User login
Depiction of Cancer in Movies: Not an Accurate Portrayal
This transcript has been edited for clarity.
I’d like to talk about a very different topic from what I normally discuss, which is probably relatively rarely addressed in clinical conversations among clinicians. There was a very provocative commentary that appeared in JCO Oncology Practice, titled “Hollywood’s Take on Oncology: Portrayal of Cancer in Movies, 2010-2020.”
All of us, as we grow up — as kids, adolescents, young adults, adults, and older individuals — watch television and movies. The older of us know that the doctor in everybody’s home that we all wanted was Marcus Welby. Of course, there was Dr. Kildare, ER, Grey’s Anatomy, and St. Elsewhere. There was Love Story and Brian’s Song. We all know about these.
This particular review was fascinating. The authors looked at 100 English-language movies that had cancer included in the storyline over the past decade. They asked some relatively simple questions: How did they discuss it? What were the tumor types they discussed? What were the outcomes?
The question is, what is the public seeing? If you watch these movies and you don’t have family experience or personal experience with cancer, what do you think about cancer? Maybe this is what you know about it. Despite what the National Cancer Institute or the American Society of Clinical Oncology tells you, this may be what you know.
What they showed was really quite interesting.
There is another very interesting phenomenon. What do you think was the most common cancer type when they did define the cancer? It was brain tumors, even though we know that brain tumors are certainly not even within the top 10. They’re obviously very serious cancers, but if you’re talking about common cancers, brain cancer doesn’t rank in the top 10, and it was the most common cancer on these shows.
The authors of this paper made the point of whether this would be an opportunity for filmmakers. Again, with the storyline, they’re trying to sell a product here, but wouldn’t this be the opportunity to provide some information about the reality of cancer? They could emphasize the fact that smokers get lung cancer. In my opinion, they could discuss cervical cancer and comment that if HPV vaccination had been done, maybe this would not have happened.
They noted that the majority of cancers in these movies were incurable, and they commented that that’s not the reality today. Today, obviously, many of our cancers that weren’t curable have become quite curable for a percentage of patients, in addition to which, obviously, with early detection, we have a very high cure rate. How about trying to get that message out, too, that we’ve actually had increasing success?
They commented that there was very rarely, if ever, a conversation about multidisciplinary care, that somehow there are multiple doctors with multiple specialties involved. They noted that this is potentially a very important message to give out. They commented that in 12 of these movies, the patient refused cancer care. Again, that happens, but it’s clearly a rare event today. Maybe this is not really a very accurate depiction of what’s going on.
They commented on the fact that, obviously, we’re going back through the past 10 years, so there were no patients who received immunotherapy or targeted therapy. Again, the goal here is not to sell oncology care but to be accurate, or more accurate, about the state of treatment to the extent you can.
They noted that, in fact, there was essentially very little, if any, comment on palliative care or hospice care. The final point they made is that there was very little conversation in these movies about what we now recognize as financial distress in many of our patients. That’s an unfortunate reality and perhaps that might come in the future.
Again, the point of this was not to tell Hollywood how to make their movies but to have the oncology community recognize that if their patients or the families of their patients are seeing these movies, they are not getting a very accurate picture of what is happening in the oncology world today and that some education may very well be required.
Maurie Markman is Professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California, and President of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed the following relevant financial relationships: income in an amount equal to or greater than $250 from: GlaxoSmithKline; AstraZeneca.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’d like to talk about a very different topic from what I normally discuss, which is probably relatively rarely addressed in clinical conversations among clinicians. There was a very provocative commentary that appeared in JCO Oncology Practice, titled “Hollywood’s Take on Oncology: Portrayal of Cancer in Movies, 2010-2020.”
All of us, as we grow up — as kids, adolescents, young adults, adults, and older individuals — watch television and movies. The older of us know that the doctor in everybody’s home that we all wanted was Marcus Welby. Of course, there was Dr. Kildare, ER, Grey’s Anatomy, and St. Elsewhere. There was Love Story and Brian’s Song. We all know about these.
This particular review was fascinating. The authors looked at 100 English-language movies that had cancer included in the storyline over the past decade. They asked some relatively simple questions: How did they discuss it? What were the tumor types they discussed? What were the outcomes?
The question is, what is the public seeing? If you watch these movies and you don’t have family experience or personal experience with cancer, what do you think about cancer? Maybe this is what you know about it. Despite what the National Cancer Institute or the American Society of Clinical Oncology tells you, this may be what you know.
What they showed was really quite interesting.
There is another very interesting phenomenon. What do you think was the most common cancer type when they did define the cancer? It was brain tumors, even though we know that brain tumors are certainly not even within the top 10. They’re obviously very serious cancers, but if you’re talking about common cancers, brain cancer doesn’t rank in the top 10, and it was the most common cancer on these shows.
The authors of this paper made the point of whether this would be an opportunity for filmmakers. Again, with the storyline, they’re trying to sell a product here, but wouldn’t this be the opportunity to provide some information about the reality of cancer? They could emphasize the fact that smokers get lung cancer. In my opinion, they could discuss cervical cancer and comment that if HPV vaccination had been done, maybe this would not have happened.
They noted that the majority of cancers in these movies were incurable, and they commented that that’s not the reality today. Today, obviously, many of our cancers that weren’t curable have become quite curable for a percentage of patients, in addition to which, obviously, with early detection, we have a very high cure rate. How about trying to get that message out, too, that we’ve actually had increasing success?
They commented that there was very rarely, if ever, a conversation about multidisciplinary care, that somehow there are multiple doctors with multiple specialties involved. They noted that this is potentially a very important message to give out. They commented that in 12 of these movies, the patient refused cancer care. Again, that happens, but it’s clearly a rare event today. Maybe this is not really a very accurate depiction of what’s going on.
They commented on the fact that, obviously, we’re going back through the past 10 years, so there were no patients who received immunotherapy or targeted therapy. Again, the goal here is not to sell oncology care but to be accurate, or more accurate, about the state of treatment to the extent you can.
They noted that, in fact, there was essentially very little, if any, comment on palliative care or hospice care. The final point they made is that there was very little conversation in these movies about what we now recognize as financial distress in many of our patients. That’s an unfortunate reality and perhaps that might come in the future.
Again, the point of this was not to tell Hollywood how to make their movies but to have the oncology community recognize that if their patients or the families of their patients are seeing these movies, they are not getting a very accurate picture of what is happening in the oncology world today and that some education may very well be required.
Maurie Markman is Professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California, and President of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed the following relevant financial relationships: income in an amount equal to or greater than $250 from: GlaxoSmithKline; AstraZeneca.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’d like to talk about a very different topic from what I normally discuss, which is probably relatively rarely addressed in clinical conversations among clinicians. There was a very provocative commentary that appeared in JCO Oncology Practice, titled “Hollywood’s Take on Oncology: Portrayal of Cancer in Movies, 2010-2020.”
All of us, as we grow up — as kids, adolescents, young adults, adults, and older individuals — watch television and movies. The older of us know that the doctor in everybody’s home that we all wanted was Marcus Welby. Of course, there was Dr. Kildare, ER, Grey’s Anatomy, and St. Elsewhere. There was Love Story and Brian’s Song. We all know about these.
This particular review was fascinating. The authors looked at 100 English-language movies that had cancer included in the storyline over the past decade. They asked some relatively simple questions: How did they discuss it? What were the tumor types they discussed? What were the outcomes?
The question is, what is the public seeing? If you watch these movies and you don’t have family experience or personal experience with cancer, what do you think about cancer? Maybe this is what you know about it. Despite what the National Cancer Institute or the American Society of Clinical Oncology tells you, this may be what you know.
What they showed was really quite interesting.
There is another very interesting phenomenon. What do you think was the most common cancer type when they did define the cancer? It was brain tumors, even though we know that brain tumors are certainly not even within the top 10. They’re obviously very serious cancers, but if you’re talking about common cancers, brain cancer doesn’t rank in the top 10, and it was the most common cancer on these shows.
The authors of this paper made the point of whether this would be an opportunity for filmmakers. Again, with the storyline, they’re trying to sell a product here, but wouldn’t this be the opportunity to provide some information about the reality of cancer? They could emphasize the fact that smokers get lung cancer. In my opinion, they could discuss cervical cancer and comment that if HPV vaccination had been done, maybe this would not have happened.
