User login
Prices for Common Procedures Not Readily Available
Clinical question: Are patients able to select health-care providers based on price of service?
Background: With health-care costs rising, patients are encouraged to take a more active role in cost containment. Many initiatives call for greater pricing transparency in the health-care system. This study evaluated price availability for a common surgical procedure.
Study design: Telephone inquiries with standardized interview script.
Setting: Twenty top-ranked orthopedic hospitals and 102 non-top-ranked U.S. hospitals.
Synopsis: Hospitals were contacted by phone with a standardized, scripted request for the price of an elective total hip arthroplasty. The script described the patient as a 62-year-old grandmother without insurance who is able to pay out of pocket and wishes to compare hospital prices. On the first or second attempt, 40% of top-ranked and 32% of non-top-ranked hospitals were able to provide their price; after five attempts, authors were unable to obtain full pricing information (both hospital and physician fee) from 40% of top-ranked and 37% of non-top-ranked hospitals. Neither fee was made available by 15% of top-ranked and 16% of non-top-ranked hospitals. Wide variation in pricing was found across hospitals. The authors commented on the difficulties they encountered, such as the transfer of calls between departments and the uncertainty of representatives on how to assist.
Bottom line: For individual patients, applying basic economic principles as a consumer might be tiresome and often impossible, with no major differences between top-ranked and non-top-ranked hospitals.
Citation: Rosenthal JA, Lu X, Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173(6):427-432.
Visit our website for more physician reviews of recent HM-relevant literature.
Clinical question: Are patients able to select health-care providers based on price of service?
Background: With health-care costs rising, patients are encouraged to take a more active role in cost containment. Many initiatives call for greater pricing transparency in the health-care system. This study evaluated price availability for a common surgical procedure.
Study design: Telephone inquiries with standardized interview script.
Setting: Twenty top-ranked orthopedic hospitals and 102 non-top-ranked U.S. hospitals.
Synopsis: Hospitals were contacted by phone with a standardized, scripted request for the price of an elective total hip arthroplasty. The script described the patient as a 62-year-old grandmother without insurance who is able to pay out of pocket and wishes to compare hospital prices. On the first or second attempt, 40% of top-ranked and 32% of non-top-ranked hospitals were able to provide their price; after five attempts, authors were unable to obtain full pricing information (both hospital and physician fee) from 40% of top-ranked and 37% of non-top-ranked hospitals. Neither fee was made available by 15% of top-ranked and 16% of non-top-ranked hospitals. Wide variation in pricing was found across hospitals. The authors commented on the difficulties they encountered, such as the transfer of calls between departments and the uncertainty of representatives on how to assist.
Bottom line: For individual patients, applying basic economic principles as a consumer might be tiresome and often impossible, with no major differences between top-ranked and non-top-ranked hospitals.
Citation: Rosenthal JA, Lu X, Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173(6):427-432.
Visit our website for more physician reviews of recent HM-relevant literature.
Clinical question: Are patients able to select health-care providers based on price of service?
Background: With health-care costs rising, patients are encouraged to take a more active role in cost containment. Many initiatives call for greater pricing transparency in the health-care system. This study evaluated price availability for a common surgical procedure.
Study design: Telephone inquiries with standardized interview script.
Setting: Twenty top-ranked orthopedic hospitals and 102 non-top-ranked U.S. hospitals.
Synopsis: Hospitals were contacted by phone with a standardized, scripted request for the price of an elective total hip arthroplasty. The script described the patient as a 62-year-old grandmother without insurance who is able to pay out of pocket and wishes to compare hospital prices. On the first or second attempt, 40% of top-ranked and 32% of non-top-ranked hospitals were able to provide their price; after five attempts, authors were unable to obtain full pricing information (both hospital and physician fee) from 40% of top-ranked and 37% of non-top-ranked hospitals. Neither fee was made available by 15% of top-ranked and 16% of non-top-ranked hospitals. Wide variation in pricing was found across hospitals. The authors commented on the difficulties they encountered, such as the transfer of calls between departments and the uncertainty of representatives on how to assist.
Bottom line: For individual patients, applying basic economic principles as a consumer might be tiresome and often impossible, with no major differences between top-ranked and non-top-ranked hospitals.
Citation: Rosenthal JA, Lu X, Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173(6):427-432.
Visit our website for more physician reviews of recent HM-relevant literature.
Physician Reviews of Hospital Medicine-Related Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- Prices for common hospital procedures not readily available
- Antibiotics associated with decreased mortality in acute COPD exacerbation
- Endovascular therapy has no benefit to systemic t-PA in acute stroke
- Net harm observed with rivaroxaban for thromboprophylaxis
- Noninvasive ventilation more effective, safer for AECOPD patients
- Synthetic cannabinoid use and acute kidney injury
- Dabigatran vs. warfarin in the extended treatment of VTE
- Spironolactone improves diastolic function
- Real-time EMR-based prediction tool for clinical deterioration
- Hypothermia protocol and cardiac arrest
Prices for Common Hospital Procedures Not Readily Available
Clinical question: Are patients able to select health-care providers based on price of service?
Background: With health-care costs rising, patients are encouraged to take a more active role in cost containment. Many initiatives call for greater pricing transparency in the health-care system. This study evaluated price availability for a common surgical procedure.
Study design: Telephone inquiries with standardized interview script.
Setting: Twenty top-ranked orthopedic hospitals and 102 non-top-ranked U.S. hospitals.
Synopsis: Hospitals were contacted by phone with a standardized, scripted request for their price of an elective total hip arthroplasty. The script described the patient as a 62-year-old grandmother without insurance who is able to pay out of pocket and wishes to compare hospital prices. On the first or second attempt, 40% of top-ranked and 32% of non-top-ranked hospitals were able to provide their price; after five attempts, authors were unable to obtain full pricing information (both hospital and physician fee) from 40% of top-ranked and 37% of non-top-ranked hospitals. Neither fee was made available by 15% of top-ranked and 16% of non-top-ranked hospitals. Wide variation of pricing was found across hospitals. The authors commented on the difficulties they encountered, such as the transfer of calls between departments and the uncertainty of representatives on how to assist.
Bottom line: For individual patients, applying basic economic principles as a consumer might be tiresome and often impossible, with no major differences between top-ranked and non-top-ranked hospitals.
Citation: Rosenthal JA, Lu X, Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173(6):427-432.
Antibiotics Associated with Decreased Mortality in Acute COPD Exacerbation
Clinical question: Do antibiotics when added to systemic steroids provide clinical benefit for patients with acute COPD exacerbation?
Background: Despite widespread use of antibiotics in the treatment of acute COPD, their benefit is not clear.
Study design: Retrospective cohort study.Setting: Four hundred ten U.S. hospitals participating in Perspective, an inpatient administrative database.
Synopsis: More than 50,000 patients treated with systemic steroids for acute COPD exacerbation were included in this study; 85% of them received empiric antibiotics within the first two hospital days. They were compared with those treated with systemic steroids alone. In-hospital mortality was 1.02% for patients on steroids plus antibiotics versus 1.78% on steroids alone. Use of antibiotics was associated with a 40% reduction in the odds of in-hospital mortality (OR, 0.60; 95% CI, 0.50-0.74) and reduced readmissions. In an analysis of matched cohorts, hospital mortality was 1% for patients on antibiotics and 1.8% for patients without antibiotics (OR, 0.53; 95% CI, 0.40-0.71). The risk for readmission for Clostridium difficile colitis was not different between the groups, but other potential adverse effects of antibiotic use, such as development of resistant micro-organisms, were not studied. In a subset analysis, three groups of antibiotics were compared: macrolides, quinolones, and cephalosporins. None was better than another, but those treated with macrolides had a lower readmission rate for C. diff.
Bottom line: Treatment with antibiotics when added to systemic steroids is associated with improved outcomes in acute COPD exacerbations, but there is no clear advantage of one antibiotic class over another.
Citation: Stefan MS, Rothberg MB, Shieh M, Pekow PS, Lindenauer PK. Association between antibiotic treatment and outcomes in patients hospitalized with acute exacerbation of COPD treated with systemic steroids. Chest. 2013;143(1):82-90.
Endovascular Therapy Added to Systemic t-PA Has No Benefit in Acute Stroke
Clinical question: Does adding endovascular therapy to intravenous tissue plasminogen activator (t-PA) reduce disability in acute stroke?
Background: Early systemic t-PA is the only proven reperfusion therapy in acute stroke, but it is unknown if adding localized endovascular therapy is beneficial.
Study design: Randomized, open-label, blinded-outcome trial.
Setting: Fifty-eight centers in North America, Europe, and Australia.
Synopsis: Patients aged 18 to 82 with acute ischemic stroke were eligible if they received t-PA within three hours of enrollment and had moderate to severe neurologic deficit (National Institutes of Health Stroke Scale [NIHSS] >10, or NIHSS 8 or 9 with CT angiographic evidence of specific major artery occlusion). All patients received standard-dose t-PA; those randomized to endovascular treatment underwent angiography, and, if indicated, underwent one of the endovascular treatments chosen by the neurointerventionalist. The primary outcome measure was a modified Rankin score of 2 or lower (indicating functional independence) at 90 days (assessed by a neurologist).
After enrollment of 656 patients, the trial was terminated early for futility. There was no significant difference in the primary outcome, with 40.8% of patients in the endovascular intervention group and 38.7% in the t-PA-only group having a modified Rankin score of 2 or lower. There was also no difference in mortality or other secondary outcomes, even when the analysis was limited to patients presenting with more severe neurologic deficits.
Bottom line: The addition of endovascular therapy to systemic t-PA in acute ischemic stroke does not improve functional outcomes or mortality.
Citation: Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893-903.
Rivaroxaban Compared with Enoxaparin for Thromboprophylaxis
Clinical question: Is extended-duration rivaroxaban more effective than standard-duration enoxaparin in preventing deep venous thrombosis in acutely ill medical patients?
Background: Trials have shown benefits of thromboprophylaxis in acutely ill medical patients at increased risk of venous thrombosis, but the optimal duration and type of anticoagulation is unknown.
Study design: Prospective, randomized, double-blinded, active-comparator controlled trial.
Setting: Five hundred fifty-two centers in 52 countries.
Synopsis: The trial enrolled 8,428 patients hospitalized with an acute medical condition and reduced mobility. Patients were randomized to receive either enoxaparin for 10 (+/-4) days or rivaroxaban for 35 (+/-4) days. The co-primary composite outcomes were the incidence of asymptomatic proximal deep venous thrombosis, symptomatic deep venous thrombosis, pulmonary embolism, or death related to venous thromboembolism over 10 days and over 35 days.
Both groups had a 2.7% incidence of the primary endpoint over 10 days; over 35 days, the extended-duration rivaroxaban group had a reduced incidence of the primary endpoint of 4.4% compared with 5.7% for enoxaparin. However, there was an increase of clinically relevant bleeding in the rivaroxaban group, occurring in 2.8% and 4.1% of patients over 10 and 35 days, respectively, compared with 1.2% and 1.7% for enoxaparin.
Overall, there was net harm with rivaroxaban over both time periods: 6.6% and 9.4% of patients in the rivaroxaban group had a negative outcome at 10 and 35 days, compared with 4.4% and 7.8% with enoxaparin.
Bottom line: There was net harm with extended-duration rivaroxaban versus standard-duration enoxaparin for thromboprophylaxis in hospitalized medical patients.
Citation: Cohen AT, Spiro TE, Büller HR, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368:513-523.
Noninvasive Ventilation More Effective, Safer for Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD)
Clinical question: What are the patterns in use of noninvasive ventilation (NIV) and invasive mechanical ventilation (IMV) in patients with AECOPD, and which method produces better outcomes?
Background: Multiple randomized controlled trials and meta-analyses have suggested a mortality benefit with NIV compared to standard medical care in AECOPD. However, little evidence exists on head-to-head comparisons of NIV and IMV.
Study design: Retrospective cohort study.
Setting: Non-federal, short-term, general, and other specialty hospitals nationwide.
Synopsis: A sample of 67,651 ED visits for AECOPD with acute respiratory failure was analyzed from the National Emergency Department Sample (NEDS) database between 2006 and 2008. The study found that NIV use increased to 16% in 2008 from 14% in 2006. Use varied widely between hospitals and was more utilized in higher-case-volume, nonmetropolitan, and Northeastern hospitals. Compared with IMV, NIV was associated with 46% lower inpatient mortality (risk ratio 0.54, 95% confidence interval [CI] 0.50-0.59), shortened hospital length of stay (-3.2 days, 95% CI -3.4 to -2.9), lower hospital charges (-$35,012, 95% CI -$36,848 to -$33,176), and lower risk of iatrogenic pneumothorax (0.05% vs. 0.5%, P<0.001). Causality could not be established given the observational study design.
Bottom line: NIV is associated with better outcomes than IMV in the management of AECOPD, and might be underutilized.
Citation: Tsai CL, Lee WY, Delclos GL, Hanania NA, Camargo CA Jr. Comparative effectiveness of noninvasive ventilation vs. invasive mechanical ventilation in chronic obstructive pulmonary disease patients with acute respiratory failure. J Hosp Med. 2013;8(4):165-172.
Synthetic Cannabinoid Use May Cause Acute Kidney Injury
Clinical question: Are synthetic cannabinoids associated with acute kidney injury (AKI)?
Background: Synthetic cannabinoids are designer drugs of abuse with a growing popularity in the U.S.
Study design: Retrospective case series.
Setting: Hospitals in Wyoming, Oklahoma, Rhode Island, New York, Kansas, and Oregon.
Synopsis: The Centers for Disease Control and Prevention (CDC) issued an alert when 16 cases of unexplained AKI after exposure to synthetic cannabinoids were reported between March and December 2012. Synthetic cannabinoid use is associated with neurologic, sympathomimetic, and cardiovascular toxicity; however, this is the first case series reporting renal toxicity. The 16 patients included 15 males and one female, aged 15-33 years, with no pre-existing renal disease or nephrotoxic medication consumption. All used synthetic cannabinoids within hours to days before developing nausea, vomiting, abdominal, and flank and/or back pain.
Creatinine peaked one to six days after symptom onset. Five patients required hemodialysis, and all 16 recovered. There was no finding specific for all cases on ultrasound and/or biopsy. Toxicologic analysis of specimens was possible in seven cases and revealed a previously unreported fluorinated synthetic cannabinoid compound XLR-11 in all clinical specimens of patients who used the drug within two days of being tested.
Overall, the analysis did not reveal any single compound or brand that could explain all cases.
Bottom line: Clinicians should be aware of the potential for renal or other toxicities in users of synthetic cannabinoid products and should ask about their use in cases of unexplained AKI.
Citation: Murphy TD, Weidenbach KN, Van Houten C, et al. Centers for Disease Control and Prevention. Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(6):93-98.
Dabigatran versus Warfarin in Extended VTE Treatment
Clinical question: Is dabigatran suitable for extended treatment VTE?
Background: In contrast to warfarin (Coumadin), dabigatran (Pradaxa) is given in a fixed dose and does not require frequent laboratory monitoring. Dabigatran has been shown to be noninferior to warfarin in the initial six-month treatment of VTE.
Study design: Two double-blinded, randomized trials: an active-control study and a placebo-control study.
Setting: Two hundred sixty-five sites in 33 countries for the active-control study, and 147 sites in 21 countries for the placebo-control study.
Synopsis: This study enrolled 4,299 adult patients with objectively confirmed, symptomatic, proximal deep vein thrombosis or pulmonary embolism. In the active-control study comparing warfarin and dabigatran, recurrent objectively confirmed symptomatic or fatal VTE was observed in 1.8% of patients in the dabigatran group compared with 1.3% of patients in the warfarin group (P=0.01 for noninferiority). While major or clinically relevant bleeding was less frequent with dabigatran compared to warfarin (hazard ratio, 0.54), more acute coronary syndromes were observed with dabigatran (0.9% vs. 0.2%, P=0.02). In the placebo-control study, symptomatic or fatal VTE was observed in 0.4% of patients in the dabigatran group compared with 5.6% in the placebo group. Clinically relevant bleeding was more common with dabigatran (5.3% vs. 1.8%; hazard ratio 2.92).
Bottom line: Treatment with dabigatran met the pre-specified noninferiority margin in this study. However, it is worth noting that patients with VTE given extended treatment with dabigatran had significantly higher rates of recurrent symptomatic or fatal VTE than patients treated with warfarin.
Citation: Schulman S, Kearson C, Kakkar AK, et al. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med. 2013;368(8):709-718.
Spironolactone Improves Diastolic Function
Clinical question: What is the efficacy of aldosterone receptor blockers on diastolic function and exercise capacity?
Background: Mineralocorticoid receptor activation by aldosterone contributes to the pathophysiology of heart failure (HF) in patients with and without reduced ejection fraction (EF). Aldosterone receptor blockers (spironolactone) reduce overall and cardiovascular mortality in HF patients with reduced EF; however, its effect on HF patients with preserved EF is unknown.
Study design: Prospective, randomized, double-blinded, placebo-controlled trial.
Setting: Ten ambulatory sites in Germany and Austria.
Synopsis: This study enrolled 422 men and women, aged 50 or older, with New York Heart Association (NYHA) Class II or III HF and preserved EF, and randomized them to receive spironolactone 25 mg daily or placebo for one year.
The endpoints included echocardiographic measures of diastolic function and remodeling; N-terminal pro b-type natriuretic peptide (NT pro-BNP) levels; exercise capacity; quality of life; and HF symptoms.
In the spironolactone group, there was significant improvement in echocardiographic measures of diastolic function and remodeling as well as NT pro-BNP levels. However, there was no difference in exercise capacity, quality of life, or HF symptoms when compared to placebo.
The spironolactone group had significantly lower blood pressure than the control group, which may account for some of the remodeling effects. The study may have been underpowered, and the study population might not have had severe enough disease to detect a difference in clinical measures. It remains unknown if structural changes on echocardiography will translate into clinical benefits.
Bottom line: Compared to placebo, spironolactone did improve diastolic function by echo but did not improve exercise capacity.
Citation: Edelmann F, Wachter R, Schmidt A, et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA. 2013;309(8):781-791.
Real-Time, EMR-Based Prediction Tool Accurately Predicts ICU Transfer Risks
Clinical question: Can clinical deterioration be accurately predicted using real-time data from an electronic medical record (EMR), and can it lead to better outcomes using a floor-based intervention?
Background: Research has shown that EMR-based prediction tools can help identify real-time clinical deterioration in ward patients, but an intervention based on these computer-based alerts has not been shown to be effective.
Study design: Randomized controlled crossover study.
Setting: Eight adult medicine wards in an academic medical center in the Midwest.
Synopsis: There were 20,031 patients assigned to intervention versus control based on their floor location. Computerized alerts were generated using a prediction algorithm. For patients admitted to intervention wards, the alerts were sent to the charge nurse via pager. Patients meeting the alert threshold based on the computerized prediction tool had five times higher risk of ICU transfer, and nine times higher risk of death than patients not meeting the alert threshold. Intervention of charge nurse notification via pager did not result in any significant change in length of stay (LOS), ICU transfer, or mortality. Charge nurses in the intervention group were supposed to alert a physician after receiving the computer alert, but the authors did not measure how often this occurred.
Bottom line: A real-time EMR-based prediction tool accurately predicts higher risk of ICU transfer and death, as well as LOS, but a floor-based intervention to alert the charge nurse in real time did not lead to better outcomes.
Citation: Bailey TC, Chen Y, Mao Y, et al. A trial of a real-time alert for clinical deterioration in patients hospitalized on general medicine wards. J Hosp Med. 2013 Feb 25. doi: 10.1002/jhm.2009 [Epub ahead of print].
Hypothermia Protocol and Cardiac Arrest
Clinical question: Is mild therapeutic hypothermia (MTH) following cardiac arrest beneficial and safe?
Background: Those with sudden cardiac arrest often have poor neurologic outcome. There are some studies that show benefit with hypothermia, but information on safety is limited.
Study design: Meta-analysis.
Setting: Europe, the United Kingdom, the U.S., Canada, Japan, and South Korea.
Synopsis: This study pooled data from 63 studies that looked at MTH protocols in the setting of comatose patients as a result of cardiac arrest. The end points included mortality and any complication potentially attributed to the MTH.
When restricting the analysis to include only randomized controlled trials, MTH was associated with decreased risk of in-hospital mortality (RR=0.75, 95% CI: 0.62-0.92), 30-day mortality (RR=0.61, 95% CI 0.45-0.81), and six-month mortality (RR=0.73, 95% CI 0.61-0.88). MTH was associated with increased risk of arrhythmia (RR=1.25, 95% CI: 1.00-1.55) and hypokalemia (RR=2.35, 95% CI: 1.35-4.11); all other complications were similar between groups.
There were inconsistent results regarding benefit in pediatric patients, as well as comatose patients with non-ventricular fibrillation (non-v-fib) arrest (i.e. asystole or pulseless electrical activity).
Bottom line: Mild therapeutic hypothermia can improve survival of comatose patients after v-fib cardiac arrest and is generally safe.
Citation: Xiao G, Guo Q, Xie X, et al. Safety profile and outcome of mild therapeutic hypothermia in patients following cardiac arrest: systematic review and meta-analysis. Emerg Med J. 2013;30:90-100.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Prices for common hospital procedures not readily available
- Antibiotics associated with decreased mortality in acute COPD exacerbation
- Endovascular therapy has no benefit to systemic t-PA in acute stroke
- Net harm observed with rivaroxaban for thromboprophylaxis
- Noninvasive ventilation more effective, safer for AECOPD patients
- Synthetic cannabinoid use and acute kidney injury
- Dabigatran vs. warfarin in the extended treatment of VTE
- Spironolactone improves diastolic function
- Real-time EMR-based prediction tool for clinical deterioration
- Hypothermia protocol and cardiac arrest
Prices for Common Hospital Procedures Not Readily Available
Clinical question: Are patients able to select health-care providers based on price of service?
