hospital and a PCP is immediate and seamless. When Clarke was discharged and she returned home, she scheduled an appointment with her PCP. “When I first called, my [PCP] had not even heard I had been admitted,” Clarke says. But by the time she visited the PCP, “she knew everything. … I think it would have been good if sometime during that five-day hospitalization, she had been told—not afterward. Not that she would have come in, because that is not her policy, but just to know she knew.”
HM’s Role: Extended Education
Many HM groups have designated policies for educating patients and assuaging their fears. Because some PCPs might feel left out of the loop when hospitalists care for their patients, these strategies go beyond patient education.
One of the first steps is to involve PCPs in meaningful ways in their patients’ hospital care. When a patient is particularly angered by his PCP’s absence, invite the PCP to visit, or call the PCP more often and let the patient know you’re doing so. As proposed by Bob Wachter, MD, professor and chief of the division of hospital medicine at the University of California at San Francisco, a former SHM president, and author of the blog “Wachter’s World,” and Steven Pantilat, MD, FHM, professor of clinical medicine in the division of hospital medicine at UCSF, and a former SHM president, “the PCP can endorse the hospitalist model and the individual hospitalist, notice subtle findings that differ from the patient’s baseline, and help clarify patient preferences regarding difficult situations by drawing on their previous relationship with the patient. This visit may also benefit the PCP by providing insights into the patient’s illness, personality, or social support that he or she was unaware of previously.”2,3
Cogent Healthcare uses an outreach program to calm patient fears and connect with PCPs. The Brentwood, Tenn.-based hospitalist company distributes patient education pamphlets to the PCPs with whom they work, and distributes a flier on admission to show patients the photographs and names of their HM team (see “Make Patient Education A Priority,” p. 29).
Hospitalist training in this arena helps prepare physicians for a potentially uncomfortable work environment. “We need to stress in residency training the specific issue of helping make the patient feel comfortable when their own doctor is not seeing them in the hospital,” Dr. Centor says. “Most young hospitalists right out of their residencies have not experienced primary-care practice, and, so far, we don’t know how to get around that.”
Hospitalist groups also should consider broad initiatives to bring hospitalists together with patient representatives and other volunteers who work with patients. If volunteers are ignored in the educational outreach process, it could exacerbate patients’ negative reactions. Teach volunteers what hospitalists are, their benefit to care delivery, and their value in upholding the mission of quality HM. TH
Andrea Sattinger is a freelance writer based in North Carolina.
References
- Centor RM. A hospitalist inpatient system does not improve patient care outcomes. Arch Intern Med. 2008;168(12):1257-1258.
- Lo B. Ethical and policy implications of hospitalist systems. Dis Mon. 2002;48(4):281-290.
- Wachter RM, Pantilat SZ. The “continuity visit” and the hospitalist model of care. Dis Mon. 2002;48(4): 267-272.
Image Source: PETRI ARTTURI ASIKAINEN / GETTY IMAGES
Susan Connelly of Fruitland Park, Fla., is a volunteer at her local community hospital who until recently had never heard of a hospitalist. One day, she entered a hospital room and, as she regularly did with patients she visited, asked if there was anything the man in the bed needed.
“I want to know where my doctor is,” the patient said.
“You mean your doctor hasn’t seen you?” Connelly asked.
“No,” he said. “I’m not even sure he knows I’m here.”
Somewhat incredulous, Connelly retrieved the hospital’s physician handbook and helped the patient look up his physician’s phone number. “I didn’t think too much about it,” she says. But the following week, when she appeared at the hospital to volunteer, a supervisor called her into the office. The supervisor asked Connelly about the incident and gently admonished her for encouraging the patient to call his primary-care physician (PCP), as “a hospitalist is working with him now.”
“A what? I had never even heard the term,” Connelly says. She asked her fellow volunteers, known as patient representatives at her hospital, if they had ever heard of a hospitalist. One had, but only because her husband had been admitted for a hospital stay. Concerned, Connelly wrote letters to the editors of two local newspapers. Both were published (see Figure 2, “Familiar Face Gone Missing,” p. 30).
—Robert Centor, MD, associate dean of medicine, University of Alabama at Birmingham
“If I am admitted to the hospital, my doctor will most likely ‘dump’ me on what is now called a ‘hospitalist,’ ” she wrote. “Information gathered [by the hospitalist] should be forwarded to your doctor; the key word is ‘should.’ Why develop this long-term relationship with a doctor, if when you really need him, he is not there for you and you are dealing with a stranger?”
Why indeed?
It might not happen with every new admission, but patient fears are a reality. The uncertainty of a hospital stay, a new physician, and new medications can take their toll on the human psyche. Patients are upset with their PCP, the hospital, the system; many times it’s the hospitalist who feels the brunt of their anger. Not only do hospitalists have to calm a patient worried about PCP disconnect, but they also have to reassure the patient that they will be attentive to their needs, provide a high quality of care during the hospital stay, and communicate with their PCP about diagnoses, medications, and follow-up care. Hospitalists should weave in some of the documented plusses a hospitalist brings to the table: shorter length of stays, greater patient access and availability, and improved quality of care.
Although some patients might view hospitalists as “strangers,” HM physicians can learn methods to ease patient anxiety and answer tough questions from patients about the role they play in hospital care.
Restore Confidence
Simple conversations can help hospitalists defuse patient dissatisfaction. When a patient asks why their PCP won’t be seeing them in the hospital, it’s best to begin with a reassuring approach. For example, introduce yourself and say you have reviewed the case with their PCP. You can include key information from their medical history and recent hospitalizations, if appropriate.
Robert Centor, MD, a hospitalist and associate dean of medicine at the University of Alabama at Birmingham, suggests a few other key behaviors for initial patient visits. He finds a way to make appropriate physical contact by taking a pulse, checking the heart and lungs, or patting a shoulder to clearly embody the role of the physician in charge.
“And pull up a chair,” he says. “If there is no chair, bring in a chair. But sit down—always.”
Dr. Centor also recommends a transparent approach, “especially in hospital medicine,” he explains. “Be explicit about what you’re thinking, what you’re doing, and why you’re doing it.”1
Transparency can protect you as it informs and comforts patients and their families. For instance, “hospitalized patients are probably hearing from every relative they have and half the friends they have,” Dr. Centor says. “If one of those people is a physician, they may be second-guessing you. You can overcome their wariness by remembering that this is all about bedside manner and the explanations you give them, including discharge instructions.”
Dr. Centor says your bedside manner needs to fit your personality. When you talk to a patient, use language that matches your personality. You can adopt someone else’s introductory script; just make sure to modify it to fit your work environment (see “Strategies to Ease Patient Concerns,” p. 29).
“What Is This?”
Earlier this year, CJ Clarke of Leesburg, Fla., underwent a colonoscopy screening at a local doctor’s office. She had been kept on warfarin (Coumadin) to prevent complications, but after she bled for four days from a puncture sustained during the procedure, she went to the ED. She was admitted, but it wasn’t until the following afternoon that she learned that hospitalists—not her PCP— would be taking care of her.
“This totally unknown guy came in and said he would be filling in for my doctor and communicating with [my PCP],” Clarke says. “It was a weekend, and it turns out the first hospitalist was a substitute hospitalist, so then I got another hospitalist. The first one was subbing for the first hospitalist. I wasn’t exactly mad, but I thought, what is this?”
Clarke thought the first hospitalist was knowledgeable; she took comfort in that. “But the second one was extremely knowledgeable and explained the differences between Coumadin and heparin. He really knew his stuff. He talked to my cardiologist when she came in,” Clarke says. “The only thing that I was sorry about was that my primary didn’t seem to get the information very rapidly.”
Care coordination is a vital step in the discharge process, especially when patients think the flow of information between a hospital and a PCP is immediate and seamless. When Clarke was discharged and she returned home, she scheduled an appointment with her PCP. “When I first called, my [PCP] had not even heard I had been admitted,” Clarke says. But by the time she visited the PCP, “she knew everything. … I think it would have been good if sometime during that five-day hospitalization, she had been told—not afterward. Not that she would have come in, because that is not her policy, but just to know she knew.”
HM’s Role: Extended Education
Many HM groups have designated policies for educating patients and assuaging their fears. Because some PCPs might feel left out of the loop when hospitalists care for their patients, these strategies go beyond patient education.
One of the first steps is to involve PCPs in meaningful ways in their patients’ hospital care. When a patient is particularly angered by his PCP’s absence, invite the PCP to visit, or call the PCP more often and let the patient know you’re doing so. As proposed by Bob Wachter, MD, professor and chief of the division of hospital medicine at the University of California at San Francisco, a former SHM president, and author of the blog “Wachter’s World,” and Steven Pantilat, MD, FHM, professor of clinical medicine in the division of hospital medicine at UCSF, and a former SHM president, “the PCP can endorse the hospitalist model and the individual hospitalist, notice subtle findings that differ from the patient’s baseline, and help clarify patient preferences regarding difficult situations by drawing on their previous relationship with the patient. This visit may also benefit the PCP by providing insights into the patient’s illness, personality, or social support that he or she was unaware of previously.”2,3
Cogent Healthcare uses an outreach program to calm patient fears and connect with PCPs. The Brentwood, Tenn.-based hospitalist company distributes patient education pamphlets to the PCPs with whom they work, and distributes a flier on admission to show patients the photographs and names of their HM team (see “Make Patient Education A Priority,” p. 29).
Hospitalist training in this arena helps prepare physicians for a potentially uncomfortable work environment. “We need to stress in residency training the specific issue of helping make the patient feel comfortable when their own doctor is not seeing them in the hospital,” Dr. Centor says. “Most young hospitalists right out of their residencies have not experienced primary-care practice, and, so far, we don’t know how to get around that.”
Hospitalist groups also should consider broad initiatives to bring hospitalists together with patient representatives and other volunteers who work with patients. If volunteers are ignored in the educational outreach process, it could exacerbate patients’ negative reactions. Teach volunteers what hospitalists are, their benefit to care delivery, and their value in upholding the mission of quality HM. TH
Andrea Sattinger is a freelance writer based in North Carolina.
References
- Centor RM. A hospitalist inpatient system does not improve patient care outcomes. Arch Intern Med. 2008;168(12):1257-1258.
- Lo B. Ethical and policy implications of hospitalist systems. Dis Mon. 2002;48(4):281-290.
- Wachter RM, Pantilat SZ. The “continuity visit” and the hospitalist model of care. Dis Mon. 2002;48(4): 267-272.
Image Source: PETRI ARTTURI ASIKAINEN / GETTY IMAGES
Social Work
Editors’ note: “Alliances” is a new series written about the relationships that hospitalists have with members of the clinical care team—from the team members’ points of view. It’s our hope that each installment of “Alliances” will provide valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
Social workers are a natural fit with hospitalists and the hospitalist’s strongest allies and staunchest supporters, wrote Bradley Flansbaum, DO, MPH, in his Nov./Dec. 2003 article in The Hospitalist. What makes this collaboration such a positive one and what can members of these two professions learn from each other?
Dr. Flansbaum, a hospitalist and internist with the Division of Internal Medicine/Primary Care at Lenox Hill Hospital, Bronx, N.Y., and a former SHM board member, recently reiterated the benefits of the hospitalist-social worker relationship. In general, he believes that hospitalists provide a unique history-taking perspective that is useful to social workers in their work. Foremost, social workers bring a rich understanding of the available resources that patients need after discharge and a view of the patient’s nonmedical circumstances. Together, the two professionals’ daily interactions generate more effective discharge planning as a part of the multidisciplinary team.
ALWAYS THERE
Amy Lingg, MS, MPA, works on the general medicine unit at Greenwich Hospital (Conn). She says the role of the hospitalist is fairly new at Greenwich. In fact Sabitha Rajan, MD, MS, was the first one at Greenwich Hospital.
In Lingg’s view, nothing can replace the availability of the hospitalist to discuss patient cases, not only with the social worker but also as a team with the patient and family.
“[Attendings] are not there for the moment-by-moment events that happen on the unit, including availability when families are here,” says Lingg. “If I need to speak with a family and the physician’s input is important there, I can just page the hospitalist, she’s here. Whereas with an attending you have to make an appointment; you have to schedule around them. It can become difficult.”
Lingg, who works with hospitalist Dr. Rajan, director of hospitalist services at Greenwich Hospital, cites an example of the benefits of hospitalists’ 24/7 availability: “We had a fairly young woman in her mid-40s who was the divorced mother of a 17-year-old son. The father was not in the picture, and the woman was dying of alcoholic cirrhosis and liver failure. She was Dr. Rajan’s patient. One of the issues was the fact that there was no adult guardian for the son although he was going to be 18 in two months.
“So it involved a lot of talking with friends of the woman, who were sort of stepping in as surrogate guardians to him,” Lingg continues. “There were a lot of logistics [regarding] what would happen with him. We were trying to call the grandfather who was estranged. It was a very, very sensitive, very, very tricky case. It went on for days and days. … Dr. Rajan and I could work on this together on a dayto-day basis, [including] … the counseling, relaying medical knowledge to the family, what was going on clinically, trying to deal with that in a way where she was talking in one way to [the] adults and in a different, more appropriate [for the boy’s age] way to the 17-yearold son. And I can be there to help with that process.”
The situation was resolved to the satisfaction of the mother, the son, the friends, and the providers. “It was really pretty extraordinary,” she said. “I’ve talked about that a couple of times, including at a staff meetings when we were talking about getting new hospitalists. That is something I’ve described because, really, it was very special.”
TRUE TEAMWORK
Although everyone on a multidisciplinary team can bring something to the discussion that makes the team work better, social workers and hospitalists collaborate well in painting a more comprehensive picture of the patient’s lifestyle, living habits, and needs.
“In many hospitals … there’s a pattern that develops [whereby at] some time in the morning the hospitalist and social worker will get together and talk,” says Dr. Flansbaum “The hospitalist speaks the language of the social worker and knows what to tell them and how to direct them rather than just saying, ‘the patient’s homeless or the patient needs help at home.’”
After working regularly with social workers and recognizing what they need to know, he says, “the hospitalist is more likely to say, ‘the patient has Medicaid,’ or ‘the patient has this insurance,’ [or] ‘the patient has a home-health [caregiver] four hours a day and needs six or eight hours a day,’ or ‘the patient’s going to need a subacute nursing facility.’ … I think our insights are different from voluntary physicians and our face-time with social workers is more efficient.”
Sylvia Krafcik, MSSA, LISW, with MetroHealth Medical Center, Cleveland, says hospitalists are “great to work with because they’re very dedicated to the population they’re caring for, because this is their whole responsibility; they don’t have a private caseload.”
But in her view most hospitalists are focused on patients’ medical conditions and some of them are not as tuned in to all the other aspects of the patient, such as all the psychosocial dynamics.
“A lot of them are, but some aren’t,” Krafcik says. “Especially at MetroHealth, we’re a county hospital. So many of the patients that come here are poor. A lot of them are alcoholics or drug abusers. They’re homeless. They live on the streets. They don’t have a primary doctor. They’re usually not compliant with their medications.”
“Here at Metro we have a lot of patients who have extreme social circumstances that affect their medical issues so much,” says Sara Dunson, MSW, LSW, who also works as a social worker at Metro-Health. “I think the hospitalist has greater insight into the person’s environment and all the social structures that they have at home and that are going on in their life [than other physicians might].”
But there is always room for improvement.
“We had one patient who wasn’t able to read, and he never told anybody this,” says Dunson. “And as social workers, we have more of a way of finding that kind of stuff out from patients than the doctors might. And he kept coming in and coming in and was noncompliant with his medication. We eventually determined that this was why he was noncompliant and was causing all these medical issues. The doctors finally [understood] why this gentleman kept coming in with the same problems and he wasn’t taking care of himself. It wasn’t that he didn’t want to, it was just that he was having problems reading all the medications and all the discharge paperwork, and he was too ashamed to tell anybody. [Once the social workers questioned him and got this] out in the open, we were able to get him help with that.”
The doctors focused on what he was or wasn’t doing, but they hadn’t looked at why he wasn’t adherent, explains Dunson. If hospitalists do that more often, she thinks, they could save time and get better outcomes sooner.
COMMUNICATING WITH PATIENTS AND FAMILIES
“I think where hospitalists are coming from is a whole different mindset than a physician who has mainly an office practice,” said Lingg. “The office practice comes first [for them]. Some of our physicians have huge practices in town. And they’ll visit the hospital very early in the morning or in the evening. ... So if I need something in a case like that, if there was not a hospitalist involved, it would have been separate meetings for the family with the physician … and [with] me at another time.”
To hospitalists, a social worker can serve as an important adjunct in talking to the patient and family. “For example, if [social workers] are giving bad news, they warn the physician first,” says Dr. Rajan. “If they’re going to go in and tell the patient that they’re not going to qualify for any home services, they tell the physician as well so that [the hospitalist will not later be] meeting an angry patient.” In addition, she says, “for critically ill or long-term patients, social workers [can] help family members cope. Sometimes as physicians we don’t have the time or we don’t have the resources to do that.”
But this doesn’t let doctors off the hook in regard to addressing the whole person’s needs. Especially if someone has multiple medical problems, the social worker needs to know the availability and level of support for which the family can be counted.
“Social workers will ask questions such as: Are the families involved? or Is there any family?” says Krafcik. “Do they need to go in a nursing home or do they need 24-hour care at home? Is the family able to provide that? [E]very morning we meet to have team rounds. And the [team] go[es] over every patient on the floor, and then I will ask those questions if the doctor hasn’t given me that information.”
Social workers appreciate and would like hospitalists to do more listening to the patient and family for the aspects of the history and psychosocial status that the social worker will need to know.
TEACHING POINTS
In the course of their interactions, what do hospitalists and social workers teach each other that could lead to working a case more effectively and to the greater satisfaction of all involved?
Most of those we interviewed seem to think that the greatest service hospitalists provide is to teach the social worker the medical components that go along with what the social worker does every day.
“[Social workers] get a better understanding of [whether] someone comes in with heart failure or a fall or a stroke, just by repetition and also education; they get to understand after a while what’s needed for individual medical diagnoses,” says Dr. Flansbaum.
“When I know [better] what the medical condition is,” says Krafcik, “I have an idea of how much help [the patient] would need at home and their ability to function. And I would make sure that the patient gets physical therapy or occupational therapy referral or speech therapy.”
Again, perhaps the area where the social worker most teaches the hospitalist regards available resources to solve problems over and above the purely medical. “They know the social system and the needs of different forms and eligibility and what different patients are entitled to and what the system will provide,” says Dr. Flansbaum.
Dunson believes hospitalists are perceived as being more involved in a holistic way with the patient. “I always stress that it is so important to look at the whole person and not just the medical aspects,” she says. “It’s hard for the doctor sometimes to realize that this person might not be able to afford this medication and that’s why they’re noncompliant and all the other issues. So I think is important to open up to the other aspects of a person’s life and not just the medical aspects.”
CONCLUSION
Social workers’ knowledge of medical and nonmedical resources, both locally and nationally, offer hospitalists essential information that leads to designing more appropriate and effective post-discharge plans. Hospitalists can best team with social workers by consistently keeping in mind the patient’s overall circumstances and informing their colleagues of the medical information that can help social workers do their best work. TH
Writer Andrea Sattinger will write about the effect of poor communication skills in the November issue of The Hospitalist.
Editors’ note: “Alliances” is a new series written about the relationships that hospitalists have with members of the clinical care team—from the team members’ points of view. It’s our hope that each installment of “Alliances” will provide valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
Social workers are a natural fit with hospitalists and the hospitalist’s strongest allies and staunchest supporters, wrote Bradley Flansbaum, DO, MPH, in his Nov./Dec. 2003 article in The Hospitalist. What makes this collaboration such a positive one and what can members of these two professions learn from each other?
Dr. Flansbaum, a hospitalist and internist with the Division of Internal Medicine/Primary Care at Lenox Hill Hospital, Bronx, N.Y., and a former SHM board member, recently reiterated the benefits of the hospitalist-social worker relationship. In general, he believes that hospitalists provide a unique history-taking perspective that is useful to social workers in their work. Foremost, social workers bring a rich understanding of the available resources that patients need after discharge and a view of the patient’s nonmedical circumstances. Together, the two professionals’ daily interactions generate more effective discharge planning as a part of the multidisciplinary team.
ALWAYS THERE
Amy Lingg, MS, MPA, works on the general medicine unit at Greenwich Hospital (Conn). She says the role of the hospitalist is fairly new at Greenwich. In fact Sabitha Rajan, MD, MS, was the first one at Greenwich Hospital.
In Lingg’s view, nothing can replace the availability of the hospitalist to discuss patient cases, not only with the social worker but also as a team with the patient and family.
“[Attendings] are not there for the moment-by-moment events that happen on the unit, including availability when families are here,” says Lingg. “If I need to speak with a family and the physician’s input is important there, I can just page the hospitalist, she’s here. Whereas with an attending you have to make an appointment; you have to schedule around them. It can become difficult.”
Lingg, who works with hospitalist Dr. Rajan, director of hospitalist services at Greenwich Hospital, cites an example of the benefits of hospitalists’ 24/7 availability: “We had a fairly young woman in her mid-40s who was the divorced mother of a 17-year-old son. The father was not in the picture, and the woman was dying of alcoholic cirrhosis and liver failure. She was Dr. Rajan’s patient. One of the issues was the fact that there was no adult guardian for the son although he was going to be 18 in two months.
“So it involved a lot of talking with friends of the woman, who were sort of stepping in as surrogate guardians to him,” Lingg continues. “There were a lot of logistics [regarding] what would happen with him. We were trying to call the grandfather who was estranged. It was a very, very sensitive, very, very tricky case. It went on for days and days. … Dr. Rajan and I could work on this together on a dayto-day basis, [including] … the counseling, relaying medical knowledge to the family, what was going on clinically, trying to deal with that in a way where she was talking in one way to [the] adults and in a different, more appropriate [for the boy’s age] way to the 17-yearold son. And I can be there to help with that process.”
The situation was resolved to the satisfaction of the mother, the son, the friends, and the providers. “It was really pretty extraordinary,” she said. “I’ve talked about that a couple of times, including at a staff meetings when we were talking about getting new hospitalists. That is something I’ve described because, really, it was very special.”