They noted that the majority of cancers in these movies were incurable, and they commented that that’s not the reality today. Today, obviously, many of our cancers that weren’t curable have become quite curable for a percentage of patients, in addition to which, obviously, with early detection, we have a very high cure rate. How about trying to get that message out, too, that we’ve actually had increasing success?
They commented that there was very rarely, if ever, a conversation about multidisciplinary care, that somehow there are multiple doctors with multiple specialties involved. They noted that this is potentially a very important message to give out. They commented that in 12 of these movies, the patient refused cancer care. Again, that happens, but it’s clearly a rare event today. Maybe this is not really a very accurate depiction of what’s going on.
They commented on the fact that, obviously, we’re going back through the past 10 years, so there were no patients who received immunotherapy or targeted therapy. Again, the goal here is not to sell oncology care but to be accurate, or more accurate, about the state of treatment to the extent you can.
They noted that, in fact, there was essentially very little, if any, comment on palliative care or hospice care. The final point they made is that there was very little conversation in these movies about what we now recognize as financial distress in many of our patients. That’s an unfortunate reality and perhaps that might come in the future.
Again, the point of this was not to tell Hollywood how to make their movies but to have the oncology community recognize that if their patients or the families of their patients are seeing these movies, they are not getting a very accurate picture of what is happening in the oncology world today and that some education may very well be required.
Maurie Markman is Professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California, and President of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed the following relevant financial relationships: income in an amount equal to or greater than $250 from: GlaxoSmithKline; AstraZeneca.
A version of this article first appeared on Medscape.com.
Low HPV Vaccination in the United States Is a Public Health ‘Failure’
This transcript has been edited for clarity.
I would like to briefly discuss what I consider to be a very discouraging report and one that I believe we as an oncology society and, quite frankly, as a medical community need to deal with.
The manuscript I’m referring to is from the United States Department of Health and Human Services, titled, “Human Papillomavirus Vaccination Coverage in Children Ages 9-17 Years: United States, 2022.” This particular analysis looked at the coverage of both men and women — young boys and young girls, I would say — receiving at least one dose of the recommended human papillomavirus (HPV) vaccination.
Since 2006, girls have been recommended to receive HPV vaccination; for boys, it’s been since 2011. Certainly, the time period that we’re considering falls within the recommendations based on overwhelmingly positive data. Now, today, still, the recommendation is for more than one vaccine. Obviously, there may be evidence in the future that a single vaccination may be acceptable or appropriate. But today, it’s more than one.
In this particular analysis, they were looking at just a single vaccination. The vaccines have targeted young individuals, both male and female children aged 11-12 years, but it’s certainly acceptable to look starting at age 9.
What is the bottom line? At least one dose of the HPV vaccination was given to 38.6% of children aged 9-17 years in 2022. We are talking about a cancer-preventive vaccine, which on the basis of population-based data in the United States, but also in other countries, is incredibly effective in preventing HPV-associated cancers. This not only includes cervical cancer, but also a large percentage of head and neck cancers.
For this vaccine, which is incredibly safe and incredibly effective, in this country, only 38.6% have received even a single dose. It is noted that the individuals with private insurance had a higher rate, at 41.5%, than individuals with no insurance, at only 20.7%.
In my opinion, this is clearly a failure of our public health establishment at all levels. My own focus has been in gynecologic cancers. I’ve seen young women with advanced cervical cancer, and this is a disease we can prevent. Yet, this is where we are.
For those of you who are interested in cancer prevention or public health, I think this is a very sobering statistic. It’s my plea and my hope that we can, as a society, somehow do something about it.
I thank you for listening. I would encourage you to think about this question if you’re in this area.
Dr. Markman, professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California, and president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix, disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I would like to briefly discuss what I consider to be a very discouraging report and one that I believe we as an oncology society and, quite frankly, as a medical community need to deal with.
The manuscript I’m referring to is from the United States Department of Health and Human Services, titled, “Human Papillomavirus Vaccination Coverage in Children Ages 9-17 Years: United States, 2022.” This particular analysis looked at the coverage of both men and women — young boys and young girls, I would say — receiving at least one dose of the recommended human papillomavirus (HPV) vaccination.
Since 2006, girls have been recommended to receive HPV vaccination; for boys, it’s been since 2011. Certainly, the time period that we’re considering falls within the recommendations based on overwhelmingly positive data. Now, today, still, the recommendation is for more than one vaccine. Obviously, there may be evidence in the future that a single vaccination may be acceptable or appropriate. But today, it’s more than one.
In this particular analysis, they were looking at just a single vaccination. The vaccines have targeted young individuals, both male and female children aged 11-12 years, but it’s certainly acceptable to look starting at age 9.
What is the bottom line? At least one dose of the HPV vaccination was given to 38.6% of children aged 9-17 years in 2022. We are talking about a cancer-preventive vaccine, which on the basis of population-based data in the United States, but also in other countries, is incredibly effective in preventing HPV-associated cancers. This not only includes cervical cancer, but also a large percentage of head and neck cancers.
For this vaccine, which is incredibly safe and incredibly effective, in this country, only 38.6% have received even a single dose. It is noted that the individuals with private insurance had a higher rate, at 41.5%, than individuals with no insurance, at only 20.7%.
In my opinion, this is clearly a failure of our public health establishment at all levels. My own focus has been in gynecologic cancers. I’ve seen young women with advanced cervical cancer, and this is a disease we can prevent. Yet, this is where we are.
For those of you who are interested in cancer prevention or public health, I think this is a very sobering statistic. It’s my plea and my hope that we can, as a society, somehow do something about it.
I thank you for listening. I would encourage you to think about this question if you’re in this area.
Dr. Markman, professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California, and president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix, disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I would like to briefly discuss what I consider to be a very discouraging report and one that I believe we as an oncology society and, quite frankly, as a medical community need to deal with.
The manuscript I’m referring to is from the United States Department of Health and Human Services, titled, “Human Papillomavirus Vaccination Coverage in Children Ages 9-17 Years: United States, 2022.” This particular analysis looked at the coverage of both men and women — young boys and young girls, I would say — receiving at least one dose of the recommended human papillomavirus (HPV) vaccination.
Since 2006, girls have been recommended to receive HPV vaccination; for boys, it’s been since 2011. Certainly, the time period that we’re considering falls within the recommendations based on overwhelmingly positive data. Now, today, still, the recommendation is for more than one vaccine. Obviously, there may be evidence in the future that a single vaccination may be acceptable or appropriate. But today, it’s more than one.
In this particular analysis, they were looking at just a single vaccination. The vaccines have targeted young individuals, both male and female children aged 11-12 years, but it’s certainly acceptable to look starting at age 9.
What is the bottom line? At least one dose of the HPV vaccination was given to 38.6% of children aged 9-17 years in 2022. We are talking about a cancer-preventive vaccine, which on the basis of population-based data in the United States, but also in other countries, is incredibly effective in preventing HPV-associated cancers. This not only includes cervical cancer, but also a large percentage of head and neck cancers.
For this vaccine, which is incredibly safe and incredibly effective, in this country, only 38.6% have received even a single dose. It is noted that the individuals with private insurance had a higher rate, at 41.5%, than individuals with no insurance, at only 20.7%.
In my opinion, this is clearly a failure of our public health establishment at all levels. My own focus has been in gynecologic cancers. I’ve seen young women with advanced cervical cancer, and this is a disease we can prevent. Yet, this is where we are.
For those of you who are interested in cancer prevention or public health, I think this is a very sobering statistic. It’s my plea and my hope that we can, as a society, somehow do something about it.
I thank you for listening. I would encourage you to think about this question if you’re in this area.
Dr. Markman, professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California, and president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix, disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
Poor Quality of Cancer Content on Social Media
This transcript has been edited for clarity.
I’m delighted to talk about a very interesting topic in this commentary. This is an area that we generally don’t discuss, but it’s one that’s obviously very topical, which includes the question of social media.
The paper I’m referring to is entitled, “More Than a Song and Dance”: Exploration of Patient Perspectives and Educational Quality of Gynecologic Cancer Content on TikTok. The paper was published in Gynecologic Oncology in 2023.
They had a total of 466.7 million views. They looked at 430 of the 500 top posts that were eligible, looked at 11 central themes, did an objective analysis of educational content based on published strategy for looking at this.