Background: With health-care costs rising, patients are encouraged to take a more active role in cost containment. Many initiatives call for greater pricing transparency in the health-care system. This study evaluated price availability for a common surgical procedure.
Study design: Telephone inquiries with standardized interview script.
Setting: Twenty top-ranked orthopedic hospitals and 102 non-top-ranked U.S. hospitals.
Synopsis: Hospitals were contacted by phone with a standardized, scripted request for their price of an elective total hip arthroplasty. The script described the patient as a 62-year-old grandmother without insurance who is able to pay out of pocket and wishes to compare hospital prices. On the first or second attempt, 40% of top-ranked and 32% of non-top-ranked hospitals were able to provide their price; after five attempts, authors were unable to obtain full pricing information (both hospital and physician fee) from 40% of top-ranked and 37% of non-top-ranked hospitals. Neither fee was made available by 15% of top-ranked and 16% of non-top-ranked hospitals. Wide variation of pricing was found across hospitals. The authors commented on the difficulties they encountered, such as the transfer of calls between departments and the uncertainty of representatives on how to assist.
Bottom line: For individual patients, applying basic economic principles as a consumer might be tiresome and often impossible, with no major differences between top-ranked and non-top-ranked hospitals.
Citation: Rosenthal JA, Lu X, Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173(6):427-432.
Antibiotics Associated with Decreased Mortality in Acute COPD Exacerbation
Clinical question: Do antibiotics when added to systemic steroids provide clinical benefit for patients with acute COPD exacerbation?
Background: Despite widespread use of antibiotics in the treatment of acute COPD, their benefit is not clear.
Study design: Retrospective cohort study.Setting: Four hundred ten U.S. hospitals participating in Perspective, an inpatient administrative database.
Synopsis: More than 50,000 patients treated with systemic steroids for acute COPD exacerbation were included in this study; 85% of them received empiric antibiotics within the first two hospital days. They were compared with those treated with systemic steroids alone. In-hospital mortality was 1.02% for patients on steroids plus antibiotics versus 1.78% on steroids alone. Use of antibiotics was associated with a 40% reduction in the odds of in-hospital mortality (OR, 0.60; 95% CI, 0.50-0.74) and reduced readmissions. In an analysis of matched cohorts, hospital mortality was 1% for patients on antibiotics and 1.8% for patients without antibiotics (OR, 0.53; 95% CI, 0.40-0.71). The risk for readmission for Clostridium difficile colitis was not different between the groups, but other potential adverse effects of antibiotic use, such as development of resistant micro-organisms, were not studied. In a subset analysis, three groups of antibiotics were compared: macrolides, quinolones, and cephalosporins. None was better than another, but those treated with macrolides had a lower readmission rate for C. diff.
Bottom line: Treatment with antibiotics when added to systemic steroids is associated with improved outcomes in acute COPD exacerbations, but there is no clear advantage of one antibiotic class over another.
Citation: Stefan MS, Rothberg MB, Shieh M, Pekow PS, Lindenauer PK. Association between antibiotic treatment and outcomes in patients hospitalized with acute exacerbation of COPD treated with systemic steroids. Chest. 2013;143(1):82-90.
Endovascular Therapy Added to Systemic t-PA Has No Benefit in Acute Stroke
Clinical question: Does adding endovascular therapy to intravenous tissue plasminogen activator (t-PA) reduce disability in acute stroke?
Background: Early systemic t-PA is the only proven reperfusion therapy in acute stroke, but it is unknown if adding localized endovascular therapy is beneficial.
Study design: Randomized, open-label, blinded-outcome trial.
Setting: Fifty-eight centers in North America, Europe, and Australia.
Synopsis: Patients aged 18 to 82 with acute ischemic stroke were eligible if they received t-PA within three hours of enrollment and had moderate to severe neurologic deficit (National Institutes of Health Stroke Scale [NIHSS] >10, or NIHSS 8 or 9 with CT angiographic evidence of specific major artery occlusion). All patients received standard-dose t-PA; those randomized to endovascular treatment underwent angiography, and, if indicated, underwent one of the endovascular treatments chosen by the neurointerventionalist. The primary outcome measure was a modified Rankin score of 2 or lower (indicating functional independence) at 90 days (assessed by a neurologist).
After enrollment of 656 patients, the trial was terminated early for futility. There was no significant difference in the primary outcome, with 40.8% of patients in the endovascular intervention group and 38.7% in the t-PA-only group having a modified Rankin score of 2 or lower. There was also no difference in mortality or other secondary outcomes, even when the analysis was limited to patients presenting with more severe neurologic deficits.
Bottom line: The addition of endovascular therapy to systemic t-PA in acute ischemic stroke does not improve functional outcomes or mortality.
Citation: Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893-903.
Rivaroxaban Compared with Enoxaparin for Thromboprophylaxis
Clinical question: Is extended-duration rivaroxaban more effective than standard-duration enoxaparin in preventing deep venous thrombosis in acutely ill medical patients?
Background: Trials have shown benefits of thromboprophylaxis in acutely ill medical patients at increased risk of venous thrombosis, but the optimal duration and type of anticoagulation is unknown.
Study design: Prospective, randomized, double-blinded, active-comparator controlled trial.
Setting: Five hundred fifty-two centers in 52 countries.
Synopsis: The trial enrolled 8,428 patients hospitalized with an acute medical condition and reduced mobility. Patients were randomized to receive either enoxaparin for 10 (+/-4) days or rivaroxaban for 35 (+/-4) days. The co-primary composite outcomes were the incidence of asymptomatic proximal deep venous thrombosis, symptomatic deep venous thrombosis, pulmonary embolism, or death related to venous thromboembolism over 10 days and over 35 days.
Both groups had a 2.7% incidence of the primary endpoint over 10 days; over 35 days, the extended-duration rivaroxaban group had a reduced incidence of the primary endpoint of 4.4% compared with 5.7% for enoxaparin. However, there was an increase of clinically relevant bleeding in the rivaroxaban group, occurring in 2.8% and 4.1% of patients over 10 and 35 days, respectively, compared with 1.2% and 1.7% for enoxaparin.
Overall, there was net harm with rivaroxaban over both time periods: 6.6% and 9.4% of patients in the rivaroxaban group had a negative outcome at 10 and 35 days, compared with 4.4% and 7.8% with enoxaparin.
Bottom line: There was net harm with extended-duration rivaroxaban versus standard-duration enoxaparin for thromboprophylaxis in hospitalized medical patients.
Citation: Cohen AT, Spiro TE, Büller HR, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368:513-523.
Noninvasive Ventilation More Effective, Safer for Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD)
Clinical question: What are the patterns in use of noninvasive ventilation (NIV) and invasive mechanical ventilation (IMV) in patients with AECOPD, and which method produces better outcomes?
Background: Multiple randomized controlled trials and meta-analyses have suggested a mortality benefit with NIV compared to standard medical care in AECOPD. However, little evidence exists on head-to-head comparisons of NIV and IMV.
Study design: Retrospective cohort study.
Setting: Non-federal, short-term, general, and other specialty hospitals nationwide.
Synopsis: A sample of 67,651 ED visits for AECOPD with acute respiratory failure was analyzed from the National Emergency Department Sample (NEDS) database between 2006 and 2008. The study found that NIV use increased to 16% in 2008 from 14% in 2006. Use varied widely between hospitals and was more utilized in higher-case-volume, nonmetropolitan, and Northeastern hospitals. Compared with IMV, NIV was associated with 46% lower inpatient mortality (risk ratio 0.54, 95% confidence interval [CI] 0.50-0.59), shortened hospital length of stay (-3.2 days, 95% CI -3.4 to -2.9), lower hospital charges (-$35,012, 95% CI -$36,848 to -$33,176), and lower risk of iatrogenic pneumothorax (0.05% vs. 0.5%, P<0.001). Causality could not be established given the observational study design.
Bottom line: NIV is associated with better outcomes than IMV in the management of AECOPD, and might be underutilized.
Citation: Tsai CL, Lee WY, Delclos GL, Hanania NA, Camargo CA Jr. Comparative effectiveness of noninvasive ventilation vs. invasive mechanical ventilation in chronic obstructive pulmonary disease patients with acute respiratory failure. J Hosp Med. 2013;8(4):165-172.
Synthetic Cannabinoid Use May Cause Acute Kidney Injury
Clinical question: Are synthetic cannabinoids associated with acute kidney injury (AKI)?
Background: Synthetic cannabinoids are designer drugs of abuse with a growing popularity in the U.S.
Study design: Retrospective case series.
Setting: Hospitals in Wyoming, Oklahoma, Rhode Island, New York, Kansas, and Oregon.
Synopsis: The Centers for Disease Control and Prevention (CDC) issued an alert when 16 cases of unexplained AKI after exposure to synthetic cannabinoids were reported between March and December 2012. Synthetic cannabinoid use is associated with neurologic, sympathomimetic, and cardiovascular toxicity; however, this is the first case series reporting renal toxicity. The 16 patients included 15 males and one female, aged 15-33 years, with no pre-existing renal disease or nephrotoxic medication consumption. All used synthetic cannabinoids within hours to days before developing nausea, vomiting, abdominal, and flank and/or back pain.
Creatinine peaked one to six days after symptom onset. Five patients required hemodialysis, and all 16 recovered. There was no finding specific for all cases on ultrasound and/or biopsy. Toxicologic analysis of specimens was possible in seven cases and revealed a previously unreported fluorinated synthetic cannabinoid compound XLR-11 in all clinical specimens of patients who used the drug within two days of being tested.
Overall, the analysis did not reveal any single compound or brand that could explain all cases.
Bottom line: Clinicians should be aware of the potential for renal or other toxicities in users of synthetic cannabinoid products and should ask about their use in cases of unexplained AKI.
Citation: Murphy TD, Weidenbach KN, Van Houten C, et al. Centers for Disease Control and Prevention. Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(6):93-98.
Dabigatran versus Warfarin in Extended VTE Treatment
Clinical question: Is dabigatran suitable for extended treatment VTE?
Background: In contrast to warfarin (Coumadin), dabigatran (Pradaxa) is given in a fixed dose and does not require frequent laboratory monitoring. Dabigatran has been shown to be noninferior to warfarin in the initial six-month treatment of VTE.
Study design: Two double-blinded, randomized trials: an active-control study and a placebo-control study.
Setting: Two hundred sixty-five sites in 33 countries for the active-control study, and 147 sites in 21 countries for the placebo-control study.
Synopsis: This study enrolled 4,299 adult patients with objectively confirmed, symptomatic, proximal deep vein thrombosis or pulmonary embolism. In the active-control study comparing warfarin and dabigatran, recurrent objectively confirmed symptomatic or fatal VTE was observed in 1.8% of patients in the dabigatran group compared with 1.3% of patients in the warfarin group (P=0.01 for noninferiority). While major or clinically relevant bleeding was less frequent with dabigatran compared to warfarin (hazard ratio, 0.54), more acute coronary syndromes were observed with dabigatran (0.9% vs. 0.2%, P=0.02). In the placebo-control study, symptomatic or fatal VTE was observed in 0.4% of patients in the dabigatran group compared with 5.6% in the placebo group. Clinically relevant bleeding was more common with dabigatran (5.3% vs. 1.8%; hazard ratio 2.92).
Bottom line: Treatment with dabigatran met the pre-specified noninferiority margin in this study. However, it is worth noting that patients with VTE given extended treatment with dabigatran had significantly higher rates of recurrent symptomatic or fatal VTE than patients treated with warfarin.
Citation: Schulman S, Kearson C, Kakkar AK, et al. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med. 2013;368(8):709-718.
Spironolactone Improves Diastolic Function
Clinical question: What is the efficacy of aldosterone receptor blockers on diastolic function and exercise capacity?
Background: Mineralocorticoid receptor activation by aldosterone contributes to the pathophysiology of heart failure (HF) in patients with and without reduced ejection fraction (EF). Aldosterone receptor blockers (spironolactone) reduce overall and cardiovascular mortality in HF patients with reduced EF; however, its effect on HF patients with preserved EF is unknown.
Study design: Prospective, randomized, double-blinded, placebo-controlled trial.
Setting: Ten ambulatory sites in Germany and Austria.
Synopsis: This study enrolled 422 men and women, aged 50 or older, with New York Heart Association (NYHA) Class II or III HF and preserved EF, and randomized them to receive spironolactone 25 mg daily or placebo for one year.
The endpoints included echocardiographic measures of diastolic function and remodeling; N-terminal pro b-type natriuretic peptide (NT pro-BNP) levels; exercise capacity; quality of life; and HF symptoms.
In the spironolactone group, there was significant improvement in echocardiographic measures of diastolic function and remodeling as well as NT pro-BNP levels. However, there was no difference in exercise capacity, quality of life, or HF symptoms when compared to placebo.
The spironolactone group had significantly lower blood pressure than the control group, which may account for some of the remodeling effects. The study may have been underpowered, and the study population might not have had severe enough disease to detect a difference in clinical measures. It remains unknown if structural changes on echocardiography will translate into clinical benefits.
Bottom line: Compared to placebo, spironolactone did improve diastolic function by echo but did not improve exercise capacity.
Citation: Edelmann F, Wachter R, Schmidt A, et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA. 2013;309(8):781-791.
Real-Time, EMR-Based Prediction Tool Accurately Predicts ICU Transfer Risks
Clinical question: Can clinical deterioration be accurately predicted using real-time data from an electronic medical record (EMR), and can it lead to better outcomes using a floor-based intervention?
Background: Research has shown that EMR-based prediction tools can help identify real-time clinical deterioration in ward patients, but an intervention based on these computer-based alerts has not been shown to be effective.
Study design: Randomized controlled crossover study.
Setting: Eight adult medicine wards in an academic medical center in the Midwest.
Synopsis: There were 20,031 patients assigned to intervention versus control based on their floor location. Computerized alerts were generated using a prediction algorithm. For patients admitted to intervention wards, the alerts were sent to the charge nurse via pager. Patients meeting the alert threshold based on the computerized prediction tool had five times higher risk of ICU transfer, and nine times higher risk of death than patients not meeting the alert threshold. Intervention of charge nurse notification via pager did not result in any significant change in length of stay (LOS), ICU transfer, or mortality. Charge nurses in the intervention group were supposed to alert a physician after receiving the computer alert, but the authors did not measure how often this occurred.
Bottom line: A real-time EMR-based prediction tool accurately predicts higher risk of ICU transfer and death, as well as LOS, but a floor-based intervention to alert the charge nurse in real time did not lead to better outcomes.
Citation: Bailey TC, Chen Y, Mao Y, et al. A trial of a real-time alert for clinical deterioration in patients hospitalized on general medicine wards. J Hosp Med. 2013 Feb 25. doi: 10.1002/jhm.2009 [Epub ahead of print].
Hypothermia Protocol and Cardiac Arrest
Clinical question: Is mild therapeutic hypothermia (MTH) following cardiac arrest beneficial and safe?
Background: Those with sudden cardiac arrest often have poor neurologic outcome. There are some studies that show benefit with hypothermia, but information on safety is limited.
Study design: Meta-analysis.
Setting: Europe, the United Kingdom, the U.S., Canada, Japan, and South Korea.
Synopsis: This study pooled data from 63 studies that looked at MTH protocols in the setting of comatose patients as a result of cardiac arrest. The end points included mortality and any complication potentially attributed to the MTH.
When restricting the analysis to include only randomized controlled trials, MTH was associated with decreased risk of in-hospital mortality (RR=0.75, 95% CI: 0.62-0.92), 30-day mortality (RR=0.61, 95% CI 0.45-0.81), and six-month mortality (RR=0.73, 95% CI 0.61-0.88). MTH was associated with increased risk of arrhythmia (RR=1.25, 95% CI: 1.00-1.55) and hypokalemia (RR=2.35, 95% CI: 1.35-4.11); all other complications were similar between groups.
There were inconsistent results regarding benefit in pediatric patients, as well as comatose patients with non-ventricular fibrillation (non-v-fib) arrest (i.e. asystole or pulseless electrical activity).
Bottom line: Mild therapeutic hypothermia can improve survival of comatose patients after v-fib cardiac arrest and is generally safe.
Citation: Xiao G, Guo Q, Xie X, et al. Safety profile and outcome of mild therapeutic hypothermia in patients following cardiac arrest: systematic review and meta-analysis. Emerg Med J. 2013;30:90-100.
In This Edition
Literature At A Glance
A guide to this month’s studies
- Prices for common hospital procedures not readily available
- Antibiotics associated with decreased mortality in acute COPD exacerbation
- Endovascular therapy has no benefit to systemic t-PA in acute stroke
- Net harm observed with rivaroxaban for thromboprophylaxis
- Noninvasive ventilation more effective, safer for AECOPD patients
- Synthetic cannabinoid use and acute kidney injury
- Dabigatran vs. warfarin in the extended treatment of VTE
- Spironolactone improves diastolic function
- Real-time EMR-based prediction tool for clinical deterioration
- Hypothermia protocol and cardiac arrest
Prices for Common Hospital Procedures Not Readily Available
Clinical question: Are patients able to select health-care providers based on price of service?
Background: With health-care costs rising, patients are encouraged to take a more active role in cost containment. Many initiatives call for greater pricing transparency in the health-care system. This study evaluated price availability for a common surgical procedure.
Study design: Telephone inquiries with standardized interview script.
Setting: Twenty top-ranked orthopedic hospitals and 102 non-top-ranked U.S. hospitals.
Synopsis: Hospitals were contacted by phone with a standardized, scripted request for their price of an elective total hip arthroplasty. The script described the patient as a 62-year-old grandmother without insurance who is able to pay out of pocket and wishes to compare hospital prices. On the first or second attempt, 40% of top-ranked and 32% of non-top-ranked hospitals were able to provide their price; after five attempts, authors were unable to obtain full pricing information (both hospital and physician fee) from 40% of top-ranked and 37% of non-top-ranked hospitals. Neither fee was made available by 15% of top-ranked and 16% of non-top-ranked hospitals. Wide variation of pricing was found across hospitals. The authors commented on the difficulties they encountered, such as the transfer of calls between departments and the uncertainty of representatives on how to assist.
Bottom line: For individual patients, applying basic economic principles as a consumer might be tiresome and often impossible, with no major differences between top-ranked and non-top-ranked hospitals.
Citation: Rosenthal JA, Lu X, Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173(6):427-432.
Antibiotics Associated with Decreased Mortality in Acute COPD Exacerbation
Clinical question: Do antibiotics when added to systemic steroids provide clinical benefit for patients with acute COPD exacerbation?
Background: Despite widespread use of antibiotics in the treatment of acute COPD, their benefit is not clear.
Study design: Retrospective cohort study.Setting: Four hundred ten U.S. hospitals participating in Perspective, an inpatient administrative database.
Synopsis: More than 50,000 patients treated with systemic steroids for acute COPD exacerbation were included in this study; 85% of them received empiric antibiotics within the first two hospital days. They were compared with those treated with systemic steroids alone. In-hospital mortality was 1.02% for patients on steroids plus antibiotics versus 1.78% on steroids alone. Use of antibiotics was associated with a 40% reduction in the odds of in-hospital mortality (OR, 0.60; 95% CI, 0.50-0.74) and reduced readmissions. In an analysis of matched cohorts, hospital mortality was 1% for patients on antibiotics and 1.8% for patients without antibiotics (OR, 0.53; 95% CI, 0.40-0.71). The risk for readmission for Clostridium difficile colitis was not different between the groups, but other potential adverse effects of antibiotic use, such as development of resistant micro-organisms, were not studied. In a subset analysis, three groups of antibiotics were compared: macrolides, quinolones, and cephalosporins. None was better than another, but those treated with macrolides had a lower readmission rate for C. diff.
Bottom line: Treatment with antibiotics when added to systemic steroids is associated with improved outcomes in acute COPD exacerbations, but there is no clear advantage of one antibiotic class over another.
Citation: Stefan MS, Rothberg MB, Shieh M, Pekow PS, Lindenauer PK. Association between antibiotic treatment and outcomes in patients hospitalized with acute exacerbation of COPD treated with systemic steroids. Chest. 2013;143(1):82-90.
Endovascular Therapy Added to Systemic t-PA Has No Benefit in Acute Stroke
Clinical question: Does adding endovascular therapy to intravenous tissue plasminogen activator (t-PA) reduce disability in acute stroke?
Background: Early systemic t-PA is the only proven reperfusion therapy in acute stroke, but it is unknown if adding localized endovascular therapy is beneficial.
Study design: Randomized, open-label, blinded-outcome trial.
Setting: Fifty-eight centers in North America, Europe, and Australia.
Synopsis: Patients aged 18 to 82 with acute ischemic stroke were eligible if they received t-PA within three hours of enrollment and had moderate to severe neurologic deficit (National Institutes of Health Stroke Scale [NIHSS] >10, or NIHSS 8 or 9 with CT angiographic evidence of specific major artery occlusion). All patients received standard-dose t-PA; those randomized to endovascular treatment underwent angiography, and, if indicated, underwent one of the endovascular treatments chosen by the neurointerventionalist. The primary outcome measure was a modified Rankin score of 2 or lower (indicating functional independence) at 90 days (assessed by a neurologist).
After enrollment of 656 patients, the trial was terminated early for futility. There was no significant difference in the primary outcome, with 40.8% of patients in the endovascular intervention group and 38.7% in the t-PA-only group having a modified Rankin score of 2 or lower. There was also no difference in mortality or other secondary outcomes, even when the analysis was limited to patients presenting with more severe neurologic deficits.
Bottom line: The addition of endovascular therapy to systemic t-PA in acute ischemic stroke does not improve functional outcomes or mortality.
Citation: Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368:893-903.
Rivaroxaban Compared with Enoxaparin for Thromboprophylaxis
Clinical question: Is extended-duration rivaroxaban more effective than standard-duration enoxaparin in preventing deep venous thrombosis in acutely ill medical patients?