TRUE TEAMWORK
Although everyone on a multidisciplinary team can bring something to the discussion that makes the team work better, social workers and hospitalists collaborate well in painting a more comprehensive picture of the patient’s lifestyle, living habits, and needs.
“In many hospitals … there’s a pattern that develops [whereby at] some time in the morning the hospitalist and social worker will get together and talk,” says Dr. Flansbaum “The hospitalist speaks the language of the social worker and knows what to tell them and how to direct them rather than just saying, ‘the patient’s homeless or the patient needs help at home.’”
After working regularly with social workers and recognizing what they need to know, he says, “the hospitalist is more likely to say, ‘the patient has Medicaid,’ or ‘the patient has this insurance,’ [or] ‘the patient has a home-health [caregiver] four hours a day and needs six or eight hours a day,’ or ‘the patient’s going to need a subacute nursing facility.’ … I think our insights are different from voluntary physicians and our face-time with social workers is more efficient.”
Sylvia Krafcik, MSSA, LISW, with MetroHealth Medical Center, Cleveland, says hospitalists are “great to work with because they’re very dedicated to the population they’re caring for, because this is their whole responsibility; they don’t have a private caseload.”
But in her view most hospitalists are focused on patients’ medical conditions and some of them are not as tuned in to all the other aspects of the patient, such as all the psychosocial dynamics.
“A lot of them are, but some aren’t,” Krafcik says. “Especially at MetroHealth, we’re a county hospital. So many of the patients that come here are poor. A lot of them are alcoholics or drug abusers. They’re homeless. They live on the streets. They don’t have a primary doctor. They’re usually not compliant with their medications.”
“Here at Metro we have a lot of patients who have extreme social circumstances that affect their medical issues so much,” says Sara Dunson, MSW, LSW, who also works as a social worker at Metro-Health. “I think the hospitalist has greater insight into the person’s environment and all the social structures that they have at home and that are going on in their life [than other physicians might].”
But there is always room for improvement.
“We had one patient who wasn’t able to read, and he never told anybody this,” says Dunson. “And as social workers, we have more of a way of finding that kind of stuff out from patients than the doctors might. And he kept coming in and coming in and was noncompliant with his medication. We eventually determined that this was why he was noncompliant and was causing all these medical issues. The doctors finally [understood] why this gentleman kept coming in with the same problems and he wasn’t taking care of himself. It wasn’t that he didn’t want to, it was just that he was having problems reading all the medications and all the discharge paperwork, and he was too ashamed to tell anybody. [Once the social workers questioned him and got this] out in the open, we were able to get him help with that.”
The doctors focused on what he was or wasn’t doing, but they hadn’t looked at why he wasn’t adherent, explains Dunson. If hospitalists do that more often, she thinks, they could save time and get better outcomes sooner.
COMMUNICATING WITH PATIENTS AND FAMILIES
“I think where hospitalists are coming from is a whole different mindset than a physician who has mainly an office practice,” said Lingg. “The office practice comes first [for them]. Some of our physicians have huge practices in town. And they’ll visit the hospital very early in the morning or in the evening. ... So if I need something in a case like that, if there was not a hospitalist involved, it would have been separate meetings for the family with the physician … and [with] me at another time.”
To hospitalists, a social worker can serve as an important adjunct in talking to the patient and family. “For example, if [social workers] are giving bad news, they warn the physician first,” says Dr. Rajan. “If they’re going to go in and tell the patient that they’re not going to qualify for any home services, they tell the physician as well so that [the hospitalist will not later be] meeting an angry patient.” In addition, she says, “for critically ill or long-term patients, social workers [can] help family members cope. Sometimes as physicians we don’t have the time or we don’t have the resources to do that.”
But this doesn’t let doctors off the hook in regard to addressing the whole person’s needs. Especially if someone has multiple medical problems, the social worker needs to know the availability and level of support for which the family can be counted.
“Social workers will ask questions such as: Are the families involved? or Is there any family?” says Krafcik. “Do they need to go in a nursing home or do they need 24-hour care at home? Is the family able to provide that? [E]very morning we meet to have team rounds. And the [team] go[es] over every patient on the floor, and then I will ask those questions if the doctor hasn’t given me that information.”
Social workers appreciate and would like hospitalists to do more listening to the patient and family for the aspects of the history and psychosocial status that the social worker will need to know.
TEACHING POINTS
In the course of their interactions, what do hospitalists and social workers teach each other that could lead to working a case more effectively and to the greater satisfaction of all involved?
Most of those we interviewed seem to think that the greatest service hospitalists provide is to teach the social worker the medical components that go along with what the social worker does every day.
“[Social workers] get a better understanding of [whether] someone comes in with heart failure or a fall or a stroke, just by repetition and also education; they get to understand after a while what’s needed for individual medical diagnoses,” says Dr. Flansbaum.
“When I know [better] what the medical condition is,” says Krafcik, “I have an idea of how much help [the patient] would need at home and their ability to function. And I would make sure that the patient gets physical therapy or occupational therapy referral or speech therapy.”
Again, perhaps the area where the social worker most teaches the hospitalist regards available resources to solve problems over and above the purely medical. “They know the social system and the needs of different forms and eligibility and what different patients are entitled to and what the system will provide,” says Dr. Flansbaum.
Dunson believes hospitalists are perceived as being more involved in a holistic way with the patient. “I always stress that it is so important to look at the whole person and not just the medical aspects,” she says. “It’s hard for the doctor sometimes to realize that this person might not be able to afford this medication and that’s why they’re noncompliant and all the other issues. So I think is important to open up to the other aspects of a person’s life and not just the medical aspects.”
CONCLUSION
Social workers’ knowledge of medical and nonmedical resources, both locally and nationally, offer hospitalists essential information that leads to designing more appropriate and effective post-discharge plans. Hospitalists can best team with social workers by consistently keeping in mind the patient’s overall circumstances and informing their colleagues of the medical information that can help social workers do their best work. TH
Writer Andrea Sattinger will write about the effect of poor communication skills in the November issue of The Hospitalist.
Editors’ note: “Alliances” is a new series written about the relationships that hospitalists have with members of the clinical care team—from the team members’ points of view. It’s our hope that each installment of “Alliances” will provide valuable, revealing feedback that hospitalists can use to continually improve their intrateam relationships and, ultimately, patient care.
Social workers are a natural fit with hospitalists and the hospitalist’s strongest allies and staunchest supporters, wrote Bradley Flansbaum, DO, MPH, in his Nov./Dec. 2003 article in The Hospitalist. What makes this collaboration such a positive one and what can members of these two professions learn from each other?
Dr. Flansbaum, a hospitalist and internist with the Division of Internal Medicine/Primary Care at Lenox Hill Hospital, Bronx, N.Y., and a former SHM board member, recently reiterated the benefits of the hospitalist-social worker relationship. In general, he believes that hospitalists provide a unique history-taking perspective that is useful to social workers in their work. Foremost, social workers bring a rich understanding of the available resources that patients need after discharge and a view of the patient’s nonmedical circumstances. Together, the two professionals’ daily interactions generate more effective discharge planning as a part of the multidisciplinary team.
ALWAYS THERE
Amy Lingg, MS, MPA, works on the general medicine unit at Greenwich Hospital (Conn). She says the role of the hospitalist is fairly new at Greenwich. In fact Sabitha Rajan, MD, MS, was the first one at Greenwich Hospital.
In Lingg’s view, nothing can replace the availability of the hospitalist to discuss patient cases, not only with the social worker but also as a team with the patient and family.
“[Attendings] are not there for the moment-by-moment events that happen on the unit, including availability when families are here,” says Lingg. “If I need to speak with a family and the physician’s input is important there, I can just page the hospitalist, she’s here. Whereas with an attending you have to make an appointment; you have to schedule around them. It can become difficult.”
Lingg, who works with hospitalist Dr. Rajan, director of hospitalist services at Greenwich Hospital, cites an example of the benefits of hospitalists’ 24/7 availability: “We had a fairly young woman in her mid-40s who was the divorced mother of a 17-year-old son. The father was not in the picture, and the woman was dying of alcoholic cirrhosis and liver failure. She was Dr. Rajan’s patient. One of the issues was the fact that there was no adult guardian for the son although he was going to be 18 in two months.
“So it involved a lot of talking with friends of the woman, who were sort of stepping in as surrogate guardians to him,” Lingg continues. “There were a lot of logistics [regarding] what would happen with him. We were trying to call the grandfather who was estranged. It was a very, very sensitive, very, very tricky case. It went on for days and days. … Dr. Rajan and I could work on this together on a dayto-day basis, [including] … the counseling, relaying medical knowledge to the family, what was going on clinically, trying to deal with that in a way where she was talking in one way to [the] adults and in a different, more appropriate [for the boy’s age] way to the 17-yearold son. And I can be there to help with that process.”
The situation was resolved to the satisfaction of the mother, the son, the friends, and the providers. “It was really pretty extraordinary,” she said. “I’ve talked about that a couple of times, including at a staff meetings when we were talking about getting new hospitalists. That is something I’ve described because, really, it was very special.”
TRUE TEAMWORK
Although everyone on a multidisciplinary team can bring something to the discussion that makes the team work better, social workers and hospitalists collaborate well in painting a more comprehensive picture of the patient’s lifestyle, living habits, and needs.
“In many hospitals … there’s a pattern that develops [whereby at] some time in the morning the hospitalist and social worker will get together and talk,” says Dr. Flansbaum “The hospitalist speaks the language of the social worker and knows what to tell them and how to direct them rather than just saying, ‘the patient’s homeless or the patient needs help at home.’”
After working regularly with social workers and recognizing what they need to know, he says, “the hospitalist is more likely to say, ‘the patient has Medicaid,’ or ‘the patient has this insurance,’ [or] ‘the patient has a home-health [caregiver] four hours a day and needs six or eight hours a day,’ or ‘the patient’s going to need a subacute nursing facility.’ … I think our insights are different from voluntary physicians and our face-time with social workers is more efficient.”
Sylvia Krafcik, MSSA, LISW, with MetroHealth Medical Center, Cleveland, says hospitalists are “great to work with because they’re very dedicated to the population they’re caring for, because this is their whole responsibility; they don’t have a private caseload.”
But in her view most hospitalists are focused on patients’ medical conditions and some of them are not as tuned in to all the other aspects of the patient, such as all the psychosocial dynamics.
“A lot of them are, but some aren’t,” Krafcik says. “Especially at MetroHealth, we’re a county hospital. So many of the patients that come here are poor. A lot of them are alcoholics or drug abusers. They’re homeless. They live on the streets. They don’t have a primary doctor. They’re usually not compliant with their medications.”
“Here at Metro we have a lot of patients who have extreme social circumstances that affect their medical issues so much,” says Sara Dunson, MSW, LSW, who also works as a social worker at Metro-Health. “I think the hospitalist has greater insight into the person’s environment and all the social structures that they have at home and that are going on in their life [than other physicians might].”
But there is always room for improvement.
“We had one patient who wasn’t able to read, and he never told anybody this,” says Dunson. “And as social workers, we have more of a way of finding that kind of stuff out from patients than the doctors might. And he kept coming in and coming in and was noncompliant with his medication. We eventually determined that this was why he was noncompliant and was causing all these medical issues. The doctors finally [understood] why this gentleman kept coming in with the same problems and he wasn’t taking care of himself. It wasn’t that he didn’t want to, it was just that he was having problems reading all the medications and all the discharge paperwork, and he was too ashamed to tell anybody. [Once the social workers questioned him and got this] out in the open, we were able to get him help with that.”
The doctors focused on what he was or wasn’t doing, but they hadn’t looked at why he wasn’t adherent, explains Dunson. If hospitalists do that more often, she thinks, they could save time and get better outcomes sooner.
COMMUNICATING WITH PATIENTS AND FAMILIES
“I think where hospitalists are coming from is a whole different mindset than a physician who has mainly an office practice,” said Lingg. “The office practice comes first [for them]. Some of our physicians have huge practices in town. And they’ll visit the hospital very early in the morning or in the evening. ... So if I need something in a case like that, if there was not a hospitalist involved, it would have been separate meetings for the family with the physician … and [with] me at another time.”
To hospitalists, a social worker can serve as an important adjunct in talking to the patient and family. “For example, if [social workers] are giving bad news, they warn the physician first,” says Dr. Rajan. “If they’re going to go in and tell the patient that they’re not going to qualify for any home services, they tell the physician as well so that [the hospitalist will not later be] meeting an angry patient.” In addition, she says, “for critically ill or long-term patients, social workers [can] help family members cope. Sometimes as physicians we don’t have the time or we don’t have the resources to do that.”
But this doesn’t let doctors off the hook in regard to addressing the whole person’s needs. Especially if someone has multiple medical problems, the social worker needs to know the availability and level of support for which the family can be counted.
“Social workers will ask questions such as: Are the families involved? or Is there any family?” says Krafcik. “Do they need to go in a nursing home or do they need 24-hour care at home? Is the family able to provide that? [E]very morning we meet to have team rounds. And the [team] go[es] over every patient on the floor, and then I will ask those questions if the doctor hasn’t given me that information.”
Social workers appreciate and would like hospitalists to do more listening to the patient and family for the aspects of the history and psychosocial status that the social worker will need to know.
TEACHING POINTS
In the course of their interactions, what do hospitalists and social workers teach each other that could lead to working a case more effectively and to the greater satisfaction of all involved?
Most of those we interviewed seem to think that the greatest service hospitalists provide is to teach the social worker the medical components that go along with what the social worker does every day.
“[Social workers] get a better understanding of [whether] someone comes in with heart failure or a fall or a stroke, just by repetition and also education; they get to understand after a while what’s needed for individual medical diagnoses,” says Dr. Flansbaum.
“When I know [better] what the medical condition is,” says Krafcik, “I have an idea of how much help [the patient] would need at home and their ability to function. And I would make sure that the patient gets physical therapy or occupational therapy referral or speech therapy.”
Again, perhaps the area where the social worker most teaches the hospitalist regards available resources to solve problems over and above the purely medical. “They know the social system and the needs of different forms and eligibility and what different patients are entitled to and what the system will provide,” says Dr. Flansbaum.
Dunson believes hospitalists are perceived as being more involved in a holistic way with the patient. “I always stress that it is so important to look at the whole person and not just the medical aspects,” she says. “It’s hard for the doctor sometimes to realize that this person might not be able to afford this medication and that’s why they’re noncompliant and all the other issues. So I think is important to open up to the other aspects of a person’s life and not just the medical aspects.”
CONCLUSION
Social workers’ knowledge of medical and nonmedical resources, both locally and nationally, offer hospitalists essential information that leads to designing more appropriate and effective post-discharge plans. Hospitalists can best team with social workers by consistently keeping in mind the patient’s overall circumstances and informing their colleagues of the medical information that can help social workers do their best work. TH
Writer Andrea Sattinger will write about the effect of poor communication skills in the November issue of The Hospitalist.
Problem Docs
In a survey distributed to 50 member hospitals by Allen Rosenstein, MD, and his colleagues at VHA Inc. (an alliance of 2,400 nonprofit health care organizations) more than 1,500 participants responded to questions pertaining to their colleagues’ behavior.1 Of the 965 respondents to the question Have you ever witnessed disruptive behavior from a physician at your hospital?, nearly 68% said yes. Of the 675 nurses who responded to the question, 86% said they had witnessed it; almost half of the 249 physician respondents said they had witnessed it from their peers. Most respondents estimated the number of either nurses or physicians who exhibited disruptive behavior to be 1%-3%.
Of the 1,416 respondents who answered the question How often does physician disruptive behavior occur at your hospital?, 22% answered “weekly,” 26% answered “1 to 2 times per month,” and 33% answered “1 to 5 times per year.” Interestingly, 11% of the respondents said that such behavior by physicians never occurs, but 8% said it’s a daily occurrence.
—Scott Flanders, associate professor of medicine at the University of Michigan and director of the Hospitalist Program, Ann Arbor
Disruptive Behavior Defined
Disruptive behavior includes anything that interferes with the ability of a healthcare professional to effectively perform his or her duties or any behavior that undermines confidence in the hospital or its workers.2-4 In general, “disruptive” refers to behaviors that are abusive, disrespectful, sexual, angry, critical, negative, inappropriate, or unethical.2 (See “What Is Disruptive Behavior?” p. 40.) Individuals termed “impaired” are those who have active addictions or psychiatric problems and who exhibit the disruptive, intimidating, or abusive behavior.
Most respondents to the above-mentioned survey reported that disruptive behavior had negative or worsening effects on stress, frustration, concentration, communication, collaboration, information transfer, and workplace relationships. (See Figure 1, p. 41.)
“Physicians whose performance persistently falters pose a substantial threat to patient safety that is often unrecognized or unsatisfactorily addressed in hospitals and other healthcare organizations,” writes Lucian Leape, MD, adjunct professor of health policy in the Department of Health Policy and Management at the Harvard School of Public Health.2
“Whoever tells you that they have not experienced any kind of disruptive behavior is either lying or … in neglect, because there are always certain types of disruptive behaviors [among healthcare workers],” says Martin Izakovic, MD, medical director, Hospitalist Program, Mercy Hospital, Iowa City, Iowa.
Effects of Disruptive Behavior
Can we go so far as to say disruptive behavior affects clinical outcomes?
“It has to,” says Scott Flanders, MD, associate professor of medicine at the University of Michigan and director of the hospitalist program, Ann Arbor, and member of SHM’s board of directors. “People clearly understand the importance of teamwork in hospital medicine. If one member of the team is dysfunctional from an emotional intelligence/behavioral standpoint, that drags down the team in its entirety and impacts patient care.”
Providing safe and effective care should be the first priority of all healthcare professionals. Excellent outcomes have been associated with procedural efficiency and the use of evidence-based standards and tools designed to reduce the likelihood of medical error. The effects of work relationships on clinical outcomes are less well documented, but attention to the matter is increasing in parallel with the focus on patient safety.3,5
Dr. Leape, one of the founders of the National Patient Safety Foundation, devotes concerted energy to making organizations aware of the need to upgrade systems to diagnose and treat this problem.2 “Physician performance failures are not rare and pose substantial threats to patient welfare and safety,” he writes. “Few hospitals respond to such failures promptly or effectively. Failure to ensure the quality and safety of the performance of colleagues is a breach of medicine’s fiduciary responsibility to the public.”6
When it comes to the issues of behavior, besides monitoring their own performance, what do hospitalists do when they come up against colleagues whose shortcomings require correction in order for the entire institution to uphold its legal obligation to each patient?
Physician, Heal Thyself
A study published by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) reported that 24% of sentinel events could be attributed to problems referred to as human factors, including communication gaps, staffing issues, and lack of teamwork.2, 5 The March 2004 issue of the Institute for Safe Medication Practice’s (ISMP) Medication Safety Alert reported that 7% of medication errors could be attributed to nurses feeling intimidated by physicians.4 And, as a response to this growing problem, the Institute of Medicine’s groundbreaking report on medical errors and patient safety, To Err is Human, shifted the focus from individual blame to that of preventing errors through efforts to “design safety into systems.”7
Dr. Flanders, who is also associate chief for the Division of General Internal Medicine for Inpatient Programs at the University of Michigan Medical Center (Ann Arbor), certainly understands the need to grapple with these types of issues. He is a member of his institution’s interdisciplinary Medical Staff Quality Committee (MSQC), which works to get a better handle on individual physician-level quality and performance.
“A lot stems from JCAHO’s increased focus on institutions doing a better job of trying to figure out, in short, who’s a good doctor and who’s a bad doctor,” he says, “And having medical staff appointments, privileging, and assessment of clinical skills be something a little more robust than just asking four of your friends if they think you’re a good doctor.”
One of the charges of the MSQC is developing a better system of tracking physicians’ clinical skills down to the individual level, which Dr. Flanders says is a difficult task. But their second charge is even more elusive to track: examining “the range of daily activities, behaviors, and actions that encompass being a physician.” As part of that, the committee deals with interpersonal relations: interactions with other staff and behavioral issues.
Make the Diagnosis, Initiate Treatment
As with most academic medical centers, when someone at MSQC observes a behavioral issue, that person’s supervisor (often a department chair) is the next place for the buck to stop. There are clearly defined lines of communication and “very robust systems” to deal with these kinds of things, says Dr. Flanders.
MSQC is assisting department chairs in dealing with a particular behavior or problem. “It is a venue to vet particular problems and solutions,” he says. Ultimately, if there are repeated transgressions and administration is not satisfied that their directives have been followed, the committee can recommend revoking a physician’s medical staff privileges and implementing a remediation plan.
Those robust systems have not differed in medical institutions for the last 50 years. “I think what has changed is people are less willing to tolerate this persistently,” says Dr. Flanders. “People used to put up with the disruptive physician, the badly behaving physician, and if he was bringing in lots of research dollars or if he was a great scientist, [they’d be more likely to] accept bad behavior.”
With the increased risk of litigation and the increasing scrutiny on patient safety, these offenses can no longer be tolerated.8
At a community hospital, the hierarchies and channels of communication for handling behavioral issues are different. Because of the different atmosphere and mood of a hospitalist department, says Dr. Izakovic, who is also adjunct clinical assistant professor, Department of Internal Medicine, University of Iowa–Carver College of Medicine, Iowa City, “plus word of mouth, it is easier to either enforce or, even more, lead by example [such that] certain behaviors are [encouraged] and certain behavior types are suppressed.”
Michael Zavarin, MD, director of the hospitalist group at Jordan Hospital in Plymouth, Mass., agrees that the environment of a community hospital may be different enough so that handling disruptive behavior also occurs differently than it does in an academic medical center.
Dr. Zavarin’s group is composed of 6.5 full-time day hospitalists and one full-time night hospitalist, as well as two nurse practitioners. Disruptive behavior in his group “really hasn’t been an issue, so I guess it is [dealt with] on an as-needed basis,” he says, and he can only speculate that the proper channel for dealing with situations involving disruptive behavior would be his institution’s medical executive committee.
