User login
Watchful waiting up for low-risk prostate cancer
Conservative management for low-risk localized prostate cancer is up recently, in line with clinical practice guideline changes, while in high-risk disease, use of radical prostatectomy has increased despite a lack of new high-level evidence supporting the approach, according to researchers.
Active surveillance or watchful waiting surpassed both radical prostatectomy and radiotherapy to become the most common management strategy in low-risk disease over the 2010-2015 time period, according to their analysis of a Surveillance, Epidemiology, and End Results (SEER) database.
Meanwhile, radical prostatectomy use declined in low-risk patients, but increased in those with higher-risk disease at the expense of radiotherapy, said authors of the analysis, led by Brandon A. Mahal, MD, and Paul L. Nguyen, MD, of Dana-Farber Cancer Institute, Boston.
“Although increasing use of active surveillance or watchful waiting for low-risk disease has been supported by high-level evidence and guidelines since 2010, shifting management patterns toward more radical prostatectomy in higher-risk disease and away from radiotherapy does not coincide with any new level 1 evidence or guideline changes,” Dr. Mahal, Dr. Nguyen, and coauthors said in JAMA.
The analysis included 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database. Of that group, 12.7% were managed by active surveillance or watchful waiting, while 41.5% underwent radiotherapy and 45.8% had a radical prostatectomy.
For men with low-risk disease, active surveillance or watchful waiting increased from just 14.5% in 2010 to 42.1% in 2015, investigators found. Radical prostatectomy decreased from 47.4% to 31.3% over that 5-year period, while radiotherapy likewise decreased from 38.0% to 26.6% (P less than .001 for all three trends).
By contrast, in men with high-risk disease, use of radical prostatectomy increased from 38.0% to 42.8%, while radiotherapy decreased from 60.1% to 55.0% (P less than .001 for both trends), and use of active surveillance remained low and steady at 1.9% in 2010 to 2.2% in 2015.
Intermediate-risk disease saw a significant increase in active surveillance, from 5.8% to 9.6% over the time period, with commensurate decreases in both radical prostatectomy and radiotherapy, according to the report.
While low-risk prostate cancer was traditionally managed with radical prostatectomy, national clinical practice guidelines starting in 2010 began recommending conservative management with active surveillance or watchful waiting, researchers noted in their report.
These epidemiologic data don’t provide any insights on clinical outcomes related to the management changes, investigators acknowledged. They said further study is needed to determine the “downstream effects” of increased active surveillance or watchful waiting in low-risk prostate cancer.
Dr. Mahal reported no conflicts of interest, while Dr. Nguyen provided disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, and Astellas. Coauthors had disclosures relate to Janssen, Blue Earth, and the National Institutes of Health.
SOURCE: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
Conservative management for low-risk localized prostate cancer is up recently, in line with clinical practice guideline changes, while in high-risk disease, use of radical prostatectomy has increased despite a lack of new high-level evidence supporting the approach, according to researchers.
Active surveillance or watchful waiting surpassed both radical prostatectomy and radiotherapy to become the most common management strategy in low-risk disease over the 2010-2015 time period, according to their analysis of a Surveillance, Epidemiology, and End Results (SEER) database.
Meanwhile, radical prostatectomy use declined in low-risk patients, but increased in those with higher-risk disease at the expense of radiotherapy, said authors of the analysis, led by Brandon A. Mahal, MD, and Paul L. Nguyen, MD, of Dana-Farber Cancer Institute, Boston.
“Although increasing use of active surveillance or watchful waiting for low-risk disease has been supported by high-level evidence and guidelines since 2010, shifting management patterns toward more radical prostatectomy in higher-risk disease and away from radiotherapy does not coincide with any new level 1 evidence or guideline changes,” Dr. Mahal, Dr. Nguyen, and coauthors said in JAMA.
The analysis included 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database. Of that group, 12.7% were managed by active surveillance or watchful waiting, while 41.5% underwent radiotherapy and 45.8% had a radical prostatectomy.
For men with low-risk disease, active surveillance or watchful waiting increased from just 14.5% in 2010 to 42.1% in 2015, investigators found. Radical prostatectomy decreased from 47.4% to 31.3% over that 5-year period, while radiotherapy likewise decreased from 38.0% to 26.6% (P less than .001 for all three trends).
By contrast, in men with high-risk disease, use of radical prostatectomy increased from 38.0% to 42.8%, while radiotherapy decreased from 60.1% to 55.0% (P less than .001 for both trends), and use of active surveillance remained low and steady at 1.9% in 2010 to 2.2% in 2015.
Intermediate-risk disease saw a significant increase in active surveillance, from 5.8% to 9.6% over the time period, with commensurate decreases in both radical prostatectomy and radiotherapy, according to the report.
While low-risk prostate cancer was traditionally managed with radical prostatectomy, national clinical practice guidelines starting in 2010 began recommending conservative management with active surveillance or watchful waiting, researchers noted in their report.
These epidemiologic data don’t provide any insights on clinical outcomes related to the management changes, investigators acknowledged. They said further study is needed to determine the “downstream effects” of increased active surveillance or watchful waiting in low-risk prostate cancer.
Dr. Mahal reported no conflicts of interest, while Dr. Nguyen provided disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, and Astellas. Coauthors had disclosures relate to Janssen, Blue Earth, and the National Institutes of Health.
SOURCE: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
Conservative management for low-risk localized prostate cancer is up recently, in line with clinical practice guideline changes, while in high-risk disease, use of radical prostatectomy has increased despite a lack of new high-level evidence supporting the approach, according to researchers.
Active surveillance or watchful waiting surpassed both radical prostatectomy and radiotherapy to become the most common management strategy in low-risk disease over the 2010-2015 time period, according to their analysis of a Surveillance, Epidemiology, and End Results (SEER) database.
Meanwhile, radical prostatectomy use declined in low-risk patients, but increased in those with higher-risk disease at the expense of radiotherapy, said authors of the analysis, led by Brandon A. Mahal, MD, and Paul L. Nguyen, MD, of Dana-Farber Cancer Institute, Boston.
“Although increasing use of active surveillance or watchful waiting for low-risk disease has been supported by high-level evidence and guidelines since 2010, shifting management patterns toward more radical prostatectomy in higher-risk disease and away from radiotherapy does not coincide with any new level 1 evidence or guideline changes,” Dr. Mahal, Dr. Nguyen, and coauthors said in JAMA.
The analysis included 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database. Of that group, 12.7% were managed by active surveillance or watchful waiting, while 41.5% underwent radiotherapy and 45.8% had a radical prostatectomy.
For men with low-risk disease, active surveillance or watchful waiting increased from just 14.5% in 2010 to 42.1% in 2015, investigators found. Radical prostatectomy decreased from 47.4% to 31.3% over that 5-year period, while radiotherapy likewise decreased from 38.0% to 26.6% (P less than .001 for all three trends).
By contrast, in men with high-risk disease, use of radical prostatectomy increased from 38.0% to 42.8%, while radiotherapy decreased from 60.1% to 55.0% (P less than .001 for both trends), and use of active surveillance remained low and steady at 1.9% in 2010 to 2.2% in 2015.
Intermediate-risk disease saw a significant increase in active surveillance, from 5.8% to 9.6% over the time period, with commensurate decreases in both radical prostatectomy and radiotherapy, according to the report.
While low-risk prostate cancer was traditionally managed with radical prostatectomy, national clinical practice guidelines starting in 2010 began recommending conservative management with active surveillance or watchful waiting, researchers noted in their report.
These epidemiologic data don’t provide any insights on clinical outcomes related to the management changes, investigators acknowledged. They said further study is needed to determine the “downstream effects” of increased active surveillance or watchful waiting in low-risk prostate cancer.
Dr. Mahal reported no conflicts of interest, while Dr. Nguyen provided disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, and Astellas. Coauthors had disclosures relate to Janssen, Blue Earth, and the National Institutes of Health.
SOURCE: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
FROM JAMA
Key clinical point: Conservative management for low-risk localized prostate cancer is up, in line with guidelines, while radical prostatectomy use has increased in high-risk disease despite a lack of new high-level evidence to support that approach.
Major finding: In men with low-risk disease, active surveillance or watchful waiting increased from 14.5% in 2010 to 42.1% in 2015, while in high-risk disease, radical prostatectomy increased from 38.0% to 42.8%
Study details: Analysis including 164,760 men with a diagnosis of localized prostate cancer between 2010 and 2015 in the SEER Prostate Active Surveillance/Watchful Waiting database.
Disclosures: Study authors reported disclosures related to Ferring, Augmenix, Bayer, Janssen, Astellas, Dendreon, Genome DX, Blue Earth Diagnostics, Cota, Nanobiotix, Janssen, Astellas, and the National Institutes of Health.
Source: Mahal BA et al. JAMA. 2019 Feb 11. doi: 10.1001/jama.2018.19941.
Anthracyclines, bendamustine are options for grade 3A follicular lymphoma
While optimal treatment for grade 3A follicular lymphoma remains in question, either anthracycline-based chemotherapy or bendamustine appear to be preferable to cyclophosphamide, vincristine, and prednisone (CVP), results of a recent analysis suggest.
Time to progression with anthracycline-based chemotherapy was superior to that of CVP in the retrospective, multicenter study.
At the same time, clinical outcomes were comparable between anthracycline-based chemotherapy and bendamustine, according to Nirav N. Shah, MD, of the Medical College of Wisconsin, Milwaukee, and his coinvestigators.
“Both remain appropriate frontline options for this patient population,” Dr. Shah and his colleagues wrote in Clinical Lymphoma, Myeloma & Leukemia.
Frontline therapy for follicular lymphoma has evolved, and recently shifted toward bendamustine-based chemotherapy regimens in light of two large randomized trials, according to the investigators. However, optimal therapy – specifically for grade 3A follicular lymphoma – has been debated for more than 20 years, they added.
“While some approach it as an aggressive malignancy, others treat it as an indolent lymphoma,” they wrote.
Accordingly, Dr. Shah and his colleagues sought to evaluate treatment outcomes with these regimens in 103 advanced stage 3/4 follicular lymphoma patients from six centers seen over a 10-year period.
Of those patients, 65 had received anthracycline-based chemotherapy, 30 received bendamustine, and 8 received CVP. All received either rituximab or ofatumumab in combination with the chemotherapy, and about one-third went on to receive maintenance treatment with one of those two anti-CD20 antibodies.
The proportion of patients not experiencing disease progression at 24 months from the initiation of treatment was significantly different between arms, at 72% for those receiving anthracyclines, 79% for bendamustine, and 50% for CVP (P = .01).
Patients who received CVP had a significantly poorer time-to-progression outcomes versus anthracycline-based chemotherapy, an adjusted analysis showed (hazard ratio, 3.22; 95% confidence interval, 1.26-8.25; P = .01), while by contrast, there was no significant difference between bendamustine and anthracyclines on this endpoint.
Progression-free survival was likewise worse for CVP compared with anthracycline-based chemotherapy, but there was no significant difference in overall survival for either CVP or bendamustine compared with anthracycline-based chemotherapy, the investigators said.
The 5-year overall survival was estimated to be 82% for anthracycline-based chemotherapy, 74% for bendamustine, and 58% for CVP (P = .23).
Optimal treatment of grade 3A follicular lymphoma remains controversial despite these findings, the investigators noted.
“Unfortunately, this specific histology was excluded from pivotal trials comparing anthracycline-based chemotherapy to bendamustine, leaving the question of optimal frontline treatment unanswered in this subset,” they wrote.
The situation could change with a subgroup analysis of GALLIUM, which might provide some prospective data for this histology. Beyond that, it would be helpful to have prospective, randomized studies specifically enrolling grade 3A disease, Dr. Shah and his coauthors wrote.
Dr. Shah reported disclosures related to Exelixis, Oncosec, Geron, Jazz, Kite, Juno, and Lentigen Technology. Coauthors provided disclosures related to Sanofi-Genzyme, Celgene, Takeda, Otsuka, Spectrum, Merck, and Astellas, among others.
SOURCE: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Feb;19(2):95-102.
While optimal treatment for grade 3A follicular lymphoma remains in question, either anthracycline-based chemotherapy or bendamustine appear to be preferable to cyclophosphamide, vincristine, and prednisone (CVP), results of a recent analysis suggest.
Time to progression with anthracycline-based chemotherapy was superior to that of CVP in the retrospective, multicenter study.