Background: Trials have shown benefits of thromboprophylaxis in acutely ill medical patients at increased risk of venous thrombosis, but the optimal duration and type of anticoagulation is unknown.
Study design: Prospective, randomized, double-blinded, active-comparator controlled trial.
Setting: Five hundred fifty-two centers in 52 countries.
Synopsis: The trial enrolled 8,428 patients hospitalized with an acute medical condition and reduced mobility. Patients were randomized to receive either enoxaparin for 10 (+/-4) days or rivaroxaban for 35 (+/-4) days. The co-primary composite outcomes were the incidence of asymptomatic proximal deep venous thrombosis, symptomatic deep venous thrombosis, pulmonary embolism, or death related to venous thromboembolism over 10 days and over 35 days.
Both groups had a 2.7% incidence of the primary endpoint over 10 days; over 35 days, the extended-duration rivaroxaban group had a reduced incidence of the primary endpoint of 4.4% compared with 5.7% for enoxaparin. However, there was an increase of clinically relevant bleeding in the rivaroxaban group, occurring in 2.8% and 4.1% of patients over 10 and 35 days, respectively, compared with 1.2% and 1.7% for enoxaparin.
Overall, there was net harm with rivaroxaban over both time periods: 6.6% and 9.4% of patients in the rivaroxaban group had a negative outcome at 10 and 35 days, compared with 4.4% and 7.8% with enoxaparin.
Bottom line: There was net harm with extended-duration rivaroxaban versus standard-duration enoxaparin for thromboprophylaxis in hospitalized medical patients.
Citation: Cohen AT, Spiro TE, Büller HR, et al. Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368:513-523.
Noninvasive Ventilation More Effective, Safer for Acute Exacerbation of Chronic Obstructive Pulmonary Disease (AECOPD)
Clinical question: What are the patterns in use of noninvasive ventilation (NIV) and invasive mechanical ventilation (IMV) in patients with AECOPD, and which method produces better outcomes?
Background: Multiple randomized controlled trials and meta-analyses have suggested a mortality benefit with NIV compared to standard medical care in AECOPD. However, little evidence exists on head-to-head comparisons of NIV and IMV.
Study design: Retrospective cohort study.
Setting: Non-federal, short-term, general, and other specialty hospitals nationwide.
Synopsis: A sample of 67,651 ED visits for AECOPD with acute respiratory failure was analyzed from the National Emergency Department Sample (NEDS) database between 2006 and 2008. The study found that NIV use increased to 16% in 2008 from 14% in 2006. Use varied widely between hospitals and was more utilized in higher-case-volume, nonmetropolitan, and Northeastern hospitals. Compared with IMV, NIV was associated with 46% lower inpatient mortality (risk ratio 0.54, 95% confidence interval [CI] 0.50-0.59), shortened hospital length of stay (-3.2 days, 95% CI -3.4 to -2.9), lower hospital charges (-$35,012, 95% CI -$36,848 to -$33,176), and lower risk of iatrogenic pneumothorax (0.05% vs. 0.5%, P<0.001). Causality could not be established given the observational study design.
Bottom line: NIV is associated with better outcomes than IMV in the management of AECOPD, and might be underutilized.
Citation: Tsai CL, Lee WY, Delclos GL, Hanania NA, Camargo CA Jr. Comparative effectiveness of noninvasive ventilation vs. invasive mechanical ventilation in chronic obstructive pulmonary disease patients with acute respiratory failure. J Hosp Med. 2013;8(4):165-172.
Synthetic Cannabinoid Use May Cause Acute Kidney Injury
Clinical question: Are synthetic cannabinoids associated with acute kidney injury (AKI)?
Background: Synthetic cannabinoids are designer drugs of abuse with a growing popularity in the U.S.
Study design: Retrospective case series.
Setting: Hospitals in Wyoming, Oklahoma, Rhode Island, New York, Kansas, and Oregon.
Synopsis: The Centers for Disease Control and Prevention (CDC) issued an alert when 16 cases of unexplained AKI after exposure to synthetic cannabinoids were reported between March and December 2012. Synthetic cannabinoid use is associated with neurologic, sympathomimetic, and cardiovascular toxicity; however, this is the first case series reporting renal toxicity. The 16 patients included 15 males and one female, aged 15-33 years, with no pre-existing renal disease or nephrotoxic medication consumption. All used synthetic cannabinoids within hours to days before developing nausea, vomiting, abdominal, and flank and/or back pain.
Creatinine peaked one to six days after symptom onset. Five patients required hemodialysis, and all 16 recovered. There was no finding specific for all cases on ultrasound and/or biopsy. Toxicologic analysis of specimens was possible in seven cases and revealed a previously unreported fluorinated synthetic cannabinoid compound XLR-11 in all clinical specimens of patients who used the drug within two days of being tested.
Overall, the analysis did not reveal any single compound or brand that could explain all cases.
Bottom line: Clinicians should be aware of the potential for renal or other toxicities in users of synthetic cannabinoid products and should ask about their use in cases of unexplained AKI.
Citation: Murphy TD, Weidenbach KN, Van Houten C, et al. Centers for Disease Control and Prevention. Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(6):93-98.
Dabigatran versus Warfarin in Extended VTE Treatment
Clinical question: Is dabigatran suitable for extended treatment VTE?
Background: In contrast to warfarin (Coumadin), dabigatran (Pradaxa) is given in a fixed dose and does not require frequent laboratory monitoring. Dabigatran has been shown to be noninferior to warfarin in the initial six-month treatment of VTE.
Study design: Two double-blinded, randomized trials: an active-control study and a placebo-control study.
Setting: Two hundred sixty-five sites in 33 countries for the active-control study, and 147 sites in 21 countries for the placebo-control study.
Synopsis: This study enrolled 4,299 adult patients with objectively confirmed, symptomatic, proximal deep vein thrombosis or pulmonary embolism. In the active-control study comparing warfarin and dabigatran, recurrent objectively confirmed symptomatic or fatal VTE was observed in 1.8% of patients in the dabigatran group compared with 1.3% of patients in the warfarin group (P=0.01 for noninferiority). While major or clinically relevant bleeding was less frequent with dabigatran compared to warfarin (hazard ratio, 0.54), more acute coronary syndromes were observed with dabigatran (0.9% vs. 0.2%, P=0.02). In the placebo-control study, symptomatic or fatal VTE was observed in 0.4% of patients in the dabigatran group compared with 5.6% in the placebo group. Clinically relevant bleeding was more common with dabigatran (5.3% vs. 1.8%; hazard ratio 2.92).
Bottom line: Treatment with dabigatran met the pre-specified noninferiority margin in this study. However, it is worth noting that patients with VTE given extended treatment with dabigatran had significantly higher rates of recurrent symptomatic or fatal VTE than patients treated with warfarin.
Citation: Schulman S, Kearson C, Kakkar AK, et al. Extended use of dabigatran, warfarin, or placebo in venous thromboembolism. N Engl J Med. 2013;368(8):709-718.
Spironolactone Improves Diastolic Function
Clinical question: What is the efficacy of aldosterone receptor blockers on diastolic function and exercise capacity?
Background: Mineralocorticoid receptor activation by aldosterone contributes to the pathophysiology of heart failure (HF) in patients with and without reduced ejection fraction (EF). Aldosterone receptor blockers (spironolactone) reduce overall and cardiovascular mortality in HF patients with reduced EF; however, its effect on HF patients with preserved EF is unknown.
Study design: Prospective, randomized, double-blinded, placebo-controlled trial.
Setting: Ten ambulatory sites in Germany and Austria.
Synopsis: This study enrolled 422 men and women, aged 50 or older, with New York Heart Association (NYHA) Class II or III HF and preserved EF, and randomized them to receive spironolactone 25 mg daily or placebo for one year.
The endpoints included echocardiographic measures of diastolic function and remodeling; N-terminal pro b-type natriuretic peptide (NT pro-BNP) levels; exercise capacity; quality of life; and HF symptoms.
In the spironolactone group, there was significant improvement in echocardiographic measures of diastolic function and remodeling as well as NT pro-BNP levels. However, there was no difference in exercise capacity, quality of life, or HF symptoms when compared to placebo.
The spironolactone group had significantly lower blood pressure than the control group, which may account for some of the remodeling effects. The study may have been underpowered, and the study population might not have had severe enough disease to detect a difference in clinical measures. It remains unknown if structural changes on echocardiography will translate into clinical benefits.
Bottom line: Compared to placebo, spironolactone did improve diastolic function by echo but did not improve exercise capacity.
Citation: Edelmann F, Wachter R, Schmidt A, et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: the Aldo-DHF randomized controlled trial. JAMA. 2013;309(8):781-791.
Real-Time, EMR-Based Prediction Tool Accurately Predicts ICU Transfer Risks
Clinical question: Can clinical deterioration be accurately predicted using real-time data from an electronic medical record (EMR), and can it lead to better outcomes using a floor-based intervention?
Background: Research has shown that EMR-based prediction tools can help identify real-time clinical deterioration in ward patients, but an intervention based on these computer-based alerts has not been shown to be effective.
Study design: Randomized controlled crossover study.
Setting: Eight adult medicine wards in an academic medical center in the Midwest.
Synopsis: There were 20,031 patients assigned to intervention versus control based on their floor location. Computerized alerts were generated using a prediction algorithm. For patients admitted to intervention wards, the alerts were sent to the charge nurse via pager. Patients meeting the alert threshold based on the computerized prediction tool had five times higher risk of ICU transfer, and nine times higher risk of death than patients not meeting the alert threshold. Intervention of charge nurse notification via pager did not result in any significant change in length of stay (LOS), ICU transfer, or mortality. Charge nurses in the intervention group were supposed to alert a physician after receiving the computer alert, but the authors did not measure how often this occurred.
Bottom line: A real-time EMR-based prediction tool accurately predicts higher risk of ICU transfer and death, as well as LOS, but a floor-based intervention to alert the charge nurse in real time did not lead to better outcomes.
Citation: Bailey TC, Chen Y, Mao Y, et al. A trial of a real-time alert for clinical deterioration in patients hospitalized on general medicine wards. J Hosp Med. 2013 Feb 25. doi: 10.1002/jhm.2009 [Epub ahead of print].
Hypothermia Protocol and Cardiac Arrest
Clinical question: Is mild therapeutic hypothermia (MTH) following cardiac arrest beneficial and safe?
Background: Those with sudden cardiac arrest often have poor neurologic outcome. There are some studies that show benefit with hypothermia, but information on safety is limited.
Study design: Meta-analysis.
Setting: Europe, the United Kingdom, the U.S., Canada, Japan, and South Korea.
Synopsis: This study pooled data from 63 studies that looked at MTH protocols in the setting of comatose patients as a result of cardiac arrest. The end points included mortality and any complication potentially attributed to the MTH.
When restricting the analysis to include only randomized controlled trials, MTH was associated with decreased risk of in-hospital mortality (RR=0.75, 95% CI: 0.62-0.92), 30-day mortality (RR=0.61, 95% CI 0.45-0.81), and six-month mortality (RR=0.73, 95% CI 0.61-0.88). MTH was associated with increased risk of arrhythmia (RR=1.25, 95% CI: 1.00-1.55) and hypokalemia (RR=2.35, 95% CI: 1.35-4.11); all other complications were similar between groups.
There were inconsistent results regarding benefit in pediatric patients, as well as comatose patients with non-ventricular fibrillation (non-v-fib) arrest (i.e. asystole or pulseless electrical activity).
Bottom line: Mild therapeutic hypothermia can improve survival of comatose patients after v-fib cardiac arrest and is generally safe.
Citation: Xiao G, Guo Q, Xie X, et al. Safety profile and outcome of mild therapeutic hypothermia in patients following cardiac arrest: systematic review and meta-analysis. Emerg Med J. 2013;30:90-100.
How is Acute Pericarditis Diagnosed and Treated?
Case
A 32-year-old female with no significant past medical history is evaluated for sharp, left-sided chest pain for five days. Her pain is intermittent, worse with deep inspiration and in the supine position. She denies any shortness of breath. Her temperature is 100.8ºF, but otherwise her vital signs are normal. The physical exam and chest radiograph are unremarkable, but an electrocardiogram shows diffuse ST-segment elevations. The initial troponin is mildly elevated at 0.35 ng/ml.
Could this patient have acute pericarditis? If so, how should she be managed?
Background
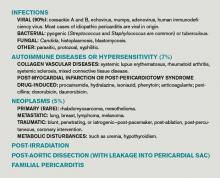
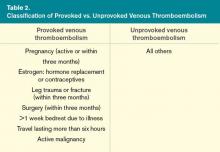
Pericarditis is the most common pericardial disease encountered by hospitalists. As many as 5% of chest pain cases unattributable to myocardial infarction (MI) are diagnosed with pericarditis.1 In immunocompetent individuals, as many as 90% of acute pericarditis cases are viral or idiopathic in etiology.1,2 Human immunodeficiency virus (HIV) and tuberculosis are common culprits in developing countries and immunocompromised hosts.3 Other specific etiologies of acute pericarditis include autoimmune diseases, neoplasms, chest irradiation, trauma, and metabolic disturbances (e.g. uremia). An etiologic classification of acute pericarditis is shown in Table 2 (p. 16).
Pericarditis primarily is a clinical diagnosis. Most patients present with chest pain.4 A pericardial friction rub may or may not be heard (sensitivity 16% to 85%), but when present is nearly 100% specific for pericarditis.2,5 Diffuse ST-segment elevation on electrocardiogram (EKG) is present in 60% to 90% of cases, but it can be difficult to differentiate from ST-segment elevations in acute MI.4,6
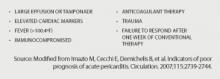
Uncomplicated acute pericarditis often is treated successfully as an outpatient.4 However, patients with high-risk features (see Table 1, right) should be hospitalized for identification and treatment of specific underlying etiology and for monitoring of complications, such as tamponade.7
Our patient has features consistent with pericarditis. In the following sections, we will review the diagnosis and treatment of acute pericarditis.
Review of the Data
How is acute pericarditis diagnosed?
Acute pericarditis is a clinical diagnosis supported by EKG and echocardiogram. At least two of the following four criteria must be present for the diagnosis: pleuritic chest pain, pericardial rub, diffuse ST-segment elevation on EKG, and pericardial effusion.8
History. Patients may report fever (46% in one small study of 69 patients) or a recent history of respiratory or gastrointestinal infection (40%).5 Most patients will report pleuritic chest pain. Typically, the pain is improved when sitting up and leaning forward, and gets worse when lying supine.4 Pain might radiate to the trapezius muscle ridge due to the common phrenic nerve innervation of pericardium and trapezius.9 However, pain might be minimal or absent in patients with uremic, neoplastic, tuberculous, or post-irradiation pericarditis.
Physical exam. A pericardial friction rub is nearly 100% specific for a pericarditis diagnosis, but sensitivity can vary (16% to 85%) depending on the frequency of auscultation and underlying etiology.2,5 It is thought to be caused by friction between the parietal and visceral layers of inflamed pericardium. A pericardial rub classically is described as a superficial, high-pitched, scratchy, or squeaking sound best heard with the diaphragm of the stethoscope at the lower left sternal border with the patient leaning forward.
Laboratory data. A complete blood count, metabolic panel, and cardiac enzymes should be checked in all patients with suspected acute pericarditis. Troponin values are elevated in up to one-third of patients, indicating cardiac muscle injury or myopericarditis, but have not been shown to adversely impact hospital length of stay, readmission, or complication rates.5,10 Markers of inflammation (e.g. erythrocyte sedimentation rate or C-reactive protein) are frequently elevated but do not point to a specific underlying etiology. Routine viral cultures and antibody titers are not useful.11
Most cases of pericarditis are presumed idiopathic (viral); however, finding a specific etiology should be considered in patients who do not respond after one week of therapy. Anti-nuclear antibody, complement levels, and rheumatoid factor can serve as screening tests for autoimmune disease. Purified protein derivative or quantiferon testing and HIV testing might be indicated in patients with appropriate risk factors. In cases of suspected tuberculous or neoplastic pericarditis, pericardial fluid analysis and biopsy could be warranted.
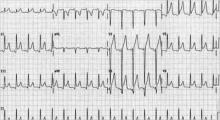
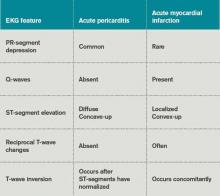
Electrocardiography. The EKG is the most useful test in diagnosing acute pericarditis. EKG changes in acute pericarditis can progress over four stages:
- Stage 1: diffuse ST elevations with or without PR depressions, initially;
- Stage 2: normalization of ST and PR segments, typically after several days;
- Stage 3: diffuse T-wave inversions; and
- Stage 4: normalization of T-waves, typically after weeks or months.
While all four stages are unlikely to be present in a given case, 80% of patients with pericarditis will demonstrate diffuse ST-segment elevations and PR-segment depression (see Figure 2, above).12
Table 3 lists EKG features helpful in differentiating acute pericarditis from acute myocardial infarction.
Chest radiography. Because a pericardial effusion often accompanies pericarditis, a chest radiograph (CXR) should be performed in all suspected cases. The CXR might show enlargement of the cardiac silhouette if more than 250 ml of pericardial fluid is present.3 A CXR also is helpful to diagnose concomitant pulmonary infection, pleural effusion, or mediastinal mass—all findings that could point to an underlying specific etiology of pericarditis and/or pericardial effusion.
Echocardiography. An echocardiogram should be performed in all patients with suspected pericarditis to detect effusion, associated myocardial, or paracardial disease.13 The echocardiogram frequently is normal but could show an effusion in 60%, and tamponade (see Figure 1, p. 15) in 5%, of cases.4
Computed tomography (CT) and cardiac magnetic resonance imaging (CMR).CT or CMR are the imaging modalities of choice when an echocardiogram is inconclusive or in cases of pericarditis complicated by a hemorrhagic or localized effusion, pericardial thickening, or pericardial mass.14 They also help in precise imaging of neighboring structures, such as lungs or mediastinum.
Pericardial fluid analysis and pericardial biopsy. In cases of refractory pericarditis with effusion, pericardial fluid analysis might provide clues to the underlying etiology. Routine chemistry, cell count, gram and acid fast staining, culture, and cytology should be sent. In addition, acid-fast bacillus staining and culture, adenosine deaminase, and interferon-gamma testing should be ordered when tuberculous pericarditis is suspected. A pericardial biopsy may show granulomas or neoplastic cells. Overall, pericardial fluid analysis and biopsy reveal a diagnosis in roughly 20% of cases.11
How is acute pericarditis treated?
Most cases of uncomplicated acute pericarditis are viral and respond well to NSAID plus colchicine therapy.2,4 Failure to respond to NSAIDs plus colchicine—evidenced by persistent fever, pericardial chest pain, new pericardial effusion, or worsening of general illness—within a week of treatment should prompt a search for an underlying systemic illness. If found, treatment should be aimed at the causative illness.
Bacterial pericarditis usually requires surgical drainage in addition to treatment with appropriate antibiotics.11 Tuberculous pericarditis is treated with multidrug therapy; when underlying HIV is present, patients should receive highly active anti-retroviral therapy as well. Steroids and immunosuppressants should be considered in addition to NSAIDs and colchicine in autoimmune pericarditis.10 Neoplastic pericarditis may resolve with chemotherapy but it has a high recurrence rate.13 Uremic pericarditis requires intensified dialysis.
Treatment options for uncomplicated idiopathic or viral pericarditis include:
NSAIDs. It is important to adequately dose NSAIDs when treating acute pericarditis. Initial treatment options include ibuprofen (1,600 to 3,200 mg daily), indomethacin (75 to 150 mg daily) or aspirin (2 to 4 gm daily) for one week.11,15 Aspirin is preferred in patients with ischemic heart disease. For patients with symptoms that persist longer than a week, NSAIDS may be continued, but investigation for an underlying etiology is indicated. Concomitant proton-pump-inhibitor therapy should be considered in patients at high risk for peptic ulcer disease to minimize gastric side effects.
Colchicine. Colchicine has a favorable risk-benefit profile as an adjunct treatment for acute and recurrent pericarditis. Patients experience better symptom relief when treated with both colchicine and an NSAID, compared with NSAIDs alone (88% versus 63%). Recurrence rates are lower with combined therapy (11% versus 32%).16 Colchicine treatment (0.6 mg twice daily after a loading dose of up to 2 mg) is recommended for several months to greater than one year.13,16,17
Glucocorticoids. Routine glucocorticoid use should be avoided in the treatment of acute pericarditis, as it has been associated with an increased risk for recurrence (OR 4.3).16,18 Glucocorticoid use should be considered in cases of pericarditis refractory to NSAIDs and colchicine, cases in which NSAIDs and or colchicine are contraindicated, and in autoimmune or connective-tissue-disease-related pericarditis. Prednisone should be dosed up to 1 mg/kg/day for at least one month, depending on symptom resolution, then tapered after either NSAIDs or colchicine have been started.13 Smaller prednisone doses of up to 0.5 mg/kg/day could be as effective, with the added benefit of reduced side effects and recurrences.19
Invasive treatment. Pericardiocentesis and/or pericardiectomy should be considered when pericarditis is complicated by a large effusion or tamponade, constrictive physiology, or recurrent effusion.11 Pericardiocentesis is the least invasive option and helps provide immediate relief in cases of tamponade or large symptomatic effusions. It is the preferred modality for obtaining pericardial fluid for diagnostic analysis. However, effusions can recur and in those cases pericardial window is preferred, as it provides continued outflow of pericardial fluid. Pericardiectomy is recommended in cases of symptomatic constrictive pericarditis unresponsive to medical therapy.15
Back to the Case
The patient’s presentation—prodrome followed by fever and pleuritic chest pain—is characteristic of acute idiopathic pericarditis. No pericardial rub was heard, but EKG findings were typical. Troponin I elevation suggested underlying myopericarditis. An echocardiogram was unremarkable. Given the likely viral or idiopathic etiology, no further diagnostic tests were ordered to explore the possibility of an underlying systemic illness.
