User login
Newer antihyperglycemic drugs have distinctive CV, kidney benefits
The two newer classes of antihyperglycemic drugs that lower cardiovascular risk have different effects on specific cardiovascular and kidney disease outcomes in patients with type 2 diabetes, results of a meta-analysis suggest. Sodium-glucose contransporter-2 (SGLT2) inhibitors significantly reduced hospitalization from heart failure, whereas glucagon-like peptide-1 receptor agonists (GLP-1 RAs) did not, according to the reported results.
The GLP-1–RA class reduced risk of kidney disease progression, largely driven by a reduction in macroalbuminuria, according to the authors, whereas only the SGLT2 inhibitors reduced adverse kidney disease outcomes in a composite excluding that biomarker.
“The prevention of heart failure and progression of kidney disease by SGLT2 [inhibitors] should be considered in the decision-making process when treating patients with type 2 diabetes,” study senior author Marc S. Sabatine, MD, MPH, of Brigham and Women’s Hospital, Boston, and his coauthors wrote in a report on the study appearing in Circulation.
Both GLP-1 RAs and SGLT2 inhibitors significantly reduced major adverse cardiovascular events (MACE) and, as shown in other recent findings, their benefits were confined to patients with established atherosclerotic cardiovascular disease, Dr. Sabatine and his colleagues wrote.
The systematic review and meta-analysis of eight cardiovascular outcomes trials included 77,242 patients, of whom about 56% participated in GLP-1–RA studies and 44% in SGLT2-inhibitor trials. Just under three-quarters of the patients had established atherosclerotic cardiovascular disease, while the remainder had multiple risk factors for it.
Relative risk of hospitalization for heart failure was reduced by 31% with SGLT2 inhibitors, but it was not significantly reduced by GLP-1 RAs, the authors noted.
Risk of kidney disease progression was reduced by 38% with SGLT2 inhibitors and by 18% with GLP-1 RAs when the researchers used a broad composite endpoint including macroalbuminuria, estimated glomerular filtration rate (eGFR), end-stage kidney disease, and death due to renal causes.
By contrast, SGLT2 inhibitors reduced by 45% the relative risk of a narrower kidney outcome that excluded macroalbuminuria, whereas GLP-1 RAs had only a nonsignificant effect on the risk of doubling serum creatinine. That suggests the relative risk reduction of the kidney composite with GLP-1 RAs was driven mainly by a reduction in macroalbuminuria, the authors wrote.
Although albuminuria is an established biomarker for kidney and cardiovascular disease, it is a surrogate marker and can even be absent in patients with reduced eGFR, they said.
“Reduction in eGFR has emerged as a more meaningful endpoint of greater importance and is used in ongoing diabetes trials for kidney outcomes,” the authors said in a discussion of their results.
Relative risk of the composite MACE endpoint, including myocardial infarction, stroke, and cardiovascular death, was reduced by 12% for GLP-1 RAs and by 11% for SGLT2 [inhibitors], according to results of the analysis. However, the benefit was confined to patients with established cardiovascular disease, who had a 14% reduction of risk, compared with no treatment effect in patients who had multiple risk factors only.
Looking at individual MACE components, investigators found that both drug classes significantly reduced relative risk of myocardial infarction and of cardiovascular death, whereas only GLP-1 RAs significantly reduced relative risk of stroke.
Study authors provided disclosures related to AstraZeneca, Amgen, Daiichi-Sankyo, Eisai, GlaxoSmithKline, Intarcia, Janssen Research and Development, and Medimmune, among others.
SOURCE: Zelniker TA et al. Circulation. 2019 Feb 21. doi: 10.1161/CIRCULATIONAHA.118.038868.
The two newer classes of antihyperglycemic drugs that lower cardiovascular risk have different effects on specific cardiovascular and kidney disease outcomes in patients with type 2 diabetes, results of a meta-analysis suggest. Sodium-glucose contransporter-2 (SGLT2) inhibitors significantly reduced hospitalization from heart failure, whereas glucagon-like peptide-1 receptor agonists (GLP-1 RAs) did not, according to the reported results.
The GLP-1–RA class reduced risk of kidney disease progression, largely driven by a reduction in macroalbuminuria, according to the authors, whereas only the SGLT2 inhibitors reduced adverse kidney disease outcomes in a composite excluding that biomarker.
“The prevention of heart failure and progression of kidney disease by SGLT2 [inhibitors] should be considered in the decision-making process when treating patients with type 2 diabetes,” study senior author Marc S. Sabatine, MD, MPH, of Brigham and Women’s Hospital, Boston, and his coauthors wrote in a report on the study appearing in Circulation.
Both GLP-1 RAs and SGLT2 inhibitors significantly reduced major adverse cardiovascular events (MACE) and, as shown in other recent findings, their benefits were confined to patients with established atherosclerotic cardiovascular disease, Dr. Sabatine and his colleagues wrote.
The systematic review and meta-analysis of eight cardiovascular outcomes trials included 77,242 patients, of whom about 56% participated in GLP-1–RA studies and 44% in SGLT2-inhibitor trials. Just under three-quarters of the patients had established atherosclerotic cardiovascular disease, while the remainder had multiple risk factors for it.
Relative risk of hospitalization for heart failure was reduced by 31% with SGLT2 inhibitors, but it was not significantly reduced by GLP-1 RAs, the authors noted.
Risk of kidney disease progression was reduced by 38% with SGLT2 inhibitors and by 18% with GLP-1 RAs when the researchers used a broad composite endpoint including macroalbuminuria, estimated glomerular filtration rate (eGFR), end-stage kidney disease, and death due to renal causes.
By contrast, SGLT2 inhibitors reduced by 45% the relative risk of a narrower kidney outcome that excluded macroalbuminuria, whereas GLP-1 RAs had only a nonsignificant effect on the risk of doubling serum creatinine. That suggests the relative risk reduction of the kidney composite with GLP-1 RAs was driven mainly by a reduction in macroalbuminuria, the authors wrote.
Although albuminuria is an established biomarker for kidney and cardiovascular disease, it is a surrogate marker and can even be absent in patients with reduced eGFR, they said.
“Reduction in eGFR has emerged as a more meaningful endpoint of greater importance and is used in ongoing diabetes trials for kidney outcomes,” the authors said in a discussion of their results.
Relative risk of the composite MACE endpoint, including myocardial infarction, stroke, and cardiovascular death, was reduced by 12% for GLP-1 RAs and by 11% for SGLT2 [inhibitors], according to results of the analysis. However, the benefit was confined to patients with established cardiovascular disease, who had a 14% reduction of risk, compared with no treatment effect in patients who had multiple risk factors only.
Looking at individual MACE components, investigators found that both drug classes significantly reduced relative risk of myocardial infarction and of cardiovascular death, whereas only GLP-1 RAs significantly reduced relative risk of stroke.
Study authors provided disclosures related to AstraZeneca, Amgen, Daiichi-Sankyo, Eisai, GlaxoSmithKline, Intarcia, Janssen Research and Development, and Medimmune, among others.
SOURCE: Zelniker TA et al. Circulation. 2019 Feb 21. doi: 10.1161/CIRCULATIONAHA.118.038868.
The two newer classes of antihyperglycemic drugs that lower cardiovascular risk have different effects on specific cardiovascular and kidney disease outcomes in patients with type 2 diabetes, results of a meta-analysis suggest. Sodium-glucose contransporter-2 (SGLT2) inhibitors significantly reduced hospitalization from heart failure, whereas glucagon-like peptide-1 receptor agonists (GLP-1 RAs) did not, according to the reported results.
The GLP-1–RA class reduced risk of kidney disease progression, largely driven by a reduction in macroalbuminuria, according to the authors, whereas only the SGLT2 inhibitors reduced adverse kidney disease outcomes in a composite excluding that biomarker.
“The prevention of heart failure and progression of kidney disease by SGLT2 [inhibitors] should be considered in the decision-making process when treating patients with type 2 diabetes,” study senior author Marc S. Sabatine, MD, MPH, of Brigham and Women’s Hospital, Boston, and his coauthors wrote in a report on the study appearing in Circulation.
Both GLP-1 RAs and SGLT2 inhibitors significantly reduced major adverse cardiovascular events (MACE) and, as shown in other recent findings, their benefits were confined to patients with established atherosclerotic cardiovascular disease, Dr. Sabatine and his colleagues wrote.
The systematic review and meta-analysis of eight cardiovascular outcomes trials included 77,242 patients, of whom about 56% participated in GLP-1–RA studies and 44% in SGLT2-inhibitor trials. Just under three-quarters of the patients had established atherosclerotic cardiovascular disease, while the remainder had multiple risk factors for it.
Relative risk of hospitalization for heart failure was reduced by 31% with SGLT2 inhibitors, but it was not significantly reduced by GLP-1 RAs, the authors noted.
Risk of kidney disease progression was reduced by 38% with SGLT2 inhibitors and by 18% with GLP-1 RAs when the researchers used a broad composite endpoint including macroalbuminuria, estimated glomerular filtration rate (eGFR), end-stage kidney disease, and death due to renal causes.
By contrast, SGLT2 inhibitors reduced by 45% the relative risk of a narrower kidney outcome that excluded macroalbuminuria, whereas GLP-1 RAs had only a nonsignificant effect on the risk of doubling serum creatinine. That suggests the relative risk reduction of the kidney composite with GLP-1 RAs was driven mainly by a reduction in macroalbuminuria, the authors wrote.
Although albuminuria is an established biomarker for kidney and cardiovascular disease, it is a surrogate marker and can even be absent in patients with reduced eGFR, they said.
“Reduction in eGFR has emerged as a more meaningful endpoint of greater importance and is used in ongoing diabetes trials for kidney outcomes,” the authors said in a discussion of their results.
Relative risk of the composite MACE endpoint, including myocardial infarction, stroke, and cardiovascular death, was reduced by 12% for GLP-1 RAs and by 11% for SGLT2 [inhibitors], according to results of the analysis. However, the benefit was confined to patients with established cardiovascular disease, who had a 14% reduction of risk, compared with no treatment effect in patients who had multiple risk factors only.
Looking at individual MACE components, investigators found that both drug classes significantly reduced relative risk of myocardial infarction and of cardiovascular death, whereas only GLP-1 RAs significantly reduced relative risk of stroke.
Study authors provided disclosures related to AstraZeneca, Amgen, Daiichi-Sankyo, Eisai, GlaxoSmithKline, Intarcia, Janssen Research and Development, and Medimmune, among others.
SOURCE: Zelniker TA et al. Circulation. 2019 Feb 21. doi: 10.1161/CIRCULATIONAHA.118.038868.
FROM CIRCULATION
‘Trigger zone’ resection ups seizure-free odds in temporal lobe epilepsy
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
Resection of a brain area implicated in seizure modulation improves the odds of being seizure free in patients with temporal lobe epilepsy, according to results of a recent multicenter analysis.
Patients with long-term postoperative freedom from seizures had a larger proportion of the piriform cortex resected versus patients who were not seizure free. Removing at least half the piriform cortex was associated with a 1500% increase in odds of seizure freedom, first author Marian Galovic, MD, of the department of clinical and experimental epilepsy at the University College London’s Queen Square Institute of Neurology and his colleagues reported in JAMA Neurology.
