User login
DIAGNOSTIC CHALLENGES: Differentiating Nighttime GERD
- Reflux episodes with nighttime GERD occur less frequently but are more prolonged than those with daytime GERD. (SOR: B)
- Esophageal complications are generally more severe and nonesophageal complications more common in nighttime than in daytime GERD. (SOR: B)
- Nighttime GERD-induced alterations in sleep cause significant patient morbidity and reduced quality of life and productivity. (SOR: B)
- Several factors are associated with nighttime GERD, including increased body mass index, carbonated soft drink consumption, hypertension, benzodiazepine use, obstructive sleep apnea, and asthma. (SOR: B)
- The history and physical examination generally provide the most useful information in making the diagnosis. (SOR: C)
- Sleep-induced physiologic alterations are thought to be important factors responsible for the more common and severe symptoms and complications in nighttime vs daytime GERD. (SOR: C)
Prevalence estimates for gastroesophageal reflux disease (GERD) range from 8% to 40%, depending on the definition and diagnostic criteria.1-4 While heartburn and regurgitation are considered the hallmark symptoms, GERD actually represents a spectrum of disorders that generally result from transient relaxations of the lower esophageal sphincter (LES), so that gastric refluxate comes into contact with the esophageal epithelium. Additionally, differences in rates of acid secretion and clearance and the time since food ingestion affect symptoms, potentially leading to differing presentations of GERD associated with daytime and nocturnal episodes. To facilitate accurate diagnosis of GERD, it may be helpful for clinicians to distinguish between the symptoms that occur during the day or in an upright position and those that occur at night or when a person is supine.4 This paper reviews the differences in symptoms and explains the pathophysiologic mechanisms involved.
Issues of GERD and quality of life
Patients’ quality of life and ability to function is negatively impacted by factors associated specifically with nocturnal episodes of GERD. Patients who experience GERD primarily at night may complain of sleep disturbances. Symptoms associated with nighttime GERD generally are more severe,5 and the complications more diverse and frequent,4 due to the prolonged length of nighttime reflux.6 For these reasons, determining if the underlying cause of a group of symptoms is nighttime episodes of GERD is an important treatment step.
Complications of reflux: associations with nighttime occurrences
Esophageal complications of GERD include erosive esophagitis, esophageal hemorrhage, ulceration, and strictures and appear to be more severe in patients with nighttime episodes of GERD than in those complaining of daytime reflux. An early study showed that patients who experience reflux only in the supine position have a higher incidence of esophagitis compared with patients who only refluxed in an upright position.7 Prolonged acid contact time increases the risk that esophagitis will become erosive. This was demonstrated in a study that concluded particularly that the presence of nocturnal reflux events lasting more than 5 minutes was a powerful predictor of erosive damage.6
Overall, approximately 7% to 12% of patients with chronic GERD develop Barrett’s esophagus compared with fewer than 1% of those in the general population.8 Potentially, more severe nocturnal symptoms may be among the factors that increase the risk of Barrett’s esophagus.9,10 Esophageal adenocarcinoma also is more likely in patients with nocturnal episodes of GERD: In a national, population-based, case-controlled trial, an 11-fold increased risk for esophageal adenocarcinoma was reported in patients who experienced once-weekly episodes of nighttime heartburn, regurgitation, or both. Overall, an 8-fold increased risk of esophageal adenocarcinoma was observed in all patients with GERD.11
Impact of nighttime episodes on sleep
Not surprisingly, sleep is significantly affected by nighttime GERD episodes. A recent Internet-based survey of full-time working adults in the United States identified 1002 patients with symptomatic GERD.12 Using the validated GERD Symptom and Medication Questionnaire, symptomatic GERD was defined as a score of 10 or greater for at least one episode of heartburn or acid regurgitation within the past 7 days. Symptomatic nighttime GERD was defined as at least 2 nights with symptoms during the past 7 days. GERD-related sleep problems were twice as frequent in patients with nighttime compared with daytime GERD. Patients with nighttime episodes of GERD experienced GERD-related sleep impairment an average of 1.6 to 1.9 nights per week compared with 0.3 to 0.4 nights per week for the daytime GERD group.
In both groups, the most commonly reported sleep problem was awakening due to symptoms (75% vs 37%, respectively). Sixty-five percent of nighttime and 28% of daytime GERD patients indicated that GERD symptoms prevented them from feeling rested in the morning.12 In addition, respondents with nighttime GERD experienced an additional 2.7 hours per week of lost work productivity when compared to those with daytime GERD.13 A similar survey also found that in those with nighttime GERD, the number of nights with sleep interference was associated with reduced work productivity.14
These results are consistent with 2 previous telephone surveys. In one survey, 13% of 1000 adults who experienced heartburn at least weekly had only nighttime episodes; 20% reported only daytime heartburn.15 Altogether, 79% of the heartburn sufferers reported experiencing heartburn at night. Of these, 75% reported that heartburn had a negative impact on sleep; 63% indicated that heartburn adversely affected their ability to sleep well; and 40% reported impaired functioning the next day. The prevalence of sleep disturbances increased directly with the incidence of nighttime heartburn.
The second telephone survey of persons with nighttime GERD had lower scores using the Short-Form 36 Health Survey (a measure of quality of life) than did persons with daytime GERD or controls (TABLE 1).4 In another study, the greatest differences between groups occurred in terms of physical and emotional role functioning, vitality, and general health.16 A comparison with other major disorders affirmed the substantial impairment in health-related quality of life caused by nighttime GERD (TABLE 2).4
In summary, although heartburn and regurgitation are common in daytime and nighttime GERD, patients with nighttime GERD are more likely to experience impaired sleep, fatigue, reduced work productivity, and decreased quality of life.
TABLE 1
Adjusted medical outcomes study Short-Form 36 Health Survey scores
| Scale | Nocturnal GERD (n=945) | Non-nocturnal GERD (n=339) | Controls (n=268) |
|---|---|---|---|
| Physical functioning | 63† | 68† | 69 |
| Role limitations—physical | 53*† | 64† | 67* |
| Bodily pain | 54*† | 63† | 69* |
| General health | 48*† | 53†‡ | 59*‡ |
| Vitality | 41*† | 47†‡ | 54*‡ |
| Social functioning | 70*† | 76† | 78* |
| Role limitations—emotional | 69*† | 80† | 81* |
| Mental health | 66*† | 71† | 74* |
| Physical component summary | 39*† | 42† | 43* |
| Mental component summary | 47† | 50† | 51 |
| Analysis of covariance, adjusted for age, sex, and comorbidity. | |||
| *P<.001 nocturnal GERD vs controls; †P<.001 nocturnal vs non-nocturnal; ‡P<.001 non-nocturnal GERD vs controls. | |||
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 | |||
| Copyright © 2001 American Medical Association. Reproduced with permission. | |||
TABLE 2
Mean medical outcomes study Short-Form 36 Health Survey scores
| Scale | Nocturnal GERD (n=945) | Hypertension (n=2089) | Type 2 diabetes (n=541) | Congestive heart failure (n=216) | Clinical depression (n=502) | Angina (n=256) |
|---|---|---|---|---|---|---|
| Physical functioning | 77 | 73 | 68* | 48* | 72* | 63* |
| Role limitations—physical | 69 | 62* | 57* | 34* | 44* | 44* |
| Bodily pain | 62 | 72* | 69* | 63 | 59 | 62 |
| General health | 63 | 63 | 56* | 47* | 53* | 52* |
| Vitality | 49 | 58* | 56* | 44 | 40* | 49 |
| Social functioning | 79 | 87* | 82 | 71 | 57* | 80 |
| Role limitations—emotional | 75 | 77 | 76 | 64* | 39* | 70 |
| Mental health | 71 | 78* | 77* | 75 | 46* | 73 |
| Physical component summary | 45 | 44 | 42* | 35* | 45 | 39* |
| Mental component summary | 48 | 52* | 52* | 50 | 35* | 50 |
| *P<.001 vs nocturnal GERD Norms for non-GERD disorders were obtained from the Short-Form 36 Health Survey: Manual and Interpretation Guide. | ||||||
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 Copyright © 2001 American Medical Association. Reproduced with permission. | ||||||
Diagnosis: evaluation of symptoms
Physicians should inquire specifically about GERD symptoms to ensure diagnosis, as the signs of GERD are often subtle, nonspecific, or judged to be trivial by patients. Symptoms of GERD may include esophageal or nonesophageal complaints, or both. Importantly, heartburn or regurgitation may be absent in many patients: One group of investigators reported that neither heartburn nor regurgitation was experienced by approximately half of all patients who had nonclassical symptoms of GERD.3
Nonesophageal symptoms associated with GERD
Laryngitis, laryngospasm, chronic cough, hoarseness, excessive throat clearing, and globus pharyngeus are common nonesophageal symptoms in patients with GERD (TABLE 3).17,18 In a recent investigation, 86% and 77% of patients with nighttime and daytime episodes of GERD, respectively, reported one or more nonesophageal symptom. In patients experiencing GERD at night, the most common symptoms were sinusitis (52%), dry cough/throat clearing (49%), and snoring (47%). Symptom severity scores were significantly higher in the nighttime vs daytime GERD groups (2.42 vs 1.80, respectively).5
In a cross-sectional international population survey of 2202 randomly selected persons and 459 additional individuals with asthma, Gislason et al estimated the possible association between reported symptoms of nighttime GERD, sleep-disordered breathing, respiratory symptoms, and asthma. The investigators reported a 2- to 3-fold increased prevalence of asthma and other respiratory symptoms (such as wheezing, chest tightness, breathlessness, and nighttime cough) in patients with nighttime reflux.19
TABLE 3
Nonesophageal conditions associated with GERD
|
| Fass R, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):26-38.17 |
| McGuigan JE, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):57-72.18 |
Patient history
The patient’s history is the primary focus of the diagnostic workup and the physician should explore patient risk factors for GERD. For patients with atypical symptoms of GERD, the history is especially important to determine the diagnosis.
The presence of at least one esophageal or non-esophageal sign and symptom should prompt consideration of GERD as the cause, and discussion with the patient may help classify GERD further. The symptoms of nighttime GERD range from mild to severe. Though they can be similar to the symptoms of daytime GERD, nocturnal symptoms may be exacerbated by lying down or may differ in their manifestation. Asking questions about a patient’s quality of sleep, with input from the patient’s sleep partner, if possible, is useful in assessing nighttime GERD (TABLE 4).
TABLE 4
Key questions in the assessment of nighttime GERD
|
| Note: Input should also be sought from the patient’s sleep partner. |
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 |
Predictors of nighttime reflux
A high body mass index (BMI) may lead to a reduction in LES pressure and is a risk factor for GERD.20,21 Social habits such as smoking and alcohol use are often cited as risk factors for GERD; however, data to confirm this premise are lacking.11 Several other factors and the presence of some pulmonary disorders may be specific predictors and indications of nighttime GERD episodes.
A recent large prospective cohort study specifically evaluated predictors of heartburn during sleep. Symptoms of GERD were strongly associated with increased BMI, carbonated soft drink consumption (possibly due to low pH), snoring and daytime sleepiness, insomnia, hypertension, asthma, and usage of benzodiazepines (TABLE 5).20 It was noted that the association of hypertension with nighttime heartburn likely is a reflection of factors associated with hypertension rather than hypertension itself. Possible factors of hypertension include antihypertensive medications, comorbidities, diet, and body habitus.20
Several sleep-related and respiratory factors are associated with nighttime GERD. Among these, insomnia and sleepiness are probably consequences rather than causes of nighttime reflux. An association of GERD with obstructive sleep apnea has been established, although causality has not been determined. Similarly, asthma is clearly associated with GERD, but the extent of causality remains unclear. Nonetheless, nighttime GERD should be suspected in patients who present with one of these sleep disturbances, particularly obstructive sleep apnea, or adult-onset or difficult-to-treat asthma.20
TABLE 5
Factors associated with nighttime GERD
|
| Lagergren J, et al. N Engl J Med. 1999;340:825-831.11 |
| Fass R, et al. Chest. 2005;127:1658-1666.20 |
| Fisher BL, et al. Dig Dis Sci. 1999;44:2290-2294.21 |
Diagnostic tests for GERD
Various tests have been investigated for the diagnosis of all types of GERD, and there is no difference in the tests used when nighttime GERD is suspected. Endoscopy is an important diagnostic tool for either identifying or ruling out complications such as erosions or Barrett’s esophagus. Esophageal pH monitoring can be helpful in diagnosis.
Pathophysiology: potential differences between daytime and nighttime GERD
Several mechanisms have been established to contribute to the development of GERD. Included are transient LES relaxations and, less frequently, sustained LES pressure abnormalities. Other factors that contribute to the pathophysiology of GERD include hiatal hernia, which reduces LES pressure and impairs acid clearance, and poor esophageal clearance.22
Despite their similarities, important pathophysiologic differences between daytime and nighttime gastroesophageal reflux can be seen. Increased acid secretion and gastric volume are associated with food consumption, so daytime reflux and associated symptoms tend to occur after meals. Nighttime gastroesophageal reflux occurs less frequently, but the episodes are of longer duration than those of daytime reflux, as a result of delayed acid clearance from the esophagus at night.6,7,23
Sleep-related mechanisms combined with impairment of the LES and the supine position help explain the more common and severe symptoms and wider range of complications seen in nighttime compared with daytime GERD.
Protective processes impaired during sleep
Differences between daytime and nighttime GERD are thought to be due to the sleep state rather than just to differences in posture (TABLE 6).24,25 Processes that occur normally during the day to facilitate refluxed acid clearance from the esophagus, such as swallowing and acid neutralization (via bicarbonate-containing salivation), are suppressed during sleep.25
Saliva, composed of mucus, bicarbonate, and epidermal growth factor, neutralizes refluxed acid and protects esophageal tissue. Saliva production is diminished during sleep, with implications for GERD symptoms.26,27 Swallowing is reduced during sleep and may not occur during deeper stages of sleep.28 Absence of the voluntary swallow-initiated peristaltic wave of esophageal contractions during sleep also results in reduced volume clearance.29
Delayed gastric emptying during sleep may result in increased gastric distention and contribute to the occurrence of nighttime reflux.25,30
TABLE 6
Sleep-related mechanisms contributing to nighttime GERD
|
| Orr WC, et al. Am J Gastroenterol. 2000;95:37-42.24 |
| Orr WC, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):39-46.25 |
Effect of reduced consciousness
Reflux during sleep may be accompanied by a brief period of arousal, which helps to hasten esophageal clearance of refluxate and protect the airway against aspiration and acid exposure.25 However, arousal does not occur in all reflux episodes, since the conscious perception of heartburn is absent during sleep. Consequently, the sleep-induced mechanisms are allowed to persist leading to prolonged periods of acid exposure.25
Summary
For the purposes of understanding symptoms and facilitating diagnosis, GERD can be divided into daytime and nighttime GERD. Compared with daytime GERD, nighttime reflux episodes occur less frequently but are more prolonged. In addition, nighttime symptoms are more common and more severe, and esophageal and nonesophageal complications are more likely. The presence of severe symptoms or at least one esophageal and/or nonesophageal symptom should prompt an investigation of nighttime GERD. In doing so, the history and physical examination findings are the most helpful; laboratory values and other test results are generally less so. Physiologic alterations during sleep are thought to be the primary factors that contribute to nighttime symptoms.
EDITOR’S NOTE:
This article is meant to alert the reader to different symptomatology in GERD at night; therefore, treatment will not be discussed.
1. Jones R, Galmiche JP. Review: what do we mean by GERD?—definition and diagnosis. Aliment Pharmacol Ther. 2005;22(suppl 1):2-10.
2. Frank L, Kleinman L, Ganoczy D, et al. Upper gastrointestinal symptoms in North America: prevalence and relationship to healthcare utilization and quality of life. Dig Dis Sci. 2000;45:809-818.
3. Locke GR, III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ, III. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448-1456.
4. Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med. 2001;161:45-52.
5. Dubois RW, Fass R, Johnson LF, et al. Atypical nighttime symptoms of GERD among individuals with nighttime versus daytime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A288.-Abstract M999.
6. Orr WC, Allen ML, Robinson M. The pattern of nocturnal and diurnal esophageal acid exposure in the pathogenesis of erosive mucosal damage. Am J Gastroenterol. 1994;89:509-512.
7. Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976;184:459-470.
8. Cameron AJ, Lomboy CT. Barrett’s esophagus: age, prevalence, and extent of columnar epithelium. Gastroenterology. 1992;103:1241-1245.
9. Orr WC, Lackey C, Robinson MG, Johnson LF, Welsh JD. Esophageal acid clearance during sleep in patients with Barrett’s esophagus. Dig Dis Sci. 1988;33:654-659.
10. Eisen GM, Sandler RS, Murray S, Gottfried M. The relationship between gastroesophageal reflux disease and its complications with Barrett’s esophagus. Am J Gastroenterol. 1997;92:27-31.
11. Lagergren J, Bergstrom R, Lindgren A, Nyren O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825-831.
12. Dubois RW, Orr WC, Lange SM, et al. GERD-related sleep impairment among individuals with nighttime versus daytime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A288.-Abstract M998.
13. Dubois RW, Lange SM, Fass R, et al. Work productivity loss associated with nighttime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A286.-Abstract M988.
14. Dean BB, Crawley JA, Schmitt CM, Wong J, Ofman JJ. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther. 2003;17:1309-1317.
15. Shaker R, Castell DO, Schoenfeld PS, Spechler SJ. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function the results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol. 2003;98:1487-1493.
16. Dubois RW, Fass R, Lange SM, et al. Impact of nighttime GERD on health-related quality of life [abstract]. Gastroenterology. 2005;128:(4 Suppl 2):A286.-Abstract M989.
17. Fass R, Achem SR, Harding S, Mittal RK, Quigley E. Review article: supra-oesophageal manifestations of gastro-oesophageal reflux disease and the role of night-time gastro-oesophageal reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):26-38.
18. McGuigan JE, Belafsky PC, Fromer L, et al. Review article: diagnosis and management of night-time reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):57-72.
19. Gislason T, Janson C, Vermeire P, et al. Respiratory symptoms and nocturnal gastroesophageal reflux: a population-based study of young adults in three European countries. Chest. 2002;121:158-163.
20. Fass R, Quan SF, O’Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127:1658-1666.
21. Fisher BL, Pennathur A, Mutnick JL, Little AG. Obesity correlates with gastroesophageal reflux. Dig Dis Sci. 1999;44:2290-2294.
22. Castell DO, Murray JA, Tutuian R, Orlando RC, Arnold R. Review article: the pathophysiology of gastro-oesophageal reflux disease - oesophageal manifestations. Aliment Pharmacol Ther. 2004;20(suppl 9):14-25.
23. Orr WC, Johnson LF. Responses to different levels of esophageal acidification during waking and sleeping. Dig Dis Sci. 1998;43:241-245.
24. Orr WC, Elsenbruch S, Harnish MJ, Johnson LF. Proximal migration of esophageal acid perfusions during waking and sleep. Am J Gastroenterol. 2000;95:37-42.
25. Orr WC, Heading R, Johnson LF, Kryger M. Review article: sleep and its relationship to gastro-oesophageal reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):39-46.
26. Schneyer LH, Pigman WW, Hanahan LL, Gilmore R. Rate of flow of human parotid sublingual, and submaxillary secretions during sleep. J Dent Res. 1956;35:109-114.
27. Dawes C. Circadian rhythms in human salivary flow rate and composition. J Physiol. 1972;220:529-545.
28. Lear CS, Flanagan JB, Jr, Moorrees CF. The frequency of deglutition in man. Arch Oral Biol. 1965;10:83-100.
29. Orr WC, Johnson LF, Robinson MG. Effect of sleep on swallowing, esophageal peristalsis, and acid clearance. Gastroenterology. 1984;86 (pt 1):814-819.
30. Elsenbruch S, Orr WC, Harnish MJ, Chen JD. Disruption of normal gastric myoelectric functioning by sleep. Sleep. 1999;22:453-458.
- Reflux episodes with nighttime GERD occur less frequently but are more prolonged than those with daytime GERD. (SOR: B)
- Esophageal complications are generally more severe and nonesophageal complications more common in nighttime than in daytime GERD. (SOR: B)
- Nighttime GERD-induced alterations in sleep cause significant patient morbidity and reduced quality of life and productivity. (SOR: B)
- Several factors are associated with nighttime GERD, including increased body mass index, carbonated soft drink consumption, hypertension, benzodiazepine use, obstructive sleep apnea, and asthma. (SOR: B)
- The history and physical examination generally provide the most useful information in making the diagnosis. (SOR: C)
- Sleep-induced physiologic alterations are thought to be important factors responsible for the more common and severe symptoms and complications in nighttime vs daytime GERD. (SOR: C)
Prevalence estimates for gastroesophageal reflux disease (GERD) range from 8% to 40%, depending on the definition and diagnostic criteria.1-4 While heartburn and regurgitation are considered the hallmark symptoms, GERD actually represents a spectrum of disorders that generally result from transient relaxations of the lower esophageal sphincter (LES), so that gastric refluxate comes into contact with the esophageal epithelium. Additionally, differences in rates of acid secretion and clearance and the time since food ingestion affect symptoms, potentially leading to differing presentations of GERD associated with daytime and nocturnal episodes. To facilitate accurate diagnosis of GERD, it may be helpful for clinicians to distinguish between the symptoms that occur during the day or in an upright position and those that occur at night or when a person is supine.4 This paper reviews the differences in symptoms and explains the pathophysiologic mechanisms involved.
Issues of GERD and quality of life
Patients’ quality of life and ability to function is negatively impacted by factors associated specifically with nocturnal episodes of GERD. Patients who experience GERD primarily at night may complain of sleep disturbances. Symptoms associated with nighttime GERD generally are more severe,5 and the complications more diverse and frequent,4 due to the prolonged length of nighttime reflux.6 For these reasons, determining if the underlying cause of a group of symptoms is nighttime episodes of GERD is an important treatment step.
Complications of reflux: associations with nighttime occurrences
Esophageal complications of GERD include erosive esophagitis, esophageal hemorrhage, ulceration, and strictures and appear to be more severe in patients with nighttime episodes of GERD than in those complaining of daytime reflux. An early study showed that patients who experience reflux only in the supine position have a higher incidence of esophagitis compared with patients who only refluxed in an upright position.7 Prolonged acid contact time increases the risk that esophagitis will become erosive. This was demonstrated in a study that concluded particularly that the presence of nocturnal reflux events lasting more than 5 minutes was a powerful predictor of erosive damage.6
Overall, approximately 7% to 12% of patients with chronic GERD develop Barrett’s esophagus compared with fewer than 1% of those in the general population.8 Potentially, more severe nocturnal symptoms may be among the factors that increase the risk of Barrett’s esophagus.9,10 Esophageal adenocarcinoma also is more likely in patients with nocturnal episodes of GERD: In a national, population-based, case-controlled trial, an 11-fold increased risk for esophageal adenocarcinoma was reported in patients who experienced once-weekly episodes of nighttime heartburn, regurgitation, or both. Overall, an 8-fold increased risk of esophageal adenocarcinoma was observed in all patients with GERD.11
Impact of nighttime episodes on sleep
Not surprisingly, sleep is significantly affected by nighttime GERD episodes. A recent Internet-based survey of full-time working adults in the United States identified 1002 patients with symptomatic GERD.12 Using the validated GERD Symptom and Medication Questionnaire, symptomatic GERD was defined as a score of 10 or greater for at least one episode of heartburn or acid regurgitation within the past 7 days. Symptomatic nighttime GERD was defined as at least 2 nights with symptoms during the past 7 days. GERD-related sleep problems were twice as frequent in patients with nighttime compared with daytime GERD. Patients with nighttime episodes of GERD experienced GERD-related sleep impairment an average of 1.6 to 1.9 nights per week compared with 0.3 to 0.4 nights per week for the daytime GERD group.
In both groups, the most commonly reported sleep problem was awakening due to symptoms (75% vs 37%, respectively). Sixty-five percent of nighttime and 28% of daytime GERD patients indicated that GERD symptoms prevented them from feeling rested in the morning.12 In addition, respondents with nighttime GERD experienced an additional 2.7 hours per week of lost work productivity when compared to those with daytime GERD.13 A similar survey also found that in those with nighttime GERD, the number of nights with sleep interference was associated with reduced work productivity.14
These results are consistent with 2 previous telephone surveys. In one survey, 13% of 1000 adults who experienced heartburn at least weekly had only nighttime episodes; 20% reported only daytime heartburn.15 Altogether, 79% of the heartburn sufferers reported experiencing heartburn at night. Of these, 75% reported that heartburn had a negative impact on sleep; 63% indicated that heartburn adversely affected their ability to sleep well; and 40% reported impaired functioning the next day. The prevalence of sleep disturbances increased directly with the incidence of nighttime heartburn.
The second telephone survey of persons with nighttime GERD had lower scores using the Short-Form 36 Health Survey (a measure of quality of life) than did persons with daytime GERD or controls (TABLE 1).4 In another study, the greatest differences between groups occurred in terms of physical and emotional role functioning, vitality, and general health.16 A comparison with other major disorders affirmed the substantial impairment in health-related quality of life caused by nighttime GERD (TABLE 2).4
In summary, although heartburn and regurgitation are common in daytime and nighttime GERD, patients with nighttime GERD are more likely to experience impaired sleep, fatigue, reduced work productivity, and decreased quality of life.
TABLE 1
Adjusted medical outcomes study Short-Form 36 Health Survey scores
| Scale | Nocturnal GERD (n=945) | Non-nocturnal GERD (n=339) | Controls (n=268) |
|---|---|---|---|
| Physical functioning | 63† | 68† | 69 |
| Role limitations—physical | 53*† | 64† | 67* |
| Bodily pain | 54*† | 63† | 69* |
| General health | 48*† | 53†‡ | 59*‡ |
| Vitality | 41*† | 47†‡ | 54*‡ |
| Social functioning | 70*† | 76† | 78* |
| Role limitations—emotional | 69*† | 80† | 81* |
| Mental health | 66*† | 71† | 74* |
| Physical component summary | 39*† | 42† | 43* |
| Mental component summary | 47† | 50† | 51 |
| Analysis of covariance, adjusted for age, sex, and comorbidity. | |||
| *P<.001 nocturnal GERD vs controls; †P<.001 nocturnal vs non-nocturnal; ‡P<.001 non-nocturnal GERD vs controls. | |||
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 | |||
| Copyright © 2001 American Medical Association. Reproduced with permission. | |||
TABLE 2
Mean medical outcomes study Short-Form 36 Health Survey scores
| Scale | Nocturnal GERD (n=945) | Hypertension (n=2089) | Type 2 diabetes (n=541) | Congestive heart failure (n=216) | Clinical depression (n=502) | Angina (n=256) |
|---|---|---|---|---|---|---|
| Physical functioning | 77 | 73 | 68* | 48* | 72* | 63* |
| Role limitations—physical | 69 | 62* | 57* | 34* | 44* | 44* |
| Bodily pain | 62 | 72* | 69* | 63 | 59 | 62 |
| General health | 63 | 63 | 56* | 47* | 53* | 52* |
| Vitality | 49 | 58* | 56* | 44 | 40* | 49 |
| Social functioning | 79 | 87* | 82 | 71 | 57* | 80 |
| Role limitations—emotional | 75 | 77 | 76 | 64* | 39* | 70 |
| Mental health | 71 | 78* | 77* | 75 | 46* | 73 |
| Physical component summary | 45 | 44 | 42* | 35* | 45 | 39* |
| Mental component summary | 48 | 52* | 52* | 50 | 35* | 50 |
| *P<.001 vs nocturnal GERD Norms for non-GERD disorders were obtained from the Short-Form 36 Health Survey: Manual and Interpretation Guide. | ||||||
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 Copyright © 2001 American Medical Association. Reproduced with permission. | ||||||
Diagnosis: evaluation of symptoms
Physicians should inquire specifically about GERD symptoms to ensure diagnosis, as the signs of GERD are often subtle, nonspecific, or judged to be trivial by patients. Symptoms of GERD may include esophageal or nonesophageal complaints, or both. Importantly, heartburn or regurgitation may be absent in many patients: One group of investigators reported that neither heartburn nor regurgitation was experienced by approximately half of all patients who had nonclassical symptoms of GERD.3
Nonesophageal symptoms associated with GERD
Laryngitis, laryngospasm, chronic cough, hoarseness, excessive throat clearing, and globus pharyngeus are common nonesophageal symptoms in patients with GERD (TABLE 3).17,18 In a recent investigation, 86% and 77% of patients with nighttime and daytime episodes of GERD, respectively, reported one or more nonesophageal symptom. In patients experiencing GERD at night, the most common symptoms were sinusitis (52%), dry cough/throat clearing (49%), and snoring (47%). Symptom severity scores were significantly higher in the nighttime vs daytime GERD groups (2.42 vs 1.80, respectively).5
In a cross-sectional international population survey of 2202 randomly selected persons and 459 additional individuals with asthma, Gislason et al estimated the possible association between reported symptoms of nighttime GERD, sleep-disordered breathing, respiratory symptoms, and asthma. The investigators reported a 2- to 3-fold increased prevalence of asthma and other respiratory symptoms (such as wheezing, chest tightness, breathlessness, and nighttime cough) in patients with nighttime reflux.19
TABLE 3
Nonesophageal conditions associated with GERD
|
| Fass R, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):26-38.17 |
| McGuigan JE, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):57-72.18 |
Patient history
The patient’s history is the primary focus of the diagnostic workup and the physician should explore patient risk factors for GERD. For patients with atypical symptoms of GERD, the history is especially important to determine the diagnosis.
The presence of at least one esophageal or non-esophageal sign and symptom should prompt consideration of GERD as the cause, and discussion with the patient may help classify GERD further. The symptoms of nighttime GERD range from mild to severe. Though they can be similar to the symptoms of daytime GERD, nocturnal symptoms may be exacerbated by lying down or may differ in their manifestation. Asking questions about a patient’s quality of sleep, with input from the patient’s sleep partner, if possible, is useful in assessing nighttime GERD (TABLE 4).
TABLE 4
Key questions in the assessment of nighttime GERD
|
| Note: Input should also be sought from the patient’s sleep partner. |
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 |
Predictors of nighttime reflux
A high body mass index (BMI) may lead to a reduction in LES pressure and is a risk factor for GERD.20,21 Social habits such as smoking and alcohol use are often cited as risk factors for GERD; however, data to confirm this premise are lacking.11 Several other factors and the presence of some pulmonary disorders may be specific predictors and indications of nighttime GERD episodes.
A recent large prospective cohort study specifically evaluated predictors of heartburn during sleep. Symptoms of GERD were strongly associated with increased BMI, carbonated soft drink consumption (possibly due to low pH), snoring and daytime sleepiness, insomnia, hypertension, asthma, and usage of benzodiazepines (TABLE 5).20 It was noted that the association of hypertension with nighttime heartburn likely is a reflection of factors associated with hypertension rather than hypertension itself. Possible factors of hypertension include antihypertensive medications, comorbidities, diet, and body habitus.20
Several sleep-related and respiratory factors are associated with nighttime GERD. Among these, insomnia and sleepiness are probably consequences rather than causes of nighttime reflux. An association of GERD with obstructive sleep apnea has been established, although causality has not been determined. Similarly, asthma is clearly associated with GERD, but the extent of causality remains unclear. Nonetheless, nighttime GERD should be suspected in patients who present with one of these sleep disturbances, particularly obstructive sleep apnea, or adult-onset or difficult-to-treat asthma.20
TABLE 5
Factors associated with nighttime GERD
|
| Lagergren J, et al. N Engl J Med. 1999;340:825-831.11 |
| Fass R, et al. Chest. 2005;127:1658-1666.20 |
| Fisher BL, et al. Dig Dis Sci. 1999;44:2290-2294.21 |
Diagnostic tests for GERD
Various tests have been investigated for the diagnosis of all types of GERD, and there is no difference in the tests used when nighttime GERD is suspected. Endoscopy is an important diagnostic tool for either identifying or ruling out complications such as erosions or Barrett’s esophagus. Esophageal pH monitoring can be helpful in diagnosis.
Pathophysiology: potential differences between daytime and nighttime GERD
Several mechanisms have been established to contribute to the development of GERD. Included are transient LES relaxations and, less frequently, sustained LES pressure abnormalities. Other factors that contribute to the pathophysiology of GERD include hiatal hernia, which reduces LES pressure and impairs acid clearance, and poor esophageal clearance.22
Despite their similarities, important pathophysiologic differences between daytime and nighttime gastroesophageal reflux can be seen. Increased acid secretion and gastric volume are associated with food consumption, so daytime reflux and associated symptoms tend to occur after meals. Nighttime gastroesophageal reflux occurs less frequently, but the episodes are of longer duration than those of daytime reflux, as a result of delayed acid clearance from the esophagus at night.6,7,23
Sleep-related mechanisms combined with impairment of the LES and the supine position help explain the more common and severe symptoms and wider range of complications seen in nighttime compared with daytime GERD.
Protective processes impaired during sleep
Differences between daytime and nighttime GERD are thought to be due to the sleep state rather than just to differences in posture (TABLE 6).24,25 Processes that occur normally during the day to facilitate refluxed acid clearance from the esophagus, such as swallowing and acid neutralization (via bicarbonate-containing salivation), are suppressed during sleep.25
Saliva, composed of mucus, bicarbonate, and epidermal growth factor, neutralizes refluxed acid and protects esophageal tissue. Saliva production is diminished during sleep, with implications for GERD symptoms.26,27 Swallowing is reduced during sleep and may not occur during deeper stages of sleep.28 Absence of the voluntary swallow-initiated peristaltic wave of esophageal contractions during sleep also results in reduced volume clearance.29
Delayed gastric emptying during sleep may result in increased gastric distention and contribute to the occurrence of nighttime reflux.25,30
TABLE 6
Sleep-related mechanisms contributing to nighttime GERD
|
| Orr WC, et al. Am J Gastroenterol. 2000;95:37-42.24 |
| Orr WC, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):39-46.25 |
Effect of reduced consciousness
Reflux during sleep may be accompanied by a brief period of arousal, which helps to hasten esophageal clearance of refluxate and protect the airway against aspiration and acid exposure.25 However, arousal does not occur in all reflux episodes, since the conscious perception of heartburn is absent during sleep. Consequently, the sleep-induced mechanisms are allowed to persist leading to prolonged periods of acid exposure.25
Summary
For the purposes of understanding symptoms and facilitating diagnosis, GERD can be divided into daytime and nighttime GERD. Compared with daytime GERD, nighttime reflux episodes occur less frequently but are more prolonged. In addition, nighttime symptoms are more common and more severe, and esophageal and nonesophageal complications are more likely. The presence of severe symptoms or at least one esophageal and/or nonesophageal symptom should prompt an investigation of nighttime GERD. In doing so, the history and physical examination findings are the most helpful; laboratory values and other test results are generally less so. Physiologic alterations during sleep are thought to be the primary factors that contribute to nighttime symptoms.
EDITOR’S NOTE:
This article is meant to alert the reader to different symptomatology in GERD at night; therefore, treatment will not be discussed.
- Reflux episodes with nighttime GERD occur less frequently but are more prolonged than those with daytime GERD. (SOR: B)
- Esophageal complications are generally more severe and nonesophageal complications more common in nighttime than in daytime GERD. (SOR: B)
- Nighttime GERD-induced alterations in sleep cause significant patient morbidity and reduced quality of life and productivity. (SOR: B)
- Several factors are associated with nighttime GERD, including increased body mass index, carbonated soft drink consumption, hypertension, benzodiazepine use, obstructive sleep apnea, and asthma. (SOR: B)
- The history and physical examination generally provide the most useful information in making the diagnosis. (SOR: C)
- Sleep-induced physiologic alterations are thought to be important factors responsible for the more common and severe symptoms and complications in nighttime vs daytime GERD. (SOR: C)
Prevalence estimates for gastroesophageal reflux disease (GERD) range from 8% to 40%, depending on the definition and diagnostic criteria.1-4 While heartburn and regurgitation are considered the hallmark symptoms, GERD actually represents a spectrum of disorders that generally result from transient relaxations of the lower esophageal sphincter (LES), so that gastric refluxate comes into contact with the esophageal epithelium. Additionally, differences in rates of acid secretion and clearance and the time since food ingestion affect symptoms, potentially leading to differing presentations of GERD associated with daytime and nocturnal episodes. To facilitate accurate diagnosis of GERD, it may be helpful for clinicians to distinguish between the symptoms that occur during the day or in an upright position and those that occur at night or when a person is supine.4 This paper reviews the differences in symptoms and explains the pathophysiologic mechanisms involved.
Issues of GERD and quality of life
Patients’ quality of life and ability to function is negatively impacted by factors associated specifically with nocturnal episodes of GERD. Patients who experience GERD primarily at night may complain of sleep disturbances. Symptoms associated with nighttime GERD generally are more severe,5 and the complications more diverse and frequent,4 due to the prolonged length of nighttime reflux.6 For these reasons, determining if the underlying cause of a group of symptoms is nighttime episodes of GERD is an important treatment step.