The patient was started on ibuprofen 600 mg every eight hours. She had significant relief of her symptoms within two days. A routine fever workup was negative. She was discharged the following day.
The patient was readmitted three months later with recurrent pleuritic chest pain, which did not improve with resumption of NSAID therapy. Initial troponin I was 0.22 ng/ml, electrocardiogram was unchanged, and an echocardiogram showed small effusion. She was started on ibuprofen 800 mg every eight hours, as well as colchicine 0.6 mg twice daily. Her symptoms resolved the next day and she was discharged with prescriptions for ibuprofen and colchicine. She was instructed to follow up with a primary-care doctor in one week.
At the clinic visit, ibuprofen was tapered but colchicine was continued for another six months. She remained asymptomatic at her six-month clinic follow-up.
Bottom Line
Acute pericarditis is a clinical diagnosis supported by EKG findings. Most cases are idiopathic or viral, and can be treated successfully with NSAIDs and colchicine. For cases that do not respond to initial therapy, or cases that present with high-risk features, a specific etiology should be sought.
Dr. Southern is chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y. Dr. Galhorta is an instructor and Drs. Martin, Korcak, and Stehlihova are assistant professors in the department of medicine at Albert Einstein.
References
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351:2195-2202.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378-382.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717-727.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042-1046.
- Bonnefoy E, Godon P, Kirkorian G, et al. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832-836.
- Salisbury AC, Olalla-Gomez C, Rihal CS, et al. Frequency and predictors of urgent coronary angiography in patients with acute pericarditis. Mayo Clin Proc. 2009;84(1):11-15.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739-2744.
- Imazio M, Spodick DH, Brucato A, et al. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64(10):1384-1392.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150-1153.
- Imazio M, Demichelis B, Cecchi E. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144-2148.
- Sagristà Sauleda J, Permanyer Miralda G, Soler Soler J. Diagnosis and management of pericardial syndromes. Rev Esp Cardiol. 2005;58(7):830-841.
- Bruce MA, Spodick DH. Atypical electrocardiogram in acute pericarditis: characteristics and prevalence. J Electrocardiol. 1980;13:61-66.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004; 25(7):587-610.
- Verhaert D, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333-343.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-928.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (COPE) trial. Circulation. 2005;112(13):2012-2016.
- Adler Y, Finkelstein Y, Guindo J, et al. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183-185.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the colchicine for recurrent pericarditis (CORE) trial. Arch Intern Med. 2005;165:1987-1991.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation. 2008;118:667-771.
Case
A 32-year-old female with no significant past medical history is evaluated for sharp, left-sided chest pain for five days. Her pain is intermittent, worse with deep inspiration and in the supine position. She denies any shortness of breath. Her temperature is 100.8ºF, but otherwise her vital signs are normal. The physical exam and chest radiograph are unremarkable, but an electrocardiogram shows diffuse ST-segment elevations. The initial troponin is mildly elevated at 0.35 ng/ml.
Could this patient have acute pericarditis? If so, how should she be managed?
Background
Pericarditis is the most common pericardial disease encountered by hospitalists. As many as 5% of chest pain cases unattributable to myocardial infarction (MI) are diagnosed with pericarditis.1 In immunocompetent individuals, as many as 90% of acute pericarditis cases are viral or idiopathic in etiology.1,2 Human immunodeficiency virus (HIV) and tuberculosis are common culprits in developing countries and immunocompromised hosts.3 Other specific etiologies of acute pericarditis include autoimmune diseases, neoplasms, chest irradiation, trauma, and metabolic disturbances (e.g. uremia). An etiologic classification of acute pericarditis is shown in Table 2 (p. 16).
Pericarditis primarily is a clinical diagnosis. Most patients present with chest pain.4 A pericardial friction rub may or may not be heard (sensitivity 16% to 85%), but when present is nearly 100% specific for pericarditis.2,5 Diffuse ST-segment elevation on electrocardiogram (EKG) is present in 60% to 90% of cases, but it can be difficult to differentiate from ST-segment elevations in acute MI.4,6
Uncomplicated acute pericarditis often is treated successfully as an outpatient.4 However, patients with high-risk features (see Table 1, right) should be hospitalized for identification and treatment of specific underlying etiology and for monitoring of complications, such as tamponade.7
Our patient has features consistent with pericarditis. In the following sections, we will review the diagnosis and treatment of acute pericarditis.
Review of the Data
How is acute pericarditis diagnosed?
Acute pericarditis is a clinical diagnosis supported by EKG and echocardiogram. At least two of the following four criteria must be present for the diagnosis: pleuritic chest pain, pericardial rub, diffuse ST-segment elevation on EKG, and pericardial effusion.8
History. Patients may report fever (46% in one small study of 69 patients) or a recent history of respiratory or gastrointestinal infection (40%).5 Most patients will report pleuritic chest pain. Typically, the pain is improved when sitting up and leaning forward, and gets worse when lying supine.4 Pain might radiate to the trapezius muscle ridge due to the common phrenic nerve innervation of pericardium and trapezius.9 However, pain might be minimal or absent in patients with uremic, neoplastic, tuberculous, or post-irradiation pericarditis.
Physical exam. A pericardial friction rub is nearly 100% specific for a pericarditis diagnosis, but sensitivity can vary (16% to 85%) depending on the frequency of auscultation and underlying etiology.2,5 It is thought to be caused by friction between the parietal and visceral layers of inflamed pericardium. A pericardial rub classically is described as a superficial, high-pitched, scratchy, or squeaking sound best heard with the diaphragm of the stethoscope at the lower left sternal border with the patient leaning forward.
Laboratory data. A complete blood count, metabolic panel, and cardiac enzymes should be checked in all patients with suspected acute pericarditis. Troponin values are elevated in up to one-third of patients, indicating cardiac muscle injury or myopericarditis, but have not been shown to adversely impact hospital length of stay, readmission, or complication rates.5,10 Markers of inflammation (e.g. erythrocyte sedimentation rate or C-reactive protein) are frequently elevated but do not point to a specific underlying etiology. Routine viral cultures and antibody titers are not useful.11
Most cases of pericarditis are presumed idiopathic (viral); however, finding a specific etiology should be considered in patients who do not respond after one week of therapy. Anti-nuclear antibody, complement levels, and rheumatoid factor can serve as screening tests for autoimmune disease. Purified protein derivative or quantiferon testing and HIV testing might be indicated in patients with appropriate risk factors. In cases of suspected tuberculous or neoplastic pericarditis, pericardial fluid analysis and biopsy could be warranted.
Electrocardiography. The EKG is the most useful test in diagnosing acute pericarditis. EKG changes in acute pericarditis can progress over four stages:
- Stage 1: diffuse ST elevations with or without PR depressions, initially;
- Stage 2: normalization of ST and PR segments, typically after several days;
- Stage 3: diffuse T-wave inversions; and
- Stage 4: normalization of T-waves, typically after weeks or months.
While all four stages are unlikely to be present in a given case, 80% of patients with pericarditis will demonstrate diffuse ST-segment elevations and PR-segment depression (see Figure 2, above).12
Table 3 lists EKG features helpful in differentiating acute pericarditis from acute myocardial infarction.
Chest radiography. Because a pericardial effusion often accompanies pericarditis, a chest radiograph (CXR) should be performed in all suspected cases. The CXR might show enlargement of the cardiac silhouette if more than 250 ml of pericardial fluid is present.3 A CXR also is helpful to diagnose concomitant pulmonary infection, pleural effusion, or mediastinal mass—all findings that could point to an underlying specific etiology of pericarditis and/or pericardial effusion.
Echocardiography. An echocardiogram should be performed in all patients with suspected pericarditis to detect effusion, associated myocardial, or paracardial disease.13 The echocardiogram frequently is normal but could show an effusion in 60%, and tamponade (see Figure 1, p. 15) in 5%, of cases.4
Computed tomography (CT) and cardiac magnetic resonance imaging (CMR).CT or CMR are the imaging modalities of choice when an echocardiogram is inconclusive or in cases of pericarditis complicated by a hemorrhagic or localized effusion, pericardial thickening, or pericardial mass.14 They also help in precise imaging of neighboring structures, such as lungs or mediastinum.
Pericardial fluid analysis and pericardial biopsy. In cases of refractory pericarditis with effusion, pericardial fluid analysis might provide clues to the underlying etiology. Routine chemistry, cell count, gram and acid fast staining, culture, and cytology should be sent. In addition, acid-fast bacillus staining and culture, adenosine deaminase, and interferon-gamma testing should be ordered when tuberculous pericarditis is suspected. A pericardial biopsy may show granulomas or neoplastic cells. Overall, pericardial fluid analysis and biopsy reveal a diagnosis in roughly 20% of cases.11
How is acute pericarditis treated?
Most cases of uncomplicated acute pericarditis are viral and respond well to NSAID plus colchicine therapy.2,4 Failure to respond to NSAIDs plus colchicine—evidenced by persistent fever, pericardial chest pain, new pericardial effusion, or worsening of general illness—within a week of treatment should prompt a search for an underlying systemic illness. If found, treatment should be aimed at the causative illness.
Bacterial pericarditis usually requires surgical drainage in addition to treatment with appropriate antibiotics.11 Tuberculous pericarditis is treated with multidrug therapy; when underlying HIV is present, patients should receive highly active anti-retroviral therapy as well. Steroids and immunosuppressants should be considered in addition to NSAIDs and colchicine in autoimmune pericarditis.10 Neoplastic pericarditis may resolve with chemotherapy but it has a high recurrence rate.13 Uremic pericarditis requires intensified dialysis.
Treatment options for uncomplicated idiopathic or viral pericarditis include:
NSAIDs. It is important to adequately dose NSAIDs when treating acute pericarditis. Initial treatment options include ibuprofen (1,600 to 3,200 mg daily), indomethacin (75 to 150 mg daily) or aspirin (2 to 4 gm daily) for one week.11,15 Aspirin is preferred in patients with ischemic heart disease. For patients with symptoms that persist longer than a week, NSAIDS may be continued, but investigation for an underlying etiology is indicated. Concomitant proton-pump-inhibitor therapy should be considered in patients at high risk for peptic ulcer disease to minimize gastric side effects.
Colchicine. Colchicine has a favorable risk-benefit profile as an adjunct treatment for acute and recurrent pericarditis. Patients experience better symptom relief when treated with both colchicine and an NSAID, compared with NSAIDs alone (88% versus 63%). Recurrence rates are lower with combined therapy (11% versus 32%).16 Colchicine treatment (0.6 mg twice daily after a loading dose of up to 2 mg) is recommended for several months to greater than one year.13,16,17
Glucocorticoids. Routine glucocorticoid use should be avoided in the treatment of acute pericarditis, as it has been associated with an increased risk for recurrence (OR 4.3).16,18 Glucocorticoid use should be considered in cases of pericarditis refractory to NSAIDs and colchicine, cases in which NSAIDs and or colchicine are contraindicated, and in autoimmune or connective-tissue-disease-related pericarditis. Prednisone should be dosed up to 1 mg/kg/day for at least one month, depending on symptom resolution, then tapered after either NSAIDs or colchicine have been started.13 Smaller prednisone doses of up to 0.5 mg/kg/day could be as effective, with the added benefit of reduced side effects and recurrences.19
Invasive treatment. Pericardiocentesis and/or pericardiectomy should be considered when pericarditis is complicated by a large effusion or tamponade, constrictive physiology, or recurrent effusion.11 Pericardiocentesis is the least invasive option and helps provide immediate relief in cases of tamponade or large symptomatic effusions. It is the preferred modality for obtaining pericardial fluid for diagnostic analysis. However, effusions can recur and in those cases pericardial window is preferred, as it provides continued outflow of pericardial fluid. Pericardiectomy is recommended in cases of symptomatic constrictive pericarditis unresponsive to medical therapy.15
Back to the Case
The patient’s presentation—prodrome followed by fever and pleuritic chest pain—is characteristic of acute idiopathic pericarditis. No pericardial rub was heard, but EKG findings were typical. Troponin I elevation suggested underlying myopericarditis. An echocardiogram was unremarkable. Given the likely viral or idiopathic etiology, no further diagnostic tests were ordered to explore the possibility of an underlying systemic illness.
The patient was started on ibuprofen 600 mg every eight hours. She had significant relief of her symptoms within two days. A routine fever workup was negative. She was discharged the following day.
The patient was readmitted three months later with recurrent pleuritic chest pain, which did not improve with resumption of NSAID therapy. Initial troponin I was 0.22 ng/ml, electrocardiogram was unchanged, and an echocardiogram showed small effusion. She was started on ibuprofen 800 mg every eight hours, as well as colchicine 0.6 mg twice daily. Her symptoms resolved the next day and she was discharged with prescriptions for ibuprofen and colchicine. She was instructed to follow up with a primary-care doctor in one week.
At the clinic visit, ibuprofen was tapered but colchicine was continued for another six months. She remained asymptomatic at her six-month clinic follow-up.
Bottom Line
Acute pericarditis is a clinical diagnosis supported by EKG findings. Most cases are idiopathic or viral, and can be treated successfully with NSAIDs and colchicine. For cases that do not respond to initial therapy, or cases that present with high-risk features, a specific etiology should be sought.
Dr. Southern is chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y. Dr. Galhorta is an instructor and Drs. Martin, Korcak, and Stehlihova are assistant professors in the department of medicine at Albert Einstein.
References
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351:2195-2202.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378-382.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717-727.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042-1046.
- Bonnefoy E, Godon P, Kirkorian G, et al. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832-836.
- Salisbury AC, Olalla-Gomez C, Rihal CS, et al. Frequency and predictors of urgent coronary angiography in patients with acute pericarditis. Mayo Clin Proc. 2009;84(1):11-15.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739-2744.
- Imazio M, Spodick DH, Brucato A, et al. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64(10):1384-1392.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150-1153.
- Imazio M, Demichelis B, Cecchi E. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144-2148.
- Sagristà Sauleda J, Permanyer Miralda G, Soler Soler J. Diagnosis and management of pericardial syndromes. Rev Esp Cardiol. 2005;58(7):830-841.
- Bruce MA, Spodick DH. Atypical electrocardiogram in acute pericarditis: characteristics and prevalence. J Electrocardiol. 1980;13:61-66.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004; 25(7):587-610.
- Verhaert D, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333-343.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-928.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (COPE) trial. Circulation. 2005;112(13):2012-2016.
- Adler Y, Finkelstein Y, Guindo J, et al. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183-185.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the colchicine for recurrent pericarditis (CORE) trial. Arch Intern Med. 2005;165:1987-1991.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation. 2008;118:667-771.
Case
A 32-year-old female with no significant past medical history is evaluated for sharp, left-sided chest pain for five days. Her pain is intermittent, worse with deep inspiration and in the supine position. She denies any shortness of breath. Her temperature is 100.8ºF, but otherwise her vital signs are normal. The physical exam and chest radiograph are unremarkable, but an electrocardiogram shows diffuse ST-segment elevations. The initial troponin is mildly elevated at 0.35 ng/ml.
Could this patient have acute pericarditis? If so, how should she be managed?
Background
Pericarditis is the most common pericardial disease encountered by hospitalists. As many as 5% of chest pain cases unattributable to myocardial infarction (MI) are diagnosed with pericarditis.1 In immunocompetent individuals, as many as 90% of acute pericarditis cases are viral or idiopathic in etiology.1,2 Human immunodeficiency virus (HIV) and tuberculosis are common culprits in developing countries and immunocompromised hosts.3 Other specific etiologies of acute pericarditis include autoimmune diseases, neoplasms, chest irradiation, trauma, and metabolic disturbances (e.g. uremia). An etiologic classification of acute pericarditis is shown in Table 2 (p. 16).
Pericarditis primarily is a clinical diagnosis. Most patients present with chest pain.4 A pericardial friction rub may or may not be heard (sensitivity 16% to 85%), but when present is nearly 100% specific for pericarditis.2,5 Diffuse ST-segment elevation on electrocardiogram (EKG) is present in 60% to 90% of cases, but it can be difficult to differentiate from ST-segment elevations in acute MI.4,6
Uncomplicated acute pericarditis often is treated successfully as an outpatient.4 However, patients with high-risk features (see Table 1, right) should be hospitalized for identification and treatment of specific underlying etiology and for monitoring of complications, such as tamponade.7
Our patient has features consistent with pericarditis. In the following sections, we will review the diagnosis and treatment of acute pericarditis.
Review of the Data
How is acute pericarditis diagnosed?
Acute pericarditis is a clinical diagnosis supported by EKG and echocardiogram. At least two of the following four criteria must be present for the diagnosis: pleuritic chest pain, pericardial rub, diffuse ST-segment elevation on EKG, and pericardial effusion.8
History. Patients may report fever (46% in one small study of 69 patients) or a recent history of respiratory or gastrointestinal infection (40%).5 Most patients will report pleuritic chest pain. Typically, the pain is improved when sitting up and leaning forward, and gets worse when lying supine.4 Pain might radiate to the trapezius muscle ridge due to the common phrenic nerve innervation of pericardium and trapezius.9 However, pain might be minimal or absent in patients with uremic, neoplastic, tuberculous, or post-irradiation pericarditis.
Physical exam. A pericardial friction rub is nearly 100% specific for a pericarditis diagnosis, but sensitivity can vary (16% to 85%) depending on the frequency of auscultation and underlying etiology.2,5 It is thought to be caused by friction between the parietal and visceral layers of inflamed pericardium. A pericardial rub classically is described as a superficial, high-pitched, scratchy, or squeaking sound best heard with the diaphragm of the stethoscope at the lower left sternal border with the patient leaning forward.
Laboratory data. A complete blood count, metabolic panel, and cardiac enzymes should be checked in all patients with suspected acute pericarditis. Troponin values are elevated in up to one-third of patients, indicating cardiac muscle injury or myopericarditis, but have not been shown to adversely impact hospital length of stay, readmission, or complication rates.5,10 Markers of inflammation (e.g. erythrocyte sedimentation rate or C-reactive protein) are frequently elevated but do not point to a specific underlying etiology. Routine viral cultures and antibody titers are not useful.11
Most cases of pericarditis are presumed idiopathic (viral); however, finding a specific etiology should be considered in patients who do not respond after one week of therapy. Anti-nuclear antibody, complement levels, and rheumatoid factor can serve as screening tests for autoimmune disease. Purified protein derivative or quantiferon testing and HIV testing might be indicated in patients with appropriate risk factors. In cases of suspected tuberculous or neoplastic pericarditis, pericardial fluid analysis and biopsy could be warranted.
Electrocardiography. The EKG is the most useful test in diagnosing acute pericarditis. EKG changes in acute pericarditis can progress over four stages:
- Stage 1: diffuse ST elevations with or without PR depressions, initially;
- Stage 2: normalization of ST and PR segments, typically after several days;
- Stage 3: diffuse T-wave inversions; and
- Stage 4: normalization of T-waves, typically after weeks or months.
While all four stages are unlikely to be present in a given case, 80% of patients with pericarditis will demonstrate diffuse ST-segment elevations and PR-segment depression (see Figure 2, above).12
Table 3 lists EKG features helpful in differentiating acute pericarditis from acute myocardial infarction.
Chest radiography. Because a pericardial effusion often accompanies pericarditis, a chest radiograph (CXR) should be performed in all suspected cases. The CXR might show enlargement of the cardiac silhouette if more than 250 ml of pericardial fluid is present.3 A CXR also is helpful to diagnose concomitant pulmonary infection, pleural effusion, or mediastinal mass—all findings that could point to an underlying specific etiology of pericarditis and/or pericardial effusion.
Echocardiography. An echocardiogram should be performed in all patients with suspected pericarditis to detect effusion, associated myocardial, or paracardial disease.13 The echocardiogram frequently is normal but could show an effusion in 60%, and tamponade (see Figure 1, p. 15) in 5%, of cases.4
Computed tomography (CT) and cardiac magnetic resonance imaging (CMR).CT or CMR are the imaging modalities of choice when an echocardiogram is inconclusive or in cases of pericarditis complicated by a hemorrhagic or localized effusion, pericardial thickening, or pericardial mass.14 They also help in precise imaging of neighboring structures, such as lungs or mediastinum.
Pericardial fluid analysis and pericardial biopsy. In cases of refractory pericarditis with effusion, pericardial fluid analysis might provide clues to the underlying etiology. Routine chemistry, cell count, gram and acid fast staining, culture, and cytology should be sent. In addition, acid-fast bacillus staining and culture, adenosine deaminase, and interferon-gamma testing should be ordered when tuberculous pericarditis is suspected. A pericardial biopsy may show granulomas or neoplastic cells. Overall, pericardial fluid analysis and biopsy reveal a diagnosis in roughly 20% of cases.11
How is acute pericarditis treated?
Most cases of uncomplicated acute pericarditis are viral and respond well to NSAID plus colchicine therapy.2,4 Failure to respond to NSAIDs plus colchicine—evidenced by persistent fever, pericardial chest pain, new pericardial effusion, or worsening of general illness—within a week of treatment should prompt a search for an underlying systemic illness. If found, treatment should be aimed at the causative illness.
Bacterial pericarditis usually requires surgical drainage in addition to treatment with appropriate antibiotics.11 Tuberculous pericarditis is treated with multidrug therapy; when underlying HIV is present, patients should receive highly active anti-retroviral therapy as well. Steroids and immunosuppressants should be considered in addition to NSAIDs and colchicine in autoimmune pericarditis.10 Neoplastic pericarditis may resolve with chemotherapy but it has a high recurrence rate.13 Uremic pericarditis requires intensified dialysis.
