User login
Looking for lower Medicare drug costs? Ask your pharmacist for the cash price
As part of President Donald Trump’s blueprint to bring down prescription costs, Medicare officials have warned insurers that “gag orders” keeping pharmacists from alerting seniors that they could save money by paying cash – rather than using their insurance – are “unacceptable and contrary” to the government’s effort to promote price transparency.
But the agency stopped short of requiring insurers to lift such restrictions on pharmacists.
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.
“If they bring it up, then we can inform them of those prices,” said Nick Newman, PharmD, a pharmacist and the manager at Essentra Pharmacy in rural Marengo, Ohio. “It’s a moral dilemma for the pharmacist, knowing what would be best for the patient, but not being able to help them and hoping they will ask you about the comparison.”
A simple question could unlock some savings for millions of beneficiaries.
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
“If you don’t know that there are a bunch of different prices that could be available at any given pharmacy, you don’t know what you don’t know,” said Leigh Purvis, the AARP Public Policy Institute’s director of health services research.
Researchers analyzing 9.5 million Part D prescription claims reported in a letter in the Journal of the American Medical Association in March that a patient’s copayment was higher than the cash price for nearly one in four drugs purchased in 2013. For 12 of the 20 most commonly prescribed drugs, patients overpaid by more than 33%.
Although the study found that the average overpayment for a single prescription was relatively small, Dr. Newman said he had seen consumers pay as much as $30 more than the cash price.
And many beneficiaries may not know that, if they pay a lower cash price for a covered drug at a pharmacy that participates in their insurance plan and then submit the proper documentation, insurers must count it toward their out-of-pocket expenses. The total of those expenses can trigger the drug coverage gap, commonly called the doughnut hole. (This year, the gap begins after the plan and beneficiary spend $3,750 and ends once the beneficiary has spent a total of $5,000.)
Daniel Nam, executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter in May 2018, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
UnitedHealthcare, whose popular prescription drug plans dominate the market, does not include them in any of its Medicare, Medicaid, or commercial insurance contracts, said Matt Burns, a company spokesman.
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
However, some pharmacists disagree. Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
In Ohio, one of several states that have banned gag orders in insurance contracts, including some Medicare drug plans, officials responded to complaints about the problem.
“The Department has received inquiries related to entities withholding cost-saving information from consumers, which sometimes results in an insured [patient] paying more for pharmacy benefits than the actual cost of such pharmacy benefits,” the department said in April.
Illinois and Ohio state legislators are considering bills to make such restrictions illegal, and similar legislation has been introduced in the U.S. Senate.
“If we didn’t have these gag clauses, there would not be a need for the legislation and policy changes movement that’s going on in the country,” said Garth Reynolds, executive director of the Illinois Pharmacists Association.
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
As part of President Donald Trump’s blueprint to bring down prescription costs, Medicare officials have warned insurers that “gag orders” keeping pharmacists from alerting seniors that they could save money by paying cash – rather than using their insurance – are “unacceptable and contrary” to the government’s effort to promote price transparency.
But the agency stopped short of requiring insurers to lift such restrictions on pharmacists.
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.
“If they bring it up, then we can inform them of those prices,” said Nick Newman, PharmD, a pharmacist and the manager at Essentra Pharmacy in rural Marengo, Ohio. “It’s a moral dilemma for the pharmacist, knowing what would be best for the patient, but not being able to help them and hoping they will ask you about the comparison.”
A simple question could unlock some savings for millions of beneficiaries.
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
“If you don’t know that there are a bunch of different prices that could be available at any given pharmacy, you don’t know what you don’t know,” said Leigh Purvis, the AARP Public Policy Institute’s director of health services research.
Researchers analyzing 9.5 million Part D prescription claims reported in a letter in the Journal of the American Medical Association in March that a patient’s copayment was higher than the cash price for nearly one in four drugs purchased in 2013. For 12 of the 20 most commonly prescribed drugs, patients overpaid by more than 33%.
Although the study found that the average overpayment for a single prescription was relatively small, Dr. Newman said he had seen consumers pay as much as $30 more than the cash price.