Complications of reflux: associations with nighttime occurrences
Esophageal complications of GERD include erosive esophagitis, esophageal hemorrhage, ulceration, and strictures and appear to be more severe in patients with nighttime episodes of GERD than in those complaining of daytime reflux. An early study showed that patients who experience reflux only in the supine position have a higher incidence of esophagitis compared with patients who only refluxed in an upright position.7 Prolonged acid contact time increases the risk that esophagitis will become erosive. This was demonstrated in a study that concluded particularly that the presence of nocturnal reflux events lasting more than 5 minutes was a powerful predictor of erosive damage.6
Overall, approximately 7% to 12% of patients with chronic GERD develop Barrett’s esophagus compared with fewer than 1% of those in the general population.8 Potentially, more severe nocturnal symptoms may be among the factors that increase the risk of Barrett’s esophagus.9,10 Esophageal adenocarcinoma also is more likely in patients with nocturnal episodes of GERD: In a national, population-based, case-controlled trial, an 11-fold increased risk for esophageal adenocarcinoma was reported in patients who experienced once-weekly episodes of nighttime heartburn, regurgitation, or both. Overall, an 8-fold increased risk of esophageal adenocarcinoma was observed in all patients with GERD.11
Impact of nighttime episodes on sleep
Not surprisingly, sleep is significantly affected by nighttime GERD episodes. A recent Internet-based survey of full-time working adults in the United States identified 1002 patients with symptomatic GERD.12 Using the validated GERD Symptom and Medication Questionnaire, symptomatic GERD was defined as a score of 10 or greater for at least one episode of heartburn or acid regurgitation within the past 7 days. Symptomatic nighttime GERD was defined as at least 2 nights with symptoms during the past 7 days. GERD-related sleep problems were twice as frequent in patients with nighttime compared with daytime GERD. Patients with nighttime episodes of GERD experienced GERD-related sleep impairment an average of 1.6 to 1.9 nights per week compared with 0.3 to 0.4 nights per week for the daytime GERD group.
In both groups, the most commonly reported sleep problem was awakening due to symptoms (75% vs 37%, respectively). Sixty-five percent of nighttime and 28% of daytime GERD patients indicated that GERD symptoms prevented them from feeling rested in the morning.12 In addition, respondents with nighttime GERD experienced an additional 2.7 hours per week of lost work productivity when compared to those with daytime GERD.13 A similar survey also found that in those with nighttime GERD, the number of nights with sleep interference was associated with reduced work productivity.14
These results are consistent with 2 previous telephone surveys. In one survey, 13% of 1000 adults who experienced heartburn at least weekly had only nighttime episodes; 20% reported only daytime heartburn.15 Altogether, 79% of the heartburn sufferers reported experiencing heartburn at night. Of these, 75% reported that heartburn had a negative impact on sleep; 63% indicated that heartburn adversely affected their ability to sleep well; and 40% reported impaired functioning the next day. The prevalence of sleep disturbances increased directly with the incidence of nighttime heartburn.
The second telephone survey of persons with nighttime GERD had lower scores using the Short-Form 36 Health Survey (a measure of quality of life) than did persons with daytime GERD or controls (TABLE 1).4 In another study, the greatest differences between groups occurred in terms of physical and emotional role functioning, vitality, and general health.16 A comparison with other major disorders affirmed the substantial impairment in health-related quality of life caused by nighttime GERD (TABLE 2).4
In summary, although heartburn and regurgitation are common in daytime and nighttime GERD, patients with nighttime GERD are more likely to experience impaired sleep, fatigue, reduced work productivity, and decreased quality of life.
TABLE 1
Adjusted medical outcomes study Short-Form 36 Health Survey scores
| Scale | Nocturnal GERD (n=945) | Non-nocturnal GERD (n=339) | Controls (n=268) |
|---|---|---|---|
| Physical functioning | 63† | 68† | 69 |
| Role limitations—physical | 53*† | 64† | 67* |
| Bodily pain | 54*† | 63† | 69* |
| General health | 48*† | 53†‡ | 59*‡ |
| Vitality | 41*† | 47†‡ | 54*‡ |
| Social functioning | 70*† | 76† | 78* |
| Role limitations—emotional | 69*† | 80† | 81* |
| Mental health | 66*† | 71† | 74* |
| Physical component summary | 39*† | 42† | 43* |
| Mental component summary | 47† | 50† | 51 |
| Analysis of covariance, adjusted for age, sex, and comorbidity. | |||
| *P<.001 nocturnal GERD vs controls; †P<.001 nocturnal vs non-nocturnal; ‡P<.001 non-nocturnal GERD vs controls. | |||
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 | |||
| Copyright © 2001 American Medical Association. Reproduced with permission. | |||
TABLE 2
Mean medical outcomes study Short-Form 36 Health Survey scores
| Scale | Nocturnal GERD (n=945) | Hypertension (n=2089) | Type 2 diabetes (n=541) | Congestive heart failure (n=216) | Clinical depression (n=502) | Angina (n=256) |
|---|---|---|---|---|---|---|
| Physical functioning | 77 | 73 | 68* | 48* | 72* | 63* |
| Role limitations—physical | 69 | 62* | 57* | 34* | 44* | 44* |
| Bodily pain | 62 | 72* | 69* | 63 | 59 | 62 |
| General health | 63 | 63 | 56* | 47* | 53* | 52* |
| Vitality | 49 | 58* | 56* | 44 | 40* | 49 |
| Social functioning | 79 | 87* | 82 | 71 | 57* | 80 |
| Role limitations—emotional | 75 | 77 | 76 | 64* | 39* | 70 |
| Mental health | 71 | 78* | 77* | 75 | 46* | 73 |
| Physical component summary | 45 | 44 | 42* | 35* | 45 | 39* |
| Mental component summary | 48 | 52* | 52* | 50 | 35* | 50 |
| *P<.001 vs nocturnal GERD Norms for non-GERD disorders were obtained from the Short-Form 36 Health Survey: Manual and Interpretation Guide. | ||||||
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 Copyright © 2001 American Medical Association. Reproduced with permission. | ||||||
Diagnosis: evaluation of symptoms
Physicians should inquire specifically about GERD symptoms to ensure diagnosis, as the signs of GERD are often subtle, nonspecific, or judged to be trivial by patients. Symptoms of GERD may include esophageal or nonesophageal complaints, or both. Importantly, heartburn or regurgitation may be absent in many patients: One group of investigators reported that neither heartburn nor regurgitation was experienced by approximately half of all patients who had nonclassical symptoms of GERD.3
Nonesophageal symptoms associated with GERD
Laryngitis, laryngospasm, chronic cough, hoarseness, excessive throat clearing, and globus pharyngeus are common nonesophageal symptoms in patients with GERD (TABLE 3).17,18 In a recent investigation, 86% and 77% of patients with nighttime and daytime episodes of GERD, respectively, reported one or more nonesophageal symptom. In patients experiencing GERD at night, the most common symptoms were sinusitis (52%), dry cough/throat clearing (49%), and snoring (47%). Symptom severity scores were significantly higher in the nighttime vs daytime GERD groups (2.42 vs 1.80, respectively).5
In a cross-sectional international population survey of 2202 randomly selected persons and 459 additional individuals with asthma, Gislason et al estimated the possible association between reported symptoms of nighttime GERD, sleep-disordered breathing, respiratory symptoms, and asthma. The investigators reported a 2- to 3-fold increased prevalence of asthma and other respiratory symptoms (such as wheezing, chest tightness, breathlessness, and nighttime cough) in patients with nighttime reflux.19
TABLE 3
Nonesophageal conditions associated with GERD
|
| Fass R, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):26-38.17 |
| McGuigan JE, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):57-72.18 |
Patient history
The patient’s history is the primary focus of the diagnostic workup and the physician should explore patient risk factors for GERD. For patients with atypical symptoms of GERD, the history is especially important to determine the diagnosis.
The presence of at least one esophageal or non-esophageal sign and symptom should prompt consideration of GERD as the cause, and discussion with the patient may help classify GERD further. The symptoms of nighttime GERD range from mild to severe. Though they can be similar to the symptoms of daytime GERD, nocturnal symptoms may be exacerbated by lying down or may differ in their manifestation. Asking questions about a patient’s quality of sleep, with input from the patient’s sleep partner, if possible, is useful in assessing nighttime GERD (TABLE 4).
TABLE 4
Key questions in the assessment of nighttime GERD
|
| Note: Input should also be sought from the patient’s sleep partner. |
| Farup C, et al. Arch Intern Med. 2001;161:45-52.4 |
Predictors of nighttime reflux
A high body mass index (BMI) may lead to a reduction in LES pressure and is a risk factor for GERD.20,21 Social habits such as smoking and alcohol use are often cited as risk factors for GERD; however, data to confirm this premise are lacking.11 Several other factors and the presence of some pulmonary disorders may be specific predictors and indications of nighttime GERD episodes.
A recent large prospective cohort study specifically evaluated predictors of heartburn during sleep. Symptoms of GERD were strongly associated with increased BMI, carbonated soft drink consumption (possibly due to low pH), snoring and daytime sleepiness, insomnia, hypertension, asthma, and usage of benzodiazepines (TABLE 5).20 It was noted that the association of hypertension with nighttime heartburn likely is a reflection of factors associated with hypertension rather than hypertension itself. Possible factors of hypertension include antihypertensive medications, comorbidities, diet, and body habitus.20
Several sleep-related and respiratory factors are associated with nighttime GERD. Among these, insomnia and sleepiness are probably consequences rather than causes of nighttime reflux. An association of GERD with obstructive sleep apnea has been established, although causality has not been determined. Similarly, asthma is clearly associated with GERD, but the extent of causality remains unclear. Nonetheless, nighttime GERD should be suspected in patients who present with one of these sleep disturbances, particularly obstructive sleep apnea, or adult-onset or difficult-to-treat asthma.20
TABLE 5
Factors associated with nighttime GERD
|
| Lagergren J, et al. N Engl J Med. 1999;340:825-831.11 |
| Fass R, et al. Chest. 2005;127:1658-1666.20 |
| Fisher BL, et al. Dig Dis Sci. 1999;44:2290-2294.21 |
Diagnostic tests for GERD
Various tests have been investigated for the diagnosis of all types of GERD, and there is no difference in the tests used when nighttime GERD is suspected. Endoscopy is an important diagnostic tool for either identifying or ruling out complications such as erosions or Barrett’s esophagus. Esophageal pH monitoring can be helpful in diagnosis.
Pathophysiology: potential differences between daytime and nighttime GERD
Several mechanisms have been established to contribute to the development of GERD. Included are transient LES relaxations and, less frequently, sustained LES pressure abnormalities. Other factors that contribute to the pathophysiology of GERD include hiatal hernia, which reduces LES pressure and impairs acid clearance, and poor esophageal clearance.22
Despite their similarities, important pathophysiologic differences between daytime and nighttime gastroesophageal reflux can be seen. Increased acid secretion and gastric volume are associated with food consumption, so daytime reflux and associated symptoms tend to occur after meals. Nighttime gastroesophageal reflux occurs less frequently, but the episodes are of longer duration than those of daytime reflux, as a result of delayed acid clearance from the esophagus at night.6,7,23
Sleep-related mechanisms combined with impairment of the LES and the supine position help explain the more common and severe symptoms and wider range of complications seen in nighttime compared with daytime GERD.
Protective processes impaired during sleep
Differences between daytime and nighttime GERD are thought to be due to the sleep state rather than just to differences in posture (TABLE 6).24,25 Processes that occur normally during the day to facilitate refluxed acid clearance from the esophagus, such as swallowing and acid neutralization (via bicarbonate-containing salivation), are suppressed during sleep.25
Saliva, composed of mucus, bicarbonate, and epidermal growth factor, neutralizes refluxed acid and protects esophageal tissue. Saliva production is diminished during sleep, with implications for GERD symptoms.26,27 Swallowing is reduced during sleep and may not occur during deeper stages of sleep.28 Absence of the voluntary swallow-initiated peristaltic wave of esophageal contractions during sleep also results in reduced volume clearance.29
Delayed gastric emptying during sleep may result in increased gastric distention and contribute to the occurrence of nighttime reflux.25,30
TABLE 6
Sleep-related mechanisms contributing to nighttime GERD
|
| Orr WC, et al. Am J Gastroenterol. 2000;95:37-42.24 |
| Orr WC, et al. Aliment Pharmacol Ther. 2004;20(suppl 9):39-46.25 |
Effect of reduced consciousness
Reflux during sleep may be accompanied by a brief period of arousal, which helps to hasten esophageal clearance of refluxate and protect the airway against aspiration and acid exposure.25 However, arousal does not occur in all reflux episodes, since the conscious perception of heartburn is absent during sleep. Consequently, the sleep-induced mechanisms are allowed to persist leading to prolonged periods of acid exposure.25
Summary
For the purposes of understanding symptoms and facilitating diagnosis, GERD can be divided into daytime and nighttime GERD. Compared with daytime GERD, nighttime reflux episodes occur less frequently but are more prolonged. In addition, nighttime symptoms are more common and more severe, and esophageal and nonesophageal complications are more likely. The presence of severe symptoms or at least one esophageal and/or nonesophageal symptom should prompt an investigation of nighttime GERD. In doing so, the history and physical examination findings are the most helpful; laboratory values and other test results are generally less so. Physiologic alterations during sleep are thought to be the primary factors that contribute to nighttime symptoms.
EDITOR’S NOTE:
This article is meant to alert the reader to different symptomatology in GERD at night; therefore, treatment will not be discussed.
1. Jones R, Galmiche JP. Review: what do we mean by GERD?—definition and diagnosis. Aliment Pharmacol Ther. 2005;22(suppl 1):2-10.
2. Frank L, Kleinman L, Ganoczy D, et al. Upper gastrointestinal symptoms in North America: prevalence and relationship to healthcare utilization and quality of life. Dig Dis Sci. 2000;45:809-818.
3. Locke GR, III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ, III. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448-1456.
4. Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med. 2001;161:45-52.
5. Dubois RW, Fass R, Johnson LF, et al. Atypical nighttime symptoms of GERD among individuals with nighttime versus daytime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A288.-Abstract M999.
6. Orr WC, Allen ML, Robinson M. The pattern of nocturnal and diurnal esophageal acid exposure in the pathogenesis of erosive mucosal damage. Am J Gastroenterol. 1994;89:509-512.
7. Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976;184:459-470.
8. Cameron AJ, Lomboy CT. Barrett’s esophagus: age, prevalence, and extent of columnar epithelium. Gastroenterology. 1992;103:1241-1245.
9. Orr WC, Lackey C, Robinson MG, Johnson LF, Welsh JD. Esophageal acid clearance during sleep in patients with Barrett’s esophagus. Dig Dis Sci. 1988;33:654-659.
10. Eisen GM, Sandler RS, Murray S, Gottfried M. The relationship between gastroesophageal reflux disease and its complications with Barrett’s esophagus. Am J Gastroenterol. 1997;92:27-31.
11. Lagergren J, Bergstrom R, Lindgren A, Nyren O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825-831.
12. Dubois RW, Orr WC, Lange SM, et al. GERD-related sleep impairment among individuals with nighttime versus daytime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A288.-Abstract M998.
13. Dubois RW, Lange SM, Fass R, et al. Work productivity loss associated with nighttime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A286.-Abstract M988.
14. Dean BB, Crawley JA, Schmitt CM, Wong J, Ofman JJ. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther. 2003;17:1309-1317.
15. Shaker R, Castell DO, Schoenfeld PS, Spechler SJ. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function the results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol. 2003;98:1487-1493.
16. Dubois RW, Fass R, Lange SM, et al. Impact of nighttime GERD on health-related quality of life [abstract]. Gastroenterology. 2005;128:(4 Suppl 2):A286.-Abstract M989.
17. Fass R, Achem SR, Harding S, Mittal RK, Quigley E. Review article: supra-oesophageal manifestations of gastro-oesophageal reflux disease and the role of night-time gastro-oesophageal reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):26-38.
18. McGuigan JE, Belafsky PC, Fromer L, et al. Review article: diagnosis and management of night-time reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):57-72.
19. Gislason T, Janson C, Vermeire P, et al. Respiratory symptoms and nocturnal gastroesophageal reflux: a population-based study of young adults in three European countries. Chest. 2002;121:158-163.
20. Fass R, Quan SF, O’Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127:1658-1666.
21. Fisher BL, Pennathur A, Mutnick JL, Little AG. Obesity correlates with gastroesophageal reflux. Dig Dis Sci. 1999;44:2290-2294.
22. Castell DO, Murray JA, Tutuian R, Orlando RC, Arnold R. Review article: the pathophysiology of gastro-oesophageal reflux disease - oesophageal manifestations. Aliment Pharmacol Ther. 2004;20(suppl 9):14-25.
23. Orr WC, Johnson LF. Responses to different levels of esophageal acidification during waking and sleeping. Dig Dis Sci. 1998;43:241-245.
24. Orr WC, Elsenbruch S, Harnish MJ, Johnson LF. Proximal migration of esophageal acid perfusions during waking and sleep. Am J Gastroenterol. 2000;95:37-42.
25. Orr WC, Heading R, Johnson LF, Kryger M. Review article: sleep and its relationship to gastro-oesophageal reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):39-46.
26. Schneyer LH, Pigman WW, Hanahan LL, Gilmore R. Rate of flow of human parotid sublingual, and submaxillary secretions during sleep. J Dent Res. 1956;35:109-114.
27. Dawes C. Circadian rhythms in human salivary flow rate and composition. J Physiol. 1972;220:529-545.
28. Lear CS, Flanagan JB, Jr, Moorrees CF. The frequency of deglutition in man. Arch Oral Biol. 1965;10:83-100.
29. Orr WC, Johnson LF, Robinson MG. Effect of sleep on swallowing, esophageal peristalsis, and acid clearance. Gastroenterology. 1984;86 (pt 1):814-819.
30. Elsenbruch S, Orr WC, Harnish MJ, Chen JD. Disruption of normal gastric myoelectric functioning by sleep. Sleep. 1999;22:453-458.
1. Jones R, Galmiche JP. Review: what do we mean by GERD?—definition and diagnosis. Aliment Pharmacol Ther. 2005;22(suppl 1):2-10.
2. Frank L, Kleinman L, Ganoczy D, et al. Upper gastrointestinal symptoms in North America: prevalence and relationship to healthcare utilization and quality of life. Dig Dis Sci. 2000;45:809-818.
3. Locke GR, III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ, III. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448-1456.
4. Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med. 2001;161:45-52.
5. Dubois RW, Fass R, Johnson LF, et al. Atypical nighttime symptoms of GERD among individuals with nighttime versus daytime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A288.-Abstract M999.
6. Orr WC, Allen ML, Robinson M. The pattern of nocturnal and diurnal esophageal acid exposure in the pathogenesis of erosive mucosal damage. Am J Gastroenterol. 1994;89:509-512.
7. Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976;184:459-470.
8. Cameron AJ, Lomboy CT. Barrett’s esophagus: age, prevalence, and extent of columnar epithelium. Gastroenterology. 1992;103:1241-1245.
9. Orr WC, Lackey C, Robinson MG, Johnson LF, Welsh JD. Esophageal acid clearance during sleep in patients with Barrett’s esophagus. Dig Dis Sci. 1988;33:654-659.
10. Eisen GM, Sandler RS, Murray S, Gottfried M. The relationship between gastroesophageal reflux disease and its complications with Barrett’s esophagus. Am J Gastroenterol. 1997;92:27-31.
11. Lagergren J, Bergstrom R, Lindgren A, Nyren O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825-831.
12. Dubois RW, Orr WC, Lange SM, et al. GERD-related sleep impairment among individuals with nighttime versus daytime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A288.-Abstract M998.
13. Dubois RW, Lange SM, Fass R, et al. Work productivity loss associated with nighttime GERD [abstract]. Gastroenterology. 2005;128(suppl 2):A286.-Abstract M988.
14. Dean BB, Crawley JA, Schmitt CM, Wong J, Ofman JJ. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther. 2003;17:1309-1317.
15. Shaker R, Castell DO, Schoenfeld PS, Spechler SJ. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function the results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol. 2003;98:1487-1493.
16. Dubois RW, Fass R, Lange SM, et al. Impact of nighttime GERD on health-related quality of life [abstract]. Gastroenterology. 2005;128:(4 Suppl 2):A286.-Abstract M989.
17. Fass R, Achem SR, Harding S, Mittal RK, Quigley E. Review article: supra-oesophageal manifestations of gastro-oesophageal reflux disease and the role of night-time gastro-oesophageal reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):26-38.
18. McGuigan JE, Belafsky PC, Fromer L, et al. Review article: diagnosis and management of night-time reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):57-72.
19. Gislason T, Janson C, Vermeire P, et al. Respiratory symptoms and nocturnal gastroesophageal reflux: a population-based study of young adults in three European countries. Chest. 2002;121:158-163.
20. Fass R, Quan SF, O’Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127:1658-1666.
21. Fisher BL, Pennathur A, Mutnick JL, Little AG. Obesity correlates with gastroesophageal reflux. Dig Dis Sci. 1999;44:2290-2294.
22. Castell DO, Murray JA, Tutuian R, Orlando RC, Arnold R. Review article: the pathophysiology of gastro-oesophageal reflux disease - oesophageal manifestations. Aliment Pharmacol Ther. 2004;20(suppl 9):14-25.
23. Orr WC, Johnson LF. Responses to different levels of esophageal acidification during waking and sleeping. Dig Dis Sci. 1998;43:241-245.
24. Orr WC, Elsenbruch S, Harnish MJ, Johnson LF. Proximal migration of esophageal acid perfusions during waking and sleep. Am J Gastroenterol. 2000;95:37-42.
25. Orr WC, Heading R, Johnson LF, Kryger M. Review article: sleep and its relationship to gastro-oesophageal reflux. Aliment Pharmacol Ther. 2004;20(suppl 9):39-46.
26. Schneyer LH, Pigman WW, Hanahan LL, Gilmore R. Rate of flow of human parotid sublingual, and submaxillary secretions during sleep. J Dent Res. 1956;35:109-114.
27. Dawes C. Circadian rhythms in human salivary flow rate and composition. J Physiol. 1972;220:529-545.
28. Lear CS, Flanagan JB, Jr, Moorrees CF. The frequency of deglutition in man. Arch Oral Biol. 1965;10:83-100.
29. Orr WC, Johnson LF, Robinson MG. Effect of sleep on swallowing, esophageal peristalsis, and acid clearance. Gastroenterology. 1984;86 (pt 1):814-819.
30. Elsenbruch S, Orr WC, Harnish MJ, Chen JD. Disruption of normal gastric myoelectric functioning by sleep. Sleep. 1999;22:453-458.
Acute Otitis Media: Influence of the PCV-7 vaccine on changes in the disease and its management
- Widespread use of the 7-valent pneumococcal conjugate vaccine has resulted in a shift in frequency of causative bacterial pathogens responsible for recurrent and persistent acute otitis media (AOM); disease management practice should encompass this change (SOR: B).
- High-dose amoxicillin is the first choice for antibiotic therapy in uncomplicated bacterial AOM, although β-lactamase–producing pathogens are increasingly common primary causative agents, and amoxicillin is susceptible to β-lactamase (SOR: B).
- Adding clavulanate to amoxicillin increases resistance to and improves effectiveness against β-lactamase–producing pathogens. Specific third-generation cephalosporins also should be included as antibiotic choices because of excellent activity against β-lactamase–producing pathogens and because of compliance advantages, such as better taste, less frequent dosing, and even shorter duration of therapy (SOR: B).
Since the approval of the 7-valent pneumococcal conjugate vaccine (PCV-7) for use in children younger than 24 months in February 2000, occurrences of acute otitis media (AOM) and the frequency of recurrent AOM have declined. Based on results from early clinical trials, PCV-7 may reduce total AOM by 6% to 8%, recurrent AOM by 10% to 26%, and tympanostomy tube placements by 24%.1,2
Acute otitis media occurs most frequently in children between the ages of 6 months and 18 months. By the end of their first year, approximately 86% of children will experience at least 1 episode of AOM.3
The condition remains a leading reason for visits to pediatricians and family physicians in the United States.4 It accounted for 16 million visits in 2000.4 This is a decrease from almost 25 million visits in 1995, prior to use of PCV-7. Additionally, AOM is associated with significant costs: In 1995, the direct and indirect costs of AOM were estimated to be about $3 billion.5
Changes in pathogen frequency for AOM in the ERA of PCV-7
The true impact of PCV-7 on management practice is not characterized by the modest reduction in incidence of uncomplicated AOM but in the PCV-7–associated shift in causative pathogens. Pre-PCV-7, 40% to 50% of cases of AOM in young children were caused by Streptococcus pneumoniae, 20% to 30% by Haemophilus influenzae, and 10% to 15% by Moraxella catarrhalis.6 In studies conducted prior to 2000, diagnostic tympanocentesis isolated S pneumoniae from 25% to 55% of all middle ear aspirates from children with AOM.6-8
Conversely, 1 study published in 2001 and 2 studies published in 2004 appear to document a reverse trend with the advent of the conjugate pneumococcal vaccine.9,10 Compared with children studied in an earlier era, those vaccinated with PCV-7 may be more likely to have H influenzae isolates. These studies will be described in detail below.
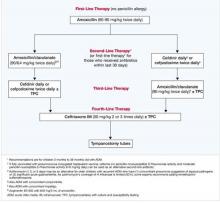
Bacterial AOM: initial antibiotic therapy and specific pathogens
Current guidelines recommend amoxicillin (45 mg/kg/day) or high-dose amoxicillin (80-90 mg/kg/day) as initial therapy in presumed or documented bacterial AOM.5 Although amoxicillin is effective against pneumococcus and β-lactamase–negative strains of H influenzae, it is ineffective against β-lactamase–positive strains of H influenzae.9 Significant initial failures may point to a changing pathogen per population frequency. A 2004 review assessed children with continued (persistence of infection detected within 30 days after treatment completion) or refractory (clinical failure while receiving antimicrobial therapy) AOM who have received high-dose amoxicillin as initial empiric therapy. The authors noted that the rate of infection due to H influenzae has increased from 43% among those treated prior to the licensure of PCV-7 to 57% among those who received 2 or more doses of PCV-7.10
Evidence from the medical literature
Three studies provide the major evidence concerning the pathogen shift associated with the adoption of the PCV-7 conjugate vaccine:
- The Finnish Otitis Media Vaccine Trial2
- A published collection of clinical trial results from a rural practice in Kentucky in which 94% of children were immunized with PCV-79
- A prospective study conducted in a suburban community-based private practice in Rochester, NY that evaluated children with persistent or nonresponsive AOM.10
The Finnish Otitis Media Vaccine Trial
In this trial, 1662 infants received either the PCV-7 vaccine or a control vaccine at ages 2, 4, 6, and 12 months and were monitored from ages 6.5 months to 24 months.2 An overall 6.9% reduction in episodes of clinical AOM were diagnosed (n=1251) in PCV-7–vaccinated children compared with the control group (n=1345). This suggested that fewer AOM cases were caused by the S pneumoniae vaccine serotypes than nonvaccine serotypes. The bacteriologic findings in the samples of middle ear fluid taken during 93% of the visits for AOM (TABLE 1) show a 34% reduction in culture-confirmed episodes in the PCV-7–vaccinated group, a decrease of more than 50% in pneumococcal AOM episodes caused by vaccine or vaccine cross-reactive serotypes, a 33% increase in infections caused by other pneumococcal serotypes, and an 11% increase in the proportion of AOM cases due to H influenzae.2
TABLE 1
Finnish Otitis Media Vaccine Trial: Causes of AOM Episodes and Impact of PCV-7 Immunization on Incidence
| CAUSE | PCV-7 EPISODES | CONTROL EPISODES | DIFFERENCE (%) |
|---|---|---|---|
| Culture-confirmed pneumococcus | 271 | 414 | 34 |
| Pneumococcal serotype in vaccine | 107 | 250 | 57 |
| Vaccine cross-reactive serotypes* | 41 | 84 | 51 |
| Other pneumococcal serotypes | 125 | 95 | 33 |
| Haemophilus influenzae | 315 | 287 | 11 |
| Moraxella catarrhalis | 379 | 381 | 1 |
| *6A, 9N, 18B, 19A, 23A. | |||
| AOM, acute otitis media; PCV-7, 7-valent pneumococcal conjugate vaccine. | |||
| Adapted with permission from Eskola J, et al. N Engl J Med. 2001;344:403-409. Copyright 2001 Massachusetts Medical Society. All rights reserved. | |||
Study Results From a Rural Kentucky Practice
In this practice, data on isolates from middle ear fluid were collected in children with severe or refractory AOM aged 7 to 24 months.9 Data were obtained from 1992 to 1998, before the introduction of PCV-7, and from 2000 to 2003, following immunization with 3 or 4 doses of PCV-7 during the first 18 months of life.
As shown in TABLE 2, the pre-PCV-7 group of children (N=336; 1992-1998) had a proportion of 48% culture-confirmed pneumococcus vs a proportion of 31% in the PCV-7-vaccinated group (N=83; 2000-2003), a 17% decrease. The decrease in proportion of AOM episodes resulting from vaccine serotypes was 34%.
In this investigation, 28% of the pre-PCV-7 group and 34% of the post-PCV-7 group had received antibiotic therapy within the previous 3 days. Additionally, 59% and 76%, respectively, had received antibiotic therapy within the preceding 30 days. There were increases of 30% in vaccine cross-reactive serotypes and 45% in nonvaccine serotypes. Vaccine cross-reactive serotypes 6A and 19A accounted for most of the penicillin-nonsusceptible S pneumoniae strains in the vaccinated population.
Most impressive, however, in the post-PCV-7 group, was that gram-negative bacteria, mainly H influenzae, accounted for two thirds of AOM isolates, an increase from 41% in the pre-PCV-7 group to 56% in the vaccinated group. A 56% increase was noted in β-lactamase–positive organisms from the pre-PCV-7 group to the post-PCV-7 group. The combined H influenzae and M catarrhalis β-lactamase–producing organisms accounted for nearly half of all isolates.9
TABLE 2
Results From a Rural Kentucky Practice: Change in AOM Microbiology From Pre-PCV-7 (1992–1998) to Post-PCV-7 (2000–2003)
| PATHOGEN | PRE-PCV-7 1992-1998 (N=336) | POST-PCV-7 2000-2003 (N=83) | CHANGE (%) | P VALUE | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Culture-confirmed pneumococcus | 160 | 48 | 26 | 31 | 17 | .007 |
| Pneumococcal serotype in vaccine | 236 | 70 | 30 | 36 | 34 | .003 |
| Vaccine cross-reactive serotypes* | 27 | 8 | 27 | 32 | 24 | .003 |
| Other pneumococcal serotypes† | 74 | 22 | 27 | 32 | 10 | NS |
| Haemophilus influenzae | 137 | 41 | 46 | 32 | 15 | .01 |
| β-lactamase-positive | 108 | 23 | 39 | 36 | 15 | .007 |
| Moraxella catarrhalis, β-lactamase-positive | 31 | 9 | 9 | 11 | 2 | NS |
| AOM, acute otitis media; n, total isolates; NS, nonsignificant; PCV-7, 7-valent pneumococcal conjugate vaccine. | ||||||
| *Includes 6A and 19A. | ||||||
| †Nonvaccine serotypes in post-PCV-7 group: 1, 11A, 15A, 29, and 33F. | ||||||
| Adapted with permission from Block SL, et al. Pediatr Infect Dis J. 2004;23:829-833. | ||||||
The Prospective Rochester, New York Study
Changes in pre- and post-PVC-7 patterns also were seen in a prospective study of 551 children with persistent or nonresponsive AOM (defined as nonresponders after 1 or 2 empiric antibiotic courses or failures after 48 hours of treatment). These children underwent tympanocentesis to identify bacterial isolates during the 9-year period from 1995 to 2003.10
From 1995 to 1997, enrollees received a standard dose of amoxicillin (40-50 mg/kg, divided into 3 doses daily) as initial empiric treatment. From 1998 to 2000 and 2001 to 2003, all children received high-dose amoxicillin (80-100 mg/kg, divided into twice-daily doses).
During the latter period, the children also were vaccinated with PCV-7, with 63% receiving the primary series of 3 doses and 10% receiving the booster dose. In this investigation, shortages in vaccine supply, discussed below, caused vaccination schedules to be compromised.
Study results (TABLE 3) show that in the post-PCV-7 group, there was a 13% decrease in the proportion of S pneumoniae isolates and a 14% increase in the proportion of H influenzae isolates compared with the pre-PCV-7 group (1998-2000 enrollees). An increase of 22% for β-lactamase–positive bacteria was also observed, along with a trend toward an increased proportion of penicillin-susceptible S pneumoniae isolates (58% vs 72%; P=.017) post-PCV-7.10 A 24% reduction (P=.009) in the frequency of the diagnosis of persistent or AOM treatment failure occurred in the period after PCV-7 vaccination. These changes were considered to be the result of the use of the conjugate pneumococcal vaccine rather than of the change in amoxicillin dosing.10
TABLE 3
The Prospective Rochester, New York Study: Pathogens Isolated in Persistent AOM and AOM Treatment Failure Pre- and Post-PCV-7
| PATHOGEN | PRE-PCV-7 1998-2000 (N=204) | POST-PCV-7 2000-2003 (N=152) | CHANGE (%) | P VALUE | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Streptococcus pneumoniae* | 50 | 44 | 28 | 31 | 13 | .017 |
| Penicillin nonsusceptible | 12 | 24 | 4 | 14 | 10 | NS |
| Haemophilus influenzae | 49 | 43 | 51 | 57 | 14 | .012 |
| β-lactamase-positive | 16 | 33 | 28 | 55 | 22 | .044 |
| Moraxella catarrhalis | 6 | 5 | 1 | 1 | 4 | NS |
| AOM, acute otitis media; N, total isolates; NS, nonsignificant; PCV-7, 7-valent pneumococcal conjugate vaccine. | ||||||
| *Pneumococcal serotyping was not done. | ||||||
| Adapted with permission from Casey JR, Pichichero ME. Pediatr Infect Dis J. 2004;23:824-828. | ||||||
Pneumococcal serotype shifts
In addition to the change in causative pathogens, use of the conjugate pneumococcal vaccine appears to have led to a significant shift in the pneumococcal strains causing AOM. Studies at urban medical centers and in the Kentucky practice documented an increase in the proportion of nonvaccine serotypes, accounting for 32% to 38% of pneumococcal AOM.10-12 A 33% increase was seen in the Finnish Trial.2 These nonvaccine pneumococcal serotypes do not carry the same level of resistance seen with those serotypes included in PCV-7.
PCV-7 conjugate vaccine
The PCV-7 conjugate vaccine was approved for use in February 2000. It is a 7-valent pneumococcal conjugate of the capsular antigens of the S pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F, individually conjugated to diphtheria CRM197 protein.13 These serotypes have been responsible for approximately 80% of invasive pneumococcal disease in children younger than 6 years in the United States.13,14 They also accounted for 74% of penicillin-susceptible S pneumoniae and 100% of pneumococci with high-level penicillin resistance isolated from children younger than age 6 years with invasive disease during a 1993-1994 surveillance by the Centers for Disease Control and Prevention (CDC).13
Mechanism of Action and Recommended Immunization Schedule
The conjugate vaccine is converted to a T-cell–dependent antigen, antibody formation is enhanced, and memory B cells are primed.14
The recommended immunization schedule was established as 3 primary doses at ages 2, 4, and 6 months and a booster dose at 12 to 15 months.1 It is the first multivalent pneumococcal vaccine approved for use in children younger than 24 months.
An 89% reduction in invasive pneumococcal disease was observed in children receiving 1 or more doses, and the vaccine appears to reduce nasopharyngeal carriage of vaccine serotypes.15,16
The older 23-valent polysaccharide vaccine does not stimulate good response in children younger than 2 years of age14 and does not reduce mucosal carriage or limit the spread of resistant strains.15
PCV-7 Supply Since 2000
In August 2001, a serious shortage of the vaccine developed in 34 state immunization programs.17 The following month, the CDC advised physicians to administer it only to children younger than 12 months and to those aged 1 to 5 years at increased risk of pneumococcal disease.18 As demand continued despite the change in recommendations, the CDC further changed recommendations to conserve vaccine supply, first suspending the fourth dose temporarily in healthy children19 and then discontinuing both the third and fourth doses.11 In July 2004, production problems seemed to have resolved; the CDC recommended that every child receive 3 doses. In September, supplies were adequate for return to the 4-dose schedule.12 As of June 2004, 67.7% of children aged 24 months had received 3 or more doses of PCV-7.20 Thus, the effects of PCV-7 on the changing microbiology of AOM may only now, at the end of 2005, be fully realized.
Herd Immunity and Reduction in Carriage
Despite the shortages of vaccine during the first years of use, evidence of herd immunity and a decrease in antibiotic resistance in pneumococcal pathogens has been reported throughout the United States.21,22 A 29% decrease in the rate of pneumococcal disease in both young children and adults has also been observed, along with a 35% reduction in the rate of disease caused by nonpenicillin-susceptible pneumococcal strains.21 The reduction in carriage among vaccinated children may be the reason.21,22 Because of the impact of PCV-7, it will be important to record immunization history when collecting AOM data.
AOM treatment choices
The basis of recommendations for treating AOM depends on the presumed responsible pathogens, their susceptibility to antibiotics, and concerns for developing resistance, all influenced by clinical trial data. In practice, however, empiric choices are often made based on knowledge of local resistance patterns and of other patient characteristics; that is cost concerns, adverse event profiles, need to avoid initial treatment failure, adherence issues (eg, taste or palatability), convenience, and duration of dosing regimen.