“If confirmed in prospective interventional trials, these findings will have practical implications for guiding neurosurgeons about the extent of the surgical resection,” Dr. Galovic and his coinvestigators wrote.
The area tempestas in the piriform cortex has been identified as an epileptic trigger zone in animal studies, but to date, evidence of a human epileptic trigger zone in this area remain limited, according to the investigators.
To evaluate the impact of resection in this area, Dr. Galovic and his colleagues evaluated 107 patients with temporal lobe epilepsy from an ongoing, single-center, prospective study, and validated their findings with 31 patients from two other independent cohorts.
Of the 107 patients in the main cohort, 46% were completely seizure free for a median of 5 years after epilepsy surgery, with results of voxel-based morphometry showing that those patients had a more pronounced loss of gray matter in the ipsilateral piriform, compared with non–seizure-free patients.
The seizure-free patients had a median of 83% of the piriform cortex resected, compared with 52% for the non–seizure-free patients (P less than .001), results of a volumetric analysis confirmed.
Anxiety or psychosis outcomes were not influenced by the extent of piriform cortex resection, the investigators wrote, adding that poor verbal memory outcome was linked to the extent of resection of other brain regions, but not the piriform cortex.
The investigators confirmed these findings in the 31 patients of the validation cohort, with significant associations between extent of piriform cortex resection and postsurgical outcomes.
Resecting at least half of the region increased odds of being seizure free by a factor of 16 (95% CI, 5-47; P less than .001), Dr. Galovic and his colleagues added.
“Our results provide evidence suggesting that the human piriform cortex has a role in the generation of seizures that involve the temporal lobe,” they wrote in a discussion of their results.
The findings, if confirmed, could have implications not only for surgical practice, they wrote, but also for the understanding of the mechanisms underlying epileptic networks, which could lead to new drug and nondrug interventions to mitigate seizure activity.
Dr. Galovic reported receiving a grant from the Medical Research Council. His coauthors reported disclosures with the Medical Research Council, Wellcome Trust, Medtronic, Neuropace, Nevro, Eisai, UCB, and Mallinckrodt, among other entities.
SOURCE: Galovic M et al. JAMA Neurol. 2019 Mar 11. doi: 10.1001/jamaneurol.2019.0204.
FROM JAMA NEUROLOGY
Distinct features found in young-onset CRC
Young-onset colorectal cancer (CRC) has distinct clinical and molecular features, compared with disease diagnosed later in life, according to investigators who conducted a review that included more than 36,000 patients.
investigators said. Conversely, those younger patients were less likely to have BRAF V600 mutations than were patients 50 years old and older, the investigators reported in the journal Cancer.
Very young patients were more likely to have signet ring histology and less likely to have adenomatous polyposis coli (APC) mutations, according to senior study author Jonathan M. Loree, MD, and his coinvestigators at The University of Texas MD Anderson Cancer Center, Houston.
“We need to appreciate that there are unique biologic subtypes within young patients that may affect how their cancers behave and may require a personalized approach to treatment,” Dr. Loree said in a press statement. “Going forward, special clinical consideration should be given to, and further scientific investigations should be performed for, both very young patients with colorectal cancer and those with predisposing medical conditions.”
The incidence of young-onset CRC has increased 1%-3% annually in recent years, Dr. Loree and colleagues wrote in their report.
Although smaller studies have characterized molecular features of CRC in younger patients, there has so far been no comprehensive molecular characterization of these patients, they added. Accordingly, the investigators conducted a retrospective analysis that included more than 36,000 patients in four different patient cohorts.
Patients under 50 years more likely had synchronous metastases (P = .009), more likely had primary tumors in the distal colon and rectum (P less than .0001), and were more likely to be MSI-high (P = .038), compared with their older counterparts, Dr. Loree and coauthors reported.
BRAF V600 mutations were infrequent in patients under 30 years of age, at a prevalence of 4% or less, increasing to a high of 13% in patients aged 70 years or older (P less than 0.001), investigators also reported.
Very young patients, or those aged 18-29 years, had a higher prevalence of signet ring histology, compared with the other age groups (P = .0003), and they had a nearly fivefold increased odds of signet ring histology compared with patients in the 30-49 year age range, investigators wrote.
There were also considerably fewer APC mutations in the patients younger than 30 years, compared with older patients in the young-onset CRC group, with an odds ratio of 0.56 (95% confidence interval, 0.35-0.90; P = .015).
Hispanic patients were significantly overrepresented in the under-30-years age group (P = .0015), according to the report.
For patients under 50 years who also had inflammatory bowel disease, odds of mucinous or signet ring histology were higher (OR, 5.54; 95% CI, 2.24-13.74; P = .0004), and odds of APC mutations were lower (OR, 0.24; 95% CI, 0.07-0.75; P = .019), compared with younger patients with no such predisposing conditions.
“These notable differences in very young patients with CRC and those with predisposing conditions highlight that early-onset CRC has unique subsets within the population of patients younger than 50 years,” Dr. Loree and coauthors concluded.
Support to investigators in the study came from the National Cancer Institute, National Institutes of Health, and the MD Anderson Colorectal Cancer Moon Shot Program. One coinvestigator reported disclosures related to Roche, Genentech, EMD Serono, Merck, Karyopharm, Amal, Navire, Symphogen, Holystone, Biocartis, Amgen, and Novartis.
SOURCE: Willauer AN et al. Cancer. 2019 Mar 11. doi: 10.1002/cncr.31994
Young-onset colorectal cancer (CRC) has distinct clinical and molecular features, compared with disease diagnosed later in life, according to investigators who conducted a review that included more than 36,000 patients.
investigators said. Conversely, those younger patients were less likely to have BRAF V600 mutations than were patients 50 years old and older, the investigators reported in the journal Cancer.
Very young patients were more likely to have signet ring histology and less likely to have adenomatous polyposis coli (APC) mutations, according to senior study author Jonathan M. Loree, MD, and his coinvestigators at The University of Texas MD Anderson Cancer Center, Houston.
“We need to appreciate that there are unique biologic subtypes within young patients that may affect how their cancers behave and may require a personalized approach to treatment,” Dr. Loree said in a press statement. “Going forward, special clinical consideration should be given to, and further scientific investigations should be performed for, both very young patients with colorectal cancer and those with predisposing medical conditions.”
The incidence of young-onset CRC has increased 1%-3% annually in recent years, Dr. Loree and colleagues wrote in their report.
Although smaller studies have characterized molecular features of CRC in younger patients, there has so far been no comprehensive molecular characterization of these patients, they added. Accordingly, the investigators conducted a retrospective analysis that included more than 36,000 patients in four different patient cohorts.
Patients under 50 years more likely had synchronous metastases (P = .009), more likely had primary tumors in the distal colon and rectum (P less than .0001), and were more likely to be MSI-high (P = .038), compared with their older counterparts, Dr. Loree and coauthors reported.
BRAF V600 mutations were infrequent in patients under 30 years of age, at a prevalence of 4% or less, increasing to a high of 13% in patients aged 70 years or older (P less than 0.001), investigators also reported.
Very young patients, or those aged 18-29 years, had a higher prevalence of signet ring histology, compared with the other age groups (P = .0003), and they had a nearly fivefold increased odds of signet ring histology compared with patients in the 30-49 year age range, investigators wrote.
There were also considerably fewer APC mutations in the patients younger than 30 years, compared with older patients in the young-onset CRC group, with an odds ratio of 0.56 (95% confidence interval, 0.35-0.90; P = .015).
Hispanic patients were significantly overrepresented in the under-30-years age group (P = .0015), according to the report.
For patients under 50 years who also had inflammatory bowel disease, odds of mucinous or signet ring histology were higher (OR, 5.54; 95% CI, 2.24-13.74; P = .0004), and odds of APC mutations were lower (OR, 0.24; 95% CI, 0.07-0.75; P = .019), compared with younger patients with no such predisposing conditions.
“These notable differences in very young patients with CRC and those with predisposing conditions highlight that early-onset CRC has unique subsets within the population of patients younger than 50 years,” Dr. Loree and coauthors concluded.
Support to investigators in the study came from the National Cancer Institute, National Institutes of Health, and the MD Anderson Colorectal Cancer Moon Shot Program. One coinvestigator reported disclosures related to Roche, Genentech, EMD Serono, Merck, Karyopharm, Amal, Navire, Symphogen, Holystone, Biocartis, Amgen, and Novartis.
SOURCE: Willauer AN et al. Cancer. 2019 Mar 11. doi: 10.1002/cncr.31994
Young-onset colorectal cancer (CRC) has distinct clinical and molecular features, compared with disease diagnosed later in life, according to investigators who conducted a review that included more than 36,000 patients.
investigators said. Conversely, those younger patients were less likely to have BRAF V600 mutations than were patients 50 years old and older, the investigators reported in the journal Cancer.
Very young patients were more likely to have signet ring histology and less likely to have adenomatous polyposis coli (APC) mutations, according to senior study author Jonathan M. Loree, MD, and his coinvestigators at The University of Texas MD Anderson Cancer Center, Houston.
“We need to appreciate that there are unique biologic subtypes within young patients that may affect how their cancers behave and may require a personalized approach to treatment,” Dr. Loree said in a press statement. “Going forward, special clinical consideration should be given to, and further scientific investigations should be performed for, both very young patients with colorectal cancer and those with predisposing medical conditions.”
The incidence of young-onset CRC has increased 1%-3% annually in recent years, Dr. Loree and colleagues wrote in their report.
Although smaller studies have characterized molecular features of CRC in younger patients, there has so far been no comprehensive molecular characterization of these patients, they added. Accordingly, the investigators conducted a retrospective analysis that included more than 36,000 patients in four different patient cohorts.
Patients under 50 years more likely had synchronous metastases (P = .009), more likely had primary tumors in the distal colon and rectum (P less than .0001), and were more likely to be MSI-high (P = .038), compared with their older counterparts, Dr. Loree and coauthors reported.
BRAF V600 mutations were infrequent in patients under 30 years of age, at a prevalence of 4% or less, increasing to a high of 13% in patients aged 70 years or older (P less than 0.001), investigators also reported.
Very young patients, or those aged 18-29 years, had a higher prevalence of signet ring histology, compared with the other age groups (P = .0003), and they had a nearly fivefold increased odds of signet ring histology compared with patients in the 30-49 year age range, investigators wrote.
There were also considerably fewer APC mutations in the patients younger than 30 years, compared with older patients in the young-onset CRC group, with an odds ratio of 0.56 (95% confidence interval, 0.35-0.90; P = .015).
Hispanic patients were significantly overrepresented in the under-30-years age group (P = .0015), according to the report.
For patients under 50 years who also had inflammatory bowel disease, odds of mucinous or signet ring histology were higher (OR, 5.54; 95% CI, 2.24-13.74; P = .0004), and odds of APC mutations were lower (OR, 0.24; 95% CI, 0.07-0.75; P = .019), compared with younger patients with no such predisposing conditions.