What they found, unfortunately but not surprisingly, overall was that the educational quality and reliability were quite poor. They also noticed considerable differences in disparities based on racial background and really emphasized in their analysis not only how common it is for individuals to look at this content on TikTok but also concerns about what it is that the public, patients, and their families are actually seeing.
This, of course, specifically relates to gynecologic cancers, but almost certainly relates to other cancers as well. Clearly, this is a topic that needs to be discussed widely. It’s very complex and very controversial, but when you think about the information that might be provided to our patients and their families going to social media, it’s important that we understand what they’re seeing, what they’re hearing, what they’re viewing, and the impact this might have on their care and outcomes.
I encourage you to read this very interesting paper if you have an interest in this topic. Again, it was recently published in Gynecologic Oncology. I thank you for your attention.
Dr. Markman is professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California; president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m delighted to talk about a very interesting topic in this commentary. This is an area that we generally don’t discuss, but it’s one that’s obviously very topical, which includes the question of social media.
The paper I’m referring to is entitled, “More Than a Song and Dance”: Exploration of Patient Perspectives and Educational Quality of Gynecologic Cancer Content on TikTok. The paper was published in Gynecologic Oncology in 2023.
They had a total of 466.7 million views. They looked at 430 of the 500 top posts that were eligible, looked at 11 central themes, did an objective analysis of educational content based on published strategy for looking at this.
What they found, unfortunately but not surprisingly, overall was that the educational quality and reliability were quite poor. They also noticed considerable differences in disparities based on racial background and really emphasized in their analysis not only how common it is for individuals to look at this content on TikTok but also concerns about what it is that the public, patients, and their families are actually seeing.
This, of course, specifically relates to gynecologic cancers, but almost certainly relates to other cancers as well. Clearly, this is a topic that needs to be discussed widely. It’s very complex and very controversial, but when you think about the information that might be provided to our patients and their families going to social media, it’s important that we understand what they’re seeing, what they’re hearing, what they’re viewing, and the impact this might have on their care and outcomes.
I encourage you to read this very interesting paper if you have an interest in this topic. Again, it was recently published in Gynecologic Oncology. I thank you for your attention.
Dr. Markman is professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California; president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I’m delighted to talk about a very interesting topic in this commentary. This is an area that we generally don’t discuss, but it’s one that’s obviously very topical, which includes the question of social media.
The paper I’m referring to is entitled, “More Than a Song and Dance”: Exploration of Patient Perspectives and Educational Quality of Gynecologic Cancer Content on TikTok. The paper was published in Gynecologic Oncology in 2023.
They had a total of 466.7 million views. They looked at 430 of the 500 top posts that were eligible, looked at 11 central themes, did an objective analysis of educational content based on published strategy for looking at this.
What they found, unfortunately but not surprisingly, overall was that the educational quality and reliability were quite poor. They also noticed considerable differences in disparities based on racial background and really emphasized in their analysis not only how common it is for individuals to look at this content on TikTok but also concerns about what it is that the public, patients, and their families are actually seeing.
This, of course, specifically relates to gynecologic cancers, but almost certainly relates to other cancers as well. Clearly, this is a topic that needs to be discussed widely. It’s very complex and very controversial, but when you think about the information that might be provided to our patients and their families going to social media, it’s important that we understand what they’re seeing, what they’re hearing, what they’re viewing, and the impact this might have on their care and outcomes.
I encourage you to read this very interesting paper if you have an interest in this topic. Again, it was recently published in Gynecologic Oncology. I thank you for your attention.
Dr. Markman is professor, Department of Medical Oncology and Therapeutics Research, City of Hope, Duarte, California; president of Medicine & Science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article appeared on Medscape.com.
Long-Term Follow-Up Emphasizes HPV Vaccination Importance
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly discuss a critically important topic that cannot be overly emphasized. It is the relevance, the importance, the benefits, and the outcome of HPV vaccination.
The paper I’m referring to was published in Pediatrics in October 2023. It’s titled, “Ten-Year Follow-up of 9-Valent Human Papillomavirus Vaccine: Immunogenicity, Effectiveness, and Safety.”
Let me emphasize that we’re talking about a 10-year follow-up. In this particular paper and analysis, 301 boys — I emphasize boys — were included and 971 girls at 40 different sites in 13 countries, who received the 9-valent vaccine, which includes HPV 16, 18, and seven other types.
Most importantly, there was not a single case. Not one. Let me repeat this: There was not a single case of high-grade intraepithelial neoplasia, or worse, or condyloma in either males or females. There was not a single case in over 1000 individuals with a follow-up of more than 10 years.
It is difficult to overstate the magnitude of the benefit associated with HPV vaccination for our children and young adults on their risk of developing highly relevant, life-changing, potentially deadly cancers.
For those of you who are interested in this topic — which should include almost all of you, if not all of you — I encourage you to read this very important follow-up paper, again, demonstrating the simple, overwhelming magnitude of the benefit of HPV vaccination. I thank you for your attention.
Dr. Markman is a professor in the department of medical oncology and therapeutics research, City of Hope, Duarte, California, and president of medicine and science, City of Hope Atlanta, Chicago, and Phoenix. He disclosed ties with GlaxoSmithKline; AstraZeneca.
A version of this article appeared on Medscape.com.
Two landmark papers change treatment paradigm for advanced endometrial cancer
I wanted to very briefly highlight a truly extraordinary event in my professional experience as a clinical investigator for almost 40 years in the area of the gynecologic malignancies:
In my career, of course, I’ve treated endometrial cancer, but the paradigm, the algorithms, and the strategies we’ve used have, for the most part, simply followed what we’ve done for ovarian cancer. If platinums worked in ovarian cancer, they probably worked in endometrial cancer, and that was true. If paclitaxel worked and had activity in ovarian cancer, it probably would in endometrial cancer, and that was true. It took some time, but basically, we use the same frontline chemotherapy in advanced or recurrent endometrial cancer as we’ve used in ovarian cancer, and on and on.
That world has changed, very much for the positive. Not only have pharmaceutical companies, academic investigators, and individual investigators in the community setting seen endometrial cancer as a major priority, but we have exciting new developments, and very specifically, of course, the immunotherapeutic agents known as checkpoint inhibitors.
One of these two papers was titled “Pembrolizumab Plus Chemotherapy in Advanced Endometrial Cancer” and the second one was titled “Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer.” Obviously, these were separate studies, but both used checkpoint inhibitor plus the chemotherapeutic agents carboplatin-paclitaxel, compared with chemotherapy alone as frontline therapy for advanced or recurrent ovarian cancer and demonstrated a statistically significant, and in my opinion, highly clinically meaningful improvement, in progression-free survival in favor of the regimen that included the checkpoint inhibitors.
Clearly, we will need longer follow-up to see both the overall magnitude of the effect of these therapies on overall survival and the duration of the effect – the shape of the curve. Do we cure many more people? Do we delay time to progression and death? That remains to be seen.
But the outcomes we have now are remarkably positive for patients and have absolutely changed the standard of care in the management of recurrent or advanced endometrial cancer.
I should note that this includes both patients who have evidence of mismatch repair deficiency and those patients who do not have evidence of deficiency, which is a large patient population. These studies demonstrated the benefit to the entire population of patients.
However, on the basis of the data that we have – not only in endometrial cancer, but in other tumor types – the greatest impact was seen in patients with evidence of mismatch repair deficiency, where the immunotherapy agent has been shown to be most relevant; not exclusively, but most relevant.
These are very important papers. If you have an interest in endometrial cancer or immunotherapy, I would encourage you to read these papers. They change the paradigm of management for advanced endometrial cancer, and they clearly point out directions for future research in the management of this class of gynecologic cancers.
Dr. Markman is a professor in the department of medical oncology and therapeutics research at City of Hope in Duarte, Calif., and the president of Medicine & Science at City of Hope Atlanta, Chicago, and Phoenix. He reported conflicts of interest with AstraZeneca and GlaxoSmithKline.
This transcript has been edited for clarity. A version of this article first appeared on Medscape.com.
I wanted to very briefly highlight a truly extraordinary event in my professional experience as a clinical investigator for almost 40 years in the area of the gynecologic malignancies:
In my career, of course, I’ve treated endometrial cancer, but the paradigm, the algorithms, and the strategies we’ve used have, for the most part, simply followed what we’ve done for ovarian cancer. If platinums worked in ovarian cancer, they probably worked in endometrial cancer, and that was true. If paclitaxel worked and had activity in ovarian cancer, it probably would in endometrial cancer, and that was true. It took some time, but basically, we use the same frontline chemotherapy in advanced or recurrent endometrial cancer as we’ve used in ovarian cancer, and on and on.