At the same time, clinical outcomes were comparable between anthracycline-based chemotherapy and bendamustine, according to Nirav N. Shah, MD, of the Medical College of Wisconsin, Milwaukee, and his coinvestigators.
“Both remain appropriate frontline options for this patient population,” Dr. Shah and his colleagues wrote in Clinical Lymphoma, Myeloma & Leukemia.
Frontline therapy for follicular lymphoma has evolved, and recently shifted toward bendamustine-based chemotherapy regimens in light of two large randomized trials, according to the investigators. However, optimal therapy – specifically for grade 3A follicular lymphoma – has been debated for more than 20 years, they added.
“While some approach it as an aggressive malignancy, others treat it as an indolent lymphoma,” they wrote.
Accordingly, Dr. Shah and his colleagues sought to evaluate treatment outcomes with these regimens in 103 advanced stage 3/4 follicular lymphoma patients from six centers seen over a 10-year period.
Of those patients, 65 had received anthracycline-based chemotherapy, 30 received bendamustine, and 8 received CVP. All received either rituximab or ofatumumab in combination with the chemotherapy, and about one-third went on to receive maintenance treatment with one of those two anti-CD20 antibodies.
The proportion of patients not experiencing disease progression at 24 months from the initiation of treatment was significantly different between arms, at 72% for those receiving anthracyclines, 79% for bendamustine, and 50% for CVP (P = .01).
Patients who received CVP had a significantly poorer time-to-progression outcomes versus anthracycline-based chemotherapy, an adjusted analysis showed (hazard ratio, 3.22; 95% confidence interval, 1.26-8.25; P = .01), while by contrast, there was no significant difference between bendamustine and anthracyclines on this endpoint.
Progression-free survival was likewise worse for CVP compared with anthracycline-based chemotherapy, but there was no significant difference in overall survival for either CVP or bendamustine compared with anthracycline-based chemotherapy, the investigators said.
The 5-year overall survival was estimated to be 82% for anthracycline-based chemotherapy, 74% for bendamustine, and 58% for CVP (P = .23).
Optimal treatment of grade 3A follicular lymphoma remains controversial despite these findings, the investigators noted.
“Unfortunately, this specific histology was excluded from pivotal trials comparing anthracycline-based chemotherapy to bendamustine, leaving the question of optimal frontline treatment unanswered in this subset,” they wrote.
The situation could change with a subgroup analysis of GALLIUM, which might provide some prospective data for this histology. Beyond that, it would be helpful to have prospective, randomized studies specifically enrolling grade 3A disease, Dr. Shah and his coauthors wrote.
Dr. Shah reported disclosures related to Exelixis, Oncosec, Geron, Jazz, Kite, Juno, and Lentigen Technology. Coauthors provided disclosures related to Sanofi-Genzyme, Celgene, Takeda, Otsuka, Spectrum, Merck, and Astellas, among others.
SOURCE: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Feb;19(2):95-102.
While optimal treatment for grade 3A follicular lymphoma remains in question, either anthracycline-based chemotherapy or bendamustine appear to be preferable to cyclophosphamide, vincristine, and prednisone (CVP), results of a recent analysis suggest.
Time to progression with anthracycline-based chemotherapy was superior to that of CVP in the retrospective, multicenter study.
At the same time, clinical outcomes were comparable between anthracycline-based chemotherapy and bendamustine, according to Nirav N. Shah, MD, of the Medical College of Wisconsin, Milwaukee, and his coinvestigators.
“Both remain appropriate frontline options for this patient population,” Dr. Shah and his colleagues wrote in Clinical Lymphoma, Myeloma & Leukemia.
Frontline therapy for follicular lymphoma has evolved, and recently shifted toward bendamustine-based chemotherapy regimens in light of two large randomized trials, according to the investigators. However, optimal therapy – specifically for grade 3A follicular lymphoma – has been debated for more than 20 years, they added.
“While some approach it as an aggressive malignancy, others treat it as an indolent lymphoma,” they wrote.
Accordingly, Dr. Shah and his colleagues sought to evaluate treatment outcomes with these regimens in 103 advanced stage 3/4 follicular lymphoma patients from six centers seen over a 10-year period.
Of those patients, 65 had received anthracycline-based chemotherapy, 30 received bendamustine, and 8 received CVP. All received either rituximab or ofatumumab in combination with the chemotherapy, and about one-third went on to receive maintenance treatment with one of those two anti-CD20 antibodies.
The proportion of patients not experiencing disease progression at 24 months from the initiation of treatment was significantly different between arms, at 72% for those receiving anthracyclines, 79% for bendamustine, and 50% for CVP (P = .01).
Patients who received CVP had a significantly poorer time-to-progression outcomes versus anthracycline-based chemotherapy, an adjusted analysis showed (hazard ratio, 3.22; 95% confidence interval, 1.26-8.25; P = .01), while by contrast, there was no significant difference between bendamustine and anthracyclines on this endpoint.
Progression-free survival was likewise worse for CVP compared with anthracycline-based chemotherapy, but there was no significant difference in overall survival for either CVP or bendamustine compared with anthracycline-based chemotherapy, the investigators said.
The 5-year overall survival was estimated to be 82% for anthracycline-based chemotherapy, 74% for bendamustine, and 58% for CVP (P = .23).
Optimal treatment of grade 3A follicular lymphoma remains controversial despite these findings, the investigators noted.
“Unfortunately, this specific histology was excluded from pivotal trials comparing anthracycline-based chemotherapy to bendamustine, leaving the question of optimal frontline treatment unanswered in this subset,” they wrote.
The situation could change with a subgroup analysis of GALLIUM, which might provide some prospective data for this histology. Beyond that, it would be helpful to have prospective, randomized studies specifically enrolling grade 3A disease, Dr. Shah and his coauthors wrote.
Dr. Shah reported disclosures related to Exelixis, Oncosec, Geron, Jazz, Kite, Juno, and Lentigen Technology. Coauthors provided disclosures related to Sanofi-Genzyme, Celgene, Takeda, Otsuka, Spectrum, Merck, and Astellas, among others.
SOURCE: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Feb;19(2):95-102.
FROM CLINICAL LYMPHOMA, MYELOMA & LEUKEMIA
Key clinical point:
Major finding: Patients who received CVP had a significantly poorer time-to-progression outcome versus anthracycline-based chemotherapy (hazard ratio, 3.22; 95% CI, 1.26-8.25; P = .01), while there was no significant difference between bendamustine and anthracyclines.
Study details: A multicenter analysis including 103 patients with advanced stage grade 3A follicular lymphoma.
Disclosures: The authors reported disclosures related to Exelixis, OncoSec, Geron, Jazz, Kite, Juno, Lentigen Technology, Sanofi-Genzyme, Celgene, Takeda, Otsuka, Spectrum, Merck, and Astellas, among others.
Source: Shah NN et al. Clin Lymphoma Myeloma Leuk. 2019 Feb;19(2):95-102.
BCL expression intensity key in distinguishing FL lesions
Intensity of BCL2 expression, and to a lesser extent expression of t(14;18), may help distinguish common and indolent cutaneous lymphomas from poorer-prognosis cutaneous lesions secondary to systemic follicular lymphomas, results of a recent investigation show.
Strong expression of BCL2 was almost always associated with secondary cutaneous follicular lymphoma (SCFL), and infrequently associated with primary cutaneous follicular center-cell lymphoma (PCFCL), according to the study results.
The translocation t(14;18) was likewise linked to secondary lesions, occurring less frequently in PCFCL in the study, reported recently in the Journal of Cutaneous Pathology.
“BCL2 expression intensity is the single most valuable clue in differentiating PCFCL from SCFL cases on histopathological grounds,” said Ramon M. Pujol, MD, PhD, of Hospital del Mar, Barcelona, Spain, and colleagues.
One of the main cutaneous B-cell lymphoma subtypes, PCFCL is marked by frequent relapses, but little incidence of systemic spread, meaning that conservative, skin-based therapies are usually warranted. By contrast, patients with SCFLs have a poor prognosis and may require systemic therapy, the investigators noted in their report.
Previous investigations have yielded conflicting results on the role of BCL2 expression, CD10 expression, and presence of t(14;18) translocation in distinguishing PCFCL from SCFL.
While early studies suggested most PCFCLs were negative for these markers, some recent reports suggested BCL positivity in PCFCLs is as high as 86%, the investigators said.
Accordingly, Dr. Pujol and colleagues evaluated clinicopathologic and genetic features in a large series of patients, including 59 with PCFCL and 22 with SCFL.
Significant BCL2 expression was seen in 69% of PCFCLs and in 100% of SCFLs (P = .003) in this patient series; however, when looking at BCL2 intensity, investigators found strong expression almost exclusively in SCFL. Strong expression was seen in 46% of those patients with secondary lymphomas, versus just 4%, or two cases, in the PCFCL group (P = .001).
The t(14;18) translocation was seen in 64% of SCFLs and only 9.1% of PCFCLs (P = .001).
Similar to what was seen for BCL2, expression of CD10 was observed in 66% of PCFCLs and 91% of SCFLs, and again, intensity differences mattered. Strong CD10 expression was seen in 62% of secondary lymphomas and 16% of PCFCLs (P = .01). But the high number of positive PCFCLs made this marker less useful than BCL2, the investigators said.
“We believe that differences in BCL2 and CD10 expression between our results and older previous studies could reflect the improvement of antigen retrieval laboratory techniques,” they said.
The investigators did not report disclosures related to the research.
SOURCE: Servitje O et al. J Cutan Pathol. 2019;46:182-9.
Intensity of BCL2 expression, and to a lesser extent expression of t(14;18), may help distinguish common and indolent cutaneous lymphomas from poorer-prognosis cutaneous lesions secondary to systemic follicular lymphomas, results of a recent investigation show.
Strong expression of BCL2 was almost always associated with secondary cutaneous follicular lymphoma (SCFL), and infrequently associated with primary cutaneous follicular center-cell lymphoma (PCFCL), according to the study results.
The translocation t(14;18) was likewise linked to secondary lesions, occurring less frequently in PCFCL in the study, reported recently in the Journal of Cutaneous Pathology.
“BCL2 expression intensity is the single most valuable clue in differentiating PCFCL from SCFL cases on histopathological grounds,” said Ramon M. Pujol, MD, PhD, of Hospital del Mar, Barcelona, Spain, and colleagues.
One of the main cutaneous B-cell lymphoma subtypes, PCFCL is marked by frequent relapses, but little incidence of systemic spread, meaning that conservative, skin-based therapies are usually warranted. By contrast, patients with SCFLs have a poor prognosis and may require systemic therapy, the investigators noted in their report.
Previous investigations have yielded conflicting results on the role of BCL2 expression, CD10 expression, and presence of t(14;18) translocation in distinguishing PCFCL from SCFL.
While early studies suggested most PCFCLs were negative for these markers, some recent reports suggested BCL positivity in PCFCLs is as high as 86%, the investigators said.
Accordingly, Dr. Pujol and colleagues evaluated clinicopathologic and genetic features in a large series of patients, including 59 with PCFCL and 22 with SCFL.
Significant BCL2 expression was seen in 69% of PCFCLs and in 100% of SCFLs (P = .003) in this patient series; however, when looking at BCL2 intensity, investigators found strong expression almost exclusively in SCFL. Strong expression was seen in 46% of those patients with secondary lymphomas, versus just 4%, or two cases, in the PCFCL group (P = .001).
The t(14;18) translocation was seen in 64% of SCFLs and only 9.1% of PCFCLs (P = .001).
Similar to what was seen for BCL2, expression of CD10 was observed in 66% of PCFCLs and 91% of SCFLs, and again, intensity differences mattered. Strong CD10 expression was seen in 62% of secondary lymphomas and 16% of PCFCLs (P = .01). But the high number of positive PCFCLs made this marker less useful than BCL2, the investigators said.
“We believe that differences in BCL2 and CD10 expression between our results and older previous studies could reflect the improvement of antigen retrieval laboratory techniques,” they said.
The investigators did not report disclosures related to the research.
SOURCE: Servitje O et al. J Cutan Pathol. 2019;46:182-9.
Intensity of BCL2 expression, and to a lesser extent expression of t(14;18), may help distinguish common and indolent cutaneous lymphomas from poorer-prognosis cutaneous lesions secondary to systemic follicular lymphomas, results of a recent investigation show.
Strong expression of BCL2 was almost always associated with secondary cutaneous follicular lymphoma (SCFL), and infrequently associated with primary cutaneous follicular center-cell lymphoma (PCFCL), according to the study results.