“These notable differences in very young patients with CRC and those with predisposing conditions highlight that early-onset CRC has unique subsets within the population of patients younger than 50 years,” Dr. Loree and coauthors concluded.
Support to investigators in the study came from the National Cancer Institute, National Institutes of Health, and the MD Anderson Colorectal Cancer Moon Shot Program. One coinvestigator reported disclosures related to Roche, Genentech, EMD Serono, Merck, Karyopharm, Amal, Navire, Symphogen, Holystone, Biocartis, Amgen, and Novartis.
SOURCE: Willauer AN et al. Cancer. 2019 Mar 11. doi: 10.1002/cncr.31994
FROM CANCER
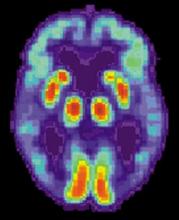
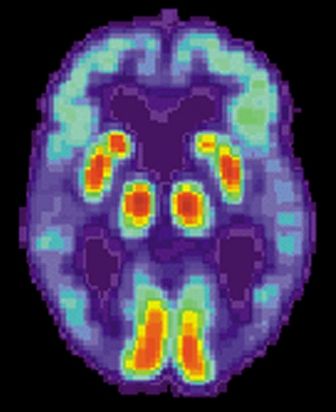
Blood-based signature helps predict status of early AD indicator
A recently developed blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator with high accuracy, investigators are reporting.
By analyzing as few as four proteins, the machine learning-derived test can predict the status of cerebrospinal fluid (CSF) amyloid beta1-42 (Abeta1-42), according to Noel G. Faux, PHD, of IBM Australia and the University of Melbourne, and co-investigators.
While shifts in Abeta1-42 may signal the presence of disease long before significant cognitive decline is clinically apparent, collection of CSF is highly invasive and expensive, Faux and investigators said in their report.
By contrast, blood biomarkers could prove to be a useful alternative not only to invasive lumbar punctures, they said, but also to the positron emission tomography (PET) evaluation of Abeta1-42, which is expensive and limited in some regions.
“In conjunction with biomarkers for neocortical amyloid burden, the CSF Abeta1-42biomarkers presented in this work may help yield a cheap, non-invasive tool for both improving clinical trials targeting amyloid and population screening,” Dr. Faux and co-authors said in Scientific Reports.
Dr. Faux and colleagues used a Random Forest approach to build models for CSF Abeta1-42 using blood biomarkers and other variables.
They found that a model incorporating age, APOEe4 carrier status, and a number of plasma protein levels predicted Abeta1-42 normal/abnormalstatus with an AUC, sensitivity and specificity of 0.84, 0.78 and 0.73 respectively.
In a model they said was more suitable for clinical application, they narrowed down the variables to 4 plasma analytes and APOEe4 carrier status, which had an AUC, sensitivity, and specificity of 0.81, 0.81 and 0.64 respectively.
They validated the models on a cohort of individuals in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a large, longitudinal, multicenter study.
Patients with mild cognitive impairment with predicted abnormal CSF Abeta1-42 levels indeed did transition to a diagnosis of Alzheimer’s disease more quickly than those with predicted normal levels, according to investigators.
That helps provide “strong evidence” that the blood-based model is generalizable, robust, and could help stratify patients based on risk of progressing to Alzheimer’s disease, they said in their report.
Dr. Faux and colleagues declared no conflicts of interest related to the research.
SOURCE: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
A recently developed blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator with high accuracy, investigators are reporting.
By analyzing as few as four proteins, the machine learning-derived test can predict the status of cerebrospinal fluid (CSF) amyloid beta1-42 (Abeta1-42), according to Noel G. Faux, PHD, of IBM Australia and the University of Melbourne, and co-investigators.
While shifts in Abeta1-42 may signal the presence of disease long before significant cognitive decline is clinically apparent, collection of CSF is highly invasive and expensive, Faux and investigators said in their report.
By contrast, blood biomarkers could prove to be a useful alternative not only to invasive lumbar punctures, they said, but also to the positron emission tomography (PET) evaluation of Abeta1-42, which is expensive and limited in some regions.
“In conjunction with biomarkers for neocortical amyloid burden, the CSF Abeta1-42biomarkers presented in this work may help yield a cheap, non-invasive tool for both improving clinical trials targeting amyloid and population screening,” Dr. Faux and co-authors said in Scientific Reports.
Dr. Faux and colleagues used a Random Forest approach to build models for CSF Abeta1-42 using blood biomarkers and other variables.
They found that a model incorporating age, APOEe4 carrier status, and a number of plasma protein levels predicted Abeta1-42 normal/abnormalstatus with an AUC, sensitivity and specificity of 0.84, 0.78 and 0.73 respectively.
In a model they said was more suitable for clinical application, they narrowed down the variables to 4 plasma analytes and APOEe4 carrier status, which had an AUC, sensitivity, and specificity of 0.81, 0.81 and 0.64 respectively.
They validated the models on a cohort of individuals in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a large, longitudinal, multicenter study.
Patients with mild cognitive impairment with predicted abnormal CSF Abeta1-42 levels indeed did transition to a diagnosis of Alzheimer’s disease more quickly than those with predicted normal levels, according to investigators.
That helps provide “strong evidence” that the blood-based model is generalizable, robust, and could help stratify patients based on risk of progressing to Alzheimer’s disease, they said in their report.
Dr. Faux and colleagues declared no conflicts of interest related to the research.
SOURCE: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
A recently developed blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator with high accuracy, investigators are reporting.
By analyzing as few as four proteins, the machine learning-derived test can predict the status of cerebrospinal fluid (CSF) amyloid beta1-42 (Abeta1-42), according to Noel G. Faux, PHD, of IBM Australia and the University of Melbourne, and co-investigators.
While shifts in Abeta1-42 may signal the presence of disease long before significant cognitive decline is clinically apparent, collection of CSF is highly invasive and expensive, Faux and investigators said in their report.
By contrast, blood biomarkers could prove to be a useful alternative not only to invasive lumbar punctures, they said, but also to the positron emission tomography (PET) evaluation of Abeta1-42, which is expensive and limited in some regions.
“In conjunction with biomarkers for neocortical amyloid burden, the CSF Abeta1-42biomarkers presented in this work may help yield a cheap, non-invasive tool for both improving clinical trials targeting amyloid and population screening,” Dr. Faux and co-authors said in Scientific Reports.
Dr. Faux and colleagues used a Random Forest approach to build models for CSF Abeta1-42 using blood biomarkers and other variables.
They found that a model incorporating age, APOEe4 carrier status, and a number of plasma protein levels predicted Abeta1-42 normal/abnormalstatus with an AUC, sensitivity and specificity of 0.84, 0.78 and 0.73 respectively.
In a model they said was more suitable for clinical application, they narrowed down the variables to 4 plasma analytes and APOEe4 carrier status, which had an AUC, sensitivity, and specificity of 0.81, 0.81 and 0.64 respectively.
They validated the models on a cohort of individuals in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), a large, longitudinal, multicenter study.
Patients with mild cognitive impairment with predicted abnormal CSF Abeta1-42 levels indeed did transition to a diagnosis of Alzheimer’s disease more quickly than those with predicted normal levels, according to investigators.
That helps provide “strong evidence” that the blood-based model is generalizable, robust, and could help stratify patients based on risk of progressing to Alzheimer’s disease, they said in their report.
Dr. Faux and colleagues declared no conflicts of interest related to the research.
SOURCE: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
FROM SCIENTIFIC REPORTS
Key clinical point: A blood-based signature can help predict the status of an early Alzheimer’s disease risk indicator.
Major finding:
Study details: Machine learning analysis of blood biomarkers and other variables in a validation cohort of 198 individuals.
Disclosures: The study authors declared no conflicts of interest.
Source: Goudey B, et al. Sci Rep. 2019 Mar 10. doi: 10.1101/190207v3.
Engraftment achieved after conditioning without radiation, alkylating agents
HOUSTON – Use of an alemtuzumab/fludarabine conditioning regimen – without any radiation or alkylating agents – was effective in patients with a systemic regenerative disease who experienced myeloid failure after allogeneic transplantation, according to an investigator.
Of the 20 patients with dyskeratosis congenita who received the regimen, 19 achieved primary engraftment within 42 days of transplant, according to Suneet Agarwal, MD, PhD, of Dana-Farber/Boston Children’s Cancer & Blood Disorders Center and Harvard Medical School, Boston.
However, these findings may have broader implications beyond this rare disease, as this is the first reported series of patients undergoing allogeneic bone marrow transplant to achieve durable myeloid engraftment without receiving alkylating agents or radiation, Dr. Agarwal said at the Transplantation & Cellular Therapy Meetings.
In a late-breaking clinical trial presentation of the results, Dr. Agarwal noted that patients in this study all had telomere disease, defined by clinical syndrome, gene mutation, or short lymphocyte telomere length. That’s because the investigators hypothesized that telomere defects would result in a “replicative disadvantage” in hematopoietic and immune cells, which would favor engraftment.
Dyskeratosis congenita is a prototypic telomere biology disorder caused by mutations that impair telomere maintenance, he said, adding that the disease has high rates of cancer, pulmonary disease, and hepatic disease.
While allogeneic transplants are curative in the disorder, outcomes after transplantation are typically poor, with high rates of bone marrow failure, he added. By eliminating radiation and alkylator exposure, the investigators hoped salvage bone marrow transplant would be more feasible, with lower risks of organ failure and secondary malignancy.
The 20 patients Dr. Agarwal reported on were aged from 30 months to 65 years. They all received alemtuzumab/fludarabine conditioning starting at day 9 before bone marrow graft, along with graft-versus-host disease (GVHD) prophylaxis through the pre- to posttransplant period. Two had matched siblings, while 18 had unrelated donors.
Of those 20 patients, 19 achieved primary engraftment at a median of 22 days after transplant, Dr. Agarwal reported. There was no acute GVHD and four cases of chronic GVHD that resolved with oral or topical steroids.
Of the 20 patients, 18 were alive at a median follow-up of 24 months, which compares favorably with historically reported cases, according to the investigator. There was one disease-related death and one treatment-related death caused by fungal infection at 3 months post transplant, he said.
These results suggest the radiation- and alkylator-free conditioning regimen is “effective,” Dr. Agarwal said, adding that exposure to those modalities is not required for myeloid engraftment in certain clinical settings.
The meeting is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Agarwal reported having no conflicts of interest.
SOURCE: Agarwal S et al. TCT 2019, Abstract LBA2.
HOUSTON – Use of an alemtuzumab/fludarabine conditioning regimen – without any radiation or alkylating agents – was effective in patients with a systemic regenerative disease who experienced myeloid failure after allogeneic transplantation, according to an investigator.
Of the 20 patients with dyskeratosis congenita who received the regimen, 19 achieved primary engraftment within 42 days of transplant, according to Suneet Agarwal, MD, PhD, of Dana-Farber/Boston Children’s Cancer & Blood Disorders Center and Harvard Medical School, Boston.
However, these findings may have broader implications beyond this rare disease, as this is the first reported series of patients undergoing allogeneic bone marrow transplant to achieve durable myeloid engraftment without receiving alkylating agents or radiation, Dr. Agarwal said at the Transplantation & Cellular Therapy Meetings.