That world has changed, very much for the positive. Not only have pharmaceutical companies, academic investigators, and individual investigators in the community setting seen endometrial cancer as a major priority, but we have exciting new developments, and very specifically, of course, the immunotherapeutic agents known as checkpoint inhibitors.
One of these two papers was titled “Pembrolizumab Plus Chemotherapy in Advanced Endometrial Cancer” and the second one was titled “Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer.” Obviously, these were separate studies, but both used checkpoint inhibitor plus the chemotherapeutic agents carboplatin-paclitaxel, compared with chemotherapy alone as frontline therapy for advanced or recurrent ovarian cancer and demonstrated a statistically significant, and in my opinion, highly clinically meaningful improvement, in progression-free survival in favor of the regimen that included the checkpoint inhibitors.
Clearly, we will need longer follow-up to see both the overall magnitude of the effect of these therapies on overall survival and the duration of the effect – the shape of the curve. Do we cure many more people? Do we delay time to progression and death? That remains to be seen.
But the outcomes we have now are remarkably positive for patients and have absolutely changed the standard of care in the management of recurrent or advanced endometrial cancer.
I should note that this includes both patients who have evidence of mismatch repair deficiency and those patients who do not have evidence of deficiency, which is a large patient population. These studies demonstrated the benefit to the entire population of patients.
However, on the basis of the data that we have – not only in endometrial cancer, but in other tumor types – the greatest impact was seen in patients with evidence of mismatch repair deficiency, where the immunotherapy agent has been shown to be most relevant; not exclusively, but most relevant.
These are very important papers. If you have an interest in endometrial cancer or immunotherapy, I would encourage you to read these papers. They change the paradigm of management for advanced endometrial cancer, and they clearly point out directions for future research in the management of this class of gynecologic cancers.
Dr. Markman is a professor in the department of medical oncology and therapeutics research at City of Hope in Duarte, Calif., and the president of Medicine & Science at City of Hope Atlanta, Chicago, and Phoenix. He reported conflicts of interest with AstraZeneca and GlaxoSmithKline.
This transcript has been edited for clarity. A version of this article first appeared on Medscape.com.
I wanted to very briefly highlight a truly extraordinary event in my professional experience as a clinical investigator for almost 40 years in the area of the gynecologic malignancies:
In my career, of course, I’ve treated endometrial cancer, but the paradigm, the algorithms, and the strategies we’ve used have, for the most part, simply followed what we’ve done for ovarian cancer. If platinums worked in ovarian cancer, they probably worked in endometrial cancer, and that was true. If paclitaxel worked and had activity in ovarian cancer, it probably would in endometrial cancer, and that was true. It took some time, but basically, we use the same frontline chemotherapy in advanced or recurrent endometrial cancer as we’ve used in ovarian cancer, and on and on.
That world has changed, very much for the positive. Not only have pharmaceutical companies, academic investigators, and individual investigators in the community setting seen endometrial cancer as a major priority, but we have exciting new developments, and very specifically, of course, the immunotherapeutic agents known as checkpoint inhibitors.
One of these two papers was titled “Pembrolizumab Plus Chemotherapy in Advanced Endometrial Cancer” and the second one was titled “Dostarlimab for Primary Advanced or Recurrent Endometrial Cancer.” Obviously, these were separate studies, but both used checkpoint inhibitor plus the chemotherapeutic agents carboplatin-paclitaxel, compared with chemotherapy alone as frontline therapy for advanced or recurrent ovarian cancer and demonstrated a statistically significant, and in my opinion, highly clinically meaningful improvement, in progression-free survival in favor of the regimen that included the checkpoint inhibitors.
Clearly, we will need longer follow-up to see both the overall magnitude of the effect of these therapies on overall survival and the duration of the effect – the shape of the curve. Do we cure many more people? Do we delay time to progression and death? That remains to be seen.
But the outcomes we have now are remarkably positive for patients and have absolutely changed the standard of care in the management of recurrent or advanced endometrial cancer.
I should note that this includes both patients who have evidence of mismatch repair deficiency and those patients who do not have evidence of deficiency, which is a large patient population. These studies demonstrated the benefit to the entire population of patients.
However, on the basis of the data that we have – not only in endometrial cancer, but in other tumor types – the greatest impact was seen in patients with evidence of mismatch repair deficiency, where the immunotherapy agent has been shown to be most relevant; not exclusively, but most relevant.
These are very important papers. If you have an interest in endometrial cancer or immunotherapy, I would encourage you to read these papers. They change the paradigm of management for advanced endometrial cancer, and they clearly point out directions for future research in the management of this class of gynecologic cancers.
Dr. Markman is a professor in the department of medical oncology and therapeutics research at City of Hope in Duarte, Calif., and the president of Medicine & Science at City of Hope Atlanta, Chicago, and Phoenix. He reported conflicts of interest with AstraZeneca and GlaxoSmithKline.
This transcript has been edited for clarity. A version of this article first appeared on Medscape.com.
Pleural Effusion and an Axillary Mass in a Woman With Hypertension
Editor's Note:
The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .
Background
A 58-year-old woman seeks medical attention after she discovered a new mass in her left axilla during a routine monthly breast self-examination while showering. She has not noted any changes in either of her breasts. The mass in her left axilla is not tender, and she has not felt any other abnormal masses, including in her right axilla. She reports no other symptoms and specifically has no pain anywhere in her body. She also does not have shortness of breath, fever, night sweats, fatigue, rash, or abdominal discomfort or bloating.
Fifteen years earlier, the patient was diagnosed with high-grade, stage 1 cervical cancer and underwent surgery and chemoradiation. She has been closely monitored since that time with physical examinations and abdominal CT, with no evidence of recurrent disease. The patient has not had any other surgical procedure, except for removal of two basal cell carcinomas on her neck 4 years ago. She has had yearly routine mammograms for at least the past 15 years.
The patient has hypertension, which has been well controlled with the same medications for the past 10 years. She also has a 25-year history of type 2 diabetes mellitus, which is currently managed with diet alone. She had a "silent myocardial infarction" sometime within the past 5 years but has had no cardiac symptoms and is not taking any cardiac medications. She smoked approximately one pack of cigarettes a day for less than 2 years when she was "in her teens" but has not had any tobacco products since that time.
Pancreatic cancer was diagnosed in the patient's father at age 49 years, and breast cancer was diagnosed in her aunt on her father's side at age 67 years. Her paternal grandmother is reported to have died in her 60s after diagnosis of a "cancer in her stomach." No further information is available regarding either the actual diagnosis or the medical care provided to this individual.
To the best of the patient's knowledge, her mother's side of the family and her two brothers have no history of cancer. She has no sisters. Her mother is in her 80s and has mild dementia. The patient is not aware of any member of her family having undergone genetic testing.
Physical Examination and Workup
The patient appears well and is in no acute distress. The patient is afebrile, with a blood pressure of 135/85 mm Hg, a respiratory rate of 16 breaths/min, and a pulse of 72 beats/min. Her weight is 148 lb (67 kg), and she has no reported recent weight loss.
Examination of the skin reveals no suspicious lesions. Scars from the previous removal of the basal cell carcinomas are noted, but no evidence suggests recurrence.
Results of the head and neck examination are unremarkable; specifically, no abnormal cervical lymphadenopathy is detected. The cardiac and chest examination results are normal. The lungs are clear to percussion and auscultation. The breast examination reveals no abnormal masses. The right axilla is unremarkable; however, a single 3 × 2 cm, nontender, firm, movable but partially fixed mass is noted in the left axilla.
The abdomen appears normal, with no ascites or enlargement of the liver. The pelvic examination reveals evidence of previous surgery and local radiation but no signs of recurrence of cervical cancer. The lymph nodes appear normal, except for the findings noted above. Results of the neurologic examination are unremarkable.
Complete blood cell count, serum electrolyte levels, renal function tests, and urinalysis are all normal. Liver function tests are normal except for a mildly elevated serum alkaline phosphatase level. The fecal occult blood test result is negative.
Chest radiography reveals a suspicious small left-sided pleural effusion. No other abnormalities are observed, and no prior chest radiographs are available to compare with the current findings.