Treatment options for uncomplicated idiopathic or viral pericarditis include:
NSAIDs. It is important to adequately dose NSAIDs when treating acute pericarditis. Initial treatment options include ibuprofen (1,600 to 3,200 mg daily), indomethacin (75 to 150 mg daily) or aspirin (2 to 4 gm daily) for one week.11,15 Aspirin is preferred in patients with ischemic heart disease. For patients with symptoms that persist longer than a week, NSAIDS may be continued, but investigation for an underlying etiology is indicated. Concomitant proton-pump-inhibitor therapy should be considered in patients at high risk for peptic ulcer disease to minimize gastric side effects.
Colchicine. Colchicine has a favorable risk-benefit profile as an adjunct treatment for acute and recurrent pericarditis. Patients experience better symptom relief when treated with both colchicine and an NSAID, compared with NSAIDs alone (88% versus 63%). Recurrence rates are lower with combined therapy (11% versus 32%).16 Colchicine treatment (0.6 mg twice daily after a loading dose of up to 2 mg) is recommended for several months to greater than one year.13,16,17
Glucocorticoids. Routine glucocorticoid use should be avoided in the treatment of acute pericarditis, as it has been associated with an increased risk for recurrence (OR 4.3).16,18 Glucocorticoid use should be considered in cases of pericarditis refractory to NSAIDs and colchicine, cases in which NSAIDs and or colchicine are contraindicated, and in autoimmune or connective-tissue-disease-related pericarditis. Prednisone should be dosed up to 1 mg/kg/day for at least one month, depending on symptom resolution, then tapered after either NSAIDs or colchicine have been started.13 Smaller prednisone doses of up to 0.5 mg/kg/day could be as effective, with the added benefit of reduced side effects and recurrences.19
Invasive treatment. Pericardiocentesis and/or pericardiectomy should be considered when pericarditis is complicated by a large effusion or tamponade, constrictive physiology, or recurrent effusion.11 Pericardiocentesis is the least invasive option and helps provide immediate relief in cases of tamponade or large symptomatic effusions. It is the preferred modality for obtaining pericardial fluid for diagnostic analysis. However, effusions can recur and in those cases pericardial window is preferred, as it provides continued outflow of pericardial fluid. Pericardiectomy is recommended in cases of symptomatic constrictive pericarditis unresponsive to medical therapy.15
Back to the Case
The patient’s presentation—prodrome followed by fever and pleuritic chest pain—is characteristic of acute idiopathic pericarditis. No pericardial rub was heard, but EKG findings were typical. Troponin I elevation suggested underlying myopericarditis. An echocardiogram was unremarkable. Given the likely viral or idiopathic etiology, no further diagnostic tests were ordered to explore the possibility of an underlying systemic illness.
The patient was started on ibuprofen 600 mg every eight hours. She had significant relief of her symptoms within two days. A routine fever workup was negative. She was discharged the following day.
The patient was readmitted three months later with recurrent pleuritic chest pain, which did not improve with resumption of NSAID therapy. Initial troponin I was 0.22 ng/ml, electrocardiogram was unchanged, and an echocardiogram showed small effusion. She was started on ibuprofen 800 mg every eight hours, as well as colchicine 0.6 mg twice daily. Her symptoms resolved the next day and she was discharged with prescriptions for ibuprofen and colchicine. She was instructed to follow up with a primary-care doctor in one week.
At the clinic visit, ibuprofen was tapered but colchicine was continued for another six months. She remained asymptomatic at her six-month clinic follow-up.
Bottom Line
Acute pericarditis is a clinical diagnosis supported by EKG findings. Most cases are idiopathic or viral, and can be treated successfully with NSAIDs and colchicine. For cases that do not respond to initial therapy, or cases that present with high-risk features, a specific etiology should be sought.
Dr. Southern is chief of the division of hospital medicine at Montefiore Medical Center in Bronx, N.Y. Dr. Galhorta is an instructor and Drs. Martin, Korcak, and Stehlihova are assistant professors in the department of medicine at Albert Einstein.
References
- Lange RA, Hillis LD. Clinical practice. Acute pericarditis. N Engl J Med. 2004;351:2195-2202.
- Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378-382.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717-727.
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042-1046.
- Bonnefoy E, Godon P, Kirkorian G, et al. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832-836.
- Salisbury AC, Olalla-Gomez C, Rihal CS, et al. Frequency and predictors of urgent coronary angiography in patients with acute pericarditis. Mayo Clin Proc. 2009;84(1):11-15.
- Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation. 2007;115:2739-2744.
- Imazio M, Spodick DH, Brucato A, et al. Diagnostic issues in the clinical management of pericarditis. Int J Clin Pract. 2010;64(10):1384-1392.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150-1153.
- Imazio M, Demichelis B, Cecchi E. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42(12):2144-2148.
- Sagristà Sauleda J, Permanyer Miralda G, Soler Soler J. Diagnosis and management of pericardial syndromes. Rev Esp Cardiol. 2005;58(7):830-841.
- Bruce MA, Spodick DH. Atypical electrocardiogram in acute pericarditis: characteristics and prevalence. J Electrocardiol. 1980;13:61-66.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Eur Heart J. 2004; 25(7):587-610.
- Verhaert D, Gabriel RS, Johnston D, et al. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333-343.
- Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation. 2010;121:916-928.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the colchicine for acute pericarditis (COPE) trial. Circulation. 2005;112(13):2012-2016.
- Adler Y, Finkelstein Y, Guindo J, et al. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183-185.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the colchicine for recurrent pericarditis (CORE) trial. Arch Intern Med. 2005;165:1987-1991.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation. 2008;118:667-771.
When Is Testing for Thrombophilia Indicated?
The Case
A healthy 42-year-old woman presents to the hospital with acute-onset pleuritic chest pain and shortness of breath. She has not had any recent surgeries, takes no medications, and is very active. A lung ventilation-perfusion scan reveals a high probability of pulmonary embolism (PE). The patient’s history is notable for two second-trimester pregnancy losses. The patient is started on low-molecular heparin and warfarin (LMHW).
Should this patient be tested for thrombophilia?
Background
Thrombophilia can now be identified in more than half of all patients presenting with VTE, and testing for underlying causes of thrombophilia has become widespread.1 Physicians believe that thrombophilia testing frequently changes management of patients with VTE.2
Thrombophilias can be classified into three major categories: deficiency of natural inhibitors of coagulation, abnormal function or elevated level of coagulation factors, and acquired thrombophilias (see Table 1).
The prevalence of specific thrombophilias varies widely. For example, the prevalence of activated protein C resistance (the factor V Leiden mutation) is 3% to 7%. In comparison, the prevalence of antithrombin deficiency is estimated at 0.02%. Each thrombophilia is associated with an increased VTE risk, but the level of risk associated with a given thrombophilia varies greatly.1
Before testing for thrombophilia in acute VTE, assess the risk of recurrent VTE by determining if the thrombosis was provoked or unprovoked. A VTE event is considered provoked if it occurs in the setting of pregnancy within the previous three months; estrogen therapy; immobility from acute illness for more than one week; travel lasting for more than six hours; leg trauma, fracture, or surgery within the previous three months; or active malignancy (see Table 2,).3 Unprovoked VTE has a recurrence rate of 7.4% per patient year, compared with 3.3% per patient year for a provoked VTE; the risk is even lower (0.7% per patient year) if the risk factor for the provoked VTE was surgical.4
Testing for thrombophilia is indicated if the results would add significant prognostic information beyond the clinical history, or if it would change patient management—in particular, the intensity or the duration of anticoagulation.
Review of the Data
Does presence of thrombophilia alter the intensity of anticoagulation for VTE?
If thrombophilia increases the risk of VTE recurrence while on anticoagulation, then a more intense level of anticoagulation might prevent future VTE. There are no studies investigating higher intensity of anticoagulation, but if standard anticoagulation were insufficient for patients with identifiable thrombophilia, one might expect to observe increased recurrence rates among patients with thrombophilia treated with standard warfarin therapy.
In a substudy of the Extended Low-Intensity Anticoagulation for Unprovoked Venous ThromboEmbolism (ELATE) trial, the risk of recurrence of VTE among treated subjects was very low overall, and the presence of thrombophilic abnormalities was not associated with significantly higher risk.5 Observational studies have found VTE recurrence rates are low in patients treated with warfarin, with or without thrombophilia.6-8
The impact of the initial level of anticoagulation on recurrence after the completion of the treatment period has been evaluated. Although one study suggested that patients with substandard levels of anticoagulation were at an increased risk of subsequent VTE, this was not confirmed in the Leiden Thrombophilia Study (LETS). 9,10
In sum, the majority of data do not suggest a significantly increased risk of recurrent VTE in patients with thrombophilia treated with standard anticoagulation. Therefore, treatment with warfarin to a goal INR of 2 to 3 is sufficient.
Does presence of thrombophilia alter duration of VTE treatment?
A major decision clinicians face when caring for VTE patients is the duration of anticoagulation treatment. The current ACCP recommendation for treatment of a provoked VTE is three months, with treatment for an unprovoked VTE three months or lifelong.11 If the presence of thrombophilia increases the risk of recurrence after cessation of anticoagulation treatment, longer duration of treatment might be indicated. One of the goals of thrombophilia testing should be to identify those patients.
Overall, the recurrence rate after first VTE is high, with a cumulative incidence of 25% at five years, 30% at eight years, and 56% at 20 years.12,13
Deficiency of natural inhibitors of coagulation.
Deficiency of a natural inhibitor of coagulation has been associated with a risk of recurrence of VTE of as much as 10% per year, according to some studies.6,14 However, the estimates are based on studies that include individuals from thrombosis-prone families, and selection bias might have contributed to the high recurrence rates.1 In the unselected population represented in the LETS study, only a modest elevation was seen in the estimated risk of recurrence for patients with inhibitor deficiencies.15
Testing for deficiency of inhibitors offers little prognostic information beyond that obtained when determining whether a VTE event is provoked or unprovoked. In studies that have separately examined subjects with provoked vs. unprovoked VTE, deficiency of an inhibitor is not associated with increased risk of recurrence.15,16
Abnormal function or level of anticoagulation factors.
Factor V Leiden (FVL) is the most common cause of inherited thrombophilia and is associated with as much as a sixfold increase in VTE risk, while the prothrombin gene mutation is associated with a twofold increase.17,18
In contrast, the evidence associating these mutations with recurrent VTE risk is not as consistent. Although a study conducted at a referral center in Italy found an increased risk of recurrence with either Factor V Leiden or prothrombin gene mutation, a large meta-analysis of 23 studies found increased risk only with Factor V Leiden.19,20 Another meta-analysis demonstrated only a modest increased risk of recurrence in subjects with Factor V Leiden or prothrombin gene mutation, and a prospective study from Austria found no increased risk of recurrence with Factor V Leiden two years after discontinuation of anticoagulation.18,21 Additionally, when using patients with unprovoked VTE as reference, there was no increased risk of recurrence among patients homozygous for Factor V Leiden or the prothrombin gene mutation.22
In summary, although Factor V Leiden and prothrombin gene defects are associated with increased risk of recurrent VTE, the magnitude of the risk increase is modest and, therefore, should not alter duration of therapy.
Acquired thrombophilia.
It appears that the only thrombophilic state that might have a significant impact on the risk of recurrence is the antiphospholipid syndrome. The cessation of warfarin therapy in patients with thrombosis associated with antiphospholipid antibodies carries a 69% risk of recurrent thrombosis within a year.23 Some studies have suggested that the presence of specific antibodies (i.e. anticardiolipin antibodies) is associated with increased risk in patients with antiphospholipid syndrome.24
However, at present, all patients with VTE and antiphospholipid syndrome should be candidates for lifelong anticoagulation. Antiphospholipid antibody testing should be performed in patients with a suggestive history, including those with recurrent fetal loss or a single fetal loss after 10 weeks, or known collagen vascular disease.25
The role of provoked vs. unprovoked VTE.
Identifying whether a VTE is provoked or unprovoked has been shown to be an important predictor of recurrence. For example, one prospective, cohort study found two-year recurrence rates of zero in patients with a surgery or pregnancy-related VTE, 9% with other provoked VTE, and 19% with unprovoked VTE.26 In the same study, thrombophilia testing failed to reliably predict recurrence risk. Patients with unprovoked VTE who were tested and found to not have a defect were at equally high risk of recurrent VTE as those found to have a thrombophilia.27
The most significant predictor for VTE recurrence is whether the first event was provoked, and thrombophilia testing offers little additional prognostic information.28
VTE as a multifactorial disorder.
It is becoming increasingly clear that VTE is multifactorial disorder, caused by the interactions of genotypic, phenotypic, and environmental factors. In the case of an unprovoked VTE, the patient already carries a significantly elevated risk for recurrence, and further testing for known causes of thrombophilia appears to add very little additional information. The optimal duration of anticoagulation for unprovoked VTE is unclear, but current guidelines suggest at least three months—and clinicians should consider lifelong treatment.
In the vast majority of cases, testing for thrombophilia has no impact on the management of VTE and is not warranted. In patients with antiphospholipid-antibody syndrome, given the high risk of recurrence, long-term anticoagulation after a first VTE might be indicated. In select patients with a clinical picture suggestive of antiphospholipid-antibody syndrome, or a strong family history, testing should be considered.
Back to the Case
Our patient appears to have an unprovoked VTE. She should receive regular anticoagulation with warfarin, with a goal INR of 2 to 3, for at least three months. Lifelong anticoagulation therapy should be considered. Testing for heritable thrombophilia will not change the current management or treatment duration and, hence, is not indicated. However, the patient’s history is suggestive of antiphospholipid-antibody syndrome, so she should be tested. If the diagnosis of antiphospholipid syndrome is made, lifelong anticoagulation should be considered.
Bottom Line
Unprovoked VTE provides the strongest predictor for recurrence. Thrombophilia testing adds little in predicting recurrence and rarely is indicated.
Dr. Stehlikova is a clinical hospitalist in the division of hospital medicine, department of medicine, at Albert Einstein College of Medicine and Montefiore Medical Center in Bronx, N.Y. Dr. Martin is director of the Einstein Hospitalist Service. Dr. Janakiram is a fellow in the department of hematology at Einstein, and Dr. Korcak is an instructor at Einstein in the department of medicine and director of the Weiler Medical Service. Dr. Galhotra is associate director for inpatient quality in the department of medicine at Einstein; Dr. Averbukh is an academic hospitalist; and Dr. Southern is chief of the division of hospital medicine at Einstein.
References
- Middeldorp S, van Hylckama Vlieg A. Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143:321-335.
- Coppens M, van Mourik JA, Eckmann CM, Büller HR, Middeldorp S. Current practise of testing for inherited thrombophilia. J Thromb Haemost. 2007;5:1979-1981.
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199-205.
- Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170:1710-1716.
- Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood. 2008;112:4432-4436.
- Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol. 2005;25:1992-1997.
- Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3'-untranslated region of the prothrombin gene. Br J Haematol. 1997;98:907-909.
- Schulman S, Tengborn L. Treatment of venous thromboembolism in patients with congenital deficiency of antithrombin III. Thromb Haemost. 1992;68:634-636.
- Palareti G, Legnani C, Cosmi B, Guazzaloca G, Cini M, Mattarozzi S. Poor anticoagulation quality in the first 3 months after unprovoked venous thromboembolism is a risk factor for long-term recurrence. J Thromb Haemost. 2005;3:955-961.
- Gadisseur AP, Christiansen SC, van der Meer FJ, Rosendaal FR. The quality of oral anticoagulant therapy and recurrent venous thrombotic events in the Leiden Thrombophilia Study. J Thromb Haemost. 2007;5:931-936.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
- Laczkovics C, Grafenhofer H, Kaider A, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201-1207.
- Brouwer JL, Lijfering WM, Ten Kate MK, Kluin-Nelemans HC, Veeger NJ, van der Meer J. High long-term absolute risk of recurrent venous thromboembolism in patients with hereditary deficiencies of protein S, protein C or antithrombin. Thromb Haemost. 2009;101:93-99.
- Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352-2361.
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695-698.
- Price DT, Ridker PM. Factor V Leiden mutation and the risks for thromboembolic disease: a clinical perspective. Ann Intern Med. 1997;127:895-903.
- Ho WK, Hankey GJ, Quinlan DJ, Eikelboom JW. Risk of recurrent venous thromboembolism in patients with common thrombophilia: a systematic review. Arch Intern Med. 2006;166:729-736.
- Simioni P, Prandoni P, Lensing AW, et al. Risk for subsequent venous thromboembolic complications in carriers of the prothrombin or the factor V gene mutation with a first episode of deep-vein thrombosis. Blood. 2000;96:3329-3333.
- Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301:2472-2485.
- Eichinger S, Pabinger I, Stumpflen A, et al. The risk of recurrent venous thromboembolism in patients with and without factor V Leiden. Thromb Haemost. 1997;77:624-628.
- Lijfering WM, Middeldorp S, Veeger NJ, et al. Risk of recurrent venous thrombosis in homozygous carriers and double heterozygous carriers of factor V Leiden and prothrombin G20210A. Circulation. 2010;121(15):1706-1712.
- Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993-997.
- Schulman S, Svenungsson E, Granqvist S. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Duration of Anticoagulation Study Group. Am J Med. 1998;104:332-338.
- Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009;7:1737-1740.
- Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523-526.
- Rosendaal FR. Once and only once. Circulation. 2010;121:1688-1690.
- Dalen JE. Should patients with venous thromboembolism be screened for thrombophilia? Am J Med. 2008;121:458-463.
The Case
A healthy 42-year-old woman presents to the hospital with acute-onset pleuritic chest pain and shortness of breath. She has not had any recent surgeries, takes no medications, and is very active. A lung ventilation-perfusion scan reveals a high probability of pulmonary embolism (PE). The patient’s history is notable for two second-trimester pregnancy losses. The patient is started on low-molecular heparin and warfarin (LMHW).
Should this patient be tested for thrombophilia?
Background
Thrombophilia can now be identified in more than half of all patients presenting with VTE, and testing for underlying causes of thrombophilia has become widespread.1 Physicians believe that thrombophilia testing frequently changes management of patients with VTE.2
Thrombophilias can be classified into three major categories: deficiency of natural inhibitors of coagulation, abnormal function or elevated level of coagulation factors, and acquired thrombophilias (see Table 1).
The prevalence of specific thrombophilias varies widely. For example, the prevalence of activated protein C resistance (the factor V Leiden mutation) is 3% to 7%. In comparison, the prevalence of antithrombin deficiency is estimated at 0.02%. Each thrombophilia is associated with an increased VTE risk, but the level of risk associated with a given thrombophilia varies greatly.1
Before testing for thrombophilia in acute VTE, assess the risk of recurrent VTE by determining if the thrombosis was provoked or unprovoked. A VTE event is considered provoked if it occurs in the setting of pregnancy within the previous three months; estrogen therapy; immobility from acute illness for more than one week; travel lasting for more than six hours; leg trauma, fracture, or surgery within the previous three months; or active malignancy (see Table 2,).3 Unprovoked VTE has a recurrence rate of 7.4% per patient year, compared with 3.3% per patient year for a provoked VTE; the risk is even lower (0.7% per patient year) if the risk factor for the provoked VTE was surgical.4
Testing for thrombophilia is indicated if the results would add significant prognostic information beyond the clinical history, or if it would change patient management—in particular, the intensity or the duration of anticoagulation.
Review of the Data
Does presence of thrombophilia alter the intensity of anticoagulation for VTE?
If thrombophilia increases the risk of VTE recurrence while on anticoagulation, then a more intense level of anticoagulation might prevent future VTE. There are no studies investigating higher intensity of anticoagulation, but if standard anticoagulation were insufficient for patients with identifiable thrombophilia, one might expect to observe increased recurrence rates among patients with thrombophilia treated with standard warfarin therapy.
In a substudy of the Extended Low-Intensity Anticoagulation for Unprovoked Venous ThromboEmbolism (ELATE) trial, the risk of recurrence of VTE among treated subjects was very low overall, and the presence of thrombophilic abnormalities was not associated with significantly higher risk.5 Observational studies have found VTE recurrence rates are low in patients treated with warfarin, with or without thrombophilia.6-8
The impact of the initial level of anticoagulation on recurrence after the completion of the treatment period has been evaluated. Although one study suggested that patients with substandard levels of anticoagulation were at an increased risk of subsequent VTE, this was not confirmed in the Leiden Thrombophilia Study (LETS). 9,10
In sum, the majority of data do not suggest a significantly increased risk of recurrent VTE in patients with thrombophilia treated with standard anticoagulation. Therefore, treatment with warfarin to a goal INR of 2 to 3 is sufficient.
Does presence of thrombophilia alter duration of VTE treatment?
A major decision clinicians face when caring for VTE patients is the duration of anticoagulation treatment. The current ACCP recommendation for treatment of a provoked VTE is three months, with treatment for an unprovoked VTE three months or lifelong.11 If the presence of thrombophilia increases the risk of recurrence after cessation of anticoagulation treatment, longer duration of treatment might be indicated. One of the goals of thrombophilia testing should be to identify those patients.
Overall, the recurrence rate after first VTE is high, with a cumulative incidence of 25% at five years, 30% at eight years, and 56% at 20 years.12,13
Deficiency of natural inhibitors of coagulation.
Deficiency of a natural inhibitor of coagulation has been associated with a risk of recurrence of VTE of as much as 10% per year, according to some studies.6,14 However, the estimates are based on studies that include individuals from thrombosis-prone families, and selection bias might have contributed to the high recurrence rates.1 In the unselected population represented in the LETS study, only a modest elevation was seen in the estimated risk of recurrence for patients with inhibitor deficiencies.15
Testing for deficiency of inhibitors offers little prognostic information beyond that obtained when determining whether a VTE event is provoked or unprovoked. In studies that have separately examined subjects with provoked vs. unprovoked VTE, deficiency of an inhibitor is not associated with increased risk of recurrence.15,16
Abnormal function or level of anticoagulation factors.