And many beneficiaries may not know that, if they pay a lower cash price for a covered drug at a pharmacy that participates in their insurance plan and then submit the proper documentation, insurers must count it toward their out-of-pocket expenses. The total of those expenses can trigger the drug coverage gap, commonly called the doughnut hole. (This year, the gap begins after the plan and beneficiary spend $3,750 and ends once the beneficiary has spent a total of $5,000.)
Daniel Nam, executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter in May 2018, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
UnitedHealthcare, whose popular prescription drug plans dominate the market, does not include them in any of its Medicare, Medicaid, or commercial insurance contracts, said Matt Burns, a company spokesman.
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
However, some pharmacists disagree. Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
In Ohio, one of several states that have banned gag orders in insurance contracts, including some Medicare drug plans, officials responded to complaints about the problem.
“The Department has received inquiries related to entities withholding cost-saving information from consumers, which sometimes results in an insured [patient] paying more for pharmacy benefits than the actual cost of such pharmacy benefits,” the department said in April.
Illinois and Ohio state legislators are considering bills to make such restrictions illegal, and similar legislation has been introduced in the U.S. Senate.
“If we didn’t have these gag clauses, there would not be a need for the legislation and policy changes movement that’s going on in the country,” said Garth Reynolds, executive director of the Illinois Pharmacists Association.
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
As part of President Donald Trump’s blueprint to bring down prescription costs, Medicare officials have warned insurers that “gag orders” keeping pharmacists from alerting seniors that they could save money by paying cash – rather than using their insurance – are “unacceptable and contrary” to the government’s effort to promote price transparency.
But the agency stopped short of requiring insurers to lift such restrictions on pharmacists.
That doesn’t mean people with Medicare drug coverage are destined to overpay for prescriptions. But first, they must ask the pharmacist about that option, said Julie Carter, federal policy associate at the Medicare Rights Center, a patient advocacy group.
“If they bring it up, then we can inform them of those prices,” said Nick Newman, PharmD, a pharmacist and the manager at Essentra Pharmacy in rural Marengo, Ohio. “It’s a moral dilemma for the pharmacist, knowing what would be best for the patient, but not being able to help them and hoping they will ask you about the comparison.”
A simple question could unlock some savings for millions of beneficiaries.
But details may be hard to find: Medicare’s website and annual handbook don’t mention it.
“If you don’t know that there are a bunch of different prices that could be available at any given pharmacy, you don’t know what you don’t know,” said Leigh Purvis, the AARP Public Policy Institute’s director of health services research.
Researchers analyzing 9.5 million Part D prescription claims reported in a letter in the Journal of the American Medical Association in March that a patient’s copayment was higher than the cash price for nearly one in four drugs purchased in 2013. For 12 of the 20 most commonly prescribed drugs, patients overpaid by more than 33%.
Although the study found that the average overpayment for a single prescription was relatively small, Dr. Newman said he had seen consumers pay as much as $30 more than the cash price.
And many beneficiaries may not know that, if they pay a lower cash price for a covered drug at a pharmacy that participates in their insurance plan and then submit the proper documentation, insurers must count it toward their out-of-pocket expenses. The total of those expenses can trigger the drug coverage gap, commonly called the doughnut hole. (This year, the gap begins after the plan and beneficiary spend $3,750 and ends once the beneficiary has spent a total of $5,000.)
Daniel Nam, executive director of federal programs at America’s Health Insurance Plans, a trade group, agreed that “patients should have access to the lowest price possible at the pharmacy.” But he said Medicare’s warning, contained in a letter in May 2018, takes aim at an increasingly rare occurrence. Gag order clauses are “not something they are incorporating into their contracts,” he said.
UnitedHealthcare, whose popular prescription drug plans dominate the market, does not include them in any of its Medicare, Medicaid, or commercial insurance contracts, said Matt Burns, a company spokesman.
Pharmacy benefit managers also said gag orders are not typical. “If it is happening, it is very much an outlier,” said Mark Merritt, president and CEO of the Pharmaceutical Care Management Association.
However, some pharmacists disagree. Kala Shankle, policy and regulatory affairs director for the National Community Pharmacists Association, which represents 22,000 independent pharmacies, said insurers have punished pharmacists who violate gag orders by dropping them from the plan’s network.