All current guidelines recommend oral amoxicillin as first-line therapy in documented or presumed bacterial AOM. The 2004 American Academy of Pediatrics/American Academy of Family Physicians’ (AAP/AAFP) guidelines4 recommended increasing the dosage used for empiric treatment from 40 to 45 mg/kg/day to 80 to 90 mg/kg/day for all children. This was a result of concerns about the prevalence of penicillin-resistant S pneumoniae for which standard-dose amoxicillin is inadequate.23
The guidelines were written and published before the data from the Kentucky and New York studies were available; therefore, although the guidelines recommended that empiric treatment of bacterial AOM should target S pneumoniae, H influenzae, and M catarrhalis, the pathogen shift discussed previously might today produce a modified antibiotic selection paradigm. The pathogen mix in persistent or recurrent AOM has already led to a guideline recommendation for high-dose amoxicillin/clavulanate, 90/6.4 mg/kg/day, cefdinir, cefprozil, cefpodoxime, cefuroxime, or ceftriaxone in these patients.23
If an increase in the proportion of β-lactamase–producing pathogens due to PCV-7 occurs, amoxicillin may no longer be the best first choice.
Selecting Among Recommended Antibiotic Choices
As antibiotic preparations for treating bacterial AOM are oral suspensions, taste is a major factor for pediatric patients. TABLE 4 summarizes comparative taste ratings for antibiotic suspensions based on several studies and shows the range, from those that can enhance compliance to those that discourage compliance.23
Adverse events, especially diarrhea, nausea/vomiting, and gastritis, are also of concern. These are shortcomings of amoxicillin/clavulanate, which has a higher incidence of diarrhea and nausea than cephalosporins.24
Dosing frequency is also a factor among recommended agents. Amoxicillin, amoxicillin/clavulanate, cefprozil, and cefpodoxime require twice-daily dosing. Cefdinir can be effective at once-daily dosing.24
Duration of approved therapy is perhaps the most critical selection factor given the reality of patient behaviors. Cefpodoxime and cefdinir are the only 2 FDA-approved agents for 5-day treatment of bacterial AOM that are also guideline-recommended.
TABLE 4
Compliance-Enhancing Ranking of Antibiotic Suspensions
| STRONGLY COMPLIANCE-ENHANCING | |
|
|
| MODERATELY COMPLIANCE-ENHANCING | |
|
|
| EQUIVOCAL COMPLIANCE-ENHANCING | |
| |
| NOT COMPLIANCE-ENHANCING | |
| |
| DISCOURAGES COMPLIANCE | |
|
|
| TMP-SMX, trimethoprim sulfamethoxazole | |
| Sources: Adapted from Steele RW, et al. Pediatr Infect Dis J. 2001;20:1-5. | |
| Demers DM, et al. Pediatr Infect Dis J. 1994;13:87-89. | |
| Ruff ME, et al. Pediatr Infect Dis J. 1991;10:30-33. | |
Choices for Effective Initial Therapy
Considering the changing microbial population in bacterial AOM and the increasing concern of effectiveness of amoxicillin and other antibiotics against β-lactamase–producing H influenzae, the choice of therapy may need modification. Specifically, that may mean changing the choice of effective antibiotic, taking into consideration the compliance-enhancing advantages of available options.
Based on efficacy, the overall prevalence of antibiotic-resistant AOM pathogens for PCV-7-vaccinated children, the potential for adverse effects, and patient compliance issues, Block and Harrison developed an algorithm (FIGURE) for the management of AOM diagnosed by strict criteria in an otherwise healthy child between 4 months and 36 months old.24 As the environment of AOM evolves, the choices for treatment must be not only effective but also the best and most appropriate.
FIGURE Antibiotic Choices for Acute Otitis Media in the 2000s
1. Fireman B, Black SB, Shinefield HR, et al. Impact of the pneumococcal conjugate vaccine on otitis media. Pediatr Infect Dis J. 2003;22:10-16.
2. Eskola J, Kilpi T, Palmu A, et al. Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med. 2001;344:403-409.
3. Block SL, Harrison CH, Hedrick J, et al. Restricted use of antibiotic prophylaxis for recurrent acute otitis media in the era of penicillin non-susceptible Streptococcus pneumoniae. Int J Pediatr Otorhinolaryngol. 2001;61:47-60.
4. Advisory Committee on Immunization Practices. Preventing pneumococcal disease among infants and young children: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2000;49(RR-9):1-35.
5. American Academy of Family Physicians Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451-1465.
6. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999;18:1-9.
7. Block SL. Causative pathogens, antibiotic resistance and therapeutic considerations in acute otitis media. Pediatr Infect Dis J. 1997;16:449-456.
8. Bluestone CD, Stephenson JS, Martin LM. Ten-year review of otitis media pathogens. Pediatr Infect Dis J. 1992;11(suppl 8):S7-S11.
9. Block SL, Hedrick J, Harrison CJ, et al. Community-wide vaccination with the heptavalent pneumococcal conjugate significantly alters the microbiology of acute otitis media. Pediatr Infect Dis J. 2004;23:829-833.
10. Casey JR, Pichichero ME. Changes in frequency and pathogens causing acute otitis media in 1995-2003. Pediatr Infect Dis J. 2004;23:824-828.
11. Centers for Disease Control and Prevention. Updated recommendations on the use of pneumococcal conjugate vaccine: suspension of recommendation for third and fourth dose. MMWR Morb Mortal Wkly Rep. 2004;53:177-178.
12. Centers for Disease Control and Prevention. Pneumococcal conjugate vaccine shortage resolved. MMWR Morb Mortal Wkly Rep. 2004;53:851-852.
13. Prevnar® (pneumococcal 7-valent vaccine) [prescribing information]. Philadelphia, Pa: Wyeth Pharmaceuticals. Rev. 01/04.
14. Watson W. Pneumococcal conjugate vaccines. Pediatr Infect Dis J. 2000;19:331-332.
15. Giebink GS. The prevention of pneumococcal disease in children. N Engl J Med. 2001;345:1177-1183.
16. Pelton SI, Loughlin AM, Marchand CD. Seven valent pneumococcal conjugate vaccine immunization in two Boston communities: changes in serotypes and antimicrobial susceptibility among Streptococcus pneumoniae isolates. Pediatr Infect Dis J. 2003;23:1015-1022.
17. Freed GL, Davis MM, Clark SJ. Variation in public and private supply of pneumococcal conjugate vaccine during a shortage. JAMA. 2003;289:575-578.
18. Centers for Disease Control and Prevention. Decreased availability of pneumococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep. 2001;50:783-784.
19. Centers for Disease Control and Prevention. Limited supply of pneumococcal conjugate vaccine: suspension of recommendation for fourth dose. MMWR Morb Mortal Wkly Rep. 2004;53:108-109.
20. CDC National Immunization Survey. Estimated vaccination coverage with individual vaccines and selected vaccination series by 24 months of age by state and immunization action plan area US, Q3/2003-Q4/2004. Available at: http://www2a.cdc.gov/nip/coverage/nis/nis_iap.asp?fmt=v&rpt=tab09_24mo_iap_0304&qtr=Q3/2003-Q2/2004. Accessed September 20, 2005.
21. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348:1737-1746.
22. Black S, Shinefield H, Baxter R, et al. Postlicensure surveillance for pneumococcal invasive disease after use of heptavalent pneumococcal vaccine in Northern California Kaiser Permanente. Pediatr Infect Dis J. 2004;23:485-489.
23. Pichichero ME, Casey JR. Acute otitis media: Making sense of recent guidelines on antimicrobial treatment. J Fam Pract. 2005;54:313-332.
24. Block SL, Harrison CJ. Diagnosis and Management of Acute Otitis Media, 3rd ed. In press.
- Widespread use of the 7-valent pneumococcal conjugate vaccine has resulted in a shift in frequency of causative bacterial pathogens responsible for recurrent and persistent acute otitis media (AOM); disease management practice should encompass this change (SOR: B).
- High-dose amoxicillin is the first choice for antibiotic therapy in uncomplicated bacterial AOM, although β-lactamase–producing pathogens are increasingly common primary causative agents, and amoxicillin is susceptible to β-lactamase (SOR: B).
- Adding clavulanate to amoxicillin increases resistance to and improves effectiveness against β-lactamase–producing pathogens. Specific third-generation cephalosporins also should be included as antibiotic choices because of excellent activity against β-lactamase–producing pathogens and because of compliance advantages, such as better taste, less frequent dosing, and even shorter duration of therapy (SOR: B).
Since the approval of the 7-valent pneumococcal conjugate vaccine (PCV-7) for use in children younger than 24 months in February 2000, occurrences of acute otitis media (AOM) and the frequency of recurrent AOM have declined. Based on results from early clinical trials, PCV-7 may reduce total AOM by 6% to 8%, recurrent AOM by 10% to 26%, and tympanostomy tube placements by 24%.1,2
Acute otitis media occurs most frequently in children between the ages of 6 months and 18 months. By the end of their first year, approximately 86% of children will experience at least 1 episode of AOM.3
The condition remains a leading reason for visits to pediatricians and family physicians in the United States.4 It accounted for 16 million visits in 2000.4 This is a decrease from almost 25 million visits in 1995, prior to use of PCV-7. Additionally, AOM is associated with significant costs: In 1995, the direct and indirect costs of AOM were estimated to be about $3 billion.5
Changes in pathogen frequency for AOM in the ERA of PCV-7
The true impact of PCV-7 on management practice is not characterized by the modest reduction in incidence of uncomplicated AOM but in the PCV-7–associated shift in causative pathogens. Pre-PCV-7, 40% to 50% of cases of AOM in young children were caused by Streptococcus pneumoniae, 20% to 30% by Haemophilus influenzae, and 10% to 15% by Moraxella catarrhalis.6 In studies conducted prior to 2000, diagnostic tympanocentesis isolated S pneumoniae from 25% to 55% of all middle ear aspirates from children with AOM.6-8
Conversely, 1 study published in 2001 and 2 studies published in 2004 appear to document a reverse trend with the advent of the conjugate pneumococcal vaccine.9,10 Compared with children studied in an earlier era, those vaccinated with PCV-7 may be more likely to have H influenzae isolates. These studies will be described in detail below.
Bacterial AOM: initial antibiotic therapy and specific pathogens
Current guidelines recommend amoxicillin (45 mg/kg/day) or high-dose amoxicillin (80-90 mg/kg/day) as initial therapy in presumed or documented bacterial AOM.5 Although amoxicillin is effective against pneumococcus and β-lactamase–negative strains of H influenzae, it is ineffective against β-lactamase–positive strains of H influenzae.9 Significant initial failures may point to a changing pathogen per population frequency. A 2004 review assessed children with continued (persistence of infection detected within 30 days after treatment completion) or refractory (clinical failure while receiving antimicrobial therapy) AOM who have received high-dose amoxicillin as initial empiric therapy. The authors noted that the rate of infection due to H influenzae has increased from 43% among those treated prior to the licensure of PCV-7 to 57% among those who received 2 or more doses of PCV-7.10
Evidence from the medical literature
Three studies provide the major evidence concerning the pathogen shift associated with the adoption of the PCV-7 conjugate vaccine:
- The Finnish Otitis Media Vaccine Trial2
- A published collection of clinical trial results from a rural practice in Kentucky in which 94% of children were immunized with PCV-79
- A prospective study conducted in a suburban community-based private practice in Rochester, NY that evaluated children with persistent or nonresponsive AOM.10
The Finnish Otitis Media Vaccine Trial
In this trial, 1662 infants received either the PCV-7 vaccine or a control vaccine at ages 2, 4, 6, and 12 months and were monitored from ages 6.5 months to 24 months.2 An overall 6.9% reduction in episodes of clinical AOM were diagnosed (n=1251) in PCV-7–vaccinated children compared with the control group (n=1345). This suggested that fewer AOM cases were caused by the S pneumoniae vaccine serotypes than nonvaccine serotypes. The bacteriologic findings in the samples of middle ear fluid taken during 93% of the visits for AOM (TABLE 1) show a 34% reduction in culture-confirmed episodes in the PCV-7–vaccinated group, a decrease of more than 50% in pneumococcal AOM episodes caused by vaccine or vaccine cross-reactive serotypes, a 33% increase in infections caused by other pneumococcal serotypes, and an 11% increase in the proportion of AOM cases due to H influenzae.2
TABLE 1
Finnish Otitis Media Vaccine Trial: Causes of AOM Episodes and Impact of PCV-7 Immunization on Incidence
| CAUSE | PCV-7 EPISODES | CONTROL EPISODES | DIFFERENCE (%) |
|---|---|---|---|
| Culture-confirmed pneumococcus | 271 | 414 | 34 |
| Pneumococcal serotype in vaccine | 107 | 250 | 57 |
| Vaccine cross-reactive serotypes* | 41 | 84 | 51 |
| Other pneumococcal serotypes | 125 | 95 | 33 |
| Haemophilus influenzae | 315 | 287 | 11 |
| Moraxella catarrhalis | 379 | 381 | 1 |
| *6A, 9N, 18B, 19A, 23A. | |||
| AOM, acute otitis media; PCV-7, 7-valent pneumococcal conjugate vaccine. | |||
| Adapted with permission from Eskola J, et al. N Engl J Med. 2001;344:403-409. Copyright 2001 Massachusetts Medical Society. All rights reserved. | |||
Study Results From a Rural Kentucky Practice
In this practice, data on isolates from middle ear fluid were collected in children with severe or refractory AOM aged 7 to 24 months.9 Data were obtained from 1992 to 1998, before the introduction of PCV-7, and from 2000 to 2003, following immunization with 3 or 4 doses of PCV-7 during the first 18 months of life.
As shown in TABLE 2, the pre-PCV-7 group of children (N=336; 1992-1998) had a proportion of 48% culture-confirmed pneumococcus vs a proportion of 31% in the PCV-7-vaccinated group (N=83; 2000-2003), a 17% decrease. The decrease in proportion of AOM episodes resulting from vaccine serotypes was 34%.
In this investigation, 28% of the pre-PCV-7 group and 34% of the post-PCV-7 group had received antibiotic therapy within the previous 3 days. Additionally, 59% and 76%, respectively, had received antibiotic therapy within the preceding 30 days. There were increases of 30% in vaccine cross-reactive serotypes and 45% in nonvaccine serotypes. Vaccine cross-reactive serotypes 6A and 19A accounted for most of the penicillin-nonsusceptible S pneumoniae strains in the vaccinated population.
Most impressive, however, in the post-PCV-7 group, was that gram-negative bacteria, mainly H influenzae, accounted for two thirds of AOM isolates, an increase from 41% in the pre-PCV-7 group to 56% in the vaccinated group. A 56% increase was noted in β-lactamase–positive organisms from the pre-PCV-7 group to the post-PCV-7 group. The combined H influenzae and M catarrhalis β-lactamase–producing organisms accounted for nearly half of all isolates.9
TABLE 2
Results From a Rural Kentucky Practice: Change in AOM Microbiology From Pre-PCV-7 (1992–1998) to Post-PCV-7 (2000–2003)
| PATHOGEN | PRE-PCV-7 1992-1998 (N=336) | POST-PCV-7 2000-2003 (N=83) | CHANGE (%) | P VALUE | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Culture-confirmed pneumococcus | 160 | 48 | 26 | 31 | 17 | .007 |
| Pneumococcal serotype in vaccine | 236 | 70 | 30 | 36 | 34 | .003 |
| Vaccine cross-reactive serotypes* | 27 | 8 | 27 | 32 | 24 | .003 |
| Other pneumococcal serotypes† | 74 | 22 | 27 | 32 | 10 | NS |
| Haemophilus influenzae | 137 | 41 | 46 | 32 | 15 | .01 |
| β-lactamase-positive | 108 | 23 | 39 | 36 | 15 | .007 |
| Moraxella catarrhalis, β-lactamase-positive | 31 | 9 | 9 | 11 | 2 | NS |
| AOM, acute otitis media; n, total isolates; NS, nonsignificant; PCV-7, 7-valent pneumococcal conjugate vaccine. | ||||||
| *Includes 6A and 19A. | ||||||
| †Nonvaccine serotypes in post-PCV-7 group: 1, 11A, 15A, 29, and 33F. | ||||||
| Adapted with permission from Block SL, et al. Pediatr Infect Dis J. 2004;23:829-833. | ||||||
The Prospective Rochester, New York Study
Changes in pre- and post-PVC-7 patterns also were seen in a prospective study of 551 children with persistent or nonresponsive AOM (defined as nonresponders after 1 or 2 empiric antibiotic courses or failures after 48 hours of treatment). These children underwent tympanocentesis to identify bacterial isolates during the 9-year period from 1995 to 2003.10
From 1995 to 1997, enrollees received a standard dose of amoxicillin (40-50 mg/kg, divided into 3 doses daily) as initial empiric treatment. From 1998 to 2000 and 2001 to 2003, all children received high-dose amoxicillin (80-100 mg/kg, divided into twice-daily doses).
During the latter period, the children also were vaccinated with PCV-7, with 63% receiving the primary series of 3 doses and 10% receiving the booster dose. In this investigation, shortages in vaccine supply, discussed below, caused vaccination schedules to be compromised.
Study results (TABLE 3) show that in the post-PCV-7 group, there was a 13% decrease in the proportion of S pneumoniae isolates and a 14% increase in the proportion of H influenzae isolates compared with the pre-PCV-7 group (1998-2000 enrollees). An increase of 22% for β-lactamase–positive bacteria was also observed, along with a trend toward an increased proportion of penicillin-susceptible S pneumoniae isolates (58% vs 72%; P=.017) post-PCV-7.10 A 24% reduction (P=.009) in the frequency of the diagnosis of persistent or AOM treatment failure occurred in the period after PCV-7 vaccination. These changes were considered to be the result of the use of the conjugate pneumococcal vaccine rather than of the change in amoxicillin dosing.10
TABLE 3
The Prospective Rochester, New York Study: Pathogens Isolated in Persistent AOM and AOM Treatment Failure Pre- and Post-PCV-7
| PATHOGEN | PRE-PCV-7 1998-2000 (N=204) | POST-PCV-7 2000-2003 (N=152) | CHANGE (%) | P VALUE | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Streptococcus pneumoniae* | 50 | 44 | 28 | 31 | 13 | .017 |
| Penicillin nonsusceptible | 12 | 24 | 4 | 14 | 10 | NS |
| Haemophilus influenzae | 49 | 43 | 51 | 57 | 14 | .012 |
| β-lactamase-positive | 16 | 33 | 28 | 55 | 22 | .044 |
| Moraxella catarrhalis | 6 | 5 | 1 | 1 | 4 | NS |
| AOM, acute otitis media; N, total isolates; NS, nonsignificant; PCV-7, 7-valent pneumococcal conjugate vaccine. | ||||||
| *Pneumococcal serotyping was not done. | ||||||
| Adapted with permission from Casey JR, Pichichero ME. Pediatr Infect Dis J. 2004;23:824-828. | ||||||
Pneumococcal serotype shifts
In addition to the change in causative pathogens, use of the conjugate pneumococcal vaccine appears to have led to a significant shift in the pneumococcal strains causing AOM. Studies at urban medical centers and in the Kentucky practice documented an increase in the proportion of nonvaccine serotypes, accounting for 32% to 38% of pneumococcal AOM.10-12 A 33% increase was seen in the Finnish Trial.2 These nonvaccine pneumococcal serotypes do not carry the same level of resistance seen with those serotypes included in PCV-7.
PCV-7 conjugate vaccine
The PCV-7 conjugate vaccine was approved for use in February 2000. It is a 7-valent pneumococcal conjugate of the capsular antigens of the S pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F, individually conjugated to diphtheria CRM197 protein.13 These serotypes have been responsible for approximately 80% of invasive pneumococcal disease in children younger than 6 years in the United States.13,14 They also accounted for 74% of penicillin-susceptible S pneumoniae and 100% of pneumococci with high-level penicillin resistance isolated from children younger than age 6 years with invasive disease during a 1993-1994 surveillance by the Centers for Disease Control and Prevention (CDC).13
Mechanism of Action and Recommended Immunization Schedule
The conjugate vaccine is converted to a T-cell–dependent antigen, antibody formation is enhanced, and memory B cells are primed.14
The recommended immunization schedule was established as 3 primary doses at ages 2, 4, and 6 months and a booster dose at 12 to 15 months.1 It is the first multivalent pneumococcal vaccine approved for use in children younger than 24 months.
An 89% reduction in invasive pneumococcal disease was observed in children receiving 1 or more doses, and the vaccine appears to reduce nasopharyngeal carriage of vaccine serotypes.15,16
The older 23-valent polysaccharide vaccine does not stimulate good response in children younger than 2 years of age14 and does not reduce mucosal carriage or limit the spread of resistant strains.15
PCV-7 Supply Since 2000
In August 2001, a serious shortage of the vaccine developed in 34 state immunization programs.17 The following month, the CDC advised physicians to administer it only to children younger than 12 months and to those aged 1 to 5 years at increased risk of pneumococcal disease.18 As demand continued despite the change in recommendations, the CDC further changed recommendations to conserve vaccine supply, first suspending the fourth dose temporarily in healthy children19 and then discontinuing both the third and fourth doses.11 In July 2004, production problems seemed to have resolved; the CDC recommended that every child receive 3 doses. In September, supplies were adequate for return to the 4-dose schedule.12 As of June 2004, 67.7% of children aged 24 months had received 3 or more doses of PCV-7.20 Thus, the effects of PCV-7 on the changing microbiology of AOM may only now, at the end of 2005, be fully realized.
Herd Immunity and Reduction in Carriage
Despite the shortages of vaccine during the first years of use, evidence of herd immunity and a decrease in antibiotic resistance in pneumococcal pathogens has been reported throughout the United States.21,22 A 29% decrease in the rate of pneumococcal disease in both young children and adults has also been observed, along with a 35% reduction in the rate of disease caused by nonpenicillin-susceptible pneumococcal strains.21 The reduction in carriage among vaccinated children may be the reason.21,22 Because of the impact of PCV-7, it will be important to record immunization history when collecting AOM data.
AOM treatment choices
The basis of recommendations for treating AOM depends on the presumed responsible pathogens, their susceptibility to antibiotics, and concerns for developing resistance, all influenced by clinical trial data. In practice, however, empiric choices are often made based on knowledge of local resistance patterns and of other patient characteristics; that is cost concerns, adverse event profiles, need to avoid initial treatment failure, adherence issues (eg, taste or palatability), convenience, and duration of dosing regimen.
All current guidelines recommend oral amoxicillin as first-line therapy in documented or presumed bacterial AOM. The 2004 American Academy of Pediatrics/American Academy of Family Physicians’ (AAP/AAFP) guidelines4 recommended increasing the dosage used for empiric treatment from 40 to 45 mg/kg/day to 80 to 90 mg/kg/day for all children. This was a result of concerns about the prevalence of penicillin-resistant S pneumoniae for which standard-dose amoxicillin is inadequate.23
The guidelines were written and published before the data from the Kentucky and New York studies were available; therefore, although the guidelines recommended that empiric treatment of bacterial AOM should target S pneumoniae, H influenzae, and M catarrhalis, the pathogen shift discussed previously might today produce a modified antibiotic selection paradigm. The pathogen mix in persistent or recurrent AOM has already led to a guideline recommendation for high-dose amoxicillin/clavulanate, 90/6.4 mg/kg/day, cefdinir, cefprozil, cefpodoxime, cefuroxime, or ceftriaxone in these patients.23
If an increase in the proportion of β-lactamase–producing pathogens due to PCV-7 occurs, amoxicillin may no longer be the best first choice.
Selecting Among Recommended Antibiotic Choices
As antibiotic preparations for treating bacterial AOM are oral suspensions, taste is a major factor for pediatric patients. TABLE 4 summarizes comparative taste ratings for antibiotic suspensions based on several studies and shows the range, from those that can enhance compliance to those that discourage compliance.23
Adverse events, especially diarrhea, nausea/vomiting, and gastritis, are also of concern. These are shortcomings of amoxicillin/clavulanate, which has a higher incidence of diarrhea and nausea than cephalosporins.24
Dosing frequency is also a factor among recommended agents. Amoxicillin, amoxicillin/clavulanate, cefprozil, and cefpodoxime require twice-daily dosing. Cefdinir can be effective at once-daily dosing.24
Duration of approved therapy is perhaps the most critical selection factor given the reality of patient behaviors. Cefpodoxime and cefdinir are the only 2 FDA-approved agents for 5-day treatment of bacterial AOM that are also guideline-recommended.
TABLE 4
Compliance-Enhancing Ranking of Antibiotic Suspensions
| STRONGLY COMPLIANCE-ENHANCING | |
|
|
| MODERATELY COMPLIANCE-ENHANCING | |
|
|
| EQUIVOCAL COMPLIANCE-ENHANCING | |
| |
| NOT COMPLIANCE-ENHANCING | |
| |
| DISCOURAGES COMPLIANCE | |
|
|
| TMP-SMX, trimethoprim sulfamethoxazole | |
| Sources: Adapted from Steele RW, et al. Pediatr Infect Dis J. 2001;20:1-5. | |
| Demers DM, et al. Pediatr Infect Dis J. 1994;13:87-89. | |
| Ruff ME, et al. Pediatr Infect Dis J. 1991;10:30-33. | |
Choices for Effective Initial Therapy
Considering the changing microbial population in bacterial AOM and the increasing concern of effectiveness of amoxicillin and other antibiotics against β-lactamase–producing H influenzae, the choice of therapy may need modification. Specifically, that may mean changing the choice of effective antibiotic, taking into consideration the compliance-enhancing advantages of available options.
Based on efficacy, the overall prevalence of antibiotic-resistant AOM pathogens for PCV-7-vaccinated children, the potential for adverse effects, and patient compliance issues, Block and Harrison developed an algorithm (FIGURE) for the management of AOM diagnosed by strict criteria in an otherwise healthy child between 4 months and 36 months old.24 As the environment of AOM evolves, the choices for treatment must be not only effective but also the best and most appropriate.
FIGURE Antibiotic Choices for Acute Otitis Media in the 2000s
- Widespread use of the 7-valent pneumococcal conjugate vaccine has resulted in a shift in frequency of causative bacterial pathogens responsible for recurrent and persistent acute otitis media (AOM); disease management practice should encompass this change (SOR: B).
- High-dose amoxicillin is the first choice for antibiotic therapy in uncomplicated bacterial AOM, although β-lactamase–producing pathogens are increasingly common primary causative agents, and amoxicillin is susceptible to β-lactamase (SOR: B).
- Adding clavulanate to amoxicillin increases resistance to and improves effectiveness against β-lactamase–producing pathogens. Specific third-generation cephalosporins also should be included as antibiotic choices because of excellent activity against β-lactamase–producing pathogens and because of compliance advantages, such as better taste, less frequent dosing, and even shorter duration of therapy (SOR: B).
Since the approval of the 7-valent pneumococcal conjugate vaccine (PCV-7) for use in children younger than 24 months in February 2000, occurrences of acute otitis media (AOM) and the frequency of recurrent AOM have declined. Based on results from early clinical trials, PCV-7 may reduce total AOM by 6% to 8%, recurrent AOM by 10% to 26%, and tympanostomy tube placements by 24%.1,2
Acute otitis media occurs most frequently in children between the ages of 6 months and 18 months. By the end of their first year, approximately 86% of children will experience at least 1 episode of AOM.3
The condition remains a leading reason for visits to pediatricians and family physicians in the United States.4 It accounted for 16 million visits in 2000.4 This is a decrease from almost 25 million visits in 1995, prior to use of PCV-7. Additionally, AOM is associated with significant costs: In 1995, the direct and indirect costs of AOM were estimated to be about $3 billion.5
Changes in pathogen frequency for AOM in the ERA of PCV-7
The true impact of PCV-7 on management practice is not characterized by the modest reduction in incidence of uncomplicated AOM but in the PCV-7–associated shift in causative pathogens. Pre-PCV-7, 40% to 50% of cases of AOM in young children were caused by Streptococcus pneumoniae, 20% to 30% by Haemophilus influenzae, and 10% to 15% by Moraxella catarrhalis.6 In studies conducted prior to 2000, diagnostic tympanocentesis isolated S pneumoniae from 25% to 55% of all middle ear aspirates from children with AOM.6-8
Conversely, 1 study published in 2001 and 2 studies published in 2004 appear to document a reverse trend with the advent of the conjugate pneumococcal vaccine.9,10 Compared with children studied in an earlier era, those vaccinated with PCV-7 may be more likely to have H influenzae isolates. These studies will be described in detail below.
Bacterial AOM: initial antibiotic therapy and specific pathogens
Current guidelines recommend amoxicillin (45 mg/kg/day) or high-dose amoxicillin (80-90 mg/kg/day) as initial therapy in presumed or documented bacterial AOM.5 Although amoxicillin is effective against pneumococcus and β-lactamase–negative strains of H influenzae, it is ineffective against β-lactamase–positive strains of H influenzae.9 Significant initial failures may point to a changing pathogen per population frequency. A 2004 review assessed children with continued (persistence of infection detected within 30 days after treatment completion) or refractory (clinical failure while receiving antimicrobial therapy) AOM who have received high-dose amoxicillin as initial empiric therapy. The authors noted that the rate of infection due to H influenzae has increased from 43% among those treated prior to the licensure of PCV-7 to 57% among those who received 2 or more doses of PCV-7.10
Evidence from the medical literature
Three studies provide the major evidence concerning the pathogen shift associated with the adoption of the PCV-7 conjugate vaccine:
- The Finnish Otitis Media Vaccine Trial2
- A published collection of clinical trial results from a rural practice in Kentucky in which 94% of children were immunized with PCV-79
- A prospective study conducted in a suburban community-based private practice in Rochester, NY that evaluated children with persistent or nonresponsive AOM.10
The Finnish Otitis Media Vaccine Trial
In this trial, 1662 infants received either the PCV-7 vaccine or a control vaccine at ages 2, 4, 6, and 12 months and were monitored from ages 6.5 months to 24 months.2 An overall 6.9% reduction in episodes of clinical AOM were diagnosed (n=1251) in PCV-7–vaccinated children compared with the control group (n=1345). This suggested that fewer AOM cases were caused by the S pneumoniae vaccine serotypes than nonvaccine serotypes. The bacteriologic findings in the samples of middle ear fluid taken during 93% of the visits for AOM (TABLE 1) show a 34% reduction in culture-confirmed episodes in the PCV-7–vaccinated group, a decrease of more than 50% in pneumococcal AOM episodes caused by vaccine or vaccine cross-reactive serotypes, a 33% increase in infections caused by other pneumococcal serotypes, and an 11% increase in the proportion of AOM cases due to H influenzae.2
TABLE 1
Finnish Otitis Media Vaccine Trial: Causes of AOM Episodes and Impact of PCV-7 Immunization on Incidence
| CAUSE | PCV-7 EPISODES | CONTROL EPISODES | DIFFERENCE (%) |
|---|---|---|---|
| Culture-confirmed pneumococcus | 271 | 414 | 34 |
| Pneumococcal serotype in vaccine | 107 | 250 | 57 |
| Vaccine cross-reactive serotypes* | 41 | 84 | 51 |
| Other pneumococcal serotypes | 125 | 95 | 33 |
| Haemophilus influenzae | 315 | 287 | 11 |
| Moraxella catarrhalis | 379 | 381 | 1 |
| *6A, 9N, 18B, 19A, 23A. | |||
| AOM, acute otitis media; PCV-7, 7-valent pneumococcal conjugate vaccine. | |||
| Adapted with permission from Eskola J, et al. N Engl J Med. 2001;344:403-409. Copyright 2001 Massachusetts Medical Society. All rights reserved. | |||
Study Results From a Rural Kentucky Practice
In this practice, data on isolates from middle ear fluid were collected in children with severe or refractory AOM aged 7 to 24 months.9 Data were obtained from 1992 to 1998, before the introduction of PCV-7, and from 2000 to 2003, following immunization with 3 or 4 doses of PCV-7 during the first 18 months of life.
As shown in TABLE 2, the pre-PCV-7 group of children (N=336; 1992-1998) had a proportion of 48% culture-confirmed pneumococcus vs a proportion of 31% in the PCV-7-vaccinated group (N=83; 2000-2003), a 17% decrease. The decrease in proportion of AOM episodes resulting from vaccine serotypes was 34%.
In this investigation, 28% of the pre-PCV-7 group and 34% of the post-PCV-7 group had received antibiotic therapy within the previous 3 days. Additionally, 59% and 76%, respectively, had received antibiotic therapy within the preceding 30 days. There were increases of 30% in vaccine cross-reactive serotypes and 45% in nonvaccine serotypes. Vaccine cross-reactive serotypes 6A and 19A accounted for most of the penicillin-nonsusceptible S pneumoniae strains in the vaccinated population.
Most impressive, however, in the post-PCV-7 group, was that gram-negative bacteria, mainly H influenzae, accounted for two thirds of AOM isolates, an increase from 41% in the pre-PCV-7 group to 56% in the vaccinated group. A 56% increase was noted in β-lactamase–positive organisms from the pre-PCV-7 group to the post-PCV-7 group. The combined H influenzae and M catarrhalis β-lactamase–producing organisms accounted for nearly half of all isolates.9
TABLE 2
Results From a Rural Kentucky Practice: Change in AOM Microbiology From Pre-PCV-7 (1992–1998) to Post-PCV-7 (2000–2003)
| PATHOGEN | PRE-PCV-7 1992-1998 (N=336) | POST-PCV-7 2000-2003 (N=83) | CHANGE (%) | P VALUE | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Culture-confirmed pneumococcus | 160 | 48 | 26 | 31 | 17 | .007 |
| Pneumococcal serotype in vaccine | 236 | 70 | 30 | 36 | 34 | .003 |
| Vaccine cross-reactive serotypes* | 27 | 8 | 27 | 32 | 24 | .003 |
| Other pneumococcal serotypes† | 74 | 22 | 27 | 32 | 10 | NS |
| Haemophilus influenzae | 137 | 41 | 46 | 32 | 15 | .01 |
| β-lactamase-positive | 108 | 23 | 39 | 36 | 15 | .007 |
| Moraxella catarrhalis, β-lactamase-positive | 31 | 9 | 9 | 11 | 2 | NS |
| AOM, acute otitis media; n, total isolates; NS, nonsignificant; PCV-7, 7-valent pneumococcal conjugate vaccine. | ||||||
| *Includes 6A and 19A. | ||||||
| †Nonvaccine serotypes in post-PCV-7 group: 1, 11A, 15A, 29, and 33F. | ||||||
| Adapted with permission from Block SL, et al. Pediatr Infect Dis J. 2004;23:829-833. | ||||||
The Prospective Rochester, New York Study
Changes in pre- and post-PVC-7 patterns also were seen in a prospective study of 551 children with persistent or nonresponsive AOM (defined as nonresponders after 1 or 2 empiric antibiotic courses or failures after 48 hours of treatment). These children underwent tympanocentesis to identify bacterial isolates during the 9-year period from 1995 to 2003.10
From 1995 to 1997, enrollees received a standard dose of amoxicillin (40-50 mg/kg, divided into 3 doses daily) as initial empiric treatment. From 1998 to 2000 and 2001 to 2003, all children received high-dose amoxicillin (80-100 mg/kg, divided into twice-daily doses).
During the latter period, the children also were vaccinated with PCV-7, with 63% receiving the primary series of 3 doses and 10% receiving the booster dose. In this investigation, shortages in vaccine supply, discussed below, caused vaccination schedules to be compromised.
Study results (TABLE 3) show that in the post-PCV-7 group, there was a 13% decrease in the proportion of S pneumoniae isolates and a 14% increase in the proportion of H influenzae isolates compared with the pre-PCV-7 group (1998-2000 enrollees). An increase of 22% for β-lactamase–positive bacteria was also observed, along with a trend toward an increased proportion of penicillin-susceptible S pneumoniae isolates (58% vs 72%; P=.017) post-PCV-7.10 A 24% reduction (P=.009) in the frequency of the diagnosis of persistent or AOM treatment failure occurred in the period after PCV-7 vaccination. These changes were considered to be the result of the use of the conjugate pneumococcal vaccine rather than of the change in amoxicillin dosing.10
TABLE 3
The Prospective Rochester, New York Study: Pathogens Isolated in Persistent AOM and AOM Treatment Failure Pre- and Post-PCV-7
| PATHOGEN | PRE-PCV-7 1998-2000 (N=204) | POST-PCV-7 2000-2003 (N=152) | CHANGE (%) | P VALUE | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Streptococcus pneumoniae* | 50 | 44 | 28 | 31 | 13 | .017 |
| Penicillin nonsusceptible | 12 | 24 | 4 | 14 | 10 | NS |
| Haemophilus influenzae | 49 | 43 | 51 | 57 | 14 | .012 |
| β-lactamase-positive | 16 | 33 | 28 | 55 | 22 | .044 |
| Moraxella catarrhalis | 6 | 5 | 1 | 1 | 4 | NS |
| AOM, acute otitis media; N, total isolates; NS, nonsignificant; PCV-7, 7-valent pneumococcal conjugate vaccine. | ||||||
| *Pneumococcal serotyping was not done. | ||||||
| Adapted with permission from Casey JR, Pichichero ME. Pediatr Infect Dis J. 2004;23:824-828. | ||||||
Pneumococcal serotype shifts
In addition to the change in causative pathogens, use of the conjugate pneumococcal vaccine appears to have led to a significant shift in the pneumococcal strains causing AOM. Studies at urban medical centers and in the Kentucky practice documented an increase in the proportion of nonvaccine serotypes, accounting for 32% to 38% of pneumococcal AOM.10-12 A 33% increase was seen in the Finnish Trial.2 These nonvaccine pneumococcal serotypes do not carry the same level of resistance seen with those serotypes included in PCV-7.