When Dr. Izakovic faces situations involving disruptive behavior, he says, it is generally an instance in which a hospitalist has “a good intention, but feels pressured by overwork or patient care circumstances, or [has] difficulty communicating or handling the nursing staff … who perceive [the physician’s behavior] as being either threatening or disrespectful or just not called for.”9
He estimates that these instances occur most often when a physician’s expectations are not met regarding duties being performed in a timely manner. Formal complaints are rarely made in his group—maybe two or three times a year. In those cases, he is responsible for formal follow-up, which requires having a one-on-one conversation with the physician and reporting back to the risk management department. But he prefers doing what is necessary to avoid a situation getting to that stage. Informal behavior-related events happen at least monthly, he estimates. “I’d rather hear earlier than later, with no formal complaint, no formal channel,” says Dr. Izakovic.
Blow the Whistle
What are the political ramifications of blowing the whistle on a disruptive colleague? The University of Michigan’s MSQC was created largely to help get at that issue and to create a place where such subjects can be brought up anonymously. [It can be done] if the reporting person wishes. In most situations, there has been a concerted effort against backlash just as there is when incidents and errors are reported to improve or maintain patient safety.
“As the patient safety culture changes, and I think it is changing, it’s going to facilitate culture change on this issue, too,” says Dr. Flanders, “because I think people are beginning to recognize, appropriately so, that some of these behavioral issues are safety issues.”
Do nurses feel comfortable reporting such instances? “I think it depends on the personality,” says Dr. Izakovic. “Some do, and some feel less comfortable; there are nurses who never complain and nurses who always complain, like doctors and everybody else. But I think that the climate is changing [so] that raising your voice and pointing toward deficiency and/or imperfection is becoming, if not [socially] acceptable, then [at least] a standard of behavior.”
Behavior, Safety, and Quality
“Communication is the key to success in today’s medicine,” says Dr. Izakovic. “Specifically among hospitalists: You communicate with the family physician, the patient, the referring specialist, or specialist that you called, the family, nurses, and patients all around the hospital.” And although communication is the most important part of the hospitalist’s practice, he says, “it sometimes leads to tension, and it’s not as much the message that you want to convey as the form [you use] and how it is transferred.”
Nurses are key stakeholders in reporting these behaviors, just as they are encouraged to report errors as an expression of their professionalism. Certainly, Dr. Flanders says, reporting a behavioral incident is “a lot more personal and less tangible than reporting a wrong dose on a medication.”
He has noticed a dramatic increase in the number of messages he receives about inappropriate or dangerous behavior among physicians. Everyone has a bad day from time to time, he says, but at the end of the year, “if I have one physician who has been mentioned 15 times, that helps me assess that person overall as a professional and be able to say, ‘Listen, there may be some red flags here’ and [then we can] begin to intervene and try to change that behavior.”
Effective systems employed to adequately address performance problems should be fair, objective, and responsive, writes Dr. Leape.2,6 Strategies available to handle incidents of disruptive behavior include adopting performance standards for behavior as well as competence. All physicians should be required to acknowledge in writing that they have read and understood these standards and that persistent failure to uphold them will result in loss of clinical privileges. Adherence to standards should be monitored annually and provided confidentially to each individual. Finally, assessment and treatment programs must be available to manage all the underlying causes of sub-par performance. The long-term objective is to enable physicians to continue to practice, as opposed to attempting to “weed them out.”
Prevention
According to Balazs Zsenits, MD, director, Division of Hospital Medicine at Rochester General Hospital, Rochester, N.Y., two mechanisms should be applied when discussing the prevention of disruptive behavior.
“First, physician selection should be conducted by a thorough interview process,” he says, “including at least a full-day face-to-face interview, discussion with previous employers, assessment of team-participation experience, and communication skills.”
Also, you need to clarify your expectations by means of “written policies, leading by example, promoting this culture in meetings, etc., and proactively monitoring performance,” says Dr. Zsenits. That means talking with doctors, nurses, and families and actively looking for feedback. “This process is time-intensive and may be under-recognized during resource allocation, but I believe it is a tool that may prevent this and many other common problems from growing out of control.”
A director of a hospital medicine group may have to deal with the perception of an escalating number of complaints about physician behaviors. “The growth of a hospitalist program that goes from seeing a small fraction of patients within a hospital to seeing the majority of medical admissions creates challenges beyond just simply managing the increased number of doctors and complaints,” says Dr. Zsenits. “Our co-workers and stakeholders might develop an impression that ‘most doctor problems’ in the hospital are related to the hospitalists. Even if this is [because] the hospitalists actually take care of most patients in house, and each hospitalist takes care of many more patients than private attendings used to, avoiding the perception that this single group is associated with most complaints is a difficult task.”
Although hospitalists’ focus on teamwork and quality of care may improve the actual statistics, he adds, “some factors may create more feedback, including more complaints; for example, being new docs to patients and relatives at times of stress, and having a closer working relationship with nurses, which may [be problematic] by creating heightened expectations or [because you are working with] a young workforce … .”
Conclusion
Hospitalists can increase their capacities to observe, document, address, consult on, and refer instances of disruptive behavior appropriately. Although incidents of disruption may be relatively infrequent and may involve a few perpetrators, when they occur they should be addressed promptly and appropriately. Strategies to address the issue of disruptive behavior include conducting an organizational assessment; opening up lines of communication, including inviting nurses as well as physicians to submit anonymous notes or suggestions; and increasing staff awareness of the nature and severity of the issue.
As Dr. Flanders and colleagues have written, hospitalists should be the “fulcrum” we use to improve patient safety.10 The advantage of having just a few hospitalists influencing the healthcare of many patients can be a detriment if a colleague is a “problem doctor.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Rosenstein AH, O'Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006 Jul;203(1):96-105. Epub 2006 Jun 5.
- Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Intern Med. 2006 Jan 17;144(2):107-115.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthcare. 2006 Jul-Aug;3:16-24.
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I) ISMP Medication Safety Alert. Available at: www.ismp.org/MSAarticles/intimidation.htm. Accessed on October 16, 2006.
- Rosenstein AH, O'Daniel M. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians. Am J Nurs. 2005 Jan;105(1):54-64; quiz 64-55.
- Leape LL. Physician self-examination. Int J Qual Health Care. 1998;10(4):289-290.
- Kohn L, Corrigan J, Donaldson M, eds. To Err is Human: Building a Safer Health System. Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: National Academies Press; 2000.
- Linney BJ. Confronting the disruptive physician. Physician Exec. 1997 Sep-Oct;23(7):55-58.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-251.
- Flanders SA, Kaufman SR, Saint S. Hospitalists as emerging leaders in patient safety: targeting a few to affect many. J Patient Safety. 2005 Jun;1(2):78-82.
In a survey distributed to 50 member hospitals by Allen Rosenstein, MD, and his colleagues at VHA Inc. (an alliance of 2,400 nonprofit health care organizations) more than 1,500 participants responded to questions pertaining to their colleagues’ behavior.1 Of the 965 respondents to the question Have you ever witnessed disruptive behavior from a physician at your hospital?, nearly 68% said yes. Of the 675 nurses who responded to the question, 86% said they had witnessed it; almost half of the 249 physician respondents said they had witnessed it from their peers. Most respondents estimated the number of either nurses or physicians who exhibited disruptive behavior to be 1%-3%.
Of the 1,416 respondents who answered the question How often does physician disruptive behavior occur at your hospital?, 22% answered “weekly,” 26% answered “1 to 2 times per month,” and 33% answered “1 to 5 times per year.” Interestingly, 11% of the respondents said that such behavior by physicians never occurs, but 8% said it’s a daily occurrence.
—Scott Flanders, associate professor of medicine at the University of Michigan and director of the Hospitalist Program, Ann Arbor
Disruptive Behavior Defined
Disruptive behavior includes anything that interferes with the ability of a healthcare professional to effectively perform his or her duties or any behavior that undermines confidence in the hospital or its workers.2-4 In general, “disruptive” refers to behaviors that are abusive, disrespectful, sexual, angry, critical, negative, inappropriate, or unethical.2 (See “What Is Disruptive Behavior?” p. 40.) Individuals termed “impaired” are those who have active addictions or psychiatric problems and who exhibit the disruptive, intimidating, or abusive behavior.
Most respondents to the above-mentioned survey reported that disruptive behavior had negative or worsening effects on stress, frustration, concentration, communication, collaboration, information transfer, and workplace relationships. (See Figure 1, p. 41.)
“Physicians whose performance persistently falters pose a substantial threat to patient safety that is often unrecognized or unsatisfactorily addressed in hospitals and other healthcare organizations,” writes Lucian Leape, MD, adjunct professor of health policy in the Department of Health Policy and Management at the Harvard School of Public Health.2
“Whoever tells you that they have not experienced any kind of disruptive behavior is either lying or … in neglect, because there are always certain types of disruptive behaviors [among healthcare workers],” says Martin Izakovic, MD, medical director, Hospitalist Program, Mercy Hospital, Iowa City, Iowa.
Effects of Disruptive Behavior
Can we go so far as to say disruptive behavior affects clinical outcomes?
“It has to,” says Scott Flanders, MD, associate professor of medicine at the University of Michigan and director of the hospitalist program, Ann Arbor, and member of SHM’s board of directors. “People clearly understand the importance of teamwork in hospital medicine. If one member of the team is dysfunctional from an emotional intelligence/behavioral standpoint, that drags down the team in its entirety and impacts patient care.”
Providing safe and effective care should be the first priority of all healthcare professionals. Excellent outcomes have been associated with procedural efficiency and the use of evidence-based standards and tools designed to reduce the likelihood of medical error. The effects of work relationships on clinical outcomes are less well documented, but attention to the matter is increasing in parallel with the focus on patient safety.3,5
Dr. Leape, one of the founders of the National Patient Safety Foundation, devotes concerted energy to making organizations aware of the need to upgrade systems to diagnose and treat this problem.2 “Physician performance failures are not rare and pose substantial threats to patient welfare and safety,” he writes. “Few hospitals respond to such failures promptly or effectively. Failure to ensure the quality and safety of the performance of colleagues is a breach of medicine’s fiduciary responsibility to the public.”6
When it comes to the issues of behavior, besides monitoring their own performance, what do hospitalists do when they come up against colleagues whose shortcomings require correction in order for the entire institution to uphold its legal obligation to each patient?
Physician, Heal Thyself
A study published by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) reported that 24% of sentinel events could be attributed to problems referred to as human factors, including communication gaps, staffing issues, and lack of teamwork.2, 5 The March 2004 issue of the Institute for Safe Medication Practice’s (ISMP) Medication Safety Alert reported that 7% of medication errors could be attributed to nurses feeling intimidated by physicians.4 And, as a response to this growing problem, the Institute of Medicine’s groundbreaking report on medical errors and patient safety, To Err is Human, shifted the focus from individual blame to that of preventing errors through efforts to “design safety into systems.”7
Dr. Flanders, who is also associate chief for the Division of General Internal Medicine for Inpatient Programs at the University of Michigan Medical Center (Ann Arbor), certainly understands the need to grapple with these types of issues. He is a member of his institution’s interdisciplinary Medical Staff Quality Committee (MSQC), which works to get a better handle on individual physician-level quality and performance.
“A lot stems from JCAHO’s increased focus on institutions doing a better job of trying to figure out, in short, who’s a good doctor and who’s a bad doctor,” he says, “And having medical staff appointments, privileging, and assessment of clinical skills be something a little more robust than just asking four of your friends if they think you’re a good doctor.”
One of the charges of the MSQC is developing a better system of tracking physicians’ clinical skills down to the individual level, which Dr. Flanders says is a difficult task. But their second charge is even more elusive to track: examining “the range of daily activities, behaviors, and actions that encompass being a physician.” As part of that, the committee deals with interpersonal relations: interactions with other staff and behavioral issues.
Make the Diagnosis, Initiate Treatment
As with most academic medical centers, when someone at MSQC observes a behavioral issue, that person’s supervisor (often a department chair) is the next place for the buck to stop. There are clearly defined lines of communication and “very robust systems” to deal with these kinds of things, says Dr. Flanders.
MSQC is assisting department chairs in dealing with a particular behavior or problem. “It is a venue to vet particular problems and solutions,” he says. Ultimately, if there are repeated transgressions and administration is not satisfied that their directives have been followed, the committee can recommend revoking a physician’s medical staff privileges and implementing a remediation plan.
Those robust systems have not differed in medical institutions for the last 50 years. “I think what has changed is people are less willing to tolerate this persistently,” says Dr. Flanders. “People used to put up with the disruptive physician, the badly behaving physician, and if he was bringing in lots of research dollars or if he was a great scientist, [they’d be more likely to] accept bad behavior.”
With the increased risk of litigation and the increasing scrutiny on patient safety, these offenses can no longer be tolerated.8
At a community hospital, the hierarchies and channels of communication for handling behavioral issues are different. Because of the different atmosphere and mood of a hospitalist department, says Dr. Izakovic, who is also adjunct clinical assistant professor, Department of Internal Medicine, University of Iowa–Carver College of Medicine, Iowa City, “plus word of mouth, it is easier to either enforce or, even more, lead by example [such that] certain behaviors are [encouraged] and certain behavior types are suppressed.”
Michael Zavarin, MD, director of the hospitalist group at Jordan Hospital in Plymouth, Mass., agrees that the environment of a community hospital may be different enough so that handling disruptive behavior also occurs differently than it does in an academic medical center.
Dr. Zavarin’s group is composed of 6.5 full-time day hospitalists and one full-time night hospitalist, as well as two nurse practitioners. Disruptive behavior in his group “really hasn’t been an issue, so I guess it is [dealt with] on an as-needed basis,” he says, and he can only speculate that the proper channel for dealing with situations involving disruptive behavior would be his institution’s medical executive committee.
When Dr. Izakovic faces situations involving disruptive behavior, he says, it is generally an instance in which a hospitalist has “a good intention, but feels pressured by overwork or patient care circumstances, or [has] difficulty communicating or handling the nursing staff … who perceive [the physician’s behavior] as being either threatening or disrespectful or just not called for.”9
He estimates that these instances occur most often when a physician’s expectations are not met regarding duties being performed in a timely manner. Formal complaints are rarely made in his group—maybe two or three times a year. In those cases, he is responsible for formal follow-up, which requires having a one-on-one conversation with the physician and reporting back to the risk management department. But he prefers doing what is necessary to avoid a situation getting to that stage. Informal behavior-related events happen at least monthly, he estimates. “I’d rather hear earlier than later, with no formal complaint, no formal channel,” says Dr. Izakovic.
Blow the Whistle
What are the political ramifications of blowing the whistle on a disruptive colleague? The University of Michigan’s MSQC was created largely to help get at that issue and to create a place where such subjects can be brought up anonymously. [It can be done] if the reporting person wishes. In most situations, there has been a concerted effort against backlash just as there is when incidents and errors are reported to improve or maintain patient safety.
“As the patient safety culture changes, and I think it is changing, it’s going to facilitate culture change on this issue, too,” says Dr. Flanders, “because I think people are beginning to recognize, appropriately so, that some of these behavioral issues are safety issues.”
Do nurses feel comfortable reporting such instances? “I think it depends on the personality,” says Dr. Izakovic. “Some do, and some feel less comfortable; there are nurses who never complain and nurses who always complain, like doctors and everybody else. But I think that the climate is changing [so] that raising your voice and pointing toward deficiency and/or imperfection is becoming, if not [socially] acceptable, then [at least] a standard of behavior.”
Behavior, Safety, and Quality
“Communication is the key to success in today’s medicine,” says Dr. Izakovic. “Specifically among hospitalists: You communicate with the family physician, the patient, the referring specialist, or specialist that you called, the family, nurses, and patients all around the hospital.” And although communication is the most important part of the hospitalist’s practice, he says, “it sometimes leads to tension, and it’s not as much the message that you want to convey as the form [you use] and how it is transferred.”
Nurses are key stakeholders in reporting these behaviors, just as they are encouraged to report errors as an expression of their professionalism. Certainly, Dr. Flanders says, reporting a behavioral incident is “a lot more personal and less tangible than reporting a wrong dose on a medication.”
He has noticed a dramatic increase in the number of messages he receives about inappropriate or dangerous behavior among physicians. Everyone has a bad day from time to time, he says, but at the end of the year, “if I have one physician who has been mentioned 15 times, that helps me assess that person overall as a professional and be able to say, ‘Listen, there may be some red flags here’ and [then we can] begin to intervene and try to change that behavior.”
Effective systems employed to adequately address performance problems should be fair, objective, and responsive, writes Dr. Leape.2,6 Strategies available to handle incidents of disruptive behavior include adopting performance standards for behavior as well as competence. All physicians should be required to acknowledge in writing that they have read and understood these standards and that persistent failure to uphold them will result in loss of clinical privileges. Adherence to standards should be monitored annually and provided confidentially to each individual. Finally, assessment and treatment programs must be available to manage all the underlying causes of sub-par performance. The long-term objective is to enable physicians to continue to practice, as opposed to attempting to “weed them out.”
Prevention
According to Balazs Zsenits, MD, director, Division of Hospital Medicine at Rochester General Hospital, Rochester, N.Y., two mechanisms should be applied when discussing the prevention of disruptive behavior.
“First, physician selection should be conducted by a thorough interview process,” he says, “including at least a full-day face-to-face interview, discussion with previous employers, assessment of team-participation experience, and communication skills.”
Also, you need to clarify your expectations by means of “written policies, leading by example, promoting this culture in meetings, etc., and proactively monitoring performance,” says Dr. Zsenits. That means talking with doctors, nurses, and families and actively looking for feedback. “This process is time-intensive and may be under-recognized during resource allocation, but I believe it is a tool that may prevent this and many other common problems from growing out of control.”
A director of a hospital medicine group may have to deal with the perception of an escalating number of complaints about physician behaviors. “The growth of a hospitalist program that goes from seeing a small fraction of patients within a hospital to seeing the majority of medical admissions creates challenges beyond just simply managing the increased number of doctors and complaints,” says Dr. Zsenits. “Our co-workers and stakeholders might develop an impression that ‘most doctor problems’ in the hospital are related to the hospitalists. Even if this is [because] the hospitalists actually take care of most patients in house, and each hospitalist takes care of many more patients than private attendings used to, avoiding the perception that this single group is associated with most complaints is a difficult task.”
Although hospitalists’ focus on teamwork and quality of care may improve the actual statistics, he adds, “some factors may create more feedback, including more complaints; for example, being new docs to patients and relatives at times of stress, and having a closer working relationship with nurses, which may [be problematic] by creating heightened expectations or [because you are working with] a young workforce … .”
Conclusion
Hospitalists can increase their capacities to observe, document, address, consult on, and refer instances of disruptive behavior appropriately. Although incidents of disruption may be relatively infrequent and may involve a few perpetrators, when they occur they should be addressed promptly and appropriately. Strategies to address the issue of disruptive behavior include conducting an organizational assessment; opening up lines of communication, including inviting nurses as well as physicians to submit anonymous notes or suggestions; and increasing staff awareness of the nature and severity of the issue.
As Dr. Flanders and colleagues have written, hospitalists should be the “fulcrum” we use to improve patient safety.10 The advantage of having just a few hospitalists influencing the healthcare of many patients can be a detriment if a colleague is a “problem doctor.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Rosenstein AH, O'Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006 Jul;203(1):96-105. Epub 2006 Jun 5.
- Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Intern Med. 2006 Jan 17;144(2):107-115.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthcare. 2006 Jul-Aug;3:16-24.
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I) ISMP Medication Safety Alert. Available at: www.ismp.org/MSAarticles/intimidation.htm. Accessed on October 16, 2006.
- Rosenstein AH, O'Daniel M. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians. Am J Nurs. 2005 Jan;105(1):54-64; quiz 64-55.
- Leape LL. Physician self-examination. Int J Qual Health Care. 1998;10(4):289-290.
- Kohn L, Corrigan J, Donaldson M, eds. To Err is Human: Building a Safer Health System. Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: National Academies Press; 2000.
- Linney BJ. Confronting the disruptive physician. Physician Exec. 1997 Sep-Oct;23(7):55-58.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-251.
- Flanders SA, Kaufman SR, Saint S. Hospitalists as emerging leaders in patient safety: targeting a few to affect many. J Patient Safety. 2005 Jun;1(2):78-82.
In a survey distributed to 50 member hospitals by Allen Rosenstein, MD, and his colleagues at VHA Inc. (an alliance of 2,400 nonprofit health care organizations) more than 1,500 participants responded to questions pertaining to their colleagues’ behavior.1 Of the 965 respondents to the question Have you ever witnessed disruptive behavior from a physician at your hospital?, nearly 68% said yes. Of the 675 nurses who responded to the question, 86% said they had witnessed it; almost half of the 249 physician respondents said they had witnessed it from their peers. Most respondents estimated the number of either nurses or physicians who exhibited disruptive behavior to be 1%-3%.
Of the 1,416 respondents who answered the question How often does physician disruptive behavior occur at your hospital?, 22% answered “weekly,” 26% answered “1 to 2 times per month,” and 33% answered “1 to 5 times per year.” Interestingly, 11% of the respondents said that such behavior by physicians never occurs, but 8% said it’s a daily occurrence.
—Scott Flanders, associate professor of medicine at the University of Michigan and director of the Hospitalist Program, Ann Arbor
Disruptive Behavior Defined
Disruptive behavior includes anything that interferes with the ability of a healthcare professional to effectively perform his or her duties or any behavior that undermines confidence in the hospital or its workers.2-4 In general, “disruptive” refers to behaviors that are abusive, disrespectful, sexual, angry, critical, negative, inappropriate, or unethical.2 (See “What Is Disruptive Behavior?” p. 40.) Individuals termed “impaired” are those who have active addictions or psychiatric problems and who exhibit the disruptive, intimidating, or abusive behavior.
Most respondents to the above-mentioned survey reported that disruptive behavior had negative or worsening effects on stress, frustration, concentration, communication, collaboration, information transfer, and workplace relationships. (See Figure 1, p. 41.)
“Physicians whose performance persistently falters pose a substantial threat to patient safety that is often unrecognized or unsatisfactorily addressed in hospitals and other healthcare organizations,” writes Lucian Leape, MD, adjunct professor of health policy in the Department of Health Policy and Management at the Harvard School of Public Health.2
“Whoever tells you that they have not experienced any kind of disruptive behavior is either lying or … in neglect, because there are always certain types of disruptive behaviors [among healthcare workers],” says Martin Izakovic, MD, medical director, Hospitalist Program, Mercy Hospital, Iowa City, Iowa.