In Ohio, one of several states that have banned gag orders in insurance contracts, including some Medicare drug plans, officials responded to complaints about the problem.
“The Department has received inquiries related to entities withholding cost-saving information from consumers, which sometimes results in an insured [patient] paying more for pharmacy benefits than the actual cost of such pharmacy benefits,” the department said in April.
Illinois and Ohio state legislators are considering bills to make such restrictions illegal, and similar legislation has been introduced in the U.S. Senate.
“If we didn’t have these gag clauses, there would not be a need for the legislation and policy changes movement that’s going on in the country,” said Garth Reynolds, executive director of the Illinois Pharmacists Association.
KHN’s coverage of prescription drug development, costs and pricing is supported by the Laura and John Arnold Foundation. Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
21 Medicare health plans warned to fix provider directory errors
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.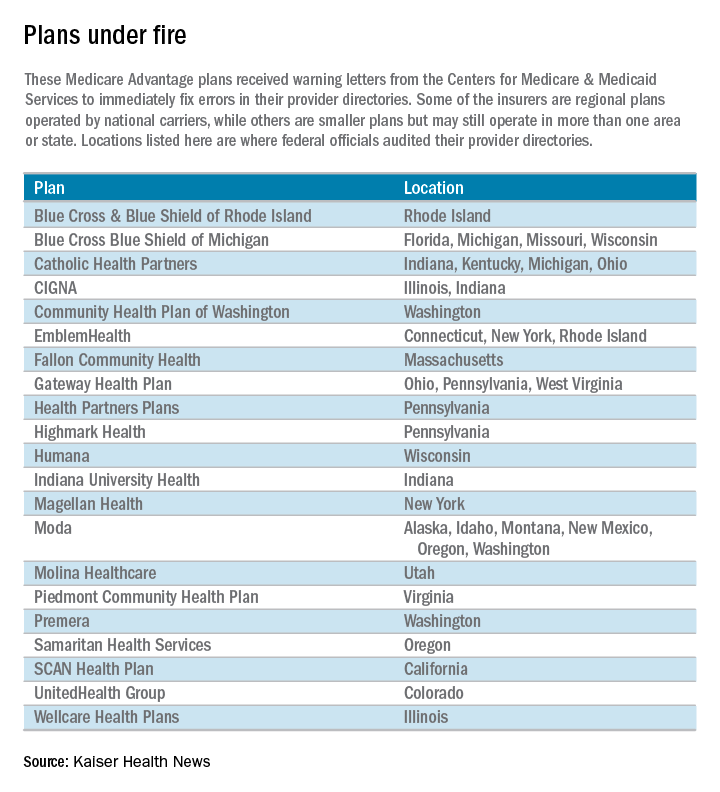
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.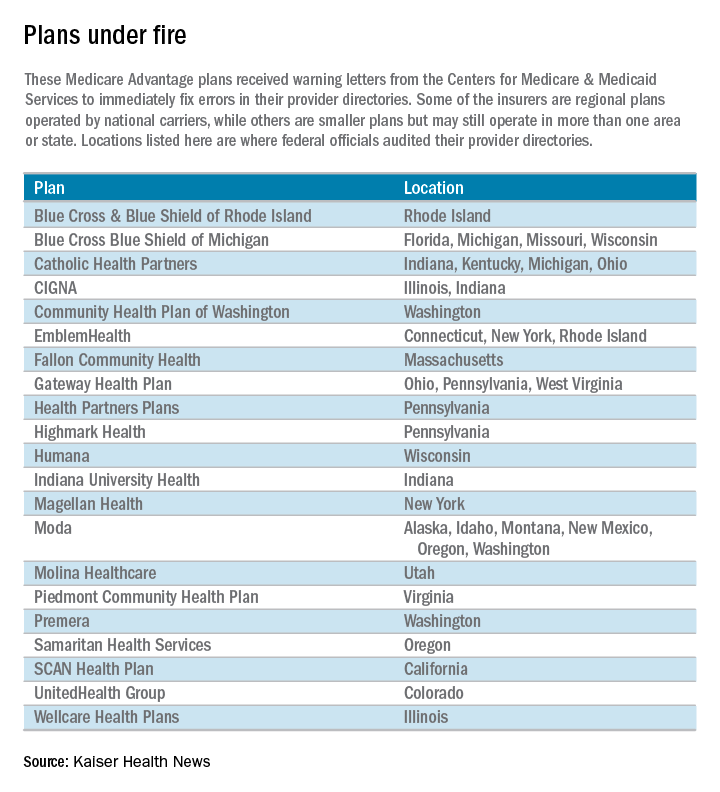
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
Federal officials this month warned 21 Medicare Advantage insurers with high rates of errors in their online network directories that they could face heavy fines or have to stop enrolling people if the problems are not fixed by Feb. 6.