PCV-7 conjugate vaccine
The PCV-7 conjugate vaccine was approved for use in February 2000. It is a 7-valent pneumococcal conjugate of the capsular antigens of the S pneumoniae serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F, individually conjugated to diphtheria CRM197 protein.13 These serotypes have been responsible for approximately 80% of invasive pneumococcal disease in children younger than 6 years in the United States.13,14 They also accounted for 74% of penicillin-susceptible S pneumoniae and 100% of pneumococci with high-level penicillin resistance isolated from children younger than age 6 years with invasive disease during a 1993-1994 surveillance by the Centers for Disease Control and Prevention (CDC).13
Mechanism of Action and Recommended Immunization Schedule
The conjugate vaccine is converted to a T-cell–dependent antigen, antibody formation is enhanced, and memory B cells are primed.14
The recommended immunization schedule was established as 3 primary doses at ages 2, 4, and 6 months and a booster dose at 12 to 15 months.1 It is the first multivalent pneumococcal vaccine approved for use in children younger than 24 months.
An 89% reduction in invasive pneumococcal disease was observed in children receiving 1 or more doses, and the vaccine appears to reduce nasopharyngeal carriage of vaccine serotypes.15,16
The older 23-valent polysaccharide vaccine does not stimulate good response in children younger than 2 years of age14 and does not reduce mucosal carriage or limit the spread of resistant strains.15
PCV-7 Supply Since 2000
In August 2001, a serious shortage of the vaccine developed in 34 state immunization programs.17 The following month, the CDC advised physicians to administer it only to children younger than 12 months and to those aged 1 to 5 years at increased risk of pneumococcal disease.18 As demand continued despite the change in recommendations, the CDC further changed recommendations to conserve vaccine supply, first suspending the fourth dose temporarily in healthy children19 and then discontinuing both the third and fourth doses.11 In July 2004, production problems seemed to have resolved; the CDC recommended that every child receive 3 doses. In September, supplies were adequate for return to the 4-dose schedule.12 As of June 2004, 67.7% of children aged 24 months had received 3 or more doses of PCV-7.20 Thus, the effects of PCV-7 on the changing microbiology of AOM may only now, at the end of 2005, be fully realized.
Herd Immunity and Reduction in Carriage
Despite the shortages of vaccine during the first years of use, evidence of herd immunity and a decrease in antibiotic resistance in pneumococcal pathogens has been reported throughout the United States.21,22 A 29% decrease in the rate of pneumococcal disease in both young children and adults has also been observed, along with a 35% reduction in the rate of disease caused by nonpenicillin-susceptible pneumococcal strains.21 The reduction in carriage among vaccinated children may be the reason.21,22 Because of the impact of PCV-7, it will be important to record immunization history when collecting AOM data.
AOM treatment choices
The basis of recommendations for treating AOM depends on the presumed responsible pathogens, their susceptibility to antibiotics, and concerns for developing resistance, all influenced by clinical trial data. In practice, however, empiric choices are often made based on knowledge of local resistance patterns and of other patient characteristics; that is cost concerns, adverse event profiles, need to avoid initial treatment failure, adherence issues (eg, taste or palatability), convenience, and duration of dosing regimen.
All current guidelines recommend oral amoxicillin as first-line therapy in documented or presumed bacterial AOM. The 2004 American Academy of Pediatrics/American Academy of Family Physicians’ (AAP/AAFP) guidelines4 recommended increasing the dosage used for empiric treatment from 40 to 45 mg/kg/day to 80 to 90 mg/kg/day for all children. This was a result of concerns about the prevalence of penicillin-resistant S pneumoniae for which standard-dose amoxicillin is inadequate.23
The guidelines were written and published before the data from the Kentucky and New York studies were available; therefore, although the guidelines recommended that empiric treatment of bacterial AOM should target S pneumoniae, H influenzae, and M catarrhalis, the pathogen shift discussed previously might today produce a modified antibiotic selection paradigm. The pathogen mix in persistent or recurrent AOM has already led to a guideline recommendation for high-dose amoxicillin/clavulanate, 90/6.4 mg/kg/day, cefdinir, cefprozil, cefpodoxime, cefuroxime, or ceftriaxone in these patients.23
If an increase in the proportion of β-lactamase–producing pathogens due to PCV-7 occurs, amoxicillin may no longer be the best first choice.
Selecting Among Recommended Antibiotic Choices
As antibiotic preparations for treating bacterial AOM are oral suspensions, taste is a major factor for pediatric patients. TABLE 4 summarizes comparative taste ratings for antibiotic suspensions based on several studies and shows the range, from those that can enhance compliance to those that discourage compliance.23
Adverse events, especially diarrhea, nausea/vomiting, and gastritis, are also of concern. These are shortcomings of amoxicillin/clavulanate, which has a higher incidence of diarrhea and nausea than cephalosporins.24
Dosing frequency is also a factor among recommended agents. Amoxicillin, amoxicillin/clavulanate, cefprozil, and cefpodoxime require twice-daily dosing. Cefdinir can be effective at once-daily dosing.24
Duration of approved therapy is perhaps the most critical selection factor given the reality of patient behaviors. Cefpodoxime and cefdinir are the only 2 FDA-approved agents for 5-day treatment of bacterial AOM that are also guideline-recommended.
TABLE 4
Compliance-Enhancing Ranking of Antibiotic Suspensions
| STRONGLY COMPLIANCE-ENHANCING | |
|
|
| MODERATELY COMPLIANCE-ENHANCING | |
|
|
| EQUIVOCAL COMPLIANCE-ENHANCING | |
| |
| NOT COMPLIANCE-ENHANCING | |
| |
| DISCOURAGES COMPLIANCE | |
|
|
| TMP-SMX, trimethoprim sulfamethoxazole | |
| Sources: Adapted from Steele RW, et al. Pediatr Infect Dis J. 2001;20:1-5. | |
| Demers DM, et al. Pediatr Infect Dis J. 1994;13:87-89. | |
| Ruff ME, et al. Pediatr Infect Dis J. 1991;10:30-33. | |
Choices for Effective Initial Therapy
Considering the changing microbial population in bacterial AOM and the increasing concern of effectiveness of amoxicillin and other antibiotics against β-lactamase–producing H influenzae, the choice of therapy may need modification. Specifically, that may mean changing the choice of effective antibiotic, taking into consideration the compliance-enhancing advantages of available options.
Based on efficacy, the overall prevalence of antibiotic-resistant AOM pathogens for PCV-7-vaccinated children, the potential for adverse effects, and patient compliance issues, Block and Harrison developed an algorithm (FIGURE) for the management of AOM diagnosed by strict criteria in an otherwise healthy child between 4 months and 36 months old.24 As the environment of AOM evolves, the choices for treatment must be not only effective but also the best and most appropriate.
FIGURE Antibiotic Choices for Acute Otitis Media in the 2000s
1. Fireman B, Black SB, Shinefield HR, et al. Impact of the pneumococcal conjugate vaccine on otitis media. Pediatr Infect Dis J. 2003;22:10-16.
2. Eskola J, Kilpi T, Palmu A, et al. Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med. 2001;344:403-409.
3. Block SL, Harrison CH, Hedrick J, et al. Restricted use of antibiotic prophylaxis for recurrent acute otitis media in the era of penicillin non-susceptible Streptococcus pneumoniae. Int J Pediatr Otorhinolaryngol. 2001;61:47-60.
4. Advisory Committee on Immunization Practices. Preventing pneumococcal disease among infants and young children: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2000;49(RR-9):1-35.
5. American Academy of Family Physicians Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451-1465.
6. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999;18:1-9.
7. Block SL. Causative pathogens, antibiotic resistance and therapeutic considerations in acute otitis media. Pediatr Infect Dis J. 1997;16:449-456.
8. Bluestone CD, Stephenson JS, Martin LM. Ten-year review of otitis media pathogens. Pediatr Infect Dis J. 1992;11(suppl 8):S7-S11.
9. Block SL, Hedrick J, Harrison CJ, et al. Community-wide vaccination with the heptavalent pneumococcal conjugate significantly alters the microbiology of acute otitis media. Pediatr Infect Dis J. 2004;23:829-833.
10. Casey JR, Pichichero ME. Changes in frequency and pathogens causing acute otitis media in 1995-2003. Pediatr Infect Dis J. 2004;23:824-828.
11. Centers for Disease Control and Prevention. Updated recommendations on the use of pneumococcal conjugate vaccine: suspension of recommendation for third and fourth dose. MMWR Morb Mortal Wkly Rep. 2004;53:177-178.
12. Centers for Disease Control and Prevention. Pneumococcal conjugate vaccine shortage resolved. MMWR Morb Mortal Wkly Rep. 2004;53:851-852.
13. Prevnar® (pneumococcal 7-valent vaccine) [prescribing information]. Philadelphia, Pa: Wyeth Pharmaceuticals. Rev. 01/04.
14. Watson W. Pneumococcal conjugate vaccines. Pediatr Infect Dis J. 2000;19:331-332.
15. Giebink GS. The prevention of pneumococcal disease in children. N Engl J Med. 2001;345:1177-1183.
16. Pelton SI, Loughlin AM, Marchand CD. Seven valent pneumococcal conjugate vaccine immunization in two Boston communities: changes in serotypes and antimicrobial susceptibility among Streptococcus pneumoniae isolates. Pediatr Infect Dis J. 2003;23:1015-1022.
17. Freed GL, Davis MM, Clark SJ. Variation in public and private supply of pneumococcal conjugate vaccine during a shortage. JAMA. 2003;289:575-578.
18. Centers for Disease Control and Prevention. Decreased availability of pneumococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep. 2001;50:783-784.
19. Centers for Disease Control and Prevention. Limited supply of pneumococcal conjugate vaccine: suspension of recommendation for fourth dose. MMWR Morb Mortal Wkly Rep. 2004;53:108-109.
20. CDC National Immunization Survey. Estimated vaccination coverage with individual vaccines and selected vaccination series by 24 months of age by state and immunization action plan area US, Q3/2003-Q4/2004. Available at: http://www2a.cdc.gov/nip/coverage/nis/nis_iap.asp?fmt=v&rpt=tab09_24mo_iap_0304&qtr=Q3/2003-Q2/2004. Accessed September 20, 2005.
21. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348:1737-1746.
22. Black S, Shinefield H, Baxter R, et al. Postlicensure surveillance for pneumococcal invasive disease after use of heptavalent pneumococcal vaccine in Northern California Kaiser Permanente. Pediatr Infect Dis J. 2004;23:485-489.
23. Pichichero ME, Casey JR. Acute otitis media: Making sense of recent guidelines on antimicrobial treatment. J Fam Pract. 2005;54:313-332.
24. Block SL, Harrison CJ. Diagnosis and Management of Acute Otitis Media, 3rd ed. In press.
1. Fireman B, Black SB, Shinefield HR, et al. Impact of the pneumococcal conjugate vaccine on otitis media. Pediatr Infect Dis J. 2003;22:10-16.
2. Eskola J, Kilpi T, Palmu A, et al. Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med. 2001;344:403-409.
3. Block SL, Harrison CH, Hedrick J, et al. Restricted use of antibiotic prophylaxis for recurrent acute otitis media in the era of penicillin non-susceptible Streptococcus pneumoniae. Int J Pediatr Otorhinolaryngol. 2001;61:47-60.
4. Advisory Committee on Immunization Practices. Preventing pneumococcal disease among infants and young children: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2000;49(RR-9):1-35.
5. American Academy of Family Physicians Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113:1451-1465.
6. Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the Drug-resistant Streptococcus pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999;18:1-9.
7. Block SL. Causative pathogens, antibiotic resistance and therapeutic considerations in acute otitis media. Pediatr Infect Dis J. 1997;16:449-456.
8. Bluestone CD, Stephenson JS, Martin LM. Ten-year review of otitis media pathogens. Pediatr Infect Dis J. 1992;11(suppl 8):S7-S11.
9. Block SL, Hedrick J, Harrison CJ, et al. Community-wide vaccination with the heptavalent pneumococcal conjugate significantly alters the microbiology of acute otitis media. Pediatr Infect Dis J. 2004;23:829-833.
10. Casey JR, Pichichero ME. Changes in frequency and pathogens causing acute otitis media in 1995-2003. Pediatr Infect Dis J. 2004;23:824-828.
11. Centers for Disease Control and Prevention. Updated recommendations on the use of pneumococcal conjugate vaccine: suspension of recommendation for third and fourth dose. MMWR Morb Mortal Wkly Rep. 2004;53:177-178.
12. Centers for Disease Control and Prevention. Pneumococcal conjugate vaccine shortage resolved. MMWR Morb Mortal Wkly Rep. 2004;53:851-852.
13. Prevnar® (pneumococcal 7-valent vaccine) [prescribing information]. Philadelphia, Pa: Wyeth Pharmaceuticals. Rev. 01/04.
14. Watson W. Pneumococcal conjugate vaccines. Pediatr Infect Dis J. 2000;19:331-332.
15. Giebink GS. The prevention of pneumococcal disease in children. N Engl J Med. 2001;345:1177-1183.
16. Pelton SI, Loughlin AM, Marchand CD. Seven valent pneumococcal conjugate vaccine immunization in two Boston communities: changes in serotypes and antimicrobial susceptibility among Streptococcus pneumoniae isolates. Pediatr Infect Dis J. 2003;23:1015-1022.
17. Freed GL, Davis MM, Clark SJ. Variation in public and private supply of pneumococcal conjugate vaccine during a shortage. JAMA. 2003;289:575-578.
18. Centers for Disease Control and Prevention. Decreased availability of pneumococcal conjugate vaccine. MMWR Morb Mortal Wkly Rep. 2001;50:783-784.
19. Centers for Disease Control and Prevention. Limited supply of pneumococcal conjugate vaccine: suspension of recommendation for fourth dose. MMWR Morb Mortal Wkly Rep. 2004;53:108-109.
20. CDC National Immunization Survey. Estimated vaccination coverage with individual vaccines and selected vaccination series by 24 months of age by state and immunization action plan area US, Q3/2003-Q4/2004. Available at: http://www2a.cdc.gov/nip/coverage/nis/nis_iap.asp?fmt=v&rpt=tab09_24mo_iap_0304&qtr=Q3/2003-Q2/2004. Accessed September 20, 2005.
21. Whitney CG, Farley MM, Hadler J, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med. 2003;348:1737-1746.
22. Black S, Shinefield H, Baxter R, et al. Postlicensure surveillance for pneumococcal invasive disease after use of heptavalent pneumococcal vaccine in Northern California Kaiser Permanente. Pediatr Infect Dis J. 2004;23:485-489.
23. Pichichero ME, Casey JR. Acute otitis media: Making sense of recent guidelines on antimicrobial treatment. J Fam Pract. 2005;54:313-332.
24. Block SL, Harrison CJ. Diagnosis and Management of Acute Otitis Media, 3rd ed. In press.
Treating Community-acquired Bacterial Respiratory Tract Infections: Update on Etiology, Diagnosis, and Antimicrobial Therapy
Acute bacterial sinusitis (ABS), acute bacterial exacerbations of chronic bronchitis (ABECB), and community-acquired pneumonia (CAP) are 3 respiratory tract infections (RTIs) in adults that pose a treatment challenge for clinicians in the primary care setting. Each of these conditions requires prompt initiation of therapy to achieve optimal patient outcomes, but diagnosis and selection of treatment typically are made without the benefit of diagnostic tests. Due to increasingly high levels of antibiotic resistance,1,2 the decision to treat and the selection of therapy are critically important.3-5
This article briefly reviews the etiology of community-acquired bacterial RTIs, important diagnostic considerations, and current treatment options for patients who have these infections.
- Most community-acquired respiratory tract infections (RTIs) are not bacterial; therefore, patients do not require antibiotic treatment.
- Antibiotic therapy for community-acquired bacterial RTIs, including acute bacterial sinusitis (ABS), acute bacterial exacerbations of chronic bronchitis (ABECB), and community-acquired pneumonia (CAP), is typically empiric and requires careful evaluation of patients and antibiotics.
- Common respiratory tract pathogens, including Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, are becoming increasingly resistant to currently used antibiotics.
- To reduce the development of drug-resistant bacteria and maintain their effectiveness, new-generation antimicrobials should be used only to treat infections that have been proven or are strongly suspected to be caused by bacteria.
Community-acquired respiratory tract infections: Viral vs bacterial
The debate regarding whether to prescribe antibiotics for patients with community-acquired RTIs continues, since most of these infections are viral. Approximately 2% of patients with acute sinusitis have a bacterial infection.4,6 The etiology of acute exacerbations of chronic bronchitis (AECB) is only about 50% bacterial; other causes for these exacerbations include viruses, allergens, and environmental pollutants.3 Among ambulatory patients with CAP, even when diagnostic testing is performed, the causative pathogen cannot be identified in 40% to 50% of patients.7 All of these findings support the view that many cases of acute sinusitis, AECB, or CAP are not caused by bacteria and patients with these types of infections will not benefit from antimicrobial therapy. A diagnostic challenge to primary care physicians is determining which patients have a bacterial infection.
Differential diagnosis of bacterial infection in patients with community-acquired respiratory tract infections
National and international guidelines have been developed to assist clinicians in the differential diagnosis of bacterial infections.7-11
Acute sinusitis
Clinical diagnosis of acute sinusitis is based primarily on medical history, symptoms, and physical findings.14 A wide range of symptoms may occur in patients with acute sinusitis, as it does in patients with a common cold; TABLE 1shows the symptoms most likely to be associated with sinusitis.12 No single clinical sign or symptom distinguishes between bacterial and viral causes of acute sinusitis; rather, it is the combination of these signs or symptoms that may lead to the diagnosis of bacterial sinusitis. A history of purulent secretions and symptoms that appear more severe than those typically associated with an upper RTI suggests ABS;13 however, purulent discharge alone is not always indicative of a bacterial infection. “Double-sickening,” in which the patient becomes ill and then gets worse, combined with elevation in Creactive protein may indicate a bacterial infection.14 Williams et al15 recommended that clinical diagnosis emphasize key features such as maxillary toothache, poor response to over-the counter decongestants or antihistamines, a history of colored nasal discharge, abnormal transillumination, and mucopurulent discharge on examination. A diagnosis of ABS may be made if symptoms persist for more than 10 days, worsen after 5 to 7 days, or are more severe than those normally associated with viral upper respiratory illness.8,13
TABLE 1
Signs and symptoms associated with community-acquired respiratory tract infections3,13,14,17
| Acute sinusitis | |
| Major | Minor |
|
|
| Acute exacerbation of chronic bronchitis | |
| Increased | |
| |
| Community-acquired pneumonia | |
| |
| *Facial pain/pressure alone does not constitute a suggestive history in the absence of another finding listed in the “major” category. | |
| †Fever in acute sinusitis alone does not constitute a suggestive history in the absence of another finding listed in the “major” category. | |
Acute exacerbations of chronic bronchitis
There is no definitive agreement regarding what constitutes an AECB. Symptoms originally described by Anthonisen et al16 are commonly used to define AECB: increased cough and sputum, increased sputum purulence, and increased dyspnea over baseline (TABLE 1).17 A thorough physical and detailed medical history usually are sufficient to diagnose AECB while ruling out conditions such as pneumonia, congestive heart failure, myocardial ischemia, upper RTI, pulmonary embolism, and recurrent aspiration. A chest x-ray or an electrocardiogram may help with differential diagnosis in some patients.17,18 Nevertheless, determination of whether an acute exacerbation is bacterial or viral may be difficult because many patients with this disease have persistent airway colonization with the same bacteria thought to be responsible for AECB. To help physicians decide if antibiotics are necessary, practice guidelines have stratified patients by type of exacerbation (mild, moderate, or severe) and risk factors (TABLE 2).
TABLE 2
Treatment of acute exacerbations of chronic bronchitis8
| Type | Symptoms* | Antimicrobial therapy |
|---|---|---|
| Type 1 — Severe exacerbation | 3 of 3 symptoms | More benefit than when treated with placebo |
| Type 2 — Moderate exacerbation | 2 of 3 symptoms | Less benefit than when treated with placebo |
| Type 3 — Mild exacerbation | 1 of 3 symptoms | No benefit |
| * Increased dyspnea, increased sputum volume, and increased sputum purulence. | ||
Community-acquired pneumonia
Patients with CAP usually present with acute onset of lower respiratory symptoms (TABLE 1). Older and immunosuppressed patients may present with nonrespiratory symptoms, such as confusion, worsening of a chronic condition, or even falls. It is important to note that no combination of clinical signs and symptoms is a definitive diagnosis of CAP.19 All patients with suspected CAP should have a chest radiograph with posteroanterior and lateral views, as radiographs are essential for confirming a diagnosis.3 The Infectious Diseases Society of America (IDSA) and the American Thoracic Society support use of the Pneumonia PORT (Pneumonia Outcomes Research Team) Severity Index (PSI) as a means of risk stratification, combined with careful assessment of the patient and use of clinical judgment when determining whether a patient can be treated on an outpatient basis or should be hospitalized.10
Although it is important to attempt to identify the infecting organism, antimicrobial treatment for CAP is empiric because of the time it takes to get laboratory results and the potential for rapid deterioration of the patient’s condition. Further, patients with CAP may not produce sputum for Gram stain and culture; or, if they do, it may be mixed with upper respiratory tract secretions. Streptococcus pneumoniae may not grow from sputum culture; or, if found, it may be unclear whether the patient is colonized or infected.20 Bacteria cultures may not be helpful either, as blood cultures usually are sterile in patients with CAP.20
Selection of antimicrobial therapy
Once a bacterial infection is suspected, antibiotic treatment should be initiated promptly. Antibiotic therapy for ABS, ABECB, and CAP is simplified somewhat because the distributions of bacterial pathogens associated with each infection overlap substantially. The pathogens encountered most often in patients with ABS are Spneumoniae, Haemophilusinfluenzae, and Moraxella catarrhalis. To a lesser extent, anaerobic bacteria, other streptococcal species (including S pyogenes, S intermedius, and ahemolytic streptococci), and Staphylococcus aureusalso have been shown to cause ABS.21
Bacteria are isolated from the sputum of 40% to 60% of patients with AECB, and the predominant species are consistent with those listed for ABS. Atypical respiratory pathogens, most notably Chlamydophila(previously Chlamydia) pneumoniae, account for about 5% to 10% of organisms isolated from patients with ABECB.17 Patients with CAP also tend to be infected with the above-listed typical pathogens as well as the atypical Mycoplasma pneumoniae, C pneumoniae, and Legionella pneumophila. TABLE 3 lists pathogens associated with community-acquired bacterial RTIs and the effectiveness of commonly used antibiotics and telithromycin, a recently approved antimicrobial agent.
TABLE 3
Pathogens associated with ABS, CAP, and ABECB and in vitro effectiveness of commonly used antibiotics and telithromycin40
| Amoxicillin | Amoxicillin/Clavulanate | Cefuroxime | Erythro-mycin | Clarithro-mycin | Azithro-mycin | Moxi-floxacin | Telithro-mycin | |
|---|---|---|---|---|---|---|---|---|
| Streptococcus pneumoniae* | + | + | + | + | + | + | + | + |
| Resistant | ±† | – | – | – | – | – | + | + |
| Haemophilus influenzae | ||||||||
| β-lactamase negative | + | + | + | ± | ± | ± | + | + |
| β-lactamase positive | – | + | + | ± | ± | ± | + | + |
| Moraxella catarrhalis | + | + | + | + | + | + | + | + |
| Mycoplasma pneumoniae | – | – | – | + | + | + | + | + |
| Chlamydophila pneumonoae | – | – | – | + | + | + | + | + |
| Legionellasp | – | – | – | + | + | + | + | + |
| ABS = acute bacterial sinusitis | ||||||||
| CAP = community-acquired pneumonia | ||||||||
| ABECB = acute bacterial exacerbations of chronic bronchitis | ||||||||
| + = effective. | ||||||||
| – = not active. | ||||||||
| ±= significant resistance, but active against most strains. | ||||||||
| *Resistance is increasing; nationwide survey suggests 21% to 43% resistance to penicillin. | ||||||||
| †Amoxicillin doses of 80 mg/kg/d may be effective against nonmeningeal, penicillin-resistant S pneumoniae. | ||||||||
Resistance of bacterial pathogens
Although the common causative pathogens for community-acquired bacterial RTIs are few, selection of antibiotic therapy is becoming more complicated by the increasing rate of bacterial resistance to many of the antibiotics commonly used to treat these RTIs.
Resistance has been documented for all organisms associated with community-acquired RTIs. Current estimates indicate that 25% to more than 50% of Spneumoniaestrains are not completely susceptible to penicillin and that nearly one third of strains may be resistant to macrolides.22 Penicillin-resistant Spneumoniaealso may have reduced susceptibility to other antibiotics, including tetracycline, erythromycin, azithromycin, cephalosporins, clindamycin, trimethoprim/sulfamethoxazole (TMP/ SMX), and chloramphenicol.23Streptococcuspneumoniae have developed resistance to fluoroquinolones as well. This is of particular concern to the Centers for Disease Control and Prevention (CDC), having influenced its recommendations regarding empiric treatment of pneumonia.10 Macrolides have been mainstays in empiric therapy of CAP because of their activity against both typical and atypical respiratory pathogens; however, their effectiveness has been compromised by a rapid rise in resistance by S pneumoniae. Recent evaluation of Spneumoniae isolates collected between 2000 and 2001 showed that resistance rates to erythromycin, clarithromycin, and azithromycin had increased to 31.0%, 30.7%, and 31.0%, respectively.24 Further, results from 1 recent surveillance study that examined macrolide resistance among patients with community-acquired RTIs being treated by primary care physicians indicated that 23% to 33% of Spneumoniaeisolates were resistant to macrolides.24,25 Resistance also is becoming prevalent among other pathogens associated with community-acquired RTIs, including H influenzaeand Mcatarrhalis.25-27 This may complicate management of patients with community-acquired RTIs; infection with a treatment-resistant pathogen can increase risk for morbidity and mortality if treatment fails to eradicate the bacteria.20,28 However, the clinical impact of resistance remains controversial. Resistance may be overcome with the use of an antibiotic with pharmacokinetic properties or a dosing regimen that achieves very high drug concentrations at sites of infection. Host defense mechanisms also may contribute to eradication of organisms with in vitro resistance to an antibiotic.29,30 Further, since many infections are caused by viruses with high-resolution rates and since some bacterial infections resolve due to host response, the in vivo efficacy of an antibiotic may be much higher than its in vitro sensitivity.
Antibiotics currently prescribed for patients with community-acquired bacterialRTIs
Empiric antibiotic therapy for patients with community-acquired bacterial RTIs should provide coverage against clinically important pathogens likely to be associated with these infections, including resistant strains (TABLE 3). The antibiotic selected should specifically target respiratory pathogens. For example, broad-spectrum antibiotics are not the optimum choice, as they affect both respiratory and nonrespiratory pathogens (eg, gram-negative enterics; Escherichia coliand Klebsiella pneumoniae), which may result in resistance among these organisms.1,31
Antibiotics suitable for treatment of patients with ABS are summarized inTABLE 4. These agents vary widely in their spectra of activity as well as their ability to overcome pathogen resistance (TABLE 3). Amoxicillin, a very narrow-spectrum -lactam, generally is considered to be first-line therapy for children and adults who have ABS32 but may have little activity against resistant strains of S pneumoniae, H influenzae, and M catarrhalis.2
An analysis by the Agency for Healthcare Research and Quality concluded that amoxicillin or folate inhibitors (eg, TMP/SMX) are the most cost-effective choices for initial therapy in an otherwise healthy adult population with uncomplicated ABS.33 For adults who fail to improve after 2 to 3 days, broad-spectrum and β-lactamase-resistant antibiotics for 7 to 14 days should be considered. A clinical practice guideline sponsored by the American Academy of Family Physicians, the American College of Physicians-Society of Internal Medicine, the CDC, and the IDSA recommends initiating treatment with narrow-spectrum agents, eg, amoxicillin, doxycycline, or TMP-SMX for patients with severe or persistent moderate symptoms of ABS.34,35
High-dose amoxicillin/clavulanate 2000/125 mg, twice daily, was shown to be effective in treating patients with ABS, ABECB, and CAP caused by S pneumoniae, including penicillin-resistant S pneumoniae.29
The macrolides erythromycin, clarithromycin, and azithromycin are effective against susceptible strains of all organisms commonly associated with ABS, but many strains of S pneumoniaealso are resistant to these drugs.23,26 Respiratory fluoroquinolones are effective against all pathogens commonly associated with ABS, including resistant strains;26 however, they also have significant activity against gram-negative enterobacteriaceae and thus may increase the potential for emergence of resistant strains of these organisms.36 Ketolides are derived from the macrolide class and were designed to be effective against macrolide-resistant, gram-positive cocci.10 The first ketolide, telithromycin, is an alternative to macrolides for the treatment of patients with ABS, ABECB, and CAP. It is highly active against both common and atypical respiratory pathogens, including resistant strains, but has little activity against either enterobacteriaceae or anaerobes.37
All of the same considerations mentioned for the treatment of ABS also apply to the selection of therapy for patients with ABECB or CAP (TABLE 4). Empiric antimicrobial therapy for these 2 conditions, particularly CAP, also must cover atypical respiratory pathogens.17,38 For a number of years, monotherapy with a macrolide provided coverage against all of the pathogens likely to be associated with CAP and ABECB. In light of the emergence of resistance to these drugs by S pneumoniae, physicians should consider local and regional resistance rates before prescribing. In fact, File and colleagues39 have suggested that current recommendations favoring the use of macrolides in patients with CAP may have to be reconsidered if clinical failure continues to be observed with these agents. Cunha38 has taken an even stronger position, stating that macrolide monotherapy should be avoided in patients with CAP because of the high prevalence of S pneumoni-aeresistance to this class of antibiotics. These authors’ conclusions should be carefully weighed against the CDC’s and IDSA’s recommendations. The CDC previously recommended combination of macrolides and ceftriaxone for hospitalized patients to avoid emergence of fluoroquinolone resistance. The IDSA recommended empiric use of fluoroquinolones with conversion based on culture sensitivities when available.
TABLE 4
Antibiotics currently being used for the treatment of community-acquired bacterial respiratory tract infections41-44
| Generic | ABS* | CAP† | ABECB‡ |
|---|---|---|---|
| β-Lactams | |||
| Amoxicillin | 500 mg every 8 hours | 500 mg to 1 g every 8 hours | 500 mg 3 times daily |
| Amoxicillin/clavulanate | 500 mg every 8 hours | 500 mg/125 mg every 8 hours or 875 mg/125 mg every 12 hours | 875/125 mg bid |
| Cefuroxime | 250 to 500 mg twice daily | 500 mg twice daily | 500 mg twice daily |
| Macrolides | |||
| Clarithromycin | 500 mg every 12 hours for 14 days | 250–500 mg every 12 hours | 500 or 750 mg every 12 hours for 7 to 14 days |
| Clarithromycin extended- release tablets | 1000 mg once daily for 14 days | 1000 mg once daily for 7 days | 1000 mg once daily for 7 days |
| Azithromycin | 500 mg once daily for 3 days | 500 mg first day, then 250 mg/day for 2 to 5 days | 500 mg once daily for 3 days or 500 mg first day, then 250 mg/day for 4 days |
| Erythromycin | 250 to 500 mg twice daily | 250 or 500 mg 3 or 4 times daily | |
| Fluoroquinolone | |||
| Moxifloxacin | 400 mg once daily for 10 days | 400 mg once daily for 7 to 14 days | 400 mg once daily for 5 days |
| Ketolide | |||
| Telithromycin | 800 mg once daily for 5 days | 800 mg once daily for 7 to 10 days | 800 mg once daily for 5 days |
| Other Antibiotics | |||
| Trimethoprim- Sulfamethoxazole | 160 mg trimethoprim and 800 mg sulfamethoxale every 12 hours for 14 days | ||
| *Treatment is for 10 to 14 days unless otherwise indicated. | |||
| †Treatment ranges from 7 to 14 days unless otherwise noted. | |||
| ‡Treatment is for 10 days unless otherwise noted. | |||
Conclusions
Appropriate prescribing of antibiotics can effectively slow the development of bacterial resistance. Before selecting an antibiotic for a patient with a community-acquired RTI, primary care clinicians should first evaluate whether such treatment is even necessary. Treatment of ABS, ABECB, or CAP is compromised by increasing pathogen resistance to the currently used antibiotics. Use of high-dose amoxicillin and the other “older” antibiotics may delay the emergence of resistance to “newer” drugs, making newer drugs useful for treatment of more difficult cases. New agents to the antibiotic armamentarium give primary care physicians additional therapeutic options for patients who present with bacterial RTIs.
Financial disclosure:
Stephen Brunton, MD, is a consultant for and a member of the speakers’ bureaus for Aventis Pharmaceuticals Inc and Ortho-McNeil Pharmaceutical Inc.
1. Whitney CG, Farley MM, Hadler J, et al. for the Active Bacterial Core Surveillance Program of the Emerging Infections Program network. Increasing prevalence of multidrug-resistant Streptococcus pneumoniaein the United States. N Engl J Med. 2000;343:1917-1924.
2. Jacobs MR, Felmingham D, Appelbaum PC, Grüneberg RN; the Alexander Project Group. The Alexander Project 1998-2000: susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother. 2003;52:229-246.
3. File TM, , Jr. Overview of community-acquired respiratory tract infections. In: Nightingale CH, Ambrose PG, File TM, Jr., eds. Community-Acquired Respiratory Infections: Antimicrobial Management. New York, NY: Marcel Dekker, Inc; 2003;1-30.
4. Ben-David D, Rubinstein E. Appropriate use of antibiotics for respiratory infections: review of recent statements and position papers. Curr Opin Infect Dis. 2002;15:151-156.
5. Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. 2001;33:757-762.
6. Gwaltney JM, , Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996;23:1209-1225.
7. Niederman MS, Mandell LA, Anzueto A, et al. American Thoracic Society Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163:1730-1754.
8. Anon JB, Jacobs MR, Poole MD, et al. Sinus and Allergy Health Partnership Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130:1-45.
9. Snow V, Mottur-Pilson C, Gonzales R. for the American College of Physicians-American Society of Internal Medicine Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med. 2001;134:518-520.
10. Mandell LA, Bartlett JG, Dowell SF, File TM, , Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003;37:1405-1433.
11. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med. 2001;134:521-529.
12. Bishai WR. I>ssues in the management of bacterial sinusitis. Otolaryngol Head Neck Surg. 2002;127:S3-S9.
13. Osguthorpe JD. Adult rhinosinusitis: diagnosis and management. Am Fam Physician. 2001;63:69-76.
14. Lindbaek M, Hjortdahl P, Johnsen UL. Use of symptoms, signs, and blood tests to diagnose acute sinus infections in primary care: comparison with computed tomography. Fam Med .1996;28:183-188.
15. Williams JW, Jr, Holleman DR, Jr, Samsa GP, Simel DL. Randomized controlled trial of 3 vs 10 days of trimethoprim/sulfamethoxazole for acute maxillary sinusitis. JAMA. 1995;273:1015-1021.
16. Anthonisen NR, Manfreda J, Warren CPW, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
17. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117:380S-385S.
18. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117:398S-401S.
19. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440-1445.
20. Lonks JR. What is the clinical impact of macrolide resistance? Curr Infect Dis Rep. 2004;6:7-12.
21. Sokol W. Epidemiology of sinusitis in the primary care setting: results from the 1999-2000 Respiratory Surveillance Program. Am J Med. 2001;111(suppl 9A):19S-24S.
22. Appelbaum PC. Resistance among Streptococcus pneumoniae: implications for drug selection. Clin Infect Dis. 2002;34:1613-1620.
23. Doern GV, Brueggemann AB, Huynh H, Wingert E, Rhomberg P. Antimicrobial resistance with Streptococcus pneumoniae in the United States, 1997-1998. Emerg Infect Dis. 1999;5:757-765.
24. Doern GV, Brown SD. Antimicrobial susceptibility among community-acquired respiratory tract pathogens in the USA: data from PROTEKT US 2000-01. J Infect. 2004;48:56-65.
25. Pfaller MA, Jones RN. Gatifloxacin phase IV surveillance trial (TeqCES study) utilizing 5000 primary care physician practices: report of pathogens isolated and susceptibility patterns in community-acquired respiratory tract infections. Diagn Microbiol Infect Dis. 2002;44:77-84.
26. Hoban D, Waites K, Felmingham D. Antimicrobial susceptibility of community-acquired respiratory tract pathogens in North America in 1999-2000: findings of the PROTEKT surveillance study. Diagn Microbiol Infect Dis. 2003;45:251-259.
27. Dunbar LM. Current issues in the management of bacterial respiratory tract disease: the challenge of antibacterial resistance. Am J Med Sci. 2003;326:360-368.
28. Garau J. The hidden impact of antibacterial resistance in respiratory tract infection. Clinical failures: the tip of the iceberg? Respir Med. 2001;95(suppl A)-S5-11.