In a late-breaking clinical trial presentation of the results, Dr. Agarwal noted that patients in this study all had telomere disease, defined by clinical syndrome, gene mutation, or short lymphocyte telomere length. That’s because the investigators hypothesized that telomere defects would result in a “replicative disadvantage” in hematopoietic and immune cells, which would favor engraftment.
Dyskeratosis congenita is a prototypic telomere biology disorder caused by mutations that impair telomere maintenance, he said, adding that the disease has high rates of cancer, pulmonary disease, and hepatic disease.
While allogeneic transplants are curative in the disorder, outcomes after transplantation are typically poor, with high rates of bone marrow failure, he added. By eliminating radiation and alkylator exposure, the investigators hoped salvage bone marrow transplant would be more feasible, with lower risks of organ failure and secondary malignancy.
The 20 patients Dr. Agarwal reported on were aged from 30 months to 65 years. They all received alemtuzumab/fludarabine conditioning starting at day 9 before bone marrow graft, along with graft-versus-host disease (GVHD) prophylaxis through the pre- to posttransplant period. Two had matched siblings, while 18 had unrelated donors.
Of those 20 patients, 19 achieved primary engraftment at a median of 22 days after transplant, Dr. Agarwal reported. There was no acute GVHD and four cases of chronic GVHD that resolved with oral or topical steroids.
Of the 20 patients, 18 were alive at a median follow-up of 24 months, which compares favorably with historically reported cases, according to the investigator. There was one disease-related death and one treatment-related death caused by fungal infection at 3 months post transplant, he said.
These results suggest the radiation- and alkylator-free conditioning regimen is “effective,” Dr. Agarwal said, adding that exposure to those modalities is not required for myeloid engraftment in certain clinical settings.
The meeting is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Agarwal reported having no conflicts of interest.
SOURCE: Agarwal S et al. TCT 2019, Abstract LBA2.
HOUSTON – Use of an alemtuzumab/fludarabine conditioning regimen – without any radiation or alkylating agents – was effective in patients with a systemic regenerative disease who experienced myeloid failure after allogeneic transplantation, according to an investigator.
Of the 20 patients with dyskeratosis congenita who received the regimen, 19 achieved primary engraftment within 42 days of transplant, according to Suneet Agarwal, MD, PhD, of Dana-Farber/Boston Children’s Cancer & Blood Disorders Center and Harvard Medical School, Boston.
However, these findings may have broader implications beyond this rare disease, as this is the first reported series of patients undergoing allogeneic bone marrow transplant to achieve durable myeloid engraftment without receiving alkylating agents or radiation, Dr. Agarwal said at the Transplantation & Cellular Therapy Meetings.
In a late-breaking clinical trial presentation of the results, Dr. Agarwal noted that patients in this study all had telomere disease, defined by clinical syndrome, gene mutation, or short lymphocyte telomere length. That’s because the investigators hypothesized that telomere defects would result in a “replicative disadvantage” in hematopoietic and immune cells, which would favor engraftment.
Dyskeratosis congenita is a prototypic telomere biology disorder caused by mutations that impair telomere maintenance, he said, adding that the disease has high rates of cancer, pulmonary disease, and hepatic disease.
While allogeneic transplants are curative in the disorder, outcomes after transplantation are typically poor, with high rates of bone marrow failure, he added. By eliminating radiation and alkylator exposure, the investigators hoped salvage bone marrow transplant would be more feasible, with lower risks of organ failure and secondary malignancy.
The 20 patients Dr. Agarwal reported on were aged from 30 months to 65 years. They all received alemtuzumab/fludarabine conditioning starting at day 9 before bone marrow graft, along with graft-versus-host disease (GVHD) prophylaxis through the pre- to posttransplant period. Two had matched siblings, while 18 had unrelated donors.
Of those 20 patients, 19 achieved primary engraftment at a median of 22 days after transplant, Dr. Agarwal reported. There was no acute GVHD and four cases of chronic GVHD that resolved with oral or topical steroids.
Of the 20 patients, 18 were alive at a median follow-up of 24 months, which compares favorably with historically reported cases, according to the investigator. There was one disease-related death and one treatment-related death caused by fungal infection at 3 months post transplant, he said.
These results suggest the radiation- and alkylator-free conditioning regimen is “effective,” Dr. Agarwal said, adding that exposure to those modalities is not required for myeloid engraftment in certain clinical settings.
The meeting is held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research. At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
Dr. Agarwal reported having no conflicts of interest.
SOURCE: Agarwal S et al. TCT 2019, Abstract LBA2.
REPORTING FROM TCT 2019
Lentiviral gene therapy appears effective in X-CGD
HOUSTON – , said Donald B. Kohn, MD, of the University of California, Los Angeles.
Seven of nine patients treated were “alive and well” at 12 months’ follow-up after receiving lentiviral vector transduced CD34+ cells, Dr. Kohn reported in a late-breaking clinical trial session at the Transplantation & Cellular Therapy Meetings.
Most patients were able to discontinue antibiotic prophylaxis for this disease, which is associated with severe, recurrent, and prolonged life-threatening infections, he said.
Results of the small study provide “proof of concept” for use of the gene therapy in the disease, though additional studies are needed to formally assess the clinical safety and efficacy of the approach, he said.
The estimated incidence of chronic granulomatous disease is 1 in 200,000 births in the United States, and the X-linked form is most common, occurring in about 60% of patients, Dr. Kohn told attendees of the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Most of these patients are treated with antibacterial or antifungal prophylaxis. While allogeneic hematopoietic stem cell transplantation is also an option, according to Dr. Kohn, the approach is limited by a lack of matched donors and graft-versus-host disease.
Dr. Kohn reported results for nine patients in the United States and the United Kingdom who were treated with the same G1XCGD lentiviral vector. The patients, who ranged in age from 2 to 27 years, underwent CD34+ cell mobilization or bone marrow isolation, transduction with the lentiviral vector, busulfan conditioning, and autologous transplantation.
All patients had confirmed X-linked chronic granulomatous disease, and had had at least one severe infection or inflammatory complication requiring hospitalization.
There were no infusion-related adverse events, and one serious adverse event, which was an inflammatory syndrome that resolved with steroids. Two patients died from complications unrelated to gene therapy, Dr. Kohn reported.
“The other patients are basically doing quite well,” he said.
Of the seven patients alive at the 12-month follow up, six were reported as “clinically well” and off antibiotic prophylaxis, according to Dr. Kohn, while the seventh patient was clinically well and receiving antimicrobial support.
Dr. Kohn is a scientific advisory board member for Orchard Therapeutics, which licensed the lentiviral gene therapy for X-CGD discussed in his presentation. He is also an inventor of intellectual property related to the therapy that UCLA has licensed to Orchard.
At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Kohn DB et al. TCT 2019, Abstract LBA1.
HOUSTON – , said Donald B. Kohn, MD, of the University of California, Los Angeles.
Seven of nine patients treated were “alive and well” at 12 months’ follow-up after receiving lentiviral vector transduced CD34+ cells, Dr. Kohn reported in a late-breaking clinical trial session at the Transplantation & Cellular Therapy Meetings.
Most patients were able to discontinue antibiotic prophylaxis for this disease, which is associated with severe, recurrent, and prolonged life-threatening infections, he said.
Results of the small study provide “proof of concept” for use of the gene therapy in the disease, though additional studies are needed to formally assess the clinical safety and efficacy of the approach, he said.
The estimated incidence of chronic granulomatous disease is 1 in 200,000 births in the United States, and the X-linked form is most common, occurring in about 60% of patients, Dr. Kohn told attendees of the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Most of these patients are treated with antibacterial or antifungal prophylaxis. While allogeneic hematopoietic stem cell transplantation is also an option, according to Dr. Kohn, the approach is limited by a lack of matched donors and graft-versus-host disease.
Dr. Kohn reported results for nine patients in the United States and the United Kingdom who were treated with the same G1XCGD lentiviral vector. The patients, who ranged in age from 2 to 27 years, underwent CD34+ cell mobilization or bone marrow isolation, transduction with the lentiviral vector, busulfan conditioning, and autologous transplantation.
All patients had confirmed X-linked chronic granulomatous disease, and had had at least one severe infection or inflammatory complication requiring hospitalization.
There were no infusion-related adverse events, and one serious adverse event, which was an inflammatory syndrome that resolved with steroids. Two patients died from complications unrelated to gene therapy, Dr. Kohn reported.
“The other patients are basically doing quite well,” he said.
Of the seven patients alive at the 12-month follow up, six were reported as “clinically well” and off antibiotic prophylaxis, according to Dr. Kohn, while the seventh patient was clinically well and receiving antimicrobial support.
Dr. Kohn is a scientific advisory board member for Orchard Therapeutics, which licensed the lentiviral gene therapy for X-CGD discussed in his presentation. He is also an inventor of intellectual property related to the therapy that UCLA has licensed to Orchard.
At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Kohn DB et al. TCT 2019, Abstract LBA1.
HOUSTON – , said Donald B. Kohn, MD, of the University of California, Los Angeles.
Seven of nine patients treated were “alive and well” at 12 months’ follow-up after receiving lentiviral vector transduced CD34+ cells, Dr. Kohn reported in a late-breaking clinical trial session at the Transplantation & Cellular Therapy Meetings.
Most patients were able to discontinue antibiotic prophylaxis for this disease, which is associated with severe, recurrent, and prolonged life-threatening infections, he said.
Results of the small study provide “proof of concept” for use of the gene therapy in the disease, though additional studies are needed to formally assess the clinical safety and efficacy of the approach, he said.
The estimated incidence of chronic granulomatous disease is 1 in 200,000 births in the United States, and the X-linked form is most common, occurring in about 60% of patients, Dr. Kohn told attendees of the meeting held by the American Society for Blood and Marrow Transplantation and the Center for International Blood and Marrow Transplant Research.
Most of these patients are treated with antibacterial or antifungal prophylaxis. While allogeneic hematopoietic stem cell transplantation is also an option, according to Dr. Kohn, the approach is limited by a lack of matched donors and graft-versus-host disease.
Dr. Kohn reported results for nine patients in the United States and the United Kingdom who were treated with the same G1XCGD lentiviral vector. The patients, who ranged in age from 2 to 27 years, underwent CD34+ cell mobilization or bone marrow isolation, transduction with the lentiviral vector, busulfan conditioning, and autologous transplantation.
All patients had confirmed X-linked chronic granulomatous disease, and had had at least one severe infection or inflammatory complication requiring hospitalization.
There were no infusion-related adverse events, and one serious adverse event, which was an inflammatory syndrome that resolved with steroids. Two patients died from complications unrelated to gene therapy, Dr. Kohn reported.
“The other patients are basically doing quite well,” he said.
Of the seven patients alive at the 12-month follow up, six were reported as “clinically well” and off antibiotic prophylaxis, according to Dr. Kohn, while the seventh patient was clinically well and receiving antimicrobial support.