Among the plans that were cited are Blue Cross Blue Shield of Michigan, Highmark of Pennsylvania, SCAN Health Plan of California as well as some regional plans owned by national carriers such as UnitedHealthcare and Humana.
The action follows the government’s first in-depth review of the accuracy of Medicare Advantage provider directories, which consumers and advocates have complained about for years. More than 17 million Americans, or nearly a third of Medicare beneficiaries, get coverage through private Medicare Advantage plans.
The Centers for Medicare & Medicaid Services in October reported some of the results of the audit, but they had not released names or statistics from the individual plans.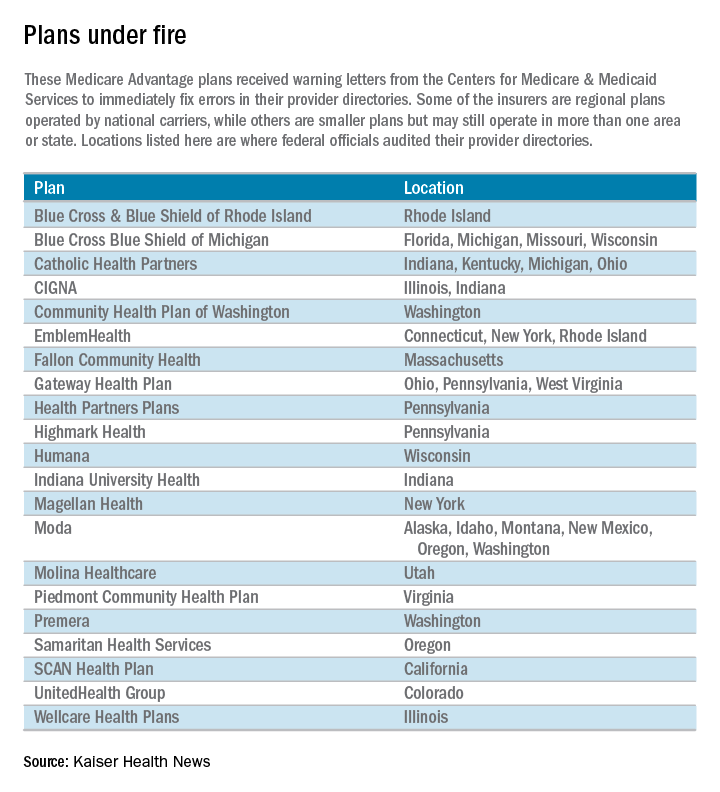
“Because Medicare Advantage members rely on provider directories to locate an in-network provider, these inaccuracies pose a significant access-to-care barrier,” Medicare officials wrote in a report outlining the problems.
Unlike traditional Medicare, the private Medicare plans typically restrict beneficiaries to a network of doctors and hospitals.
Piedmont Community Health Plan, a small Medicare plan with about 5,200 members in southwest Virginia, had the highest rate of inaccuracies among the 54 insurers examined. Officials found errors in the listings of 87 of 108 doctors checked in Piedmont’s directory, according to the report. Most of the errors involved providing the wrong locations for doctors and doctors who should not have been listed. Piedmont officials did not return calls for comment.
Piedmont and two other plans with the highest error rates – a WellCare plan in Illinois and Emblem Health’s ConnectiCare subsidiary – were required by Medicare to submit specific business plans detailing how they intend to address the issue.
The individual plans receiving warning letters cover more than 1.4 million beneficiaries. Most operate in numerous states, although CMS generally limited its review to a specific state or geographic area.