Factor V Leiden (FVL) is the most common cause of inherited thrombophilia and is associated with as much as a sixfold increase in VTE risk, while the prothrombin gene mutation is associated with a twofold increase.17,18
In contrast, the evidence associating these mutations with recurrent VTE risk is not as consistent. Although a study conducted at a referral center in Italy found an increased risk of recurrence with either Factor V Leiden or prothrombin gene mutation, a large meta-analysis of 23 studies found increased risk only with Factor V Leiden.19,20 Another meta-analysis demonstrated only a modest increased risk of recurrence in subjects with Factor V Leiden or prothrombin gene mutation, and a prospective study from Austria found no increased risk of recurrence with Factor V Leiden two years after discontinuation of anticoagulation.18,21 Additionally, when using patients with unprovoked VTE as reference, there was no increased risk of recurrence among patients homozygous for Factor V Leiden or the prothrombin gene mutation.22
In summary, although Factor V Leiden and prothrombin gene defects are associated with increased risk of recurrent VTE, the magnitude of the risk increase is modest and, therefore, should not alter duration of therapy.
Acquired thrombophilia.
It appears that the only thrombophilic state that might have a significant impact on the risk of recurrence is the antiphospholipid syndrome. The cessation of warfarin therapy in patients with thrombosis associated with antiphospholipid antibodies carries a 69% risk of recurrent thrombosis within a year.23 Some studies have suggested that the presence of specific antibodies (i.e. anticardiolipin antibodies) is associated with increased risk in patients with antiphospholipid syndrome.24
However, at present, all patients with VTE and antiphospholipid syndrome should be candidates for lifelong anticoagulation. Antiphospholipid antibody testing should be performed in patients with a suggestive history, including those with recurrent fetal loss or a single fetal loss after 10 weeks, or known collagen vascular disease.25
The role of provoked vs. unprovoked VTE.
Identifying whether a VTE is provoked or unprovoked has been shown to be an important predictor of recurrence. For example, one prospective, cohort study found two-year recurrence rates of zero in patients with a surgery or pregnancy-related VTE, 9% with other provoked VTE, and 19% with unprovoked VTE.26 In the same study, thrombophilia testing failed to reliably predict recurrence risk. Patients with unprovoked VTE who were tested and found to not have a defect were at equally high risk of recurrent VTE as those found to have a thrombophilia.27
The most significant predictor for VTE recurrence is whether the first event was provoked, and thrombophilia testing offers little additional prognostic information.28
VTE as a multifactorial disorder.
It is becoming increasingly clear that VTE is multifactorial disorder, caused by the interactions of genotypic, phenotypic, and environmental factors. In the case of an unprovoked VTE, the patient already carries a significantly elevated risk for recurrence, and further testing for known causes of thrombophilia appears to add very little additional information. The optimal duration of anticoagulation for unprovoked VTE is unclear, but current guidelines suggest at least three months—and clinicians should consider lifelong treatment.
In the vast majority of cases, testing for thrombophilia has no impact on the management of VTE and is not warranted. In patients with antiphospholipid-antibody syndrome, given the high risk of recurrence, long-term anticoagulation after a first VTE might be indicated. In select patients with a clinical picture suggestive of antiphospholipid-antibody syndrome, or a strong family history, testing should be considered.
Back to the Case
Our patient appears to have an unprovoked VTE. She should receive regular anticoagulation with warfarin, with a goal INR of 2 to 3, for at least three months. Lifelong anticoagulation therapy should be considered. Testing for heritable thrombophilia will not change the current management or treatment duration and, hence, is not indicated. However, the patient’s history is suggestive of antiphospholipid-antibody syndrome, so she should be tested. If the diagnosis of antiphospholipid syndrome is made, lifelong anticoagulation should be considered.
Bottom Line
Unprovoked VTE provides the strongest predictor for recurrence. Thrombophilia testing adds little in predicting recurrence and rarely is indicated.
Dr. Stehlikova is a clinical hospitalist in the division of hospital medicine, department of medicine, at Albert Einstein College of Medicine and Montefiore Medical Center in Bronx, N.Y. Dr. Martin is director of the Einstein Hospitalist Service. Dr. Janakiram is a fellow in the department of hematology at Einstein, and Dr. Korcak is an instructor at Einstein in the department of medicine and director of the Weiler Medical Service. Dr. Galhotra is associate director for inpatient quality in the department of medicine at Einstein; Dr. Averbukh is an academic hospitalist; and Dr. Southern is chief of the division of hospital medicine at Einstein.
References
- Middeldorp S, van Hylckama Vlieg A. Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143:321-335.
- Coppens M, van Mourik JA, Eckmann CM, Büller HR, Middeldorp S. Current practise of testing for inherited thrombophilia. J Thromb Haemost. 2007;5:1979-1981.
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199-205.
- Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170:1710-1716.
- Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood. 2008;112:4432-4436.
- Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol. 2005;25:1992-1997.
- Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3'-untranslated region of the prothrombin gene. Br J Haematol. 1997;98:907-909.
- Schulman S, Tengborn L. Treatment of venous thromboembolism in patients with congenital deficiency of antithrombin III. Thromb Haemost. 1992;68:634-636.
- Palareti G, Legnani C, Cosmi B, Guazzaloca G, Cini M, Mattarozzi S. Poor anticoagulation quality in the first 3 months after unprovoked venous thromboembolism is a risk factor for long-term recurrence. J Thromb Haemost. 2005;3:955-961.
- Gadisseur AP, Christiansen SC, van der Meer FJ, Rosendaal FR. The quality of oral anticoagulant therapy and recurrent venous thrombotic events in the Leiden Thrombophilia Study. J Thromb Haemost. 2007;5:931-936.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
- Laczkovics C, Grafenhofer H, Kaider A, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201-1207.
- Brouwer JL, Lijfering WM, Ten Kate MK, Kluin-Nelemans HC, Veeger NJ, van der Meer J. High long-term absolute risk of recurrent venous thromboembolism in patients with hereditary deficiencies of protein S, protein C or antithrombin. Thromb Haemost. 2009;101:93-99.
- Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352-2361.
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695-698.
- Price DT, Ridker PM. Factor V Leiden mutation and the risks for thromboembolic disease: a clinical perspective. Ann Intern Med. 1997;127:895-903.
- Ho WK, Hankey GJ, Quinlan DJ, Eikelboom JW. Risk of recurrent venous thromboembolism in patients with common thrombophilia: a systematic review. Arch Intern Med. 2006;166:729-736.
- Simioni P, Prandoni P, Lensing AW, et al. Risk for subsequent venous thromboembolic complications in carriers of the prothrombin or the factor V gene mutation with a first episode of deep-vein thrombosis. Blood. 2000;96:3329-3333.
- Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301:2472-2485.
- Eichinger S, Pabinger I, Stumpflen A, et al. The risk of recurrent venous thromboembolism in patients with and without factor V Leiden. Thromb Haemost. 1997;77:624-628.
- Lijfering WM, Middeldorp S, Veeger NJ, et al. Risk of recurrent venous thrombosis in homozygous carriers and double heterozygous carriers of factor V Leiden and prothrombin G20210A. Circulation. 2010;121(15):1706-1712.
- Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993-997.
- Schulman S, Svenungsson E, Granqvist S. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Duration of Anticoagulation Study Group. Am J Med. 1998;104:332-338.
- Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009;7:1737-1740.
- Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523-526.
- Rosendaal FR. Once and only once. Circulation. 2010;121:1688-1690.
- Dalen JE. Should patients with venous thromboembolism be screened for thrombophilia? Am J Med. 2008;121:458-463.
The Case
A healthy 42-year-old woman presents to the hospital with acute-onset pleuritic chest pain and shortness of breath. She has not had any recent surgeries, takes no medications, and is very active. A lung ventilation-perfusion scan reveals a high probability of pulmonary embolism (PE). The patient’s history is notable for two second-trimester pregnancy losses. The patient is started on low-molecular heparin and warfarin (LMHW).
Should this patient be tested for thrombophilia?
Background
Thrombophilia can now be identified in more than half of all patients presenting with VTE, and testing for underlying causes of thrombophilia has become widespread.1 Physicians believe that thrombophilia testing frequently changes management of patients with VTE.2
Thrombophilias can be classified into three major categories: deficiency of natural inhibitors of coagulation, abnormal function or elevated level of coagulation factors, and acquired thrombophilias (see Table 1).
The prevalence of specific thrombophilias varies widely. For example, the prevalence of activated protein C resistance (the factor V Leiden mutation) is 3% to 7%. In comparison, the prevalence of antithrombin deficiency is estimated at 0.02%. Each thrombophilia is associated with an increased VTE risk, but the level of risk associated with a given thrombophilia varies greatly.1
Before testing for thrombophilia in acute VTE, assess the risk of recurrent VTE by determining if the thrombosis was provoked or unprovoked. A VTE event is considered provoked if it occurs in the setting of pregnancy within the previous three months; estrogen therapy; immobility from acute illness for more than one week; travel lasting for more than six hours; leg trauma, fracture, or surgery within the previous three months; or active malignancy (see Table 2,).3 Unprovoked VTE has a recurrence rate of 7.4% per patient year, compared with 3.3% per patient year for a provoked VTE; the risk is even lower (0.7% per patient year) if the risk factor for the provoked VTE was surgical.4
Testing for thrombophilia is indicated if the results would add significant prognostic information beyond the clinical history, or if it would change patient management—in particular, the intensity or the duration of anticoagulation.
Review of the Data
Does presence of thrombophilia alter the intensity of anticoagulation for VTE?
If thrombophilia increases the risk of VTE recurrence while on anticoagulation, then a more intense level of anticoagulation might prevent future VTE. There are no studies investigating higher intensity of anticoagulation, but if standard anticoagulation were insufficient for patients with identifiable thrombophilia, one might expect to observe increased recurrence rates among patients with thrombophilia treated with standard warfarin therapy.
In a substudy of the Extended Low-Intensity Anticoagulation for Unprovoked Venous ThromboEmbolism (ELATE) trial, the risk of recurrence of VTE among treated subjects was very low overall, and the presence of thrombophilic abnormalities was not associated with significantly higher risk.5 Observational studies have found VTE recurrence rates are low in patients treated with warfarin, with or without thrombophilia.6-8
The impact of the initial level of anticoagulation on recurrence after the completion of the treatment period has been evaluated. Although one study suggested that patients with substandard levels of anticoagulation were at an increased risk of subsequent VTE, this was not confirmed in the Leiden Thrombophilia Study (LETS). 9,10
In sum, the majority of data do not suggest a significantly increased risk of recurrent VTE in patients with thrombophilia treated with standard anticoagulation. Therefore, treatment with warfarin to a goal INR of 2 to 3 is sufficient.
Does presence of thrombophilia alter duration of VTE treatment?
A major decision clinicians face when caring for VTE patients is the duration of anticoagulation treatment. The current ACCP recommendation for treatment of a provoked VTE is three months, with treatment for an unprovoked VTE three months or lifelong.11 If the presence of thrombophilia increases the risk of recurrence after cessation of anticoagulation treatment, longer duration of treatment might be indicated. One of the goals of thrombophilia testing should be to identify those patients.
Overall, the recurrence rate after first VTE is high, with a cumulative incidence of 25% at five years, 30% at eight years, and 56% at 20 years.12,13
Deficiency of natural inhibitors of coagulation.
Deficiency of a natural inhibitor of coagulation has been associated with a risk of recurrence of VTE of as much as 10% per year, according to some studies.6,14 However, the estimates are based on studies that include individuals from thrombosis-prone families, and selection bias might have contributed to the high recurrence rates.1 In the unselected population represented in the LETS study, only a modest elevation was seen in the estimated risk of recurrence for patients with inhibitor deficiencies.15
Testing for deficiency of inhibitors offers little prognostic information beyond that obtained when determining whether a VTE event is provoked or unprovoked. In studies that have separately examined subjects with provoked vs. unprovoked VTE, deficiency of an inhibitor is not associated with increased risk of recurrence.15,16
Abnormal function or level of anticoagulation factors.
Factor V Leiden (FVL) is the most common cause of inherited thrombophilia and is associated with as much as a sixfold increase in VTE risk, while the prothrombin gene mutation is associated with a twofold increase.17,18
In contrast, the evidence associating these mutations with recurrent VTE risk is not as consistent. Although a study conducted at a referral center in Italy found an increased risk of recurrence with either Factor V Leiden or prothrombin gene mutation, a large meta-analysis of 23 studies found increased risk only with Factor V Leiden.19,20 Another meta-analysis demonstrated only a modest increased risk of recurrence in subjects with Factor V Leiden or prothrombin gene mutation, and a prospective study from Austria found no increased risk of recurrence with Factor V Leiden two years after discontinuation of anticoagulation.18,21 Additionally, when using patients with unprovoked VTE as reference, there was no increased risk of recurrence among patients homozygous for Factor V Leiden or the prothrombin gene mutation.22
In summary, although Factor V Leiden and prothrombin gene defects are associated with increased risk of recurrent VTE, the magnitude of the risk increase is modest and, therefore, should not alter duration of therapy.
Acquired thrombophilia.
It appears that the only thrombophilic state that might have a significant impact on the risk of recurrence is the antiphospholipid syndrome. The cessation of warfarin therapy in patients with thrombosis associated with antiphospholipid antibodies carries a 69% risk of recurrent thrombosis within a year.23 Some studies have suggested that the presence of specific antibodies (i.e. anticardiolipin antibodies) is associated with increased risk in patients with antiphospholipid syndrome.24
However, at present, all patients with VTE and antiphospholipid syndrome should be candidates for lifelong anticoagulation. Antiphospholipid antibody testing should be performed in patients with a suggestive history, including those with recurrent fetal loss or a single fetal loss after 10 weeks, or known collagen vascular disease.25
The role of provoked vs. unprovoked VTE.
Identifying whether a VTE is provoked or unprovoked has been shown to be an important predictor of recurrence. For example, one prospective, cohort study found two-year recurrence rates of zero in patients with a surgery or pregnancy-related VTE, 9% with other provoked VTE, and 19% with unprovoked VTE.26 In the same study, thrombophilia testing failed to reliably predict recurrence risk. Patients with unprovoked VTE who were tested and found to not have a defect were at equally high risk of recurrent VTE as those found to have a thrombophilia.27
The most significant predictor for VTE recurrence is whether the first event was provoked, and thrombophilia testing offers little additional prognostic information.28
VTE as a multifactorial disorder.
It is becoming increasingly clear that VTE is multifactorial disorder, caused by the interactions of genotypic, phenotypic, and environmental factors. In the case of an unprovoked VTE, the patient already carries a significantly elevated risk for recurrence, and further testing for known causes of thrombophilia appears to add very little additional information. The optimal duration of anticoagulation for unprovoked VTE is unclear, but current guidelines suggest at least three months—and clinicians should consider lifelong treatment.
In the vast majority of cases, testing for thrombophilia has no impact on the management of VTE and is not warranted. In patients with antiphospholipid-antibody syndrome, given the high risk of recurrence, long-term anticoagulation after a first VTE might be indicated. In select patients with a clinical picture suggestive of antiphospholipid-antibody syndrome, or a strong family history, testing should be considered.
Back to the Case
Our patient appears to have an unprovoked VTE. She should receive regular anticoagulation with warfarin, with a goal INR of 2 to 3, for at least three months. Lifelong anticoagulation therapy should be considered. Testing for heritable thrombophilia will not change the current management or treatment duration and, hence, is not indicated. However, the patient’s history is suggestive of antiphospholipid-antibody syndrome, so she should be tested. If the diagnosis of antiphospholipid syndrome is made, lifelong anticoagulation should be considered.
Bottom Line
Unprovoked VTE provides the strongest predictor for recurrence. Thrombophilia testing adds little in predicting recurrence and rarely is indicated.
Dr. Stehlikova is a clinical hospitalist in the division of hospital medicine, department of medicine, at Albert Einstein College of Medicine and Montefiore Medical Center in Bronx, N.Y. Dr. Martin is director of the Einstein Hospitalist Service. Dr. Janakiram is a fellow in the department of hematology at Einstein, and Dr. Korcak is an instructor at Einstein in the department of medicine and director of the Weiler Medical Service. Dr. Galhotra is associate director for inpatient quality in the department of medicine at Einstein; Dr. Averbukh is an academic hospitalist; and Dr. Southern is chief of the division of hospital medicine at Einstein.
References
- Middeldorp S, van Hylckama Vlieg A. Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143:321-335.
- Coppens M, van Mourik JA, Eckmann CM, Büller HR, Middeldorp S. Current practise of testing for inherited thrombophilia. J Thromb Haemost. 2007;5:1979-1981.
- Prandoni P, Noventa F, Ghirarduzzi A, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199-205.
- Iorio A, Kearon C, Filippucci E, et al. Risk of recurrence after a first episode of symptomatic venous thromboembolism provoked by a transient risk factor: a systematic review. Arch Intern Med. 2010;170:1710-1716.
- Kearon C, Julian JA, Kovacs MJ, et al. Influence of thrombophilia on risk of recurrent venous thromboembolism while on warfarin: results from a randomized trial. Blood. 2008;112:4432-4436.
- Vossen CY, Walker ID, Svensson P, et al. Recurrence rate after a first venous thrombosis in patients with familial thrombophilia. Arterioscler Thromb Vasc Biol. 2005;25:1992-1997.
- Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3'-untranslated region of the prothrombin gene. Br J Haematol. 1997;98:907-909.
- Schulman S, Tengborn L. Treatment of venous thromboembolism in patients with congenital deficiency of antithrombin III. Thromb Haemost. 1992;68:634-636.
- Palareti G, Legnani C, Cosmi B, Guazzaloca G, Cini M, Mattarozzi S. Poor anticoagulation quality in the first 3 months after unprovoked venous thromboembolism is a risk factor for long-term recurrence. J Thromb Haemost. 2005;3:955-961.
- Gadisseur AP, Christiansen SC, van der Meer FJ, Rosendaal FR. The quality of oral anticoagulant therapy and recurrent venous thrombotic events in the Leiden Thrombophilia Study. J Thromb Haemost. 2007;5:931-936.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008;133:454S-545S.
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
- Laczkovics C, Grafenhofer H, Kaider A, et al. Risk of recurrence after a first venous thromboembolic event in young women. Haematologica. 2007;92:1201-1207.
- Brouwer JL, Lijfering WM, Ten Kate MK, Kluin-Nelemans HC, Veeger NJ, van der Meer J. High long-term absolute risk of recurrent venous thromboembolism in patients with hereditary deficiencies of protein S, protein C or antithrombin. Thromb Haemost. 2009;101:93-99.
- Christiansen SC, Cannegieter SC, Koster T, Vandenbroucke JP, Rosendaal FR. Thrombophilia, clinical factors, and recurrent venous thrombotic events. JAMA. 2005;293:2352-2361.
- De Stefano V, Simioni P, Rossi E, et al. The risk of recurrent venous thromboembolism in patients with inherited deficiency of natural anticoagulants antithrombin, protein C and protein S. Haematologica. 2006;91:695-698.
- Price DT, Ridker PM. Factor V Leiden mutation and the risks for thromboembolic disease: a clinical perspective. Ann Intern Med. 1997;127:895-903.
- Ho WK, Hankey GJ, Quinlan DJ, Eikelboom JW. Risk of recurrent venous thromboembolism in patients with common thrombophilia: a systematic review. Arch Intern Med. 2006;166:729-736.
- Simioni P, Prandoni P, Lensing AW, et al. Risk for subsequent venous thromboembolic complications in carriers of the prothrombin or the factor V gene mutation with a first episode of deep-vein thrombosis. Blood. 2000;96:3329-3333.
- Segal JB, Brotman DJ, Necochea AJ, et al. Predictive value of factor V Leiden and prothrombin G20210A in adults with venous thromboembolism and in family members of those with a mutation: a systematic review. JAMA. 2009;301:2472-2485.
- Eichinger S, Pabinger I, Stumpflen A, et al. The risk of recurrent venous thromboembolism in patients with and without factor V Leiden. Thromb Haemost. 1997;77:624-628.
- Lijfering WM, Middeldorp S, Veeger NJ, et al. Risk of recurrent venous thrombosis in homozygous carriers and double heterozygous carriers of factor V Leiden and prothrombin G20210A. Circulation. 2010;121(15):1706-1712.
- Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GR. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 1995;332:993-997.
- Schulman S, Svenungsson E, Granqvist S. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. Duration of Anticoagulation Study Group. Am J Med. 1998;104:332-338.
- Pengo V, Tripodi A, Reber G, et al. Update of the guidelines for lupus anticoagulant detection. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibody of the Scientific and Standardisation Committee of the International Society on Thrombosis and Haemostasis. J Thromb Haemost. 2009;7:1737-1740.
- Baglin T, Luddington R, Brown K, Baglin C. Incidence of recurrent venous thromboembolism in relation to clinical and thrombophilic risk factors: prospective cohort study. Lancet. 2003;362:523-526.
- Rosendaal FR. Once and only once. Circulation. 2010;121:1688-1690.
- Dalen JE. Should patients with venous thromboembolism be screened for thrombophilia? Am J Med. 2008;121:458-463.
ITL: Physician Reviews of HM-Relevant Research
In This Edition
Literature At A Glance
A guide to this month’s studies
- Nearly all CDIs Related to Exposure in Healthcare Setting
- In Suspected Acute Coronary Syndrome, CT Angiography Identifies Patients Safe for Discharge
- Impending Physiological Deterioration Can Be Predicted Using Data from a Comprehensive EHR
- Rapid Influenza Diagnostic Tests Have Low Sensitivity and High Specificity
- Multifaceted QI Intervention Increases Adherence to Evidence-Based Therapy in Acute Coronary Syndrome
- Rivaroxaban for the Treatment of Acute Pulmonary Embolism
- Coronary Stent Implantation Provides No Additional Benefit when Compared with Medical Therapy Alone in Patients with Stable Coronary Artery Disease
- Prolonged Versus Standard Duration Venous Thromboprophylaxis after Major Orthopedic Surgery
Nearly all CDIs Related to Exposure in Healthcare Setting
Clinical question: What is the contribution of non-hospital healthcare exposures to the burden of Clostridium difficile infection (CDI)?