Dr. Kohn is a scientific advisory board member for Orchard Therapeutics, which licensed the lentiviral gene therapy for X-CGD discussed in his presentation. He is also an inventor of intellectual property related to the therapy that UCLA has licensed to Orchard.
At its meeting, the American Society for Blood and Marrow Transplantation announced a new name for the society: American Society for Transplantation and Cellular Therapy (ASTCT).
SOURCE: Kohn DB et al. TCT 2019, Abstract LBA1.
REPORTING FROM TCT 2019
Report: Cutting sodium consumption recommended
according to a report outlining the first-ever Dietary Reference Intakes (DRIs) recommendation intended to address chronic disease risk.
For individuals aged 14 years and older consuming sodium above that level, cutting back could reduce their risk for hypertension and other chronic diseases, according to the report from the National Academies of Sciences, Engineering, and Medicine.
That cutoff, referred to as a Chronic Disease Risk Reduction Intake (CDRR), represents an expansion of the DRIs model beyond the Recommended Dietary Allowance (RDA) and other measures of adequacy, and the Tolerable Upper Intake Level (UL), which is the maximum intake unlikely to result in adverse health effects, a report author said in a press conference.
“CDRR is a level now that will join all the rest of the alphabet soup and be a part of how we describe recommended dietary intakes,” said Virginia A. Stallings, MD, chair of the committee that reviewed the sodium and potassium DRIs. Most U.S. adults are already consuming sodium above the recommended CDRR, said Dr. Stallings, who is a professor of pediatrics at the University of Pennsylvania, Philadelphia, and the director of the Nutrition Center at Children’s Hospital of Philadelphia.
The recommendation to reduce sodium intakes to below 2,300 mg/day applies to both hypertensive and normotensive individuals, and it could be particularly beneficial in older adults, non-Hispanic blacks, and other groups at higher risk of cardiovascular disease, Dr. Stallings and her coauthors of the new report wrote. The DRIs established in 2005 for both sodium and potassium are also updated based on new methodology in this report
Lower sodium CDRRs were set for younger individuals. Children aged 1-3 years should cut back if sodium intake is above 1,200 mg/day, while the levels for children aged 4-8 years and 9-13 years were set at 1,500 and 1,800 mg/day, respectively, according to the report.
By contrast, authors of this report were unable to establish a CDRR level for potassium based on current evidence. However, that doesn’t rule out the possibility that changing potassium intake could be beneficial, they suggested, adding that the effects of potassium need to be further explored.
Sodium and potassium play important roles in maintaining physiologic homeostasis, and they have also been implicated in risk of cardiovascular disease, mainly through their effects on blood pressure, and other chronic diseases.
“The unique nature of potassium and sodium – that is, the coexistence of their essentiality with a relationship to adverse health effects, including chronic disease risk – necessitated a new approach to the review of intake recommendations for these nutrients within the [DRI] context,” the report reads. The report also affirms, and in some cases revises, levels of sodium and potassium assumed to be adequate in healthy individuals that had been established in 2005. The sodium Adequate Intake (AI) levels for individuals aged 14-50 years is unchanged at 1,500 mg daily, but that for individuals aged 51 years and older has been increased to the 1,500-mg level.
“As we examined the evidence and looked specifically at those age cuts, there was no evidence that older people needed less sodium,” Dr. Stallings said in the press conference.
Potassium AIs were decreased for most age groups. For adults, the new recommended potassium AIs are 3,400 mg/day in men and 2,600 mg/day in women, whereas the AI for potassium was 4,700 mg/day for all adults in the 2005 recommendations.
In 2005, much of the evidence used to establish the potassium AI values was based on research studies that included potassium supplementation, rather than simply potassium intake in the usual diet. “In our process, we did not use supplementation studies, but we used the intake of apparently healthy people,” Dr. Stallings said in the press conference.
Less than half of U.S. and Canadian adults have potassium intakes that meet or exceed the potassium AI, with intakes lowest among non-Hispanic blacks, Dr. Stallings said in the press conference.
Dietary potassium intake is related to fruit and vegetable consumption, which rarely meets the recommended servings per day, Dr. Stallings and her colleagues wrote in a preface to the National Academies report. Milk, white potatoes, and fruit are higher sources of dietary potassium, she said, while coffee is the leading source of potassium for Americans aged 51 years and older.
By contrast, most sodium in the modern diet comes from commercially prepared foods and beverages, instead of consumers adding salt at the time of cooking or eating, Dr. Stallings wrote.
“For the desired public health benefit of reduced sodium intake to be achieved, more attention must be paid by industry to reducing sodium in the food supply and by consumers who have the needed sodium content information and an understanding of how to make health-inspired food choices,” they wrote in the report.
The American Heart Association’s CEO, Nancy Brown, expressed her support for the new recommendation for sodium intake. The recommendation “aligns with what the American Heart Association and other prominent public health organizations have been saying for years: We must eat less salt,” she said.
“Our excessive sodium intake isn’t entirely driven by the salt shaker; it’s largely controlled by the food industry. More than 70 percent of sodium consumed is added to food before it reaches our plates. It is added in restaurants and during the manufacturing of processed and prepackaged foods,” she claimed. “We hope this report encourages the Food and Drug Administration to quickly release its voluntary sodium reduction targets for the food industry. School leaders should also take note and reject the recent U.S. Department of Agriculture decision to weaken sodium standards in school meals and continue their commitment to serve students healthier foods.”
The DRIs report on sodium and potassium was supported by contracts between the National Academy of Sciences and the Centers for Disease Control, Food and Drug Administration, Health Canada, National Institutes of Health, Public Health Agency of Canada, and the Department of Agriculture. Partial support also came from the National Academy of Sciences W. K. Kellogg Foundation Fund and the National Academy of Medicine.
SOURCE: National Academies of Sciences, Engineering, and Medicine. 2019. Dietary Reference Intakes for sodium and potassium. Washington: The National Academies Press. doi: 10.17226/25353.
according to a report outlining the first-ever Dietary Reference Intakes (DRIs) recommendation intended to address chronic disease risk.
For individuals aged 14 years and older consuming sodium above that level, cutting back could reduce their risk for hypertension and other chronic diseases, according to the report from the National Academies of Sciences, Engineering, and Medicine.
That cutoff, referred to as a Chronic Disease Risk Reduction Intake (CDRR), represents an expansion of the DRIs model beyond the Recommended Dietary Allowance (RDA) and other measures of adequacy, and the Tolerable Upper Intake Level (UL), which is the maximum intake unlikely to result in adverse health effects, a report author said in a press conference.
“CDRR is a level now that will join all the rest of the alphabet soup and be a part of how we describe recommended dietary intakes,” said Virginia A. Stallings, MD, chair of the committee that reviewed the sodium and potassium DRIs. Most U.S. adults are already consuming sodium above the recommended CDRR, said Dr. Stallings, who is a professor of pediatrics at the University of Pennsylvania, Philadelphia, and the director of the Nutrition Center at Children’s Hospital of Philadelphia.
The recommendation to reduce sodium intakes to below 2,300 mg/day applies to both hypertensive and normotensive individuals, and it could be particularly beneficial in older adults, non-Hispanic blacks, and other groups at higher risk of cardiovascular disease, Dr. Stallings and her coauthors of the new report wrote. The DRIs established in 2005 for both sodium and potassium are also updated based on new methodology in this report
Lower sodium CDRRs were set for younger individuals. Children aged 1-3 years should cut back if sodium intake is above 1,200 mg/day, while the levels for children aged 4-8 years and 9-13 years were set at 1,500 and 1,800 mg/day, respectively, according to the report.
By contrast, authors of this report were unable to establish a CDRR level for potassium based on current evidence. However, that doesn’t rule out the possibility that changing potassium intake could be beneficial, they suggested, adding that the effects of potassium need to be further explored.
Sodium and potassium play important roles in maintaining physiologic homeostasis, and they have also been implicated in risk of cardiovascular disease, mainly through their effects on blood pressure, and other chronic diseases.
“The unique nature of potassium and sodium – that is, the coexistence of their essentiality with a relationship to adverse health effects, including chronic disease risk – necessitated a new approach to the review of intake recommendations for these nutrients within the [DRI] context,” the report reads. The report also affirms, and in some cases revises, levels of sodium and potassium assumed to be adequate in healthy individuals that had been established in 2005. The sodium Adequate Intake (AI) levels for individuals aged 14-50 years is unchanged at 1,500 mg daily, but that for individuals aged 51 years and older has been increased to the 1,500-mg level.
“As we examined the evidence and looked specifically at those age cuts, there was no evidence that older people needed less sodium,” Dr. Stallings said in the press conference.
Potassium AIs were decreased for most age groups. For adults, the new recommended potassium AIs are 3,400 mg/day in men and 2,600 mg/day in women, whereas the AI for potassium was 4,700 mg/day for all adults in the 2005 recommendations.
In 2005, much of the evidence used to establish the potassium AI values was based on research studies that included potassium supplementation, rather than simply potassium intake in the usual diet. “In our process, we did not use supplementation studies, but we used the intake of apparently healthy people,” Dr. Stallings said in the press conference.
Less than half of U.S. and Canadian adults have potassium intakes that meet or exceed the potassium AI, with intakes lowest among non-Hispanic blacks, Dr. Stallings said in the press conference.
Dietary potassium intake is related to fruit and vegetable consumption, which rarely meets the recommended servings per day, Dr. Stallings and her colleagues wrote in a preface to the National Academies report. Milk, white potatoes, and fruit are higher sources of dietary potassium, she said, while coffee is the leading source of potassium for Americans aged 51 years and older.
By contrast, most sodium in the modern diet comes from commercially prepared foods and beverages, instead of consumers adding salt at the time of cooking or eating, Dr. Stallings wrote.
“For the desired public health benefit of reduced sodium intake to be achieved, more attention must be paid by industry to reducing sodium in the food supply and by consumers who have the needed sodium content information and an understanding of how to make health-inspired food choices,” they wrote in the report.
The American Heart Association’s CEO, Nancy Brown, expressed her support for the new recommendation for sodium intake. The recommendation “aligns with what the American Heart Association and other prominent public health organizations have been saying for years: We must eat less salt,” she said.
“Our excessive sodium intake isn’t entirely driven by the salt shaker; it’s largely controlled by the food industry. More than 70 percent of sodium consumed is added to food before it reaches our plates. It is added in restaurants and during the manufacturing of processed and prepackaged foods,” she claimed. “We hope this report encourages the Food and Drug Administration to quickly release its voluntary sodium reduction targets for the food industry. School leaders should also take note and reject the recent U.S. Department of Agriculture decision to weaken sodium standards in school meals and continue their commitment to serve students healthier foods.”
The DRIs report on sodium and potassium was supported by contracts between the National Academy of Sciences and the Centers for Disease Control, Food and Drug Administration, Health Canada, National Institutes of Health, Public Health Agency of Canada, and the Department of Agriculture. Partial support also came from the National Academy of Sciences W. K. Kellogg Foundation Fund and the National Academy of Medicine.
SOURCE: National Academies of Sciences, Engineering, and Medicine. 2019. Dietary Reference Intakes for sodium and potassium. Washington: The National Academies Press. doi: 10.17226/25353.
according to a report outlining the first-ever Dietary Reference Intakes (DRIs) recommendation intended to address chronic disease risk.