The translocation t(14;18) was likewise linked to secondary lesions, occurring less frequently in PCFCL in the study, reported recently in the Journal of Cutaneous Pathology.
“BCL2 expression intensity is the single most valuable clue in differentiating PCFCL from SCFL cases on histopathological grounds,” said Ramon M. Pujol, MD, PhD, of Hospital del Mar, Barcelona, Spain, and colleagues.
One of the main cutaneous B-cell lymphoma subtypes, PCFCL is marked by frequent relapses, but little incidence of systemic spread, meaning that conservative, skin-based therapies are usually warranted. By contrast, patients with SCFLs have a poor prognosis and may require systemic therapy, the investigators noted in their report.
Previous investigations have yielded conflicting results on the role of BCL2 expression, CD10 expression, and presence of t(14;18) translocation in distinguishing PCFCL from SCFL.
While early studies suggested most PCFCLs were negative for these markers, some recent reports suggested BCL positivity in PCFCLs is as high as 86%, the investigators said.
Accordingly, Dr. Pujol and colleagues evaluated clinicopathologic and genetic features in a large series of patients, including 59 with PCFCL and 22 with SCFL.
Significant BCL2 expression was seen in 69% of PCFCLs and in 100% of SCFLs (P = .003) in this patient series; however, when looking at BCL2 intensity, investigators found strong expression almost exclusively in SCFL. Strong expression was seen in 46% of those patients with secondary lymphomas, versus just 4%, or two cases, in the PCFCL group (P = .001).
The t(14;18) translocation was seen in 64% of SCFLs and only 9.1% of PCFCLs (P = .001).
Similar to what was seen for BCL2, expression of CD10 was observed in 66% of PCFCLs and 91% of SCFLs, and again, intensity differences mattered. Strong CD10 expression was seen in 62% of secondary lymphomas and 16% of PCFCLs (P = .01). But the high number of positive PCFCLs made this marker less useful than BCL2, the investigators said.
“We believe that differences in BCL2 and CD10 expression between our results and older previous studies could reflect the improvement of antigen retrieval laboratory techniques,” they said.
The investigators did not report disclosures related to the research.
SOURCE: Servitje O et al. J Cutan Pathol. 2019;46:182-9.
FROM THE JOURNAL OF CUTANEOUS PATHOLOGY
Key clinical point:
Major finding: Strong BCL2 expression was seen in 46% of secondary lymphomas, versus just 4% of primary cutaneous follicular center-cell lymphomas (P = .001).
Study details: A comparative study evaluating clinicopathologic and genetic features in a series of patients, including 59 with PCFCL and 22 with SCFL.
Disclosures: Investigators did not report disclosures related to the research.
Source: Servitje O et al. J Cutan Pathol. 2019;46:182-9.
Laparoscopic distal gastrectomy safe alternative to open surgery
When experienced surgeons are involved, laparoscopic distal gastrectomy is a safe alternative to open surgery in patients with early-stage gastric cancer, results of a randomized trial suggest.
Five-year overall survival exceeded 93% for both laparoscopic and open surgery groups in the multicenter trial, which included 1,416 patients with stage I gastric cancer treated by 15 surgeons who each had performed at least 100 gastrectomies.
Cancer-specific survival and recurrence were not significantly different between groups, while an intent-to-treat analysis confirmed the noninferiority of laparoscopic gastrectomy versus the open procedure, said investigators, led by Hyung-Ho Kim MD, PhD, of the Korean Laparoendoscopic Gastrointestinal Surgery Study (KLASS) group.
“Our trial supports the use of laparoscopic distal gastrectomy as a standard treatment option for clinical stage I distal gastric cancer when it can be performed by surgeons with sufficient experience,” Dr. Kim and his coauthors wrote in JAMA Oncology.
Some had doubted the oncologic safety of the laparoscopic approach because of the potential for inadequate lymphadenectomy leading to an increased risk of locoregional recurrence, said Dr. Kim and his coauthors in the KLASS group, “which includes 15 surgeons from 13 institutes.” However, among patients in this phase 3 randomized trial, known as KLASS-01, the mean number of retrieved lymph nodes was similar for the laparoscopic and open surgery groups, and there was no surgical margin involvement in any patient, investigators reported.
“We thus anticipated comparable long-term oncologic outcomes for overall and cancer-specific survival because these early outcomes indicated the oncologic safety of the laparoscopic procedure,” they said. Moreover, they said, earlier publications on the KLASS-01 study demonstrated that the laparoscopic approach was associated with less blood loss, fewer wound complications, and shorter hospital stays, compared with open distal gastrectomy.
In the current study, Dr. Kim and his coauthors reported that, with a median follow-up of about 100 months, the 5-year overall survival rate was 94.2% for the laparoscopic group and 93.3% for the open group (P = .64), while Similarly, the 5-year cancer-specific survival rates were 97.1% and 97.2% for the laparoscopic and open approach, respectively (P = .91), while recurrence was not significantly different at 5.6% and 4.8% (P = .49).
The investigators cited several limitations. One is that the investigators looked only at patients with stage I cancer “suitable for distal subtotal gastrectomy. Applying laparoscopic surgery for more advanced cancers and different operations, such as total gastrectomy, needs to be verified through other clinical trials,” they said.
Nevertheless, they wrote, “These long-term oncologic outcomes of [laparoscopy-assisted distal gastrectomy] support the adoption of this procedure as a standard treatment for clinical stage I gastric cancer.”
Dr. Kim and his coauthors reported no conflicts of interest related to the study, which was supported by a grant from the Ministry of Health & Welfare, Republic of Korea.
SOURCE: Kim HH et al. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6727.
When experienced surgeons are involved, laparoscopic distal gastrectomy is a safe alternative to open surgery in patients with early-stage gastric cancer, results of a randomized trial suggest.
Five-year overall survival exceeded 93% for both laparoscopic and open surgery groups in the multicenter trial, which included 1,416 patients with stage I gastric cancer treated by 15 surgeons who each had performed at least 100 gastrectomies.
Cancer-specific survival and recurrence were not significantly different between groups, while an intent-to-treat analysis confirmed the noninferiority of laparoscopic gastrectomy versus the open procedure, said investigators, led by Hyung-Ho Kim MD, PhD, of the Korean Laparoendoscopic Gastrointestinal Surgery Study (KLASS) group.
“Our trial supports the use of laparoscopic distal gastrectomy as a standard treatment option for clinical stage I distal gastric cancer when it can be performed by surgeons with sufficient experience,” Dr. Kim and his coauthors wrote in JAMA Oncology.
Some had doubted the oncologic safety of the laparoscopic approach because of the potential for inadequate lymphadenectomy leading to an increased risk of locoregional recurrence, said Dr. Kim and his coauthors in the KLASS group, “which includes 15 surgeons from 13 institutes.” However, among patients in this phase 3 randomized trial, known as KLASS-01, the mean number of retrieved lymph nodes was similar for the laparoscopic and open surgery groups, and there was no surgical margin involvement in any patient, investigators reported.
“We thus anticipated comparable long-term oncologic outcomes for overall and cancer-specific survival because these early outcomes indicated the oncologic safety of the laparoscopic procedure,” they said. Moreover, they said, earlier publications on the KLASS-01 study demonstrated that the laparoscopic approach was associated with less blood loss, fewer wound complications, and shorter hospital stays, compared with open distal gastrectomy.
In the current study, Dr. Kim and his coauthors reported that, with a median follow-up of about 100 months, the 5-year overall survival rate was 94.2% for the laparoscopic group and 93.3% for the open group (P = .64), while Similarly, the 5-year cancer-specific survival rates were 97.1% and 97.2% for the laparoscopic and open approach, respectively (P = .91), while recurrence was not significantly different at 5.6% and 4.8% (P = .49).
The investigators cited several limitations. One is that the investigators looked only at patients with stage I cancer “suitable for distal subtotal gastrectomy. Applying laparoscopic surgery for more advanced cancers and different operations, such as total gastrectomy, needs to be verified through other clinical trials,” they said.
Nevertheless, they wrote, “These long-term oncologic outcomes of [laparoscopy-assisted distal gastrectomy] support the adoption of this procedure as a standard treatment for clinical stage I gastric cancer.”
Dr. Kim and his coauthors reported no conflicts of interest related to the study, which was supported by a grant from the Ministry of Health & Welfare, Republic of Korea.
SOURCE: Kim HH et al. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6727.
When experienced surgeons are involved, laparoscopic distal gastrectomy is a safe alternative to open surgery in patients with early-stage gastric cancer, results of a randomized trial suggest.
Five-year overall survival exceeded 93% for both laparoscopic and open surgery groups in the multicenter trial, which included 1,416 patients with stage I gastric cancer treated by 15 surgeons who each had performed at least 100 gastrectomies.
Cancer-specific survival and recurrence were not significantly different between groups, while an intent-to-treat analysis confirmed the noninferiority of laparoscopic gastrectomy versus the open procedure, said investigators, led by Hyung-Ho Kim MD, PhD, of the Korean Laparoendoscopic Gastrointestinal Surgery Study (KLASS) group.
“Our trial supports the use of laparoscopic distal gastrectomy as a standard treatment option for clinical stage I distal gastric cancer when it can be performed by surgeons with sufficient experience,” Dr. Kim and his coauthors wrote in JAMA Oncology.
Some had doubted the oncologic safety of the laparoscopic approach because of the potential for inadequate lymphadenectomy leading to an increased risk of locoregional recurrence, said Dr. Kim and his coauthors in the KLASS group, “which includes 15 surgeons from 13 institutes.” However, among patients in this phase 3 randomized trial, known as KLASS-01, the mean number of retrieved lymph nodes was similar for the laparoscopic and open surgery groups, and there was no surgical margin involvement in any patient, investigators reported.
“We thus anticipated comparable long-term oncologic outcomes for overall and cancer-specific survival because these early outcomes indicated the oncologic safety of the laparoscopic procedure,” they said. Moreover, they said, earlier publications on the KLASS-01 study demonstrated that the laparoscopic approach was associated with less blood loss, fewer wound complications, and shorter hospital stays, compared with open distal gastrectomy.
In the current study, Dr. Kim and his coauthors reported that, with a median follow-up of about 100 months, the 5-year overall survival rate was 94.2% for the laparoscopic group and 93.3% for the open group (P = .64), while Similarly, the 5-year cancer-specific survival rates were 97.1% and 97.2% for the laparoscopic and open approach, respectively (P = .91), while recurrence was not significantly different at 5.6% and 4.8% (P = .49).
The investigators cited several limitations. One is that the investigators looked only at patients with stage I cancer “suitable for distal subtotal gastrectomy. Applying laparoscopic surgery for more advanced cancers and different operations, such as total gastrectomy, needs to be verified through other clinical trials,” they said.
Nevertheless, they wrote, “These long-term oncologic outcomes of [laparoscopy-assisted distal gastrectomy] support the adoption of this procedure as a standard treatment for clinical stage I gastric cancer.”
Dr. Kim and his coauthors reported no conflicts of interest related to the study, which was supported by a grant from the Ministry of Health & Welfare, Republic of Korea.
SOURCE: Kim HH et al. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6727.
FROM JAMA ONCOLOGY
Key clinical point: Laparoscopic distal gastrectomy performed by experienced surgeons is a safe alternative to open surgery in patient with early-stage gastric cancer.
Major finding: The 5-year overall survival rate was 94.2% for the laparoscopic group and 93.3% for the open group (P = .64).
Study details: The KLASS-01 trial, which included 1,416 patients with stage I gastric cancer treated by 15 experienced surgeons.
Disclosures: The coauthors reported no conflicts of interest related to the study, which was supported by a grant from the Ministry of Health &Welfare, Republic of Korea.
Source: Kim HH et al. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6727.
Checkpoint inhibitors ‘viable treatment option’ in HIV-infected individuals
Immune checkpoint inhibitors are safe and effective in HIV-infected patients with advanced cancers, according to authors of a recently published systematic review.
The treatment was well tolerated and associated with a 9% rate of grade 3 or higher immune-related adverse events, according to results of the review of 73 patient cases.
There were no adverse impacts on HIV load or CD4 cell count detected in the patients, according to researchers Michael R. Cook, MD, and Chul Kim, MD, MPH, of Georgetown University, Washington.