29. File TM, , Jr, Jacobs MR, Poole MD, Wynne B. 546, 547, 548, 549, 550, 551, 556, 557 and 592 Clinical Study Groups. Outcome of treatment of respiratory tract infections due to Streptococcus pneumoniae, including drug-resistant strains, with pharmacokinetically enhanced amoxycillin/clavulanate. Int J Antimicrob Agents. 2002;20:235-247.
30. Amsden GW. Pneumococcal macrolide resistance: myth or reality? J Antimicrob Chemother. 1999;44:1-6.
31. Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units. Implications for fluoroquinolone use. JAMA. 2003;289:885-888.
32. Brook I, Gooch WM 3rd, Jenkins SG, et al. Medical management of acute bacterial sinusitis. Recommendations of a clinical advisory committee on pediatric and adult sinusitis. Ann Otol Rhinol Laryngol Suppl. 2000;182:2-20.
33. Benninger MS, Sedory Holzer SE, Lau J. Diagnosis and treatment of uncomplicated acute bacterial rhinosinusitis: summary of the Agency for Health Care Policy and Research evidence-based report. Otolaryngol Head Neck Surg 2000;123:665-667.
34. Snow V, Mottur-Pilson C, Hickner JM. Principles of appropriate antibiotic use for acute sinusitis in adults. Ann Intern Med 2001;134:495-497.
35. Hickner JM, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for acute rhinosinustis in adults. Background. Ann Intern Med 2001;123:498-505.
36. Tankovic J, Bachoual R, Ouabdesselam S, Boudjadja A, Soussy CJ. In-vitro activity of moxifloxacin against fluoroquinolone-resistant strains of aerobic gram-negative bacilli and Enterococcus faecalis. J Antimicrob Chemother. 1999;43 (suppl B):19-23.
37. Andrews JM, Weller TMA, Ashby JP, Walker RM, Wise R. The in vitro activity of ABT773, a new ketolide antimicrobial agent. J Antimicrob Chemother. 2000;46:1017-1022.
38. Cunha BA. Empiric therapy of community-acquired pneumonia: guidelines for the perplexed? Chest. 2004;125:1913-1919.
39. File TM, Jr, Garau J, Blasi F, et al. Guidelines for empiric antimicrobial prescribing in community-acquired pneumonia. Chest 2004;125:1888-1901.
40. Maglio D, Nicolau DP. Antimicrobial efficacy review. Infect Dis. 2004;7:33-36.
41. Sobol SE, Schloss MD, Tewfik TL. Sinus, acute, medical treatment. Available at:http://www.emedicine.com/ENT/ topic337.htm Accessed January 4, 2005.
42. Tse J, Cosep ML, Aminimanizani A, Gill MA. Communityacquired pneumonia. California Pharmacist Winter. 2002;2003:54-65.
43. Full US Prescribing Information for Ketek Available at: http://www.aventis-US.com/PIs/ketek_TXT.html Accessed January 4, 2005.
44. Full US Prescribing Information for Avelox Available at: http://www.univgraph.com/bayer/inserts/Avelox.pdf .Accessed January 4, 2005.
Acute bacterial sinusitis (ABS), acute bacterial exacerbations of chronic bronchitis (ABECB), and community-acquired pneumonia (CAP) are 3 respiratory tract infections (RTIs) in adults that pose a treatment challenge for clinicians in the primary care setting. Each of these conditions requires prompt initiation of therapy to achieve optimal patient outcomes, but diagnosis and selection of treatment typically are made without the benefit of diagnostic tests. Due to increasingly high levels of antibiotic resistance,1,2 the decision to treat and the selection of therapy are critically important.3-5
This article briefly reviews the etiology of community-acquired bacterial RTIs, important diagnostic considerations, and current treatment options for patients who have these infections.
- Most community-acquired respiratory tract infections (RTIs) are not bacterial; therefore, patients do not require antibiotic treatment.
- Antibiotic therapy for community-acquired bacterial RTIs, including acute bacterial sinusitis (ABS), acute bacterial exacerbations of chronic bronchitis (ABECB), and community-acquired pneumonia (CAP), is typically empiric and requires careful evaluation of patients and antibiotics.
- Common respiratory tract pathogens, including Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, are becoming increasingly resistant to currently used antibiotics.
- To reduce the development of drug-resistant bacteria and maintain their effectiveness, new-generation antimicrobials should be used only to treat infections that have been proven or are strongly suspected to be caused by bacteria.
Community-acquired respiratory tract infections: Viral vs bacterial
The debate regarding whether to prescribe antibiotics for patients with community-acquired RTIs continues, since most of these infections are viral. Approximately 2% of patients with acute sinusitis have a bacterial infection.4,6 The etiology of acute exacerbations of chronic bronchitis (AECB) is only about 50% bacterial; other causes for these exacerbations include viruses, allergens, and environmental pollutants.3 Among ambulatory patients with CAP, even when diagnostic testing is performed, the causative pathogen cannot be identified in 40% to 50% of patients.7 All of these findings support the view that many cases of acute sinusitis, AECB, or CAP are not caused by bacteria and patients with these types of infections will not benefit from antimicrobial therapy. A diagnostic challenge to primary care physicians is determining which patients have a bacterial infection.
Differential diagnosis of bacterial infection in patients with community-acquired respiratory tract infections
National and international guidelines have been developed to assist clinicians in the differential diagnosis of bacterial infections.7-11
Acute sinusitis
Clinical diagnosis of acute sinusitis is based primarily on medical history, symptoms, and physical findings.14 A wide range of symptoms may occur in patients with acute sinusitis, as it does in patients with a common cold; TABLE 1shows the symptoms most likely to be associated with sinusitis.12 No single clinical sign or symptom distinguishes between bacterial and viral causes of acute sinusitis; rather, it is the combination of these signs or symptoms that may lead to the diagnosis of bacterial sinusitis. A history of purulent secretions and symptoms that appear more severe than those typically associated with an upper RTI suggests ABS;13 however, purulent discharge alone is not always indicative of a bacterial infection. “Double-sickening,” in which the patient becomes ill and then gets worse, combined with elevation in Creactive protein may indicate a bacterial infection.14 Williams et al15 recommended that clinical diagnosis emphasize key features such as maxillary toothache, poor response to over-the counter decongestants or antihistamines, a history of colored nasal discharge, abnormal transillumination, and mucopurulent discharge on examination. A diagnosis of ABS may be made if symptoms persist for more than 10 days, worsen after 5 to 7 days, or are more severe than those normally associated with viral upper respiratory illness.8,13
TABLE 1
Signs and symptoms associated with community-acquired respiratory tract infections3,13,14,17
| Acute sinusitis | |
| Major | Minor |
|
|
| Acute exacerbation of chronic bronchitis | |
| Increased | |
| |
| Community-acquired pneumonia | |
| |
| *Facial pain/pressure alone does not constitute a suggestive history in the absence of another finding listed in the “major” category. | |
| †Fever in acute sinusitis alone does not constitute a suggestive history in the absence of another finding listed in the “major” category. | |
Acute exacerbations of chronic bronchitis
There is no definitive agreement regarding what constitutes an AECB. Symptoms originally described by Anthonisen et al16 are commonly used to define AECB: increased cough and sputum, increased sputum purulence, and increased dyspnea over baseline (TABLE 1).17 A thorough physical and detailed medical history usually are sufficient to diagnose AECB while ruling out conditions such as pneumonia, congestive heart failure, myocardial ischemia, upper RTI, pulmonary embolism, and recurrent aspiration. A chest x-ray or an electrocardiogram may help with differential diagnosis in some patients.17,18 Nevertheless, determination of whether an acute exacerbation is bacterial or viral may be difficult because many patients with this disease have persistent airway colonization with the same bacteria thought to be responsible for AECB. To help physicians decide if antibiotics are necessary, practice guidelines have stratified patients by type of exacerbation (mild, moderate, or severe) and risk factors (TABLE 2).
TABLE 2
Treatment of acute exacerbations of chronic bronchitis8
| Type | Symptoms* | Antimicrobial therapy |
|---|---|---|
| Type 1 — Severe exacerbation | 3 of 3 symptoms | More benefit than when treated with placebo |
| Type 2 — Moderate exacerbation | 2 of 3 symptoms | Less benefit than when treated with placebo |
| Type 3 — Mild exacerbation | 1 of 3 symptoms | No benefit |
| * Increased dyspnea, increased sputum volume, and increased sputum purulence. | ||
Community-acquired pneumonia
Patients with CAP usually present with acute onset of lower respiratory symptoms (TABLE 1). Older and immunosuppressed patients may present with nonrespiratory symptoms, such as confusion, worsening of a chronic condition, or even falls. It is important to note that no combination of clinical signs and symptoms is a definitive diagnosis of CAP.19 All patients with suspected CAP should have a chest radiograph with posteroanterior and lateral views, as radiographs are essential for confirming a diagnosis.3 The Infectious Diseases Society of America (IDSA) and the American Thoracic Society support use of the Pneumonia PORT (Pneumonia Outcomes Research Team) Severity Index (PSI) as a means of risk stratification, combined with careful assessment of the patient and use of clinical judgment when determining whether a patient can be treated on an outpatient basis or should be hospitalized.10
Although it is important to attempt to identify the infecting organism, antimicrobial treatment for CAP is empiric because of the time it takes to get laboratory results and the potential for rapid deterioration of the patient’s condition. Further, patients with CAP may not produce sputum for Gram stain and culture; or, if they do, it may be mixed with upper respiratory tract secretions. Streptococcus pneumoniae may not grow from sputum culture; or, if found, it may be unclear whether the patient is colonized or infected.20 Bacteria cultures may not be helpful either, as blood cultures usually are sterile in patients with CAP.20
Selection of antimicrobial therapy
Once a bacterial infection is suspected, antibiotic treatment should be initiated promptly. Antibiotic therapy for ABS, ABECB, and CAP is simplified somewhat because the distributions of bacterial pathogens associated with each infection overlap substantially. The pathogens encountered most often in patients with ABS are Spneumoniae, Haemophilusinfluenzae, and Moraxella catarrhalis. To a lesser extent, anaerobic bacteria, other streptococcal species (including S pyogenes, S intermedius, and ahemolytic streptococci), and Staphylococcus aureusalso have been shown to cause ABS.21
Bacteria are isolated from the sputum of 40% to 60% of patients with AECB, and the predominant species are consistent with those listed for ABS. Atypical respiratory pathogens, most notably Chlamydophila(previously Chlamydia) pneumoniae, account for about 5% to 10% of organisms isolated from patients with ABECB.17 Patients with CAP also tend to be infected with the above-listed typical pathogens as well as the atypical Mycoplasma pneumoniae, C pneumoniae, and Legionella pneumophila. TABLE 3 lists pathogens associated with community-acquired bacterial RTIs and the effectiveness of commonly used antibiotics and telithromycin, a recently approved antimicrobial agent.
TABLE 3
Pathogens associated with ABS, CAP, and ABECB and in vitro effectiveness of commonly used antibiotics and telithromycin40
| Amoxicillin | Amoxicillin/Clavulanate | Cefuroxime | Erythro-mycin | Clarithro-mycin | Azithro-mycin | Moxi-floxacin | Telithro-mycin | |
|---|---|---|---|---|---|---|---|---|
| Streptococcus pneumoniae* | + | + | + | + | + | + | + | + |
| Resistant | ±† | – | – | – | – | – | + | + |
| Haemophilus influenzae | ||||||||
| β-lactamase negative | + | + | + | ± | ± | ± | + | + |
| β-lactamase positive | – | + | + | ± | ± | ± | + | + |
| Moraxella catarrhalis | + | + | + | + | + | + | + | + |
| Mycoplasma pneumoniae | – | – | – | + | + | + | + | + |
| Chlamydophila pneumonoae | – | – | – | + | + | + | + | + |
| Legionellasp | – | – | – | + | + | + | + | + |
| ABS = acute bacterial sinusitis | ||||||||
| CAP = community-acquired pneumonia | ||||||||
| ABECB = acute bacterial exacerbations of chronic bronchitis | ||||||||
| + = effective. | ||||||||
| – = not active. | ||||||||
| ±= significant resistance, but active against most strains. | ||||||||
| *Resistance is increasing; nationwide survey suggests 21% to 43% resistance to penicillin. | ||||||||
| †Amoxicillin doses of 80 mg/kg/d may be effective against nonmeningeal, penicillin-resistant S pneumoniae. | ||||||||
Resistance of bacterial pathogens
Although the common causative pathogens for community-acquired bacterial RTIs are few, selection of antibiotic therapy is becoming more complicated by the increasing rate of bacterial resistance to many of the antibiotics commonly used to treat these RTIs.
Resistance has been documented for all organisms associated with community-acquired RTIs. Current estimates indicate that 25% to more than 50% of Spneumoniaestrains are not completely susceptible to penicillin and that nearly one third of strains may be resistant to macrolides.22 Penicillin-resistant Spneumoniaealso may have reduced susceptibility to other antibiotics, including tetracycline, erythromycin, azithromycin, cephalosporins, clindamycin, trimethoprim/sulfamethoxazole (TMP/ SMX), and chloramphenicol.23Streptococcuspneumoniae have developed resistance to fluoroquinolones as well. This is of particular concern to the Centers for Disease Control and Prevention (CDC), having influenced its recommendations regarding empiric treatment of pneumonia.10 Macrolides have been mainstays in empiric therapy of CAP because of their activity against both typical and atypical respiratory pathogens; however, their effectiveness has been compromised by a rapid rise in resistance by S pneumoniae. Recent evaluation of Spneumoniae isolates collected between 2000 and 2001 showed that resistance rates to erythromycin, clarithromycin, and azithromycin had increased to 31.0%, 30.7%, and 31.0%, respectively.24 Further, results from 1 recent surveillance study that examined macrolide resistance among patients with community-acquired RTIs being treated by primary care physicians indicated that 23% to 33% of Spneumoniaeisolates were resistant to macrolides.24,25 Resistance also is becoming prevalent among other pathogens associated with community-acquired RTIs, including H influenzaeand Mcatarrhalis.25-27 This may complicate management of patients with community-acquired RTIs; infection with a treatment-resistant pathogen can increase risk for morbidity and mortality if treatment fails to eradicate the bacteria.20,28 However, the clinical impact of resistance remains controversial. Resistance may be overcome with the use of an antibiotic with pharmacokinetic properties or a dosing regimen that achieves very high drug concentrations at sites of infection. Host defense mechanisms also may contribute to eradication of organisms with in vitro resistance to an antibiotic.29,30 Further, since many infections are caused by viruses with high-resolution rates and since some bacterial infections resolve due to host response, the in vivo efficacy of an antibiotic may be much higher than its in vitro sensitivity.
Antibiotics currently prescribed for patients with community-acquired bacterialRTIs
Empiric antibiotic therapy for patients with community-acquired bacterial RTIs should provide coverage against clinically important pathogens likely to be associated with these infections, including resistant strains (TABLE 3). The antibiotic selected should specifically target respiratory pathogens. For example, broad-spectrum antibiotics are not the optimum choice, as they affect both respiratory and nonrespiratory pathogens (eg, gram-negative enterics; Escherichia coliand Klebsiella pneumoniae), which may result in resistance among these organisms.1,31
Antibiotics suitable for treatment of patients with ABS are summarized inTABLE 4. These agents vary widely in their spectra of activity as well as their ability to overcome pathogen resistance (TABLE 3). Amoxicillin, a very narrow-spectrum -lactam, generally is considered to be first-line therapy for children and adults who have ABS32 but may have little activity against resistant strains of S pneumoniae, H influenzae, and M catarrhalis.2
An analysis by the Agency for Healthcare Research and Quality concluded that amoxicillin or folate inhibitors (eg, TMP/SMX) are the most cost-effective choices for initial therapy in an otherwise healthy adult population with uncomplicated ABS.33 For adults who fail to improve after 2 to 3 days, broad-spectrum and β-lactamase-resistant antibiotics for 7 to 14 days should be considered. A clinical practice guideline sponsored by the American Academy of Family Physicians, the American College of Physicians-Society of Internal Medicine, the CDC, and the IDSA recommends initiating treatment with narrow-spectrum agents, eg, amoxicillin, doxycycline, or TMP-SMX for patients with severe or persistent moderate symptoms of ABS.34,35
High-dose amoxicillin/clavulanate 2000/125 mg, twice daily, was shown to be effective in treating patients with ABS, ABECB, and CAP caused by S pneumoniae, including penicillin-resistant S pneumoniae.29
The macrolides erythromycin, clarithromycin, and azithromycin are effective against susceptible strains of all organisms commonly associated with ABS, but many strains of S pneumoniaealso are resistant to these drugs.23,26 Respiratory fluoroquinolones are effective against all pathogens commonly associated with ABS, including resistant strains;26 however, they also have significant activity against gram-negative enterobacteriaceae and thus may increase the potential for emergence of resistant strains of these organisms.36 Ketolides are derived from the macrolide class and were designed to be effective against macrolide-resistant, gram-positive cocci.10 The first ketolide, telithromycin, is an alternative to macrolides for the treatment of patients with ABS, ABECB, and CAP. It is highly active against both common and atypical respiratory pathogens, including resistant strains, but has little activity against either enterobacteriaceae or anaerobes.37
All of the same considerations mentioned for the treatment of ABS also apply to the selection of therapy for patients with ABECB or CAP (TABLE 4). Empiric antimicrobial therapy for these 2 conditions, particularly CAP, also must cover atypical respiratory pathogens.17,38 For a number of years, monotherapy with a macrolide provided coverage against all of the pathogens likely to be associated with CAP and ABECB. In light of the emergence of resistance to these drugs by S pneumoniae, physicians should consider local and regional resistance rates before prescribing. In fact, File and colleagues39 have suggested that current recommendations favoring the use of macrolides in patients with CAP may have to be reconsidered if clinical failure continues to be observed with these agents. Cunha38 has taken an even stronger position, stating that macrolide monotherapy should be avoided in patients with CAP because of the high prevalence of S pneumoni-aeresistance to this class of antibiotics. These authors’ conclusions should be carefully weighed against the CDC’s and IDSA’s recommendations. The CDC previously recommended combination of macrolides and ceftriaxone for hospitalized patients to avoid emergence of fluoroquinolone resistance. The IDSA recommended empiric use of fluoroquinolones with conversion based on culture sensitivities when available.
TABLE 4
Antibiotics currently being used for the treatment of community-acquired bacterial respiratory tract infections41-44
| Generic | ABS* | CAP† | ABECB‡ |
|---|---|---|---|
| β-Lactams | |||
| Amoxicillin | 500 mg every 8 hours | 500 mg to 1 g every 8 hours | 500 mg 3 times daily |
| Amoxicillin/clavulanate | 500 mg every 8 hours | 500 mg/125 mg every 8 hours or 875 mg/125 mg every 12 hours | 875/125 mg bid |
| Cefuroxime | 250 to 500 mg twice daily | 500 mg twice daily | 500 mg twice daily |
| Macrolides | |||
| Clarithromycin | 500 mg every 12 hours for 14 days | 250–500 mg every 12 hours | 500 or 750 mg every 12 hours for 7 to 14 days |
| Clarithromycin extended- release tablets | 1000 mg once daily for 14 days | 1000 mg once daily for 7 days | 1000 mg once daily for 7 days |
| Azithromycin | 500 mg once daily for 3 days | 500 mg first day, then 250 mg/day for 2 to 5 days | 500 mg once daily for 3 days or 500 mg first day, then 250 mg/day for 4 days |
| Erythromycin | 250 to 500 mg twice daily | 250 or 500 mg 3 or 4 times daily | |
| Fluoroquinolone | |||
| Moxifloxacin | 400 mg once daily for 10 days | 400 mg once daily for 7 to 14 days | 400 mg once daily for 5 days |
| Ketolide | |||
| Telithromycin | 800 mg once daily for 5 days | 800 mg once daily for 7 to 10 days | 800 mg once daily for 5 days |
| Other Antibiotics | |||
| Trimethoprim- Sulfamethoxazole | 160 mg trimethoprim and 800 mg sulfamethoxale every 12 hours for 14 days | ||
| *Treatment is for 10 to 14 days unless otherwise indicated. | |||
| †Treatment ranges from 7 to 14 days unless otherwise noted. | |||
| ‡Treatment is for 10 days unless otherwise noted. | |||
Conclusions
Appropriate prescribing of antibiotics can effectively slow the development of bacterial resistance. Before selecting an antibiotic for a patient with a community-acquired RTI, primary care clinicians should first evaluate whether such treatment is even necessary. Treatment of ABS, ABECB, or CAP is compromised by increasing pathogen resistance to the currently used antibiotics. Use of high-dose amoxicillin and the other “older” antibiotics may delay the emergence of resistance to “newer” drugs, making newer drugs useful for treatment of more difficult cases. New agents to the antibiotic armamentarium give primary care physicians additional therapeutic options for patients who present with bacterial RTIs.
Financial disclosure:
Stephen Brunton, MD, is a consultant for and a member of the speakers’ bureaus for Aventis Pharmaceuticals Inc and Ortho-McNeil Pharmaceutical Inc.
Acute bacterial sinusitis (ABS), acute bacterial exacerbations of chronic bronchitis (ABECB), and community-acquired pneumonia (CAP) are 3 respiratory tract infections (RTIs) in adults that pose a treatment challenge for clinicians in the primary care setting. Each of these conditions requires prompt initiation of therapy to achieve optimal patient outcomes, but diagnosis and selection of treatment typically are made without the benefit of diagnostic tests. Due to increasingly high levels of antibiotic resistance,1,2 the decision to treat and the selection of therapy are critically important.3-5
This article briefly reviews the etiology of community-acquired bacterial RTIs, important diagnostic considerations, and current treatment options for patients who have these infections.
- Most community-acquired respiratory tract infections (RTIs) are not bacterial; therefore, patients do not require antibiotic treatment.
- Antibiotic therapy for community-acquired bacterial RTIs, including acute bacterial sinusitis (ABS), acute bacterial exacerbations of chronic bronchitis (ABECB), and community-acquired pneumonia (CAP), is typically empiric and requires careful evaluation of patients and antibiotics.
- Common respiratory tract pathogens, including Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis, are becoming increasingly resistant to currently used antibiotics.
- To reduce the development of drug-resistant bacteria and maintain their effectiveness, new-generation antimicrobials should be used only to treat infections that have been proven or are strongly suspected to be caused by bacteria.
Community-acquired respiratory tract infections: Viral vs bacterial
The debate regarding whether to prescribe antibiotics for patients with community-acquired RTIs continues, since most of these infections are viral. Approximately 2% of patients with acute sinusitis have a bacterial infection.4,6 The etiology of acute exacerbations of chronic bronchitis (AECB) is only about 50% bacterial; other causes for these exacerbations include viruses, allergens, and environmental pollutants.3 Among ambulatory patients with CAP, even when diagnostic testing is performed, the causative pathogen cannot be identified in 40% to 50% of patients.7 All of these findings support the view that many cases of acute sinusitis, AECB, or CAP are not caused by bacteria and patients with these types of infections will not benefit from antimicrobial therapy. A diagnostic challenge to primary care physicians is determining which patients have a bacterial infection.
Differential diagnosis of bacterial infection in patients with community-acquired respiratory tract infections
National and international guidelines have been developed to assist clinicians in the differential diagnosis of bacterial infections.7-11
Acute sinusitis
Clinical diagnosis of acute sinusitis is based primarily on medical history, symptoms, and physical findings.14 A wide range of symptoms may occur in patients with acute sinusitis, as it does in patients with a common cold; TABLE 1shows the symptoms most likely to be associated with sinusitis.12 No single clinical sign or symptom distinguishes between bacterial and viral causes of acute sinusitis; rather, it is the combination of these signs or symptoms that may lead to the diagnosis of bacterial sinusitis. A history of purulent secretions and symptoms that appear more severe than those typically associated with an upper RTI suggests ABS;13 however, purulent discharge alone is not always indicative of a bacterial infection. “Double-sickening,” in which the patient becomes ill and then gets worse, combined with elevation in Creactive protein may indicate a bacterial infection.14 Williams et al15 recommended that clinical diagnosis emphasize key features such as maxillary toothache, poor response to over-the counter decongestants or antihistamines, a history of colored nasal discharge, abnormal transillumination, and mucopurulent discharge on examination. A diagnosis of ABS may be made if symptoms persist for more than 10 days, worsen after 5 to 7 days, or are more severe than those normally associated with viral upper respiratory illness.8,13
TABLE 1
Signs and symptoms associated with community-acquired respiratory tract infections3,13,14,17
| Acute sinusitis | |
| Major | Minor |
|
|
| Acute exacerbation of chronic bronchitis | |
| Increased | |
| |
| Community-acquired pneumonia | |
| |
| *Facial pain/pressure alone does not constitute a suggestive history in the absence of another finding listed in the “major” category. | |
| †Fever in acute sinusitis alone does not constitute a suggestive history in the absence of another finding listed in the “major” category. | |
Acute exacerbations of chronic bronchitis
There is no definitive agreement regarding what constitutes an AECB. Symptoms originally described by Anthonisen et al16 are commonly used to define AECB: increased cough and sputum, increased sputum purulence, and increased dyspnea over baseline (TABLE 1).17 A thorough physical and detailed medical history usually are sufficient to diagnose AECB while ruling out conditions such as pneumonia, congestive heart failure, myocardial ischemia, upper RTI, pulmonary embolism, and recurrent aspiration. A chest x-ray or an electrocardiogram may help with differential diagnosis in some patients.17,18 Nevertheless, determination of whether an acute exacerbation is bacterial or viral may be difficult because many patients with this disease have persistent airway colonization with the same bacteria thought to be responsible for AECB. To help physicians decide if antibiotics are necessary, practice guidelines have stratified patients by type of exacerbation (mild, moderate, or severe) and risk factors (TABLE 2).
TABLE 2
Treatment of acute exacerbations of chronic bronchitis8
| Type | Symptoms* | Antimicrobial therapy |
|---|---|---|
| Type 1 — Severe exacerbation | 3 of 3 symptoms | More benefit than when treated with placebo |
| Type 2 — Moderate exacerbation | 2 of 3 symptoms | Less benefit than when treated with placebo |
| Type 3 — Mild exacerbation | 1 of 3 symptoms | No benefit |
| * Increased dyspnea, increased sputum volume, and increased sputum purulence. | ||
Community-acquired pneumonia
Patients with CAP usually present with acute onset of lower respiratory symptoms (TABLE 1). Older and immunosuppressed patients may present with nonrespiratory symptoms, such as confusion, worsening of a chronic condition, or even falls. It is important to note that no combination of clinical signs and symptoms is a definitive diagnosis of CAP.19 All patients with suspected CAP should have a chest radiograph with posteroanterior and lateral views, as radiographs are essential for confirming a diagnosis.3 The Infectious Diseases Society of America (IDSA) and the American Thoracic Society support use of the Pneumonia PORT (Pneumonia Outcomes Research Team) Severity Index (PSI) as a means of risk stratification, combined with careful assessment of the patient and use of clinical judgment when determining whether a patient can be treated on an outpatient basis or should be hospitalized.10
Although it is important to attempt to identify the infecting organism, antimicrobial treatment for CAP is empiric because of the time it takes to get laboratory results and the potential for rapid deterioration of the patient’s condition. Further, patients with CAP may not produce sputum for Gram stain and culture; or, if they do, it may be mixed with upper respiratory tract secretions. Streptococcus pneumoniae may not grow from sputum culture; or, if found, it may be unclear whether the patient is colonized or infected.20 Bacteria cultures may not be helpful either, as blood cultures usually are sterile in patients with CAP.20
Selection of antimicrobial therapy
Once a bacterial infection is suspected, antibiotic treatment should be initiated promptly. Antibiotic therapy for ABS, ABECB, and CAP is simplified somewhat because the distributions of bacterial pathogens associated with each infection overlap substantially. The pathogens encountered most often in patients with ABS are Spneumoniae, Haemophilusinfluenzae, and Moraxella catarrhalis. To a lesser extent, anaerobic bacteria, other streptococcal species (including S pyogenes, S intermedius, and ahemolytic streptococci), and Staphylococcus aureusalso have been shown to cause ABS.21
Bacteria are isolated from the sputum of 40% to 60% of patients with AECB, and the predominant species are consistent with those listed for ABS. Atypical respiratory pathogens, most notably Chlamydophila(previously Chlamydia) pneumoniae, account for about 5% to 10% of organisms isolated from patients with ABECB.17 Patients with CAP also tend to be infected with the above-listed typical pathogens as well as the atypical Mycoplasma pneumoniae, C pneumoniae, and Legionella pneumophila. TABLE 3 lists pathogens associated with community-acquired bacterial RTIs and the effectiveness of commonly used antibiotics and telithromycin, a recently approved antimicrobial agent.
TABLE 3
Pathogens associated with ABS, CAP, and ABECB and in vitro effectiveness of commonly used antibiotics and telithromycin40
| Amoxicillin | Amoxicillin/Clavulanate | Cefuroxime | Erythro-mycin | Clarithro-mycin | Azithro-mycin | Moxi-floxacin | Telithro-mycin | |
|---|---|---|---|---|---|---|---|---|
| Streptococcus pneumoniae* | + | + | + | + | + | + | + | + |
| Resistant | ±† | – | – | – | – | – | + | + |
| Haemophilus influenzae | ||||||||
| β-lactamase negative | + | + | + | ± | ± | ± | + | + |
| β-lactamase positive | – | + | + | ± | ± | ± | + | + |
| Moraxella catarrhalis | + | + | + | + | + | + | + | + |
| Mycoplasma pneumoniae | – | – | – | + | + | + | + | + |
| Chlamydophila pneumonoae | – | – | – | + | + | + | + | + |
| Legionellasp | – | – | – | + | + | + | + | + |
| ABS = acute bacterial sinusitis | ||||||||
| CAP = community-acquired pneumonia | ||||||||
| ABECB = acute bacterial exacerbations of chronic bronchitis | ||||||||
| + = effective. | ||||||||
| – = not active. | ||||||||
| ±= significant resistance, but active against most strains. | ||||||||
| *Resistance is increasing; nationwide survey suggests 21% to 43% resistance to penicillin. | ||||||||
| †Amoxicillin doses of 80 mg/kg/d may be effective against nonmeningeal, penicillin-resistant S pneumoniae. | ||||||||
Resistance of bacterial pathogens
Although the common causative pathogens for community-acquired bacterial RTIs are few, selection of antibiotic therapy is becoming more complicated by the increasing rate of bacterial resistance to many of the antibiotics commonly used to treat these RTIs.
Resistance has been documented for all organisms associated with community-acquired RTIs. Current estimates indicate that 25% to more than 50% of Spneumoniaestrains are not completely susceptible to penicillin and that nearly one third of strains may be resistant to macrolides.22 Penicillin-resistant Spneumoniaealso may have reduced susceptibility to other antibiotics, including tetracycline, erythromycin, azithromycin, cephalosporins, clindamycin, trimethoprim/sulfamethoxazole (TMP/ SMX), and chloramphenicol.23Streptococcuspneumoniae have developed resistance to fluoroquinolones as well. This is of particular concern to the Centers for Disease Control and Prevention (CDC), having influenced its recommendations regarding empiric treatment of pneumonia.10 Macrolides have been mainstays in empiric therapy of CAP because of their activity against both typical and atypical respiratory pathogens; however, their effectiveness has been compromised by a rapid rise in resistance by S pneumoniae. Recent evaluation of Spneumoniae isolates collected between 2000 and 2001 showed that resistance rates to erythromycin, clarithromycin, and azithromycin had increased to 31.0%, 30.7%, and 31.0%, respectively.24 Further, results from 1 recent surveillance study that examined macrolide resistance among patients with community-acquired RTIs being treated by primary care physicians indicated that 23% to 33% of Spneumoniaeisolates were resistant to macrolides.24,25 Resistance also is becoming prevalent among other pathogens associated with community-acquired RTIs, including H influenzaeand Mcatarrhalis.25-27 This may complicate management of patients with community-acquired RTIs; infection with a treatment-resistant pathogen can increase risk for morbidity and mortality if treatment fails to eradicate the bacteria.20,28 However, the clinical impact of resistance remains controversial. Resistance may be overcome with the use of an antibiotic with pharmacokinetic properties or a dosing regimen that achieves very high drug concentrations at sites of infection. Host defense mechanisms also may contribute to eradication of organisms with in vitro resistance to an antibiotic.29,30 Further, since many infections are caused by viruses with high-resolution rates and since some bacterial infections resolve due to host response, the in vivo efficacy of an antibiotic may be much higher than its in vitro sensitivity.
Antibiotics currently prescribed for patients with community-acquired bacterialRTIs
Empiric antibiotic therapy for patients with community-acquired bacterial RTIs should provide coverage against clinically important pathogens likely to be associated with these infections, including resistant strains (TABLE 3). The antibiotic selected should specifically target respiratory pathogens. For example, broad-spectrum antibiotics are not the optimum choice, as they affect both respiratory and nonrespiratory pathogens (eg, gram-negative enterics; Escherichia coliand Klebsiella pneumoniae), which may result in resistance among these organisms.1,31
Antibiotics suitable for treatment of patients with ABS are summarized inTABLE 4. These agents vary widely in their spectra of activity as well as their ability to overcome pathogen resistance (TABLE 3). Amoxicillin, a very narrow-spectrum -lactam, generally is considered to be first-line therapy for children and adults who have ABS32 but may have little activity against resistant strains of S pneumoniae, H influenzae, and M catarrhalis.2
An analysis by the Agency for Healthcare Research and Quality concluded that amoxicillin or folate inhibitors (eg, TMP/SMX) are the most cost-effective choices for initial therapy in an otherwise healthy adult population with uncomplicated ABS.33 For adults who fail to improve after 2 to 3 days, broad-spectrum and β-lactamase-resistant antibiotics for 7 to 14 days should be considered. A clinical practice guideline sponsored by the American Academy of Family Physicians, the American College of Physicians-Society of Internal Medicine, the CDC, and the IDSA recommends initiating treatment with narrow-spectrum agents, eg, amoxicillin, doxycycline, or TMP-SMX for patients with severe or persistent moderate symptoms of ABS.34,35
High-dose amoxicillin/clavulanate 2000/125 mg, twice daily, was shown to be effective in treating patients with ABS, ABECB, and CAP caused by S pneumoniae, including penicillin-resistant S pneumoniae.29
The macrolides erythromycin, clarithromycin, and azithromycin are effective against susceptible strains of all organisms commonly associated with ABS, but many strains of S pneumoniaealso are resistant to these drugs.23,26 Respiratory fluoroquinolones are effective against all pathogens commonly associated with ABS, including resistant strains;26 however, they also have significant activity against gram-negative enterobacteriaceae and thus may increase the potential for emergence of resistant strains of these organisms.36 Ketolides are derived from the macrolide class and were designed to be effective against macrolide-resistant, gram-positive cocci.10 The first ketolide, telithromycin, is an alternative to macrolides for the treatment of patients with ABS, ABECB, and CAP. It is highly active against both common and atypical respiratory pathogens, including resistant strains, but has little activity against either enterobacteriaceae or anaerobes.37
All of the same considerations mentioned for the treatment of ABS also apply to the selection of therapy for patients with ABECB or CAP (TABLE 4). Empiric antimicrobial therapy for these 2 conditions, particularly CAP, also must cover atypical respiratory pathogens.17,38 For a number of years, monotherapy with a macrolide provided coverage against all of the pathogens likely to be associated with CAP and ABECB. In light of the emergence of resistance to these drugs by S pneumoniae, physicians should consider local and regional resistance rates before prescribing. In fact, File and colleagues39 have suggested that current recommendations favoring the use of macrolides in patients with CAP may have to be reconsidered if clinical failure continues to be observed with these agents. Cunha38 has taken an even stronger position, stating that macrolide monotherapy should be avoided in patients with CAP because of the high prevalence of S pneumoni-aeresistance to this class of antibiotics. These authors’ conclusions should be carefully weighed against the CDC’s and IDSA’s recommendations. The CDC previously recommended combination of macrolides and ceftriaxone for hospitalized patients to avoid emergence of fluoroquinolone resistance. The IDSA recommended empiric use of fluoroquinolones with conversion based on culture sensitivities when available.