Effects of Disruptive Behavior
Can we go so far as to say disruptive behavior affects clinical outcomes?
“It has to,” says Scott Flanders, MD, associate professor of medicine at the University of Michigan and director of the hospitalist program, Ann Arbor, and member of SHM’s board of directors. “People clearly understand the importance of teamwork in hospital medicine. If one member of the team is dysfunctional from an emotional intelligence/behavioral standpoint, that drags down the team in its entirety and impacts patient care.”
Providing safe and effective care should be the first priority of all healthcare professionals. Excellent outcomes have been associated with procedural efficiency and the use of evidence-based standards and tools designed to reduce the likelihood of medical error. The effects of work relationships on clinical outcomes are less well documented, but attention to the matter is increasing in parallel with the focus on patient safety.3,5
Dr. Leape, one of the founders of the National Patient Safety Foundation, devotes concerted energy to making organizations aware of the need to upgrade systems to diagnose and treat this problem.2 “Physician performance failures are not rare and pose substantial threats to patient welfare and safety,” he writes. “Few hospitals respond to such failures promptly or effectively. Failure to ensure the quality and safety of the performance of colleagues is a breach of medicine’s fiduciary responsibility to the public.”6
When it comes to the issues of behavior, besides monitoring their own performance, what do hospitalists do when they come up against colleagues whose shortcomings require correction in order for the entire institution to uphold its legal obligation to each patient?
Physician, Heal Thyself
A study published by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) reported that 24% of sentinel events could be attributed to problems referred to as human factors, including communication gaps, staffing issues, and lack of teamwork.2, 5 The March 2004 issue of the Institute for Safe Medication Practice’s (ISMP) Medication Safety Alert reported that 7% of medication errors could be attributed to nurses feeling intimidated by physicians.4 And, as a response to this growing problem, the Institute of Medicine’s groundbreaking report on medical errors and patient safety, To Err is Human, shifted the focus from individual blame to that of preventing errors through efforts to “design safety into systems.”7
Dr. Flanders, who is also associate chief for the Division of General Internal Medicine for Inpatient Programs at the University of Michigan Medical Center (Ann Arbor), certainly understands the need to grapple with these types of issues. He is a member of his institution’s interdisciplinary Medical Staff Quality Committee (MSQC), which works to get a better handle on individual physician-level quality and performance.
“A lot stems from JCAHO’s increased focus on institutions doing a better job of trying to figure out, in short, who’s a good doctor and who’s a bad doctor,” he says, “And having medical staff appointments, privileging, and assessment of clinical skills be something a little more robust than just asking four of your friends if they think you’re a good doctor.”
One of the charges of the MSQC is developing a better system of tracking physicians’ clinical skills down to the individual level, which Dr. Flanders says is a difficult task. But their second charge is even more elusive to track: examining “the range of daily activities, behaviors, and actions that encompass being a physician.” As part of that, the committee deals with interpersonal relations: interactions with other staff and behavioral issues.
Make the Diagnosis, Initiate Treatment
As with most academic medical centers, when someone at MSQC observes a behavioral issue, that person’s supervisor (often a department chair) is the next place for the buck to stop. There are clearly defined lines of communication and “very robust systems” to deal with these kinds of things, says Dr. Flanders.
MSQC is assisting department chairs in dealing with a particular behavior or problem. “It is a venue to vet particular problems and solutions,” he says. Ultimately, if there are repeated transgressions and administration is not satisfied that their directives have been followed, the committee can recommend revoking a physician’s medical staff privileges and implementing a remediation plan.
Those robust systems have not differed in medical institutions for the last 50 years. “I think what has changed is people are less willing to tolerate this persistently,” says Dr. Flanders. “People used to put up with the disruptive physician, the badly behaving physician, and if he was bringing in lots of research dollars or if he was a great scientist, [they’d be more likely to] accept bad behavior.”
With the increased risk of litigation and the increasing scrutiny on patient safety, these offenses can no longer be tolerated.8
At a community hospital, the hierarchies and channels of communication for handling behavioral issues are different. Because of the different atmosphere and mood of a hospitalist department, says Dr. Izakovic, who is also adjunct clinical assistant professor, Department of Internal Medicine, University of Iowa–Carver College of Medicine, Iowa City, “plus word of mouth, it is easier to either enforce or, even more, lead by example [such that] certain behaviors are [encouraged] and certain behavior types are suppressed.”
Michael Zavarin, MD, director of the hospitalist group at Jordan Hospital in Plymouth, Mass., agrees that the environment of a community hospital may be different enough so that handling disruptive behavior also occurs differently than it does in an academic medical center.
Dr. Zavarin’s group is composed of 6.5 full-time day hospitalists and one full-time night hospitalist, as well as two nurse practitioners. Disruptive behavior in his group “really hasn’t been an issue, so I guess it is [dealt with] on an as-needed basis,” he says, and he can only speculate that the proper channel for dealing with situations involving disruptive behavior would be his institution’s medical executive committee.
When Dr. Izakovic faces situations involving disruptive behavior, he says, it is generally an instance in which a hospitalist has “a good intention, but feels pressured by overwork or patient care circumstances, or [has] difficulty communicating or handling the nursing staff … who perceive [the physician’s behavior] as being either threatening or disrespectful or just not called for.”9
He estimates that these instances occur most often when a physician’s expectations are not met regarding duties being performed in a timely manner. Formal complaints are rarely made in his group—maybe two or three times a year. In those cases, he is responsible for formal follow-up, which requires having a one-on-one conversation with the physician and reporting back to the risk management department. But he prefers doing what is necessary to avoid a situation getting to that stage. Informal behavior-related events happen at least monthly, he estimates. “I’d rather hear earlier than later, with no formal complaint, no formal channel,” says Dr. Izakovic.
Blow the Whistle
What are the political ramifications of blowing the whistle on a disruptive colleague? The University of Michigan’s MSQC was created largely to help get at that issue and to create a place where such subjects can be brought up anonymously. [It can be done] if the reporting person wishes. In most situations, there has been a concerted effort against backlash just as there is when incidents and errors are reported to improve or maintain patient safety.
“As the patient safety culture changes, and I think it is changing, it’s going to facilitate culture change on this issue, too,” says Dr. Flanders, “because I think people are beginning to recognize, appropriately so, that some of these behavioral issues are safety issues.”
Do nurses feel comfortable reporting such instances? “I think it depends on the personality,” says Dr. Izakovic. “Some do, and some feel less comfortable; there are nurses who never complain and nurses who always complain, like doctors and everybody else. But I think that the climate is changing [so] that raising your voice and pointing toward deficiency and/or imperfection is becoming, if not [socially] acceptable, then [at least] a standard of behavior.”
Behavior, Safety, and Quality
“Communication is the key to success in today’s medicine,” says Dr. Izakovic. “Specifically among hospitalists: You communicate with the family physician, the patient, the referring specialist, or specialist that you called, the family, nurses, and patients all around the hospital.” And although communication is the most important part of the hospitalist’s practice, he says, “it sometimes leads to tension, and it’s not as much the message that you want to convey as the form [you use] and how it is transferred.”
Nurses are key stakeholders in reporting these behaviors, just as they are encouraged to report errors as an expression of their professionalism. Certainly, Dr. Flanders says, reporting a behavioral incident is “a lot more personal and less tangible than reporting a wrong dose on a medication.”
He has noticed a dramatic increase in the number of messages he receives about inappropriate or dangerous behavior among physicians. Everyone has a bad day from time to time, he says, but at the end of the year, “if I have one physician who has been mentioned 15 times, that helps me assess that person overall as a professional and be able to say, ‘Listen, there may be some red flags here’ and [then we can] begin to intervene and try to change that behavior.”
Effective systems employed to adequately address performance problems should be fair, objective, and responsive, writes Dr. Leape.2,6 Strategies available to handle incidents of disruptive behavior include adopting performance standards for behavior as well as competence. All physicians should be required to acknowledge in writing that they have read and understood these standards and that persistent failure to uphold them will result in loss of clinical privileges. Adherence to standards should be monitored annually and provided confidentially to each individual. Finally, assessment and treatment programs must be available to manage all the underlying causes of sub-par performance. The long-term objective is to enable physicians to continue to practice, as opposed to attempting to “weed them out.”
Prevention
According to Balazs Zsenits, MD, director, Division of Hospital Medicine at Rochester General Hospital, Rochester, N.Y., two mechanisms should be applied when discussing the prevention of disruptive behavior.
“First, physician selection should be conducted by a thorough interview process,” he says, “including at least a full-day face-to-face interview, discussion with previous employers, assessment of team-participation experience, and communication skills.”
Also, you need to clarify your expectations by means of “written policies, leading by example, promoting this culture in meetings, etc., and proactively monitoring performance,” says Dr. Zsenits. That means talking with doctors, nurses, and families and actively looking for feedback. “This process is time-intensive and may be under-recognized during resource allocation, but I believe it is a tool that may prevent this and many other common problems from growing out of control.”
A director of a hospital medicine group may have to deal with the perception of an escalating number of complaints about physician behaviors. “The growth of a hospitalist program that goes from seeing a small fraction of patients within a hospital to seeing the majority of medical admissions creates challenges beyond just simply managing the increased number of doctors and complaints,” says Dr. Zsenits. “Our co-workers and stakeholders might develop an impression that ‘most doctor problems’ in the hospital are related to the hospitalists. Even if this is [because] the hospitalists actually take care of most patients in house, and each hospitalist takes care of many more patients than private attendings used to, avoiding the perception that this single group is associated with most complaints is a difficult task.”
Although hospitalists’ focus on teamwork and quality of care may improve the actual statistics, he adds, “some factors may create more feedback, including more complaints; for example, being new docs to patients and relatives at times of stress, and having a closer working relationship with nurses, which may [be problematic] by creating heightened expectations or [because you are working with] a young workforce … .”
Conclusion
Hospitalists can increase their capacities to observe, document, address, consult on, and refer instances of disruptive behavior appropriately. Although incidents of disruption may be relatively infrequent and may involve a few perpetrators, when they occur they should be addressed promptly and appropriately. Strategies to address the issue of disruptive behavior include conducting an organizational assessment; opening up lines of communication, including inviting nurses as well as physicians to submit anonymous notes or suggestions; and increasing staff awareness of the nature and severity of the issue.
As Dr. Flanders and colleagues have written, hospitalists should be the “fulcrum” we use to improve patient safety.10 The advantage of having just a few hospitalists influencing the healthcare of many patients can be a detriment if a colleague is a “problem doctor.” TH
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Rosenstein AH, O'Daniel M. Impact and implications of disruptive behavior in the perioperative arena. J Am Coll Surg. 2006 Jul;203(1):96-105. Epub 2006 Jun 5.
- Leape LL, Fromson JA. Problem doctors: is there a system-level solution? Ann Intern Med. 2006 Jan 17;144(2):107-115.
- Porto G, Lauve R. Disruptive clinician behavior: a persistent threat to patient safety. Patient Safety Qual Healthcare. 2006 Jul-Aug;3:16-24.
- Institute for Safe Medication Practice. Intimidation: practitioners speak up about this unresolved problem (Part I) ISMP Medication Safety Alert. Available at: www.ismp.org/MSAarticles/intimidation.htm. Accessed on October 16, 2006.
- Rosenstein AH, O'Daniel M. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians. Am J Nurs. 2005 Jan;105(1):54-64; quiz 64-55.
- Leape LL. Physician self-examination. Int J Qual Health Care. 1998;10(4):289-290.
- Kohn L, Corrigan J, Donaldson M, eds. To Err is Human: Building a Safer Health System. Committee on Quality of Health Care in America, Institute of Medicine. Washington, DC: National Academies Press; 2000.
- Linney BJ. Confronting the disruptive physician. Physician Exec. 1997 Sep-Oct;23(7):55-58.
- Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. Results of the Harvard Medical Practice Study III. N Engl J Med. 1991 Jul 25;325(4):245-251.
- Flanders SA, Kaufman SR, Saint S. Hospitalists as emerging leaders in patient safety: targeting a few to affect many. J Patient Safety. 2005 Jun;1(2):78-82.
Subtle Skills
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Safety Sentries
At Mercy Hospital in Iowa City, Iowa, the implementation of safety and quality systems is “stirring up the pot,” says Mercy hospitalist and medical director Martin Izakovic, MD.
He has been recruited to supervise Mercy’s latest safety initiatives, including electronic medical records, pay-for-performance measures, development of treatment protocols, standardization of care, and deep-vein thrombosis prophylaxis.
Hospitalists at Mercy face the challenges their peers around the country face in their quest to improve quality and safeguard patients. The leader in these areas needs to be a role model and respected peer for the physicians he or she must lead day after day, says Dr. Izakovic.
How do hospitalists, who are so well-positioned to become leaders in patient safety, develop in that direction?
“The biggest challenge I see is the spectrum of polarization between clinicians and administrators,” he says. “One of the most important qualities that a patient safety officer needs is the ability to overbridge the doctors on one hand and the administrators on the other.”
What They Need
A patient safety officer (PSO) requires a critical mix of clinical and administrative skills, says Peter B. Angood, MD, vice president and chief patient safety officer for The Joint Commission, in Oakbrook, Ill.
On the clinical side, the hospitalist who wishes to be a PSO needs more than awareness of safety and quality improvement processes. He or she must be knowledgeable about and conversant in safety science in industries beyond healthcare. That expertise needs to encompass leadership, behaviors and cultures, human factors, and process redesign or systems engineering. Important, too, is training in how to corral the pieces of an organization and ensure they operate well together.
An understanding of organizational behavior is of great value. The potential PSO should understand how the key players interact: the board of directors with chief executives, chief executives with senior management, senior management with all staff (including the allied professionals), and medical staff with the organization as a whole.
“Because safety is a systemwide process, the patient safety [person] is pivotal in forming a hub from which much of the quality, safety, and process improvement occurs,” says Dr. Angood.
Jason Adelman, MD, MS, former hospitalist and current PSO at Montefiore Medical Center in New York City, says developing patient safety leaders should embrace technology. “Pay attention to the latest and greatest ideas, products, and services,” he urges. “Come up with strategic plans to implement in healthcare, get the information quickly into the hands of physicians, have physicians report, and include forcing functions [whereby computers will not process to completion when key data are missing].”
Above all, the patient safety officer must train to be a change agent. “Influencing patient safety means you have to be there in the capital-allocation process,” says David Shulkin, MD, chief executive officer at Beth Israel Medical Center in New York City. “You have to be there when they’re designing facilities. You have to understand your human resource policies and the skill sets and aptitudes of the people that the hospital is hiring. To be a good patient safety officer, the training needs to involve broad exposure with a slant toward operations.”
Build a Bridge
As a young physician who wanted to develop as a leader in the field of quality and safety, Dr. Shulkin had to forge his own path. In 1992, after he became chief medical officer (CMO) at the Hospital of the University of Pennsylvania in Philadelphia, he fielded several inquiries a month from young physicians who wanted to pursue a similar career. In response to that need, he designed a quality improvement/patient safety fellowship at his school.
David Bernard, MD, now chief medical officer at Beth Israel, had been practicing medicine for 30 years when at age 50 he took a year’s leave of absence from Boston University and enrolled as Dr. Shulkin’s first fellow in 1994. Dr. Bernard, a nephrologist, was a vice dean in the school of medicine at Boston University Medical Center, a hospital vice president for clinical affairs, and a senior clinician in his specialty group.
Drs. Shulkin and Bernard left the University of Pennsylvania in 1999 to take the concepts of quality transparency to a higher level and formed DoctorQuality Inc. in Conshohocken, Pa. To continue their work, DoctorQuality funded the fellowship. In 2005 when Dr. Shulkin went to Beth Israel in New York, the fellowship was restarted as the Don Hoskins Quality Improvement/Patient Safety program and funded for five years with private philanthropy.
Modeled after graduate medical education, the fellowship is predominantly hands-on. Fellows work on real projects alongside professionals in management, quality, and safety.
Under the Hood
Giving trainees the inside view into the intricacies of how to change physician behavior and cultural issues in hospitals is the backbone of Beth Israel’s program. Fellows see what clinicians rarely see: the real-world complexity of hospitals, why there is so much inertia, and the reasons changing systems can be so difficult. Fellows learn how almost every hospital issue involves financial, personnel, facility, policy and political considerations. By allowing entrée into the executive offices, the fellow gets to hear the many different perspectives when people react to an issue.
“After a quality-improvement meeting, for instance, where people are positioning and requesting different things rather than taking action,” says Dr. Shulkin, “the fellow gets to hear the behind-the-scenes analysis—how executives sometimes label people and develop strategies to overcome some of these barriers.”
Understanding how administrators, directors of social work, or nurses, for instance, view situations and understand their culture helps the leader be more effective.
“To get both leadership and clinician buy-in, and to get leadership to motivate clinicians to participate in system changes, you also need to be politically savvy,” says Dr. Adelman. “Plenty of people resist change. The PSO needs to come off as sincere, passionate, and smart, and has to be able to answer people’s tough questions.”
It can take an ambassador’s touch to make headway in the traditional physician culture.
“The patient safety officers, the chief medical officers, often have to function as diplomats,” says Dr. Angood. “This physician engagement piece is one of the most complicated issues out there, and it arises because physicians historically are trained to be autonomous, to be independent, and to expect that institutions are there to serve them.”
—Latha Sivaprasad, MD, Don Hoskins Quality Improvement/Patient Safety fellow, Beth Israel Medical Center, New York City
One Hospitalist’s View
When Latha Sivaprasad, MD, current Don Hoskins fellow at Beth Israel, started her fellowship six months ago, she was astonished how little she knew about patient safety and quality. Although she felt she knew the day-to-day deficiencies in the hospital and on the front line—and despite having practiced in three other hospitals—she wasn’t prepared to learn what she hadn’t known she didn’t know.
“In my five years as a hospitalist, I knew very little about patient safety and quality—to my shock now,” she says. “Since I’ve been a fellow here, I realize how much I had been underutilized and how much more I could have contributed to making my respective hospitals run more safely.”
Understanding people’s motivations and meeting their needs to make a hospital safer is an intricate process.
“I think it is important for hospitalists to understand how complicated and time-consuming system changes are,” she says. “You do not have that perspective as a clinician. You think that change can occur from a memo or from good intentions to do the right thing.”
She has learned to think about the bigger world outside the clinical portion of running a hospital.
“To be a change agent you really need to appreciate the hospital from the penthouse view, which is what this fellowship provides,” she says. “You need to have access to every meeting, every record, every clinician, and every senior executive to put the pieces of the puzzle together to understand how things change.”
The hospital is working to apply the Toyota method of employee involvement to the issue of how an obstetric patient progresses from triage in the emergency department (ED) to labor and delivery, and how much time passes before the triage the patient is discharged or admitted. Their focus first targeted convening the right group to discuss the issue and identify the details of the problem, then put a plan in place to track ED triage. They looked for ways to make that process more efficient, met again to determine how to implement a new version of that process, then tracked the difference. “All of this was a multihour ordeal,” she says.
It’s exhilarating, frustrating, and intriguing—and sometimes discouraging. “It’s very tedious making change, and I didn’t appreciate that before the fellowship,” she says.
Dr. Sivaprasad advises hospitalists that to be effective in patient safety efforts means being a problem solver, highly empathetic, sensitive to others, and above all, extremely patient. But results often emerge slowly.
“You must have several things brewing at once because if certain programs’ changes are taking time, you need to complete the loop on something else,” she advises.
The Ideal Candidate
Of the 20 fellows Dr. Shulkin has mentored, about half were older and more experienced than he was. Reflecting on the successful fellows and those who benefited less makes him think the distinction of experience and age is less important than the individual’s personality.
“What is important is the personality and motivation and self-directedness of the fellow,” says Dr. Shulkin. “This is a very autonomous fellowship. One of the pluses and minuses of working with senior executives is that they are very busy; they don’t have time the way traditional academic program directors or residency directors do to think, ‘Where are my fellows and what are they doing?’”
Those who will get the most out of this type of experience know how to be delicately assertive yet drive their own agendas.
To Drs. Shulkin and Bernard, a good patient safety leader is naturally curious about what makes healthcare organizations tick. The ideal candidate has an appreciation for hospital financing and the science behind physician behavior change, and the capacity to be a good listener. The trainee also needs to put aside his or her ego while transitioning from a physician in charge to stepping back into the student role to learn the new language and environment.
—David Shulkin, MD, chief executive officer, Beth Israel Medical Center, New York City
Where to Begin
The institution sponsoring the development of the patient safety officer is just as important as who that candidate is.
“The administration has to have a visionary leadership that recognizes that healthcare quality and safety is the way you do business,” says Dr. Bernard. “You have to be in an institution that is not just paying lip service to moving quality and safety. It has to be part of the fabric of the institution.”
The institution also has to be able to offer a variety of experiences, making this kind of training difficult in a nonacademic setting.
For those interested in pursuing this area of leadership, the natural first step is to meet with the CMO or CEO to explore whether the individual’s and hospital’s interests can be aligned.
“But you can’t force it,” warns Dr. Shulkin. “If that is not a natural fit, if the CMO or CEO doesn’t see their role as, or have an interest in, training faculty people; or if they don’t have the expertise to do it, it’s not going to be a good experience. In those cases, the hospitalist should look elsewhere. An increasing number of centers can offer this kind of experience for a year,” he says. “Then the hospitalist might return to their institution to take on a leadership role there.”
Creating a costly infrastructure to train a patient safety officer is not required. What is necessary is chemistry in the mentor-trainee relationship.
“This is the first time in my postgraduate career that I actually have consistently committed mentors who care about how I am molded as a physician and what my ultimate contribution to the medical field will be,” says Dr. Sivaprasad. TH
Andrea Sattinger is a medical writer based in North Carolina.
At Mercy Hospital in Iowa City, Iowa, the implementation of safety and quality systems is “stirring up the pot,” says Mercy hospitalist and medical director Martin Izakovic, MD.