Chest CT confirms the presence of a possible small pleural effusion, with no other abnormalities noted. The radiologist suggests it will not be possible to obtain fluid safely through an interventional procedure, owing to the limited (if any) amount of fluid present. Furthermore, the radiologist recommends PET/CT to look for other evidence of metastatic cancer in the lungs or elsewhere.
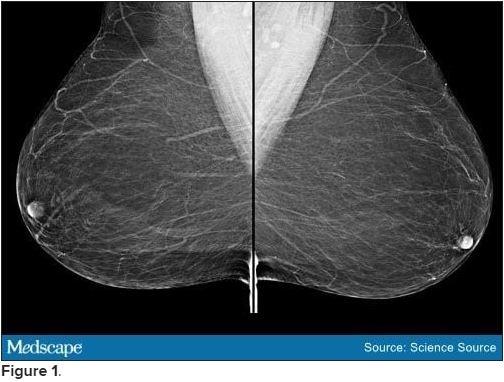
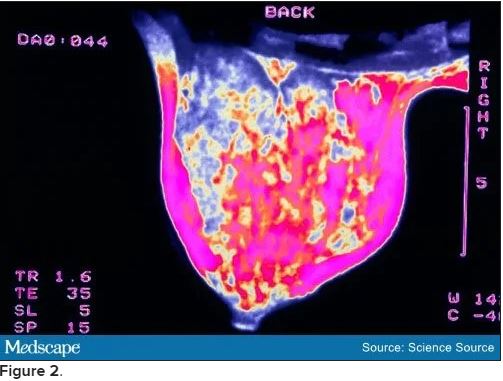
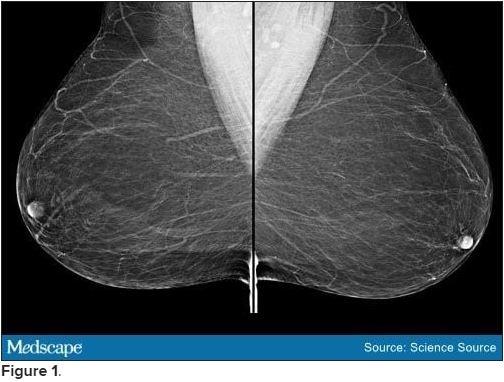
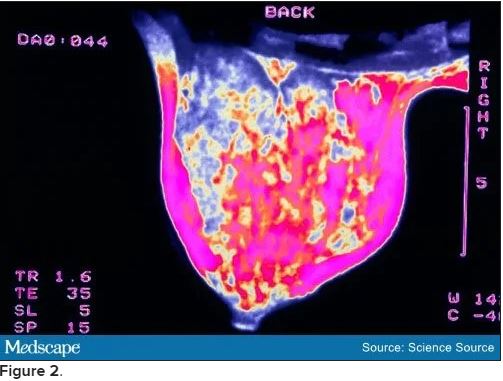
Bilateral mammograms reveal no suspicious abnormalities, and the results are unchanged from a previous examination 11 months earlier. Figure 1 shows a similar bilateral mammogram in another patient. Breast MRI shows no evidence of cancer. Figure 2 shows similar breast MRI findings in another patient.
CT of the abdomen and pelvis reveals no changes compared with a scan obtained 2 years earlier for follow-up of the previous diagnosis of cervical cancer. Specifically, no evidence suggests ascites or any pelvic masses.
An incisional biopsy sample is obtained from the left axillary mass. Light microscopy reveals a moderately well-differentiated adenocarcinoma. Immunostaining shows the cancer to be cytokeratin (CK) 7 positive and CK 20 negative (CK 7+/CK 20-, thyroid transcription factor 1 (TTF-1) negative, thyroglobulin negative, napsin A negative, and mammaglobin positive. The tumor is estrogen receptor positive (2% staining), progesterone receptor negative, and human epidermal growth factor receptor 2 (HER2) negative.
[polldaddy:10837180]
Discussion
The correct answer: Breast.
This case is a classic example of cancer of unknown primary site or origin (CUP). CUP represents approximately 5% of cancers diagnosed in the United States (50,000 to 60,000 cases each year), with various series reporting that the site of origin is not diagnosed in between 2% and 6% of all cancer cases.[1] Worldwide, the incidence of CUP is even higher, resulting from the limited availability of sophisticated (and expensive) diagnostic technology in many regions. The median age at diagnosis of CUP is 60 years, and men and women are equally likely to be affected.
A cancer is considered a CUP if, after routine clinical assessment, physical and laboratory examination, standard imaging studies, and routine pathologic evaluation (biopsy or surgical removal of a metastatic mass lesion), a site of origin cannot be defined. With the availability of more sophisticated imaging technologies (eg, MRI), the overall percentage of cancers that are defined as a CUP has been reduced. However, even at autopsy, the site of origin of such cancer is often unable to be determined if the location was unknown before the patient's death.
Several theories have been proposed for why a metastatic lesion becomes clinically evident despite the site of origin of the cancer remaining obscure. These include (1) very slow growth of the primary cancer compared with that of the metastasis; (2) spontaneous regression of the primary cancer; (3) a prominent vascular component of the cancer, which enhances the rate of spread; and (4) unique molecular events associated with the cancer, which result in rapid progression and the growth of metastatic lesions.
Approximately 60% of CUPs are adenocarcinomas (well or moderately well differentiated); 25%-30% are poorly differentiated (including poorly differentiated adenocarcinomas); 5% are completely undifferentiated, with no defining histologic features; 5% are squamous cell cancers; and approximately 1% are carcinomas, with evidence of neuroendocrine differentiation.[1]
Immunohistochemical staining of biopsy material can be helpful in narrowing the possible anatomical sites of origin. The results are particularly relevant in the selection of therapeutic strategies and in ensuring that a rare, potentially highly curable cancer is not missed (eg, lymphoma, germ cell tumor).[2]
A critical initial test is examination of several CK subtypes that are more likely to be expressed in certain carcinomas than in others. For example, the CK 7+/CK 20- staining seen in this patient is characteristic of breast and lung cancers (among others), whereas CK 7+/CK 20+ staining would be expected in pancreatic, gastric, and urothelial cancers. A CK 7-/CK 20+ finding would be more suggestive of colon or mucinous ovarian cancer. Furthermore, approximately 70% of lung adenocarcinomas are TTF-1 positive and 60%-80% are napsin A positive. The negative findings in this patient's case make the diagnosis of metastatic lung cancer less likely.
Examination for the presence (or absence) of well-established biomarkers for breast cancer can potentially be helpful in suggesting the site of origin or in helping to define subsequent therapy. These markers include estrogen and progesterone receptors and HER2 overexpression. An additional biomarker, mammaglobin, has been reported to be expressed in 48% of breast cancers but is absent in cancers of the lung, gastrointestinal tract, ovary, and head and neck region.[2]
Of note, mammaglobin was found to be expressed in this patient. Although only 2% of the cells were reported to stain for the estrogen receptor, this finding is still considered positive and supports breast cancer as the correct diagnosis.
Recognized relevant prognostic factors in CUP include baseline performance status, the number and location of metastatic lesions, and the response to cytotoxic chemotherapy.
Unfortunately, the overall prognosis associated with a diagnosis of CUP is poor, with median survival in various series reported to be less than 6 months. However, important exceptions to this outcome include women who present with an isolated metastatic axillary mass, as described in this case.
Previous reports of axillary adenopathy as the initial presentation of cancer in women revealed that the majority had evidence of cancer in the breast at the time of subsequent mastectomy.[3,4] As a result, in the absence of other indications found during routine workup (eg, a single pulmonary lesion suggestive of a primary lung cancer, pathologic findings inconsistent with breast cancer), an isolated adenocarcinoma in the breast (with no evidence of metastatic cancer elsewhere) should be treated as either stage II or stage III breast cancer. Note that this recommendation specifically relates to female patients. If a male patient has CUP with an isolated axillary mass, it is generally assumed that the lung is the origin of the malignancy.
In a female patient with negative mammographic findings, breast MRI can be helpful. In one series, 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram were found to have a breast abnormality on MRI.[5] Of note, and of considerable relevance to subsequent disease management, five of the 12 women with negative findings in this series underwent surgery, and in four of the cases no cancer was found. Although the number of participants in this series is limited, the absence of an MRI abnormality in the patient in this case can reasonably be considered in her future treatment plans.