TABLE 4
Antibiotics currently being used for the treatment of community-acquired bacterial respiratory tract infections41-44
| Generic | ABS* | CAP† | ABECB‡ |
|---|---|---|---|
| β-Lactams | |||
| Amoxicillin | 500 mg every 8 hours | 500 mg to 1 g every 8 hours | 500 mg 3 times daily |
| Amoxicillin/clavulanate | 500 mg every 8 hours | 500 mg/125 mg every 8 hours or 875 mg/125 mg every 12 hours | 875/125 mg bid |
| Cefuroxime | 250 to 500 mg twice daily | 500 mg twice daily | 500 mg twice daily |
| Macrolides | |||
| Clarithromycin | 500 mg every 12 hours for 14 days | 250–500 mg every 12 hours | 500 or 750 mg every 12 hours for 7 to 14 days |
| Clarithromycin extended- release tablets | 1000 mg once daily for 14 days | 1000 mg once daily for 7 days | 1000 mg once daily for 7 days |
| Azithromycin | 500 mg once daily for 3 days | 500 mg first day, then 250 mg/day for 2 to 5 days | 500 mg once daily for 3 days or 500 mg first day, then 250 mg/day for 4 days |
| Erythromycin | 250 to 500 mg twice daily | 250 or 500 mg 3 or 4 times daily | |
| Fluoroquinolone | |||
| Moxifloxacin | 400 mg once daily for 10 days | 400 mg once daily for 7 to 14 days | 400 mg once daily for 5 days |
| Ketolide | |||
| Telithromycin | 800 mg once daily for 5 days | 800 mg once daily for 7 to 10 days | 800 mg once daily for 5 days |
| Other Antibiotics | |||
| Trimethoprim- Sulfamethoxazole | 160 mg trimethoprim and 800 mg sulfamethoxale every 12 hours for 14 days | ||
| *Treatment is for 10 to 14 days unless otherwise indicated. | |||
| †Treatment ranges from 7 to 14 days unless otherwise noted. | |||
| ‡Treatment is for 10 days unless otherwise noted. | |||
Conclusions
Appropriate prescribing of antibiotics can effectively slow the development of bacterial resistance. Before selecting an antibiotic for a patient with a community-acquired RTI, primary care clinicians should first evaluate whether such treatment is even necessary. Treatment of ABS, ABECB, or CAP is compromised by increasing pathogen resistance to the currently used antibiotics. Use of high-dose amoxicillin and the other “older” antibiotics may delay the emergence of resistance to “newer” drugs, making newer drugs useful for treatment of more difficult cases. New agents to the antibiotic armamentarium give primary care physicians additional therapeutic options for patients who present with bacterial RTIs.
Financial disclosure:
Stephen Brunton, MD, is a consultant for and a member of the speakers’ bureaus for Aventis Pharmaceuticals Inc and Ortho-McNeil Pharmaceutical Inc.
1. Whitney CG, Farley MM, Hadler J, et al. for the Active Bacterial Core Surveillance Program of the Emerging Infections Program network. Increasing prevalence of multidrug-resistant Streptococcus pneumoniaein the United States. N Engl J Med. 2000;343:1917-1924.
2. Jacobs MR, Felmingham D, Appelbaum PC, Grüneberg RN; the Alexander Project Group. The Alexander Project 1998-2000: susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother. 2003;52:229-246.
3. File TM, , Jr. Overview of community-acquired respiratory tract infections. In: Nightingale CH, Ambrose PG, File TM, Jr., eds. Community-Acquired Respiratory Infections: Antimicrobial Management. New York, NY: Marcel Dekker, Inc; 2003;1-30.
4. Ben-David D, Rubinstein E. Appropriate use of antibiotics for respiratory infections: review of recent statements and position papers. Curr Opin Infect Dis. 2002;15:151-156.
5. Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. 2001;33:757-762.
6. Gwaltney JM, , Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996;23:1209-1225.
7. Niederman MS, Mandell LA, Anzueto A, et al. American Thoracic Society Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163:1730-1754.
8. Anon JB, Jacobs MR, Poole MD, et al. Sinus and Allergy Health Partnership Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130:1-45.
9. Snow V, Mottur-Pilson C, Gonzales R. for the American College of Physicians-American Society of Internal Medicine Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med. 2001;134:518-520.
10. Mandell LA, Bartlett JG, Dowell SF, File TM, , Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003;37:1405-1433.
11. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med. 2001;134:521-529.
12. Bishai WR. I>ssues in the management of bacterial sinusitis. Otolaryngol Head Neck Surg. 2002;127:S3-S9.
13. Osguthorpe JD. Adult rhinosinusitis: diagnosis and management. Am Fam Physician. 2001;63:69-76.
14. Lindbaek M, Hjortdahl P, Johnsen UL. Use of symptoms, signs, and blood tests to diagnose acute sinus infections in primary care: comparison with computed tomography. Fam Med .1996;28:183-188.
15. Williams JW, Jr, Holleman DR, Jr, Samsa GP, Simel DL. Randomized controlled trial of 3 vs 10 days of trimethoprim/sulfamethoxazole for acute maxillary sinusitis. JAMA. 1995;273:1015-1021.
16. Anthonisen NR, Manfreda J, Warren CPW, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
17. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117:380S-385S.
18. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117:398S-401S.
19. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440-1445.
20. Lonks JR. What is the clinical impact of macrolide resistance? Curr Infect Dis Rep. 2004;6:7-12.
21. Sokol W. Epidemiology of sinusitis in the primary care setting: results from the 1999-2000 Respiratory Surveillance Program. Am J Med. 2001;111(suppl 9A):19S-24S.
22. Appelbaum PC. Resistance among Streptococcus pneumoniae: implications for drug selection. Clin Infect Dis. 2002;34:1613-1620.
23. Doern GV, Brueggemann AB, Huynh H, Wingert E, Rhomberg P. Antimicrobial resistance with Streptococcus pneumoniae in the United States, 1997-1998. Emerg Infect Dis. 1999;5:757-765.
24. Doern GV, Brown SD. Antimicrobial susceptibility among community-acquired respiratory tract pathogens in the USA: data from PROTEKT US 2000-01. J Infect. 2004;48:56-65.
25. Pfaller MA, Jones RN. Gatifloxacin phase IV surveillance trial (TeqCES study) utilizing 5000 primary care physician practices: report of pathogens isolated and susceptibility patterns in community-acquired respiratory tract infections. Diagn Microbiol Infect Dis. 2002;44:77-84.
26. Hoban D, Waites K, Felmingham D. Antimicrobial susceptibility of community-acquired respiratory tract pathogens in North America in 1999-2000: findings of the PROTEKT surveillance study. Diagn Microbiol Infect Dis. 2003;45:251-259.
27. Dunbar LM. Current issues in the management of bacterial respiratory tract disease: the challenge of antibacterial resistance. Am J Med Sci. 2003;326:360-368.
28. Garau J. The hidden impact of antibacterial resistance in respiratory tract infection. Clinical failures: the tip of the iceberg? Respir Med. 2001;95(suppl A)-S5-11.
29. File TM, , Jr, Jacobs MR, Poole MD, Wynne B. 546, 547, 548, 549, 550, 551, 556, 557 and 592 Clinical Study Groups. Outcome of treatment of respiratory tract infections due to Streptococcus pneumoniae, including drug-resistant strains, with pharmacokinetically enhanced amoxycillin/clavulanate. Int J Antimicrob Agents. 2002;20:235-247.
30. Amsden GW. Pneumococcal macrolide resistance: myth or reality? J Antimicrob Chemother. 1999;44:1-6.
31. Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units. Implications for fluoroquinolone use. JAMA. 2003;289:885-888.
32. Brook I, Gooch WM 3rd, Jenkins SG, et al. Medical management of acute bacterial sinusitis. Recommendations of a clinical advisory committee on pediatric and adult sinusitis. Ann Otol Rhinol Laryngol Suppl. 2000;182:2-20.
33. Benninger MS, Sedory Holzer SE, Lau J. Diagnosis and treatment of uncomplicated acute bacterial rhinosinusitis: summary of the Agency for Health Care Policy and Research evidence-based report. Otolaryngol Head Neck Surg 2000;123:665-667.
34. Snow V, Mottur-Pilson C, Hickner JM. Principles of appropriate antibiotic use for acute sinusitis in adults. Ann Intern Med 2001;134:495-497.
35. Hickner JM, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for acute rhinosinustis in adults. Background. Ann Intern Med 2001;123:498-505.
36. Tankovic J, Bachoual R, Ouabdesselam S, Boudjadja A, Soussy CJ. In-vitro activity of moxifloxacin against fluoroquinolone-resistant strains of aerobic gram-negative bacilli and Enterococcus faecalis. J Antimicrob Chemother. 1999;43 (suppl B):19-23.
37. Andrews JM, Weller TMA, Ashby JP, Walker RM, Wise R. The in vitro activity of ABT773, a new ketolide antimicrobial agent. J Antimicrob Chemother. 2000;46:1017-1022.
38. Cunha BA. Empiric therapy of community-acquired pneumonia: guidelines for the perplexed? Chest. 2004;125:1913-1919.
39. File TM, Jr, Garau J, Blasi F, et al. Guidelines for empiric antimicrobial prescribing in community-acquired pneumonia. Chest 2004;125:1888-1901.
40. Maglio D, Nicolau DP. Antimicrobial efficacy review. Infect Dis. 2004;7:33-36.
41. Sobol SE, Schloss MD, Tewfik TL. Sinus, acute, medical treatment. Available at:http://www.emedicine.com/ENT/ topic337.htm Accessed January 4, 2005.
42. Tse J, Cosep ML, Aminimanizani A, Gill MA. Communityacquired pneumonia. California Pharmacist Winter. 2002;2003:54-65.
43. Full US Prescribing Information for Ketek Available at: http://www.aventis-US.com/PIs/ketek_TXT.html Accessed January 4, 2005.
44. Full US Prescribing Information for Avelox Available at: http://www.univgraph.com/bayer/inserts/Avelox.pdf .Accessed January 4, 2005.
1. Whitney CG, Farley MM, Hadler J, et al. for the Active Bacterial Core Surveillance Program of the Emerging Infections Program network. Increasing prevalence of multidrug-resistant Streptococcus pneumoniaein the United States. N Engl J Med. 2000;343:1917-1924.
2. Jacobs MR, Felmingham D, Appelbaum PC, Grüneberg RN; the Alexander Project Group. The Alexander Project 1998-2000: susceptibility of pathogens isolated from community-acquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother. 2003;52:229-246.
3. File TM, , Jr. Overview of community-acquired respiratory tract infections. In: Nightingale CH, Ambrose PG, File TM, Jr., eds. Community-Acquired Respiratory Infections: Antimicrobial Management. New York, NY: Marcel Dekker, Inc; 2003;1-30.
4. Ben-David D, Rubinstein E. Appropriate use of antibiotics for respiratory infections: review of recent statements and position papers. Curr Opin Infect Dis. 2002;15:151-156.
5. Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. 2001;33:757-762.
6. Gwaltney JM, , Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996;23:1209-1225.
7. Niederman MS, Mandell LA, Anzueto A, et al. American Thoracic Society Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163:1730-1754.
8. Anon JB, Jacobs MR, Poole MD, et al. Sinus and Allergy Health Partnership Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130:1-45.
9. Snow V, Mottur-Pilson C, Gonzales R. for the American College of Physicians-American Society of Internal Medicine Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med. 2001;134:518-520.
10. Mandell LA, Bartlett JG, Dowell SF, File TM, , Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003;37:1405-1433.
11. Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med. 2001;134:521-529.
12. Bishai WR. I>ssues in the management of bacterial sinusitis. Otolaryngol Head Neck Surg. 2002;127:S3-S9.
13. Osguthorpe JD. Adult rhinosinusitis: diagnosis and management. Am Fam Physician. 2001;63:69-76.
14. Lindbaek M, Hjortdahl P, Johnsen UL. Use of symptoms, signs, and blood tests to diagnose acute sinus infections in primary care: comparison with computed tomography. Fam Med .1996;28:183-188.
15. Williams JW, Jr, Holleman DR, Jr, Samsa GP, Simel DL. Randomized controlled trial of 3 vs 10 days of trimethoprim/sulfamethoxazole for acute maxillary sinusitis. JAMA. 1995;273:1015-1021.
16. Anthonisen NR, Manfreda J, Warren CPW, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
17. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117:380S-385S.
18. Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117:398S-401S.
19. Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA. 1997;278:1440-1445.
20. Lonks JR. What is the clinical impact of macrolide resistance? Curr Infect Dis Rep. 2004;6:7-12.
21. Sokol W. Epidemiology of sinusitis in the primary care setting: results from the 1999-2000 Respiratory Surveillance Program. Am J Med. 2001;111(suppl 9A):19S-24S.
22. Appelbaum PC. Resistance among Streptococcus pneumoniae: implications for drug selection. Clin Infect Dis. 2002;34:1613-1620.
23. Doern GV, Brueggemann AB, Huynh H, Wingert E, Rhomberg P. Antimicrobial resistance with Streptococcus pneumoniae in the United States, 1997-1998. Emerg Infect Dis. 1999;5:757-765.
24. Doern GV, Brown SD. Antimicrobial susceptibility among community-acquired respiratory tract pathogens in the USA: data from PROTEKT US 2000-01. J Infect. 2004;48:56-65.
25. Pfaller MA, Jones RN. Gatifloxacin phase IV surveillance trial (TeqCES study) utilizing 5000 primary care physician practices: report of pathogens isolated and susceptibility patterns in community-acquired respiratory tract infections. Diagn Microbiol Infect Dis. 2002;44:77-84.
26. Hoban D, Waites K, Felmingham D. Antimicrobial susceptibility of community-acquired respiratory tract pathogens in North America in 1999-2000: findings of the PROTEKT surveillance study. Diagn Microbiol Infect Dis. 2003;45:251-259.
27. Dunbar LM. Current issues in the management of bacterial respiratory tract disease: the challenge of antibacterial resistance. Am J Med Sci. 2003;326:360-368.
28. Garau J. The hidden impact of antibacterial resistance in respiratory tract infection. Clinical failures: the tip of the iceberg? Respir Med. 2001;95(suppl A)-S5-11.
29. File TM, , Jr, Jacobs MR, Poole MD, Wynne B. 546, 547, 548, 549, 550, 551, 556, 557 and 592 Clinical Study Groups. Outcome of treatment of respiratory tract infections due to Streptococcus pneumoniae, including drug-resistant strains, with pharmacokinetically enhanced amoxycillin/clavulanate. Int J Antimicrob Agents. 2002;20:235-247.
30. Amsden GW. Pneumococcal macrolide resistance: myth or reality? J Antimicrob Chemother. 1999;44:1-6.
31. Neuhauser MM, Weinstein RA, Rydman R, Danziger LH, Karam G, Quinn JP. Antibiotic resistance among gram-negative bacilli in US intensive care units. Implications for fluoroquinolone use. JAMA. 2003;289:885-888.
32. Brook I, Gooch WM 3rd, Jenkins SG, et al. Medical management of acute bacterial sinusitis. Recommendations of a clinical advisory committee on pediatric and adult sinusitis. Ann Otol Rhinol Laryngol Suppl. 2000;182:2-20.
33. Benninger MS, Sedory Holzer SE, Lau J. Diagnosis and treatment of uncomplicated acute bacterial rhinosinusitis: summary of the Agency for Health Care Policy and Research evidence-based report. Otolaryngol Head Neck Surg 2000;123:665-667.
34. Snow V, Mottur-Pilson C, Hickner JM. Principles of appropriate antibiotic use for acute sinusitis in adults. Ann Intern Med 2001;134:495-497.
35. Hickner JM, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for acute rhinosinustis in adults. Background. Ann Intern Med 2001;123:498-505.
36. Tankovic J, Bachoual R, Ouabdesselam S, Boudjadja A, Soussy CJ. In-vitro activity of moxifloxacin against fluoroquinolone-resistant strains of aerobic gram-negative bacilli and Enterococcus faecalis. J Antimicrob Chemother. 1999;43 (suppl B):19-23.
37. Andrews JM, Weller TMA, Ashby JP, Walker RM, Wise R. The in vitro activity of ABT773, a new ketolide antimicrobial agent. J Antimicrob Chemother. 2000;46:1017-1022.
38. Cunha BA. Empiric therapy of community-acquired pneumonia: guidelines for the perplexed? Chest. 2004;125:1913-1919.
39. File TM, Jr, Garau J, Blasi F, et al. Guidelines for empiric antimicrobial prescribing in community-acquired pneumonia. Chest 2004;125:1888-1901.
40. Maglio D, Nicolau DP. Antimicrobial efficacy review. Infect Dis. 2004;7:33-36.
41. Sobol SE, Schloss MD, Tewfik TL. Sinus, acute, medical treatment. Available at:http://www.emedicine.com/ENT/ topic337.htm Accessed January 4, 2005.
42. Tse J, Cosep ML, Aminimanizani A, Gill MA. Communityacquired pneumonia. California Pharmacist Winter. 2002;2003:54-65.
43. Full US Prescribing Information for Ketek Available at: http://www.aventis-US.com/PIs/ketek_TXT.html Accessed January 4, 2005.
44. Full US Prescribing Information for Avelox Available at: http://www.univgraph.com/bayer/inserts/Avelox.pdf .Accessed January 4, 2005.
Community-acquired Bacterial Respiratory Tract Infections: Consensus Recommendations
- To minimize development and spread of antibiotic resistance, it is important to administer the correct antibacterial, by the best route, in the right amount, at optimum intervals, and for the appropriate duration.
- Streptococcus pneumoniae and Haemophilus influenzae are the 2 most common bacterial pathogens observed in community-acquired respiratory tract infections.
- Surveillance studies indicate increasing rates of in vitro resistance by S pneumoniae to many β-lactam and macrolide antibiotics.
- To minimize risk of resistance-associated recurrence or relapse, antibacterial agents should be prescribed in accordance with existing guidelines and local resistance patterns. Patient compliance with dosage and duration of therapy should be fostered.
- Preliminary data suggest that high-dose, short-course antibacterial therapy may be as effective as longer courses of low-dose therapy.
Community-acquired respiratory tract infections (CARTIs) are a reason for seeking medical attention. In 2001, there were 28.4 million office visits in the United States for an acute respiratory tract infection (excluding pharyngitis).1
Management of CARTIs poses several challenges. According to the World Health Organization (WHO), “for every 100 respiratory infections, only 20% require antibiotic treatment”2 —the remaining 80 infections most likely have a viral origin. Thus, antibacterial therapy should be avoided unless a bacterial cause has been confirmed or is deemed likely.
Once that determination has been made, clinicians need to separate patients who can be safely managed as outpatients from those who need to be hospitalized. Disease severity is, of course, an important consideration in this selection process.3-8
For management of patients who will not be hospitalized, the WHO and the Society for Healthcare Epidemiology of America/Infectious Diseases Society of America (SHEA/IDSA) offer the 3 Ds: administer the correct drug, at the right dose, and for the appropriate duration, to minimize development and spread of resistance.9,10 A recent consensus conference coordinated by the Primary Care Education Consortium and Texas Academy of Family Physicians elaborated on this mnemonic as it relates to outpatient management of 3 CARTIs: community-acquired pneumonia, acute bacterial exacerbations of chronic bronchitis, and acute bacterial rhinosinusitis. Its recommendations, which have been drawn largely from existing evidence-based guidelines, form the basis for this review.
Drug selection
Treatment with an antibacterial agent will not be medically warranted in the majority of patients with a CARTI. Many of these patients will, however, expect to go home with an antibiotic prescription. The primary care clinician can reduce such expectations and prevent unnecessary reconsultations by briefly addressing four issues: 1) the natural course of the viral illness, 2) the lack of effectiveness of antibiotics, 3) the problem of antibiotic resistance, and 4) the side effects of antibiotics.11
When selecting an antibacterial agent for patients with pneumonia, bronchitis, or rhinosinusitis for which a bacterial cause has been identified or deemed likely, several factors need to be taken into account, including the suspected or identified pathogens, local resistance patterns, previous therapy, patient allergies, and the patient’s ability to tolerate treatment failure. Many of these factors are considered by professional organizations that regularly develop guidelines for CARTIs based on the best available evidence. Perhaps most critical for decision-making in the primary care setting is an understanding of evolving microbiology and resistance patterns.
Common pathogens
There is considerable overlap among pathogens commonly found in CARTIs. Streptococcus pneumoniae and Haemophilus influenzae are most often observed in the outpatient setting.
Community-acquired pneumonia. In outpatients with mild illness, S pneumoniae, Mycoplasma pneumoniae, Chlamydia species (particularly Chlamydia pneumoniae, now called Chlamydophilia pneumoniae), and H influenzae are the most common pathogens.12,13 In patients younger than 50 years without significant comorbidity, Mycoplasma species are the most common pathogens. Older patients and those with significant comorbidity are more likely infected with S pneumoniae,13 a Gram-negative enteric bacillus, Pseudomonas aeruginosa, or Legionella.5,14
Bacterial bronchitis. In addition to S pneumoniae and H influenzae, Moraxella catarrhalis is a frequent pathogen in bacterial exacerbations of chronic bronchitis.15P aeruginosa and other Gram-negative bacilli are also seen, especially in patients with a severe acute exacerbation who have a forced expiratory volume in 1 second (FEV1) of 35% of predicted or less.16 Infection due to multiple pathogens occurs in a small percentage of all patients with chronic bronchitis, particularly those with severe exacerbations. Fewer than 10% of acute exacerbations are due to an atypical bacterium, usually C pneumoniae. M pneumoniae and Legionella pneumophila are implicated even less frequently.15
Bacterial rhinosinusitis.S pneumoniae and H influenzae also are frequent causes of acute bacterial rhinosinusitis. Other pathogens commonly seen in this condition include other Streptococcus species, M catarrhalis, oral anaerobes, Staphylococcus aureus in adults, and M catarrhalis, Streptococcus pyogenes, and anaerobes in children.17
Resistance
Antibiotic resistance is an important consideration in the management of CARTIs. There is little doubt that widespread use of antibiotics leads to in vitro bacterial resistance.18-20 However, because clinical success has been observed in the presence of pathogens with low-level resistance, there is some debate as to whether low-level antibiotic resistance has a significant effect on clinical outcomes.18,21-29 Even so, the US Centers for Disease Control and Prevention has determined that people who attend or work at child-care centers and those who recently used antimicrobial agents are at increased risk for infection with drug-resistant S pneumoniae.30 Moreover, the WHO has stated that infection with resistant pathogens prolongs illness and increases the probability of a fatal outcome.31
Several surveillance programs that monitor antibiotic resistance patterns—including the Alexander Project32 and Tracking Resistance in the United States Today (TRUST)33-36 —have confirmed widespread resistance to antibiotics commonly used to treat CARTIs in the United States. β-Lactam resistance due to penicillin-binding protein changes in S pneumoniae has increased significantly over the past decade. Generally, more than 30% of S pneumoniae are now resistant to penicillins and macrolides (including azithromycin and clarithromycin, the ‘advanced’ agents in this group). A smaller number (6%) are resistant to amoxicillin/clavulanate, although this appears to be a result of in vitro test parameters involving primarily strains with high-level β-lactam resistance. Some cephalosporins also show greater activity than penicillin against intermediately susceptible S pneumoniae, but are not effective against highly resistant strains. In contrast, fewer than 1% of all pneumococci are resistant to newer fluoroquinolones (the so-called respiratory fluoroquinolones, such as gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin) and the ketolide telithromycin.
The prevalence of β-lactamase–producing strains of H influenzae appears to have leveled off. Approximately 30% of H influenzae strains are resistant to ampicillin, while fewer than 1% are resistant to amoxicillin/clavulanate, cefuroxime, macrolides, and newer fluoroquinolones.
More than 90% of M catarrhalis isolates produce β-lactamase, thereby conferring resistance to ampicillin and amoxicillin.
Significant geographical variation in resistance has been observed. The prevalence of penicillin-resistant S pneumoniae ranges from 8% in New England to 25% in the South Atlantic, while ampicillin-resistant H influenzae is seen most often in New England (35%) and least often in the Rocky Mountain region (24%).33,34,36 Significant differences within a community also have been observed.37 Thus, knowledge of local resistance patterns is necessary. This information generally is available from local hospitals, although such data may be more reflective of nosocomial pathogens, or state health departments.
Community-acquired pneumonia
The 2003 guidelines of the IDSA give advanced macrolides and respiratory fluoroquinolones a prominent role in the management of community-acquired pneumonia (TABLE 1).5 The IDSA reviewed data from more than 150 clinical trials conducted in adults over 15 years. The IDSA panel acknowledged the increasing in vitro resistance of S pneumoniae to the macrolides, but noted that reports of clinical failure have not paralleled this. The panel also pointed out the significantly lower rates of resistance to the respiratory fluoroquinolones and expressed concern that abuse of these agents could lead to increased resistance by S pneumoniae.
In a previously healthy person who has not taken an antibiotic in the last 3 months, the IDSA recommends a macrolide or doxycycline as first-line therapy, whereas a fluoroquinolone, high-dose amoxicillin/clavulanate, or a macrolide plus high-dose amoxicillin should be used if an antibiotic has been taken during the last 3 months. Patients with a significant comorbidity can be treated with a fluoroquinolone without regard to recent antibiotic use. Alternatively, a macrolide can be used alone in patients who have not taken an antibiotic in 3 months, but otherwise must be used in combination with high-dose amoxicillin. High-dose amoxicillin/clavulanate or cefpodoxime, cefprozil, or cefuroxime can be used in those with a significant comorbidity and recent antibiotic use.
TABLE 1
Initial empiric therapy in outpatients with community-acquired pneumonia
| Clinical characteristics | No recent antibiotic therapy | Antibiotics during past 3 months |
|---|---|---|
| Previously healthy |
|
|
| Comorbidities (chronic obstructive pulmonary disease, diabetes, renal failure, congestive heart failure, malignancy) |
|
|
| Suspected aspiration with infection |
| |
| Influenza with bacterial superinfection |
| |
| Adapted from Mandell et al.5 © 2003 Infectious Diseases Society of America. | ||
Bacterial bronchitis
A panel of primary care physicians and specialists convened by the Canadian Thoracic Society (CTS) reviewed nearly 400 published articles on acute bacterial exacerbations of chronic bronchitis, including evidence-based reviews such as the Cochrane Database. The 2003 CTS guidelines recommend that treatment be based on the risk for treatment failure (TABLE 2).8
Antibacterial treatment is not recommended for patients whose clinical history and symptoms suggest a viral infection (group 0) unless symptoms persist for more than 10 to 14 days. In those cases, bacterial superinfection with M pneumoniae, C pneumoniae, or Bordetella pertussis is possible. Patients with chronic bronchitis but without risk factors for treatment failure (group 1) may be treated with a variety of first-line agents, including azithromycin, clarithromycin, cefuroxime, cefprozil, cefixime, amoxicillin, doxycycline, or trimethoprim/sulfamethoxazole. For patients in group 1 who fail first-line therapy, and as first-line therapy for patients in group 2, a fluoroquinolone or amoxicillin/clavulanate is recommended. Patients in group 3 are more likely to be infected with a Gram-negative pathogen, such as Ps aeruginosa or Enterobacter species, and are least able to tolerate treatment failure. Hence, ciprofloxacin is appropriate in the outpatient setting.
TABLE 2
Initial empiric therapy in outpatients with acute bacterial exacerbations of chronic bronchitis
| Group | Clinical status | Symptoms/risk factors | Initial treatment | Alternative when 1st-line agent fails |
|---|---|---|---|---|
| 0 | Acute tracheobronchitis |
|
|
|
| 1 | Chronic bronchitis without risk factors |
|
|
|
| 2 | Chronic bronchitis with risk factors |
|
|
|
| 3 | Chronic suppurative bronchitis |
|
| |
| Adapted from Balter et al,8 with permission. The publisher of Can Respir J does not assume responsibility for errors or discrepancies that may have occurred. | ||||
Bacterial rhinosinusitis
The recommendations for management of acute bacterial rhinosinusitis issued by the Sinus and Allergy Health Partnership (SAHP), a not-for-profit organization created by the American Academy of Otolaryngic Allergy, the American Academy of Otolaryngology-Head and Neck Surgery, and the American Rhinologic Society, are based on a variety of factors. These include rate of spontaneous resolution, pathogen distribution, antibacterial resistance data, the importance of S pneumoniae in intracranial and extrasinus complications, and the ability of a patient to tolerate treatment failure (TABLE 3).17 The panel reviewed more than 150 published articles on management of children and adults with bacterial rhinosinusitis.
As in the pneumonia guidelines, recent antibiotic use is an important consideration when selecting an antibiotic since resistant pathogens are likely. β-Lactam agents play a major role as initial therapy in both children and adults. This recommendation is consistent with those of Williams et al who reviewed 49 clinical trials involving 13,660 patients. These investigators recommended 7 to 14 days of penicillin or amoxicillin for acute maxillary sinusitis confirmed radiographically or by aspiration.38
The SAHP recommended higher doses of amoxicillin (with or without clavulanate) in patients who have recently taken an antibiotic or who have moderate disease. Fluoroquinolones are recommended as alternatives in patients with mild disease who have not taken an antibiotic in the last 4 to 6 weeks. However, in patients with mild disease who have taken antibiotics recently or who have moderate disease, fluoroquinolones are recommended as first-line therapy. Macrolides are recommended only for patients with a β-lactam allergy since failure rates of 20% to 25% are possible. Lack of improvement or worsening symptoms after 72 hours should prompt reevaluation, may necessitate cultures and/or a CT scan, and should raise the possibility of causal organisms other than S pneumoniae, H influenzae, and M catarrhalis.
TABLE 3
Initial empiric therapy in outpatients with acute bacterial rhinosinusitis
| Initial therapy | Alternative agent if no improvement or worsening after 72 hours | |
|---|---|---|
| Mild disease, no antibiotic during past 4 to 6 weeks | ||
| Children |
|
|
| Children with β-lactam allergy |
|
|
| Adults |
|
|
| Adults with β-lactam allergy |
|
|
| Mild disease and antibiotic during past 4 to 6 weeks or moderate disease | ||
| Children |
|
|
| Children with β-lactam allergy |
|
|
| Adults |
|
|
| Adults with β-lactam allergy |
|
|
| Adapted from Anon et al17 © 2004, with permission from American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. | ||
Dose and duration
While each of the three guidelines provides detailed recommendations regarding selection of an antibacterial agent, the dose and duration of therapy generally are not well defined. Fortunately, other sources provide guidance in these 2 areas.
First, an independent international panel of infectious diseases experts, whose goal was to identify ways to improve prescription of antibiotics for lower respiratory tract infections, stressed that an important purpose of therapy is to reduce bacterial load and, in fact, treat to bacteriologic cure.19 Antibiotic therapy that allows some bacteria to survive increases the risk of early recurrence or relapse and encourages resistance selection. Such therapy is, therefore, inappropriate. The panel concurred with the WHO and others that the likelihood of bacterial persistence increases when antibiotics are prescribed in low doses, especially if given over long periods.18,39-41 Prolonged low-dose antibiotic therapy, which has been common practice for many infections, is contrary to the WHO Global Strategy for Containment of Antimicrobial Resistance, which notes that single-agent therapy for a short duration is 1 of several actions that can be taken to minimize bacterial resistance.42 Shorter courses of antibiotic therapy also are consistent with SHEA/IDSA recommendations.10
The clinical appropriateness of this recommendation is reinforced by the changes that have occurred during the past decade in the management of selected urinary tract infections (UTIs). Some UTIs that previously had been treated with low-dose antibiotics for 10 to 14 days now are treated with only 1 or a few high doses of a single agent. Other infections for which clinical data support shorter courses of antibiotic therapy include uncomplicated cellulitis,43 ventilator-associated pneumonia,44 and meningococcal disease.45
Shorter-course antibacterial therapy for CARTIs increasingly has been the focus of clinical trials. The focus is not unreasonable. Many of the antibiotics used for CARTIs are very potent against the pathogens commonly encountered, penetrate infected tissues well, are available in oral formulations, and are generally well tolerated. However, to optimize an antibiotic’s bactericidal potential, it is necessary to base the dosing regimen on its pharmacodynamics. From a pharmacodynamic perspective, there are 2 groups of antibiotics, those with concentration-dependent killing and those with time-dependent killing. For agents with concentration-dependent killing, such as fluoroquinolones, ketolides, and aminoglycosides, the goal is to select a dose that achieves a higher peak concentration and/or a larger area under the plasma concentration curve, with acceptable tolerability. In contrast, antibiotics that rely on time-dependent killing, such as β-lactams, macrolides, azalides, tetracyclines, and some others, require extended durations of concentrations above the MIC90 of the bacterial pathogen(s). Consequently, multiple daily dosing may be preferable.46
Dose. A few studies have compared high-dose, short-course therapy with therapy using standard doses and durations (TABLE 4). To assess the impact of highdose, short-course therapy on post-treatment resistant pneumococcal carriage, Schrag compared amoxicillin given either as 90 mg/kg/day for 5 days (high-dose, short-course) or 40 mg/kg/day for 10 days (standard) in 797 children with a respiratory tract infection.47 At day 28, nasal carriage of penicillin-resistant S pneumoniae was detected in 24% of the high-dose, shortcourse group and in 32% of the standard group (relative risk, 0.77; P=0.03). Among the pneumococcal carriers, the risk of penicillin-resistant S pneumoniae was significantly lower in the high-dose, short-course group than in the standard therapy group (relative risk, 0.78; P=0.01)
Another study investigated high-dose, short-course therapy with levofloxacin in patients with mild to severe community-acquired pneumonia. Patients received levofloxacin 750 mg/d for 5 days or 500 mg/d for 10 days.48 The clinical success rates were 92.4% and 91.1%, respectively, while the bacteriologic eradication rates at 7 to 14 days post-therapy were 93.2% and 92.4%, respectively, thereby demonstrating that high-dose, shortcourse levofloxacin therapy is at least as effective as standard levofloxacin therapy.
Duration. Short-course therapy using standard doses of azithromycin, gemifloxacin, levofloxacin, moxifloxacin, and telithromycin has been investigated in clinical trials of CARTIs (FIGURE). In patients with community-acquired pneumonia, 5 days of therapy with telithromycin was shown to be equivalent to a 7-day course (both using a single daily dose of 800 mg), as well as to clarithromycin 500 mg bid for 10 days.49
In studies of acute exacerbations of chronic bronchitis, a 3-day course of azithromycin was equivalent to clarithromycin for 10 days50 and gemifloxacin for 5 days was equivalent to a sequential combination of ceftriaxone and cefuroxime axetil for up to 10 days.51 Levofloxacin for 3 days and azithromycin for 5 days provided equivalent outcomes,52 as did levofloxacin for 5 days and amoxicillin/clavulanate for 10 days.52 Moxifloxacin for 5 days provided results equivalent to those of 7 days of amoxicillin, clarithromycin, or cefuroxime axetil.53 Five days of telithromycin was shown to be equivalent to 10 days of amoxicillin/clavu-lanate54 or cefuroxime axetil.55
Studies of acute bacterial rhinosinusitis have demonstrated equivalent results with azithromycin for 3 days and amoxicillin/clavulanate for 10 days.50 Similarly, telithromycin for 5 days was equivalent to 10 days of telithromycin, amoxicillin/clavulanate, or cefuroxime axetil.56
These clinical trials demonstrate that short-course therapy achieves clinical cure and/or bacteriologic eradication rates that are at least equivalent to those of standard therapy, with no significant difference in safety. Symptomatic improvement is faster and total antibiotic exposure is reduced with short-course therapy.
A significant advantage of short-course antibacterial therapy is improved patient adherence. Adherence is 10% to 20% better with 5-day courses than with 10-day courses,47,57 and is significantly better with 1 or 2 daily doses than with 3 or more daily doses.58-60 In fact, a recent market research study showed that patients perceive once-daily, short-course antibiotic treatment to be significantly more effective than longer courses. This may be due to faster improvement of infection-related symptoms.61 For example, Dunbar et al observed that significantly more patients treated with high-dose, short-course levofloxacin experienced subjective and objective resolution of fever by day 3 compared with those who received standard-dose, short-course levofloxacin.48
TABLE 4
Clinical trials of high-dose, short-course antibiotic therapy
| Drug regimen | N (ref) | Outcome |
|---|---|---|
| Amoxicillin 90 mg/kg/d x 5 d vs Amoxicillin 40 mg/kg/d x 10 d | 797 |
|
| (47) | ||
| Levofloxacin 750 mg/d x 5d vs Levofloxacin 500 mg/d x 10 d | 390 |
|
| (48) |
TABLE 5 Clinical trials of standard-dose, short-course antibiotic therapy
Summary
Essential questions that need to be answered for every patient who presents with a possible CARTI include : 1) Is antibacterial therapy necessary? 2) If so, what is the best antibiotic and at what dose and for how long should it be administered? Accumulating evidence indicates that some antibiotics when given in high doses for a short duration are as effective and safe as standard therapy for CARTIs. Short-course therapy also promotes patient compliance.
Disclosures:
The authors reported the following financial relationships: Dr Brunton: consultant to Abbott, Ortho-McNeil Pharmaceutical, Inc., and SanofiAventis. Dr Carmichael: consultant to Ortho-McNeil Pharmaceutical, Inc.; on the speakers’ bureaus for Bristol-Myers Squibb Company, Merck & Co., OrthoMcNeil Pharmaceutical, Inc., and Pfizer Inc. Dr Fitzgerald: on the speakers’ bureaus for Boehringer Ingelheim, GlaxoSmithKline, Ortho-McNeil Pharmaceutical, Inc., Pfizer Inc., Sepracor Inc., and 3M. Dr Liu: on the speakers’ bureaus for Aventis Pharmaceuticals, Bayer Pharmaceuticals Corporation, Bristol-Myers Squibb Company, Cobist, GlaxoSmithKline, Merck & Co., Ortho-McNeil Pharmaceutical, Inc., Pfizer Inc., Purdue Pharma, Oscient Pharmaceuticals Corporation, and Wyeth Pharmaceuticals. Dr Varon: on the speakers’ bureau for Ortho-McNeil Pharmaceutical, Inc. Dr. Weiland: consultant to Abbott Laboratories, Ortho-McNeil Pharmaceutical, Inc., and Pfizer Inc.
This supplement to The Journal of Family Practice is supported by a grant from Ortho-McNeil Pharmaceutical, Inc. It was adapted from a consensus conference coordinated by the Primary Care Education Consortium and Texas Academy of Family Physicians and was edited and peer-reviewed by The Journal of Family Practice. © 2005 Quadrant HealthCom Inc. and Primary Care Education Consortium.