The federal review focused on primary care doctors, cardiologists, ophthalmologists, and oncologists. It involved individual calls to check on the listings for 108 doctors in each health plan. “We encountered several instances where a call to a provider’s office resulted in determining that the provider had been retired or deceased for a long period of time, sometimes years,” the report said.
Almost half of the 5,832 doctors listed had incorrect information, including wrong addresses and wrong phone numbers. Most health plans had inaccurate information for 30%-60% of their providers’ offices, the report said. The report blamed the insurers for failing to do enough to keep their directories accurate.
“We saw a general lack of internal audit and testing of directory accuracy among many” Medicare Advantage organizations, the report said.
CMS’ survey found the most error-prone listings involved doctors with multiple offices that did not serve health plan members at each location.
The health plans were sent the warning letters Jan. 6 and given 30 days to fix the mistakes or face possible fines or sanctions, which could include suspending marketing and enrollment. CMS officials said the report was not issued before the annual open enrollment period – which ended Dec. 7 – because of the need to allow the health plans to review the findings before the report was made public.
Medicare Advantage members have until Feb. 14 to disenroll and join traditional Medicare but after that they are locked into their plan for the rest of the year. Seniors may be able to request permission to change plans on a case-by-case basis by calling 800-MEDICARE.
Another 32 companies with less serious mistakes also received letters saying their directories did not comply with a rule that took effect last year requiring plans to contact doctors and other providers every 3 months and to update their online directories in “real time.”
ConnectiCare spokeswoman Kimberly Kann acknowledged the difficulties. “Keeping these directories up to date is a two-way street and we are working with doctors and other medical professionals to continue providing quality service,” she said.
WellCare spokeswoman Crystal Warwell Walker said the Tampa, Fla.–based company took the survey results seriously. “We modified our data gathering techniques and online reporting options to ensure that when more than one address is listed for a provider, that provider is practicing at that location on a routine basis and access to care is not compromised,” she said.
CMS is continuing its investigation of provider directories this year and expects to examine all 300 companies by end of 2018.
Kaiser Health News is a national health policy news service that is part of the nonpartisan Henry J. Kaiser Family Foundation.
HHS proposes to streamline Medicare appeals process
The Department of Health and Human Services on June 28 proposed key changes in the Medicare appeals process to help reduce the backlog of more than 700,000 cases.
The measures “will help us get a leg up on this problem,” said Nancy Griswold, chief law judge of the Office of Medicare Hearings and Appeals.
If there was not a single additional appeal filed and no changes in the system, it would take 11 years to eliminate the backlog, Ms. Griswold said in an interview.
Her office has faced increased criticism from health care providers and beneficiary advocates for its inability to speed up appeals and reduce the backlog. The latest critique came earlier this month in an investigation from the Government Accountability Office.
This latest effort still falls short of what is needed, said Tom Nickels, executive vice president at the American Hospital Association. “We are deeply disappointed that HHS has not made more progress in addressing the delays despite the more than 2 years since the delays began,” he said.
The new proposals, as well as increased funding requests, are expected to eliminate the backlog by 2021 by streamlining the decision-making process and reducing the number of cases that go to the third level of appeals, where many cases linger waiting for a hearing and then a decision from an administrative law judge. From the day of the hearing, it currently takes an average of slightly more than 2 years for a decision in appeals from hospitals, nursing homes, medical device suppliers and other health care providers.
Among the proposed changes:
• Designate some decisions from the Medicare Appeals Council, the last of four stages of appeals, as precedents that decision-makers at lower levels would have to follow. That could eliminate redundant appeals and resolve inconsistencies in interpretation of Medicare policies.
• Allow senior attorneys to handle some of the procedural matters that come before the administrative law judges, such as dismissing a request for a hearing after the appellant has withdrawn the request, Ms. Griswold said.
• Revise how the minimum amount necessary to lodge an appeal is determined. Under current rules, an appeal must involve payment of at least $150, based on the amount the provider charged. HHS is proposing to use Medicare’s allowed amount instead, which tends to be lower, and that could reduce the number of claims that could be appealed.
• Eliminate some steps in the appeals process to simplify the system.
Although advocates have sought changes to speed up the appeal process, Alice Bers, an attorney at the Center for Medicare Advocacy, said she was skeptical about some of the proposals. The effort to set up a system of precedents “could restrict coverage for needed items and benefits for seniors that they are entitled to by law.”