For individuals aged 14 years and older consuming sodium above that level, cutting back could reduce their risk for hypertension and other chronic diseases, according to the report from the National Academies of Sciences, Engineering, and Medicine.
That cutoff, referred to as a Chronic Disease Risk Reduction Intake (CDRR), represents an expansion of the DRIs model beyond the Recommended Dietary Allowance (RDA) and other measures of adequacy, and the Tolerable Upper Intake Level (UL), which is the maximum intake unlikely to result in adverse health effects, a report author said in a press conference.
“CDRR is a level now that will join all the rest of the alphabet soup and be a part of how we describe recommended dietary intakes,” said Virginia A. Stallings, MD, chair of the committee that reviewed the sodium and potassium DRIs. Most U.S. adults are already consuming sodium above the recommended CDRR, said Dr. Stallings, who is a professor of pediatrics at the University of Pennsylvania, Philadelphia, and the director of the Nutrition Center at Children’s Hospital of Philadelphia.
The recommendation to reduce sodium intakes to below 2,300 mg/day applies to both hypertensive and normotensive individuals, and it could be particularly beneficial in older adults, non-Hispanic blacks, and other groups at higher risk of cardiovascular disease, Dr. Stallings and her coauthors of the new report wrote. The DRIs established in 2005 for both sodium and potassium are also updated based on new methodology in this report
Lower sodium CDRRs were set for younger individuals. Children aged 1-3 years should cut back if sodium intake is above 1,200 mg/day, while the levels for children aged 4-8 years and 9-13 years were set at 1,500 and 1,800 mg/day, respectively, according to the report.
By contrast, authors of this report were unable to establish a CDRR level for potassium based on current evidence. However, that doesn’t rule out the possibility that changing potassium intake could be beneficial, they suggested, adding that the effects of potassium need to be further explored.
Sodium and potassium play important roles in maintaining physiologic homeostasis, and they have also been implicated in risk of cardiovascular disease, mainly through their effects on blood pressure, and other chronic diseases.
“The unique nature of potassium and sodium – that is, the coexistence of their essentiality with a relationship to adverse health effects, including chronic disease risk – necessitated a new approach to the review of intake recommendations for these nutrients within the [DRI] context,” the report reads. The report also affirms, and in some cases revises, levels of sodium and potassium assumed to be adequate in healthy individuals that had been established in 2005. The sodium Adequate Intake (AI) levels for individuals aged 14-50 years is unchanged at 1,500 mg daily, but that for individuals aged 51 years and older has been increased to the 1,500-mg level.
“As we examined the evidence and looked specifically at those age cuts, there was no evidence that older people needed less sodium,” Dr. Stallings said in the press conference.
Potassium AIs were decreased for most age groups. For adults, the new recommended potassium AIs are 3,400 mg/day in men and 2,600 mg/day in women, whereas the AI for potassium was 4,700 mg/day for all adults in the 2005 recommendations.
In 2005, much of the evidence used to establish the potassium AI values was based on research studies that included potassium supplementation, rather than simply potassium intake in the usual diet. “In our process, we did not use supplementation studies, but we used the intake of apparently healthy people,” Dr. Stallings said in the press conference.
Less than half of U.S. and Canadian adults have potassium intakes that meet or exceed the potassium AI, with intakes lowest among non-Hispanic blacks, Dr. Stallings said in the press conference.
Dietary potassium intake is related to fruit and vegetable consumption, which rarely meets the recommended servings per day, Dr. Stallings and her colleagues wrote in a preface to the National Academies report. Milk, white potatoes, and fruit are higher sources of dietary potassium, she said, while coffee is the leading source of potassium for Americans aged 51 years and older.
By contrast, most sodium in the modern diet comes from commercially prepared foods and beverages, instead of consumers adding salt at the time of cooking or eating, Dr. Stallings wrote.
“For the desired public health benefit of reduced sodium intake to be achieved, more attention must be paid by industry to reducing sodium in the food supply and by consumers who have the needed sodium content information and an understanding of how to make health-inspired food choices,” they wrote in the report.
The American Heart Association’s CEO, Nancy Brown, expressed her support for the new recommendation for sodium intake. The recommendation “aligns with what the American Heart Association and other prominent public health organizations have been saying for years: We must eat less salt,” she said.
“Our excessive sodium intake isn’t entirely driven by the salt shaker; it’s largely controlled by the food industry. More than 70 percent of sodium consumed is added to food before it reaches our plates. It is added in restaurants and during the manufacturing of processed and prepackaged foods,” she claimed. “We hope this report encourages the Food and Drug Administration to quickly release its voluntary sodium reduction targets for the food industry. School leaders should also take note and reject the recent U.S. Department of Agriculture decision to weaken sodium standards in school meals and continue their commitment to serve students healthier foods.”
The DRIs report on sodium and potassium was supported by contracts between the National Academy of Sciences and the Centers for Disease Control, Food and Drug Administration, Health Canada, National Institutes of Health, Public Health Agency of Canada, and the Department of Agriculture. Partial support also came from the National Academy of Sciences W. K. Kellogg Foundation Fund and the National Academy of Medicine.
SOURCE: National Academies of Sciences, Engineering, and Medicine. 2019. Dietary Reference Intakes for sodium and potassium. Washington: The National Academies Press. doi: 10.17226/25353.
No increased pregnancy loss risk for women conceiving soon after stillbirth
according to authors of a large, international observational study.
There was no significantly increased risk of stillbirth, preterm birth, or small-for-gestational-age birth in the next pregnancy for women who conceived in that 12-month time period, according to results of the study, which was based on birth records for nearly 14,500 women in Finland, Norway, and Australia.
“We hope that our findings can provide reassurance to women who wish to become pregnant or unexpectedly become pregnant shortly after a stillbirth,” study author Annette K. Regan, PhD, of Curtin University, Perth, Australia, said in a statement on the study, which appears in The Lancet.
Judette Marie Louis, MD, MPH, said that while data are conflicting on optimal interpregnancy interval following stillbirth, large population-based studies such as this one may provide an indication of the relative safety of an interval of 12 months or less. (She was not involved in this study.)
“This paper is good news for a lot of women,” Dr. Louis, associate professor of obstetrics and gynecology at the University of South Florida, Tampa, said in an interview. “After a stillbirth, it’s such a traumatic experience that some do want to move on, and these findings suggest that, yes, you don’t have to wait that long to have a successful pregnancy.”
These results are for women living in relatively high-income countries, so the findings might not apply to every population, she added. Dr. Louis was the first author of a recent interpregnancy care consensus statement by the American College of Obstetricians and Gynecologists and the Society of Maternal-Fetal Medicine, and was asked to comment on this study.
The World Health Organization recommends interpregnancy intervals of 2 years or more after live births and 6 months or more after miscarriage, but currently has no specific recommendations on the optimal interpregnancy interval after a stillbirth, according to Dr. Regan and her colleagues.
“Because length of gestation might affect nutrient concentrations and health status in women, it is plausible that the optimal interval after stillbirth is somewhere between the optimal interval after miscarriage and live birth,” they said in their report.
Researchers for two previous studies also have reported on the link between the interpregnancy interval after stillbirth and birth outcomes in the next pregnancy, but neither was specifically designed to evaluate that outcome, they added.
Dr. Regan and her coauthors used birth record data spanning several decades from three high-income countries to identify 14,452 women who had stillbirths. Of those, 63% conceived within the next 12 months, and for 37%, it was as early as 6 months.
Overall, 2% of the subsequent pregnancies ended in stillbirth, while 9% were small-for-gestational-age and 18% were preterm, according to the report.
In analyses adjusted for variables such as age, smoking, and education level, there was no association between short interpregnancy intervals and subsequent stillbirths, compared with longer intervals (24-59 months), with odds ratios of 1.09 for an interval shorter than 6 months and 0.90 for 6-11 months.
Likewise, there was no link between shorter intervals and subsequent small-for-gestational-age birth, with odds ratios of 0.66 for less than 6 months and 0.64 for 6-11 months, and no link between interval and subsequent preterm births, with odds ratios of 0.91 for both short-interval groups.
That data could be useful to health care providers who do postpartum counseling after stillbirths, and could potentially inform future recommendations on pregnancy spacing, Dr. Regan and her coauthors said.
“These results apply to a large proportion of women conceiving after a stillbirth,” they noted.
This study included countries with access to universal health care, with populations that are mostly white, so the results may not apply to low- or middle-income countries without universal health care or with significant ethnic minority populations, they added.
Dr. Regan and her colleagues declared no competing interests related to the study, which was funded the National Health and Medical Research Council of Australia, among other sources.
SOURCE: Regan AK et al. Lancet. 2019 Feb 28. doi: 10.1016/S0140-6736(18)32266-9.
The interval between pregnancy loss and the next conception may be less important than previously assumed, based on the results of this and other recent studies, according to Mark A Klebanoff, MD, MPH.
“Rather than adhering to hard and fast rules, clinical recommendations should consider a woman’s current health status, her current age in conjunction with her desires regarding child spacing and ultimate family size, and particularly following a loss, her emotional readiness to become pregnant again,” he said in a commentary accompanying the article by Regan et al.
However, these results are specific to high-income countries, and might not extrapolate to women in “less favorable situations” where poor access to quality medical and obstetric care, malnutrition, and untreated chronic conditions are more common, Dr. Klebanoff added.
Another limitation of the study, acknowledged by Regan and coauthors, is the relatively small number of stillbirths in subsequent pregnancies (228) despite this being the largest study of its kind to date.
“The fairly small number of women included in this report dictates that replication, probably using other large, linked, population-level databases, is required,” Dr. Klebanoff said in his commentary.
Dr. Klebanoff is with the Center for Perinatal Research, The Research Institute at Nationwide Children’s Hospital; and the departments of pediatrics and obstetrics and gynecology at the College of Medicine, and division of epidemiology at the College of Public Health, at The Ohio State University, all in Columbus. This is a summarization of his commentary (Lancet. 2019 Feb 28. doi: 10.1016/S0140-6736(18)32430-9 ). Dr. Klebanoff said he had a pending grant application to the National Institutes of Health to study the association between interpregnancy interval and birth outcomes, and had no other competing interests.
The interval between pregnancy loss and the next conception may be less important than previously assumed, based on the results of this and other recent studies, according to Mark A Klebanoff, MD, MPH.
“Rather than adhering to hard and fast rules, clinical recommendations should consider a woman’s current health status, her current age in conjunction with her desires regarding child spacing and ultimate family size, and particularly following a loss, her emotional readiness to become pregnant again,” he said in a commentary accompanying the article by Regan et al.
However, these results are specific to high-income countries, and might not extrapolate to women in “less favorable situations” where poor access to quality medical and obstetric care, malnutrition, and untreated chronic conditions are more common, Dr. Klebanoff added.
Another limitation of the study, acknowledged by Regan and coauthors, is the relatively small number of stillbirths in subsequent pregnancies (228) despite this being the largest study of its kind to date.
