User login
Caught in the Hotbox
A 19-year-old woman presented to the emergency department (ED) with a 14-day history of progressive fevers, night sweats, abdominal pain, nonbloody and nonbilious vomiting, diarrhea, cough, and myalgia. The fever occurred daily with no noted temporal pattern, and she had no significant weight loss. The abdominal pain was diffuse and exacerbated by eating. She experienced multiple sporadic episodes of vomiting and diarrhea daily. She denied any rash or arthralgia.
She had no known medical history and took no medications. Family history was negative for autoinflammatory and autoimmune conditions. She had emigrated from Kenya to the United States 28 days ago. Her immunization status was unknown.
This patient has prolonged fevers and evidence of multisystem involvement. The most likely etiologic categories are infectious, inflammatory, rheumatologic, and neoplastic. For febrile patients who have recently emigrated to or travelled outside of the United States, it is important to consider common infections, as well as those endemic to the nation of exposure, which in this case includes malaria, typhoid fever, tuberculosis, cholera, acute viral hepatitis, chikungunya fever, dengue fever, yellow fever, and rickettsial disease. All of these, other than tuberculosis, commonly present with fever, vomiting, diarrhea, and myalgia. She may also have bacterial pneumonia or influenza given her fever and cough, although the chronicity and persistence of symptoms would be atypical. Acute infectious gastroenteritis is a common cause of fever, vomiting, and diarrhea. Most cases resolve in 7 to 10 days, so the duration raises suspicion for a nonviral etiology or an immunocompromised state.
Inflammatory causes could include the first presentation of inflammatory bowel disease (IBD), particularly if the patient develops weight loss or eye, skin, or joint manifestations. The lack of rash or arthralgia makes rheumatologic conditions less likely. Prolonged fevers and night sweats could indicate malignancy such as intra-abdominal lymphoma, although infectious etiologies should be ruled out first.
Previously, on day 9 of symptoms, the patient presented to an ED at another institution. Laboratory evaluation at that time demonstrated an elevated aspartate aminotransferase (AST) level of 229 IU/L (reference, 0-40 IU/L) and alanine aminotransferase (ALT) level of 60 IU/L (reference, 0-32 IU/L) with normal alkaline phosphatase and bilirubin levels, proteinuria to 3+ (normal, negative/trace), ketonuria to 2+ (normal, negative), and hematuria to 2+ (normal, negative). Complete blood count and electrolytes were normal. Computed tomography (CT) scans of the chest, abdomen, and pelvis with intravenous contrast were normal and without evidence of organomegaly.
AST and ALT elevations often indicate hepatocellular damage, although the normal bilirubin levels suggest normal hepatic function. Because CT may miss extrahepatic biliary pathology, a right upper quadrant ultrasound should be obtained to better evaluate patency of the biliary system and hepatic echotexture. Coagulation studies and viral hepatitis serology should be obtained. The disproportionate elevation of AST versus ALT can suggest alcohol use or nonhepatic etiologies such as myositis. Acute viral hepatitis is less likely given there is only mild to moderate elevation in aminotransferase levels. However, the remaining infectious etiologies can have this level of elevation and should still be considered.
Enteritis and IBD are still considerations despite the normal CT results. Transient asymptomatic hematuria or proteinuria can be seen in multiple conditions, particularly proteinuria with febrile illnesses. Urine microscopy to evaluate for casts could indicate a glomerular origin of the hematuria. First morning urine protein-to-creatinine ratio would help quantify the degree of proteinuria. Serum creatinine level should be measured to determine whether there is any renal dysfunction.
While early imaging can be falsely negative, the unremarkable chest CT makes pneumonia and active pulmonary tuberculosis less likely.
Vital signs during this presentation were: temperature, 39.7 °C; heart rate, 126 beats per minute; blood pressure, 109/64 mm Hg; respiratory rate, 20 breaths per minute; and oxygen saturation, 98% on room air. She was ill-appearing, with diffuse abdominal tenderness without peritoneal signs. Other than her tachycardia, findings from her cardiopulmonary, neurologic, and skin exams were normal.
Laboratory testing revealed a white blood cell count of 4,300/µL (reference range, 4,500-13,000/µL), a hemoglobin level of 10.9 g/dL (reference range, 11.7-15.7 g/dL) with a mean corpuscular volume of 77 fL (reference range, 80-96 fL) and reticulocyte percentage of 0.5% (reference range, 0.5%-1.5%), and a platelet count of 59,000/µL (reference range, 135,000-466,000/µL). Her prothrombin time was 13.5 seconds (reference range, 9.6-11.6 seconds) with an international normalized ratio of 1.3 (reference range, 0.8-1.1), erythrocyte sedimentation rate of 46 mm/h (reference range, 0-20 mm/h), C-reactive protein level of 7.49 mg/dL (reference range, <0.3 mg/dL), and AST level of 194 units/L (reference range, 9-35 units/L). ALT, total and direct bilirubin, lipase, electrolytes, and creatinine levels were normal. An abdominal x-ray showed scattered air-fluid levels in a nonobstructed pattern.
Her mildly elevated prothrombin time and international normalized ratio suggest a coagulopathy involving either her extrinsic or common coagulation pathway, with disseminated intravascular coagulation (DIC) being most likely given her new thrombocytopenia and anemia. Hemolytic uremic syndrome and thrombotic thrombocytopenic purpura should be considered but would not cause coagulopathy. A peripheral smear to evaluate for schistocytes associated with microangiopathic hemolysis and serum fibrinogen to distinguish between DIC (low) and thrombocytopenic purpura or hemolytic uremic syndrome (normal or elevated) should be obtained. A thick and thin smear for malaria should also be performed.
Her new pancytopenia suggests bone marrow suppression or infiltration with or without a concomitant consumptive process such as sepsis with resulting DIC. Given her clinical picture, marrow infiltrative processes might include tuberculosis or malignancy, and marrow suppression may be caused by HIV or other viral infection. If she is found to have HIV, disseminated fungal or mycobacterial infections would become more likely. She now has an isolated elevated AST level, which could be secondary to hemolysis rather than hepatocyte damage. Findings from her abdominal exam are nonfocal; this is consistent with her x-ray findings, which reflect possible enteritis or colitis.
The most likely diagnosis currently is an infectious enteritis with resulting hematologic and hepatic abnormalities. Given her recent emigration from Kenya, typhoid fever and cholera are both possible, although cholera typically does not present with prolonged fever or severe abdominal pain. The severity and duration of her illness, and the abnormalities of her laboratory findings, warrant empiric therapy with ceftriaxone to treat possible severe Salmonella enterica infection while awaiting blood and stool cultures.
The patient was admitted to the hospital and her symptoms continued. Results of serum HIV 1 and 2 polymerase chain reactions, herpes simplex virus 1 and 2 polymerase chain reactions, three malaria smears, human T-lymphotropic virus serologies, Toxoplasma serology, Bartonella serology, a stool culture, and multiple large volume blood cultures were negative. Serologic testing for hepatitis A, B, and C, Epstein-Barr virus, cytomegalovirus, and dengue virus were negative for acute infection. Results of an interferon-gamma release assay were indeterminate; results of purified protein derivative (PPD) and Candida antigen control testing were both negative. Ceruloplasmin and α1-antitrypsin levels were normal. An abdominal ultrasound showed central intrahepatic biliary duct dilatation, splenomegaly, and sluggish portal venous flow.
While central intrahepatic biliary ductal dilation could be caused by an obstructive lesion, none were seen on CT or ultrasound. Her normal alkaline phosphatase and bilirbuin levels also suggest functional patency of the biliary system. The thrombocytopenia, splenomegaly, and sluggish portal venous flow suggest possible portal hypertension, though no cirrhotic changes were noted on the ultrasound or abdominal CT. Her negative PPD and Candida antigen control results may suggest underlying immune dysregulation or suppression, though anergy could be secondary to sepsis.
Given her negative initial infectious evaluation, other etiologies such as atypical infections, rheumatologic disorders, and malignancies warrant consideration. She has no murmur; however, subacute bacterial endocarditis with a fastidious organism is possible, which could be investigated with a transthoracic echocardiogram. Other tests to consider include blood cultures for fungi and atypical mycobacterial species, and serology for Coxiella burnetii, chikungunya virus, and yellow fever. Rheumatologic conditions such as systemic lupus erythematosus, hemophagocytic lymphohistiocytosis (HLH), or adult Still’s disease should be considered. Complement levels and an antinuclear antibody panel, including those for dsDNA and Smith antigen, should be performed to evaluate for systemic lupus erythematosus. Serum ferritin, fibrinogen, and triglyceride levels should be measured to evaluate for HLH. Hematologic malignancy is also a consideration, particularly given her pancytopenia. Multicentric Castleman disease can cause prolonged fevers, pancytopenia, and elevated inflammatory markers, but is less likely without lymphadenopathy. A peripheral blood smear should be sent, and a bone marrow biopsy may be needed.
Empiric ciprofloxacin was initiated; however, the patient continued to have fevers up to 39.9 °C, abdominal pain, and myalgia. Ferritin level was over 3,000 ng/mL (reference range, 8-255 ng/mL), and a soluble interleukin-2 (IL-2) receptor level was 1,188 units/mL (reference range, 45-1,105 units/mL). Triglycerides were normal.
The elevated ferritin and soluble IL-2 levels raise concern for HLH. Hyperferritinemia is relatively nonspecific because extremely elevated ferritin can be seen with other conditions, such as renal failure, hepatocellular injury, infection, rheumatologic conditions, and hematologic malignancy. Soluble IL-2 receptor elevation is more specific for HLH than ferritin or triglycerides, but alone does not make the diagnosis because it can be elevated in other rheumatologic disorders and malignancy. The HLH-2004 criteria are commonly used and require either molecular diagnostic testing or meeting at least five out of eight clinical and lab criteria to make the diagnosis. Our patient currently meets three criteria (fever, splenomegaly, and elevated ferritin). Elevated soluble IL-2 is part of the HLH-2004 criteria, but her level of elevation does not meet the required threshold (≥2,400 units/mL). Her cytopenias have also not quite met the HLH-2004 thresholds (two of the following three: hemoglobin <9 g/dL, platelets <100,000/µL, and/or absolute neutrophil count <1,000/µL). Elevated aminotransferase levels and DIC are not part of the HLH-2004 criteria but are often seen with HLH.
Evaluation for an underlying infectious, rheumatologic, or malignant trigger should continue as previously discussed. If this patient does have HLH, it is most likely secondary to an infection, autoimmune disease, or malignancy rather than genetic HLH. HLH has a high mortality rate, but before beginning treatment with immunosuppressive agents, a peripheral smear and a bone marrow biopsy should be performed to evaluate for hematologic malignancy or signs of hemophagocytosis.
Empiric ciprofloxacin covers most bacterial etiologies of diarrhea, including those previously mentioned such as cholera and most strains of S enterica. Her symptoms and laboratory findings (including cytopenias, elevated aminotransferases, and coagulopathy) could suggest enteric fever due to S enterica serovar Typhi, which is endemic in Kenya. Results of blood and stool cultures, though negative, are relatively insensitive for this organism, particularly this far into the illness course. A bone marrow biopsy may also help with diagnosis of occult typhoid fever because marrow culture can be more sensitive than blood or stool culture.
A bone marrow aspiration revealed hemophagocytic histiocytes, no malignant cells, and negative bacterial (including anaerobic), fungal, and acid-fast bacilli cultures. Considering the high mortality rate of untreated HLH/macrophage activation syndrome (MAS), empiric glucocorticoid administration was considered. However, this was withheld due to concern for ongoing undetected infection given her persistent fever and systemic symptoms.
There should still be high suspicion for HLH. Further evaluation for other laboratory manifestations of HLH such as fibrinogen and natural killer cell activity should be considered, as well as repeating her complete blood count to see if her cytopenias have progressed. Her marrow shows no evidence of hematologic malignancy, so other triggers of possible HLH should be sought out by continuing the workup. Consulting specialists from rheumatology and infectious disease may help clarify possible underlying diagnoses and the best management plan. If she continues to have organ damage or clinically worsens, it may be prudent to empirically broaden her antibiotic coverage and begin antifungal agents while starting glucocorticoid therapy for suspected HLH.
A stool molecular screen from admission was returned positive for S enterica serovar Typhi. Ciprofloxacin was discontinued and ceftriaxone was started out of concern for antibiotic resistance. On hospital day 14, the patient’s brother presented to the ED with fever. His blood and stool cultures were positive for S enterica serovar Typhi with intermediate sensitivity to ciprofloxacin and sensitivity to ceftriaxone. With continued treatment with ceftriaxone, the patient improved significantly. Following discharge, she remained afebrile and asymptomatic. During outpatient follow up, a repeat PPD was positive and she was diagnosed with and treated for latent tuberculosis.
COMMENTARY
The evaluation of a patient who has recently emigrated from a foreign nation requires a broad differential diagnosis and a keen awareness of the clinical conditions present in the patient’s country of origin. This often involves knowledge of diseases infrequently encountered in daily practice, as well as awareness of the nuances of rare presentations and possible complications. When the presentation is not classic for a relevant infectious disease and clinical conditions from other diagnostic classes are considered, the evaluation and management of the patient is particularly challenging.
Typhoid fever is a severe systemic illness caused by the organism S enterica serovar Typhi. The organism is ingested, penetrates the small intestinal epithelium, enters the lymphoid tissue, and disseminates via the lymphatic and hematogenous routes. Onset of symptoms typically occurs 5 to 21 days after ingestion of contaminated food or water. Clinical features include fever, chills, relative bradycardia (pulse-temperature dissociation), abdominal pain, rose spots (salmon-colored macules) on the trunk and abdomen, and hepatosplenomegaly. Diarrhea is not a typical symptom of patients with typhoid fever, which can lead to a delayed or missed diagnosis. Life-threatening complications can be seen, including gastrointestinal bleeding, intestinal perforation, and meningitis.1 Typhoid fever is most prevalent in impoverished areas with poor access to sanitation. Regions with the highest incidence include south-central Asia, southeast Asia, and southern Africa.2-4 Approximately 200 to 300 cases are reported in the United States each year.5
Classically, the diagnosis is made by means of clinical symptoms and a positive culture from a sterile site. A recent study of 529 patients found that 61% had positive blood cultures and 96% had positive bone marrow cultures.6 Our patient’s diagnosis was significantly delayed by multiple negative cultures and failure to improve on first-line antibiotics, which initially suggested that the S enterica serovar Typhi stool molecular screen likely represented carriage caused by colonization. Chronic S enterica serovar Typhi carriage is defined as excretion of the organism in stool or urine 1 year or longer after acute infection. Rates of carriage range from 1% to 6%, and up to 25% of carriers have no history of typhoid fever.1,7,8 Carriage is more common in females and in those with biliary tract abnormalities.9,10
Once a presumptive diagnosis is made, antibiotic choice remains a challenge. Resistance to fluoroquinolones, the preferred drug for multidrug-resistant typhoid fever, is growing but remains rare, at approximately 5%.11,12 Ceftriaxone and azithromycin have been used successfully in areas with high resistance.13 Given the patient’s slow response to therapy even after transitioning from ciprofloxacin to ceftriaxone, her brother’s presentation and obtaining the antibiotic sensitivities for his organism were critical to confirming that our diagnosis and management decisions were correct.
One strongly considered diagnosis was HLH/MAS. MAS is an aggressive syndrome of excessive inflammation and tissue destruction caused by inappropriate immune system activation. It belongs to a group of histiocytic disorders collectively known as HLH. Aside from primary (genetic) forms, secondary forms exist that can be triggered by malignancy, infection, or rheumatologic disorders. In infection-associated HLH/MAS, viral infections are a common trigger, with Epstein-Barr virus being the most common. Association with bacterial infections, including tuberculosis and typhoid fever, has also been reported.14 Prompt therapy, often with immunosuppressive agents such as glucocorticoids, is essential for survival because there is a reported mortality rate of up to 50% when untreated.15 When infection-induced HLH/MAS occurs, treatment of the underlying infection is critical.14,15 The greatest barrier to a favorable outcome from HLH/MAS is often a delay in diagnosis because the rarity of this disease, the variable clinical presentation, and the lack of specificity of the clinical and laboratory findings make a conclusive diagnosis challenging.
In the presented case, diagnostic uncertainty challenged the decision to administer systemic glucocorticoids. Glucocorticoids conferred a risk of harm for multiple diagnoses that remained on the differential, including malignancy and infection. Her diagnostic evaluation made malignancy less likely, but because testing was unable to rule out tuberculosis as either the underlying cause or coinfection, the team opted to defer initiating glucocorticoids and instead closely monitor for a worsening inflammatory response. Following appropriate treatment of her systemic infection, her PPD was repeated and became positive. The negative PPD and Candida control obtained during her hospitalization were, therefore, likely caused by anergy in the setting of overwhelming systemic illness. Initiation of glucocorticoids prematurely in this case could have led to further harm because immunosuppression may have led to reactivation of latent tuberculosis or exacerbation of illness from an alternative but then undiagnosed infection.
The patient’s ultimate unifying diagnosis was typhoid fever; however, there are mixed expert opinions as to whether the systemic immune activation was significant enough to merit the diagnosis of infection-induced secondary HLH/MAS. Despite the high morbidity and mortality that can accompany HLH/MAS, it has been reported that a significant proportion of cases of secondary HLH/MAS can be managed effectively with treatment of the underlying etiology; this may have been the case for our patient.14,15 The clinicians in this case were caught between diagnoses, unable to safely reach either one—much like a baseball player stranded between bases. Fortunately for this patient, the diagnosis ultimately emerged after a careful and thorough workup, assisted by the more straightforward diagnosis of her brother with the same disease.
KEY TEACHING POINTS
- Salmonella enterica serovar Typhi has a high false-negative rate in blood and stool cultures; therefore, clinical suspicion should remain high in the setting of a high pre-test probability.
- Fluoroquinolones are traditionally first-line therapy for typhoid fever, but the use of ceftriaxone and azithromycin is increasing because of rising fluoroquinolone resistance.
- Hemophagocytic lymphohistiocytosis/macrophage activation syndrome is characterized by excessive inflammation and tissue destruction caused by inappropriate immune system activation. This syndrome can be fatal without appropriate immunosuppressive therapy; however, glucocorticoid administration must be pursued with caution when infection and malignancy are on the differential diagnosis.
1. Parry CM, Hien TT, Dougan G, et al. Typhoid fever. N Engl J Med. 2002;347(22):1770-1782. https://doi.org/10.1056/nejmra020201
2. Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82(5):346-353.
3. Buckle GC, Walker CL, Black RE. Typhoid fever and paratyphoid fever: systematic review to estimate global morbidity and mortality for 2010. J Glob Health. 2012;2(1):010401. https://doi.org/10.7189/jogh.02.010401
4. Mogasale V, Maskery B, Ochiai RL, et al. Burden of typhoid fever in low-income and middle-income countries: a systematic, literature-based update with risk-factor adjustment. Lancet Glob Health. 2014;2(10):e570-e580. https://doi.org/10.1016/s2214-109x(14)70301-8
5. Lynch MF, Blanton EM, Bulens S, et al. Typhoid fever in the United States, 1999-2006. JAMA. 2009;302(8):859-865. https://doi.org/10.1001/jama.2009.1229
6. Mogasale V, Ramani E, Mogasale VV, Park J. What proportion of Salmonella typhi cases are detected by blood culture? a systematic literature review. Ann Clin Microbiol Antimicrob. 2016;15(1):32. https://doi.org/10.1186/s12941-016-0147-z
7. Merselis JG Jr, Kaye D, Connolly CS, Hook EW. Quantitative bacteriology of the Typhoid carrier state. Am J Trop Med Hyg. 1964;13:425-429. https://doi.org/10.4269/ajtmh.1964.13.425
8. Lanata CF, Levine MM, Ristori C, et al. Vi serology in detection of chronic Salmonella typhi carriers in an endemic area. Lancet. 1983;2(8347):441-443. https://doi.org/10.1016/s0140-6736(83)90401-4
9. Lai CW, Chan RC, Cheng AF, Sung JY, Leung JW. Common bile duct stones: a cause of chronic salmonellosis. Am J Gastroenterol. 1992;87(9):1198-1199.
10. Hofmann E, Chianale J, Rollán A, Pereira J, Ferrecio C, Sotomayor V. Blood group antigen secretion and gallstone disease in the Salmonella typhi chronic carrier state. J Infect Dis. 1993;167(4):993-994. https://doi.org/10.1093/infdis/167.4.993
11. Steel AD, Hay Burgess DC, Diaz Z, Carey ME, Zaidi AKM. Challenges and opportunities for typhoid fever control: a call for coordinated action. Clin Infect Dis. 2016;62 (Suppl 1):S4-S8. https://doi.org/10.1093/cid/civ976
12. Hendriksen RS, Leekitcharoenphon P, Lukjancenko O, et al. Genomic signature of multidrug resistant Salmonella enterica serovar Typhi isolates related to a massive outbreak in Zambia between 2010 and 2012. J Clin Microbiol. 2015;53(1):262-272. https://doi.org/10.1128/jcm.02026-14
13. Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of Salmonella infections. Clin Microbiol Rev. 2015;28(4):901-936. https://doi.org/10.1128/cmr.00002-15
14. Rouphael NG, Talati NJ, Vaughan C, Cunningham K, Moreira R, Gould C. Infections associated with haemophagocytic syndrome. Lancet Infect Dis. 2007;7(12):814-822. https://doi.org/10.1016/s1473-3099(07)70290-6
15. Fisman DN. Hemophagocytic syndromes and infection. Emerg Infect Dis. 2000;6(6):601-608. https://doi.org/10.3201/eid0606.000608
A 19-year-old woman presented to the emergency department (ED) with a 14-day history of progressive fevers, night sweats, abdominal pain, nonbloody and nonbilious vomiting, diarrhea, cough, and myalgia. The fever occurred daily with no noted temporal pattern, and she had no significant weight loss. The abdominal pain was diffuse and exacerbated by eating. She experienced multiple sporadic episodes of vomiting and diarrhea daily. She denied any rash or arthralgia.
She had no known medical history and took no medications. Family history was negative for autoinflammatory and autoimmune conditions. She had emigrated from Kenya to the United States 28 days ago. Her immunization status was unknown.
This patient has prolonged fevers and evidence of multisystem involvement. The most likely etiologic categories are infectious, inflammatory, rheumatologic, and neoplastic. For febrile patients who have recently emigrated to or travelled outside of the United States, it is important to consider common infections, as well as those endemic to the nation of exposure, which in this case includes malaria, typhoid fever, tuberculosis, cholera, acute viral hepatitis, chikungunya fever, dengue fever, yellow fever, and rickettsial disease. All of these, other than tuberculosis, commonly present with fever, vomiting, diarrhea, and myalgia. She may also have bacterial pneumonia or influenza given her fever and cough, although the chronicity and persistence of symptoms would be atypical. Acute infectious gastroenteritis is a common cause of fever, vomiting, and diarrhea. Most cases resolve in 7 to 10 days, so the duration raises suspicion for a nonviral etiology or an immunocompromised state.
Inflammatory causes could include the first presentation of inflammatory bowel disease (IBD), particularly if the patient develops weight loss or eye, skin, or joint manifestations. The lack of rash or arthralgia makes rheumatologic conditions less likely. Prolonged fevers and night sweats could indicate malignancy such as intra-abdominal lymphoma, although infectious etiologies should be ruled out first.
Previously, on day 9 of symptoms, the patient presented to an ED at another institution. Laboratory evaluation at that time demonstrated an elevated aspartate aminotransferase (AST) level of 229 IU/L (reference, 0-40 IU/L) and alanine aminotransferase (ALT) level of 60 IU/L (reference, 0-32 IU/L) with normal alkaline phosphatase and bilirubin levels, proteinuria to 3+ (normal, negative/trace), ketonuria to 2+ (normal, negative), and hematuria to 2+ (normal, negative). Complete blood count and electrolytes were normal. Computed tomography (CT) scans of the chest, abdomen, and pelvis with intravenous contrast were normal and without evidence of organomegaly.
AST and ALT elevations often indicate hepatocellular damage, although the normal bilirubin levels suggest normal hepatic function. Because CT may miss extrahepatic biliary pathology, a right upper quadrant ultrasound should be obtained to better evaluate patency of the biliary system and hepatic echotexture. Coagulation studies and viral hepatitis serology should be obtained. The disproportionate elevation of AST versus ALT can suggest alcohol use or nonhepatic etiologies such as myositis. Acute viral hepatitis is less likely given there is only mild to moderate elevation in aminotransferase levels. However, the remaining infectious etiologies can have this level of elevation and should still be considered.
Enteritis and IBD are still considerations despite the normal CT results. Transient asymptomatic hematuria or proteinuria can be seen in multiple conditions, particularly proteinuria with febrile illnesses. Urine microscopy to evaluate for casts could indicate a glomerular origin of the hematuria. First morning urine protein-to-creatinine ratio would help quantify the degree of proteinuria. Serum creatinine level should be measured to determine whether there is any renal dysfunction.
While early imaging can be falsely negative, the unremarkable chest CT makes pneumonia and active pulmonary tuberculosis less likely.
Vital signs during this presentation were: temperature, 39.7 °C; heart rate, 126 beats per minute; blood pressure, 109/64 mm Hg; respiratory rate, 20 breaths per minute; and oxygen saturation, 98% on room air. She was ill-appearing, with diffuse abdominal tenderness without peritoneal signs. Other than her tachycardia, findings from her cardiopulmonary, neurologic, and skin exams were normal.
Laboratory testing revealed a white blood cell count of 4,300/µL (reference range, 4,500-13,000/µL), a hemoglobin level of 10.9 g/dL (reference range, 11.7-15.7 g/dL) with a mean corpuscular volume of 77 fL (reference range, 80-96 fL) and reticulocyte percentage of 0.5% (reference range, 0.5%-1.5%), and a platelet count of 59,000/µL (reference range, 135,000-466,000/µL). Her prothrombin time was 13.5 seconds (reference range, 9.6-11.6 seconds) with an international normalized ratio of 1.3 (reference range, 0.8-1.1), erythrocyte sedimentation rate of 46 mm/h (reference range, 0-20 mm/h), C-reactive protein level of 7.49 mg/dL (reference range, <0.3 mg/dL), and AST level of 194 units/L (reference range, 9-35 units/L). ALT, total and direct bilirubin, lipase, electrolytes, and creatinine levels were normal. An abdominal x-ray showed scattered air-fluid levels in a nonobstructed pattern.
Her mildly elevated prothrombin time and international normalized ratio suggest a coagulopathy involving either her extrinsic or common coagulation pathway, with disseminated intravascular coagulation (DIC) being most likely given her new thrombocytopenia and anemia. Hemolytic uremic syndrome and thrombotic thrombocytopenic purpura should be considered but would not cause coagulopathy. A peripheral smear to evaluate for schistocytes associated with microangiopathic hemolysis and serum fibrinogen to distinguish between DIC (low) and thrombocytopenic purpura or hemolytic uremic syndrome (normal or elevated) should be obtained. A thick and thin smear for malaria should also be performed.
Her new pancytopenia suggests bone marrow suppression or infiltration with or without a concomitant consumptive process such as sepsis with resulting DIC. Given her clinical picture, marrow infiltrative processes might include tuberculosis or malignancy, and marrow suppression may be caused by HIV or other viral infection. If she is found to have HIV, disseminated fungal or mycobacterial infections would become more likely. She now has an isolated elevated AST level, which could be secondary to hemolysis rather than hepatocyte damage. Findings from her abdominal exam are nonfocal; this is consistent with her x-ray findings, which reflect possible enteritis or colitis.
The most likely diagnosis currently is an infectious enteritis with resulting hematologic and hepatic abnormalities. Given her recent emigration from Kenya, typhoid fever and cholera are both possible, although cholera typically does not present with prolonged fever or severe abdominal pain. The severity and duration of her illness, and the abnormalities of her laboratory findings, warrant empiric therapy with ceftriaxone to treat possible severe Salmonella enterica infection while awaiting blood and stool cultures.
The patient was admitted to the hospital and her symptoms continued. Results of serum HIV 1 and 2 polymerase chain reactions, herpes simplex virus 1 and 2 polymerase chain reactions, three malaria smears, human T-lymphotropic virus serologies, Toxoplasma serology, Bartonella serology, a stool culture, and multiple large volume blood cultures were negative. Serologic testing for hepatitis A, B, and C, Epstein-Barr virus, cytomegalovirus, and dengue virus were negative for acute infection. Results of an interferon-gamma release assay were indeterminate; results of purified protein derivative (PPD) and Candida antigen control testing were both negative. Ceruloplasmin and α1-antitrypsin levels were normal. An abdominal ultrasound showed central intrahepatic biliary duct dilatation, splenomegaly, and sluggish portal venous flow.
While central intrahepatic biliary ductal dilation could be caused by an obstructive lesion, none were seen on CT or ultrasound. Her normal alkaline phosphatase and bilirbuin levels also suggest functional patency of the biliary system. The thrombocytopenia, splenomegaly, and sluggish portal venous flow suggest possible portal hypertension, though no cirrhotic changes were noted on the ultrasound or abdominal CT. Her negative PPD and Candida antigen control results may suggest underlying immune dysregulation or suppression, though anergy could be secondary to sepsis.
Given her negative initial infectious evaluation, other etiologies such as atypical infections, rheumatologic disorders, and malignancies warrant consideration. She has no murmur; however, subacute bacterial endocarditis with a fastidious organism is possible, which could be investigated with a transthoracic echocardiogram. Other tests to consider include blood cultures for fungi and atypical mycobacterial species, and serology for Coxiella burnetii, chikungunya virus, and yellow fever. Rheumatologic conditions such as systemic lupus erythematosus, hemophagocytic lymphohistiocytosis (HLH), or adult Still’s disease should be considered. Complement levels and an antinuclear antibody panel, including those for dsDNA and Smith antigen, should be performed to evaluate for systemic lupus erythematosus. Serum ferritin, fibrinogen, and triglyceride levels should be measured to evaluate for HLH. Hematologic malignancy is also a consideration, particularly given her pancytopenia. Multicentric Castleman disease can cause prolonged fevers, pancytopenia, and elevated inflammatory markers, but is less likely without lymphadenopathy. A peripheral blood smear should be sent, and a bone marrow biopsy may be needed.
Empiric ciprofloxacin was initiated; however, the patient continued to have fevers up to 39.9 °C, abdominal pain, and myalgia. Ferritin level was over 3,000 ng/mL (reference range, 8-255 ng/mL), and a soluble interleukin-2 (IL-2) receptor level was 1,188 units/mL (reference range, 45-1,105 units/mL). Triglycerides were normal.
The elevated ferritin and soluble IL-2 levels raise concern for HLH. Hyperferritinemia is relatively nonspecific because extremely elevated ferritin can be seen with other conditions, such as renal failure, hepatocellular injury, infection, rheumatologic conditions, and hematologic malignancy. Soluble IL-2 receptor elevation is more specific for HLH than ferritin or triglycerides, but alone does not make the diagnosis because it can be elevated in other rheumatologic disorders and malignancy. The HLH-2004 criteria are commonly used and require either molecular diagnostic testing or meeting at least five out of eight clinical and lab criteria to make the diagnosis. Our patient currently meets three criteria (fever, splenomegaly, and elevated ferritin). Elevated soluble IL-2 is part of the HLH-2004 criteria, but her level of elevation does not meet the required threshold (≥2,400 units/mL). Her cytopenias have also not quite met the HLH-2004 thresholds (two of the following three: hemoglobin <9 g/dL, platelets <100,000/µL, and/or absolute neutrophil count <1,000/µL). Elevated aminotransferase levels and DIC are not part of the HLH-2004 criteria but are often seen with HLH.
Evaluation for an underlying infectious, rheumatologic, or malignant trigger should continue as previously discussed. If this patient does have HLH, it is most likely secondary to an infection, autoimmune disease, or malignancy rather than genetic HLH. HLH has a high mortality rate, but before beginning treatment with immunosuppressive agents, a peripheral smear and a bone marrow biopsy should be performed to evaluate for hematologic malignancy or signs of hemophagocytosis.
Empiric ciprofloxacin covers most bacterial etiologies of diarrhea, including those previously mentioned such as cholera and most strains of S enterica. Her symptoms and laboratory findings (including cytopenias, elevated aminotransferases, and coagulopathy) could suggest enteric fever due to S enterica serovar Typhi, which is endemic in Kenya. Results of blood and stool cultures, though negative, are relatively insensitive for this organism, particularly this far into the illness course. A bone marrow biopsy may also help with diagnosis of occult typhoid fever because marrow culture can be more sensitive than blood or stool culture.