He has been recruited to supervise Mercy’s latest safety initiatives, including electronic medical records, pay-for-performance measures, development of treatment protocols, standardization of care, and deep-vein thrombosis prophylaxis.
Hospitalists at Mercy face the challenges their peers around the country face in their quest to improve quality and safeguard patients. The leader in these areas needs to be a role model and respected peer for the physicians he or she must lead day after day, says Dr. Izakovic.
How do hospitalists, who are so well-positioned to become leaders in patient safety, develop in that direction?
“The biggest challenge I see is the spectrum of polarization between clinicians and administrators,” he says. “One of the most important qualities that a patient safety officer needs is the ability to overbridge the doctors on one hand and the administrators on the other.”
What They Need
A patient safety officer (PSO) requires a critical mix of clinical and administrative skills, says Peter B. Angood, MD, vice president and chief patient safety officer for The Joint Commission, in Oakbrook, Ill.
On the clinical side, the hospitalist who wishes to be a PSO needs more than awareness of safety and quality improvement processes. He or she must be knowledgeable about and conversant in safety science in industries beyond healthcare. That expertise needs to encompass leadership, behaviors and cultures, human factors, and process redesign or systems engineering. Important, too, is training in how to corral the pieces of an organization and ensure they operate well together.
An understanding of organizational behavior is of great value. The potential PSO should understand how the key players interact: the board of directors with chief executives, chief executives with senior management, senior management with all staff (including the allied professionals), and medical staff with the organization as a whole.
“Because safety is a systemwide process, the patient safety [person] is pivotal in forming a hub from which much of the quality, safety, and process improvement occurs,” says Dr. Angood.
Jason Adelman, MD, MS, former hospitalist and current PSO at Montefiore Medical Center in New York City, says developing patient safety leaders should embrace technology. “Pay attention to the latest and greatest ideas, products, and services,” he urges. “Come up with strategic plans to implement in healthcare, get the information quickly into the hands of physicians, have physicians report, and include forcing functions [whereby computers will not process to completion when key data are missing].”
Above all, the patient safety officer must train to be a change agent. “Influencing patient safety means you have to be there in the capital-allocation process,” says David Shulkin, MD, chief executive officer at Beth Israel Medical Center in New York City. “You have to be there when they’re designing facilities. You have to understand your human resource policies and the skill sets and aptitudes of the people that the hospital is hiring. To be a good patient safety officer, the training needs to involve broad exposure with a slant toward operations.”
Build a Bridge
As a young physician who wanted to develop as a leader in the field of quality and safety, Dr. Shulkin had to forge his own path. In 1992, after he became chief medical officer (CMO) at the Hospital of the University of Pennsylvania in Philadelphia, he fielded several inquiries a month from young physicians who wanted to pursue a similar career. In response to that need, he designed a quality improvement/patient safety fellowship at his school.
David Bernard, MD, now chief medical officer at Beth Israel, had been practicing medicine for 30 years when at age 50 he took a year’s leave of absence from Boston University and enrolled as Dr. Shulkin’s first fellow in 1994. Dr. Bernard, a nephrologist, was a vice dean in the school of medicine at Boston University Medical Center, a hospital vice president for clinical affairs, and a senior clinician in his specialty group.
Drs. Shulkin and Bernard left the University of Pennsylvania in 1999 to take the concepts of quality transparency to a higher level and formed DoctorQuality Inc. in Conshohocken, Pa. To continue their work, DoctorQuality funded the fellowship. In 2005 when Dr. Shulkin went to Beth Israel in New York, the fellowship was restarted as the Don Hoskins Quality Improvement/Patient Safety program and funded for five years with private philanthropy.
Modeled after graduate medical education, the fellowship is predominantly hands-on. Fellows work on real projects alongside professionals in management, quality, and safety.
Under the Hood
Giving trainees the inside view into the intricacies of how to change physician behavior and cultural issues in hospitals is the backbone of Beth Israel’s program. Fellows see what clinicians rarely see: the real-world complexity of hospitals, why there is so much inertia, and the reasons changing systems can be so difficult. Fellows learn how almost every hospital issue involves financial, personnel, facility, policy and political considerations. By allowing entrée into the executive offices, the fellow gets to hear the many different perspectives when people react to an issue.
“After a quality-improvement meeting, for instance, where people are positioning and requesting different things rather than taking action,” says Dr. Shulkin, “the fellow gets to hear the behind-the-scenes analysis—how executives sometimes label people and develop strategies to overcome some of these barriers.”
Understanding how administrators, directors of social work, or nurses, for instance, view situations and understand their culture helps the leader be more effective.
“To get both leadership and clinician buy-in, and to get leadership to motivate clinicians to participate in system changes, you also need to be politically savvy,” says Dr. Adelman. “Plenty of people resist change. The PSO needs to come off as sincere, passionate, and smart, and has to be able to answer people’s tough questions.”
It can take an ambassador’s touch to make headway in the traditional physician culture.
“The patient safety officers, the chief medical officers, often have to function as diplomats,” says Dr. Angood. “This physician engagement piece is one of the most complicated issues out there, and it arises because physicians historically are trained to be autonomous, to be independent, and to expect that institutions are there to serve them.”
—Latha Sivaprasad, MD, Don Hoskins Quality Improvement/Patient Safety fellow, Beth Israel Medical Center, New York City
One Hospitalist’s View
When Latha Sivaprasad, MD, current Don Hoskins fellow at Beth Israel, started her fellowship six months ago, she was astonished how little she knew about patient safety and quality. Although she felt she knew the day-to-day deficiencies in the hospital and on the front line—and despite having practiced in three other hospitals—she wasn’t prepared to learn what she hadn’t known she didn’t know.
“In my five years as a hospitalist, I knew very little about patient safety and quality—to my shock now,” she says. “Since I’ve been a fellow here, I realize how much I had been underutilized and how much more I could have contributed to making my respective hospitals run more safely.”
Understanding people’s motivations and meeting their needs to make a hospital safer is an intricate process.
“I think it is important for hospitalists to understand how complicated and time-consuming system changes are,” she says. “You do not have that perspective as a clinician. You think that change can occur from a memo or from good intentions to do the right thing.”
She has learned to think about the bigger world outside the clinical portion of running a hospital.
“To be a change agent you really need to appreciate the hospital from the penthouse view, which is what this fellowship provides,” she says. “You need to have access to every meeting, every record, every clinician, and every senior executive to put the pieces of the puzzle together to understand how things change.”
The hospital is working to apply the Toyota method of employee involvement to the issue of how an obstetric patient progresses from triage in the emergency department (ED) to labor and delivery, and how much time passes before the triage the patient is discharged or admitted. Their focus first targeted convening the right group to discuss the issue and identify the details of the problem, then put a plan in place to track ED triage. They looked for ways to make that process more efficient, met again to determine how to implement a new version of that process, then tracked the difference. “All of this was a multihour ordeal,” she says.
It’s exhilarating, frustrating, and intriguing—and sometimes discouraging. “It’s very tedious making change, and I didn’t appreciate that before the fellowship,” she says.
Dr. Sivaprasad advises hospitalists that to be effective in patient safety efforts means being a problem solver, highly empathetic, sensitive to others, and above all, extremely patient. But results often emerge slowly.
“You must have several things brewing at once because if certain programs’ changes are taking time, you need to complete the loop on something else,” she advises.
The Ideal Candidate
Of the 20 fellows Dr. Shulkin has mentored, about half were older and more experienced than he was. Reflecting on the successful fellows and those who benefited less makes him think the distinction of experience and age is less important than the individual’s personality.
“What is important is the personality and motivation and self-directedness of the fellow,” says Dr. Shulkin. “This is a very autonomous fellowship. One of the pluses and minuses of working with senior executives is that they are very busy; they don’t have time the way traditional academic program directors or residency directors do to think, ‘Where are my fellows and what are they doing?’”
Those who will get the most out of this type of experience know how to be delicately assertive yet drive their own agendas.
To Drs. Shulkin and Bernard, a good patient safety leader is naturally curious about what makes healthcare organizations tick. The ideal candidate has an appreciation for hospital financing and the science behind physician behavior change, and the capacity to be a good listener. The trainee also needs to put aside his or her ego while transitioning from a physician in charge to stepping back into the student role to learn the new language and environment.
—David Shulkin, MD, chief executive officer, Beth Israel Medical Center, New York City
Where to Begin
The institution sponsoring the development of the patient safety officer is just as important as who that candidate is.
“The administration has to have a visionary leadership that recognizes that healthcare quality and safety is the way you do business,” says Dr. Bernard. “You have to be in an institution that is not just paying lip service to moving quality and safety. It has to be part of the fabric of the institution.”
The institution also has to be able to offer a variety of experiences, making this kind of training difficult in a nonacademic setting.
For those interested in pursuing this area of leadership, the natural first step is to meet with the CMO or CEO to explore whether the individual’s and hospital’s interests can be aligned.
“But you can’t force it,” warns Dr. Shulkin. “If that is not a natural fit, if the CMO or CEO doesn’t see their role as, or have an interest in, training faculty people; or if they don’t have the expertise to do it, it’s not going to be a good experience. In those cases, the hospitalist should look elsewhere. An increasing number of centers can offer this kind of experience for a year,” he says. “Then the hospitalist might return to their institution to take on a leadership role there.”
Creating a costly infrastructure to train a patient safety officer is not required. What is necessary is chemistry in the mentor-trainee relationship.
“This is the first time in my postgraduate career that I actually have consistently committed mentors who care about how I am molded as a physician and what my ultimate contribution to the medical field will be,” says Dr. Sivaprasad. TH
Andrea Sattinger is a medical writer based in North Carolina.
At Mercy Hospital in Iowa City, Iowa, the implementation of safety and quality systems is “stirring up the pot,” says Mercy hospitalist and medical director Martin Izakovic, MD.
He has been recruited to supervise Mercy’s latest safety initiatives, including electronic medical records, pay-for-performance measures, development of treatment protocols, standardization of care, and deep-vein thrombosis prophylaxis.
Hospitalists at Mercy face the challenges their peers around the country face in their quest to improve quality and safeguard patients. The leader in these areas needs to be a role model and respected peer for the physicians he or she must lead day after day, says Dr. Izakovic.
How do hospitalists, who are so well-positioned to become leaders in patient safety, develop in that direction?
“The biggest challenge I see is the spectrum of polarization between clinicians and administrators,” he says. “One of the most important qualities that a patient safety officer needs is the ability to overbridge the doctors on one hand and the administrators on the other.”
What They Need
A patient safety officer (PSO) requires a critical mix of clinical and administrative skills, says Peter B. Angood, MD, vice president and chief patient safety officer for The Joint Commission, in Oakbrook, Ill.
On the clinical side, the hospitalist who wishes to be a PSO needs more than awareness of safety and quality improvement processes. He or she must be knowledgeable about and conversant in safety science in industries beyond healthcare. That expertise needs to encompass leadership, behaviors and cultures, human factors, and process redesign or systems engineering. Important, too, is training in how to corral the pieces of an organization and ensure they operate well together.
An understanding of organizational behavior is of great value. The potential PSO should understand how the key players interact: the board of directors with chief executives, chief executives with senior management, senior management with all staff (including the allied professionals), and medical staff with the organization as a whole.
“Because safety is a systemwide process, the patient safety [person] is pivotal in forming a hub from which much of the quality, safety, and process improvement occurs,” says Dr. Angood.
Jason Adelman, MD, MS, former hospitalist and current PSO at Montefiore Medical Center in New York City, says developing patient safety leaders should embrace technology. “Pay attention to the latest and greatest ideas, products, and services,” he urges. “Come up with strategic plans to implement in healthcare, get the information quickly into the hands of physicians, have physicians report, and include forcing functions [whereby computers will not process to completion when key data are missing].”
Above all, the patient safety officer must train to be a change agent. “Influencing patient safety means you have to be there in the capital-allocation process,” says David Shulkin, MD, chief executive officer at Beth Israel Medical Center in New York City. “You have to be there when they’re designing facilities. You have to understand your human resource policies and the skill sets and aptitudes of the people that the hospital is hiring. To be a good patient safety officer, the training needs to involve broad exposure with a slant toward operations.”
Build a Bridge
As a young physician who wanted to develop as a leader in the field of quality and safety, Dr. Shulkin had to forge his own path. In 1992, after he became chief medical officer (CMO) at the Hospital of the University of Pennsylvania in Philadelphia, he fielded several inquiries a month from young physicians who wanted to pursue a similar career. In response to that need, he designed a quality improvement/patient safety fellowship at his school.
David Bernard, MD, now chief medical officer at Beth Israel, had been practicing medicine for 30 years when at age 50 he took a year’s leave of absence from Boston University and enrolled as Dr. Shulkin’s first fellow in 1994. Dr. Bernard, a nephrologist, was a vice dean in the school of medicine at Boston University Medical Center, a hospital vice president for clinical affairs, and a senior clinician in his specialty group.
Drs. Shulkin and Bernard left the University of Pennsylvania in 1999 to take the concepts of quality transparency to a higher level and formed DoctorQuality Inc. in Conshohocken, Pa. To continue their work, DoctorQuality funded the fellowship. In 2005 when Dr. Shulkin went to Beth Israel in New York, the fellowship was restarted as the Don Hoskins Quality Improvement/Patient Safety program and funded for five years with private philanthropy.
Modeled after graduate medical education, the fellowship is predominantly hands-on. Fellows work on real projects alongside professionals in management, quality, and safety.
Under the Hood
Giving trainees the inside view into the intricacies of how to change physician behavior and cultural issues in hospitals is the backbone of Beth Israel’s program. Fellows see what clinicians rarely see: the real-world complexity of hospitals, why there is so much inertia, and the reasons changing systems can be so difficult. Fellows learn how almost every hospital issue involves financial, personnel, facility, policy and political considerations. By allowing entrée into the executive offices, the fellow gets to hear the many different perspectives when people react to an issue.
“After a quality-improvement meeting, for instance, where people are positioning and requesting different things rather than taking action,” says Dr. Shulkin, “the fellow gets to hear the behind-the-scenes analysis—how executives sometimes label people and develop strategies to overcome some of these barriers.”
Understanding how administrators, directors of social work, or nurses, for instance, view situations and understand their culture helps the leader be more effective.
“To get both leadership and clinician buy-in, and to get leadership to motivate clinicians to participate in system changes, you also need to be politically savvy,” says Dr. Adelman. “Plenty of people resist change. The PSO needs to come off as sincere, passionate, and smart, and has to be able to answer people’s tough questions.”
It can take an ambassador’s touch to make headway in the traditional physician culture.
“The patient safety officers, the chief medical officers, often have to function as diplomats,” says Dr. Angood. “This physician engagement piece is one of the most complicated issues out there, and it arises because physicians historically are trained to be autonomous, to be independent, and to expect that institutions are there to serve them.”
—Latha Sivaprasad, MD, Don Hoskins Quality Improvement/Patient Safety fellow, Beth Israel Medical Center, New York City
One Hospitalist’s View
When Latha Sivaprasad, MD, current Don Hoskins fellow at Beth Israel, started her fellowship six months ago, she was astonished how little she knew about patient safety and quality. Although she felt she knew the day-to-day deficiencies in the hospital and on the front line—and despite having practiced in three other hospitals—she wasn’t prepared to learn what she hadn’t known she didn’t know.
“In my five years as a hospitalist, I knew very little about patient safety and quality—to my shock now,” she says. “Since I’ve been a fellow here, I realize how much I had been underutilized and how much more I could have contributed to making my respective hospitals run more safely.”
Understanding people’s motivations and meeting their needs to make a hospital safer is an intricate process.
“I think it is important for hospitalists to understand how complicated and time-consuming system changes are,” she says. “You do not have that perspective as a clinician. You think that change can occur from a memo or from good intentions to do the right thing.”
She has learned to think about the bigger world outside the clinical portion of running a hospital.
“To be a change agent you really need to appreciate the hospital from the penthouse view, which is what this fellowship provides,” she says. “You need to have access to every meeting, every record, every clinician, and every senior executive to put the pieces of the puzzle together to understand how things change.”
The hospital is working to apply the Toyota method of employee involvement to the issue of how an obstetric patient progresses from triage in the emergency department (ED) to labor and delivery, and how much time passes before the triage the patient is discharged or admitted. Their focus first targeted convening the right group to discuss the issue and identify the details of the problem, then put a plan in place to track ED triage. They looked for ways to make that process more efficient, met again to determine how to implement a new version of that process, then tracked the difference. “All of this was a multihour ordeal,” she says.
It’s exhilarating, frustrating, and intriguing—and sometimes discouraging. “It’s very tedious making change, and I didn’t appreciate that before the fellowship,” she says.
Dr. Sivaprasad advises hospitalists that to be effective in patient safety efforts means being a problem solver, highly empathetic, sensitive to others, and above all, extremely patient. But results often emerge slowly.
“You must have several things brewing at once because if certain programs’ changes are taking time, you need to complete the loop on something else,” she advises.
The Ideal Candidate
Of the 20 fellows Dr. Shulkin has mentored, about half were older and more experienced than he was. Reflecting on the successful fellows and those who benefited less makes him think the distinction of experience and age is less important than the individual’s personality.
“What is important is the personality and motivation and self-directedness of the fellow,” says Dr. Shulkin. “This is a very autonomous fellowship. One of the pluses and minuses of working with senior executives is that they are very busy; they don’t have time the way traditional academic program directors or residency directors do to think, ‘Where are my fellows and what are they doing?’”
Those who will get the most out of this type of experience know how to be delicately assertive yet drive their own agendas.
To Drs. Shulkin and Bernard, a good patient safety leader is naturally curious about what makes healthcare organizations tick. The ideal candidate has an appreciation for hospital financing and the science behind physician behavior change, and the capacity to be a good listener. The trainee also needs to put aside his or her ego while transitioning from a physician in charge to stepping back into the student role to learn the new language and environment.
—David Shulkin, MD, chief executive officer, Beth Israel Medical Center, New York City
Where to Begin
The institution sponsoring the development of the patient safety officer is just as important as who that candidate is.
“The administration has to have a visionary leadership that recognizes that healthcare quality and safety is the way you do business,” says Dr. Bernard. “You have to be in an institution that is not just paying lip service to moving quality and safety. It has to be part of the fabric of the institution.”
The institution also has to be able to offer a variety of experiences, making this kind of training difficult in a nonacademic setting.
For those interested in pursuing this area of leadership, the natural first step is to meet with the CMO or CEO to explore whether the individual’s and hospital’s interests can be aligned.
“But you can’t force it,” warns Dr. Shulkin. “If that is not a natural fit, if the CMO or CEO doesn’t see their role as, or have an interest in, training faculty people; or if they don’t have the expertise to do it, it’s not going to be a good experience. In those cases, the hospitalist should look elsewhere. An increasing number of centers can offer this kind of experience for a year,” he says. “Then the hospitalist might return to their institution to take on a leadership role there.”
Creating a costly infrastructure to train a patient safety officer is not required. What is necessary is chemistry in the mentor-trainee relationship.
“This is the first time in my postgraduate career that I actually have consistently committed mentors who care about how I am molded as a physician and what my ultimate contribution to the medical field will be,” says Dr. Sivaprasad. TH
Andrea Sattinger is a medical writer based in North Carolina.
Tackle TB
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Safety in Numbers
Patient safety organizations, commonly referred to as PSOs, are about to take off. And when they do, PSOs should provide hospitalists with invaluable data on improving patient safety.
“PSOs are a great concept, but even though it’s been around since 2005, I haven’t seen it clinically,” says Janet Nagamine, RN, MD, hospitalist at Kaiser Permanente in Santa Clara, Calif., and chair of SHM’s Hospital Quality and Patient Safety Committee.
This calendar year, Nagamine and the rest of hospital medicine should start to see some movement—“PSO 1.0,” if you will.
Background
PSOs are public and private organizations approved by the Agency for Healthcare Research and Quality (AHRQ); they include such groups as Health Watch Inc., Human Performance Technology Group, and the Institute for Safe Medication Practices, which will collect, aggregate, and analyze data on patient safety events. Hospitals and other healthcare providers will voluntarily and confidentially report data. The ultimate goal is to advance changes in culture, processes, and systems to enhance patient safety.
PSOs grew out of the Patient Safety and Quality Improvement Act of 2005, which was a response to the Institute of Medicine’s landmark report “To Err Is Human: Building a Safer Health System.” But it wasn’t until last year that the U.S. Department of Health and Human Services issued a final rule outlining PSO requirements and procedures. The rule became effective Jan. 19, 2009.
AHRQ is responsible for coordinating the development of a set of common definitions and reporting formats, called common formats, for collecting the data. Eventually, AHRQ will create a network of patient safety databases to which PSOs, providers, and others can voluntarily contribute non-identifiable patient safety information. This network will serve as an interactive evidence-based management resource for providers, PSOs, and other entities. AHRQ will use data from the network to analyze national and regional statistics regarding patient safety events. Findings will be made public and will be included in AHRQ’s annual National Healthcare Quality Report.
IT Example
To date, the only comparable data-collection system is MedMarx, which compiles information on medication errors. The Joint Commission requires providers to supply a root-cause analysis on every Level 1 incident, “but that’s just scratching the surface of what occurs,” Dr. Nagamine says. “There are far many more Level 2 and Level 3 events with the same precursors, and that information would be very valuable.”
By collecting nationwide data on patient safety events, PSOs will be able to bridge the gaps in the reporting system and provide crucial patient safety information to the healthcare industry. “In general, the concept of aggregate information that allows us to compare events is incredibly important,” Dr. Nagamine says. “A hospitalist working in one hospital has only the information about events in that hospital, but 5,000 hospitals can provide more specific and actionable information. We just haven’t seen this operationalized yet.”
Dr. Nagamine uses a technology example to show the value PSOs could have in identifying patterns or problems that threaten patient safety: “Every hospital has a horror story of implementing a new information technology (IT) system, and we’re getting some very interesting feedback from hospitals about unintended consequences,” she says. “We’re hearing that patients are being hurt because of mistakes in systems—the use of dropdown menus (on computer screens) that don’t drop down far enough to reveal all options, or a screen where it’s easy to click the wrong item.”