And the change in calculating the minimal amounts “could make it harder for beneficiaries to reach that threshold,” said Ms. Bers. It might not sound like a lot of money, Ms. Bers said, “but for an elderly woman living on Social Security that’s several meals or copays for medicine.”
The proposals do not address what hospital representatives say is a key cause of increasing appeals, independent audit contractors who can reject payments to hospitals. The American Hospital Association contends that those contractors unnecessarily cut off many payments and that hospitals frequently win the appeals.
According to the GAO study, audit-related appeals decided at the administrative law judge stage – the third level of appeals – increased 37-fold from 2010 through 2014, compared to only 1.5 times for appeals of other kinds of claims.
But Ms. Griswold said that currently only about a third of the pending cases at this stage involved recovery audit contractors, after settlements were reached with appellants who agreed to accept partial payment. As a result of these agreements, 4,245 cases from just 16 appellants were withdrawn from the system as of May 12, according to government statistics.
Ms. Griswold also said Medicare will continue to process beneficiary appeals before those from hospitals, doctors, and other health care providers. The practice began in 2014.
The proposed changes will be posted on the Federal Register website and open to comments through Aug. 29.
This story appears courtesy of Kaiser Health News (KHN). KHN’s coverage of aging and long-term care issues is supported in part by a grant from The SCAN Foundation.
The Department of Health and Human Services on June 28 proposed key changes in the Medicare appeals process to help reduce the backlog of more than 700,000 cases.
The measures “will help us get a leg up on this problem,” said Nancy Griswold, chief law judge of the Office of Medicare Hearings and Appeals.
If there was not a single additional appeal filed and no changes in the system, it would take 11 years to eliminate the backlog, Ms. Griswold said in an interview.
Her office has faced increased criticism from health care providers and beneficiary advocates for its inability to speed up appeals and reduce the backlog. The latest critique came earlier this month in an investigation from the Government Accountability Office.
This latest effort still falls short of what is needed, said Tom Nickels, executive vice president at the American Hospital Association. “We are deeply disappointed that HHS has not made more progress in addressing the delays despite the more than 2 years since the delays began,” he said.
The new proposals, as well as increased funding requests, are expected to eliminate the backlog by 2021 by streamlining the decision-making process and reducing the number of cases that go to the third level of appeals, where many cases linger waiting for a hearing and then a decision from an administrative law judge. From the day of the hearing, it currently takes an average of slightly more than 2 years for a decision in appeals from hospitals, nursing homes, medical device suppliers and other health care providers.
Among the proposed changes:
• Designate some decisions from the Medicare Appeals Council, the last of four stages of appeals, as precedents that decision-makers at lower levels would have to follow. That could eliminate redundant appeals and resolve inconsistencies in interpretation of Medicare policies.
• Allow senior attorneys to handle some of the procedural matters that come before the administrative law judges, such as dismissing a request for a hearing after the appellant has withdrawn the request, Ms. Griswold said.
• Revise how the minimum amount necessary to lodge an appeal is determined. Under current rules, an appeal must involve payment of at least $150, based on the amount the provider charged. HHS is proposing to use Medicare’s allowed amount instead, which tends to be lower, and that could reduce the number of claims that could be appealed.
• Eliminate some steps in the appeals process to simplify the system.
Although advocates have sought changes to speed up the appeal process, Alice Bers, an attorney at the Center for Medicare Advocacy, said she was skeptical about some of the proposals. The effort to set up a system of precedents “could restrict coverage for needed items and benefits for seniors that they are entitled to by law.”
And the change in calculating the minimal amounts “could make it harder for beneficiaries to reach that threshold,” said Ms. Bers. It might not sound like a lot of money, Ms. Bers said, “but for an elderly woman living on Social Security that’s several meals or copays for medicine.”
The proposals do not address what hospital representatives say is a key cause of increasing appeals, independent audit contractors who can reject payments to hospitals. The American Hospital Association contends that those contractors unnecessarily cut off many payments and that hospitals frequently win the appeals.
According to the GAO study, audit-related appeals decided at the administrative law judge stage – the third level of appeals – increased 37-fold from 2010 through 2014, compared to only 1.5 times for appeals of other kinds of claims.