A bone marrow aspiration revealed hemophagocytic histiocytes, no malignant cells, and negative bacterial (including anaerobic), fungal, and acid-fast bacilli cultures. Considering the high mortality rate of untreated HLH/macrophage activation syndrome (MAS), empiric glucocorticoid administration was considered. However, this was withheld due to concern for ongoing undetected infection given her persistent fever and systemic symptoms.
There should still be high suspicion for HLH. Further evaluation for other laboratory manifestations of HLH such as fibrinogen and natural killer cell activity should be considered, as well as repeating her complete blood count to see if her cytopenias have progressed. Her marrow shows no evidence of hematologic malignancy, so other triggers of possible HLH should be sought out by continuing the workup. Consulting specialists from rheumatology and infectious disease may help clarify possible underlying diagnoses and the best management plan. If she continues to have organ damage or clinically worsens, it may be prudent to empirically broaden her antibiotic coverage and begin antifungal agents while starting glucocorticoid therapy for suspected HLH.
A stool molecular screen from admission was returned positive for S enterica serovar Typhi. Ciprofloxacin was discontinued and ceftriaxone was started out of concern for antibiotic resistance. On hospital day 14, the patient’s brother presented to the ED with fever. His blood and stool cultures were positive for S enterica serovar Typhi with intermediate sensitivity to ciprofloxacin and sensitivity to ceftriaxone. With continued treatment with ceftriaxone, the patient improved significantly. Following discharge, she remained afebrile and asymptomatic. During outpatient follow up, a repeat PPD was positive and she was diagnosed with and treated for latent tuberculosis.
COMMENTARY
The evaluation of a patient who has recently emigrated from a foreign nation requires a broad differential diagnosis and a keen awareness of the clinical conditions present in the patient’s country of origin. This often involves knowledge of diseases infrequently encountered in daily practice, as well as awareness of the nuances of rare presentations and possible complications. When the presentation is not classic for a relevant infectious disease and clinical conditions from other diagnostic classes are considered, the evaluation and management of the patient is particularly challenging.
Typhoid fever is a severe systemic illness caused by the organism S enterica serovar Typhi. The organism is ingested, penetrates the small intestinal epithelium, enters the lymphoid tissue, and disseminates via the lymphatic and hematogenous routes. Onset of symptoms typically occurs 5 to 21 days after ingestion of contaminated food or water. Clinical features include fever, chills, relative bradycardia (pulse-temperature dissociation), abdominal pain, rose spots (salmon-colored macules) on the trunk and abdomen, and hepatosplenomegaly. Diarrhea is not a typical symptom of patients with typhoid fever, which can lead to a delayed or missed diagnosis. Life-threatening complications can be seen, including gastrointestinal bleeding, intestinal perforation, and meningitis.1 Typhoid fever is most prevalent in impoverished areas with poor access to sanitation. Regions with the highest incidence include south-central Asia, southeast Asia, and southern Africa.2-4 Approximately 200 to 300 cases are reported in the United States each year.5
Classically, the diagnosis is made by means of clinical symptoms and a positive culture from a sterile site. A recent study of 529 patients found that 61% had positive blood cultures and 96% had positive bone marrow cultures.6 Our patient’s diagnosis was significantly delayed by multiple negative cultures and failure to improve on first-line antibiotics, which initially suggested that the S enterica serovar Typhi stool molecular screen likely represented carriage caused by colonization. Chronic S enterica serovar Typhi carriage is defined as excretion of the organism in stool or urine 1 year or longer after acute infection. Rates of carriage range from 1% to 6%, and up to 25% of carriers have no history of typhoid fever.1,7,8 Carriage is more common in females and in those with biliary tract abnormalities.9,10
Once a presumptive diagnosis is made, antibiotic choice remains a challenge. Resistance to fluoroquinolones, the preferred drug for multidrug-resistant typhoid fever, is growing but remains rare, at approximately 5%.11,12 Ceftriaxone and azithromycin have been used successfully in areas with high resistance.13 Given the patient’s slow response to therapy even after transitioning from ciprofloxacin to ceftriaxone, her brother’s presentation and obtaining the antibiotic sensitivities for his organism were critical to confirming that our diagnosis and management decisions were correct.
One strongly considered diagnosis was HLH/MAS. MAS is an aggressive syndrome of excessive inflammation and tissue destruction caused by inappropriate immune system activation. It belongs to a group of histiocytic disorders collectively known as HLH. Aside from primary (genetic) forms, secondary forms exist that can be triggered by malignancy, infection, or rheumatologic disorders. In infection-associated HLH/MAS, viral infections are a common trigger, with Epstein-Barr virus being the most common. Association with bacterial infections, including tuberculosis and typhoid fever, has also been reported.14 Prompt therapy, often with immunosuppressive agents such as glucocorticoids, is essential for survival because there is a reported mortality rate of up to 50% when untreated.15 When infection-induced HLH/MAS occurs, treatment of the underlying infection is critical.14,15 The greatest barrier to a favorable outcome from HLH/MAS is often a delay in diagnosis because the rarity of this disease, the variable clinical presentation, and the lack of specificity of the clinical and laboratory findings make a conclusive diagnosis challenging.
In the presented case, diagnostic uncertainty challenged the decision to administer systemic glucocorticoids. Glucocorticoids conferred a risk of harm for multiple diagnoses that remained on the differential, including malignancy and infection. Her diagnostic evaluation made malignancy less likely, but because testing was unable to rule out tuberculosis as either the underlying cause or coinfection, the team opted to defer initiating glucocorticoids and instead closely monitor for a worsening inflammatory response. Following appropriate treatment of her systemic infection, her PPD was repeated and became positive. The negative PPD and Candida control obtained during her hospitalization were, therefore, likely caused by anergy in the setting of overwhelming systemic illness. Initiation of glucocorticoids prematurely in this case could have led to further harm because immunosuppression may have led to reactivation of latent tuberculosis or exacerbation of illness from an alternative but then undiagnosed infection.
The patient’s ultimate unifying diagnosis was typhoid fever; however, there are mixed expert opinions as to whether the systemic immune activation was significant enough to merit the diagnosis of infection-induced secondary HLH/MAS. Despite the high morbidity and mortality that can accompany HLH/MAS, it has been reported that a significant proportion of cases of secondary HLH/MAS can be managed effectively with treatment of the underlying etiology; this may have been the case for our patient.14,15 The clinicians in this case were caught between diagnoses, unable to safely reach either one—much like a baseball player stranded between bases. Fortunately for this patient, the diagnosis ultimately emerged after a careful and thorough workup, assisted by the more straightforward diagnosis of her brother with the same disease.
KEY TEACHING POINTS
- Salmonella enterica serovar Typhi has a high false-negative rate in blood and stool cultures; therefore, clinical suspicion should remain high in the setting of a high pre-test probability.
- Fluoroquinolones are traditionally first-line therapy for typhoid fever, but the use of ceftriaxone and azithromycin is increasing because of rising fluoroquinolone resistance.
- Hemophagocytic lymphohistiocytosis/macrophage activation syndrome is characterized by excessive inflammation and tissue destruction caused by inappropriate immune system activation. This syndrome can be fatal without appropriate immunosuppressive therapy; however, glucocorticoid administration must be pursued with caution when infection and malignancy are on the differential diagnosis.
A 19-year-old woman presented to the emergency department (ED) with a 14-day history of progressive fevers, night sweats, abdominal pain, nonbloody and nonbilious vomiting, diarrhea, cough, and myalgia. The fever occurred daily with no noted temporal pattern, and she had no significant weight loss. The abdominal pain was diffuse and exacerbated by eating. She experienced multiple sporadic episodes of vomiting and diarrhea daily. She denied any rash or arthralgia.
She had no known medical history and took no medications. Family history was negative for autoinflammatory and autoimmune conditions. She had emigrated from Kenya to the United States 28 days ago. Her immunization status was unknown.
This patient has prolonged fevers and evidence of multisystem involvement. The most likely etiologic categories are infectious, inflammatory, rheumatologic, and neoplastic. For febrile patients who have recently emigrated to or travelled outside of the United States, it is important to consider common infections, as well as those endemic to the nation of exposure, which in this case includes malaria, typhoid fever, tuberculosis, cholera, acute viral hepatitis, chikungunya fever, dengue fever, yellow fever, and rickettsial disease. All of these, other than tuberculosis, commonly present with fever, vomiting, diarrhea, and myalgia. She may also have bacterial pneumonia or influenza given her fever and cough, although the chronicity and persistence of symptoms would be atypical. Acute infectious gastroenteritis is a common cause of fever, vomiting, and diarrhea. Most cases resolve in 7 to 10 days, so the duration raises suspicion for a nonviral etiology or an immunocompromised state.
Inflammatory causes could include the first presentation of inflammatory bowel disease (IBD), particularly if the patient develops weight loss or eye, skin, or joint manifestations. The lack of rash or arthralgia makes rheumatologic conditions less likely. Prolonged fevers and night sweats could indicate malignancy such as intra-abdominal lymphoma, although infectious etiologies should be ruled out first.
Previously, on day 9 of symptoms, the patient presented to an ED at another institution. Laboratory evaluation at that time demonstrated an elevated aspartate aminotransferase (AST) level of 229 IU/L (reference, 0-40 IU/L) and alanine aminotransferase (ALT) level of 60 IU/L (reference, 0-32 IU/L) with normal alkaline phosphatase and bilirubin levels, proteinuria to 3+ (normal, negative/trace), ketonuria to 2+ (normal, negative), and hematuria to 2+ (normal, negative). Complete blood count and electrolytes were normal. Computed tomography (CT) scans of the chest, abdomen, and pelvis with intravenous contrast were normal and without evidence of organomegaly.
AST and ALT elevations often indicate hepatocellular damage, although the normal bilirubin levels suggest normal hepatic function. Because CT may miss extrahepatic biliary pathology, a right upper quadrant ultrasound should be obtained to better evaluate patency of the biliary system and hepatic echotexture. Coagulation studies and viral hepatitis serology should be obtained. The disproportionate elevation of AST versus ALT can suggest alcohol use or nonhepatic etiologies such as myositis. Acute viral hepatitis is less likely given there is only mild to moderate elevation in aminotransferase levels. However, the remaining infectious etiologies can have this level of elevation and should still be considered.
Enteritis and IBD are still considerations despite the normal CT results. Transient asymptomatic hematuria or proteinuria can be seen in multiple conditions, particularly proteinuria with febrile illnesses. Urine microscopy to evaluate for casts could indicate a glomerular origin of the hematuria. First morning urine protein-to-creatinine ratio would help quantify the degree of proteinuria. Serum creatinine level should be measured to determine whether there is any renal dysfunction.
While early imaging can be falsely negative, the unremarkable chest CT makes pneumonia and active pulmonary tuberculosis less likely.
Vital signs during this presentation were: temperature, 39.7 °C; heart rate, 126 beats per minute; blood pressure, 109/64 mm Hg; respiratory rate, 20 breaths per minute; and oxygen saturation, 98% on room air. She was ill-appearing, with diffuse abdominal tenderness without peritoneal signs. Other than her tachycardia, findings from her cardiopulmonary, neurologic, and skin exams were normal.
Laboratory testing revealed a white blood cell count of 4,300/µL (reference range, 4,500-13,000/µL), a hemoglobin level of 10.9 g/dL (reference range, 11.7-15.7 g/dL) with a mean corpuscular volume of 77 fL (reference range, 80-96 fL) and reticulocyte percentage of 0.5% (reference range, 0.5%-1.5%), and a platelet count of 59,000/µL (reference range, 135,000-466,000/µL). Her prothrombin time was 13.5 seconds (reference range, 9.6-11.6 seconds) with an international normalized ratio of 1.3 (reference range, 0.8-1.1), erythrocyte sedimentation rate of 46 mm/h (reference range, 0-20 mm/h), C-reactive protein level of 7.49 mg/dL (reference range, <0.3 mg/dL), and AST level of 194 units/L (reference range, 9-35 units/L). ALT, total and direct bilirubin, lipase, electrolytes, and creatinine levels were normal. An abdominal x-ray showed scattered air-fluid levels in a nonobstructed pattern.
Her mildly elevated prothrombin time and international normalized ratio suggest a coagulopathy involving either her extrinsic or common coagulation pathway, with disseminated intravascular coagulation (DIC) being most likely given her new thrombocytopenia and anemia. Hemolytic uremic syndrome and thrombotic thrombocytopenic purpura should be considered but would not cause coagulopathy. A peripheral smear to evaluate for schistocytes associated with microangiopathic hemolysis and serum fibrinogen to distinguish between DIC (low) and thrombocytopenic purpura or hemolytic uremic syndrome (normal or elevated) should be obtained. A thick and thin smear for malaria should also be performed.
Her new pancytopenia suggests bone marrow suppression or infiltration with or without a concomitant consumptive process such as sepsis with resulting DIC. Given her clinical picture, marrow infiltrative processes might include tuberculosis or malignancy, and marrow suppression may be caused by HIV or other viral infection. If she is found to have HIV, disseminated fungal or mycobacterial infections would become more likely. She now has an isolated elevated AST level, which could be secondary to hemolysis rather than hepatocyte damage. Findings from her abdominal exam are nonfocal; this is consistent with her x-ray findings, which reflect possible enteritis or colitis.
The most likely diagnosis currently is an infectious enteritis with resulting hematologic and hepatic abnormalities. Given her recent emigration from Kenya, typhoid fever and cholera are both possible, although cholera typically does not present with prolonged fever or severe abdominal pain. The severity and duration of her illness, and the abnormalities of her laboratory findings, warrant empiric therapy with ceftriaxone to treat possible severe Salmonella enterica infection while awaiting blood and stool cultures.
The patient was admitted to the hospital and her symptoms continued. Results of serum HIV 1 and 2 polymerase chain reactions, herpes simplex virus 1 and 2 polymerase chain reactions, three malaria smears, human T-lymphotropic virus serologies, Toxoplasma serology, Bartonella serology, a stool culture, and multiple large volume blood cultures were negative. Serologic testing for hepatitis A, B, and C, Epstein-Barr virus, cytomegalovirus, and dengue virus were negative for acute infection. Results of an interferon-gamma release assay were indeterminate; results of purified protein derivative (PPD) and Candida antigen control testing were both negative. Ceruloplasmin and α1-antitrypsin levels were normal. An abdominal ultrasound showed central intrahepatic biliary duct dilatation, splenomegaly, and sluggish portal venous flow.
While central intrahepatic biliary ductal dilation could be caused by an obstructive lesion, none were seen on CT or ultrasound. Her normal alkaline phosphatase and bilirbuin levels also suggest functional patency of the biliary system. The thrombocytopenia, splenomegaly, and sluggish portal venous flow suggest possible portal hypertension, though no cirrhotic changes were noted on the ultrasound or abdominal CT. Her negative PPD and Candida antigen control results may suggest underlying immune dysregulation or suppression, though anergy could be secondary to sepsis.
Given her negative initial infectious evaluation, other etiologies such as atypical infections, rheumatologic disorders, and malignancies warrant consideration. She has no murmur; however, subacute bacterial endocarditis with a fastidious organism is possible, which could be investigated with a transthoracic echocardiogram. Other tests to consider include blood cultures for fungi and atypical mycobacterial species, and serology for Coxiella burnetii, chikungunya virus, and yellow fever. Rheumatologic conditions such as systemic lupus erythematosus, hemophagocytic lymphohistiocytosis (HLH), or adult Still’s disease should be considered. Complement levels and an antinuclear antibody panel, including those for dsDNA and Smith antigen, should be performed to evaluate for systemic lupus erythematosus. Serum ferritin, fibrinogen, and triglyceride levels should be measured to evaluate for HLH. Hematologic malignancy is also a consideration, particularly given her pancytopenia. Multicentric Castleman disease can cause prolonged fevers, pancytopenia, and elevated inflammatory markers, but is less likely without lymphadenopathy. A peripheral blood smear should be sent, and a bone marrow biopsy may be needed.
Empiric ciprofloxacin was initiated; however, the patient continued to have fevers up to 39.9 °C, abdominal pain, and myalgia. Ferritin level was over 3,000 ng/mL (reference range, 8-255 ng/mL), and a soluble interleukin-2 (IL-2) receptor level was 1,188 units/mL (reference range, 45-1,105 units/mL). Triglycerides were normal.
The elevated ferritin and soluble IL-2 levels raise concern for HLH. Hyperferritinemia is relatively nonspecific because extremely elevated ferritin can be seen with other conditions, such as renal failure, hepatocellular injury, infection, rheumatologic conditions, and hematologic malignancy. Soluble IL-2 receptor elevation is more specific for HLH than ferritin or triglycerides, but alone does not make the diagnosis because it can be elevated in other rheumatologic disorders and malignancy. The HLH-2004 criteria are commonly used and require either molecular diagnostic testing or meeting at least five out of eight clinical and lab criteria to make the diagnosis. Our patient currently meets three criteria (fever, splenomegaly, and elevated ferritin). Elevated soluble IL-2 is part of the HLH-2004 criteria, but her level of elevation does not meet the required threshold (≥2,400 units/mL). Her cytopenias have also not quite met the HLH-2004 thresholds (two of the following three: hemoglobin <9 g/dL, platelets <100,000/µL, and/or absolute neutrophil count <1,000/µL). Elevated aminotransferase levels and DIC are not part of the HLH-2004 criteria but are often seen with HLH.
Evaluation for an underlying infectious, rheumatologic, or malignant trigger should continue as previously discussed. If this patient does have HLH, it is most likely secondary to an infection, autoimmune disease, or malignancy rather than genetic HLH. HLH has a high mortality rate, but before beginning treatment with immunosuppressive agents, a peripheral smear and a bone marrow biopsy should be performed to evaluate for hematologic malignancy or signs of hemophagocytosis.
Empiric ciprofloxacin covers most bacterial etiologies of diarrhea, including those previously mentioned such as cholera and most strains of S enterica. Her symptoms and laboratory findings (including cytopenias, elevated aminotransferases, and coagulopathy) could suggest enteric fever due to S enterica serovar Typhi, which is endemic in Kenya. Results of blood and stool cultures, though negative, are relatively insensitive for this organism, particularly this far into the illness course. A bone marrow biopsy may also help with diagnosis of occult typhoid fever because marrow culture can be more sensitive than blood or stool culture.
A bone marrow aspiration revealed hemophagocytic histiocytes, no malignant cells, and negative bacterial (including anaerobic), fungal, and acid-fast bacilli cultures. Considering the high mortality rate of untreated HLH/macrophage activation syndrome (MAS), empiric glucocorticoid administration was considered. However, this was withheld due to concern for ongoing undetected infection given her persistent fever and systemic symptoms.
There should still be high suspicion for HLH. Further evaluation for other laboratory manifestations of HLH such as fibrinogen and natural killer cell activity should be considered, as well as repeating her complete blood count to see if her cytopenias have progressed. Her marrow shows no evidence of hematologic malignancy, so other triggers of possible HLH should be sought out by continuing the workup. Consulting specialists from rheumatology and infectious disease may help clarify possible underlying diagnoses and the best management plan. If she continues to have organ damage or clinically worsens, it may be prudent to empirically broaden her antibiotic coverage and begin antifungal agents while starting glucocorticoid therapy for suspected HLH.
A stool molecular screen from admission was returned positive for S enterica serovar Typhi. Ciprofloxacin was discontinued and ceftriaxone was started out of concern for antibiotic resistance. On hospital day 14, the patient’s brother presented to the ED with fever. His blood and stool cultures were positive for S enterica serovar Typhi with intermediate sensitivity to ciprofloxacin and sensitivity to ceftriaxone. With continued treatment with ceftriaxone, the patient improved significantly. Following discharge, she remained afebrile and asymptomatic. During outpatient follow up, a repeat PPD was positive and she was diagnosed with and treated for latent tuberculosis.
COMMENTARY
The evaluation of a patient who has recently emigrated from a foreign nation requires a broad differential diagnosis and a keen awareness of the clinical conditions present in the patient’s country of origin. This often involves knowledge of diseases infrequently encountered in daily practice, as well as awareness of the nuances of rare presentations and possible complications. When the presentation is not classic for a relevant infectious disease and clinical conditions from other diagnostic classes are considered, the evaluation and management of the patient is particularly challenging.
Typhoid fever is a severe systemic illness caused by the organism S enterica serovar Typhi. The organism is ingested, penetrates the small intestinal epithelium, enters the lymphoid tissue, and disseminates via the lymphatic and hematogenous routes. Onset of symptoms typically occurs 5 to 21 days after ingestion of contaminated food or water. Clinical features include fever, chills, relative bradycardia (pulse-temperature dissociation), abdominal pain, rose spots (salmon-colored macules) on the trunk and abdomen, and hepatosplenomegaly. Diarrhea is not a typical symptom of patients with typhoid fever, which can lead to a delayed or missed diagnosis. Life-threatening complications can be seen, including gastrointestinal bleeding, intestinal perforation, and meningitis.1 Typhoid fever is most prevalent in impoverished areas with poor access to sanitation. Regions with the highest incidence include south-central Asia, southeast Asia, and southern Africa.2-4 Approximately 200 to 300 cases are reported in the United States each year.5
Classically, the diagnosis is made by means of clinical symptoms and a positive culture from a sterile site. A recent study of 529 patients found that 61% had positive blood cultures and 96% had positive bone marrow cultures.6 Our patient’s diagnosis was significantly delayed by multiple negative cultures and failure to improve on first-line antibiotics, which initially suggested that the S enterica serovar Typhi stool molecular screen likely represented carriage caused by colonization. Chronic S enterica serovar Typhi carriage is defined as excretion of the organism in stool or urine 1 year or longer after acute infection. Rates of carriage range from 1% to 6%, and up to 25% of carriers have no history of typhoid fever.1,7,8 Carriage is more common in females and in those with biliary tract abnormalities.9,10
Once a presumptive diagnosis is made, antibiotic choice remains a challenge. Resistance to fluoroquinolones, the preferred drug for multidrug-resistant typhoid fever, is growing but remains rare, at approximately 5%.11,12 Ceftriaxone and azithromycin have been used successfully in areas with high resistance.13 Given the patient’s slow response to therapy even after transitioning from ciprofloxacin to ceftriaxone, her brother’s presentation and obtaining the antibiotic sensitivities for his organism were critical to confirming that our diagnosis and management decisions were correct.
One strongly considered diagnosis was HLH/MAS. MAS is an aggressive syndrome of excessive inflammation and tissue destruction caused by inappropriate immune system activation. It belongs to a group of histiocytic disorders collectively known as HLH. Aside from primary (genetic) forms, secondary forms exist that can be triggered by malignancy, infection, or rheumatologic disorders. In infection-associated HLH/MAS, viral infections are a common trigger, with Epstein-Barr virus being the most common. Association with bacterial infections, including tuberculosis and typhoid fever, has also been reported.14 Prompt therapy, often with immunosuppressive agents such as glucocorticoids, is essential for survival because there is a reported mortality rate of up to 50% when untreated.15 When infection-induced HLH/MAS occurs, treatment of the underlying infection is critical.14,15 The greatest barrier to a favorable outcome from HLH/MAS is often a delay in diagnosis because the rarity of this disease, the variable clinical presentation, and the lack of specificity of the clinical and laboratory findings make a conclusive diagnosis challenging.
In the presented case, diagnostic uncertainty challenged the decision to administer systemic glucocorticoids. Glucocorticoids conferred a risk of harm for multiple diagnoses that remained on the differential, including malignancy and infection. Her diagnostic evaluation made malignancy less likely, but because testing was unable to rule out tuberculosis as either the underlying cause or coinfection, the team opted to defer initiating glucocorticoids and instead closely monitor for a worsening inflammatory response. Following appropriate treatment of her systemic infection, her PPD was repeated and became positive. The negative PPD and Candida control obtained during her hospitalization were, therefore, likely caused by anergy in the setting of overwhelming systemic illness. Initiation of glucocorticoids prematurely in this case could have led to further harm because immunosuppression may have led to reactivation of latent tuberculosis or exacerbation of illness from an alternative but then undiagnosed infection.
The patient’s ultimate unifying diagnosis was typhoid fever; however, there are mixed expert opinions as to whether the systemic immune activation was significant enough to merit the diagnosis of infection-induced secondary HLH/MAS. Despite the high morbidity and mortality that can accompany HLH/MAS, it has been reported that a significant proportion of cases of secondary HLH/MAS can be managed effectively with treatment of the underlying etiology; this may have been the case for our patient.14,15 The clinicians in this case were caught between diagnoses, unable to safely reach either one—much like a baseball player stranded between bases. Fortunately for this patient, the diagnosis ultimately emerged after a careful and thorough workup, assisted by the more straightforward diagnosis of her brother with the same disease.
KEY TEACHING POINTS
- Salmonella enterica serovar Typhi has a high false-negative rate in blood and stool cultures; therefore, clinical suspicion should remain high in the setting of a high pre-test probability.
- Fluoroquinolones are traditionally first-line therapy for typhoid fever, but the use of ceftriaxone and azithromycin is increasing because of rising fluoroquinolone resistance.
- Hemophagocytic lymphohistiocytosis/macrophage activation syndrome is characterized by excessive inflammation and tissue destruction caused by inappropriate immune system activation. This syndrome can be fatal without appropriate immunosuppressive therapy; however, glucocorticoid administration must be pursued with caution when infection and malignancy are on the differential diagnosis.
1. Parry CM, Hien TT, Dougan G, et al. Typhoid fever. N Engl J Med. 2002;347(22):1770-1782. https://doi.org/10.1056/nejmra020201
2. Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82(5):346-353.
3. Buckle GC, Walker CL, Black RE. Typhoid fever and paratyphoid fever: systematic review to estimate global morbidity and mortality for 2010. J Glob Health. 2012;2(1):010401. https://doi.org/10.7189/jogh.02.010401
4. Mogasale V, Maskery B, Ochiai RL, et al. Burden of typhoid fever in low-income and middle-income countries: a systematic, literature-based update with risk-factor adjustment. Lancet Glob Health. 2014;2(10):e570-e580. https://doi.org/10.1016/s2214-109x(14)70301-8
5. Lynch MF, Blanton EM, Bulens S, et al. Typhoid fever in the United States, 1999-2006. JAMA. 2009;302(8):859-865. https://doi.org/10.1001/jama.2009.1229
6. Mogasale V, Ramani E, Mogasale VV, Park J. What proportion of Salmonella typhi cases are detected by blood culture? a systematic literature review. Ann Clin Microbiol Antimicrob. 2016;15(1):32. https://doi.org/10.1186/s12941-016-0147-z
7. Merselis JG Jr, Kaye D, Connolly CS, Hook EW. Quantitative bacteriology of the Typhoid carrier state. Am J Trop Med Hyg. 1964;13:425-429. https://doi.org/10.4269/ajtmh.1964.13.425
8. Lanata CF, Levine MM, Ristori C, et al. Vi serology in detection of chronic Salmonella typhi carriers in an endemic area. Lancet. 1983;2(8347):441-443. https://doi.org/10.1016/s0140-6736(83)90401-4
9. Lai CW, Chan RC, Cheng AF, Sung JY, Leung JW. Common bile duct stones: a cause of chronic salmonellosis. Am J Gastroenterol. 1992;87(9):1198-1199.
10. Hofmann E, Chianale J, Rollán A, Pereira J, Ferrecio C, Sotomayor V. Blood group antigen secretion and gallstone disease in the Salmonella typhi chronic carrier state. J Infect Dis. 1993;167(4):993-994. https://doi.org/10.1093/infdis/167.4.993
11. Steel AD, Hay Burgess DC, Diaz Z, Carey ME, Zaidi AKM. Challenges and opportunities for typhoid fever control: a call for coordinated action. Clin Infect Dis. 2016;62 (Suppl 1):S4-S8. https://doi.org/10.1093/cid/civ976
12. Hendriksen RS, Leekitcharoenphon P, Lukjancenko O, et al. Genomic signature of multidrug resistant Salmonella enterica serovar Typhi isolates related to a massive outbreak in Zambia between 2010 and 2012. J Clin Microbiol. 2015;53(1):262-272. https://doi.org/10.1128/jcm.02026-14
13. Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of Salmonella infections. Clin Microbiol Rev. 2015;28(4):901-936. https://doi.org/10.1128/cmr.00002-15
14. Rouphael NG, Talati NJ, Vaughan C, Cunningham K, Moreira R, Gould C. Infections associated with haemophagocytic syndrome. Lancet Infect Dis. 2007;7(12):814-822. https://doi.org/10.1016/s1473-3099(07)70290-6
15. Fisman DN. Hemophagocytic syndromes and infection. Emerg Infect Dis. 2000;6(6):601-608. https://doi.org/10.3201/eid0606.000608
1. Parry CM, Hien TT, Dougan G, et al. Typhoid fever. N Engl J Med. 2002;347(22):1770-1782. https://doi.org/10.1056/nejmra020201
2. Crump JA, Luby SP, Mintz ED. The global burden of typhoid fever. Bull World Health Organ. 2004;82(5):346-353.
3. Buckle GC, Walker CL, Black RE. Typhoid fever and paratyphoid fever: systematic review to estimate global morbidity and mortality for 2010. J Glob Health. 2012;2(1):010401. https://doi.org/10.7189/jogh.02.010401
4. Mogasale V, Maskery B, Ochiai RL, et al. Burden of typhoid fever in low-income and middle-income countries: a systematic, literature-based update with risk-factor adjustment. Lancet Glob Health. 2014;2(10):e570-e580. https://doi.org/10.1016/s2214-109x(14)70301-8
5. Lynch MF, Blanton EM, Bulens S, et al. Typhoid fever in the United States, 1999-2006. JAMA. 2009;302(8):859-865. https://doi.org/10.1001/jama.2009.1229
6. Mogasale V, Ramani E, Mogasale VV, Park J. What proportion of Salmonella typhi cases are detected by blood culture? a systematic literature review. Ann Clin Microbiol Antimicrob. 2016;15(1):32. https://doi.org/10.1186/s12941-016-0147-z
7. Merselis JG Jr, Kaye D, Connolly CS, Hook EW. Quantitative bacteriology of the Typhoid carrier state. Am J Trop Med Hyg. 1964;13:425-429. https://doi.org/10.4269/ajtmh.1964.13.425
8. Lanata CF, Levine MM, Ristori C, et al. Vi serology in detection of chronic Salmonella typhi carriers in an endemic area. Lancet. 1983;2(8347):441-443. https://doi.org/10.1016/s0140-6736(83)90401-4
9. Lai CW, Chan RC, Cheng AF, Sung JY, Leung JW. Common bile duct stones: a cause of chronic salmonellosis. Am J Gastroenterol. 1992;87(9):1198-1199.
10. Hofmann E, Chianale J, Rollán A, Pereira J, Ferrecio C, Sotomayor V. Blood group antigen secretion and gallstone disease in the Salmonella typhi chronic carrier state. J Infect Dis. 1993;167(4):993-994. https://doi.org/10.1093/infdis/167.4.993
11. Steel AD, Hay Burgess DC, Diaz Z, Carey ME, Zaidi AKM. Challenges and opportunities for typhoid fever control: a call for coordinated action. Clin Infect Dis. 2016;62 (Suppl 1):S4-S8. https://doi.org/10.1093/cid/civ976
12. Hendriksen RS, Leekitcharoenphon P, Lukjancenko O, et al. Genomic signature of multidrug resistant Salmonella enterica serovar Typhi isolates related to a massive outbreak in Zambia between 2010 and 2012. J Clin Microbiol. 2015;53(1):262-272. https://doi.org/10.1128/jcm.02026-14
13. Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of Salmonella infections. Clin Microbiol Rev. 2015;28(4):901-936. https://doi.org/10.1128/cmr.00002-15
14. Rouphael NG, Talati NJ, Vaughan C, Cunningham K, Moreira R, Gould C. Infections associated with haemophagocytic syndrome. Lancet Infect Dis. 2007;7(12):814-822. https://doi.org/10.1016/s1473-3099(07)70290-6
15. Fisman DN. Hemophagocytic syndromes and infection. Emerg Infect Dis. 2000;6(6):601-608. https://doi.org/10.3201/eid0606.000608
© 2021 Society of Hospital Medicine
Striking While the Iron Is Hot: Using the Updated PHM Competencies in Time-Variable Training
In July 2020, the revision of The Pediatric Hospital Medicine Core Competencies was published, bringing to fruition three years of meticulous work.1 The working group produced 66 chapters outlining the knowledge, skills, and attitudes needed for competent pediatric hospitalist practice. The arrival of these competencies is especially prescient given pediatric hospital medicine’s (PHM’s) relatively new standing as an American Board of Medical Specialties certified subspecialty, as the competencies can serve as a guide for improvement of fellowship curricula, assessment systems, and faculty development. The competencies also represent an opportunity for PHM to take a bold step forward in the world of graduate medical education (GME) by realizing a key tenet of competency-based medical education (CBME)—competency-based, time-variable training (CBTVT), in which learners train until competence is achieved rather than for a predetermined duration.2,3 In this perspective, we describe how medical education in the United States adopted a time-based training paradigm (in which time-in-training is a surrogate for competence), how CBME has brought time-variable training to the fore, and how PHM has an opportunity to be on the leading edge of education innovation.