Antitumor activity of the checkpoint inhibitors in lung cancer patients was comparable to what has been seen in previous randomized clinical trials that excluded HIV-infected individuals, Dr. Cook and Dr. Kim reported in JAMA Oncology.
“Based on the results of the present systematic review, and in the absence of definitive prospective data suggesting an unfavorable risk-to-benefit ratio, immune checkpoint inhibitor therapy may be considered as a viable treatment option for HIV-infected patients with advanced cancer,” they said.
There are preclinical data suggesting that immune checkpoint modulation could improve function of HIV-specific T cells, the investigators added.
“Prospective trials of immune checkpoint inhibitors are necessary to elucidate the antiviral efficacy of immune checkpoint inhibitor therapy in patients with HIV infection and cancer,” they said.
Several such trials are underway to evaluate the role of the pembrolizumab, nivolumab, nivolumab plus ipilimumab, and durvalumab in HIV-infected patients with advanced-stage cancers, according to the review authors.
In the present systematic review, Dr. Cook and Dr. Kim conducted a literature search and reviewed presentations from major annual medical conferences.
Of the 73 HIV-infected patients they identified, most had non–small cell lung cancer (34.2%), melanoma (21.9%), or Kaposi sarcoma (12.3%), while the rest had anal cancer, head and neck cancer, or other malignancies. Most patients had received either nivolumab (39.7%) or pembrolizumab (35.6%).
There were “no concerning findings” among these patients with regard to immune-mediated toxicities or changes in HIV-related parameters.
Six of 70 patients had immune-related adverse events of grade 3 or greater.
Thirty-four patients had documented HIV loads before and after receiving an immune checkpoint inhibitor. Of those, 28 had undetectable HIV loads at baseline, and all but 2 (7%) maintained undetectable loads in the posttreatment evaluation.
Of the remaining six with detectable HIV loads before treatment, five had a decrease in viral load, to the point that four had undetectable HIV viral load in the posttreatment evaluation, the investigators reported.
The overall response rate was 30% for the lung cancer patients, 27% for melanoma, and 63% for Kaposi sarcoma.
In the non–small cell lung cancer subset, response rates were 26% for those who had received previous systemic treatment, and 50% for those who had not, which was similar to findings from major checkpoint inhibitor trials that excluded HIV-infected individuals, the investigators said.
The American Society of Clinical Oncology Conquer Cancer Foundation and Georgetown University supported the study. Dr. Kim reported disclosures related to CARIS Life Science and AstraZeneca.
SOURCE: Cook MR and Kim C. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6737.
Immune checkpoint inhibitors are safe and effective in HIV-infected patients with advanced cancers, according to authors of a recently published systematic review.
The treatment was well tolerated and associated with a 9% rate of grade 3 or higher immune-related adverse events, according to results of the review of 73 patient cases.
There were no adverse impacts on HIV load or CD4 cell count detected in the patients, according to researchers Michael R. Cook, MD, and Chul Kim, MD, MPH, of Georgetown University, Washington.
Antitumor activity of the checkpoint inhibitors in lung cancer patients was comparable to what has been seen in previous randomized clinical trials that excluded HIV-infected individuals, Dr. Cook and Dr. Kim reported in JAMA Oncology.
“Based on the results of the present systematic review, and in the absence of definitive prospective data suggesting an unfavorable risk-to-benefit ratio, immune checkpoint inhibitor therapy may be considered as a viable treatment option for HIV-infected patients with advanced cancer,” they said.
There are preclinical data suggesting that immune checkpoint modulation could improve function of HIV-specific T cells, the investigators added.
“Prospective trials of immune checkpoint inhibitors are necessary to elucidate the antiviral efficacy of immune checkpoint inhibitor therapy in patients with HIV infection and cancer,” they said.
Several such trials are underway to evaluate the role of the pembrolizumab, nivolumab, nivolumab plus ipilimumab, and durvalumab in HIV-infected patients with advanced-stage cancers, according to the review authors.
In the present systematic review, Dr. Cook and Dr. Kim conducted a literature search and reviewed presentations from major annual medical conferences.
Of the 73 HIV-infected patients they identified, most had non–small cell lung cancer (34.2%), melanoma (21.9%), or Kaposi sarcoma (12.3%), while the rest had anal cancer, head and neck cancer, or other malignancies. Most patients had received either nivolumab (39.7%) or pembrolizumab (35.6%).
There were “no concerning findings” among these patients with regard to immune-mediated toxicities or changes in HIV-related parameters.
Six of 70 patients had immune-related adverse events of grade 3 or greater.
Thirty-four patients had documented HIV loads before and after receiving an immune checkpoint inhibitor. Of those, 28 had undetectable HIV loads at baseline, and all but 2 (7%) maintained undetectable loads in the posttreatment evaluation.
Of the remaining six with detectable HIV loads before treatment, five had a decrease in viral load, to the point that four had undetectable HIV viral load in the posttreatment evaluation, the investigators reported.
The overall response rate was 30% for the lung cancer patients, 27% for melanoma, and 63% for Kaposi sarcoma.
In the non–small cell lung cancer subset, response rates were 26% for those who had received previous systemic treatment, and 50% for those who had not, which was similar to findings from major checkpoint inhibitor trials that excluded HIV-infected individuals, the investigators said.
The American Society of Clinical Oncology Conquer Cancer Foundation and Georgetown University supported the study. Dr. Kim reported disclosures related to CARIS Life Science and AstraZeneca.
SOURCE: Cook MR and Kim C. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6737.
Immune checkpoint inhibitors are safe and effective in HIV-infected patients with advanced cancers, according to authors of a recently published systematic review.
The treatment was well tolerated and associated with a 9% rate of grade 3 or higher immune-related adverse events, according to results of the review of 73 patient cases.
There were no adverse impacts on HIV load or CD4 cell count detected in the patients, according to researchers Michael R. Cook, MD, and Chul Kim, MD, MPH, of Georgetown University, Washington.
Antitumor activity of the checkpoint inhibitors in lung cancer patients was comparable to what has been seen in previous randomized clinical trials that excluded HIV-infected individuals, Dr. Cook and Dr. Kim reported in JAMA Oncology.
“Based on the results of the present systematic review, and in the absence of definitive prospective data suggesting an unfavorable risk-to-benefit ratio, immune checkpoint inhibitor therapy may be considered as a viable treatment option for HIV-infected patients with advanced cancer,” they said.
There are preclinical data suggesting that immune checkpoint modulation could improve function of HIV-specific T cells, the investigators added.
“Prospective trials of immune checkpoint inhibitors are necessary to elucidate the antiviral efficacy of immune checkpoint inhibitor therapy in patients with HIV infection and cancer,” they said.
Several such trials are underway to evaluate the role of the pembrolizumab, nivolumab, nivolumab plus ipilimumab, and durvalumab in HIV-infected patients with advanced-stage cancers, according to the review authors.
In the present systematic review, Dr. Cook and Dr. Kim conducted a literature search and reviewed presentations from major annual medical conferences.
Of the 73 HIV-infected patients they identified, most had non–small cell lung cancer (34.2%), melanoma (21.9%), or Kaposi sarcoma (12.3%), while the rest had anal cancer, head and neck cancer, or other malignancies. Most patients had received either nivolumab (39.7%) or pembrolizumab (35.6%).
There were “no concerning findings” among these patients with regard to immune-mediated toxicities or changes in HIV-related parameters.
Six of 70 patients had immune-related adverse events of grade 3 or greater.
Thirty-four patients had documented HIV loads before and after receiving an immune checkpoint inhibitor. Of those, 28 had undetectable HIV loads at baseline, and all but 2 (7%) maintained undetectable loads in the posttreatment evaluation.
Of the remaining six with detectable HIV loads before treatment, five had a decrease in viral load, to the point that four had undetectable HIV viral load in the posttreatment evaluation, the investigators reported.
The overall response rate was 30% for the lung cancer patients, 27% for melanoma, and 63% for Kaposi sarcoma.
In the non–small cell lung cancer subset, response rates were 26% for those who had received previous systemic treatment, and 50% for those who had not, which was similar to findings from major checkpoint inhibitor trials that excluded HIV-infected individuals, the investigators said.
The American Society of Clinical Oncology Conquer Cancer Foundation and Georgetown University supported the study. Dr. Kim reported disclosures related to CARIS Life Science and AstraZeneca.
SOURCE: Cook MR and Kim C. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6737.
FROM JAMA ONCOLOGY
Key clinical point: Immune checkpoint inhibitors are a viable treatment option for HIV-infected patients, according to data supporting their safety and efficacy in this patient population.
Major finding: The treatment was well tolerated, with an 8.6% rate of grade 3 or greater immune-related adverse events, and no impact on HIV-related parameters.
Study details: A systematic review of 73 patients with HIV infection who had received treatment with a checkpoint inhibitor.
Disclosures: The American Society of Clinical Oncology Conquer Cancer Foundation and Georgetown University supported the study. One study author reported disclosures related to CARIS Life Science and AstraZeneca.
Source: Cook MR and Kim C. JAMA Oncol. 2019 Feb 7. doi: 10.1001/jamaoncol.2018.6737.
Different disease features found with family history of psoriasis versus PsA
the results of a retrospective cohort study suggest.
A family history of psoriasis was associated with younger onset of psoriatic disease and the presence of enthesitis, while by contrast, a family history of psoriatic arthritis (PsA) was associated with lower risk of plaque psoriasis and higher risk of deformities, according to Dilek Solmaz, MD, of the University of Ottawa and her coauthors, who reported their findings in Arthritis Care & Research.
“The link between family history of psoriasis/psoriatic arthritis and pustular/plaque phenotypes may point to a different genetic background and pathogenic mechanisms in these subsets,” the investigators wrote.
Most, if not all, previous studies evaluating family history have grouped psoriasis and PsA together, according to Dr. Solmaz and her colleagues, rather than looking at the individual effects of psoriasis or PsA family history that may lead to unique disease phenotypes, as was done in the present study.
The investigators based their retrospective analysis on patients recruited in a longitudinal, multicenter database in Turkey and Canada. The mean age of patients in the study was 48 years; nearly 65% were female.
Out of 1,393 patients in the database, 444 had a family history of psoriasis or PsA. That included 335 patients with a psoriasis-only family history and 74 with a family history of PsA; another 35 patients weren’t sure about having a family history of PsA or psoriasis and were left out of the analysis.
Plaque psoriasis was more common in individuals with a family history of only psoriasis, while pustular psoriasis was more common in those with a PsA family history, the investigators reported.
In multivariate analyses, having a family member with psoriasis was a risk factor for younger age of psoriasis onset (odds ratio, 0.976; 95% confidence interval, 0.964-0.989; P less than .001) as well as a higher risk for enthesitis (OR, 1.931; 95% CI, 1.276-2.922; P = .002) when compared against patients without a family history of psoriasis.
Patients with a family history of PsA were more likely to have deformities (OR, 2.557; 95% CI, 1.250-5.234; P less than .010) and lower risk of plaque-type psoriasis (OR, 0.417; 95% CI, 0.213-0.816; P less than .011) than patients without a family history of PsA.
Disease onset was earlier among patients with a family history of psoriasis at a mean of 28.1 years versus 31.9 years for those with a family history of PsA (P less than .001).
Dr. Solmaz and her colleagues reported no conflicts of interest related to the research, which was supported in part by the Turkish Society for Rheumatology, the Scientific and Technological Research Council of Turkey, and Union Chimique Belge.
SOURCE: Solmaz D et al. Arthritis Care Res (Hoboken). 2019 Jan 25. doi: 10.1002/acr.23836.
the results of a retrospective cohort study suggest.
A family history of psoriasis was associated with younger onset of psoriatic disease and the presence of enthesitis, while by contrast, a family history of psoriatic arthritis (PsA) was associated with lower risk of plaque psoriasis and higher risk of deformities, according to Dilek Solmaz, MD, of the University of Ottawa and her coauthors, who reported their findings in Arthritis Care & Research.
“The link between family history of psoriasis/psoriatic arthritis and pustular/plaque phenotypes may point to a different genetic background and pathogenic mechanisms in these subsets,” the investigators wrote.
Most, if not all, previous studies evaluating family history have grouped psoriasis and PsA together, according to Dr. Solmaz and her colleagues, rather than looking at the individual effects of psoriasis or PsA family history that may lead to unique disease phenotypes, as was done in the present study.
The investigators based their retrospective analysis on patients recruited in a longitudinal, multicenter database in Turkey and Canada. The mean age of patients in the study was 48 years; nearly 65% were female.