Current systems might not allow problems like these to be highlighted. Even if staff knows of a problem, their hospital’s coding system might not allow them to detail it. “It may fall under ‘communications’ or ‘physician computerized order entry’ or something vague, so the data won’t show the specifics of what happened,” Dr. Nagamine points out. “If we had aggregate data on issues like this, we could address it. Right now, we just have word of mouth.”
An isolated event at a hospital is one thing, but similar data from around the nation is significant. “Drug companies or IT vendors confronted with (patterns) might make some changes,” she says. “That kind of data is powerful.”
Hospital Medicine on Board
When hospitals start reporting data to PSOs, where will hospitalists fit into the process? Hospitalists likely will be interviewed to answer some of the PSO’s questions, but they will not be the ones filling out the forms, Dr. Nagamine says. Hospitalists also will be among the ranks of healthcare professionals eagerly awaiting the release of the data. “The way that PSOs approach patient safety and quality—what’s near and dear to our hearts—is it gives us more data,” Dr. Nagamine says. This is crucial for hospitalists leading quality-improvement projects and similar tasks. “Without that data, it’s hard to get traction and movement. That data will help convince someone to invest more time and money in a particular problem area.”
Phase One: Participation
AHRQ has established a comprehensive Web site (www.pso.ahrq.gov) that includes information on the first draft of common formats for use with hospital inpatients. These are found on downloadable paper forms, available at the PSO Privacy Protection Center (PPC) Web site at www.psoppc.org/ web/patientsafety/paperforms.
“The forms are a first step,” Dr. Nagamine explains. “If we had these data points on every incident at every hospital, we’d know a lot more than we do now. We’d be able to harness that information.”
It will be a while before healthcare providers can search the data for patterns and possible solutions in patient safety, but the wait should be worth it. “You’ve got to start somewhere, and it’s not going to happen in one sweep,” Dr. Nagamine says. “This is simply a start. Hopefully, in a decade, we’ll have a lot more actionable information.” TH
Jane Jerrard is a medical writer based in Chicago.
Patient safety organizations, commonly referred to as PSOs, are about to take off. And when they do, PSOs should provide hospitalists with invaluable data on improving patient safety.
“PSOs are a great concept, but even though it’s been around since 2005, I haven’t seen it clinically,” says Janet Nagamine, RN, MD, hospitalist at Kaiser Permanente in Santa Clara, Calif., and chair of SHM’s Hospital Quality and Patient Safety Committee.
This calendar year, Nagamine and the rest of hospital medicine should start to see some movement—“PSO 1.0,” if you will.
Background
PSOs are public and private organizations approved by the Agency for Healthcare Research and Quality (AHRQ); they include such groups as Health Watch Inc., Human Performance Technology Group, and the Institute for Safe Medication Practices, which will collect, aggregate, and analyze data on patient safety events. Hospitals and other healthcare providers will voluntarily and confidentially report data. The ultimate goal is to advance changes in culture, processes, and systems to enhance patient safety.
PSOs grew out of the Patient Safety and Quality Improvement Act of 2005, which was a response to the Institute of Medicine’s landmark report “To Err Is Human: Building a Safer Health System.” But it wasn’t until last year that the U.S. Department of Health and Human Services issued a final rule outlining PSO requirements and procedures. The rule became effective Jan. 19, 2009.
AHRQ is responsible for coordinating the development of a set of common definitions and reporting formats, called common formats, for collecting the data. Eventually, AHRQ will create a network of patient safety databases to which PSOs, providers, and others can voluntarily contribute non-identifiable patient safety information. This network will serve as an interactive evidence-based management resource for providers, PSOs, and other entities. AHRQ will use data from the network to analyze national and regional statistics regarding patient safety events. Findings will be made public and will be included in AHRQ’s annual National Healthcare Quality Report.
IT Example
To date, the only comparable data-collection system is MedMarx, which compiles information on medication errors. The Joint Commission requires providers to supply a root-cause analysis on every Level 1 incident, “but that’s just scratching the surface of what occurs,” Dr. Nagamine says. “There are far many more Level 2 and Level 3 events with the same precursors, and that information would be very valuable.”
By collecting nationwide data on patient safety events, PSOs will be able to bridge the gaps in the reporting system and provide crucial patient safety information to the healthcare industry. “In general, the concept of aggregate information that allows us to compare events is incredibly important,” Dr. Nagamine says. “A hospitalist working in one hospital has only the information about events in that hospital, but 5,000 hospitals can provide more specific and actionable information. We just haven’t seen this operationalized yet.”
Dr. Nagamine uses a technology example to show the value PSOs could have in identifying patterns or problems that threaten patient safety: “Every hospital has a horror story of implementing a new information technology (IT) system, and we’re getting some very interesting feedback from hospitals about unintended consequences,” she says. “We’re hearing that patients are being hurt because of mistakes in systems—the use of dropdown menus (on computer screens) that don’t drop down far enough to reveal all options, or a screen where it’s easy to click the wrong item.”
Current systems might not allow problems like these to be highlighted. Even if staff knows of a problem, their hospital’s coding system might not allow them to detail it. “It may fall under ‘communications’ or ‘physician computerized order entry’ or something vague, so the data won’t show the specifics of what happened,” Dr. Nagamine points out. “If we had aggregate data on issues like this, we could address it. Right now, we just have word of mouth.”
An isolated event at a hospital is one thing, but similar data from around the nation is significant. “Drug companies or IT vendors confronted with (patterns) might make some changes,” she says. “That kind of data is powerful.”
Hospital Medicine on Board
When hospitals start reporting data to PSOs, where will hospitalists fit into the process? Hospitalists likely will be interviewed to answer some of the PSO’s questions, but they will not be the ones filling out the forms, Dr. Nagamine says. Hospitalists also will be among the ranks of healthcare professionals eagerly awaiting the release of the data. “The way that PSOs approach patient safety and quality—what’s near and dear to our hearts—is it gives us more data,” Dr. Nagamine says. This is crucial for hospitalists leading quality-improvement projects and similar tasks. “Without that data, it’s hard to get traction and movement. That data will help convince someone to invest more time and money in a particular problem area.”
Phase One: Participation
AHRQ has established a comprehensive Web site (www.pso.ahrq.gov) that includes information on the first draft of common formats for use with hospital inpatients. These are found on downloadable paper forms, available at the PSO Privacy Protection Center (PPC) Web site at www.psoppc.org/ web/patientsafety/paperforms.
“The forms are a first step,” Dr. Nagamine explains. “If we had these data points on every incident at every hospital, we’d know a lot more than we do now. We’d be able to harness that information.”
It will be a while before healthcare providers can search the data for patterns and possible solutions in patient safety, but the wait should be worth it. “You’ve got to start somewhere, and it’s not going to happen in one sweep,” Dr. Nagamine says. “This is simply a start. Hopefully, in a decade, we’ll have a lot more actionable information.” TH
Jane Jerrard is a medical writer based in Chicago.
Patient safety organizations, commonly referred to as PSOs, are about to take off. And when they do, PSOs should provide hospitalists with invaluable data on improving patient safety.
“PSOs are a great concept, but even though it’s been around since 2005, I haven’t seen it clinically,” says Janet Nagamine, RN, MD, hospitalist at Kaiser Permanente in Santa Clara, Calif., and chair of SHM’s Hospital Quality and Patient Safety Committee.
This calendar year, Nagamine and the rest of hospital medicine should start to see some movement—“PSO 1.0,” if you will.
Background
PSOs are public and private organizations approved by the Agency for Healthcare Research and Quality (AHRQ); they include such groups as Health Watch Inc., Human Performance Technology Group, and the Institute for Safe Medication Practices, which will collect, aggregate, and analyze data on patient safety events. Hospitals and other healthcare providers will voluntarily and confidentially report data. The ultimate goal is to advance changes in culture, processes, and systems to enhance patient safety.
PSOs grew out of the Patient Safety and Quality Improvement Act of 2005, which was a response to the Institute of Medicine’s landmark report “To Err Is Human: Building a Safer Health System.” But it wasn’t until last year that the U.S. Department of Health and Human Services issued a final rule outlining PSO requirements and procedures. The rule became effective Jan. 19, 2009.
AHRQ is responsible for coordinating the development of a set of common definitions and reporting formats, called common formats, for collecting the data. Eventually, AHRQ will create a network of patient safety databases to which PSOs, providers, and others can voluntarily contribute non-identifiable patient safety information. This network will serve as an interactive evidence-based management resource for providers, PSOs, and other entities. AHRQ will use data from the network to analyze national and regional statistics regarding patient safety events. Findings will be made public and will be included in AHRQ’s annual National Healthcare Quality Report.
IT Example
To date, the only comparable data-collection system is MedMarx, which compiles information on medication errors. The Joint Commission requires providers to supply a root-cause analysis on every Level 1 incident, “but that’s just scratching the surface of what occurs,” Dr. Nagamine says. “There are far many more Level 2 and Level 3 events with the same precursors, and that information would be very valuable.”
By collecting nationwide data on patient safety events, PSOs will be able to bridge the gaps in the reporting system and provide crucial patient safety information to the healthcare industry. “In general, the concept of aggregate information that allows us to compare events is incredibly important,” Dr. Nagamine says. “A hospitalist working in one hospital has only the information about events in that hospital, but 5,000 hospitals can provide more specific and actionable information. We just haven’t seen this operationalized yet.”
Dr. Nagamine uses a technology example to show the value PSOs could have in identifying patterns or problems that threaten patient safety: “Every hospital has a horror story of implementing a new information technology (IT) system, and we’re getting some very interesting feedback from hospitals about unintended consequences,” she says. “We’re hearing that patients are being hurt because of mistakes in systems—the use of dropdown menus (on computer screens) that don’t drop down far enough to reveal all options, or a screen where it’s easy to click the wrong item.”
Current systems might not allow problems like these to be highlighted. Even if staff knows of a problem, their hospital’s coding system might not allow them to detail it. “It may fall under ‘communications’ or ‘physician computerized order entry’ or something vague, so the data won’t show the specifics of what happened,” Dr. Nagamine points out. “If we had aggregate data on issues like this, we could address it. Right now, we just have word of mouth.”
An isolated event at a hospital is one thing, but similar data from around the nation is significant. “Drug companies or IT vendors confronted with (patterns) might make some changes,” she says. “That kind of data is powerful.”
Hospital Medicine on Board
When hospitals start reporting data to PSOs, where will hospitalists fit into the process? Hospitalists likely will be interviewed to answer some of the PSO’s questions, but they will not be the ones filling out the forms, Dr. Nagamine says. Hospitalists also will be among the ranks of healthcare professionals eagerly awaiting the release of the data. “The way that PSOs approach patient safety and quality—what’s near and dear to our hearts—is it gives us more data,” Dr. Nagamine says. This is crucial for hospitalists leading quality-improvement projects and similar tasks. “Without that data, it’s hard to get traction and movement. That data will help convince someone to invest more time and money in a particular problem area.”
Phase One: Participation
AHRQ has established a comprehensive Web site (www.pso.ahrq.gov) that includes information on the first draft of common formats for use with hospital inpatients. These are found on downloadable paper forms, available at the PSO Privacy Protection Center (PPC) Web site at www.psoppc.org/ web/patientsafety/paperforms.
“The forms are a first step,” Dr. Nagamine explains. “If we had these data points on every incident at every hospital, we’d know a lot more than we do now. We’d be able to harness that information.”
It will be a while before healthcare providers can search the data for patterns and possible solutions in patient safety, but the wait should be worth it. “You’ve got to start somewhere, and it’s not going to happen in one sweep,” Dr. Nagamine says. “This is simply a start. Hopefully, in a decade, we’ll have a lot more actionable information.” TH
Jane Jerrard is a medical writer based in Chicago.
Hospitalists Find Writing Makes Them Better Doctors
When people hear that Ruben J. Nazario, MD, a pediatric hospitalist at Kentucky Children’s Hospital in Lexington, writes in his spare time, they assume he writes for children. “But my writing is very non-pediatric,” he says. “I’m two people in one.”
A native of Puerto Rico, Dr. Nazario primarily writes poetry in English and stories in Spanish. His short stories and novels deal with what he calls “the fun stuff”: passion, violence, death.
For example, a speck of tomato sauce falling on the floor when his wife served him a plate of spaghetti became the inspiration for a story in which the same thing happens. But in his story, the characters argue and the husband licks up the sauce from the floor. “That part didn’t really happen,” he laughs.
One might imagine writing as merely a hobby or diversion for practicing hospitalists. But those who indulge in the craft say it hones their medical skills.
Ron Grant, MD, pediatric hospitalist at the University of Arizona Medical Center in Tucson says writing affects his mood, which subsequently affects his practice. “It allows you to speak out [about] frustrations that arise, interesting situations that arise, and I find that very valuable,” he says.
The therapeutic experience is common to hospitalist writers.
Sandi Verbin, MD, a pediatric hospitalist at Holy Redeemer Hospital in Meadowbrook, Pa., says writing brings out her sense of humor, which helps with everything in medical practice. “Fortunately, with pediatrics, most of our patients get better,” she says.
But of course that’s not always the case. When a 7-year-old patient, who was in his care on and off for three years during his training, died of leukemia, Randy Ferrance, MD, a hospitalist at Riverside Tappahannock Hospital in Va., filtered the experience into a story.
“The piece was mostly biographical, but I put it in a fictional context,” says Dr. Ferrance. “I wrote it to say some of the things that I never did say, and work through things I never had worked through, with the patient and family. Writing helps me to clear my head and put things in a better perspective. It’s worth the time I carve out. It doesn’t affect the medical end of things, but it helps my ability to continue doing what I do.”
Many hospitalist writers say their art makes them more empathetic.
Joseph Geskey, DO, the division chief of pediatric hospital medicine at Penn State M.S. Hershey Medical Center in Pa., has published poetry in the Journal of the American Medical Association, an anthology in a book, essays, and fiction. “Writing allows you to clarify your thoughts, so it allows for some epiphanies, not only [regarding] writing but about life in general,” he says.
Preliminary studies suggest writing may have medical benefits such as reducing stress catecholamines and inflammatory markers. Though hard data are still to come, Dr. Geskey believes writing has made him a better physician. He says he is more patient, a better listener, and lets patients digress in their stories, revealing information he might not otherwise have learned. “If I’m able to use my rudimentary senses in my writing to evoke a scene or an image, how do I use those same senses to color in my interaction with patients, to help them feel better?” he asks.
The Trend Grows
There are a number of doctors who teach creative writing around the country, and writing workshops for physicians are popping up in and outside medical education curricula.
In Durham, N.C., Dr. Geskey participated in a Duke University poetry and medicine conference that he describes as “probably the most creative three or four days of my life.”
For three years, Bryan R. Fine, MD, MPH, pediatric hospitalist at Children’s National Medical Center in Washington, D.C., ran a creative writing elective for fourth-year medical students at George Washington University. Dr. Fine often writes during down time at work, especially on the night shift. He writes stories, nonfiction essays, and songs, which he performs publicly on occasion, including a few weeks each year at Club Med and other Caribbean locales.
Dr. Verbin has taken seminars in writing for children. “I’ve made some baby steps in that direction, but progress has been slow and mostly relegated to someday,’” she says.
In 1998, Dr. Grant left the University of Arizona, where he was practicing as a hospitalist for Cleo Hardin, MD, section chief of pediatric hospital medicine and herself a writer. (She is revising a memoir she wrote a couple years ago and beginning a novel about mothers and daughters). He traveled to Israel and Poland and wrote about that experience, then realized he wanted more. He returned to his school to pursue a master’s in creative writing. A year ago, at Dr. Hardin’s urging, he returned to medicine, now describing himself as a part-time hospitalist and full-time writer.
“I was overwhelmed by a lot of strange sensations when I went back to the hospital—all of which really informed my writing,” says Dr. Grant.
He is working on a memoir about leaving medicine after becoming uncomfortable with the ethical and personal dilemmas he faced as a pediatrician and as a father. “It’s hard to watch children die, but unbearable when you have children of your own,” he says.
Dr. Grant works nights, teaches medical students an elective in creative writing, and occasionally teaches at a community college. His most exciting teaching outlet is as an instructor in the Czech Republic at the prestigious Prague Summer Program, a study-abroad program offered through Western Michigan University. Those who take his the two-week memoir-writing workshop bring complete manuscripts for review and critique.
“The whole philosophy behind teaching writing and taking humanities classes is that there are unexplored areas of the brain that get withered as you go through medical school and residency,” Dr. Grant says. “Re-exploring that creative side allows us to become better physicians. Becoming more in touch with your own humanity allows you to be a more human practitioner, Even though I only practice part time, I’m certainly different as a practitioner than I was before [I started writing].”
As a full-time writer, Dr. Grant is the exception. But Dr. Nazario recalls a quote from physician Anton Chekhov that may sum things up for other hospitalist writers: “Medicine is my lawful wife, and literature is my mistress. When I get fed up with one, I spend the night with the other.” TH
Andrea Sattinger is a medical writer based in North Carolina.
When people hear that Ruben J. Nazario, MD, a pediatric hospitalist at Kentucky Children’s Hospital in Lexington, writes in his spare time, they assume he writes for children. “But my writing is very non-pediatric,” he says. “I’m two people in one.”
A native of Puerto Rico, Dr. Nazario primarily writes poetry in English and stories in Spanish. His short stories and novels deal with what he calls “the fun stuff”: passion, violence, death.
For example, a speck of tomato sauce falling on the floor when his wife served him a plate of spaghetti became the inspiration for a story in which the same thing happens. But in his story, the characters argue and the husband licks up the sauce from the floor. “That part didn’t really happen,” he laughs.
One might imagine writing as merely a hobby or diversion for practicing hospitalists. But those who indulge in the craft say it hones their medical skills.
Ron Grant, MD, pediatric hospitalist at the University of Arizona Medical Center in Tucson says writing affects his mood, which subsequently affects his practice. “It allows you to speak out [about] frustrations that arise, interesting situations that arise, and I find that very valuable,” he says.
The therapeutic experience is common to hospitalist writers.
Sandi Verbin, MD, a pediatric hospitalist at Holy Redeemer Hospital in Meadowbrook, Pa., says writing brings out her sense of humor, which helps with everything in medical practice. “Fortunately, with pediatrics, most of our patients get better,” she says.
But of course that’s not always the case. When a 7-year-old patient, who was in his care on and off for three years during his training, died of leukemia, Randy Ferrance, MD, a hospitalist at Riverside Tappahannock Hospital in Va., filtered the experience into a story.
“The piece was mostly biographical, but I put it in a fictional context,” says Dr. Ferrance. “I wrote it to say some of the things that I never did say, and work through things I never had worked through, with the patient and family. Writing helps me to clear my head and put things in a better perspective. It’s worth the time I carve out. It doesn’t affect the medical end of things, but it helps my ability to continue doing what I do.”
Many hospitalist writers say their art makes them more empathetic.
Joseph Geskey, DO, the division chief of pediatric hospital medicine at Penn State M.S. Hershey Medical Center in Pa., has published poetry in the Journal of the American Medical Association, an anthology in a book, essays, and fiction. “Writing allows you to clarify your thoughts, so it allows for some epiphanies, not only [regarding] writing but about life in general,” he says.
Preliminary studies suggest writing may have medical benefits such as reducing stress catecholamines and inflammatory markers. Though hard data are still to come, Dr. Geskey believes writing has made him a better physician. He says he is more patient, a better listener, and lets patients digress in their stories, revealing information he might not otherwise have learned. “If I’m able to use my rudimentary senses in my writing to evoke a scene or an image, how do I use those same senses to color in my interaction with patients, to help them feel better?” he asks.
The Trend Grows
There are a number of doctors who teach creative writing around the country, and writing workshops for physicians are popping up in and outside medical education curricula.
In Durham, N.C., Dr. Geskey participated in a Duke University poetry and medicine conference that he describes as “probably the most creative three or four days of my life.”
For three years, Bryan R. Fine, MD, MPH, pediatric hospitalist at Children’s National Medical Center in Washington, D.C., ran a creative writing elective for fourth-year medical students at George Washington University. Dr. Fine often writes during down time at work, especially on the night shift. He writes stories, nonfiction essays, and songs, which he performs publicly on occasion, including a few weeks each year at Club Med and other Caribbean locales.
Dr. Verbin has taken seminars in writing for children. “I’ve made some baby steps in that direction, but progress has been slow and mostly relegated to someday,’” she says.
In 1998, Dr. Grant left the University of Arizona, where he was practicing as a hospitalist for Cleo Hardin, MD, section chief of pediatric hospital medicine and herself a writer. (She is revising a memoir she wrote a couple years ago and beginning a novel about mothers and daughters). He traveled to Israel and Poland and wrote about that experience, then realized he wanted more. He returned to his school to pursue a master’s in creative writing. A year ago, at Dr. Hardin’s urging, he returned to medicine, now describing himself as a part-time hospitalist and full-time writer.
“I was overwhelmed by a lot of strange sensations when I went back to the hospital—all of which really informed my writing,” says Dr. Grant.
He is working on a memoir about leaving medicine after becoming uncomfortable with the ethical and personal dilemmas he faced as a pediatrician and as a father. “It’s hard to watch children die, but unbearable when you have children of your own,” he says.
Dr. Grant works nights, teaches medical students an elective in creative writing, and occasionally teaches at a community college. His most exciting teaching outlet is as an instructor in the Czech Republic at the prestigious Prague Summer Program, a study-abroad program offered through Western Michigan University. Those who take his the two-week memoir-writing workshop bring complete manuscripts for review and critique.
“The whole philosophy behind teaching writing and taking humanities classes is that there are unexplored areas of the brain that get withered as you go through medical school and residency,” Dr. Grant says. “Re-exploring that creative side allows us to become better physicians. Becoming more in touch with your own humanity allows you to be a more human practitioner, Even though I only practice part time, I’m certainly different as a practitioner than I was before [I started writing].”
As a full-time writer, Dr. Grant is the exception. But Dr. Nazario recalls a quote from physician Anton Chekhov that may sum things up for other hospitalist writers: “Medicine is my lawful wife, and literature is my mistress. When I get fed up with one, I spend the night with the other.” TH
Andrea Sattinger is a medical writer based in North Carolina.