But Ms. Griswold said that currently only about a third of the pending cases at this stage involved recovery audit contractors, after settlements were reached with appellants who agreed to accept partial payment. As a result of these agreements, 4,245 cases from just 16 appellants were withdrawn from the system as of May 12, according to government statistics.
Ms. Griswold also said Medicare will continue to process beneficiary appeals before those from hospitals, doctors, and other health care providers. The practice began in 2014.
The proposed changes will be posted on the Federal Register website and open to comments through Aug. 29.
This story appears courtesy of Kaiser Health News (KHN). KHN’s coverage of aging and long-term care issues is supported in part by a grant from The SCAN Foundation.
The Department of Health and Human Services on June 28 proposed key changes in the Medicare appeals process to help reduce the backlog of more than 700,000 cases.
The measures “will help us get a leg up on this problem,” said Nancy Griswold, chief law judge of the Office of Medicare Hearings and Appeals.
If there was not a single additional appeal filed and no changes in the system, it would take 11 years to eliminate the backlog, Ms. Griswold said in an interview.
Her office has faced increased criticism from health care providers and beneficiary advocates for its inability to speed up appeals and reduce the backlog. The latest critique came earlier this month in an investigation from the Government Accountability Office.
This latest effort still falls short of what is needed, said Tom Nickels, executive vice president at the American Hospital Association. “We are deeply disappointed that HHS has not made more progress in addressing the delays despite the more than 2 years since the delays began,” he said.
The new proposals, as well as increased funding requests, are expected to eliminate the backlog by 2021 by streamlining the decision-making process and reducing the number of cases that go to the third level of appeals, where many cases linger waiting for a hearing and then a decision from an administrative law judge. From the day of the hearing, it currently takes an average of slightly more than 2 years for a decision in appeals from hospitals, nursing homes, medical device suppliers and other health care providers.
Among the proposed changes:
• Designate some decisions from the Medicare Appeals Council, the last of four stages of appeals, as precedents that decision-makers at lower levels would have to follow. That could eliminate redundant appeals and resolve inconsistencies in interpretation of Medicare policies.
• Allow senior attorneys to handle some of the procedural matters that come before the administrative law judges, such as dismissing a request for a hearing after the appellant has withdrawn the request, Ms. Griswold said.
• Revise how the minimum amount necessary to lodge an appeal is determined. Under current rules, an appeal must involve payment of at least $150, based on the amount the provider charged. HHS is proposing to use Medicare’s allowed amount instead, which tends to be lower, and that could reduce the number of claims that could be appealed.
• Eliminate some steps in the appeals process to simplify the system.
Although advocates have sought changes to speed up the appeal process, Alice Bers, an attorney at the Center for Medicare Advocacy, said she was skeptical about some of the proposals. The effort to set up a system of precedents “could restrict coverage for needed items and benefits for seniors that they are entitled to by law.”
And the change in calculating the minimal amounts “could make it harder for beneficiaries to reach that threshold,” said Ms. Bers. It might not sound like a lot of money, Ms. Bers said, “but for an elderly woman living on Social Security that’s several meals or copays for medicine.”
The proposals do not address what hospital representatives say is a key cause of increasing appeals, independent audit contractors who can reject payments to hospitals. The American Hospital Association contends that those contractors unnecessarily cut off many payments and that hospitals frequently win the appeals.
According to the GAO study, audit-related appeals decided at the administrative law judge stage – the third level of appeals – increased 37-fold from 2010 through 2014, compared to only 1.5 times for appeals of other kinds of claims.
But Ms. Griswold said that currently only about a third of the pending cases at this stage involved recovery audit contractors, after settlements were reached with appellants who agreed to accept partial payment. As a result of these agreements, 4,245 cases from just 16 appellants were withdrawn from the system as of May 12, according to government statistics.
Ms. Griswold also said Medicare will continue to process beneficiary appeals before those from hospitals, doctors, and other health care providers. The practice began in 2014.
The proposed changes will be posted on the Federal Register website and open to comments through Aug. 29.
This story appears courtesy of Kaiser Health News (KHN). KHN’s coverage of aging and long-term care issues is supported in part by a grant from The SCAN Foundation.