Out of 1,393 patients in the database, 444 had a family history of psoriasis or PsA. That included 335 patients with a psoriasis-only family history and 74 with a family history of PsA; another 35 patients weren’t sure about having a family history of PsA or psoriasis and were left out of the analysis.
Plaque psoriasis was more common in individuals with a family history of only psoriasis, while pustular psoriasis was more common in those with a PsA family history, the investigators reported.
In multivariate analyses, having a family member with psoriasis was a risk factor for younger age of psoriasis onset (odds ratio, 0.976; 95% confidence interval, 0.964-0.989; P less than .001) as well as a higher risk for enthesitis (OR, 1.931; 95% CI, 1.276-2.922; P = .002) when compared against patients without a family history of psoriasis.
Patients with a family history of PsA were more likely to have deformities (OR, 2.557; 95% CI, 1.250-5.234; P less than .010) and lower risk of plaque-type psoriasis (OR, 0.417; 95% CI, 0.213-0.816; P less than .011) than patients without a family history of PsA.
Disease onset was earlier among patients with a family history of psoriasis at a mean of 28.1 years versus 31.9 years for those with a family history of PsA (P less than .001).
Dr. Solmaz and her colleagues reported no conflicts of interest related to the research, which was supported in part by the Turkish Society for Rheumatology, the Scientific and Technological Research Council of Turkey, and Union Chimique Belge.
SOURCE: Solmaz D et al. Arthritis Care Res (Hoboken). 2019 Jan 25. doi: 10.1002/acr.23836.
the results of a retrospective cohort study suggest.
A family history of psoriasis was associated with younger onset of psoriatic disease and the presence of enthesitis, while by contrast, a family history of psoriatic arthritis (PsA) was associated with lower risk of plaque psoriasis and higher risk of deformities, according to Dilek Solmaz, MD, of the University of Ottawa and her coauthors, who reported their findings in Arthritis Care & Research.
“The link between family history of psoriasis/psoriatic arthritis and pustular/plaque phenotypes may point to a different genetic background and pathogenic mechanisms in these subsets,” the investigators wrote.
Most, if not all, previous studies evaluating family history have grouped psoriasis and PsA together, according to Dr. Solmaz and her colleagues, rather than looking at the individual effects of psoriasis or PsA family history that may lead to unique disease phenotypes, as was done in the present study.
The investigators based their retrospective analysis on patients recruited in a longitudinal, multicenter database in Turkey and Canada. The mean age of patients in the study was 48 years; nearly 65% were female.
Out of 1,393 patients in the database, 444 had a family history of psoriasis or PsA. That included 335 patients with a psoriasis-only family history and 74 with a family history of PsA; another 35 patients weren’t sure about having a family history of PsA or psoriasis and were left out of the analysis.
Plaque psoriasis was more common in individuals with a family history of only psoriasis, while pustular psoriasis was more common in those with a PsA family history, the investigators reported.
In multivariate analyses, having a family member with psoriasis was a risk factor for younger age of psoriasis onset (odds ratio, 0.976; 95% confidence interval, 0.964-0.989; P less than .001) as well as a higher risk for enthesitis (OR, 1.931; 95% CI, 1.276-2.922; P = .002) when compared against patients without a family history of psoriasis.
Patients with a family history of PsA were more likely to have deformities (OR, 2.557; 95% CI, 1.250-5.234; P less than .010) and lower risk of plaque-type psoriasis (OR, 0.417; 95% CI, 0.213-0.816; P less than .011) than patients without a family history of PsA.
Disease onset was earlier among patients with a family history of psoriasis at a mean of 28.1 years versus 31.9 years for those with a family history of PsA (P less than .001).
Dr. Solmaz and her colleagues reported no conflicts of interest related to the research, which was supported in part by the Turkish Society for Rheumatology, the Scientific and Technological Research Council of Turkey, and Union Chimique Belge.
SOURCE: Solmaz D et al. Arthritis Care Res (Hoboken). 2019 Jan 25. doi: 10.1002/acr.23836.
FROM ARTHRITIS CARE & RESEARCH
Key clinical point: Family histories of psoriasis and psoriatic arthritis were linked to different skin phenotypes, disease severity, and musculoskeletal features.
Major finding: Compared with no family history, psoriasis family history was a risk factor for enthesitis (odds ratio, 1.931) and younger age of onset (OR, 0.976) while psoriatic arthritis family history was linked to higher risk of deformities (OR, 2.557) and lower risk of plaque-type psoriasis (OR, 0.417).
Study details: A retrospective analysis including 1,393 Turkish or Canadian patients enrolled in a psoriatic arthritis database.
Disclosures: The study authors reported no conflicts of interest related to the research, which was supported in part by the Turkish Society for Rheumatology, the Scientific and Technological Research Council of Turkey, and Union Chimique Belge.
Source: Solmaz D et al. Arthritis Care Res (Hoboken). 2019 Jan 25. doi: 10.1002/acr.23836.
Liver resection outcomes similar for robotic and open surgery
according to researchers who conducted a recent multi-institutional analysis.
The proportion of margin-negative resections was 92% in a series of 59 patients who underwent resection at one of three tertiary hospitals, the study authors reported.
The 3-year disease-free survival and overall survival rates were 41.9% and 66%, respectively, in the 44 patients for whom longer-term follow-up was available, according to the investigators, led by Francesco Guerra, MD, of Ospedali Riuniti Marche Nord Hospital in Pesaro, Italy.
“These findings are consistent with those of patients resected via conventional laparoscopy or open surgery in contemporary series,” Dr. Guerra and his coauthors wrote in a report published in Surgical Oncology.
It’s still a matter of debate, however, whether robotic surgery has clear advantages over conventional laparoscopy for liver surgery, according to the investigators. Direct comparisons of robotic versus conventional laparoscopic liver resection are scarce, with most available data stemming from often heterogeneous case-control series with no long-term oncologic outcome data.
“Most centers have consolidated experience either in laparoscopic or in robotic liver resection,” the authors wrote. “Hence, reliable comparative analyses are likely difficult to carry out.”
Because of the scarcity of results, Dr. Guerra and his colleagues sought to investigate short- and long-term outcomes for a consecutive series of 59 patients who underwent minimally invasive, ultrasound-guided robotic surgery between 2008 and 2018 at one of three tertiary facilities. Each procedure had been performed by surgeons experienced in both liver surgery and robotics. The median age of patients undergoing the procedure was 64 years, 63% were male, and the median body mass index was 26 kg/m2.
Almost half the patients (46%) had multiple lesions removed, while about one-quarter had concomitant procedures, mainly cholecystectomy, according to the report.
Robotic surgeries were converted to open procedures in seven patients, or about 12%, a statistic comparable with other reports of laparoscopic or robotic surgery, the investigators noted.
Postoperative complications were seen in 16 patients, or 27%. That included 13 patients with class I-II complications and 3 patients with class III-IV complications, including 2 cases of heart failure and 1 case of postoperative bile leak requiring radiologic and endoscopic therapy.
The reported 3-year disease-free and overall survival of 41.9% and 66.1% was based on a mean follow-up of 19.5 months in 44 patients for whom longer-term data were available. There were 16 cases of recurrent disease, including 10 patients with evidence of liver recurrence.
“Taken together, our data show that robotics is an effective option to resect colorectal liver metastases, providing an oncological outcome similar to that of laparoscopy and open surgery,” the investigators wrote.
Dr. Guerra and colleagues reported no disclosures related to their research.
SOURCE: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
according to researchers who conducted a recent multi-institutional analysis.
The proportion of margin-negative resections was 92% in a series of 59 patients who underwent resection at one of three tertiary hospitals, the study authors reported.
The 3-year disease-free survival and overall survival rates were 41.9% and 66%, respectively, in the 44 patients for whom longer-term follow-up was available, according to the investigators, led by Francesco Guerra, MD, of Ospedali Riuniti Marche Nord Hospital in Pesaro, Italy.
“These findings are consistent with those of patients resected via conventional laparoscopy or open surgery in contemporary series,” Dr. Guerra and his coauthors wrote in a report published in Surgical Oncology.
It’s still a matter of debate, however, whether robotic surgery has clear advantages over conventional laparoscopy for liver surgery, according to the investigators. Direct comparisons of robotic versus conventional laparoscopic liver resection are scarce, with most available data stemming from often heterogeneous case-control series with no long-term oncologic outcome data.
“Most centers have consolidated experience either in laparoscopic or in robotic liver resection,” the authors wrote. “Hence, reliable comparative analyses are likely difficult to carry out.”
Because of the scarcity of results, Dr. Guerra and his colleagues sought to investigate short- and long-term outcomes for a consecutive series of 59 patients who underwent minimally invasive, ultrasound-guided robotic surgery between 2008 and 2018 at one of three tertiary facilities. Each procedure had been performed by surgeons experienced in both liver surgery and robotics. The median age of patients undergoing the procedure was 64 years, 63% were male, and the median body mass index was 26 kg/m2.
Almost half the patients (46%) had multiple lesions removed, while about one-quarter had concomitant procedures, mainly cholecystectomy, according to the report.
Robotic surgeries were converted to open procedures in seven patients, or about 12%, a statistic comparable with other reports of laparoscopic or robotic surgery, the investigators noted.
Postoperative complications were seen in 16 patients, or 27%. That included 13 patients with class I-II complications and 3 patients with class III-IV complications, including 2 cases of heart failure and 1 case of postoperative bile leak requiring radiologic and endoscopic therapy.
The reported 3-year disease-free and overall survival of 41.9% and 66.1% was based on a mean follow-up of 19.5 months in 44 patients for whom longer-term data were available. There were 16 cases of recurrent disease, including 10 patients with evidence of liver recurrence.
“Taken together, our data show that robotics is an effective option to resect colorectal liver metastases, providing an oncological outcome similar to that of laparoscopy and open surgery,” the investigators wrote.
Dr. Guerra and colleagues reported no disclosures related to their research.
SOURCE: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
according to researchers who conducted a recent multi-institutional analysis.
The proportion of margin-negative resections was 92% in a series of 59 patients who underwent resection at one of three tertiary hospitals, the study authors reported.
The 3-year disease-free survival and overall survival rates were 41.9% and 66%, respectively, in the 44 patients for whom longer-term follow-up was available, according to the investigators, led by Francesco Guerra, MD, of Ospedali Riuniti Marche Nord Hospital in Pesaro, Italy.
“These findings are consistent with those of patients resected via conventional laparoscopy or open surgery in contemporary series,” Dr. Guerra and his coauthors wrote in a report published in Surgical Oncology.
It’s still a matter of debate, however, whether robotic surgery has clear advantages over conventional laparoscopy for liver surgery, according to the investigators. Direct comparisons of robotic versus conventional laparoscopic liver resection are scarce, with most available data stemming from often heterogeneous case-control series with no long-term oncologic outcome data.
“Most centers have consolidated experience either in laparoscopic or in robotic liver resection,” the authors wrote. “Hence, reliable comparative analyses are likely difficult to carry out.”
Because of the scarcity of results, Dr. Guerra and his colleagues sought to investigate short- and long-term outcomes for a consecutive series of 59 patients who underwent minimally invasive, ultrasound-guided robotic surgery between 2008 and 2018 at one of three tertiary facilities. Each procedure had been performed by surgeons experienced in both liver surgery and robotics. The median age of patients undergoing the procedure was 64 years, 63% were male, and the median body mass index was 26 kg/m2.
Almost half the patients (46%) had multiple lesions removed, while about one-quarter had concomitant procedures, mainly cholecystectomy, according to the report.
Robotic surgeries were converted to open procedures in seven patients, or about 12%, a statistic comparable with other reports of laparoscopic or robotic surgery, the investigators noted.
Postoperative complications were seen in 16 patients, or 27%. That included 13 patients with class I-II complications and 3 patients with class III-IV complications, including 2 cases of heart failure and 1 case of postoperative bile leak requiring radiologic and endoscopic therapy.
The reported 3-year disease-free and overall survival of 41.9% and 66.1% was based on a mean follow-up of 19.5 months in 44 patients for whom longer-term data were available. There were 16 cases of recurrent disease, including 10 patients with evidence of liver recurrence.
“Taken together, our data show that robotics is an effective option to resect colorectal liver metastases, providing an oncological outcome similar to that of laparoscopy and open surgery,” the investigators wrote.
Dr. Guerra and colleagues reported no disclosures related to their research.