Background: CDI is common among hospitalized patients and is associated with high rates of morbidity. Most CDI prevention programs are aimed at hospital-based risk factors. However, non-hospital healthcare exposures might contribute significantly to the burden of CDI, and hospital-based prevention programs might not address these risks.
Study design: Retrospective analysis of three population-based data sets.
Setting: Three population data sets tracking infections on a national and state level in the U.S.
Synopsis: This study analyzed two data sets to determine the contribution of non-hospital healthcare exposure to CDIs, and examined a third to determine whether a program addressing hospital-based exposures reduced the rate of CDI.Using data from the CDC’s Emerging Infections Program, 10,342 CDI cases from 111 hospitals were examined. Each case was classified as hospital onset (i.e. occurring three days after admission), nursing home onset, or community onset. A total of 94% of cases were associated with recent exposure to healthcare, 75% were classified as non-hospital onset, and 20% of hospital-onset cases were in patients who had recently been in a nursing home, suggesting that non-hospital-based healthcare exposures play a significant role. The second analysis used data from the National Healthcare Safety Network to examine 42,157 CDIs in 711 hospitals.
The authors found that 52% of CDIs were present on admission. The pooled rate of hospital-onset CDI was low (7.4 per 10,000 patient-days). The final analysis examined hospital-onset CDI rates across three hospital-based prevention programs over a period of nearly two years. The interventions were associated with a 20% decrease in CDI rates (to 7.5 from 9.3 per 10,000 patient days).
Bottom line: Nearly all CDIs are related to exposure in healthcare settings. Exposure to nursing home and ambulatory care seem to play a major role, and infection-control measures in addition to hospital-based strategies need to target these areas. Hospital-based interventions moderately decreased overall rates of CDI.
Citation: Centers for Disease Control and Prevention. Vital signs: preventing Clostridium difficile infections. MMWR Morb Mortal Wkly Rep. 2012;61:157-162.
In Suspected Acute Coronary Syndrome, CT Angiography Identifies Patients Safe for Discharge
Clinical question: Is a strategy utilizing CT angiography safe to allow discharge from the emergency department low- to intermediate-risk patients with possible acute coronary syndrome (ACS)?
Background: Admission rates for patients with possible acute coronary syndrome are high, but the majority of patients will not have cardiac causes of the symptoms. Coronary computed tomographic angiography (CCTA) has a high negative predictive value for the detection of coronary artery disease, but its utility in determining if a patient can be safely discharged from the emergency department has not been established.
Study design: Prospective, randomized, controlled, multicenter trial.
Setting: Five EDs in the U.S.; three included observation units.
Synopsis: The study enrolled 1,392 patients in a 2:1 ratio, with two-thirds undergoing CCTA and the other third treated with usual care (those admitted for possible ACS with a TIMI score of 0 to 2). Of 908 patients assigned to CCTA, 640 had a negative test, and none of them died or had a myocardial infarction within 30 days. Patients in the CCTA group were more likely than the group undergoing usual care to be discharged from the ED (49.6% vs. 22.7%), have a shorter length of stay (18 hours vs. 24.8 hours, P<.0001), and receive a coronary disease diagnosis.
Bottom line: In a randomized controlled trial, the use of CCTA to evaluate low- to intermediate-risk emergency department patients with possible ACS appears to be safe and effective, and leads to more discharges from the ED.
Citation: Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393-1403.
Impending Physiological Deterioration Can Be Predicted Using Data from a Comprehensive EHR
Clinical question: Can impending physiological deterioration be predicted in medical-surgical ward patients using data from a comprehensive electronic health record (EHR)?
Background: Unplanned ICU transfer is associated with increased mortality and morbidity. Previous studies have examined physiological variables and track-and-trigger systems that might help in the identification of ward patients who are at risk for deterioration and transfer to a higher level of care. More hospitals across the U.S. are using EHRs, and eventually all hospitals are expected to be using one. However, it is unclear if an EHR-based model can accurately predict patients’ clinical deterioration.
Study design: Retrospective case-control study; the unit of analysis was the “patient shift,” each defined by a particular 12-hour period and patient. A complex model to predict patient deterioration and transfer to the ICU was developed and validated using EHR data that was available prior to the deterioration shift.
Setting: Fourteen hospitals of the Northern California Kaiser Permanente Medical Care Program (an integrated healthcare delivery system) that have used an operational EHR for at least three months.
Synopsis: The study identified 4,036 patient-shifts during which a transfer to the ICU occurred, and compared these with 39,782 patient-shifts during which no transfer occurred. Variables in the model included patient demographic data, diagnoses, comorbidities, lab results, and vital signs. The EHR-based predictive model performed well at predicting clinical deterioration and transfer to the ICU (derivation c-statistic 0.84, validation c-statistic 0.77). The model performed best among patients with gastrointestinal diseases (c-statistic 0.84) and worst in patients with acute myocardial infarction (c-statistic 0.57).
Bottom line: Impending physiologic deterioration can be predicted using EHR-based models.
Citation: Escobar GJ, Laguardia JC, Turk BJ, et al. Early detection of impending physiologic deterioration among patients who are not in intensive care: Development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012:doi:10.1002/jhm.1929 [Epub ahead of print].
Rapid Influenza Diagnostic Tests Have Low Sensitivity and High Specificity
Clinical question: How accurate are rapid influenza diagnostic tests, and can they be used to guide further management?
Background: Three million to 5 million people a year develop influenza, which has a high mortality rate and potential global implications. The gold-standard diagnostic tests, PCR and viral culture, have a long turnaround time and are expensive. There have been limited systematic reviews addressing the accuracy of various rapid influenza diagnostic tests (RIDTs), especially in adults.
Study design: Systematic review and meta-analysis.
Setting: Varied.
Synopsis: Studies that compared commercial rapid influenza tests versus reference standards of PCR or viral culture were included. The 159 rapid tests were evaluated in 119 studies representing 26 different brands of commercial tests. Sixty-two of 119 studies included both adults and children, and 41 studies included children only. Overall, rapid influenza tests had a sensitivity of 62.3% and a specificity of 98.2%. There was a higher sensitivity for children than adults (67% vs. 54%) and a higher sensitivity for influenza A than influenza B (65% vs. 52%). The brand of rapid test made little difference. Most articles reviewed did not include a direct comparison between individual brands of RIDTs.
Bottom line: Rapid influenza diagnostic tests have low sensitivity and high specificity. A positive rapid test indicates likely influenza, but a negative test does not rule it out.
Citation: Chartrand C, Leeflang MM, Minion J, Brewer T, Pai M. Accuracy of rapid influenza diagnostic tests: a meta-analysis. Ann Intern Med. 2012;156:500-511.
Multifaceted QI Intervention Increases Adherence to Evidence-Based Therapy in Acute Coronary Syndrome
Clinical question: Does a multipronged approach to QI interventions improve the adherence to evidence-based therapies in acute coronary syndromes?
Background: Despite evidence-based recommendations for the use of antiplatelet medication, anticoagulants, beta-blockers, and statins in the setting of an acute coronary syndrome, adherence to these recommendations is poor, especially in low- to middle-income patients.
Study design: Cluster-randomized, prospective, blinded trial.
Setting: Thirty-six urban, public hospitals in Brazil.
Synopsis: Hospitals were randomly allocated to a multifaceted QI strategy versus routine practice. At each hospital, patients were enrolled in a consecutive manner when they presented to the emergency department with an acute coronary syndrome. The QI intervention included multiple modalities, including checklists in the ED, reminders, case management (by a trained RN) to ensure compliance, and educational materials to the staff (pocket algorithms and interactive web programs).
The primary endpoint was adherence to all available evidence-based therapies in the first 24 hours of management. Patients were more likely to receive all evidence-based therapies in hospitals that received the intervention (67.9% vs. 49.5%, P=0.01). The secondary endpoint (adherence at 24 hours and at discharge) was also significantly in favor of the intervention group (50.9% vs. 31.9%, P=0.03).
The findings might not be applicable to institutions with high adherence rates to evidence-based therapy.
Bottom line: A multifaceted QI intervention improves adherence to evidence-based therapies in urban hospitals in medium-income countries.
Citation: Berwanger O, Guimaraes HP, Lanranjeira LN, et al. Effect of a multifaceted intervention on use of evidence-based therapies in patients with acute coronary syndromes in Brazil: the BRIDGE-ACS randomized trial. JAMA. 2012 [Epub ahead of print].
Rivaroxaban for the Treatment of Acute Pulmonary Embolism
Clinical question: How does the efficacy and safety of rivaroxaban compare with low-molecular-weight heparin (LMWH) plus vitamin K antagonist (VKA) for treatment of acute pulmonary embolism (PE)?
Background: Data support the use of rivaroxaban for stroke prevention in atrial fibrillation, for VTE prophylaxis after orthopedic surgery, and for the treatment of acute coronary syndromes and acute deep vein thromboses. The EINSTEIN-PE investigators now study rivaroxaban for the treatment of acute symptomatic PE.
Study design: Randomized, open-label, noninferiority trial.
Setting: Two hundred sixty-three sites in 38 countries.
Synopsis: The investigators enrolled 4,832 patients with acute symptomatic PE (with or without DVT). Rivaroxaban alone was compared with standard therapy (enoxaparin followed by VKA to an international normalized ratio [INR] of 2 to 3) for three, six, or 12 months. The mean study duration was nine months. INR was in the therapeutic range 62.7% of the time.
The combined primary endpoint of fatal or nonfatal PE, or DVT, occurred in 2.1% in the rivaroxaban group and 1.8% in the standard-therapy group, meeting the pre-specified criteria for non-inferiority (HR 1.12; 95% CI: 0.75-1.68). There were no significant differences in the primary safety outcome of bleeding (HR, 0.90; 95% CI: 0.76-1.07). However, major bleeding events favored rivaroxaban, with events in 1.1% vs. 2.2% of those on VKA (HR 0.49, CI 0.31-0.79, P=0.003). Efficacy and safety of fixed-dose rivaroxaban did not vary by age, sex, weight, glomerular filtration rate, or extent of initial PE.
Bottom line: In patients with symptomatic acute PE, rivaroxaban is noninferior to standard treatment with LMWH plus VKA and might have a safety benefit of less major bleeding. Rivaroxaban and other new oral anticoagulants are likely to be used more frequently as more data is accumulated, but at this time, the guidelines continue to recommend VKA and LMWH as first-line agents.
Citation: The EINSTEIN-PE Investigators, Büller HR, Prins MH, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287-1297.
Coronary Stent Implantation Provides No Additional Benefit when Compared with Medical Therapy Alone in Patients with Stable Coronary Artery Disease
Clinical question: Does stent implantation lead to better outcomes when compared to medical therapy in patients with stable coronary artery disease (CAD)?
Background: It is unclear whether stent implantation improves outcomes any more than medical therapy in patients with stable CAD. This is a meta-analysis of trials comparing outcomes of coronary stent implantation with optimal medical therapy.
Study design: Meta-analysis of eight prospective randomized nonblinded trials comparing stent implantation plus medical therapy to medical therapy alone in patients with stable CAD. Outcomes of death, nonfatal myocardial infarction, unplanned revascularization, and persistent angina were compared between the two groups.
Setting: Varied.
Synopsis: Eight trials with 7,229 patients were included with an average follow-up of 4.3 years. In a pooled analysis, coronary stenting versus medical therapy was associated with similar risk of death (8.9% vs. 9.1% P=0.83); nonfatal myocardial infarction (8.9% vs. 8.1%, P=0.22); and persistent angina (29% vs. 33%, P=0.10). Coronary stenting was associated with decreased risk of unplanned revascularization, but the difference was not significant (21.4% vs. 30.7%, P=0.11).
Bottom line: In stable CAD, coronary stent implantation provides no additional benefit when compared to medical therapy.
Citation: Stergiopoulos K, Brown DL. Initial coronary stent implantation with medical therapy vs. medical therapy alone for stable coronary artery disease: meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172:312-319.
Prolonged Versus Standard Duration Venous Thromboprophylaxis after Major Orthopedic Surgery
Clinical question: Should patients with hip or knee surgery receive venous thromboprophylaxis (VTE) prophylaxis for seven to 10 days post-operatively or for 21 days or more?
Background: Venous thromboembolism is the most frequent medical complication of knee and hip surgeries. Routine prophylaxis is recommended for minimum of seven to 10 days, but a longer duration might be more beneficial.
Study design: Systemic review and meta-analysis of eight randomized, controlled trials comparing different duration of VTE prophylaxis after hip fracture surgery and total hip or knee replacement.
Setting: Varied.
Synopsis: Eight trials with 2,917 patients met inclusion criteria. Pharmacological agents used for VTE prophylaxis in these trials were coumadin, enoxaparin, dalteparin, and fondaparinux. In patients with hip replacement, undergoing VTE prophylaxis for ≥21 days (compared with seven to 10 days) was associated with a decreased risk of pulmonary embolism (odds ratio [OR] 0.14, 95% CI 0.04-0.47), symptomatic DVTs (OR 0.36, 95% CI 0.16-0.81), asymptomatic DVTs (OR 0.48, 95% CI 0.31-0.75), and proximal DVTs (RR 0.29, CI 0.16-0.52). Prophylaxis for ≥21 days was also associated with an increased risk of minor bleeding (OR 7.55, 95% CI 1.51-37.64).
Data were not sufficient for evaluation of prolonged prophylaxis for total knee replacement and hip fracture surgery.
Bottom line: Prolonged prophylaxis is associated with fewer VTE events in patients with hip replacement but also carries increased risk of minor bleeding.
Citation: Sobieraj DM, Lee S, Coleman CI, et al. Prolonged versus standard-duration venous thromboprophylaxis in major orthopedic surgery: a systematic review. Ann Intern Med. 2012 May 15 [Epub ahead of print].
In This Edition
Literature At A Glance
A guide to this month’s studies
- Nearly all CDIs Related to Exposure in Healthcare Setting
- In Suspected Acute Coronary Syndrome, CT Angiography Identifies Patients Safe for Discharge
- Impending Physiological Deterioration Can Be Predicted Using Data from a Comprehensive EHR
- Rapid Influenza Diagnostic Tests Have Low Sensitivity and High Specificity
- Multifaceted QI Intervention Increases Adherence to Evidence-Based Therapy in Acute Coronary Syndrome
- Rivaroxaban for the Treatment of Acute Pulmonary Embolism
- Coronary Stent Implantation Provides No Additional Benefit when Compared with Medical Therapy Alone in Patients with Stable Coronary Artery Disease
- Prolonged Versus Standard Duration Venous Thromboprophylaxis after Major Orthopedic Surgery
Nearly all CDIs Related to Exposure in Healthcare Setting
Clinical question: What is the contribution of non-hospital healthcare exposures to the burden of Clostridium difficile infection (CDI)?
Background: CDI is common among hospitalized patients and is associated with high rates of morbidity. Most CDI prevention programs are aimed at hospital-based risk factors. However, non-hospital healthcare exposures might contribute significantly to the burden of CDI, and hospital-based prevention programs might not address these risks.
Study design: Retrospective analysis of three population-based data sets.
Setting: Three population data sets tracking infections on a national and state level in the U.S.
Synopsis: This study analyzed two data sets to determine the contribution of non-hospital healthcare exposure to CDIs, and examined a third to determine whether a program addressing hospital-based exposures reduced the rate of CDI.Using data from the CDC’s Emerging Infections Program, 10,342 CDI cases from 111 hospitals were examined. Each case was classified as hospital onset (i.e. occurring three days after admission), nursing home onset, or community onset. A total of 94% of cases were associated with recent exposure to healthcare, 75% were classified as non-hospital onset, and 20% of hospital-onset cases were in patients who had recently been in a nursing home, suggesting that non-hospital-based healthcare exposures play a significant role. The second analysis used data from the National Healthcare Safety Network to examine 42,157 CDIs in 711 hospitals.
The authors found that 52% of CDIs were present on admission. The pooled rate of hospital-onset CDI was low (7.4 per 10,000 patient-days). The final analysis examined hospital-onset CDI rates across three hospital-based prevention programs over a period of nearly two years. The interventions were associated with a 20% decrease in CDI rates (to 7.5 from 9.3 per 10,000 patient days).
Bottom line: Nearly all CDIs are related to exposure in healthcare settings. Exposure to nursing home and ambulatory care seem to play a major role, and infection-control measures in addition to hospital-based strategies need to target these areas. Hospital-based interventions moderately decreased overall rates of CDI.
Citation: Centers for Disease Control and Prevention. Vital signs: preventing Clostridium difficile infections. MMWR Morb Mortal Wkly Rep. 2012;61:157-162.
In Suspected Acute Coronary Syndrome, CT Angiography Identifies Patients Safe for Discharge
Clinical question: Is a strategy utilizing CT angiography safe to allow discharge from the emergency department low- to intermediate-risk patients with possible acute coronary syndrome (ACS)?
Background: Admission rates for patients with possible acute coronary syndrome are high, but the majority of patients will not have cardiac causes of the symptoms. Coronary computed tomographic angiography (CCTA) has a high negative predictive value for the detection of coronary artery disease, but its utility in determining if a patient can be safely discharged from the emergency department has not been established.
Study design: Prospective, randomized, controlled, multicenter trial.
Setting: Five EDs in the U.S.; three included observation units.
Synopsis: The study enrolled 1,392 patients in a 2:1 ratio, with two-thirds undergoing CCTA and the other third treated with usual care (those admitted for possible ACS with a TIMI score of 0 to 2). Of 908 patients assigned to CCTA, 640 had a negative test, and none of them died or had a myocardial infarction within 30 days. Patients in the CCTA group were more likely than the group undergoing usual care to be discharged from the ED (49.6% vs. 22.7%), have a shorter length of stay (18 hours vs. 24.8 hours, P<.0001), and receive a coronary disease diagnosis.
Bottom line: In a randomized controlled trial, the use of CCTA to evaluate low- to intermediate-risk emergency department patients with possible ACS appears to be safe and effective, and leads to more discharges from the ED.
Citation: Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393-1403.
Impending Physiological Deterioration Can Be Predicted Using Data from a Comprehensive EHR
Clinical question: Can impending physiological deterioration be predicted in medical-surgical ward patients using data from a comprehensive electronic health record (EHR)?
Background: Unplanned ICU transfer is associated with increased mortality and morbidity. Previous studies have examined physiological variables and track-and-trigger systems that might help in the identification of ward patients who are at risk for deterioration and transfer to a higher level of care. More hospitals across the U.S. are using EHRs, and eventually all hospitals are expected to be using one. However, it is unclear if an EHR-based model can accurately predict patients’ clinical deterioration.
Study design: Retrospective case-control study; the unit of analysis was the “patient shift,” each defined by a particular 12-hour period and patient. A complex model to predict patient deterioration and transfer to the ICU was developed and validated using EHR data that was available prior to the deterioration shift.
Setting: Fourteen hospitals of the Northern California Kaiser Permanente Medical Care Program (an integrated healthcare delivery system) that have used an operational EHR for at least three months.
Synopsis: The study identified 4,036 patient-shifts during which a transfer to the ICU occurred, and compared these with 39,782 patient-shifts during which no transfer occurred. Variables in the model included patient demographic data, diagnoses, comorbidities, lab results, and vital signs. The EHR-based predictive model performed well at predicting clinical deterioration and transfer to the ICU (derivation c-statistic 0.84, validation c-statistic 0.77). The model performed best among patients with gastrointestinal diseases (c-statistic 0.84) and worst in patients with acute myocardial infarction (c-statistic 0.57).
Bottom line: Impending physiologic deterioration can be predicted using EHR-based models.
Citation: Escobar GJ, Laguardia JC, Turk BJ, et al. Early detection of impending physiologic deterioration among patients who are not in intensive care: Development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012:doi:10.1002/jhm.1929 [Epub ahead of print].
Rapid Influenza Diagnostic Tests Have Low Sensitivity and High Specificity
Clinical question: How accurate are rapid influenza diagnostic tests, and can they be used to guide further management?
Background: Three million to 5 million people a year develop influenza, which has a high mortality rate and potential global implications. The gold-standard diagnostic tests, PCR and viral culture, have a long turnaround time and are expensive. There have been limited systematic reviews addressing the accuracy of various rapid influenza diagnostic tests (RIDTs), especially in adults.
Study design: Systematic review and meta-analysis.
Setting: Varied.
Synopsis: Studies that compared commercial rapid influenza tests versus reference standards of PCR or viral culture were included. The 159 rapid tests were evaluated in 119 studies representing 26 different brands of commercial tests. Sixty-two of 119 studies included both adults and children, and 41 studies included children only. Overall, rapid influenza tests had a sensitivity of 62.3% and a specificity of 98.2%. There was a higher sensitivity for children than adults (67% vs. 54%) and a higher sensitivity for influenza A than influenza B (65% vs. 52%). The brand of rapid test made little difference. Most articles reviewed did not include a direct comparison between individual brands of RIDTs.
Bottom line: Rapid influenza diagnostic tests have low sensitivity and high specificity. A positive rapid test indicates likely influenza, but a negative test does not rule it out.
Citation: Chartrand C, Leeflang MM, Minion J, Brewer T, Pai M. Accuracy of rapid influenza diagnostic tests: a meta-analysis. Ann Intern Med. 2012;156:500-511.
Multifaceted QI Intervention Increases Adherence to Evidence-Based Therapy in Acute Coronary Syndrome
Clinical question: Does a multipronged approach to QI interventions improve the adherence to evidence-based therapies in acute coronary syndromes?