TIME-BASED TRAINING IN THE UNITED STATES
In the 1800s, during the time of the “Wild West,” medical education in the United States matched this moniker. There was little standardization across the multiple training pathways to become a practicing physician, including apprenticeships, lecture series, and university courses.4 Predictably, this led to significant heterogeneity in the quality of medical care that a patient of the day received. This problem became clearer as Americans traveled to Europe and witnessed more structured and rigorous training programs, only to return to the comparatively poor state of medical education back home.5 There was a clear need for curricular standardization.
In 1876, the American Medical College Association (which later became the Association of American Medical Colleges [AAMC]) was founded to meet this need, and in 1905 the Association adopted a set of minimum standards for medical training that included the now-familiar two years of basic sciences and two years of clinical training.6 Two subsequent national surveys in the United States were commissioned to evaluate whether medical schools met this new standard, with both surveys finding that roughly half of existing programs passed muster.7,8 As a result, nearly half of US medical schools had closed by 1920 in a crusade to standardize curricula and produce competent physicians. By the time the American Medical Association established initial standards for internship (an archetype of GME),4 time-based medical training was the dominant paradigm. This historical perspective highlights the rationale for standardization of education processes and curricula, particularly in terms of accountability to the American public. But heralded by the 1978 landmark paper by McGaghie et al,9 the paradigm began to shift in the late twentieth century from a focus on the process of physician training to outcomes.
CBME AND TIME VARIABILITY
In contrast to the process-focused model of the early 1900s, CBME starts by identifying patient and healthcare system needs, defining competencies required to meet those needs, and then designing curricular and assessment processes to help learners achieve those competencies.2 This outcomes-based approach grew as a response to calls for greater accountability to the public due to evidence that some graduates were unprepared for unsupervised practice, raising concerns that strictly time-based training was no longer defensible.10 CBME aims to mitigate these concerns by starting with desired outcomes of training and working backward to ensure those outcomes are met.
While many programs have attempted to implement CBME, most still rely heavily on time-in-training to determine competence. Learners participate in structured curricula and, unless they are extreme outliers, are deemed ready for unsupervised practice after a predetermined duration. This model presumes that competence and time are related in a fixed, predictable manner and that learners gain competence at a uniform rate. However, learners do not, in fact, progress uniformly. A study by Schumacher et al11 involving 23 pediatric residency programs showed significant interlearner variability in rates of entrustment (used as a surrogate for competence), leading the authors to call for time-variable training in GME. Significant interlearner variation in rates of competence attainment have been shown in other specialties as well.12 As more CBME studies on training outcomes emerge, the evidence is mounting that not all learners need the same duration of training to become competent providers. Time-in-training and competence attainment are not related in a fixed manner. As Dr Jason13 wrote in 1969, “By making time a constant, we make achievement a variable.” Variable achievement (competence, outcomes) was the very driver for medical education’s shift to a competency-based approach. If variable competence was not acceptable then, why should it be now? The goal of CBTVT is not shorter training, but rather flexible, individualized training both in terms of content and duration. While this also means some learners may need to extend their training, this should already be part of GME programs that are required to have remediation policies for learners who are not progressing as expected.
AN OPPORTUNITY FOR PHM
Time variability is an oft-cited tenet of CBME,2,3 but one that is being piloted by relatively few programs in the United States, mostly in undergraduate medical education (UME).14-16 The Education in Pediatrics Across the Continuum (EPAC), a consortium consisting of four institutions piloting CBTVT in UME,14 has shown early evidence of feasibility17 and that UME graduates from CBTVT programs enter residency with levels of competence similar to those of graduates of traditional time-based programs.18 We believe that PHM can take a step toward truly realizing CBME by implementing CBTVT in fellowship programs.
There are multiple reasons why this is an opportune time for PHM fellowships to consider CBTVT. First, PHM is a relatively new board-certified subspecialty with a recently revised set of core competencies1 that are likely to catalyze programmatic innovation. A key step in change management is building on previous efforts to generate more change.19 Programs can leverage the momentum from current and impending change initiatives to innovate and implement CBTVT. Second, the revised PHM competencies provide the first crucial step in implementing a CBME program by defining desired training outcomes necessary to deliver high-quality patient care. With PHM competencies now well defined, programs can focus on developing programs of assessment and corresponding faculty development, which can help deliver valid, defensible decisions about fellow competence.
Finally, PHM has a workforce that can support CBTVT. A major barrier to time-variable training in GME is the need for trainees-as-workforce. In many GME programs, residents and fellows provide a relatively inexpensive, renewable workforce. Trainees’ clinical rotations are often scheduled up to 1 year in advance to ensure care teams are fully staffed, particularly in the inpatient setting, creating a system where flexibility in training is impossible without creating gaps in clinical coverage. However, many PHM fellowships do not completely rely on fellows to cover clinical service lines. PHM fellows spend 32 weeks over 2 years in core clinical rotations with faculty supervision, in accordance with the Accreditation Council for Graduate Medical Education program requirements, both for 2- and 3-year programs. Some CBME experts estimate (based on previous and ongoing CBTVT pilots) that training duration is likely to vary by roughly 20% from current time-based practices when CBTVT is initially implemented.20 Thus, only a small number of clinical service weeks are likely to be affected. If a fellow were deemed ready for unsupervised practice before finishing 2 years of fellowship in a CBTVT program, the corresponding faculty supervisor could use the time previously assigned for supervision to pursue other priorities, such as education, scholarship, or quality improvement. Why provide supervision if a clinical competency committee has deemed a fellow ready for unsupervised practice? Some level of observation and formative feedback could continue, but full supervision would be redundant and unnecessary. CBTVT would allow for some fellows to experience the uncertainty that comes with unsupervised decision-making while still in an environment with trusted fellowship mentors and advisors.
STEPS TOWARD CHANGE
PHM fellowship programs likely cannot flip a switch to “turn on” CBTVT immediately, but they can take steps toward making the transition. Validity, or defensibility of decisions, will be crucial for assessment in CBTVT systems. Programs will need to develop robust assessment systems that collect myriad data to answer the question, “When is this learner competent to deliver high-quality care without supervision?” Programs can align assessment instruments, faculty-development initiatives, and clinical competency committee (CCC) processes with the 2020 PHM competencies to provide a defensible answer. Program leaders should then seek validity evidence, either in existing literature or through novel scholarly initiatives, to support these summative decisions. Engaging all fellowship stakeholders in transitions to CBTVT will be important and should include fellows, program directors, CCC members, clinical leadership, and members from accrediting and credentialing bodies.
CONCLUSION
As fellowship programs review and revise curricula and assessment systems around the updated PHM core competencies, they should also consider what changes are necessary to implement CBTVT. Time variability is not a novelty but, rather, is a corollary to the outcomes-based approach of CBME. PHM fellowships should strike while the iron is hot and build on current change initiatives prompted by the growth of our specialty to be leaders in CBTVT.
1. Maniscalco J, Gage S, Sofia Teferi M, Fisher ES. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
2. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
3. Lucey CR, Thibault GE, Ten Cate O. Competency-based, tme-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1-S5. https://doi.org/10.1097/ACM.0000000000002080
4. Custers EJFM, Ten Cate O. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49-S54. https://doi.org/10.1097/ACM.0000000000002079
5. Barr DA. Revolution or evolution? Putting the Flexner Report in context. Med Educ. 2011;45(1):17-22. https://doi.org/10.1111/j.1365-2923.2010.03850.x
6. Association of American Medical Colleges. Minutes of the Fifteenth Annual Meeting. April 10, 1905; Chicago, IL.
7. Bevan A. Council on Medical Education of the American Medical Association. JAMA. 1907;48(20):1701-1707.
8. Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
9. McGaghie WC, Sajid AW, Miller GE, et al. Competency-based curriculum development in medical education: an introduction. Public Health Pap. 1978;(68):11-91.
10. Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568-573. https://doi.org/10.1080/0142159X.2017.1315069
11. Schumacher DJ, West DC, Schwartz A, et al. Longitudinal assessment of resident performance using entrustable professional activities. JAMA Netw Open. 2020;3(1):e1919316. https://doi.org/10.1001/jamanetworkopen.2019.19316
12. Warm EJ, Held J, Hellman M, et al. Entrusting observable practice activities and milestones over the 36 months of an internal medicine residency. Acad Med. 2016;91(10):1398-1405. https://doi.org/10.1097/ACM.0000000000001292
13. Jason H. Effective medical instruction: requirements and possibilities. In: Proceedings of a 1969 International Symposium on Medical Education. Medica; 1970:5-8.
14. Andrews JS, Bale JF Jr, Soep JB, et al. Education in Pediatrics Across the Continuum (EPAC): first steps toward realizing the dream of competency-based education. Acad Med. 2018;93(3):414-420. https://doi.org/10.1097/ACM.0000000000002020
15. Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42-S48. https://doi.org/10.1097/ACM.0000000000002068
16. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
17. Murray KE, Lane JL, Carraccio C, et al. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94(3):338-345. https://doi.org/10.1097/ACM.0000000000002535
18. Schwartz A, Balmer DF, Borman-Shoap E, et al. Shared mental models among clinical competency committees in the context of time-variable, competency-based advancement to residency. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S95-S102. https://doi.org/10.1097/ACM.0000000000003638
19. Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review. May-June 1995. Accessed March 1, 2021. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
20. Schumacher DJ, Caretta-Weyer H, Busari J, et al. Competency-based time-variable training internationally: ensuring practical next steps. Med Teach. Forthcoming.
In July 2020, the revision of The Pediatric Hospital Medicine Core Competencies was published, bringing to fruition three years of meticulous work.1 The working group produced 66 chapters outlining the knowledge, skills, and attitudes needed for competent pediatric hospitalist practice. The arrival of these competencies is especially prescient given pediatric hospital medicine’s (PHM’s) relatively new standing as an American Board of Medical Specialties certified subspecialty, as the competencies can serve as a guide for improvement of fellowship curricula, assessment systems, and faculty development. The competencies also represent an opportunity for PHM to take a bold step forward in the world of graduate medical education (GME) by realizing a key tenet of competency-based medical education (CBME)—competency-based, time-variable training (CBTVT), in which learners train until competence is achieved rather than for a predetermined duration.2,3 In this perspective, we describe how medical education in the United States adopted a time-based training paradigm (in which time-in-training is a surrogate for competence), how CBME has brought time-variable training to the fore, and how PHM has an opportunity to be on the leading edge of education innovation.
TIME-BASED TRAINING IN THE UNITED STATES
In the 1800s, during the time of the “Wild West,” medical education in the United States matched this moniker. There was little standardization across the multiple training pathways to become a practicing physician, including apprenticeships, lecture series, and university courses.4 Predictably, this led to significant heterogeneity in the quality of medical care that a patient of the day received. This problem became clearer as Americans traveled to Europe and witnessed more structured and rigorous training programs, only to return to the comparatively poor state of medical education back home.5 There was a clear need for curricular standardization.
In 1876, the American Medical College Association (which later became the Association of American Medical Colleges [AAMC]) was founded to meet this need, and in 1905 the Association adopted a set of minimum standards for medical training that included the now-familiar two years of basic sciences and two years of clinical training.6 Two subsequent national surveys in the United States were commissioned to evaluate whether medical schools met this new standard, with both surveys finding that roughly half of existing programs passed muster.7,8 As a result, nearly half of US medical schools had closed by 1920 in a crusade to standardize curricula and produce competent physicians. By the time the American Medical Association established initial standards for internship (an archetype of GME),4 time-based medical training was the dominant paradigm. This historical perspective highlights the rationale for standardization of education processes and curricula, particularly in terms of accountability to the American public. But heralded by the 1978 landmark paper by McGaghie et al,9 the paradigm began to shift in the late twentieth century from a focus on the process of physician training to outcomes.
CBME AND TIME VARIABILITY
In contrast to the process-focused model of the early 1900s, CBME starts by identifying patient and healthcare system needs, defining competencies required to meet those needs, and then designing curricular and assessment processes to help learners achieve those competencies.2 This outcomes-based approach grew as a response to calls for greater accountability to the public due to evidence that some graduates were unprepared for unsupervised practice, raising concerns that strictly time-based training was no longer defensible.10 CBME aims to mitigate these concerns by starting with desired outcomes of training and working backward to ensure those outcomes are met.
While many programs have attempted to implement CBME, most still rely heavily on time-in-training to determine competence. Learners participate in structured curricula and, unless they are extreme outliers, are deemed ready for unsupervised practice after a predetermined duration. This model presumes that competence and time are related in a fixed, predictable manner and that learners gain competence at a uniform rate. However, learners do not, in fact, progress uniformly. A study by Schumacher et al11 involving 23 pediatric residency programs showed significant interlearner variability in rates of entrustment (used as a surrogate for competence), leading the authors to call for time-variable training in GME. Significant interlearner variation in rates of competence attainment have been shown in other specialties as well.12 As more CBME studies on training outcomes emerge, the evidence is mounting that not all learners need the same duration of training to become competent providers. Time-in-training and competence attainment are not related in a fixed manner. As Dr Jason13 wrote in 1969, “By making time a constant, we make achievement a variable.” Variable achievement (competence, outcomes) was the very driver for medical education’s shift to a competency-based approach. If variable competence was not acceptable then, why should it be now? The goal of CBTVT is not shorter training, but rather flexible, individualized training both in terms of content and duration. While this also means some learners may need to extend their training, this should already be part of GME programs that are required to have remediation policies for learners who are not progressing as expected.
AN OPPORTUNITY FOR PHM
Time variability is an oft-cited tenet of CBME,2,3 but one that is being piloted by relatively few programs in the United States, mostly in undergraduate medical education (UME).14-16 The Education in Pediatrics Across the Continuum (EPAC), a consortium consisting of four institutions piloting CBTVT in UME,14 has shown early evidence of feasibility17 and that UME graduates from CBTVT programs enter residency with levels of competence similar to those of graduates of traditional time-based programs.18 We believe that PHM can take a step toward truly realizing CBME by implementing CBTVT in fellowship programs.
There are multiple reasons why this is an opportune time for PHM fellowships to consider CBTVT. First, PHM is a relatively new board-certified subspecialty with a recently revised set of core competencies1 that are likely to catalyze programmatic innovation. A key step in change management is building on previous efforts to generate more change.19 Programs can leverage the momentum from current and impending change initiatives to innovate and implement CBTVT. Second, the revised PHM competencies provide the first crucial step in implementing a CBME program by defining desired training outcomes necessary to deliver high-quality patient care. With PHM competencies now well defined, programs can focus on developing programs of assessment and corresponding faculty development, which can help deliver valid, defensible decisions about fellow competence.
Finally, PHM has a workforce that can support CBTVT. A major barrier to time-variable training in GME is the need for trainees-as-workforce. In many GME programs, residents and fellows provide a relatively inexpensive, renewable workforce. Trainees’ clinical rotations are often scheduled up to 1 year in advance to ensure care teams are fully staffed, particularly in the inpatient setting, creating a system where flexibility in training is impossible without creating gaps in clinical coverage. However, many PHM fellowships do not completely rely on fellows to cover clinical service lines. PHM fellows spend 32 weeks over 2 years in core clinical rotations with faculty supervision, in accordance with the Accreditation Council for Graduate Medical Education program requirements, both for 2- and 3-year programs. Some CBME experts estimate (based on previous and ongoing CBTVT pilots) that training duration is likely to vary by roughly 20% from current time-based practices when CBTVT is initially implemented.20 Thus, only a small number of clinical service weeks are likely to be affected. If a fellow were deemed ready for unsupervised practice before finishing 2 years of fellowship in a CBTVT program, the corresponding faculty supervisor could use the time previously assigned for supervision to pursue other priorities, such as education, scholarship, or quality improvement. Why provide supervision if a clinical competency committee has deemed a fellow ready for unsupervised practice? Some level of observation and formative feedback could continue, but full supervision would be redundant and unnecessary. CBTVT would allow for some fellows to experience the uncertainty that comes with unsupervised decision-making while still in an environment with trusted fellowship mentors and advisors.
STEPS TOWARD CHANGE
PHM fellowship programs likely cannot flip a switch to “turn on” CBTVT immediately, but they can take steps toward making the transition. Validity, or defensibility of decisions, will be crucial for assessment in CBTVT systems. Programs will need to develop robust assessment systems that collect myriad data to answer the question, “When is this learner competent to deliver high-quality care without supervision?” Programs can align assessment instruments, faculty-development initiatives, and clinical competency committee (CCC) processes with the 2020 PHM competencies to provide a defensible answer. Program leaders should then seek validity evidence, either in existing literature or through novel scholarly initiatives, to support these summative decisions. Engaging all fellowship stakeholders in transitions to CBTVT will be important and should include fellows, program directors, CCC members, clinical leadership, and members from accrediting and credentialing bodies.
CONCLUSION
As fellowship programs review and revise curricula and assessment systems around the updated PHM core competencies, they should also consider what changes are necessary to implement CBTVT. Time variability is not a novelty but, rather, is a corollary to the outcomes-based approach of CBME. PHM fellowships should strike while the iron is hot and build on current change initiatives prompted by the growth of our specialty to be leaders in CBTVT.
In July 2020, the revision of The Pediatric Hospital Medicine Core Competencies was published, bringing to fruition three years of meticulous work.1 The working group produced 66 chapters outlining the knowledge, skills, and attitudes needed for competent pediatric hospitalist practice. The arrival of these competencies is especially prescient given pediatric hospital medicine’s (PHM’s) relatively new standing as an American Board of Medical Specialties certified subspecialty, as the competencies can serve as a guide for improvement of fellowship curricula, assessment systems, and faculty development. The competencies also represent an opportunity for PHM to take a bold step forward in the world of graduate medical education (GME) by realizing a key tenet of competency-based medical education (CBME)—competency-based, time-variable training (CBTVT), in which learners train until competence is achieved rather than for a predetermined duration.2,3 In this perspective, we describe how medical education in the United States adopted a time-based training paradigm (in which time-in-training is a surrogate for competence), how CBME has brought time-variable training to the fore, and how PHM has an opportunity to be on the leading edge of education innovation.
TIME-BASED TRAINING IN THE UNITED STATES
In the 1800s, during the time of the “Wild West,” medical education in the United States matched this moniker. There was little standardization across the multiple training pathways to become a practicing physician, including apprenticeships, lecture series, and university courses.4 Predictably, this led to significant heterogeneity in the quality of medical care that a patient of the day received. This problem became clearer as Americans traveled to Europe and witnessed more structured and rigorous training programs, only to return to the comparatively poor state of medical education back home.5 There was a clear need for curricular standardization.
In 1876, the American Medical College Association (which later became the Association of American Medical Colleges [AAMC]) was founded to meet this need, and in 1905 the Association adopted a set of minimum standards for medical training that included the now-familiar two years of basic sciences and two years of clinical training.6 Two subsequent national surveys in the United States were commissioned to evaluate whether medical schools met this new standard, with both surveys finding that roughly half of existing programs passed muster.7,8 As a result, nearly half of US medical schools had closed by 1920 in a crusade to standardize curricula and produce competent physicians. By the time the American Medical Association established initial standards for internship (an archetype of GME),4 time-based medical training was the dominant paradigm. This historical perspective highlights the rationale for standardization of education processes and curricula, particularly in terms of accountability to the American public. But heralded by the 1978 landmark paper by McGaghie et al,9 the paradigm began to shift in the late twentieth century from a focus on the process of physician training to outcomes.
CBME AND TIME VARIABILITY
In contrast to the process-focused model of the early 1900s, CBME starts by identifying patient and healthcare system needs, defining competencies required to meet those needs, and then designing curricular and assessment processes to help learners achieve those competencies.2 This outcomes-based approach grew as a response to calls for greater accountability to the public due to evidence that some graduates were unprepared for unsupervised practice, raising concerns that strictly time-based training was no longer defensible.10 CBME aims to mitigate these concerns by starting with desired outcomes of training and working backward to ensure those outcomes are met.
While many programs have attempted to implement CBME, most still rely heavily on time-in-training to determine competence. Learners participate in structured curricula and, unless they are extreme outliers, are deemed ready for unsupervised practice after a predetermined duration. This model presumes that competence and time are related in a fixed, predictable manner and that learners gain competence at a uniform rate. However, learners do not, in fact, progress uniformly. A study by Schumacher et al11 involving 23 pediatric residency programs showed significant interlearner variability in rates of entrustment (used as a surrogate for competence), leading the authors to call for time-variable training in GME. Significant interlearner variation in rates of competence attainment have been shown in other specialties as well.12 As more CBME studies on training outcomes emerge, the evidence is mounting that not all learners need the same duration of training to become competent providers. Time-in-training and competence attainment are not related in a fixed manner. As Dr Jason13 wrote in 1969, “By making time a constant, we make achievement a variable.” Variable achievement (competence, outcomes) was the very driver for medical education’s shift to a competency-based approach. If variable competence was not acceptable then, why should it be now? The goal of CBTVT is not shorter training, but rather flexible, individualized training both in terms of content and duration. While this also means some learners may need to extend their training, this should already be part of GME programs that are required to have remediation policies for learners who are not progressing as expected.
AN OPPORTUNITY FOR PHM
Time variability is an oft-cited tenet of CBME,2,3 but one that is being piloted by relatively few programs in the United States, mostly in undergraduate medical education (UME).14-16 The Education in Pediatrics Across the Continuum (EPAC), a consortium consisting of four institutions piloting CBTVT in UME,14 has shown early evidence of feasibility17 and that UME graduates from CBTVT programs enter residency with levels of competence similar to those of graduates of traditional time-based programs.18 We believe that PHM can take a step toward truly realizing CBME by implementing CBTVT in fellowship programs.
There are multiple reasons why this is an opportune time for PHM fellowships to consider CBTVT. First, PHM is a relatively new board-certified subspecialty with a recently revised set of core competencies1 that are likely to catalyze programmatic innovation. A key step in change management is building on previous efforts to generate more change.19 Programs can leverage the momentum from current and impending change initiatives to innovate and implement CBTVT. Second, the revised PHM competencies provide the first crucial step in implementing a CBME program by defining desired training outcomes necessary to deliver high-quality patient care. With PHM competencies now well defined, programs can focus on developing programs of assessment and corresponding faculty development, which can help deliver valid, defensible decisions about fellow competence.
Finally, PHM has a workforce that can support CBTVT. A major barrier to time-variable training in GME is the need for trainees-as-workforce. In many GME programs, residents and fellows provide a relatively inexpensive, renewable workforce. Trainees’ clinical rotations are often scheduled up to 1 year in advance to ensure care teams are fully staffed, particularly in the inpatient setting, creating a system where flexibility in training is impossible without creating gaps in clinical coverage. However, many PHM fellowships do not completely rely on fellows to cover clinical service lines. PHM fellows spend 32 weeks over 2 years in core clinical rotations with faculty supervision, in accordance with the Accreditation Council for Graduate Medical Education program requirements, both for 2- and 3-year programs. Some CBME experts estimate (based on previous and ongoing CBTVT pilots) that training duration is likely to vary by roughly 20% from current time-based practices when CBTVT is initially implemented.20 Thus, only a small number of clinical service weeks are likely to be affected. If a fellow were deemed ready for unsupervised practice before finishing 2 years of fellowship in a CBTVT program, the corresponding faculty supervisor could use the time previously assigned for supervision to pursue other priorities, such as education, scholarship, or quality improvement. Why provide supervision if a clinical competency committee has deemed a fellow ready for unsupervised practice? Some level of observation and formative feedback could continue, but full supervision would be redundant and unnecessary. CBTVT would allow for some fellows to experience the uncertainty that comes with unsupervised decision-making while still in an environment with trusted fellowship mentors and advisors.
STEPS TOWARD CHANGE
PHM fellowship programs likely cannot flip a switch to “turn on” CBTVT immediately, but they can take steps toward making the transition. Validity, or defensibility of decisions, will be crucial for assessment in CBTVT systems. Programs will need to develop robust assessment systems that collect myriad data to answer the question, “When is this learner competent to deliver high-quality care without supervision?” Programs can align assessment instruments, faculty-development initiatives, and clinical competency committee (CCC) processes with the 2020 PHM competencies to provide a defensible answer. Program leaders should then seek validity evidence, either in existing literature or through novel scholarly initiatives, to support these summative decisions. Engaging all fellowship stakeholders in transitions to CBTVT will be important and should include fellows, program directors, CCC members, clinical leadership, and members from accrediting and credentialing bodies.
CONCLUSION
As fellowship programs review and revise curricula and assessment systems around the updated PHM core competencies, they should also consider what changes are necessary to implement CBTVT. Time variability is not a novelty but, rather, is a corollary to the outcomes-based approach of CBME. PHM fellowships should strike while the iron is hot and build on current change initiatives prompted by the growth of our specialty to be leaders in CBTVT.
1. Maniscalco J, Gage S, Sofia Teferi M, Fisher ES. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
2. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
3. Lucey CR, Thibault GE, Ten Cate O. Competency-based, tme-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1-S5. https://doi.org/10.1097/ACM.0000000000002080
4. Custers EJFM, Ten Cate O. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49-S54. https://doi.org/10.1097/ACM.0000000000002079
5. Barr DA. Revolution or evolution? Putting the Flexner Report in context. Med Educ. 2011;45(1):17-22. https://doi.org/10.1111/j.1365-2923.2010.03850.x
6. Association of American Medical Colleges. Minutes of the Fifteenth Annual Meeting. April 10, 1905; Chicago, IL.
7. Bevan A. Council on Medical Education of the American Medical Association. JAMA. 1907;48(20):1701-1707.
8. Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
9. McGaghie WC, Sajid AW, Miller GE, et al. Competency-based curriculum development in medical education: an introduction. Public Health Pap. 1978;(68):11-91.
10. Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568-573. https://doi.org/10.1080/0142159X.2017.1315069
11. Schumacher DJ, West DC, Schwartz A, et al. Longitudinal assessment of resident performance using entrustable professional activities. JAMA Netw Open. 2020;3(1):e1919316. https://doi.org/10.1001/jamanetworkopen.2019.19316
12. Warm EJ, Held J, Hellman M, et al. Entrusting observable practice activities and milestones over the 36 months of an internal medicine residency. Acad Med. 2016;91(10):1398-1405. https://doi.org/10.1097/ACM.0000000000001292
13. Jason H. Effective medical instruction: requirements and possibilities. In: Proceedings of a 1969 International Symposium on Medical Education. Medica; 1970:5-8.
14. Andrews JS, Bale JF Jr, Soep JB, et al. Education in Pediatrics Across the Continuum (EPAC): first steps toward realizing the dream of competency-based education. Acad Med. 2018;93(3):414-420. https://doi.org/10.1097/ACM.0000000000002020
15. Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42-S48. https://doi.org/10.1097/ACM.0000000000002068
16. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
17. Murray KE, Lane JL, Carraccio C, et al. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94(3):338-345. https://doi.org/10.1097/ACM.0000000000002535
18. Schwartz A, Balmer DF, Borman-Shoap E, et al. Shared mental models among clinical competency committees in the context of time-variable, competency-based advancement to residency. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S95-S102. https://doi.org/10.1097/ACM.0000000000003638
19. Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review. May-June 1995. Accessed March 1, 2021. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
20. Schumacher DJ, Caretta-Weyer H, Busari J, et al. Competency-based time-variable training internationally: ensuring practical next steps. Med Teach. Forthcoming.
1. Maniscalco J, Gage S, Sofia Teferi M, Fisher ES. The Pediatric Hospital Medicine Core Competencies: 2020 Revision. J Hosp Med. 2020;15(7):389-394. https://doi.org/10.12788/jhm.3391
2. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
3. Lucey CR, Thibault GE, Ten Cate O. Competency-based, tme-variable education in the health professions: crossroads. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S1-S5. https://doi.org/10.1097/ACM.0000000000002080
4. Custers EJFM, Ten Cate O. The history of medical education in Europe and the United States, with respect to time and proficiency. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S49-S54. https://doi.org/10.1097/ACM.0000000000002079
5. Barr DA. Revolution or evolution? Putting the Flexner Report in context. Med Educ. 2011;45(1):17-22. https://doi.org/10.1111/j.1365-2923.2010.03850.x
6. Association of American Medical Colleges. Minutes of the Fifteenth Annual Meeting. April 10, 1905; Chicago, IL.
7. Bevan A. Council on Medical Education of the American Medical Association. JAMA. 1907;48(20):1701-1707.
8. Flexner A. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, Bulletin Number Four, 1910. Bull World Health Organ. 2002;80(7):594-602.
9. McGaghie WC, Sajid AW, Miller GE, et al. Competency-based curriculum development in medical education: an introduction. Public Health Pap. 1978;(68):11-91.
10. Frank JR, Snell L, Englander R, Holmboe ES, ICBME Collaborators. Implementing competency-based medical education: moving forward. Med Teach. 2017;39(6):568-573. https://doi.org/10.1080/0142159X.2017.1315069
11. Schumacher DJ, West DC, Schwartz A, et al. Longitudinal assessment of resident performance using entrustable professional activities. JAMA Netw Open. 2020;3(1):e1919316. https://doi.org/10.1001/jamanetworkopen.2019.19316
12. Warm EJ, Held J, Hellman M, et al. Entrusting observable practice activities and milestones over the 36 months of an internal medicine residency. Acad Med. 2016;91(10):1398-1405. https://doi.org/10.1097/ACM.0000000000001292
13. Jason H. Effective medical instruction: requirements and possibilities. In: Proceedings of a 1969 International Symposium on Medical Education. Medica; 1970:5-8.
14. Andrews JS, Bale JF Jr, Soep JB, et al. Education in Pediatrics Across the Continuum (EPAC): first steps toward realizing the dream of competency-based education. Acad Med. 2018;93(3):414-420. https://doi.org/10.1097/ACM.0000000000002020
15. Mejicano GC, Bumsted TN. Describing the journey and lessons learned implementing a competency-based, time-variable undergraduate medical education curriculum. Acad Med. 2018;93(3S Competency-Based, Time-Variable Education in the Health Professions):S42-S48. https://doi.org/10.1097/ACM.0000000000002068
16. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
17. Murray KE, Lane JL, Carraccio C, et al. Crossing the gap: using competency-based assessment to determine whether learners are ready for the undergraduate-to-graduate transition. Acad Med. 2019;94(3):338-345. https://doi.org/10.1097/ACM.0000000000002535
18. Schwartz A, Balmer DF, Borman-Shoap E, et al. Shared mental models among clinical competency committees in the context of time-variable, competency-based advancement to residency. Acad Med. 2020;95(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 59th Annual Research in Medical Education Presentations):S95-S102. https://doi.org/10.1097/ACM.0000000000003638
19. Kotter JP. Leading change: why transformation efforts fail. Harvard Business Review. May-June 1995. Accessed March 1, 2021. https://hbr.org/1995/05/leading-change-why-transformation-efforts-fail-2
20. Schumacher DJ, Caretta-Weyer H, Busari J, et al. Competency-based time-variable training internationally: ensuring practical next steps. Med Teach. Forthcoming.
© 2021 Society of Hospital Medicine
Professional Identity Formation During the COVID-19 Pandemic
In 1957, Merton wrote that the primary aim of medical education should be “to provide [learners] with a professional identity so that [they] come to think, act, and feel like a physician.”1 More than a half-century later, the Carnegie Foundation for the Advancement of Teaching echoed his sentiments in its landmark examination of the United States medical education system, which produced four key recommendations for curricular reform, including explicitly addressing professional identity formation (PIF).2 PIF is a process by which a learner transforms into a physician with the values, dispositions, and aspirations of the physician community.3 It is now recognized as crucial to developing physicians who can deliver high-quality care.2
Major changes to the learning environment can impact PIF. For example, when the Accreditation Committee for Graduate Medical Education duty-hour restrictions were implemented in 2003, several educators were concerned that the changes may negatively affect resident PIF,4 whereas others saw an opportunity to refocus curricular efforts on PIF.5 Medical education is now in the midst of another radical change with the novel coronavirus disease 2019 (COVID-19) pandemic. Over the past several months, we have begun to understand the pandemic’s effects on medical education in terms of learner welfare, educational experiences/value, innovation, and assessment.6-8 However, little has been published on the pandemic’s effect on PIF.9 We explore the impact of COVID-19 on physicians’ PIF and identify strategies to support PIF in physicians and other healthcare professionals during times of crisis.