1. Centers for Disease Control and Prevention. National Center for Health Statistics website. National Ambulatory Medical Care Survey: 2001 Summary. Available at: http://www.cdc.gov/nchs/data/ad/ad337.pdf. Accessed February 2, 2005.
2. World Health Organization.World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 4. Big guns of resistance. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
3. Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med. 2003;138:109-118.
4. File TM. Community-acquired pneumonia. Lancet. 2003;362:1991-2001.
5. Mandell LA, Bartlett JG, Dowell SF, File TM, Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003;37:1405-1433.
6. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243-250.
7. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
8. Balter MS, La Forge J, Low DE, Mandell L, Grossman RF. Canadian guidelines for the management of acute exacerbations of chronic bronchitis. Can Respir J. 2003;10(suppl B):3B-32B.
9. World Health Organization. World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 5. A call to action: A massive effort to provide proper treatment. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
10. Shlaes DM, Gerding DN, John JF, Jr, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25:584-599.
11. Scottish Intercollegiate Guidelines Network. National Guideline Clearinghouse website. Community management of lower respiratory tract infection in adults. A national clinical guideline. Available at: http://www.guideline.gov/summary/summary.aspx?ss=15& doc_id=3361&nbr=2587&string=respiratory%20AND%20tract%20AND% 20infection. Accessed December 17, 2004.
12. Bochud PY, Moser F, Erard P, et al. Community-acquired pneumonia. A prospective outpatient study. Medicine (Baltimore). 2001;80:75-87.
13. Falguera M, Sacristan O, Nogues A, et al. Nonsevere community-acquired pneumonia: correlation between cause and severity or comorbidity. Arch Intern Med. 2001;161:1866-1872.
14. Ruiz M, Ewig S, Marcos MA, et al. Etiology of community-acquired pneumonia: impact of age, comorbidity, and severity. Am J Respir Crit Care Med. 1999;160:397-405.
15. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117(5 Suppl 2):380S-385S.
16. Eller J, Ede A, Schaberg T, Niederman MS, Mauch H, Lode H. Infective exacerbations of chronic bronchitis: relation between bacteriologic etiology and lung function. Chest. 1998;113:1542-1548.
17. Anon JB, Jacobs MR, Poole MD, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130(1 Suppl):1-45.
18. Albrich WC, Monnet DL, Harbarth S. Antibiotic selection pressure and resistance in Streptococcus pneumoniae. and Streptococcus pyogenes. Emerg Infect Dis. 2004;10:514-517.
19. Ball P, Baquero F, Cars O, et al. Antibiotic therapy of community respiratory tract infections: strategies for optimal outcomes and minimized resistance emergence. J Antimicrob Chemother. 2002;49:31-40.
20. Harbarth S, Albrich W, Brun-Buisson C. Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg Infect Dis. 2002;8:1460-1467.
21. Lonks JR, Garau J, Medeiros AA. Implications of antimicrobial resistance in the empirical treatment of community-acquired respiratory tract infections: the case of macrolides. J Antimicrob Chemother. 2002;50(Suppl S2):87-92.
22. Lonks JR, Garau J, Gomez L, et al. Failure of macrolide antibiotic treatment in patients with bacteremia due to erythromycin-resistant Streptococcus pneumoniae. Clin Infect Dis. 2002;35:556-564.
23. Moellering RC, Jr, Craig W, Edmond M, et al. Clinical and public health implications of macrolide-resistant Streptococcus pneumoniae. J Chemother. 2002;14(suppl 3):42-56.
24. Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:747-750.
25. Musher DM, Dowell ME, Shortridge VD, et al. Emergence of macrolide resistance during treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:630-631.
26. Waterer GW, Buckingham SC, Kessler LA, Quasney MW, Wunderink RG. Decreasing β-lactam resistance in Pneumococci. from the Memphis region: analysis of 2,152 isolates From 1996 to 2001. Chest. 2003;124:519-525.
27. Nuermberger E, Bishai WR. The clinical significance of macrolide-resistant Streptococcus pneumoniae.: it’s all relative. Clin Infect Dis. 2004;38:99-103.
28. Yu VL, Chiou CC, Feldman C, et al. An international prospective study of pneumococcal bacteremia: correlation with in vitro resistance, antibiotics administered, and clinical outcome. Clin Infect Dis. 2003;37:230-237.
29. Metlay JP. Update on community-acquired pneumonia: impact of antibiotic resistance on clinical outcomes. Curr Opin Infect Dis. 2002;15:163-167.
30. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention web site. Drug-resistant Streptococcus pneumoniae disease. Available at: http://www.cdc.gov/ncidod/dbmd/diseaseinfo/drugresisstreppneum_t.htm. Accessed January 4, 2005.
31. World Health Organization World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 3. Factors contributing to resistance. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
32. Jacobs MR, Felmingham D, Appelbaum PC, Gruneberg RN. The Alexander Project 1998-2000: susceptibility of pathogens isolated from communityacquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother. 2003;52:229-246.
33. Thornsberry C, Sahm DF, Kelly LJ, et al. Regional trends in antimicrobial resistance among clinical isolates of Streptococcus pneumoniae., Haemophilus influenzae., and Moraxella catarrhalis. in the United States: results from the TRUST Surveillance Program, 1999-2000. Clin Infect Dis. 2002;34(suppl 1):S4-S16.
34. Karlowsky JA, Thornsberry C, Jones ME, Evangelista AT, Critchley IA, Sahm DF. Factors associated with relative rates of antimicrobial resistance among Streptococcus pneumoniae. in the United States: results from the TRUST Surveillance Program (1998-2002). Clin Infect Dis. 2003;36:963-970.
35. Karlowsky JA, Kelly LJ, Thornsberry C, et al. Susceptibility to fluoroquinolones among commonly isolated Gram-negative bacilli in 2000: TRUST and TSN data for the United States. Tracking Resistance in the United States Today. The Surveillance Network. Int J Antimicrob Agents. 2002;19:21-31.
36. Karlowsky JA, Thornsberry C, Critchley IA, et al. Susceptibilities to levofloxacin in Streptococcus pneumoniae., Haemophilus influenzae., and Moraxella catarrhalis. clinical isolates from children: results from 2000-2001 and 2001-2002 TRUST studies in the United States. Antimicrob Agents Chemother. 2003;47:1790-1797.
37. Quale J, Landman D, Ravishankar J, Flores C, Bratu S. Streptococcus pneumo.-niae., Brooklyn, New York: fluoroquinolone resistance at our doorstep. Emerg Infect Dis. 2002;8:594-597.
38. Williams JW, Jr, Aguilar C, Cornell J, et al. Antibiotics for acute maxillary sinusitis. Cochrane Database Syst Rev. 2004;2:CD000243.-
39. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of β-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365-370.
40. Scheld WM. Maintaining fluoroquinolone class efficacy: review of influencing factors. Emerg Infect Dis. 2003;9:1-9.
41. Thomson KS. Minimizing quinolone resistance: are the new agents more or less likely to cause resistance? J Antimicrob Chemother. 2000;45:719-723.
42. World Health Organization. World Health Organization web site. WHO global strategy for containment of antimicrobial resistance. Available at: http://www.who.int/csr/resources/publications/drugresist/en/EGlobal_Strat.pdf. Accessed February 2, 2005.
43. Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164:1669-1674.
44. Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290:2588-2598.
45. Ellis-Pegler R, Galler L, Roberts S, Thomas M, Woodhouse A. Three days of intravenous benzyl penicillin treatment of meningococcal disease in adults. Clin Infect Dis. 2003;37:658-662.
46. Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of β-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am. 2003;17:479-501.
47. Schrag SJ, Pena C, Fernandez J, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA. 2001;286:49-56.
48. Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
49. Tellier G, Niederman MS, Nusrat R, Patel M, Lavin B. Clinical and bacteriological efficacy and safety of 5 and 7 day regimens of telithromycin once daily compared with a 10 day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother. 2004;54:515-523.
50. Zithromax [prescribing information] New York, NY: Pfizer Labs; 2004.
51. Wilson R, Langan C, Ball P, Bateman K, Pypstra R. Oral gemifloxacin once daily for 5 days compared with sequential therapy with i.v. ceftriaxone/oral cefuroxime (maximum of 10 days) in the treatment of hospitalized patients with acute exacerbations of chronic bronchitis. Respir Med. 2003;97:242-249.
52. Tennenberg A, Walker K, Khashab M, Zadelkis N. The safety and efficacy of short-course (3-5 days), 750 mg levofloxacin (LVX) for acute bacterial exacerbation of chronic bronchitis (ABECB). Presented at: American Thoracic Society 100th International Conference, May 21-26, 2004, Orlando, Fl.
53. Wilson R, Allegra L, Huchon G, et al. Short-term and long-term outcomes of moxifloxacin compared to standard antibiotic treatment in acute exacerbations of chronic bronchitis. Chest. 2004;125:953-964.
54. Aubier M, Aldons PM, Leak A, et al. Telithromycin is as effective as amoxicillin/clavulanate in acute exacerbations of chronic bronchitis. Respir Med. 2002;96:862-871.
55. Zervos MJ, Heyder AM, Leroy B. Oral telithromycin 800 mg once daily for 5 days versus cefuroxime axetil 500 mg twice daily for 10 days in adults with acute exacerbations of chronic bronchitis. J Int Med Res. 2003;31:157-169.
56. Ketek [prescribing information]. Kansas City, Mo: Aventis Pharmaceuticals Inc.; 2004.
57. Carbon C, Chatelin A, Bingen E, et al. A double-blind randomized trial comparing the efficacy and safety of a 5-day course of cefotiam hexetil with that of a 10-day course of penicillin V in adult patients with pharyngitis caused by group A β-haemolytic streptococci. J Antimicrob Chemother 1995;35:843-854.
58. Cockburn J, Gibberd RW, Reid AL, Sanson-Fisher RW. Determinants of noncompliance with short term antibiotic regimens. Br Med J (Clin Res Ed). 1987;295:814-818.
59. Greenberg RN. Overview of patient compliance with medication dosing: a literature review. Clin Ther. 1984;6:592-599.
60. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296-1310.
61. Perez-Gorricho B, Ripoll M. Does short-course antibiotic therapy better meet patient expectations? Int J Antimicrob Agents. 2003;21:222-228.
- To minimize development and spread of antibiotic resistance, it is important to administer the correct antibacterial, by the best route, in the right amount, at optimum intervals, and for the appropriate duration.
- Streptococcus pneumoniae and Haemophilus influenzae are the 2 most common bacterial pathogens observed in community-acquired respiratory tract infections.
- Surveillance studies indicate increasing rates of in vitro resistance by S pneumoniae to many β-lactam and macrolide antibiotics.
- To minimize risk of resistance-associated recurrence or relapse, antibacterial agents should be prescribed in accordance with existing guidelines and local resistance patterns. Patient compliance with dosage and duration of therapy should be fostered.
- Preliminary data suggest that high-dose, short-course antibacterial therapy may be as effective as longer courses of low-dose therapy.
Community-acquired respiratory tract infections (CARTIs) are a reason for seeking medical attention. In 2001, there were 28.4 million office visits in the United States for an acute respiratory tract infection (excluding pharyngitis).1
Management of CARTIs poses several challenges. According to the World Health Organization (WHO), “for every 100 respiratory infections, only 20% require antibiotic treatment”2 —the remaining 80 infections most likely have a viral origin. Thus, antibacterial therapy should be avoided unless a bacterial cause has been confirmed or is deemed likely.
Once that determination has been made, clinicians need to separate patients who can be safely managed as outpatients from those who need to be hospitalized. Disease severity is, of course, an important consideration in this selection process.3-8
For management of patients who will not be hospitalized, the WHO and the Society for Healthcare Epidemiology of America/Infectious Diseases Society of America (SHEA/IDSA) offer the 3 Ds: administer the correct drug, at the right dose, and for the appropriate duration, to minimize development and spread of resistance.9,10 A recent consensus conference coordinated by the Primary Care Education Consortium and Texas Academy of Family Physicians elaborated on this mnemonic as it relates to outpatient management of 3 CARTIs: community-acquired pneumonia, acute bacterial exacerbations of chronic bronchitis, and acute bacterial rhinosinusitis. Its recommendations, which have been drawn largely from existing evidence-based guidelines, form the basis for this review.
Drug selection
Treatment with an antibacterial agent will not be medically warranted in the majority of patients with a CARTI. Many of these patients will, however, expect to go home with an antibiotic prescription. The primary care clinician can reduce such expectations and prevent unnecessary reconsultations by briefly addressing four issues: 1) the natural course of the viral illness, 2) the lack of effectiveness of antibiotics, 3) the problem of antibiotic resistance, and 4) the side effects of antibiotics.11
When selecting an antibacterial agent for patients with pneumonia, bronchitis, or rhinosinusitis for which a bacterial cause has been identified or deemed likely, several factors need to be taken into account, including the suspected or identified pathogens, local resistance patterns, previous therapy, patient allergies, and the patient’s ability to tolerate treatment failure. Many of these factors are considered by professional organizations that regularly develop guidelines for CARTIs based on the best available evidence. Perhaps most critical for decision-making in the primary care setting is an understanding of evolving microbiology and resistance patterns.
Common pathogens
There is considerable overlap among pathogens commonly found in CARTIs. Streptococcus pneumoniae and Haemophilus influenzae are most often observed in the outpatient setting.
Community-acquired pneumonia. In outpatients with mild illness, S pneumoniae, Mycoplasma pneumoniae, Chlamydia species (particularly Chlamydia pneumoniae, now called Chlamydophilia pneumoniae), and H influenzae are the most common pathogens.12,13 In patients younger than 50 years without significant comorbidity, Mycoplasma species are the most common pathogens. Older patients and those with significant comorbidity are more likely infected with S pneumoniae,13 a Gram-negative enteric bacillus, Pseudomonas aeruginosa, or Legionella.5,14
Bacterial bronchitis. In addition to S pneumoniae and H influenzae, Moraxella catarrhalis is a frequent pathogen in bacterial exacerbations of chronic bronchitis.15P aeruginosa and other Gram-negative bacilli are also seen, especially in patients with a severe acute exacerbation who have a forced expiratory volume in 1 second (FEV1) of 35% of predicted or less.16 Infection due to multiple pathogens occurs in a small percentage of all patients with chronic bronchitis, particularly those with severe exacerbations. Fewer than 10% of acute exacerbations are due to an atypical bacterium, usually C pneumoniae. M pneumoniae and Legionella pneumophila are implicated even less frequently.15
Bacterial rhinosinusitis.S pneumoniae and H influenzae also are frequent causes of acute bacterial rhinosinusitis. Other pathogens commonly seen in this condition include other Streptococcus species, M catarrhalis, oral anaerobes, Staphylococcus aureus in adults, and M catarrhalis, Streptococcus pyogenes, and anaerobes in children.17
Resistance
Antibiotic resistance is an important consideration in the management of CARTIs. There is little doubt that widespread use of antibiotics leads to in vitro bacterial resistance.18-20 However, because clinical success has been observed in the presence of pathogens with low-level resistance, there is some debate as to whether low-level antibiotic resistance has a significant effect on clinical outcomes.18,21-29 Even so, the US Centers for Disease Control and Prevention has determined that people who attend or work at child-care centers and those who recently used antimicrobial agents are at increased risk for infection with drug-resistant S pneumoniae.30 Moreover, the WHO has stated that infection with resistant pathogens prolongs illness and increases the probability of a fatal outcome.31
Several surveillance programs that monitor antibiotic resistance patterns—including the Alexander Project32 and Tracking Resistance in the United States Today (TRUST)33-36 —have confirmed widespread resistance to antibiotics commonly used to treat CARTIs in the United States. β-Lactam resistance due to penicillin-binding protein changes in S pneumoniae has increased significantly over the past decade. Generally, more than 30% of S pneumoniae are now resistant to penicillins and macrolides (including azithromycin and clarithromycin, the ‘advanced’ agents in this group). A smaller number (6%) are resistant to amoxicillin/clavulanate, although this appears to be a result of in vitro test parameters involving primarily strains with high-level β-lactam resistance. Some cephalosporins also show greater activity than penicillin against intermediately susceptible S pneumoniae, but are not effective against highly resistant strains. In contrast, fewer than 1% of all pneumococci are resistant to newer fluoroquinolones (the so-called respiratory fluoroquinolones, such as gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin) and the ketolide telithromycin.
The prevalence of β-lactamase–producing strains of H influenzae appears to have leveled off. Approximately 30% of H influenzae strains are resistant to ampicillin, while fewer than 1% are resistant to amoxicillin/clavulanate, cefuroxime, macrolides, and newer fluoroquinolones.
More than 90% of M catarrhalis isolates produce β-lactamase, thereby conferring resistance to ampicillin and amoxicillin.
Significant geographical variation in resistance has been observed. The prevalence of penicillin-resistant S pneumoniae ranges from 8% in New England to 25% in the South Atlantic, while ampicillin-resistant H influenzae is seen most often in New England (35%) and least often in the Rocky Mountain region (24%).33,34,36 Significant differences within a community also have been observed.37 Thus, knowledge of local resistance patterns is necessary. This information generally is available from local hospitals, although such data may be more reflective of nosocomial pathogens, or state health departments.
Community-acquired pneumonia
The 2003 guidelines of the IDSA give advanced macrolides and respiratory fluoroquinolones a prominent role in the management of community-acquired pneumonia (TABLE 1).5 The IDSA reviewed data from more than 150 clinical trials conducted in adults over 15 years. The IDSA panel acknowledged the increasing in vitro resistance of S pneumoniae to the macrolides, but noted that reports of clinical failure have not paralleled this. The panel also pointed out the significantly lower rates of resistance to the respiratory fluoroquinolones and expressed concern that abuse of these agents could lead to increased resistance by S pneumoniae.
In a previously healthy person who has not taken an antibiotic in the last 3 months, the IDSA recommends a macrolide or doxycycline as first-line therapy, whereas a fluoroquinolone, high-dose amoxicillin/clavulanate, or a macrolide plus high-dose amoxicillin should be used if an antibiotic has been taken during the last 3 months. Patients with a significant comorbidity can be treated with a fluoroquinolone without regard to recent antibiotic use. Alternatively, a macrolide can be used alone in patients who have not taken an antibiotic in 3 months, but otherwise must be used in combination with high-dose amoxicillin. High-dose amoxicillin/clavulanate or cefpodoxime, cefprozil, or cefuroxime can be used in those with a significant comorbidity and recent antibiotic use.
TABLE 1
Initial empiric therapy in outpatients with community-acquired pneumonia
| Clinical characteristics | No recent antibiotic therapy | Antibiotics during past 3 months |
|---|---|---|
| Previously healthy |
|
|
| Comorbidities (chronic obstructive pulmonary disease, diabetes, renal failure, congestive heart failure, malignancy) |
|
|
| Suspected aspiration with infection |
| |
| Influenza with bacterial superinfection |
| |
| Adapted from Mandell et al.5 © 2003 Infectious Diseases Society of America. | ||
Bacterial bronchitis
A panel of primary care physicians and specialists convened by the Canadian Thoracic Society (CTS) reviewed nearly 400 published articles on acute bacterial exacerbations of chronic bronchitis, including evidence-based reviews such as the Cochrane Database. The 2003 CTS guidelines recommend that treatment be based on the risk for treatment failure (TABLE 2).8
Antibacterial treatment is not recommended for patients whose clinical history and symptoms suggest a viral infection (group 0) unless symptoms persist for more than 10 to 14 days. In those cases, bacterial superinfection with M pneumoniae, C pneumoniae, or Bordetella pertussis is possible. Patients with chronic bronchitis but without risk factors for treatment failure (group 1) may be treated with a variety of first-line agents, including azithromycin, clarithromycin, cefuroxime, cefprozil, cefixime, amoxicillin, doxycycline, or trimethoprim/sulfamethoxazole. For patients in group 1 who fail first-line therapy, and as first-line therapy for patients in group 2, a fluoroquinolone or amoxicillin/clavulanate is recommended. Patients in group 3 are more likely to be infected with a Gram-negative pathogen, such as Ps aeruginosa or Enterobacter species, and are least able to tolerate treatment failure. Hence, ciprofloxacin is appropriate in the outpatient setting.
TABLE 2
Initial empiric therapy in outpatients with acute bacterial exacerbations of chronic bronchitis
| Group | Clinical status | Symptoms/risk factors | Initial treatment | Alternative when 1st-line agent fails |
|---|---|---|---|---|
| 0 | Acute tracheobronchitis |
|
|
|
| 1 | Chronic bronchitis without risk factors |
|
|
|
| 2 | Chronic bronchitis with risk factors |
|
|
|
| 3 | Chronic suppurative bronchitis |
|
| |
| Adapted from Balter et al,8 with permission. The publisher of Can Respir J does not assume responsibility for errors or discrepancies that may have occurred. | ||||
Bacterial rhinosinusitis
The recommendations for management of acute bacterial rhinosinusitis issued by the Sinus and Allergy Health Partnership (SAHP), a not-for-profit organization created by the American Academy of Otolaryngic Allergy, the American Academy of Otolaryngology-Head and Neck Surgery, and the American Rhinologic Society, are based on a variety of factors. These include rate of spontaneous resolution, pathogen distribution, antibacterial resistance data, the importance of S pneumoniae in intracranial and extrasinus complications, and the ability of a patient to tolerate treatment failure (TABLE 3).17 The panel reviewed more than 150 published articles on management of children and adults with bacterial rhinosinusitis.
As in the pneumonia guidelines, recent antibiotic use is an important consideration when selecting an antibiotic since resistant pathogens are likely. β-Lactam agents play a major role as initial therapy in both children and adults. This recommendation is consistent with those of Williams et al who reviewed 49 clinical trials involving 13,660 patients. These investigators recommended 7 to 14 days of penicillin or amoxicillin for acute maxillary sinusitis confirmed radiographically or by aspiration.38
The SAHP recommended higher doses of amoxicillin (with or without clavulanate) in patients who have recently taken an antibiotic or who have moderate disease. Fluoroquinolones are recommended as alternatives in patients with mild disease who have not taken an antibiotic in the last 4 to 6 weeks. However, in patients with mild disease who have taken antibiotics recently or who have moderate disease, fluoroquinolones are recommended as first-line therapy. Macrolides are recommended only for patients with a β-lactam allergy since failure rates of 20% to 25% are possible. Lack of improvement or worsening symptoms after 72 hours should prompt reevaluation, may necessitate cultures and/or a CT scan, and should raise the possibility of causal organisms other than S pneumoniae, H influenzae, and M catarrhalis.
TABLE 3
Initial empiric therapy in outpatients with acute bacterial rhinosinusitis
| Initial therapy | Alternative agent if no improvement or worsening after 72 hours | |
|---|---|---|
| Mild disease, no antibiotic during past 4 to 6 weeks | ||
| Children |
|
|
| Children with β-lactam allergy |
|
|
| Adults |
|
|
| Adults with β-lactam allergy |
|
|
| Mild disease and antibiotic during past 4 to 6 weeks or moderate disease | ||
| Children |
|
|
| Children with β-lactam allergy |
|
|
| Adults |
|
|
| Adults with β-lactam allergy |
|
|
| Adapted from Anon et al17 © 2004, with permission from American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. | ||
Dose and duration
While each of the three guidelines provides detailed recommendations regarding selection of an antibacterial agent, the dose and duration of therapy generally are not well defined. Fortunately, other sources provide guidance in these 2 areas.
First, an independent international panel of infectious diseases experts, whose goal was to identify ways to improve prescription of antibiotics for lower respiratory tract infections, stressed that an important purpose of therapy is to reduce bacterial load and, in fact, treat to bacteriologic cure.19 Antibiotic therapy that allows some bacteria to survive increases the risk of early recurrence or relapse and encourages resistance selection. Such therapy is, therefore, inappropriate. The panel concurred with the WHO and others that the likelihood of bacterial persistence increases when antibiotics are prescribed in low doses, especially if given over long periods.18,39-41 Prolonged low-dose antibiotic therapy, which has been common practice for many infections, is contrary to the WHO Global Strategy for Containment of Antimicrobial Resistance, which notes that single-agent therapy for a short duration is 1 of several actions that can be taken to minimize bacterial resistance.42 Shorter courses of antibiotic therapy also are consistent with SHEA/IDSA recommendations.10
The clinical appropriateness of this recommendation is reinforced by the changes that have occurred during the past decade in the management of selected urinary tract infections (UTIs). Some UTIs that previously had been treated with low-dose antibiotics for 10 to 14 days now are treated with only 1 or a few high doses of a single agent. Other infections for which clinical data support shorter courses of antibiotic therapy include uncomplicated cellulitis,43 ventilator-associated pneumonia,44 and meningococcal disease.45
Shorter-course antibacterial therapy for CARTIs increasingly has been the focus of clinical trials. The focus is not unreasonable. Many of the antibiotics used for CARTIs are very potent against the pathogens commonly encountered, penetrate infected tissues well, are available in oral formulations, and are generally well tolerated. However, to optimize an antibiotic’s bactericidal potential, it is necessary to base the dosing regimen on its pharmacodynamics. From a pharmacodynamic perspective, there are 2 groups of antibiotics, those with concentration-dependent killing and those with time-dependent killing. For agents with concentration-dependent killing, such as fluoroquinolones, ketolides, and aminoglycosides, the goal is to select a dose that achieves a higher peak concentration and/or a larger area under the plasma concentration curve, with acceptable tolerability. In contrast, antibiotics that rely on time-dependent killing, such as β-lactams, macrolides, azalides, tetracyclines, and some others, require extended durations of concentrations above the MIC90 of the bacterial pathogen(s). Consequently, multiple daily dosing may be preferable.46
Dose. A few studies have compared high-dose, short-course therapy with therapy using standard doses and durations (TABLE 4). To assess the impact of highdose, short-course therapy on post-treatment resistant pneumococcal carriage, Schrag compared amoxicillin given either as 90 mg/kg/day for 5 days (high-dose, short-course) or 40 mg/kg/day for 10 days (standard) in 797 children with a respiratory tract infection.47 At day 28, nasal carriage of penicillin-resistant S pneumoniae was detected in 24% of the high-dose, shortcourse group and in 32% of the standard group (relative risk, 0.77; P=0.03). Among the pneumococcal carriers, the risk of penicillin-resistant S pneumoniae was significantly lower in the high-dose, short-course group than in the standard therapy group (relative risk, 0.78; P=0.01)
Another study investigated high-dose, short-course therapy with levofloxacin in patients with mild to severe community-acquired pneumonia. Patients received levofloxacin 750 mg/d for 5 days or 500 mg/d for 10 days.48 The clinical success rates were 92.4% and 91.1%, respectively, while the bacteriologic eradication rates at 7 to 14 days post-therapy were 93.2% and 92.4%, respectively, thereby demonstrating that high-dose, shortcourse levofloxacin therapy is at least as effective as standard levofloxacin therapy.
Duration. Short-course therapy using standard doses of azithromycin, gemifloxacin, levofloxacin, moxifloxacin, and telithromycin has been investigated in clinical trials of CARTIs (FIGURE). In patients with community-acquired pneumonia, 5 days of therapy with telithromycin was shown to be equivalent to a 7-day course (both using a single daily dose of 800 mg), as well as to clarithromycin 500 mg bid for 10 days.49
In studies of acute exacerbations of chronic bronchitis, a 3-day course of azithromycin was equivalent to clarithromycin for 10 days50 and gemifloxacin for 5 days was equivalent to a sequential combination of ceftriaxone and cefuroxime axetil for up to 10 days.51 Levofloxacin for 3 days and azithromycin for 5 days provided equivalent outcomes,52 as did levofloxacin for 5 days and amoxicillin/clavulanate for 10 days.52 Moxifloxacin for 5 days provided results equivalent to those of 7 days of amoxicillin, clarithromycin, or cefuroxime axetil.53 Five days of telithromycin was shown to be equivalent to 10 days of amoxicillin/clavu-lanate54 or cefuroxime axetil.55
Studies of acute bacterial rhinosinusitis have demonstrated equivalent results with azithromycin for 3 days and amoxicillin/clavulanate for 10 days.50 Similarly, telithromycin for 5 days was equivalent to 10 days of telithromycin, amoxicillin/clavulanate, or cefuroxime axetil.56
These clinical trials demonstrate that short-course therapy achieves clinical cure and/or bacteriologic eradication rates that are at least equivalent to those of standard therapy, with no significant difference in safety. Symptomatic improvement is faster and total antibiotic exposure is reduced with short-course therapy.
A significant advantage of short-course antibacterial therapy is improved patient adherence. Adherence is 10% to 20% better with 5-day courses than with 10-day courses,47,57 and is significantly better with 1 or 2 daily doses than with 3 or more daily doses.58-60 In fact, a recent market research study showed that patients perceive once-daily, short-course antibiotic treatment to be significantly more effective than longer courses. This may be due to faster improvement of infection-related symptoms.61 For example, Dunbar et al observed that significantly more patients treated with high-dose, short-course levofloxacin experienced subjective and objective resolution of fever by day 3 compared with those who received standard-dose, short-course levofloxacin.48
TABLE 4
Clinical trials of high-dose, short-course antibiotic therapy
| Drug regimen | N (ref) | Outcome |
|---|---|---|
| Amoxicillin 90 mg/kg/d x 5 d vs Amoxicillin 40 mg/kg/d x 10 d | 797 |
|
| (47) | ||
| Levofloxacin 750 mg/d x 5d vs Levofloxacin 500 mg/d x 10 d | 390 |
|
| (48) |
TABLE 5 Clinical trials of standard-dose, short-course antibiotic therapy
Summary
Essential questions that need to be answered for every patient who presents with a possible CARTI include : 1) Is antibacterial therapy necessary? 2) If so, what is the best antibiotic and at what dose and for how long should it be administered? Accumulating evidence indicates that some antibiotics when given in high doses for a short duration are as effective and safe as standard therapy for CARTIs. Short-course therapy also promotes patient compliance.
Disclosures:
The authors reported the following financial relationships: Dr Brunton: consultant to Abbott, Ortho-McNeil Pharmaceutical, Inc., and SanofiAventis. Dr Carmichael: consultant to Ortho-McNeil Pharmaceutical, Inc.; on the speakers’ bureaus for Bristol-Myers Squibb Company, Merck & Co., OrthoMcNeil Pharmaceutical, Inc., and Pfizer Inc. Dr Fitzgerald: on the speakers’ bureaus for Boehringer Ingelheim, GlaxoSmithKline, Ortho-McNeil Pharmaceutical, Inc., Pfizer Inc., Sepracor Inc., and 3M. Dr Liu: on the speakers’ bureaus for Aventis Pharmaceuticals, Bayer Pharmaceuticals Corporation, Bristol-Myers Squibb Company, Cobist, GlaxoSmithKline, Merck & Co., Ortho-McNeil Pharmaceutical, Inc., Pfizer Inc., Purdue Pharma, Oscient Pharmaceuticals Corporation, and Wyeth Pharmaceuticals. Dr Varon: on the speakers’ bureau for Ortho-McNeil Pharmaceutical, Inc. Dr. Weiland: consultant to Abbott Laboratories, Ortho-McNeil Pharmaceutical, Inc., and Pfizer Inc.
This supplement to The Journal of Family Practice is supported by a grant from Ortho-McNeil Pharmaceutical, Inc. It was adapted from a consensus conference coordinated by the Primary Care Education Consortium and Texas Academy of Family Physicians and was edited and peer-reviewed by The Journal of Family Practice. © 2005 Quadrant HealthCom Inc. and Primary Care Education Consortium.
- To minimize development and spread of antibiotic resistance, it is important to administer the correct antibacterial, by the best route, in the right amount, at optimum intervals, and for the appropriate duration.
- Streptococcus pneumoniae and Haemophilus influenzae are the 2 most common bacterial pathogens observed in community-acquired respiratory tract infections.
- Surveillance studies indicate increasing rates of in vitro resistance by S pneumoniae to many β-lactam and macrolide antibiotics.
- To minimize risk of resistance-associated recurrence or relapse, antibacterial agents should be prescribed in accordance with existing guidelines and local resistance patterns. Patient compliance with dosage and duration of therapy should be fostered.
- Preliminary data suggest that high-dose, short-course antibacterial therapy may be as effective as longer courses of low-dose therapy.
Community-acquired respiratory tract infections (CARTIs) are a reason for seeking medical attention. In 2001, there were 28.4 million office visits in the United States for an acute respiratory tract infection (excluding pharyngitis).1
Management of CARTIs poses several challenges. According to the World Health Organization (WHO), “for every 100 respiratory infections, only 20% require antibiotic treatment”2 —the remaining 80 infections most likely have a viral origin. Thus, antibacterial therapy should be avoided unless a bacterial cause has been confirmed or is deemed likely.
Once that determination has been made, clinicians need to separate patients who can be safely managed as outpatients from those who need to be hospitalized. Disease severity is, of course, an important consideration in this selection process.3-8
For management of patients who will not be hospitalized, the WHO and the Society for Healthcare Epidemiology of America/Infectious Diseases Society of America (SHEA/IDSA) offer the 3 Ds: administer the correct drug, at the right dose, and for the appropriate duration, to minimize development and spread of resistance.9,10 A recent consensus conference coordinated by the Primary Care Education Consortium and Texas Academy of Family Physicians elaborated on this mnemonic as it relates to outpatient management of 3 CARTIs: community-acquired pneumonia, acute bacterial exacerbations of chronic bronchitis, and acute bacterial rhinosinusitis. Its recommendations, which have been drawn largely from existing evidence-based guidelines, form the basis for this review.
Drug selection
Treatment with an antibacterial agent will not be medically warranted in the majority of patients with a CARTI. Many of these patients will, however, expect to go home with an antibiotic prescription. The primary care clinician can reduce such expectations and prevent unnecessary reconsultations by briefly addressing four issues: 1) the natural course of the viral illness, 2) the lack of effectiveness of antibiotics, 3) the problem of antibiotic resistance, and 4) the side effects of antibiotics.11
When selecting an antibacterial agent for patients with pneumonia, bronchitis, or rhinosinusitis for which a bacterial cause has been identified or deemed likely, several factors need to be taken into account, including the suspected or identified pathogens, local resistance patterns, previous therapy, patient allergies, and the patient’s ability to tolerate treatment failure. Many of these factors are considered by professional organizations that regularly develop guidelines for CARTIs based on the best available evidence. Perhaps most critical for decision-making in the primary care setting is an understanding of evolving microbiology and resistance patterns.
Common pathogens
There is considerable overlap among pathogens commonly found in CARTIs. Streptococcus pneumoniae and Haemophilus influenzae are most often observed in the outpatient setting.
Community-acquired pneumonia. In outpatients with mild illness, S pneumoniae, Mycoplasma pneumoniae, Chlamydia species (particularly Chlamydia pneumoniae, now called Chlamydophilia pneumoniae), and H influenzae are the most common pathogens.12,13 In patients younger than 50 years without significant comorbidity, Mycoplasma species are the most common pathogens. Older patients and those with significant comorbidity are more likely infected with S pneumoniae,13 a Gram-negative enteric bacillus, Pseudomonas aeruginosa, or Legionella.5,14
Bacterial bronchitis. In addition to S pneumoniae and H influenzae, Moraxella catarrhalis is a frequent pathogen in bacterial exacerbations of chronic bronchitis.15P aeruginosa and other Gram-negative bacilli are also seen, especially in patients with a severe acute exacerbation who have a forced expiratory volume in 1 second (FEV1) of 35% of predicted or less.16 Infection due to multiple pathogens occurs in a small percentage of all patients with chronic bronchitis, particularly those with severe exacerbations. Fewer than 10% of acute exacerbations are due to an atypical bacterium, usually C pneumoniae. M pneumoniae and Legionella pneumophila are implicated even less frequently.15
Bacterial rhinosinusitis.S pneumoniae and H influenzae also are frequent causes of acute bacterial rhinosinusitis. Other pathogens commonly seen in this condition include other Streptococcus species, M catarrhalis, oral anaerobes, Staphylococcus aureus in adults, and M catarrhalis, Streptococcus pyogenes, and anaerobes in children.17
Resistance
Antibiotic resistance is an important consideration in the management of CARTIs. There is little doubt that widespread use of antibiotics leads to in vitro bacterial resistance.18-20 However, because clinical success has been observed in the presence of pathogens with low-level resistance, there is some debate as to whether low-level antibiotic resistance has a significant effect on clinical outcomes.18,21-29 Even so, the US Centers for Disease Control and Prevention has determined that people who attend or work at child-care centers and those who recently used antimicrobial agents are at increased risk for infection with drug-resistant S pneumoniae.30 Moreover, the WHO has stated that infection with resistant pathogens prolongs illness and increases the probability of a fatal outcome.31
Several surveillance programs that monitor antibiotic resistance patterns—including the Alexander Project32 and Tracking Resistance in the United States Today (TRUST)33-36 —have confirmed widespread resistance to antibiotics commonly used to treat CARTIs in the United States. β-Lactam resistance due to penicillin-binding protein changes in S pneumoniae has increased significantly over the past decade. Generally, more than 30% of S pneumoniae are now resistant to penicillins and macrolides (including azithromycin and clarithromycin, the ‘advanced’ agents in this group). A smaller number (6%) are resistant to amoxicillin/clavulanate, although this appears to be a result of in vitro test parameters involving primarily strains with high-level β-lactam resistance. Some cephalosporins also show greater activity than penicillin against intermediately susceptible S pneumoniae, but are not effective against highly resistant strains. In contrast, fewer than 1% of all pneumococci are resistant to newer fluoroquinolones (the so-called respiratory fluoroquinolones, such as gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin) and the ketolide telithromycin.