“The fairly small number of women included in this report dictates that replication, probably using other large, linked, population-level databases, is required,” Dr. Klebanoff said in his commentary.
Dr. Klebanoff is with the Center for Perinatal Research, The Research Institute at Nationwide Children’s Hospital; and the departments of pediatrics and obstetrics and gynecology at the College of Medicine, and division of epidemiology at the College of Public Health, at The Ohio State University, all in Columbus. This is a summarization of his commentary (Lancet. 2019 Feb 28. doi: 10.1016/S0140-6736(18)32430-9 ). Dr. Klebanoff said he had a pending grant application to the National Institutes of Health to study the association between interpregnancy interval and birth outcomes, and had no other competing interests.
The interval between pregnancy loss and the next conception may be less important than previously assumed, based on the results of this and other recent studies, according to Mark A Klebanoff, MD, MPH.
“Rather than adhering to hard and fast rules, clinical recommendations should consider a woman’s current health status, her current age in conjunction with her desires regarding child spacing and ultimate family size, and particularly following a loss, her emotional readiness to become pregnant again,” he said in a commentary accompanying the article by Regan et al.
However, these results are specific to high-income countries, and might not extrapolate to women in “less favorable situations” where poor access to quality medical and obstetric care, malnutrition, and untreated chronic conditions are more common, Dr. Klebanoff added.
Another limitation of the study, acknowledged by Regan and coauthors, is the relatively small number of stillbirths in subsequent pregnancies (228) despite this being the largest study of its kind to date.
“The fairly small number of women included in this report dictates that replication, probably using other large, linked, population-level databases, is required,” Dr. Klebanoff said in his commentary.
Dr. Klebanoff is with the Center for Perinatal Research, The Research Institute at Nationwide Children’s Hospital; and the departments of pediatrics and obstetrics and gynecology at the College of Medicine, and division of epidemiology at the College of Public Health, at The Ohio State University, all in Columbus. This is a summarization of his commentary (Lancet. 2019 Feb 28. doi: 10.1016/S0140-6736(18)32430-9 ). Dr. Klebanoff said he had a pending grant application to the National Institutes of Health to study the association between interpregnancy interval and birth outcomes, and had no other competing interests.
according to authors of a large, international observational study.
There was no significantly increased risk of stillbirth, preterm birth, or small-for-gestational-age birth in the next pregnancy for women who conceived in that 12-month time period, according to results of the study, which was based on birth records for nearly 14,500 women in Finland, Norway, and Australia.
“We hope that our findings can provide reassurance to women who wish to become pregnant or unexpectedly become pregnant shortly after a stillbirth,” study author Annette K. Regan, PhD, of Curtin University, Perth, Australia, said in a statement on the study, which appears in The Lancet.
Judette Marie Louis, MD, MPH, said that while data are conflicting on optimal interpregnancy interval following stillbirth, large population-based studies such as this one may provide an indication of the relative safety of an interval of 12 months or less. (She was not involved in this study.)
“This paper is good news for a lot of women,” Dr. Louis, associate professor of obstetrics and gynecology at the University of South Florida, Tampa, said in an interview. “After a stillbirth, it’s such a traumatic experience that some do want to move on, and these findings suggest that, yes, you don’t have to wait that long to have a successful pregnancy.”
These results are for women living in relatively high-income countries, so the findings might not apply to every population, she added. Dr. Louis was the first author of a recent interpregnancy care consensus statement by the American College of Obstetricians and Gynecologists and the Society of Maternal-Fetal Medicine, and was asked to comment on this study.
The World Health Organization recommends interpregnancy intervals of 2 years or more after live births and 6 months or more after miscarriage, but currently has no specific recommendations on the optimal interpregnancy interval after a stillbirth, according to Dr. Regan and her colleagues.
“Because length of gestation might affect nutrient concentrations and health status in women, it is plausible that the optimal interval after stillbirth is somewhere between the optimal interval after miscarriage and live birth,” they said in their report.
Researchers for two previous studies also have reported on the link between the interpregnancy interval after stillbirth and birth outcomes in the next pregnancy, but neither was specifically designed to evaluate that outcome, they added.
Dr. Regan and her coauthors used birth record data spanning several decades from three high-income countries to identify 14,452 women who had stillbirths. Of those, 63% conceived within the next 12 months, and for 37%, it was as early as 6 months.
Overall, 2% of the subsequent pregnancies ended in stillbirth, while 9% were small-for-gestational-age and 18% were preterm, according to the report.
In analyses adjusted for variables such as age, smoking, and education level, there was no association between short interpregnancy intervals and subsequent stillbirths, compared with longer intervals (24-59 months), with odds ratios of 1.09 for an interval shorter than 6 months and 0.90 for 6-11 months.
Likewise, there was no link between shorter intervals and subsequent small-for-gestational-age birth, with odds ratios of 0.66 for less than 6 months and 0.64 for 6-11 months, and no link between interval and subsequent preterm births, with odds ratios of 0.91 for both short-interval groups.
That data could be useful to health care providers who do postpartum counseling after stillbirths, and could potentially inform future recommendations on pregnancy spacing, Dr. Regan and her coauthors said.
“These results apply to a large proportion of women conceiving after a stillbirth,” they noted.
This study included countries with access to universal health care, with populations that are mostly white, so the results may not apply to low- or middle-income countries without universal health care or with significant ethnic minority populations, they added.
Dr. Regan and her colleagues declared no competing interests related to the study, which was funded the National Health and Medical Research Council of Australia, among other sources.
SOURCE: Regan AK et al. Lancet. 2019 Feb 28. doi: 10.1016/S0140-6736(18)32266-9.
according to authors of a large, international observational study.
There was no significantly increased risk of stillbirth, preterm birth, or small-for-gestational-age birth in the next pregnancy for women who conceived in that 12-month time period, according to results of the study, which was based on birth records for nearly 14,500 women in Finland, Norway, and Australia.
“We hope that our findings can provide reassurance to women who wish to become pregnant or unexpectedly become pregnant shortly after a stillbirth,” study author Annette K. Regan, PhD, of Curtin University, Perth, Australia, said in a statement on the study, which appears in The Lancet.
Judette Marie Louis, MD, MPH, said that while data are conflicting on optimal interpregnancy interval following stillbirth, large population-based studies such as this one may provide an indication of the relative safety of an interval of 12 months or less. (She was not involved in this study.)
“This paper is good news for a lot of women,” Dr. Louis, associate professor of obstetrics and gynecology at the University of South Florida, Tampa, said in an interview. “After a stillbirth, it’s such a traumatic experience that some do want to move on, and these findings suggest that, yes, you don’t have to wait that long to have a successful pregnancy.”
These results are for women living in relatively high-income countries, so the findings might not apply to every population, she added. Dr. Louis was the first author of a recent interpregnancy care consensus statement by the American College of Obstetricians and Gynecologists and the Society of Maternal-Fetal Medicine, and was asked to comment on this study.
The World Health Organization recommends interpregnancy intervals of 2 years or more after live births and 6 months or more after miscarriage, but currently has no specific recommendations on the optimal interpregnancy interval after a stillbirth, according to Dr. Regan and her colleagues.
“Because length of gestation might affect nutrient concentrations and health status in women, it is plausible that the optimal interval after stillbirth is somewhere between the optimal interval after miscarriage and live birth,” they said in their report.
Researchers for two previous studies also have reported on the link between the interpregnancy interval after stillbirth and birth outcomes in the next pregnancy, but neither was specifically designed to evaluate that outcome, they added.
Dr. Regan and her coauthors used birth record data spanning several decades from three high-income countries to identify 14,452 women who had stillbirths. Of those, 63% conceived within the next 12 months, and for 37%, it was as early as 6 months.
Overall, 2% of the subsequent pregnancies ended in stillbirth, while 9% were small-for-gestational-age and 18% were preterm, according to the report.
In analyses adjusted for variables such as age, smoking, and education level, there was no association between short interpregnancy intervals and subsequent stillbirths, compared with longer intervals (24-59 months), with odds ratios of 1.09 for an interval shorter than 6 months and 0.90 for 6-11 months.
Likewise, there was no link between shorter intervals and subsequent small-for-gestational-age birth, with odds ratios of 0.66 for less than 6 months and 0.64 for 6-11 months, and no link between interval and subsequent preterm births, with odds ratios of 0.91 for both short-interval groups.
That data could be useful to health care providers who do postpartum counseling after stillbirths, and could potentially inform future recommendations on pregnancy spacing, Dr. Regan and her coauthors said.
“These results apply to a large proportion of women conceiving after a stillbirth,” they noted.
This study included countries with access to universal health care, with populations that are mostly white, so the results may not apply to low- or middle-income countries without universal health care or with significant ethnic minority populations, they added.
Dr. Regan and her colleagues declared no competing interests related to the study, which was funded the National Health and Medical Research Council of Australia, among other sources.
SOURCE: Regan AK et al. Lancet. 2019 Feb 28. doi: 10.1016/S0140-6736(18)32266-9.
FROM THE LANCET
Sperm counts largely stable after adjuvant treatment of clinical stage I testicular cancer
Adjuvant treatments appear to have no significant detrimental long-term effects on sperm count in men being treated for clinical stage I testicular cancer, results of a recent investigation suggest.
Sperm number and concentration were largely stable over time in patients who received a round of chemotherapy or radiation to lymph nodes following orchiectomy, according to results of the 182-patient study.
Investigators said they still offer sperm banking before orchiectomy, since some patients will have low sperm counts prior to orchiectomy that persist after the procedure.
Moreover, the type of testicular cancer and the potential need for other postorchiectomy treatments are often “unknown factors” that underscore the importance of sperm banking, said the researchers, led by Kristina Weibring, MD, of Karolinska University Hospital, Stockholm.
“Assisted reproductive measures may be necessary for these patients regardless of any treatment given,” the researchers noted. The report is in Annals of Oncology.
The lack of effect on sperm counts in this study stands in contrast to previous studies, which clearly show the detrimental effects of multiple chemotherapy cycles on sperm recovery, the investigators said.
Their study comprised 182 patients 18-50 years of age with clinical stage I testicular cancer who underwent unilateral orchiectomy. Depending on tumor characteristics, the patients then received one cycle of adjuvant carboplatin, one cycle of a bleomycin, etoposide, and cisplatin (BEP) regimen, surveillance, or adjuvant radiotherapy to the infradiaphragmal para-aortic and ipsilateral iliac lymph nodes. Sperm samples were obtained at 6, 12, 24, 36, and 60 months after the completion of treatment.
While there was a transient drop in the radiation-treated patients at the 6-month evaluation, mean total sperm number otherwise increased over time in all groups, according to the investigators’ report.
Similarly, mean sperm concentration significantly increased from baseline to 12 months post treatment in the surveillance, BEP, and carboplatin groups, with a nonsignificant decrease in the radiotherapy group, they said in the report.
There were generally no significant differences in sperm count or concentration for the treatments, compared with surveillance, beyond a significant decrease in mean sperm count for radiation versus surveillance, they added.
There were likewise no significant changes in sperm measures for seminoma and nonseminoma patients at any point over the 5 years of evaluation, reported data show.