SOCIALIZATION AND COMMUNITIES OF PRACTICE
PIF is dynamic and nonlinear, occurring at every level of the medical education hierarchy (medical student, resident, fellow, attending).10 Emphasis on PIF has grown in recent years as a response to the limitations of behavior-based educational frameworks such as competency-based medical education (CBME),3 which focuses on what the learner can “do.” PIF moves beyond “doing” to consider who the learner “is.”11 PIF occurs at the individual level as learners progress through multiple distinct identity stages during their longitudinal formation10,12-14 but also at the level of the collective. Socialization plays a crucial role; thus, PIF is heavily influenced by the environment, context, and other individuals.10
Medicine can be conceptualized as a community of practice, which is a sustaining network of individuals who share knowledge, beliefs, values, and experiences related to a common practice or purpose.15,16 In a community of practice, learning is social, includes knowledge that is tacit to the community, and is situated within the context in which it will be applied. PIF involves learners moving from “legitimate peripheral participation,” whereby they are accepted as novice community members, to “full participation,” which involves gaining competence in relevant tasks and internalizing community principles to become full partners in the community.13 Critical to this process is exposure to socializing agents (eg, attendings, nurses, peers), observation of community interactions, experiential learning in the clinical environment, and access to role models.10,16 Immersion in the clinical environment with other community members is thus crucial to PIF. This is especially important, as “medicine” is not truly a single community, but rather a “landscape of communities,” each with its own identity.17 Learners must therefore be immersed in many different clinical environments to experience the various communities within our field.
COVID-19 CHANGING THE LEARNING ENVIRONMENT
The pandemic is drastically altering the learning environment in medical education.8 Several institutions temporarily removed medical students from clinical rotations to reduce learner exposure and conserve personal protective equipment. Some residents were removed from nonessential clinical activities for similar reasons. Many attendings have been asked to work from home when not required to be present for clinical care duties. Common medical community activities, such as group meals and conferences, have been altered for physical distancing or simply canceled. Usual clinical care has rapidly evolved, with changes in rounding practices, a boon of telehealth, and cancellations of nonessential procedures. These necessary changes present constantly shifting grounds for anyone trying to integrate into a community and develop a professional identity.
Changes outside of the clinical learning environment are also affecting PIF. Social interactions, such as dinners and peer gatherings, occur via video conference or not at all. Most in-person contact happens with masks in place, physically distanced, and in smaller groups. Resident and student lounges are being modified to physically distance or reduce the number of occupants. There is often variable adherence, both intentional and unintentional, to physical distance and mask mandates, creating potential for confusion as learners try to internalize the values and norms of the medical community. Common professional rituals, such as white coat ceremonies, orientation events, and graduations, have been curtailed or canceled. Even experiences that are not commonly seen as social events but are important in the physician’s journey, such as the residency and fellowship application processes and standardized tests, are being transformed. These changes alter typical social patterns that are important in PIF and may adversely affect high-value social group interactions that serve as buffers against stressors during training.18
Finally, the pandemic has altered the timeline for many learners. Medical students at several institutions graduated early to join the workforce and help care for escalating numbers of patients during the pandemic.7 Some see the pandemic as a catalyst to move toward competency-based time-variable training, in which learners progress through training at variable rates depending on their individual performance and learning needs.19 These changes could shorten the amount of time some learners spend in a given role (eg, medical student, intern). In such situations, it is unclear whether a minimal maturational time is necessary for most learners to fully develop a professional identity.
SUPPORTING PIF DURING THE PANDEMIC
In 2019, Cruess et al published general principles for supporting PIF,17 which have been used to support PIF during the COVID-19 pandemic.20 In the Table, we describe these principles and provide examples of how to implement them in the context of the pandemic. We believe these principles are applicable for PIF in undergraduate medical education, graduate medical education, and faculty development programs. A common thread throughout the principles is that PIF is not a process that should be left to chance, but rather explicitly nurtured through systematic support and curricular initiatives.5 This may be challenging while the COVID-19 pandemic is sapping financial resources and requiring rapid changes to clinical systems, but given the central role PIF plays in physician development, it should be prioritized by educational leaders.
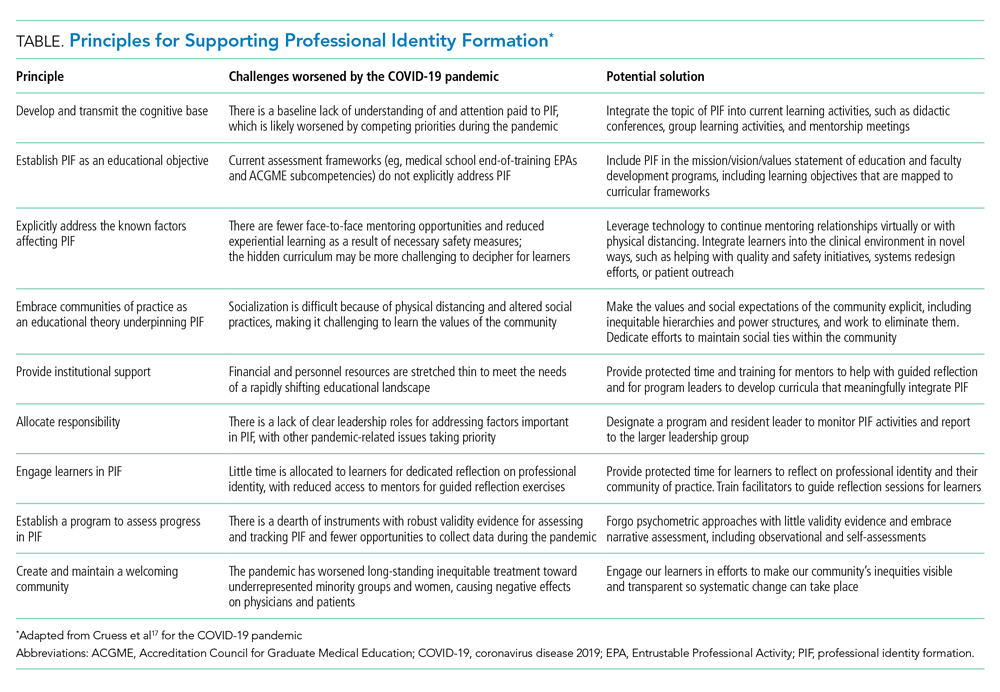
CREATING AND MAINTAINING A WELCOMING COMMUNITY: AN OPPORTUNITY
One of the final principles from Cruess et al is to create and maintain a welcoming community.17 This prompts questions such as: Is our community welcoming to everyone, where “everyone” really does mean everyone? Like other social structures, communities of practice tend to perpetuate existing power structures and inequities.17 It is no secret that medicine, like other professions, is riddled with inequities and bias based on factors such as race, gender, and socioeconomic status.21-23 The COVID-19 pandemic is likely exacerbating these inequities, such as the adverse impacts that are specifically affecting women physicians, who take on a disproportionate share of the child care at home.23 These biases impact not only the members of our professional community but also our patients, contributing to disparities in care and outcomes.
Physicians who have received inequitable treatment have laid bare the ways in which our communities of practice are failing them, and also outlined a better path on which to move forward.21,23 In addition to recruitment practices that promote diversity, meaningful programs should be developed to support inclusion, equity (in recognition, support, compensation), retention, and advancement. The disruption caused by COVID-19 can be a catalyst for this change. By taking this moment of crisis to examine the values and norms of medicine and how we systematically perpetuate harmful inequities and biases, we have an opportunity to deliberately rebuild our community of practice in a manner that helps shape the next generation’s professional identities to be better than we have been. This should always be the aim of education.
1. Merton RK. Some Preliminaries to a Sociology of Medical Education. Harvard University Press; 1957.
2. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. Jossey-Bass; 2010.
3. Irby DM, Hamstra SJ. Parting the clouds: three professionalism frameworks in medical education. Acad Med. 2016;91(12):1606-1611. https://doi.org/10.1097/ACM.0000000000001190
4. Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487-1492. https://doi.org/10.1001/archinte.167.14.1487
5. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-888. https://doi.org/10.1097/ACM.0b013e318257d57d
6. Anderson ML, Turbow S, Willgerodt MA, Ruhnke GW. Education in a crisis: the opportunity of our lives. J Hosp Med. 2020;15(5):287-291. https://doi.org/10.12788/jhm.3431
7. Kinnear B, Kelleher M, Olson AP, Sall D, Schumacher DJ. Developing trust with early medical school graduates during the COVID-19 pandemic. J Hosp Med. 2020;15(6):367-369. https://doi.org/10.12788/jhm.3463
8. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-1142. https://doi.org/10.1097/ACM.0000000000003402
9. Cullum RJ, Shaughnessy A, Mayat NY, Brown ME. Identity in lockdown: supporting primary care professional identity development in the COVID-19 generation. Educ Prim Care. 2020;31(4):200-204. https://doi.org/10.1080/14739879.2020.1779616
10. Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185-1190. https://doi.org/10.1097/ACM.0b013e3182604968
11. Al‐Eraky M, Marei H. A fresh look at Miller’s pyramid: assessment at the ‘Is’ and ‘Do’ levels. Med Educ. 2016;50(12):1253-1257. https://doi.org/10.1111/medu.13101
12. Forsythe GB. Identity development in professional education. Acad Med. 2005;80(10 Suppl):S112-S117. https://doi.org/10.1097/00001888-200510001-0002913.
13. Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718-725. https://doi.org/10.1097/ACM.0000000000000700
14. Kegan R. The Evolving Self: Problem and Process in Human Development. Harvard University Press; 1982.
15. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
16. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press; 1991.
17. Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: general principles. Med Teach. 2019;41(6):641-649. https://doi.org/10.1080/0142159X.2018.1536260
18. Mavor KI, McNeill KG, Anderson K, Kerr A, O’Reilly E, Platow MJ. Beyond prevalence to process: the role of self and identity in medical student well‐being. Med Educ. 2014;48(4):351-360. https://doi.org/10.1111/medu.12375
19. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
20. Stetson GV, Kryzhanovskaya IV, Lomen‐Hoerth C, Hauer KE. Professional identity formation in disorienting times. Med Educ. 2020;54(8):765-766. https://doi.org/10.1111/medu.14202
21. Unaka NI, Reynolds KL. Truth in tension: reflections on racism in medicine. J Hosp Med. 2020;15(9):572-573. https://doi.org/10.12788/jhm.3492
22. Beagan BL. Everyday classism in medical school: experiencing marginality and resistance. Med Educ. 2005;39(8):777-784. https://doi.org/10.1111/j.1365-2929.2005.02225.x
23. Jones Y, Durand V, Morton K, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
In 1957, Merton wrote that the primary aim of medical education should be “to provide [learners] with a professional identity so that [they] come to think, act, and feel like a physician.”1 More than a half-century later, the Carnegie Foundation for the Advancement of Teaching echoed his sentiments in its landmark examination of the United States medical education system, which produced four key recommendations for curricular reform, including explicitly addressing professional identity formation (PIF).2 PIF is a process by which a learner transforms into a physician with the values, dispositions, and aspirations of the physician community.3 It is now recognized as crucial to developing physicians who can deliver high-quality care.2
Major changes to the learning environment can impact PIF. For example, when the Accreditation Committee for Graduate Medical Education duty-hour restrictions were implemented in 2003, several educators were concerned that the changes may negatively affect resident PIF,4 whereas others saw an opportunity to refocus curricular efforts on PIF.5 Medical education is now in the midst of another radical change with the novel coronavirus disease 2019 (COVID-19) pandemic. Over the past several months, we have begun to understand the pandemic’s effects on medical education in terms of learner welfare, educational experiences/value, innovation, and assessment.6-8 However, little has been published on the pandemic’s effect on PIF.9 We explore the impact of COVID-19 on physicians’ PIF and identify strategies to support PIF in physicians and other healthcare professionals during times of crisis.
SOCIALIZATION AND COMMUNITIES OF PRACTICE
PIF is dynamic and nonlinear, occurring at every level of the medical education hierarchy (medical student, resident, fellow, attending).10 Emphasis on PIF has grown in recent years as a response to the limitations of behavior-based educational frameworks such as competency-based medical education (CBME),3 which focuses on what the learner can “do.” PIF moves beyond “doing” to consider who the learner “is.”11 PIF occurs at the individual level as learners progress through multiple distinct identity stages during their longitudinal formation10,12-14 but also at the level of the collective. Socialization plays a crucial role; thus, PIF is heavily influenced by the environment, context, and other individuals.10
Medicine can be conceptualized as a community of practice, which is a sustaining network of individuals who share knowledge, beliefs, values, and experiences related to a common practice or purpose.15,16 In a community of practice, learning is social, includes knowledge that is tacit to the community, and is situated within the context in which it will be applied. PIF involves learners moving from “legitimate peripheral participation,” whereby they are accepted as novice community members, to “full participation,” which involves gaining competence in relevant tasks and internalizing community principles to become full partners in the community.13 Critical to this process is exposure to socializing agents (eg, attendings, nurses, peers), observation of community interactions, experiential learning in the clinical environment, and access to role models.10,16 Immersion in the clinical environment with other community members is thus crucial to PIF. This is especially important, as “medicine” is not truly a single community, but rather a “landscape of communities,” each with its own identity.17 Learners must therefore be immersed in many different clinical environments to experience the various communities within our field.
COVID-19 CHANGING THE LEARNING ENVIRONMENT
The pandemic is drastically altering the learning environment in medical education.8 Several institutions temporarily removed medical students from clinical rotations to reduce learner exposure and conserve personal protective equipment. Some residents were removed from nonessential clinical activities for similar reasons. Many attendings have been asked to work from home when not required to be present for clinical care duties. Common medical community activities, such as group meals and conferences, have been altered for physical distancing or simply canceled. Usual clinical care has rapidly evolved, with changes in rounding practices, a boon of telehealth, and cancellations of nonessential procedures. These necessary changes present constantly shifting grounds for anyone trying to integrate into a community and develop a professional identity.
Changes outside of the clinical learning environment are also affecting PIF. Social interactions, such as dinners and peer gatherings, occur via video conference or not at all. Most in-person contact happens with masks in place, physically distanced, and in smaller groups. Resident and student lounges are being modified to physically distance or reduce the number of occupants. There is often variable adherence, both intentional and unintentional, to physical distance and mask mandates, creating potential for confusion as learners try to internalize the values and norms of the medical community. Common professional rituals, such as white coat ceremonies, orientation events, and graduations, have been curtailed or canceled. Even experiences that are not commonly seen as social events but are important in the physician’s journey, such as the residency and fellowship application processes and standardized tests, are being transformed. These changes alter typical social patterns that are important in PIF and may adversely affect high-value social group interactions that serve as buffers against stressors during training.18
Finally, the pandemic has altered the timeline for many learners. Medical students at several institutions graduated early to join the workforce and help care for escalating numbers of patients during the pandemic.7 Some see the pandemic as a catalyst to move toward competency-based time-variable training, in which learners progress through training at variable rates depending on their individual performance and learning needs.19 These changes could shorten the amount of time some learners spend in a given role (eg, medical student, intern). In such situations, it is unclear whether a minimal maturational time is necessary for most learners to fully develop a professional identity.
SUPPORTING PIF DURING THE PANDEMIC
In 2019, Cruess et al published general principles for supporting PIF,17 which have been used to support PIF during the COVID-19 pandemic.20 In the Table, we describe these principles and provide examples of how to implement them in the context of the pandemic. We believe these principles are applicable for PIF in undergraduate medical education, graduate medical education, and faculty development programs. A common thread throughout the principles is that PIF is not a process that should be left to chance, but rather explicitly nurtured through systematic support and curricular initiatives.5 This may be challenging while the COVID-19 pandemic is sapping financial resources and requiring rapid changes to clinical systems, but given the central role PIF plays in physician development, it should be prioritized by educational leaders.
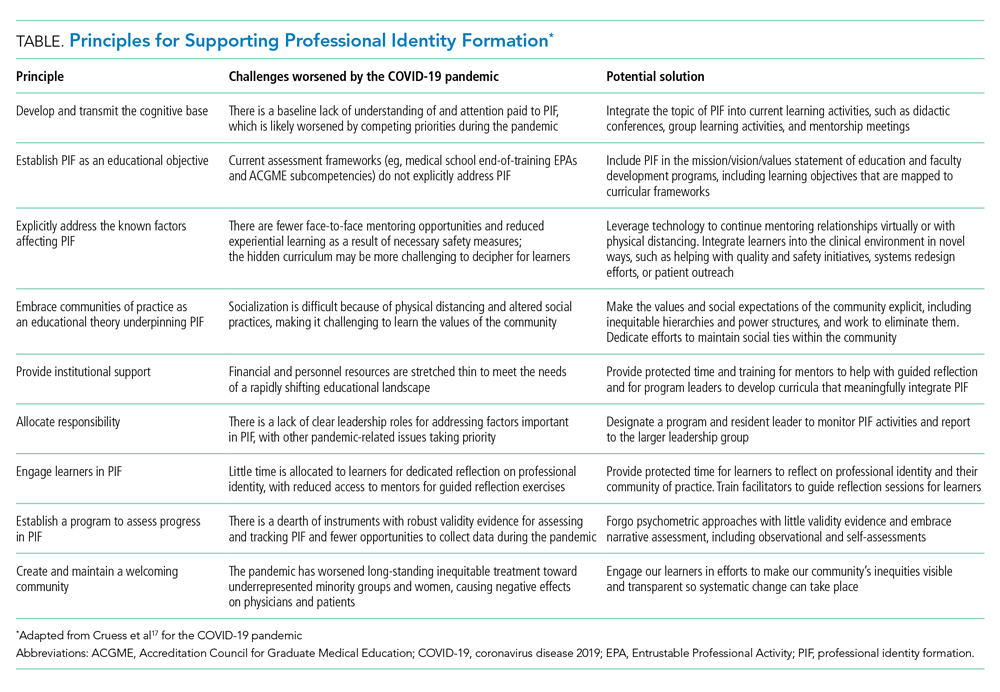
CREATING AND MAINTAINING A WELCOMING COMMUNITY: AN OPPORTUNITY
One of the final principles from Cruess et al is to create and maintain a welcoming community.17 This prompts questions such as: Is our community welcoming to everyone, where “everyone” really does mean everyone? Like other social structures, communities of practice tend to perpetuate existing power structures and inequities.17 It is no secret that medicine, like other professions, is riddled with inequities and bias based on factors such as race, gender, and socioeconomic status.21-23 The COVID-19 pandemic is likely exacerbating these inequities, such as the adverse impacts that are specifically affecting women physicians, who take on a disproportionate share of the child care at home.23 These biases impact not only the members of our professional community but also our patients, contributing to disparities in care and outcomes.
Physicians who have received inequitable treatment have laid bare the ways in which our communities of practice are failing them, and also outlined a better path on which to move forward.21,23 In addition to recruitment practices that promote diversity, meaningful programs should be developed to support inclusion, equity (in recognition, support, compensation), retention, and advancement. The disruption caused by COVID-19 can be a catalyst for this change. By taking this moment of crisis to examine the values and norms of medicine and how we systematically perpetuate harmful inequities and biases, we have an opportunity to deliberately rebuild our community of practice in a manner that helps shape the next generation’s professional identities to be better than we have been. This should always be the aim of education.
In 1957, Merton wrote that the primary aim of medical education should be “to provide [learners] with a professional identity so that [they] come to think, act, and feel like a physician.”1 More than a half-century later, the Carnegie Foundation for the Advancement of Teaching echoed his sentiments in its landmark examination of the United States medical education system, which produced four key recommendations for curricular reform, including explicitly addressing professional identity formation (PIF).2 PIF is a process by which a learner transforms into a physician with the values, dispositions, and aspirations of the physician community.3 It is now recognized as crucial to developing physicians who can deliver high-quality care.2
Major changes to the learning environment can impact PIF. For example, when the Accreditation Committee for Graduate Medical Education duty-hour restrictions were implemented in 2003, several educators were concerned that the changes may negatively affect resident PIF,4 whereas others saw an opportunity to refocus curricular efforts on PIF.5 Medical education is now in the midst of another radical change with the novel coronavirus disease 2019 (COVID-19) pandemic. Over the past several months, we have begun to understand the pandemic’s effects on medical education in terms of learner welfare, educational experiences/value, innovation, and assessment.6-8 However, little has been published on the pandemic’s effect on PIF.9 We explore the impact of COVID-19 on physicians’ PIF and identify strategies to support PIF in physicians and other healthcare professionals during times of crisis.
SOCIALIZATION AND COMMUNITIES OF PRACTICE
PIF is dynamic and nonlinear, occurring at every level of the medical education hierarchy (medical student, resident, fellow, attending).10 Emphasis on PIF has grown in recent years as a response to the limitations of behavior-based educational frameworks such as competency-based medical education (CBME),3 which focuses on what the learner can “do.” PIF moves beyond “doing” to consider who the learner “is.”11 PIF occurs at the individual level as learners progress through multiple distinct identity stages during their longitudinal formation10,12-14 but also at the level of the collective. Socialization plays a crucial role; thus, PIF is heavily influenced by the environment, context, and other individuals.10
Medicine can be conceptualized as a community of practice, which is a sustaining network of individuals who share knowledge, beliefs, values, and experiences related to a common practice or purpose.15,16 In a community of practice, learning is social, includes knowledge that is tacit to the community, and is situated within the context in which it will be applied. PIF involves learners moving from “legitimate peripheral participation,” whereby they are accepted as novice community members, to “full participation,” which involves gaining competence in relevant tasks and internalizing community principles to become full partners in the community.13 Critical to this process is exposure to socializing agents (eg, attendings, nurses, peers), observation of community interactions, experiential learning in the clinical environment, and access to role models.10,16 Immersion in the clinical environment with other community members is thus crucial to PIF. This is especially important, as “medicine” is not truly a single community, but rather a “landscape of communities,” each with its own identity.17 Learners must therefore be immersed in many different clinical environments to experience the various communities within our field.
COVID-19 CHANGING THE LEARNING ENVIRONMENT
The pandemic is drastically altering the learning environment in medical education.8 Several institutions temporarily removed medical students from clinical rotations to reduce learner exposure and conserve personal protective equipment. Some residents were removed from nonessential clinical activities for similar reasons. Many attendings have been asked to work from home when not required to be present for clinical care duties. Common medical community activities, such as group meals and conferences, have been altered for physical distancing or simply canceled. Usual clinical care has rapidly evolved, with changes in rounding practices, a boon of telehealth, and cancellations of nonessential procedures. These necessary changes present constantly shifting grounds for anyone trying to integrate into a community and develop a professional identity.
Changes outside of the clinical learning environment are also affecting PIF. Social interactions, such as dinners and peer gatherings, occur via video conference or not at all. Most in-person contact happens with masks in place, physically distanced, and in smaller groups. Resident and student lounges are being modified to physically distance or reduce the number of occupants. There is often variable adherence, both intentional and unintentional, to physical distance and mask mandates, creating potential for confusion as learners try to internalize the values and norms of the medical community. Common professional rituals, such as white coat ceremonies, orientation events, and graduations, have been curtailed or canceled. Even experiences that are not commonly seen as social events but are important in the physician’s journey, such as the residency and fellowship application processes and standardized tests, are being transformed. These changes alter typical social patterns that are important in PIF and may adversely affect high-value social group interactions that serve as buffers against stressors during training.18
Finally, the pandemic has altered the timeline for many learners. Medical students at several institutions graduated early to join the workforce and help care for escalating numbers of patients during the pandemic.7 Some see the pandemic as a catalyst to move toward competency-based time-variable training, in which learners progress through training at variable rates depending on their individual performance and learning needs.19 These changes could shorten the amount of time some learners spend in a given role (eg, medical student, intern). In such situations, it is unclear whether a minimal maturational time is necessary for most learners to fully develop a professional identity.
SUPPORTING PIF DURING THE PANDEMIC
In 2019, Cruess et al published general principles for supporting PIF,17 which have been used to support PIF during the COVID-19 pandemic.20 In the Table, we describe these principles and provide examples of how to implement them in the context of the pandemic. We believe these principles are applicable for PIF in undergraduate medical education, graduate medical education, and faculty development programs. A common thread throughout the principles is that PIF is not a process that should be left to chance, but rather explicitly nurtured through systematic support and curricular initiatives.5 This may be challenging while the COVID-19 pandemic is sapping financial resources and requiring rapid changes to clinical systems, but given the central role PIF plays in physician development, it should be prioritized by educational leaders.
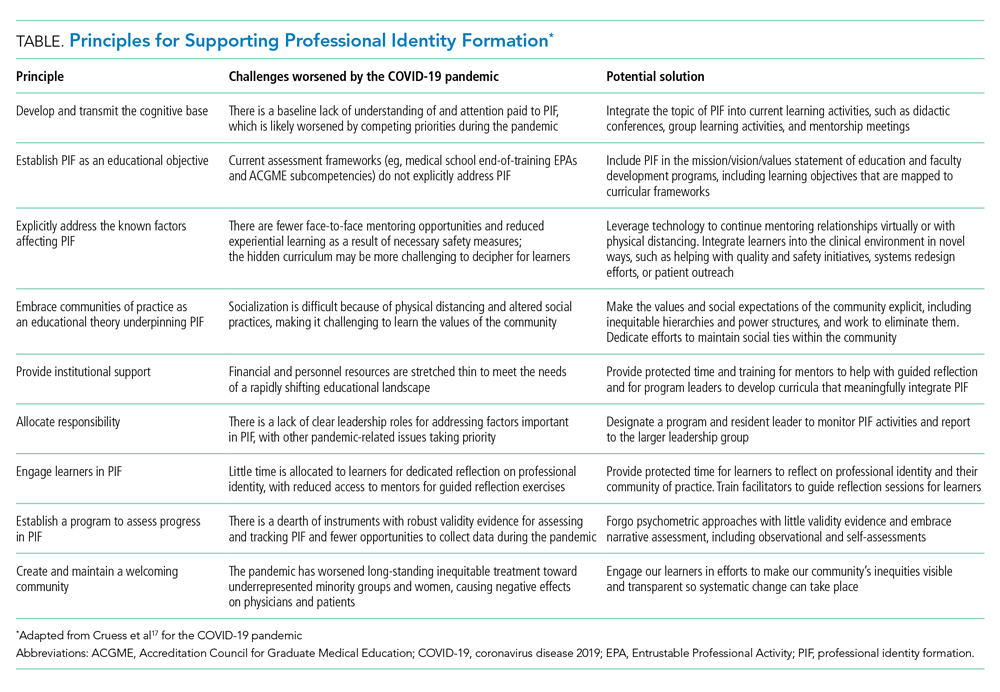
CREATING AND MAINTAINING A WELCOMING COMMUNITY: AN OPPORTUNITY
One of the final principles from Cruess et al is to create and maintain a welcoming community.17 This prompts questions such as: Is our community welcoming to everyone, where “everyone” really does mean everyone? Like other social structures, communities of practice tend to perpetuate existing power structures and inequities.17 It is no secret that medicine, like other professions, is riddled with inequities and bias based on factors such as race, gender, and socioeconomic status.21-23 The COVID-19 pandemic is likely exacerbating these inequities, such as the adverse impacts that are specifically affecting women physicians, who take on a disproportionate share of the child care at home.23 These biases impact not only the members of our professional community but also our patients, contributing to disparities in care and outcomes.
Physicians who have received inequitable treatment have laid bare the ways in which our communities of practice are failing them, and also outlined a better path on which to move forward.21,23 In addition to recruitment practices that promote diversity, meaningful programs should be developed to support inclusion, equity (in recognition, support, compensation), retention, and advancement. The disruption caused by COVID-19 can be a catalyst for this change. By taking this moment of crisis to examine the values and norms of medicine and how we systematically perpetuate harmful inequities and biases, we have an opportunity to deliberately rebuild our community of practice in a manner that helps shape the next generation’s professional identities to be better than we have been. This should always be the aim of education.
1. Merton RK. Some Preliminaries to a Sociology of Medical Education. Harvard University Press; 1957.
2. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. Jossey-Bass; 2010.
3. Irby DM, Hamstra SJ. Parting the clouds: three professionalism frameworks in medical education. Acad Med. 2016;91(12):1606-1611. https://doi.org/10.1097/ACM.0000000000001190
4. Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487-1492. https://doi.org/10.1001/archinte.167.14.1487
5. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-888. https://doi.org/10.1097/ACM.0b013e318257d57d
6. Anderson ML, Turbow S, Willgerodt MA, Ruhnke GW. Education in a crisis: the opportunity of our lives. J Hosp Med. 2020;15(5):287-291. https://doi.org/10.12788/jhm.3431
7. Kinnear B, Kelleher M, Olson AP, Sall D, Schumacher DJ. Developing trust with early medical school graduates during the COVID-19 pandemic. J Hosp Med. 2020;15(6):367-369. https://doi.org/10.12788/jhm.3463
8. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-1142. https://doi.org/10.1097/ACM.0000000000003402
9. Cullum RJ, Shaughnessy A, Mayat NY, Brown ME. Identity in lockdown: supporting primary care professional identity development in the COVID-19 generation. Educ Prim Care. 2020;31(4):200-204. https://doi.org/10.1080/14739879.2020.1779616
10. Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185-1190. https://doi.org/10.1097/ACM.0b013e3182604968
11. Al‐Eraky M, Marei H. A fresh look at Miller’s pyramid: assessment at the ‘Is’ and ‘Do’ levels. Med Educ. 2016;50(12):1253-1257. https://doi.org/10.1111/medu.13101
12. Forsythe GB. Identity development in professional education. Acad Med. 2005;80(10 Suppl):S112-S117. https://doi.org/10.1097/00001888-200510001-0002913.
13. Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718-725. https://doi.org/10.1097/ACM.0000000000000700
14. Kegan R. The Evolving Self: Problem and Process in Human Development. Harvard University Press; 1982.
15. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
16. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press; 1991.
17. Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: general principles. Med Teach. 2019;41(6):641-649. https://doi.org/10.1080/0142159X.2018.1536260
18. Mavor KI, McNeill KG, Anderson K, Kerr A, O’Reilly E, Platow MJ. Beyond prevalence to process: the role of self and identity in medical student well‐being. Med Educ. 2014;48(4):351-360. https://doi.org/10.1111/medu.12375
19. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
20. Stetson GV, Kryzhanovskaya IV, Lomen‐Hoerth C, Hauer KE. Professional identity formation in disorienting times. Med Educ. 2020;54(8):765-766. https://doi.org/10.1111/medu.14202
21. Unaka NI, Reynolds KL. Truth in tension: reflections on racism in medicine. J Hosp Med. 2020;15(9):572-573. https://doi.org/10.12788/jhm.3492
22. Beagan BL. Everyday classism in medical school: experiencing marginality and resistance. Med Educ. 2005;39(8):777-784. https://doi.org/10.1111/j.1365-2929.2005.02225.x
23. Jones Y, Durand V, Morton K, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
1. Merton RK. Some Preliminaries to a Sociology of Medical Education. Harvard University Press; 1957.
2. Cooke M, Irby DM, O’Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. Jossey-Bass; 2010.
3. Irby DM, Hamstra SJ. Parting the clouds: three professionalism frameworks in medical education. Acad Med. 2016;91(12):1606-1611. https://doi.org/10.1097/ACM.0000000000001190
4. Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487-1492. https://doi.org/10.1001/archinte.167.14.1487
5. Schumacher DJ, Slovin SR, Riebschleger MP, Englander R, Hicks PJ, Carraccio C. Perspective: beyond counting hours: the importance of supervision, professionalism, transitions of care, and workload in residency training. Acad Med. 2012;87(7):883-888. https://doi.org/10.1097/ACM.0b013e318257d57d
6. Anderson ML, Turbow S, Willgerodt MA, Ruhnke GW. Education in a crisis: the opportunity of our lives. J Hosp Med. 2020;15(5):287-291. https://doi.org/10.12788/jhm.3431
7. Kinnear B, Kelleher M, Olson AP, Sall D, Schumacher DJ. Developing trust with early medical school graduates during the COVID-19 pandemic. J Hosp Med. 2020;15(6):367-369. https://doi.org/10.12788/jhm.3463
8. Woolliscroft JO. Innovation in response to the COVID-19 pandemic crisis. Acad Med. 2020;95(8):1140-1142. https://doi.org/10.1097/ACM.0000000000003402
9. Cullum RJ, Shaughnessy A, Mayat NY, Brown ME. Identity in lockdown: supporting primary care professional identity development in the COVID-19 generation. Educ Prim Care. 2020;31(4):200-204. https://doi.org/10.1080/14739879.2020.1779616
10. Jarvis-Selinger S, Pratt DD, Regehr G. Competency is not enough: integrating identity formation into the medical education discourse. Acad Med. 2012;87(9):1185-1190. https://doi.org/10.1097/ACM.0b013e3182604968
11. Al‐Eraky M, Marei H. A fresh look at Miller’s pyramid: assessment at the ‘Is’ and ‘Do’ levels. Med Educ. 2016;50(12):1253-1257. https://doi.org/10.1111/medu.13101
12. Forsythe GB. Identity development in professional education. Acad Med. 2005;80(10 Suppl):S112-S117. https://doi.org/10.1097/00001888-200510001-0002913.
13. Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718-725. https://doi.org/10.1097/ACM.0000000000000700
14. Kegan R. The Evolving Self: Problem and Process in Human Development. Harvard University Press; 1982.
15. Cruess RL, Cruess SR, Steinert Y. Medicine as a community of practice: implications for medical education. Acad Med. 2018;93(2):185-191. https://doi.org/10.1097/ACM.0000000000001826
16. Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge University Press; 1991.
17. Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: general principles. Med Teach. 2019;41(6):641-649. https://doi.org/10.1080/0142159X.2018.1536260
18. Mavor KI, McNeill KG, Anderson K, Kerr A, O’Reilly E, Platow MJ. Beyond prevalence to process: the role of self and identity in medical student well‐being. Med Educ. 2014;48(4):351-360. https://doi.org/10.1111/medu.12375
19. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570
20. Stetson GV, Kryzhanovskaya IV, Lomen‐Hoerth C, Hauer KE. Professional identity formation in disorienting times. Med Educ. 2020;54(8):765-766. https://doi.org/10.1111/medu.14202
21. Unaka NI, Reynolds KL. Truth in tension: reflections on racism in medicine. J Hosp Med. 2020;15(9):572-573. https://doi.org/10.12788/jhm.3492
22. Beagan BL. Everyday classism in medical school: experiencing marginality and resistance. Med Educ. 2005;39(8):777-784. https://doi.org/10.1111/j.1365-2929.2005.02225.x
23. Jones Y, Durand V, Morton K, et al. Collateral damage: how COVID-19 is adversely impacting women physicians. J Hosp Med. 2020;15(8):507-509. https://doi.org/10.12788/jhm.3470
© 2021 Society of Hospital Medicine
Developing Trust With Early Medical School Graduates During the COVID-19 Pandemic
The coronavirus disease of 2019 (COVID-19) pandemic has strained the healthcare system by rapidly depleting multiple resources including hospital space, medications, ventilators, personal protective equipment (PPE), clinical revenue, and morale. One of the most essential at-risk resources is healthcare providers. Healthcare providers have been overwhelmed as hospital systems have experienced local surges in COVID-19 patients. Compounding this is the fact that providers are more likely to contract COVID-19, which could sideline portions of an already taxed workforce.
Multiple “surge” interventions have been planned or implemented to mitigate a current or anticipated dearth of physicians. Some institutions are reallocating subspecialists and surgeons to general ward and intensive care unit (ICU) roles, often with support from hospitalists and ICU physicians.1 Others have used telemedicine to reduce personnel exposure and conserve PPE.2 A novel and perhaps paradigm-shifting solution arose in March 2020 when several medical schools around the world announced they would graduate final year students early to allow them to join the workforce during the COVID-19 surge.3-7 In the United States, fourth-year medical students at multiple institutions in cities such as New York, Boston, Phoenix, Tucson, Newark, Portland, and Bethesda were offered the opportunity to graduate in April rather than in May or June. The Liaison Committee on Medical Education stated that for students to graduate early, they must have already met all curricular requirements and be deemed ready by an evaluations and promotions committee.8 What these early graduates do with their “gap time” before residency is neither standardized nor prescribed. The Accreditation Council for Graduate Medical Education has discouraged individuals from joining their newly matched residency programs early.9 Some early graduates who wish to bolster the workforce have signed temporary training agreements with local healthcare systems to work for a 1- to 2-month period before moving on to their matched residency program. Some institutions have already been working with local and state officials to rapidly grant provisional temporary licenses for this purpose.10
Early medical school graduation in times of international crisis is not without precedent. When faced with physician shortages during World War II, the United States federal government urged medical colleges to graduate trainees in 3 years.11 The national medical education milieu was different then, with standardized medical school training still crystalizing merely 30 years following the Flexner report. However, there was pressure from the federal government during World War II, whereas decisions around early graduation today are driven by institutional and local officials. While a few accelerated programs persist today, there has not been an urgent, unplanned early release of graduates to meet a public health need on such a large scale in recent history. The seasonal timing of the pandemic surge in the United States may have been a key factor in deciding to graduate students early. With a late winter and early spring peak, final year students are graduating only 2 to 3 months early. But what if another peak occurs in late summer or early fall, and some students are graduated even earlier? With which aspects of patient care would hospitalists trust these graduates, and with what level of supervision? Whether now or with a future COVID-19 peak, we describe how trust develops with learners and provide hospitalists with a framework for deliberate entrustment if and when they are asked to integrate early medical school graduates into their workforce.
PROGRESSION OF TRUST WITH LEARNERS
The degree of supervision that is provided to a learner is linked to how much a supervisor trusts the learner, as well as the specific context. Trust has many forms, often depending on what type of information informs it. Presumptive trust is trust based on credentials, without any actual interaction with the learner.12 Healthcare systems typically assume that medical school graduates are ready to perform intern-level tasks based on their medical degree. This presumptive trust may be bolstered by the assumption that a residency program director has vetted a learner’s credentials during the match process. On meeting a learner, we develop initial trust, which is based on first impressions and snap-judgment. Over time, presumptive and initial trust can be replaced by grounded trust, or trust based on demonstrated performance after prolonged experience with a learner. Under normal circumstances, supervisors use observations of learner performance in the clinical environment to develop grounded trust. With early graduates, especially those who sign temporary work agreements, the usual progression of trust may be compressed. Hospitalists may have less presumptive trust because these students graduated early and little time to develop grounded trust before integrating new graduates into patient care. How should hospitalists navigate supervision in this setting?
PRESUMPTIVE TRUST FOR CURRENT EARLY GRADUATES
Missing a few months at the end of medical school likely does not significantly affect competence and, therefore, should not affect presumptive trust. The value of the fourth year of medical school has been questioned because, after fulfilling graduation requirements, students often spend significant amounts of time interviewing, traveling, taking electives with lighter workloads, or exploring nonclinical interests late in the year.13 More intense “subintern” rotations, which are important for the residency application process, occur earlier in the academic year. It is therefore reasonable to presume that most students graduating in April are not less prepared than those graduating in June.
Additionally, there is significant interlearner variability in rates of competence attainment.14 This means that there is no magic point in time at which students are fully ready for resident-level responsibilities. Some students are likely competent to be interns without a fourth year at all, while others are still facing challenges in their development at the end of medical school. As Englander and Carraccio wrote, “The notion that every medical student across the nation has somehow achieved all the competencies necessary to start residency training on July 1 of their graduation year is magical thinking.”15 Since there is no universal, time-based finish line for competence, we should not be thrown by a slight change in the arbitrary line currently drawn in June. Whether students graduate in April or June, it remains true that some will be more ready than others.
INITIAL TRUST—HIGH RISK FOR BIAS
With compressed timelines, hospitalists may default to initial trust, relying heavily on first impressions to determine how much supervision an early graduate requires. For example, a graduate who is extroverted, assertive, and articulate may give off an air of confidence, which could entice a supervising hospitalist to give a “longer leash” with higher-risk patient care tasks. It is easy to fall prey to the “confidence equals competence” heuristic, but this has been shown to be unreliable.16 Initial trust is influenced by both social biases (eg, gender, race, age) and cognitive biases (eg, halo effect) that have little or nothing to do with the actual abilities of learners. While initial trust and accompanying biases often develop unconsciously, it is important to reflect on how unfounded first impressions can influence trust and supervision decisions.
GROUNDED TRUST BUILT THROUGH DIRECT OBSERVATION
Hospitalists must be deliberate with entrustment decisions, especially in a pandemic environment. There are useful guides for making these decisions that can be used in a point-of-care manner.17 First, it is important to acknowledge that entrustment is based in part on the perceived trustworthiness of a person. Kennedy and colleagues have described four components of trustworthiness, all of which can be assessed by hospitalists in the moment of care delivery: (1) knowledge and skill (Does the trainee possess the requisite knowledge and skill to perform the task?), (2) conscientiousness (Does the trainee follow through on tasks? Are they thorough and dependable?), (3) discernment (Does the trainee recognize personal limitations and seek help when needed?), and (4) truthfulness (Does the trainee tell the truth?).17
Entrustment decisions also depend on the specific task being observed (eg, high risk vs low risk) and context (eg, severity of illness of the patient, acuity of the setting).18 Trust is linked with perceived risk and benefits.19 More entrustment (less supervision) may be given when perceived risk is low, such as prescribing acetaminophen on a stable patient or taking an initial history. Less entrustment (more supervision) may be given when perceived risk is high, such as with managing septic shock or inserting a central venous catheter. However, the duress of the COVID-19 pandemic may tilt the risk/benefit balance toward less-than-usual supervision if an early graduate is the only provider available for some higher-risk tasks. This underscores the importance of direct observation leading to grounded trust with progressively higher-risk tasks as dictated by the local pandemic environment.
As much as possible, trust should be determined based on direct observation, not fallible first impressions or inference. Supervisors often use inference when assuming that performance on one task reflects performance on others. For example, if learners are observed to be competent when interpreting electrocardiograms, one might infer they also know how to manage tachyarrhythmias. If they can manage tachyarrhythmias, one might infer they also know how to manage acute coronary syndrome. These inferences are not the way to build grounded trust because competence is task and context dependent.
Direct observation can include watching patient interactions, being present for procedures, think-alouds during didactics, cognitive autopsies, reviewing notes, and informal conversations. Being deliberate with direct observation and entrustment decision-making can be challenging because of the high cognitive load of caring for sick and complex patients, maintaining proper PPE practices, and simultaneously assessing an early graduate’s performance. However, maintaining a level of supervision that is appropriate for trainee competence is paramount for patient safety. It may be valuable to identify tasks needing to be performed by early graduates and using focused simulation to generate a significant number of observations over a short period of time. Trust should be gained once competence is observed, not inferred or assumed. Instead of “trust, but verify,” we should “observe, then trust.”
CONCLUSION
There is a moral obligation to patients to avoid placing trainees in situations for which they are ill prepared based on their current abilities. We must balance the risk that exists both in leaving early graduates on the sidelines (overprotecting them as learners) and in asking them to perform tasks for which they are not prepared (overextending them as a workforce). Focusing on grounded trust derived from direct observation of performance while also balancing the risks and benefits inherent in the local pandemic context can help hospitalists calibrate supervision to a level that helps extend the workforce in a time of crisis while maintaining patient safety.
1. Cram P, Anderson ML, Shaughnessy EE. All hands on deck: learning to “unspecialize” in the COVID-19 pandemic. J Hosp Med. 2020;15(5):314‐315. https://doi.org/10.12788/jhm.3426.
2. Doshi A, Platt Y, Dressen JR, Mathews BK, Siy JC. Keep calm and log on: telemedicine for COVID-19 pandemic response. J Hosp Med. 2020;15(5):302‐304 https://doi.org/10.12788/jhm.3419.
3. Cole B. 10,000 med school graduates in Italy skip final exam, get sent directly into health service to help fight COVID-19. Newsweek. March 18, 2020. https://www.newsweek.com/italy-coronavirus-covid-19-medical-students-1492996. Accessed April 18, 2020.
4. Goldberg E. Early graduation could send medical students to virus front lines. New York Times. March 26, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-medical-students-graduation.html. Accessed April 18, 2020.
5. OHSU students enter medical residency early to aid in battle against COVID-19. MSN News. March 28, 2020. https://www.msn.com/en-us/news/us/ohsu-students-enter-medical-residency-early-to-aid-in-battle-against-covid-19/ar-BB11QlM4. Accessed April 18, 2020.
6. Siddique H. Final-year medical students graduate early to fight Covid-19. The Guardian. March 20, 2020. https://www.theguardian.com/world/2020/mar/20/final-year-medical-students-graduate-early-fight-coronavirus-covid-19. Accessed April 18, 2020.
7. Kime P. Military medical school to graduate students early, rush to COVID-19 response. Military.com. March 27, 2020. https://www.military.com/daily-news/2020/03/27/military-medical-school-graduate-students-early-rush-covid-19-response.html. Accessed April 18, 2020.
8. Barzansky B, Catanese VM. LCME update of medical students, patients, and COVID-19: guiding principles for early graduation of final-year medical students. March 25, 2020. https://lcme.org/wp-content/uploads/filebase/March-25-2020-LCME-Guidance-for-Medical-Schools-Considering-Early-Graduation-Option.pdf. Accessed April 18, 2020.
9. ACGME statement on early graduation from US medical schools and early appointment to the clinical learning environment. ACGME News. April 3, 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10184/ACGME-Statement-on-Early-Graduation-from-US-Medical-Schools-and-Early-Appointment-to-ACGME-Accredited-Programs. Accessed April 18, 2020.
10. Mitchell J. Baker requests federal disaster assistance, asks med schools to graduate students early. WBUR News. March 26, 2020. https://www.wbur.org/news/2020/03/26/baker-massachusetts-coronavirus. Accessed April 18, 2020.
11. Schwartz CC, Ajjarapu AS, Stamy CD, Schwinn DA. Comprehensive history of 3-year and accelerated US medical school programs: a century in review. Med Educ Online. 2018;23(1):1530557. https://doi.org/10.1080/10872981.2018.1530557.
12. Ten Cate O, Hart D, Ankel F, et al. Entrustment decision making in clinical training. Acad Med. 2016;91(2):191-198. https://doi.org/10.1097/acm.0000000000001044.
13. Walling A, Merando A. The fourth year of medical education: a literature review. Acad Med. 2010;85(11):1698-1704. https://doi.org/10.1097/acm.0b013e3181f52dc6.
14. Pusic MV, Boutis K, Hatala R, Cook DA. Learning curves in health professions education. Acad Med. 2015;90(8):1034-1042. https://doi.org/10.1097/acm.0000000000000681.
15. Englander R, Carraccio C. A lack of continuity in education, training, and practice violates the “do no harm” principle. Acad Med. 2018;93(3S):S12-S16. https://doi.org/10.1097/acm.0000000000002071.
16. Dunning D, Heath C, Suls JM. Flawed self-assessment: implications for health, education, and the workplace. Psychol Sci Public Interest. 2004;5(3):69-106. https://doi.org/10.1111/j.1529-1006.2004.00018.x.
17. Kennedy TJ, Regehr G, Baker GR, Lingard L. Point-of-care assessment of medical trainee competence for independent clinical work. Acad Med. 2008;83(10 Suppl):S89-S92. https://doi.org/10.1097/acm.0b013e318183c8b7.
18. Hauer KE, Ten Cate O, Boscardin C, Irby DM, Iobst W, O’Sullivan PS. Understanding trust as an essential element of trainee supervision and learning in the workplace. Adv Health Sci Educ Theory Pract. 2014;19(3):435-456. https://doi.org/10.1007/s10459-013-9474-4.
19. Ten Cate O. Managing risks and benefits: key issues in entrustment decisions. Med Educ. 2017;51(9):879-881. https://doi.org/10.1111/medu.13362.
The coronavirus disease of 2019 (COVID-19) pandemic has strained the healthcare system by rapidly depleting multiple resources including hospital space, medications, ventilators, personal protective equipment (PPE), clinical revenue, and morale. One of the most essential at-risk resources is healthcare providers. Healthcare providers have been overwhelmed as hospital systems have experienced local surges in COVID-19 patients. Compounding this is the fact that providers are more likely to contract COVID-19, which could sideline portions of an already taxed workforce.
Multiple “surge” interventions have been planned or implemented to mitigate a current or anticipated dearth of physicians. Some institutions are reallocating subspecialists and surgeons to general ward and intensive care unit (ICU) roles, often with support from hospitalists and ICU physicians.1 Others have used telemedicine to reduce personnel exposure and conserve PPE.2 A novel and perhaps paradigm-shifting solution arose in March 2020 when several medical schools around the world announced they would graduate final year students early to allow them to join the workforce during the COVID-19 surge.3-7 In the United States, fourth-year medical students at multiple institutions in cities such as New York, Boston, Phoenix, Tucson, Newark, Portland, and Bethesda were offered the opportunity to graduate in April rather than in May or June. The Liaison Committee on Medical Education stated that for students to graduate early, they must have already met all curricular requirements and be deemed ready by an evaluations and promotions committee.8 What these early graduates do with their “gap time” before residency is neither standardized nor prescribed. The Accreditation Council for Graduate Medical Education has discouraged individuals from joining their newly matched residency programs early.9 Some early graduates who wish to bolster the workforce have signed temporary training agreements with local healthcare systems to work for a 1- to 2-month period before moving on to their matched residency program. Some institutions have already been working with local and state officials to rapidly grant provisional temporary licenses for this purpose.10
Early medical school graduation in times of international crisis is not without precedent. When faced with physician shortages during World War II, the United States federal government urged medical colleges to graduate trainees in 3 years.11 The national medical education milieu was different then, with standardized medical school training still crystalizing merely 30 years following the Flexner report. However, there was pressure from the federal government during World War II, whereas decisions around early graduation today are driven by institutional and local officials. While a few accelerated programs persist today, there has not been an urgent, unplanned early release of graduates to meet a public health need on such a large scale in recent history. The seasonal timing of the pandemic surge in the United States may have been a key factor in deciding to graduate students early. With a late winter and early spring peak, final year students are graduating only 2 to 3 months early. But what if another peak occurs in late summer or early fall, and some students are graduated even earlier? With which aspects of patient care would hospitalists trust these graduates, and with what level of supervision? Whether now or with a future COVID-19 peak, we describe how trust develops with learners and provide hospitalists with a framework for deliberate entrustment if and when they are asked to integrate early medical school graduates into their workforce.
PROGRESSION OF TRUST WITH LEARNERS
The degree of supervision that is provided to a learner is linked to how much a supervisor trusts the learner, as well as the specific context. Trust has many forms, often depending on what type of information informs it. Presumptive trust is trust based on credentials, without any actual interaction with the learner.12 Healthcare systems typically assume that medical school graduates are ready to perform intern-level tasks based on their medical degree. This presumptive trust may be bolstered by the assumption that a residency program director has vetted a learner’s credentials during the match process. On meeting a learner, we develop initial trust, which is based on first impressions and snap-judgment. Over time, presumptive and initial trust can be replaced by grounded trust, or trust based on demonstrated performance after prolonged experience with a learner. Under normal circumstances, supervisors use observations of learner performance in the clinical environment to develop grounded trust. With early graduates, especially those who sign temporary work agreements, the usual progression of trust may be compressed. Hospitalists may have less presumptive trust because these students graduated early and little time to develop grounded trust before integrating new graduates into patient care. How should hospitalists navigate supervision in this setting?
PRESUMPTIVE TRUST FOR CURRENT EARLY GRADUATES
Missing a few months at the end of medical school likely does not significantly affect competence and, therefore, should not affect presumptive trust. The value of the fourth year of medical school has been questioned because, after fulfilling graduation requirements, students often spend significant amounts of time interviewing, traveling, taking electives with lighter workloads, or exploring nonclinical interests late in the year.13 More intense “subintern” rotations, which are important for the residency application process, occur earlier in the academic year. It is therefore reasonable to presume that most students graduating in April are not less prepared than those graduating in June.
Additionally, there is significant interlearner variability in rates of competence attainment.14 This means that there is no magic point in time at which students are fully ready for resident-level responsibilities. Some students are likely competent to be interns without a fourth year at all, while others are still facing challenges in their development at the end of medical school. As Englander and Carraccio wrote, “The notion that every medical student across the nation has somehow achieved all the competencies necessary to start residency training on July 1 of their graduation year is magical thinking.”15 Since there is no universal, time-based finish line for competence, we should not be thrown by a slight change in the arbitrary line currently drawn in June. Whether students graduate in April or June, it remains true that some will be more ready than others.
INITIAL TRUST—HIGH RISK FOR BIAS
With compressed timelines, hospitalists may default to initial trust, relying heavily on first impressions to determine how much supervision an early graduate requires. For example, a graduate who is extroverted, assertive, and articulate may give off an air of confidence, which could entice a supervising hospitalist to give a “longer leash” with higher-risk patient care tasks. It is easy to fall prey to the “confidence equals competence” heuristic, but this has been shown to be unreliable.16 Initial trust is influenced by both social biases (eg, gender, race, age) and cognitive biases (eg, halo effect) that have little or nothing to do with the actual abilities of learners. While initial trust and accompanying biases often develop unconsciously, it is important to reflect on how unfounded first impressions can influence trust and supervision decisions.
GROUNDED TRUST BUILT THROUGH DIRECT OBSERVATION
Hospitalists must be deliberate with entrustment decisions, especially in a pandemic environment. There are useful guides for making these decisions that can be used in a point-of-care manner.17 First, it is important to acknowledge that entrustment is based in part on the perceived trustworthiness of a person. Kennedy and colleagues have described four components of trustworthiness, all of which can be assessed by hospitalists in the moment of care delivery: (1) knowledge and skill (Does the trainee possess the requisite knowledge and skill to perform the task?), (2) conscientiousness (Does the trainee follow through on tasks? Are they thorough and dependable?), (3) discernment (Does the trainee recognize personal limitations and seek help when needed?), and (4) truthfulness (Does the trainee tell the truth?).17
Entrustment decisions also depend on the specific task being observed (eg, high risk vs low risk) and context (eg, severity of illness of the patient, acuity of the setting).18 Trust is linked with perceived risk and benefits.19 More entrustment (less supervision) may be given when perceived risk is low, such as prescribing acetaminophen on a stable patient or taking an initial history. Less entrustment (more supervision) may be given when perceived risk is high, such as with managing septic shock or inserting a central venous catheter. However, the duress of the COVID-19 pandemic may tilt the risk/benefit balance toward less-than-usual supervision if an early graduate is the only provider available for some higher-risk tasks. This underscores the importance of direct observation leading to grounded trust with progressively higher-risk tasks as dictated by the local pandemic environment.
As much as possible, trust should be determined based on direct observation, not fallible first impressions or inference. Supervisors often use inference when assuming that performance on one task reflects performance on others. For example, if learners are observed to be competent when interpreting electrocardiograms, one might infer they also know how to manage tachyarrhythmias. If they can manage tachyarrhythmias, one might infer they also know how to manage acute coronary syndrome. These inferences are not the way to build grounded trust because competence is task and context dependent.
Direct observation can include watching patient interactions, being present for procedures, think-alouds during didactics, cognitive autopsies, reviewing notes, and informal conversations. Being deliberate with direct observation and entrustment decision-making can be challenging because of the high cognitive load of caring for sick and complex patients, maintaining proper PPE practices, and simultaneously assessing an early graduate’s performance. However, maintaining a level of supervision that is appropriate for trainee competence is paramount for patient safety. It may be valuable to identify tasks needing to be performed by early graduates and using focused simulation to generate a significant number of observations over a short period of time. Trust should be gained once competence is observed, not inferred or assumed. Instead of “trust, but verify,” we should “observe, then trust.”
CONCLUSION
There is a moral obligation to patients to avoid placing trainees in situations for which they are ill prepared based on their current abilities. We must balance the risk that exists both in leaving early graduates on the sidelines (overprotecting them as learners) and in asking them to perform tasks for which they are not prepared (overextending them as a workforce). Focusing on grounded trust derived from direct observation of performance while also balancing the risks and benefits inherent in the local pandemic context can help hospitalists calibrate supervision to a level that helps extend the workforce in a time of crisis while maintaining patient safety.
The coronavirus disease of 2019 (COVID-19) pandemic has strained the healthcare system by rapidly depleting multiple resources including hospital space, medications, ventilators, personal protective equipment (PPE), clinical revenue, and morale. One of the most essential at-risk resources is healthcare providers. Healthcare providers have been overwhelmed as hospital systems have experienced local surges in COVID-19 patients. Compounding this is the fact that providers are more likely to contract COVID-19, which could sideline portions of an already taxed workforce.
Multiple “surge” interventions have been planned or implemented to mitigate a current or anticipated dearth of physicians. Some institutions are reallocating subspecialists and surgeons to general ward and intensive care unit (ICU) roles, often with support from hospitalists and ICU physicians.1 Others have used telemedicine to reduce personnel exposure and conserve PPE.2 A novel and perhaps paradigm-shifting solution arose in March 2020 when several medical schools around the world announced they would graduate final year students early to allow them to join the workforce during the COVID-19 surge.3-7 In the United States, fourth-year medical students at multiple institutions in cities such as New York, Boston, Phoenix, Tucson, Newark, Portland, and Bethesda were offered the opportunity to graduate in April rather than in May or June. The Liaison Committee on Medical Education stated that for students to graduate early, they must have already met all curricular requirements and be deemed ready by an evaluations and promotions committee.8 What these early graduates do with their “gap time” before residency is neither standardized nor prescribed. The Accreditation Council for Graduate Medical Education has discouraged individuals from joining their newly matched residency programs early.9 Some early graduates who wish to bolster the workforce have signed temporary training agreements with local healthcare systems to work for a 1- to 2-month period before moving on to their matched residency program. Some institutions have already been working with local and state officials to rapidly grant provisional temporary licenses for this purpose.10
Early medical school graduation in times of international crisis is not without precedent. When faced with physician shortages during World War II, the United States federal government urged medical colleges to graduate trainees in 3 years.11 The national medical education milieu was different then, with standardized medical school training still crystalizing merely 30 years following the Flexner report. However, there was pressure from the federal government during World War II, whereas decisions around early graduation today are driven by institutional and local officials. While a few accelerated programs persist today, there has not been an urgent, unplanned early release of graduates to meet a public health need on such a large scale in recent history. The seasonal timing of the pandemic surge in the United States may have been a key factor in deciding to graduate students early. With a late winter and early spring peak, final year students are graduating only 2 to 3 months early. But what if another peak occurs in late summer or early fall, and some students are graduated even earlier? With which aspects of patient care would hospitalists trust these graduates, and with what level of supervision? Whether now or with a future COVID-19 peak, we describe how trust develops with learners and provide hospitalists with a framework for deliberate entrustment if and when they are asked to integrate early medical school graduates into their workforce.
PROGRESSION OF TRUST WITH LEARNERS
The degree of supervision that is provided to a learner is linked to how much a supervisor trusts the learner, as well as the specific context. Trust has many forms, often depending on what type of information informs it. Presumptive trust is trust based on credentials, without any actual interaction with the learner.12 Healthcare systems typically assume that medical school graduates are ready to perform intern-level tasks based on their medical degree. This presumptive trust may be bolstered by the assumption that a residency program director has vetted a learner’s credentials during the match process. On meeting a learner, we develop initial trust, which is based on first impressions and snap-judgment. Over time, presumptive and initial trust can be replaced by grounded trust, or trust based on demonstrated performance after prolonged experience with a learner. Under normal circumstances, supervisors use observations of learner performance in the clinical environment to develop grounded trust. With early graduates, especially those who sign temporary work agreements, the usual progression of trust may be compressed. Hospitalists may have less presumptive trust because these students graduated early and little time to develop grounded trust before integrating new graduates into patient care. How should hospitalists navigate supervision in this setting?
PRESUMPTIVE TRUST FOR CURRENT EARLY GRADUATES
Missing a few months at the end of medical school likely does not significantly affect competence and, therefore, should not affect presumptive trust. The value of the fourth year of medical school has been questioned because, after fulfilling graduation requirements, students often spend significant amounts of time interviewing, traveling, taking electives with lighter workloads, or exploring nonclinical interests late in the year.13 More intense “subintern” rotations, which are important for the residency application process, occur earlier in the academic year. It is therefore reasonable to presume that most students graduating in April are not less prepared than those graduating in June.
Additionally, there is significant interlearner variability in rates of competence attainment.14 This means that there is no magic point in time at which students are fully ready for resident-level responsibilities. Some students are likely competent to be interns without a fourth year at all, while others are still facing challenges in their development at the end of medical school. As Englander and Carraccio wrote, “The notion that every medical student across the nation has somehow achieved all the competencies necessary to start residency training on July 1 of their graduation year is magical thinking.”15 Since there is no universal, time-based finish line for competence, we should not be thrown by a slight change in the arbitrary line currently drawn in June. Whether students graduate in April or June, it remains true that some will be more ready than others.
INITIAL TRUST—HIGH RISK FOR BIAS
With compressed timelines, hospitalists may default to initial trust, relying heavily on first impressions to determine how much supervision an early graduate requires. For example, a graduate who is extroverted, assertive, and articulate may give off an air of confidence, which could entice a supervising hospitalist to give a “longer leash” with higher-risk patient care tasks. It is easy to fall prey to the “confidence equals competence” heuristic, but this has been shown to be unreliable.16 Initial trust is influenced by both social biases (eg, gender, race, age) and cognitive biases (eg, halo effect) that have little or nothing to do with the actual abilities of learners. While initial trust and accompanying biases often develop unconsciously, it is important to reflect on how unfounded first impressions can influence trust and supervision decisions.
GROUNDED TRUST BUILT THROUGH DIRECT OBSERVATION
Hospitalists must be deliberate with entrustment decisions, especially in a pandemic environment. There are useful guides for making these decisions that can be used in a point-of-care manner.17 First, it is important to acknowledge that entrustment is based in part on the perceived trustworthiness of a person. Kennedy and colleagues have described four components of trustworthiness, all of which can be assessed by hospitalists in the moment of care delivery: (1) knowledge and skill (Does the trainee possess the requisite knowledge and skill to perform the task?), (2) conscientiousness (Does the trainee follow through on tasks? Are they thorough and dependable?), (3) discernment (Does the trainee recognize personal limitations and seek help when needed?), and (4) truthfulness (Does the trainee tell the truth?).17
Entrustment decisions also depend on the specific task being observed (eg, high risk vs low risk) and context (eg, severity of illness of the patient, acuity of the setting).18 Trust is linked with perceived risk and benefits.19 More entrustment (less supervision) may be given when perceived risk is low, such as prescribing acetaminophen on a stable patient or taking an initial history. Less entrustment (more supervision) may be given when perceived risk is high, such as with managing septic shock or inserting a central venous catheter. However, the duress of the COVID-19 pandemic may tilt the risk/benefit balance toward less-than-usual supervision if an early graduate is the only provider available for some higher-risk tasks. This underscores the importance of direct observation leading to grounded trust with progressively higher-risk tasks as dictated by the local pandemic environment.
As much as possible, trust should be determined based on direct observation, not fallible first impressions or inference. Supervisors often use inference when assuming that performance on one task reflects performance on others. For example, if learners are observed to be competent when interpreting electrocardiograms, one might infer they also know how to manage tachyarrhythmias. If they can manage tachyarrhythmias, one might infer they also know how to manage acute coronary syndrome. These inferences are not the way to build grounded trust because competence is task and context dependent.
Direct observation can include watching patient interactions, being present for procedures, think-alouds during didactics, cognitive autopsies, reviewing notes, and informal conversations. Being deliberate with direct observation and entrustment decision-making can be challenging because of the high cognitive load of caring for sick and complex patients, maintaining proper PPE practices, and simultaneously assessing an early graduate’s performance. However, maintaining a level of supervision that is appropriate for trainee competence is paramount for patient safety. It may be valuable to identify tasks needing to be performed by early graduates and using focused simulation to generate a significant number of observations over a short period of time. Trust should be gained once competence is observed, not inferred or assumed. Instead of “trust, but verify,” we should “observe, then trust.”