The prevalence of β-lactamase–producing strains of H influenzae appears to have leveled off. Approximately 30% of H influenzae strains are resistant to ampicillin, while fewer than 1% are resistant to amoxicillin/clavulanate, cefuroxime, macrolides, and newer fluoroquinolones.
More than 90% of M catarrhalis isolates produce β-lactamase, thereby conferring resistance to ampicillin and amoxicillin.
Significant geographical variation in resistance has been observed. The prevalence of penicillin-resistant S pneumoniae ranges from 8% in New England to 25% in the South Atlantic, while ampicillin-resistant H influenzae is seen most often in New England (35%) and least often in the Rocky Mountain region (24%).33,34,36 Significant differences within a community also have been observed.37 Thus, knowledge of local resistance patterns is necessary. This information generally is available from local hospitals, although such data may be more reflective of nosocomial pathogens, or state health departments.
Community-acquired pneumonia
The 2003 guidelines of the IDSA give advanced macrolides and respiratory fluoroquinolones a prominent role in the management of community-acquired pneumonia (TABLE 1).5 The IDSA reviewed data from more than 150 clinical trials conducted in adults over 15 years. The IDSA panel acknowledged the increasing in vitro resistance of S pneumoniae to the macrolides, but noted that reports of clinical failure have not paralleled this. The panel also pointed out the significantly lower rates of resistance to the respiratory fluoroquinolones and expressed concern that abuse of these agents could lead to increased resistance by S pneumoniae.
In a previously healthy person who has not taken an antibiotic in the last 3 months, the IDSA recommends a macrolide or doxycycline as first-line therapy, whereas a fluoroquinolone, high-dose amoxicillin/clavulanate, or a macrolide plus high-dose amoxicillin should be used if an antibiotic has been taken during the last 3 months. Patients with a significant comorbidity can be treated with a fluoroquinolone without regard to recent antibiotic use. Alternatively, a macrolide can be used alone in patients who have not taken an antibiotic in 3 months, but otherwise must be used in combination with high-dose amoxicillin. High-dose amoxicillin/clavulanate or cefpodoxime, cefprozil, or cefuroxime can be used in those with a significant comorbidity and recent antibiotic use.
TABLE 1
Initial empiric therapy in outpatients with community-acquired pneumonia
| Clinical characteristics | No recent antibiotic therapy | Antibiotics during past 3 months |
|---|---|---|
| Previously healthy |
|
|
| Comorbidities (chronic obstructive pulmonary disease, diabetes, renal failure, congestive heart failure, malignancy) |
|
|
| Suspected aspiration with infection |
| |
| Influenza with bacterial superinfection |
| |
| Adapted from Mandell et al.5 © 2003 Infectious Diseases Society of America. | ||
Bacterial bronchitis
A panel of primary care physicians and specialists convened by the Canadian Thoracic Society (CTS) reviewed nearly 400 published articles on acute bacterial exacerbations of chronic bronchitis, including evidence-based reviews such as the Cochrane Database. The 2003 CTS guidelines recommend that treatment be based on the risk for treatment failure (TABLE 2).8
Antibacterial treatment is not recommended for patients whose clinical history and symptoms suggest a viral infection (group 0) unless symptoms persist for more than 10 to 14 days. In those cases, bacterial superinfection with M pneumoniae, C pneumoniae, or Bordetella pertussis is possible. Patients with chronic bronchitis but without risk factors for treatment failure (group 1) may be treated with a variety of first-line agents, including azithromycin, clarithromycin, cefuroxime, cefprozil, cefixime, amoxicillin, doxycycline, or trimethoprim/sulfamethoxazole. For patients in group 1 who fail first-line therapy, and as first-line therapy for patients in group 2, a fluoroquinolone or amoxicillin/clavulanate is recommended. Patients in group 3 are more likely to be infected with a Gram-negative pathogen, such as Ps aeruginosa or Enterobacter species, and are least able to tolerate treatment failure. Hence, ciprofloxacin is appropriate in the outpatient setting.
TABLE 2
Initial empiric therapy in outpatients with acute bacterial exacerbations of chronic bronchitis
| Group | Clinical status | Symptoms/risk factors | Initial treatment | Alternative when 1st-line agent fails |
|---|---|---|---|---|
| 0 | Acute tracheobronchitis |
|
|
|
| 1 | Chronic bronchitis without risk factors |
|
|
|
| 2 | Chronic bronchitis with risk factors |
|
|
|
| 3 | Chronic suppurative bronchitis |
|
| |
| Adapted from Balter et al,8 with permission. The publisher of Can Respir J does not assume responsibility for errors or discrepancies that may have occurred. | ||||
Bacterial rhinosinusitis
The recommendations for management of acute bacterial rhinosinusitis issued by the Sinus and Allergy Health Partnership (SAHP), a not-for-profit organization created by the American Academy of Otolaryngic Allergy, the American Academy of Otolaryngology-Head and Neck Surgery, and the American Rhinologic Society, are based on a variety of factors. These include rate of spontaneous resolution, pathogen distribution, antibacterial resistance data, the importance of S pneumoniae in intracranial and extrasinus complications, and the ability of a patient to tolerate treatment failure (TABLE 3).17 The panel reviewed more than 150 published articles on management of children and adults with bacterial rhinosinusitis.
As in the pneumonia guidelines, recent antibiotic use is an important consideration when selecting an antibiotic since resistant pathogens are likely. β-Lactam agents play a major role as initial therapy in both children and adults. This recommendation is consistent with those of Williams et al who reviewed 49 clinical trials involving 13,660 patients. These investigators recommended 7 to 14 days of penicillin or amoxicillin for acute maxillary sinusitis confirmed radiographically or by aspiration.38
The SAHP recommended higher doses of amoxicillin (with or without clavulanate) in patients who have recently taken an antibiotic or who have moderate disease. Fluoroquinolones are recommended as alternatives in patients with mild disease who have not taken an antibiotic in the last 4 to 6 weeks. However, in patients with mild disease who have taken antibiotics recently or who have moderate disease, fluoroquinolones are recommended as first-line therapy. Macrolides are recommended only for patients with a β-lactam allergy since failure rates of 20% to 25% are possible. Lack of improvement or worsening symptoms after 72 hours should prompt reevaluation, may necessitate cultures and/or a CT scan, and should raise the possibility of causal organisms other than S pneumoniae, H influenzae, and M catarrhalis.
TABLE 3
Initial empiric therapy in outpatients with acute bacterial rhinosinusitis
| Initial therapy | Alternative agent if no improvement or worsening after 72 hours | |
|---|---|---|
| Mild disease, no antibiotic during past 4 to 6 weeks | ||
| Children |
|
|
| Children with β-lactam allergy |
|
|
| Adults |
|
|
| Adults with β-lactam allergy |
|
|
| Mild disease and antibiotic during past 4 to 6 weeks or moderate disease | ||
| Children |
|
|
| Children with β-lactam allergy |
|
|
| Adults |
|
|
| Adults with β-lactam allergy |
|
|
| Adapted from Anon et al17 © 2004, with permission from American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. | ||
Dose and duration
While each of the three guidelines provides detailed recommendations regarding selection of an antibacterial agent, the dose and duration of therapy generally are not well defined. Fortunately, other sources provide guidance in these 2 areas.
First, an independent international panel of infectious diseases experts, whose goal was to identify ways to improve prescription of antibiotics for lower respiratory tract infections, stressed that an important purpose of therapy is to reduce bacterial load and, in fact, treat to bacteriologic cure.19 Antibiotic therapy that allows some bacteria to survive increases the risk of early recurrence or relapse and encourages resistance selection. Such therapy is, therefore, inappropriate. The panel concurred with the WHO and others that the likelihood of bacterial persistence increases when antibiotics are prescribed in low doses, especially if given over long periods.18,39-41 Prolonged low-dose antibiotic therapy, which has been common practice for many infections, is contrary to the WHO Global Strategy for Containment of Antimicrobial Resistance, which notes that single-agent therapy for a short duration is 1 of several actions that can be taken to minimize bacterial resistance.42 Shorter courses of antibiotic therapy also are consistent with SHEA/IDSA recommendations.10
The clinical appropriateness of this recommendation is reinforced by the changes that have occurred during the past decade in the management of selected urinary tract infections (UTIs). Some UTIs that previously had been treated with low-dose antibiotics for 10 to 14 days now are treated with only 1 or a few high doses of a single agent. Other infections for which clinical data support shorter courses of antibiotic therapy include uncomplicated cellulitis,43 ventilator-associated pneumonia,44 and meningococcal disease.45
Shorter-course antibacterial therapy for CARTIs increasingly has been the focus of clinical trials. The focus is not unreasonable. Many of the antibiotics used for CARTIs are very potent against the pathogens commonly encountered, penetrate infected tissues well, are available in oral formulations, and are generally well tolerated. However, to optimize an antibiotic’s bactericidal potential, it is necessary to base the dosing regimen on its pharmacodynamics. From a pharmacodynamic perspective, there are 2 groups of antibiotics, those with concentration-dependent killing and those with time-dependent killing. For agents with concentration-dependent killing, such as fluoroquinolones, ketolides, and aminoglycosides, the goal is to select a dose that achieves a higher peak concentration and/or a larger area under the plasma concentration curve, with acceptable tolerability. In contrast, antibiotics that rely on time-dependent killing, such as β-lactams, macrolides, azalides, tetracyclines, and some others, require extended durations of concentrations above the MIC90 of the bacterial pathogen(s). Consequently, multiple daily dosing may be preferable.46
Dose. A few studies have compared high-dose, short-course therapy with therapy using standard doses and durations (TABLE 4). To assess the impact of highdose, short-course therapy on post-treatment resistant pneumococcal carriage, Schrag compared amoxicillin given either as 90 mg/kg/day for 5 days (high-dose, short-course) or 40 mg/kg/day for 10 days (standard) in 797 children with a respiratory tract infection.47 At day 28, nasal carriage of penicillin-resistant S pneumoniae was detected in 24% of the high-dose, shortcourse group and in 32% of the standard group (relative risk, 0.77; P=0.03). Among the pneumococcal carriers, the risk of penicillin-resistant S pneumoniae was significantly lower in the high-dose, short-course group than in the standard therapy group (relative risk, 0.78; P=0.01)
Another study investigated high-dose, short-course therapy with levofloxacin in patients with mild to severe community-acquired pneumonia. Patients received levofloxacin 750 mg/d for 5 days or 500 mg/d for 10 days.48 The clinical success rates were 92.4% and 91.1%, respectively, while the bacteriologic eradication rates at 7 to 14 days post-therapy were 93.2% and 92.4%, respectively, thereby demonstrating that high-dose, shortcourse levofloxacin therapy is at least as effective as standard levofloxacin therapy.
Duration. Short-course therapy using standard doses of azithromycin, gemifloxacin, levofloxacin, moxifloxacin, and telithromycin has been investigated in clinical trials of CARTIs (FIGURE). In patients with community-acquired pneumonia, 5 days of therapy with telithromycin was shown to be equivalent to a 7-day course (both using a single daily dose of 800 mg), as well as to clarithromycin 500 mg bid for 10 days.49
In studies of acute exacerbations of chronic bronchitis, a 3-day course of azithromycin was equivalent to clarithromycin for 10 days50 and gemifloxacin for 5 days was equivalent to a sequential combination of ceftriaxone and cefuroxime axetil for up to 10 days.51 Levofloxacin for 3 days and azithromycin for 5 days provided equivalent outcomes,52 as did levofloxacin for 5 days and amoxicillin/clavulanate for 10 days.52 Moxifloxacin for 5 days provided results equivalent to those of 7 days of amoxicillin, clarithromycin, or cefuroxime axetil.53 Five days of telithromycin was shown to be equivalent to 10 days of amoxicillin/clavu-lanate54 or cefuroxime axetil.55
Studies of acute bacterial rhinosinusitis have demonstrated equivalent results with azithromycin for 3 days and amoxicillin/clavulanate for 10 days.50 Similarly, telithromycin for 5 days was equivalent to 10 days of telithromycin, amoxicillin/clavulanate, or cefuroxime axetil.56
These clinical trials demonstrate that short-course therapy achieves clinical cure and/or bacteriologic eradication rates that are at least equivalent to those of standard therapy, with no significant difference in safety. Symptomatic improvement is faster and total antibiotic exposure is reduced with short-course therapy.
A significant advantage of short-course antibacterial therapy is improved patient adherence. Adherence is 10% to 20% better with 5-day courses than with 10-day courses,47,57 and is significantly better with 1 or 2 daily doses than with 3 or more daily doses.58-60 In fact, a recent market research study showed that patients perceive once-daily, short-course antibiotic treatment to be significantly more effective than longer courses. This may be due to faster improvement of infection-related symptoms.61 For example, Dunbar et al observed that significantly more patients treated with high-dose, short-course levofloxacin experienced subjective and objective resolution of fever by day 3 compared with those who received standard-dose, short-course levofloxacin.48
TABLE 4
Clinical trials of high-dose, short-course antibiotic therapy
| Drug regimen | N (ref) | Outcome |
|---|---|---|
| Amoxicillin 90 mg/kg/d x 5 d vs Amoxicillin 40 mg/kg/d x 10 d | 797 |
|
| (47) | ||
| Levofloxacin 750 mg/d x 5d vs Levofloxacin 500 mg/d x 10 d | 390 |
|
| (48) |
TABLE 5 Clinical trials of standard-dose, short-course antibiotic therapy
Summary
Essential questions that need to be answered for every patient who presents with a possible CARTI include : 1) Is antibacterial therapy necessary? 2) If so, what is the best antibiotic and at what dose and for how long should it be administered? Accumulating evidence indicates that some antibiotics when given in high doses for a short duration are as effective and safe as standard therapy for CARTIs. Short-course therapy also promotes patient compliance.
Disclosures:
The authors reported the following financial relationships: Dr Brunton: consultant to Abbott, Ortho-McNeil Pharmaceutical, Inc., and SanofiAventis. Dr Carmichael: consultant to Ortho-McNeil Pharmaceutical, Inc.; on the speakers’ bureaus for Bristol-Myers Squibb Company, Merck & Co., OrthoMcNeil Pharmaceutical, Inc., and Pfizer Inc. Dr Fitzgerald: on the speakers’ bureaus for Boehringer Ingelheim, GlaxoSmithKline, Ortho-McNeil Pharmaceutical, Inc., Pfizer Inc., Sepracor Inc., and 3M. Dr Liu: on the speakers’ bureaus for Aventis Pharmaceuticals, Bayer Pharmaceuticals Corporation, Bristol-Myers Squibb Company, Cobist, GlaxoSmithKline, Merck & Co., Ortho-McNeil Pharmaceutical, Inc., Pfizer Inc., Purdue Pharma, Oscient Pharmaceuticals Corporation, and Wyeth Pharmaceuticals. Dr Varon: on the speakers’ bureau for Ortho-McNeil Pharmaceutical, Inc. Dr. Weiland: consultant to Abbott Laboratories, Ortho-McNeil Pharmaceutical, Inc., and Pfizer Inc.
This supplement to The Journal of Family Practice is supported by a grant from Ortho-McNeil Pharmaceutical, Inc. It was adapted from a consensus conference coordinated by the Primary Care Education Consortium and Texas Academy of Family Physicians and was edited and peer-reviewed by The Journal of Family Practice. © 2005 Quadrant HealthCom Inc. and Primary Care Education Consortium.
1. Centers for Disease Control and Prevention. National Center for Health Statistics website. National Ambulatory Medical Care Survey: 2001 Summary. Available at: http://www.cdc.gov/nchs/data/ad/ad337.pdf. Accessed February 2, 2005.
2. World Health Organization.World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 4. Big guns of resistance. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
3. Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med. 2003;138:109-118.
4. File TM. Community-acquired pneumonia. Lancet. 2003;362:1991-2001.
5. Mandell LA, Bartlett JG, Dowell SF, File TM, Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003;37:1405-1433.
6. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243-250.
7. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
8. Balter MS, La Forge J, Low DE, Mandell L, Grossman RF. Canadian guidelines for the management of acute exacerbations of chronic bronchitis. Can Respir J. 2003;10(suppl B):3B-32B.
9. World Health Organization. World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 5. A call to action: A massive effort to provide proper treatment. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
10. Shlaes DM, Gerding DN, John JF, Jr, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25:584-599.
11. Scottish Intercollegiate Guidelines Network. National Guideline Clearinghouse website. Community management of lower respiratory tract infection in adults. A national clinical guideline. Available at: http://www.guideline.gov/summary/summary.aspx?ss=15& doc_id=3361&nbr=2587&string=respiratory%20AND%20tract%20AND% 20infection. Accessed December 17, 2004.
12. Bochud PY, Moser F, Erard P, et al. Community-acquired pneumonia. A prospective outpatient study. Medicine (Baltimore). 2001;80:75-87.
13. Falguera M, Sacristan O, Nogues A, et al. Nonsevere community-acquired pneumonia: correlation between cause and severity or comorbidity. Arch Intern Med. 2001;161:1866-1872.
14. Ruiz M, Ewig S, Marcos MA, et al. Etiology of community-acquired pneumonia: impact of age, comorbidity, and severity. Am J Respir Crit Care Med. 1999;160:397-405.
15. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117(5 Suppl 2):380S-385S.
16. Eller J, Ede A, Schaberg T, Niederman MS, Mauch H, Lode H. Infective exacerbations of chronic bronchitis: relation between bacteriologic etiology and lung function. Chest. 1998;113:1542-1548.
17. Anon JB, Jacobs MR, Poole MD, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130(1 Suppl):1-45.
18. Albrich WC, Monnet DL, Harbarth S. Antibiotic selection pressure and resistance in Streptococcus pneumoniae. and Streptococcus pyogenes. Emerg Infect Dis. 2004;10:514-517.
19. Ball P, Baquero F, Cars O, et al. Antibiotic therapy of community respiratory tract infections: strategies for optimal outcomes and minimized resistance emergence. J Antimicrob Chemother. 2002;49:31-40.
20. Harbarth S, Albrich W, Brun-Buisson C. Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg Infect Dis. 2002;8:1460-1467.
21. Lonks JR, Garau J, Medeiros AA. Implications of antimicrobial resistance in the empirical treatment of community-acquired respiratory tract infections: the case of macrolides. J Antimicrob Chemother. 2002;50(Suppl S2):87-92.
22. Lonks JR, Garau J, Gomez L, et al. Failure of macrolide antibiotic treatment in patients with bacteremia due to erythromycin-resistant Streptococcus pneumoniae. Clin Infect Dis. 2002;35:556-564.
23. Moellering RC, Jr, Craig W, Edmond M, et al. Clinical and public health implications of macrolide-resistant Streptococcus pneumoniae. J Chemother. 2002;14(suppl 3):42-56.
24. Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:747-750.
25. Musher DM, Dowell ME, Shortridge VD, et al. Emergence of macrolide resistance during treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:630-631.
26. Waterer GW, Buckingham SC, Kessler LA, Quasney MW, Wunderink RG. Decreasing β-lactam resistance in Pneumococci. from the Memphis region: analysis of 2,152 isolates From 1996 to 2001. Chest. 2003;124:519-525.
27. Nuermberger E, Bishai WR. The clinical significance of macrolide-resistant Streptococcus pneumoniae.: it’s all relative. Clin Infect Dis. 2004;38:99-103.
28. Yu VL, Chiou CC, Feldman C, et al. An international prospective study of pneumococcal bacteremia: correlation with in vitro resistance, antibiotics administered, and clinical outcome. Clin Infect Dis. 2003;37:230-237.
29. Metlay JP. Update on community-acquired pneumonia: impact of antibiotic resistance on clinical outcomes. Curr Opin Infect Dis. 2002;15:163-167.
30. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention web site. Drug-resistant Streptococcus pneumoniae disease. Available at: http://www.cdc.gov/ncidod/dbmd/diseaseinfo/drugresisstreppneum_t.htm. Accessed January 4, 2005.
31. World Health Organization World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 3. Factors contributing to resistance. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
32. Jacobs MR, Felmingham D, Appelbaum PC, Gruneberg RN. The Alexander Project 1998-2000: susceptibility of pathogens isolated from communityacquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother. 2003;52:229-246.
33. Thornsberry C, Sahm DF, Kelly LJ, et al. Regional trends in antimicrobial resistance among clinical isolates of Streptococcus pneumoniae., Haemophilus influenzae., and Moraxella catarrhalis. in the United States: results from the TRUST Surveillance Program, 1999-2000. Clin Infect Dis. 2002;34(suppl 1):S4-S16.
34. Karlowsky JA, Thornsberry C, Jones ME, Evangelista AT, Critchley IA, Sahm DF. Factors associated with relative rates of antimicrobial resistance among Streptococcus pneumoniae. in the United States: results from the TRUST Surveillance Program (1998-2002). Clin Infect Dis. 2003;36:963-970.
35. Karlowsky JA, Kelly LJ, Thornsberry C, et al. Susceptibility to fluoroquinolones among commonly isolated Gram-negative bacilli in 2000: TRUST and TSN data for the United States. Tracking Resistance in the United States Today. The Surveillance Network. Int J Antimicrob Agents. 2002;19:21-31.
36. Karlowsky JA, Thornsberry C, Critchley IA, et al. Susceptibilities to levofloxacin in Streptococcus pneumoniae., Haemophilus influenzae., and Moraxella catarrhalis. clinical isolates from children: results from 2000-2001 and 2001-2002 TRUST studies in the United States. Antimicrob Agents Chemother. 2003;47:1790-1797.
37. Quale J, Landman D, Ravishankar J, Flores C, Bratu S. Streptococcus pneumo.-niae., Brooklyn, New York: fluoroquinolone resistance at our doorstep. Emerg Infect Dis. 2002;8:594-597.
38. Williams JW, Jr, Aguilar C, Cornell J, et al. Antibiotics for acute maxillary sinusitis. Cochrane Database Syst Rev. 2004;2:CD000243.-
39. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of β-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365-370.
40. Scheld WM. Maintaining fluoroquinolone class efficacy: review of influencing factors. Emerg Infect Dis. 2003;9:1-9.
41. Thomson KS. Minimizing quinolone resistance: are the new agents more or less likely to cause resistance? J Antimicrob Chemother. 2000;45:719-723.
42. World Health Organization. World Health Organization web site. WHO global strategy for containment of antimicrobial resistance. Available at: http://www.who.int/csr/resources/publications/drugresist/en/EGlobal_Strat.pdf. Accessed February 2, 2005.
43. Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164:1669-1674.
44. Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290:2588-2598.
45. Ellis-Pegler R, Galler L, Roberts S, Thomas M, Woodhouse A. Three days of intravenous benzyl penicillin treatment of meningococcal disease in adults. Clin Infect Dis. 2003;37:658-662.
46. Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of β-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am. 2003;17:479-501.
47. Schrag SJ, Pena C, Fernandez J, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA. 2001;286:49-56.
48. Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
49. Tellier G, Niederman MS, Nusrat R, Patel M, Lavin B. Clinical and bacteriological efficacy and safety of 5 and 7 day regimens of telithromycin once daily compared with a 10 day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother. 2004;54:515-523.
50. Zithromax [prescribing information] New York, NY: Pfizer Labs; 2004.
51. Wilson R, Langan C, Ball P, Bateman K, Pypstra R. Oral gemifloxacin once daily for 5 days compared with sequential therapy with i.v. ceftriaxone/oral cefuroxime (maximum of 10 days) in the treatment of hospitalized patients with acute exacerbations of chronic bronchitis. Respir Med. 2003;97:242-249.
52. Tennenberg A, Walker K, Khashab M, Zadelkis N. The safety and efficacy of short-course (3-5 days), 750 mg levofloxacin (LVX) for acute bacterial exacerbation of chronic bronchitis (ABECB). Presented at: American Thoracic Society 100th International Conference, May 21-26, 2004, Orlando, Fl.
53. Wilson R, Allegra L, Huchon G, et al. Short-term and long-term outcomes of moxifloxacin compared to standard antibiotic treatment in acute exacerbations of chronic bronchitis. Chest. 2004;125:953-964.
54. Aubier M, Aldons PM, Leak A, et al. Telithromycin is as effective as amoxicillin/clavulanate in acute exacerbations of chronic bronchitis. Respir Med. 2002;96:862-871.
55. Zervos MJ, Heyder AM, Leroy B. Oral telithromycin 800 mg once daily for 5 days versus cefuroxime axetil 500 mg twice daily for 10 days in adults with acute exacerbations of chronic bronchitis. J Int Med Res. 2003;31:157-169.
56. Ketek [prescribing information]. Kansas City, Mo: Aventis Pharmaceuticals Inc.; 2004.
57. Carbon C, Chatelin A, Bingen E, et al. A double-blind randomized trial comparing the efficacy and safety of a 5-day course of cefotiam hexetil with that of a 10-day course of penicillin V in adult patients with pharyngitis caused by group A β-haemolytic streptococci. J Antimicrob Chemother 1995;35:843-854.
58. Cockburn J, Gibberd RW, Reid AL, Sanson-Fisher RW. Determinants of noncompliance with short term antibiotic regimens. Br Med J (Clin Res Ed). 1987;295:814-818.
59. Greenberg RN. Overview of patient compliance with medication dosing: a literature review. Clin Ther. 1984;6:592-599.
60. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296-1310.
61. Perez-Gorricho B, Ripoll M. Does short-course antibiotic therapy better meet patient expectations? Int J Antimicrob Agents. 2003;21:222-228.
1. Centers for Disease Control and Prevention. National Center for Health Statistics website. National Ambulatory Medical Care Survey: 2001 Summary. Available at: http://www.cdc.gov/nchs/data/ad/ad337.pdf. Accessed February 2, 2005.
2. World Health Organization.World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 4. Big guns of resistance. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
3. Metlay JP, Fine MJ. Testing strategies in the initial management of patients with community-acquired pneumonia. Ann Intern Med. 2003;138:109-118.
4. File TM. Community-acquired pneumonia. Lancet. 2003;362:1991-2001.
5. Mandell LA, Bartlett JG, Dowell SF, File TM, Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003;37:1405-1433.
6. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243-250.
7. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196-204.
8. Balter MS, La Forge J, Low DE, Mandell L, Grossman RF. Canadian guidelines for the management of acute exacerbations of chronic bronchitis. Can Respir J. 2003;10(suppl B):3B-32B.
9. World Health Organization. World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 5. A call to action: A massive effort to provide proper treatment. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
10. Shlaes DM, Gerding DN, John JF, Jr, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis. 1997;25:584-599.
11. Scottish Intercollegiate Guidelines Network. National Guideline Clearinghouse website. Community management of lower respiratory tract infection in adults. A national clinical guideline. Available at: http://www.guideline.gov/summary/summary.aspx?ss=15& doc_id=3361&nbr=2587&string=respiratory%20AND%20tract%20AND% 20infection. Accessed December 17, 2004.
12. Bochud PY, Moser F, Erard P, et al. Community-acquired pneumonia. A prospective outpatient study. Medicine (Baltimore). 2001;80:75-87.
13. Falguera M, Sacristan O, Nogues A, et al. Nonsevere community-acquired pneumonia: correlation between cause and severity or comorbidity. Arch Intern Med. 2001;161:1866-1872.
14. Ruiz M, Ewig S, Marcos MA, et al. Etiology of community-acquired pneumonia: impact of age, comorbidity, and severity. Am J Respir Crit Care Med. 1999;160:397-405.
15. Sethi S. Infectious etiology of acute exacerbations of chronic bronchitis. Chest. 2000;117(5 Suppl 2):380S-385S.
16. Eller J, Ede A, Schaberg T, Niederman MS, Mauch H, Lode H. Infective exacerbations of chronic bronchitis: relation between bacteriologic etiology and lung function. Chest. 1998;113:1542-1548.
17. Anon JB, Jacobs MR, Poole MD, et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg. 2004;130(1 Suppl):1-45.
18. Albrich WC, Monnet DL, Harbarth S. Antibiotic selection pressure and resistance in Streptococcus pneumoniae. and Streptococcus pyogenes. Emerg Infect Dis. 2004;10:514-517.
19. Ball P, Baquero F, Cars O, et al. Antibiotic therapy of community respiratory tract infections: strategies for optimal outcomes and minimized resistance emergence. J Antimicrob Chemother. 2002;49:31-40.
20. Harbarth S, Albrich W, Brun-Buisson C. Outpatient antibiotic use and prevalence of antibiotic-resistant pneumococci in France and Germany: a sociocultural perspective. Emerg Infect Dis. 2002;8:1460-1467.
21. Lonks JR, Garau J, Medeiros AA. Implications of antimicrobial resistance in the empirical treatment of community-acquired respiratory tract infections: the case of macrolides. J Antimicrob Chemother. 2002;50(Suppl S2):87-92.
22. Lonks JR, Garau J, Gomez L, et al. Failure of macrolide antibiotic treatment in patients with bacteremia due to erythromycin-resistant Streptococcus pneumoniae. Clin Infect Dis. 2002;35:556-564.
23. Moellering RC, Jr, Craig W, Edmond M, et al. Clinical and public health implications of macrolide-resistant Streptococcus pneumoniae. J Chemother. 2002;14(suppl 3):42-56.
24. Davidson R, Cavalcanti R, Brunton JL, et al. Resistance to levofloxacin and failure of treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:747-750.
25. Musher DM, Dowell ME, Shortridge VD, et al. Emergence of macrolide resistance during treatment of pneumococcal pneumonia. N Engl J Med. 2002;346:630-631.
26. Waterer GW, Buckingham SC, Kessler LA, Quasney MW, Wunderink RG. Decreasing β-lactam resistance in Pneumococci. from the Memphis region: analysis of 2,152 isolates From 1996 to 2001. Chest. 2003;124:519-525.
27. Nuermberger E, Bishai WR. The clinical significance of macrolide-resistant Streptococcus pneumoniae.: it’s all relative. Clin Infect Dis. 2004;38:99-103.
28. Yu VL, Chiou CC, Feldman C, et al. An international prospective study of pneumococcal bacteremia: correlation with in vitro resistance, antibiotics administered, and clinical outcome. Clin Infect Dis. 2003;37:230-237.
29. Metlay JP. Update on community-acquired pneumonia: impact of antibiotic resistance on clinical outcomes. Curr Opin Infect Dis. 2002;15:163-167.
30. Centers for Disease Control and Prevention. Centers for Disease Control and Prevention web site. Drug-resistant Streptococcus pneumoniae disease. Available at: http://www.cdc.gov/ncidod/dbmd/diseaseinfo/drugresisstreppneum_t.htm. Accessed January 4, 2005.
31. World Health Organization World Health Organization web site. World Health Organization Report on Infectious Diseases 2000. Overcoming antimicrobial resistance. Chapter 3. Factors contributing to resistance. Available at: http://www.who.int/infectious-disease-report/2000/. Accessed February 2, 2005.
32. Jacobs MR, Felmingham D, Appelbaum PC, Gruneberg RN. The Alexander Project 1998-2000: susceptibility of pathogens isolated from communityacquired respiratory tract infection to commonly used antimicrobial agents. J Antimicrob Chemother. 2003;52:229-246.
33. Thornsberry C, Sahm DF, Kelly LJ, et al. Regional trends in antimicrobial resistance among clinical isolates of Streptococcus pneumoniae., Haemophilus influenzae., and Moraxella catarrhalis. in the United States: results from the TRUST Surveillance Program, 1999-2000. Clin Infect Dis. 2002;34(suppl 1):S4-S16.
34. Karlowsky JA, Thornsberry C, Jones ME, Evangelista AT, Critchley IA, Sahm DF. Factors associated with relative rates of antimicrobial resistance among Streptococcus pneumoniae. in the United States: results from the TRUST Surveillance Program (1998-2002). Clin Infect Dis. 2003;36:963-970.
35. Karlowsky JA, Kelly LJ, Thornsberry C, et al. Susceptibility to fluoroquinolones among commonly isolated Gram-negative bacilli in 2000: TRUST and TSN data for the United States. Tracking Resistance in the United States Today. The Surveillance Network. Int J Antimicrob Agents. 2002;19:21-31.
36. Karlowsky JA, Thornsberry C, Critchley IA, et al. Susceptibilities to levofloxacin in Streptococcus pneumoniae., Haemophilus influenzae., and Moraxella catarrhalis. clinical isolates from children: results from 2000-2001 and 2001-2002 TRUST studies in the United States. Antimicrob Agents Chemother. 2003;47:1790-1797.
37. Quale J, Landman D, Ravishankar J, Flores C, Bratu S. Streptococcus pneumo.-niae., Brooklyn, New York: fluoroquinolone resistance at our doorstep. Emerg Infect Dis. 2002;8:594-597.
38. Williams JW, Jr, Aguilar C, Cornell J, et al. Antibiotics for acute maxillary sinusitis. Cochrane Database Syst Rev. 2004;2:CD000243.-
39. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of β-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365-370.
40. Scheld WM. Maintaining fluoroquinolone class efficacy: review of influencing factors. Emerg Infect Dis. 2003;9:1-9.
41. Thomson KS. Minimizing quinolone resistance: are the new agents more or less likely to cause resistance? J Antimicrob Chemother. 2000;45:719-723.
42. World Health Organization. World Health Organization web site. WHO global strategy for containment of antimicrobial resistance. Available at: http://www.who.int/csr/resources/publications/drugresist/en/EGlobal_Strat.pdf. Accessed February 2, 2005.
43. Hepburn MJ, Dooley DP, Skidmore PJ, Ellis MW, Starnes WF, Hasewinkle WC. Comparison of short-course (5 days) and standard (10 days) treatment for uncomplicated cellulitis. Arch Intern Med. 2004;164:1669-1674.
44. Chastre J, Wolff M, Fagon JY, et al. Comparison of 8 vs 15 days of antibiotic therapy for ventilator-associated pneumonia in adults: a randomized trial. JAMA. 2003;290:2588-2598.
45. Ellis-Pegler R, Galler L, Roberts S, Thomas M, Woodhouse A. Three days of intravenous benzyl penicillin treatment of meningococcal disease in adults. Clin Infect Dis. 2003;37:658-662.
46. Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of β-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am. 2003;17:479-501.
47. Schrag SJ, Pena C, Fernandez J, et al. Effect of short-course, high-dose amoxicillin therapy on resistant pneumococcal carriage: a randomized trial. JAMA. 2001;286:49-56.
48. Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752-760.
49. Tellier G, Niederman MS, Nusrat R, Patel M, Lavin B. Clinical and bacteriological efficacy and safety of 5 and 7 day regimens of telithromycin once daily compared with a 10 day regimen of clarithromycin twice daily in patients with mild to moderate community-acquired pneumonia. J Antimicrob Chemother. 2004;54:515-523.
50. Zithromax [prescribing information] New York, NY: Pfizer Labs; 2004.
51. Wilson R, Langan C, Ball P, Bateman K, Pypstra R. Oral gemifloxacin once daily for 5 days compared with sequential therapy with i.v. ceftriaxone/oral cefuroxime (maximum of 10 days) in the treatment of hospitalized patients with acute exacerbations of chronic bronchitis. Respir Med. 2003;97:242-249.
52. Tennenberg A, Walker K, Khashab M, Zadelkis N. The safety and efficacy of short-course (3-5 days), 750 mg levofloxacin (LVX) for acute bacterial exacerbation of chronic bronchitis (ABECB). Presented at: American Thoracic Society 100th International Conference, May 21-26, 2004, Orlando, Fl.
53. Wilson R, Allegra L, Huchon G, et al. Short-term and long-term outcomes of moxifloxacin compared to standard antibiotic treatment in acute exacerbations of chronic bronchitis. Chest. 2004;125:953-964.
54. Aubier M, Aldons PM, Leak A, et al. Telithromycin is as effective as amoxicillin/clavulanate in acute exacerbations of chronic bronchitis. Respir Med. 2002;96:862-871.
55. Zervos MJ, Heyder AM, Leroy B. Oral telithromycin 800 mg once daily for 5 days versus cefuroxime axetil 500 mg twice daily for 10 days in adults with acute exacerbations of chronic bronchitis. J Int Med Res. 2003;31:157-169.
56. Ketek [prescribing information]. Kansas City, Mo: Aventis Pharmaceuticals Inc.; 2004.
57. Carbon C, Chatelin A, Bingen E, et al. A double-blind randomized trial comparing the efficacy and safety of a 5-day course of cefotiam hexetil with that of a 10-day course of penicillin V in adult patients with pharyngitis caused by group A β-haemolytic streptococci. J Antimicrob Chemother 1995;35:843-854.
58. Cockburn J, Gibberd RW, Reid AL, Sanson-Fisher RW. Determinants of noncompliance with short term antibiotic regimens. Br Med J (Clin Res Ed). 1987;295:814-818.
59. Greenberg RN. Overview of patient compliance with medication dosing: a literature review. Clin Ther. 1984;6:592-599.
60. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296-1310.
61. Perez-Gorricho B, Ripoll M. Does short-course antibiotic therapy better meet patient expectations? Int J Antimicrob Agents. 2003;21:222-228.