SOURCE: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
FROM SURGICAL ONCOLOGY
Key clinical point: Outcomes for robotic surgery for colorectal liver metastases are not inferior to laparoscopic and open surgical approaches.
Major finding: Negative margins were achieved in 92% of lesions, while 3-year disease-free and overall survival were 41.9% and 66.1%, respectively.
Study details: An analysis of 59 patients undergoing robotic surgery for colorectal liver metastases at one of three institutions between 2008 and 2018.
Disclosures: The study authors reported no disclosures.
Source: Guerra F et al. Surg Oncol. 2018 Nov 1. doi: 10.1016/j.suronc.2018.10.011.
AHA report highlights CVD burden, declines in smoking, sleep importance
Almost half of U.S. adults now have some form of cardiovascular disease, according to the latest annual statistical update from the American Heart Association.
The prevalence is driven in part by the recently changed definition of hypertension, from 140/90 to 130/80 mm Hg, said authors of the American Heart Association Heart Disease and Stroke Statistics–2019 Update.
Cardiovascular disease (CVD) deaths are up, though smoking rates continue to decline, and adults are getting more exercise (Circulation. 2019;139. doi: 10.1161/CIR.0000000000000659).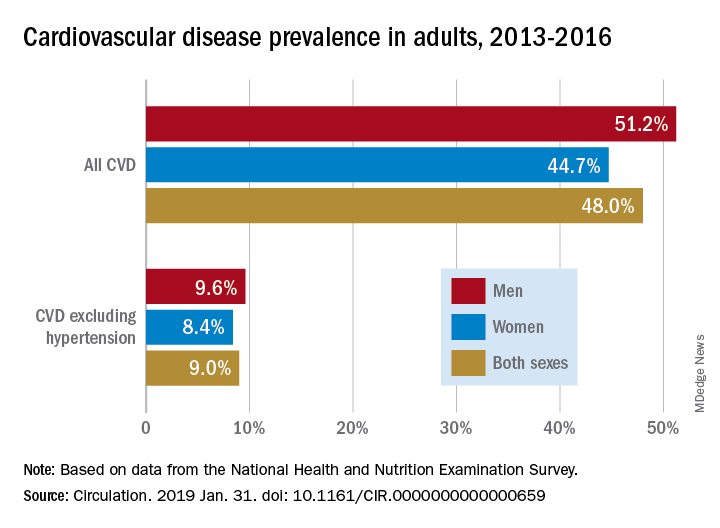
The update includes a new section on sleep and cardiovascular health, an enhanced focus on social determinants of health, and further evidence-based approaches to behavior change, according to the update’s authors, led by chair Emelia J. Benjamin, MD, professor of medicine and epidemiology at Boston University, and vice chair Paul Muntner, PhD, professor of epidemiology at the University of Alabama, Birmingham.
High blood pressure is an “overwhelming presence” that drives heart disease and stroke and can’t be dismissed in the fight against cardiovascular disease, AHA President Ivor J. Benjamin, MD, said in a statement. “Eliminating high blood pressure could have a larger impact on CVD deaths than the elimination of all other risk factors among women, and all except smoking among men.”
Using data from 2013 to 2016, 46% of adults in the United States had hypertension, and in 2016 there were 82,735 deaths attributable primarily to high blood pressure, according to the update.
Total direct costs of hypertension could approach $221 billion by 2035, according to projections in the report.
After decades of decline, U.S. cardiovascular disease deaths increased to 840,678 in 2016, up from 836,546 in 2015, the report says.
Smoking rate declines represent some of the most significant improvements outlined in the report, according to an AHA news release.
Ninety-four percent of adolescents were nonsmokers in the 2015-2016 period, which is up from 76% in 1999-2000, according to the report. The proportion of adult nonsmokers increased to 79% in 2015-2016, up from 73% in 1999-2000.
The new chapter on the importance of sleep cites data from the Centers for Disease Control and Prevention that only 65.2% of Americans have a healthy sleep duration (at least 7 hours), with even lower rates among non-Hispanic blacks, native Hawaiians and Pacific Islanders, and multiracial non-Hispanic individuals.
Short sleep duration is associated with a higher risk of all-cause mortality, total CVD, and coronary heart disease, according to a meta-analysis cited in the report. Long sleep duration, defined as greater than 8 hours, also was associated with higher risk of all-cause mortality, total CVD, coronary heart disease, and stroke.
Members of the statistical update writing group reported disclosures related to the American Heart Association, National Institutes of Health, Amgen, Sanofi, Roche, Abbott, Biogen, Medtronic, and others.
SOURCE: Benjamin EJ et al. Circulation. 2019 Jan 31.
The latest statistics on heart disease and stroke include some metrics that indicate progress, and others that suggest opportunities for improvement.
Tobacco use continues to decline; however, among high school students, e-cigarette use is up to 11.3%, which is concerning.
One bright spot is that the proportion of inactive adults has dropped to 30% in 2016, down from 40% in 2007. Despite that improvement, however, the prevalence of obesity increased significantly over the decade, to the point where nearly 40% of adults are obese and 7.7% are severely obese.
Although 48% of U.S. adults now have cardiovascular disease, according to this latest update, the number drops to just 9% when hypertension is excluded. Even so, 9% represents more than 24.3 million Americans who have coronary artery disease, stroke, or heart failure.
The cost of cardiovascular disease is astronomical, exceeding $351 billion in 2014-1205, with costs projected to increase sharply for older adults over the next few decades.
Starting in 2020, the AHA will begin charting progress in CVD using a metric called health-adjusted life expectancy (HALE), which relies on morbidity and mortality patterns to reflect the number of years a person can expect to live. Patients and the general public may find this metric more understandable than statistics about death rates and cardiovascular risk factors.
Mariell Jessup, MD, is chief science and medical officer for the American Heart Association. Her view on the latest statistical update was derived from a commentary that accompanied the update.
The latest statistics on heart disease and stroke include some metrics that indicate progress, and others that suggest opportunities for improvement.
Tobacco use continues to decline; however, among high school students, e-cigarette use is up to 11.3%, which is concerning.
One bright spot is that the proportion of inactive adults has dropped to 30% in 2016, down from 40% in 2007. Despite that improvement, however, the prevalence of obesity increased significantly over the decade, to the point where nearly 40% of adults are obese and 7.7% are severely obese.
Although 48% of U.S. adults now have cardiovascular disease, according to this latest update, the number drops to just 9% when hypertension is excluded. Even so, 9% represents more than 24.3 million Americans who have coronary artery disease, stroke, or heart failure.
The cost of cardiovascular disease is astronomical, exceeding $351 billion in 2014-1205, with costs projected to increase sharply for older adults over the next few decades.
Starting in 2020, the AHA will begin charting progress in CVD using a metric called health-adjusted life expectancy (HALE), which relies on morbidity and mortality patterns to reflect the number of years a person can expect to live. Patients and the general public may find this metric more understandable than statistics about death rates and cardiovascular risk factors.
Mariell Jessup, MD, is chief science and medical officer for the American Heart Association. Her view on the latest statistical update was derived from a commentary that accompanied the update.
The latest statistics on heart disease and stroke include some metrics that indicate progress, and others that suggest opportunities for improvement.
Tobacco use continues to decline; however, among high school students, e-cigarette use is up to 11.3%, which is concerning.
One bright spot is that the proportion of inactive adults has dropped to 30% in 2016, down from 40% in 2007. Despite that improvement, however, the prevalence of obesity increased significantly over the decade, to the point where nearly 40% of adults are obese and 7.7% are severely obese.
Although 48% of U.S. adults now have cardiovascular disease, according to this latest update, the number drops to just 9% when hypertension is excluded. Even so, 9% represents more than 24.3 million Americans who have coronary artery disease, stroke, or heart failure.
The cost of cardiovascular disease is astronomical, exceeding $351 billion in 2014-1205, with costs projected to increase sharply for older adults over the next few decades.
Starting in 2020, the AHA will begin charting progress in CVD using a metric called health-adjusted life expectancy (HALE), which relies on morbidity and mortality patterns to reflect the number of years a person can expect to live. Patients and the general public may find this metric more understandable than statistics about death rates and cardiovascular risk factors.
Mariell Jessup, MD, is chief science and medical officer for the American Heart Association. Her view on the latest statistical update was derived from a commentary that accompanied the update.
Almost half of U.S. adults now have some form of cardiovascular disease, according to the latest annual statistical update from the American Heart Association.
The prevalence is driven in part by the recently changed definition of hypertension, from 140/90 to 130/80 mm Hg, said authors of the American Heart Association Heart Disease and Stroke Statistics–2019 Update.
Cardiovascular disease (CVD) deaths are up, though smoking rates continue to decline, and adults are getting more exercise (Circulation. 2019;139. doi: 10.1161/CIR.0000000000000659).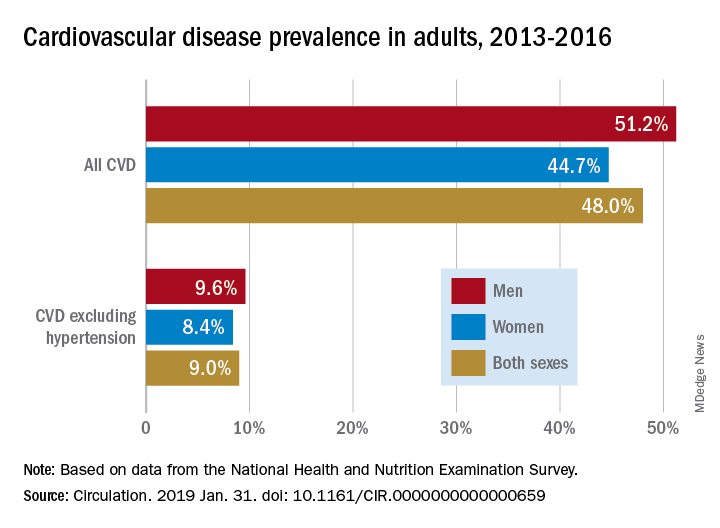
The update includes a new section on sleep and cardiovascular health, an enhanced focus on social determinants of health, and further evidence-based approaches to behavior change, according to the update’s authors, led by chair Emelia J. Benjamin, MD, professor of medicine and epidemiology at Boston University, and vice chair Paul Muntner, PhD, professor of epidemiology at the University of Alabama, Birmingham.
High blood pressure is an “overwhelming presence” that drives heart disease and stroke and can’t be dismissed in the fight against cardiovascular disease, AHA President Ivor J. Benjamin, MD, said in a statement. “Eliminating high blood pressure could have a larger impact on CVD deaths than the elimination of all other risk factors among women, and all except smoking among men.”
Using data from 2013 to 2016, 46% of adults in the United States had hypertension, and in 2016 there were 82,735 deaths attributable primarily to high blood pressure, according to the update.
Total direct costs of hypertension could approach $221 billion by 2035, according to projections in the report.
After decades of decline, U.S. cardiovascular disease deaths increased to 840,678 in 2016, up from 836,546 in 2015, the report says.
Smoking rate declines represent some of the most significant improvements outlined in the report, according to an AHA news release.
Ninety-four percent of adolescents were nonsmokers in the 2015-2016 period, which is up from 76% in 1999-2000, according to the report. The proportion of adult nonsmokers increased to 79% in 2015-2016, up from 73% in 1999-2000.
The new chapter on the importance of sleep cites data from the Centers for Disease Control and Prevention that only 65.2% of Americans have a healthy sleep duration (at least 7 hours), with even lower rates among non-Hispanic blacks, native Hawaiians and Pacific Islanders, and multiracial non-Hispanic individuals.
Short sleep duration is associated with a higher risk of all-cause mortality, total CVD, and coronary heart disease, according to a meta-analysis cited in the report. Long sleep duration, defined as greater than 8 hours, also was associated with higher risk of all-cause mortality, total CVD, coronary heart disease, and stroke.
Members of the statistical update writing group reported disclosures related to the American Heart Association, National Institutes of Health, Amgen, Sanofi, Roche, Abbott, Biogen, Medtronic, and others.
SOURCE: Benjamin EJ et al. Circulation. 2019 Jan 31.
Almost half of U.S. adults now have some form of cardiovascular disease, according to the latest annual statistical update from the American Heart Association.
The prevalence is driven in part by the recently changed definition of hypertension, from 140/90 to 130/80 mm Hg, said authors of the American Heart Association Heart Disease and Stroke Statistics–2019 Update.