CONCLUSION
There is a moral obligation to patients to avoid placing trainees in situations for which they are ill prepared based on their current abilities. We must balance the risk that exists both in leaving early graduates on the sidelines (overprotecting them as learners) and in asking them to perform tasks for which they are not prepared (overextending them as a workforce). Focusing on grounded trust derived from direct observation of performance while also balancing the risks and benefits inherent in the local pandemic context can help hospitalists calibrate supervision to a level that helps extend the workforce in a time of crisis while maintaining patient safety.
1. Cram P, Anderson ML, Shaughnessy EE. All hands on deck: learning to “unspecialize” in the COVID-19 pandemic. J Hosp Med. 2020;15(5):314‐315. https://doi.org/10.12788/jhm.3426.
2. Doshi A, Platt Y, Dressen JR, Mathews BK, Siy JC. Keep calm and log on: telemedicine for COVID-19 pandemic response. J Hosp Med. 2020;15(5):302‐304 https://doi.org/10.12788/jhm.3419.
3. Cole B. 10,000 med school graduates in Italy skip final exam, get sent directly into health service to help fight COVID-19. Newsweek. March 18, 2020. https://www.newsweek.com/italy-coronavirus-covid-19-medical-students-1492996. Accessed April 18, 2020.
4. Goldberg E. Early graduation could send medical students to virus front lines. New York Times. March 26, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-medical-students-graduation.html. Accessed April 18, 2020.
5. OHSU students enter medical residency early to aid in battle against COVID-19. MSN News. March 28, 2020. https://www.msn.com/en-us/news/us/ohsu-students-enter-medical-residency-early-to-aid-in-battle-against-covid-19/ar-BB11QlM4. Accessed April 18, 2020.
6. Siddique H. Final-year medical students graduate early to fight Covid-19. The Guardian. March 20, 2020. https://www.theguardian.com/world/2020/mar/20/final-year-medical-students-graduate-early-fight-coronavirus-covid-19. Accessed April 18, 2020.
7. Kime P. Military medical school to graduate students early, rush to COVID-19 response. Military.com. March 27, 2020. https://www.military.com/daily-news/2020/03/27/military-medical-school-graduate-students-early-rush-covid-19-response.html. Accessed April 18, 2020.
8. Barzansky B, Catanese VM. LCME update of medical students, patients, and COVID-19: guiding principles for early graduation of final-year medical students. March 25, 2020. https://lcme.org/wp-content/uploads/filebase/March-25-2020-LCME-Guidance-for-Medical-Schools-Considering-Early-Graduation-Option.pdf. Accessed April 18, 2020.
9. ACGME statement on early graduation from US medical schools and early appointment to the clinical learning environment. ACGME News. April 3, 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10184/ACGME-Statement-on-Early-Graduation-from-US-Medical-Schools-and-Early-Appointment-to-ACGME-Accredited-Programs. Accessed April 18, 2020.
10. Mitchell J. Baker requests federal disaster assistance, asks med schools to graduate students early. WBUR News. March 26, 2020. https://www.wbur.org/news/2020/03/26/baker-massachusetts-coronavirus. Accessed April 18, 2020.
11. Schwartz CC, Ajjarapu AS, Stamy CD, Schwinn DA. Comprehensive history of 3-year and accelerated US medical school programs: a century in review. Med Educ Online. 2018;23(1):1530557. https://doi.org/10.1080/10872981.2018.1530557.
12. Ten Cate O, Hart D, Ankel F, et al. Entrustment decision making in clinical training. Acad Med. 2016;91(2):191-198. https://doi.org/10.1097/acm.0000000000001044.
13. Walling A, Merando A. The fourth year of medical education: a literature review. Acad Med. 2010;85(11):1698-1704. https://doi.org/10.1097/acm.0b013e3181f52dc6.
14. Pusic MV, Boutis K, Hatala R, Cook DA. Learning curves in health professions education. Acad Med. 2015;90(8):1034-1042. https://doi.org/10.1097/acm.0000000000000681.
15. Englander R, Carraccio C. A lack of continuity in education, training, and practice violates the “do no harm” principle. Acad Med. 2018;93(3S):S12-S16. https://doi.org/10.1097/acm.0000000000002071.
16. Dunning D, Heath C, Suls JM. Flawed self-assessment: implications for health, education, and the workplace. Psychol Sci Public Interest. 2004;5(3):69-106. https://doi.org/10.1111/j.1529-1006.2004.00018.x.
17. Kennedy TJ, Regehr G, Baker GR, Lingard L. Point-of-care assessment of medical trainee competence for independent clinical work. Acad Med. 2008;83(10 Suppl):S89-S92. https://doi.org/10.1097/acm.0b013e318183c8b7.
18. Hauer KE, Ten Cate O, Boscardin C, Irby DM, Iobst W, O’Sullivan PS. Understanding trust as an essential element of trainee supervision and learning in the workplace. Adv Health Sci Educ Theory Pract. 2014;19(3):435-456. https://doi.org/10.1007/s10459-013-9474-4.
19. Ten Cate O. Managing risks and benefits: key issues in entrustment decisions. Med Educ. 2017;51(9):879-881. https://doi.org/10.1111/medu.13362.
1. Cram P, Anderson ML, Shaughnessy EE. All hands on deck: learning to “unspecialize” in the COVID-19 pandemic. J Hosp Med. 2020;15(5):314‐315. https://doi.org/10.12788/jhm.3426.
2. Doshi A, Platt Y, Dressen JR, Mathews BK, Siy JC. Keep calm and log on: telemedicine for COVID-19 pandemic response. J Hosp Med. 2020;15(5):302‐304 https://doi.org/10.12788/jhm.3419.
3. Cole B. 10,000 med school graduates in Italy skip final exam, get sent directly into health service to help fight COVID-19. Newsweek. March 18, 2020. https://www.newsweek.com/italy-coronavirus-covid-19-medical-students-1492996. Accessed April 18, 2020.
4. Goldberg E. Early graduation could send medical students to virus front lines. New York Times. March 26, 2020. https://www.nytimes.com/2020/03/26/health/coronavirus-medical-students-graduation.html. Accessed April 18, 2020.
5. OHSU students enter medical residency early to aid in battle against COVID-19. MSN News. March 28, 2020. https://www.msn.com/en-us/news/us/ohsu-students-enter-medical-residency-early-to-aid-in-battle-against-covid-19/ar-BB11QlM4. Accessed April 18, 2020.
6. Siddique H. Final-year medical students graduate early to fight Covid-19. The Guardian. March 20, 2020. https://www.theguardian.com/world/2020/mar/20/final-year-medical-students-graduate-early-fight-coronavirus-covid-19. Accessed April 18, 2020.
7. Kime P. Military medical school to graduate students early, rush to COVID-19 response. Military.com. March 27, 2020. https://www.military.com/daily-news/2020/03/27/military-medical-school-graduate-students-early-rush-covid-19-response.html. Accessed April 18, 2020.
8. Barzansky B, Catanese VM. LCME update of medical students, patients, and COVID-19: guiding principles for early graduation of final-year medical students. March 25, 2020. https://lcme.org/wp-content/uploads/filebase/March-25-2020-LCME-Guidance-for-Medical-Schools-Considering-Early-Graduation-Option.pdf. Accessed April 18, 2020.
9. ACGME statement on early graduation from US medical schools and early appointment to the clinical learning environment. ACGME News. April 3, 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10184/ACGME-Statement-on-Early-Graduation-from-US-Medical-Schools-and-Early-Appointment-to-ACGME-Accredited-Programs. Accessed April 18, 2020.
10. Mitchell J. Baker requests federal disaster assistance, asks med schools to graduate students early. WBUR News. March 26, 2020. https://www.wbur.org/news/2020/03/26/baker-massachusetts-coronavirus. Accessed April 18, 2020.
11. Schwartz CC, Ajjarapu AS, Stamy CD, Schwinn DA. Comprehensive history of 3-year and accelerated US medical school programs: a century in review. Med Educ Online. 2018;23(1):1530557. https://doi.org/10.1080/10872981.2018.1530557.
12. Ten Cate O, Hart D, Ankel F, et al. Entrustment decision making in clinical training. Acad Med. 2016;91(2):191-198. https://doi.org/10.1097/acm.0000000000001044.
13. Walling A, Merando A. The fourth year of medical education: a literature review. Acad Med. 2010;85(11):1698-1704. https://doi.org/10.1097/acm.0b013e3181f52dc6.
14. Pusic MV, Boutis K, Hatala R, Cook DA. Learning curves in health professions education. Acad Med. 2015;90(8):1034-1042. https://doi.org/10.1097/acm.0000000000000681.
15. Englander R, Carraccio C. A lack of continuity in education, training, and practice violates the “do no harm” principle. Acad Med. 2018;93(3S):S12-S16. https://doi.org/10.1097/acm.0000000000002071.
16. Dunning D, Heath C, Suls JM. Flawed self-assessment: implications for health, education, and the workplace. Psychol Sci Public Interest. 2004;5(3):69-106. https://doi.org/10.1111/j.1529-1006.2004.00018.x.
17. Kennedy TJ, Regehr G, Baker GR, Lingard L. Point-of-care assessment of medical trainee competence for independent clinical work. Acad Med. 2008;83(10 Suppl):S89-S92. https://doi.org/10.1097/acm.0b013e318183c8b7.
18. Hauer KE, Ten Cate O, Boscardin C, Irby DM, Iobst W, O’Sullivan PS. Understanding trust as an essential element of trainee supervision and learning in the workplace. Adv Health Sci Educ Theory Pract. 2014;19(3):435-456. https://doi.org/10.1007/s10459-013-9474-4.
19. Ten Cate O. Managing risks and benefits: key issues in entrustment decisions. Med Educ. 2017;51(9):879-881. https://doi.org/10.1111/medu.13362.
© 2020 Society of Hospital Medicine
Clinical Progress Note: Point-of-Care Ultrasound in the Evaluation of the Dyspneic Adult
Point-of-care ultrasound (POCUS) continues to gain traction in contemporary clinical practice both as a diagnostic tool and as an extension of the physical examination. Hospital Medicine (HM) lags behind Emergency Medicine (EM) and Critical Care (CC) in our uptake of such technology, although momentum is gaining. Leaders in HM have published frameworks for competency and credentialing, and the Society for Hospital Medicine has created a pathway for certification.1 POCUS use is the standard of care for several bedside procedures, but evidence for diagnostic applications is changing rapidly as the literature expands. However, the applicability of this evidence to HM patients can be challenging as most published studies are still from EM and CC settings. This Progress Note focuses on how a hospitalist might incorporate POCUS in the evaluation of adult patients with dyspnea. This topic was chosen after reviewing several relevant studies published in the past five years and recognizing the importance of dyspnea in HM. The Progress Note begins with a review of POCUS for undifferentiated dyspnea before exploring studies of common diagnoses that present with dyspnea, including pneumonia, pleural effusion, and acute decompensated heart failure (ADHF), aiming to update the knowledge of HM providers regarding this technology as well as to stimulate further study in this field.
SEARCH STRATEGY
In collaboration with an academic librarian in March 2019, PubMed was searched for studies published within the past five years using several MESH search terms for POCUS. The search was originally focused to the field of HM using specific search terms, but this yielded a very limited number of studies. Therefore, the search strategy was expanded to include EM and CC studies. This final search generated 346 papers that were supplemented with additional literature searches using references from studies found in the initial search.
UNDIFFERENTIATED DYSPNEA
Dyspnea is common in HM, both as the reason for a patient’s admission and as a symptom that develops during hospitalization such as after intravenous fluid resuscitation, a possible aspiration event, or central line placement. The differential diagnosis is broad, and multiple studies suggest that POCUS can aid in the evaluation of undifferentiated dyspnea while also being cost effective and avoiding the potential radiation of other testing modalities. The pulmonary POCUS evaluation incorporates a combination of several findings, including “A-lines” or horizontal artifacts from normal aerated lung; “B-lines”, vertical artifacts generated by extra-alveolar fluid, consolidation or “tissue-like pattern”; air bronchograms, consolidated lung surrounding airways; anechoic or hypoechoic areas in dependent zones of the lung; and the presence or absence of pleural sliding.2
In one prospective observational study of five internal medicine residents with no prior POCUS experience and three hours of training, the addition of handheld POCUS devices to usual clinical information improved the diagnostic accuracy for pneumonia, pulmonary edema, pleural effusion, and obstructive lung disease when evaluating patients with a primary complaint of dyspnea (area under the curve [AUC] 0.81 vs 0.87, P < .01).2 However, the largest improvements in the operating characteristics were observed with the two residents who received an extended two-week elective of training.
In another study of 383 consecutive patients presenting to the ED with dyspnea, physicians with basic and advanced POCUS training were blinded to all clinical information and recorded a diagnosis after performing a lung POCUS examination. The “ultrasound physician’s” diagnosis was then compared to the treating emergency department (ED) physician’s diagnosis using history, physical, and other diagnostic data. Lung POCUS had a sensitivity and a specificity of 87.6% and 96.2% for pulmonary edema, 85.7% and 99% for pneumonia, 98.2% and 67.3% for asthma/chronic obstructive pulmonary disease (COPD), 46.2% and 100% for pulmonary embolus (PE), and 71.4% and 100% for pneumothorax, respectively.3 The scanning protocol used, the BLUE (Bedside Lung Ultrasound Examination) protocol, was focused on ruling out significant pulmonary etiologies of dyspnea. The protocol classified the finding of normal lung ultrasound (A-line profile) as COPD or asthma since these conditions will have a normal sonographic appearance. This approach could lead to incorrect labeling of other extrapulmonary causes of dyspnea as COPD or asthma. The findings of this study suggest that POCUS is most effective at ruling in pulmonary edema and pneumonia while being most effective at ruling out asthma or COPD as causes of dyspnea. It is both sensitive and specific for pneumothorax. However, as other studies have found, the sensitivity of POCUS for COPD, asthma, and PE was inferior to traditional clinical evaluation.4 One of the few studies looking specifically at hospitalized ward patients compared a blinded lung POCUS diagnosis and a discharge clinical diagnosis classified as cardiac, pulmonary, or mixed dyspnea. The authors of that study found an “interstitial pattern” (two areas with more than two B-lines) in 94% of those classified as cardiac on discharge, but POCUS findings were less precise for those discharged with a pulmonary etiology of dyspnea.5 Identifying B-lines on lung POCUS appears to be helpful in rapidly differentiating cardiac from pulmonary etiologies of dyspnea.
An additional advantage of POCUS is that multiple organ systems can be evaluated in rapid succession when the etiology of dyspnea is unknown. In a smaller ED study of patients presenting with undifferentiated dyspnea, a diagnosis was recorded after history-taking and physical examination and then recorded again after lung, cardiac, and inferior vena cava POCUS. Clinician diagnostic accuracy improved from 53% to 77% with the use of POCUS (P = .003) compared with the final diagnosis.6 The treating physician’s primary impression changed in almost 50% of cases after using POCUS, most of which was driven by improved sensitivity and specificity of ADHF. In another study of 2,700 patients presenting to the ED with dyspnea, cardiopulmonary POCUS shortened the time to diagnosis (186 ± 72 minutes vs 24 ± 10 minutes, P = .025).4 These studies suggest that the use of POCUS in the initial evaluation of patients with undifferentiated dyspnea is a valuable tool with respect to diagnostic accuracy and timeliness.
PNEUMONIA
There are several different sonographic findings that can indicate pneumonia, such as consolidation or “hepatization”, the “shred” sign of an irregular border between consolidated lung and aerated lung, unilateral B-lines, and dynamic air bronchograms. Several recent systematic reviews and meta-analyses have investigated the operating characteristics of POCUS for the diagnosis of pneumonia. These reviews are limited by heterogeneity with respect to different patient populations, sonographers, and reference standards, but all three reviews found similar results, with the pooled AUC values ranging from 95% to 98%.7-9 This recent evidence along with other reviews suggests that lung ultrasound can serve as a primary diagnostic tool in pneumonia and is probably superior to chest radiography.
PLEURAL EFFUSION
Pleural effusions are observed with POCUS as anechoic or hypoechoic areas, generally in dependent lung zones. POCUS may provide additional benefit by better characterizing the effusion as having septations or floating fibrin strands. One recent systematic review and meta-analysis including 1,554 patients found that POCUS had excellent sensitivity and specificity (94% and 98%, respectively) in detecting pleural effusion versus chest radiography (51% and 91%, respectively), both compared with reference standard imaging such as computed tomography. The subgroup analysis found that sensitivity was higher for scanners who were intensivists or radiologists than for other physicians (97% vs 90%; P ≤ .001) and also found a nonstatistically significant trend toward reduced sensitivity when pocket-sized devices were used (90% vs 95%, P = .09).10
ACUTE DECOMPENSATED HEART FAILURE
It is extremely important to recognize that a POCUS finding of decreased left ventricular ejection fraction is not synonymous with a diagnosis of ADHF. Bedside providers can use POCUS to estimate cardiac function, but other clinical information is required to determine whether the syndrome of ADHF is present. In one study, examinations performed by 10 internists with approximately 18 hours of training in focused cardiac POCUS had a sensitivity and a specificity of 91% and 88%, respectively, for classifying left ventricular systolic function as normal or mildly, moderately, or severely depressed with “good/substantial” agreement (k = 0.77) compared with formal echocardiography.11 The presence of bilateral B-lines as a sign of pulmonary edema suggests accompanying functional decompensation. A meta-analysis of seven articles including 1075 patients in various clinical settings (ED, ICU, and inpatient wards) found a sensitivity of 94.1% and a specificity of 92.4% for using B-lines to diagnose acute cardiogenic pulmonary edema compared with the final clinical diagnosis.12 Al Deeb et al. examined 226 patients and found similar sensitivity (95.3%) and specificity (88.2%) for diagnosing acute cardiogenic pulmonary edema when nurses were trained to evaluate for bilateral B-lines in dyspneic patients admitted to the hospital, also compared with the adjudicated final diagnosis.13 Carlino et al. evaluated dyspneic patients using a three-minute pocket-sized device scan of the heart, lungs, and inferior vena cava and found that no single view offered a substantial improvement in diagnostic accuracy; however, the combination of bilateral B-lines and/or pleural effusion and either a dilated left atrium or left ventricular ejection fraction (LVEF) of <40% had a very high diagnostic accuracy (AUC 0.97).14 Russell et al. performed a secondary analysis of a prospective observational study of patients with dyspnea and found that a simple three-view scanning protocol looking for the presence of B-lines on the right and left anterior superior lung zones and an LVEF of <45% took an average of one minute and 32 seconds to perform and had 100% specificity for ADHF if all three were positive.15 Another recent systematic review and meta-analysis of six studies and 1,827 patients found a sensitivity of 88% (CI 75%-95%) for lung POCUS compared with a chest radiography at a sensitivity of 73% (70%-76%) for the diagnosis of ADHF.16 All these studies suggest that improving the diagnosis of ADHF does not require complex echocardiographic views and is probably more feasible and accessible than many expect.
SUMMARY
POCUS continues to show promise for evaluating patients with dyspnea. It is clear that adding a few POCUS examination maneuvers to a provider’s toolbox, such as looking for B-lines and overall cardiac function, can improve
1. Soni NJ, Schnobrich D, Matthews BK, et al. Point-of-care ultrasound for hospitalists: a position statement of the Society of Hospital Medicine. J Hosp Med. Published online only January 2, 2019. https://doi.org/10.12788/jhm.3079.
2. Filopei J, Siedenburg H, Rattner P, Fukaya E, Kory P. Impact of pocket ultrasound use by internal medicine housestaff in the diagnosis of dyspnea. J Hosp Med. 2014;9(9):594-597. https://doi.org/10.1002/jhm.2219.
3. Bekgoz B, Kilicaslan I, Bildik F, et al. BLUE protocol ultrasonography in emergency department patients presenting with acute dyspnea. Am J Emerg Med. 2019. https://doi.org/10.1016/j.ajem.2019.02.028.
4. Zanobetti M, Scorpiniti M, Gigli C, et al. Point-of-care ultrasonography for evaluation of acute dyspnea in the ED. Chest. 2017;151(6):1295-1301. https://doi.org/10.1016/j.chest.2017.02.003.
5. Perrone T, Maggi A, Sgarlata C, et al. Lung ultrasound in internal medicine: a bedside help to increase accuracy in the diagnosis of dyspnea. Eur J Intern Med. 2017;46:61-65. https://doi.org/10.1016/j.ejim.2017.07.034.
6. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-care multi-organ ultrasound improves diagnostic accuracy in adults presenting to the emergency department with acute dyspnea. West J Emerg Med. 2016;17(1):46-53. https://doi.org/10.5811/westjem.2015.11.28525.
7. Orso D, Guglielmo N, Copetti R. Lung ultrasound in diagnosing pneumonia in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med. 2018;25(5):312-321. https://doi.org/10.1097/MEJ.0000000000000517.
8. Alzahrani SA, Al-Salamah MA, Al-Madani WH, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9(1):6. https://doi.org/10.1186/s13089-017-0059-y
9. Long L, Zhao HT, Zhang ZY, Wang GY, Zhao HL. Lung ultrasound for the diagnosis of pneumonia in adults: a meta-analysis. Medicine . 2017;96(3):e5713. https://doi.org/10.1097/MD.0000000000005713.
10. Yousefifard M, Baikpour M, Ghelichkhani P, et al. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion; a meta-analysis. Emerg (Tehran). 2016;4(1):1-10.
11. Johnson BK, Tierney DM, Rosborough TK, Harris KM, Newell MC. Internal medicine point-of-care ultrasound assessment of left ventricular function correlates with formal echocardiography. J Clin Ultrasound. 2016;44(2):92-99. https://doi.org/10.1002/jcu.22272.
12. Al Deeb M, Barbic S, Featherstone R, Dankoff J, Barbic D. Point-of-care ultrasonography for the diagnosis of acute cardiogenic pulmonary edema in patients presenting with acute dyspnea: a systematic review and meta-analysis. Acad Emerg Med. 2014;21(8):843-852. https://doi.org/10.1111/acem.12435.
13. Mumoli N, Vitale J, Giorgi-Pierfranceschi M, et al. Accuracy of nurse-performed lung ultrasound in patients with acute dyspnea: a prospective observational study. Medicine (Baltimore). 2016;95(9):e2925. https://doi.org/10.1097/MD.0000000000002925.
14. Carlino MV, Paladino F, Sforza A, et al. Assessment of left atrial size in addition to focused cardiopulmonary ultrasound improves diagnostic accuracy of acute heart failure in the emergency department. Echocardiography (Mount Kisco, NY). 2018;35(6):785-791. https://doi.org/10.1111/echo.13851.
15. Russell FM, Ehrman RR. A modified lung and cardiac ultrasound protocol saves time and rules in the diagnosis of acute heart failure. J Emerg Med. 2017;52(6):839-845. https://doi.org/10.1016/j.jemermed.2017.02.003.
16. Maw AM, Hassanin A, Ho PM, et al. diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(3):e190703. https://doi.org/10.1001/jamanetworkopen.2019.0703.
Point-of-care ultrasound (POCUS) continues to gain traction in contemporary clinical practice both as a diagnostic tool and as an extension of the physical examination. Hospital Medicine (HM) lags behind Emergency Medicine (EM) and Critical Care (CC) in our uptake of such technology, although momentum is gaining. Leaders in HM have published frameworks for competency and credentialing, and the Society for Hospital Medicine has created a pathway for certification.1 POCUS use is the standard of care for several bedside procedures, but evidence for diagnostic applications is changing rapidly as the literature expands. However, the applicability of this evidence to HM patients can be challenging as most published studies are still from EM and CC settings. This Progress Note focuses on how a hospitalist might incorporate POCUS in the evaluation of adult patients with dyspnea. This topic was chosen after reviewing several relevant studies published in the past five years and recognizing the importance of dyspnea in HM. The Progress Note begins with a review of POCUS for undifferentiated dyspnea before exploring studies of common diagnoses that present with dyspnea, including pneumonia, pleural effusion, and acute decompensated heart failure (ADHF), aiming to update the knowledge of HM providers regarding this technology as well as to stimulate further study in this field.
SEARCH STRATEGY
In collaboration with an academic librarian in March 2019, PubMed was searched for studies published within the past five years using several MESH search terms for POCUS. The search was originally focused to the field of HM using specific search terms, but this yielded a very limited number of studies. Therefore, the search strategy was expanded to include EM and CC studies. This final search generated 346 papers that were supplemented with additional literature searches using references from studies found in the initial search.
UNDIFFERENTIATED DYSPNEA
Dyspnea is common in HM, both as the reason for a patient’s admission and as a symptom that develops during hospitalization such as after intravenous fluid resuscitation, a possible aspiration event, or central line placement. The differential diagnosis is broad, and multiple studies suggest that POCUS can aid in the evaluation of undifferentiated dyspnea while also being cost effective and avoiding the potential radiation of other testing modalities. The pulmonary POCUS evaluation incorporates a combination of several findings, including “A-lines” or horizontal artifacts from normal aerated lung; “B-lines”, vertical artifacts generated by extra-alveolar fluid, consolidation or “tissue-like pattern”; air bronchograms, consolidated lung surrounding airways; anechoic or hypoechoic areas in dependent zones of the lung; and the presence or absence of pleural sliding.2
In one prospective observational study of five internal medicine residents with no prior POCUS experience and three hours of training, the addition of handheld POCUS devices to usual clinical information improved the diagnostic accuracy for pneumonia, pulmonary edema, pleural effusion, and obstructive lung disease when evaluating patients with a primary complaint of dyspnea (area under the curve [AUC] 0.81 vs 0.87, P < .01).2 However, the largest improvements in the operating characteristics were observed with the two residents who received an extended two-week elective of training.
In another study of 383 consecutive patients presenting to the ED with dyspnea, physicians with basic and advanced POCUS training were blinded to all clinical information and recorded a diagnosis after performing a lung POCUS examination. The “ultrasound physician’s” diagnosis was then compared to the treating emergency department (ED) physician’s diagnosis using history, physical, and other diagnostic data. Lung POCUS had a sensitivity and a specificity of 87.6% and 96.2% for pulmonary edema, 85.7% and 99% for pneumonia, 98.2% and 67.3% for asthma/chronic obstructive pulmonary disease (COPD), 46.2% and 100% for pulmonary embolus (PE), and 71.4% and 100% for pneumothorax, respectively.3 The scanning protocol used, the BLUE (Bedside Lung Ultrasound Examination) protocol, was focused on ruling out significant pulmonary etiologies of dyspnea. The protocol classified the finding of normal lung ultrasound (A-line profile) as COPD or asthma since these conditions will have a normal sonographic appearance. This approach could lead to incorrect labeling of other extrapulmonary causes of dyspnea as COPD or asthma. The findings of this study suggest that POCUS is most effective at ruling in pulmonary edema and pneumonia while being most effective at ruling out asthma or COPD as causes of dyspnea. It is both sensitive and specific for pneumothorax. However, as other studies have found, the sensitivity of POCUS for COPD, asthma, and PE was inferior to traditional clinical evaluation.4 One of the few studies looking specifically at hospitalized ward patients compared a blinded lung POCUS diagnosis and a discharge clinical diagnosis classified as cardiac, pulmonary, or mixed dyspnea. The authors of that study found an “interstitial pattern” (two areas with more than two B-lines) in 94% of those classified as cardiac on discharge, but POCUS findings were less precise for those discharged with a pulmonary etiology of dyspnea.5 Identifying B-lines on lung POCUS appears to be helpful in rapidly differentiating cardiac from pulmonary etiologies of dyspnea.
An additional advantage of POCUS is that multiple organ systems can be evaluated in rapid succession when the etiology of dyspnea is unknown. In a smaller ED study of patients presenting with undifferentiated dyspnea, a diagnosis was recorded after history-taking and physical examination and then recorded again after lung, cardiac, and inferior vena cava POCUS. Clinician diagnostic accuracy improved from 53% to 77% with the use of POCUS (P = .003) compared with the final diagnosis.6 The treating physician’s primary impression changed in almost 50% of cases after using POCUS, most of which was driven by improved sensitivity and specificity of ADHF. In another study of 2,700 patients presenting to the ED with dyspnea, cardiopulmonary POCUS shortened the time to diagnosis (186 ± 72 minutes vs 24 ± 10 minutes, P = .025).4 These studies suggest that the use of POCUS in the initial evaluation of patients with undifferentiated dyspnea is a valuable tool with respect to diagnostic accuracy and timeliness.
PNEUMONIA
There are several different sonographic findings that can indicate pneumonia, such as consolidation or “hepatization”, the “shred” sign of an irregular border between consolidated lung and aerated lung, unilateral B-lines, and dynamic air bronchograms. Several recent systematic reviews and meta-analyses have investigated the operating characteristics of POCUS for the diagnosis of pneumonia. These reviews are limited by heterogeneity with respect to different patient populations, sonographers, and reference standards, but all three reviews found similar results, with the pooled AUC values ranging from 95% to 98%.7-9 This recent evidence along with other reviews suggests that lung ultrasound can serve as a primary diagnostic tool in pneumonia and is probably superior to chest radiography.
PLEURAL EFFUSION
Pleural effusions are observed with POCUS as anechoic or hypoechoic areas, generally in dependent lung zones. POCUS may provide additional benefit by better characterizing the effusion as having septations or floating fibrin strands. One recent systematic review and meta-analysis including 1,554 patients found that POCUS had excellent sensitivity and specificity (94% and 98%, respectively) in detecting pleural effusion versus chest radiography (51% and 91%, respectively), both compared with reference standard imaging such as computed tomography. The subgroup analysis found that sensitivity was higher for scanners who were intensivists or radiologists than for other physicians (97% vs 90%; P ≤ .001) and also found a nonstatistically significant trend toward reduced sensitivity when pocket-sized devices were used (90% vs 95%, P = .09).10
ACUTE DECOMPENSATED HEART FAILURE
It is extremely important to recognize that a POCUS finding of decreased left ventricular ejection fraction is not synonymous with a diagnosis of ADHF. Bedside providers can use POCUS to estimate cardiac function, but other clinical information is required to determine whether the syndrome of ADHF is present. In one study, examinations performed by 10 internists with approximately 18 hours of training in focused cardiac POCUS had a sensitivity and a specificity of 91% and 88%, respectively, for classifying left ventricular systolic function as normal or mildly, moderately, or severely depressed with “good/substantial” agreement (k = 0.77) compared with formal echocardiography.11 The presence of bilateral B-lines as a sign of pulmonary edema suggests accompanying functional decompensation. A meta-analysis of seven articles including 1075 patients in various clinical settings (ED, ICU, and inpatient wards) found a sensitivity of 94.1% and a specificity of 92.4% for using B-lines to diagnose acute cardiogenic pulmonary edema compared with the final clinical diagnosis.12 Al Deeb et al. examined 226 patients and found similar sensitivity (95.3%) and specificity (88.2%) for diagnosing acute cardiogenic pulmonary edema when nurses were trained to evaluate for bilateral B-lines in dyspneic patients admitted to the hospital, also compared with the adjudicated final diagnosis.13 Carlino et al. evaluated dyspneic patients using a three-minute pocket-sized device scan of the heart, lungs, and inferior vena cava and found that no single view offered a substantial improvement in diagnostic accuracy; however, the combination of bilateral B-lines and/or pleural effusion and either a dilated left atrium or left ventricular ejection fraction (LVEF) of <40% had a very high diagnostic accuracy (AUC 0.97).14 Russell et al. performed a secondary analysis of a prospective observational study of patients with dyspnea and found that a simple three-view scanning protocol looking for the presence of B-lines on the right and left anterior superior lung zones and an LVEF of <45% took an average of one minute and 32 seconds to perform and had 100% specificity for ADHF if all three were positive.15 Another recent systematic review and meta-analysis of six studies and 1,827 patients found a sensitivity of 88% (CI 75%-95%) for lung POCUS compared with a chest radiography at a sensitivity of 73% (70%-76%) for the diagnosis of ADHF.16 All these studies suggest that improving the diagnosis of ADHF does not require complex echocardiographic views and is probably more feasible and accessible than many expect.