“With the results of this study, we can now inform our patients that adjuvant chemotherapy does not seem to affect the testicular function,” Dr. Weibring and her colleagues concluded.
The authors reported that they had no conflicts of interest related to the study, which was supported by the Swedish Cancer Society, among other sources.
SOURCE: Weibring K et al. Ann Oncol. 2019 Feb 25. doi: 10.1093/annonc/mdz017/5348526.
Adjuvant treatments appear to have no significant detrimental long-term effects on sperm count in men being treated for clinical stage I testicular cancer, results of a recent investigation suggest.
Sperm number and concentration were largely stable over time in patients who received a round of chemotherapy or radiation to lymph nodes following orchiectomy, according to results of the 182-patient study.
Investigators said they still offer sperm banking before orchiectomy, since some patients will have low sperm counts prior to orchiectomy that persist after the procedure.
Moreover, the type of testicular cancer and the potential need for other postorchiectomy treatments are often “unknown factors” that underscore the importance of sperm banking, said the researchers, led by Kristina Weibring, MD, of Karolinska University Hospital, Stockholm.
“Assisted reproductive measures may be necessary for these patients regardless of any treatment given,” the researchers noted. The report is in Annals of Oncology.
The lack of effect on sperm counts in this study stands in contrast to previous studies, which clearly show the detrimental effects of multiple chemotherapy cycles on sperm recovery, the investigators said.
Their study comprised 182 patients 18-50 years of age with clinical stage I testicular cancer who underwent unilateral orchiectomy. Depending on tumor characteristics, the patients then received one cycle of adjuvant carboplatin, one cycle of a bleomycin, etoposide, and cisplatin (BEP) regimen, surveillance, or adjuvant radiotherapy to the infradiaphragmal para-aortic and ipsilateral iliac lymph nodes. Sperm samples were obtained at 6, 12, 24, 36, and 60 months after the completion of treatment.
While there was a transient drop in the radiation-treated patients at the 6-month evaluation, mean total sperm number otherwise increased over time in all groups, according to the investigators’ report.
Similarly, mean sperm concentration significantly increased from baseline to 12 months post treatment in the surveillance, BEP, and carboplatin groups, with a nonsignificant decrease in the radiotherapy group, they said in the report.
There were generally no significant differences in sperm count or concentration for the treatments, compared with surveillance, beyond a significant decrease in mean sperm count for radiation versus surveillance, they added.
There were likewise no significant changes in sperm measures for seminoma and nonseminoma patients at any point over the 5 years of evaluation, reported data show.
“With the results of this study, we can now inform our patients that adjuvant chemotherapy does not seem to affect the testicular function,” Dr. Weibring and her colleagues concluded.
The authors reported that they had no conflicts of interest related to the study, which was supported by the Swedish Cancer Society, among other sources.
SOURCE: Weibring K et al. Ann Oncol. 2019 Feb 25. doi: 10.1093/annonc/mdz017/5348526.
Adjuvant treatments appear to have no significant detrimental long-term effects on sperm count in men being treated for clinical stage I testicular cancer, results of a recent investigation suggest.
Sperm number and concentration were largely stable over time in patients who received a round of chemotherapy or radiation to lymph nodes following orchiectomy, according to results of the 182-patient study.
Investigators said they still offer sperm banking before orchiectomy, since some patients will have low sperm counts prior to orchiectomy that persist after the procedure.
Moreover, the type of testicular cancer and the potential need for other postorchiectomy treatments are often “unknown factors” that underscore the importance of sperm banking, said the researchers, led by Kristina Weibring, MD, of Karolinska University Hospital, Stockholm.
“Assisted reproductive measures may be necessary for these patients regardless of any treatment given,” the researchers noted. The report is in Annals of Oncology.
The lack of effect on sperm counts in this study stands in contrast to previous studies, which clearly show the detrimental effects of multiple chemotherapy cycles on sperm recovery, the investigators said.
Their study comprised 182 patients 18-50 years of age with clinical stage I testicular cancer who underwent unilateral orchiectomy. Depending on tumor characteristics, the patients then received one cycle of adjuvant carboplatin, one cycle of a bleomycin, etoposide, and cisplatin (BEP) regimen, surveillance, or adjuvant radiotherapy to the infradiaphragmal para-aortic and ipsilateral iliac lymph nodes. Sperm samples were obtained at 6, 12, 24, 36, and 60 months after the completion of treatment.
While there was a transient drop in the radiation-treated patients at the 6-month evaluation, mean total sperm number otherwise increased over time in all groups, according to the investigators’ report.
Similarly, mean sperm concentration significantly increased from baseline to 12 months post treatment in the surveillance, BEP, and carboplatin groups, with a nonsignificant decrease in the radiotherapy group, they said in the report.
There were generally no significant differences in sperm count or concentration for the treatments, compared with surveillance, beyond a significant decrease in mean sperm count for radiation versus surveillance, they added.
There were likewise no significant changes in sperm measures for seminoma and nonseminoma patients at any point over the 5 years of evaluation, reported data show.
“With the results of this study, we can now inform our patients that adjuvant chemotherapy does not seem to affect the testicular function,” Dr. Weibring and her colleagues concluded.
The authors reported that they had no conflicts of interest related to the study, which was supported by the Swedish Cancer Society, among other sources.
SOURCE: Weibring K et al. Ann Oncol. 2019 Feb 25. doi: 10.1093/annonc/mdz017/5348526.
FROM ANNALS OF ONCOLOGY
Delaying antibiotics in elderly with UTI linked to higher sepsis, death rates
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
This study linking primary care prescribing to serious infections in elderly patients with urinary tract infections is timely, as rates of bloodstream infection and mortality are increasing in this age group, according to Alastair D. Hay, MB.ChB, a professor at University of Bristol, England.
“Prompt treatment should be offered to older patients, men (who are at higher risk than women), and those living in areas of greater socioeconomic deprivation who are at the highest risk of bloodstream infections,” Dr. Hay said in an editorial accompanying the report by Gharbi et al.
That said, the link between prescribing and infection in this particular study may not be causal: “The implications are likely to be more nuanced than primary care doctors risking the health of older adults to meet targets for antimicrobial stewardship,” Dr. Hay noted.
Doctors are cautious when managing infections in vulnerable groups, evidence shows, and the deferred prescribing reported in this study is likely not the same as the delayed prescribing seen in primary care, he explained.
“Most clinicians issue a prescription on the day of presentation, with verbal advice to delay treatment, rather than waiting for a patient to return or issuing a postdated prescription,” he said. “The group given immediate antibiotics in the study by Gharbi and colleagues likely contained some patients managed in this way.”
Patients who apparently had no prescription in this retrospective analysis may have had a same-day admission with a bloodstream infection; moreover, a number of bloodstream infections in older people are due to urinary tract bacteria, and so would not be prevented by treatment for urinary tract infection, Dr. Hay said.
“Further research is needed to establish whether treatment should be initiated with a broad or a narrow spectrum antibiotic and to identify those in whom delaying treatment (while awaiting investigation) is safe,” he concluded.
Dr. Hay is a professor in the Centre for Academic Primary Care, University of Bristol, England. His editorial appears in The BMJ (2019 Feb 27. doi: 10.1136/bmj.l780). Dr. Hay declared that he is a member of the managing common infections guideline committee for the National Institute for Health and Care Excellence (NICE).
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
results of a large, population-based study suggest.
The risk of bloodstream infection was more than seven times greater in patients who did not receive antibiotics immediately after seeing a general practitioner for a UTI versus those who did, according to results of the study based on primary care records and other data for nearly 160,000 U.K. patients aged 65 years or older. Death rates and hospital admissions were significantly higher for these patients, according to the study published in The BMJ by Myriam Gharbi, PharmD, Phd, Imperial College London, and her colleagues.
The publication of these findings coincides with an increase in Escherichia coli bloodstream infections in England.
“Our study suggests the early initiation of antibiotics for UTI in older high risk adult populations (especially men aged [older than] 85 years) should be recommended to prevent serious complications,” Dr. Gharbi and her coauthors said in their report.
The population-based cohort study comprised 157,264 adult primary care patients at least 65 years of age who had one or more suspected or confirmed lower UTIs from November 2007 to May 2015. The researchers found that health care providers had diagnosed a total of 312,896 UTI episodes in these patients during the period they studied. In 7.2% (22,534) of the UTI episodes, the researchers were unable to find records of the patients having been prescribed antibiotics by a general practitioner within 7 days of the UTI diagnosis. These 22,534 episodes included those that occurred in patients who had a complication before an antibiotic was prescribed. An additional 6.2% (19,292) of the episodes occurred in patients who were prescribed antibiotics, but not during their first UTI-related visit to a general practitioner or on the same day of such a visit. The researchers classified this group of patients as having been prescribed antibiotics on a deferred or delayed basis, as they were not prescribed such drugs within 7 days of their visit.
Overall, there were 1,539 cases (0.5% of the total number of UTIs) of bloodstream infection within 60 days of the initial urinary tract infection diagnosis, the researchers reported.
The bloodstream infection rate was 2.9% for patients who were not prescribed antibiotics ever or prior to an infection occurring, 2.2% in those who were prescribed antibiotics on a deferred basis, and 0.2% in those who were prescribed antibiotics immediately, meaning during their first visit to a general practitioner for a UTI or on the same day of such a visit (P less than .001). After adjustment for potential confounding variables such as age, sex, and region, the patients classified as having not been prescribed antibiotics or having been prescribed antibiotics on a deferred basis were significantly more likely to have a bloodstream infection within 60 days of their visit to a health care provider, compared with those who received antibiotics immediately, with odds ratios of 8.08 (95% confidence interval, 7.12-9.16) and 7.12 (95% CI, 6.22-8.14), respectively.
Hospital admissions after a UTI episode were nearly twice as high in the no- or deferred-antibiotics groups (27.0% and 26.8%, respectively), compared with the group that received antibiotics right away (14.8%), the investigators reported. The lengths of hospital stays were 12.1 days for the group classified as having not been prescribed antibiotics, 7.7 days for the group subject to delayed antibiotic prescribing, and 6.3 days for the group who received antibiotics immediately.
Deaths within 60 days of experiencing a urinary tract infection occurred in 5.4% of patients in the no-antibiotics group, 2.8% of the deferred-antibiotics group, and 1.6% of the immediate-antibiotics group. After adjustment for covariates, a regression analysis showed the risks for all-cause mortality were 1.16 and 2.18 times higher in the deferred-antibiotics group and the no-antibiotics group, respectively, according to the paper.
In the immediate-antibiotics group, those patients who received nitrofurantoin had a “small but significant increase” in 60-day survival versus those who received trimethoprim, the investigators noted in the discussion section of their report.
“This increase could reflect either higher levels of resistance to trimethoprim or a healthier population treated with nitrofurantoin, the latest being not recommended for patients with poor kidney function,” the researchers wrote.
This study was supported by the National Institute for Health Research and other U.K. sources. One study coauthor reported working as an epidemiologist with GSK in areas not related to the study.
SOURCE: Gharbi M et al. BMJ. 2019 Feb 27. doi: 10.1136/bmj.l525.
FROM THE BMJ