When people hear that Ruben J. Nazario, MD, a pediatric hospitalist at Kentucky Children’s Hospital in Lexington, writes in his spare time, they assume he writes for children. “But my writing is very non-pediatric,” he says. “I’m two people in one.”
A native of Puerto Rico, Dr. Nazario primarily writes poetry in English and stories in Spanish. His short stories and novels deal with what he calls “the fun stuff”: passion, violence, death.
For example, a speck of tomato sauce falling on the floor when his wife served him a plate of spaghetti became the inspiration for a story in which the same thing happens. But in his story, the characters argue and the husband licks up the sauce from the floor. “That part didn’t really happen,” he laughs.
One might imagine writing as merely a hobby or diversion for practicing hospitalists. But those who indulge in the craft say it hones their medical skills.
Ron Grant, MD, pediatric hospitalist at the University of Arizona Medical Center in Tucson says writing affects his mood, which subsequently affects his practice. “It allows you to speak out [about] frustrations that arise, interesting situations that arise, and I find that very valuable,” he says.
The therapeutic experience is common to hospitalist writers.
Sandi Verbin, MD, a pediatric hospitalist at Holy Redeemer Hospital in Meadowbrook, Pa., says writing brings out her sense of humor, which helps with everything in medical practice. “Fortunately, with pediatrics, most of our patients get better,” she says.
But of course that’s not always the case. When a 7-year-old patient, who was in his care on and off for three years during his training, died of leukemia, Randy Ferrance, MD, a hospitalist at Riverside Tappahannock Hospital in Va., filtered the experience into a story.
“The piece was mostly biographical, but I put it in a fictional context,” says Dr. Ferrance. “I wrote it to say some of the things that I never did say, and work through things I never had worked through, with the patient and family. Writing helps me to clear my head and put things in a better perspective. It’s worth the time I carve out. It doesn’t affect the medical end of things, but it helps my ability to continue doing what I do.”
Many hospitalist writers say their art makes them more empathetic.
Joseph Geskey, DO, the division chief of pediatric hospital medicine at Penn State M.S. Hershey Medical Center in Pa., has published poetry in the Journal of the American Medical Association, an anthology in a book, essays, and fiction. “Writing allows you to clarify your thoughts, so it allows for some epiphanies, not only [regarding] writing but about life in general,” he says.
Preliminary studies suggest writing may have medical benefits such as reducing stress catecholamines and inflammatory markers. Though hard data are still to come, Dr. Geskey believes writing has made him a better physician. He says he is more patient, a better listener, and lets patients digress in their stories, revealing information he might not otherwise have learned. “If I’m able to use my rudimentary senses in my writing to evoke a scene or an image, how do I use those same senses to color in my interaction with patients, to help them feel better?” he asks.
The Trend Grows
There are a number of doctors who teach creative writing around the country, and writing workshops for physicians are popping up in and outside medical education curricula.
In Durham, N.C., Dr. Geskey participated in a Duke University poetry and medicine conference that he describes as “probably the most creative three or four days of my life.”
For three years, Bryan R. Fine, MD, MPH, pediatric hospitalist at Children’s National Medical Center in Washington, D.C., ran a creative writing elective for fourth-year medical students at George Washington University. Dr. Fine often writes during down time at work, especially on the night shift. He writes stories, nonfiction essays, and songs, which he performs publicly on occasion, including a few weeks each year at Club Med and other Caribbean locales.
Dr. Verbin has taken seminars in writing for children. “I’ve made some baby steps in that direction, but progress has been slow and mostly relegated to someday,’” she says.
In 1998, Dr. Grant left the University of Arizona, where he was practicing as a hospitalist for Cleo Hardin, MD, section chief of pediatric hospital medicine and herself a writer. (She is revising a memoir she wrote a couple years ago and beginning a novel about mothers and daughters). He traveled to Israel and Poland and wrote about that experience, then realized he wanted more. He returned to his school to pursue a master’s in creative writing. A year ago, at Dr. Hardin’s urging, he returned to medicine, now describing himself as a part-time hospitalist and full-time writer.
“I was overwhelmed by a lot of strange sensations when I went back to the hospital—all of which really informed my writing,” says Dr. Grant.
He is working on a memoir about leaving medicine after becoming uncomfortable with the ethical and personal dilemmas he faced as a pediatrician and as a father. “It’s hard to watch children die, but unbearable when you have children of your own,” he says.
Dr. Grant works nights, teaches medical students an elective in creative writing, and occasionally teaches at a community college. His most exciting teaching outlet is as an instructor in the Czech Republic at the prestigious Prague Summer Program, a study-abroad program offered through Western Michigan University. Those who take his the two-week memoir-writing workshop bring complete manuscripts for review and critique.
“The whole philosophy behind teaching writing and taking humanities classes is that there are unexplored areas of the brain that get withered as you go through medical school and residency,” Dr. Grant says. “Re-exploring that creative side allows us to become better physicians. Becoming more in touch with your own humanity allows you to be a more human practitioner, Even though I only practice part time, I’m certainly different as a practitioner than I was before [I started writing].”
As a full-time writer, Dr. Grant is the exception. But Dr. Nazario recalls a quote from physician Anton Chekhov that may sum things up for other hospitalist writers: “Medicine is my lawful wife, and literature is my mistress. When I get fed up with one, I spend the night with the other.” TH
Andrea Sattinger is a medical writer based in North Carolina.
A Fine Formation
In the football-loving state of Michigan, legendary athletes take their cues from a coach and map their strategies for one big group effort. But Michigan is also home to what may be the first-ever homegrown regional consortium for patient safety and quality improvement—and in this case—after a huddle each team member gets to call his own plays.
The Hospitalists as Emerging Leaders in Patient Safety (HELPS) Consortium of Southeastern Michigan (funded by a grant from the Blue Cross Blue Shield of Michigan Foundation) includes representatives from nine regional hospitalist programs representing 11 hospitals and approximately 75,000 patients.1
The participants in this program identify proven patient safety practices and facilitate widespread dissemination of those practices among hospitalists.
The member institutions include academic medical centers, large private teaching and non-teaching hospitals, federal facilities, and urban and rural hospitals.
Each institution is represented by a hospitalist—usually the director of the hospitalist program or the individual most interested in and familiar with quality improvement—and a representative from quality improvement or patient safety. The issues they have addressed, which emerged from a variety of sources, such as the Agency of Healthcare Research and Quality, the National Quality Forum, and the Joint Commission on Accreditation of Healthcare Organizations, are those that are commonly encountered in hospitalist practice. These physicians “are bridging the gap between that which they know to be effective and that which is actually practiced.”1
HELPS builds on the experience of medical professionals who have united geographically dispersed physicians from the same specialty to boost quality. The HELPS consortium also aids participating institutions in evaluating outcomes after implementing a targeted patient safety practice, thereby allowing rapid cycle improvement while identifying factors associated with success.
“We have gotten the work that is being done by these different organizations out there, brought it up a notch in certain situations—we like to think—and have gotten it effectively disseminated to a larger group of hospitalists,” says Scott Flanders, MD, an associate professor of medicine at the University of Michigan (Ann Arbor), director of the hospital medicine program there, and an SHM board member.
Where They Are
The consortium is about three-quarters of the way through its overall estimated project period, says Dr. Flanders. It originally planned to have nine gatherings over two years. (See Table 1, p. 35.) To date the consortium has held seven of those sessions and have met roughly every two to three months. End-of-life care and the final wrap-up are the only sessions still to be completed.
The individual sites took on projects that included reducing errors with heparin use in hospitalized patients, reducing falls in hospitalized patients, improving care transitions (a collaborative multidisciplinary approach), reducing unnecessary ICU admission and preventing in-hospital cardiac arrests, reducing urinary catheter infections, improving rates of appropriate deep vein thrombosis prophylaxis, and implementing best practices for reducing central line infections. A national expert conducted a session on implementing a program to reduce perioperative cardiovascular events while ensuring the appropriate use of perioperative beta-blockers.
Challenges and Lessons Learned
From the outset, the HELPS group knew that its primary challenge would be to fulfill the intention to meet as a complete group four or five times per year. “There aren’t a lot of hospitalists who have big parts of their jobs carved out for dedicated time to work on quality improvement research or patient safety,” says Dr. Flanders. “It’s part of what we do in our day, but in terms of taking on a big project, designing it, implementing it, and measuring its effect, it is hard to do in the day-to-day job of most hospitalist groups.”
He suspects that hospitalists frequently help steering committees address certain issues, “but it may not be the individual hospitalist group that is managing or driving the quality issue for an entire hospital or health system.” The HELPS physicians knew that if they could surmount the scheduling challenge, however, they would have a terrific opportunity to learn from each other and move their individual institutional patient safety initiatives forward.
They also knew that the majority of hospitalized patients receive care in community hospitals and that the culture of a community hospital differed dramatically from a tertiary-care academic medical center. Interventions would need to be tried at varied settings, and HELPS would allow that to happen. In addition, few clinically active hospitalists have developed the research expertise to evaluate an intervention rigorously at their own institution, yet decision makers often require such an evaluation when they are considering adopting a new intervention. Using the resources of an academic center such as the University of Michigan, where evaluative and methodologic expertise is available, allowed them to facilitate a resolution for that problem. “As physicians, we are helping [smaller hospitals] by facilitating data collection and data analysis for their ongoing projects,” says Dr. Flanders.
Another challenge the hospitalists faced pertained to the relative instability of hospital medicine compared with other specialties. For instance, it is probably far easier for the members of the consortium of cardiology groups working on best practices for managing acute myocardial infarction to find time to work together. In contrast, because hospital medicine is a relatively new specialty, “we are seeing a certain amount of instability,” explains Dr. Flanders. “Of our nine involved health systems, at least two had dramatic organizational and structural changes within their hospital medicine group over the last year and a half.” One hospital medicine director left, with repercussions in several areas, and, in another group, the practice was sold to a large physician management company, which meant that the HELPS data that had been collected was no longer owned by the [original] group, making their activities more complex.
What They’ve Done So Far
Dr. Flanders is not aware of any other groups of physicians from another state who have undertaken such a project. The Institute for Healthcare Improvement’s “100,000 Lives Campaign” may be similar in some ways, focusing on a few key topic areas. The Michigan Keystone Project, which concentrated on various ICU patient safety topics, is another example of a regional consortium. “But the difference is that they basically drive the agenda,” he says. “They say, ‘This is what we want you all to do, and let’s figure out how we can all do it.’ In our case, we focused on some key areas, but we did not dictate what the project was.”
The following brief recaps represent some of the projects undertaken by consortium member sites.
Falls
The University of Michigan-affiliated Ann Arbor Veterans Affairs (VA) Hospital, where Sanjay Saint, MD, MPH, is a hospitalist, has many elderly and cognitively impaired patients, so preventing falls is a big issue. “My responsibility isn’t to prevent falls but to share these best practices with others in my organization,” he says. “In fact, each project team points out where to look with a certain problem but not necessarily what to do.”
Dr. Saint brought up the issue of mattresses with lipped/raised edges to prevent patients from rolling out of bed. Following that, at least one other consortium hospital suggested to its fall prevention group that they explore the use of these lipped mattresses.
Bed alarms were another problem. Participants shared a common problem: Often, nurses wouldn’t hear a patient’s alarm go off. Other providers might reset them, but if they neglected to let the assigned nurse know the patient was calling, the patient might get tired of waiting, attempt to get out of bed, and sustain a fall. Consequently, providers in most institutions thought the alarms were not useful. But one institution identified a novel way to use bed alarms: attaching them to the nurse’s pager. Now, when the alarm goes off, it alerts the appropriate nurse directly, and because that nurse is responsible for resetting the alarm, she knows that the patient has called and needs help.
Changing Names: CARE Assistants
To avoid the use of physical or chemical restraints, many institutions have resorted to hiring “sitters” who stay at the bedside of confused or delirious patients to calm them; if patients try to get out of bed, sitters are there to coax them back in. A number of HELPS institutions shared the idea that using the term “sitter” might have been inadvertently encouraging inactivity: Too many sitters were doing just that, sitting all day, often watching television.
One of the collaborative sites now calls these employees CARE assistants, an acronym for Caring Alternative to a Restraint-free Environment. The group has predicted that calling them something different will inspire these people to “do more caring and less sitting,” says Dr. Saint. After a HELPS session, Dr. Saint submitted this idea to the key decision makers at the VA. “I could have tried by myself to resolve this dilemma for years and not come up with that idea,” he says. “Why not just take what they’ve done and modify it to suit your own environment?”
Weighty Problem: Heparin Dosing
One hospital in the consortium conducted a project on medication safety that focused on appropriate use of heparin in hospitalized patients. When the site’s hospitalists began studying the problems they were having, they realized that the weights they were using for dosing decisions were being generated in the emergency department (ED). Studying it further, they saw that, most of the time, those patients weren’t actually being weighed; nurses were simply estimating their weights. Having traced the problem to the ED, they were then able to intervene, fix the problem, and show that by doing so their rates of bleeding complications from inappropriate dosing of anticoagulants improved.
At his own institution, Dr. Flanders was participating in a group committee meeting discussing this problem. Consequently, “I was able to ask, ‘Have we looked at weights [being assessed] in the emergency department?’ Everyone involved with that project said, ‘No, why?’ And, sure enough, a similar problem existed.”
Care Transitions and Multidisciplinary Rounding
One member-team of the consortium was able to come up with a multidisciplinary team that met and rounded on patients each day and focused on the care transitions. They were able to dramatically improve staff communication, the overall discharge process, and patient satisfaction. As a result of what he learned of their successes, Dr. Flanders’ institution plans to use a similar strategy to enhance communication among healthcare providers involved in the discharge process on their hospitalist unit.
Rapid Response Teams and Input from Residents
“It’s very helpful to hear, from another site, the challenges and benefits of having hospitalists involved with the rapid response teams,” says Dr. Saint. “How did they operationalize it? What were the remaining challenges? What outcome measures did they use? How do you assess whether it’s worth the cost? What do residents think about this?
This last point turned out to be a valuable question to ask. The group included some residents at the site where this project was piloted and had a fruitful discussion. Adding the perspective of residents along with faculty, says Dr. Saint, as well as a couple of nurses and quality care managers, allows a synergy and combination of ideas that led to effective solutions. “Those are exactly the individuals who need to be around a table to overcome some of the challenges.” They have also considered inviting nursing students. “Before they get inculcated in thinking a certain way,” he says, “why not hear what they have to say?”
Dr. Saint believes, however, that this is not a step to be taken lightly. If you are going to include people, “then you have to act on their suggestions or at least hear them out and say why you’re not going to take their suggestions because a good way to get people to become jaded is to listen to their feedback and then just ignore it.”
Calling in Outside Experts
To focus on the issue of preventing hospital-acquired urinary tract infections (UTIs), the consortium invited Russell Olmstead, MPH, an infection control expert and epidemiologist at one of the HELPS sites and past president of the Michigan Society of Infection Control.
“We’d like to do a Keystone[-type] UTI project,” says Dr. Saint, referring to the federally funded statewide three-year initiative, conducted in collaboration with the Michigan Hospital Association and Johns Hopkins Research and Safety Group, that focused on applying evidence-based medicine and quality improvement efforts to prevent ventilator-associated pneumonia and central line-related infections. “We’ve called it the Bladder Bundle; that is, you bundle a group of practices together, and you give the hospitalists who want to participate a toolkit in order to roll this out.”
Although the details still need to be finalized, the project would include ensuring that patients have appropriate indication for an indwelling catheter, that the indwelling catheter is inserted in an aseptic manner, that there was some type of assessment of discontinuation after a certain amount of time, and that alternatives to an indwelling catheter are considered.
Another expert consulting with the consortium was Peter Lindenauer, MD, MSc, with the Division of Healthcare Quality, Baystate Medical Center, Springfield, Mass., and the Department of Medicine, Tufts University School of Medicine, Boston. Dr. Lindenauer came to discuss lessons he and his colleagues have learned from efforts to improve appropriate perioperative beta blocker use.
The final HELPS wrap-up session for the group will include another nationally renowned expert in patient safety.
SHARP: Research Translated into Practice
Another project initiated by the Michigan hospitalists will generate and disseminate new knowledge in the realm of clinical research. The Specialist-Hospitalist Allied Research Program (SHARP), directed by Dr. Flanders and Brahmajee Nallamothu, MD, MPH, an interventional cardiologist, is the first specialist-hospitalist clinical research program in the United States. This hospitalist delivery model alters the way clinical problems are approached and creates opportunities and challenges in implementing best practices, including those surrounding drugs and devices. A successful clinical and translational research program will combine specialists and hospitalists working collaboratively to better understand the best ways to care for inpatients.
This project is similar to what cardiology and oncology specialties have done over the last several decades, says Dr. Saint. In the future, he foresees that the NIH will increasingly focus on translating research into practice in diverse settings. Both specialists and hospitalists who work in a particular area together—such as prevention of lower extremity clots or of nosocomial infections—can use the health consortium to roll out protocols and studies in order to tackle some of the important inpatient topics.
SHARP was awarded funding through the University of Michigan Department of Medicine and was scheduled to take off in February. “Our hope is that we will be able to take advantage of and build upon the health collaborative that we have and bring in our subspecialty expertise to help inform clinical investigations,” says Dr. Saint.
Where They’re Going
Both Dr. Flanders and Dr. Saint are pleased about the HELPS consortium’s progress so far. They believe that they have found a group of people who are interested in patient safety and are willing to learn from one another and that they have done an excellent job of disseminating the best practices they have been exploring.
Ultimately, their goal is to grow this into a “more robust clinical research consortium,” says Dr. Flanders. Instead of disseminating best practices and focusing on just a few targeted patient safety quality improvement areas, they will begin to take on studies that could center around patient safety and quality improvement but will also move toward multi-center projects that might address issues related to management of common clinical problems that hospitalists are now managing and focusing on.
“We’re really excited about what we have been able to accomplish,” he says. “We’ve learned a lot about the challenges of doing this, and of course it’s never perfect. We wish we could always do more, but we’ve learned why we can’t. That will be helpful in future projects and helpful for others who are trying to tackle this same problem.” TH
Reference
- Flanders SA, Kaufman SR, Saint S. Hospitalists as emerging leaders in patient safety: targeting a few to affect many. J Patient Safety. 2005;1(2):78-82.
In the football-loving state of Michigan, legendary athletes take their cues from a coach and map their strategies for one big group effort. But Michigan is also home to what may be the first-ever homegrown regional consortium for patient safety and quality improvement—and in this case—after a huddle each team member gets to call his own plays.
The Hospitalists as Emerging Leaders in Patient Safety (HELPS) Consortium of Southeastern Michigan (funded by a grant from the Blue Cross Blue Shield of Michigan Foundation) includes representatives from nine regional hospitalist programs representing 11 hospitals and approximately 75,000 patients.1
The participants in this program identify proven patient safety practices and facilitate widespread dissemination of those practices among hospitalists.
The member institutions include academic medical centers, large private teaching and non-teaching hospitals, federal facilities, and urban and rural hospitals.
Each institution is represented by a hospitalist—usually the director of the hospitalist program or the individual most interested in and familiar with quality improvement—and a representative from quality improvement or patient safety. The issues they have addressed, which emerged from a variety of sources, such as the Agency of Healthcare Research and Quality, the National Quality Forum, and the Joint Commission on Accreditation of Healthcare Organizations, are those that are commonly encountered in hospitalist practice. These physicians “are bridging the gap between that which they know to be effective and that which is actually practiced.”1
HELPS builds on the experience of medical professionals who have united geographically dispersed physicians from the same specialty to boost quality. The HELPS consortium also aids participating institutions in evaluating outcomes after implementing a targeted patient safety practice, thereby allowing rapid cycle improvement while identifying factors associated with success.
“We have gotten the work that is being done by these different organizations out there, brought it up a notch in certain situations—we like to think—and have gotten it effectively disseminated to a larger group of hospitalists,” says Scott Flanders, MD, an associate professor of medicine at the University of Michigan (Ann Arbor), director of the hospital medicine program there, and an SHM board member.
Where They Are
The consortium is about three-quarters of the way through its overall estimated project period, says Dr. Flanders. It originally planned to have nine gatherings over two years. (See Table 1, p. 35.) To date the consortium has held seven of those sessions and have met roughly every two to three months. End-of-life care and the final wrap-up are the only sessions still to be completed.
The individual sites took on projects that included reducing errors with heparin use in hospitalized patients, reducing falls in hospitalized patients, improving care transitions (a collaborative multidisciplinary approach), reducing unnecessary ICU admission and preventing in-hospital cardiac arrests, reducing urinary catheter infections, improving rates of appropriate deep vein thrombosis prophylaxis, and implementing best practices for reducing central line infections. A national expert conducted a session on implementing a program to reduce perioperative cardiovascular events while ensuring the appropriate use of perioperative beta-blockers.
Challenges and Lessons Learned
From the outset, the HELPS group knew that its primary challenge would be to fulfill the intention to meet as a complete group four or five times per year. “There aren’t a lot of hospitalists who have big parts of their jobs carved out for dedicated time to work on quality improvement research or patient safety,” says Dr. Flanders. “It’s part of what we do in our day, but in terms of taking on a big project, designing it, implementing it, and measuring its effect, it is hard to do in the day-to-day job of most hospitalist groups.”
He suspects that hospitalists frequently help steering committees address certain issues, “but it may not be the individual hospitalist group that is managing or driving the quality issue for an entire hospital or health system.” The HELPS physicians knew that if they could surmount the scheduling challenge, however, they would have a terrific opportunity to learn from each other and move their individual institutional patient safety initiatives forward.
They also knew that the majority of hospitalized patients receive care in community hospitals and that the culture of a community hospital differed dramatically from a tertiary-care academic medical center. Interventions would need to be tried at varied settings, and HELPS would allow that to happen. In addition, few clinically active hospitalists have developed the research expertise to evaluate an intervention rigorously at their own institution, yet decision makers often require such an evaluation when they are considering adopting a new intervention. Using the resources of an academic center such as the University of Michigan, where evaluative and methodologic expertise is available, allowed them to facilitate a resolution for that problem. “As physicians, we are helping [smaller hospitals] by facilitating data collection and data analysis for their ongoing projects,” says Dr. Flanders.