SUMMARY
POCUS continues to show promise for evaluating patients with dyspnea. It is clear that adding a few POCUS examination maneuvers to a provider’s toolbox, such as looking for B-lines and overall cardiac function, can improve
Point-of-care ultrasound (POCUS) continues to gain traction in contemporary clinical practice both as a diagnostic tool and as an extension of the physical examination. Hospital Medicine (HM) lags behind Emergency Medicine (EM) and Critical Care (CC) in our uptake of such technology, although momentum is gaining. Leaders in HM have published frameworks for competency and credentialing, and the Society for Hospital Medicine has created a pathway for certification.1 POCUS use is the standard of care for several bedside procedures, but evidence for diagnostic applications is changing rapidly as the literature expands. However, the applicability of this evidence to HM patients can be challenging as most published studies are still from EM and CC settings. This Progress Note focuses on how a hospitalist might incorporate POCUS in the evaluation of adult patients with dyspnea. This topic was chosen after reviewing several relevant studies published in the past five years and recognizing the importance of dyspnea in HM. The Progress Note begins with a review of POCUS for undifferentiated dyspnea before exploring studies of common diagnoses that present with dyspnea, including pneumonia, pleural effusion, and acute decompensated heart failure (ADHF), aiming to update the knowledge of HM providers regarding this technology as well as to stimulate further study in this field.
SEARCH STRATEGY
In collaboration with an academic librarian in March 2019, PubMed was searched for studies published within the past five years using several MESH search terms for POCUS. The search was originally focused to the field of HM using specific search terms, but this yielded a very limited number of studies. Therefore, the search strategy was expanded to include EM and CC studies. This final search generated 346 papers that were supplemented with additional literature searches using references from studies found in the initial search.
UNDIFFERENTIATED DYSPNEA
Dyspnea is common in HM, both as the reason for a patient’s admission and as a symptom that develops during hospitalization such as after intravenous fluid resuscitation, a possible aspiration event, or central line placement. The differential diagnosis is broad, and multiple studies suggest that POCUS can aid in the evaluation of undifferentiated dyspnea while also being cost effective and avoiding the potential radiation of other testing modalities. The pulmonary POCUS evaluation incorporates a combination of several findings, including “A-lines” or horizontal artifacts from normal aerated lung; “B-lines”, vertical artifacts generated by extra-alveolar fluid, consolidation or “tissue-like pattern”; air bronchograms, consolidated lung surrounding airways; anechoic or hypoechoic areas in dependent zones of the lung; and the presence or absence of pleural sliding.2
In one prospective observational study of five internal medicine residents with no prior POCUS experience and three hours of training, the addition of handheld POCUS devices to usual clinical information improved the diagnostic accuracy for pneumonia, pulmonary edema, pleural effusion, and obstructive lung disease when evaluating patients with a primary complaint of dyspnea (area under the curve [AUC] 0.81 vs 0.87, P < .01).2 However, the largest improvements in the operating characteristics were observed with the two residents who received an extended two-week elective of training.
In another study of 383 consecutive patients presenting to the ED with dyspnea, physicians with basic and advanced POCUS training were blinded to all clinical information and recorded a diagnosis after performing a lung POCUS examination. The “ultrasound physician’s” diagnosis was then compared to the treating emergency department (ED) physician’s diagnosis using history, physical, and other diagnostic data. Lung POCUS had a sensitivity and a specificity of 87.6% and 96.2% for pulmonary edema, 85.7% and 99% for pneumonia, 98.2% and 67.3% for asthma/chronic obstructive pulmonary disease (COPD), 46.2% and 100% for pulmonary embolus (PE), and 71.4% and 100% for pneumothorax, respectively.3 The scanning protocol used, the BLUE (Bedside Lung Ultrasound Examination) protocol, was focused on ruling out significant pulmonary etiologies of dyspnea. The protocol classified the finding of normal lung ultrasound (A-line profile) as COPD or asthma since these conditions will have a normal sonographic appearance. This approach could lead to incorrect labeling of other extrapulmonary causes of dyspnea as COPD or asthma. The findings of this study suggest that POCUS is most effective at ruling in pulmonary edema and pneumonia while being most effective at ruling out asthma or COPD as causes of dyspnea. It is both sensitive and specific for pneumothorax. However, as other studies have found, the sensitivity of POCUS for COPD, asthma, and PE was inferior to traditional clinical evaluation.4 One of the few studies looking specifically at hospitalized ward patients compared a blinded lung POCUS diagnosis and a discharge clinical diagnosis classified as cardiac, pulmonary, or mixed dyspnea. The authors of that study found an “interstitial pattern” (two areas with more than two B-lines) in 94% of those classified as cardiac on discharge, but POCUS findings were less precise for those discharged with a pulmonary etiology of dyspnea.5 Identifying B-lines on lung POCUS appears to be helpful in rapidly differentiating cardiac from pulmonary etiologies of dyspnea.
An additional advantage of POCUS is that multiple organ systems can be evaluated in rapid succession when the etiology of dyspnea is unknown. In a smaller ED study of patients presenting with undifferentiated dyspnea, a diagnosis was recorded after history-taking and physical examination and then recorded again after lung, cardiac, and inferior vena cava POCUS. Clinician diagnostic accuracy improved from 53% to 77% with the use of POCUS (P = .003) compared with the final diagnosis.6 The treating physician’s primary impression changed in almost 50% of cases after using POCUS, most of which was driven by improved sensitivity and specificity of ADHF. In another study of 2,700 patients presenting to the ED with dyspnea, cardiopulmonary POCUS shortened the time to diagnosis (186 ± 72 minutes vs 24 ± 10 minutes, P = .025).4 These studies suggest that the use of POCUS in the initial evaluation of patients with undifferentiated dyspnea is a valuable tool with respect to diagnostic accuracy and timeliness.
PNEUMONIA
There are several different sonographic findings that can indicate pneumonia, such as consolidation or “hepatization”, the “shred” sign of an irregular border between consolidated lung and aerated lung, unilateral B-lines, and dynamic air bronchograms. Several recent systematic reviews and meta-analyses have investigated the operating characteristics of POCUS for the diagnosis of pneumonia. These reviews are limited by heterogeneity with respect to different patient populations, sonographers, and reference standards, but all three reviews found similar results, with the pooled AUC values ranging from 95% to 98%.7-9 This recent evidence along with other reviews suggests that lung ultrasound can serve as a primary diagnostic tool in pneumonia and is probably superior to chest radiography.
PLEURAL EFFUSION
Pleural effusions are observed with POCUS as anechoic or hypoechoic areas, generally in dependent lung zones. POCUS may provide additional benefit by better characterizing the effusion as having septations or floating fibrin strands. One recent systematic review and meta-analysis including 1,554 patients found that POCUS had excellent sensitivity and specificity (94% and 98%, respectively) in detecting pleural effusion versus chest radiography (51% and 91%, respectively), both compared with reference standard imaging such as computed tomography. The subgroup analysis found that sensitivity was higher for scanners who were intensivists or radiologists than for other physicians (97% vs 90%; P ≤ .001) and also found a nonstatistically significant trend toward reduced sensitivity when pocket-sized devices were used (90% vs 95%, P = .09).10
ACUTE DECOMPENSATED HEART FAILURE
It is extremely important to recognize that a POCUS finding of decreased left ventricular ejection fraction is not synonymous with a diagnosis of ADHF. Bedside providers can use POCUS to estimate cardiac function, but other clinical information is required to determine whether the syndrome of ADHF is present. In one study, examinations performed by 10 internists with approximately 18 hours of training in focused cardiac POCUS had a sensitivity and a specificity of 91% and 88%, respectively, for classifying left ventricular systolic function as normal or mildly, moderately, or severely depressed with “good/substantial” agreement (k = 0.77) compared with formal echocardiography.11 The presence of bilateral B-lines as a sign of pulmonary edema suggests accompanying functional decompensation. A meta-analysis of seven articles including 1075 patients in various clinical settings (ED, ICU, and inpatient wards) found a sensitivity of 94.1% and a specificity of 92.4% for using B-lines to diagnose acute cardiogenic pulmonary edema compared with the final clinical diagnosis.12 Al Deeb et al. examined 226 patients and found similar sensitivity (95.3%) and specificity (88.2%) for diagnosing acute cardiogenic pulmonary edema when nurses were trained to evaluate for bilateral B-lines in dyspneic patients admitted to the hospital, also compared with the adjudicated final diagnosis.13 Carlino et al. evaluated dyspneic patients using a three-minute pocket-sized device scan of the heart, lungs, and inferior vena cava and found that no single view offered a substantial improvement in diagnostic accuracy; however, the combination of bilateral B-lines and/or pleural effusion and either a dilated left atrium or left ventricular ejection fraction (LVEF) of <40% had a very high diagnostic accuracy (AUC 0.97).14 Russell et al. performed a secondary analysis of a prospective observational study of patients with dyspnea and found that a simple three-view scanning protocol looking for the presence of B-lines on the right and left anterior superior lung zones and an LVEF of <45% took an average of one minute and 32 seconds to perform and had 100% specificity for ADHF if all three were positive.15 Another recent systematic review and meta-analysis of six studies and 1,827 patients found a sensitivity of 88% (CI 75%-95%) for lung POCUS compared with a chest radiography at a sensitivity of 73% (70%-76%) for the diagnosis of ADHF.16 All these studies suggest that improving the diagnosis of ADHF does not require complex echocardiographic views and is probably more feasible and accessible than many expect.
SUMMARY
POCUS continues to show promise for evaluating patients with dyspnea. It is clear that adding a few POCUS examination maneuvers to a provider’s toolbox, such as looking for B-lines and overall cardiac function, can improve
1. Soni NJ, Schnobrich D, Matthews BK, et al. Point-of-care ultrasound for hospitalists: a position statement of the Society of Hospital Medicine. J Hosp Med. Published online only January 2, 2019. https://doi.org/10.12788/jhm.3079.
2. Filopei J, Siedenburg H, Rattner P, Fukaya E, Kory P. Impact of pocket ultrasound use by internal medicine housestaff in the diagnosis of dyspnea. J Hosp Med. 2014;9(9):594-597. https://doi.org/10.1002/jhm.2219.
3. Bekgoz B, Kilicaslan I, Bildik F, et al. BLUE protocol ultrasonography in emergency department patients presenting with acute dyspnea. Am J Emerg Med. 2019. https://doi.org/10.1016/j.ajem.2019.02.028.
4. Zanobetti M, Scorpiniti M, Gigli C, et al. Point-of-care ultrasonography for evaluation of acute dyspnea in the ED. Chest. 2017;151(6):1295-1301. https://doi.org/10.1016/j.chest.2017.02.003.
5. Perrone T, Maggi A, Sgarlata C, et al. Lung ultrasound in internal medicine: a bedside help to increase accuracy in the diagnosis of dyspnea. Eur J Intern Med. 2017;46:61-65. https://doi.org/10.1016/j.ejim.2017.07.034.
6. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-care multi-organ ultrasound improves diagnostic accuracy in adults presenting to the emergency department with acute dyspnea. West J Emerg Med. 2016;17(1):46-53. https://doi.org/10.5811/westjem.2015.11.28525.
7. Orso D, Guglielmo N, Copetti R. Lung ultrasound in diagnosing pneumonia in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med. 2018;25(5):312-321. https://doi.org/10.1097/MEJ.0000000000000517.
8. Alzahrani SA, Al-Salamah MA, Al-Madani WH, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9(1):6. https://doi.org/10.1186/s13089-017-0059-y
9. Long L, Zhao HT, Zhang ZY, Wang GY, Zhao HL. Lung ultrasound for the diagnosis of pneumonia in adults: a meta-analysis. Medicine . 2017;96(3):e5713. https://doi.org/10.1097/MD.0000000000005713.
10. Yousefifard M, Baikpour M, Ghelichkhani P, et al. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion; a meta-analysis. Emerg (Tehran). 2016;4(1):1-10.
11. Johnson BK, Tierney DM, Rosborough TK, Harris KM, Newell MC. Internal medicine point-of-care ultrasound assessment of left ventricular function correlates with formal echocardiography. J Clin Ultrasound. 2016;44(2):92-99. https://doi.org/10.1002/jcu.22272.
12. Al Deeb M, Barbic S, Featherstone R, Dankoff J, Barbic D. Point-of-care ultrasonography for the diagnosis of acute cardiogenic pulmonary edema in patients presenting with acute dyspnea: a systematic review and meta-analysis. Acad Emerg Med. 2014;21(8):843-852. https://doi.org/10.1111/acem.12435.
13. Mumoli N, Vitale J, Giorgi-Pierfranceschi M, et al. Accuracy of nurse-performed lung ultrasound in patients with acute dyspnea: a prospective observational study. Medicine (Baltimore). 2016;95(9):e2925. https://doi.org/10.1097/MD.0000000000002925.
14. Carlino MV, Paladino F, Sforza A, et al. Assessment of left atrial size in addition to focused cardiopulmonary ultrasound improves diagnostic accuracy of acute heart failure in the emergency department. Echocardiography (Mount Kisco, NY). 2018;35(6):785-791. https://doi.org/10.1111/echo.13851.
15. Russell FM, Ehrman RR. A modified lung and cardiac ultrasound protocol saves time and rules in the diagnosis of acute heart failure. J Emerg Med. 2017;52(6):839-845. https://doi.org/10.1016/j.jemermed.2017.02.003.
16. Maw AM, Hassanin A, Ho PM, et al. diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(3):e190703. https://doi.org/10.1001/jamanetworkopen.2019.0703.
1. Soni NJ, Schnobrich D, Matthews BK, et al. Point-of-care ultrasound for hospitalists: a position statement of the Society of Hospital Medicine. J Hosp Med. Published online only January 2, 2019. https://doi.org/10.12788/jhm.3079.
2. Filopei J, Siedenburg H, Rattner P, Fukaya E, Kory P. Impact of pocket ultrasound use by internal medicine housestaff in the diagnosis of dyspnea. J Hosp Med. 2014;9(9):594-597. https://doi.org/10.1002/jhm.2219.
3. Bekgoz B, Kilicaslan I, Bildik F, et al. BLUE protocol ultrasonography in emergency department patients presenting with acute dyspnea. Am J Emerg Med. 2019. https://doi.org/10.1016/j.ajem.2019.02.028.
4. Zanobetti M, Scorpiniti M, Gigli C, et al. Point-of-care ultrasonography for evaluation of acute dyspnea in the ED. Chest. 2017;151(6):1295-1301. https://doi.org/10.1016/j.chest.2017.02.003.
5. Perrone T, Maggi A, Sgarlata C, et al. Lung ultrasound in internal medicine: a bedside help to increase accuracy in the diagnosis of dyspnea. Eur J Intern Med. 2017;46:61-65. https://doi.org/10.1016/j.ejim.2017.07.034.
6. Mantuani D, Frazee BW, Fahimi J, Nagdev A. Point-of-care multi-organ ultrasound improves diagnostic accuracy in adults presenting to the emergency department with acute dyspnea. West J Emerg Med. 2016;17(1):46-53. https://doi.org/10.5811/westjem.2015.11.28525.
7. Orso D, Guglielmo N, Copetti R. Lung ultrasound in diagnosing pneumonia in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med. 2018;25(5):312-321. https://doi.org/10.1097/MEJ.0000000000000517.
8. Alzahrani SA, Al-Salamah MA, Al-Madani WH, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9(1):6. https://doi.org/10.1186/s13089-017-0059-y
9. Long L, Zhao HT, Zhang ZY, Wang GY, Zhao HL. Lung ultrasound for the diagnosis of pneumonia in adults: a meta-analysis. Medicine . 2017;96(3):e5713. https://doi.org/10.1097/MD.0000000000005713.
10. Yousefifard M, Baikpour M, Ghelichkhani P, et al. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion; a meta-analysis. Emerg (Tehran). 2016;4(1):1-10.
11. Johnson BK, Tierney DM, Rosborough TK, Harris KM, Newell MC. Internal medicine point-of-care ultrasound assessment of left ventricular function correlates with formal echocardiography. J Clin Ultrasound. 2016;44(2):92-99. https://doi.org/10.1002/jcu.22272.
12. Al Deeb M, Barbic S, Featherstone R, Dankoff J, Barbic D. Point-of-care ultrasonography for the diagnosis of acute cardiogenic pulmonary edema in patients presenting with acute dyspnea: a systematic review and meta-analysis. Acad Emerg Med. 2014;21(8):843-852. https://doi.org/10.1111/acem.12435.
13. Mumoli N, Vitale J, Giorgi-Pierfranceschi M, et al. Accuracy of nurse-performed lung ultrasound in patients with acute dyspnea: a prospective observational study. Medicine (Baltimore). 2016;95(9):e2925. https://doi.org/10.1097/MD.0000000000002925.
14. Carlino MV, Paladino F, Sforza A, et al. Assessment of left atrial size in addition to focused cardiopulmonary ultrasound improves diagnostic accuracy of acute heart failure in the emergency department. Echocardiography (Mount Kisco, NY). 2018;35(6):785-791. https://doi.org/10.1111/echo.13851.
15. Russell FM, Ehrman RR. A modified lung and cardiac ultrasound protocol saves time and rules in the diagnosis of acute heart failure. J Emerg Med. 2017;52(6):839-845. https://doi.org/10.1016/j.jemermed.2017.02.003.
16. Maw AM, Hassanin A, Ho PM, et al. diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(3):e190703. https://doi.org/10.1001/jamanetworkopen.2019.0703.
© 2020 Society of Hospital Medicine
Leadership & Professional Development: Get to the “Both/And”
“For every complex problem there is a simple solution. And it’s wrong.”
—Anonymous as quoted in Barry Johnson’s Polarity Management1
Hospital medicine leaders often face what seem like unsolvable problems involving two opposing sides or viewpoints. Examples include individual versus team, margin versus mission, learner autonomy versus supervision, and customization versus standardization. Dr. Barry Johnson describes these dyads as polarities, which are two different values or points of view that are interdependent.1,2 Leaders who fail to realize this concept create a problem by artificially inserting the word ‘versus’ between the poles.
Polarities are not problems to be solved. How does one solve individual? Or team? How can a hospital have one without the other? When leaders treat polarities like problems to be solved, they typically crusade for one side over the other, until the losing side rises up for its own cause, causing a perpetual back and forth cycle described as an infinity loop where nobody is happy for long.1
How then can leaders avoid getting caught in this fruitless cycle?
Instead of trying to solve the unsolvable, learn to manage polarities. Polarity management seeks to maximize the best of both poles while minimizing the worst. Both sides of a polarity carry upsides and downsides. When leaders want change, or want to resist change, it is the fear of being caught in the downsides of the opposite pole that motivates behavior, and dominates conversation. The first step to changing this conversation is to introduce the concept to your team so they recognize polarities when they arise and model approaching issues in this manner.
Some issues truly are problems to be solved (for example, the ultrasound machine is broken and needs to be repaired), but many conflicts are polarities masquerading as problems. To identify polarities, ask two questions. (1) Is the situation ongoing? (2) Are there two interdependent poles? If yes, then the issue is a polarity. Ideal polarity management involves maximizing the upside values of both poles before potential conflict even begins. People often force themselves into unnecessary “either/or” mindsets rather than striving for “both/and”.
Here is a classic example in Hospital Medicine: Pole 1: customization Pole 2: standardization -- The Chief Medical Information Officer (CMIO) wants everyone to use the same electronic health record (EHR) template, while the hospitalist group wants to innovate templates using rapid cycles of change. Typical patterns of conflict: the CMIO releases a template and the hospitalists resent it, or the hospitalists each create their own notes but the CMIO bemoans the variability.
Once polarities are recognized, teams can draw a ‘polarity map’ to see the whole picture, identifying the upside values and downside fears of each pole.1,2 For example, standardization reduces unnecessary variation, but stifles innovation, while customization does the opposite. In fact, the upside values of one pole are usually the opposite of the downside fears of the other.
Leaders can actively engage people in both poles to make opposing views productive rather than destructive. The CMIO in our standardization/customization example could insist that everyone begins with the same template, but allow hospitalists to innovate to find a better way. Now the most resistant hospitalists become improvement agents. If a better way is found, then this becomes the new template that all hospitalists use, until the next better way is found. If an innovation is not an improvement, then hospitalists agree to return to the most recent successful template until a better way is found. This method of action and compromise produces both standardization and customization.
Using polarity management strategies does not guarantee success, but it can help engage all stakeholders, and break the frustrating cycle of repeatedly trying to solve the unsolvable.
Disclosures
The authors report no conflicts of interest or sources of funding.
1. Johnson B. Polarity management: Identifying and managing unsolvable problems. Human Resource Development; 1992.
2. Wesorick BL. Polarity thinking: An essential skill for those leading interprofessional integration. J Interprofessional Healthcare. 2014;1(1):12.
“For every complex problem there is a simple solution. And it’s wrong.”
—Anonymous as quoted in Barry Johnson’s Polarity Management1
Hospital medicine leaders often face what seem like unsolvable problems involving two opposing sides or viewpoints. Examples include individual versus team, margin versus mission, learner autonomy versus supervision, and customization versus standardization. Dr. Barry Johnson describes these dyads as polarities, which are two different values or points of view that are interdependent.1,2 Leaders who fail to realize this concept create a problem by artificially inserting the word ‘versus’ between the poles.
Polarities are not problems to be solved. How does one solve individual? Or team? How can a hospital have one without the other? When leaders treat polarities like problems to be solved, they typically crusade for one side over the other, until the losing side rises up for its own cause, causing a perpetual back and forth cycle described as an infinity loop where nobody is happy for long.1
How then can leaders avoid getting caught in this fruitless cycle?
Instead of trying to solve the unsolvable, learn to manage polarities. Polarity management seeks to maximize the best of both poles while minimizing the worst. Both sides of a polarity carry upsides and downsides. When leaders want change, or want to resist change, it is the fear of being caught in the downsides of the opposite pole that motivates behavior, and dominates conversation. The first step to changing this conversation is to introduce the concept to your team so they recognize polarities when they arise and model approaching issues in this manner.
Some issues truly are problems to be solved (for example, the ultrasound machine is broken and needs to be repaired), but many conflicts are polarities masquerading as problems. To identify polarities, ask two questions. (1) Is the situation ongoing? (2) Are there two interdependent poles? If yes, then the issue is a polarity. Ideal polarity management involves maximizing the upside values of both poles before potential conflict even begins. People often force themselves into unnecessary “either/or” mindsets rather than striving for “both/and”.
Here is a classic example in Hospital Medicine: Pole 1: customization Pole 2: standardization -- The Chief Medical Information Officer (CMIO) wants everyone to use the same electronic health record (EHR) template, while the hospitalist group wants to innovate templates using rapid cycles of change. Typical patterns of conflict: the CMIO releases a template and the hospitalists resent it, or the hospitalists each create their own notes but the CMIO bemoans the variability.
Once polarities are recognized, teams can draw a ‘polarity map’ to see the whole picture, identifying the upside values and downside fears of each pole.1,2 For example, standardization reduces unnecessary variation, but stifles innovation, while customization does the opposite. In fact, the upside values of one pole are usually the opposite of the downside fears of the other.
Leaders can actively engage people in both poles to make opposing views productive rather than destructive. The CMIO in our standardization/customization example could insist that everyone begins with the same template, but allow hospitalists to innovate to find a better way. Now the most resistant hospitalists become improvement agents. If a better way is found, then this becomes the new template that all hospitalists use, until the next better way is found. If an innovation is not an improvement, then hospitalists agree to return to the most recent successful template until a better way is found. This method of action and compromise produces both standardization and customization.
Using polarity management strategies does not guarantee success, but it can help engage all stakeholders, and break the frustrating cycle of repeatedly trying to solve the unsolvable.
Disclosures
The authors report no conflicts of interest or sources of funding.
“For every complex problem there is a simple solution. And it’s wrong.”
—Anonymous as quoted in Barry Johnson’s Polarity Management1
Hospital medicine leaders often face what seem like unsolvable problems involving two opposing sides or viewpoints. Examples include individual versus team, margin versus mission, learner autonomy versus supervision, and customization versus standardization. Dr. Barry Johnson describes these dyads as polarities, which are two different values or points of view that are interdependent.1,2 Leaders who fail to realize this concept create a problem by artificially inserting the word ‘versus’ between the poles.
Polarities are not problems to be solved. How does one solve individual? Or team? How can a hospital have one without the other? When leaders treat polarities like problems to be solved, they typically crusade for one side over the other, until the losing side rises up for its own cause, causing a perpetual back and forth cycle described as an infinity loop where nobody is happy for long.1
How then can leaders avoid getting caught in this fruitless cycle?
Instead of trying to solve the unsolvable, learn to manage polarities. Polarity management seeks to maximize the best of both poles while minimizing the worst. Both sides of a polarity carry upsides and downsides. When leaders want change, or want to resist change, it is the fear of being caught in the downsides of the opposite pole that motivates behavior, and dominates conversation. The first step to changing this conversation is to introduce the concept to your team so they recognize polarities when they arise and model approaching issues in this manner.
Some issues truly are problems to be solved (for example, the ultrasound machine is broken and needs to be repaired), but many conflicts are polarities masquerading as problems. To identify polarities, ask two questions. (1) Is the situation ongoing? (2) Are there two interdependent poles? If yes, then the issue is a polarity. Ideal polarity management involves maximizing the upside values of both poles before potential conflict even begins. People often force themselves into unnecessary “either/or” mindsets rather than striving for “both/and”.
Here is a classic example in Hospital Medicine: Pole 1: customization Pole 2: standardization -- The Chief Medical Information Officer (CMIO) wants everyone to use the same electronic health record (EHR) template, while the hospitalist group wants to innovate templates using rapid cycles of change. Typical patterns of conflict: the CMIO releases a template and the hospitalists resent it, or the hospitalists each create their own notes but the CMIO bemoans the variability.
Once polarities are recognized, teams can draw a ‘polarity map’ to see the whole picture, identifying the upside values and downside fears of each pole.1,2 For example, standardization reduces unnecessary variation, but stifles innovation, while customization does the opposite. In fact, the upside values of one pole are usually the opposite of the downside fears of the other.
Leaders can actively engage people in both poles to make opposing views productive rather than destructive. The CMIO in our standardization/customization example could insist that everyone begins with the same template, but allow hospitalists to innovate to find a better way. Now the most resistant hospitalists become improvement agents. If a better way is found, then this becomes the new template that all hospitalists use, until the next better way is found. If an innovation is not an improvement, then hospitalists agree to return to the most recent successful template until a better way is found. This method of action and compromise produces both standardization and customization.
Using polarity management strategies does not guarantee success, but it can help engage all stakeholders, and break the frustrating cycle of repeatedly trying to solve the unsolvable.
Disclosures
The authors report no conflicts of interest or sources of funding.
1. Johnson B. Polarity management: Identifying and managing unsolvable problems. Human Resource Development; 1992.
2. Wesorick BL. Polarity thinking: An essential skill for those leading interprofessional integration. J Interprofessional Healthcare. 2014;1(1):12.
1. Johnson B. Polarity management: Identifying and managing unsolvable problems. Human Resource Development; 1992.
2. Wesorick BL. Polarity thinking: An essential skill for those leading interprofessional integration. J Interprofessional Healthcare. 2014;1(1):12.
© 2019 Society of Hospital Medicine
Clinical Progress Note: Point-of-Care Ultrasound for the Pediatric Hospitalist
The recent designation of Pediatric Hospital Medicine (PHM) as a board-certified subspecialty has provided the opportunity to define which skills are core to hospitalist practice. One skill that is novel to the field and gaining traction is point-of-care ultrasonography (POCUS). POCUS differs from traditional ultrasonography in that it is performed at the bedside by the primary clinician and aims to answer a focused clinical question (eg, does this patient have a skin abscess?) rather than to provide a comprehensive evaluation of the anatomy and physiology. The proposed advantages of POCUS include real-time image interpretation, cost savings, procedural guidance to minimize complications, and reduction of ionizing radiation. Although specialties such as Critical Care (CC) and Emergency Medicine (EM) have integrated POCUS into their practice and training, best practices in PHM have not been defined. This Progress Note is a summary of recent evidence to update past reviews and set the stage for future PHM POCUS research and education.
LITERATURE SEARCH STRATEGY AND TOPIC SELECTION
We met with an academic librarian in March 2019 and performed a search of PubMed using Medical Subject Headings (MESH) terms associated with POCUS as well as Pediatrics. We limited our search to studies published within the past five years. The search was originally focused to the field of PHM before expanding to a broader search since very few studies were found that focused on Hospital Medicine or general pediatric ward populations. This initial search generated 274 publications. We then performed a supplemental literature search using references from studies found in our initial search, as well as further ad hoc searching in Embase and Google Scholar.
After our literature search, we reviewed the PHM core competencies and identified the common clinical diagnoses and core skills for which there is POCUS literature published in the past five years. These included acute abdominal pain, bronchiolitis, pneumonia, skin and soft tissue infection, newborn care/delivery room management, bladder catheterization, fluid management, intravenous access, and lumbar puncture (LP). We chose to focus on one skill and two diagnoses that were generalizable to pediatric hospitalists across different settings and for which there was compelling evidence for POCUS use, such as pneumonia, skin abscess, and LP. We found few studies that included general pediatric ward patients, but we considered EM and CC studies to be relevant as several pediatric hospitalists practice in these clinical settings and with these patient populations.
PNEUMONIA
POCUS can be useful for diagnosing pneumonia by direct visualization of lung consolidation or by identification of various sonographic artifacts that suggest pathology. For example, “B-lines” are vertical artifacts that extend from the pleura and suggest interstitial fluid or pneumonia when they are present in abnormally high numbers or density. POCUS can also be used to diagnose parapneumonic effusions by scanning dependent areas of the lung (eg, the diaphragm in children sitting upright) and looking for anechoic or hypoechoic areas.
Three recent meta-analyses found favorable operating characteristics when using POCUS for the diagnosis of pneumonia in children, with summary sensitivities of 93%-94% and specificities of 92%-96%.1-3 However, these meta-analyses were limited by high heterogeneity due to the inclusion of multiple different care settings and the use of variable reference standards and sonographic criteria for diagnosing pneumonia. POCUS is superior to chest radiography for evaluating parapneumonic pleural effusions,4 allowing for rapid identification of loculations, fibrin strands, and proteinaceous material, and for serial bedside evaluation of effusion size and characteristics.
Additional advantages of POCUS include avoidance of ionizing radiation and the potential for cost and time savings. Two studies demonstrated reductions in radiography use and improved cost, although they were not conducted on hospitalized patients. One randomized controlled trial (RCT) conducted in a pediatric emergency department (ED) demonstrated a 38.8% reduction in chest radiography use without increasing the ED length of stay (EDLOS), antibiotic use, or unscheduled follow-up visits.5 A retrospective matched cohort study conducted in another pediatric ED reported that when compared with patients evaluated by chest radiography, those evaluated by POCUS had significantly shorter EDLOS (−60.9 min) and mean health systems savings ($187 per patient).6 We believe that POCUS has value in the evaluation and management of pneumonia and parapneumonic effusions, although further studies investigating patient outcomes and involving inpatient populations are required.
SKIN ABSCESS
POCUS can augment the physical examination, helping to both avoid unnecessary incision and drainage (I+D) procedures and detect drainable fluid collections. Abscess is suggested when hypoechoic material without vascular flow is detected, and although other structures such as vessels, cysts, and lymph nodes can mimic skin abscesses, this is a relatively straightforward examination for clinicians to learn.
Two meta-analyses found that POCUS had high sensitivity for diagnosing skin abscesses in the ED.7,8 A pediatric subgroup analysis conducted in a study by Barbic et al. found a sensitivity and a specificity of 94% (95% C: 88%-98%) and 83% (95% C: 47%-97%), respectively.7 Subramaniam et al. included six studies (four pediatric) with 800 patients (653 ≤ 18 years old) and found an overall pooled sensitivity of 97% (95% C: 94%-98%) and a specificity of 83% (95% C: 75%-88%).8 No subgroup analysis was performed, but the included pediatric studies reported sensitivities and specificities between 90%-98% and 68%-87%, respectively.
Although POCUS performs better than physical examination for the diagnosis of drainable abscesses, evidence regarding patient outcomes is mixed. A retrospective review from four pediatric EDs found that integration of POCUS lowered treatment failure rates, defined as any incision and drainage (I+D) or surgical manipulation after discharge from the initial ED visit (4.4% vs 15.6%, P < .005).9 A single-center retrospective cohort study found that POCUS reduced EDLOS by a median of 73 minutes (95% C: 52-94 min) when compared with radiology-performed studies.10 The aforementioned study conducted by Barbic et al. found that in pediatric studies, POCUS led to a change in management (eg, whether or not to attempt I+D) in 14%-27% of patients.7 However, a multicenter prospective observational cohort study involving seven pediatric EDs found that despite changing the management in 22.9% of cases, POCUS was not associated with any statistically significant differences in treatment failure rates, EDLOS, discharge rates, use of sedation, or use of alternative imaging.11 These studies were limited by a lack of randomization or control group and emphasize the need for RCTs that measure patient outcomes. Future studies should investigate how POCUS can be used in inpatient settings both for initial diagnosis of drainable abscesses and for serial evaluation of evolving phlegmon or incompletely drained collections.