Specifically, it might be suggested in this case that treatment include surgical removal of the axillary mass (if possible) followed by radiation to this area and the breast (rather than performing a mastectomy). Alternatively, treatment might begin with chemotherapy (a neoadjuvant approach) followed by surgery to remove any residual axillary mass and local/regional radiation or local/regional radiation alone. Adjuvant chemotherapy and/or hormonal therapy would then be administered.
The presence of a possible small pleural effusion is a concern because it potentially indicates more widespread metastatic disease, as does the mild elevation of the serum alkaline phosphatase level (eg, suggesting metastatic disease in bone or the liver). In the absence of other evidence of tumor spread, PET would not be unreasonable. A negative scan for evidence of metastatic disease would support a "curative" approach to the management of local disease in the axilla and presumably the breast, whereas a finding of other metastatic sites would lead to the conclusion that treatment should probably be delivered with more palliative intent.
The family history of cancer (father, paternal aunt with breast cancer, paternal grandmother with possible ovarian cancer) is intriguing and would suggest a role for genetic counseling and possibly genetic testing (eg, for BRCA mutation).
The patient in this case underwent PET. The only abnormality observed was in the left axilla. The axillary mass was subsequently resected. This was followed by curative radiation to both the axilla and left breast, adjuvant chemotherapy, and 5 years of hormonal therapy. The patient has showed no evidence of recurrence 2 years after completion of the hormonal treatment.
[polldaddy:10841207]
Discussion
The correct answer: Lung
The lungs are generally assumed to be the site of origin of the cancer in a male patient who has CUP with an isolated axillary mass. In contrast, the majority of women with axillary adenopathy as the initial presentation of cancer were found to have evidence of cancer in the breast at the time of subsequent mastectomy.[3,4]
[polldaddy:10837187]
Discussion
The correct answer: MRI
Breast MRI can be helpful in a female patient with negative mammographic findings. In one series, MRI detected a breast abnormality in 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram.[5]
Editor's Note:
The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .
Background
A 58-year-old woman seeks medical attention after she discovered a new mass in her left axilla during a routine monthly breast self-examination while showering. She has not noted any changes in either of her breasts. The mass in her left axilla is not tender, and she has not felt any other abnormal masses, including in her right axilla. She reports no other symptoms and specifically has no pain anywhere in her body. She also does not have shortness of breath, fever, night sweats, fatigue, rash, or abdominal discomfort or bloating.
Fifteen years earlier, the patient was diagnosed with high-grade, stage 1 cervical cancer and underwent surgery and chemoradiation. She has been closely monitored since that time with physical examinations and abdominal CT, with no evidence of recurrent disease. The patient has not had any other surgical procedure, except for removal of two basal cell carcinomas on her neck 4 years ago. She has had yearly routine mammograms for at least the past 15 years.
The patient has hypertension, which has been well controlled with the same medications for the past 10 years. She also has a 25-year history of type 2 diabetes mellitus, which is currently managed with diet alone. She had a "silent myocardial infarction" sometime within the past 5 years but has had no cardiac symptoms and is not taking any cardiac medications. She smoked approximately one pack of cigarettes a day for less than 2 years when she was "in her teens" but has not had any tobacco products since that time.
Pancreatic cancer was diagnosed in the patient's father at age 49 years, and breast cancer was diagnosed in her aunt on her father's side at age 67 years. Her paternal grandmother is reported to have died in her 60s after diagnosis of a "cancer in her stomach." No further information is available regarding either the actual diagnosis or the medical care provided to this individual.
To the best of the patient's knowledge, her mother's side of the family and her two brothers have no history of cancer. She has no sisters. Her mother is in her 80s and has mild dementia. The patient is not aware of any member of her family having undergone genetic testing.
Physical Examination and Workup
The patient appears well and is in no acute distress. The patient is afebrile, with a blood pressure of 135/85 mm Hg, a respiratory rate of 16 breaths/min, and a pulse of 72 beats/min. Her weight is 148 lb (67 kg), and she has no reported recent weight loss.
Examination of the skin reveals no suspicious lesions. Scars from the previous removal of the basal cell carcinomas are noted, but no evidence suggests recurrence.
Results of the head and neck examination are unremarkable; specifically, no abnormal cervical lymphadenopathy is detected. The cardiac and chest examination results are normal. The lungs are clear to percussion and auscultation. The breast examination reveals no abnormal masses. The right axilla is unremarkable; however, a single 3 × 2 cm, nontender, firm, movable but partially fixed mass is noted in the left axilla.
The abdomen appears normal, with no ascites or enlargement of the liver. The pelvic examination reveals evidence of previous surgery and local radiation but no signs of recurrence of cervical cancer. The lymph nodes appear normal, except for the findings noted above. Results of the neurologic examination are unremarkable.
Complete blood cell count, serum electrolyte levels, renal function tests, and urinalysis are all normal. Liver function tests are normal except for a mildly elevated serum alkaline phosphatase level. The fecal occult blood test result is negative.
Chest radiography reveals a suspicious small left-sided pleural effusion. No other abnormalities are observed, and no prior chest radiographs are available to compare with the current findings.
Chest CT confirms the presence of a possible small pleural effusion, with no other abnormalities noted. The radiologist suggests it will not be possible to obtain fluid safely through an interventional procedure, owing to the limited (if any) amount of fluid present. Furthermore, the radiologist recommends PET/CT to look for other evidence of metastatic cancer in the lungs or elsewhere.
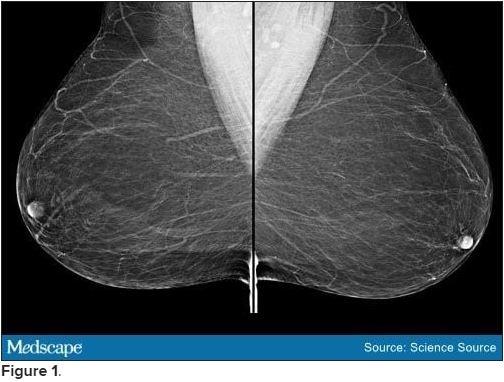
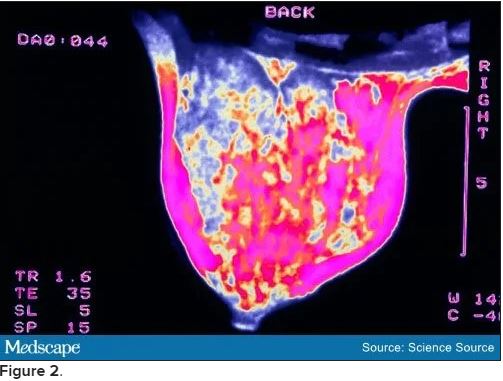
Bilateral mammograms reveal no suspicious abnormalities, and the results are unchanged from a previous examination 11 months earlier. Figure 1 shows a similar bilateral mammogram in another patient. Breast MRI shows no evidence of cancer. Figure 2 shows similar breast MRI findings in another patient.
CT of the abdomen and pelvis reveals no changes compared with a scan obtained 2 years earlier for follow-up of the previous diagnosis of cervical cancer. Specifically, no evidence suggests ascites or any pelvic masses.
An incisional biopsy sample is obtained from the left axillary mass. Light microscopy reveals a moderately well-differentiated adenocarcinoma. Immunostaining shows the cancer to be cytokeratin (CK) 7 positive and CK 20 negative (CK 7+/CK 20-, thyroid transcription factor 1 (TTF-1) negative, thyroglobulin negative, napsin A negative, and mammaglobin positive. The tumor is estrogen receptor positive (2% staining), progesterone receptor negative, and human epidermal growth factor receptor 2 (HER2) negative.
[polldaddy:10837180]
Discussion
The correct answer: Breast.
This case is a classic example of cancer of unknown primary site or origin (CUP). CUP represents approximately 5% of cancers diagnosed in the United States (50,000 to 60,000 cases each year), with various series reporting that the site of origin is not diagnosed in between 2% and 6% of all cancer cases.[1] Worldwide, the incidence of CUP is even higher, resulting from the limited availability of sophisticated (and expensive) diagnostic technology in many regions. The median age at diagnosis of CUP is 60 years, and men and women are equally likely to be affected.