Another challenge the hospitalists faced pertained to the relative instability of hospital medicine compared with other specialties. For instance, it is probably far easier for the members of the consortium of cardiology groups working on best practices for managing acute myocardial infarction to find time to work together. In contrast, because hospital medicine is a relatively new specialty, “we are seeing a certain amount of instability,” explains Dr. Flanders. “Of our nine involved health systems, at least two had dramatic organizational and structural changes within their hospital medicine group over the last year and a half.” One hospital medicine director left, with repercussions in several areas, and, in another group, the practice was sold to a large physician management company, which meant that the HELPS data that had been collected was no longer owned by the [original] group, making their activities more complex.
What They’ve Done So Far
Dr. Flanders is not aware of any other groups of physicians from another state who have undertaken such a project. The Institute for Healthcare Improvement’s “100,000 Lives Campaign” may be similar in some ways, focusing on a few key topic areas. The Michigan Keystone Project, which concentrated on various ICU patient safety topics, is another example of a regional consortium. “But the difference is that they basically drive the agenda,” he says. “They say, ‘This is what we want you all to do, and let’s figure out how we can all do it.’ In our case, we focused on some key areas, but we did not dictate what the project was.”
The following brief recaps represent some of the projects undertaken by consortium member sites.
Falls
The University of Michigan-affiliated Ann Arbor Veterans Affairs (VA) Hospital, where Sanjay Saint, MD, MPH, is a hospitalist, has many elderly and cognitively impaired patients, so preventing falls is a big issue. “My responsibility isn’t to prevent falls but to share these best practices with others in my organization,” he says. “In fact, each project team points out where to look with a certain problem but not necessarily what to do.”
Dr. Saint brought up the issue of mattresses with lipped/raised edges to prevent patients from rolling out of bed. Following that, at least one other consortium hospital suggested to its fall prevention group that they explore the use of these lipped mattresses.
Bed alarms were another problem. Participants shared a common problem: Often, nurses wouldn’t hear a patient’s alarm go off. Other providers might reset them, but if they neglected to let the assigned nurse know the patient was calling, the patient might get tired of waiting, attempt to get out of bed, and sustain a fall. Consequently, providers in most institutions thought the alarms were not useful. But one institution identified a novel way to use bed alarms: attaching them to the nurse’s pager. Now, when the alarm goes off, it alerts the appropriate nurse directly, and because that nurse is responsible for resetting the alarm, she knows that the patient has called and needs help.
Changing Names: CARE Assistants
To avoid the use of physical or chemical restraints, many institutions have resorted to hiring “sitters” who stay at the bedside of confused or delirious patients to calm them; if patients try to get out of bed, sitters are there to coax them back in. A number of HELPS institutions shared the idea that using the term “sitter” might have been inadvertently encouraging inactivity: Too many sitters were doing just that, sitting all day, often watching television.
One of the collaborative sites now calls these employees CARE assistants, an acronym for Caring Alternative to a Restraint-free Environment. The group has predicted that calling them something different will inspire these people to “do more caring and less sitting,” says Dr. Saint. After a HELPS session, Dr. Saint submitted this idea to the key decision makers at the VA. “I could have tried by myself to resolve this dilemma for years and not come up with that idea,” he says. “Why not just take what they’ve done and modify it to suit your own environment?”
Weighty Problem: Heparin Dosing
One hospital in the consortium conducted a project on medication safety that focused on appropriate use of heparin in hospitalized patients. When the site’s hospitalists began studying the problems they were having, they realized that the weights they were using for dosing decisions were being generated in the emergency department (ED). Studying it further, they saw that, most of the time, those patients weren’t actually being weighed; nurses were simply estimating their weights. Having traced the problem to the ED, they were then able to intervene, fix the problem, and show that by doing so their rates of bleeding complications from inappropriate dosing of anticoagulants improved.
At his own institution, Dr. Flanders was participating in a group committee meeting discussing this problem. Consequently, “I was able to ask, ‘Have we looked at weights [being assessed] in the emergency department?’ Everyone involved with that project said, ‘No, why?’ And, sure enough, a similar problem existed.”
Care Transitions and Multidisciplinary Rounding
One member-team of the consortium was able to come up with a multidisciplinary team that met and rounded on patients each day and focused on the care transitions. They were able to dramatically improve staff communication, the overall discharge process, and patient satisfaction. As a result of what he learned of their successes, Dr. Flanders’ institution plans to use a similar strategy to enhance communication among healthcare providers involved in the discharge process on their hospitalist unit.
Rapid Response Teams and Input from Residents
“It’s very helpful to hear, from another site, the challenges and benefits of having hospitalists involved with the rapid response teams,” says Dr. Saint. “How did they operationalize it? What were the remaining challenges? What outcome measures did they use? How do you assess whether it’s worth the cost? What do residents think about this?
This last point turned out to be a valuable question to ask. The group included some residents at the site where this project was piloted and had a fruitful discussion. Adding the perspective of residents along with faculty, says Dr. Saint, as well as a couple of nurses and quality care managers, allows a synergy and combination of ideas that led to effective solutions. “Those are exactly the individuals who need to be around a table to overcome some of the challenges.” They have also considered inviting nursing students. “Before they get inculcated in thinking a certain way,” he says, “why not hear what they have to say?”
Dr. Saint believes, however, that this is not a step to be taken lightly. If you are going to include people, “then you have to act on their suggestions or at least hear them out and say why you’re not going to take their suggestions because a good way to get people to become jaded is to listen to their feedback and then just ignore it.”
Calling in Outside Experts
To focus on the issue of preventing hospital-acquired urinary tract infections (UTIs), the consortium invited Russell Olmstead, MPH, an infection control expert and epidemiologist at one of the HELPS sites and past president of the Michigan Society of Infection Control.
“We’d like to do a Keystone[-type] UTI project,” says Dr. Saint, referring to the federally funded statewide three-year initiative, conducted in collaboration with the Michigan Hospital Association and Johns Hopkins Research and Safety Group, that focused on applying evidence-based medicine and quality improvement efforts to prevent ventilator-associated pneumonia and central line-related infections. “We’ve called it the Bladder Bundle; that is, you bundle a group of practices together, and you give the hospitalists who want to participate a toolkit in order to roll this out.”
Although the details still need to be finalized, the project would include ensuring that patients have appropriate indication for an indwelling catheter, that the indwelling catheter is inserted in an aseptic manner, that there was some type of assessment of discontinuation after a certain amount of time, and that alternatives to an indwelling catheter are considered.
Another expert consulting with the consortium was Peter Lindenauer, MD, MSc, with the Division of Healthcare Quality, Baystate Medical Center, Springfield, Mass., and the Department of Medicine, Tufts University School of Medicine, Boston. Dr. Lindenauer came to discuss lessons he and his colleagues have learned from efforts to improve appropriate perioperative beta blocker use.
The final HELPS wrap-up session for the group will include another nationally renowned expert in patient safety.
SHARP: Research Translated into Practice
Another project initiated by the Michigan hospitalists will generate and disseminate new knowledge in the realm of clinical research. The Specialist-Hospitalist Allied Research Program (SHARP), directed by Dr. Flanders and Brahmajee Nallamothu, MD, MPH, an interventional cardiologist, is the first specialist-hospitalist clinical research program in the United States. This hospitalist delivery model alters the way clinical problems are approached and creates opportunities and challenges in implementing best practices, including those surrounding drugs and devices. A successful clinical and translational research program will combine specialists and hospitalists working collaboratively to better understand the best ways to care for inpatients.
This project is similar to what cardiology and oncology specialties have done over the last several decades, says Dr. Saint. In the future, he foresees that the NIH will increasingly focus on translating research into practice in diverse settings. Both specialists and hospitalists who work in a particular area together—such as prevention of lower extremity clots or of nosocomial infections—can use the health consortium to roll out protocols and studies in order to tackle some of the important inpatient topics.
SHARP was awarded funding through the University of Michigan Department of Medicine and was scheduled to take off in February. “Our hope is that we will be able to take advantage of and build upon the health collaborative that we have and bring in our subspecialty expertise to help inform clinical investigations,” says Dr. Saint.
Where They’re Going
Both Dr. Flanders and Dr. Saint are pleased about the HELPS consortium’s progress so far. They believe that they have found a group of people who are interested in patient safety and are willing to learn from one another and that they have done an excellent job of disseminating the best practices they have been exploring.
Ultimately, their goal is to grow this into a “more robust clinical research consortium,” says Dr. Flanders. Instead of disseminating best practices and focusing on just a few targeted patient safety quality improvement areas, they will begin to take on studies that could center around patient safety and quality improvement but will also move toward multi-center projects that might address issues related to management of common clinical problems that hospitalists are now managing and focusing on.
“We’re really excited about what we have been able to accomplish,” he says. “We’ve learned a lot about the challenges of doing this, and of course it’s never perfect. We wish we could always do more, but we’ve learned why we can’t. That will be helpful in future projects and helpful for others who are trying to tackle this same problem.” TH
Reference
- Flanders SA, Kaufman SR, Saint S. Hospitalists as emerging leaders in patient safety: targeting a few to affect many. J Patient Safety. 2005;1(2):78-82.
In the football-loving state of Michigan, legendary athletes take their cues from a coach and map their strategies for one big group effort. But Michigan is also home to what may be the first-ever homegrown regional consortium for patient safety and quality improvement—and in this case—after a huddle each team member gets to call his own plays.
The Hospitalists as Emerging Leaders in Patient Safety (HELPS) Consortium of Southeastern Michigan (funded by a grant from the Blue Cross Blue Shield of Michigan Foundation) includes representatives from nine regional hospitalist programs representing 11 hospitals and approximately 75,000 patients.1
The participants in this program identify proven patient safety practices and facilitate widespread dissemination of those practices among hospitalists.
The member institutions include academic medical centers, large private teaching and non-teaching hospitals, federal facilities, and urban and rural hospitals.
Each institution is represented by a hospitalist—usually the director of the hospitalist program or the individual most interested in and familiar with quality improvement—and a representative from quality improvement or patient safety. The issues they have addressed, which emerged from a variety of sources, such as the Agency of Healthcare Research and Quality, the National Quality Forum, and the Joint Commission on Accreditation of Healthcare Organizations, are those that are commonly encountered in hospitalist practice. These physicians “are bridging the gap between that which they know to be effective and that which is actually practiced.”1
HELPS builds on the experience of medical professionals who have united geographically dispersed physicians from the same specialty to boost quality. The HELPS consortium also aids participating institutions in evaluating outcomes after implementing a targeted patient safety practice, thereby allowing rapid cycle improvement while identifying factors associated with success.
“We have gotten the work that is being done by these different organizations out there, brought it up a notch in certain situations—we like to think—and have gotten it effectively disseminated to a larger group of hospitalists,” says Scott Flanders, MD, an associate professor of medicine at the University of Michigan (Ann Arbor), director of the hospital medicine program there, and an SHM board member.
Where They Are
The consortium is about three-quarters of the way through its overall estimated project period, says Dr. Flanders. It originally planned to have nine gatherings over two years. (See Table 1, p. 35.) To date the consortium has held seven of those sessions and have met roughly every two to three months. End-of-life care and the final wrap-up are the only sessions still to be completed.
The individual sites took on projects that included reducing errors with heparin use in hospitalized patients, reducing falls in hospitalized patients, improving care transitions (a collaborative multidisciplinary approach), reducing unnecessary ICU admission and preventing in-hospital cardiac arrests, reducing urinary catheter infections, improving rates of appropriate deep vein thrombosis prophylaxis, and implementing best practices for reducing central line infections. A national expert conducted a session on implementing a program to reduce perioperative cardiovascular events while ensuring the appropriate use of perioperative beta-blockers.
Challenges and Lessons Learned
From the outset, the HELPS group knew that its primary challenge would be to fulfill the intention to meet as a complete group four or five times per year. “There aren’t a lot of hospitalists who have big parts of their jobs carved out for dedicated time to work on quality improvement research or patient safety,” says Dr. Flanders. “It’s part of what we do in our day, but in terms of taking on a big project, designing it, implementing it, and measuring its effect, it is hard to do in the day-to-day job of most hospitalist groups.”
He suspects that hospitalists frequently help steering committees address certain issues, “but it may not be the individual hospitalist group that is managing or driving the quality issue for an entire hospital or health system.” The HELPS physicians knew that if they could surmount the scheduling challenge, however, they would have a terrific opportunity to learn from each other and move their individual institutional patient safety initiatives forward.
They also knew that the majority of hospitalized patients receive care in community hospitals and that the culture of a community hospital differed dramatically from a tertiary-care academic medical center. Interventions would need to be tried at varied settings, and HELPS would allow that to happen. In addition, few clinically active hospitalists have developed the research expertise to evaluate an intervention rigorously at their own institution, yet decision makers often require such an evaluation when they are considering adopting a new intervention. Using the resources of an academic center such as the University of Michigan, where evaluative and methodologic expertise is available, allowed them to facilitate a resolution for that problem. “As physicians, we are helping [smaller hospitals] by facilitating data collection and data analysis for their ongoing projects,” says Dr. Flanders.
Another challenge the hospitalists faced pertained to the relative instability of hospital medicine compared with other specialties. For instance, it is probably far easier for the members of the consortium of cardiology groups working on best practices for managing acute myocardial infarction to find time to work together. In contrast, because hospital medicine is a relatively new specialty, “we are seeing a certain amount of instability,” explains Dr. Flanders. “Of our nine involved health systems, at least two had dramatic organizational and structural changes within their hospital medicine group over the last year and a half.” One hospital medicine director left, with repercussions in several areas, and, in another group, the practice was sold to a large physician management company, which meant that the HELPS data that had been collected was no longer owned by the [original] group, making their activities more complex.
What They’ve Done So Far
Dr. Flanders is not aware of any other groups of physicians from another state who have undertaken such a project. The Institute for Healthcare Improvement’s “100,000 Lives Campaign” may be similar in some ways, focusing on a few key topic areas. The Michigan Keystone Project, which concentrated on various ICU patient safety topics, is another example of a regional consortium. “But the difference is that they basically drive the agenda,” he says. “They say, ‘This is what we want you all to do, and let’s figure out how we can all do it.’ In our case, we focused on some key areas, but we did not dictate what the project was.”
The following brief recaps represent some of the projects undertaken by consortium member sites.
Falls
The University of Michigan-affiliated Ann Arbor Veterans Affairs (VA) Hospital, where Sanjay Saint, MD, MPH, is a hospitalist, has many elderly and cognitively impaired patients, so preventing falls is a big issue. “My responsibility isn’t to prevent falls but to share these best practices with others in my organization,” he says. “In fact, each project team points out where to look with a certain problem but not necessarily what to do.”
Dr. Saint brought up the issue of mattresses with lipped/raised edges to prevent patients from rolling out of bed. Following that, at least one other consortium hospital suggested to its fall prevention group that they explore the use of these lipped mattresses.
Bed alarms were another problem. Participants shared a common problem: Often, nurses wouldn’t hear a patient’s alarm go off. Other providers might reset them, but if they neglected to let the assigned nurse know the patient was calling, the patient might get tired of waiting, attempt to get out of bed, and sustain a fall. Consequently, providers in most institutions thought the alarms were not useful. But one institution identified a novel way to use bed alarms: attaching them to the nurse’s pager. Now, when the alarm goes off, it alerts the appropriate nurse directly, and because that nurse is responsible for resetting the alarm, she knows that the patient has called and needs help.
Changing Names: CARE Assistants
To avoid the use of physical or chemical restraints, many institutions have resorted to hiring “sitters” who stay at the bedside of confused or delirious patients to calm them; if patients try to get out of bed, sitters are there to coax them back in. A number of HELPS institutions shared the idea that using the term “sitter” might have been inadvertently encouraging inactivity: Too many sitters were doing just that, sitting all day, often watching television.
One of the collaborative sites now calls these employees CARE assistants, an acronym for Caring Alternative to a Restraint-free Environment. The group has predicted that calling them something different will inspire these people to “do more caring and less sitting,” says Dr. Saint. After a HELPS session, Dr. Saint submitted this idea to the key decision makers at the VA. “I could have tried by myself to resolve this dilemma for years and not come up with that idea,” he says. “Why not just take what they’ve done and modify it to suit your own environment?”
Weighty Problem: Heparin Dosing
One hospital in the consortium conducted a project on medication safety that focused on appropriate use of heparin in hospitalized patients. When the site’s hospitalists began studying the problems they were having, they realized that the weights they were using for dosing decisions were being generated in the emergency department (ED). Studying it further, they saw that, most of the time, those patients weren’t actually being weighed; nurses were simply estimating their weights. Having traced the problem to the ED, they were then able to intervene, fix the problem, and show that by doing so their rates of bleeding complications from inappropriate dosing of anticoagulants improved.
At his own institution, Dr. Flanders was participating in a group committee meeting discussing this problem. Consequently, “I was able to ask, ‘Have we looked at weights [being assessed] in the emergency department?’ Everyone involved with that project said, ‘No, why?’ And, sure enough, a similar problem existed.”
Care Transitions and Multidisciplinary Rounding
One member-team of the consortium was able to come up with a multidisciplinary team that met and rounded on patients each day and focused on the care transitions. They were able to dramatically improve staff communication, the overall discharge process, and patient satisfaction. As a result of what he learned of their successes, Dr. Flanders’ institution plans to use a similar strategy to enhance communication among healthcare providers involved in the discharge process on their hospitalist unit.
Rapid Response Teams and Input from Residents
“It’s very helpful to hear, from another site, the challenges and benefits of having hospitalists involved with the rapid response teams,” says Dr. Saint. “How did they operationalize it? What were the remaining challenges? What outcome measures did they use? How do you assess whether it’s worth the cost? What do residents think about this?
This last point turned out to be a valuable question to ask. The group included some residents at the site where this project was piloted and had a fruitful discussion. Adding the perspective of residents along with faculty, says Dr. Saint, as well as a couple of nurses and quality care managers, allows a synergy and combination of ideas that led to effective solutions. “Those are exactly the individuals who need to be around a table to overcome some of the challenges.” They have also considered inviting nursing students. “Before they get inculcated in thinking a certain way,” he says, “why not hear what they have to say?”
Dr. Saint believes, however, that this is not a step to be taken lightly. If you are going to include people, “then you have to act on their suggestions or at least hear them out and say why you’re not going to take their suggestions because a good way to get people to become jaded is to listen to their feedback and then just ignore it.”
Calling in Outside Experts
To focus on the issue of preventing hospital-acquired urinary tract infections (UTIs), the consortium invited Russell Olmstead, MPH, an infection control expert and epidemiologist at one of the HELPS sites and past president of the Michigan Society of Infection Control.
“We’d like to do a Keystone[-type] UTI project,” says Dr. Saint, referring to the federally funded statewide three-year initiative, conducted in collaboration with the Michigan Hospital Association and Johns Hopkins Research and Safety Group, that focused on applying evidence-based medicine and quality improvement efforts to prevent ventilator-associated pneumonia and central line-related infections. “We’ve called it the Bladder Bundle; that is, you bundle a group of practices together, and you give the hospitalists who want to participate a toolkit in order to roll this out.”
Although the details still need to be finalized, the project would include ensuring that patients have appropriate indication for an indwelling catheter, that the indwelling catheter is inserted in an aseptic manner, that there was some type of assessment of discontinuation after a certain amount of time, and that alternatives to an indwelling catheter are considered.
Another expert consulting with the consortium was Peter Lindenauer, MD, MSc, with the Division of Healthcare Quality, Baystate Medical Center, Springfield, Mass., and the Department of Medicine, Tufts University School of Medicine, Boston. Dr. Lindenauer came to discuss lessons he and his colleagues have learned from efforts to improve appropriate perioperative beta blocker use.
The final HELPS wrap-up session for the group will include another nationally renowned expert in patient safety.
SHARP: Research Translated into Practice
Another project initiated by the Michigan hospitalists will generate and disseminate new knowledge in the realm of clinical research. The Specialist-Hospitalist Allied Research Program (SHARP), directed by Dr. Flanders and Brahmajee Nallamothu, MD, MPH, an interventional cardiologist, is the first specialist-hospitalist clinical research program in the United States. This hospitalist delivery model alters the way clinical problems are approached and creates opportunities and challenges in implementing best practices, including those surrounding drugs and devices. A successful clinical and translational research program will combine specialists and hospitalists working collaboratively to better understand the best ways to care for inpatients.
This project is similar to what cardiology and oncology specialties have done over the last several decades, says Dr. Saint. In the future, he foresees that the NIH will increasingly focus on translating research into practice in diverse settings. Both specialists and hospitalists who work in a particular area together—such as prevention of lower extremity clots or of nosocomial infections—can use the health consortium to roll out protocols and studies in order to tackle some of the important inpatient topics.
SHARP was awarded funding through the University of Michigan Department of Medicine and was scheduled to take off in February. “Our hope is that we will be able to take advantage of and build upon the health collaborative that we have and bring in our subspecialty expertise to help inform clinical investigations,” says Dr. Saint.
Where They’re Going
Both Dr. Flanders and Dr. Saint are pleased about the HELPS consortium’s progress so far. They believe that they have found a group of people who are interested in patient safety and are willing to learn from one another and that they have done an excellent job of disseminating the best practices they have been exploring.
Ultimately, their goal is to grow this into a “more robust clinical research consortium,” says Dr. Flanders. Instead of disseminating best practices and focusing on just a few targeted patient safety quality improvement areas, they will begin to take on studies that could center around patient safety and quality improvement but will also move toward multi-center projects that might address issues related to management of common clinical problems that hospitalists are now managing and focusing on.
“We’re really excited about what we have been able to accomplish,” he says. “We’ve learned a lot about the challenges of doing this, and of course it’s never perfect. We wish we could always do more, but we’ve learned why we can’t. That will be helpful in future projects and helpful for others who are trying to tackle this same problem.” TH
Reference
- Flanders SA, Kaufman SR, Saint S. Hospitalists as emerging leaders in patient safety: targeting a few to affect many. J Patient Safety. 2005;1(2):78-82.