Cardiovascular disease (CVD) deaths are up, though smoking rates continue to decline, and adults are getting more exercise (Circulation. 2019;139. doi: 10.1161/CIR.0000000000000659).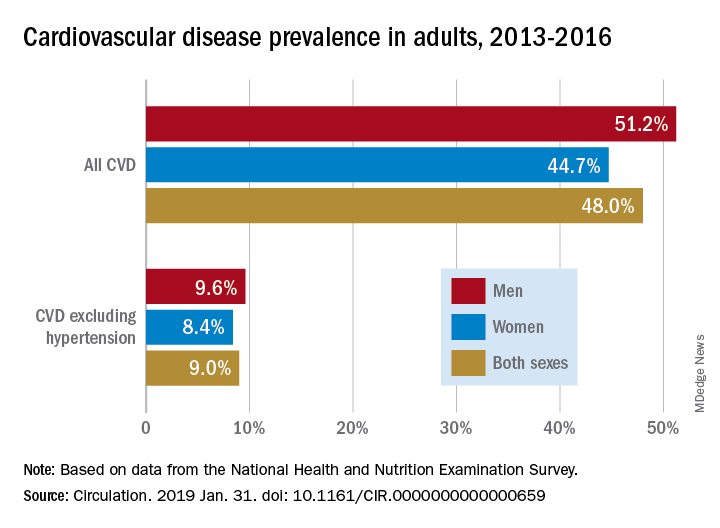
The update includes a new section on sleep and cardiovascular health, an enhanced focus on social determinants of health, and further evidence-based approaches to behavior change, according to the update’s authors, led by chair Emelia J. Benjamin, MD, professor of medicine and epidemiology at Boston University, and vice chair Paul Muntner, PhD, professor of epidemiology at the University of Alabama, Birmingham.
High blood pressure is an “overwhelming presence” that drives heart disease and stroke and can’t be dismissed in the fight against cardiovascular disease, AHA President Ivor J. Benjamin, MD, said in a statement. “Eliminating high blood pressure could have a larger impact on CVD deaths than the elimination of all other risk factors among women, and all except smoking among men.”
Using data from 2013 to 2016, 46% of adults in the United States had hypertension, and in 2016 there were 82,735 deaths attributable primarily to high blood pressure, according to the update.
Total direct costs of hypertension could approach $221 billion by 2035, according to projections in the report.
After decades of decline, U.S. cardiovascular disease deaths increased to 840,678 in 2016, up from 836,546 in 2015, the report says.
Smoking rate declines represent some of the most significant improvements outlined in the report, according to an AHA news release.
Ninety-four percent of adolescents were nonsmokers in the 2015-2016 period, which is up from 76% in 1999-2000, according to the report. The proportion of adult nonsmokers increased to 79% in 2015-2016, up from 73% in 1999-2000.
The new chapter on the importance of sleep cites data from the Centers for Disease Control and Prevention that only 65.2% of Americans have a healthy sleep duration (at least 7 hours), with even lower rates among non-Hispanic blacks, native Hawaiians and Pacific Islanders, and multiracial non-Hispanic individuals.
Short sleep duration is associated with a higher risk of all-cause mortality, total CVD, and coronary heart disease, according to a meta-analysis cited in the report. Long sleep duration, defined as greater than 8 hours, also was associated with higher risk of all-cause mortality, total CVD, coronary heart disease, and stroke.
Members of the statistical update writing group reported disclosures related to the American Heart Association, National Institutes of Health, Amgen, Sanofi, Roche, Abbott, Biogen, Medtronic, and others.
SOURCE: Benjamin EJ et al. Circulation. 2019 Jan 31.
FROM CIRCULATION
Elevated CAC not linked to increased death risk in physically active men
In highly active individuals, high levels of coronary artery calcification do not appear to confer an elevated mortality risk, a large, observational study suggests.
There was an increased risk of elevated levels of coronary artery calcification (CAC) in men with levels of exercise training comparable with that seen in master marathon runners, the study authors reported. However, elevated CAC in highly active men didn’t translate into a significant increase in all-cause or cardiovascular disease mortality risk in the study.
That result is contrary to the hypothesis that high activity levels would increase mortality risk in individuals with CAC, according to senior author Benjamin D. Levine, MD, of Texas Health Presbyterian Hospital in Dallas, and his coauthors.
“Our findings should reassure patients and their health care professionals that it appears these highly active individuals can safely continue their exercise programs,” Dr. Levine and his coauthors wrote in JAMA Cardiology.
The present analysis focused on 21,758 generally healthy men without prevalent cardiovascular disease. They were enrolled in the Cooper Center Longitudinal Study, a prospective, longitudinal study designed to assess linkages between physical activity, cardiorespiratory fitness, and health. The mean age of these men was 52 years at baseline; the mean duration of follow-up was 10.4 years.
Out of 21,758 male participants, 1,561 reported very high levels of physical activity, or at least 3,000 metabolic equivalent of task (MET) minutes per week, while 3,750 reported 1,500-2,999 MET minutes per week, and 16,477 reported low levels of physical activity, or less than 1,500 MET minutes per week.
The adjusted risk of elevated CAC, defined as at least 100 Agatston units, was 11% higher in the individuals reporting very high physical activity levels, the investigators found.
Presence of elevated CAC nearly doubled the risk of death in men with low levels of exercise, with a hazard ratio of 1.93 (95% confidence interval, 1.34-2.78), the investigators found. By contrast, there was no significant increase in all-cause mortality in the most active group (HR, 0.77; 95% CI, 0.52-1.15).
Taken together, these findings seem to provide evidence that high activity levels do not increase mortality risk, the investigators wrote, noting that the study is believed to have the “best available” mortality data in a large CAC population that includes measurement of physical activity.
The research was supported in partly through the National Space Biomedical Research Institute. One study author reported disclosures related to Abbott, AstraZeneca, and the American Heart Association.
SOURCE: Levine BD et al. JAMA Cardiol. 2019 Jan 30. doi: 10.1001/jamacardio.2018.4628.
This major study shows that, for most high-volume exercisers, very high doses of running and exercise can be performed, even among those with “hearts of stone,” wrote authors of an invited commentary.
A more novel finding, however, was that men with CAC in the highest physical activity group had lower mortality risk, compared with men without CAC who reported low levels of activity, the commentary authors wrote.
“One may speculate whether there are similarities with high-intensity statin therapy, because high-intensity physical activity and exercise may promote more calcific atherosclerosis, which may be more stable than soft, noncalcified plaques, potentially leading to coronary stability and lower propensity to more morbid CVD [cardiovascular disease] events,” the authors wrote.
Even so, CAC testing appears to “retain its utility” in high-volume exercisers, they added. “High CAC scores were still associated with higher risk at any given physical activity level in this study, which is why CAC assessment is being promoted to help risk assessment and intensify preventive therapies, such as vigorous lipid treatment.”
Dr. Lavie is with the John Ochsner Heart and Vascular Institute in New Orleans; Dr. Wisløff is with the Norwegian University of Science and Technology, Trondheim; Dr. Blumenthal is director of the Ciccarone Center for the Prevention of Cardiovascular Disease at John Hopkins Hospital, Baltimore. Their invited commentary appears in JAMA Cardiology. Authors reported conflict of interest with Mio Global Canada (Dr. Lavie) and PAI Health (Dr. Wisloff).
This major study shows that, for most high-volume exercisers, very high doses of running and exercise can be performed, even among those with “hearts of stone,” wrote authors of an invited commentary.
A more novel finding, however, was that men with CAC in the highest physical activity group had lower mortality risk, compared with men without CAC who reported low levels of activity, the commentary authors wrote.
“One may speculate whether there are similarities with high-intensity statin therapy, because high-intensity physical activity and exercise may promote more calcific atherosclerosis, which may be more stable than soft, noncalcified plaques, potentially leading to coronary stability and lower propensity to more morbid CVD [cardiovascular disease] events,” the authors wrote.
Even so, CAC testing appears to “retain its utility” in high-volume exercisers, they added. “High CAC scores were still associated with higher risk at any given physical activity level in this study, which is why CAC assessment is being promoted to help risk assessment and intensify preventive therapies, such as vigorous lipid treatment.”
Dr. Lavie is with the John Ochsner Heart and Vascular Institute in New Orleans; Dr. Wisløff is with the Norwegian University of Science and Technology, Trondheim; Dr. Blumenthal is director of the Ciccarone Center for the Prevention of Cardiovascular Disease at John Hopkins Hospital, Baltimore. Their invited commentary appears in JAMA Cardiology. Authors reported conflict of interest with Mio Global Canada (Dr. Lavie) and PAI Health (Dr. Wisloff).
This major study shows that, for most high-volume exercisers, very high doses of running and exercise can be performed, even among those with “hearts of stone,” wrote authors of an invited commentary.
A more novel finding, however, was that men with CAC in the highest physical activity group had lower mortality risk, compared with men without CAC who reported low levels of activity, the commentary authors wrote.
“One may speculate whether there are similarities with high-intensity statin therapy, because high-intensity physical activity and exercise may promote more calcific atherosclerosis, which may be more stable than soft, noncalcified plaques, potentially leading to coronary stability and lower propensity to more morbid CVD [cardiovascular disease] events,” the authors wrote.
Even so, CAC testing appears to “retain its utility” in high-volume exercisers, they added. “High CAC scores were still associated with higher risk at any given physical activity level in this study, which is why CAC assessment is being promoted to help risk assessment and intensify preventive therapies, such as vigorous lipid treatment.”
Dr. Lavie is with the John Ochsner Heart and Vascular Institute in New Orleans; Dr. Wisløff is with the Norwegian University of Science and Technology, Trondheim; Dr. Blumenthal is director of the Ciccarone Center for the Prevention of Cardiovascular Disease at John Hopkins Hospital, Baltimore. Their invited commentary appears in JAMA Cardiology. Authors reported conflict of interest with Mio Global Canada (Dr. Lavie) and PAI Health (Dr. Wisloff).
In highly active individuals, high levels of coronary artery calcification do not appear to confer an elevated mortality risk, a large, observational study suggests.
There was an increased risk of elevated levels of coronary artery calcification (CAC) in men with levels of exercise training comparable with that seen in master marathon runners, the study authors reported. However, elevated CAC in highly active men didn’t translate into a significant increase in all-cause or cardiovascular disease mortality risk in the study.
That result is contrary to the hypothesis that high activity levels would increase mortality risk in individuals with CAC, according to senior author Benjamin D. Levine, MD, of Texas Health Presbyterian Hospital in Dallas, and his coauthors.
“Our findings should reassure patients and their health care professionals that it appears these highly active individuals can safely continue their exercise programs,” Dr. Levine and his coauthors wrote in JAMA Cardiology.
The present analysis focused on 21,758 generally healthy men without prevalent cardiovascular disease. They were enrolled in the Cooper Center Longitudinal Study, a prospective, longitudinal study designed to assess linkages between physical activity, cardiorespiratory fitness, and health. The mean age of these men was 52 years at baseline; the mean duration of follow-up was 10.4 years.
Out of 21,758 male participants, 1,561 reported very high levels of physical activity, or at least 3,000 metabolic equivalent of task (MET) minutes per week, while 3,750 reported 1,500-2,999 MET minutes per week, and 16,477 reported low levels of physical activity, or less than 1,500 MET minutes per week.
The adjusted risk of elevated CAC, defined as at least 100 Agatston units, was 11% higher in the individuals reporting very high physical activity levels, the investigators found.
Presence of elevated CAC nearly doubled the risk of death in men with low levels of exercise, with a hazard ratio of 1.93 (95% confidence interval, 1.34-2.78), the investigators found. By contrast, there was no significant increase in all-cause mortality in the most active group (HR, 0.77; 95% CI, 0.52-1.15).
Taken together, these findings seem to provide evidence that high activity levels do not increase mortality risk, the investigators wrote, noting that the study is believed to have the “best available” mortality data in a large CAC population that includes measurement of physical activity.
The research was supported in partly through the National Space Biomedical Research Institute. One study author reported disclosures related to Abbott, AstraZeneca, and the American Heart Association.
SOURCE: Levine BD et al. JAMA Cardiol. 2019 Jan 30. doi: 10.1001/jamacardio.2018.4628.
In highly active individuals, high levels of coronary artery calcification do not appear to confer an elevated mortality risk, a large, observational study suggests.