LUMBAR PUNCTURE
LP is commonly performed by pediatric hospitalists, although success can be influenced by numerous factors, including provider and staff expertise, patient anatomy, and body habitus. Requiring multiple attempts can increase patient discomfort and parental anxiety. Failure to obtain cerebrospinal fluid can delay diagnosis or leave providers in uncertain clinical situations that may commit patients to prolonged antibiotic courses. POCUS can be used to identify anatomic markers such as interspinous processes, anatomic midline, and depth of the ligamentum flavum.12 It can also be used to identify epidural hematomas after failed LPs to avoid additional unsuccessful attempts.13 POCUS guidance for LP has been described using both static (preprocedural marking) and dynamic (scanning during the procedure) techniques, although most of the studies use the static approach. The Society for Hospital Medicine POCUS Task Force has recently released a position statement recommending that POCUS should be used for site selection before performing LP in adult patients when providers are adequately trained.12 Although this position statement was for adult patients, recent evidence suggests that there is also benefit in Pediatrics.
Two recent meta-analyses have investigated POCUS use for pediatric LPs.14,15 Olowoyeye et al. included four studies with a total of 277 patients and found that POCUS use was associated with a reduction in traumatic taps (risk ratio [RR] = 0.53, 95% C: 0.13-0.82) when compared with landmark approaches.14 However, there was no statistically significant reduction in LP failure, number of needle insertion attempts, or procedure length. A more recent meta-analysis performed a pediatric subgroup analysis of six studies including 452 patients and found a statistically significant reduction in traumatic taps (13.7% vs 31.8%, risk difference = −21.3%, 95% C: −38.2% to −4.3%) and number of needle insertion attempts (1.53 vs 2.07, mean difference = −0.47, 95% C: −0.73 to −0.21).15 The primary outcome of LP success trended toward favoring POCUS, but it was not statistically significant (88.4% vs 74.0%, OR = 2.55, 95% C: 0.99-6.52). We believe t
CONCLUSION
Evidence accumulated in the past five years has built on previous work suggesting that POCUS has a role in the diagnosis of pneumonia and skin abscess and in the performance of LPs. However, gaps in the literature remain when applying POCUS in PHM. Only a few studies to date were conducted in non-CC inpatient settings, and although several pediatric hospitalists work in EDs or care for critically ill children, our largest population comprises general pediatric ward patients. Studies have also used ultrasonographers with variable POCUS training and clinical experience, which makes comparing or combining studies challenging since POCUS is dependent on provider skills. Studies involving PHM providers and inpatient populations are needed. Additional studies evaluating the process and outcome measures are also needed to understand whether the theoretical advantages are consistently realized in real-world PHM practice. Finally, PHM-specific curricula should be designed in collaboration with various PHM stakeholders and with specialties who already have robust POCUS training pathways. There is opportunity within PHM for multi institutional research collaboration, identification of best practices, and development of PHM-specific training for fellowship and faculty development programs.
1. Orso D, Ban A, Guglielmo N. Lung ultrasound in diagnosing pneumonia in childhood: a systematic review and meta-analysis. J Ultrasound. 2018;21(3):183-195. https://doi.org/10.1007/s40477-018-0306-5.
2. Najgrodzka P, Buda N, Zamojska A, Marciniewicz E, Lewandowicz-Uszynska A. Lung ultrasonography in the diagnosis of pneumonia in children-a metaanalysis and a review of pediatric lung imaging. Ultrasound Q. 2019; 35(2):157-163. https://doi.org/10.1097/RUQ.0000000000000411.
3. Xin H, Li J, Hu HY. Is lung ultrasound useful for diagnosing pneumonia in children?: a meta-analysis and systematic review. Ultrasound Q. 2018;34(1):3-10. https://doi.org/10.1097/RUQ.0000000000000330.
4. Esposito S, Papa SS, Borzani I, et al. Performance of lung ultrasonography in children with community-acquired pneumonia. Ital J Pediatr. 2014;40(1):37. https://doi.org/10.1186/1824-7288-40-37.
5. Jones BP, Tay ET, Elikashvili I, et al. Feasibility and safety of substituting lung ultrasonography for chest radiography when diagnosing pneumonia in children: a randomized controlled trial. Chest. 2016;150(1):131-138. https://doi.org/10.1016/j.chest.2016.02.643.
6. Harel‐Sterling M, Diallo M, Santhirakumaran S, Maxim T, Tessaro M. Emergency department resource use in pediatric pneumonia: point‐of‐care lung ultrasonography versus chest radiography. J Ultrasound Med. 2019;38(2):407-414. https://doi.org/10.1002/jum.14703.
7. Barbic D, Chenkin J, Cho DD, Jelic T, Scheuermeyer FX. In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis. BMJ Open. 2017;7(1):e013688. https://doi.org/10.1136/bmjopen-2016-013688.
8. Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care ultrasound for diagnosis of abscess in skin and soft tissue infections. Acad Emerg Med. 2016;23(11):1298-1306. https://doi.org/10.1111/acem.13049.
9. Gaspari RJ, Sanseverino A. Ultrasound-guided drainage for pediatric soft tissue abscesses decreases clinical failure rates compared to drainage without ultrasound: a retrospective study. J Ultrasound Med. 2018;37(1):131-136. https://doi.org/10.1002/jum.14318.
10. Lin MJ, Neuman M, Rempell R, Monuteaux M, Levy J. Point-of-care ultrasound is associated with decreased length of stay in children presenting to the emergency department with soft tissue infection. J Emerg Med. 2018;54(1):96-101. https://doi.org/10.1016/j.jemermed.2017.09.017.
11. Lam SHF, Sivitz A, Alade K, et al. Comparison of ultrasound guidance vs. clinical assessment alone for management of pediatric skin and soft tissue infections. J Emerg Med. 2018;55(5):693-701. https://doi.org/10.1016/j.jemermed.2018.07.010.
12. Soni NJ, Franco-Sadud R, Kobaidze K, et al. Recommendations on the use of ultrasound guidance for adult lumbar puncture: a position statement of the society of hospital medicine [published online ahead of print June 10, 2019. J Hosp Med. 2019;14:E1-E11. https://doi.org/10.12788/jhm.3197.
13. Kusulas MP, Eutsler EP, DePiero AD. Bedside ultrasound for the evaluation of epidural hematoma after infant lumbar puncture [published online ahead of print January 2, 2018]. Pediatr Emerg Care. 2018. https://doi.org/10.1097/PEC.0000000000001383.
14. Olowoyeye A, Fadahunsi O, Okudo J, Opaneye O, Okwundu C. Ultrasound imaging versus palpation method for diagnostic lumbar puncture in neonates and infants: a systematic review and meta-analysis. BMJ Paediatr Open. 2019;3(1):e000412. https://doi.org/10.1136/bmjpo-2018-000412
15. Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2019;26(1):85-96. https://doi.org/10.1111/acem.13558.
The recent designation of Pediatric Hospital Medicine (PHM) as a board-certified subspecialty has provided the opportunity to define which skills are core to hospitalist practice. One skill that is novel to the field and gaining traction is point-of-care ultrasonography (POCUS). POCUS differs from traditional ultrasonography in that it is performed at the bedside by the primary clinician and aims to answer a focused clinical question (eg, does this patient have a skin abscess?) rather than to provide a comprehensive evaluation of the anatomy and physiology. The proposed advantages of POCUS include real-time image interpretation, cost savings, procedural guidance to minimize complications, and reduction of ionizing radiation. Although specialties such as Critical Care (CC) and Emergency Medicine (EM) have integrated POCUS into their practice and training, best practices in PHM have not been defined. This Progress Note is a summary of recent evidence to update past reviews and set the stage for future PHM POCUS research and education.
LITERATURE SEARCH STRATEGY AND TOPIC SELECTION
We met with an academic librarian in March 2019 and performed a search of PubMed using Medical Subject Headings (MESH) terms associated with POCUS as well as Pediatrics. We limited our search to studies published within the past five years. The search was originally focused to the field of PHM before expanding to a broader search since very few studies were found that focused on Hospital Medicine or general pediatric ward populations. This initial search generated 274 publications. We then performed a supplemental literature search using references from studies found in our initial search, as well as further ad hoc searching in Embase and Google Scholar.
After our literature search, we reviewed the PHM core competencies and identified the common clinical diagnoses and core skills for which there is POCUS literature published in the past five years. These included acute abdominal pain, bronchiolitis, pneumonia, skin and soft tissue infection, newborn care/delivery room management, bladder catheterization, fluid management, intravenous access, and lumbar puncture (LP). We chose to focus on one skill and two diagnoses that were generalizable to pediatric hospitalists across different settings and for which there was compelling evidence for POCUS use, such as pneumonia, skin abscess, and LP. We found few studies that included general pediatric ward patients, but we considered EM and CC studies to be relevant as several pediatric hospitalists practice in these clinical settings and with these patient populations.
PNEUMONIA
POCUS can be useful for diagnosing pneumonia by direct visualization of lung consolidation or by identification of various sonographic artifacts that suggest pathology. For example, “B-lines” are vertical artifacts that extend from the pleura and suggest interstitial fluid or pneumonia when they are present in abnormally high numbers or density. POCUS can also be used to diagnose parapneumonic effusions by scanning dependent areas of the lung (eg, the diaphragm in children sitting upright) and looking for anechoic or hypoechoic areas.
Three recent meta-analyses found favorable operating characteristics when using POCUS for the diagnosis of pneumonia in children, with summary sensitivities of 93%-94% and specificities of 92%-96%.1-3 However, these meta-analyses were limited by high heterogeneity due to the inclusion of multiple different care settings and the use of variable reference standards and sonographic criteria for diagnosing pneumonia. POCUS is superior to chest radiography for evaluating parapneumonic pleural effusions,4 allowing for rapid identification of loculations, fibrin strands, and proteinaceous material, and for serial bedside evaluation of effusion size and characteristics.
Additional advantages of POCUS include avoidance of ionizing radiation and the potential for cost and time savings. Two studies demonstrated reductions in radiography use and improved cost, although they were not conducted on hospitalized patients. One randomized controlled trial (RCT) conducted in a pediatric emergency department (ED) demonstrated a 38.8% reduction in chest radiography use without increasing the ED length of stay (EDLOS), antibiotic use, or unscheduled follow-up visits.5 A retrospective matched cohort study conducted in another pediatric ED reported that when compared with patients evaluated by chest radiography, those evaluated by POCUS had significantly shorter EDLOS (−60.9 min) and mean health systems savings ($187 per patient).6 We believe that POCUS has value in the evaluation and management of pneumonia and parapneumonic effusions, although further studies investigating patient outcomes and involving inpatient populations are required.
SKIN ABSCESS
POCUS can augment the physical examination, helping to both avoid unnecessary incision and drainage (I+D) procedures and detect drainable fluid collections. Abscess is suggested when hypoechoic material without vascular flow is detected, and although other structures such as vessels, cysts, and lymph nodes can mimic skin abscesses, this is a relatively straightforward examination for clinicians to learn.
Two meta-analyses found that POCUS had high sensitivity for diagnosing skin abscesses in the ED.7,8 A pediatric subgroup analysis conducted in a study by Barbic et al. found a sensitivity and a specificity of 94% (95% C: 88%-98%) and 83% (95% C: 47%-97%), respectively.7 Subramaniam et al. included six studies (four pediatric) with 800 patients (653 ≤ 18 years old) and found an overall pooled sensitivity of 97% (95% C: 94%-98%) and a specificity of 83% (95% C: 75%-88%).8 No subgroup analysis was performed, but the included pediatric studies reported sensitivities and specificities between 90%-98% and 68%-87%, respectively.
Although POCUS performs better than physical examination for the diagnosis of drainable abscesses, evidence regarding patient outcomes is mixed. A retrospective review from four pediatric EDs found that integration of POCUS lowered treatment failure rates, defined as any incision and drainage (I+D) or surgical manipulation after discharge from the initial ED visit (4.4% vs 15.6%, P < .005).9 A single-center retrospective cohort study found that POCUS reduced EDLOS by a median of 73 minutes (95% C: 52-94 min) when compared with radiology-performed studies.10 The aforementioned study conducted by Barbic et al. found that in pediatric studies, POCUS led to a change in management (eg, whether or not to attempt I+D) in 14%-27% of patients.7 However, a multicenter prospective observational cohort study involving seven pediatric EDs found that despite changing the management in 22.9% of cases, POCUS was not associated with any statistically significant differences in treatment failure rates, EDLOS, discharge rates, use of sedation, or use of alternative imaging.11 These studies were limited by a lack of randomization or control group and emphasize the need for RCTs that measure patient outcomes. Future studies should investigate how POCUS can be used in inpatient settings both for initial diagnosis of drainable abscesses and for serial evaluation of evolving phlegmon or incompletely drained collections.
LUMBAR PUNCTURE
LP is commonly performed by pediatric hospitalists, although success can be influenced by numerous factors, including provider and staff expertise, patient anatomy, and body habitus. Requiring multiple attempts can increase patient discomfort and parental anxiety. Failure to obtain cerebrospinal fluid can delay diagnosis or leave providers in uncertain clinical situations that may commit patients to prolonged antibiotic courses. POCUS can be used to identify anatomic markers such as interspinous processes, anatomic midline, and depth of the ligamentum flavum.12 It can also be used to identify epidural hematomas after failed LPs to avoid additional unsuccessful attempts.13 POCUS guidance for LP has been described using both static (preprocedural marking) and dynamic (scanning during the procedure) techniques, although most of the studies use the static approach. The Society for Hospital Medicine POCUS Task Force has recently released a position statement recommending that POCUS should be used for site selection before performing LP in adult patients when providers are adequately trained.12 Although this position statement was for adult patients, recent evidence suggests that there is also benefit in Pediatrics.
Two recent meta-analyses have investigated POCUS use for pediatric LPs.14,15 Olowoyeye et al. included four studies with a total of 277 patients and found that POCUS use was associated with a reduction in traumatic taps (risk ratio [RR] = 0.53, 95% C: 0.13-0.82) when compared with landmark approaches.14 However, there was no statistically significant reduction in LP failure, number of needle insertion attempts, or procedure length. A more recent meta-analysis performed a pediatric subgroup analysis of six studies including 452 patients and found a statistically significant reduction in traumatic taps (13.7% vs 31.8%, risk difference = −21.3%, 95% C: −38.2% to −4.3%) and number of needle insertion attempts (1.53 vs 2.07, mean difference = −0.47, 95% C: −0.73 to −0.21).15 The primary outcome of LP success trended toward favoring POCUS, but it was not statistically significant (88.4% vs 74.0%, OR = 2.55, 95% C: 0.99-6.52). We believe t
CONCLUSION
Evidence accumulated in the past five years has built on previous work suggesting that POCUS has a role in the diagnosis of pneumonia and skin abscess and in the performance of LPs. However, gaps in the literature remain when applying POCUS in PHM. Only a few studies to date were conducted in non-CC inpatient settings, and although several pediatric hospitalists work in EDs or care for critically ill children, our largest population comprises general pediatric ward patients. Studies have also used ultrasonographers with variable POCUS training and clinical experience, which makes comparing or combining studies challenging since POCUS is dependent on provider skills. Studies involving PHM providers and inpatient populations are needed. Additional studies evaluating the process and outcome measures are also needed to understand whether the theoretical advantages are consistently realized in real-world PHM practice. Finally, PHM-specific curricula should be designed in collaboration with various PHM stakeholders and with specialties who already have robust POCUS training pathways. There is opportunity within PHM for multi institutional research collaboration, identification of best practices, and development of PHM-specific training for fellowship and faculty development programs.
The recent designation of Pediatric Hospital Medicine (PHM) as a board-certified subspecialty has provided the opportunity to define which skills are core to hospitalist practice. One skill that is novel to the field and gaining traction is point-of-care ultrasonography (POCUS). POCUS differs from traditional ultrasonography in that it is performed at the bedside by the primary clinician and aims to answer a focused clinical question (eg, does this patient have a skin abscess?) rather than to provide a comprehensive evaluation of the anatomy and physiology. The proposed advantages of POCUS include real-time image interpretation, cost savings, procedural guidance to minimize complications, and reduction of ionizing radiation. Although specialties such as Critical Care (CC) and Emergency Medicine (EM) have integrated POCUS into their practice and training, best practices in PHM have not been defined. This Progress Note is a summary of recent evidence to update past reviews and set the stage for future PHM POCUS research and education.
LITERATURE SEARCH STRATEGY AND TOPIC SELECTION
We met with an academic librarian in March 2019 and performed a search of PubMed using Medical Subject Headings (MESH) terms associated with POCUS as well as Pediatrics. We limited our search to studies published within the past five years. The search was originally focused to the field of PHM before expanding to a broader search since very few studies were found that focused on Hospital Medicine or general pediatric ward populations. This initial search generated 274 publications. We then performed a supplemental literature search using references from studies found in our initial search, as well as further ad hoc searching in Embase and Google Scholar.
After our literature search, we reviewed the PHM core competencies and identified the common clinical diagnoses and core skills for which there is POCUS literature published in the past five years. These included acute abdominal pain, bronchiolitis, pneumonia, skin and soft tissue infection, newborn care/delivery room management, bladder catheterization, fluid management, intravenous access, and lumbar puncture (LP). We chose to focus on one skill and two diagnoses that were generalizable to pediatric hospitalists across different settings and for which there was compelling evidence for POCUS use, such as pneumonia, skin abscess, and LP. We found few studies that included general pediatric ward patients, but we considered EM and CC studies to be relevant as several pediatric hospitalists practice in these clinical settings and with these patient populations.
PNEUMONIA
POCUS can be useful for diagnosing pneumonia by direct visualization of lung consolidation or by identification of various sonographic artifacts that suggest pathology. For example, “B-lines” are vertical artifacts that extend from the pleura and suggest interstitial fluid or pneumonia when they are present in abnormally high numbers or density. POCUS can also be used to diagnose parapneumonic effusions by scanning dependent areas of the lung (eg, the diaphragm in children sitting upright) and looking for anechoic or hypoechoic areas.
Three recent meta-analyses found favorable operating characteristics when using POCUS for the diagnosis of pneumonia in children, with summary sensitivities of 93%-94% and specificities of 92%-96%.1-3 However, these meta-analyses were limited by high heterogeneity due to the inclusion of multiple different care settings and the use of variable reference standards and sonographic criteria for diagnosing pneumonia. POCUS is superior to chest radiography for evaluating parapneumonic pleural effusions,4 allowing for rapid identification of loculations, fibrin strands, and proteinaceous material, and for serial bedside evaluation of effusion size and characteristics.
Additional advantages of POCUS include avoidance of ionizing radiation and the potential for cost and time savings. Two studies demonstrated reductions in radiography use and improved cost, although they were not conducted on hospitalized patients. One randomized controlled trial (RCT) conducted in a pediatric emergency department (ED) demonstrated a 38.8% reduction in chest radiography use without increasing the ED length of stay (EDLOS), antibiotic use, or unscheduled follow-up visits.5 A retrospective matched cohort study conducted in another pediatric ED reported that when compared with patients evaluated by chest radiography, those evaluated by POCUS had significantly shorter EDLOS (−60.9 min) and mean health systems savings ($187 per patient).6 We believe that POCUS has value in the evaluation and management of pneumonia and parapneumonic effusions, although further studies investigating patient outcomes and involving inpatient populations are required.
SKIN ABSCESS
POCUS can augment the physical examination, helping to both avoid unnecessary incision and drainage (I+D) procedures and detect drainable fluid collections. Abscess is suggested when hypoechoic material without vascular flow is detected, and although other structures such as vessels, cysts, and lymph nodes can mimic skin abscesses, this is a relatively straightforward examination for clinicians to learn.
Two meta-analyses found that POCUS had high sensitivity for diagnosing skin abscesses in the ED.7,8 A pediatric subgroup analysis conducted in a study by Barbic et al. found a sensitivity and a specificity of 94% (95% C: 88%-98%) and 83% (95% C: 47%-97%), respectively.7 Subramaniam et al. included six studies (four pediatric) with 800 patients (653 ≤ 18 years old) and found an overall pooled sensitivity of 97% (95% C: 94%-98%) and a specificity of 83% (95% C: 75%-88%).8 No subgroup analysis was performed, but the included pediatric studies reported sensitivities and specificities between 90%-98% and 68%-87%, respectively.
Although POCUS performs better than physical examination for the diagnosis of drainable abscesses, evidence regarding patient outcomes is mixed. A retrospective review from four pediatric EDs found that integration of POCUS lowered treatment failure rates, defined as any incision and drainage (I+D) or surgical manipulation after discharge from the initial ED visit (4.4% vs 15.6%, P < .005).9 A single-center retrospective cohort study found that POCUS reduced EDLOS by a median of 73 minutes (95% C: 52-94 min) when compared with radiology-performed studies.10 The aforementioned study conducted by Barbic et al. found that in pediatric studies, POCUS led to a change in management (eg, whether or not to attempt I+D) in 14%-27% of patients.7 However, a multicenter prospective observational cohort study involving seven pediatric EDs found that despite changing the management in 22.9% of cases, POCUS was not associated with any statistically significant differences in treatment failure rates, EDLOS, discharge rates, use of sedation, or use of alternative imaging.11 These studies were limited by a lack of randomization or control group and emphasize the need for RCTs that measure patient outcomes. Future studies should investigate how POCUS can be used in inpatient settings both for initial diagnosis of drainable abscesses and for serial evaluation of evolving phlegmon or incompletely drained collections.
LUMBAR PUNCTURE
LP is commonly performed by pediatric hospitalists, although success can be influenced by numerous factors, including provider and staff expertise, patient anatomy, and body habitus. Requiring multiple attempts can increase patient discomfort and parental anxiety. Failure to obtain cerebrospinal fluid can delay diagnosis or leave providers in uncertain clinical situations that may commit patients to prolonged antibiotic courses. POCUS can be used to identify anatomic markers such as interspinous processes, anatomic midline, and depth of the ligamentum flavum.12 It can also be used to identify epidural hematomas after failed LPs to avoid additional unsuccessful attempts.13 POCUS guidance for LP has been described using both static (preprocedural marking) and dynamic (scanning during the procedure) techniques, although most of the studies use the static approach. The Society for Hospital Medicine POCUS Task Force has recently released a position statement recommending that POCUS should be used for site selection before performing LP in adult patients when providers are adequately trained.12 Although this position statement was for adult patients, recent evidence suggests that there is also benefit in Pediatrics.
Two recent meta-analyses have investigated POCUS use for pediatric LPs.14,15 Olowoyeye et al. included four studies with a total of 277 patients and found that POCUS use was associated with a reduction in traumatic taps (risk ratio [RR] = 0.53, 95% C: 0.13-0.82) when compared with landmark approaches.14 However, there was no statistically significant reduction in LP failure, number of needle insertion attempts, or procedure length. A more recent meta-analysis performed a pediatric subgroup analysis of six studies including 452 patients and found a statistically significant reduction in traumatic taps (13.7% vs 31.8%, risk difference = −21.3%, 95% C: −38.2% to −4.3%) and number of needle insertion attempts (1.53 vs 2.07, mean difference = −0.47, 95% C: −0.73 to −0.21).15 The primary outcome of LP success trended toward favoring POCUS, but it was not statistically significant (88.4% vs 74.0%, OR = 2.55, 95% C: 0.99-6.52). We believe t
CONCLUSION
Evidence accumulated in the past five years has built on previous work suggesting that POCUS has a role in the diagnosis of pneumonia and skin abscess and in the performance of LPs. However, gaps in the literature remain when applying POCUS in PHM. Only a few studies to date were conducted in non-CC inpatient settings, and although several pediatric hospitalists work in EDs or care for critically ill children, our largest population comprises general pediatric ward patients. Studies have also used ultrasonographers with variable POCUS training and clinical experience, which makes comparing or combining studies challenging since POCUS is dependent on provider skills. Studies involving PHM providers and inpatient populations are needed. Additional studies evaluating the process and outcome measures are also needed to understand whether the theoretical advantages are consistently realized in real-world PHM practice. Finally, PHM-specific curricula should be designed in collaboration with various PHM stakeholders and with specialties who already have robust POCUS training pathways. There is opportunity within PHM for multi institutional research collaboration, identification of best practices, and development of PHM-specific training for fellowship and faculty development programs.
1. Orso D, Ban A, Guglielmo N. Lung ultrasound in diagnosing pneumonia in childhood: a systematic review and meta-analysis. J Ultrasound. 2018;21(3):183-195. https://doi.org/10.1007/s40477-018-0306-5.
2. Najgrodzka P, Buda N, Zamojska A, Marciniewicz E, Lewandowicz-Uszynska A. Lung ultrasonography in the diagnosis of pneumonia in children-a metaanalysis and a review of pediatric lung imaging. Ultrasound Q. 2019; 35(2):157-163. https://doi.org/10.1097/RUQ.0000000000000411.
3. Xin H, Li J, Hu HY. Is lung ultrasound useful for diagnosing pneumonia in children?: a meta-analysis and systematic review. Ultrasound Q. 2018;34(1):3-10. https://doi.org/10.1097/RUQ.0000000000000330.
4. Esposito S, Papa SS, Borzani I, et al. Performance of lung ultrasonography in children with community-acquired pneumonia. Ital J Pediatr. 2014;40(1):37. https://doi.org/10.1186/1824-7288-40-37.
5. Jones BP, Tay ET, Elikashvili I, et al. Feasibility and safety of substituting lung ultrasonography for chest radiography when diagnosing pneumonia in children: a randomized controlled trial. Chest. 2016;150(1):131-138. https://doi.org/10.1016/j.chest.2016.02.643.
6. Harel‐Sterling M, Diallo M, Santhirakumaran S, Maxim T, Tessaro M. Emergency department resource use in pediatric pneumonia: point‐of‐care lung ultrasonography versus chest radiography. J Ultrasound Med. 2019;38(2):407-414. https://doi.org/10.1002/jum.14703.
7. Barbic D, Chenkin J, Cho DD, Jelic T, Scheuermeyer FX. In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis. BMJ Open. 2017;7(1):e013688. https://doi.org/10.1136/bmjopen-2016-013688.
8. Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care ultrasound for diagnosis of abscess in skin and soft tissue infections. Acad Emerg Med. 2016;23(11):1298-1306. https://doi.org/10.1111/acem.13049.
9. Gaspari RJ, Sanseverino A. Ultrasound-guided drainage for pediatric soft tissue abscesses decreases clinical failure rates compared to drainage without ultrasound: a retrospective study. J Ultrasound Med. 2018;37(1):131-136. https://doi.org/10.1002/jum.14318.
10. Lin MJ, Neuman M, Rempell R, Monuteaux M, Levy J. Point-of-care ultrasound is associated with decreased length of stay in children presenting to the emergency department with soft tissue infection. J Emerg Med. 2018;54(1):96-101. https://doi.org/10.1016/j.jemermed.2017.09.017.
11. Lam SHF, Sivitz A, Alade K, et al. Comparison of ultrasound guidance vs. clinical assessment alone for management of pediatric skin and soft tissue infections. J Emerg Med. 2018;55(5):693-701. https://doi.org/10.1016/j.jemermed.2018.07.010.
12. Soni NJ, Franco-Sadud R, Kobaidze K, et al. Recommendations on the use of ultrasound guidance for adult lumbar puncture: a position statement of the society of hospital medicine [published online ahead of print June 10, 2019. J Hosp Med. 2019;14:E1-E11. https://doi.org/10.12788/jhm.3197.
13. Kusulas MP, Eutsler EP, DePiero AD. Bedside ultrasound for the evaluation of epidural hematoma after infant lumbar puncture [published online ahead of print January 2, 2018]. Pediatr Emerg Care. 2018. https://doi.org/10.1097/PEC.0000000000001383.
14. Olowoyeye A, Fadahunsi O, Okudo J, Opaneye O, Okwundu C. Ultrasound imaging versus palpation method for diagnostic lumbar puncture in neonates and infants: a systematic review and meta-analysis. BMJ Paediatr Open. 2019;3(1):e000412. https://doi.org/10.1136/bmjpo-2018-000412
15. Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2019;26(1):85-96. https://doi.org/10.1111/acem.13558.
1. Orso D, Ban A, Guglielmo N. Lung ultrasound in diagnosing pneumonia in childhood: a systematic review and meta-analysis. J Ultrasound. 2018;21(3):183-195. https://doi.org/10.1007/s40477-018-0306-5.
2. Najgrodzka P, Buda N, Zamojska A, Marciniewicz E, Lewandowicz-Uszynska A. Lung ultrasonography in the diagnosis of pneumonia in children-a metaanalysis and a review of pediatric lung imaging. Ultrasound Q. 2019; 35(2):157-163. https://doi.org/10.1097/RUQ.0000000000000411.
3. Xin H, Li J, Hu HY. Is lung ultrasound useful for diagnosing pneumonia in children?: a meta-analysis and systematic review. Ultrasound Q. 2018;34(1):3-10. https://doi.org/10.1097/RUQ.0000000000000330.
4. Esposito S, Papa SS, Borzani I, et al. Performance of lung ultrasonography in children with community-acquired pneumonia. Ital J Pediatr. 2014;40(1):37. https://doi.org/10.1186/1824-7288-40-37.
5. Jones BP, Tay ET, Elikashvili I, et al. Feasibility and safety of substituting lung ultrasonography for chest radiography when diagnosing pneumonia in children: a randomized controlled trial. Chest. 2016;150(1):131-138. https://doi.org/10.1016/j.chest.2016.02.643.
6. Harel‐Sterling M, Diallo M, Santhirakumaran S, Maxim T, Tessaro M. Emergency department resource use in pediatric pneumonia: point‐of‐care lung ultrasonography versus chest radiography. J Ultrasound Med. 2019;38(2):407-414. https://doi.org/10.1002/jum.14703.
7. Barbic D, Chenkin J, Cho DD, Jelic T, Scheuermeyer FX. In patients presenting to the emergency department with skin and soft tissue infections what is the diagnostic accuracy of point-of-care ultrasonography for the diagnosis of abscess compared to the current standard of care? A systematic review and meta-analysis. BMJ Open. 2017;7(1):e013688. https://doi.org/10.1136/bmjopen-2016-013688.
8. Subramaniam S, Bober J, Chao J, Zehtabchi S. Point-of-care ultrasound for diagnosis of abscess in skin and soft tissue infections. Acad Emerg Med. 2016;23(11):1298-1306. https://doi.org/10.1111/acem.13049.
9. Gaspari RJ, Sanseverino A. Ultrasound-guided drainage for pediatric soft tissue abscesses decreases clinical failure rates compared to drainage without ultrasound: a retrospective study. J Ultrasound Med. 2018;37(1):131-136. https://doi.org/10.1002/jum.14318.
10. Lin MJ, Neuman M, Rempell R, Monuteaux M, Levy J. Point-of-care ultrasound is associated with decreased length of stay in children presenting to the emergency department with soft tissue infection. J Emerg Med. 2018;54(1):96-101. https://doi.org/10.1016/j.jemermed.2017.09.017.
11. Lam SHF, Sivitz A, Alade K, et al. Comparison of ultrasound guidance vs. clinical assessment alone for management of pediatric skin and soft tissue infections. J Emerg Med. 2018;55(5):693-701. https://doi.org/10.1016/j.jemermed.2018.07.010.
12. Soni NJ, Franco-Sadud R, Kobaidze K, et al. Recommendations on the use of ultrasound guidance for adult lumbar puncture: a position statement of the society of hospital medicine [published online ahead of print June 10, 2019. J Hosp Med. 2019;14:E1-E11. https://doi.org/10.12788/jhm.3197.
13. Kusulas MP, Eutsler EP, DePiero AD. Bedside ultrasound for the evaluation of epidural hematoma after infant lumbar puncture [published online ahead of print January 2, 2018]. Pediatr Emerg Care. 2018. https://doi.org/10.1097/PEC.0000000000001383.
14. Olowoyeye A, Fadahunsi O, Okudo J, Opaneye O, Okwundu C. Ultrasound imaging versus palpation method for diagnostic lumbar puncture in neonates and infants: a systematic review and meta-analysis. BMJ Paediatr Open. 2019;3(1):e000412. https://doi.org/10.1136/bmjpo-2018-000412
15. Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2019;26(1):85-96. https://doi.org/10.1111/acem.13558.
© 2020 Society of Hospital Medicine