Background: Despite evidence-based recommendations for the use of antiplatelet medication, anticoagulants, beta-blockers, and statins in the setting of an acute coronary syndrome, adherence to these recommendations is poor, especially in low- to middle-income patients.
Study design: Cluster-randomized, prospective, blinded trial.
Setting: Thirty-six urban, public hospitals in Brazil.
Synopsis: Hospitals were randomly allocated to a multifaceted QI strategy versus routine practice. At each hospital, patients were enrolled in a consecutive manner when they presented to the emergency department with an acute coronary syndrome. The QI intervention included multiple modalities, including checklists in the ED, reminders, case management (by a trained RN) to ensure compliance, and educational materials to the staff (pocket algorithms and interactive web programs).
The primary endpoint was adherence to all available evidence-based therapies in the first 24 hours of management. Patients were more likely to receive all evidence-based therapies in hospitals that received the intervention (67.9% vs. 49.5%, P=0.01). The secondary endpoint (adherence at 24 hours and at discharge) was also significantly in favor of the intervention group (50.9% vs. 31.9%, P=0.03).
The findings might not be applicable to institutions with high adherence rates to evidence-based therapy.
Bottom line: A multifaceted QI intervention improves adherence to evidence-based therapies in urban hospitals in medium-income countries.
Citation: Berwanger O, Guimaraes HP, Lanranjeira LN, et al. Effect of a multifaceted intervention on use of evidence-based therapies in patients with acute coronary syndromes in Brazil: the BRIDGE-ACS randomized trial. JAMA. 2012 [Epub ahead of print].
Rivaroxaban for the Treatment of Acute Pulmonary Embolism
Clinical question: How does the efficacy and safety of rivaroxaban compare with low-molecular-weight heparin (LMWH) plus vitamin K antagonist (VKA) for treatment of acute pulmonary embolism (PE)?
Background: Data support the use of rivaroxaban for stroke prevention in atrial fibrillation, for VTE prophylaxis after orthopedic surgery, and for the treatment of acute coronary syndromes and acute deep vein thromboses. The EINSTEIN-PE investigators now study rivaroxaban for the treatment of acute symptomatic PE.
Study design: Randomized, open-label, noninferiority trial.
Setting: Two hundred sixty-three sites in 38 countries.
Synopsis: The investigators enrolled 4,832 patients with acute symptomatic PE (with or without DVT). Rivaroxaban alone was compared with standard therapy (enoxaparin followed by VKA to an international normalized ratio [INR] of 2 to 3) for three, six, or 12 months. The mean study duration was nine months. INR was in the therapeutic range 62.7% of the time.
The combined primary endpoint of fatal or nonfatal PE, or DVT, occurred in 2.1% in the rivaroxaban group and 1.8% in the standard-therapy group, meeting the pre-specified criteria for non-inferiority (HR 1.12; 95% CI: 0.75-1.68). There were no significant differences in the primary safety outcome of bleeding (HR, 0.90; 95% CI: 0.76-1.07). However, major bleeding events favored rivaroxaban, with events in 1.1% vs. 2.2% of those on VKA (HR 0.49, CI 0.31-0.79, P=0.003). Efficacy and safety of fixed-dose rivaroxaban did not vary by age, sex, weight, glomerular filtration rate, or extent of initial PE.
Bottom line: In patients with symptomatic acute PE, rivaroxaban is noninferior to standard treatment with LMWH plus VKA and might have a safety benefit of less major bleeding. Rivaroxaban and other new oral anticoagulants are likely to be used more frequently as more data is accumulated, but at this time, the guidelines continue to recommend VKA and LMWH as first-line agents.
Citation: The EINSTEIN-PE Investigators, Büller HR, Prins MH, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287-1297.
Coronary Stent Implantation Provides No Additional Benefit when Compared with Medical Therapy Alone in Patients with Stable Coronary Artery Disease
Clinical question: Does stent implantation lead to better outcomes when compared to medical therapy in patients with stable coronary artery disease (CAD)?
Background: It is unclear whether stent implantation improves outcomes any more than medical therapy in patients with stable CAD. This is a meta-analysis of trials comparing outcomes of coronary stent implantation with optimal medical therapy.
Study design: Meta-analysis of eight prospective randomized nonblinded trials comparing stent implantation plus medical therapy to medical therapy alone in patients with stable CAD. Outcomes of death, nonfatal myocardial infarction, unplanned revascularization, and persistent angina were compared between the two groups.
Setting: Varied.
Synopsis: Eight trials with 7,229 patients were included with an average follow-up of 4.3 years. In a pooled analysis, coronary stenting versus medical therapy was associated with similar risk of death (8.9% vs. 9.1% P=0.83); nonfatal myocardial infarction (8.9% vs. 8.1%, P=0.22); and persistent angina (29% vs. 33%, P=0.10). Coronary stenting was associated with decreased risk of unplanned revascularization, but the difference was not significant (21.4% vs. 30.7%, P=0.11).
Bottom line: In stable CAD, coronary stent implantation provides no additional benefit when compared to medical therapy.
Citation: Stergiopoulos K, Brown DL. Initial coronary stent implantation with medical therapy vs. medical therapy alone for stable coronary artery disease: meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172:312-319.
Prolonged Versus Standard Duration Venous Thromboprophylaxis after Major Orthopedic Surgery
Clinical question: Should patients with hip or knee surgery receive venous thromboprophylaxis (VTE) prophylaxis for seven to 10 days post-operatively or for 21 days or more?
Background: Venous thromboembolism is the most frequent medical complication of knee and hip surgeries. Routine prophylaxis is recommended for minimum of seven to 10 days, but a longer duration might be more beneficial.
Study design: Systemic review and meta-analysis of eight randomized, controlled trials comparing different duration of VTE prophylaxis after hip fracture surgery and total hip or knee replacement.
Setting: Varied.
Synopsis: Eight trials with 2,917 patients met inclusion criteria. Pharmacological agents used for VTE prophylaxis in these trials were coumadin, enoxaparin, dalteparin, and fondaparinux. In patients with hip replacement, undergoing VTE prophylaxis for ≥21 days (compared with seven to 10 days) was associated with a decreased risk of pulmonary embolism (odds ratio [OR] 0.14, 95% CI 0.04-0.47), symptomatic DVTs (OR 0.36, 95% CI 0.16-0.81), asymptomatic DVTs (OR 0.48, 95% CI 0.31-0.75), and proximal DVTs (RR 0.29, CI 0.16-0.52). Prophylaxis for ≥21 days was also associated with an increased risk of minor bleeding (OR 7.55, 95% CI 1.51-37.64).
Data were not sufficient for evaluation of prolonged prophylaxis for total knee replacement and hip fracture surgery.
Bottom line: Prolonged prophylaxis is associated with fewer VTE events in patients with hip replacement but also carries increased risk of minor bleeding.
Citation: Sobieraj DM, Lee S, Coleman CI, et al. Prolonged versus standard-duration venous thromboprophylaxis in major orthopedic surgery: a systematic review. Ann Intern Med. 2012 May 15 [Epub ahead of print].
In This Edition
Literature At A Glance
A guide to this month’s studies
- Nearly all CDIs Related to Exposure in Healthcare Setting
- In Suspected Acute Coronary Syndrome, CT Angiography Identifies Patients Safe for Discharge
- Impending Physiological Deterioration Can Be Predicted Using Data from a Comprehensive EHR
- Rapid Influenza Diagnostic Tests Have Low Sensitivity and High Specificity
- Multifaceted QI Intervention Increases Adherence to Evidence-Based Therapy in Acute Coronary Syndrome
- Rivaroxaban for the Treatment of Acute Pulmonary Embolism
- Coronary Stent Implantation Provides No Additional Benefit when Compared with Medical Therapy Alone in Patients with Stable Coronary Artery Disease
- Prolonged Versus Standard Duration Venous Thromboprophylaxis after Major Orthopedic Surgery
Nearly all CDIs Related to Exposure in Healthcare Setting
Clinical question: What is the contribution of non-hospital healthcare exposures to the burden of Clostridium difficile infection (CDI)?
Background: CDI is common among hospitalized patients and is associated with high rates of morbidity. Most CDI prevention programs are aimed at hospital-based risk factors. However, non-hospital healthcare exposures might contribute significantly to the burden of CDI, and hospital-based prevention programs might not address these risks.
Study design: Retrospective analysis of three population-based data sets.
Setting: Three population data sets tracking infections on a national and state level in the U.S.
Synopsis: This study analyzed two data sets to determine the contribution of non-hospital healthcare exposure to CDIs, and examined a third to determine whether a program addressing hospital-based exposures reduced the rate of CDI.Using data from the CDC’s Emerging Infections Program, 10,342 CDI cases from 111 hospitals were examined. Each case was classified as hospital onset (i.e. occurring three days after admission), nursing home onset, or community onset. A total of 94% of cases were associated with recent exposure to healthcare, 75% were classified as non-hospital onset, and 20% of hospital-onset cases were in patients who had recently been in a nursing home, suggesting that non-hospital-based healthcare exposures play a significant role. The second analysis used data from the National Healthcare Safety Network to examine 42,157 CDIs in 711 hospitals.
The authors found that 52% of CDIs were present on admission. The pooled rate of hospital-onset CDI was low (7.4 per 10,000 patient-days). The final analysis examined hospital-onset CDI rates across three hospital-based prevention programs over a period of nearly two years. The interventions were associated with a 20% decrease in CDI rates (to 7.5 from 9.3 per 10,000 patient days).
Bottom line: Nearly all CDIs are related to exposure in healthcare settings. Exposure to nursing home and ambulatory care seem to play a major role, and infection-control measures in addition to hospital-based strategies need to target these areas. Hospital-based interventions moderately decreased overall rates of CDI.
Citation: Centers for Disease Control and Prevention. Vital signs: preventing Clostridium difficile infections. MMWR Morb Mortal Wkly Rep. 2012;61:157-162.
In Suspected Acute Coronary Syndrome, CT Angiography Identifies Patients Safe for Discharge
Clinical question: Is a strategy utilizing CT angiography safe to allow discharge from the emergency department low- to intermediate-risk patients with possible acute coronary syndrome (ACS)?
Background: Admission rates for patients with possible acute coronary syndrome are high, but the majority of patients will not have cardiac causes of the symptoms. Coronary computed tomographic angiography (CCTA) has a high negative predictive value for the detection of coronary artery disease, but its utility in determining if a patient can be safely discharged from the emergency department has not been established.
Study design: Prospective, randomized, controlled, multicenter trial.
Setting: Five EDs in the U.S.; three included observation units.
Synopsis: The study enrolled 1,392 patients in a 2:1 ratio, with two-thirds undergoing CCTA and the other third treated with usual care (those admitted for possible ACS with a TIMI score of 0 to 2). Of 908 patients assigned to CCTA, 640 had a negative test, and none of them died or had a myocardial infarction within 30 days. Patients in the CCTA group were more likely than the group undergoing usual care to be discharged from the ED (49.6% vs. 22.7%), have a shorter length of stay (18 hours vs. 24.8 hours, P<.0001), and receive a coronary disease diagnosis.
Bottom line: In a randomized controlled trial, the use of CCTA to evaluate low- to intermediate-risk emergency department patients with possible ACS appears to be safe and effective, and leads to more discharges from the ED.
Citation: Litt HI, Gatsonis C, Snyder B, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med. 2012;366:1393-1403.
Impending Physiological Deterioration Can Be Predicted Using Data from a Comprehensive EHR
Clinical question: Can impending physiological deterioration be predicted in medical-surgical ward patients using data from a comprehensive electronic health record (EHR)?
Background: Unplanned ICU transfer is associated with increased mortality and morbidity. Previous studies have examined physiological variables and track-and-trigger systems that might help in the identification of ward patients who are at risk for deterioration and transfer to a higher level of care. More hospitals across the U.S. are using EHRs, and eventually all hospitals are expected to be using one. However, it is unclear if an EHR-based model can accurately predict patients’ clinical deterioration.
Study design: Retrospective case-control study; the unit of analysis was the “patient shift,” each defined by a particular 12-hour period and patient. A complex model to predict patient deterioration and transfer to the ICU was developed and validated using EHR data that was available prior to the deterioration shift.
Setting: Fourteen hospitals of the Northern California Kaiser Permanente Medical Care Program (an integrated healthcare delivery system) that have used an operational EHR for at least three months.
Synopsis: The study identified 4,036 patient-shifts during which a transfer to the ICU occurred, and compared these with 39,782 patient-shifts during which no transfer occurred. Variables in the model included patient demographic data, diagnoses, comorbidities, lab results, and vital signs. The EHR-based predictive model performed well at predicting clinical deterioration and transfer to the ICU (derivation c-statistic 0.84, validation c-statistic 0.77). The model performed best among patients with gastrointestinal diseases (c-statistic 0.84) and worst in patients with acute myocardial infarction (c-statistic 0.57).
Bottom line: Impending physiologic deterioration can be predicted using EHR-based models.
Citation: Escobar GJ, Laguardia JC, Turk BJ, et al. Early detection of impending physiologic deterioration among patients who are not in intensive care: Development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012:doi:10.1002/jhm.1929 [Epub ahead of print].
Rapid Influenza Diagnostic Tests Have Low Sensitivity and High Specificity
Clinical question: How accurate are rapid influenza diagnostic tests, and can they be used to guide further management?
Background: Three million to 5 million people a year develop influenza, which has a high mortality rate and potential global implications. The gold-standard diagnostic tests, PCR and viral culture, have a long turnaround time and are expensive. There have been limited systematic reviews addressing the accuracy of various rapid influenza diagnostic tests (RIDTs), especially in adults.
Study design: Systematic review and meta-analysis.
Setting: Varied.
Synopsis: Studies that compared commercial rapid influenza tests versus reference standards of PCR or viral culture were included. The 159 rapid tests were evaluated in 119 studies representing 26 different brands of commercial tests. Sixty-two of 119 studies included both adults and children, and 41 studies included children only. Overall, rapid influenza tests had a sensitivity of 62.3% and a specificity of 98.2%. There was a higher sensitivity for children than adults (67% vs. 54%) and a higher sensitivity for influenza A than influenza B (65% vs. 52%). The brand of rapid test made little difference. Most articles reviewed did not include a direct comparison between individual brands of RIDTs.
Bottom line: Rapid influenza diagnostic tests have low sensitivity and high specificity. A positive rapid test indicates likely influenza, but a negative test does not rule it out.
Citation: Chartrand C, Leeflang MM, Minion J, Brewer T, Pai M. Accuracy of rapid influenza diagnostic tests: a meta-analysis. Ann Intern Med. 2012;156:500-511.
Multifaceted QI Intervention Increases Adherence to Evidence-Based Therapy in Acute Coronary Syndrome
Clinical question: Does a multipronged approach to QI interventions improve the adherence to evidence-based therapies in acute coronary syndromes?
Background: Despite evidence-based recommendations for the use of antiplatelet medication, anticoagulants, beta-blockers, and statins in the setting of an acute coronary syndrome, adherence to these recommendations is poor, especially in low- to middle-income patients.
Study design: Cluster-randomized, prospective, blinded trial.
Setting: Thirty-six urban, public hospitals in Brazil.
Synopsis: Hospitals were randomly allocated to a multifaceted QI strategy versus routine practice. At each hospital, patients were enrolled in a consecutive manner when they presented to the emergency department with an acute coronary syndrome. The QI intervention included multiple modalities, including checklists in the ED, reminders, case management (by a trained RN) to ensure compliance, and educational materials to the staff (pocket algorithms and interactive web programs).
The primary endpoint was adherence to all available evidence-based therapies in the first 24 hours of management. Patients were more likely to receive all evidence-based therapies in hospitals that received the intervention (67.9% vs. 49.5%, P=0.01). The secondary endpoint (adherence at 24 hours and at discharge) was also significantly in favor of the intervention group (50.9% vs. 31.9%, P=0.03).
The findings might not be applicable to institutions with high adherence rates to evidence-based therapy.
Bottom line: A multifaceted QI intervention improves adherence to evidence-based therapies in urban hospitals in medium-income countries.
Citation: Berwanger O, Guimaraes HP, Lanranjeira LN, et al. Effect of a multifaceted intervention on use of evidence-based therapies in patients with acute coronary syndromes in Brazil: the BRIDGE-ACS randomized trial. JAMA. 2012 [Epub ahead of print].
Rivaroxaban for the Treatment of Acute Pulmonary Embolism
Clinical question: How does the efficacy and safety of rivaroxaban compare with low-molecular-weight heparin (LMWH) plus vitamin K antagonist (VKA) for treatment of acute pulmonary embolism (PE)?
Background: Data support the use of rivaroxaban for stroke prevention in atrial fibrillation, for VTE prophylaxis after orthopedic surgery, and for the treatment of acute coronary syndromes and acute deep vein thromboses. The EINSTEIN-PE investigators now study rivaroxaban for the treatment of acute symptomatic PE.
Study design: Randomized, open-label, noninferiority trial.
Setting: Two hundred sixty-three sites in 38 countries.
Synopsis: The investigators enrolled 4,832 patients with acute symptomatic PE (with or without DVT). Rivaroxaban alone was compared with standard therapy (enoxaparin followed by VKA to an international normalized ratio [INR] of 2 to 3) for three, six, or 12 months. The mean study duration was nine months. INR was in the therapeutic range 62.7% of the time.
The combined primary endpoint of fatal or nonfatal PE, or DVT, occurred in 2.1% in the rivaroxaban group and 1.8% in the standard-therapy group, meeting the pre-specified criteria for non-inferiority (HR 1.12; 95% CI: 0.75-1.68). There were no significant differences in the primary safety outcome of bleeding (HR, 0.90; 95% CI: 0.76-1.07). However, major bleeding events favored rivaroxaban, with events in 1.1% vs. 2.2% of those on VKA (HR 0.49, CI 0.31-0.79, P=0.003). Efficacy and safety of fixed-dose rivaroxaban did not vary by age, sex, weight, glomerular filtration rate, or extent of initial PE.
Bottom line: In patients with symptomatic acute PE, rivaroxaban is noninferior to standard treatment with LMWH plus VKA and might have a safety benefit of less major bleeding. Rivaroxaban and other new oral anticoagulants are likely to be used more frequently as more data is accumulated, but at this time, the guidelines continue to recommend VKA and LMWH as first-line agents.
Citation: The EINSTEIN-PE Investigators, Büller HR, Prins MH, et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287-1297.
Coronary Stent Implantation Provides No Additional Benefit when Compared with Medical Therapy Alone in Patients with Stable Coronary Artery Disease
Clinical question: Does stent implantation lead to better outcomes when compared to medical therapy in patients with stable coronary artery disease (CAD)?
Background: It is unclear whether stent implantation improves outcomes any more than medical therapy in patients with stable CAD. This is a meta-analysis of trials comparing outcomes of coronary stent implantation with optimal medical therapy.
Study design: Meta-analysis of eight prospective randomized nonblinded trials comparing stent implantation plus medical therapy to medical therapy alone in patients with stable CAD. Outcomes of death, nonfatal myocardial infarction, unplanned revascularization, and persistent angina were compared between the two groups.
Setting: Varied.
Synopsis: Eight trials with 7,229 patients were included with an average follow-up of 4.3 years. In a pooled analysis, coronary stenting versus medical therapy was associated with similar risk of death (8.9% vs. 9.1% P=0.83); nonfatal myocardial infarction (8.9% vs. 8.1%, P=0.22); and persistent angina (29% vs. 33%, P=0.10). Coronary stenting was associated with decreased risk of unplanned revascularization, but the difference was not significant (21.4% vs. 30.7%, P=0.11).
Bottom line: In stable CAD, coronary stent implantation provides no additional benefit when compared to medical therapy.
Citation: Stergiopoulos K, Brown DL. Initial coronary stent implantation with medical therapy vs. medical therapy alone for stable coronary artery disease: meta-analysis of randomized controlled trials. Arch Intern Med. 2012;172:312-319.
Prolonged Versus Standard Duration Venous Thromboprophylaxis after Major Orthopedic Surgery
Clinical question: Should patients with hip or knee surgery receive venous thromboprophylaxis (VTE) prophylaxis for seven to 10 days post-operatively or for 21 days or more?
Background: Venous thromboembolism is the most frequent medical complication of knee and hip surgeries. Routine prophylaxis is recommended for minimum of seven to 10 days, but a longer duration might be more beneficial.
Study design: Systemic review and meta-analysis of eight randomized, controlled trials comparing different duration of VTE prophylaxis after hip fracture surgery and total hip or knee replacement.
Setting: Varied.
Synopsis: Eight trials with 2,917 patients met inclusion criteria. Pharmacological agents used for VTE prophylaxis in these trials were coumadin, enoxaparin, dalteparin, and fondaparinux. In patients with hip replacement, undergoing VTE prophylaxis for ≥21 days (compared with seven to 10 days) was associated with a decreased risk of pulmonary embolism (odds ratio [OR] 0.14, 95% CI 0.04-0.47), symptomatic DVTs (OR 0.36, 95% CI 0.16-0.81), asymptomatic DVTs (OR 0.48, 95% CI 0.31-0.75), and proximal DVTs (RR 0.29, CI 0.16-0.52). Prophylaxis for ≥21 days was also associated with an increased risk of minor bleeding (OR 7.55, 95% CI 1.51-37.64).
Data were not sufficient for evaluation of prolonged prophylaxis for total knee replacement and hip fracture surgery.
Bottom line: Prolonged prophylaxis is associated with fewer VTE events in patients with hip replacement but also carries increased risk of minor bleeding.
Citation: Sobieraj DM, Lee S, Coleman CI, et al. Prolonged versus standard-duration venous thromboprophylaxis in major orthopedic surgery: a systematic review. Ann Intern Med. 2012 May 15 [Epub ahead of print].