A cancer is considered a CUP if, after routine clinical assessment, physical and laboratory examination, standard imaging studies, and routine pathologic evaluation (biopsy or surgical removal of a metastatic mass lesion), a site of origin cannot be defined. With the availability of more sophisticated imaging technologies (eg, MRI), the overall percentage of cancers that are defined as a CUP has been reduced. However, even at autopsy, the site of origin of such cancer is often unable to be determined if the location was unknown before the patient's death.
Several theories have been proposed for why a metastatic lesion becomes clinically evident despite the site of origin of the cancer remaining obscure. These include (1) very slow growth of the primary cancer compared with that of the metastasis; (2) spontaneous regression of the primary cancer; (3) a prominent vascular component of the cancer, which enhances the rate of spread; and (4) unique molecular events associated with the cancer, which result in rapid progression and the growth of metastatic lesions.
Approximately 60% of CUPs are adenocarcinomas (well or moderately well differentiated); 25%-30% are poorly differentiated (including poorly differentiated adenocarcinomas); 5% are completely undifferentiated, with no defining histologic features; 5% are squamous cell cancers; and approximately 1% are carcinomas, with evidence of neuroendocrine differentiation.[1]
Immunohistochemical staining of biopsy material can be helpful in narrowing the possible anatomical sites of origin. The results are particularly relevant in the selection of therapeutic strategies and in ensuring that a rare, potentially highly curable cancer is not missed (eg, lymphoma, germ cell tumor).[2]
A critical initial test is examination of several CK subtypes that are more likely to be expressed in certain carcinomas than in others. For example, the CK 7+/CK 20- staining seen in this patient is characteristic of breast and lung cancers (among others), whereas CK 7+/CK 20+ staining would be expected in pancreatic, gastric, and urothelial cancers. A CK 7-/CK 20+ finding would be more suggestive of colon or mucinous ovarian cancer. Furthermore, approximately 70% of lung adenocarcinomas are TTF-1 positive and 60%-80% are napsin A positive. The negative findings in this patient's case make the diagnosis of metastatic lung cancer less likely.
Examination for the presence (or absence) of well-established biomarkers for breast cancer can potentially be helpful in suggesting the site of origin or in helping to define subsequent therapy. These markers include estrogen and progesterone receptors and HER2 overexpression. An additional biomarker, mammaglobin, has been reported to be expressed in 48% of breast cancers but is absent in cancers of the lung, gastrointestinal tract, ovary, and head and neck region.[2]
Of note, mammaglobin was found to be expressed in this patient. Although only 2% of the cells were reported to stain for the estrogen receptor, this finding is still considered positive and supports breast cancer as the correct diagnosis.
Recognized relevant prognostic factors in CUP include baseline performance status, the number and location of metastatic lesions, and the response to cytotoxic chemotherapy.
Unfortunately, the overall prognosis associated with a diagnosis of CUP is poor, with median survival in various series reported to be less than 6 months. However, important exceptions to this outcome include women who present with an isolated metastatic axillary mass, as described in this case.
Previous reports of axillary adenopathy as the initial presentation of cancer in women revealed that the majority had evidence of cancer in the breast at the time of subsequent mastectomy.[3,4] As a result, in the absence of other indications found during routine workup (eg, a single pulmonary lesion suggestive of a primary lung cancer, pathologic findings inconsistent with breast cancer), an isolated adenocarcinoma in the breast (with no evidence of metastatic cancer elsewhere) should be treated as either stage II or stage III breast cancer. Note that this recommendation specifically relates to female patients. If a male patient has CUP with an isolated axillary mass, it is generally assumed that the lung is the origin of the malignancy.
In a female patient with negative mammographic findings, breast MRI can be helpful. In one series, 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram were found to have a breast abnormality on MRI.[5] Of note, and of considerable relevance to subsequent disease management, five of the 12 women with negative findings in this series underwent surgery, and in four of the cases no cancer was found. Although the number of participants in this series is limited, the absence of an MRI abnormality in the patient in this case can reasonably be considered in her future treatment plans.
Specifically, it might be suggested in this case that treatment include surgical removal of the axillary mass (if possible) followed by radiation to this area and the breast (rather than performing a mastectomy). Alternatively, treatment might begin with chemotherapy (a neoadjuvant approach) followed by surgery to remove any residual axillary mass and local/regional radiation or local/regional radiation alone. Adjuvant chemotherapy and/or hormonal therapy would then be administered.
The presence of a possible small pleural effusion is a concern because it potentially indicates more widespread metastatic disease, as does the mild elevation of the serum alkaline phosphatase level (eg, suggesting metastatic disease in bone or the liver). In the absence of other evidence of tumor spread, PET would not be unreasonable. A negative scan for evidence of metastatic disease would support a "curative" approach to the management of local disease in the axilla and presumably the breast, whereas a finding of other metastatic sites would lead to the conclusion that treatment should probably be delivered with more palliative intent.
The family history of cancer (father, paternal aunt with breast cancer, paternal grandmother with possible ovarian cancer) is intriguing and would suggest a role for genetic counseling and possibly genetic testing (eg, for BRCA mutation).
The patient in this case underwent PET. The only abnormality observed was in the left axilla. The axillary mass was subsequently resected. This was followed by curative radiation to both the axilla and left breast, adjuvant chemotherapy, and 5 years of hormonal therapy. The patient has showed no evidence of recurrence 2 years after completion of the hormonal treatment.
[polldaddy:10841207]
Discussion
The correct answer: Lung
The lungs are generally assumed to be the site of origin of the cancer in a male patient who has CUP with an isolated axillary mass. In contrast, the majority of women with axillary adenopathy as the initial presentation of cancer were found to have evidence of cancer in the breast at the time of subsequent mastectomy.[3,4]
[polldaddy:10837187]
Discussion
The correct answer: MRI
Breast MRI can be helpful in a female patient with negative mammographic findings. In one series, MRI detected a breast abnormality in 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram.[5]
Editor's Note:
The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us .
Background
A 58-year-old woman seeks medical attention after she discovered a new mass in her left axilla during a routine monthly breast self-examination while showering. She has not noted any changes in either of her breasts. The mass in her left axilla is not tender, and she has not felt any other abnormal masses, including in her right axilla. She reports no other symptoms and specifically has no pain anywhere in her body. She also does not have shortness of breath, fever, night sweats, fatigue, rash, or abdominal discomfort or bloating.
Fifteen years earlier, the patient was diagnosed with high-grade, stage 1 cervical cancer and underwent surgery and chemoradiation. She has been closely monitored since that time with physical examinations and abdominal CT, with no evidence of recurrent disease. The patient has not had any other surgical procedure, except for removal of two basal cell carcinomas on her neck 4 years ago. She has had yearly routine mammograms for at least the past 15 years.
The patient has hypertension, which has been well controlled with the same medications for the past 10 years. She also has a 25-year history of type 2 diabetes mellitus, which is currently managed with diet alone. She had a "silent myocardial infarction" sometime within the past 5 years but has had no cardiac symptoms and is not taking any cardiac medications. She smoked approximately one pack of cigarettes a day for less than 2 years when she was "in her teens" but has not had any tobacco products since that time.
Pancreatic cancer was diagnosed in the patient's father at age 49 years, and breast cancer was diagnosed in her aunt on her father's side at age 67 years. Her paternal grandmother is reported to have died in her 60s after diagnosis of a "cancer in her stomach." No further information is available regarding either the actual diagnosis or the medical care provided to this individual.
To the best of the patient's knowledge, her mother's side of the family and her two brothers have no history of cancer. She has no sisters. Her mother is in her 80s and has mild dementia. The patient is not aware of any member of her family having undergone genetic testing.
Physical Examination and Workup
The patient appears well and is in no acute distress. The patient is afebrile, with a blood pressure of 135/85 mm Hg, a respiratory rate of 16 breaths/min, and a pulse of 72 beats/min. Her weight is 148 lb (67 kg), and she has no reported recent weight loss.
Examination of the skin reveals no suspicious lesions. Scars from the previous removal of the basal cell carcinomas are noted, but no evidence suggests recurrence.
Results of the head and neck examination are unremarkable; specifically, no abnormal cervical lymphadenopathy is detected. The cardiac and chest examination results are normal. The lungs are clear to percussion and auscultation. The breast examination reveals no abnormal masses. The right axilla is unremarkable; however, a single 3 × 2 cm, nontender, firm, movable but partially fixed mass is noted in the left axilla.