There was an increased risk of elevated levels of coronary artery calcification (CAC) in men with levels of exercise training comparable with that seen in master marathon runners, the study authors reported. However, elevated CAC in highly active men didn’t translate into a significant increase in all-cause or cardiovascular disease mortality risk in the study.
That result is contrary to the hypothesis that high activity levels would increase mortality risk in individuals with CAC, according to senior author Benjamin D. Levine, MD, of Texas Health Presbyterian Hospital in Dallas, and his coauthors.
“Our findings should reassure patients and their health care professionals that it appears these highly active individuals can safely continue their exercise programs,” Dr. Levine and his coauthors wrote in JAMA Cardiology.
The present analysis focused on 21,758 generally healthy men without prevalent cardiovascular disease. They were enrolled in the Cooper Center Longitudinal Study, a prospective, longitudinal study designed to assess linkages between physical activity, cardiorespiratory fitness, and health. The mean age of these men was 52 years at baseline; the mean duration of follow-up was 10.4 years.
Out of 21,758 male participants, 1,561 reported very high levels of physical activity, or at least 3,000 metabolic equivalent of task (MET) minutes per week, while 3,750 reported 1,500-2,999 MET minutes per week, and 16,477 reported low levels of physical activity, or less than 1,500 MET minutes per week.
The adjusted risk of elevated CAC, defined as at least 100 Agatston units, was 11% higher in the individuals reporting very high physical activity levels, the investigators found.
Presence of elevated CAC nearly doubled the risk of death in men with low levels of exercise, with a hazard ratio of 1.93 (95% confidence interval, 1.34-2.78), the investigators found. By contrast, there was no significant increase in all-cause mortality in the most active group (HR, 0.77; 95% CI, 0.52-1.15).
Taken together, these findings seem to provide evidence that high activity levels do not increase mortality risk, the investigators wrote, noting that the study is believed to have the “best available” mortality data in a large CAC population that includes measurement of physical activity.
The research was supported in partly through the National Space Biomedical Research Institute. One study author reported disclosures related to Abbott, AstraZeneca, and the American Heart Association.
SOURCE: Levine BD et al. JAMA Cardiol. 2019 Jan 30. doi: 10.1001/jamacardio.2018.4628.
FROM JAMA CARDIOLOGY
Key clinical point: In highly active men, high levels of coronary artery calcification do not appear to confer an elevated mortality risk.
Major finding: Elevated coronary artery calcification nearly doubled risk of death in men with low levels of exercise (HR, 1.93), while no significant increase in all-cause mortality was seen in highly active men with coronary artery calcification.
Study details: An observational study including 21,758 generally healthy men without prevalent cardiovascular disease enrolled in the Cooper Center Longitudinal Study.
Disclosures: The research was supported in partly through the National Space Biomedical Research Institute. One study coauthor reported disclosures related to Abbott, AstraZeneca, and the American Heart Association.
Source: Levine BD et al. JAMA Cardiol. 2019 Jan 30. doi: 10.1001/jamacardio.2018.4628.
New SLE disease activity measure beats SLEDAI-2K
, according to investigators.
In terms of identifying clinically significant changes, the Systemic Lupus Erythematosus Disease Activity Score (SLE-DAS) was superior to the SLE Disease Activity Index 2000 (SLEDAI-2K), said the authors of a longitudinal cohort study comparing the two instruments.
The SLE-DAS maintained high specificity compared with the SLEDAI-2K and had a similar clinical workup time requirement, according to Diogo Jesus, MD, of the rheumatology department at Centro Hospitalar e Universitário de Coimbra, Portugal, and his colleagues.
“Such a performance can have major implications in the interpretation of clinical trials applying the disease activity as the primary endpoint, and in daily clinical practice, where SLE-DAS could provide robust guidance for treatment in the individual patient,” Dr. Jesus and his coauthors wrote in Annals of the Rheumatic Diseases.
The longitudinal cohort study by Dr. Jesus and his colleagues included 520 patients with SLE from tertiary care centers in Coimbra, Portugal, and Padova, Italy. These included a derivation cohort of 324 patients and an external validation cohort of 196 patients (the Padova Lupus Cohort).
A cutoff value of 1.72 for change in the 17-item SLE-DAS had significantly higher sensitivities to detect a clinical meaningful improvement in both the derivation (82.1%) and external validation (89.5%) cohorts, compared with a cutoff value of 4 or higher in the SLEDAI-2K at 44.8% and 47.4%, respectively, the investigators reported. Likewise, ability to detect clinically meaningful worsening was significantly higher with SLE-DAS, with sensitivities of 93.1% in the derivation cohort and 95.5% in the external validation group versus a respective 46.6% and 59.1% for SLEDAI-2K. Both clinical improvement and worsening were defined by a change in the Physician Global Assessment score of 0.3 or more.
Specificity was high for both instruments, with values around 98%-99% in both cohorts for clinically meaningful worsening and about 97%-100% for clinically meaningful improvement, the report shows.
Further analyses showed that disease activity tracked over time with SLE-DAS had a higher predictive value for damage accrual versus the SLEDAI-2K, according to the investigators.
The SLE-DAS formula, published in the journal by Dr. Jesus and his colleagues, includes a total of 17 weighted and mostly binary variables: presence or absence of alopecia, arthritis, cardiac/pulmonary involvement, generalized cutaneous rash, hemolytic anemia, hypocomplementemia, increased anti-dsDNA levels, leukopenia, localized cutaneous rash, mucocutaneous vasculitis, mucosal ulcers, myositis, neuropsychiatric involvement, proteinuria, serositis, systemic vasculitis, and thrombocytopenia.
Next, the researchers plan to define SLE-DAS cutoff values for remission, low disease activity, and moderate or high disease activity. An online calculator is also in the works, they said.
Dr. Jesus and his coauthors did not report any outside funding for the study and said they had no competing interests related to their research.
SOURCE: Jesus D et al. Ann Rheum Dis. 2019 Jan 9. doi: 10.1136/annrheumdis-2018-214502.
, according to investigators.
In terms of identifying clinically significant changes, the Systemic Lupus Erythematosus Disease Activity Score (SLE-DAS) was superior to the SLE Disease Activity Index 2000 (SLEDAI-2K), said the authors of a longitudinal cohort study comparing the two instruments.
The SLE-DAS maintained high specificity compared with the SLEDAI-2K and had a similar clinical workup time requirement, according to Diogo Jesus, MD, of the rheumatology department at Centro Hospitalar e Universitário de Coimbra, Portugal, and his colleagues.
“Such a performance can have major implications in the interpretation of clinical trials applying the disease activity as the primary endpoint, and in daily clinical practice, where SLE-DAS could provide robust guidance for treatment in the individual patient,” Dr. Jesus and his coauthors wrote in Annals of the Rheumatic Diseases.
The longitudinal cohort study by Dr. Jesus and his colleagues included 520 patients with SLE from tertiary care centers in Coimbra, Portugal, and Padova, Italy. These included a derivation cohort of 324 patients and an external validation cohort of 196 patients (the Padova Lupus Cohort).
A cutoff value of 1.72 for change in the 17-item SLE-DAS had significantly higher sensitivities to detect a clinical meaningful improvement in both the derivation (82.1%) and external validation (89.5%) cohorts, compared with a cutoff value of 4 or higher in the SLEDAI-2K at 44.8% and 47.4%, respectively, the investigators reported. Likewise, ability to detect clinically meaningful worsening was significantly higher with SLE-DAS, with sensitivities of 93.1% in the derivation cohort and 95.5% in the external validation group versus a respective 46.6% and 59.1% for SLEDAI-2K. Both clinical improvement and worsening were defined by a change in the Physician Global Assessment score of 0.3 or more.
Specificity was high for both instruments, with values around 98%-99% in both cohorts for clinically meaningful worsening and about 97%-100% for clinically meaningful improvement, the report shows.
Further analyses showed that disease activity tracked over time with SLE-DAS had a higher predictive value for damage accrual versus the SLEDAI-2K, according to the investigators.
The SLE-DAS formula, published in the journal by Dr. Jesus and his colleagues, includes a total of 17 weighted and mostly binary variables: presence or absence of alopecia, arthritis, cardiac/pulmonary involvement, generalized cutaneous rash, hemolytic anemia, hypocomplementemia, increased anti-dsDNA levels, leukopenia, localized cutaneous rash, mucocutaneous vasculitis, mucosal ulcers, myositis, neuropsychiatric involvement, proteinuria, serositis, systemic vasculitis, and thrombocytopenia.
Next, the researchers plan to define SLE-DAS cutoff values for remission, low disease activity, and moderate or high disease activity. An online calculator is also in the works, they said.
Dr. Jesus and his coauthors did not report any outside funding for the study and said they had no competing interests related to their research.
SOURCE: Jesus D et al. Ann Rheum Dis. 2019 Jan 9. doi: 10.1136/annrheumdis-2018-214502.
, according to investigators.
In terms of identifying clinically significant changes, the Systemic Lupus Erythematosus Disease Activity Score (SLE-DAS) was superior to the SLE Disease Activity Index 2000 (SLEDAI-2K), said the authors of a longitudinal cohort study comparing the two instruments.
The SLE-DAS maintained high specificity compared with the SLEDAI-2K and had a similar clinical workup time requirement, according to Diogo Jesus, MD, of the rheumatology department at Centro Hospitalar e Universitário de Coimbra, Portugal, and his colleagues.
“Such a performance can have major implications in the interpretation of clinical trials applying the disease activity as the primary endpoint, and in daily clinical practice, where SLE-DAS could provide robust guidance for treatment in the individual patient,” Dr. Jesus and his coauthors wrote in Annals of the Rheumatic Diseases.
The longitudinal cohort study by Dr. Jesus and his colleagues included 520 patients with SLE from tertiary care centers in Coimbra, Portugal, and Padova, Italy. These included a derivation cohort of 324 patients and an external validation cohort of 196 patients (the Padova Lupus Cohort).
A cutoff value of 1.72 for change in the 17-item SLE-DAS had significantly higher sensitivities to detect a clinical meaningful improvement in both the derivation (82.1%) and external validation (89.5%) cohorts, compared with a cutoff value of 4 or higher in the SLEDAI-2K at 44.8% and 47.4%, respectively, the investigators reported. Likewise, ability to detect clinically meaningful worsening was significantly higher with SLE-DAS, with sensitivities of 93.1% in the derivation cohort and 95.5% in the external validation group versus a respective 46.6% and 59.1% for SLEDAI-2K. Both clinical improvement and worsening were defined by a change in the Physician Global Assessment score of 0.3 or more.
Specificity was high for both instruments, with values around 98%-99% in both cohorts for clinically meaningful worsening and about 97%-100% for clinically meaningful improvement, the report shows.
Further analyses showed that disease activity tracked over time with SLE-DAS had a higher predictive value for damage accrual versus the SLEDAI-2K, according to the investigators.
The SLE-DAS formula, published in the journal by Dr. Jesus and his colleagues, includes a total of 17 weighted and mostly binary variables: presence or absence of alopecia, arthritis, cardiac/pulmonary involvement, generalized cutaneous rash, hemolytic anemia, hypocomplementemia, increased anti-dsDNA levels, leukopenia, localized cutaneous rash, mucocutaneous vasculitis, mucosal ulcers, myositis, neuropsychiatric involvement, proteinuria, serositis, systemic vasculitis, and thrombocytopenia.
Next, the researchers plan to define SLE-DAS cutoff values for remission, low disease activity, and moderate or high disease activity. An online calculator is also in the works, they said.
Dr. Jesus and his coauthors did not report any outside funding for the study and said they had no competing interests related to their research.
SOURCE: Jesus D et al. Ann Rheum Dis. 2019 Jan 9. doi: 10.1136/annrheumdis-2018-214502.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point: The Systemic Lupus Erythematosus Disease Activity Score (SLE-DAS) had better performance in detecting clinically significant changes, compared with the commonly used SLE Disease Activity Index 2000 (SLEDAI-2K).
Major finding: In a validation cohort, the SLE-DAS (vs. SLEDAI-2K) had a significantly higher sensitivity to detect a clinical meaningful improvement (89.5% vs. 47.4%) and clinically meaningful worsening (95.5% vs. 59.1%), with comparably high specificity for both tools.
Study details: Longitudinal cohort study including 520 patients with SLE from two tertiary care centers.
Disclosures: The study authors did not report any outside funding for the study and said they had no competing interests related to the research.
Source: Jesus D et al. Ann Rheum Dis. 2019 Jan 9. doi: 10.1136/annrheumdis-2018-214502.