The abdomen appears normal, with no ascites or enlargement of the liver. The pelvic examination reveals evidence of previous surgery and local radiation but no signs of recurrence of cervical cancer. The lymph nodes appear normal, except for the findings noted above. Results of the neurologic examination are unremarkable.
Complete blood cell count, serum electrolyte levels, renal function tests, and urinalysis are all normal. Liver function tests are normal except for a mildly elevated serum alkaline phosphatase level. The fecal occult blood test result is negative.
Chest radiography reveals a suspicious small left-sided pleural effusion. No other abnormalities are observed, and no prior chest radiographs are available to compare with the current findings.
Chest CT confirms the presence of a possible small pleural effusion, with no other abnormalities noted. The radiologist suggests it will not be possible to obtain fluid safely through an interventional procedure, owing to the limited (if any) amount of fluid present. Furthermore, the radiologist recommends PET/CT to look for other evidence of metastatic cancer in the lungs or elsewhere.
Bilateral mammograms reveal no suspicious abnormalities, and the results are unchanged from a previous examination 11 months earlier. Figure 1 shows a similar bilateral mammogram in another patient. Breast MRI shows no evidence of cancer. Figure 2 shows similar breast MRI findings in another patient.
CT of the abdomen and pelvis reveals no changes compared with a scan obtained 2 years earlier for follow-up of the previous diagnosis of cervical cancer. Specifically, no evidence suggests ascites or any pelvic masses.
An incisional biopsy sample is obtained from the left axillary mass. Light microscopy reveals a moderately well-differentiated adenocarcinoma. Immunostaining shows the cancer to be cytokeratin (CK) 7 positive and CK 20 negative (CK 7+/CK 20-, thyroid transcription factor 1 (TTF-1) negative, thyroglobulin negative, napsin A negative, and mammaglobin positive. The tumor is estrogen receptor positive (2% staining), progesterone receptor negative, and human epidermal growth factor receptor 2 (HER2) negative.
[polldaddy:10837180]
Discussion
The correct answer: Breast.
This case is a classic example of cancer of unknown primary site or origin (CUP). CUP represents approximately 5% of cancers diagnosed in the United States (50,000 to 60,000 cases each year), with various series reporting that the site of origin is not diagnosed in between 2% and 6% of all cancer cases.[1] Worldwide, the incidence of CUP is even higher, resulting from the limited availability of sophisticated (and expensive) diagnostic technology in many regions. The median age at diagnosis of CUP is 60 years, and men and women are equally likely to be affected.
A cancer is considered a CUP if, after routine clinical assessment, physical and laboratory examination, standard imaging studies, and routine pathologic evaluation (biopsy or surgical removal of a metastatic mass lesion), a site of origin cannot be defined. With the availability of more sophisticated imaging technologies (eg, MRI), the overall percentage of cancers that are defined as a CUP has been reduced. However, even at autopsy, the site of origin of such cancer is often unable to be determined if the location was unknown before the patient's death.
Several theories have been proposed for why a metastatic lesion becomes clinically evident despite the site of origin of the cancer remaining obscure. These include (1) very slow growth of the primary cancer compared with that of the metastasis; (2) spontaneous regression of the primary cancer; (3) a prominent vascular component of the cancer, which enhances the rate of spread; and (4) unique molecular events associated with the cancer, which result in rapid progression and the growth of metastatic lesions.
Approximately 60% of CUPs are adenocarcinomas (well or moderately well differentiated); 25%-30% are poorly differentiated (including poorly differentiated adenocarcinomas); 5% are completely undifferentiated, with no defining histologic features; 5% are squamous cell cancers; and approximately 1% are carcinomas, with evidence of neuroendocrine differentiation.[1]
Immunohistochemical staining of biopsy material can be helpful in narrowing the possible anatomical sites of origin. The results are particularly relevant in the selection of therapeutic strategies and in ensuring that a rare, potentially highly curable cancer is not missed (eg, lymphoma, germ cell tumor).[2]
A critical initial test is examination of several CK subtypes that are more likely to be expressed in certain carcinomas than in others. For example, the CK 7+/CK 20- staining seen in this patient is characteristic of breast and lung cancers (among others), whereas CK 7+/CK 20+ staining would be expected in pancreatic, gastric, and urothelial cancers. A CK 7-/CK 20+ finding would be more suggestive of colon or mucinous ovarian cancer. Furthermore, approximately 70% of lung adenocarcinomas are TTF-1 positive and 60%-80% are napsin A positive. The negative findings in this patient's case make the diagnosis of metastatic lung cancer less likely.
Examination for the presence (or absence) of well-established biomarkers for breast cancer can potentially be helpful in suggesting the site of origin or in helping to define subsequent therapy. These markers include estrogen and progesterone receptors and HER2 overexpression. An additional biomarker, mammaglobin, has been reported to be expressed in 48% of breast cancers but is absent in cancers of the lung, gastrointestinal tract, ovary, and head and neck region.[2]
Of note, mammaglobin was found to be expressed in this patient. Although only 2% of the cells were reported to stain for the estrogen receptor, this finding is still considered positive and supports breast cancer as the correct diagnosis.
Recognized relevant prognostic factors in CUP include baseline performance status, the number and location of metastatic lesions, and the response to cytotoxic chemotherapy.
Unfortunately, the overall prognosis associated with a diagnosis of CUP is poor, with median survival in various series reported to be less than 6 months. However, important exceptions to this outcome include women who present with an isolated metastatic axillary mass, as described in this case.
Previous reports of axillary adenopathy as the initial presentation of cancer in women revealed that the majority had evidence of cancer in the breast at the time of subsequent mastectomy.[3,4] As a result, in the absence of other indications found during routine workup (eg, a single pulmonary lesion suggestive of a primary lung cancer, pathologic findings inconsistent with breast cancer), an isolated adenocarcinoma in the breast (with no evidence of metastatic cancer elsewhere) should be treated as either stage II or stage III breast cancer. Note that this recommendation specifically relates to female patients. If a male patient has CUP with an isolated axillary mass, it is generally assumed that the lung is the origin of the malignancy.
In a female patient with negative mammographic findings, breast MRI can be helpful. In one series, 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram were found to have a breast abnormality on MRI.[5] Of note, and of considerable relevance to subsequent disease management, five of the 12 women with negative findings in this series underwent surgery, and in four of the cases no cancer was found. Although the number of participants in this series is limited, the absence of an MRI abnormality in the patient in this case can reasonably be considered in her future treatment plans.
Specifically, it might be suggested in this case that treatment include surgical removal of the axillary mass (if possible) followed by radiation to this area and the breast (rather than performing a mastectomy). Alternatively, treatment might begin with chemotherapy (a neoadjuvant approach) followed by surgery to remove any residual axillary mass and local/regional radiation or local/regional radiation alone. Adjuvant chemotherapy and/or hormonal therapy would then be administered.
The presence of a possible small pleural effusion is a concern because it potentially indicates more widespread metastatic disease, as does the mild elevation of the serum alkaline phosphatase level (eg, suggesting metastatic disease in bone or the liver). In the absence of other evidence of tumor spread, PET would not be unreasonable. A negative scan for evidence of metastatic disease would support a "curative" approach to the management of local disease in the axilla and presumably the breast, whereas a finding of other metastatic sites would lead to the conclusion that treatment should probably be delivered with more palliative intent.
The family history of cancer (father, paternal aunt with breast cancer, paternal grandmother with possible ovarian cancer) is intriguing and would suggest a role for genetic counseling and possibly genetic testing (eg, for BRCA mutation).
The patient in this case underwent PET. The only abnormality observed was in the left axilla. The axillary mass was subsequently resected. This was followed by curative radiation to both the axilla and left breast, adjuvant chemotherapy, and 5 years of hormonal therapy. The patient has showed no evidence of recurrence 2 years after completion of the hormonal treatment.
[polldaddy:10841207]
Discussion
The correct answer: Lung
The lungs are generally assumed to be the site of origin of the cancer in a male patient who has CUP with an isolated axillary mass. In contrast, the majority of women with axillary adenopathy as the initial presentation of cancer were found to have evidence of cancer in the breast at the time of subsequent mastectomy.[3,4]
[polldaddy:10837187]
Discussion
The correct answer: MRI
Breast MRI can be helpful in a female patient with negative mammographic findings. In one series, MRI detected a breast abnormality in 28 of 40 women (70%) with evidence of cancer in the axilla and a normal mammogram.[5]

